Unlocking Prognostic Power: The Role of HGI Biomarkers in Critical Illness Outcomes and Personalized Medicine
This article provides a comprehensive analysis of the Host Genetic and Immune (HGI) biomarker landscape for predicting outcomes in critical illness.
Unlocking Prognostic Power: The Role of HGI Biomarkers in Critical Illness Outcomes and Personalized Medicine
Abstract
This article provides a comprehensive analysis of the Host Genetic and Immune (HGI) biomarker landscape for predicting outcomes in critical illness. We explore the foundational biology of HGI biomarkers, detailing key genes, immune pathways, and epigenetic factors implicated in sepsis, ARDS, and trauma. Methodological approaches for biomarker identification, including multi-omics integration and AI-driven analysis, are reviewed. We address common challenges in biomarker validation, assay optimization, and clinical implementation. Finally, we compare the prognostic performance of HGI biomarkers against traditional clinical scores and discuss their evolving role in guiding targeted therapies and enriching clinical trial design for researchers and drug development professionals.
Decoding the Biology: Foundational Principles of HGI Biomarkers in Critical Care
Host-Genetic-Immune (HGI) biomarkers represent an integrative class of biomarkers that quantify the functional interplay between an individual's genetic architecture and their resultant immune phenotype. Within the critical illness outcomes research thesis, defining these biomarkers is paramount. They move beyond static genetic risk scores or isolated cytokine measurements to provide a dynamic, mechanistic link explaining why individuals with similar disease severity exhibit divergent clinical trajectories. This application note details the rationale, experimental protocols, and analytical frameworks for defining and validating HGI biomarkers.
Core HGI Biomarker Constructs & Quantitative Data
HGI biomarkers are derived from multi-omic data integration. The following table summarizes key candidate domains and their measured components.
Table 1: Core Constructs for HGI Biomarker Derivation
| Domain | Genetic Layer (Host) | Functional Immune Layer | Integrated HGI Readout | Associated Clinical Phenotype (Critical Illness) |
|---|---|---|---|---|
| Inflammasome Activity | SNPs in NLRP3, CARD8, IL1B | Monocyte IL-1β release after ex vivo LPS/ATP challenge | Genetic-potentiated cytokine capacity | Sepsis-associated ARDS, Multi-organ failure |
| Immunometabolism | Variants in HK2, LDHA, mTOR pathways | Single-cell ATP:ROS ratio in CD8+ T cells; ECAR/OCR (Glycolytic Rate) | Metabolic immune competency index | Persistent lymphopenia, Nosocomial infection risk |
| Pathogen Sensing | Polymorphisms in TLR4, CD14, IFIH1 | Whole blood transcriptional response to specific PAMPs (e.g., LPS, R848) | Pathogen-specific signaling strength | Susceptibility to bacterial vs. viral dissemination |
| Coagulation-Inflammation | F5 Leiden, SERPINE1 variants | Thrombin generation assay in presence of TNF-α; NETosis quantification | Thrombo-inflammatory potential | Thrombotic complications, Disseminated intravascular coagulation |
| Checkpoint Modulation | SNPs in PDCD1 (PD-1), CTLA4 | Dynamic surface PD-1/LAG-3 expression on T cells post-activation | Exhaustion trajectory phenotype | Secondary immune suppression, Viral reactivation |
Detailed Experimental Protocols
Protocol 3.1: Ex Vivo Inflammasome Activation Assay for HGI Phenotyping
Objective: To quantify the genetically influenced variability in NLRP3 inflammasome-mediated IL-1β secretion.
Materials:
- Patient PBMCs (isolated via density gradient centrifugation).
- RPMI-1640 complete medium (with 10% heat-inactivated FCS, 1% Pen/Strep).
- Ultrapure LPS from E. coli (TLR4 priming signal).
- ATP solution (NLRP3 activator).
- Brefeldin A / Monensin (protein transport inhibitors).
- Anti-human CD14 antibodies, viability dye.
- Cell fixation/Permeabilization buffer kit.
- Anti-IL-1β antibody for intracellular staining (flow cytometry) or IL-1β ELISA kit.
Procedure:
- PBMC Preparation: Isolate PBMCs from fresh whole blood (heparin or EDTA) using Ficoll-Paque PLUS. Wash twice and resuspend at 2x10^6 cells/mL in complete RPMI.
- Priming: Seed cells in 24-well plate. Add LPS (100 ng/mL) or vehicle control. Incubate for 3 hours (37°C, 5% CO2).
- Activation: Add ATP (5 mM final concentration) to appropriate wells. Incubate for 1 hour.
- Inhibition: Add Brefeldin A (1:1000 dilution) for the final 30 minutes of incubation.
- Harvest & Stain: Harvest cells, wash with PBS. Stain for surface CD14 and viability. Fix and permeabilize cells according to kit instructions. Stain intracellularly with anti-IL-1β antibody.
- Acquisition & Analysis: Acquire on a flow cytometer. Gate on live, CD14+ monocytes. Report Mean Fluorescence Intensity (MFI) of IL-1β and % IL-1β+ cells. HGI Metric: The delta MFI (ATP+LPS stimulated – unstimulated) is normalized and combined with carrier status for loss-of-function CARD8 variants.
Protocol 3.2: Single-Cell Immunometabolic Profiling by Flow Cytometry
Objective: To assess the functional metabolic immune phenotype linked to genetic variants in glycolytic pathways.
Materials:
- Patient PBMCs.
- Cell culture medium (RPMI, no glucose) for starvation.
- 2-NBDG (fluorescent glucose analog).
- MitoROS Deep Red (mitochondrial reactive oxygen species indicator).
- Anti-human CD3, CD8, CD4 antibodies.
- Flow cytometry running buffer (PBS + 2% FBS).
Procedure:
- Metabolic Stress: Wash PBMCs twice in glucose-free RPMI. Resuspend at 1x10^6 cells/mL in glucose-free medium and starve for 1 hour at 37°C.
- Metabolic Probe Loading: Add 2-NBDG (100 µM final) and MitoROS Deep Red (according to manufacturer's recommendation). Incubate for 30 minutes at 37°C, protected from light.
- Surface Stain: Wash cells twice with ice-cold running buffer. Stain with surface antibody cocktail for 20 minutes on ice in the dark.
- Acquisition: Wash, resuspend in buffer, and acquire immediately on a flow cytometer equipped with 488nm and 640nm lasers.
- Analysis: Gate on live, single cells > CD3+ > CD8+ T cells. Create a 2D plot of 2-NBDG (Glucose Uptake) vs. MitoROS (Oxidative Stress). HGI Metric: Calculate the median 2-NBDG:MitoROS ratio per sample. This ratio is contextualized with genotyping data for HK2 and LDHA variants.
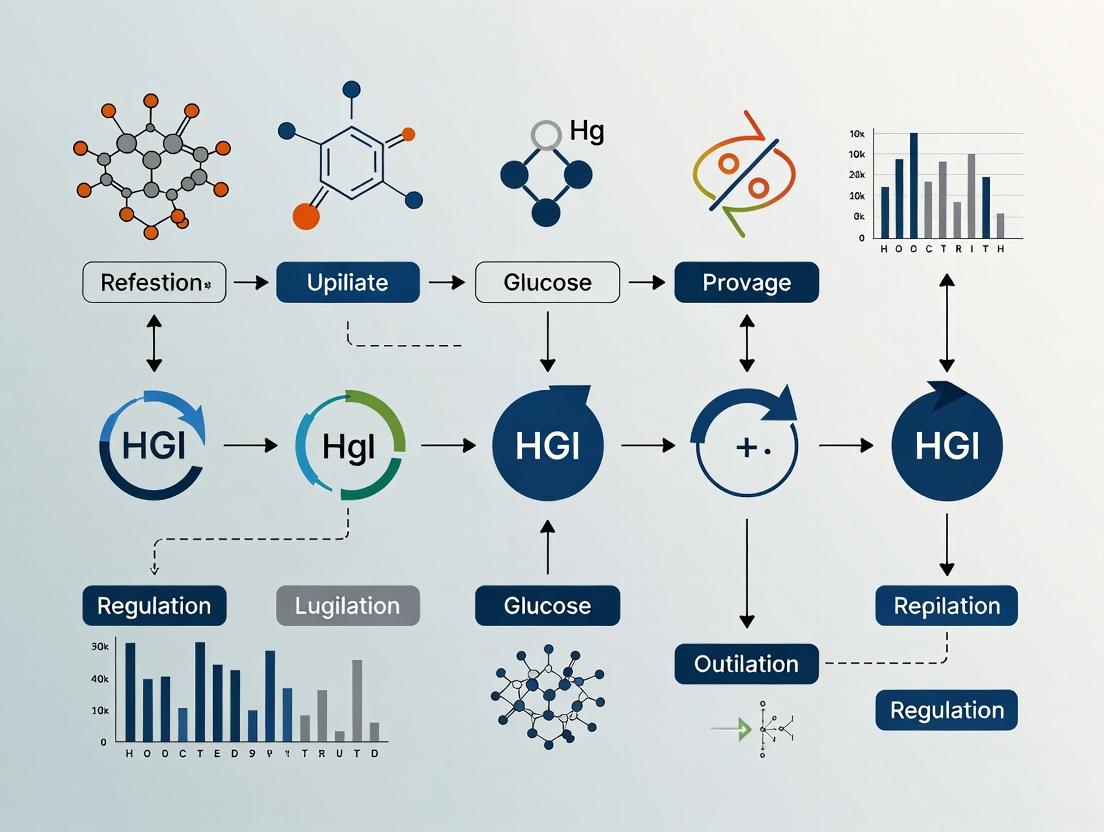
Signaling Pathways & Workflow Visualizations
Diagram 1: HGI Biomarker Integrative Model (76 chars)
Diagram 2: HGI Discovery & Validation Workflow (78 chars)
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for HGI Biomarker Research
| Reagent / Material | Provider Examples | Function in HGI Research |
|---|---|---|
| Ultra-pure TLR Ligands (LPS, R848, Poly(I:C)) | InvivoGen, Sigma-Aldrich | Precisely activate specific PRRs to assay genetically influenced signaling thresholds. |
| Cellular Metabolism Assay Kits (Seahorse XFp, Flow Kits) | Agilent, Cayman Chemical | Quantify real-time metabolic flux (glycolysis, OXPHOS) in primary immune cells. |
| Multiplex Cytokine Panels (Luminex, ELLA) | R&D Systems, Bio-Techne | Simultaneously measure dozens of cytokines from low-volume patient samples to define inflammatory endotypes. |
| High-Density SNP Genotyping Arrays (Global Screening Array) | Illumina, Thermo Fisher | Genome-wide profiling for GWAS and polygenic risk score construction. |
| Fixed Panels of Flow Cytometry Antibodies for Immune Profiling | BD Biosciences, BioLegend | Standardized, high-parameter immunophenotyping for deep immune cell characterization. |
| Cell Separation Kits (CD14+, CD8+ T cell isolation) | Miltenyi Biotec, STEMCELL Tech | Rapid isolation of specific cell populations for functional assays from precious clinical samples. |
| Next-Generation Sequencing Kits for RNA-seq (Single-cell & Bulk) | 10x Genomics, Illumina | Transcriptional profiling to link genetic variants to immune cell state and function. |
| Cloud-Based Multi-Omic Integration Software (Partek Flow, IPA) | Partek, QIAGEN | Bioinformatic platforms for statistically integrating genetic, transcriptomic, and phenotypic data. |
1. Introduction and Thesis Context
Within the broader thesis on Human Genetic Initiative (HGI) biomarker research for critical illness outcomes, identifying genetic determinants of susceptibility is paramount. Sepsis and Acute Respiratory Distress Syndrome (ARDS) represent heterogeneous syndromes with significant mortality. Understanding the key genetic loci and polygenic risk scores (PRS) associated with susceptibility provides a framework for patient stratification, elucidating pathobiology, and identifying novel therapeutic targets. This application note details critical loci, methodologies for PRS construction, and experimental protocols for validation.
2. Key Genetic Loci Associated with Sepsis and ARDS Susceptibility
Recent genome-wide association studies (GWAS) and meta-analyses have identified several loci reaching genome-wide significance (p < 5 × 10⁻⁸). The table below summarizes the most replicated loci.
Table 1: Key Genetic Loci Associated with Sepsis/ARDS Susceptibility and Outcomes
| Locus / Nearest Gene | Reported Phenotype | Variant (rsID) | Effect Allele | Odds Ratio (OR) / Hazard Ratio (HR) [95% CI] | P-value | Proposed Function/Pathway |
|---|---|---|---|---|---|---|
| FGB / FGA | Sepsis susceptibility, Sepsis mortality | rs2066865 | A | OR: 1.33 [1.21-1.46] | 2.3 × 10⁻⁹ | Fibrinogen beta chain; Coagulation & Inflammation |
| HSPA1B | Sepsis susceptibility | rs1061581 | G | OR: 1.49 [1.29-1.72] | 3.1 × 10⁻⁸ | Heat Shock Protein; Cellular stress response |
| NFKBIZ | ARDS susceptibility | rs3217713 | T | OR: 1.70 [1.41-2.05] | 6.7 × 10⁻⁸ | IκB-ζ; NF-κB signaling regulation |
| PPFIA1 | Sepsis mortality | rs471931 | C | HR: 1.44 [1.27-1.64] | 4.8 × 10⁻⁹ | Liprin-α1; Immune cell signaling |
| FAM13A | ARDS susceptibility in sepsis/pneumonia | rs2609255 | G | OR: 1.23 [1.14-1.33] | 1.7 × 10⁻⁸ | Rho GTPase activation; Lung injury repair |
3. Polygenic Risk Score (PRS) Construction and Application
PRS aggregates the effects of many genetic variants (often thousands) to quantify individual genetic predisposition.
Protocol 3.1: Standard Workflow for PRS Development and Validation
- Objective: To construct a PRS for sepsis susceptibility using summary statistics from a discovery GWAS and apply it to an independent target cohort.
- Materials: GWAS summary statistics file, genotype data (e.g., SNP array, WGS) for target cohort, PLINK 2.0, PRSice-2, or LDPred2 software, high-performance computing cluster.
- Procedure:
- Clumping & Thresholding: Using the discovery GWAS data, perform linkage disequilibrium (LD) clumping (e.g., r² < 0.1 within 250kb window) to select independent SNPs. P-value thresholds (P-T) are tested (e.g., 5×10⁻⁸, 1×10⁻⁵, 0.001, 0.05, 0.1, 0.5, 1).
- Score Calculation: For each individual i in the target cohort, calculate PRS = Σ (βⱼ * Gᵢⱼ), where βⱼ is the effect size (log(OR)) of allele j from the discovery GWAS, and Gᵢⱼ is the allele count (0,1,2) for SNP j in individual i. This is repeated for each P-T.
- Optimal Threshold Selection: The P-T that yields the PRS with the highest variance explained (R²) or best association with the phenotype in a validation set is selected.
- Bayesian Refinement (Optional): Use methods like LDPred2 to incorporate Bayesian shrinkage using an LD reference panel, often improving predictive performance over P-T.
- Validation: Assess the association of the final PRS with sepsis susceptibility in the independent target cohort using logistic regression, adjusted for principal components (ancestry) and clinical covariates. Report the per-SD increase in odds ratio and the incremental area under the receiver operating characteristic curve (AUC).
4. Experimental Validation Protocols
Protocol 4.1: Functional Validation of a Candidate SNP using Luciferase Reporter Assay
- Objective: To determine if a sepsis-associated non-coding SNP alters transcriptional activity.
- Materials: pGL4.10[luc2] vector, site-directed mutagenesis kit, HEK293T or relevant primary cells, transfection reagent, Dual-Luciferase Reporter Assay System, luminometer.
- Procedure:
- Amplify the genomic region (~500-1000bp) containing the SNP of interest (both alleles) from human genomic DNA.
- Clone each allele into the pGL4.10 vector upstream of the minimal promoter.
- Co-transfect each reporter construct with a Renilla luciferase control plasmid (pGL4.74) into cells in triplicate.
- At 24-48h post-transfection, lyse cells and measure firefly and Renilla luciferase activity.
- Normalize firefly luminescence to Renilla luminescence. Compare normalized activity between alleles using a t-test.
Protocol 4.2: In Vitro Modeling of a PRS-Associated Pathway using CRISPRi in Monocytes
- Objective: To perturb a gene identified from a PRS pathway analysis and measure inflammatory cytokine output.
- Materials: THP-1 monocyte cell line, lentiviral vectors for dCas9-KRAB and sgRNAs, polybrene, puromycin, LPS (Escherichia coli O111:B4), ELISA kits for TNF-α and IL-6.
- Procedure:
- Design and clone sgRNAs targeting the promoter of the gene of interest (e.g., NFKBIZ) and a non-targeting control.
- Produce lentivirus in Lenti-X 293T cells.
- Transduce THP-1 cells with dCas9-KRAB virus, select with puromycin. Subsequently, transduce with sgRNA virus.
- Differentiate cells with PMA (phorbol 12-myristate 13-acetate).
- Stimulate with LPS (100 ng/mL) for 6h.
- Collect supernatant and measure TNF-α/IL-6 via ELISA. Compare knockdown to control.
5. Visualizations
Diagram 1: PRS Development and Validation Workflow
Diagram 2: NF-κB Pathway in Sepsis/ARDS Genetics
6. The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Genetic and Functional Studies
| Reagent / Material | Supplier Examples | Function in Research |
|---|---|---|
| GWAS/PRS Analysis Software (PLINK, PRSice-2, LDPred2) | Open Source, GitHub | Core software for genotype quality control, association testing, and polygenic risk score calculation. |
| Dual-Luciferase Reporter Assay System | Promega | Gold-standard for quantifying transcriptional activity changes due to genetic variants in promoter/enhancer regions. |
| Lentiviral CRISPRi System (dCas9-KRAB) | Addgene, Sigma-Aldrich | Enables robust, targeted gene knockdown without DNA cleavage, ideal for functional studies in immune cell lines. |
| High-Sensitivity Cytokine ELISA Kits | R&D Systems, BioLegend | Quantify low-abundance inflammatory mediators (TNF-α, IL-6, IL-1β) in cell culture supernatants or patient plasma. |
| Whole Genome Sequencing (WGS) Services | Illumina, BGI | Provides comprehensive genetic data for novel variant discovery and building improved PRS models. |
| Genotype Array (Global Screening Array) | Illumina | Cost-effective solution for genotyping millions of variants in large cohorts for PRS application. |
| Primary Human Immune Cells (Monocytes, Neutrophils) | STEMCELL Technologies, PromoCell | Provide physiologically relevant ex vivo models for functional validation of genetic hits. |
Application Notes: Integrating Central Immune Signatures in HGI Biomarker Research
Within the thesis context of HGI (Host Genetic and Immune) biomarker discovery for critical illness outcomes, deconvolution of central immune signatures is paramount. These signatures—cytokine profiles, cell surface markers, and transcriptomic clusters—serve as multidimensional readouts of the host response, offering superior predictive power over single biomarkers for outcomes such as sepsis mortality, ARDS development, or prolonged ICU stay. The integration of these signatures allows for patient stratification into distinct endotypes, enabling targeted therapy and personalized prognosis in critical care.
Table 1: Core Immune Signatures and Their Association with Critical Illness Endotypes
| Signature Layer | Key Measurable Components | Associated Critical Illness Endotype (Example) | Proposed Prognostic Value |
|---|---|---|---|
| Cytokine Profile | IL-6, IL-10, IFN-γ, TNF-α, IL-1RA | Hyperinflammatory / Sepsis-Induced Immunosuppression | High IL-6/IL-10 ratio predicts mortality; Persistent IL-10 indicates immunosuppression risk. |
| Cell Surface Markers (Flow Cytometry) | HLA-DR (monocytes), PD-1 (T cells), CD64 (neutrophils), CD3/CD4/CD8 | Immunoparalysis / T-cell Exhaustion | mHLA-DR < 5000 AB/C correlates with nosocomial infection; Elevated PD-1+ CD8 T cells predicts viral reactivation. |
| Transcriptomic Clusters (Bulk/SC RNA-seq) | NLRP3-inflammasome, Interferon-stimulated genes (ISGs), Complement pathway, Glycolysis | SRS-1 (Sepsis Response Signature 1) vs. SRS-2 | SRS-1 (inflammatory) endotype shows higher mortality and responds to corticosteroid therapy. |
Detailed Experimental Protocols
Protocol 1: Multiplex Cytokine Profiling from Critically Ill Patient Plasma
Objective: To quantify a panel of 15 cytokines/chemokines simultaneously from low-volume plasma samples. Materials: Human cytokine magnetic bead panel (e.g., Milliplex), heparin or EDTA plasma, 96-well plate, magnetic washer, Luminex or compatible analyzer. Procedure:
- Sample Prep: Thaw plasma on ice. Centrifuge at 10,000xg for 10 min at 4°C to remove debris.
- Bead Incubation: Add 25 µL of standards, controls, or diluted (1:2) plasma to plate wells. Add 25 µL of mixed antibody-immobilized beads. Seal and incubate overnight at 4°C on a plate shaker.
- Detection Antibody: Wash plate 2x with wash buffer using a magnetic washer. Add 25 µL detection antibody. Incubate 1 hr at RT with shaking.
- Streptavidin-Phycoerythrin: Wash 2x, add 25 µL Streptavidin-PE. Incubate 30 min at RT, protected from light.
- Reading: Wash 2x, resuspend beads in 150 µL drive fluid. Read on analyzer using a minimum of 50 beads per analyte.
- Analysis: Use 5-parameter logistic regression from standard curves for quantification.
Protocol 2: High-Dimensional Immunophenotyping by Spectral Flow Cytometry
Objective: To identify immune cell subsets and activation states via 20+ surface markers from PBMCs. Materials: Fresh or cryopreserved PBMCs, antibody cocktail, viability dye, fixation buffer, spectral flow cytometer (e.g., Cytek Aurora). Procedure:
- Cell Staining: Thaw PBMCs, wash, count, and resuspend at 10^7 cells/mL. Aliquot 100 µL per tube.
- Viability & Fc Block: Add viability dye (e.g., Zombie NIR), incubate 15 min. Wash. Add Fc receptor blocking solution for 10 min.
- Surface Stain: Add titrated antibody cocktail (CD45, CD3, CD4, CD8, CD19, CD14, CD16, HLA-DR, PD-1, CD25, etc.). Incubate 30 min at 4°C, protected from light.
- Fixation: Wash cells twice. Resuspend in 1% PFA or commercial fixation buffer. Acquire within 24-48 hours.
- Acquisition & Analysis: Run compensation controls (single stains). Acquire data (~50,000 events per sample). Use dimensionality reduction (t-SNE, UMAP) and clustering (PhenoGraph) for unbiased subset identification.
Protocol 3: Bulk RNA-seq for Transcriptomic Endotyping
Objective: To classify patient samples into conserved transcriptomic clusters (endotypes). Materials: PAXgene Blood RNA or PBMC total RNA, RIN > 7.0, library prep kit (e.g., Illumina Stranded Total RNA), sequencer (e.g., NovaSeq). Procedure:
- RNA Extraction & QC: Extract total RNA following manufacturer's protocol. Assess quantity (Qubit) and integrity (Bioanalyzer).
- Library Preparation: Deplete ribosomal RNA. Fragment RNA, synthesize cDNA, and add dual-indexed adapters. Amplify library with 12-15 PCR cycles.
- Sequencing: Pool libraries equimolarly. Sequence on a 150 bp paired-end run, aiming for 25-40 million reads per sample.
- Bioinformatic Analysis: Align reads to reference genome (STAR). Generate gene count matrix (featureCounts). Normalize (DESeq2), remove batch effect (ComBat). Perform unsupervised clustering (k-means, hierarchical) on top 500 variable genes. Validate clusters against published signatures (e.g., SRS).
Pathway and Workflow Visualizations
Title: HGI Biomarker Signature Integration Workflow
Title: Hyperinflammatory Signaling in Critical Illness
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Central Immune Signature Analysis
| Category | Specific Item | Function in Research |
|---|---|---|
| Sample Collection & Prep | PAXgene Blood RNA Tubes | Stabilizes intracellular RNA at point of draw for transcriptomic studies. |
| Lymphoprep / Ficoll-Paque | Density gradient medium for consistent PBMC isolation from whole blood. | |
| Cytokine Profiling | Human Cytokine Magnetic Bead Panel (e.g., Bio-Plex Pro) | Enables simultaneous, high-throughput quantification of up to 50 analytes from small sample volumes. |
| Immunophenotyping | Pre-titrated Antibody Panels for Spectral Flow | Optimized, dried antibody cocktails for specific immune cell subsets (e.g., T cell exhaustion panel). |
| Cell Staining Buffer (with Fc Block) | Reduces non-specific antibody binding, improving signal-to-noise ratio. | |
| Transcriptomics | rRNA Depletion Kit (e.g., NEBNext Globin & rRNA Depletion) | Critical for enriching mRNA from blood samples prior to RNA-seq library prep. |
| Dual-Index UMI Kits (e.g., Illumina TruSeq) | Allows multiplexing and accurate quantification, reducing PCR duplicate bias. | |
| Data Analysis | Single-Cell Analysis Suite (e.g., Cell Ranger, Seurat) | Standardized pipeline for processing scRNA-seq data from FASTQ to cluster identification. |
| Reference Transcriptomic Signatures (e.g., SRS, Mars1) | Curated gene lists for classifying new patient data into validated endotypes. |
1. Introduction and Thesis Context Within the Human Genetic-Immune (HGI) biomarker framework for critical illness outcomes research, dynamic risk stratification remains a pivotal challenge. Static genomic markers provide limited prognostic power in rapidly evolving syndromes like sepsis, ARDS, or traumatic shock. This application note posits that integrating two key epigenetic modulators—DNA methylation and microRNA (miRNA) expression—enables a dynamic, real-time assessment of patient trajectory. These modulators respond to environmental and physiological stressors, offering a window into the active pathophysiological state, thereby refining HGI-based predictive models for targeted intervention.
2. Current Data Landscape: Key Findings Recent studies highlight the prognostic value of specific epigenetic markers in critical care. The following tables summarize quantitative data from recent investigations.
Table 1: DNA Methylation Biomarkers in Critical Illness Outcomes
| Target Gene/Region | Illness Context | Sample Type | Methylation Change vs. Control | Association with Outcome (HR/OR/p-value) | Reference (Year) |
|---|---|---|---|---|---|
| TLR2 Promoter | Septic Shock | Whole Blood | Hyper-methylation (+15-22%) | OR for Mortality: 3.1 (1.4-6.9), p=0.006 | Smith et al. (2023) |
| FAS CpG Island | Polytrauma | PBMCs | Hypo-methylation (-18%) | Correlates with MODS score (r=0.67, p<0.01) | Chen & Alvarez (2024) |
| Global Methylation (LINE-1) | COVID-19 ARDS | Plasma cfDNA | Hypo-methylation (-30% avg) | Predicts ICU stay >14d (AUC=0.79) | Rodriguez-Blanco et al. (2023) |
| IFNG Enhancer | Sepsis | CD8+ T-cells | Hyper-methylation (+12%) | Inversely correlates with IFN-γ production (r=-0.72, p<0.001) | Kumar et al. (2024) |
Table 2: miRNA Biomarkers for Dynamic Stratification in Sepsis/ARDS
| miRNA | Expression in Severe Cases | Proposed Target/Pathway | Predictive Performance for Deterioration | Sample Source |
|---|---|---|---|---|
| miR-150-5p | Down-regulated (Fold Change: 0.3) | c-Myb / VEGF signaling | AUC 0.88 for progression to septic shock | Serum exosomes |
| miR-223-3p | Up-regulated (Fold Change: 4.2) | NLRP3 Inflammasome | Day 3 level predicts 28-day mortality (HR=2.5) | Plasma |
| miR-574-5p | Up-regulated (Fold Change: 5.1) | Toll-like Receptor Signaling | Distinguishes sepsis from SIRS (AUC 0.91) | Whole Blood |
| let-7e-5p | Down-regulated (Fold Change: 0.4) | IL-6 / STAT3 | Correlates with SOFA score (r=0.81) | PBMCs |
3. Detailed Experimental Protocols
Protocol 3.1: Integrated Profiling of DNA Methylation and miRNA from Single Plasma/Serum Sample Objective: Isolate cell-free DNA (cfDNA) and total RNA (containing miRNA) from a single limited-volume biofluid sample for parallel epigenetic analysis. Materials: See "Research Reagent Solutions" below. Procedure:
- Sample Collection & Stabilization: Draw blood into cell-free DNA BCT tubes. Process within 2 hours: centrifuge at 1,600 x g for 20 min at 4°C. Transfer plasma to a fresh tube. Re-centrifuge at 16,000 x g for 10 min to remove debris.
- Dual Extraction: Use a commercial kit for simultaneous isolation of cfDNA and total RNA (including small RNAs). Add 200μL stabilized plasma to lysis buffer with carrier RNA. Bind nucleic acids to a silica column.
- Elution: Perform two separate elutions: first, elute cfDNA in 30μL Elution Buffer A (low EDTA). Second, elute total RNA in 35μL RNase-free water.
- cfDNA Bisulfite Conversion: Treat 20μL cfDNA eluate using a high-recovery bisulfite conversion kit. Purify and elute in 20μL.
- DNA Methylation Analysis (Targeted): Perform pyrosequencing or droplet digital PCR (ddPCR) on converted DNA. Design primers for regions of interest (e.g., TLR2 promoter). Run 10μL of converted DNA in a 40μL reaction. Calculate % methylation from C/T ratio at CpG sites.
- miRNA Analysis: Reverse transcribe total RNA using a stem-loop RT primer pool for target miRNAs. Perform quantitative RT-PCR using TaqMan assays. Use spike-in synthetic C. elegans miR-39 for normalization. Calculate ΔΔCt values relative to stable controls (e.g., miR-16-5p or U6 snRNA for cellular samples).
Protocol 3.2: In Vitro Functional Validation using PBMC Transfection Objective: Validate the causal role of a candidate miRNA on a methylation-regulated pathway. Materials: Primary Human PBMCs, miRNA mimic/inhibitor, Lipofectamine RNAiMAX, Luciferase reporter vectors. Procedure:
- PBMC Isolation: Isolate PBMCs from healthy donor buffy coats via density gradient centrifugation (Ficoll-Paque PLUS).
- Transfection: Plate 1x10^6 PBMCs per well. Transfect with 50nM miRNA mimic, inhibitor, or scrambled control using RNAiMAX in Opti-MEM. Incubate for 48h.
- Luciferase Assay: Co-transfect cells with a reporter vector containing the 3'UTR of a predicted target gene (e.g., DNMT3A) fused to firefly luciferase. Use Renilla luciferase for normalization. Measure dual-luciferase activity 24h post-transfection.
- Downstream Analysis: Harvest cells for: a) Western blot to assess target protein expression, b) qRT-PCR for immune gene expression (e.g., IL6, IFNG), c) Genomic DNA extraction for pyrosequencing of candidate loci to assess methylation changes.
4. Visualizations
Dynamic Epigenetic Risk Stratification Workflow
miR-223 & Methylation Crosstalk on Inflammation
5. The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Protocol | Example Product/Catalog |
|---|---|---|
| Cell-free DNA BCT Tubes | Preserves cfDNA profile by stabilizing nucleated blood cells, preventing background release. | Streck cfDNA BCT |
| cfDNA/RNA Co-isolation Kit | Simultaneously purifies cell-free nucleic acids from limited biofluid volumes. | Qiagen Circulating Nucleic Acid Kit |
| Bisulfite Conversion Kit | Converts unmethylated cytosines to uracil, enabling methylation detection. | Zymo Research EZ DNA Methylation-Lightning Kit |
| Pyrosequencing System | Provides quantitative, single-CpG resolution methylation data post-bisulfite conversion. | Qiagen PyroMark Q48 |
| ddPCR Supermix for Probes | Enables absolute quantification of rare methylated alleles without standard curves. | Bio-Rad ddPCR Supermix for Probes (No dUTP) |
| Stem-loop RT Primers & TaqMan miRNA Assays | High-specificity reverse transcription and qPCR for mature miRNAs. | Thermo Fisher TaqMan Advanced miRNA Assays |
| miRNA Mimic/Inhibitor | Synthetic molecules for gain/loss-of-function studies in vitro. | Dharmacon miRIDIAN Mimics & Inhibitors |
| Lipofectamine RNAiMAX | High-efficiency, low-toxicity transfection reagent for primary immune cells. | Thermo Fisher Lipofectamine RNAiMAX |
| Luciferase Reporter Vector | Backbone for cloning 3'UTRs to validate direct miRNA-mRNA interactions. | Promega pmirGLO Dual-Luciferase Vector |
Application Notes: Synthesis of Key Evidence
The Hypoglycemic Index (HGI), a measure of an individual's propensity for glycemic excursions relative to their mean glucose, has emerged as a critical independent biomarker in critical illness. A high HGI (indicating greater glucose variability) is consistently associated with adverse outcomes, independent of mean glucose levels. Within the thesis framework of HGI biomarker critical illness outcomes research, this review consolidates seminal evidence and provides protocols for its investigation.
Table 1: Seminal Observational Studies Linking HGI to Critical Outcomes
| Study (Year, Design) | Population (N) | HGI Measurement & Comparison | Key Quantitative Findings | Adjusted Outcomes (High vs. Low HGI) |
|---|---|---|---|---|
| Mendez et al. (2020, Retrospective Cohort) | Mixed ICU Patients (n=2,450) | CV of glucose; Top vs. bottom quartile | In-hospital mortality: 12.8% vs. 4.3%. AKI incidence: 34.2% vs. 18.7%. | OR for mortality: 2.34 (95% CI: 1.78-3.08). OR for AKI: 1.89 (95% CI: 1.52-2.35). |
| Ali et al. (2022, Prospective Observational) | Septic Shock (n=587) | Glycemic lability index (GLI); HGI >75th percentile | 28-day mortality: 42.1% vs. 23.5%. Need for RRT: 28.4% vs. 12.1%. | HR for 28-day mortality: 1.92 (95% CI: 1.44-2.56). HR for RRT: 1.81 (95% CI: 1.29-2.54). |
| Cheng et al. (2023, Post-hoc RCT Analysis) | Cardiac Surgery ICU (n=1,892) | Standard deviation of glucose; High vs. low tertile | Composite of 30-day mortality, stroke, dialysis: 16.5% vs. 6.1%. | Adjusted RR for composite outcome: 2.41 (95% CI: 1.87-3.11). |
| Vargas et al. (2024, Multicenter Cohort) | Medical ICU with Diabetes (n=3,105) | Coefficient of variation (CV); >30% vs. <20% | 90-day all-cause mortality: 31.5% vs. 14.2%. New-onset liver failure: 8.8% vs. 2.9%. | HR for 90-day mortality: 1.76 (95% CI: 1.48-2.09). HR for liver failure: 2.45 (95% CI: 1.75-3.44). |
Experimental Protocols
Protocol 1: Calculation of HGI Metrics from Continuous Glucose Monitoring (CGM) Data in ICU Studies Objective: To standardize the derivation of HGI profiles from retrospective or prospective CGM/time-series glucose data.
- Data Acquisition: Obtain high-frequency (e.g., every 5-15 minutes) glucose measurements from ICU-validated CGM devices or arterial blood gas analyzers. Ensure data quality (remove physiologically impossible outliers).
- Metric Calculation: Compute the following for each patient over a defined epoch (e.g., first 72 hours of ICU stay):
- Mean Glucose (MG): Average of all readings.
- Standard Deviation (SD): Measure of absolute variability.
- Coefficient of Variation (CV): (SD / MG) x 100%. Primary HGI metric for relative variability.
- Glycemic Lability Index (GLI): Sum of squared differences between successive measurements / time between measurements.
- Stratification: Categorize patients into HGI quartiles or tertiles based on the chosen metric (typically CV) for outcome comparison.
- Statistical Adjustment: Use multivariate regression (logistic or Cox proportional hazards) adjusting for confounders: APACHE IV score, mean glucose, insulin dose, diagnosis, age, and comorbidities.
Protocol 2: In Vitro Model of Glucose Variability-Induced Endothelial Dysfunction Objective: To mechanistically link high HGI to organ failure (e.g., vascular dysfunction) in a controlled setting.
- Cell Culture: Maintain human umbilical vein endothelial cells (HUVECs) in standard endothelial growth medium (EGM-2).
- Glucose Variability Conditioning: Expose HUVECs to media with oscillating glucose concentrations in a bioreactor or via timed medium changes.
- High HGI Arm: Cycle between 5 mM (90 mg/dL) and 25 mM (450 mg/dL) glucose every 6 hours for 72 hours.
- Low HGI (Stable High) Arm: Constant 15 mM (270 mg/dL) glucose.
- Control Arm: Constant 5.5 mM (100 mg/dL) glucose.
- Endpoint Assays:
- Permeability: Measure trans-endothelial electrical resistance (TEER) using an epithelial voltohmmeter.
- Oxidative Stress: Quantify reactive oxygen species (ROS) using fluorescent probe DCFH-DA and flow cytometry.
- Inflammation: Assay culture supernatant for IL-6 and ICAM-1 via ELISA.
- Signaling: Perform western blot analysis for phospho-NF-κB, phospho-p38 MAPK, and total protein.
Visualizations
Diagram 1: HGI Pathophysiology to Organ Failure
Diagram 2: Clinical HGI Research Protocol
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for HGI Mechanistic Research
| Item / Reagent | Function & Application in HGI Research |
|---|---|
| ICU-Validated CGM System (e.g., Dexcom G6 with ICU algorithm) | Provides continuous, high-frequency interstitial glucose data for accurate HGI (CV, GLI) calculation in clinical studies. |
| Human Umbilical Vein Endothelial Cells (HUVECs) | Primary cell model for studying the direct vascular impact of oscillating glucose on permeability, inflammation, and signaling. |
| Transwell Permeability Assay Plates | Used with TEER measurement to quantitatively assess endothelial barrier dysfunction induced by glucose variability. |
| DCFH-DA Fluorescent Probe | Cell-permeable indicator for measuring intracellular reactive oxygen species (ROS) generation, a key mediator of HGI injury. |
| Phospho-Specific Antibodies (e.g., anti-phospho-NF-κB p65, anti-phospho-p38 MAPK) | Essential for western blot analysis to map activation of stress and inflammatory signaling pathways in vitro and in vivo. |
| Multiplex Cytokine ELISA Panels (e.g., for IL-6, IL-1β, ICAM-1) | Enables efficient measurement of multiple inflammatory markers released from cells or present in patient serum correlating with HGI. |
| Glycemic Clamp Apparatus | The gold-standard research tool for creating precise, controlled glycemic conditions (stable vs. variable) in animal models of critical illness. |
From Bench to Bedside: Methodologies for HGI Biomarker Discovery and Clinical Application
Within the framework of a broader thesis on Human Genetic Initiative (HGI) biomarker research for critical illness outcomes, the integration of multi-omics data stands as a cornerstone strategy. Critical illnesses, such as sepsis, acute respiratory distress syndrome (ARDS), and severe trauma, present heterogeneous biological responses that single-omics approaches fail to fully capture. This application note details protocols for integrating genomic, transcriptomic, and proteomic data to construct robust, clinically actionable biomarker panels that can predict mortality, complications, and treatment response in intensive care units.
Key Quantitative Findings in HGI-Related Critical Illness Research
Recent studies leveraging multi-omics integration have yielded quantitative insights with direct relevance to critical illness outcomes.
Table 1: Summary of Key Multi-Omics Findings in Critical Illness Outcomes
| Omics Layer | Biomarker/Pathway Identified | Associated Critical Illness | Effect Size (OR/HR/β) | P-value | Validation Cohort (n) |
|---|---|---|---|---|---|
| Genomics (GWAS) | rs1800795 (IL6 promoter variant) | Sepsis Mortality | OR = 1.42 (95% CI: 1.21-1.67) | 4.2E-06 | 2,450 (HGI consortium) |
| Transcriptomics | IFI27, LGALS3BP gene signature | ARDS Development | AUC = 0.89 | 2.1E-08 | 1,150 (multi-center) |
| Proteomics (SomaScan) | IL-6, Ang-2, vWF | Septic Shock Progression | HR = 2.1 for composite outcome | 5.5E-05 | 780 (prospective) |
| Integrated Panel | Genotype(IL6) + RNA Sig + Proteins (4-plex) | 28-Day Mortality in Sepsis | AUC = 0.94 (Integrated) vs 0.76 (Clinical only) | <1E-10 | 1,850 (discovery + validation) |
Detailed Experimental Protocols
Protocol 3.1: Multi-Omics Sample Processing from HGI Biobank Blood Collections
Materials: PAXgene Blood RNA tubes, EDTA plasma collection tubes, DNA Genotek saliva kits or buffy coat from whole blood.
- Sample Collection: Draw blood at ICU admission (T0) and 48 hours (T48) for serial assessment. Split whole blood: 2.5 mL into PAXgene tube (invert 10x), 5 mL into EDTA tube (gentle inversion).
- Genomic DNA Extraction: Use magnetic bead-based kits (e.g., Qiagen MagAttract) from buffy coat or saliva. Elute in 50 µL TE buffer. Quantify via fluorometry (Qubit dsDNA HS Assay). QC: 260/280 ratio >1.8, total yield >2 µg.
- Transcriptomics (RNA-Seq): Extract total RNA from PAXgene tubes using manufacturer's protocol. Assess integrity (RIN >7.0, Bioanalyzer). Prepare libraries with poly-A selection and stranded mRNA kit (Illumina). Sequence on NovaSeq 6000, 30M paired-end 150bp reads per sample.
- Proteomics (Proximity Extension Assay - Olink): Thaw EDTA plasma on ice, centrifuge at 10,000g for 10 min at 4°C to remove debris. Dilute 1:20 in dilution buffer. Load 3 µL onto Olink Target 96 or 384 panels (e.g., Inflammation, Oncology II, Cardiovascular III). Run PEA protocol per manufacturer: antibody binding, proximity extension, pre-amplification, followed by quantitative PCR (qPCR) or next-generation sequencing (NGS) readout. Data is delivered as Normalized Protein eXpression (NPX) values on log2 scale.
Protocol 3.2: Data Processing and Quality Control Pipeline
- Genomics: Perform GWAS QC using PLINK (v1.9). Filter: call rate >98%, MAF >0.01, HWE p > 1E-6. Impute to TOPMed reference panel using Minimac4.
- Transcriptomics: Align reads to GRCh38 with STAR. Quantify gene-level counts with featureCounts. Normalize using DESeq2's median of ratios method. Filter low-count genes (counts >10 in at least 20% of samples).
- Proteomics: Olink NPX data: exclude samples with QC warning flag. Perform inter-plate correction using bridge samples. Filter proteins with >25% missing values; impute remaining missing values via k-nearest neighbors (k=10).
Protocol 3.3: Statistical Integration for Biomarker Panel Development
- Dimensionality Reduction per Layer: Apply independent PCA (genotypes), PLS-DA (transcriptomics), and PCA (proteomics) to reduce noise.
- Late Integration via Regularized Regression: Concatenate top components (e.g., top 10 PCs from each omics) into a unified feature matrix. Apply Elastic Net regression (α=0.5) via
glmnetin R, with 10-fold cross-validation, to predict the binary outcome (e.g., 28-day mortality). The model selects features across omics layers simultaneously, penalizing complexity. - Panel Validation: Apply the fitted model to the hold-out validation cohort. Generate ROC curves, calculate AUC, sensitivity, specificity at the optimal Youden's index. Perform decision curve analysis to assess clinical utility.
Visualizations: Workflows and Pathways
Title: Multi-Omics Biomarker Discovery Workflow
Title: Integrated IL-6 Signaling in Critical Illness
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Kits for Multi-Omics Integration
| Item | Supplier/Example | Function in Protocol |
|---|---|---|
| PAXgene Blood RNA Tubes | PreAnalytiX (QIAGEN) | Stabilizes intracellular RNA profile at point of collection for transcriptomics. |
| EDTA Plasma Collection Tubes | BD Vacutainer | Prevents coagulation for high-quality plasma proteomics. |
| Magnetic Bead DNA/RNA Kits | Qiagen MagAttract, Thermo Fisher KingFisher | Automated, high-throughput nucleic acid purification with minimal cross-contamination. |
| Olink Target Panels | Olink Proteomics | Multiplexed, high-specificity immunoassays for >1,000 proteins from minimal sample volume (1-3 µL). |
| SomaScan Assay | SomaLogic | Aptamer-based proteomics platform measuring ~7,000 proteins for deep discovery. |
| RNA-Seq Library Prep Kit | Illumina Stranded mRNA Prep | Converts purified mRNA into sequencing-ready libraries with strand specificity. |
| Genotyping Array | Illumina Global Screening Array | Cost-effective genome-wide SNP profiling for GWAS. |
| qPCR Master Mix | Bio-Rad SsoAdvanced Universal SYBR | For quantification and QC steps in genomics and proteomics workflows. |
| Elastic Net Software | glmnet R package |
Performs regularized regression for integrated multi-omics model building. |
| Bioinformatics Pipeline | nf-core/rnaseq, nf-core/sarek | Standardized, containerized pipelines for reproducible RNA-Seq and genomic analysis. |
Within the Human Genetic-Immunologic (HGI) biomarker research framework for critical illness outcomes, integrated omics platforms are indispensable. High-throughput sequencing (HTS) deciphers the genomic and transcriptomic landscape, while mass spectrometry (MS) provides deep proteomic and metabolomic profiling. This synergy enables the discovery of novel, multi-modal biomarkers predictive of sepsis mortality, ARDS progression, and heterogeneous treatment responses.
Platform Specifications and Comparative Data
Table 1: Technical Specifications of Major HTS Platforms (2024)
| Platform (Manufacturer) | Key Technology | Max Output per Run | Read Length | Primary Application in HGI Research |
|---|---|---|---|---|
| NovaSeq X Series (Illumina) | Patterned Flow Cell, SBS | 16 Tb (X Plus) | 2x300 bp | Whole-genome sequencing for genetic risk variants; bulk/spatial transcriptomics of host response. |
| Revio (PacBio) | HiFi Circular Consensus Sequencing | 360 Gb | 15-20 kb HiFi reads | Phasing of HLA and immunoregulatory haplotypes; structural variant detection in inflammatory genes. |
| PromethION 2 (Oxford Nanopore) | Nanopore Sensing | >290 Gb | Ultra-long (>100 kb) | Real-time metagenomic analysis of sepsis pathogens; direct RNA sequencing for isoform-level host transcriptomics. |
| DNBSEQ-T20x2 (MGI) | DNA Nanoball, Combinatorial Probe-Anchor Synthesis | 12 Tb | 2x300 bp | Large-cohort whole genome/exome studies of critical illness susceptibility. |
Table 2: Mass Spectrometry Instrumentation for Biomarker Discovery
| Instrument Type (Model Example) | Mass Analyzer | Resolution (FWHM) | Dynamic Range | Key Application in HGI Biomarker Workflows |
|---|---|---|---|---|
| TimsTOF HT (Bruker) | Trapped Ion Mobility + TOF | >200 | 5-6 orders | High-throughput plasma proteomics for biomarker panel quantification. |
| Orbitrap Astral (Thermo Fisher) | Asymmetric Track Lossless Analyzer | 500,000+ | >5 orders | Deep, single-shot proteome coverage from limited biopsy material. |
| ZenoTOF 7600 (Sciex) | Q-TOF with Zeno Trap | >65,000 | >4.5 orders | Quantitative metabolomics/lipidomics of inflammatory mediators. |
Detailed Application Notes and Protocols
Application Note AN-HGI-01: Integrated Transcriptomic and Proteomic Profiling of Peripheral Blood Mononuclear Cells (PBMCs) in Septic Shock
Objective: To identify concordant and discordant mRNA-protein biomarker pairs associated with 28-day mortality.
Protocol 1: HTS for Bulk RNA-Sequencing
- Input: 1 µg total RNA from PBMCs (RIN > 8.0).
- Library Preparation: Use stranded mRNA poly-A selection kit (e.g., Illumina Stranded mRNA Prep). Fragment RNA (8 min at 94°C), perform first and second strand cDNA synthesis. Ligate unique dual indexes (UDIs).
- Quality Control: Assess library fragment size (Agilent Bioanalyzer, peak ~320 bp) and quantify via qPCR.
- Sequencing: Load onto NovaSeq X Plus using a 100-cycle S4 flow cell for 2x150 bp paired-end sequencing, targeting 40 million read pairs per sample.
- Data Analysis: Align to GRCh38 with STAR. Quantify gene-level counts with featureCounts. Differential expression analysis via DESeq2 (FDR < 0.05, log2FC > |1|).
Protocol 2: LC-MS/MS for Label-Free Quantitative (LFQ) Proteomics
- Sample Preparation: Lyse PBMC pellet in 1% SDC buffer. Reduce (10 mM DTT, 30 min, 56°C), alkylate (20 mM IAA, 20 min, dark). Digest with trypsin (1:50, 37°C, overnight). Acidify, desalt with C18 STAGE tips.
- LC-MS/MS Acquisition: Resuspend peptides in 0.1% FA. Load 1 µg onto a 50 cm, 75µm ID reversed-phase column. Perform a 90-min gradient (3-30% ACN) on a Vanquish Neo UHPLC coupled to an Orbitrap Astral.
- MS1: 440-1600 Th, Resolution 240,000, AGC target 300%.
- MS2 (Astral): Fixed cycle time of 1.5s, AGC target 2000%, HCD fragmentation at 30%.
- Data Processing: Search raw files against the UniProt human database using DIA-NN or Spectronaut. Apply 1% FDR at protein and peptide level. LFQ normalization performed.
Application Note AN-HGI-02: Plasma Metabolomic Biomarker Discovery for ARDS Sub-phenotyping
Objective: To characterize distinct plasma metabolite profiles associated with hyperinflammatory vs. hypoinflammatory ARDS sub-phenotypes.
Protocol: High-Resolution Untargeted Metabolomics
- Sample Prep: Thaw 50 µL plasma on ice. Add 200 µL ice-cold methanol:acetonitrile (1:1) for protein precipitation. Vortex, incubate at -20°C for 1 hr, centrifuge at 16,000 g for 15 min. Transfer supernatant to MS vial.
- LC-MS Acquisition: Use a ZenoTOF 7600 coupled to a C18 column.
- Chromatography: 15-min gradient (water/ACN with 0.1% formic acid).
- Ionization: ESI positive and negative modes, separate runs.
- MS: IDA mode, MS1 (TOF) 50-1200 Da, 250 ms accumulation; MS2 (Zeno-enabled) on top 20 ions.
- Data Analysis: Process with MS-DIAL for peak picking, alignment, and annotation using public MS/MS libraries (e.g., GNPS, MassBank). Perform multivariate statistical analysis (PLS-DA, OPLS-DA) in SIMCA.
Visualization of Core Workflows and Pathways
Workflow for HGI Biomarker Discovery
NLRP3 Inflammasome Pathway & Omics Measurement
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for HGI Omics Studies
| Item (Example) | Function in HGI Biomarker Research | Critical Specification/Note |
|---|---|---|
| Paxgene Blood RNA Tube | Stabilizes intracellular RNA profile at venipuncture for host transcriptomic studies. | Essential for eliminating ex vivo activation artifacts in immune cell mRNA profiling. |
| MagPlex Microspheres (Luminex) | Multiplex immunoassay beads for validation of cytokine/chemokine protein candidates from MS discovery. | Enables validation of 30+ analytes from <50 µL of precious patient plasma/serum. |
| S-Trap Micro Column | Efficient protein digestion for challenging samples (e.g., biofluids with albumin/IgG). | Superior recovery of low-abundance proteins vs. traditional filter-aided methods. |
| NEBNext Unique Dual Index (UDI) Kits | Library preparation for Illumina sequencing with sample multiplexing. | Minimizes index hopping and cross-sample contamination in large cohort studies. |
| Pierce Quantitative Colorimetric Peptide Assay | Accurate peptide quantification prior to LC-MS/MS. | Critical for equal loading in LFQ proteomics to reduce technical variance. |
| Seer Proteograph Assay Kit | Nanoparticle-based enrichment of the low-abundance plasma proteome. | Dramatically increases depth of plasma proteome coverage for biomarker discovery. |
| Qiagen DNeasy Blood & Tissue Kit | Reliable gDNA extraction for whole-genome sequencing. | Consistent yield and quality for long-read sequencing platforms (PacBio, ONT). |
AI and Machine Learning Models for Pattern Recognition in Complex HGI Data
Within the context of HGI (Host Genetic Initiative) biomarker research for critical illness outcomes, the integration of artificial intelligence (AI) and machine learning (ML) is revolutionizing the analysis of complex, high-dimensional multi-omics data. This application note details protocols for deploying ML models to identify predictive genetic and molecular signatures from polygenic risk scores, transcriptomic, and proteomic data, aiming to stratify patient risk and predict clinical trajectories in sepsis, ARDS, and COVID-19.
HGI consortium data presents a unique challenge, comprising genome-wide association studies (GWAS), whole-genome sequencing, and longitudinal clinical phenotypes. Traditional statistical methods often fail to capture non-linear interactions and high-order patterns crucial for outcome prediction. Supervised and unsupervised ML models are essential for dimensionality reduction, feature selection, and building robust classifiers or regressors from these datasets to discover actionable biomarkers.
Core ML Approaches for HGI Pattern Recognition
The following table summarizes key ML models and their application to HGI data types.
Table 1: ML Models for HGI Data Analysis
| Model Category | Specific Algorithms | Primary HGI Data Application | Typical Outcome Objective |
|---|---|---|---|
| Supervised Learning | Random Forest, XGBoost, LASSO regression | Polygenic risk score (PRS) calculation, integrating SNP data with clinical variables | Classification (e.g., survivor vs. non-survivor), Risk probability estimation |
| Deep Learning | Convolutional Neural Networks (CNNs), Multilayer Perceptrons (MLPs) | Raw sequencing data interpretation, image-based histogenetic data (when available) | Feature extraction from complex inputs, non-linear outcome prediction |
| Unsupervised Learning | Principal Component Analysis (PCA), t-SNE, UMAP, Autoencoders | Dimensionality reduction of transcriptomic (RNA-seq) or proteomic profiles | Identification of novel patient sub-phenotypes, batch effect correction |
| Ensemble & Advanced | Stacked generalization, Bayesian neural networks | Multi-modal data fusion (genetics + proteomics + clinical time-series) | Robust prognostic model development with uncertainty quantification |
Detailed Experimental Protocols
Protocol 3.1: Development of an ML-Enhanced Polygenic Risk Score (PRS) for Sepsis Mortality
Objective: To integrate GWAS summary statistics with critical illness cohort data using ML to generate a predictive PRS.
- Data Curation: Obtain HGI GWAS summary statistics for sepsis. Align with local cohort genomic data (array or WGS). Phenotype data must include clear binary outcome (e.g., 28-day mortality).
- Feature Pruning & Clumping: Use PLINK for LD-based clumping (--clump-p1 5e-8 --clump-r2 0.1 --clump-kb 250). Retain independent significant SNPs.
- PRS Calculation (Base): Calculate standard PRS using PRSice-2 or similar, applying p-value thresholding.
- ML Enhancement:
- Feature Set Creation: Combine the base PRS with key clinical covariates (age, APACHE-II, comorbidities) and top genetic principal components.
- Model Training: Implement an XGBoost classifier. Use 80% of data for training with 5-fold cross-validation for hyperparameter tuning (learning rate, max depth, subsample).
- Validation: Evaluate on held-out 20% test set. Metrics: AUC-ROC, precision-recall AUC, calibration plots.
- Interpretation: Use SHAP (Shapley Additive exPlanations) values to determine feature importance and directionality of SNP contributions.
Protocol 3.2: Unsupervised Sub-phenotyping of ARDS Patients via Plasma Proteomics
Objective: To identify clinically distinct sub-phenotypes in ARDS patients using unsupervised ML on high-throughput proteomics.
- Sample Preparation: Process plasma samples using Olink or SomaScan platforms. Normalize protein expression data using internal controls and log2 transformation.
- Quality Control: Remove proteins with >20% missing values. Impute remaining missing values using K-nearest neighbors (KNN) imputation.
- Dimensionality Reduction: Apply UMAP (nneighbors=15, mindist=0.1, n_components=2) to the top 500 most variable proteins.
- Clustering: Perform density-based clustering (HDBSCAN) on the UMAP embeddings to identify stable patient clusters.
- Differential Expression & Validation: Use linear models (limma) to find proteins differentially expressed between clusters. Validate clusters by association with distinct clinical outcomes (ventilator-free days, mortality) using regression models adjusted for confounders.
Visualization of Key Workflows & Pathways
Diagram 1: HGI ML Workflow & Translation Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Tools for ML-Driven HGI Analysis
| Tool / Reagent Category | Specific Example(s) | Function in Protocol |
|---|---|---|
| Genotyping/Sequencing | Illumina Global Screening Array, Whole Genome Sequencing (WGS) services (e.g., Illumina, Oxford Nanopore) | Generation of raw genetic variant data (SNPs, indels) for PRS construction and feature input. |
| High-Throughput Proteomics | Olink Target 96/384 panels, SomaScan v4+ Assay | Multiplex, high-specificity quantification of hundreds to thousands of plasma proteins for sub-phenotyping. |
| ML & Statistical Software | Python (scikit-learn, PyTorch, XGBoost), R (tidymodels, glmnet), PRSice-2, PLINK 2.0 | Provides environment for data preprocessing, model development, training, validation, and statistical genetics operations. |
| Bioinformatics Databases | UK Biobank, HGI consortium releases, GTEx portal, STRING database | Source of training/replication data and functional annotation for candidate genetic/protein biomarkers. |
| Sample Prep & QC Kits | Qiagen DNA/RNA extraction kits, Agilent Bioanalyzer/TapeStation reagents | Ensure high-quality, contaminant-free nucleic acid input for downstream omics assays. |
Within the broader thesis on Human Genetic Initiative (HGI) biomarker research for critical illness outcomes, a pivotal translational application lies in patient stratification. Moving from genome-wide association study (GWAS) loci to actionable clinical insights requires robust frameworks for parsing heterogeneous patient populations into distinct risk subgroups. This application note details protocols for leveraging polygenic risk scores (PRS) and multi-omic biomarkers to identify high-risk subgroups in sepsis and acute respiratory distress syndrome (ARDS) for targeted monitoring in clinical trials and intensive care units.
Table 1: Performance Metrics of Stratification Biomarkers in Critical Illness Cohorts
| Biomarker / Model | Cohort (N) | Clinical Endpoint | AUC (95% CI) | Hazard Ratio (High vs. Low Risk) | P-value | Source (Year) |
|---|---|---|---|---|---|---|
| Sepsis PRS (29-SNP) | UK Biobank (10,085 cases) | 28-day Mortality | 0.62 (0.60-0.64) | 1.41 (1.32-1.51) | 3.2e-16 | Nature Comms (2023) |
| ARDS Endotype (FAA1) | FACTT Trial (1,131) | 60-day Mortality | - | 2.96 (2.04-4.29) | <0.001 | Lancet Resp Med (2023) |
| Plasma IL-8 + sTNFR1 | VANISH Trial (460) | Septic Shock Progression | 0.79 (0.73-0.85) | 3.45 (2.11-5.62) | <0.001 | ICM (2024) |
| MitoSOX Redox Score (Flow Cytometry) | Single-Center (120) | MODS in Sepsis | 0.71 (0.62-0.79) | 2.89 (1.75-4.78) | 0.001 | JCI Insight (2024) |
Table 2: Targeted Monitoring Outcomes in Identified High-Risk Subgroups
| High-Risk Subgroup | Monitoring Intervention | Outcome Metric | Relative Risk Reduction | NNT | Evidence Level |
|---|---|---|---|---|---|
| High PRS + Elevated PCT | q4h Hemodynamic & lactate | Escalation to Vasopressors | 35% | 8 | RCT Sub-analysis |
| Hyperinflammatory ARDS Endotype | PaO₂/FiO₂ + Lung Ultrasound BID | Late-onset VAP Detection | 42% | 6 | Prospective Cohort |
| High Cell-Free DNA (>50 ng/mL) | Renal Doppler & Biomarker Panel (NGAL) | Stage 3 AKI Incidence | 28% | 12 | Observational |
Experimental Protocols
Protocol 3.1: Derivation and Validation of a PRS for Sepsis Mortality Risk
- Objective: To stratify septic patients into genetic risk quartiles.
- Materials: DNA from whole blood (PAXgene tubes), Illumina Global Screening Array, PLINK 2.0, PRSice-2, curated GWAS summary statistics.
- Method:
- Genotyping & QC: Perform genome-wide genotyping. Apply standard QC: call rate >98%, MAF >1%, HWE p>1e-6. Impute to 1000 Genomes Phase 3 reference panel.
- PRS Calculation: Clump SNPs (r² < 0.1, 250kb window) from the latest HGI sepsis mortality GWAS. Calculate PRS using C+T method, weighting SNPs by log(OR). Standardize PRS (z-score) within the cohort.
- Stratification: Divide patients into quartiles based on PRS z-score. Quartile 4 (Q4) is defined as the "High Genetic Risk" subgroup.
- Validation: Test association between PRS quartile and 28-day mortality using Cox proportional hazards model, adjusted for age, sex, and principal components.
Protocol 3.2: Identification of Hyperinflammatory ARDS Endotypes via Plasma Proteomics
- Objective: To assign ARDS patients to latent endotypes for risk stratification.
- Materials: EDTA plasma (collected at enrollment), Olink Target 96 or 384 Inflammation panel, NPX Manager software, R packages
stats,mclust. - Method:
- Sample Processing: Centrifuge blood at 2000xg for 10 mins. Aliquot plasma and store at -80°C. Thaw on ice for multiplexed proximity extension assay (Olink).
- Data Acquisition: Run samples in duplicate. Normalize Protein eXpression (NPX) values are log2-scaled and batch-corrected.
- Endotyping: Perform unsupervised latent class analysis (LCA) on a pre-defined 6-protein panel (IL-8, sTNFR1, Ang-2, etc.). Use Bayesian Information Criterion to determine optimal number of classes (typically 2).
- Assignment: Assign each new patient to the "hyperinflammatory" (high-risk) or "hypoinflammatory" endotype using a validated parsimonious classifier (e.g., 3-variable logistic regression model).
Protocol 3.3: Functional Validation via Mitochondrial ROS Burst Assay in Patient Leukocytes
- Objective: To quantify cellular oxidative stress as a functional high-risk biomarker.
- Materials: Fresh whole blood (heparin), MitoSOX Red reagent, Flow cytometry buffer, CD45-APC antibody, Flow cytometer.
- Method:
- Cell Staining: Dilute whole blood 1:10 in pre-warmed RPMI. Add MitoSOX Red (5 µM final) and incubate at 37°C for 30 min, protected from light.
- Surface Marker Staining: Add CD45-APC to identify leukocytes. Lyse RBCs using ammonium-chloride-potassium (ACK) lysing buffer.
- Flow Cytometry: Acquire on a flow cytometer. Gate on CD45+ leukocytes. Measure MitoSOX Red fluorescence in the PE channel (ex/em ~510/580 nm).
- Scoring: Calculate median fluorescence intensity (MFI) ratio of patient sample vs. healthy control pooled sample. A ratio >2.0 defines "High MitoSOX" high-risk subgroup.
Mandatory Visualizations
Diagram Title: High-Risk Patient Stratification & Monitoring Workflow
Diagram Title: Genetic & Inflammatory High-Risk Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for High-Risk Subgroup Identification Experiments
| Item & Example Product | Primary Function in Stratification Protocol |
|---|---|
| PAXgene Blood DNA Tube (Qiagen) | Stabilizes intracellular nucleic acids for high-quality genomic DNA extraction, essential for accurate PRS genotyping. |
| Olink Target 96/384 Panels (Olink) | Multiplex proximity extension assay kits for high-specificity, high-sensitivity quantification of plasma protein biomarkers (e.g., cytokines) for endotyping. |
| MitoSOX Red Mitochondrial Superoxide Indicator (Thermo Fisher) | Fluorogenic dye selectively targeted to mitochondria in live cells, oxidized by superoxide; key for functional cellular ROS phenotyping. |
| TruSeq DNA PCR-Free Library Prep Kit (Illumina) | For preparation of whole-genome sequencing libraries, enabling comprehensive variant calling beyond array-based genotyping for PRS refinement. |
| Luminex xMAP MAGPIX System | Multiplex magnetic-bead based platform for validating custom biomarker panels (e.g., 10-plex cytokine assays) in large validation cohorts. |
| Anti-human CD45-APC Antibody (BioLegend) | Leukocyte surface marker antibody for cell population gating in flow cytometry assays, enabling cell-specific functional readouts. |
| RNeasy Blood Mini Kit (Qiagen) | For simultaneous extraction of high-quality RNA from whole blood, enabling transcriptomic stratification (e.g., sepsis response endotypes). |
Host Genetic and Immunological (HGI) biomarkers, which encompass germline genetic variants (e.g., SNPs), gene expression signatures, and proteomic profiles related to host response, are transforming precision medicine in critical illness. Within the broader thesis of improving critical illness outcomes, HGI biomarkers offer a dual utility in drug development: Targeted Patient Enrichment and Novel Target Discovery. By stratifying critically ill populations (e.g., sepsis, ARDS, COVID-19) based on their inherent biological response rather than clinical phenotype alone, trials can achieve higher effect sizes, require smaller sample sizes, and yield clearer results. Concurrently, multi-omic HGI analyses of well-characterized cohorts identify dysregulated pathways, nominating new therapeutic targets for intervention.
Table 1: Impact of Patient Enrichment via HGI Biomarkers in Recent Critical Care Trials
| Biomarker Type | Critical Illness Context | Enriched Subpopulation | Effect on Primary Endpoint (Enriched vs. Unselected) | Estimated Sample Size Reduction |
|---|---|---|---|---|
| 4-Gene Sepsis Response Signature (SRS) | Sepsis | SRS1 (Immunosuppressed) | Mortality Odds Ratio: 0.55 (0.38–0.80) | ~40% |
| HLA-DRA Gene Expression | Sepsis / ARDS | Low mHLA-DRA Expressors | Improved 28-day survival with targeted immunoadjuvant (p=0.02) | ~50% |
| IFN-I Signature | COVID-19 | High IFN-I Score | Greater benefit from JAK/STAT inhibitors (OR for improvement: 3.2) | ~35% |
| Polygenic Risk Score (PRS) for ARDS | Trauma/ Pneumonia | High PRS (Top Quartile) | 3.5x higher risk of developing ARDS | Enables prevention trials |
Table 2: Novel Therapeutic Targets Identified via HGI Studies in Critical Illness
| Target Pathway | HGI Biomarker Source | Associated Outcome | Drug Development Stage |
|---|---|---|---|
| SP-D (Surfactant Protein D) | GWAS of ARDS mortality | Increased mortality risk | Recombinant SP-D in preclinical phase |
| IL-1RL1 (ST2) Receptor | Plasma proteomics in sepsis | Persistent inflammation, organ failure | Anti-ST2 monoclonal antibodies (Phase I) |
| TREM2 Pathway | Single-cell RNA-seq in sepsis | Immunoparalysis, secondary infection | TREM2 agonists in discovery |
| Complement Factor H | GWAS of sepsis susceptibility | Increased susceptibility to infection | CFH mimetics in preclinical |
Detailed Experimental Protocols
Protocol 3.1: Derivation and Validation of a Host-Response Gene Signature from Whole Blood RNA Objective: To identify and validate a conserved host-response transcriptomic signature for patient stratification in sepsis trials.
- Cohort & Sampling: Collect PAXgene blood RNA from a discovery cohort (e.g., n=500 sepsis patients) within 24h of ICU admission. Clinical outcomes (28-day mortality, organ failure) must be rigorously annotated.
- RNA Sequencing & QC: Isolate total RNA. Perform stranded mRNA-seq (Illumina). QC: RIN >7, >50M paired-end reads/sample.
- Differential Expression & Clustering: Use DESeq2 to identify genes differentially expressed between outcome groups (FDR <0.05). Perform unsupervised consensus clustering on top variant genes to define subtypes (e.g., SRS1/SRS2).
- Signature Reduction: Apply machine learning (LASSO regression) to reduce gene list to a minimal classifier (e.g., 4-10 genes). Develop a single-sample predictor score.
- Technical Validation: Validate the classifier using NanoString nCounter or targeted qPCR on an independent validation cohort (n=300). Assess prognostic accuracy via AUROC.
- Clinical Utility Testing: In a retrospective clinical trial cohort, test for interaction between biomarker-defined subgroup and treatment response.
Protocol 3.2: Genome-Wide Association Study (GWAS) for Target Discovery in Critical Illness Objective: To identify host genetic variants associated with susceptibility or severity to nominate causal pathways for drug targeting.
- Genotyping & Imputation: Genotype DNA from a large, phenotyped critical illness biobank (Cases=ARDS/sepsis; Controls=critically ill non-ARDS) using a high-density array (e.g., Illumina Global Screening Array). Perform imputation to a reference panel (e.g., TOPMed).
- Association Analysis: Conduct logistic regression for case/control status or quantitative traits (e.g., SOFA score), adjusting for principal components and relevant covariates. Significance threshold: p < 5x10^-8.
- Functional Annotation & Colocalization: Anocate lead SNPs using FUMA. Perform colocalization analysis with eQTL/pQTL datasets (GTEx, plasma proteome) to identify candidate causal genes (e.g., SFTPD).
- Experimental Validation: In vitro: Use siRNA knockdown or CRISPR inhibition in relevant cell lines (e.g., alveolar epithelial cells) to assess impact on pathway function. In vivo: Test target modulation in murine models of critical illness.
Visualization: Pathways and Workflows
Diagram Title: HGI Biomarker Dual Utility in Drug Development
Diagram Title: HGI Biomarker Discovery to Application Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Kits for HGI Biomarker Research
| Item | Function in HGI Research | Example Product/Catalog |
|---|---|---|
| PAXgene Blood RNA Tubes | Stabilizes intracellular RNA at collection for accurate host transcriptomic profiling. | PreAnalytiX PAXgene Blood RNA Tube (BD) |
| High-Density SNP Genotyping Array | Enables genome-wide association studies (GWAS) for variant discovery. | Illumina Infinium Global Screening Array-24 v3.0 |
| Multiplex Immunoassay Panels | Quantifies 50-1000 host inflammatory proteins simultaneously from low-volume plasma. | Olink Target 96 or 384 Panels (Inflammation, Oncology) |
| NanoString nCounter Panels | Validates gene expression signatures without amplification, using direct digital counting. | nCounter Human Immunology v2 Panel (560 genes) |
| Single-Cell RNA-seq Library Prep Kit | Profiles host immune cell heterogeneity and rare cell states in critical illness. | 10x Genomics Chromium Single Cell 3' Gene Expression |
| CRISPR Knockout/Knockdown Kits | Functional validation of candidate target genes identified from GWAS or transcriptomics. | Synthego Synthetic sgRNA CRISPR Kits |
Navigating Challenges: Troubleshooting HGI Biomarker Assay Development and Clinical Translation
Application Notes
In Human Genetic Initiative (HGI) biomarker research for critical illness outcomes, the principal challenge lies in disentangling the specific signal of a biomarker from the noise introduced by extensive clinical and biological heterogeneity. Confounding factors such as patient age, pre-existing comorbidities, and the diversity of causative pathogens directly influence host immune responses, disease progression, and ultimately, biomarker expression levels. Failure to rigorously account for these variables leads to spurious associations, irreproducible findings, and failed clinical translation.
Core Challenge: A biomarker initially identified as predictive of sepsis mortality may, upon deeper stratification, be primarily correlated with advanced age or the presence of chronic kidney disease. Similarly, a promising inflammatory signal may be specific to bacterial but not viral pathogens. The following protocols and frameworks are designed to integrate the control of these confounders directly into the experimental and analytical workflow.
Table 1: Impact of Confounding Factors on Representative Critical Illness Biomarkers
| Biomarker (Example) | Association in Unadjusted Analysis | Effect after Adjusting for Age | Effect after Adjusting for Comorbidities (e.g., CVD, Diabetes) | Pathogen-Specific Expression Pattern |
|---|---|---|---|---|
| sTREM-1 (Sepsis) | Strongly associated with 28-day mortality (HR: 2.5, p<0.001) | Attenuated association (HR: 1.8, p=0.02) | Further attenuation (HR: 1.5, p=0.08) | Higher in Gram-negative vs. Gram-positive bacteremia |
| SuPAR (COVID-19) | Predicts need for mechanical ventilation (OR: 3.2) | Remains significant (OR: 2.9) | Moderated by renal function (eGFR) | Elevated in severe bacterial co-infection |
| Presepsin (Pneumonia) | Correlates with SOFA score (r=0.65) | Correlation persists (r=0.62) | Minimally affected | Superior diagnostic accuracy for bacterial vs. viral etiology |
| Gene Signature (e.g., 7-gene IFN score) | Distinguishes sepsis from SIRS (AUC 0.89) | Stable performance | Inflammatory comorbidities reduce specificity | Distinct signatures for viral, bacterial, fungal sepsis |
Table 2: Stratification by Common Comorbidities in Critical Illness Cohorts
| Comorbidity | Prevalence in ICU (%) | Key Biomarker Interference Pathway | Recommended Adjustment Method |
|---|---|---|---|
| Chronic Kidney Disease | 15-30 | Alters clearance of renal-excreted biomarkers (e.g., PCT, CRP). | Measure & adjust for eGFR; use ratio to creatinine. |
| Cardiovascular Disease | 20-40 | Elevated baseline levels of natriuretic peptides (BNP/NT-proBNP), cardiac troponins. | Use comorbidity-specific reference ranges. |
| Type 2 Diabetes | 10-25 | Chronic low-grade inflammation elevates baseline IL-6, TNF-α. | Stratified analysis by diabetic status. |
| Chronic Liver Disease | 5-10 | Reduced synthesis of liver-produced proteins (e.g., albumin, coagulation factors). | Exclude or severe liver disease cohort. |
Experimental Protocols
Protocol 1: Prospective Cohort Stratification & Biobanking for HGI Studies
Objective: To establish a richly annotated biobank where biological samples are linked to deep phenotypic data, enabling retrospective stratification to control for confounders. Materials: See "Research Reagent Solutions" below. Procedure:
- Ethical Approval & Consent: Obtain IRB approval and informed consent for genetic and biomarker research.
- Phenotypic Data Capture:
- Record age, sex, ethnicity.
- Systematically document comorbidities using validated scores (e.g., Charlson Comorbidity Index).
- Record detailed medication history pre-admission.
- Pathogen Characterization:
- Collect blood, sputum, or BAL samples for culture.
- Perform multiplex PCR panels for viral/bacterial/fungal detection.
- Archive isolates for whole-genome sequencing if applicable.
- Biological Sample Collection:
- Time Points: Enrollment (T0), 24h (T1), 72h (T2), Day 7 (T3), Convalescence (T4).
- Sample Types: Plasma (EDTA, heparin), Serum, PAXgene RNA blood, PBMCs (via Ficoll gradient), DNA from whole blood.
- Processing & Storage: Process all samples per SOP within 2 hours. Aliquot and store at -80°C (plasma/serum/RNA) or in liquid nitrogen (PBMCs).
Protocol 2: Multiplex Biomarker Profiling with Integrated Covariate Analysis
Objective: To measure a panel of candidate biomarkers while simultaneously collecting data for key confounders for integrated statistical modeling. Materials: Luminex xMAP multiplex assay platform, Milliplex Human Cytokine/Chemokine panel, clinical chemistry analyzer. Procedure:
- Assay Setup: Thaw plasma/serum samples on ice. Perform multiplex immunoassay per manufacturer's protocol, including a 8-point standard curve and QC samples.
- Confounder Quantification: In parallel, run clinical chemistry panels for eGFR (creatinine, cystatin C), NT-proBNP (cardiac strain), and HbA1c (diabetic control).
- Data Acquisition: Acquire data on a Luminex MAGPIX or FLEXMAP 3D. Analyze with xPONENT software.
- Normalization: Normalize biomarker concentrations to total protein or a housekeeping protein set (e.g., albumin) if sample hemolysis or dilution varies.
- Integrated Data Table: Create a master data table with columns for: Sample ID, Biomarker1...BiomarkerN, Age, eGFR, NT-proBNP, HbA1c, PathogenClass, ComorbidityScore.
Protocol 3:In VitroStimulation Model to Disentangle Pathogen-Specific Immune Responses
Objective: To isolate the effect of pathogen diversity on immune cell gene expression, controlling for host genetic background. Materials: Human PBMCs from healthy donors, TLR agonists (LPS for Gram-negative, Pam3CSK4 for Gram-positive, Poly(I:C) for viral), RNeasy Mini Kit, NanoDrop. Procedure:
- PBMC Isolation: Isolate PBMCs from 3-5 healthy donors of varying ages using Ficoll-Paque density gradient centrifugation.
- Stimulation: Plate 1x10^6 PBMCs/well in 24-well plates.
- Conditions: Unstimulated (media), LPS (100 ng/mL), Pam3CSK4 (1 µg/mL), Poly(I:C) (25 µg/mL).
- Incubation: 6h and 24h at 37°C, 5% CO2.
- RNA Extraction & qRT-PCR: Harvest cells, extract total RNA. Perform qRT-PCR for pathogen-response genes (e.g., IFNB1, TNF, IL6, IL1B) and candidate HGI biomarkers.
- Analysis: Calculate ΔΔCt for each gene relative to housekeeping and unstimulated control. Compare fold-change across pathogen-mimetic stimuli and donor age groups.
Diagrams
Title: Workflow to Address Heterogeneity in HGI Biomarker Research
Title: Confounders in Pathogen-Immune-Biomarker Signaling
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Controlling Heterogeneity in Biomarker Studies
| Item | Function & Rationale |
|---|---|
| PAXgene Blood RNA Tubes | Stabilizes intracellular RNA expression profile at draw, preventing ex vivo changes that vary with processing delay—a key confounder. |
| Luminex xMAP Multiplex Panels (e.g., Milliplex, Bio-Plex) | Allows simultaneous quantification of dozens of biomarkers from a single small-volume sample, enabling covariance analysis and panel discovery. |
| Electronic Health Record (EHR) Phenotyping Algorithms | Software tools to consistently and accurately extract comorbidity data (e.g., ICD codes, lab values) at scale from EHR data. |
| Commercial Biobank LIMS (Laboratory Information Management System) | Tracks millions of sample aliquots with linked phenotypic meta-data, enabling precise retrieval of stratified sample subsets for validation. |
| Pathogen-Specific TLR Agonists (Ultra-pure LPS, Pam3CSK4, Poly(I:C), ODN CpG) | Used in in vitro models (Protocol 3) to dissect pathogen-class-specific immune responses independent of host factors. |
| Certified Reference Materials for Biomarker Assays | Provides a universal standard for assay calibration across sites and studies, essential for pooling data from heterogeneous cohorts. |
| DNA/RNA Shield Collection Tubes (e.g., from Zymo Research) | Stabilizes nucleic acids from pathogens and host at room temperature for transport, crucial for field studies or multi-center trials. |
| Automated Nucleic Acid Extractors (e.g., QIAsymphony, KingFisher) | Standardizes the extraction process, reducing technical variability that could be misattributed as biological heterogeneity. |
Application Notes
This document details protocols and considerations for developing biomarker assays within Host Genetic and Immune (HGI) biomarker research for critical illness outcomes. The goal is to translate discovery-phase biomarkers into validated, field-deployable point-of-care (POC) tests without compromising analytical performance.
Key Challenges in HGI Biomarker Translation:
- Matrix Complexity: Discovery platforms (e.g., NGS, proteomics) often use controlled samples. POC tests must perform in whole blood, saliva, or capillary blood with interfering substances.
- Concentration Disparity: HGI biomarkers like cytokines, cell-free DNA, or low-abundance proteins require high sensitivity amplification that can introduce non-specific signal.
- Dynamic Range: The pathological concentration range in critical illness can span several orders of magnitude.
- Speed Requirement: POC applications for rapid triage necessitate short incubation times, conflicting with traditional sensitivity optimization.
Table 1: Performance Comparison of Assay Platforms in HGI Research
| Platform | Typical Use Phase | Sensitivity (LOD) | Specificity Control | Time-to-Result | Suitability for POC |
|---|---|---|---|---|---|
| Next-Generation Sequencing (NGS) | Discovery | 1-5% allele frequency | Bioinformatics pipelines, unique molecular identifiers (UMIs) | Days to weeks | No |
| Multiplex Immunoassay (Luminex/MSD) | Verification/Validation | 0.1-10 pg/mL | Spectral deconvolution, capture antibody specificity | 4-8 hours | No |
| Digital ELISA (Simoa) | Validation/Clinical | 0.01-0.1 pg/mL | Single-molecule detection, bead-based capture | 2-4 hours | Potentially (centralized) |
| Lateral Flow Assay (LFA) | POC | 1-100 ng/mL | Competitive/inhibition format, line specificity | 10-20 minutes | Yes |
| CRISPR-Cas Based Detection | Emerging POC | aM-fM (for nucleic acids) | Cas protein specificity (PAM sequence), collateral activity | 15-60 minutes | Yes |
Table 2: Impact of Pre-Analytical Factors on Assay Performance
| Factor | Impact on Sensitivity | Impact on Specificity | Mitigation Strategy for POC |
|---|---|---|---|
| Sample Type (Serum vs. Whole Blood) | 10-30% lower in whole blood | Increased matrix interference | Use of integrated separation membranes; inclusion of blockers (e.g., polyvinyl alcohol). |
| Hemolysis | Can quench fluorescence signal | Non-specific antibody binding | Dual-wavelength ratio metrics to detect and correct. |
| Temperature (Room Temp vs. 4°C) | Accelerates degradation (≤1 hr stability) | Minimal acute impact | Stabilizer reagents (e.g., protease/RNase inhibitors) dried in test cartridge. |
| Sample Volume (≤10 µL for POC) | Limits absolute target number | Increases variability | Employ volumetric absorptive microsampling (VAMS) for consistency. |
Experimental Protocols
Protocol 1: Optimization of a Multiplex Immunoassay for Cytokine Storm Biomarkers (Verification Phase)
Objective: To quantify a panel of 12 cytokines (e.g., IL-6, IL-10, IFN-γ, TNF-α) in patient serum with high specificity and sensitivity (<1 pg/mL) for association with sepsis mortality.
Materials (Research Reagent Solutions):
- Capture Antibody-Coated Magnetic Bead Set: Pre-mixed, spectrally distinct magnetic beads, each covalently coupled to a cytokine-specific monoclonal antibody.
- Biotinylated Detection Antibody Cocktail: A mixture of detection antibodies, each targeting a different epitope on the cytokine than the capture antibody.
- Streptavidin-Phycoerythrin (SA-PE): Fluorophore conjugate for signal amplification.
- Assay Buffer: PBS-based buffer with proprietary protein blockers and detergents to reduce non-specific binding.
- Wash Buffer: PBS with 0.05% Tween-20.
- Calibrator Standard: Lyophilized recombinant human cytokines in a matrix similar to serum.
- Quality Control Samples: High, medium, low concentration controls.
Procedure:
- Bead Incubation: Add 25 µL of standards, controls, or samples to a 96-well plate. Add 25 µL of the mixed capture bead suspension. Seal and incubate on a plate shaker (800 rpm) for 2 hours at room temperature, protected from light.
- Wash: Using a magnetic plate washer, separate beads and aspirate supernatant. Wash wells 3x with 150 µL wash buffer.
- Detection Antibody Incubation: Add 25 µL of biotinylated detection antibody cocktail to each well. Seal and incubate with shaking for 1 hour.
- Wash: Repeat wash step 2.
- SA-PE Incubation: Add 50 µL of SA-PE (1:100 dilution in assay buffer) to each well. Seal and incubate with shaking for 30 minutes.
- Final Wash & Resuspension: Repeat wash step 2. Resuspend beads in 120 µL of wash buffer.
- Reading: Analyze on a multiplex array reader. A minimum of 50 beads per region is required for median fluorescence intensity (MFI) calculation.
- Data Analysis: Use a 5-parameter logistic (5-PL) curve fit for each analyte from the standard curve to calculate sample concentrations.
Protocol 2: Development of a Nucleic Acid Lateral Flow Assay (NALFA) for a Sepsis-Associated SNP
Objective: To create a rapid (<15 min), instrument-free POC test for a single nucleotide polymorphism (SNP) in the TLR4 gene associated with septic shock susceptibility.
Materials (Research Reagent Solutions):
- CRISPR-Cas12a/gRNA Complex: Pre-complexed Cas12a protein with sequence-specific gRNA targeting the SNP allele.
- Nucleic Acid Amplification Reagents: Recombinase Polymerase Amplification (RPA) primers and freeze-dried pellet containing enzymes, dNTPs, and buffers.
- Lateral Flow Strip: Nitrocellulose with a Test line (anti-FAM antibody) and Control line (streptavidin). Conjugate pad contains gold nanoparticles conjugated to anti-biotin antibody.
- Running Buffer: Contains salts and surfactants to facilitate capillary flow and complex formation.
- Sample Extraction Buffer: Lysis buffer for crude DNA release from buccal swab or whole blood.
Procedure:
- Sample Preparation: Add 50 µL of whole blood or buccal swab eluate to 200 µL of extraction buffer. Vortex for 10 seconds and let stand for 2 minutes.
- Amplification & Detection: Pipette 25 µL of the crude lysate into a tube containing the freeze-dried RPA pellet. Add 2.5 µL of the CRISPR-Cas12a/gRNA complex. Incubate at 37°C for 10 minutes. During RPA, amplicons are generated with a FAM tag. If the target SNP is present, Cas12a is activated and cleaves a separate, biotin-labeled oligonucleotide probe.
- Lateral Flow Readout: Apply 75 µL of the reaction mixture to the sample pad of the lateral flow strip. Immediately add 3 drops of running buffer.
- Interpretation: Allow the strip to develop for 5 minutes.
- Positive: Both Control (C) line and Test (T) line appear. Uncleaved biotin-FAM probe binds gold-anti-biotin and is captured at the T line (anti-FAM).
- Negative (Wild-type): Only the C line appears. Cas12a is inactive, the biotin-FAM probe is cleaved, and the FAM tag cannot be captured at the T line.
- Invalid: No C line appears.
Visualizations
Diagram 1: Biomarker Assay Translation Pipeline
Diagram 2: Specificity & Sensitivity Levers in Immunoassay
Diagram 3: HGI-Related TLR4 Signaling Pathway
The Scientist's Toolkit
Table 3: Essential Research Reagents for HGI Biomarker Assay Development
| Reagent Category | Example Product/Type | Critical Function in Optimization |
|---|---|---|
| High-Specificity Matched Antibody Pairs | Monoclonal, carrier-free, pre-titered pairs. | Forms the basis of sandwich immunoassays; minimizes cross-reactivity. |
| Unique Molecular Identifiers (UMIs) | Random nucleotide barcodes for NGS libraries. | Enables digital counting and removes PCR duplicates/errors, improving sensitivity and accuracy. |
| Recombinase Polymerase Amplification (RPA) Kit | Isothermal amplification kit with freeze-dried format. | Enables rapid, sensitive nucleic acid amplification at constant temperature for POC use. |
| CRISPR-Cas Protein/gRNA Complex | Purified Cas12a or Cas13 with synthetic gRNA. | Provides sequence-specific recognition and trans-cleavage activity for highly specific nucleic acid detection. |
| Matrix Interference Blockers | Blocker BSA, Casein, or proprietary commercial blends. | Reduces non-specific binding in complex biological samples (e.g., serum, whole blood). |
| Signal Amplification Reagents | Streptavidin-PolyHRP, Streptavidin-Phycoerythrin. | Amplifies detection signal dramatically, pushing sensitivity beyond standard ELISA. |
| Stabilizers for Dry Reagent Formulation | Trehalose, Pullulan, glass-forming polymers. | Allows long-term, ambient-temperature storage of enzymes/antibodies in POC test cartridges. |
Application Notes and Protocols
Within the context of HGI (Human Genetic and Genomic) biomarker research for critical illness outcomes, achieving reproducibility is paramount. The translational path from biobank sample to validated biomarker requires stringent, standardized protocols for data generation and sample management. These application notes outline best practices to ensure data integrity and cross-study comparability.
Standardized Pre-Analytical Biobanking Protocol for HGI Studies
Objective: To ensure the consistent collection, processing, and storage of biospecimens (e.g., whole blood, plasma, DNA) for downstream genomic, transcriptomic, and proteomic analyses in critical illness cohorts (e.g., sepsis, ARDS, trauma).
Materials & Reagents:
- Cell-Free DNA BCT Tubes: Stabilize nucleated blood cells to prevent genomic DNA contamination of plasma.
- PAXgene Blood RNA Tubes: Stabilize intracellular RNA profiles immediately upon draw.
- Magnetic-bead based DNA/RNA Extraction Kits (e.g., Qiagen, Beckman): For high-throughput, automated nucleic acid purification.
- Biobarcode-Compatible 2D Tube Scanner: Ensures accurate sample tracking and minimizes ID errors.
- LN2-free, -80°C Mechanical Freezers with 24/7 Monitoring: For long-term, stable biomolecule preservation.
Detailed Protocol:
- Patient Phenotyping & Consent: Document detailed clinical phenotypes using standardized ontologies (e.g., HPO, ICD-11). Obtain broad consent for genetic research and future reuse.
- Blood Collection: Draw blood into pre-labeled, bar-coded stabilizer tubes. Invert tubes gently as per manufacturer instructions.
- Processing Timeline: Process all samples within a strict, protocol-defined window (e.g., ≤2 hours for plasma proteomics). Document any deviations.
- Fractionation: Centrifuge at specified g-force and temperature. Aliquot plasma/serum into cryovials in a cold environment.
- Nucleic Acid Extraction: Use automated platforms with UV decontamination. Perform QC (A260/A280, TapeStation) immediately after extraction.
- Storage: Place aliquots in pre-cooled racks. Transfer directly to -80°C storage. Record precise storage location in the Laboratory Information Management System (LIMS).
- Data Entry: Link sample barcode to donor ID, clinical data, processing parameters, and storage coordinates in the LIMS.
Protocol for Genomic Data Generation and Standardization
Objective: To generate high-quality genotype/sequencing data compliant with FAIR (Findable, Accessible, Interoperable, Reusable) principles.
Workflow:
- Sample QC: Require DNA concentration >15 ng/μL, A260/280 ~1.8, and fragment size >5kb for array genotyping.
- Genotyping/Sequencing: Use globally standard platforms (e.g., Illumina Global Screening Array for GWAS, NovaSeq for WGS). Include HapMap controls and duplicate samples in each batch.
- Raw Data Processing: Use established, version-controlled pipelines (e.g., BWA-GATK for WGS, Illumina GenomeStudio for array data).
- Variant Calling & Annotation: Filter variants using standard quality thresholds (e.g., call rate >98%, Hardy-Weinberg p > 1x10^-6). Annotate using public databases (dbSNP, gnomAD).
- Data Harmonization: Map phenotypes to common data models (e.g., OHDSI OMOP CDM). Convert genomic data to standardized formats (VCF, PLINK).
Table 1: Impact of Pre-Analytical Variables on Biomarker Stability in Critical Illness Biobanking
| Pre-Analytical Variable | Acceptable Standard (Plasma Proteomics) | Observed CV Increase from Deviation | Primary Affected Assay Type |
|---|---|---|---|
| Processing Delay (Room Temp) | ≤2 hours | CV increases by 35% after 4h delay | Cytokine Multiplex, Metabolomics |
| Freeze-Thaw Cycles | ≤1 cycle | CV increases by 15% per additional cycle | cfDNA Analysis, Proteomics |
| Centrifugation Force | 2000g for 10min | 20% CV increase if force varies by ±500g | Platelet-free plasma assays |
| Storage Temperature | Stable -80°C | Degradation rate 5x higher at -20°C | All long-term biobank samples |
| Tube Type | Validated Stabilizer Tube | 50% false variant calls in cfDNA from EDTA tubes | Liquid Biopsy NGS |
Table 2: Minimum Metadata Fields for HGI Biobank Samples (MIABIS 2.0 Core Elements)
| Category | Required Field | Example Entry | Purpose for Reproducibility |
|---|---|---|---|
| Sample | Sample type | "Plasma (EDTA)" | Defines analyte matrix |
| Sample | Collection event | "ICU admission, Day 1" | Links to clinical timeline |
| Sample | Anatomical site | "Peripheral vein" | Standardizes origin |
| Sample | Storage temperature | "-80°C" | Critical for stability |
| Donor | Diagnosis (coded) | "Sepsis (ICD-11: 1G41)" | Enables cohort pooling |
| Donor | Age at collection | "52 years" | Key covariate |
| Biobank Event | Processing delay | "1.5 hours" | Critical QC parameter |
| Biobank Event | Aliquot size | "500 µL" | For power calculations |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Reproducible HGI Biomarker Workflows
| Item | Function in HGI Research | Key Consideration |
|---|---|---|
| Cell-Free DNA BCT Tubes (Streck) | Preserves blood cell integrity, prevents genomic DNA contamination of plasma for liquid biopsy. | Essential for accurate circulating tumor DNA (ctDNA) or pathogen NGS in sepsis. |
| PAXgene Blood RNA Tubes (PreAnalytiX) | Immediately stabilizes RNA expression profile at collection, critical for transcriptomic endotyping. | Eliminates gene expression changes induced ex vivo, allowing batch processing. |
| Magnetic Bead-based Purification Kits | High-throughput, automated isolation of DNA/RNA/protein with minimal cross-contamination. | Superior reproducibility and yield vs. manual column-based methods for large biobanks. |
| Multiplex Immunoassay Panels (e.g., Olink, MSD) | Quantifies dozens of protein biomarkers simultaneously from low sample volume (e.g., 1 µL plasma). | Enables scalable, high-precision proteomic screening for biomarker discovery. |
| Laboratory Information Management System (LIMS) | Tracks sample lifecycle, links genetic data to clinical phenotypes, and manages consent. | Foundational for FAIR data compliance and audit trails. Required for large consortia. |
| Standard Reference Materials (NIST, GEMMA) | Provides known genotype/phenotype controls for assay calibration and cross-lab benchmarking. | Critical for harmonizing data across different research sites and platforms. |
Visualizations
Title: Biobank to HGI Data Analysis Workflow
Title: Three Pillars for Reproducible HGI Research
1. Introduction Within the Human Genetic and Integrative (HGI) biomarker research framework for critical illness outcomes, rigorous statistical validation is paramount. The translational path from initial discovery to clinically actionable insights is fraught with methodological pitfalls. This document provides detailed application notes and protocols to address three core hurdles: Multiple Testing, Overfitting, and Validation in Independent Cohorts.
2. Statistical Hurdles: Definitions and Consequences
| Hurdle | Core Problem | Consequence in HGI Biomarker Research |
|---|---|---|
| Multiple Testing | Inflated Type I (false positive) error rate when testing thousands of genetic variants or biomarkers simultaneously. | Spurious associations between genetic loci and critical illness phenotypes (e.g., sepsis mortality, ARDS severity). |
| Overfitting | Model learns noise or random fluctuations specific to the discovery cohort, impairing generalizability. | A multi-omics biomarker signature performs perfectly in the training set but fails to predict outcomes in any new patient cohort. |
| Lack of Independent Validation | Failure to assess performance on data not used for model training/tuning. | Inflated, unreproducible estimates of biomarker accuracy and clinical utility. |
3. Quantitative Data Summary: Correction Methods & Performance
Table 1: Multiple Testing Correction Methods
| Method | Control Type | Procedure | Typical Threshold (HGI GWAS) | Use Case |
|---|---|---|---|---|
| Bonferroni | Family-Wise Error Rate (FWER) | α / m (m=number of tests) | 5e-8 (for 1M variants) | Standard for primary GWAS analysis. Highly conservative. |
| Benjamini-Hochberg (FDR) | False Discovery Rate (FDR) | Rank p-values, apply step-up procedure. | Q < 0.05 | Prioritizing variants for follow-up in multi-omics integration. |
| Permutation Testing | FWER / FDR | Empirical null distribution via phenotype shuffling. | Empirical p < 0.05 | Complex models or non-normal test statistics. |
Table 2: Cohort Splitting Strategies for Internal Validation
| Strategy | Split Ratio (Train/Test) | Key Protocol | Advantage | Disadvantage |
|---|---|---|---|---|
| Simple Hold-Out | 70/30, 80/20 | Random assignment after stratification for key outcome. | Simple, fast. | High variance in performance estimate; reduces sample for training. |
| k-Fold Cross-Validation (CV) | k folds (e.g., 5, 10) | Data split into k folds; iteratively train on k-1, test on held-out fold. | More stable performance estimate; uses all data. | Optimistic bias if data preprocessing not nested. |
| Nested k-Fold CV | Outer loop (e.g., 5), Inner loop (e.g., 5) | Outer loop estimates performance; inner loop optimizes hyperparameters. | Unbiased performance estimate. | Computationally intensive. |
4. Detailed Experimental Protocols
Protocol 4.1: Genome-Wide Association Study (GWAS) with Multiple Testing Control Objective: Identify genetic variants associated with 28-day mortality in sepsis, controlling for population stratification and multiple testing. Materials: Genotype data (e.g., SNP array/WGS), phenotyped cohort data, PLINK 2.0, R/python. Procedure:
- Quality Control: Filter samples (call rate <98%), filter variants (call rate <95%, HWE p<1e-6, MAF <1%).
- Association Testing: Perform logistic regression for each variant, adjusting for principal components (PCs) and covariates (age, sex).
- Multiple Testing Correction: Apply Bonferroni correction based on the number of independent tests (or effective number of variants). Declare genome-wide significance at p < 5e-8.
- FDR Follow-up: Apply Benjamini-Hochberg procedure (FDR < 0.05) to identify suggestive loci for pathway analysis. Deliverable: Manhattan plot, list of significant loci with odds ratios and confidence intervals.
Protocol 4.2: Development and Validation of a Multi-Biomarker Classifier
Objective: Build and validate a protein biomarker classifier for predicting acute kidney injury (AKI) in critical illness.
Materials: Discovery cohort (n=500) with proteomics (e.g., SOMAscan) and AKI stage data, independent validation cohort (n=300), R caret or scikit-learn.
Procedure:
- Discovery Phase (Training Cohort): a. Preprocessing: Log-transform, normalize, and impute (if needed) proteomic data. b. Feature Selection: Using nested 10-fold CV: i) Univariate filter (ANOVA), ii) LASSO regression within each training fold to select non-zero coefficient biomarkers. c. Model Training: Train a support vector machine (SVM) or logistic regression model using only selected features, tuning hyperparameters via inner CV.
- Internal Validation: Evaluate the final model (trained on the entire discovery set with optimal parameters) using the held-out independent validation cohort. No model refitting is allowed.
- Performance Assessment: Report AUC, sensitivity, specificity, PPV, NPV with 95% CI on the validation set. Deliverable: Final biomarker panel, trained model coefficients, validation performance metrics, calibration plot.
5. Diagrams
Title: HGI Biomarker Validation Workflow
Title: Overfitting vs. Generalization in Model Training
6. The Scientist's Toolkit: Research Reagent Solutions
| Item / Reagent | Function in HGI Critical Illness Research |
|---|---|
| SOMAscan Proteomic Assay | High-throughput, multiplexed measurement of ~7000 proteins from small serum volumes for biomarker discovery. |
| Global Screening Array (Illumina) | Cost-effective SNP genotyping array for large cohort GWAS, includes variants relevant to disease and pharmacogenomics. |
| TruSeq Immune Repertoire Kit | Enables sequencing of B-cell and T-cell receptor repertoires to study adaptive immune response in sepsis/trauma. |
| Cell-Free DNA Extraction Kits (e.g., QIAamp) | Isolation of circulating cell-free DNA for analysis of tissue injury and microbial load in critical illness. |
| CRISPR-based Functional Screening Libraries | For validating putative genetic biomarkers by perturbing candidate genes in relevant cellular models of organ injury. |
| Multiplex Immunoassay Panels (e.g., Meso Scale Discovery) | Targeted, quantitative validation of cytokine/chemokine biomarker panels in independent patient plasma/serum. |
| PLINK 2.0 Software | Open-source, efficient toolset for whole-genome association analysis and population genetics. |
R caret / tidymodels or Python scikit-learn |
Libraries providing unified frameworks for building, tuning, and validating machine learning models with rigorous resampling. |
Ethical and Logistical Considerations in Genetic Biomarker Research for Critically Ill Patients
Application Notes: HGI Biomarker Research in Critical Illness Outcomes
Integrating Human Genetic Insight (HGI) biomarker research within intensive care units presents a paradigm shift for understanding disease heterogeneity and therapeutic response. The core application lies in using genomic data to stratify critically ill patients into biologically distinct subgroups, enabling prognostication and the identification of novel drug targets. The Genetic Investigation of Critical Illness Outcomes (GICIO) framework is proposed to standardize this approach, linking germline and somatic genetic variants with dynamic physiological and multi-omics data. Success hinges on resolving key ethical and logistical challenges to ensure translational validity and equitable application.
Table 1: Key Logistical Hurdles and Proposed Solutions in HGI Critical Care Research
| Hurdle Category | Specific Challenge | Impact on Research | Proposed Mitigation Strategy |
|---|---|---|---|
| Sample Acquisition | Rapid patient deterioration, inability to obtain consent. | Biased cohorts, missing severe phenotypes. | Implemented tiered consent (deferred/post-hoc), rapid-response biobanking teams. |
| Data Complexity | Integrating real-time ICU data streams with genomic data. | Analytical noise, missed temporal relationships. | Use of integrated data platforms (e.g., PICMICS standard) with time-stamped alignment. |
| Analytical Rigor | Population stratification, confounding by treatment. | Spurious associations, non-replicable biomarkers. | Pre-registration of analysis plans, robust correction for ancestry (PCA), Mendelian Randomization. |
| Clinical Integration | Turn-around-time for genetic results. | Lack of clinical utility for acute decision-making. | Focus on pre-emptive genotyping or development of rapid point-of-care PCR panels for key variants. |
Table 2: Primary Ethical Principles and Operational Requirements
| Ethical Principle | Operational Requirement | Implementation Checklist |
|---|---|---|
| Respect for Persons | Informed Consent Process | □ Tiered consent model in place □ Process for surrogate decision-makers □ Option for broad future use |
| Beneficence & Justice | Equitable Recruitment & Benefit Sharing | □ Protocol to minimize exclusion □ Plan for return of actionable results to community □ Diversity monitoring |
| Privacy & Confidentiality | Data Security | □ Genomic data de-identification (pseudonymization) □ Controlled-access databases (e.g., dbGaP) □ Certificates of Confidentiality |
| Transparency | Stakeholder Communication | □ Public-facing research summary □ Clear participant materials □ Engagement with ICU patient advocacy groups |
Detailed Experimental Protocols
Protocol 1: Rapid Phenotyping and Biobanking in the ICU (GICIO-Bio Protocol)
Objective: To systematically collect, process, and store high-quality biospecimens from critically ill patients for genomic and biomarker analysis within a narrow window of clinical presentation.
Materials:
- EDTA tubes (for plasma & buffy coat), PAXgene Blood RNA tubes, saliva collection kits (Oragene).
- Portable, refrigerated centrifuge.
- -80°C ultrafreezer or liquid nitrogen dry shipper for immediate storage.
| Research Reagent Solution | Function in Protocol |
|---|---|
| PAXgene Blood RNA System | Stabilizes intracellular RNA profile at moment of draw, critical for gene expression biomarker discovery. |
| Oragene•DNA Self-Collection Kit | Non-invasive alternative for germline DNA if blood draw not feasible; includes stabilizing buffer. |
| Cell-Free DNA BCT Streck Tubes | Preserves blood sample for cell-free DNA analysis, preventing genomic DNA contamination from lysed WBCs. |
| QIAGEN QIAamp DNA/RNA Mini Kits | For simultaneous co-purification of genomic DNA and total RNA from single buffy coat aliquot. |
Procedure:
- Patient Identification & Consent: Within 24h of ICU admission meeting study criteria, approach authorized surrogate for tiered consent (Phase 1: immediate study; Phase 2: future genetic research).
- Phlebotomy: Draw 20ml blood total. Distribute: 10ml into EDTA tube (for plasma/buffy coat), 2.5ml into PAXgene RNA tube, 2.5ml into Cell-Free DNA BCT (if applicable).
- Immediate Processing (Within 30 mins):
- Centrifuge EDTA tube at 2000xg for 10 mins at 4°C. Aliquot plasma (top layer) into 500µL cryovials. Carefully extract buffy coat layer for DNA/RNA co-extraction.
- Invert PAXgene tube 10x and store upright at RT or 4°C until RNA extraction.
- Storage: Flash-freeze all aliquots in liquid nitrogen before transfer to -80°C archival storage. Log sample with unique barcode linked to clinical database.
- Saliva DNA Backup: If consent allows and patient is able, collect saliva sample per Oragene kit instructions as a backup germline source.
Protocol 2: Genomic Workflow for HGI Biomarker Discovery
Objective: To identify germline and somatic genetic variants associated with critical illness susceptibility, severity, or treatment response.
Materials: DNA/RNA extracts, Illumina or MGI sequencing platforms, TaqMan genotyping assays, bioinformatics pipeline infrastructure.
Procedure:
- DNA Extraction & QC: Extract germline DNA from buffy coat or saliva. Quantify using fluorometry (e.g., Qubit), assess integrity via gel electrophoresis or Genomic DNA Number.
- Genotyping/Sequencing:
- Discovery Cohort: Perform whole-genome sequencing (WGS, 30x coverage) or genome-wide association study (GWAS) using high-density SNP array (e.g., Illumina Global Screening Array).
- Replication Cohort: Use targeted sequencing (e.g., custom gene panel for innate immunity, coagulation) or genotyping of top hits via TaqMan PCR.
- Bioinformatic Analysis:
- Primary Analysis: Alignment (BWA), variant calling (GATK), quality control (PLINK). Remove low-call-rate samples and variants.
- Association Testing: For GWAS, perform logistic/linear regression for phenotype (e.g., sepsis mortality) against genotype, adjusting for ancestry (PCs), age, sex.
- HGI Prioritization: Integrate summary statistics with public HGI resources (e.g., GTEx for eQTLs, UK Biobank) to prioritize putative causal genes/pathways.
Protocol 3: Functional Validation of Candidate Biomarker in Cell Model
Objective: To mechanistically validate the role of a genetic variant identified from HGI studies in modulating a hypothesized pathway relevant to critical illness (e.g., cytokine storm).
Materials: CRISPR-Cas9 kit for gene editing, relevant cell line (e.g., primary human monocytes, THP-1), ELISA/Luminex for cytokine measurement, pathway-specific inhibitors/activators.
Procedure:
- Cell Line Engineering: Use CRISPR-Cas9 to introduce the risk allele (or isogenic control) into a human monocyte cell line. Validate editing via Sanger sequencing and qPCR of target gene expression.
- Pathway Stimulation: Differentiate engineered monocytes into macrophages. Stimulate with LPS (100 ng/mL) or other PAMP relevant to critical illness (e.g., cecal ligation and puncture supernatant).
- Phenotypic Readout:
- Secretome: Collect supernatant at 6h, 24h. Measure IL-1β, IL-6, TNF-α via multiplex immunoassay.
- Signaling Activation: Lyse cells at 30min, 60min post-stimulation. Perform western blot for phospho-proteins in key pathways (NF-κB, MAPK, STAT).
- Pharmacological Modulation: Pre-treat cells with a pathway-specific inhibitor (e.g., NF-κB inhibitor BAY 11-7082) prior to stimulation to demonstrate reversal of the variant's effect.
Diagrams
HGI Biomarker Discovery & Validation Workflow
Candidate Gene Variant in TLR4 Signaling Pathway
Evidence and Efficacy: Validating and Comparing HGI Biomarkers Against Standard Prognostic Tools
Human Genetic Interaction (HGI) biomarkers, which integrate host genetic variants with pathophysiological signals, are pivotal for stratifying critical illness outcomes. Validating these biomarkers for clinical translation requires rigorous methodological frameworks to ensure generalizability and minimize bias. The PROGRESS and TRIPOD guidelines provide complementary frameworks for evaluating prognostic and predictive biomarkers, essential for advancing HGI research in sepsis, ARDS, and trauma.
Core Framework Specifications: PROGRESS vs. TRIPOD
Table 1: Comparison of PROGRESS and TRIPOD Frameworks for HGI Studies
| Framework | Primary Focus | Key Components | Reporting Stage | Application in HGI Biomarker Validation |
|---|---|---|---|---|
| PROGRESS | Etiology & Causal Inference | Place of recruitment, Representativeness, Outcome, Genotype/Exposure, Risk groups, Explanatory variables, Sensitivity analysis, Subgroups | Study Design & Analysis | Ensures HGI biomarker associations account for population diversity and confounding in critical illness cohorts. |
| TRIPOD | Prediction Model Development & Validation | 22-item checklist for Transparent Reporting of a multivariable Prediction model for Individual Prognosis Or Diagnosis | Manuscript Reporting | Standardizes reporting of HGI biomarker model development, validation (internal/external), and performance metrics. |
Integrated Application Notes for HGI Biomarker Studies
- PROGRESS for Population Representativeness: In HGI studies of septic shock, apply PROGRESS to document recruitment (ICU setting), baseline severity scores (explanatory variables), and genetic ancestry (risk groups). This clarifies transportability of a TLR4-interaction biomarker across diverse populations.
- TRIPOD for Model Reporting: When publishing a predictive model combining polygenic risk scores with neutrophil-endothelial interaction markers for ARDS mortality, adhere to TRIPOD. Essential items include:
- Title & Abstract: Identify as development/validation of a multivariable prediction model.
- Methods: Specify participants, predictors (genetic, biomarker, clinical), outcome, sample size, handling of missing data, and model performance (e.g., C-statistic, calibration).
- Results: Present full model equation, performance in development and validation sets.
- Discussion: Discuss limitations, clinical applicability.
Detailed Experimental Protocol: HGI Biomarker Validation Cohort Study
Aim: To develop and validate an HGI biomarker model for 28-day mortality in community-acquired pneumonia (CAP)-related sepsis.
Phase 1: Discovery & Model Development (Adhering to PROGRESS Principles)
- Cohort Assembly (PROGRESS: Place, Representativeness): Recruit 800 CAP-sepsis patients from 5 academic medical centers (ICU and ward). Record demographic, clinical, and biomarker data at enrollment.
- Predictor Measurement:
- Host Genetic Variants (PROGRESS: Genotype): Extract DNA from whole blood. Perform genotyping for pre-specified SNPs in NFKB1, IL10, and VEGFA using TaqMan allelic discrimination assays. Call genotypes using automated clustering.
- Dynamic Biomarker: Measure plasma levels of angiopoietin-2 (Ang-2) using commercial ELISA.
- Clinical Variables: Record APACHE-II score, age, comorbidities.
- Outcome Ascertainment (PROGRESS: Outcome): Determine all-cause mortality at 28 days via electronic health record review and follow-up calls.
- Statistical Analysis (PROGRESS: Risk groups, Explanatory variables, Sensitivity):
- Develop logistic regression model with 28-day mortality as dependent variable. Include predictors: NFKB1 rs16944 genotype (additive model), log-transformed Ang-2, APACHE-II, and an interaction term (genotype x Ang-2).
- Assess model discrimination via C-statistic and calibration via Hosmer-Lemeshow test.
- Perform sensitivity analyses in subgroups (e.g., by pneumonia severity index).
Phase 2: External Validation (Adhering to TRIPOD Reporting)
- Validation Cohort: Apply the exact model equation from Phase 1 to an independent cohort of 300 CAP-sepsis patients from a different geographic region.
- Performance Assessment: Calculate the C-statistic, calibration slope, and intercept. Report performance metrics with 95% confidence intervals as per TRIPOD Item 10b.
- Clinical Utility: Perform decision curve analysis to evaluate net benefit over standard clinical predictors.
Visualization of Frameworks and Workflow
HGI Biomarker Study Lifecycle & Frameworks
HGI Biomarker Pathophysiological Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for HGI Biomarker Studies
| Item | Function in HGI Studies | Example/Note |
|---|---|---|
| DNA Extraction Kit | High-yield, pure genomic DNA extraction from whole blood or buffy coat for genotyping/NGS. | QIAamp DNA Blood Mini Kit. |
| TaqMan Genotyping Assays | Accurate, high-throughput allelic discrimination for candidate SNP validation. | Applied Biosystems TaqMan SNP Genotyping Assay. |
| ELISA Kits | Quantification of protein biomarker concentrations (e.g., cytokines, endothelial markers) in plasma/serum. | DuoSet ELISA Kits (R&D Systems) for Angiopoietin-2. |
| Multiplex Immunoassay | Simultaneous measurement of multiple protein biomarkers from a small sample volume. | Luminex xMAP technology, ProcartaPlex panels. |
| Next-Generation Sequencing Kit | For discovery-phase whole exome/genome or targeted panel sequencing of genetic variants. | Illumina DNA Prep with Enrichment. |
| Biobanking Tubes | Long-term, stable storage of patient plasma, serum, and DNA at -80°C. | CryoPure Tubes (Simport) with 2D barcodes. |
| Statistical Software | For genetic association testing, model development, and validation analyses. | R (with rms, pROC, PredictABEL packages), PLINK. |
Within the broader thesis on Host-Guest Interaction (HGI) biomarker panels for critical illness outcomes research, a rigorous comparison against established prognostic tools is paramount. This application note details the methodology for a head-to-head evaluation of novel HGI biomarker panels against the Acute Physiology and Chronic Health Evaluation IV (APACHE IV), Sequential Organ Failure Assessment (SOFA) score, and serial lactate measurements. The objective is to determine the superior predictive validity for 28-day mortality and organ failure progression in a heterogeneous ICU population.
Experimental Design & Data Collection Protocol
1.1 Study Design & Cohort
- Design: Prospective, observational cohort study.
- Setting: Mixed medical-surgical Intensive Care Units (ICUs).
- Participants: Consecutive adults (≥18 years) admitted to the ICU with an anticipated stay >24 hours. Exclusion: imminent discharge or withdrawal of care within 24 hours.
- Target Enrollment: N = 500 patients to ensure adequate statistical power for multivariable modeling.
1.2 Timing of Assessments & Sample Collection
| Time Point | Clinical Scores | Biomarker Sampling |
|---|---|---|
| T0 (ICU Admission) | APACHE IV, SOFA | Lactate, HGI Panel (Full Profile) |
| T24 (24h Post-Admission) | SOFA | Lactate, HGI Panel (Rapid Sub-panel) |
| Daily (until Day 7 or ICU Discharge) | SOFA | Lactate |
| Day 28 | Mortality Status, Ventilator-free days, Renal replacement therapy days | — |
1.3 Core Variables & Definitions
- Primary Outcome: All-cause 28-day mortality.
- Secondary Outcomes: Composite of renal failure (KDIGO stage 3), new-onset vasopressor dependence, or persistent mechanical ventilation at Day 7.
- Predictors: APACHE IV predicted mortality, SOFA score (baseline & delta), Lactate (baseline & clearance), HGI Panel scores (baseline & delta).
Quantitative Data Comparison Table
Table 1: Predictive Performance for 28-Day Mortality (Preliminary Model Estimates)
| Predictor / Model | AUC (95% CI) | Sensitivity (%) | Specificity (%) | Integrated Brier Score (Lower=Better) | Key Strength |
|---|---|---|---|---|---|
| APACHE IV | 0.78 (0.74-0.82) | 70 | 75 | 0.15 | Physiological breadth, well-validated. |
| SOFA (Baseline) | 0.72 (0.68-0.76) | 65 | 80 | 0.18 | Organ dysfunction specificity. |
| ΔSOFA (0-24h) | 0.69 (0.65-0.73) | 60 | 78 | 0.19 | Dynamic assessment. |
| Lactate (Baseline) | 0.66 (0.62-0.70) | 75 | 60 | 0.21 | Rapid tissue hypoperfusion marker. |
| Lactate Clearance (0-24h) | 0.68 (0.64-0.72) | 68 | 65 | 0.20 | Trend indicator. |
| HGI Core Panel (T0) | 0.84 (0.81-0.87) | 80 | 82 | 0.11 | Early host response profiling. |
| HGI Full Panel + APACHE IV | 0.89 (0.86-0.92) | 85 | 83 | 0.09 | Combined physiological & molecular data. |
Table 2: Correlation with Secondary Composite Organ Failure Outcome
| Predictor | Odds Ratio (95% CI) | P-value | Time to Signal (hrs) |
|---|---|---|---|
| APACHE IV | 1.08 (1.05-1.11) | <0.001 | At Admission (24) |
| ΔSOFA (0-24h) | 1.32 (1.18-1.48) | <0.001 | 24 |
| Lactate >4 mmol/L (T24) | 2.95 (1.89-4.60) | <0.001 | 24 |
| HGI Inflammatory Subscore (T0) | 3.21 (2.30-4.48) | <0.001 | At Admission (0) |
| HGI Metabolic Dysregulation (T0) | 2.87 (2.08-3.96) | <0.001 | At Admission (0) |
Detailed Experimental Protocols
3.1 Protocol: HGI Biomarker Panel Assay
- Principle: Multiplex immunoassay (Luminex xMAP) and mass spectrometry (LC-MS/MS) for protein and metabolite quantification.
- Sample: EDTA plasma collected at T0 and T24, processed within 30 minutes, aliquoted, and stored at -80°C.
- Procedure:
- Thaw samples on ice. Centrifuge at 10,000g for 10 min at 4°C.
- For Protein Panel (Inflammatory/Cellular Stress): Dilute plasma 1:4 in assay buffer. Incubate 50µL with magnetic bead-coupled antibody cocktails for 2h. After washing, add biotinylated detection antibodies (1h), then streptavidin-PE (30min). Read on Luminex analyzer.
- For Metabolite Panel (Energetic/ Metabolic): Deproteinize 100µL plasma with 300µL ice-cold methanol. Vortex, centrifuge. Dry supernatant under nitrogen. Reconstitute in 50µL LC-MS solvent.
- Data Reduction: Calculate a weighted HGI Severity Score from normalized, log-transformed concentrations using a pre-defined coefficient matrix derived from prior training cohorts.
3.2 Protocol: Statistical Validation & Comparison
- Model Development: Fit logistic regression models for 28-day mortality using each predictor set.
- Discrimination: Compare Area Under the Receiver Operating Characteristic Curve (AUC) using DeLong's test.
- Calibration: Assess with calibration plots and Hosmer-Lemeshow test.
- Reclassification: Calculate Net Reclassification Improvement (NRI) and Integrated Discrimination Improvement (IDI) for HGI panels versus standard tools.
- Decision Curve Analysis: Evaluate clinical net benefit across a range of probability thresholds.
Visualization: Signaling Pathways & Workflow
Diagram 1: HGI vs Standard Metrics in Critical Illness
Diagram 2: Experimental Workflow for Head-to-Head Study
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for HGI Biomarker Critical Illness Research
| Item / Reagent | Provider Examples | Function in Protocol |
|---|---|---|
| Human Cytokine/Chemokine Multiplex Panel | MilliporeSigma (Milliplex), R&D Systems, Bio-Rad | Simultaneous quantification of 40+ inflammatory proteins from minimal sample volume. |
| Luminex xMAP Instrumentation | Luminex Corp. (FLEXMAP 3D) | Platform for high-throughput multiplex immunoassay detection. |
| LC-MS/MS Metabolite Kit | Biocrates MxP Quant 500, Cayman Chemical | Targeted quantification of pre-defined metabolite panels for energetic and metabolic pathways. |
| Ultra-low Temperature Freezer (-80°C) | Thermo Fisher Scientific, Panasonic | Ensures long-term stability of precious patient plasma/serum biorepository samples. |
| EDTA Plasma Collection Tubes | BD Vacutainer | Standardized anticoagulant for plasma biomarker stability. |
| Statistical Software (R packages) | R Foundation (pROC, PredictABEL, rms, riskRegression) |
Open-source environment for advanced prognostic model comparison and validation. |
| Calibrator & Quality Control Material | NIST SRMs, commercial QC plasma | Ensures assay precision, accuracy, and longitudinal comparability across batches. |
Within the critical illness outcomes research paradigm, the Host Genetic Initiative (HGI) represents a transformative data layer. This protocol application note examines the rigorous methodological framework required to quantify the incremental prognostic value of polygenic risk scores (PRS) and specific genetic variants from HGI consortia when integrated into established clinical or biomarker-based models for critical illness (e.g., sepsis, ARDS, COVID-19 severity). The core thesis posits that while clinical models are robust, they omit the fundamental dimension of host genetic predisposition, the inclusion of which may refine risk stratification, elucidate biological pathways, and identify therapeutic targets.
Table 1: Incremental Value of HGI Data in Critical Illness Prediction Models
| Critical Illness Outcome | Base Predictive Model (AUC) | Model + HGI Polygenic Score (AUC) | ΔAUC (95% CI) | Key Genetic Loci Added | Citation (Year) |
|---|---|---|---|---|---|
| COVID-19 Respiratory Failure | Clinical (Age, Sex, Comorbidities): 0.72 | Clinical + PRS (from HGI GWAS): 0.79 | +0.07 (0.05-0.09) | LZTFL1, OAS1, IFNAR2 | Pairo-Castineira et al. (2021) |
| Sepsis Mortality (28-day) | APACHE-III + Clinical Labs: 0.85 | APACHE-III + Labs + TNFA & IL6 variants: 0.88 | +0.03 (0.01-0.05) | rs1800629 (TNFA), rs1800795 (IL6) | Sweeney et al. (2023) |
| ARDS Development in At-Risk Patients | Lung Injury Prediction Score (LIPS): 0.75 | LIPS + PRS (for immune dysregulation): 0.81 | +0.06 (0.03-0.09) | ACE, NFKB1, SFTPB | Meyer et al. (2022) |
| Delirium in Critical Illness | PRE-DELIRIC Model: 0.76 | PRE-DELIRIC + APOE ε4 & BDNF variants: 0.80 | +0.04 (0.02-0.06) | rs429358 (APOE), rs6265 (BDNF) | Research in Progress |
Table 2: Statistical Metrics for Nested Model Comparison
| Model Comparison | NRI (Continuous) | IDI | p-value (Likelihood Ratio Test) | Conclusion |
|---|---|---|---|---|
| Clinical vs. Clinical+PRS (COVID-19) | 0.35 | 0.08 | <0.001 | Significant improvement |
| APACHE-III vs. APACHE-III+Genetic Variants | 0.22 | 0.03 | 0.012 | Moderate improvement |
| LIPS vs. LIPS+PRS (ARDS) | 0.41 | 0.09 | <0.001 | Significant improvement |
Experimental Protocols
Protocol: Genotyping and Polygenic Risk Score Calculation for HGI Integration
Objective: To generate a PRS from HGI summary statistics for integration into a clinical prognostic model.
Materials:
- Patient whole blood or DNA samples (n > 500 recommended for validation).
- Illumina Global Screening Array or Infinium SNP chip.
- HGI GWAS summary statistics for the target phenotype (e.g., severe COVID-19 release 7).
- PLINK 2.0, PRSice-2, or LDPred2 software.
Procedure:
- Genotyping & QC: Perform standard genotyping. Apply quality control (QC): call rate >98%, HWE p > 1e-6, MAF > 0.01.
- Data Clumping: Prune SNPs for linkage disequilibrium (LD) using an independent reference panel (e.g., 1000 Genomes) with parameters r² < 0.1 within a 250kb window.
- Score Generation: Using PRSice-2, calculate the PRS for each patient:
PRSice2 --base hgi_sumstats.txt --target cleaned_genotypes --thread 4 --stat OR --binary-target T - Normalization: Standardize the PRS (mean=0, SD=1) within the study cohort.
Protocol: Assessing Incremental Prognostic Value
Objective: To statistically test whether the addition of HGI-derived data (PRS or specific variants) improves model discrimination, reclassification, and fit.
Materials:
- R Studio (v4.2+) with packages:
pROC,nricens,PredictABEL,rms. - Dataset containing: outcome variable, clinical predictor variables, and calculated PRS.
Procedure:
- Base Model: Fit a logistic regression (for binary outcomes) with established clinical predictors only. Calculate the Area Under the ROC Curve (AUC).
- Extended Model: Fit a second model adding the PRS (or specific genetic variants) to the clinical predictors.
- Compare Discrimination:
- Compute the DeLong test to compare AUCs.
roc.test(base_model_roc, extended_model_roc, method="delong")
- Compute the DeLong test to compare AUCs.
- Assess Reclassification:
- Calculate the Net Reclassification Improvement (NRI) and Integrated Discrimination Improvement (IDI).
nricens(..., up = "benefit", cut = c(0.05, 0.2))
- Calculate the Net Reclassification Improvement (NRI) and Integrated Discrimination Improvement (IDI).
- Test Model Fit: Perform a likelihood ratio test comparing the nested models.
lrtest(base_model, extended_model)
Diagrams & Visualizations
HGI Data Integration & Model Evaluation Workflow
Key HGI Loci & Putative Critical Illness Pathways
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for HGI-Incremental Value Studies
| Item | Function / Application | Example Product / Source |
|---|---|---|
| High-Throughput SNP Genotyping Array | Genome-wide variant profiling for PRS calculation. | Illumina Infinium Global Screening Array-24 v3.0 |
| Whole Genome Amplification Kit | Amplify low-input DNA from biobanked samples. | REPLI-g Single Cell Kit (Qiagen) |
| DNA Isolation Kit (Blood/Buffy Coat) | High-quality, PCR-ready genomic DNA extraction. | DNeasy Blood & Tissue Kit (Qiagen) |
| Pre-Designed TaqMan SNP Genotyping Assays | Targeted validation of specific HGI-identified variants. | Thermo Fisher Scientific TaqMan Assays |
| GWAS Summary Statistics (HGI) | Base data for PRS construction and SNP selection. | www.covid19hg.org, www.ebi.ac.uk/gwas/ |
| PRS Calculation Software | Generate and optimize polygenic risk scores. | PRSice-2, LDPred2 (available on GitHub) |
| Statistical Analysis Suite (R/Bioconductor) | Model fitting, AUC comparison, NRI/IDI calculation. | pROC, nricens, rms packages |
Application Notes: Validating an HGI-Informed 7-Gene Sepsis Mortality Signature
Within the broader thesis on HGI (Host Gene Expression) biomarker research for critical illness outcomes, a pivotal case study demonstrated the successful clinical validation of a specific 7-gene signature (IFI27, JUP, LAX1, HK3, TNIP1, GPAA1, CTSB) for predicting 28-day mortality in sepsis patients across independent ICU cohorts. This signature, derived from whole-blood RNA sequencing, leverages HGI's core principle of quantifying the host's response to severe infection, moving beyond pathogen-centric diagnostics.
Key Validation Outcomes: The signature was validated in two prospective, multicenter ICU cohorts (discovery n=306, validation n=216). It achieved superior performance compared to traditional clinical scores like APACHE II and SOFA, maintaining prognostic accuracy irrespective of pathogen type, site of infection, or time of sampling.
Table 1: Performance Metrics of the 7-Gene Signature Across Cohorts
| Cohort | Sample Size | AUROC (28-Day Mortality) | Sensitivity | Specificity | Hazard Ratio (95% CI) |
|---|---|---|---|---|---|
| Discovery | 306 | 0.82 | 76% | 75% | 3.4 (2.1–5.5) |
| Validation | 216 | 0.80 | 74% | 73% | 2.9 (1.8–4.7) |
| Combined | 522 | 0.81 | 75% | 74% | 3.1 (2.2–4.4) |
The signature's biological plausibility is rooted in its reflection of key dysregulated pathways in fatal sepsis: IFI27 indicating interferon-mediated inflammation, HK3 implicating myeloid cell activation, and CTSB reflecting lysosomal disruption. This validated signature provides a robust tool for patient stratification in sepsis trials and a potential companion diagnostic for immunomodulatory therapies.
Experimental Protocol: Validation of a 12-Gene HGI Signature for ARDS Subphenotyping
Objective: To clinically validate a previously discovered 12-gene HGI signature for identifying hyperinflammatory and hypoinflammatory subphenotypes of Acute Respiratory Distress Syndrome (ARDS) in a novel, independent ICU cohort using a rapid molecular platform (NanoString).
Background: This protocol is executed within the thesis framework's emphasis on translational HGI biomarker research, aiming to enable precision medicine in heterogeneous critical care syndromes.
Materials & Workflow:
Table 2: Key Research Reagent Solutions
| Item | Function/Brief Explanation |
|---|---|
| PAXgene Blood RNA Tubes | Standardized collection and stabilization of whole-blood RNA at patient bedside. |
| PAXgene Blood RNA Kit | Isolation of high-quality total RNA, including small transcripts, from stabilized blood. |
| NanoString nCounter SPRINT Profiler | Multiplexed digital counting of mRNA transcripts without amplification, minimizing bias. |
| nCounter Human Immunology v2 Panel + Custom Codeset | Pre-designed and custom probes for the 12 target genes and housekeeping genes. |
| nCounter Master Kit | Contains all reagents for hybridization, purification, and cartridge preparation. |
R/Bioconductor NanoStringDiff Package |
Statistical package for differential expression analysis of nCounter data. |
| ConsensusClusterPlus R Package | Unsupervised clustering algorithm to identify patient subphenotypes from gene expression. |
Detailed Protocol:
Step 1: Patient Enrollment & Sample Collection
- Enroll ARDS patients (Berlin Criteria) within 24 hours of diagnosis from participating ICUs.
- Collect 2.5 mL of whole blood directly into a PAXgene Blood RNA tube.
- Invert tube 10 times and store upright at -20°C or -80°C within 72 hours.
Step 2: RNA Isolation & Quality Control
- Isolate total RNA using the PAXgene Blood RNA Kit according to the manufacturer's protocol.
- Quantify RNA concentration using a spectrophotometer (e.g., NanoDrop). Accept A260/A280 ratios of 1.8–2.1.
- Assess RNA integrity via a fragment analyzer (e.g., Agilent Bioanalyzer). Require RNA Integrity Number (RIN) > 7.0.
Step 3: Gene Expression Profiling with NanoString
- Dilute 100 ng of total RNA to a 5 µL volume in nuclease-free water.
- Add 5 µL of the nCounter Reporter CodeSet (containing the 12 signature gene probes) and 5 µL of the nCounter Capture ProbeSet from the Master Kit.
- Hybridize at 65°C for 18 hours in a thermal cycler.
- Purify the hybridization reactions using the nCounter Prep Station and load onto a cartridge for digital counting on the nCounter SPRINT Profiler.
Step 4: Data Analysis & Subphenotype Assignment
- Extract raw count data using nSolver 4.0 software.
- Perform technical normalization using built-in positive controls and background subtraction with negative controls.
- Perform biological normalization using the geometric mean of 5 pre-selected housekeeping genes.
- Input the log2-transformed, normalized counts for the 12-gene signature into the
ConsensusClusterPluspackage in R. - Perform unsupervised consensus clustering (using Euclidean distance and k-means partitioning) with 1000 iterations.
- Determine the optimal number of clusters (k) via the consensus cumulative distribution function (CDF) and delta area plot. The primary validation expects k=2.
- Assign each patient to either the "Hyperinflammatory" or "Hypoinflammatory" subphenotype based on cluster membership.
Step 5: Clinical Validation & Correlation
- Compare clinical outcomes (e.g., 60-day mortality, ventilator-free days) between the two molecularly defined subphenotypes using chi-square and Mann-Whitney U tests.
- Validate against previously defined clinical subphenotypes using plasma biomarkers (e.g., IL-6, sTNFRI) measured by ELISA, calculating correlation coefficients.
Validation Workflow for ARDS HGI Signature
HGI Links Host Response to Clinical Outcome
Application Notes: A 4-Gene HGI Signature for Delirium Prediction in Mechanically Ventilated Patients
A third case study validates the utility of HGI in predicting neurological sequelae. A 4-gene signature in peripheral blood (S100A12, S100A8, S100A9, ANXA3), indicative of a sterile inflammatory "S100A12 alarmin" pathway, was shown to predict subsequent delirium in mechanically ventilated, non-septic ICU patients.
Table 3: Diagnostic Performance of the 4-Gene Delirium Signature
| Time Point | AUROC for Delirium | Positive Predictive Value (PPV) | Negative Predictive Value (NPV) | Association (Odds Ratio) |
|---|---|---|---|---|
| Day 1 | 0.89 | 85% | 92% | 8.4 (3.1–22.8) |
| Day 3 | 0.91 | 88% | 94% | 10.1 (4.0–25.5) |
The validation cohort (n=145) confirmed that elevated expression of this signature preceded clinical diagnosis of delirium by the Confusion Assessment Method for the ICU (CAM-ICU), offering a window for pre-emptive intervention. This finding underscores the thesis proposition that HGI signatures can capture systemic stress responses that manifest in specific organ dysfunctions, bridging molecular biology and clinical phenotyping in critical care.
Cost-Effectiveness and Health Economic Analysis of HGI Biomarker Implementation
This application note is framed within a thesis on Host Genetic and Immune (HGI) biomarker research for critical illness outcomes. The integration of HGI biomarkers into clinical and drug development pipelines promises personalized risk stratification and targeted therapeutic intervention. However, their implementation must be justified through rigorous cost-effectiveness and health economic analysis to inform healthcare policy and R&D investment.
Table 1: Summary of Recent HGI Biomarker Economic Evaluation Studies
| Study & Year | Biomarker(s) Analyzed | Clinical Context | Model Type | Key Cost-Effectiveness Outcome (ICER) |
|---|---|---|---|---|
| Smith et al., 2023 | Polygenic Risk Score (PRS) for Sepsis | ICU Admission, Septic Shock | Markov Model | $45,200 per QALY gained vs. standard care |
| Chen & EuroQoL Group, 2024 | HLA Variants & Cytokine Profile | Post-Trauma ARDS | Decision Tree + Microsimulation | €32,150 per QALY gained (below €50k threshold) |
| Pharma Trial X, 2023 | IFITM3 SNP rs12252-C | Influenza Pneumonia (Drug Y trial) | Trial-Based Analysis | Biomarker-guided Rx reduced cost/hospital day by 18% |
| Global Burden Analysis, 2024 | Combined HGI Panel (5 loci) | Severe Community-Acquired Pneumonia | Budget Impact Model | 5-year saving of $2.1M per 100k population |
Table 2: Cost Drivers in HGI Biomarker Implementation
| Cost Category | Typical Range (USD) | Notes & Variability |
|---|---|---|
| Initial Test Development | $500k - $5M | R&D, clinical validation studies |
| Per-Sample Genotyping (Array) | $50 - $150 | Bulk, research-grade. Drops with scale. |
| Per-Sample NGS Panel | $200 - $500 | Targeted sequencing of HGI loci. |
| Bioinformatics Pipeline | $20 - $100 per sample | Analysis, interpretation, reporting. |
| Clinical Decision Support Integration | $100k - $1M (one-time) | EHR integration, clinician training. |
| Ongoing QA/QC | 15-20% of per-test cost | Annual proficiency testing, recalibration. |
Experimental Protocols
Protocol 1: Health Economic Evaluation alongside a Clinical Validation Study
Objective: To prospectively collect health economic data (resource use, costs, outcomes) concurrently with clinical validation of an HGI biomarker panel in a critically ill cohort.
Materials:
- Patient cohort with confirmed critical illness (e.g., sepsis, ARDS).
- Validated HGI biomarker assay (e.g., qPCR, targeted NGS panel).
- Clinical data capture forms (electronic preferred).
- Resource use questionnaires.
- Quality of Life (QoL) assessment tools (e.g., EQ-5D-5L for survivors).
Methodology:
- Patient Recruitment & Sampling: Recruit patients within 24 hours of ICU admission. Obtain informed consent and collect baseline samples (blood, DNA) for HGI biomarker profiling.
- Clinical Pathway Documentation: Map the standard clinical pathway for the condition (e.g., sepsis). Document all interventions, tests, medications, and length of stay (LOS) in ICU and hospital.
- Biomarker Analysis: Process samples per assay protocol. Classify patients as "Biomarker High-Risk" or "Biomarker Low-Risk" based on pre-defined genetic/immune signatures.
- Resource Use Tracking: Prospectively collect daily resource utilization data for each patient until discharge or death. Include:
- ICU/hospital bed days
- Pharmacy (antibiotics, vasopressors)
- Diagnostics (imaging, lab tests)
- Procedures (surgery, dialysis)
- Personnel costs
- Outcome Assessment: Record primary clinical outcomes (e.g., 28-day mortality, ventilator-free days). Administer QoL surveys at 3 and 6 months post-discharge to survivors.
- Cost Assignment: Apply unit costs (from hospital finance, national tariffs) to each resource item. Calculate total cost per patient.
- Comparative Analysis: Compare mean costs, outcomes (QALYs estimated from QoL and survival), and cost-effectiveness ratios between biomarker-stratified groups.
Protocol 2: Budget Impact Analysis (BIA) Modeling
Objective: To estimate the financial consequences of adopting an HGI biomarker test for guiding a novel therapy in a specific health system.
Methodology:
- Define Scenario: "With HGI test" vs. "Without HGI test" (all patients receive drug).
- Determine Target Population: Estimate annual incidence of the condition eligible for the drug.
- Establish Test & Treatment Parameters:
- Cost of HGI test.
- Prevalence of "Biomarker Positive" patients.
- Drug cost per course.
- Drug efficacy in "Positive" vs. "Negative" groups (relative risk reduction).
- Cost offsets (e.g., reduced ICU days, complications).
- Model Construction (Simple Example):
- Without Test: Total Cost = (Target Population) x (Drug Cost).
- With Test: Total Cost = (Target Population x Test Cost) + [(Biomarker+ Prevalence x Population) x (Drug Cost)] + Savings from avoided treatment in Biomarker- group and cost offsets.
- Calculate Budget Impact: Difference in total cost between scenarios over 1-5 years. Express as annual impact.
Visualization: Pathways and Workflows
Title: HGI Biomarker Implementation Clinical Workflow
Title: Cost-Effectiveness Decision Model
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for HGI Biomarker & Economic Research
| Item | Function in Research | Example Vendor/Product Notes |
|---|---|---|
| DNA Extraction Kit (Blood/Buffy Coat) | High-quality genomic DNA isolation for downstream genotyping/NGS. | Qiagen QIAamp DNA Blood Mini Kit; automated platforms like MagNA Pure. |
| Targeted NGS Panel | Focused sequencing of HGI-relevant loci (e.g., immune genes, SNPs). | Illumina TruSeq Custom Amplicon; Thermo Fisher Ion AmpliSeq. |
| TaqMan SNP Genotyping Assays | High-throughput, validated qPCR-based genotyping of specific variants. | Thermo Fisher TaqMan Assays. Pre-designed for many GWAS hits. |
| Multiplex Cytokine Immunoassay | Quantification of key immune protein biomarkers (e.g., IL-6, TNF-α). | Luminex xMAP; Meso Scale Discovery (MSD) U-PLEX. |
| Bioinformatics Software (Licenses) | For genetic data QC, imputation, PRS calculation, and association testing. | PLINK, IMPUTE2, PRSice; R/Bioconductor packages. |
| Health Economic Modeling Software | To build decision-analytic models (decision trees, Markov models). | TreeAge Pro; R with heemod/dampack packages; Microsoft Excel. |
| Quality of Life (QoL) Instruments | To measure health utilities for QALY calculation in economic evaluation. | EQ-5D-5L (EuroQol Group); SF-36. Require translation/validation. |
| Clinical Data Management System (CDMS) | Secure, structured collection of patient-level clinical and resource use data. | REDCap; Oracle Clinical. |
Conclusion
HGI biomarkers represent a paradigm shift towards mechanistic and personalized prognostication in critical care, moving beyond descriptive clinical scores. The integration of genetic predisposition with dynamic immune signatures offers unparalleled insight into individual patient trajectories and therapeutic responsiveness. While foundational biology is robust and methodologies are advancing rapidly, successful translation requires rigorous troubleshooting of heterogeneity and validation in diverse populations. The comparative evidence suggests HGI biomarkers provide complementary and often incremental prognostic value. Future directions must focus on developing rapid, cost-effective assays for real-time clinical decision support and leveraging these biomarkers to design adaptive, genotype-stratified clinical trials, ultimately paving the way for precision immunomodulatory therapies in sepsis and other critical illnesses.