Rebound Hyperglycemia and the Somogyi Effect: Evidence, Mechanisms, and Modern Clinical Management
This article provides a comprehensive analysis of rebound hyperglycemia following hypoglycemia, critically examining the scientific validity of the Somogyi effect in light of contemporary evidence.
Rebound Hyperglycemia and the Somogyi Effect: Evidence, Mechanisms, and Modern Clinical Management
Abstract
This article provides a comprehensive analysis of rebound hyperglycemia following hypoglycemia, critically examining the scientific validity of the Somogyi effect in light of contemporary evidence. Tailored for researchers, scientists, and drug development professionals, it synthesizes foundational pathophysiology with advanced methodological approaches for investigation and mitigation. The scope encompasses the evolution of the Somogyi theory, the application of continuous glucose monitoring (CGM) for objective quantification, strategies for troubleshooting glycemic instability, and a comparative validation of this phenomenon against the more prevalent dawn phenomenon. The discussion is grounded in recent large-scale clinical studies and technological advancements, offering insights for future therapeutic innovation and clinical practice guidelines.
The Somogyi Effect: Foundational Concepts and Evolving Scientific Understanding
Historical Context and Original Postulates of the Somogyi Phenomenon
FAQ: What is the Somogyi Phenomenon?
Q: What did Michael Somogyi originally postulate? A: In the 1930s, Dr. Michael Somogyi, a Hungarian-born biochemist, postulated the phenomenon of "rebound hyperglycemia" [1] [2]. He theorized that an overdose of insulin could induce hypoglycemia (low blood sugar) during the late evening or night [1] [3]. This hypoglycemic episode would then trigger a defensive counter-regulatory hormonal response, involving hormones like glucagon, adrenaline, cortisol, and growth hormone [1] [2]. These hormones stimulate the liver to produce and release large amounts of glucose, leading to paradoxical hyperglycemia (high blood sugar) by the next morning [4] [3]. For decades, this theory, known as the Somogyi effect or Somogyi hypothesis, was an axiom in diabetes treatment [5] [6].
Q: How does the Somogyi effect differ from the Dawn Phenomenon? A: Both can cause high morning blood sugar, but their proposed mechanisms are fundamentally different. The table below summarizes the key distinctions.
Table 1: Distinguishing the Somogyi Effect from the Dawn Phenomenon
| Feature | Somogyi Phenomenon | Dawn Phenomenon |
|---|---|---|
| Primary Cause | Rebound effect from nocturnal hypoglycemia [1] [3] | Natural early-morning release of insulin-antagonist hormones (e.g., growth hormone, cortisol) [1] [2] |
| Nocturnal Hypoglycemia | Present; considered the trigger [4] | Absent [1] [3] |
| Prevalence | Considered rare or debated [1] [2] [7] | More common [1] [2] |
| Theoretical Basis | A theory, with current evidence disputing its prevalence [1] [3] [7] | A well-accepted physiological occurrence [1] |
FAQ: What is the Historical and Scientific Context of Dr. Somogyi's Work?
Q: Who was Dr. Michael Somogyi? A: Michael Somogyi (1883-1971) was a Hungarian biochemist who pursued his scientific career primarily in the United States [5] [6]. He was a pioneer in the field of diabetes, involved in devising one of the first methods for insulin extraction and was part of the team that treated the first child with diabetes using insulin in the United States in 1922 [5] [6]. His personal experiences with food scarcity during his youth and World War I shaped his interest in the effects of diet on metabolic disorders [5] [6]. He was also a translational researcher who standardized numerous clinical laboratory determinations, most famously the method for measuring amylase, with results reported in "Somogyi units" for decades [5] [6].
Q: What is the modern scientific view on the Somogyi phenomenon? A: The Somogyi phenomenon is a subject of ongoing debate and is no longer considered a common cause of morning hyperglycemia [1] [3] [2]. More recent studies using continuous glucose monitoring (CGM) have challenged its validity [1] [3]. Several studies have concluded that nocturnal hypoglycemia does not commonly result in major morning hyperglycemia and that high fasting glucose is more likely a sign of insufficient insulin (hypoinsulinemia) or waning of the insulin dose overnight, rather than a rebound effect [1] [2] [7]. Some researchers have suggested that apparent rebound hyperglycemia may instead be caused by insulin-induced insulin resistance [2].
Researcher's Toolkit: Experimental Protocols & Reagents
This section provides methodologies and materials for investigating mechanisms of morning hyperglycemia.
Experimental Protocol: Investigating Nocturnal Glycemic Control
Aim: To determine the cause of persistent fasting hyperglycemia in a subject, differentiating between the Somogyi effect, the dawn phenomenon, and simple insulin deficiency.
Materials:
- Continuous Glucose Monitoring (CGM) system [1] [2] or
- Blood glucose meter and test strips for manual monitoring
- Logbook for recording food intake, insulin doses, and exercise
Method:
- For CGM-based profiling: Deploy a CGM system to capture interstitial glucose readings continuously every few minutes throughout the night and early morning. Data should be collected over several nights to establish a pattern [1] [2].
- For manual profiling: Instruct the subject to measure blood glucose at the following times for at least two consecutive nights [3]:
- Two hours after the evening meal
- At bedtime (e.g., 10:00 PM)
- Between 2:00 AM and 3:00 AM (nocturnal nadir)
- Immediately upon waking (e.g., 6:00 AM - 7:00 AM)
- Correlate glucose measurements with records of evening food intake, alcohol consumption, physical activity, and insulin administration to identify potential triggers [4].
Data Interpretation:
- Pattern A (Somogyi Effect): Blood glucose is low (e.g., <70 mg/dL or <4 mmol/L) at 3:00 AM but high upon waking [4] [3].
- Pattern B (Dawn Phenomenon): Blood glucose is stable and within range at 3:00 AM but begins to rise significantly in the pre-dawn hours until waking [1].
- Pattern C (Waning Insulin/Insulin Deficiency): Blood glucose is elevated at bedtime and remains high or continues to rise steadily throughout the night [1] [2] [7].
Research Reagent Solutions
Table 2: Essential Materials for Investigating Glucose Counter-Regulation
| Research Reagent / Material | Function in Investigation |
|---|---|
| Continuous Glucose Monitor (CGM) | Provides high-frequency, temporal data on glucose levels to identify nocturnal hypoglycemic episodes and morning rise patterns without disrupting sleep [1] [2]. |
| Insulin (various formulations) | To manipulate nocturnal insulin levels and study the effects of insulin overdose, type, and timing on morning glucose homeostasis [5] [2]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | For quantitative measurement of counter-regulatory hormones in plasma/serum (e.g., Glucagon, Cortisol, Growth Hormone, Epinephrine) to confirm their activation post-hypoglycemia [1] [8]. |
| Radioimmunoassay (RIA) Kits | A traditional method for precise measurement of hormone levels, including insulin and C-peptide, to assess endogenous insulin secretion and insulin resistance [8]. |
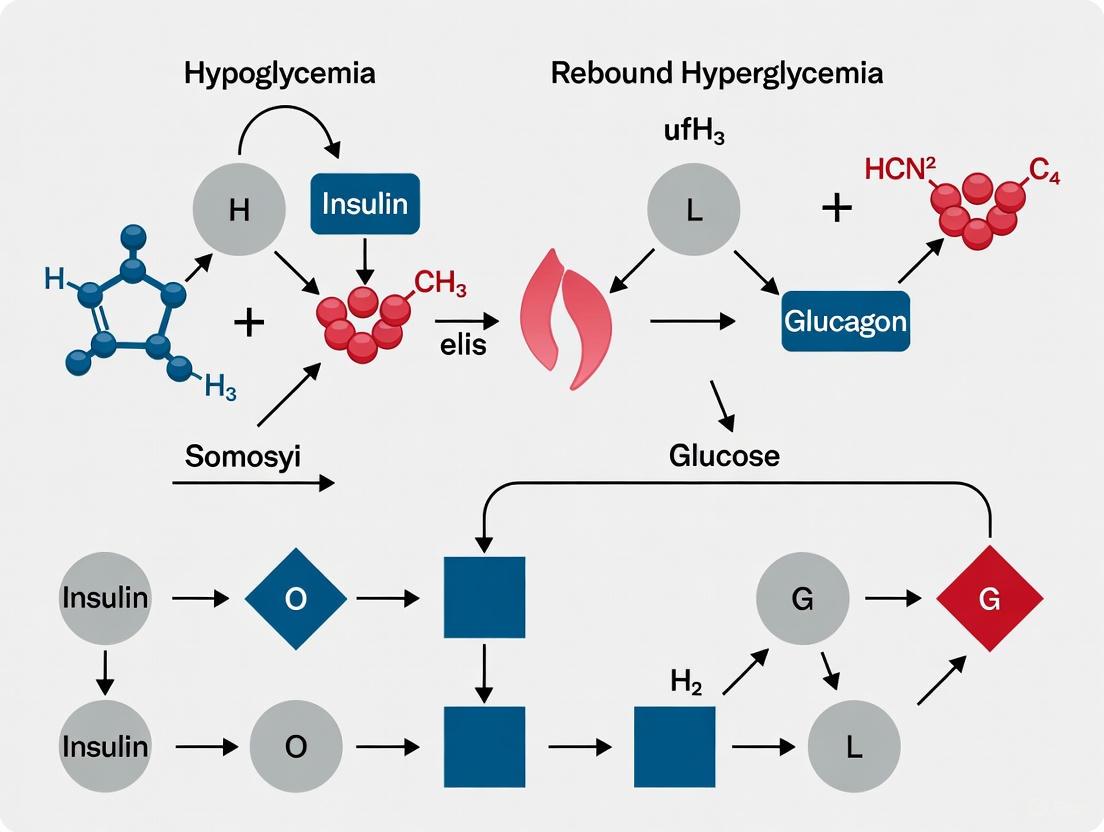
Visualization: The Hypothesized Pathway of the Somogyi Effect
The following diagram illustrates the sequence of physiological events as originally postulated by Michael Somogyi, from the initial insulin administration to the final rebound hyperglycemia.
Diagram 1: The postulated pathway of the Somogyi effect, illustrating the sequence of physiological events from the initial insulin administration to the final rebound hyperglycemia.
Frequently Asked Questions (FAQs)
1. What is a counterregulatory hormone surge in the context of hypoglycemia? A counterregulatory hormone surge describes the body's physiological defense mechanism against falling blood glucose levels. When hypoglycemia occurs, the body releases several hormones—primarily glucagon, epinephrine, cortisol, and growth hormone—that oppose the action of insulin [9] [2] [10]. These hormones work to raise blood glucose by stimulating glycogenolysis (breakdown of glycogen) and gluconeogenesis (production of new glucose), thereby counteracting the hypoglycemic state [1] [10].
2. What is the Somogyi effect, and what is its current scientific standing? The Somogyi effect is a theory proposing that nocturnal hypoglycemia can trigger a counterregulatory hormone surge, leading to rebound hyperglycemia in the morning [1] [3]. However, its validity is debated in the scientific community. Recent studies using continuous glucose monitoring (CGM) have challenged this theory, showing that nocturnal hypoglycemia often leads to normal or low fasting glucose, not hyperglycemia [1] [2]. Many experts now consider the dawn phenomenon—a natural early morning rise in blood sugar due to hormonal changes—a more common cause of morning hyperglycemia [1] [3].
3. How do counterregulatory hormones mechanistically regulate gluconeogenesis? Counterregulatory hormones regulate gluconeogenesis through rapid hormonal signaling and allosteric modulation of key enzymes.
- Glucagon: Binds to G-protein-coupled receptors, activating protein kinase A (PKA). PKA phosphorylates and inactivates pyruvate kinase, while also reducing levels of fructose-2,6-bisphosphate, a potent inhibitor of gluconeogenesis. This simultaneously halts glycolysis and promotes gluconeogenic flux [11].
- Epinephrine: Acts via beta-adrenergic receptors to stimulate glycogenolysis for immediate glucose release, and provides gluconeogenic precursors by mobilizing lactate and alanine from muscle and glycerol from adipose tissue [9] [12].
- Cortisol and Growth Hormone: These hormones promote insulin resistance in peripheral tissues over several hours, reducing glucose utilization and making more glucose available [9] [13].
4. What are the key experimental considerations for modeling the Somogyi effect in a research setting? Researchers should consider several factors and use appropriate controls to distinguish the Somogyi effect from other phenomena.
- Temporal Monitoring: It is crucial to measure blood glucose concentrations at multiple time points: after an evening meal, at bedtime, in the middle of the night (e.g., 3 AM), and upon waking [3].
- Hormone Assays: Confirm the counterregulatory surge by directly measuring plasma or urinary levels of glucagon, cortisol, epinephrine, and growth hormone [13].
- Control for Dawn Phenomenon: The dawn phenomenon also causes morning hyperglycemia but is not preceded by hypoglycemia. Including a control group or condition without induced hypoglycemia is essential for differentiation [1] [2].
- Subject Selection: The model system (e.g., animal model vs. human patients) and their insulin secretory status (e.g., C-peptide positive vs. negative) can significantly impact results, as endogenous insulin secretion influences counterregulatory responses [13].
Troubleshooting Guides
Guide 1: Investigating Unanticipated Morning Hyperglycemia in a Diabetic Research Model
Problem: Consistent, unexplained morning hyperglycemia is observed in a research model, complicating data interpretation in a study of glycemic control.
Solution: A systematic approach is required to identify the root cause.
Step 1: Differentiate Between Somogyi Effect and Dawn Phenomenon
- Action: Implement frequent nocturnal blood glucose monitoring, ideally using a continuous glucose monitoring (CGM) system [2] [3].
- Interpretation: If a hypoglycemic episode (glucose <70 mg/dL or 3.9 mmol/L) is followed by hyperglycemia, it may indicate a Somogyi-like rebound. If glucose levels are stable or steadily rise from ~3 AM onward without preceding hypoglycemia, it is likely the dawn phenomenon [1].
Step 2: Evaluate the Insulin Regimen
- Action: Audit the timing and dosage of insulin administration. An excessive dose of intermediate- or long-acting insulin in the evening is a common cause of nocturnal hypoglycemia [2].
- Interpretation: If nocturnal hypoglycemia is confirmed, the solution is often a reduction in the evening insulin dose or a change to a different insulin formulation, not an increase [2] [3].
Step 3: Assess for Hypoglycemia Unawareness
Guide 2: Inconsistent Gluconeogenesis Flux Measurements in a Hepatic Cell Model
Problem: Measurements of gluconeogenic flux in hepatocyte cultures are highly variable following the application of counterregulatory hormones.
Solution: Inconsistency often stems from unregulated variables in the cellular environment.
Step 1: Verify Substrate Availability
- Action: Ensure the culture media contains an adequate and consistent supply of gluconeogenic precursors such as lactate, pyruvate, alanine, and glycerol [11].
- Interpretation: Gluconeogenesis cannot proceed optimally without sufficient substrates. Inconsistent results may be due to depletion of these compounds.
Step 2: Monitor Cellular Energy Status
- Action: Assess the ATP/ADP and ATP/AMP ratios in cell lysates. Gluconeogenesis is an energy-intensive process that requires high ATP levels [11].
- Interpretation: Low energy charge (high ADP/ATP or AMP/ATP) will inhibit key enzymes like fructose-1,6-bisphosphatase, leading to reduced and variable flux [14] [11] [15].
Step 3: Control for Allosteric Effectors
- Action: Check for the presence and concentration of key allosteric regulators.
- Interpretation:
- Acetyl-CoA: This is a potent allosteric activator of pyruvate carboxylase, the first committed step in gluconeogenesis. Its levels must be sufficient to initiate the pathway [14] [11].
- Fructose-2,6-bisphosphate: This metabolite is a powerful allosteric inhibitor of fructose-1,6-bisphosphatase. Hormones like glucagon lower its concentration to de-repress gluconeogenesis [14] [11].
The tables below consolidate key quantitative findings on hypoglycemia thresholds and counterregulatory hormone activity for easy reference.
Table 1: Clinically Defined Thresholds for Hypoglycemia
This table standardizes the classification of hypoglycemic events based on consensus guidelines [12].
| Classification | Glucose Threshold | Clinical Significance |
|---|---|---|
| Hypoglycemia Alert (Level 1) | ≤70 mg/dL (3.9 mmol/L) | Indicates a value low enough to require intervention with fast-acting carbohydrates and/or medication adjustment. |
| Clinically Significant Hypoglycemia (Level 2) | <54 mg/dL (3.0 mmol/L) | Sufficiently low to indicate serious, clinically important hypoglycemia that is often accompanied by symptoms. |
| Severe Hypoglycemia (Level 3) | No specific glucose threshold | Defined by severe cognitive impairment requiring external assistance for recovery. |
Table 2: Representative Data on Counterregulatory Hormones in Type 1 Diabetes
This table presents sample data from a clinical study measuring hormone levels in type 1 diabetic patients, illustrating the relationship between these hormones and glucose control [13].
| Parameter | Measured Value (Mean ± SD) | Reference Range | Correlation with Fasting Blood Glucose |
|---|---|---|---|
| Plasma Glucagon | 98 ± 41 pg/mL | 40 – 180 pg/mL | Positive (R=0.378, p=0.047) |
| Urinary GH SD Score | +1.01 ± 0.70 | 0 (Population Mean) | Not Significant |
| Serum Cortisol | 21.6 ± 5.5 µg/dL | 4.0 – 18.3 µg/dL | Not Significant |
| Urinary Cortisol | 238 ± 197 ng/gCr | Not Provided | Negative (R=-0.476, p=0.010) |
Experimental Protocols
Protocol 1: Assessing the Counterregulatory Hormone Response to Induced Hypoglycemia
Objective: To quantitatively measure the secretion kinetics of glucagon, epinephrine, cortisol, and growth hormone in response to a controlled hypoglycemic clamp.
Methodology:
- Subject Preparation: After an overnight fast, insert intravenous catheters for insulin/glucose infusion and frequent blood sampling.
- Hyperinsulinemic-Hypoglycemic Clamp: Initiate a fixed-rate insulin infusion to induce and maintain hypoglycemia. A variable-rate glucose infusion is used to clamp blood glucose at a target level (~50 mg/dL or 2.8 mmol/L) for a defined period (e.g., 90 minutes) [12].
- Blood Sampling: Collect blood samples at baseline and at regular intervals during the clamp.
- Samples for Glucose: Analyze immediately with a glucose analyzer.
- Samples for Hormones: Collect in pre-chilled tubes containing appropriate preservatives (e.g., EDTA for glucagon, EGTA/glutathione for catecholamines). Centrifuge immediately at 4°C and store plasma at -80°C until assay.
- Hormone Assays: Use commercially available, validated kits:
- Glucagon: Radioimmunoassay (RIA) or ELISA.
- Epinephrine/Norepinephrine: High-performance liquid chromatography with electrochemical detection (HPLC-EC) or ELISA.
- Cortisol & Growth Hormone: Chemiluminescent immunoassay (CLIA) or ELISA.
Key Measurements:
- Glucose Infusion Rate (GIR): The amount of glucose required to maintain the hypoglycemic plateau is an inverse measure of the overall counterregulatory response.
- Hormone Peak Concentrations: The maximum plasma level reached for each hormone.
- Integrated Area Under the Curve (AUC): The total hormone output over time.
Protocol 2: Measuring Gluconeogenesis Flux in Primary Hepatocytes
Objective: To quantify the rate of gluconeogenesis in primary hepatocytes after stimulation with counterregulatory hormones.
Methodology:
- Hepatocyte Isolation and Culture: Isolate primary hepatocytes via collagenase perfusion from a model organism. Culture in a hormonally defined, serum-free medium.
- Treatment Groups:
- Control: Vehicle only.
- Glucagon Treatment: 10-100 nM glucagon.
- Cortisol Treatment: 100-500 nM cortisol.
- Combined Treatment: Glucagon + cortisol.
- Gluconeogenesis Assay:
- Incubate cells in glucose-production buffer containing a saturating concentration of a gluconeogenic precursor (e.g., 10 mM lactate + 1 mM pyruvate).
- After a set incubation period (e.g., 4-6 hours), collect the conditioned medium.
- Measure the accumulated glucose in the medium using a glucose assay kit (e.g., hexokinase/glucose-6-phosphate dehydrogenase coupled enzyme assay). Normalize the glucose concentration to total cellular protein content (e.g., via Bradford assay).
- Gene Expression Analysis (Optional): Extract RNA and perform RT-qPCR to measure the mRNA expression of key gluconeogenic enzymes, such as PEPCK and Glucose-6-Phosphatase, which are transcriptionally upregulated by these hormones [11].
The Scientist's Toolkit: Research Reagent Solutions
| Research Reagent | Function / Application in Research |
|---|---|
| Hyperinsulinemic-Hypoglycemic Clamp | The gold-standard in vivo method for inducing controlled hypoglycemia and directly quantifying the counterregulatory hormone response and glucose kinetics [12]. |
| Continuous Glucose Monitoring (CGM) | Provides high-resolution, temporal data on glucose fluctuations, essential for detecting nocturnal hypoglycemia and differentiating the Somogyi effect from the dawn phenomenon [1] [2]. |
| Specific ELISA/RIA Kits | Validated immunoassays for the accurate and sensitive quantification of hormone levels (glucagon, cortisol, epinephrine, growth hormone) in plasma, serum, or urine samples [13]. |
| Primary Hepatocytes | A key in vitro model system for studying the direct effects of counterregulatory hormones on hepatic gluconeogenesis, glycogenolysis, and insulin signaling, free from systemic influences. |
| Stable Isotope Tracers (e.g., [U-¹³C]-lactate) | Used with Mass Spectrometry to precisely track the flux of substrates through the gluconeogenic pathway, allowing for direct measurement of gluconeogenesis rates in vivo or in vitro. |
Pathway and Workflow Visualizations
Counterregulatory Hormone Response to Hypoglycemia
Hormonal Regulation of Key Gluconeogenic Enzymes
What is the defining characteristic of rebound hyperglycemia (Somogyi effect)?
Rebound hyperglycemia, or the Somogyi effect, is defined by a paradoxical rebound from nocturnal hypoglycemia to morning hyperglycemia [1] [3]. This phenomenon was first described by Dr. Michael Somogyi in the 1930s and posits that an episode of low blood glucose (hypoglycemia) during the night triggers a compensatory surge of counter-regulatory hormones (e.g., catecholamines, cortisol, growth hormone, glucagon) [1] [16]. This hormonal response stimulates hepatic glucose production via glycogenolysis and gluconeogenesis, leading to elevated blood glucose levels upon waking [1] [17]. In individuals with diabetes, the inability to secrete sufficient insulin prevents the correction of this elevated glucose, resulting in persistent hyperglycemia [3].
How does the dawn phenomenon differ from the Somogyi effect?
The dawn phenomenon is a distinct cause of morning hyperglycemia that is not preceded by hypoglycemia [18]. It is attributed to the body's normal circadian rhythm, involving a nocturnal surge of insulin-antagonistic hormones (including growth hormone, cortisol, and glucagon) in the early morning hours [19] [20]. This surge signals the liver to increase glucose output, providing energy to wake up [20]. In individuals without diabetes, a concomitant increase in insulin secretion suppresses hepatic glucose production. However, in diabetes, insufficient insulin production or insulin resistance leads to morning hyperglycemia [18] [20]. The dawn phenomenon is notably more prevalent than the Somogyi effect [1].
The table below summarizes the core differences:
| Feature | Somogyi Effect (Rebound Hyperglycemia) | Dawn Phenomenon |
|---|---|---|
| Core Mechanism | Counter-regulatory hormone response to nocturnal hypoglycemia [3] [16] | Circadian release of insulin-antagonistic hormones; not triggered by low glucose [18] [20] |
| Nocturnal Glucose Pattern | Hypoglycemia (low glucose) around 2-3 a.m., followed by hyperglycemia [17] | Normal or steadily rising glucose through the night and early morning [18] [17] |
| Primary Hormones Involved | Adrenaline, corticosteroids, growth hormone, glucagon [1] [3] | Cortisol, growth hormone, glucagon [18] [20] |
| Prevalence | Less common; subject to ongoing scientific debate [1] [3] | Very common; occurs in over 50% of individuals with both T1D and T2D [18] [20] |
The following diagram illustrates the distinct physiological pathways and resulting glucose profiles for the Somogyi effect versus the dawn phenomenon.
What is the scientific controversy surrounding the Somogyi effect?
The Somogyi effect is a subject of ongoing debate in the scientific community [1]. While it is a well-known concept among clinicians and patients, its existence as a common clinical entity is disputed by modern research utilizing continuous glucose monitoring (CGM) [1] [3].
- Evidence Against the Phenomenon: Some studies have found no correlation between nocturnal hypoglycemia and next-day hyperglycemia. For instance, one study concluded that nocturnal hypoglycemia did not cause daytime hyperglycemia and found no associated rise in counter-regulatory hormones [1]. Another CGM study on Type 1 diabetes patients found that morning hyperglycemia was not linked to nocturnal hypoglycemic events [1] [16].
- Evidence Supporting the Phenomenon: Conversely, other research has concluded that the Somogyi effect is the most common cause of fasting hyperglycemia in patients with Type 1 diabetes who have suboptimal glucose control [16].
- Current Consensus: The prevailing view in the field is shifting. Many experts now believe that early morning hyperglycemia is more frequently caused by the dawn phenomenon or simply by waning insulin levels from the previous evening's dose, rather than a rebound effect [1] [20]. Consequently, some recent clinical resources describe the Somogyi effect as a theory rather than an established fact [3].
What experimental protocols are used to distinguish these entities in a clinical research setting?
Accurate differentiation requires detailed monitoring of glucose levels throughout the night to establish the temporal sequence of events [3] [17].
Protocol 1: Continuous Glucose Monitoring (CGM)
The most effective method for diagnosis is the use of CGM, which provides a comprehensive profile of glucose fluctuations every few minutes without requiring the subject to wake up [18] [20].
- Equipment: A professional or personal CGM system.
- Procedure: Apply the CGM sensor as per manufacturer instructions. Collect data over a minimum of 2-3 consecutive nights to account for daily variability.
- Data Analysis: Plot the 24-hour glucose trace. Identify the nocturnal glucose nadir (lowest point) and the pre-breakfast glucose value.
- Somogyi Effect Profile: Glucose trace shows a distinct dip below the hypoglycemic threshold (typically <70 mg/dL) between 2:00 a.m. and 4:00 a.m., followed by a sharp rise to hyperglycemic levels by morning [16] [17].
- Dawn Phenomenon Profile: Glucose levels remain stable or gradually decline until approximately 3:00 a.m., after which a steady climb begins without any preceding hypoglycemic event [18].
Protocol 2: Intermittent Capillary Blood Glucose Testing
If CGM is unavailable, a structured intermittent testing protocol can be implemented.
- Equipment: Blood glucose meter, test strips, lancets, logbook.
- Procedure: The subject checks and records their blood glucose at the following times:
- At bedtime (e.g., 10:00 p.m.)
- Between 2:00 a.m. and 3:00 a.m.
- Immediately upon waking (e.g., 7:00 a.m.)
- Data Interpretation:
What are the key research reagents and materials for investigating these conditions?
Research into morning hyperglycemias relies on tools for precise glucose measurement, hormone assays, and controlled insulin delivery.
| Research Tool / Reagent | Primary Function in Investigation |
|---|---|
| Continuous Glucose Monitor (CGM) | Captures high-resolution, interstitial glucose data to establish definitive nocturnal glucose patterns and differentiate between phenomena [18] [20]. |
| Immunoassays (ELISA/RIA) | Quantifies plasma levels of counter-regulatory hormones (e.g., Cortisol, Glucagon, Growth Hormone, Catecholamines) to confirm the underlying endocrine physiology [1]. |
| Long-Acting & Rapid-Acing Insulin Analogs | Used in controlled studies to manipulate nocturnal insulin levels and model waning insulin versus excess insulin conditions [20] [17]. |
| Standardized Meal / Enteral Formula | Provides a controlled carbohydrate and protein load for evening meals to eliminate dietary variability as a confounder in studies [20]. |
| Insulin Pump | Allows for precise, programmable delivery of basal insulin; critical for experiments testing time-specific insulin dosing to counteract the dawn phenomenon [18] [20]. |
How does the management approach differ based on the diagnosis?
The therapeutic strategy diverges completely based on the underlying cause, highlighting the critical importance of a correct diagnosis.
| Management Strategy | Somogyi Effect | Dawn Phenomenon |
|---|---|---|
| Insulin Adjustment | Reduce the dose or change the timing of insulin that is active overnight (e.g., decrease evening long-acting insulin or avoid rapid-acting insulin at supper) [16] [17]. | Increase overnight insulin action. This can be achieved by increasing basal insulin dose, switching to a longer-acting basal insulin, or using an insulin pump to administer an increased basal rate in the early morning hours [18] [20]. |
| Adjunct Therapies | Consuming a small bedtime snack containing complex carbohydrates and/or protein to prevent nocturnal hypoglycemia [16] [17]. | Evening exercise to improve overall insulin sensitivity; consuming a breakfast meal to counter hormone-mediated glucose release [18] [20]. |
| Key Caution | Increasing insulin dose in response to morning hyperglycemia, without investigation, will worsen the nocturnal hypoglycemia and perpetuate the cycle [17]. | Increasing evening insulin without confirming the diagnosis can inadvertently induce nocturnal hypoglycemia, potentially creating a Somogyi-like effect [20]. |
Frequently Asked Questions (FAQs)
Q1: What is the Somogyi effect, and what was its original proposed mechanism?
The Somogyi effect, also known as "posthypoglycemic hyperglycemia" or "rebound hyperglycemia," is a theory proposed in the 1930s by Dr. Michael Somogyi. It describes a paradoxical reaction where the body responds to an episode of hypoglycemia (low blood sugar) by producing hyperglycemia (high blood sugar). The mechanism he proposed suggests that when blood glucose drops too low, particularly overnight, it triggers the release of counterregulatory hormones (such as adrenaline, cortisol, growth hormone, and glucagon). This hormonal surge activates gluconeogenesis and glycogenolysis, leading to a rebound high blood glucose level, most notably in the early morning [21] [1] [16].
Q2: How does Continuous Glucose Monitoring (CGM) evidence challenge the traditional Somogyi theory?
Modern CGM evidence challenges the Somogyi theory on two main fronts: frequency and causality.
- Lack of Frequent Rebound: CGM studies have shown that nocturnal hypoglycemia is more frequently followed by normal or low fasting glucose levels, not hyperglycemia. One key study of 89 patients with Type 1 Diabetes found that fasting capillary glucose was more likely to be lower following nocturnal hypoglycemia, with only two instances of glucose exceeding 180 mg/dL [2] [1].
- Questioned Hormonal Response: Research has indicated that even when rebound hyperglycemia occurs, it is not consistently associated with elevated levels of counterregulatory hormones like glucagon, epinephrine, growth hormone, or cortisol, which is a cornerstone of the original Somogyi theory [1] [16].
The table below summarizes key CGM study findings that dispute the theory:
| Study Focus | Key Findings from CGM Evidence | Interpretation |
|---|---|---|
| Frequency of Rebound Hyperglycemia [2] | Following nocturnal hypoglycemia, fasting glucose was more often low, with only 2.2% of cases (2/89) showing glucose >180 mg/dL. | The Somogyi effect is a rare occurrence, not a common cause of morning hyperglycemia. |
| Hormonal Response [1] | Daytime hyperglycemia following nocturnal hypoglycemia showed no correlation with increased levels of glucagon, epinephrine, growth hormone, or cortisol. | The postulated counterregulatory hormone surge driving the rebound is not reliably observed. |
| Causality in Morning Hyperglycemia [1] | Patients with early morning hyperglycemia were observed to have high blood glucose measurements at night rather than low ones. | Morning hyperglycemia is more likely caused by other factors, such as the dawn phenomenon or waning insulin. |
Q3: What is the difference between the Somogyi effect and the dawn phenomenon?
It is crucial for researchers to distinguish between these two concepts, as their management strategies differ. The table below outlines the key differences:
| Feature | Somogyi Effect (Theoretical) | Dawn Phenomenon (Common) |
|---|---|---|
| Primary Cause | Rebound effect from nocturnal hypoglycemia. | Natural early morning release of counterregulatory hormones (e.g., growth hormone, cortisol). |
| Nocturnal Glucose | Low (hypoglycemic) around 2:00 a.m. - 3:00 a.m. [16] [3] | Normal or steadily rising. |
| Morning Glucose | High (hyperglycemic). | High (hyperglycemic). |
| Prevalence | Considered rare and controversial [3] [2]. | A common occurrence in both diabetic and non-diabetic individuals [1]. |
| Proposed Research Solution | Reduce evening insulin dose to prevent nocturnal lows. | Increase or adjust timing of evening insulin to counteract morning hormone surge. |
Q4: What are the essential components of an experimental protocol to investigate rebound hyperglycemia?
A robust protocol to study this phenomenon requires frequent glucose measurement and careful hormone analysis.
- Participants: Recruit individuals with Type 1 Diabetes on insulin therapy.
- Glucose Monitoring: Utilize Continuous Glucose Monitoring (CGM) systems for seamless, high-frequency (e.g., every 5 minutes) glucose tracking throughout the night and day [22] [2]. This is superior to intermittent finger-stick checks.
- Critical Time Points: If CGM is unavailable, mandate manual blood glucose measurements at key intervals: two hours after the evening meal, at bedtime, at 3:00 a.m., and upon waking [3].
- Hormonal Assays: Collect blood samples during suspected hypoglycemic and subsequent hyperglycemic events to measure levels of counterregulatory hormones (glucagon, cortisol, epinephrine, growth hormone).
- Data Correlation: Analyze the data for temporal relationships between nocturnal hypoglycemia, hormone surges, and morning hyperglycemia.
Q5: What are common technical challenges when using CGM in a clinical study, and how can they be troubleshooted?
| Problem | Possible Cause | Recommended Action |
|---|---|---|
| Signal Loss Alarm | Sensor and reader are too far apart (beyond 6 meters/20 feet). | Ensure devices are within range. Try scanning the sensor manually. If persistent, replace the sensor [23]. |
| Sensor Error / Glucose Reading Unavailable | Inability to communicate with sensor; sensor too hot or too cold. | Move to a location with appropriate temperature (10°C - 45°C) and scan again after 10 minutes [23]. |
| Skin Irritation | Sensitivity to adhesive or friction from clothing. | Ensure application site is clean and dry. Consult a healthcare professional to identify hypoallergenic solutions [23]. |
| Inconsistent Data | Sensor may not be properly calibrated or may be failing. | Follow manufacturer calibration guidelines. If errors persist, replace the sensor and document the event [23]. |
Experimental Protocols & Methodologies
Protocol 1: Differentiating Causes of Morning Hyperglycemia
Objective: To determine whether a subject's morning hyperglycemia is attributable to the Somogyi effect, the dawn phenomenon, or chronic insulin underdosing.
Materials:
- Continuous Glucose Monitor (CGM) system or blood glucose meter with test strips.
- Data log sheet for food, insulin, and activity.
Methodology:
- Instruct the subject to maintain their usual insulin regimen, diet, and exercise for the study duration.
- For three consecutive nights, collect blood glucose readings at the following times:
- Between 10:00 p.m. and 11:00 p.m. (before bed)
- Between 2:00 a.m. and 3:00 a.m. (nocturnal)
- Upon waking between 6:00 a.m. and 8:00 a.m. (fasting)
- If using CGM, ensure it is active and recording data throughout this period.
- Correlate the nocturnal glucose reading with the morning fasting reading.
Interpretation of Results:
- Somogyi Effect Suspected: Nocturnal glucose is low (<70 mg/dL) followed by high morning fasting glucose [16].
- Dawn Phenomenon Suspected: Nocturnal glucose is normal or stable followed by a rise to high morning fasting glucose [2].
- Chronic Insulin Underdosing: Glucose levels are high at all measurement points (bedtime, nocturnal, and morning), indicating persistent insulin deficiency [1].
Protocol 2: Investigating the Counterregulatory Hormone Response
Objective: To quantify the relationship between nocturnal hypoglycemia and the subsequent release of counterregulatory hormones.
Materials:
- CGM system.
- Venous blood collection kits (e.g., vacutainers, butterflies).
- Centrifuge and freezer for serum/plasma separation and storage.
- ELISA or RIA kits for glucagon, cortisol, epinephrine, and growth hormone.
Methodology:
- Admit study participants to a clinical research unit for overnight monitoring.
- Set CGM alarms to alert staff at a predefined hypoglycemic threshold (e.g., 63 mg/dL).
- Upon CGM alarm confirming hypoglycemia, immediately collect a baseline blood sample for hormone analysis.
- Treat the hypoglycemic event according to a standardized protocol.
- Continue to collect blood samples at 30-minute intervals for the next 2-3 hours to track hormone levels and glucose trends.
- Compare hormone profiles from nights with hypoglycemia to control nights without hypoglycemia.
Research Reagent Solutions & Essential Materials
The table below details key materials and their functions for conducting research in this field.
| Item | Function / Application in Research |
|---|---|
| Continuous Glucose Monitor | Provides high-frequency, interstitial glucose measurements with minimal participant disturbance; essential for detecting asymptomatic nocturnal hypoglycemia and tracking glucose trends [22]. |
| Insulin Pumps | Allows for precise and programmable delivery of insulin; useful for standardizing basal rates or testing different insulin delivery patterns to provoke or prevent nocturnal hypoglycemia. |
| ELISA Kits | Enzyme-linked immunosorbent assay kits for the quantitative measurement of counterregulatory hormones (glucagon, cortisol, growth hormone) in serum/plasma samples. |
| Blood Collection Tubes | Including tubes with appropriate anticoagulants (e.g., EDTA for plasma) and preservatives for stable hormone analysis. |
| Glycated Hemoglobin (HbA1c) Test | Measures average blood glucose over the preceding 2-3 months; a low or in-range HbA1c in the context of morning hyperglycemia can support a theory of rebound from overtreatment [2]. |
Signaling Pathways and Conceptual Workflows
Somogyi Theory vs CGM Evidence
Morning Hyperglycemia Investigation
The Somogyi effect, also known as posthypoglycemic hyperglycemia or rebound hyperglycemia, is a phenomenon historically proposed to explain high morning blood glucose levels following an untreated nocturnal hypoglycemic episode. First described in the 1930s by Dr. Michael Somogyi, it theorizes that the body reacts to nighttime hypoglycemia by activating counterregulatory hormones (such as adrenaline, corticosteroids, growth hormone, and glucagon), leading to increased glucose production and resultant morning hyperglycemia [1] [3]. Within the broader context of managing hypoglycemia and rebound hyperglycemia, understanding the epidemiology and clinical relevance of the Somogyi effect is crucial for researchers and clinicians aiming to optimize glycemic control and interpret complex glucose patterns.
Frequently Asked Questions (FAQs) and Troubleshooting Guides
Q1: What is the fundamental pathophysiological pathway of the Somogyi effect?
A1: The proposed sequence involves a hypoglycemic trigger, leading to a counterregulatory hormone response, which subsequently causes rebound hyperglycemia. The diagram below illustrates this theoretical pathway.
Q2: How can I differentiate the Somogyi effect from the Dawn Phenomenon in a research or clinical setting?
A2: The key differentiator is the presence or absence of a preceding hypoglycemic event. The table below outlines the core differences.
| Feature | Somogyi Effect | Dawn Phenomenon |
|---|---|---|
| Primary Cause | Rebound from nocturnal hypoglycemia [1] [3] | Natural early-morning hormone surge (e.g., cortisol, growth hormone) [1] [20] |
| Nocturnal Glucose | Documented hypoglycemia (<70 mg/dL) [24] | Stable or steadily rising glucose without hypoglycemia [1] |
| Prevalence | Less common; recent studies question its prevalence [1] | Very common; affects up to half of people with diabetes [20] |
| Research Diagnosis | Continuous Glucose Monitoring (CGM) showing hypoglycemia followed by hyperglycemia before 6:00 am [24] | CGM showing hyperglycemia without a preceding hypoglycemic event [1] |
Q3: What does current epidemiological data reveal about the prevalence of the Somogyi effect?
A3: Recent data from a 2025 study using Continuous Glucose Monitoring (CGM) provides the most current prevalence figures. The table below summarizes key epidemiological metrics.
| Metric | Finding | Source / Study Details |
|---|---|---|
| Overall Prevalence in T1DM | 32.8% of patients experienced at least one episode of Post-Hypoglycemic Nocturnal Hyperglycemia (PHNH) over 14 days [24] | N = 755 T1DM patients using FreeStyle Libre 2 CGM [24] |
| Associated Glycemic Control | Patients with PHNH had longer Time Above Range, shorter Time in Range, and higher glucose variability than those with nocturnal hypoglycemia alone [24] | Cross-sectional study [24] |
| Controversy & Evidence | Some clinical studies and reviews dispute the theory, finding no causal link between nocturnal hypoglycemia and subsequent daytime hyperglycemia [1] | Earlier studies observed high nighttime glucose rather than low in patients with morning hyperglycemia [1] |
Q4: What are the primary risk factors associated with Post-Hypoglycemic Nocturnal Hyperglycemia (PHNH)?
A4: A 2025 study identified specific patient factors linked to a higher likelihood of experiencing PHNH. The table below lists these associated factors.
| Associated Factor | Description |
|---|---|
| Younger Age | Patients with PHNH were significantly younger [24] |
| Higher Insulin Doses | Use of higher total daily doses of insulin [24] |
| Insulin Therapy (T2DM) | Insulin use is a primary risk factor for hypoglycemia, a prerequisite for PHNH [25] [26] |
| Longer Diabetes Duration | Duration greater than 13.7 years is a key predictor of hypoglycemia [26] |
| Renal Impairment | Reduced estimated glomerular filtration rate (eGFR < 60.2 mL/min/1.73 m²) [26] |
Experimental Protocols for Investigating the Somogyi Effect
Protocol 1: Establishing Phenomena Prevalence with CGM
This protocol outlines the methodology used in a recent study to determine the frequency of PHNH [24].
- 1. Objective: To determine the frequency and associated factors of post-hypoglycemic nocturnal hyperglycemia (PHNH) in patients with Type 1 Diabetes.
- 2. Study Design: Cross-sectional observation of CGM data.
- 3. Population:
- Inclusion: Patients with T1DM (defined by positivity for pancreatic islet autoantibodies and insulin requirement), age ≥18 years, sensor usage ≥70%.
- Exclusion: Patients with stage 1 T1DM, those under 18 years, and pregnant women.
- 4. Data Collection & Tools:
- Primary Tool: FreeStyle Libre 2 CGM system [24].
- Period: Analyze a consecutive 14-day period of CGM data.
- Platform: Use cloud-based platform (e.g., LibreView) to collect glucose data.
- 5. Operational Definitions:
- Nocturnal Hypoglycemia: A glucose value <70 mg/dL recorded between 0:00 am and 6:00 am.
- PHNH Episode: Nocturnal hypoglycemia followed by a glucose value >180 mg/dL before 6:00 am.
- 6. Data Analysis:
- Categorize patients into three groups: (1) No nocturnal hypoglycemia, (2) Nocturnal hypoglycemia without hyperglycemia, (3) ≥1 PHNH episode.
- Compare glycemic metrics (Time in Range, Time Above Range, glucose variability) and patient characteristics (age, insulin dose) between groups using appropriate statistical tests (e.g., chi-square, Mann-Whitney U test) [24].
Protocol 2: Differentiating Dawn Phenomenon vs. Somogyi Effect in Individuals
This protocol provides a step-by-step guide for diagnosing the cause of morning hyperglycemia in a clinical research setting [3] [20].
- 1. Objective: To identify the etiology (Dawn Phenomenon vs. Somogyi Effect) of unexplained morning hyperglycemia in an individual subject.
- 2. Materials:
- Continuous Glucose Monitor (CGM) OR blood glucometer and test strips.
- Blood glucose and symptom log.
- 3. Procedure:
- Step 1: Instruct the subject to maintain their usual evening routine regarding diet, medication, and exercise.
- Step 2: Schedule blood glucose measurements (if not using CGM) at the following times:
- Two hours after the evening meal.
- At bedtime (e.g., 10:00-11:00 PM).
- Between 2:00 AM and 4:00 AM.
- Immediately upon waking.
- Step 3: If using CGM, ensure the device is active and functioning to automatically capture this data [24] [20].
- Step 4: Repeat this process for 3-7 nights to establish a pattern.
- 4. Data Interpretation:
- Consistent Low at 2:00-4:00 AM → High on Waking: Pattern consistent with the Somogyi effect.
- Normal at 2:00-4:00 AM → Steady Rise until Waking: Pattern consistent with the dawn phenomenon.
- High at All Measurement Points: Indicates general insulin insufficiency or dietary factors.
The Scientist's Toolkit: Essential Research Reagents and Materials
The table below details key tools and materials for conducting research on the Somogyi effect and related glycemic phenomena.
| Tool / Material | Function in Research |
|---|---|
| Continuous Glucose Monitor (CGM) | Core tool for capturing interstitial glucose levels continuously, enabling detection of asymptomatic nocturnal hypoglycemia and precise tracking of glycemic rebounds [24] [20]. |
| Cloud-Based Data Platforms (e.g., LibreView) | Facilitates the aggregation and analysis of large-scale CGM data from study participants, allowing for remote monitoring and data export [24]. |
| Standardized Hypoglycemia Definition | Critical for consistent phenotyping. Level 1: <70 mg/dL; Level 2: <54 mg/dL; Level 3: severe event requiring assistance [25] [26]. |
| Immunoassay Kits | For measuring counterregulatory hormones (glucagon, cortisol, growth hormone, epinephrine) to objectively validate the physiological response following hypoglycemia [1]. |
| Machine Learning Algorithms | Used to analyze complex, non-linear relationships between multiple risk factors (e.g., insulin dose, eGFR, age) and the incidence of hypoglycemia/PHNH in large datasets [26]. |
Advanced Methodologies for Investigating and Quantifying Rebound Hyperglycemia
The Role of Continuous Glucose Monitoring (CGM) in Phenomenon Detection
Scientific Context: CGM and the Somogyi Effect
What is the Somogyi effect and why is it a topic of research?
The Somogyi effect, also known as rebound hyperglycemia, is a theory proposing that nocturnal hypoglycemia (low blood sugar) triggers a counter-regulatory hormonal response (e.g., adrenaline, cortisol, growth hormone, glucagon), leading to hyperglycemia (high blood sugar) by morning [1] [3]. This phenomenon was named after Dr. Michael Somogyi, who described it in the 1930s [1]. For researchers, the effect highlights a complex physiological interplay between hypoglycemia and subsequent hyperglycemia, which is crucial for understanding glycemic variability and optimizing diabetes therapeutics [1] [3].
What is the current scientific consensus on the Somogyi effect?
Recent evidence from studies utilizing Continuous Glucose Monitoring (CGM) has disputed the validity of the Somogyi effect [1] [3]. Modern research indicates that morning hyperglycemia is more frequently caused by the dawn phenomenon (a natural early-morning release of hormones that increase blood sugar) or simple insulin waning overnight [1] [27]. A key study concluded that nocturnal hypoglycemia did not cause daytime hyperglycemia and found no correlation between daytime glucose levels and counter-regulatory hormones [1]. This ongoing debate underscores the importance of precise measurement tools like CGM in clinical and research settings.
CGM Troubleshooting Guide for Research Settings
What are the first steps if a research CGM sensor fails?
If a sensor fails or an applicator malfunctions during a study:
- Do not reapply or reuse the sensor [28].
- Document the incident and save the sensor and its packaging for the manufacturer's analysis [28].
- Contact the manufacturer immediately for a replacement. Provide the sensor's serial number and details of the failure [28] [29].
Table 1: Manufacturer Contact Information for Research Device Support
| Manufacturer | CGM Models | Support Contact |
|---|---|---|
| Abbott | FreeStyle Libre | 1800 801 478 [29] |
| Dexcom | Dexcom G-series | 1300 851 056 [29] |
| Medtronic | Guardian Connect | 1800 777 808 [29] |
How can we prevent sensors from detaching during long-term studies?
Proper adhesion is critical for data integrity. To ensure sensors remain secure:
- Skin Preparation: Clean the application site with an alcohol wipe and allow it to dry completely. Avoid using lotions or oils beforehand [28].
- Adhesive Enhancers: Use approved liquid adhesives or adhesive patches over the sensor for extra security, especially in studies involving exercise or water exposure [28] [29].
- Site Selection: Rotate application sites to avoid skin irritation, and choose areas less likely to be bumped or rubbed [28] [29].
How should we address signal loss between the CGM and receiver?
Signal loss can create gaps in research data. To troubleshoot:
- Proximity: Ensure the receiver (e.g., smartphone) is within 5-6 meters of the sensor [29].
- Bluetooth: Toggle the Bluetooth function on the receiver off and back on [28].
- Interference: Check for and mitigate potential electromagnetic interference from other lab equipment [29].
- Pressure: Avoid applying direct pressure to the sensor, as this can disrupt signals [28].
What steps ensure the accuracy of CGM data in a clinical trial?
To maintain data accuracy and reliability:
- Verify with Blood Glucose Meter (BGM): If CGM readings seem erratic or improbable, compare them with a fingerstick BGM measurement, especially during rapid glucose fluctuations, as CGM readings can lag behind blood glucose by 5-10 minutes [30] [29] [27].
- Check Sensor Warm-up: Ensure the sensor has completed its initial warm-up period (typically up to 2 hours) before recording data [29].
- Monitor Sensor Lifespan: Replace sensors at or before the end of their recommended usage period (usually 7-14 days) [29].
- Environmental Controls: Protect sensors from extreme temperatures, humidity, and direct sunlight [29].
Interpreting CGM Data for Phenomenon Detection
What are the key CGM metrics for analyzing glycemic patterns?
CGM provides standardized metrics that are essential for quantifying glucose control in study participants. A minimum of 14 days of data with at least 70% sensor wear is recommended for a reliable assessment [30] [27].
Table 2: Core CGM Metrics for Clinical Research
| Metric | Definition | Research Significance / Target |
|---|---|---|
| Time in Range (TIR) | % of readings/day within 70-180 mg/dL [30] [27] | Primary outcome for therapy efficacy. Goal >70% [27]. |
| Time Below Range (TBR) | % of readings/day <70 mg/dL (Level 1) and <54 mg/dL (Level 2) [30] | Key for Somogyi hypothesis. Measures hypoglycemia exposure. Goal <4% [27]. |
| Time Above Range (TAR) | % of readings/day >180 mg/dL (Level 1) and >250 mg/dL (Level 2) [30] | Measures hyperglycemia exposure. Goal <25% [27]. |
| Glucose Management Indicator (GMI) | Estimated A1C derived from mean CGM glucose [30] | Predicts lab-measured A1C for long-term control assessment. |
| Coefficient of Variation (CV) | (Standard Deviation / Mean Glucose) * 100 [30] | Measures glycemic variability. A CV <36% indicates stable glucose [30]. |
How do I use trend arrows to detect rapid glucose changes?
CGM trend arrows provide real-time direction and velocity of glucose change, which is critical for identifying rapid shifts that might be associated with rebound phenomena [31].
Table 3: Interpretation of CGM Trend Arrows
| Trend Arrow | Interpretation (Change per 30 min) | Research Context |
|---|---|---|
| Rising Rapidly | >90 mg/dL / >5.0 mmol/L [31] | Potential indicator of counter-regulatory hormone surge. |
| Rising | 60-90 mg/dL / 3.3-5.0 mmol/L [31] | Monitor for sustained upward trend. |
| Rising Slowly | 30-60 mg/dL / 1.7-3.3 mmol/L [31] | Common after meals; baseline rate. |
| Stable | Changing <30 mg/dL / <1.7 mmol/L [31] | Steady state; ideal baseline condition. |
| Falling Slowly | -30 to -60 mg/dL / -1.7 to -3.3 mmol/L [31] | Monitor for progression to hypoglycemia. |
| Falling | -60 to -90 mg/dL / -3.3 to -5.0 mmol/L [31] | May require intervention in a study protocol. |
| Falling Rapidly | >-90 mg/dL / >-5.0 mmol/L [31] | Critical for Somogyi trigger; indicates significant hypoglycemic event. |
What is the standard method for visualizing CGM data patterns?
The Ambulatory Glucose Profile (AGP) is the consensus standard for visualizing retrospective CGM data [30] [27]. This single-page report collapses 14 days of data into a single 24-hour graph, providing a modal day view that highlights patterns of hypoglycemia, hyperglycemia, and variability [27].
Experimental Protocols for Somogyi Effect Research
What is a standard protocol for investigating overnight glycemic patterns?
Objective: To detect and correlate nocturnal hypoglycemic events with morning hyperglycemia. Methodology:
- Participant Selection: Recruit insulin-dependent diabetic subjects.
- CGM Deployment: Apply a research-grade CGM device. Ensure proper calibration if required.
- Data Collection Period: Collect continuous glucose data for a minimum of 14 nights [30] [27].
- Supplementary Measurements: For validation, schedule periodic fingerstick blood glucose measurements at: Two hours after evening meal, Before bedtime, 2:00 AM - 4:00 AM, Upon waking [3].
- Data Points: Record diet, evening exercise, and insulin dosing.
Analysis:
- Use the AGP report to identify recurring patterns.
- Quantify the frequency of nocturnal hypoglycemia (glucose <70 mg/dL and <54 mg/dL) and the corresponding morning glucose values [30].
- Statistically analyze the correlation between nocturnal hypoglycemia and morning hyperglycemia.
How can we differentiate the Somogyi effect from the dawn phenomenon?
This protocol uses CGM data to distinguish between two causes of morning hyperglycemia.
Table 4: Differential Diagnosis Using CGM Data
| Characteristic | Somogyi Effect | Dawn Phenomenon |
|---|---|---|
| Overnight Pattern | Documented hypoglycemia (e.g., <70 mg/dL) between 2:00 AM - 4:00 AM [3]. | Stable glucose followed by a rise in the early morning (e.g., ~3:00 AM - 8:00 AM) [1]. |
| Morning Glucose | Hyperglycemia upon waking [3]. | Hyperglycemia upon waking [1]. |
| Primary Cause | Rebound from hypoglycemia due to counter-regulatory hormones [1]. | Natural circadian release of growth hormone, cortisol, etc. [1]. |
| Research Implication | May indicate excessive insulin therapy overnight. | May indicate insufficient insulin therapy overnight [1]. |
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Materials and Reagents for CGM-Based Investigations
| Item | Function in Research | Example Brands/Models |
|---|---|---|
| Professional CGM Systems | Clinic-owned devices for intermittent, standardized assessment of glucose patterns in study cohorts [27]. | Abbott FreeStyle Libre Pro, Dexcom G6 Pro, Medtronic iPro2 [27]. |
| Real-Time Personal CGM | For longitudinal studies requiring continuous patient feedback and real-time data collection [27]. | Dexcom G7, Abbott FreeStyle Libre 3, Medtronic Guardian Connect [28] [27]. |
| CGM Adhesive Patches | Secures the sensor for the entire wear duration, critical for data integrity in studies involving sweat or water [28]. | Various overpatches from Skin Grip, Lexcam, Fixic [28]. |
| Liquid Skin Adhesive | Enhances sensor adhesion and prevents premature detachment; essential for rigorous trials [28] [29]. | Products like Skin-Tac [28]. |
| Adhesive Remover | Safely removes sensors without damaging the skin, important for participant compliance in long-term studies [28] [29]. | Wipes containing isopropyl alcohol or specialized solutions [28]. |
| Standardized AGP Report Software | Generates consensus-based reports for uniform data analysis and presentation across research sites [30] [27]. | Software from CGM manufacturers (LibreView, Clarity, CareLink) [27]. |
| Blood Glucose Meter (BGM) | Provides fingerstick reference values to validate CGM accuracy during the study period [29]. | Contour Next One, Accu-Chek Guide, OneTouch Verio [29]. |
FAQs on Rebound Hyperglycemia (Somogyi Effect)
What is the operational definition of a Rebound Hyperglycemia (RH) event for clinical research?
An RH event is quantitatively defined as any series of one or more sensor glucose values (SGVs) >180 mg/dL that starts within two hours of an antecedent SGV <70 mg/dL [32]. Studies may also analyze a severe subset of these events, defined as hyperglycemia following an SGV nadir of <55 mg/dL [32].
What are the standard metrics for quantifying Rebound Hyperglycemia in study populations?
Research quantifies RH using three primary metrics, which allow for objective comparison between study phases or treatment groups. The table below summarizes typical findings from a real-world analysis [32].
| Metric | Definition | Example Baseline Value (Mean) | Example Reduction with Intervention |
|---|---|---|---|
| Frequency | Number of RH events per week per patient [32]. | 2.39 events/week (after hypoglycemia <70 mg/dL) [32] | 14% with rtCGM use [32]. |
| Duration | Consecutive minutes of SGVs >180 mg/dL following hypoglycemia [32]. | 215 minutes (after hypoglycemia <70 mg/dL) [32] | 12% with rtCGM use [32]. |
| Severity | Area under the curve (AUC) for glucose concentration >180 mg/dL (mg/dL × min) [32]. | 15,476 mg/dL × min (after hypoglycemia <70 mg/dL) [32] | 23% with rtCGM use [32]. |
How does the prevalence of post-hypoglycemic nocturnal hyperglycemia (PHNH) characterize a study cohort?
A 2024 study of 755 users of the FreeStyle Libre 2 CGM system found that 32.8% (248 patients) experienced at least one episode of PHNH (a specific form of RH) over a 14-day observation period [24]. This metric helps define the scale of the problem within a population. The study further characterized these patients as having poorer overall glycemic control, including longer time above range and higher glucose variability, compared to those with nocturnal hypoglycemia not followed by hyperglycemia [24].
What is the pathophysiological sequence of the Somogyi effect? The following diagram illustrates the theorized sequence of events leading to rebound hyperglycemia, driven by the body's counter-regulatory response.
Experimental Protocols & Methodologies
Protocol: Assessing Impact of Real-Time CGM (rtCGM) on RH
Objective: To evaluate the efficacy of real-time continuous glucose monitoring (rtCGM) in mitigating the frequency, duration, and severity of rebound hyperglycemia [32].
Population: Hypoglycemia-unaware individuals with type 1 diabetes (e.g., n=75 as in the HypoDE trial) [32].
- Inclusion Criteria: Type 1 diabetes, impaired awareness of hypoglycemia or recent history of severe hypoglycemia, use of multiple daily insulin injections [32].
- Intervention Group: Uses an rtCGM system (e.g., Dexcom G5/G6) with alerts enabled [32].
Study Design:
- Baseline Phase (4 weeks): Participants wear a blinded rtCGM. Data is collected but not visible to them [32].
- Intervention Phase (4 weeks): Participants wear an unblinded rtCGM and use the system's predictive alerts [32].
- Data Analysis: RH events are identified and quantified from CGM data. Within-patient comparisons of RH metrics (frequency, duration, severity) between the baseline and intervention phases are performed using paired t-tests [32].
Protocol: Analyzing Nocturnal Glycemic Profiles for PHNH
Objective: To determine the prevalence and associated factors of post-hypoglycemic nocturnal hyperglycemia (PHNH) in a type 1 diabetes cohort using CGM [24].
Population: Large cohort of CGM users with type 1 diabetes (e.g., n=755 with FreeStyle Libre 2) [24].
- Inclusion Criteria: Diagnosis of T1DM, sensor usage ≥70% over a 14-day period [24].
Methodology:
- Data Extraction: Nocturnal (00:00 - 06:00) glycemic profiles are analyzed over 14 days via a cloud-based platform (e.g., LibreView) [24].
- Event Classification: Patients are categorized into:
- No nocturnal hypoglycemia
- Nocturnal hypoglycemia only (SGVs <70 mg/dL not followed by hyperglycemia before 6:00 am)
- PHNH Group (≥1 episode of nocturnal hypoglycemia followed by SGV >180 mg/dL before 6:00 am) [24].
- Statistical Analysis: Compare patient characteristics, insulin therapy, and overall glycemic control (Time in Range, glucose variability) between groups using chi-square, Mann-Whitney tests, and multivariate logistic regression [24].
The workflow for this analysis is standardized as follows:
The Scientist's Toolkit: Research Reagent Solutions
| Research Tool | Function in RH Research |
|---|---|
| Real-Time CGM (e.g., Dexcom G6) | Provides continuous interstitial glucose measurements. The "Urgent Low Soon" predictive alert warns of impending hypoglycemia, enabling study of its preventive effect on RH [32]. |
| Intermittently Scanned CGM (e.g., FreeStyle Libre 2) | Enables large-scale, real-world observational studies of nocturnal glycemic patterns and PHNH prevalence through cloud-based data aggregation [24]. |
| Blinded CGM (e.g., Dexcom G4 with Software 505) | Serves as a critical control tool during baseline study phases to collect data without influencing patient behavior, establishing a within-subject comparative baseline [32]. |
| Cloud Data Platforms (e.g., LibreView) | Facilitates the collection, aggregation, and analysis of anonymized, large-scale CGM data from real-world users for epidemiological studies on RH [24]. |
| Counter-Regulatory Hormone Assays | Used in mechanistic studies to measure plasma levels of glucagon, epinephrine, cortisol, and growth hormone to validate the physiological response to induced hypoglycemia [1] [2]. |
Predictive Algorithms for Hypoglycemia and Mitigation of Subsequent Hyperglycemia
FAQs: Algorithm Development and Clinical Application
Q1: What types of data are most critical for building predictive models for hypoglycemia?
The most effective predictive models integrate multiple data types. Continuous Glucose Monitoring (CGM) data is foundational, providing real-time, high-frequency glucose readings [33]. From this signal, short-term (e.g., rate of change in the past hour), medium-term (e.g., standard deviation over 2-4 hours), and long-term features (e.g., percentage of time in hypo-/hyperglycemia) can be extracted [33]. Electronic Health Record (EHR) data adds crucial context, including laboratory results (e.g., HbA1c, serum creatinine), demographic information, and medication use [34] [35]. For enhanced accuracy, contextual data on insulin delivery and carbohydrate intake can be incorporated, though its impact is more pronounced for longer prediction horizons [33].
Q2: What is the typical performance of current machine learning models in predicting hypoglycemia?
Model performance varies based on the prediction horizon and data sources. The table below summarizes key performance metrics from recent studies.
Table 1: Performance Metrics of Hypoglycemia Prediction Models
| Study Context | Prediction Horizon | Sensitivity | Specificity | AUC | Key Algorithm(s) |
|---|---|---|---|---|---|
| Youth with T1D (CGM data) [33] | 30-minute | >91% | >90% | - | Machine Learning (Feature-based) |
| Youth with T1D (CGM data) [33] | 60-minute | >91% | >90% | - | Machine Learning (Feature-based) |
| Hospitalized Patients (EHR data) [34] | 7-hour (median) | 59.0% | 98.9% | - | Gradient Boosted Trees |
| Hospitalized T2DM Patients (EHR data) [35] | - | - | - | 0.960 | Random Forest |
Q3: How can researchers validate the occurrence of the Somogyi effect in a clinical study?
Validation requires frequent blood glucose monitoring to detect the characteristic pattern of nocturnal hypoglycemia followed by morning hyperglycemia [3] [4] [16]. The recommended protocol is to measure blood glucose at the following times:
- Before bed [3]
- Between 2:00 a.m. and 3:00 a.m. (or during the peak action time of evening insulin) [3] [4] [16]
- Upon waking [3]
A diagnosis of the Somogyi effect is suggested by low blood sugar (<4.0 mmol/L or 70 mg/dL) at the nighttime check and high blood sugar upon waking [4] [16]. Using Continuous Glucose Monitoring (CGM) is the most robust method, as it provides a continuous record of glucose fluctuations throughout the night [3] [33].
Q4: What are the primary challenges in differentiating the Somogyi effect from the dawn phenomenon?
The core challenge is that both conditions present with the same clinical finding: hyperglycemia upon waking [3] [1]. However, their underlying mechanisms are fundamentally different. The Somogyi effect is a rebound phenomenon triggered by nocturnal hypoglycemia, which stimulates a counter-regulatory hormone response [3] [1]. In contrast, the dawn phenomenon is a natural rise in blood sugar in the early morning due to circadian hormone secretion (e.g., growth hormone, cortisol) and is not preceded by hypoglycemia [3] [1] [16]. The only way to distinguish them is through nighttime glucose measurement [16].
Experimental Protocols
Protocol for Developing a Multiclass Blood Glucose Decompensation Prediction Model from EHR Data
This protocol is based on a large-scale retrospective study using EHR data to predict hypoglycemia and hyperglycemia [34].
1. Study Design and Cohort Selection:
- Design: Conduct a retrospective cohort study.
- Data Source: Use anonymized hospital admission data from a defined period.
- Inclusion Criteria: Include admissions for adult inpatients (≥18 years) with at least one laboratory BG measurement and one of the following:
- A diagnosis of diabetes or related syndrome (using ICD codes).
- Administration of an antidiabetic drug (ATC code A10).
- An extreme BG measurement (<4.0 or ≥11.1 mmol/L) regardless of diagnosis [34].
2. Data Preprocessing and Cleaning:
- Deduplication: Remove duplicate records based on unique case identifiers [34].
- Variable Cleaning:
3. Outcome Definition:
- Define Blood Glucose (BG) decompensation events using the following categories [34]:
- Category 0 (Nondecompensated): BG ≥3.9 to ≤10 mmol/L
- Category 1 (Hypoglycemia): BG <3.9 mmol/L
- Category 2 (Mild Hyperglycemia): BG >10 to ≤13.9 mmol/L
- Category 3 (Moderate Hyperglycemia): BG >13.9 to ≤16.7 mmol/L
- Category 4 (Severe Hyperglycemia): BG >16.7 mmol/L
4. Feature Engineering:
- For each patient admission, use data from a defined "look-back window" prior to a decompensation event.
- For each laboratory analyte in the EHR, calculate derived statistics to capture patient status, including [34]:
- Central Tendency & Spread: Mean, Standard Deviation (SD), Interquartile Range (IQR)
- Range and Extremes: Total range, Minimum value, Maximum value
- Temporal Trends: Recent trend, Most recent value
- Frequency: Analysis count
5. Model Training and Evaluation:
- Algorithm: Employ a second-level ensemble of gradient-boosted binary trees [34].
- Validation: Use appropriate cross-validation techniques suitable for time-series patient data.
- Key Metrics: Evaluate model performance using Specificity and Sensitivity for each decompensation category. Calculate the median prediction horizon (the time between the prediction and the actual event) [34].
Diagram 1: EHR Model Development Workflow
Protocol for a Feature-Based Machine Learning Model Using CGM Data
This protocol details the process for developing a model to predict short-term hypoglycemia risk from CGM data [33].
1. Data Collection:
- Source: Collect CGM data from patients under normal living conditions over an extended period (e.g., 90 days).
- Contextual Data: If available, collect corresponding data on insulin delivery (e.g., from insulin pumps) and carbohydrate intake [33].
2. Feature Extraction:
- Extract a comprehensive set of features from the CGM time-series signal. The following table catalogs a recommended set of features [33].
Table 2: Feature Categories for CGM-Based Prediction Models
| Category | Description | Example Features |
|---|---|---|
| Short-Term | Captures patterns within the last hour. | Current glucose; Difference in glucose from 10, 20, 30 mins ago; Slope over 1 hour [33]. |
| Medium-Term | Captures patterns from 1 to 4 hours prior. | Standard deviation of glucose over 2 & 4 hours; Slope over 2 hours [33]. |
| Long-Term | Captures patient-specific control patterns. | % of time below 70 mg/dL or above 200 mg/dL; Number of "rebound" highs/lows [33]. |
| Snowball Effect | Captures accruing effects of glucose changes. | Sum of all increments/decrements in the last 2 hours; Maximum increase/decrease [33]. |
| Demographic | Static patient characteristics. | Age group, gender, diabetes duration, last HbA1c [33]. |
| Contextual | Temporal and behavioral data. | Time of day, day of week, insulin-on-board, carbohydrate-on-board [33]. |
3. Model Development:
- Parsimonious Feature Selection: Identify the most influential subset of features to avoid overfitting.
- Algorithm Selection: Implement a machine learning classifier (e.g., Logistic Regression, Random Forest, XGBoost).
- Outcome Definition: Define the prediction task as a binary classification: will the patient experience hypoglycemia (BG <70 mg/dL) within a specific time horizon (e.g., 30 or 60 minutes)? [33].
4. Model Evaluation:
- Assess model performance using Sensitivity and Specificity.
- Evaluate the added value of contextual data (insulin/carbs) by comparing model performance with and without these features [33].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Hypoglycemia Prediction and Rebound Hyperglycemia Research
| Item / Resource | Function / Application in Research |
|---|---|
| Continuous Glucose Monitoring (CGM) System | Provides high-frequency, real-time interstitial glucose measurements. It is the primary data source for feature extraction in short-term prediction models and is critical for validating nocturnal hypoglycemia in Somogyi effect studies [3] [33]. |
| Electronic Health Record (EHR) Data | Serves as a source of longitudinal patient data for developing predictive models, including lab results, diagnoses, medications, and demographics. Essential for risk stratification and studying long-term outcomes [34] [35]. |
| Gradient Boosted Trees (XGBoost) | A powerful machine learning algorithm frequently used for structured data (like EHRs). It effectively handles complex, non-linear relationships between multiple clinical variables to predict events like hypoglycemia [34] [35]. |
| Random Forest (RF) Algorithm | An ensemble machine learning method that builds multiple decision trees. It has shown high accuracy and AUC in predicting hypoglycemia severity in hospitalized patients, often outperforming other models [35]. |
| Medical Dictionary for Regulatory Activities (MedDRA) | A standardized, international medical terminology used for coding and analyzing adverse event reports, such as those in pharmacovigilance studies of insulin therapies [36]. |
| FDA Adverse Event Reporting System (FAERS) | A public database containing spontaneous reports of adverse drug events. Used for post-marketing safety surveillance to identify potential rare or long-term adverse effects of antidiabetic drugs [36]. |
Signaling Pathway: Somogyi Effect Hypothesized Mechanism
The following diagram illustrates the theorized physiological pathway of the Somogyi effect, as originally proposed.
Diagram 2: Somogyi Effect Pathway
Analytical Frameworks for Nocturnal Glucose Data in Large Cohorts
FAQs: Troubleshooting Common Research Challenges
Q1: What is the primary analytical challenge in confirming the Somogyi effect in large datasets? The primary challenge is differentiating the Somogyi effect from the more common Dawn Phenomenon, as both present with morning hyperglycemia. The Somogyi effect is theorized to be a rebound from nocturnal hypoglycemia, while the Dawn Phenomenon is attributed to a natural surge of counter-regulatory hormones in the early morning without a preceding hypoglycemic event [3] [1]. Analysis requires high-frequency nocturnal glucose data to confirm or rule out a hypoglycemic episode, which was often missing in older studies.
Q2: What does current evidence suggest about the prevalence of the Somogyi effect? Recent studies using Continuous Glucose Monitoring (CGM) suggest the Somogyi effect is rare [2]. Research on Type 1 diabetic patients indicates that nocturnal hypoglycemia is more frequently associated with low morning glucose, not hyperglycemia, which refutes the classic Somogyi theory [1]. One study concluded that finding a low fasting glucose was a better indicator of nocturnal hypoglycemia than a rebound high [2].
Q3: What is a key methodological consideration when building predictive models for nocturnal hypoglycemia? A key consideration is the application of a decision-theoretic criterion to optimize the prediction threshold. This involves balancing the benefit of accurately predicting a true nocturnal hypoglycemia event against the cost of a false alarm, which could lead to unnecessary carbohydrate consumption and subsequent hyperglycemia [37]. This maximizes the clinical utility and net benefit of the algorithm.
Q4: How can researchers validate a predictive model for nocturnal hypoglycemia? Validation should occur in multiple stages. After initial training on a large dataset, the model should be tested on a separate, held-out validation set from a clinical trial. Furthermore, in-silico simulation using a virtual patient population provides a powerful tool to estimate the real-world impact and safety of the intervention (e.g., carbohydrate recommendation) before proceeding to costly clinical trials [37].
Experimental Protocols & Data Analysis
Protocol: Developing a Nocturnal Hypoglycemia Prediction Algorithm
This protocol is based on a study that used a Support Vector Regression (SVR) model to predict overnight minimum glucose [37].
1. Data Collection & Preprocessing:
- Data Sources: Utilize large-scale datasets combining CGM data (readings every 5 minutes) and insulin data (e.g., from insulin pumps). The training dataset used in the cited study included 22,804 valid nights from 124 individuals with T1D [37].
- Data Cleaning: Exclude nights with interventions that confound natural glucose fluctuations, such as meal consumption after 11 PM [37].
- Feature Engineering: Extract relevant features from CGM and insulin data leading up to bedtime. This likely includes metrics like rate of glucose change, total insulin delivered, and time in specific glucose ranges.
2. Model Training & Optimization:
- Algorithm Selection: Train a Support Vector Regression (SVR) model to predict the numerical value of the overnight minimum glucose [37].
- Decision Theory Application: Derive a binary classification threshold (e.g., hypoglycemia at <3.9 mmol/L) by applying a decision-theoretic criterion to maximize the expected net benefit of the prediction, balancing sensitivity and specificity [37].
3. Model Validation:
- Clinical Validation Set: Test the model's performance on a separate, prospectively collected dataset (e.g., from a 4-week clinical trial with 10 participants) [37].
- Performance Metrics: Evaluate using:
- Sensitivity and Specificity for predicting nocturnal hypoglycemia events.
- Correlation (R-value) between predicted and actual minimum glucose.
- Root-Mean-Square Error (RMSE).
- Area Under the Receiver Operating Characteristic Curve (AUC-ROC) [37].
4. In-Silico Impact Assessment:
- Virtual Patient Population: Use a validated computer simulation of a T1D population to test the algorithm's intervention strategy [37].
- Intervention Simulation: Simulate the effect of administering a carbohydrate snack at bedtime when the algorithm predicts hypoglycemia.
- Outcome Measurement: Quantify the potential reduction in nocturnal hypoglycemia and assess the impact on overall time-in-target glucose range [37].
Table 1: Performance Metrics of an SVR Model for Predicting Nocturnal Hypoglycemia
| Metric | Reported Performance | Context / Threshold |
|---|---|---|
| Sensitivity | 94.1% (95% CI: 71.3-99.9) | Predicting nocturnal hypoglycemia (<3.9 mmol/L) [37] |
| AUC-ROC | 0.86 (95% CI: 0.75-0.98) | Discriminatory power for hypoglycemia events [37] |
| Correlation (R) | 0.71 (P < 0.001) | Between predicted and actual minimum glucose [37] |
| Simulated Reduction | 77.0% (P = 0.006) | Reduction in nocturnal hypoglycemia with algorithm use [37] |
Table 2: Key Characteristics of Data Sets Used in Model Development
| Data Set | Subjects (n) | Nights of Data (n) | Purpose |
|---|---|---|---|
| Training Set | 124 | 22,804 | Model training and parameter optimization [37] |
| Validation Set 1 | 10 | 117 | Initial clinical validation [37] |
| Virtual Population | 20 | N/A | In-silico testing of intervention impact [37] |
Signaling Pathways and Conceptual Workflows
Theoretical Pathophysiology of the Somogyi Effect
Experimental Workflow for Predictive Model Development
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Nocturnal Glucose Research
| Item / Tool | Function in Research |
|---|---|
| Continuous Glucose Monitor (CGM) | Provides high-frequency (e.g., every 5 minutes) interstitial glucose measurements, essential for capturing nocturnal trends and asymptomatic hypoglycemia [37] [1]. |
| Insulin Pump Data | Delivers precise timing and dosing information for exogenous insulin, a critical input variable for predictive models [37]. |
| Support Vector Regression (SVR) | A machine learning algorithm effective for regression tasks like predicting continuous numerical values (e.g., overnight minimum glucose) from complex, high-dimensional data [37]. |
| Decision Theoretic Analysis | A framework to select an optimal operational threshold for a predictive model by quantitatively balancing the costs and benefits of true and false predictions [37]. |
| Virtual T1D Population (In-Silico) | A computer-simulated cohort of patients with T1D, used to safely and cost-effectively test and refine interventions and algorithms before human trials [37]. |
| Tidepool Big Data Donation | An example of a large, real-world data repository that provides the substantial datasets needed to train robust machine learning models [37]. |
In Silico Modeling of Intervention Strategies and Outcomes
Troubleshooting Guides
FAQ: Addressing Common In Silico Modeling Challenges
1. How do I troubleshoot unstable simulation results in my glucoregulatory model?
- Issue: Simulation crashes or produces physiologically impossible values (e.g., negative blood glucose).
- Solution:
- Check Numerical Integrator Settings: Reduce the simulation timestep. A timestep that is too large can lead to inaccurate solutions and instability, especially during rapid physiological changes like insulin bolus administration [38].
- Verify Model Parameters: Ensure all parameters (e.g., insulin sensitivity, glucose clearance rates) are within physiological ranges and are consistent across the model. Using parameters from unvalidated sources is a common source of error [39] [38].
- Review Initial Conditions: Start the simulation from a stable, homeostatic state (e.g., fasting blood glucose). Incorrect initial conditions can cause the model to diverge immediately [38].
2. My model fails to replicate clinical observations of the Somogyi effect. What could be wrong?
- Issue: The simulated rebound hyperglycemia is too pronounced, too weak, or non-existent.
- Solution:
- Re-evaluate Counterregulatory Hormone Dynamics: The Somogyi effect is driven by the body's release of hormones like glucagon, epinephrine, cortisol, and growth hormone in response to hypoglycemia [3] [1] [2]. Review and potentially calibrate the sub-models that govern the timing, magnitude, and duration of these hormonal responses [39].
- Confirm Insulin Pharmacokinetics: An inaccurate model of insulin absorption and clearance can lead to incorrect timing of nocturnal hypoglycemia, which is the proposed trigger for the Somogyi effect. Use a validated model for subcutaneous insulin kinetics [39] [2].
- Consider Alternative Hypotheses: Be aware that the Somogyi effect is a debated theory. Recent studies using Continuous Glucose Monitoring (CGM) suggest that morning hyperglycemia is more often caused by the dawn phenomenon or simple insulin waning, rather than a rebound from hypoglycemia [3] [1] [2].
3. How can I validate my in silico model of intervention strategies?
- Issue: Uncertainty about whether model predictions are clinically credible.
- Solution:
- Use Published Clinical Data: Compare your simulation outcomes, such as blood glucose trajectories and hypoglycemia event rates, against data from clinical trials found in the literature [40].
- Perform Face Validation: Have domain experts (e.g., endocrinologists) review the model's input-output behavior to assess its plausibility [39].
- Leverage Model Standards: Where possible, use components from regulatory-body-accepted models, like the FDA-accepted glucose simulator mentioned in the PILGRIM study [40].
Experimental Protocols for Key Studies
Protocol 1: In-Silico Evaluation of Exercise Adjustment Strategies
This protocol is based on the methodology from the 2021 study "Simulation-Based Evaluation of Treatment Adjustment to..." [39].
- 1. Research Question: How do different insulin and carbohydrate adjustment strategies for exercise affect the risk of acute and late-onset hypoglycemia in Type 1 Diabetes?
- 2. Model Setup:
- 3. Simulation Scenarios:
- Interventions: Implement published adjustment strategies (e.g., insulin bolus reduction, additional carbohydrate intake) [39].
- Exercise Modifications: Define a broad range of exercise sessions by varying:
- Intensity: (e.g., moderate, high).
- Duration: (e.g., 30, 45, 60 minutes).
- Timing: Relative to adjacent meals and bedtime [39].
- 4. Outcome Measures:
- Primary: Blood glucose trajectories.
- Secondary: Time-in-range, risk scores for hypo- and hyperglycemia, incidence of acute vs. late-onset hypoglycemia [39].
- 5. Data Analysis: Compare summary measures across all simulation scenarios to identify strategies that minimize risk and factors that impede hypoglycemia prevention [39].
Protocol 2: Feasibility of a Predictive Low Glucose Management (PLGM) System
This protocol is adapted from the PILGRIM study [40].
- 1. Research Question: Can a PLGM system reduce hypoglycemia during exercise in youth with T1D?
- 2. In-Silico Feasibility (Pilot):
- Platform: FDA-accepted glucose simulator with 100 virtual patients [40].
- Intervention: Simulate hypoglycemic challenges with and without the PLGM system active. The system suspends insulin pump delivery based on predicted sensor glucose values [40].
- Comparison: Contrast the PLGM system's performance against a threshold-based Low Glucose Suspend (LGS) system and no suspension [40].
- 3. Clinical Feasibility Study:
- Participants: 22 youth with T1D on insulin pump therapy [40].
- Procedure: Subjects exercise until the PLGM system suspends insulin delivery or a reference blood glucose value reaches the predictive suspension threshold [40].
- Measures: Sensor glucose at suspension, postsuspension nadir glucose, duration of suspension, hypoglycemia prevention rate [40].
Table 1: Performance of Predictive Low Glucose Management (PLGM) vs. Low Glucose Suspend (LGS) in Silico [40]
| Metric | No Suspension | LGS System | PLGM System |
|---|---|---|---|
| Hypoglycemia Reduction (<70 mg/dL) | Baseline | 5.3% reduction | 26.7% reduction |
| Median Duration of Hypoglycemia (min) | Not Specified | 101 | 58 |
Table 2: Clinical Feasibility Outcomes of PLGM During Exercise (n=22) [40]
| Metric | Result (Mean ± SD) |
|---|---|
| Sensor Glucose at Predictive Suspension | 92 ± 7 mg/dL |
| Post-suspension Nadir Glucose (by HemoCue) | 77 ± 22 mg/dL |
| Suspension Duration | 90 ± 35 min |
| Sensor Glucose at Insulin Resumption | 97 ± 19 mg/dL |
| Hypoglycemic Threshold Reached | 73% of patients |
| Hypoglycemia Prevented | 80% of successful experiments |
Research Reagent Solutions
Table 3: Essential Materials for In-Silico Diabetes Research
| Item | Function in Research | Example / Note |
|---|---|---|
| Glucoregulatory Model | Mathematical framework to simulate blood glucose, insulin action, and counterregulatory hormone dynamics. | Core component as described in [39]; can be custom-built or adapted from literature. |
| Continuous Glucose Monitoring (CGM) Data | Used for model calibration, validation, and as an input for predictive algorithms. | Critical for validating nocturnal glucose patterns in Somogyi effect research [3] [1] [40]. |
| Insulin Pharmacokinetic/Pharmacodynamic (PK/PD) Model | Predicts the absorption, distribution, and action of subcutaneously administered insulin. | A two-compartment model is often used [39]. |
| Virtual Patient Cohort | A population of in-silico subjects with varying physiological parameters to test robustness of interventions. | The FDA-accepted simulator used in [40] contained 100 virtual patients. |
| Counterregulatory Hormone Submodel | Models the release and action of hormones (glucagon, epinephrine, cortisol, growth hormone) in response to hypoglycemia. | Essential for investigating the Somogyi effect [39] [1] [2]. |
Signaling Pathways and Experimental Workflows
Proposed Somogyi Effect Pathway
In Silico Experiment Workflow
Troubleshooting Glycemic Instability and Optimizing Therapeutic Strategies
Nocturnal hypoglycemia represents a significant barrier in the development of insulin therapies and diabetes management strategies. For researchers investigating glycemic stability, the overnight period presents a critical challenge due to the complex interplay between exogenous insulin administration and endogenous hormonal rhythms. The prevention of nighttime hypoglycemia is particularly crucial in the context of the Somogyi effect, a theorized phenomenon of rebound hyperglycemia following an untreated hypoglycemic episode, though its clinical significance remains a subject of scientific debate [1] [3]. This technical guide examines evidence-based insulin adjustment protocols and provides detailed experimental methodologies for evaluating intervention efficacy in clinical research settings.
Key Mechanisms and Current Scientific Understanding
Pathophysiological Framework of Nocturnal Hypoglycemia
Nocturnal hypoglycemia occurs when circulating insulin levels exceed metabolic demand during the overnight fasting period. Contributing factors include:
- Excessive basal insulin from long-acting insulin formulations [41]
- Exercise-induced insulin sensitivity, particularly with evening physical activity [42] [41]
- Alcohol consumption which inhibits gluconeogenesis [41]
- Inappropriate prandial insulin dosing for evening meals, with rapid-acting analogs exhibiting activity for 5-6 hours [41]
The Somogyi effect proposes that nocturnal hypoglycemia triggers counterregulatory hormones (cortisol, growth hormone, epinephrine, glucagon), leading to rebound morning hyperglycemia [1] [3]. However, continuous glucose monitoring (CGM) studies have challenged this theory, demonstrating that nocturnal hypoglycemia more frequently results in persistent low glucose or normoglycemia rather than significant rebound [1]. The more commonly observed dawn phenomenon involves early morning hyperglycemia driven by circadian hormonal surges without preceding hypoglycemia [1] [3].
Diagram: Pathophysiological Pathways in Nocturnal Glucose Dysregulation. The schematic illustrates competing theories linking nocturnal hypoglycemia to morning hyperglycemia, with continuous glucose monitoring (CGM) evidence challenging the traditional Somogyi effect hypothesis.
Quantitative Evidence for Insulin Adjustment Strategies
Table 1: Evidence-Based Insulin Dose Adjustment Protocols for Nocturnal Hypoglycemia Prevention
| Adjustment Strategy | Protocol Specifications | Efficacy Outcomes | Study Population |
|---|---|---|---|
| Basal Insulin Reduction | 20% reduction of total daily basal insulin dose [42] | 100% protection from nocturnal hypoglycemia for 24h post-exercise [42] | Type 1 diabetes, MDI regimen (n=10) [42] |
| Bolus Insulin Reduction | 75% reduction pre-exercise; 50% reduction post-exercise meal [42] | No hypoglycemic episodes in first 6h post-exercise [42] | Type 1 diabetes, evening exercise (n=10) [42] |
| Low GI Carbohydrate Strategy | Post-exercise LGI meal + LGI bedtime snack [42] | Protection from early-onset hypoglycemia without postprandial hyperglycemia [42] | Males with type 1 diabetes, HbA1c ≈6.9% [42] |
Experimental Protocols for Nocturnal Hypoglycemia Research
Detailed Methodology: Combined Basal-Bolus Reduction with Carbohydrate Feeding
Objective: To evaluate the efficacy of combined basal insulin reduction with prandial adjustments and LGI carbohydrate feeding in preventing nocturnal hypoglycemia following evening exercise.
Population: Ten male participants with type 1 diabetes (HbA1c: 52.4±2.2 mmol/mol [6.9±0.2%]) treated with multiple daily injections [42].
Protocol Schema:
Diagram: Experimental Workflow for Evening Exercise Hypoglycemia Prevention Study. The protocol compares 80% versus 100% basal insulin dosing under conditions of reduced bolus insulin and low glycemic index (LGI) carbohydrate feeding.
Intervention Arms:
- Control: Regular total daily basal insulin dose (100%; 34±4 IU)
- Intervention: Reduced total daily basal insulin dose (80%; 27±3 IU) [42]
Key Measurements:
- Continuous glucose monitoring (CGM): Interstitial glucose monitored for 24h pre- and post-exercise
- Venous blood samples: Glucose, glucoregulatory hormones, NEFAs, β-hydroxybutyrate, IL-6, TNF-α
- Hypoglycemia definition: Glucose <70 mg/dL (3.9 mmol/L) with severity stratification [43]
Nocturnal Glucose Assessment Protocol
Objective: To determine the etiology of morning hyperglycemia and identify nocturnal hypoglycemic episodes.
Population: Patients with diabetes exhibiting inconsistent morning glucose values [3].
Assessment Schedule:
- Two hours after evening meal
- Before bedtime
- 0200-0300 hours (nocturnal assessment)
- Upon waking [3]
Data Collection:
- Concurrent recording of evening food composition, exercise timing, and insulin dosing
- CGM utilization preferred for dense temporal data collection [3]
Research Reagent Solutions and Essential Materials
Table 2: Key Research Materials for Nocturnal Hypoglycemia Investigations
| Research Tool | Specifications | Research Application | Experimental Notes |
|---|---|---|---|
| Continuous Glucose Monitor (CGM) | Medtronic Paradigm Veo with Enlite sensor [42] | Interstitial glucose monitoring with minimal physiological time lag [42] | Insert in posterolateral abdominal region; calibrate with ≥4 daily capillary tests [42] |
| Long-Acting Insulin Analogs | Insulin glargine or detemir [42] | Basal insulin reduction studies; pharmacokinetic profiling | 20% dose reduction effective for nocturnal hypoglycemia prevention [42] |
| Rapid-Acting Insulin Analogs | Insulin aspart [42] | Prandial insulin adjustment protocols | 75% reduction pre-exercise; 50% reduction post-exercise [42] |
| Low Glycemic Index Carbohydrates | Standardized LGI meals and snacks [42] | Postprandial glycemic response studies | Protection from hypoglycemia without hyperglycemia [42] |
| Hypoglycemia Rescue Agents | Glucagon kits (injection/nasal spray) [44] [43] | Severe hypoglycemia management protocols | Essential for patient safety during experimental protocols |
Frequently Asked Questions: Technical Considerations
Q1: What is the evidence supporting basal insulin reduction for nocturnal hypoglycemia prevention?
A1: A randomized controlled trial demonstrated that reducing total daily basal insulin by 20% (from 34±4 IU to 27±3 IU) in combination with bolus insulin reductions and LGI carbohydrate feeding provided complete protection from nocturnal hypoglycemia for 24 hours following evening exercise. All participants (n=10) in the 80% basal group were protected, versus widespread nocturnal hypoglycemia in the 100% control group [42].
Q2: How does the Somogyi effect influence nocturnal hypoglycemia research design?
A2: While the Somogyi effect theory suggests rebound hyperglycemia follows nocturnal hypoglycemia, recent CGM studies challenge this paradigm. Research designs should account for the possibility that nocturnal hypoglycemia may not consistently produce rebound hyperglycemia, with current evidence suggesting the dawn phenomenon is a more common cause of morning hyperglycemia [1] [3]. This necessitates controlled trials with dense glucose monitoring rather than assuming causal relationships between bedtime hypoglycemia and morning hyperglycemia.
Q3: What are the critical timepoints for glucose assessment in nocturnal hypoglycemia protocols?
A3: Essential assessment timepoints include: 2 hours post-evening meal, bedtime (2200-2300h), nocturnal (0200-0300h), and upon waking. Additional measures during exercise protocols should include pre-exercise, immediate post-exercise, and hourly for 6 hours post-exercise to capture both early and delayed hypoglycemia [42] [3].
Q4: Which patient characteristics increase susceptibility to nocturnal hypoglycemia in clinical trials?
A4: High-risk characteristics include: prior severe hypoglycemia, hypoglycemia unawareness, impaired counterregulatory response, long diabetes duration, renal impairment, and advanced age. Additional factors include evening exercise, alcohol consumption, and inappropriate insulin-to-carbohydrate ratios at evening meals [45] [41] [43].
The strategic reduction of basal insulin by 20% combined with modified bolus dosing and LGI carbohydrate intake represents an evidence-based approach to preventing nocturnal hypoglycemia in research settings. The disputed Somogyi effect hypothesis warrants careful consideration in study design, with CGM as an essential tool for capturing glucose dynamics. Future research should focus on personalized insulin adjustment algorithms incorporating real-time glucose data, exercise timing, and meal composition to optimize glycemic control while minimizing hypoglycemia risk across diverse patient populations.
Avoiding Overtreatment of Hypoglycemia to Prevent Rebound Effects
Troubleshooting Guides and FAQs
Frequently Asked Questions
| Question | Answer |
|---|---|
| What is the primary clinical risk of overtreating hypoglycemia in older adults? | Severe hypoglycemia can lead to adverse events such as falls, seizures, coma, and emergency hospitalizations. It is the second most common adverse drug event from diabetes medications in this population [46]. |
| How can a Somogyi effect be distinguished from the Dawn Phenomenon? | Continuous Glucose Monitoring (CGM) is the primary method. The Somogyi effect is preceded by nocturnal hypoglycemia, while the Dawn Phenomenon is a gradual rise in blood glucose in the early morning without a preceding low [1] [2]. |
| What defines a patient as "potentially overtreated"? | Key criteria include being on insulin or a sulfonylurea, having a most recent A1C <7.0%, and being over 74 years of age or having a diagnosis of dementia or cognitive impairment [47]. |
| Is the Somogyi effect a proven and common cause of morning hyperglycemia? | No. Recent research using CGM has disputed its existence, suggesting it is rare. Studies find nocturnal hypoglycemia is more often followed by low or normal fasting glucose, not hyperglycemia [1] [3] [2]. |
| What is a key intervention to reduce overtreatment in primary care? | Using a Clinical Decision Support (CDS) tool within electronic medical records to identify at-risk patients and facilitate shared decision-making about de-intensifying medication [46] [47]. |
Quantitative Data on Overtreatment and Interventions
Table 1: Impact of a Hypoglycemia Risk Reduction Quality Improvement Initiative [47]
| Metric | Baseline (Pre-Intervention) | 6 Months Post-Intervention | 18 Months Post-Intervention |
|---|---|---|---|
| Monthly average of potentially overtreated patients | 2,513 patients | 18% reduction | 22% reduction |
| Provider Actions via Clinical Reminder | |||
| Total patients screened | - | 2,830 patients | - |
| Overall treatment de-intensification rate | - | 9.6% | - |
| De-intensification rate in patients reporting any hypoglycemia | - | 37% | - |
Table 2: Outcomes from the HypoPrevent Study on a Primary Care Intervention [46]
| Outcome Measure | Result |
|---|---|
| Reduction in the number of older patients at risk for hypoglycemia | 46% |
| Discontinuation of hypoglycemic medications | 20% |
| Patient-reported improvement in daily functioning and well-being | Significant reductions in the negative impact of non-severe hypoglycemia |
Experimental Protocols
Protocol 1: Differentiating Somogyi Phenomenon from Dawn Phenomenon
Objective: To determine the etiology of fasting hyperglycemia in a subject with diabetes.
Methodology:
- Subjects: Patients with diabetes (Type 1 or Type 2) presenting with persistent fasting hyperglycemia.
- Tools: A Continuous Glucose Monitoring (CGM) system is the gold standard. Alternatively, frequent capillary blood glucose testing can be used [3].
- Procedure:
- Measure blood glucose levels at the following times:
- Two hours after the evening meal.
- At bedtime (approx. 10:00 PM).
- Between 2:00 AM and 4:00 AM.
- Immediately upon waking [3].
- Continue this monitoring for 3-5 consecutive nights to establish a pattern.
- Measure blood glucose levels at the following times:
- Data Interpretation:
- Somogyi Phenomenon: A blood glucose value <70 mg/dL is recorded during the 2:00 AM - 4:00 AM measurement, followed by hyperglycemia upon waking [2].
- Dawn Phenomenon: A gradual rise in blood glucose begins after 4:00 AM without any preceding hypoglycemic event (<70 mg/dL) overnight [1].
- Insufficient Insulin: Blood glucose levels remain elevated throughout the entire night without a significant dip [2].
Protocol 2: Implementing a Clinical Decision Support Intervention for Overtreatment
Objective: To systematically identify and reduce the number of older patients at high risk for treatment-related hypoglycemia.
Methodology [47]:
- Patient Identification: Use an electronic medical record (EMR) system to create a report identifying patients meeting all pre-defined "potentially overtreated" criteria.
- Clinical Reminder: Implement an EMR-based prompt that activates during a patient's routine care visit.
- Structured Assessment: The clinical reminder guides the provider through a structured hypoglycemia assessment, asking:
- "In the past few months, how often did the veteran/caregiver report that the veteran had a low blood glucose level?"
- If >0: "In the past few months, how often did the veteran/caregiver report that the veteran had blood glucose low enough to fear passing out?"
- If >0: "Did the veteran/caregiver report that the veteran passed out or fell due to low blood glucose?" and "Did the veteran/caregiver report that the veteran required a visit to the emergency department or hospital because of low blood glucose?"
- Action: Based on the assessment, the provider makes a shared decision with the patient to either:
- "Relax glycemic treatment" (de-intensify), or
- Make "No change in glycemic management at this time."
Physiological Pathway and Intervention Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Hypoglycemia Rebound Research
| Item | Function/Application |
|---|---|
| Continuous Glucose Monitor (CGM) | Provides high-frequency, real-time measurement of interstitial glucose levels, essential for detecting asymptomatic nocturnal hypoglycemia and establishing glucose trends [1] [2]. |
| HbA1C Test | Measures the average blood glucose level over the preceding 2-3 months. Used to identify patients with overall low glycemia who may be at risk for overtreatment [47]. |
| Clinical Decision Support Tool | An EMR-integrated software tool designed to identify patients meeting "potentially overtreated" criteria and guide clinicians through a structured risk-assessment and management protocol [46] [47]. |
| Counterregulatory Hormone Assays | Laboratory tests (e.g., for glucagon, epinephrine, cortisol, growth hormone) used in research to measure the body's hormonal response to a hypoglycemic event [1] [2]. |
| Patient-Reported Outcome Tool (TRIM-HYPO) | A validated questionnaire used to quantify the impact of non-severe hypoglycemic events on a patient's daily functioning, emotional well-being, and diabetes management [46]. |
Technical Support & Troubleshooting Guide
This guide provides technical support for researchers utilizing Continuous Glucose Monitoring (CGM) and insulin pumps in studies investigating nocturnal glycemic phenomena, such as rebound hyperglycemia (Somogyi effect).
Frequently Asked Questions (FAQs)
Q1: Our experimental CGM data shows morning hyperglycemia in rodent models. How can we determine if it's rebound hyperglycemia or the dawn phenomenon? A1: Differentiation requires analyzing nocturnal glucose trends. The key is identifying the presence or absence of a preceding hypoglycemic event.
- Recommended Protocol: Implement continuous glucose monitoring with frequent data logging. For animal studies, this may require telemetric systems. Analyze the trajectory of glucose values from late evening through early morning.
- Data Interpretation:
- Rebound Hyperglycemia (Somogyi Effect): Look for a characteristic sequence: a significant drop in blood glucose (e.g., below 70 mg/dL or 3.9 mmol/L) followed by a surge to hyperglycemic levels. The initial drop is the crucial differentiator [3] [20].
- Dawn Phenomenon: The data will show stable glucose levels or a gradual rise throughout the night without an intervening hypoglycemic event [1] [20]. The rise is driven by a natural surge in cortisol and growth hormone [20].
Q2: What are the primary technical factors that can lead to false hypoglycemic alerts in a CGM system, potentially confounding rebound hyperglycemia research? A2: Several technical and physiological factors can cause inaccurate readings:
- Sensor Calibration: Improper calibration, often due to incorrect blood glucose meter input, is a common source of error. Always use a calibrated and quality-controlled meter for sensor calibration [48] [49].
- Signal Artifacts: Physical pressure on the sensor (pressure-induced sensor attenuation) can cause falsely low readings. Ensure sensors are placed securely and that animal housing or human subjects avoid putting weight on the sensor site.
- Sensor Warm-up Period: Data collected during the initial sensor warm-up period (typically 30 minutes to 2 hours) can be unstable and should be excluded from analysis [50] [48].
- Physiological Lag: CGM measures glucose in interstitial fluid, which lags behind blood glucose by 5-15 minutes, particularly during periods of rapid glucose change. This can affect the precise timing of hypoglycemic nadirs [51].
Q3: How do predictive low-glucose suspend (PLGS) algorithms function, and what is their experimental relevance in hypoglycemia prevention studies? A3: PLGS systems use algorithmic predictions of future glucose levels to proactively suspend insulin delivery.
- Mechanism: The algorithm analyzes the current CGM glucose value and its rate of change. Using a projection horizon (e.g., 30-45 minutes), it forecasts if the glucose level will cross a predefined low threshold (e.g., 80 mg/dL). If so, it signals the insulin pump to suspend basal insulin infusion [51].
- Experimental Evidence: A pilot study demonstrated that using a linear prediction algorithm with an 80 mg/dL threshold and a 45-minute projection horizon prevented 80% of induced hypoglycemic episodes without causing rebound hyperglycemia [51]. This makes PLGS a critical technology for studying the prevention of hypoglycemia and its sequelae.
Q4: In an integrated pump-CGM system, what are the first-line checks if a subject develops unexplained hyperglycemia? A4: Follow a systematic troubleshooting protocol to isolate the cause:
- CGM Verification: Confirm the hyperglycemia with a fingerstick blood glucose meter to rule out a CGM sensor error [49].
- Infusion Set Inspection: Check the infusion set for kinks, dislodgement, occlusions, or air bubbles in the tubing [49].
- Insulin Pump Operation: Verify pump alerts and error logs for occlusion alarms or other malfunction indicators. Ensure the insulin reservoir has not been depleted [48] [49].
- Insulin Integrity: Consider the possibility of insulin degradation due to prolonged exposure to high temperatures or beyond its expiration date [49].
Table 1: Performance Metrics of Commercial CGM Systems in Clinical Studies
| CGM System | Mean Absolute Relative Difference (MARD)* | Sensor Duration (Days) | Warm-up Period | Key Features Relevant to Research |
|---|---|---|---|---|
| Dexcom G7 | 8.2% - 9.1% [50] | 10 [50] | 30 minutes [50] | High accuracy, predictive alerts, continuous data transmission. |
| Abbott Freestyle Libre | 9.2% - 9.7% [50] | 14 [50] | 1 hour [50] | Factory calibrated, no fingerstick calibration required. |
| Medtronic Guardian 4 | 10.1% - 11.2% [50] | 7 [50] | N/A (No-calibration) [50] | Integrated with MiniMed pumps; predictive alerts for closed-loop systems. |
Note: A lower MARD indicates higher accuracy.
Table 2: Efficacy of Predictive Alarms in Hypoglycemia Prevention
| Study Intervention / Algorithm | Threshold (mg/dL) | Projection Horizon | Hypoglycemia Prevention Rate | Notes |
|---|---|---|---|---|
| Statistical Prediction (SP) Alarm [51] | 80 | 30 minutes | 60% | Pilot study on induced hypoglycemia with pump suspension. |
| Linear Prediction (LP) Alarm [51] | 80 | 45 minutes | 80% | Longer projection horizon improved prevention rate. |
| CGM Use in T1D (Real-world) | N/A | N/A | 59% - 72% reduction in hypoglycemic events [50] | Reduction in time spent in hypoglycemia compared to SMBG. |
Experimental Protocols
Protocol 1: Investigating the Somogyi Effect in a Clinical Research Setting
This protocol outlines a method to characterize nocturnal glycemic patterns in human subjects.
- Objective: To differentiate between the Somogyi effect (rebound hyperglycemia) and the dawn phenomenon as causes of morning hyperglycemia.
- Materials:
- Continuous Glucose Monitor (CGM) system (e.g., from Table 1).
- Blood Glucose Meter for verification.
- Insulin pump (if subject is pump-treated).
- Data logging software.
- Methodology:
- Subject Preparation: Recruit subjects with diabetes presenting with consistent morning hyperglycemia. Obtain informed consent.
- CGM Deployment: Apply and calibrate the CGM according to manufacturer instructions.
- Data Collection: Monitor subjects for a minimum of 48-72 hours. Collect continuous glucose data.
- Critical Time Points: For verification without a CGM, manual blood glucose checks should be taken at: a) Two hours after evening meal, b) Bedtime, c) 2:00 AM - 3:00 AM, and d) Upon waking [3] [20].
- Data Analysis: Plot the 24-hour glucose trace. Identify the nadir (lowest point) of glucose overnight. A pattern of hypoglycemia (e.g., glucose <70 mg/dL at nadir) followed by hyperglycemia upon waking supports the Somogyi effect. A stable or gradually rising glucose level from bedtime to morning supports the dawn phenomenon [20].
- Troubleshooting: If data is inconclusive, extend the monitoring period. If CGM signal is lost, rely on verified manual blood glucose readings.
Protocol 2: Evaluating a Predictive Low-Glucose Suspend (PLGS) Algorithm
This protocol is based on a published pilot study for testing hypoglycemia prediction and prevention [51].
- Objective: To assess the efficacy of an algorithm in preventing induced hypoglycemia by suspending insulin pump delivery.
- Materials:
- Real-time CGM (e.g., FreeStyle Navigator was used in the pilot [51]).
- Insulin pump capable of remote suspension.
- Algorithm software (e.g., Linear or Statistical Prediction models).
- Clinical research center setting for supervised hypoglycemic induction.
- Methodology:
- Subject Admission: Subjects are admitted to a clinical research center on two separate days.
- Day 1 (Dose-Finding): Basal insulin infusion rates are increased in ~25% increments until blood glucose declines steadily to <60 mg/dL. This establishes the insulin dose required to induce hypoglycemia.
- Day 2 (Algorithm Test): Basal rates are again increased using the established sensitivity. Real-time CGM data is fed into the prediction algorithm.
- Intervention: When the algorithm predicts a future blood glucose <80 mg/dL, the insulin pump is suspended for a set period (e.g., 90 minutes).
- Outcome Measures: The primary endpoint is the prevention of hypoglycemia (BG <60 mg/dL) during the pump suspension period. Secondary measures include the occurrence of rebound hyperglycemia post-suspension and ketone levels.
- Troubleshooting: If the algorithm fails to prevent hypoglycemia, adjustments to the prediction horizon (e.g., extending from 30 to 45 minutes) or the glucose threshold may be necessary [51].
Signaling Pathways and System Workflows
Pathway: Somogyi Effect vs. Dawn Phenomenon
Workflow: Predictive Low-Glucose Suspend Algorithm
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Technologies for Hypoglycemia Rebound Research
| Item | Function in Research | Example/Notes |
|---|---|---|
| Real-Time CGM System | Provides continuous, high-frequency glucose data crucial for identifying nocturnal hypoglycemic nadirs and hyperglycemic rebounds [50] [52]. | Dexcom G7, Medtronic Guardian 4; select based on MARD and connectivity needs [50]. |
| Insulin Pump (Programmable) | Delivers precise basal insulin rates and can be integrated with CGM and algorithms for automated intervention studies [49] [52]. | MiniMed 770G, Tandem t:slim X2; ensure research-compatible data output. |
| Predictive Low-Glucose Suspend (PLGS) Algorithm | The core logic for forecasting hypoglycemia. Testing and refining these algorithms is a key research area [51]. | Linear extrapolation or statistical model-based algorithms [51]. |
| Blood Glucose Meter | Serves as the gold-standard reference for verifying CGM accuracy and calibrating certain sensor models [49] [52]. | Essential for protocol validation and troubleshooting sensor drift. |
| Data Logging & Analytics Software | For aggregating CGM and pump data, visualizing trends, and calculating metrics like Time in Range (TIR) and hypoglycemic events [50]. | Custom scripts or commercial platforms (e.g., Dexcom CLARITY). |
| Ketone Monitoring Tools | To assess metabolic safety during experimental insulin pump suspensions, preventing diabetic ketoacidosis (DKA) risk [51]. | Blood ketone meter or test strips. |
Frequently Asked Questions (FAQs)
Q1: What is the primary therapeutic role of glucagon in a research setting? Glucagon is a critical counter-regulatory hormone used as an emergency treatment for severe hypoglycemia, particularly in unconscious patients or those unable to take oral carbohydrates [53]. It works by rapidly stimulating hepatic glucose production through glycogenolysis and gluconeogenesis [54].
Q2: What are "stable glucagon analogs" and why are they needed? Stable glucagon analogs are engineered versions of the native hormone designed to have a longer duration of action and greater resistance to enzymatic degradation [55]. Their development is crucial because native glucagon has a very short half-life (typically 1-2 minutes) and is rapidly degraded by enzymes like dipeptidyl peptidase-4 (DPP-4) [56]. These properties make native glucagon unsuitable for chronic management strategies aimed at preventing hypoglycemia.
Q3: How does research on Glucagon-Like Peptide-1 (GLP-1) relate to glucagon studies? GLP-1 is an incretin hormone that counterbalances glucagon. While glucagon raises blood sugar, GLP-1 receptor agonists (GLP-1RAs) lower it by stimulating insulin secretion, suppressing glucagon release, and delaying gastric emptying [55] [56]. Research into dual or triple agonists that target both the GLP-1 receptor (GLP-1R) and the glucagon receptor (GCGR) is a cutting-edge area, as these compounds may offer improved glycemic control and weight loss [56].
Q4: What is the Somogyi effect and how is it investigated pharmacologically? The Somogyi effect is a contested theory proposing that nocturnal hypoglycemia triggers a rebound hyperglycemia in the morning due to a surge in counter-regulatory hormones, including glucagon, cortisol, epinephrine, and growth hormone [1] [3] [54]. Modern research using continuous glucose monitoring (CGM) often fails to confirm this pattern, and the phenomenon is now considered rare compared to the dawn phenomenon (morning hyperglycemia without preceding hypoglycemia) [1] [3]. Pharmacological research involves studying the mechanisms of these counter-regulatory hormones.
Q5: What are common challenges when using GLP-1 receptor agonists in animal studies? The most frequently reported adverse effects are gastrointestinal, including nausea, vomiting, and diarrhea [55] [57]. These symptoms are often dose-dependent and may diminish with ongoing treatment. Researchers should implement dose-titration schedules in experimental protocols to mitigate these effects [57].
Troubleshooting Guides
Issue 1: Inconsistent Glycemic Responses in Somogyi Effect Models
- Potential Cause: Failure to accurately confirm nocturnal hypoglycemia as the trigger for morning hyperglycemia. The Dawn phenomenon is a more common confounder [1] [3].
- Solution: Implement rigorous, frequent blood glucose monitoring, preferably with continuous glucose monitoring (CGM) systems. Take measurements at critical intervals: two hours after an evening meal, at bedtime, in the middle of the night (e.g., 3 a.m.), and upon waking [3]. This data is essential to distinguish a true hypoglycemia-induced rebound from other causes of hyperglycemia.
Issue 2: Instability of Native Glucagon in Experimental Preparations
- Potential Cause: The native glucagon peptide is inherently unstable in solution and prone to fibrillation and aggregation, leading to loss of bioactivity.
- Solution:
- For acute studies, use freshly reconstituted glucagon from lyophilized powder with the appropriate diluent.
- For chronic studies requiring sustained glucagon receptor activation, utilize stable glucagon analogs or dual/triple agonists (e.g., those targeting GLP-1R/GCGR/GIPR) that are engineered for prolonged stability and action [56]. These are typically supplied as stable liquid formulations.
Issue 3: Off-Target Effects of Glucagon Receptor Agonism
- Potential Cause: The systemic activation of the glucagon receptor can lead to undesirable effects such as excessive hyperglycemia, dyslipidemia, and increased energy expenditure [56].
- Solution: Explore the use of biased agonists that selectively activate beneficial signaling pathways (e.g., those promoting glycogenolysis for glucose rescue without adverse metabolic effects) or tissue-targeted agonists that primarily act on the liver.
Experimental Protocols
Protocol 1: Assessing Counter-Regulatory Hormone Response to Hypoglycemia
Objective: To quantify the plasma levels of key counter-regulatory hormones (glucagon, epinephrine, cortisol, growth hormone) following an induced hypoglycemic event in an experimental model. Materials: Experimental model, insulin for hypoglycemia induction, blood collection tubes (EDTA-coated, on ice), centrifuge, specific ELISA or RIA kits for each hormone. Methodology:
- Baseline Sampling: After an overnight fast, collect a baseline blood sample (T=0) [44].
- Hypoglycemia Induction: Administer a standardized dose of intravenous regular insulin (e.g., 0.1 U/kg).
- Serial Sampling: Monitor blood glucose frequently. At the point of confirmed hypoglycemia (e.g., <54 mg/dL or <3.0 mmol/L) [53] [58], collect the second blood sample (T=hypo).
- Recovery Sampling: After treating hypoglycemia with glucose or glucagon, collect additional samples at 30, 60, and 120 minutes post-recovery.
- Analysis: Centrifuge samples immediately to separate plasma. Store at -80°C until analysis. Use specific immunoassays to measure hormone concentrations at all time points.
Protocol 2: Evaluating the Efficacy of a Stable Glucagon Analog in Severe Hypoglycemia
Objective: To compare the efficacy of a novel stable glucagon analog versus native glucagon in reversing insulin-induced severe hypoglycemia. Materials: Animal model, insulin, native glucagon (reconstituted per manufacturer's instructions), stable glucagon analog, blood glucose meter, stopwatch. Methodology:
- Induction: Induce severe hypoglycemia (Blood Glucose < 54 mg/dL) with insulin [58].
- Randomization & Dosing: Randomly assign models to receive either a standard dose of native glucagon or an equimolar dose of the stable glucagon analog via subcutaneous or intramuscular injection [53].
- Monitoring: Measure blood glucose at time points 0 (pre-dose), 10, 20, 30, 45, 60, 90, and 120 minutes post-injection.
- Endpoint: Record the time to reach glycemic recovery (e.g., Blood Glucose > 70 mg/dL) and the duration of normoglycemia before a subsequent drop occurs.
Signaling Pathways and Experimental Workflows
Glucagon Counter-Regulatory Signaling Pathway
Hypoglycemia Rescue Experimental Workflow
Research Reagent Solutions
Table 1: Essential Reagents for Investigating Glucagon Biology and Hypoglycemia
| Reagent / Material | Primary Function in Research |
|---|---|
| Native Glucagon | The gold-standard peptide for establishing baseline bioactivity in rescue assays and for comparative studies with novel analogs [53]. |
| Stable Glucagon Analogs | Engineered peptides with prolonged half-lives; used to study sustained glucagon receptor agonism and for developing chronic therapies [56]. |
| GLP-1 Receptor Agonists (e.g., Liraglutide, Semaglutide) | Tools to study the opposing incretin system, insulin secretion, and gastric emptying. Crucial for research on dual/triple agonists [55] [56]. |
| Glucagon ELISA/RIA Kits | Immunoassays for the precise quantification of glucagon levels in plasma or serum samples during counter-regulatory response studies. |
| Continuous Glucose Monitoring (CGM) Systems | Provides high-resolution, temporal data on glucose fluctuations, essential for validating events like nocturnal hypoglycemia in Somogyi effect research [1] [3]. |
| Specific Insulin Formulations | Used to reliably and safely induce standardized hypoglycemic states in experimental models for rescue and counter-regulatory studies. |
Table 2: Quantitative Data on Hypoglycemia Classification and Glucagon Formulations
| Parameter | Classification / Value | Context / Significance |
|---|---|---|
| Hypoglycemia Alert Level (Level 1) | < 70 mg/dL (3.9 mmol/L) | Threshold for initiating counter-regulatory hormone response; requires intervention with fast-acting carbs [53] [58]. |
| Clinically Significant Hypoglycemia (Level 2) | < 54 mg/dL (3.0 mmolOL) | Level where neuroglycopenic symptoms begin; serious risk and a key threshold in research [53] [58]. |
| Severe Hypoglycemia (Level 3) | No specific glucose value | Event characterized by altered mental/physical status requiring external assistance [58]. This is the primary indication for glucagon rescue [53]. |
| Glucagon Administration Routes | Intramuscular, Subcutaneous, Intravenous, Intranasal | Different routes impact speed of onset and are suited for different experimental or clinical scenarios [53]. |
| Novel Agonist Targets | GLP-1R/GCGR, GLP-1R/GIPR/GCGR | Dual and triple agonists represent the frontier of peptide therapeutics for metabolic disease [56]. |
Troubleshooting Guide: Unexplained Hyperglycemia in Research Settings
Researchers often encounter unexplained hyperglycemia during clinical investigations of glucose metabolism. This guide helps troubleshoot experimental variables and participant-specific factors.
Q1: How should I investigate paradoxical morning hyperglycemia in a study participant?
Consideration: Verify if the hyperglycemia represents the Somogyi effect or dawn phenomenon.
Causes & Corrective Actions:
Probable Cause: The Dawn Phenomenon
- Description: A common early morning rise in blood glucose due to a natural, circadian-driven surge in insulin-antagonist hormones (like growth hormone). It is not preceded by hypoglycemia [1].
- Experimental Protocol: Instruct participants to use Continuous Glucose Monitoring (CGM) to collect nocturnal glucose data. A stable glucose level throughout the night that begins to rise around 4 a.m. to 6 a.m. supports this diagnosis [1].
- Action: In a study context, this may not be a fault condition but a physiological response to be recorded and analyzed.
Probable Cause: Suspected Somogyi Effect (Post-hypoglycemic Hyperglycemia)
- Description: A theoretical paradoxical reaction where nighttime hypoglycemia triggers a counterregulatory hormone response (e.g., adrenaline, cortisol, glucagon, growth hormone), leading to rebound hyperglycemia by morning [1].
- Experimental Protocol: CGM data is essential. Look for a documented hypoglycemic episode (typically between 2 a.m. and 4 a.m.) followed by a steep glucose rise. Recent studies using CGM have disputed this theory, finding nocturnal hypoglycemia is often followed by normal or low morning glucose, not hyperglycemia [1].
- Action: If confirmed, the research intervention (e.g., insulin dosage) may require adjustment to prevent the initial hypoglycemic event.
Probable Cause: Nocturnal Hypoglycemia followed by Overtreatment
- Description: The participant may have experienced a low glucose event and consumed carbohydrates to correct it, resulting in hyperglycemia [59].
- Experimental Protocol: Review participant logs and CGM data for signs of hypoglycemia treatment.
- Action: Reinforce study protocols for the precise treatment of hypoglycemia (typically 15-20 grams of fast-acting carbohydrates).
Consideration: Technical, behavioral, or device-related issues can skew results.
Causes & Corrective Actions:
- Probable Cause: Insulin Delivery Issues
- Description: In studies using insulin pumps, unexplained hyperglycemia can stem from a failure of insulin to reach the systemic circulation [59].
- Experimental Protocol:
- Check for Ketones: In a clinical research setting, test for blood ketones (≥ 0.6 mmol/L) as a sign of prolonged insulin deficiency [59].
- Mechanical Check: Examine the infusion set for occlusions, dislodgement, or a bent cannula. Replace the set and insulin if a problem is suspected [59].
- Insulin Integrity: Verify proper storage of insulin; exposure to extreme temperatures can cause degradation [59].
- Probable Cause: Incorrect Pump or Device Settings
- Description: The basal or bolus insulin settings programmed into the device may be incorrect for the study protocol [59].
- Action: Audit the device settings (clock, basal rates, insulin-to-carbohydrate ratios) against the study's predefined parameters.
- Probable Cause: Glucose Meter Inaccuracy
Q3: What participant-specific factors can confound hyperglycemia research data?
Consideration: Physiological and lifestyle variables must be controlled or documented.
Causes & Corrective Actions:
- Probable Cause: Behavioral and Lifestyle Factors
- Description: Participant-reported data may be incomplete [59].
- Action: Implement rigorous logging for:
- Diet: Under-bolusing for meals, high-fat/protein meals causing delayed glucose rises [59].
- Activity: Decreased physical activity reducing insulin sensitivity [59].
- Sleep: Sleep deprivation or changes in sleep cycles can increase counterregulatory hormone production [59].
- Stress: Elevated stress can raise blood glucose; document periods of high stress [59].
- Probable Cause: Biological Rhythms and Health Status
- Description: Endogenous hormonal cycles or illness can alter glucose metabolism independently of the intervention [59].
- Action: Document:
- Menstrual Cycle: Hormonal fluctuations in the days prior to menses can cause elevated glucose [59].
- Illness/Infection: These can cause significant hyperglycemia and should be noted as an exclusionary event or covariate [59].
- New Medications: Document the use of any new medications, especially steroids [59].
Quantitative Data Synthesis for Experimental Design
The following tables summarize key quantitative data from lifestyle intervention studies and recent clinical trials for experimental comparison.
| Lifestyle Intervention | Maximum Absolute Risk Reduction (%) | Key Risk Factors Modified |
|---|---|---|
| Yoga | 16.7 | SBP: -4.45 mmHg; TC: -17.00 mg/dL; HDL-C: +2.87 mg/dL [60] |
| Walking (Aerobic) | 11.4 | SBP: -3.80 mmHg; TC: -3.48 mg/dL; HDL-C: +2.32 mg/dL [60] |
| Mediterranean Diet | 9.2 | SBP: -1.70 mmHg; TC: -7.35 mg/dL; HDL-C: +0.94 mg/dL [60] |
| Group Therapy (Smoking) | 1.6 | 9.9% probability of quitting smoking (vs. 5% without intervention) [60] |
SBP: Systolic Blood Pressure; TC: Total Cholesterol; HDL-C: High-Density Lipoprotein Cholesterol.
| Technology / Company | Type | Key Feature / Update | Stage (as of ADA 2025) |
|---|---|---|---|
| Dual Glucose-Ketone Sensor (Abbott) | CGM | Single sensor measures both glucose and ketones | Potential launch in 2026 [61] |
| MiniMed 780G (Medtronic) | AID System | Improved glycemic outcomes in T2D and young children | Investigational for T2D, pending FDA approval [61] |
| Control-IQ+ (Tandem) | Algorithm | Next-gen hybrid closed-loop for T:slim X2 & Mobi pumps | Available for T1D (≥2 yrs) and adults with T2D [61] |
| Niia Signature Pump (PharmaSens/SiBionics) | All-in-one AID | Integrated CGM and pump in a single patch device | In development [61] |
| twiist AID System (Sequel Med Tech) | AID System | Directly measures each microdose of insulin delivered | U.S. launch commenced July 2025 [61] |
| Mint System (Beta Bionics) | Insulin Patch Pump | Pharmacy-channel, 3-day use patch pump | Anticipated U.S. launch by end of 2027 [61] |
CGM: Continuous Glucose Monitor; AID: Automated Insulin Delivery; T1D/T2D: Type 1/2 Diabetes.
Experimental Protocols & Methodologies
Protocol 1: Investigating Morning Hyperglycemia
Objective: To differentiate between the Dawn Phenomenon and the Somogyi Effect in a clinical study.
Methodology:
- Participant Preparation: Recruit insulin-dependent diabetic participants. Provide standardized CGMs with continuous data logging capabilities.
- Nocturnal Monitoring: Participants undergo at least 48 hours of CGM monitoring. All other variables (diet, exercise, insulin timing) should be kept as constant as possible.
- Data Analysis: Analyze CGM traces for specific patterns:
- Dawn Phenomenon: Glucose levels are stable between midnight and 3 a.m., then begin a steady rise until waking, with no intervening hypoglycemia [1].
- Somogyi Effect: A distinct hypoglycemic event (e.g., glucose <70 mg/dL) is recorded between 2 a.m. and 4 a.m., followed by a rapid increase in glucose to hyperglycemic levels by morning [1].
- Corroborative Measures: Collect morning fasting blood samples for counterregulatory hormones (cortisol, growth hormone, glucagon) in a subset of participants to biochemically confirm the hyperglycemic response.
Protocol 2: Clustering for Precision Nutrition Studies
Objective: To classify individuals into "lifemetabotypes" based on health, lifestyle, and metabolic traits for targeted interventions [62].
Methodology (Adapted from the NUTRiMDEA Cohort Study):
- Data Collection: Administer a comprehensive online survey capturing:
- Sociodemographics: Age, sex, ethnicity.
- Anthropometrics: Weight, height.
- Metabolic Background: Presence of conditions like diabetes, hypertension.
- Lifestyle Factors: Using validated questionnaires (e.g., IPAQ for physical activity, MEDAS-14 for Mediterranean diet adherence, SF-12 for health-related quality of life) [62].
- Statistical Analysis:
- Exploratory Factor Analysis: Reduce the 62+ variables into a few key latent factors (e.g., "metabolic health," "diet quality," "mental well-being") [62].
- Cluster Analysis: Apply Ward's hierarchical clustering method to the factor scores to identify distinct, homogeneous subgroups within the population [62].
- Algorithm Development: Use a forward stepwise regression followed by a machine-learning model (e.g., Random Forest) to create a computational algorithm for quick cluster assignment based on a minimal set of questions [62].
Research Workflow and Pathway Diagrams
Physiological Pathways in Glucose Dysregulation
Experimental Clustering Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Glucose Metabolism and Personalized Lifestyle Research
| Item | Function in Research |
|---|---|
| Continuous Glucose Monitor (CGM) | Provides high-frequency interstitial glucose measurements for analyzing 24-hour glucose patterns, variability, and nocturnal events [1] [61]. |
| Validated Questionnaires (IPAQ, MEDAS-14, SF-12/SF-36) | Quantify lifestyle factors (physical activity, dietary adherence, health-related quality of life) for robust phenotyping and cluster analysis [62]. |
| Automated Insulin Delivery (AID) Systems | Advanced tools for studying closed-loop glucose control. Emerging systems (e.g., Tandem Control-IQ, MiniMed 780G) allow testing of different algorithms [61] [63]. |
| Open-Source AID Systems (OpenAPS, Loop) | Research platforms enabling full access to the algorithm and customization of insulin delivery settings, useful for testing novel control strategies [63]. |
| Ketone Meters (Blood) | Critical for patient safety and research integrity to confirm or rule out ketoacidosis during periods of unexplained hyperglycemia or pump failure [59]. |
| Machine Learning Algorithms (Random Forest, etc.) | Used to develop computational models for clustering heterogeneous populations into distinct metabotypes for precision medicine approaches [62]. |
Validation Through Large-Scale Studies and Comparative Phenomenology
Frequently Asked Questions (FAQs)
1. What is the Somogyi effect and what is the current scientific consensus on its existence? The Somogyi effect is a theory proposing that nocturnal hypoglycemia (low blood sugar) triggers a counter-regulatory hormone response, leading to rebound hyperglycemia (high blood sugar) in the morning [1] [3]. Historically, it was a common consideration in diabetes management. However, evidence from large retrospective analyses and studies using continuous glucose monitoring (CGM) has largely refuted this theory, suggesting it is rare or non-existent in real-world conditions [1] [64] [3]. The prevailing scientific consensus is that the dawn phenomenon—early morning hyperglycemia due to natural hormonal surges—is a far more common cause of elevated fasting glucose [1] [2].
2. What is the key evidence from retrospective CGM analyses refuting the Somogyi effect? Large retrospective studies analyzing CGM data from thousands of patients have consistently found that morning fasting glucose levels are typically lower, not higher, following nights with nocturnal hypoglycemic episodes [64]. The more severe the nocturnal hypoglycemia, the lower the morning fasting glucose levels tend to be, directly contradicting the rebound hyperglycemia central to the Somogyi theory [64].
3. If not the Somogyi effect, what explains elevated fasting blood glucose? The most common cause of morning hyperglycemia is the dawn phenomenon, which is driven by a natural early morning surge of insulin-antagonist hormones (like cortisol and growth hormone) and is not preceded by hypoglycemia [1] [2]. Other frequent causes include simple insulin deficiency (waning of insulin levels from the previous evening's dose) and insulin resistance [1] [3] [2].
4. How should a suspected Somogyi effect be investigated in a research or clinical setting? The definitive method is to use continuous glucose monitoring (CGM) to track blood glucose trends throughout the night [64] [3] [2]. If CGM is unavailable, manual blood glucose checks at critical times—such as at bedtime, between 2:00 a.m. and 3:00 a.m., and upon waking—can provide essential data [3]. A fasting glucose level below 5 mmol/L (90 mg/dL) is a strong predictor of nocturnal hypoglycemia, while a level above 9.6 mmol/L (~173 mg/dL) is associated with no risk of nocturnal hypoglycemia [64].
5. What are the clinical implications of this evidence for therapy? Concerns about inducing the Somogyi effect should not prevent appropriate intensification of insulin therapy when persistent morning hyperglycemia is observed [64]. The evidence indicates that increasing evening doses of long-acting insulin to correct high fasting glucose is safe and does not typically trigger rebound hyperglycemia [64]. The focus should be on optimizing insulin regimens to prevent both nocturnal hypoglycemia and the dawn phenomenon.
The table below summarizes quantitative findings from major studies that have investigated the Somogyi effect.
| Study / Analysis | Study Design & Population | Key Findings Refuting Somogyi Effect |
|---|---|---|
| Furukawa et al. (2022) [64] | Retrospective CGM analysis of 2,600 insulin-treated patients with Type 2 Diabetes. | Morning fasting glucose was significantly lower after nights with nocturnal hypoglycemia (P<0.001). Fasting glucose >9.6 mmol/L was associated with a 0% risk of nocturnal hypoglycemia. |
| Choudhary et al. (2013) [64] | Study of 89 patients with Type 1 Diabetes using CGM. | Fasting capillary glucose was more likely to be lower following nocturnal hypoglycemia. Only 2 instances of fasting glucose >180 mg/dL were found after a nocturnal low, indicating the effect is rare. |
| Havlin & Cryer (1987) [1] [64] | Monitoring of patients on usual therapeutic regimens. | Noctional hypoglycemia did not commonly result in major morning hyperglycemia. Found a strong inverse correlation between morning glucose and free insulin levels, suggesting insulin deficiency was the cause. |
| Diabetologia (2005) [64] | CGM study of 262 patients with Type 1 Diabetes. | Morning glucose after nocturnal hypoglycemia was >5 mmol/L lower than after nights without hypoglycemia. No evidence for rebound hyperglycemia was found. |
Experimental Protocols for Investigation
For researchers aiming to study nocturnal glucose fluctuations, the following protocol provides a standardized methodology.
Objective: To determine the relationship between nocturnal hypoglycemic events and morning fasting blood glucose levels and to distinguish the Somogyi effect from the dawn phenomenon.
Materials: See "Research Reagent Solutions" below.
Methodology:
- Participant Selection: Recruit patients with diabetes (Type 1 or insulin-treated Type 2) who report unexplained morning hyperglycemia.
- Baseline Assessment: Collect baseline HbA1c, demographic data, and current insulin regimen.
- Glucose Monitoring:
- Data Collection: Record all glucose values, along with timing of insulin administration, evening meals, and exercise.
- Data Analysis:
- Correlate the occurrence of nocturnal hypoglycemia (e.g., glucose <3.9 mmol/L or 70 mg/dL) with the subsequent morning fasting glucose level.
- Classify the cause of morning hyperglycemia as:
- Probable Dawn Phenomenon: A gradual rise in glucose from ~3 AM to morning without preceding hypoglycemia [1].
- Insulin Deficiency (Waning Insulin): A progressive rise in glucose throughout the night without hypoglycemia [2].
- Somogyi Effect (Only if confirmed): Documented hypoglycemia followed by a sharp rebound to hyperglycemia [1].
Signaling Pathways in Glucose Counter-Regulation
The following diagram illustrates the body's physiological response to hypoglycemia, which forms the theoretical basis of the Somogyi effect.
Physiological Response to Hypoglycemia
Research Reagent Solutions
The table below details key materials and tools required for conducting research into nocturnal glucose dysregulation.
| Research Tool / Reagent | Function / Application in Research |
|---|---|
| Continuous Glucose Monitor (CGM) | Essential for capturing detailed, retrospective glucose trends and asymptomatic hypoglycemic events throughout the night [64] [2]. |
| Blood Glucose Meter | For point-of-care validation of CGM readings or for manual nocturnal sampling protocols where CGM is not available [3]. |
| HbA1c Test Kit | Provides a measure of long-term glycemic control, helping to contextualize acute nocturnal glucose findings [2]. |
| Insulin Assays | Used to measure plasma insulin levels to investigate the role of hypoinsulinemia (waning insulin) versus counter-regulatory hormones in morning hyperglycemia [1] [64]. |
| Counter-Regulatory Hormone Assays (e.g., Cortisol, Glucagon, Growth Hormone) | Critical for quantifying the hormonal response to induced or spontaneous hypoglycemia in a controlled lab setting [1] [2]. |
| Data Analysis Software (e.g., R, Python, SPSS) | For statistical analysis of large retrospective CGM datasets, including time-in-range, hypoglycemia frequency, and glucose trend analysis [64]. |
Technical Comparative Analysis
The Somogyi Effect and Dawn Phenomenon represent two distinct pathophysiological entities responsible for early morning hyperglycemia in diabetes, each requiring divergent clinical management strategies.
Table 1: Pathophysiological and Clinical Profile Comparison
| Parameter | Somogyi Effect | Dawn Phenomenon |
|---|---|---|
| Core Mechanism | Rebound hyperglycemia from nocturnal hypoglycemia-induced counterregulatory response [65] [1] [3] | Natural circadian hormone surge causing increased insulin resistance [65] [18] [66] |
| Primary Pathophysiology | Hypoglycemia → Glucagon, Epinephrine, Cortisol, Growth Hormone release → Increased hepatic gluconeogenesis/glycogenolysis [1] [2] | Nocturnal growth hormone, cortisol secretion → Increased hepatic glucose production & peripheral insulin resistance [18] [66] |
| Preceding Nocturnal Hypoglycemia | Required for diagnosis [65] [67] | Not present [18] |
| Prevalence | Rare; debated validity in recent research [1] [3] [2] | Very common (>50% of both T1D and T2D) [65] [18] |
| Typical Onset Time | Overnight hypoglycemia (e.g., 2-3 AM) → Morning hyperglycemia [65] [67] | Early morning (4-8 AM) [65] [66] |
| Key Counterregulatory Hormones | Glucagon (primary), Epinephrine, Cortisol, Growth Hormone [1] [2] | Growth Hormone (primary), Cortisol, Glucagon, Epinephrine [18] [66] |
| Recommended Treatment | Reduce evening/long-acting insulin dose; adjust bedtime snack [3] [67] [2] | Increase insulin; insulin pump; adjust medication timing; avoid bedtime carbs [65] [18] [66] |
Table 2: Diagnostic and Monitoring Approaches
| Approach | Somogyi Effect | Dawn Phenomenon |
|---|---|---|
| Gold-Standard Detection | Continuous Glucose Monitoring (CGM) documenting nocturnal hypoglycemia [65] [2] | CGM showing early morning rise without nocturnal hypoglycemia [18] |
| Alternative Diagnostic Method | Intermittent testing at 2-3 AM showing hypoglycemia [65] [3] | Calculation via pre-meal glucose: 0.49X + 15 (X = pre-breakfast - avg pre-lunch/dinner glucose) [18] |
| HbA1c Correlation | May be normal or low despite morning hyperglycemia [2] | Contributes ~0.4% increase to HbA1c [18] |
| Research Definitions | RHypo: Glucose <3.9 mmol/L preceded by >10.0 mmol/L within 120 minutes [68] | Quantified by subtracting overnight glucose nadir from pre-breakfast value [18] |
Experimental Protocols & Research Methodologies
Protocol for Nocturnal Glycemic Variation Characterization
Objective: To differentiate between Somogyi Effect and Dawn Phenomenon in diabetic subjects.
Materials: Continuous Glucose Monitoring system, standardized meals, insulin administration records.
Procedure:
- Subject Preparation: Standardize evening meal (record macronutrient composition) by 7:00 PM. No caloric intake after 9:00 PM except for hypoglycemia treatment [67]
- Baseline Monitoring: Confirm euglycemia (4-7 mmol/L) at 11:00 PM before sleep
- Nocturnal Sampling:
- Morning Assessment: Measure fasting glucose at 6:00-7:00 AM
- Data Analysis: Correlate nocturnal glucose patterns with morning values over 3-5 consecutive nights
Interpretation: Nocturnal hypoglycemia (<3.9 mmol/L) followed by morning hyperglycemia indicates Somogyi Effect; sustained euglycemia until early morning rise indicates Dawn Phenomenon [65] [18].
Protocol for Quantifying Rebound Hyperglycemia in Research Settings
Objective: To objectively quantify rebound hyperglycemia (RHyper) events following hypoglycemia.
Materials: rtCGM system, data analysis software, standardized hypoglycemia treatment protocol.
Procedure:
- Event Definition: Define RHyper as series of sensor glucose values >180 mg/dL starting within two hours of antecedent value <70 mg/dL [68] [32]
- Data Collection: Collect CGM data at 15-minute intervals for minimum 14-day observation period
- Parameters Quantified:
- Event frequency (number per week)
- Duration (consecutive minutes >180 mg/dL)
- Severity (AUC >180 mg/dL in mg/dL×min)
- Intervention Assessment: Compare parameters during control vs. intervention periods using paired t-tests
Applications: Testing insulin formulations, diabetes technologies, or counterregulatory hormone antagonists [32].
Pathophysiological Pathway Visualizations
Somogyi Effect Pathophysiology
Dawn Phenomenon Pathophysiology
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Applications
| Research Tool | Function/Application | Research Context |
|---|---|---|
| Real-time CGM (rtCGM) | Continuous interstitial glucose monitoring; detects nocturnal patterns & hypoglycemia [68] [32] | Gold-standard for differentiating phenomena; quantifies event frequency/duration |
| Intermittent-scan CGM (isCGM) | Retrospective glucose pattern analysis; user-initiated readings [68] | Large-scale observational studies; real-world evidence collection |
| Predictive Low Glucose Alert Systems | Alerts for impending hypoglycemia; enables preventive intervention [32] | Studying hypoglycemia prevention and resultant rebound hyperglycemia reduction |
| Insulin Pumps (CSII) | Programmable basal rates; micro-bolus administration [65] [18] | Investigating targeted overnight insulin delivery to counteract dawn phenomenon |
| Standardized Carbohydrate Treatments | Consistent hypoglycemia rescue; reduces treatment variability [32] | Studying rebound hyperglycemia magnitude following standardized rescue |
| Counterregulatory Hormone Assays | Measure glucagon, cortisol, epinephrine, growth hormone levels [1] [2] | Quantifying hormonal response to hypoglycemia in Somogyi effect |
| Calculated Dawn Phenomenon Magnitude Formula | 0.49X + 15 (X = pre-breakfast glucose - average pre-lunch/dinner glucose) [18] | Standardized quantification of dawn phenomenon in research settings without CGM |
Troubleshooting Guides & FAQs
FAQ 1: How can we definitively differentiate between Somogyi Effect and Dawn Phenomenon in clinical trials?
The most reliable method employs Continuous Glucose Monitoring (CGM) with specific diagnostic criteria:
For Somogyi Effect: Documented nocturnal hypoglycemia (glucose <70 mg/dL for ≥15 minutes) followed by morning hyperglycemia (>180 mg/dL) within a 2-8 hour window. The key is establishing the causal hypoglycemic event [65] [2].
For Dawn Phenomenon: Sustained euglycemia overnight with an early morning glucose rise (typically 4-8 AM) without preceding hypoglycemia. Quantify magnitude by subtracting overnight nadir from pre-breakfast value [18].
Protocol implementation should standardize evening meals, insulin administration, and utilize CGM with 15-minute sampling intervals for at least 3-5 consecutive nights to establish patterns [67].
FAQ 2: What is the current scientific consensus on the validity of the Somogyi Effect?
The Somogyi Effect remains controversial in the research community:
Supporting Evidence: The theoretical framework is physiologically plausible - hypoglycemia triggers counterregulatory hormones (glucagon, epinephrine, cortisol, growth hormone) that stimulate hepatic glucose production [1] [3].
Contradictory Evidence: Recent CGM studies question its prevalence. Research shows nocturnal hypoglycemia more frequently results in morning hypoglycemia, not hyperglycemia [1]. One study of 89 type 1 diabetics found only 2 instances of fasting glucose >180 mg/dL following nocturnal hypoglycemia [2].
Current Status: Considered rare compared to dawn phenomenon. Many cases previously attributed to Somogyi effect may represent waning insulin levels or the dawn phenomenon itself [1] [3].
FAQ 3: What are the optimal research methodologies for studying rebound hyperglycemia?
Standardized protocols should include:
Precise Definitions:
Quantification Metrics:
- Frequency (events/week)
- Duration (consecutive minutes >180 mg/dL)
- Severity (Area Under Curve >180 mg/dL)
Control for Confounders: Standardize carbohydrate treatment for hypoglycemia, monitor insulin doses, and account for individual glycemic variability [32].
FAQ 4: How does the dawn phenomenon impact long-term glycemic control outcomes?
The dawn phenomenon significantly affects overall diabetes management:
HbA1c Impact: Contributes approximately 0.4% increase to total HbA1c levels [18].
Cardiovascular Risk: A 1% increase in HbA1c associates with 15%-20% increased cardiovascular complication risk. Controlling dawn phenomenon could provide substantial risk reduction [18].
Therapeutic Implications: Requires specific management strategies including insulin pumps for early morning basal rate increases, adjusted medication timing, and dietary modifications [65] [66].
FAQ 5: What technological solutions show efficacy in mitigating these phenomena?
Research demonstrates several effective technological interventions:
Real-time CGM (rtCGM): Reduces rebound hyperglycemia frequency by 14%, duration by 12%, and severity by 23% through early hypoglycemia detection and prevention of over-treatment [32].
Predictive Low Glucose Alerts: Systems with "urgent low soon" alerts reduce rebound hyperglycemia frequency by 7%, duration by 8%, and severity by 13% compared to CGM without predictive alerts [32].
Insulin Pumps: Allow precise basal rate adjustments to counteract early morning insulin resistance in dawn phenomenon [65] [18].
Clinical Significance and Impact on Long-term Glycemic Control (A1C, TIR)
Defining the Somogyi Effect and Its Current Scientific Status
What is the Somogyi effect and how is it defined in modern research?
The Somogyi effect, also known as rebound hyperglycemia or posthypoglycemic hyperglycemia, is a theory proposing that an episode of nocturnal hypoglycemia triggers a counterregulatory hormonal response that leads to hyperglycemia the following morning [1] [3]. This phenomenon was first described in the 1930s by Dr. Michael Somogyi, who hypothesized that when blood glucose levels drop too low during sleep, the body releases hormones such as adrenaline, corticosteroids, growth hormone, and glucagon, activating gluconeogenesis and resulting in morning hyperglycemia [1].
However, recent studies utilizing continuous glucose monitoring (CGM) have challenged this theory, with some research observing that patients with morning hyperglycemia tend to have high rather than low blood glucose measurements at night [1] [2]. The scientific community continues to debate the validity of the Somogyi effect, with some researchers proposing alternative mechanisms for morning hyperglycemia, including nocturnal growth hormone secretion, hypoinsulinemia, and insulin resistance associated with metabolic syndrome [1] [2].
How does the Somogyi effect differ from the dawn phenomenon?
The Somogyi effect is often confused with the dawn phenomenon, but they have distinct underlying mechanisms [3]:
| Characteristic | Somogyi Effect | Dawn Phenomenon |
|---|---|---|
| Primary Trigger | Nocturnal hypoglycemia [3] | Natural hormonal surges in early morning (cortisol, growth hormone) [1] [3] |
| Underlying Mechanism | Counterregulatory hormone release (e.g., epinephrine, glucagon) in response to low blood glucose [1] [3] | Circadian rhythm of insulin-antagonist hormones; decreased endogenous insulin levels at night [1] |
| Prevalence | Considered rare [2] | More common [1] [3] |
Quantitative Impact on Glycemic Control Metrics
How does rebound hyperglycemia affect A1C and Time in Range (TIR) metrics?
The Somogyi effect influences long-term glycemic control through repeated cycles of hypoglycemia and subsequent hyperglycemia. While A1C provides a three-month average blood glucose level, it does not capture these glycemic excursions [69]. Rebound hyperglycemia can contribute to an increase in A1C levels over time [3]. More significantly, it directly impacts Time in Range (TIR) and Time Above Range (TAR) metrics, which are more sensitive indicators of daily glycemic variability [70] [69].
The following table summarizes the impact of rebound hyperglycemia on core CGM metrics compared to established targets [70]:
| Glycemic Metric | Target (Most Adults with Diabetes) | Impact of Rebound Hyperglycemia |
|---|---|---|
| Time in Range (TIR)(70-180 mg/dL) | ≥70% of day(~17 hours) | Decreased percentage due to post-hypoglycemic highs [3] |
| Time Above Range (TAR)(>180 mg/dL) | <25% of day | Increased percentage [3] [32] |
| Time Below Range (TBR)(<70 mg/dL) | <4% of day | Increased percentage prior to rebound [32] |
| Glucose Management Indicator (GMI) | n/a | May be elevated if hyperglycemic periods are prolonged [3] |
| Coefficient of Variation (CV) | ≤36% | Often increased due to high-amplitude glucose swings [69] |
Research by Choudhary et al. utilizing CGM found that nocturnal hypoglycemia was more frequently associated with low rather than high fasting glucose levels, suggesting the Somogyi effect is rare [2]. A study quantifying Rebound Hyperglycemia (RH) defined as sensor glucose values >180 mg/dL within two hours of an antecedent value <70 mg/dL found that fewer than half of all hypoglycemic events were followed by RH events [32].
Experimental Protocols for Investigation
What methodology can be used to detect and quantify the Somogyi effect in a clinical research setting?
A detailed protocol for investigating the Somogyi effect involves continuous glucose monitoring and specific data analysis techniques [32]:
Protocol: Detection and Quantification of Rebound Hyperglycemia (RH)
- Subject Population: Patients with type 1 diabetes or insulin-requiring type 2 diabetes. Special consideration should be given to those with impaired awareness of hypoglycemia [32].
- Equipment: Real-time Continuous Glucose Monitoring (rtCGM) system with data logging capabilities.
- Study Duration: A minimum of 14 days of CGM data is recommended, with a sensor wear time of at least 70% to ensure data reliability [70].
- Data Analysis Definitions:
- Quantification Metrics: For each RH event, calculate:
- Frequency: The number of RH events per week.
- Duration: The length of the RH event in minutes (number of consecutive SGVs >180 mg/dL × data interval).
- Severity: The area under the curve (AUC) for glucose concentration above 180 mg/dL during the event (mg/dL × minutes) [32].
- Control for Confounders: Document factors such as timing and dose of insulin/medications, meal composition and timing, alcohol intake, and physical activity.
For settings where CGM is not available, frequent manual blood glucose sampling can be used as an alternative, though it is less comprehensive. Key sampling times include [3]:
- Two hours after the evening meal
- At bedtime
- Between 2:00 a.m. and 4:00 a.m.
- Upon waking
Research Reagent Solutions and Essential Materials
What are the key reagents and tools required for studying rebound hyperglycemia?
The following table details essential materials and their research applications in the study of the Somogyi effect and glycemic control:
| Research Tool / Reagent | Primary Function in Research |
|---|---|
| Real-time CGM (rtCGM) System | Core tool for continuous, high-frequency glucose measurement; enables detection of nocturnal hypoglycemia and subsequent hyperglycemia [32] [2]. |
| CGM Data Analysis Software | Platform for calculating key metrics (TIR, TAR, TBR, GMI, CV) and identifying RH events based on predefined glucose thresholds [70] [32]. |
| Predictive Hypoglycemia Alert Algorithms | Investigational tool to study the mitigation of RH by providing early warning of impending lows, allowing for preventive action [32]. |
| Glucagon Assay Kits | To measure plasma glucagon levels and confirm its role as a counterregulatory hormone in the suspected rebound process [1] [2]. |
| Cortisol & Growth Hormone Assays | To quantify the levels of these insulin-antagonist hormones in plasma/serum during and after a hypoglycemic event [1] [2]. |
| Standardized Carbohydrate Source | For consistent treatment of induced hypoglycemia in interventional studies (e.g., 15-20g fast-acting carbs) [44] [71]. |
Signaling Pathways and Pathophysiology
What is the pathophysiological sequence of the proposed Somogyi effect?
The theoretical framework of the Somogyi effect centers on the body's counterregulatory response to hypoglycemia. The following diagram maps this proposed signaling pathway:
This counterregulatory mechanism is dependent on an intact glucose sensor system in the CNS, pancreas, and afferent nerves [2]. In individuals without diabetes, endogenous insulin secretion is suppressed, and the released glucagon effectively stimulates glucose production, normalizing blood sugar. In insulin-treated diabetes, exogenous insulin cannot be suppressed, and the glucagon response may be impaired, but other hormones like epinephrine drive the glucose rebound, often resulting in overshooting hyperglycemia [1] [2].
Frequently Asked Questions for Research Troubleshooting
FAQ 1: Our clinical data shows morning hyperglycemia, but CGM reveals no nocturnal hypoglycemia. Is this still the Somogyi effect?
No. By definition, the Somogyi effect requires an antecedent hypoglycemic event [3] [32]. If CGM data does not confirm nocturnal hypoglycemia (values <70 mg/dL), the morning hyperglycemia is likely attributable to other factors. The most common alternative is the dawn phenomenon, characterized by a natural rise in insulin-antagonist hormones in the early morning hours [1] [3]. Other causes include simple insulin waning (the dissipation of insulin action from the previous evening's dose) or insufficient overnight insulin dosing [2].
FAQ 2: How can we objectively differentiate between the Somogyi effect and the dawn phenomenon in a study cohort?
The most reliable method is to use CGM data to examine the nocturnal glucose pattern [2]. The following diagnostic workflow outlines the key differentiators:
FAQ 3: How is rebound hyperglycemia best quantified in interventional trials?
Beyond simply noting its presence, Rebound Hyperglycemia (RH) can be quantified using three key metrics derived from CGM data [32]:
- Frequency: The number of RH events per week.
- Duration: The total time in minutes that glucose remains above 180 mg/dL following a hypoglycemic event.
- Severity: The area under the curve (AUC) for glucose >180 mg/dL post-hypoglycemia, which combines the magnitude and duration of the hyperglycemic excursion [32]. These metrics provide a robust framework for assessing the impact of interventions, such as new insulin formulations or CGM alert systems, on mitigating RH.
FAQ 4: What is the clinical relevance of the ongoing debate surrounding the Somogyi effect?
Even if the classic Somogyi effect is rare, its investigation highlights two critical aspects of diabetes management that are unequivocally important [1] [3] [32]:
- The Dangers of Overnight Hypoglycemia: It reinforces the need to avoid nocturnal hypoglycemia, which can be undetected and dangerous.
- The Complexity of Glucose Dynamics: It underscores that A1C alone is insufficient for understanding glycemic control and that metrics like TIR and glucose variability (CV) are essential for a complete picture [70] [69]. Therefore, the research framework for studying rebound hyperglycemia remains valuable, regardless of the final consensus on the prevalence of the original Somogyi theory.
FAQs: Core Concepts & Patient Identification
Q1: What are the primary risk factors for nocturnal hypoglycemia in patients with diabetes? Research using continuous glucose monitoring (CGM) has identified several key modifiable and non-modifiable risk factors. A study analyzing 885 nights from 45 subjects with type 1 diabetes found that nocturnal hypoglycemia (CGM measurement of <60 mg/dL for ≥30 min) occurred in 25% of nights [72]. The significant risk factors are summarized below [72]:
| Risk Factor | Association with Nocturnal Hypoglycemia | P-value |
|---|---|---|
| Younger Age | Increased Frequency | <0.001 |
| Lower HbA1c Level | Increased Frequency | 0.006 |
| Medium/High-Intensity Exercise (preceding day) | Increased Frequency | 0.003 |
| Antecedent Daytime Hypoglycemia | Increased Frequency | 0.001 |
| Lower Bedtime Blood Glucose | Trend toward Increased Frequency | 0.10 |
Q2: How does the Somogyi effect differ from the dawn phenomenon, and what is the current scientific consensus? The Somogyi effect and dawn phenomenon are both theorized to cause morning hyperglycemia, but through different mechanisms. The scientific consensus on the Somogyi effect is now a subject of debate [1] [3].
| Feature | Somogyi Effect | Dawn Phenomenon |
|---|---|---|
| Proposed Cause | Rebound from nocturnal hypoglycemia [3] | Natural early-morning hormone surge (e.g., cortisol, growth hormone) [3] |
| Nocturnal Glucose | Theorized to drop low overnight | Typically stable or rising [1] |
| Prevalence | Considered uncommon; some studies dispute its existence [1] [3] | More common cause of morning hyperglycemia [3] |
| Clinical Implication | Older theory; may not be a primary cause [1] | Recognized as a common occurrence requiring management [1] |
Recent studies using CGM have disputed the Somogyi effect, finding that nocturnal hypoglycemia is often followed by continued hypoglycemia or normoglycemia, not hyperglycemia [1]. One study concluded that "nocturnal hypoglycemia did not cause daytime hyperglycemia" [1].
Q3: What is rebound hyperglycemia and how can it be quantified in research settings? Rebound hyperglycemia (RH) is defined as hyperglycemia that follows an antecedent hypoglycemic event, often due to excessive carbohydrate intake to correct lows or a counter-regulatory hormone response [32]. It can be objectively quantified in CGM data using the following operational definition [32]:
- RH Event: A series of one or more sensor glucose values (SGVs) >180 mg/dL that starts within two hours of an antecedent SGV <70 mg/dL.
- Metrics for Quantification:
- Frequency: Number of RH events per week.
- Duration: Consecutive minutes of SGVs >180 mg/dL.
- Severity: Area under the curve (AUC) of glucose concentration >180 mg/dL (mg/dL × min).
Q4: What patterns of nocturnal glucose are associated with hypoglycemia? Cluster analysis of CGM data from 395 adults with type 1 diabetes has identified distinct nocturnal glucose patterns. The study found that 10 clusters without hypoglycemia and 6 clusters with nocturnal hypoglycemia episode(s) exist, highlighting the diversity of nocturnal profiles [73]. Key differentiating factors include [73]:
- Initial and final glucose levels.
- The direction and magnitude of glucose change during the night (presence of uptrends or downtrends).
- The time at which glucose begins to decline.
- The finding that post-midnight hyperglycemia was present in 5 out of 10 clusters without hypoglycemia, suggesting that initially elevated glucose can sometimes prevent hypoglycemia in patterns with downtrends.
Troubleshooting Guides: Experimental Protocols & Data Interpretation
Guide 1: Protocol for Profiling Nocturnal Glycemic Patterns Using CGM Data
This protocol outlines the methodology for clustering CGM data to identify patterns of nocturnal glycemic volatility, as adapted from a study on patients with type 1 diabetes [73].
1. Objective: To identify distinct patterns (clusters) of nocturnal glucose profiles with and without hypoglycemia from retrospective CGM data.
2. Materials & Reagents:
- CGM Dataset: Data from a cohort of patients (e.g., n=395) managed with the therapy of interest [73].
- Data Processing Software: e.g., Python with pandas, NumPy.
- Clustering Algorithm: e.g., Hierarchical clustering (Ward's method) in scikit-learn.
3. Step-by-Step Procedure:
- Step 1: Data Extraction & Cleaning
- Extract nocturnal segments (e.g., 12:00 AM to 6:00 AM) from CGM records.
- Exclude time intervals with excessive missing data (e.g., ≥3 consecutive values or >10% of values). Impute small gaps using linear interpolation [73].
- Step 2: Define Nocturnal Hypoglycemia (NH)
- Label time series based on the presence of NH, defined as an episode of interstitial glucose < 3.9 mmol/L (≈70 mg/dL) lasting at least 15 minutes [73].
- Step 3: Data Standardization
- Standardize each glucose time series to have a mean of zero and a unit variance to focus on the shape of the profile rather than absolute levels [73].
- Step 4: Clustering Analysis
- Step 5: Cluster Validation
- Assess the reliability of the cluster structure using a method like the Monte Carlo technique, comparing the SS of the real data to the SS of synthetically generated data with no cluster structure [73].
CGM Nocturnal Pattern Analysis Workflow
Guide 2: Protocol for Quantifying Rebound Hyperglycemia (RH)
This protocol provides a method for quantifying RH, a key component of glycemic volatility, from CGM data traces [32].
1. Objective: To objectively quantify the frequency, duration, and severity of rebound hyperglycemia events.
2. Materials:
- CGM Data Series: Sensor glucose values (SGVs) collected at 5-minute intervals.
- Analysis Tool: Software capable of processing time-series data (e.g., Python, R, MATLAB).
3. Step-by-Step Procedure:
- Step 1: Identify Hypoglycemic Episodes
- Scan the CGM data for all series of one or more consecutive SGVs <70 mg/dL.
- Step 2: Identify Subsequent Hyperglycemia
- For each hypoglycemic episode, identify any series of one or more consecutive SGVs >180 mg/dL that begins within 120 minutes (2 hours) of the end of the hypoglycemic series. This constitutes one RH event [32].
- Step 3: Calculate RH Metrics
- Frequency: Count the total number of RH events over a defined period (e.g., per week) [32].
- Duration: Sum the consecutive minutes for which SGVs remain >180 mg/dL during the RH event (number of values × 5 minutes) [32].
- Severity (AUC): Calculate the area under the glucose concentration-time curve for the SGVs >180 mg/dL during the RH event. The trapezoidal rule can be used for this calculation [32].
Rebound Hyperglycemia Quantification
The Scientist's Toolkit: Research Reagent Solutions
This table details key resources for researchers studying nocturnal glycemic volatility and its underlying mechanisms.
| Resource / Reagent | Function in Research | Key Details / Access |
|---|---|---|
| CGM Systems | Captures continuous interstitial glucose readings, enabling the detection of asymptomatic hypoglycemia and glycemic patterns [72] [73]. | Systems from Dexcom (G5, G6) and Medtronic (Enlite) are used in clinical studies. Predictive alerts can mitigate hypoglycemia and rebound hyperglycemia [32]. |
| NIDDK Central Repositories | Provides access to data and biosamples from major NIDDK-funded clinical studies for validation and discovery research [74]. | Stores resources from studies like DCCT/EDIC, GoKinD, T1DGC, and TEDDY. Access: https://repository.niddk.nih.gov/ [74]. |
| Type 1 Diabetes TrialNet | An international network offering risk screening and conducting clinical studies on the prevention and progression of T1D. Supports ancillary studies [74]. | Researchers can submit proposals for clinical trial protocols or request biological samples via its Living Biobank [75]. |
| Integrated Islet Distribution Program (IIDP) | Supplies high-quality human cadaveric islets to the research community for basic science investigations [74]. | Critical for in vitro studies of insulin secretion and beta-cell function. Access: http://iidp.coh.org/ [74]. |
| Hierarchical Clustering Algorithms | Data mining technique to classify complex CGM data into distinct nocturnal glucose patterns without a priori assumptions [73]. | Implemented in software like Python or R. Ward's method with Euclidean distance is one effective approach for CGM time series [73]. |
Reconciling Historical Theory with Contemporary Evidence-Based Practice
Foundational Concepts: From Historical Theory to Modern Understanding
What is the Somogyi effect and how was it originally theorized?
The Somogyi effect, named after Dr. Michael Somogyi who proposed it in the 1930s, describes a theoretical cycle of rebound hyperglycemia following an episode of hypoglycemia [1] [3]. Dr. Somogyi, a Hungarian-born professor at Washington University, postulated that when blood glucose levels drop too low (often overnight due to insulin therapy), the body activates counterregulatory hormones to rescue itself [1] [2]. This hormonal surge stimulates gluconeogenesis and glycogenolysis, leading to a paradoxical overshoot into hyperglycemia by morning [1] [76]. The phenomenon was also termed "posthypoglycemic hyperglycemia" or "chronic Somogyi rebound" [1].
How does the contemporary scientific consensus view the Somogyi effect?
Modern research, particularly utilizing Continuous Glucose Monitoring (CGM), has largely disputed the Somogyi effect as a common clinical occurrence [1] [3]. Recent studies indicate that nocturnal hypoglycemia is more frequently followed by normal or even low fasting glucose levels, not hyperglycemia [1] [2]. The current scientific consensus suggests that the phenomenon is rare, and morning hyperglycemia is more likely attributable to other factors, primarily the dawn phenomenon or simple insulin waning [1] [2] [3]. The theory remains a valuable historical concept but is no longer considered a primary explanation for morning hyperglycemia in clinical practice [1].
What is the key pathophysiological difference between the Somogyi effect and the dawn phenomenon?
The fundamental distinction lies in the presence or absence of an antecedent hypoglycemic event.
- Somogyi Effect (Theoretical): Morning hyperglycemia is a rebound effect preceded by nocturnal hypoglycemia, triggering a counterregulatory hormone response [1] [3] [76].
- Dawn Phenomenon (Common): Morning hyperglycemia occurs without preceding hypoglycemia and is attributed to a natural, early-morning surge in insulin-antagonist hormones (like cortisol and growth hormone) or decreased insulin sensitivity [1] [2] [3].
The table below summarizes the core differences:
| Feature | Somogyi Effect | Dawn Phenomenon |
|---|---|---|
| Primary Cause | Rebound from nocturnal hypoglycemia | Nocturnal growth hormone surge; natural circadian hormone rhythms [1] [2] |
| Preceding Hypoglycemia | Required (theoretical) | Not present [1] [3] |
| Prevalence | Considered rare [2] [3] | Common [1] [3] |
| Counterregulatory Hormones | Activated in response to low blood glucose [1] [2] | Part of normal circadian secretion pattern [1] |
Diagram 1: The historical theoretical pathway of the Somogyi effect, as proposed by Dr. Michael Somogyi.
Troubleshooting Guides & FAQs for Researchers
How can we accurately differentiate the Somogyi effect from the dawn phenomenon in a research setting?
The definitive method for differentiation is comprehensive nocturnal glucose monitoring to establish the presence or absence of hypoglycemia [2] [3].
Experimental Protocol for Differentiation:
- Primary Tool: Utilize Continuous Glucose Monitoring (CGM) to track interstitial glucose levels throughout the night without disrupting sleep. This provides a high-resolution glucose profile [1] [32] [2].
- Manual Verification (if CGM unavailable): Schedule blood glucose measurements at critical time points:
- Data Interpretation:
- Pattern Consistent with Somogyi Theory: A glucose value <70 mg/dL (hypoglycemia) during the night, followed by a glucose value >180 mg/dL upon waking [32] [3].
- Pattern Consistent with Dawn Phenomenon: Stable glucose levels (>70 mg/dL) throughout the night, with a steady rise in the early morning hours (e.g., from 3:00 AM onwards) without an intervening low [1].
What is the clinical and research significance of "Rebound Hyperglycemia" (RH)?
Despite the debate around the Somogyi effect, Rebound Hyperglycemia (RH) is a quantifiable and clinically relevant phenomenon, often resulting from over-treatment of hypoglycemia [32]. It contributes to high glycemic variability, which is an independent risk factor for diabetes complications.
Quantifying Rebound Hyperglycemia in Clinical Studies: Recent research has established objective criteria for RH events, allowing for standardized measurement and analysis [32]. The table below defines key metrics for quantifying RH.
| Metric | Operational Definition | Research Significance |
|---|---|---|
| RH Event Frequency | Number of series of sensor glucose values (SGVs) >180 mg/dL starting within 2 hours of an SGV <70 mg/dL, per week [32]. | Measures how often the rebound cycle occurs. |
| RH Event Duration | Consecutive minutes of SGVs >180 mg/dL following the antecedent hypoglycemic event [32]. | Captures the persistence of hyperglycemia. |
| RH Event Severity | Area Under the Curve (AUC) of glucose concentration (mg/dL × minutes) for the period of SGVs >180 mg/dL [32]. | Represents the total glycemic excursion burden. |
Evidence from Intervention Studies: Studies show RH can be mitigated. For example, in the HypoDE trial, using real-time CGM (rtCGM) reduced the frequency, duration, and severity of RH events by 14%, 12%, and 23%, respectively. Furthermore, transitioning to a CGM system with predictive hypoglycemia alerts led to even greater reductions (7%, 8%, and 13% respectively) [32].
How should a suspected Somogyi effect be managed in a clinical trial protocol?
Management focuses on preventing the initiating hypoglycemic event, not treating the resultant morning hyperglycemia with more insulin.
Step-by-Step Management Guide:
- Confirm the Pattern: Use CGM or nocturnal glucose checks to verify the presence of nocturnal hypoglycemia [2] [3].
- Reduce Insuling Load: Decrease (do not increase) the dose of insulin that is causing the overnight hypoglycemia. This is often the bedtime long-acting (basal) insulin or the insulin covering the evening meal [2] [3].
- Consider Insulin Pharmacokinetics: Switch to newer insulin analogs with more stable profiles to reduce the peak action risk at night [2].
- Adjust Lifestyle Factors: Review and standardize evening meal composition (macronutrient balance) and timing, as well as evening exercise routines within the trial protocol [3] [76].
- Utilize Technology: Implement CGM with predictive alerts to warn participants of impending lows, allowing for preemptive carbohydrate intake to prevent a full hypoglycemic event and subsequent RH [32].
Diagram 2: A modern evidence-based diagnostic and management workflow for investigating morning hyperglycemia.
This table details key materials and technologies essential for conducting research in this field.
| Research Tool / Reagent | Primary Function in Research |
|---|---|
| Real-Time Continuous Glucose Monitor (rtCGM) | Captures high-resolution interstitial glucose data; enables detection of asymptomatic hypoglycemia and precise mapping of glycemic excursions [32] [2]. |
| CGM with Predictive Alerts | Provides an independent variable in interventional studies to assess the mitigation of hypoglycemia and subsequent RH [32]. |
| Insulin Analogs (Long- & Rapid-Acting) | Used to test hypotheses regarding pharmacodynamic stability and reduced risk of nocturnal hypoglycemia compared to human insulin [2]. |
| Glucagon Assay Kits | Quantify plasma glucagon levels to measure the counterregulatory hormone response to induced hypoglycemia [1] [2]. |
| ELISA Kits for Counterregulatory Hormones | Measure plasma levels of epinephrine, cortisol, and growth hormone in response to hypoglycemic clamps or nocturnal events [1]. |
| Hypoglycemic Clamp Technique | Gold-standard experimental method to induce and maintain a controlled hypoglycemic state for studying counterregulatory responses and RH [12]. |
Conclusion
The body of evidence, particularly from large-scale CGM studies, significantly challenges the historical prevalence and perhaps even the existence of the classic Somogyi effect, indicating that nocturnal hypoglycemia more commonly leads to morning normoglycemia or continued hypoglycemia, not rebound hyperglycemia. For researchers and drug developers, this underscores the paramount importance of leveraging advanced technologies like CGM and predictive algorithms to objectively quantify glycemic phenomena and move beyond contested pathophysiological models. Future directions must focus on the development of smarter, integrated systems that predict and prevent hypoglycemia without inducing significant rebound hyperglycemia, thereby minimizing glycemic variability. Research should prioritize personalized medicine approaches, accounting for individual counter-regulatory responses, and explore novel therapeutics that can more precisely manage the delicate balance between hypo- and hyperglycemia. The clinical focus should shift towards optimizing the use of existing technologies and addressing the more common dawn phenomenon and insulin regimen deficiencies as primary causes of morning hyperglycemia.
References
- 1. Somogyi Phenomenon - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK551525/]
- 2. Somogyi Phenomenon: Overview, Pathophysiology, ... [https://emedicine.medscape.com/article/125432-overview]
- 3. Somogyi Effect: What It Is, Causes, Symptoms & Treatment [https://my.clevelandclinic.org/health/diseases/11443-somogyi-effect]
- 4. The Somogyi effect or Rebound hyperglycemia [https://www.diabete.qc.ca/en/diabetes/diabetes-management/hyperglycemia/somogyi/]
- 5. a parallelism with Michael Somogyi's life - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12339641/]
- 6. The Somogyi hypothesis: a parallelism with Michael ... [https://link.springer.com/article/10.1007/s42000-024-00624-0]
- 7. The Myth of the Somogyi & How I Adjust Insulin [https://www.vin.com/apputil/content/defaultadv1.aspx?pId=20539&catId=113455&id=8506497&ind=344&objTypeID=17]
- 8. The somogyi phenomenon. A short review [https://link.springer.com/article/10.1007/BF02591583]
- 9. Counterregulatory Hormone - an overview [https://www.sciencedirect.com/topics/neuroscience/counterregulatory-hormone]
- 10. Counterregulatory hormone [https://en.wikipedia.org/wiki/Counterregulatory_hormone]
- 11. Biochemistry, Gluconeogenesis - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK544346/]
- 12. Hypoglycemia During Therapy of Diabetes - Endotext - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK279100/]
- 13. Role of Counterregulatory Hormones for Glucose Metabolism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3687642/]
- 14. 15.5: Regulation of Gluconeogenesis [https://bio.libretexts.org/Bookshelves/Biochemistry/Fundamentals_of_Biochemistry_(Jakubowski_and_Flatt)/02%3A_Unit_II-_Bioenergetics_and_Metabolism/15%3A_Glucose_Glycogen_and_Their_Metabolic_Regulation/15.05%3A_Regulation_of_Gluconeogenesis]
- 15. Regulation Of Glycolysis And Gluconeogenesis [https://jackwestin.com/resources/mcat-content/principles-of-metabolic-regulation-mcat-wiki/regulation-of-glycolysis-and-gluconeogenesis]
- 16. Somogyi effect: What it is, symptoms, and the dawn ... [https://www.medicalnewstoday.com/articles/317998]
- 17. Somogyi Effect vs. Dawn Phenomenon [https://myendoconsult.com/learn/somogyi-effect-vs-dawn-phenomenon/]
- 18. Dawn Phenomenon - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK430893/]
- 19. Causes of high morning blood sugar and how to lower it [https://www.medicalnewstoday.com/articles/317444]
- 20. High Morning Blood Glucose | ADA [https://diabetes.org/living-with-diabetes/high-morning-blood-glucose]
- 21. Phenomenon Somogyi [https://pubmed.ncbi.nlm.nih.gov/31855369/]
- 22. Frequently Asked Questions - Center for Diabetes ... [https://med.virginia.edu/diabetes-technology/research/]
- 23. Trouble Shooting Problems [https://www.freestylelibre.com.au/trouble-shooting?srsltid=AfmBOop1O0WFgUyazl7y-AdgmmWBgv3sBIWqDgG0TOFW9xDCBKE2aPq-]
- 24. Post-hypoglycemic nocturnal hyperglycemia in type 1 ... [https://link.springer.com/article/10.1007/s42000-025-00680-0]
- 25. Hypoglycemia in diabetes: An update on pathophysiology, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8696639/]
- 26. Predictive factors of hypoglycemia in type 2 diabetes [https://www.nature.com/articles/s41598-025-03030-7]
- 27. Using continuous glucose monitoring data in daily clinical ... [https://www.ccjm.org/content/91/10/611]
- 28. CGM Troubleshooting: Quick Fixes for Diabetes Devices [https://beyondtype1.org/cgm-troubleshooting-diabetes-tips/]
- 29. Diabetes at the RCH : Continuous glucose monitoring issues [https://www.rch.org.au/diabetes/diabetes-help/Continuous_glucose_monitoring_issues/]
- 30. Understanding Continuous Glucose Monitoring Data - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK538967/]
- 31. Reading trend arrows [https://www.timeinrange.org/get-started/reading-trend-arrows/]
- 32. Mitigation of Rebound Hyperglycemia With Real-Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9294577/]
- 33. Feature-Based Machine Learning Model for Real-Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8258517/]
- 34. Machine Learning Prediction of Hypoglycemia and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9345028/]
- 35. Machine learning-based prediction of hypoglycemia ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1634358/full]
- 36. Adverse drug events associated with insulin glargine: a real ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12066629/]
- 37. Predicting and Preventing Nocturnal Hypoglycemia in Type 1 Diabetes... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7698985/]
- 38. Understanding LINCS Warnings in GROMACS [https://parssilico.com/blogs/97-lincs-warnings-in-gromacs]
- 39. Simulation-Based Evaluation of Treatment Adjustment to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8417413/]
- 40. in silico modeling of a predictive low glucose management ... [https://pubmed.ncbi.nlm.nih.gov/24447074/]
- 41. Avoiding Nighttime Hypoglycemia [https://joslin.org/news-stories/all-news-stories/education/2020/03/avoiding-nighttime-hypoglycemia]
- 42. Insulin therapy and dietary adjustments to normalize ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4442134/]
- 43. Hypoglycemia [https://www.endocrine.org/patient-engagement/endocrine-library/hypoglycemia]
- 44. Hypoglycemia - Diagnosis and treatment [https://www.mayoclinic.org/diseases-conditions/hypoglycemia/diagnosis-treatment/drc-20373689]
- 45. Insulin Therapy and Hypoglycemia - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4265808/]
- 46. Primary care intervention reduces hypoglycemia risk from ... [https://www.endocrine.org/news-and-advocacy/news-room/2023/primary-care-intervention-reduces-hypoglycemia-risk-in-older-adults]
- 47. A Quality Improvement Program to Reduce Potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5556587/]
- 48. Reading Your Sensor Graphs - MiniMed™ 770G System ... [https://www.medtronicdiabetes.com/customer-support/minimed-770g-system-support/cgm-sensor-graphs]
- 49. Tips for Using Your Insulin Pump at Home [https://www.fda.gov/medical-devices/infusion-pumps/insulin-pumps-tips-using-your-insulin-pump-home]
- 50. Advances in Continuous Glucose Monitoring: Clinical ... [https://www.e-enm.org/journal/view.php?doi=10.3803%2FEnM.2025.2370]
- 51. Preventing Hypoglycemia Using Predictive Alarm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2979338/]
- 52. Diabetes Technology Guide | ADA [https://diabetes.org/living-with-diabetes/treatment-care/diabetes-technology-guide]
- 53. Diabetes: how to manage patients experiencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9205569/]
- 54. Chronic Somogyi rebound [https://grokipedia.com/page/Chronic_Somogyi_rebound]
- 55. Glucagon-Like Peptide-1 Receptor Agonists - StatPearls - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK551568/]
- 56. Glucagon-like peptide-1 receptor: mechanisms and ... [https://www.nature.com/articles/s41392-024-01931-z]
- 57. Adverse Effects of GLP-1 Receptor Agonists - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5397288/]
- 58. Hypoglycemia: Background, Pathophysiology, Etiology [https://emedicine.medscape.com/article/122122-overview]
- 59. Insulin Pumps l Troubleshooting Hyperglycemia l danatech [https://www.adces.org/education/danatech/insulin-pumps/troubleshooting-pumps/troubleshooting-unexplained-hyperglycemia]
- 60. Comparative Effectiveness of Personalized Lifestyle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4943251/]
- 61. The biggest diabetes tech stories out of ADA 2025 [https://www.drugdeliverybusiness.com/biggest-diabetes-tech-stories-ada-2025/]
- 62. Computational algorithm based on health and lifestyle ... [https://www.nature.com/articles/s41598-024-75110-z]
- 63. DIY AID User's Guide - Clinical Practice Guidelines [https://guidelines.diabetes.ca/cpg/diy-aid-users-guide]
- 64. Somogyi Phenomenon: Fact or Fiction? [https://cmeindia.in/somogyi-phenomenon-fact-or-fiction/]
- 65. Dawn Phenomenon vs. Somogyi Effect - Diabetes [https://www.webmd.com/diabetes/dawn-phenomenon-or-somogyi-effect]
- 66. The dawn phenomenon: What can you do? [https://www.mayoclinic.org/diseases-conditions/diabetes/expert-answers/dawn-effect/faq-20057937]
- 67. Dawn Phenomenon vs. Somogyi Effect: Morning High ... [https://beyondtype1.org/dawn-phenomenon-vs-somogyi-effect-morning-high-blood-sugars-explained/]
- 68. Rebound Hypoglycemia and Hyperglycemia in Type 1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11529140/]
- 69. Time in Range: How to Measure It, How to Report It, and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7755049/]
- 70. Core Glycemic Metrics Explained. TIR, TBR, TAR, GMI, CV, ... [https://www.adces.org/education/danatech/glucose-monitoring/continuous-glucose-monitors-(cgm)/glycemic-metrics--an-overview]
- 71. Low Blood Glucose (Hypoglycemia) | ADA [https://diabetes.org/living-with-diabetes/hypoglycemia-low-blood-glucose]
- 72. Factors Associated with Nocturnal Hypoglycemia in At-Risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4432491/]
- 73. Nocturnal Glucose Patterns with and without Hypoglycemia ... [https://www.mdpi.com/2075-4426/13/10/1454]
- 74. Special Diabetes Program: Research Resources - NIDDK [https://www.niddk.nih.gov/about-niddk/research-areas/diabetes/type-1-diabetes-special-statutory-funding-program/special-diabetes-program-research-resources]
- 75. Resources for Researchers [https://professional.diabetes.org/research-grants/resources-researchers]
- 76. Understanding the Somogyi Effect: Causes, Symptoms ... [https://www.africanjournalofdiabetesmedicine.com/articles/understanding-the-somogyi-effect-causes-symptoms-and-management-109987.html]