Overcoming the Lag: Advanced Strategies for Continuous Glucose Monitoring Sensor Delay Compensation in Clinical Research and Drug Development
Continuous Glucose Monitoring (CGM) has revolutionized metabolic research and therapy development, yet the inherent time lag between blood and interstitial fluid glucose measurements remains a critical challenge.
Overcoming the Lag: Advanced Strategies for Continuous Glucose Monitoring Sensor Delay Compensation in Clinical Research and Drug Development
Abstract
Continuous Glucose Monitoring (CGM) has revolutionized metabolic research and therapy development, yet the inherent time lag between blood and interstitial fluid glucose measurements remains a critical challenge. This article provides a comprehensive analysis for researchers and drug development professionals on the sources, implications, and compensation strategies for CGM sensor delay. We explore the physiological and technical foundations of delay, evaluate algorithmic and model-based compensation methodologies, and present optimization techniques for enhancing accuracy. The content synthesizes recent evidence on validation frameworks and comparative performance of leading CGM systems, offering a scientific foundation for improving clinical trial design, biomarker validation, and therapeutic intervention studies in diabetes and metabolic disorders.
The Physiology and Impact of CGM Sensor Delay: From Interstitial Fluid Dynamics to Clinical Consequences
Continuous Glucose Monitor latency originates from two primary sources: physiological lag and technical delay. The physiological lag, estimated at 6-10 minutes, stems from the time required for glucose to passively diffuse from blood capillaries into the interstitial fluid (ISF) where the sensor is located [1]. This delay can extend during rapid glucose changes, such as after a meal or insulin administration. The technical delay encompasses the time for glucose diffusion through sensor membranes, the electrochemical reaction time with the glucose oxidase enzyme, and the application of calibration algorithms to smooth the raw sensor signal [1]. Combined, these factors create a total time lag that typically ranges between 10-15 minutes compared to plasma glucose measurements [2] [1].
FAQ: How can researchers quantitatively measure and characterize CGM latency?
Researchers can employ standardized protocols to measure the total CGM latency. One key method involves conducting Oral Glucose Tolerance Tests (OGTT) while collecting paired plasma glucose (PG) and CGM measurements at regular intervals [2]. Two analytical approaches for quantifying the delay from this data are:
- MARD Minimization: The interstitial glucose measurements are systematically shifted in time (e.g., by 5, 10, and 15 minutes), and the time shift that results in the minimum Mean Absolute Relative Difference (MARD) between the CGM and PG values is identified as the total delay [2].
- Minimum Deviation Match: For each PG measurement, the CGM value that provides the smallest absolute difference within a plausible delay window (e.g., 0-15 minutes after the blood draw) is identified. The average of these optimal time shifts across all data points represents the delay [2]. Studies suggest this method may be more suitable due to less variability in timing glucose peaks [2].
The table below summarizes performance data from a latency characterization study using the SiJoy GS1 CGM during an OGTT [2].
Table 1: CGM Performance and Latency Data from an OGTT Study (n=129)
| Metric | Result | Context/Description |
|---|---|---|
| Overall MARD | 8.01% (± 4.9%) | Measured during the fasting phase [2]. |
| Consensus Error Grid | 89.22% in Zone A; 100% in Zones A+B | Indicates clinical accuracy [2]. |
| Suggested Delay (MARD Minimization) | 15 minutes | Identified at 30 minutes post-OGTT [2]. |
| Suggested Delay (Min. Deviation Match) | 10 minutes | Identified as the average delay time [2]. |
FAQ: What experimental protocols are used to evaluate CGM latency?
A detailed protocol for evaluating CGM sensor performance and latency is outlined below. This methodology is adapted from a clinical study performance evaluation [2].
Protocol: Evaluating CGM Latency via Oral Glucose Tolerance Test (OGTT)
- Objective: To assess the performance of a CGM system and characterize the time lag between plasma glucose (PG) and CGM measurements during rapid glucose excursions.
- Study Design: Cross-sectional observational study.
- Participants:
- Number: 129 participants with complete OGTT records [2].
- Inclusion Criteria: Healthy adults (aged 20-60 years), non-smokers, no history of diabetes, no recent medication use, blood pressure < 140/90 mmHg [2].
- Key Demographic Characteristics: Mean age 37.6 (± 11.2) years; 51.9% female, 48.1% male [2].
- Pre-Test Procedures:
- OGTT Execution:
- Data Management & Analysis:
- PG measurements are aligned with CGM values recorded at the same timestamp.
- Apply the MARD Minimization and Minimum Deviation Match methods to estimate the total time delay as described in FAQ #2.
- Calculate overall MARD and Consensus Error Grid analysis to determine clinical accuracy.
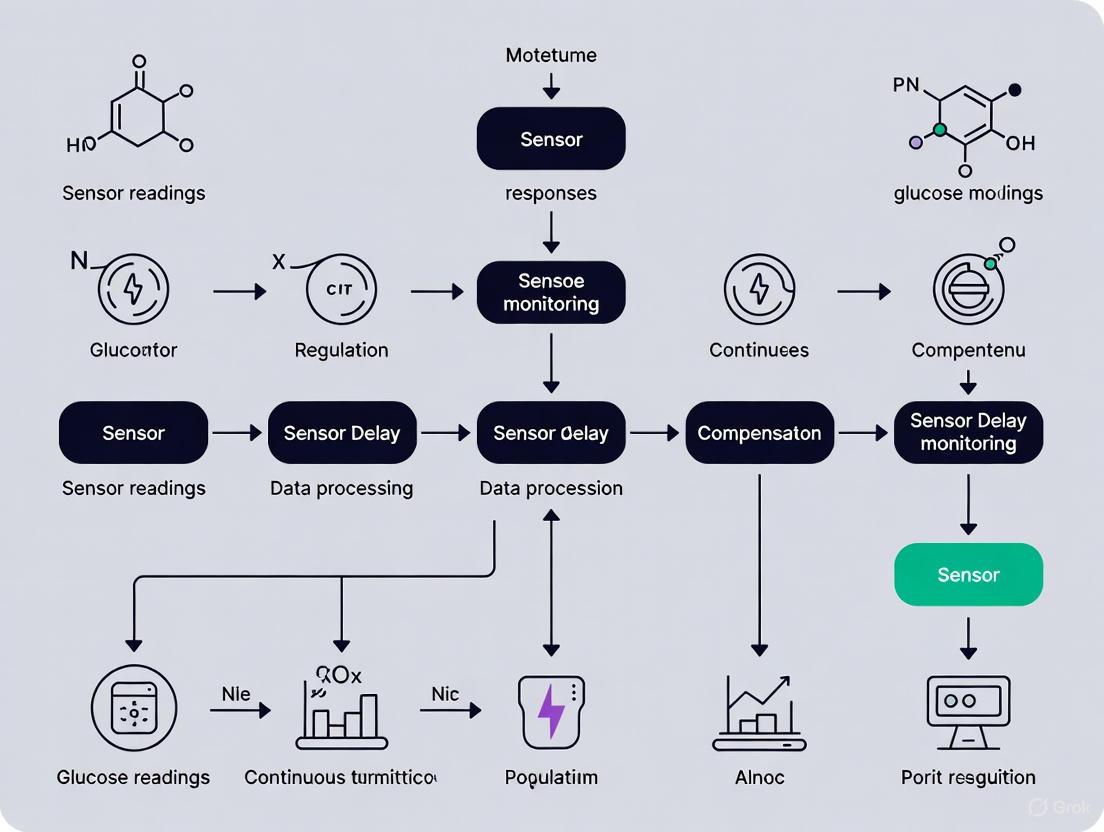
Diagram: Experimental Workflow for CGM Latency Characterization
FAQ: What are the clinical implications of CGM latency, especially during rapid glucose changes?
The intrinsic latency of CGM systems has direct clinical implications for data interpretation and patient management. During periods of rapidly changing glucose levels (e.g., postprandially or after insulin administration), the discrepancy between plasma glucose and the delayed interstitial glucose reading can be significant [1]. For instance, if blood glucose is dropping rapidly into a hypoglycemic range, the CGM value may still appear normal, potentially delaying critical alerts and interventions [1]. This is a key limitation that compensation algorithms aim to address. Modern CGM systems incorporate predictive alerts for upward and downward trends to partially mitigate this risk, providing warnings before severe hyperglycemia or hypoglycemia occurs [1].
FAQ: What novel computational approaches are being developed to compensate for CGM latency?
Emerging research focuses on using artificial intelligence (AI) and deep learning models to compensate for latency and improve glucose prediction. One innovative approach is the development of a "virtual CGM" [3]. This framework utilizes a deep learning model, specifically a bidirectional Long Short-Term Memory (LSTM) network with an encoder-decoder architecture, to infer current and future glucose levels [3]. Crucially, this model can operate independently of prior CGM readings during inference by leveraging comprehensive "life-log" data as input, including [3]:
- Dietary intake (calories, macronutrients)
- Physical activity (MET values, step counts)
- Temporal data (time of day)
This approach demonstrates the potential to maintain glucose monitoring during periods of CGM signal dropout or to support intermittent monitoring scenarios, effectively compensating for physical sensor limitations and delays [3].
Diagram: "Virtual CGM" Deep Learning Framework for Latency Compensation
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials and Reagents for CGM Latency Research
| Item / Solution | Function in Research Context |
|---|---|
| CGM Systems (e.g., SiJoy GS1, Dexcom G7) | The primary device under test; provides continuous interstitial glucose measurements for comparison against gold standard methods [2] [3]. |
| Oral Glucose Tolerance Test (OGTT) Kit | A standardized provocative test (typically 75g glucose) to induce rapid glycemic excursions, essential for characterizing sensor performance and latency under dynamic conditions [2]. |
| Enzymatic Plasma Glucose Assays | Gold-standard reference method for measuring glucose concentration in plasma samples obtained during venipuncture; used for calibrating and validating CGM accuracy [2]. |
| Biocompatible Skinfold Calipers | Tools to measure subcutaneous fat thickness at sensor insertion sites, a potential variable affecting physiological glucose diffusion time and sensor signal stability. |
| Data Analysis Software (e.g., Python with scikit-learn, TensorFlow/PyTorch) | Platforms for implementing MARD calculations, error grid analysis, and developing advanced machine learning models (e.g., LSTM networks) for latency prediction and compensation [2] [3]. |
This technical support document provides evidence-based troubleshooting guidance for researchers investigating the time lag between plasma and interstitial glucose dynamics. The physiological delay in glucose transport from the vascular compartment to the interstitial space is a critical factor affecting the accuracy of continuous glucose monitoring (CGM) systems. This guide synthesizes findings from recent Oral Glucose Tolerance Test (OGTT) studies to help you design better experiments and optimize sensor delay compensation algorithms.
Frequently Asked Questions (FAQs)
FAQ 1: What is the typical physiological time lag between plasma and interstitial glucose? The intrinsic physiological time lag—the time required for glucose to travel from blood capillaries to the interstitial fluid—is generally shorter than the total lag observed with CGM systems. Direct measurement using glucose tracers and microdialysis in fasted, healthy adults has found this physiological delay to be approximately 5-6 minutes [4]. Another study using multitracer plasma and interstitium data reported an "equilibration time" of 9.1 and 11.0 minutes in healthy and type 1 diabetic subjects, respectively [5]. The total observed lag during an OGTT is often longer due to additional technical factors.
FAQ 2: Why does the observed lag during an OGTT often exceed the physiological lag? The lag reported in OGTT studies (often 10-15 minutes) represents the combined effect of the physiological lag and technical delays introduced by the CGM system itself [2]. Technical factors include the sensor's electrochemical response time and the signal processing algorithms (such as filtering) applied to raw CGM data to reduce noise [5] [6]. This is why the total lag is greater than the pure physiological transport time.
FAQ 3: How does the plasma-interstitium glucose relationship change during rapid glucose shifts? The agreement between plasma and interstitial glucose values is not constant. During the dynamic phases of an OGTT (e.g., at 30 and 60 minutes), CGM devices tend to underestimate plasma glucose levels, with mean differences of -1.1 mmol/L at 30 min and -1.4 mmol/L at 60 min reported in one study [7]. This phenomenon, where CGM underestimates high plasma glucose values, can lead to an underestimation of hyperglycemic excursions [7].
FAQ 4: Is the time lag consistent across all patient populations? No, the lag can vary based on population characteristics. For instance, one study noted a proportional bias at 0 and 120 minutes of the OGTT, meaning the difference between CGM and OGTT values increased as the mean glucose concentration increased [7]. Furthermore, glucose kinetics may differ between healthy individuals and those with diabetes [5].
FAQ 5: Can CGM replace plasma glucose measurements for assessing glucose tolerance? Current evidence suggests caution. One study in a prediabetic population concluded that due to poor agreement with wide 95% limits of agreement and proportional bias, the potential for using CGM alone to assess glucose tolerance is questionable [7]. However, other research indicates that CGM glucose can be a viable alternative for calibrating personalized models of glucose-insulin dynamics, with the advantage of being minimally invasive [8].
Table 1: Reported Time Lags Between Plasma and Interstitial Glucose
| Study Population | Experimental Condition | Reported Time Lag (minutes) | Key Findings |
|---|---|---|---|
| Healthy Adults [4] | Fasting; Intravenous Tracer Bolus | 5.3 - 6.2 | Direct measurement of physiological glucose transport using tracers and microdialysis. |
| Healthy & T1DM Subjects [5] | Fasting; Multitracer & Microdialysis | 9.1 (Healthy), 11.0 (T1DM) | Model-derived "equilibration time." Suggests a slightly longer lag in T1DM. |
| Prediabetes & Overweight [7] | OGTT; CGM (Medtronic iPro2) | Best match found within a 0-15 min window | CGM values were consistently below OGTT values during post-challenge period. |
| Healthy Adults [2] | OGTT; CGM (SiJoy GS1) | 10-15 (Method-dependent) | One minimization method suggested a 15-min delay; another proposed 10 min. |
Table 2: Mean Differences Between CGM and OGTT Plasma Glucose Values During an OGTT in Prediabetes [7]
| OGTT Time Point (minutes) | Mean Difference (CGM - OGTT) mmol/L (SD) |
|---|---|
| 0 (Fasting) | 0.2 (0.7) |
| 30 | -1.1 (1.3) |
| 60 | -1.4 (1.8) |
| 120 | -0.5 (1.1) |
Experimental Protocols for Lag Assessment
Protocol 1: Lag Assessment During a Standard OGTT
This protocol is suitable for evaluating the combined physiological and technical lag of a CGM system in a clinical setting [7] [2].
- Participant Preparation: Participants should fast for ≥10 hours overnight. Avoid vigorous exercise, illness, and medications that affect glucose tolerance for at least 3 days prior to the test.
- Sensor Insertion: Insert the CGM sensor (e.g., on the abdomen or posterior upper arm) at least 48 hours before the OGTT to allow the sensor to stabilize and the local tissue trauma to subside [2].
- OGTT Execution:
- Collect a baseline venous blood sample (t=0 min).
- Administer a standardized 75g glucose drink within 5 minutes.
- Collect subsequent venous plasma samples at key time points (e.g., 30, 60, 120 minutes post-load).
- CGM Data Collection: Ensure the CGM device is set to record glucose concentrations every 5 minutes throughout the OGTT.
- Calibration: Calibrate the CGM device according to the manufacturer's instructions using capillary or plasma glucose values. Note the timing of calibration as it can affect accuracy.
- Data Alignment and Analysis:
- Minimum Deviation Match: For each post-challenge plasma glucose value, find the CGM value within a 0-15 minute window that results in the smallest absolute difference. Record the time difference for each match [7] [2].
- MARD Minimization: Shift the entire CGM time-series by fixed intervals (e.g., 5, 10, 15 minutes) and calculate the Mean Absolute Relative Difference (MARD) between the shifted CGM values and the plasma glucose values at the corresponding OGTT time points. The shift with the lowest MARD indicates the optimal lag compensation [2].
Protocol 2: Advanced Tracer Protocol for Physiological Lag
This complex protocol uses glucose tracers to isolate the physiological component of the lag [5] [4].
- Tracer Administration: Intravenously administer a bolus of stable or radioactive glucose tracers (e.g., [1-13C] glucose, [6,6-2H2] glucose).
- Simultaneous Sampling: Frequently and simultaneously collect timed samples of arterialized venous plasma and subcutaneous interstitial fluid using a technique like microdialysis with multiple catheters.
- Microdialysis Considerations: Account for the dead space and time delay inherent in the microdialysis system itself (e.g., a 6.2-minute transit time correction may be required) [4].
- Biochemical Analysis: Analyze plasma and microdialysate samples for glucose tracer enrichments using mass spectrometry.
- Kinetic Modeling: Model the plasma-to-ISF glucose kinetics using linear time-invariant compartmental models. The "equilibration time" (time constant) of the model characterizes the intrinsic delay [5].
Signaling Pathways and Experimental Workflows
Diagram 1: Glucose pathway from ingestion to CGM signal.
Diagram 2: Workflow for OGTT-based CGM lag assessment.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for Plasma-Interstitium Glucose Studies
| Item | Function / Application | Examples / Specifications |
|---|---|---|
| Continuous Glucose Monitors | Measures interstitial glucose concentrations at regular intervals (e.g., every 5 mins). | Medtronic iPro2 with Enlite sensor [7], SiJoy GS1 [2], DexCom, Abbott systems. |
| Glucose Tracers | Allows direct tracking of glucose kinetics between compartments without isotopic effects. | Stable isotopes: [1-13C] glucose, [6,6-2H2] glucose [5] [4]. |
| Microdialysis System | Directly samples interstitial fluid from subcutaneous tissue for quantitative analysis. | CMA microdialysis catheters (e.g., CMA 63) and perfusion pumps [4]. |
| Enzymatic Assays | Precisely measures glucose concentrations in plasma and microdialysate samples. | Hexokinase method (high precision) [9], Glucose Oxidase method. |
| Calibration Glucometer | Provides reference blood glucose values for CGM calibration during wear. | Contour XT glucometer [7]. |
| Mass Spectrometry | Measures very low concentrations and enrichment of glucose tracers in plasma and ISF. | Gas Chromatography-Mass Spectrometry (GC-MS) [4]. |
FAQ: Understanding Sensor Delay
What is sensor delay, and what causes it? Sensor delay, or lag time, refers to the phenomenon where Continuous Glucose Monitor (CGM) readings from interstitial fluid (ISF) lag behind blood glucose meter readings from capillary blood. This occurs for two main reasons:
- Physiological Delay: Glucose moves from the blood vessels into the interstitial fluid, a process that takes time, especially during periods of rapid glucose change [10].
- Technical Delay: The sensor itself requires time to process the glucose signal from the interstitial fluid [11]. The combined delay is typically up to 15 minutes [10] [11].
Why is sensor delay a critical concern for hypoglycemia detection? Sensor delay can postpone the recognition of a rapidly falling or low blood glucose event. A CGM might display a near-normal glucose value while the actual blood glucose level is already at or below the hypoglycemic threshold (≤4 mmol/L) [12] [10]. This lag can delay corrective action, increasing the risk and duration of a hypoglycemic episode, which is a leading cause of hospitalization in vulnerable populations like long-term care residents [12].
How does sensor delay affect core glycemic metrics like Time in Range (TIR)? Sensor delay can introduce inaccuracies into glycemic variability metrics. During rapid glucose transitions, the delay means CGM data does not reflect the real-time glycemic state. This can lead to:
- Underestimation of Hypoglycemia: The duration and severity of hypoglycemic events may be inaccurately represented, affecting the "Time Below Range" metric [12].
- Inaccurate Glycemic Excursion Mapping: The precise timing and amplitude of glucose peaks and troughs are shifted, which can skew the calculation of Time in Range and Glucose Management Indicator (GMI) [11].
Troubleshooting Guide: Mitigating the Impact of Sensor Delay in Research
Issue: Hypoglycemia events detected by CGM are not aligned with clinical observations or blood glucose measurements. Solution:
- Validate with Blood Glucose Meter (BGM): Always corroborate CGM readings below 4 mmol/L or during periods of rapid change with a fingerstick test from a calibrated BGM [13].
- Understand Lag Dynamics: Recognize that the delay is most pronounced when glucose levels are changing rapidly. Inform study protocols to account for this inherent limitation [10].
- Analyze Trend Arrows: Use the CGM's trend arrows (e.g., ↓→) as a more actionable indicator of glucose direction than a single, potentially lagging, glucose value.
Issue: Experimental data shows a systematic time shift between CGM and plasma glucose (PG) during an Oral Glucose Tolerance Test (OGTT). Solution: This is an expected physiological phenomenon. Implement a data processing methodology to quantify and compensate for the delay [11].
- MARD Minimization Method: Shift the CGM-derived ISF glucose measurements by set intervals (e.g., 5, 10, 15 minutes) and calculate the Mean Absolute Relative Difference (MARD) at each interval against PG. The optimal delay is determined by the shift that produces the minimum MARD [11].
- Minimum Deviation Match Method: Align each PG measurement with the CGM value that provides the smallest absolute difference within a plausible delay window (e.g., 0-15 minutes) after the blood draw. This method can be advantageous when there is high variability in individual glucose peak times [11].
Quantitative Data on Sensor Performance and Delay
Table 1: Clinical Performance of a CGM Sensor (SiJoy GS1) During OGTT [11]
| Performance Metric | Result (Fasting Phase) | Description |
|---|---|---|
| MARD | 8.01% (± 4.9) | Lower MARD indicates superior sensor accuracy. |
| 20/20% Consensus | 96.6% | Percentage of sensor values within 20% of reference value or within 20 mg/dL for values <100 mg/dL. |
| Error Grid (Zone A) | 89.22% | Values indicating clinically accurate readings. |
| Error Grid (Zone A+B) | 100% | Values indicating clinically acceptable readings. |
Table 2: Impact of CGM Implementation in Long-Term Care (LTC) [12]
| Metric | Baseline (Fingerstick) | Post-CGM Implementation | Change |
|---|---|---|---|
| Nursing Time per Test | 5.1 minutes | 3.1 minutes | 40% reduction |
| Total Glucose Readings | 19,438 | 35,971 | Increased frequency |
| Detected Hypoglycemic Events | 88 | 1,049 | 12-fold increase |
Experimental Protocols for Delay Compensation Research
Protocol: Quantifying Time Lag During an Oral Glucose Tolerance Test (OGTT) [11]
Objective: To evaluate the total time delay (physiological and technical) between plasma glucose (PG) and interstitial fluid glucose (ISFG) measured by CGM during standardized glucose excursions.
Materials:
- CGM system (e.g., SiJoy GS1, FreeStyle Libre 2, Dexcom G6)
- Participants (e.g., healthy adults or individuals with prediabetes/diabetes)
- Standard 75g glucose solution for OGTT
- Venous blood collection equipment
- Laboratory chemistry analyzer for PG measurement
Methodology:
- Sensor Placement: Apply the CGM sensor to the participant's posterior upper arm at least 48 hours before the OGTT to ensure stabilization.
- OGTT Procedure: After an overnight fast, participants ingest the 75g glucose solution within 10 minutes.
- Blood Sampling: Collect venous blood samples for PG measurement at predefined intervals (e.g., 0, 30, 60, 120, and 180 minutes).
- Data Collection: Record concurrent CGM values every 5 minutes throughout the test.
- Data Analysis: Apply the MARD Minimization or Minimum Deviation Match method (described above) to the paired PG-CGM data sets to calculate the optimal time delay.
Signaling Pathways and Experimental Workflows
CGM Sensor Delay Pathway
OGTT-Based Sensor Delay Evaluation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for CGM Delay Compensation Research
| Item | Function in Research |
|---|---|
| CGM Systems (e.g., Dexcom G6, Abbott Libre 2, SiJoy GS1, Medtronic Guardian) | The primary devices under investigation for their delay characteristics and accuracy metrics (MARD) [12] [11]. |
| Calibrated Blood Glucose Meter (BGM) | Provides the point-of-care reference value for validating CGM readings, especially during hypoglycemia or rapid glucose changes [13]. |
| Oral Glucose Tolerance Test (OGTT) Kit | A standardized tool (75g glucose) for creating a controlled and reproducible glycemic excursion to study sensor performance dynamics [11]. |
| Laboratory Plasma Glucose Analyzer | The gold-standard method for measuring venous plasma glucose, used as the primary reference for assessing CGM accuracy and calculating time lag [11]. |
| Data Analysis Software (e.g., Python, R, MATLAB) | Used to implement and run delay compensation algorithms (MARD minimization, deviation matching) on synchronized PG and CGM data sets [11]. |
For researchers developing non-adjunctive glucose monitoring systems—where patients make therapy decisions without confirmatory fingerstick testing—establishing robust accuracy thresholds is paramount. The Mean Absolute Relative Difference (MARD) serves as the primary benchmark for quantifying Continuous Glucose Monitoring (CGM) sensor performance [14]. A lower MARD value indicates higher accuracy, with a MARD under 10% generally considered acceptable for insulin dosing decisions [14]. However, MARD is an average value and may mask clinically significant inaccuracies at glycemic extremes (hypoglycemia or hyperglycemia), necessitating complementary metrics for a complete performance evaluation [14].
Regulatory distinctions critically impact therapy development. Devices are categorized as either adjunctive (requiring confirmation via finger-prick testing before insulin dosing) or non-adjunctive (approved for independent insulin-dosing decisions) [14]. The regulatory bar is higher for non-adjunctive use. In the US, this typically involves the FDA's "integrated CGM" (iCGM) designation and Class III pre-market approval, which demands stricter criteria for accuracy, reliability, and interoperability [14]. CE or UKCA marking, while necessary for market access in Europe, does not itself guarantee a device's suitability for non-adjunctive insulin dosing [14].
Essential Accuracy Metrics & Performance Data
Beyond MARD, a comprehensive sensor evaluation requires additional metrics that provide a more nuanced view of clinical accuracy, especially in hypoglycemic and hyperglycemic ranges critical for patient safety.
Table 1: Key CGM Accuracy Metrics for Non-Adjunct Use Evaluation
| Metric | Definition | Clinical Significance for Therapy Development |
|---|---|---|
| MARD | Mean Absolute Relative Difference; the average variance between CGM readings and reference values [14]. | Primary benchmark; a value <10% is a common target for insulin-dosing systems [14]. |
| 20/20 Accuracy | Percentage of CGM values within ±1.1 mmol/L (±20 mg/dL) of reference at glucose <5.5 mmol/L, or within ±20% at glucose ≥5.5 mmol/L [14]. | Measures clinically accurate readings; higher percentages indicate greater reliability for safe dosing. |
| 40/40 Accuracy | Percentage of CGM values within ±2.2 mmol/L (±40 mg/dL) of reference at glucose <5.5 mmol/L, or within ±40% at glucose ≥5.5 mmol/L [14]. | Identifies readings with larger errors that could lead to significant insulin dosing mistakes. |
The following diagram illustrates the foundational workflow for establishing CGM accuracy, integrating these core metrics and regulatory considerations.
CGM Accuracy Evaluation Workflow
Researcher FAQs on CGM Performance
Q: What are the internationally accepted criteria for a robust CGM performance study design? A: A trustworthy study design for non-adjunctive use should meet five key criteria endorsed by the Clinical and Laboratory Standards Institute (CLSI) and the International Federation for Clinical Chemistry (IFCC) Working Group [14]:
- Peer-reviewed data
- Population: Inclusion of more than 70% of participants with type 1 diabetes.
- Challenges: Use of meal and insulin challenges to test performance under real-world conditions.
- Range: Evaluation across a broad glucose range (typically 2.2–22.2 mmol/L).
- Episodes: Inclusion of both hypoglycemic and hyperglycemic episodes.
Q: Why is MARD alone an insufficient metric for certifying a device for non-adjunctive use? A: While MARD is a valuable average, it can obscure critical performance issues. A device might have a low overall MARD yet perform poorly in the hypoglycemic range, where accurate readings are most critical for preventing severe adverse events. Therefore, regulators and developers must analyze metrics like 20/20 and 40/40 accuracy, which provide a clearer picture of performance at the clinically critical extremes [14].
Q: What are common real-world failure modes that performance studies should seek to replicate? A: Beyond controlled clinical settings, researchers must account for scenarios reported by users [15] [16]:
- Compression Lows: Falsely low readings caused by pressure on the sensor (e.g., during sleep), which can lead to unnecessary carbohydrate intake or ignored alarms [15] [16].
- Sensor Displacement/Adhesive Failure: Physical issues leading to sensor detachment or erroneous data [15].
- Connectivity Issues: Bluetooth drops or smartphone notification settings that prevent critical alerts from reaching the user [15].
- Algorithmic Drift: Sensor inaccuracies that develop over the wear period due to manufacturing defects or body chemistry interactions [15].
Troubleshooting Guide: Experimental & Device Errors
This guide addresses specific issues researchers might encounter during bench testing and clinical validation of CGM systems.
Table 2: Troubleshooting CGM Research & Development Challenges
| Problem Scenario | Root Cause | Investigation & Resolution Protocol |
|---|---|---|
| Unexplained MARD Increase | Sensor manufacturing batch defects, unstable enzyme chemistry, or biocompatibility issues (foreign body response). | 1. Lot Analysis: Compare MARD by sensor lot number. 2. Accelerated Aging: Test sensor stability under various environmental conditions. 3. Histology: In animal studies, examine tissue surrounding the sensor for inflammation. |
| Compression Lows in Data | Physical pressure on sensor site altering interstitial fluid dynamics [15] [16]. | 1. Algorithm Filtering: Develop and validate algorithms to detect and flag pressure-artifact signals. 2. Placement Guidance: Define and validate optimal anatomical placement sites to minimize pressure in protocols. 3. Subject Reporting: Implement robust participant reporting for sleep position and physical activity. |
| Connectivity Gaps in Data Stream | Bluetooth interference, receiver hardware failure, or software bugs in data handling [15]. | 1. Signal Mapping: Document signal strength and drop-out locations in clinical settings. 2. Hardware Diagnostics: Implement built-in receiver diagnostics to log connection health. 3. Data Bridging: Develop algorithms to intelligently bridge short data gaps. |
| Inaccurate Hyperglycemia Readings | Sensor "drift" due to biofouling, delayed interstitial fluid (ISF) equilibrium, or calibration errors. | 1. ISF Lag Characterization: Quantify plasma-to-ISF lag time under hyperglycemic clamps. 2. Dynamic Calibration: Investigate multi-point calibration models that account for rate-of-change. 3. Reference Verification: Ensure frequent and accurate reference measurements (e.g., YSI) during high glucose periods. |
The signaling pathway below outlines the logical relationship between a CGM reading error and its potential downstream consequences, which is vital for risk assessment in therapy development.
CGM Error Consequence Pathway
Experimental Protocols for Sensor Validation
Protocol 1: Assessing Clinical Accuracy Against Reference Standards Objective: To determine the MARD, 20/20, and 40/40 accuracy of a CGM system across the glycemic range. Methodology:
- Participant Cohort: Recruit a minimum of 100 subjects, with over 70% having type 1 diabetes to ensure testing under conditions of significant glycemic variability [14].
- Reference Method: Use a clinically approved reference method such as a YSI blood analyzer or frequent capillary blood glucose testing with a validated meter.
- Clamp Protocol: Implement glucose challenges, including meal tests and insulin-induced hypoglycemia, to generate a wide range of glucose values (target: 2.2 to 22.2 mmol/L) [14].
- Data Pairing: Collect a minimum of 150-200 paired data points (CGM vs. reference) per subject over the sensor's wear period.
- Analysis: Calculate overall MARD, MARD by glucose range, and the percentages of points meeting 20/20 and 40/40 criteria [14].
Protocol 2: Investigating Sensor Delay (ISF Lag) Compensation Objective: To characterize and model the physiological time lag between blood and interstitial fluid glucose. Methodology:
- Hyperglycemic Clamp: Establish a steady-state hyperglycemic level in a clinical research unit.
- High-Frequency Sampling: Measure plasma glucose and CGM values simultaneously at 1-5 minute intervals during the clamp's upward ramp and subsequent decline.
- Time-Series Analysis: Use cross-correlation analysis to determine the average time lag between plasma and ISF glucose trajectories.
- Algorithm Development: Train a predictive compensation algorithm (e.g., using Kalman filtering or a machine learning model) on one dataset and validate it on a separate hold-out dataset to improve real-time accuracy.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for CGM Performance and Delay Research
| Research Tool | Function in CGM Development |
|---|---|
| YSI 2300 STAT Plus Analyzer | The gold-standard reference instrument for measuring plasma glucose in clinical studies, providing the benchmark for MARD calculation [14]. |
| Glucose Clamp Apparatus | A system for performing hyperinsulinemic-euglycemic or hyperglycemic clamps, allowing controlled manipulation of blood glucose to test sensor performance and lag [17]. |
| Continuous Glucose Monitoring Simulator (e.g., UVA/Padova Simulator) | A validated computer model of the glucose-insulin system that allows for in-silico testing of sensor algorithms and lag compensation methods without initial human trials. |
| Biofouling Characterization Materials | Tools (e.g., ELISA kits, histology stains) to analyze protein adsorption and inflammatory cell attachment on explanted sensors, investigating causes of signal drift. |
| Kalman Filter / Machine Learning Framework | A software framework (e.g., in Python/MATLAB) for developing and testing predictive algorithms that compensate for sensor noise and physiological ISF lag. |
This technical support center is designed for researchers and scientists investigating the interindividual variability in metabolic rate and physiology, with a specific focus on its implications for continuous glucose monitoring (CGM) sensor delay compensation. A profound understanding of these biological variabilities is critical for developing next-generation CGM systems and robust compensation algorithms. The guides and FAQs that follow address common experimental challenges, provide standardized protocols for measuring key metabolic parameters, and offer resources for troubleshooting CGM data acquisition in a research setting. The core premise is that the delay characteristics observed in CGM signals are not merely a technological artifact but are significantly influenced by the underlying physiological heterogeneity of the human body.
Researcher FAQs & Troubleshooting Guides
Frequently Asked Questions (FAQs)
FAQ 1: Why is understanding interindividual variability in metabolic rate crucial for CGM delay compensation research?
Interindividual variability in metabolic rate signifies that the same physiological event (e.g., a glucose bolus) will be processed at different rates by different individuals. This metabolic heterogeneity is a primary source of the variability observed in the physiological lag between blood glucose and interstitial fluid glucose. Compensation algorithms that assume a fixed population-wide delay will therefore be inherently inaccurate for a significant portion of users. Research into this variability allows for the development of personalized delay models that can significantly improve CGM accuracy [18].
FAQ 2: What are the primary physiological factors contributing to CGM sensor delay?
The sensor delay is a composite of several physiological processes:
- Physiological Lag: The time required for glucose to diffuse from capillaries into the interstitial fluid (ISF). This is influenced by local blood flow, capillary wall permeability, and the metabolic rate of the subcutaneous tissue.
- Sensor Response Time: The electrochemical reaction time of the sensor itself, which is typically a constant but can be influenced by local tissue reactions that vary between individuals.
- Data Processing and Smoothing: The algorithmic processing applied by the CGM system to raw sensor data. The interplay of these factors means that the total observed delay is not a static value but can fluctuate within and between individuals based on their unique and dynamic physiology [19].
FAQ 3: How can I control for intra-individual variation in metabolic rate during my experiments?
Intra-individual variation in Basal Metabolic Rate (BMR) can be significant. Key experimental controls include:
- Strict Fasting Protocol: Ensure subjects are in a true post-absorptive state. Non-compliance with fasting can increase the within-subject coefficient of variation (CV) in BMR measurements [20].
- Standardize Pre-Test Activity: Monitor and, if possible, standardize physical activity levels for 24-72 hours prior to metabolic testing using tools like tri-axial accelerometers. While one study found BMR measurements were reproducible despite day-to-day activity variations, controlling for this variable reduces unexplained noise [20].
- Regular Equipment Calibration: Conduct regular function checks of metabolic measurement systems (e.g., ventilated-hood systems) to account for within-machine variability [20].
FAQ 4: My research CGM system is experiencing frequent signal loss. What are the common causes?
Signal loss interrupts the continuous data stream, which is fatal for delay characterization studies. Common causes include:
- Bluetooth Connectivity Issues: The display device (smartphone/receiver) is too far from the sensor (beyond ~20 feet) or has obstructions (walls, water) between them [21] [22].
- Device-Specific Software: Outdated CGM app versions may not be compatible with new transmitter serial numbers or operating systems (e.g., iOS/Android updates) [23] [22].
- Incorrect Device Settings: Features like "Locked and Hidden apps" in iOS 18 can block critical glucose alarms and data transmission [22].
Step-by-Step Troubleshooting Guides
Problem: Inconsistent CGM Sensor Accuracy During a Clinical Study
| Step | Action | Rationale & Reference |
|---|---|---|
| 1 | Verify sensor code entry and warm-up period completion. | An incorrect sensor code or interrupted warm-up can compromise factory calibration. The G6 and G7 are factory-calibrated and should not require user calibration if the code is entered correctly [23] [24]. |
| 2 | Inspect the sensor insertion site for pressure (pressure-induced sensor attenuation) or irritation. | Mechanical pressure on the sensor can cause falsely low readings. Ensure the site is free from tight clothing or positions that cause pressure during sleep or rest [23]. |
| 3 | Cross-validate with a reference method (e.g., Yellow Springs Instrument). | If readings seem inaccurate, use a high-quality, calibrated reference method to establish ground truth. Note that temporary mismatches can occur, but values should converge over time [23]. |
| 4 | Check for confounding medications. | Unlike earlier models, Dexcom G6 and G7 are not affected by common NSAIDs like ibuprofen, but it is critical to verify the latest drug-interaction charts for the specific sensor model in use [21]. |
| 5 | Document and report the sensor. | For a systematic study, note the sensor's serial number and session details. Manufacturers have replacement policies for confirmed sensor failures, which can be tracked for quality control in your research [21] [23]. |
Problem: Connectivity and Data Transmission Failure to Research Display Device
| Step | Action | Rationale & Reference |
|---|---|---|
| 1 | Confirm proximity and clear line-of-sight between sensor and display device. | Bluetooth has a limited range (~20 feet) and can be blocked by physical obstacles. Keep the devices in close, unobstructed proximity [22]. |
| 2 | Toggle device Bluetooth off and on. | This resets the Bluetooth stack and can often re-establish a lost connection [22]. |
| 3 | Restart the display device (smartphone/receiver). | A device reboot clears temporary software glitches that may be preventing communication [22]. |
| 4 | Update the CGM application to the latest version. | Older app versions may lack compatibility with new transmitters or operating systems. Always use the latest verified research-compatible version [23]. |
| 5 | Check for operating system compatibility. | Before updating phone OS (e.g., to iOS 18), consult the manufacturer's compatibility guide. New OS features can interfere with app functionality and alarm delivery [22]. |
Quantitative Data & Sensor Specifications
CGM Sensor Performance Metrics for Research Selection
The following table summarizes key performance characteristics of common CGM sensors, which are critical for designing experiments on delay compensation. Accuracy, measured by MARD, is a primary differentiator.
Table 1: Comparative Performance Metrics of Dexcom CGM Sensors for Research Applications
| Sensor Model | MARD (%) | Warm-up Time (min) | Sensor Life (days) | Calibration Required? | Key Research Application |
|---|---|---|---|---|---|
| Dexcom G7 | 8.2 [24] | 30 [24] | 10.5 | No | Ideal for studies requiring the lowest intrinsic sensor delay and highest accuracy. |
| Dexcom G6 | 9.0 [24] | 120 [24] | 10 | No | The established benchmark; extensive literature for validation and comparison studies. |
| Dexcom ONE+ | Not specified (Marketed as "most accurate") [24] | Not specified | 10 | No | A cost-effective option for large-scale population studies on variability. |
Quantitative Data on Metabolic Rate Variability
Understanding the expected range of metabolic variability is essential for powering studies and interpreting results.
Table 2: Measured Variability in Human Metabolic Parameters
| Metabolic Parameter | Type of Variability | Measured Coefficient of Variation (CV) | Key Influencing Factors | Experimental Control Recommendations |
|---|---|---|---|---|
| Basal Metabolic Rate (BMR) | Intra-individual | 3.3% (range 0.4% - 7.2%) [20] | Fasting status, physical activity prior to testing, machine variability [20]. | Strict fasting, pre-test activity monitoring, regular equipment calibration [20]. |
| Basal Metabolic Rate (BMR) | Interindividual | Can be "significant" after controlling for known factors [18] | Body composition, age, sex, genetic factors, thyroid function [18]. | Precise phenotyping of participants (e.g., DEXA scans) for use as covariates in analysis. |
| Total Daily Energy Expenditure | Interindividual | Significant variability exists beyond BMR [18] | Diet-induced thermogenesis, exercise, non-exercise activity thermogenesis (NEAT) [18]. | Standardized diet and activity protocols in controlled settings. |
Standardized Experimental Protocols
Protocol for Assessing Intra-Individual BMR Variation
Objective: To reliably measure the within-subject variation in Basal Metabolic Rate using a standard out-patient protocol. Materials: Ventilated-hood indirect calorimetry system, tri-axial accelerometer, subject questionnaire. Methodology:
- Participant Preparation: Participants spend the night before testing at home and transport themselves to the lab. They must fast for a minimum of 12 hours prior to the measurement.
- Pre-Test Activity Monitoring: Participants wear a tri-axial accelerometer for the 3 days preceding each BMR measurement to quantify habitual physical activity.
- BMR Measurement: Upon arrival, the subject rests in a supine position in a thermoneutral, quiet, and dimly lit room for 30 minutes. BMR is then measured via indirect calorimetry for a minimum of 30 minutes, following manufacturer guidelines.
- Replication: The measurement is repeated three times with 2-week intervals to assess variability.
- Data Validation: Exclude measurements from analysis if protocol non-compliance is reported (e.g., non-fasting). Correct for within-machine variability based on regular system checks [20].
Protocol for Correlating Metabolic Phenotypes with CGM Delay
Objective: To characterize the relationship between an individual's metabolic phenotype and the observed physiological delay in CGM readings. Materials: CGM system (e.g., Dexcom G7), reference blood glucose analyzer (e.g., YSI), indirect calorimeter, food and exercise standardization materials. Methodology:
- Participant Phenotyping:
- Measure BMR via indirect calorimetry as in Protocol 4.1.
- Conduct body composition analysis (e.g., DEXA or BIA).
- Administer an oral glucose tolerance test (OGTT) with frequent venous blood sampling to establish individual glucose metabolism dynamics.
- CGM Data Collection: Apply a CGM sensor to each participant according to manufacturer instructions. Simultaneously, collect frequent capillary or venous blood samples over a 24-48 hour period that includes standardized meals and activities for reference glucose values.
- Delay Calculation: For each meal or glucose excursion, calculate the physiological lag by cross-correlating the CGM trace with the reference blood glucose trace to find the time shift that produces the maximum correlation.
- Data Analysis: Use multiple regression analysis to model the calculated delay time as a function of the phenotypic variables (BMR, body composition indices, OGTT results).
Conceptual Diagrams & Workflows
Factors of Sensor Delay
Experiment Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for Metabolic and CGM Delay Research
| Item | Function in Research | Example/Notes |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Captures continuous interstitial glucose readings for delay analysis. | Dexcom G7 (high accuracy, short warm-up) [24] or Dexcom G6 (extensively validated) [24]. |
| Reference Blood Glucose Analyzer | Provides the "gold standard" blood glucose measurement for calibrating and validating CGM delay. | Yellow Springs Instruments (YSI) Life Sciences analyzer. |
| Indirect Calorimeter | Precisely measures Basal Metabolic Rate (BMR) and Resting Energy Expenditure (REE) for metabolic phenotyping. | Ventilated-hood systems (e.g., Cosmed Quark CPET). |
| Tri-axial Accelerometer | Objectively quantifies physical activity levels before and during metabolic testing to control for this variable. | Devices used for research-grade activity monitoring. |
| Body Composition Analyzer | Quantifies fat mass, lean body mass, and total body water, which are key covariates for metabolic rate. | Dual-Energy X-ray Absorptiometry (DEXA) scanner or Bioelectrical Impedance Analysis (BIA) scale. |
| Data Analysis Software | For statistical modeling, cross-correlation analysis, and development of machine learning algorithms for delay compensation. | Python/R, Dexcom Clarity Software [24], custom signal processing toolboxes. |
Algorithmic Solutions and Technical Approaches for Real-Time Sensor Delay Compensation
Troubleshooting Guide and FAQs
Frequently Asked Questions (FAQs)
Q1: What are the primary sources of time delay in Continuous Glucose Monitoring (CGM) signals, and how do they impact sensor performance? CGM signals are affected by a combination of physiological and technological time delays. The physiological delay, primarily due to the time required for glucose to diffuse from blood capillaries to the interstitial fluid (ISF) where most sensors are placed, is estimated to be 5-10 minutes on average [25]. The technological delay arises from sensor-specific factors, including the diffusion of glucose through the sensor's protective membranes, the speed of the electrochemical reaction, and the mathematical filtering applied to the raw signal to reduce noise. The total time delay can range from 5 to 40 minutes [25]. This delay can hamper the detection of rapid glucose changes, such as impending hypoglycemic events, and negatively impact the calculated Mean Absolute Relative Difference (MARD), a key metric for sensor accuracy [25].
Q2: How does a Kalman filter improve real-time CGM signal processing? The Kalman filter is a recursive algorithm ideally suited for real-time analysis of nonstationary time series data, such as CGM signals [26]. Its primary advantages include:
- Real-time Adaptation: It can adapt, in real-time, to abrupt changes in the signal baseline caused by external disturbances or physiological changes [26].
- Noise Reduction: It effectively reduces measurement noise without introducing significant lag, providing a smoother and more reliable glucose trend [26].
- Predictive Capability: By leveraging the dynamics of glucose diffusion between blood and tissue, the Kalman filter can estimate current blood glucose levels from interstitial fluid measurements, accounting for the inherent time delay [27]. One implementation uses the filter to improve the estimation accuracy of blood glucose levels from interstitial measurements [27].
Q3: What is time-dependent zero-signal correction, and what problem does it solve? Time-dependent zero-signal correction is a method to compensate for a sensor's baseline drift over time. The "zero-signal" refers to the sensor's output in the absence of the target analyte (e.g., glucose). This baseline is not static and can drift due to factors like sensor aging and material degradation [28] [29]. The method involves accurately determining this time-dependent zero-signal level and subtracting it from the continuous sensor signal [27]. This compensates for drift and interference, resulting in a more accurate representation of the actual glucose concentration in the body fluid [27].
Q4: My CGM data shows sudden, sharp drops. Could this be a compression artifact, and how can it be detected? Yes, sudden, sharp drops can be caused by compression artifacts, which occur when pressure is applied to the sensor site, temporarily disrupting the ISF glucose reading and potentially causing false hypoglycemia alarms. A patented method for real-time detection involves comparing clearance values between consecutive CGM readings to their normal distributions. If the clearance values fall outside these normal distributions, it indicates a compression artifact, allowing the system to flag the data point and prevent false alarms or inappropriate insulin shutoff [27].
Q5: What advanced machine learning approaches are being used for long-term drift compensation? Beyond traditional filters, advanced AI techniques are being explored to handle complex, nonlinear drift patterns. One novel framework combines an iterative random forest-based algorithm for real-time error correction with an Incremental Domain-Adversarial Network (IDAN) for long-term drift compensation [29]. The random forest algorithm leverages data from multiple sensor channels to identify and rectify abnormal responses, while the IDAN uses domain-adversarial learning to manage temporal variations in sensor data, significantly enhancing long-term data integrity [29].
Troubleshooting Common Experimental Issues
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| High signal noise obscuring trends | Intrinsic electronic noise; environmental interference. | Apply a Kalman filter [26] or moving average filter. Balance filter length to avoid introducing excessive time delay [25]. |
| Systematic drift over sensor lifetime | Sensor aging (biofouling, material degradation) [25] [29]. | Implement time-dependent zero-signal correction [27] or employ machine learning models (e.g., Incremental Domain-Adversarial Network) trained for long-term drift compensation [29]. |
| Discrepancy between CGM and blood glucose during rapid changes | Physiological time lag (BG-to-ISF delay) and technological delay [25]. | Use a prediction algorithm or a Kalman filter to estimate blood glucose from ISF measurements, reducing the effective delay by several minutes [25] [27]. |
| Sudden, unrealistic signal dips | Compression artifact from physical pressure on the sensor [27]. | Implement a real-time detection algorithm that analyzes signal clearance values to identify and flag compression events [27]. |
| Declining sensor accuracy after initial calibration | Time-varying sensor sensitivity and calibration error [30]. | Utilize factory calibration parameters with machine learning or adopt dual-sensor calibration methods to estimate personalized, time-varying constants [27]. |
Experimental Protocols and Methodologies
Protocol 1: Implementing a Kalman Filter for CGM Signal Enhancement
Objective: To reduce noise and improve the real-time estimation of blood glucose from CGM (interstitial fluid) data.
Principles: The Kalman filter is a recursive estimator that optimally combines predictions from a process model with new measurements, each with known uncertainty. For CGM, the process model often describes glucose flux dynamics [27] [26].
Methodology:
- State Definition: Define the state vector. In its simplest form, this could be the true glucose level and its rate of change (e.g., ( xk = [Gk, Ḡk]^T ), where ( Gk ) is glucose concentration and ( Ḡ_k ) is its derivative at time ( k )).
- Process Model: Define a state transition model that predicts the next state. For example: ( x{k+1} = F \cdot xk + wk ), where ( F ) is the state transition matrix and ( wk ) is the process noise (assumed to be normally distributed).
- Measurement Model: Define how the sensor measurements relate to the state. Typically, ( zk = H \cdot xk + vk ), where ( zk ) is the CGM measurement, ( H ) is the observation matrix, and ( v_k ) is the measurement noise.
- Algorithm Execution: For each new CGM reading, execute the two-step Kalman filter algorithm:
- Predict Step: Project the previous state and error covariance forward.
- Update Step: Compute the Kalman gain, update the state estimate with the new measurement, and update the error covariance.
The filter's capability to adapt to nonstationary data makes it particularly valuable for handling the abrupt signal changes common in CGM data [26].
Protocol 2: Applying Time-Dependent Zero-Signal Correction
Objective: To compensate for the long-term baseline drift of a CGM sensor, thereby improving accuracy over its functional lifetime.
Principles: This method addresses the systematic deviation of a sensor's baseline (zero-signal) over time, which is a key component of sensor drift [27] [29].
Methodology:
- Baseline Characterization: During sensor development or a dedicated calibration period, characterize the zero-signal output of the sensor over time in a controlled, analyte-free environment.
- Model Fitting: Model the zero-signal drift as a function of time. This model could be a simple linear function, a polynomial, or a more complex machine-learned model, depending on the observed drift behavior.
- Real-time Correction: During sensor operation, continuously or periodically calculate the estimated zero-signal level based on the model and the sensor's elapsed operational time.
- Signal Adjustment: Subtract the estimated zero-signal value from the raw sensor signal to obtain the corrected glucose value:
Corrected Signal = Raw Sensor Signal - Time-Dependent Zero-Signal[27].
This approach directly counters one of the fundamental causes of inaccuracy in long-term sensor deployments [29].
Performance Data and Technical Specifications
Table 1: Quantitative Performance of Signal Processing Algorithms
| Algorithm / Method | Key Performance Metric | Result / Value | Context / Conditions |
|---|---|---|---|
| Kalman Filter [27] | Improved delay estimation | Enables real-time BG estimation from ISF | Accounts for BG-to-ISF glucose diffusion dynamics. |
| Time-Dependent Zero-Signal Correction [27] | Compensates for sensor drift | Results in a more accurate glucose representation | Applied to raw CGM signal to counter drift and interference. |
| Prediction Algorithm [25] | Reduction in time delay | Average reduction of 4 minutes | Applied to CGM raw signals with an overall mean delay of 9.5 minutes. |
| Iterative Random Forest + IDAN [29] | Data integrity & drift compensation | Achieved robust accuracy with severe drift | Tested on a metal-oxide gas sensor array dataset over 36 months. |
| Random Forest Regressor [30] | Mean Absolute Error (MAE) | 16.13 mg/dL | Model trained on a generated dataset of 500 sensor responses. |
| Support Vector Regressor [30] | Mean Absolute Error (MAE) | 16.22 mg/dL | Model trained on a generated dataset of 500 sensor responses. |
Table 2: Research Reagent Solutions and Essential Materials
| Item | Function in Research | Example / Specification |
|---|---|---|
| CGM Sensor Simulator | Generates realistic glucose and sensor response data for algorithm development and testing. | Simglucose (FDA-approved UVa/Padova Simulator) [30]. |
| Long-term Drift Dataset | Provides benchmark data for developing and evaluating drift compensation algorithms. | Gas Sensor Array Drift (GSAD) Dataset [29] or a modern 62-sensor E-nose dataset [28]. |
| Metal-Oxide Sensor Array | Serves as a test platform for studying generalized drift phenomena in electrochemical sensors. | Commercial electronic nose (e.g., Smelldect) with multiple SnO2 sensors [28]. |
| Machine Learning Framework | Enables the implementation of complex correction models (Random Forest, SVMs, Neural Networks). | Python with scikit-learn, TensorFlow/PyTorch [29] [30]. |
| TinyML Platform | Allows the deployment of optimized ML models onto low-power, embedded micro-controllers for edge processing. | STM32 micro-controllers [30]. |
Signaling Pathways and Workflow Diagrams
Kalman Filter Process Flow
Zero-Signal Correction Logic
CGM Signal Delay Composition
Frequently Asked Questions (FAQs) & Troubleshooting
This section addresses common technical and methodological questions researchers encounter when implementing SCINet architectures for Continuous Glucose Monitoring (CGM) sensor delay compensation.
General SCINet Architecture
Q1: What is the core innovation of the SCINet architecture in processing glucose time-series data? SCINet (Simplified Complex Interval Neural Network) introduces a unique recursive down-sampling structure. It effectively captures multi-scale dynamic features in time-series data by recursively splitting the input sequence into sub-sequences at odd and even time positions. This process allows the network to extract features at different temporal resolutions, making it particularly suited for capturing the complex, multi-scale dynamics of glucose fluctuations [31].
Q2: How does the double-layer stacked SCINet model improve prediction performance? Stacking multiple SCINet layers creates a deeper hierarchical feature extraction process. The first layer captures fundamental temporal patterns, while the subsequent layer learns more complex, higher-order features from the first layer's output. This stacked architecture has demonstrated superior predictive performance across various prediction horizons (e.g., 15, 30, 60 minutes) compared to single-layer models and other time-series forecasting algorithms [31].
Sensor Delay & Lag Compensation
Q3: What is the physiological basis for CGM sensor delay, and how can SCINet models compensate for it? CGM sensors measure glucose concentration in the interstitial fluid, not the blood. This results in a physiological delay of approximately 10-20 minutes compared to fingerstick blood glucose measurements due to the time required for glucose to equilibrate across the capillary membrane [31] [32]. SCINet models address this through two primary strategies [31]:
- Extended Look-back Window: Using a 30-minute historical data window ensures the model input encompasses the period of physiological delay.
- Sensor Parameter Integration: Incorporating "sensor response time" (
sensor_k) as an input feature allows the model to learn and adjust for the specific delay characteristics of the sensor hardware.
Q4: My model's hypoglycemia alerts are delayed. How can I improve alert accuracy using the SCINet framework? Experimental results with the SCINet architecture show that explicit lag compensation, as described above, can improve hypoglycemia alert accuracy by up to 12% (e.g., from 78% to 90%). Ensure your model training pipeline includes sensor-specific delay parameters and that the prediction horizon accounts for both the physiological and algorithmic processing delays [31].
Data & Experimental Setup
Q5: What are the critical input features for training a robust SCINet glucose prediction model? Beyond the core CGM time-series, feature optimization is crucial. Key features include [31] [32]:
- Historical CGM values over a sufficiently long window (e.g., 30-60 minutes).
- Sensor-specific parameters, such as sensor response time (
sensor_k). - Physiological context from health records (e.g., HbA1c, weight, age) in a multimodal setup, which helps inform patient-specific glucose variations [32].
Q6: My model performs well on one sensor type but poorly on another. How can I improve generalizability? This is a common challenge due to inter-sensor variability. Employ a multimodal approach that incorporates sensor-type as a categorical feature or meta-parameter. Furthermore, training on datasets from multiple sensor types, like the Menarini and Abbott sensors used in related research, can enhance model robustness and generalizability across different hardware [32].
Quantitative Performance Data
The following tables summarize key performance metrics from recent studies utilizing advanced neural networks for glucose prediction, providing benchmarks for your SCINet experiments.
Table 1: Multimodal Deep Learning Model Performance
Performance of a CNN-BiLSTM with attention on different CGM sensors (Prediction Horizon: PH) [32].
| CGM Sensor Type | PH: 15 min MAPE (mg/dL) | PH: 30 min MAPE (mg/dL) | PH: 60 min MAPE (mg/dL) |
|---|---|---|---|
| Menarini | 14 - 24 | 19 - 22 | 25 - 26 |
| Abbott | 6 - 11 | 9 - 14 | 12 - 18 |
Table 2: Comparative Model Performance on Ohio T1DM Dataset
Root Mean Square Error (RMSE) of various models for 30-minute and 60-minute prediction horizons [31].
| Model Architecture | 30-min RMSE (mg/dL) | 60-min RMSE (mg/dL) |
|---|---|---|
| Support Vector Regression (SVR) | ~20.38 (with feature engineering) | - |
| Recurrent Neural Network (RNN) | 20.7 ± 3.2 | 33.6 ± 3.2 |
| Artificial Neural Network (ANN) | 19.33 | 31.72 |
| SCINet (Proposed) | Outperforms above models | Outperforms above models |
Experimental Protocols & Workflows
Core Protocol: Implementing a SCINet for Glucose Prediction
This protocol outlines the key steps for building and evaluating a SCINet model, incorporating lag compensation.
1. Data Preprocessing & Lag Compensation Setup:
- Data Sourcing: Utilize CGM data from real-patient records. Example sources include hospital inpatient data or publicly available datasets like Ohio T1DM [31].
- Data Cleansing: Handle signal loss and sensor failure artifacts using interpolation or data rejection strategies [32].
- Lag Compensation: Integrate the sensor response time parameter (
sensor_k) as a model feature. Structure the input data with a look-back window that covers the physiological delay period (e.g., 30 minutes) [31].
2. Model Architecture Configuration:
- SCI-Block: Implement the basic building block of SCINet, which decomposes input features into two sub-features through splitting and interactive learning operations [31].
- Stacking: Construct a double-layer SCINet stack to enable multi-scale feature learning. The first layer processes the original sequence, while the second layer processes the transformed features from the first, capturing hierarchical temporal patterns [31].
- Output: Configure the final layers for regression to predict future glucose values (e.g., 15, 30, 60 minutes ahead).
3. Training & Validation:
- Training Dataset: Train the model using multiple continuous glucose monitoring datasets.
- Hyperparameter Tuning: Conduct multiple experiments to optimize hyperparameters (e.g., learning rate, number of filters, depth of recursion).
- Performance Validation: Validate predictive performance on a held-out test dataset. Use metrics like RMSE and MAPE, and compare against baseline time-series prediction algorithms [31].
The workflow for this protocol, including the crucial step of lag compensation, is visualized below.
The Lag Compensation Mechanism
The following diagram details the internal process of the Lag Compensation Module, a critical component for accurate prediction.
The Scientist's Toolkit: Research Reagent Solutions
This table details essential computational and data components for conducting research in this field.
| Item/Resource | Function & Application in Research |
|---|---|
| CGM Datasets (e.g., Ohio T1DM, Yixing People's Hospital data) | Provides the foundational time-series data for model training and validation. Essential for benchmarking algorithm performance [31]. |
| SCINet Architecture | The core neural network model for multi-scale temporal feature extraction. Replaces traditional RNNs/CNNs for potentially superior performance on glucose prediction tasks [31]. |
| Sensor Response Parameter (sensor_k) | A critical input feature that models the relationship between signal delay and specific sensor hardware parameters, directly enabling lag compensation [31]. |
| Multimodal Health Data (e.g., HbA1c, weight, age) | Provides physiological context. When fused with CGM data in a model, it helps account for inter-individual variability and improves personalization [32]. |
| High-Performance Computing (HPC) Cluster | Necessary for efficient training of deep learning models like stacked SCINet, which require significant computational resources for hyperparameter tuning and multiple experiments [31]. |
What are Hybrid Monitoring Systems in Glucose Research? Hybrid monitoring systems combine invasive (or minimally invasive) and non-invasive sensors to continuously measure blood glucose levels. The primary goal is to leverage the proven accuracy of invasive methods, such as Continuous Glucose Monitors (CGMs), to validate and enhance the performance of non-invasive sensors, which are often affected by physiological and technical challenges [2] [33]. A central research focus is sensor delay compensation, which addresses the time lag between glucose levels in the blood plasma and the readings from interstitial fluid or non-invasive sensors [2].
Why is Data Correlation Crucial? Correlating data from these different sensor types is essential for developing accurate and clinically reliable non-invasive monitoring devices. This process helps overcome issues like:
- Physiological Delays: The natural time lag (estimated at 6-10 minutes) for glucose to diffuse from blood vessels into the interstitial fluid where some sensors operate [2].
- Technical Delays: Latency introduced by the sensor's own technology and signal processing algorithms [2].
- Signal Interference: Non-invasive optical signals can be affected by skin color, ambient light, finger pressure, and other biological components, making calibration with a trusted reference vital [33].
Troubleshooting Common Integration Issues
FAQ 1: How do I resolve a consistent time lag between my invasive and non-invasive sensor readings?
- Problem: A persistent delay is observed between the glucose value from the reference CGM and the non-invasive sensor.
- Solution: This is often an expected physiological and technical delay. Implement and compare these two data alignment methods:
- MARD Minimization: Shift the non-invasive sensor's glucose values in time (e.g., by 5, 10, or 15 minutes) and calculate the Mean Absolute Relative Difference (MARD) at each shift point. The time shift that yields the minimum MARD is the optimal delay for your system [2].
- Minimum Deviation Match: For each reference plasma glucose measurement, find the non-invasive sensor value within a subsequent time window (e.g., 0-15 minutes) that has the smallest absolute difference. This method can account for variable delays, especially during rapid glucose changes like an Oral Glucose Tolerance Test (OGTT) [2].
FAQ 2: What should I check if the correlation between sensors is weak or inconsistent?
- Problem: The data from the invasive and non-invasive sensors show poor correlation, making reliable calibration impossible.
- Solution: Follow this troubleshooting checklist:
- Verify Sensor Placement and Operation: Ensure the non-invasive sensor (e.g., an optical unit) is correctly positioned and making consistent contact. Loose connections or movement artifacts can corrupt data [33].
- Check for Environmental Interference: Ambient light or significant temperature fluctuations can interfere with optical sensors. Conduct experiments in a controlled environment and use sensor designs that shield against such noise [33].
- Inspect Data Quality: Examine the raw signal from the non-invasive sensor for anomalies or dropouts. Algorithms may struggle with poor-quality input data.
- Validate Reference Method: Ensure the invasive reference sensor (CGM) is properly calibrated and functioning correctly. A faulty reference will lead to incorrect correlation.
FAQ 3: How can I improve the accuracy of my non-invasive glucose predictions?
- Problem: Even after correlation, the non-invasive sensor's glucose predictions have unacceptably high error.
- Solution: Move beyond simple linear regression models. Employ advanced machine learning techniques:
- Use Classification over Regression: Instead of predicting a continuous glucose value, train a model to classify readings into discrete glucose ranges (e.g., bins of 10 mg/dL). This can significantly improve the accuracy of identifying clinically critical hypoglycemic or hyperglycemic states [34].
- Leverage Multiple Wavelengths: If using an optical sensor, utilize multiple light wavelengths (e.g., 485, 645, 860, and 940 nm) instead of a single one. This multi-wavelength approach helps compensate for errors caused by inter-individual differences in tissue and blood components [34].
- Implement Robust Algorithms: Studies have shown that Support Vector Machines (SVM) and other classification models can achieve high accuracy (F1-scores of 99%) and place over 99% of readings in clinically acceptable zones of a Clarke Error Grid analysis [34].
Experimental Protocols for Data Correlation
The following workflow details a standardized method for correlating data from invasive and non-invasive sensors, crucial for delay compensation research.
Detailed Methodology:
Participant Preparation & Sensor Deployment:
- Recruit participants according to study protocol (e.g., healthy adults or diabetic patients) with informed consent [2].
- Place the reference sensor (e.g., a CGM like the SiJoy GS1 on the posterior upper arm) at least 48 hours before intensive testing to allow for stabilization [2].
- Deploy the non-invasive sensor (e.g., a custom NIR optical sensor with wavelengths such as 940 nm on the finger or wrist) [34] [33].
Provocative Testing & Data Collection:
- After an overnight fast, perform an Oral Glucose Tolerance Test (OGTT) by administering 75g of glucose solution [2].
- Collect venous Plasma Glucose (PG) samples at key time points: 0 (fasting), 30, 60, 120, and 180 minutes. This provides the gold-standard reference [2].
- Simultaneously, record glucose readings from both the CGM and the non-invasive sensor at high frequency (e.g., every 5 minutes). Also, record any potential confounding factors like skin temperature or patient activity [2] [33].
Data Pre-processing & Synchronization:
- Synchronize all datasets (PG, CGM, non-invasive) using precise timestamps.
- Clean the data by handling outliers and correcting for any baseline drift in sensor signals.
Time Lag Analysis and Data Alignment:
- Use one of the two methods described in the FAQs to determine the optimal time shift between the PG reference and the sensor signals.
- Align the datasets based on the calculated delay.
Model Training and Validation:
- Use the aligned data to train a machine learning model. The features could be raw optical intensities from multiple wavelengths, and the target is the reference PG value (for regression) or its class (for classification) [34] [33].
- Validate the model's performance on a separate, unseen dataset.
- Use robust metrics and tools like the Clarke Error Grid (CEG) to analyze clinical accuracy, Bland-Altman plots to assess agreement, and Mean Absolute Relative Difference (MARD) to quantify overall error [2] [33].
The table below summarizes key performance metrics from recent studies, providing benchmarks for your hybrid system's evaluation.
Table 1: Performance Metrics of Glucose Monitoring Systems from Recent Research
| System / Study Focus | Key Performance Metrics | Data Analysis Method | Reported Outcome |
|---|---|---|---|
| Non-invasive Optical Sensor [34] | Prediction Accuracy, F1-Score, Clarke Error Grid | Support Vector Machine (SVM) Classification | 99% F1-Score; 99.75% of readings in clinically acceptable zones (CEG) |
| SiJoy GS1 CGM Evaluation [2] | MARD, Clarke Error Grid | MARD Minimization & Minimum Deviation Match | Overall MARD of 8.01%; 89.22% in CEG Zone A, 100% in Zone A+B |
| niGLUC-2.0v Sensor Prototype [33] | Accuracy, Mean Absolute Error (MAE), Clarke Error Grid | Ridge Regression (RR) | Wrist prototype Accuracy: 99.96%, MAE: 0.06; 100% in CEG Zone A |
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Essential Materials for Hybrid Glucose Sensor Research
| Item | Specification / Example | Primary Function in Research |
|---|---|---|
| Reference CGM | SiJoy GS1, Dexcom G6 | Provides calibrated, continuous interstitial glucose readings to serve as a benchmark for correlation [2]. |
| Non-Invasive Sensor Prototype | Custom NIR sensor (e.g., 940 nm LED, 900-1700 nm detector) | Measures optical properties (absorption/scattering) correlated with glucose levels without breaking the skin [34] [33]. |
| Clinical Glucose Analyzer | AU5800 (Beckman Coulter) | Provides gold-standard Plasma Glucose (PG) measurements from venous blood draws for ultimate validation [2]. |
| Data Acquisition System | Custom PCB with microcontroll-er, Triad AS7265x Spectrometer | Captures raw analog signals from sensors and converts them to digital data for analysis [34]. |
| Standardized Glucose Challenge | 75g Oral Glucose Tolerance Test (OGTT) | Induces rapid and predictable changes in blood glucose, essential for studying dynamic response and time lags [2]. |
System Calibration and Validation Logic
Achieving a clinically acceptable system requires a rigorous, iterative process of calibration and validation, as outlined below.
FAQs: Understanding Compression in Monitoring Systems
Q1: What is a compression artifact and how does it affect data? A compression artifact is a noticeable distortion of media (including images, audio, and video) caused by the application of lossy data compression [35]. This occurs when data is discarded to reduce file size for storage or transmission, potentially introducing errors. In the context of Continuous Glucose Monitoring (CGM), failures such as compression artifacts can impact both real-time and retrospective data analysis [36]. These artifacts can obscure true physiological signals, such as glucose fluctuations, leading to inaccurate clinical interpretations.
Q2: Why is real-time artifact detection and compensation crucial for CGM systems? CGM systems measure glucose in the interstitial fluid, not in blood. Rapid changes in blood glucose are not accompanied by similar immediate changes in the interstitial fluid but follow with a physiological time delay [37]. This delay, with a mean of approximately 9.5 minutes [37], hampers the detection of fast glucose changes, such as the onset of hypoglycemia. When compression artifacts affect the data stream, they compound this inherent delay, further degrading data quality and reliability for real-time therapy decisions like insulin dosing.
Q3: What are the common types of artifacts in data streams? Artifacts manifest differently depending on the data type:
- In Video/Imaging: Common artifacts include "blockiness" (also called blocking or quilting), "ringing" around edges, and "mosquito noise" (a shimmering blur of dots around edges) [35]. These are prevalent in formats like MPEG and JPEG.
- In Sensor Data (e.g., CGM): Artifacts can appear as physiologically implausible signal drop-outs, rapid fluctuations, or "spikes" [36]. These are distinct from the sensor's inherent time delay and represent data integrity failures.
Q4: How can researchers detect compression artifacts in CGM data? A data-driven, supervised approach can be effective. One method involves generating an in-silico dataset (e.g., using the T1D UVa/Padova simulator) and adding compression artifacts at known positions to create a labeled dataset. The detection problem can then be addressed using supervised algorithms like Random Forest, which has shown satisfactory performance in detecting these faults on simulated data [36].
Q5: What methods can compensate for time delays and artifacts in CGM? The primary method for compensating CGM time delays is the use of prediction algorithms. These algorithms use past CGM readings and signal trends to forecast future glucose values, effectively reducing the apparent lag. Research shows such algorithms can reduce the mean time delay by 4 minutes on average [37]. Furthermore, frameworks like SCOPE used in other fields demonstrate that joint compression and artifact correction in a single system can preserve critical signal details while maintaining low-bitrate transmission [38].
Experimental Protocols for Artifact Analysis
Protocol: Data-Driven Supervised Detection of Compression Artifacts
This protocol is based on the methodology employed for CGM data [36].
Objective: To develop and validate a model for the retrospective detection of compression artifacts in continuous sensor data.
Materials:
- A validated simulator for the physiological data of interest (e.g., T1D UVa/Padova simulator for glucose data).
- Computational environment for data analysis (e.g., Python with scikit-learn, R).
Methodology:
- Dataset Generation:
- Use the simulator to generate a large, clean dataset of the physiological signal (e.g., glucose levels) under various conditions.
- Systematically inject compression artifacts into the clean dataset at known positions and with varying severities. This creates a "ground truth" dataset where the presence and location of artifacts are perfectly labeled (faulty/not-faulty).
Feature Engineering:
- Extract relevant features from the raw signal data that may characterize artifacts. These could include:
- Statistical features: rolling mean, standard deviation, skewness.
- Signal-based features: rate of change, acceleration, short-term volatility.
- Model-based features: residual errors from a simple smoothing filter.
- Extract relevant features from the raw signal data that may characterize artifacts. These could include:
Model Training:
- Divide the labeled dataset into training and testing sets.
- Train a supervised machine learning classifier, such as a Random Forest algorithm, using the extracted features to predict the presence of an artifact.
- Optimize hyperparameters via cross-validation.
Performance Validation:
- Evaluate the trained model on the held-out test set.
- Quantify performance using metrics such as Accuracy, Sensitivity (Recall), Specificity, and Precision.
Protocol: Evaluating Prediction-Based Delay Compensation
This protocol outlines a method to assess the efficacy of prediction algorithms in reducing the effective time delay of CGM sensors [37].
Objective: To quantify the reduction in effective time delay achieved by a real-time prediction algorithm applied to CGM raw signals.
Materials:
- A clinical dataset comprising paired CGM raw signals and reference blood glucose (BG) measurements from a cohort of patients (e.g., 37 patients with 108 data sets).
- A proposed real-time prediction algorithm.
Methodology:
- Data Collection:
- Collect synchronized CGM raw signals and frequent reference BG measurements (e.g., via fingerstick) in a clinical setting.
Baseline Delay Calculation:
- Calculate the native time delay of the CGM raw signal with respect to BG. This can be done using statistical methods (e.g., cross-correlation) to find the time shift that maximizes alignment between the CGM trend and BG values. One study reported an overall mean (SD) time delay of 9.5 (3.7) minutes [37].
Algorithm Application:
- Process the CGM raw signals through the prediction algorithm to generate "predictive" glucose readings.
Delay Comparison:
- Calculate the time delay of the algorithm-processed predictive readings against the same reference BG measurements.
- Compare the delay before and after algorithm application. A successful algorithm will show a statistically significant reduction. For example, one study demonstrated a reduction of 4 minutes on average [37].
Patient-Specific Analysis:
- Analyze the results on a per-patient basis, as evidence suggests time delays may be patient-dependent [37].
Table 1: Characteristics of CGM Sensor Time Delay
| Metric | Value | Context / Method |
|---|---|---|
| Mean Time Delay (Raw Signal) | 9.5 ± 3.7 minutes | Measured against reference blood glucose [37] |
| Median Time Delay | 9 minutes | [37] |
| Interquartile Range | 4 minutes | [37] |
| Delay Reduction with Prediction | ~4 minutes | Achieved through application of a prediction algorithm [37] |
| Key Factor | Patient specificity | Suggests delay may vary individually [37] |
Table 2: Comparison of Artifact Handling Methodologies
| Method | Principle | Application Context | Key Advantage |
|---|---|---|---|
| Supervised Detection (Random Forest) | Uses labeled data to learn features of artifacts [36] | Retrospective analysis of CGM data [36] | High accuracy with accurate labels; explainable model |
| Prediction Algorithms | Forecasts future values to compensate for lag [37] | Real-time CGM delay compensation [37] | Directly addresses physiological time delay |
| Self-Supervised Joint Framework (SCOPE) | Learns frequency-encoded representations to compress and correct simultaneously [38] | Real-time sonar video streaming [38] | Does not require clean-noisy data pairs; improves data fidelity for downstream tasks |
Workflow Visualization
CGM Delay Compensation Workflow
Artifact Detection Model Training
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for CGM Delay and Artifact Research
| Item / Solution | Function in Research |
|---|---|
| T1D UVa/Padova Simulator | A widely accepted simulation platform for generating in-silico type 1 diabetes data. Used to create controlled, labeled datasets for developing and testing artifact detection algorithms [36]. |
| Continuous Glucose Monitoring (CGM) System | The core sensor technology under investigation. Provides the raw signal data containing both physiological information and artifacts for analysis [19] [37]. |
| Reference Blood Glucose (BG) Measurements | Gold-standard measurements (e.g., via Yellow Springs Instrument or fingerstick meters) used as a benchmark to calculate sensor time delays and validate compensation algorithms [37]. |
| Random Forest Algorithm | A versatile supervised machine learning classifier. Effective for classification tasks like distinguishing faulty from non-faulty sensor readings based on extracted signal features [36]. |
| Prediction Algorithm (e.g., for time series) | A core computational tool for delay compensation. Uses past CGM values and trends to forecast future glucose levels, effectively reducing the impact of the physiological time lag [37]. |
| Statistical Analysis Software (e.g., R, Python with Pandas/NumPy) | The computational environment for data processing, feature extraction, model training, and statistical validation of results [36] [37]. |
Core Concepts and FAQs
What is the fundamental principle behind dual-sensor calibration for glucose monitoring?
Dual-sensor calibration improves glucose monitoring accuracy by accounting for subject-specific differences in how glucose diffuses from the blood into the interstitial fluid. This method uses two glucose sensors implanted at different depths beneath the skin to estimate personalized time constants for glucose diffusion. By understanding an individual's unique interstitial glucose dynamics, the system can more accurately calculate true blood glucose levels from sensor measurements, compensating for the physiological time lag that often plagues continuous glucose monitoring systems. [27]
What specific problem does depth-dependent time constant estimation solve?
This approach directly addresses the physiological time lag between blood glucose changes and their detection in interstitial fluid, which is a major source of inaccuracy in continuous glucose monitoring. The time lag varies significantly between individuals due to factors like skin thickness, blood flow, and metabolism. By estimating personalized time constants using dual sensors at different depths, researchers can develop subject-specific diffusion models that substantially improve the accuracy and reliability of glucose trend predictions, especially during rapid glucose changes after meals or exercise. [27] [8]
What are the most common experimental challenges in dual-sensor setups?
Sensor Placement Precision: Consistent depth placement between sensors is critical yet challenging. Even minor variations can significantly impact time constant estimations.
Signal Synchronization: Precisely aligning temporal data from multiple sensors requires sophisticated timestamping and sampling rate management.
Cross-Talk Interference: Closely placed sensors may interfere with each other's measurements, requiring electromagnetic shielding or algorithmic compensation.
Tissue Response Variability: The body's natural foreign body response can create variable tissue encapsulation around sensors, altering diffusion characteristics over time.
Environmental Factor Control: Temperature fluctuations, compression artifacts, and local blood flow changes can all confound results if not properly controlled. [27] [15]
How can researchers validate the accuracy of personalized diffusion models?
Model validation should employ multiple complementary approaches: comparison against gold-standard blood glucose measurements during oral glucose tolerance tests; statistical analysis using Mean Absolute Relative Difference (MARD) calculations; consensus error grid analysis for clinical significance assessment; and cross-validation with hyperinsulinemic-euglycemic clamp data when available. The model should demonstrate consistent performance across both steady-state and dynamic glucose conditions. [8] [11]
Experimental Protocols & Methodologies
Protocol: Dual-Sensor Implantation and Data Collection for Time Constant Estimation
Objective: To determine subject-specific glucose diffusion time constants using sensors at multiple tissue depths.
Materials Required:
- Two identical glucose sensors with known depth characteristics
- Precision insertion device with depth control
- Data acquisition system with synchronized sampling
- Calibration solutions for sensor verification
- Temperature monitoring equipment
- Secure fixation materials to prevent sensor migration
Procedure:
- Pre-calibration: Verify sensor performance in standardized glucose solutions prior to implantation.
- Site Preparation: Identify and prepare insertion sites with appropriate antiseptic protocol.
- Sensor Placement: Using a precision insertion device, implant sensors at two distinct subcutaneous depths (typically 2-3mm depth difference).
- Stabilization Period: Allow 2-6 hours for tissue recovery and sensor stabilization before data collection.
- Data Collection: Record simultaneous measurements from both sensors at 1-5 minute intervals during:
- Fasting baseline period (30-60 minutes)
- Controlled glucose challenge (OGTT or meal tolerance test)
- Recovery period (2-3 hours post-challenge)
- Reference Sampling: Collect periodic capillary or venous blood samples as reference measurements.
- Environmental Monitoring: Continuously record local tissue temperature and note any compression events.
Data Analysis:
- Calculate cross-correlation between sensor signals to determine initial time lag estimates
- Apply mathematical modeling (e.g., compartmental diffusion models) to derive time constants
- Validate models against reference blood glucose measurements
- Calculate confidence intervals for parameter estimates [27] [11]
Protocol: Oral Glucose Tolerance Test (OGTT) for Sensor Performance Validation
Objective: To evaluate sensor accuracy and characterize time lags during dynamic glucose changes.
Materials Required:
- Standardized 75g glucose solution
- Venous blood collection equipment
- Centrifuge for plasma separation
- Laboratory glucose analyzer
- Continuous glucose monitoring system
- Timer and standardized protocols
Procedure:
- Participant Preparation: 10-hour overnight fast with ad libitum water intake.
- Baseline Sampling: Collect fasting blood sample (t=0 minutes) and record sensor values.
- Glucose Administration: Ingest 75g glucose solution within 5-minute window.
- Serial Sampling: Collect blood samples at t=15, 30, 45, 60, 90, and 120 minutes post-ingestion.
- Continuous Monitoring: Record sensor values every 5 minutes throughout the protocol.
- Sample Processing: Immediately centrifuge blood samples and analyze plasma glucose.
- Data Recording: Document exact sampling times and any protocol deviations.
Analysis Approach:
- Use MARD minimization to determine optimal time shift between plasma and sensor glucose
- Apply inter-individual difference minimization to align post-challenge measurements
- Generate consensus error grid analysis for clinical accuracy assessment
- Calculate time-to-peak differences between plasma and interstitial glucose [8] [11]
Performance Data & Technical Specifications
Quantitative Sensor Performance Metrics
Table 1: Clinical Accuracy Metrics for Glucose Monitoring Systems
| Performance Parameter | SiJoy GS1 CGM Performance | Traditional CGM Targets | Assessment Method |
|---|---|---|---|
| Overall MARD | 8.01% (±4.9%) in fasting phase | 7.5%-15.3% | ISO 15197:2013 |
| Consensus Error Grid (Zone A) | 89.22% of values | >70% clinically acceptable | Clinical significance analysis |
| Consensus Error Grid (Zone A+B) | 100% of values | >99% required | Clinical significance analysis |
| 20/20% Consistency | 96.6% | Variable by manufacturer | ISO 15197:2013 criteria |
| Time Lag Estimation | 10-15 minutes post-OGTT | 5-15 minutes typical | MARD minimization analysis |
Table 2: Troubleshooting Guide for Common Experimental Issues
| Problem | Potential Causes | Diagnostic Steps | Resolution Strategies |
|---|---|---|---|
| Diverging Sensor Readings | Different tissue environments, Sensor drift, Compression artifacts | Compare with reference measurements, Check insertion depth documentation, Review signal stability | Recalibrate using reference values, Reposition if compressed, Use depth-compensation algorithms |
| Poor MARD Values | Incorrect time constant estimation, Signal processing delays, Sensor calibration issues | Analyze during different glucose phases (fasting, postprandial), Check calibration protocol adherence | Optimize time shift parameters (5,10,15min tested in studies), Implement dynamic calibration approaches |
| Signal Artifacts | Sensor compression, Local inflammation, Electrical interference | Review for pressure patterns (compression lows), Check tissue temperature changes, Examine signal noise characteristics | Implement compression artifact detection algorithms, Allow tissue recovery time, Apply signal filtering techniques |
| Model Instability | Insufficient data during transitions, Parameter identifiability issues, Subject movement | Assess parameter confidence intervals, Check data collection during rapid glucose changes, Review sensor fixation | Extend data collection during dynamic periods, Incorporate Bayesian priors for parameters, Improve sensor securement |
Research Reagent Solutions & Essential Materials
Table 3: Essential Research Materials for Dual-Sensor Glucose Studies
| Material/Reagent | Specification Purpose | Experimental Function | Technical Notes |
|---|---|---|---|
| Dual-depth Sensor Platform | Depth differentiation of 2-3mm between sensors | Enables simultaneous measurement from different tissue compartments | Depth must be verified through insertion device calibration; Materials should be biocompatible |
| Continuous Glucose Monitoring System | 5-minute sampling capability minimum | Provides high-temporal resolution interstitial glucose data | Systems from Dexcom, Medtronic, Abbott, or research-grade systems commonly used |
| Oral Glucose Tolerance Test Materials | 75g standardized glucose solution | Creates controlled glycemic challenge for dynamic response characterization | Preparation and administration must follow standardized protocols for valid comparisons |
| Reference Glucose Analyzer | Laboratory-grade plasma glucose measurement | Provides gold-standard reference for sensor accuracy validation | Yellow-top sodium fluoride tubes prevent glycolysis in samples |
| Kalman Filter Algorithms | Real-time blood glucose estimation from interstitial measurements | Compensates for physiological time lags between compartments | Particularly valuable during rapid glucose transitions; improves prediction accuracy |
| Temperature Monitoring System | Local tissue temperature measurement | Controls for temperature-induced measurement variations | Essential as glucose oxidase-based sensors are temperature sensitive |
Experimental Workflows & Signaling Pathways
For researchers in continuous glucose monitoring (CGM) and drug development, maintaining uninterrupted data streams during sensor transitions is critical for data integrity and patient safety. Sensor delays and transmission interruptions can compromise research outcomes and clinical decision-making. This technical support center provides targeted troubleshooting guides and FAQs to address data-stream bridging challenges specific to medical monitoring research, enabling robust delay compensation and seamless sensor transitions in experimental and clinical settings.
Troubleshooting Guides
Data Stream Configuration and Connectivity Issues
Problem: Active stream with no data received at destination This commonly occurs when the data stream behavior is not properly enabled in your property configuration or when destination details are invalid [39].
- Solution:
- Verify that the DataStream behavior is enabled for your property and included in the same Property Manager configuration version selected during stream creation/editing [39].
- Validate destination configuration details, including hostname, VPN, and authentication credentials [40] [39].
- Check for HTTP 429 or 5XX errors at the destination, which may cause data loss after multiple retry attempts [39].
Problem: Stream enters "Failed" or "Failed Permanently" state This typically indicates connection issues with the source database or destination configuration problems [41].
- Solution:
- For "Failed" states: Address connection errors with the source database credentials or destination configuration [41].
- For "Failed Permanently" states: This may require recovering the stream from the most recent position, which might involve truncating affected tables in the destination and triggering data backfills to restore historical data [41].
Sensor-Specific Data Transmission Issues
Problem: Sensor detection failures during transitions When targets are not detected during sensor handoffs, multiple factors require investigation [42].
- Solution:
- Verify sensor properties: Confirm operating distance specifications, switching element function (NPN/PNP, NC/NO), and supply voltage (typically 10V-30V for industrial sensors) [42].
- Validate target characteristics: Ensure target materials are detectable (metallic for inductive sensors), confirm target size meets specifications, and verify sensor-target alignment and movement speed doesn't exceed switching frequency limits [42].
- Check for electromagnetic interference from other sensors or equipment that may disrupt detection fields [42].
Problem: Premature switching during sensor handoffs Early switching can compromise transition timing and data continuity [42].
- Solution:
- Verify installation conditions: Ensure proper flush or non-flush mounting according to technical specifications [42].
- Inspect for environmental interference: Check for metal objects in the vicinity and clean sensors of contamination using appropriate cleaning agents [42].
- Validate switching element function configuration matches application requirements [42].
Data Quality and Integrity Issues
Problem: Incomplete dataset fields in streamed data Selected data set fields may not appear in logs or return null values [39].
- Solution:
Problem: Discrepancy between expected and actual data volume Stream is active but contains less data than traffic edge hits suggest [39].
- Solution:
- Verify that criteria triggering DataStream behavior in property configuration (Rules and Matches) don't exclude portions of traffic [39].
- Check sampling rate settings; values below 100% will omit some log data [39].
- Confirm log data time frame alignment with traffic edge hits metric, using "Traffic by hostname" report for more reliable comparison [39].
Frequently Asked Questions (FAQs)
Sensor Selection and Configuration
Q: What factors determine optimal sensor selection for monitoring applications? A: Selection depends on two primary factors: (1) available mounting space and (2) required sensing distance [43]. Additionally, consider environmental conditions, as LiDAR sensors may be affected by heavy rain or snow, while radar operates reliably in adverse weather [44].
Q: When should I choose capacitive versus inductive sensors? A: Inductive sensors only detect metallic objects, while capacitive sensors detect materials including wood, paper, liquids, and cardboard [43]. For CGM applications involving non-metallic materials or liquid detection, capacitive sensors may be preferable.
Q: What is the significance of switching frequency in sensor applications? A: Switching frequency determines how quickly a sensor can detect an object, reset, and detect another object [43]. For example, a 100 Hz sensor can detect up to 100 objects per second, which is critical for applications requiring rapid measurements such as gear rotation or high-frequency physiological monitoring [43].
Data Stream Management
Q: How do I enable Data Stream functionality? A: Navigate to Administration > Settings in your management interface, select the Data Stream line, and click Edit. Change from "Disabled" to "Enabled," then enter the appropriate Hostname (IP address or hostname for device access) and associated VPN [40].
Q: Why can't I select certain data set fields for logging? A: Some data sets and fields require specific product configurations. Consult the data set parameters list to verify support for your product [39]. Some fields may also require enabling additional behaviors in Property Manager [39].
Q: What are the limitations of speed testing for data streams? A: Speed tests are generally limited to approximately 215-250 Mbps due to CPU processing constraints, as testing is single-threaded and pinned to the control core [40]. These tests also don't account for tunnel overhead such as IPsec headers [40].
Performance Optimization
Q: How can I optimize data transmission in challenging environments? A: Implement a multi-sensor configuration with complementary technologies. LiDAR provides high-resolution 3D spatial data but can be affected by precipitation; radar performs reliably in adverse weather but generates sparser data; cameras offer rich semantic context but struggle in low-light conditions [44]. This heterogeneous approach ensures redundancy and operational resilience [44].
Q: What methods can compensate for data transmission delays? A: Advanced approaches include signal denoising methods using Lagrange multiplier symplectic singular value mode decomposition, weak communication signal compensation through feature enhancement, neural network algorithms based on long short-term memory for delay prediction, and PID controllers to calculate and implement transmission delay compensation [45].
Q: What is the minimum distance required between parallel sensors? A: When placing sensors parallel to each other, maintain a minimum distance equal to the sensor diameter (e.g., 12mm, 18mm, or 30mm) [43].
Experimental Protocols and Methodologies
Real-World Sensor Deployment and Validation Protocol
Based on successful deployment of multi-sensor systems in operational environments [44], this protocol validates sensor performance during transitions:
Equipment Requirements:
- Heterogeneous sensor suite (LiDAR, radar, camera systems)
- Edge computing platform with sufficient processing capability (e.g., NVIDIA Jetson AGX Orin)
- High-accuracy reference system (e.g., GNSS receiver with IMU)
- Mounting infrastructure stable against environmental vibrations
Methodology:
- Site Assessment: Identify monitoring area with representative operational characteristics, including transition zones and potential obstructions [44].
- Sensor Placement: Deploy sensors to ensure overlapping coverage in transition areas, considering height and angle for optimal line of sight [44].
- Coordinate System Alignment: Implement spatial calibration across all sensors to establish unified reference frame [44].
- Ground Truth Validation: Equate reference vehicle with high-accuracy GNSS/IMU system (e.g., NovAtel CPT7700 with TerraStar-L correction) to capture ground truth positioning [44].
- Data Synchronization: Implement temporal alignment across all sensor data streams and reference system [44].
- Performance Metrics: Calculate detection accuracy, tracking consistency, and transition smoothness by comparing sensor data against ground truth [44].
Data Transmission Delay Compensation Protocol
Based on innovative approaches for delay compensation in interactive communication networks [45], this protocol addresses sensor transition delays:
Equipment Requirements:
- Signal processing platform with implementation of symplectic singular value decomposition
- Neural network implementation for delay prediction (LSTM-based)
- PID controller for compensation calculation
- Delay compensator hardware/software
Methodology:
- Signal Denoising: Implement communication network signal denoising using Lagrange multiplier symplectic singular value mode decomposition through five stages: phase-space reconstruction, symplectic geometric similarity transformation, grouping, diagonal averaging, and adaptive reconstruction [45].
- Signal Enhancement: Capture and compensate weak communication signals by enhancing signal characteristics [45].
- Delay Prediction: Collect communication network signals to obtain delay information, then apply long short-term memory (LSTM) neural network algorithms to predict data transmission delays [45].
- Compensation Calculation: Using predicted delay values, employ PID controller to calculate precise transmission delay compensation amounts [45].
- Compensation Implementation: Input calculated compensation values into delay compensator to achieve effective transmission delay compensation [45].
Data Presentation Tables
Sensor Performance Characteristics Under Various Conditions
Table: Comparative analysis of sensor technologies for monitoring applications
| Sensor Type | Optimal Range | Weather Limitations | Data Output | Transition Readiness |
|---|---|---|---|---|
| LiDAR [44] | Long-range, high-resolution 3D spatial data | Performance hampered by rain/snow (particles disperse laser beam) | Dense 3D point cloud with depth information | Excellent in clear conditions, degraded in precipitation |
| Radar [44] | Reliable under adverse weather conditions | Minimal weather impact; operates reliably in rain, fog, snow | Sparse point cloud with precise Doppler-based velocity | High reliability across weather conditions |
| Camera [44] | Short to medium range with rich semantic context | Accuracy drops under adverse weather and low visibility | 2D visual imagery with classification capabilities | Limited by lighting and visibility conditions |
| Inductive [43] | Metallic object detection only | Insensitive to environmental contaminants like humidity, oil, dust | Digital switching signal | Limited to metallic targets only |
| Capacitive [43] | Broad material detection (wood, paper, liquids, etc.) | Performance may vary with material dielectric properties | Digital switching signal | Broad material detection capability |
Data Stream Troubleshooting Reference
Table: Common data stream issues and resolution approaches
| Problem Symptom | Potential Causes | Immediate Actions | Long-term Solutions |
|---|---|---|---|
| No data at destination despite active stream [39] | - DataStream behavior not enabled- Invalid destination details- HTTP errors at destination | - Verify Property Manager configuration- Validate destination parameters | - Implement alerting for upload failures- Establish destination monitoring |
| Stream in "Failed" state [41] | - Source database connection issues- Credential problems- Destination configuration errors | - Check connection profiles- Verify source database accessibility | - Implement connection health monitoring- Establish automated recovery protocols |
| Incomplete dataset fields [39] | - Additional behaviors not enabled in Property Manager- Geographic restrictions for certain fields | - Consult data set parameters list- Enable required behaviors | - Document field requirements for all datasets- Establish configuration checklist |
| Lower than expected data volume [39] | - Exclusionary rules in configuration- Sampling rate below 100%- Time frame misalignment | - Review configuration rules and matches- Verify sampling settings | - Standardize configuration templates- Implement volume anomaly detection |
Visualization Diagrams
Data-Stream Bridging Architecture for Sensor Transitions
Diagram Title: Data-Stream Bridging System Architecture
Sensor Transition Troubleshooting Workflow
Diagram Title: Sensor Data Stream Troubleshooting Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential components for data-stream bridging experiments
| Component | Specification | Research Function | Implementation Example |
|---|---|---|---|
| Edge Computing Platform [44] | NVIDIA Jetson AGX Orin (32GB RAM, 275 TOPS) | Real-time processing of sensor data streams during transitions | Processes dense LiDAR point clouds and implements delay compensation algorithms |
| Reference Localization System [44] | GNSS/IMU system (NovAtel CPT7700 with HG4930 IMU) | Provides ground truth validation for sensor transition accuracy | Captures vehicle positioning at 10Hz frequency with TerraStar-L correction services |
| Heterogeneous Sensor Suite [44] | LiDAR, radar, and camera systems | Ensures redundant monitoring across diverse environmental conditions | Provides complementary data streams resilient to individual sensor limitations |
| Signal Processing Module [45] | Lagrange multiplier symplectic singular value decomposition | Denoises communication network signals for cleaner data transmission | Implements five-stage decomposition: phase-space reconstruction to adaptive reconstruction |
| Delay Prediction Engine [45] | LSTM-based neural network algorithm | Predicts data transmission delays for proactive compensation | Analyzes historical delay information to forecast future transmission bottlenecks |
| Compensation Controller [45] | PID controller with delay compensator | Calculates and implements precise transmission delay compensation | Receives prediction results and computes compensation amounts for seamless transitions |
Optimizing Compensation Algorithms: Addressing Performance Gaps and Enhancing Robustness
Frequently Asked Questions (FAQs)
Q1: What are the primary causes of time delay in Continuous Glucose Monitoring (CGM) systems? Time delays in CGM systems are a combination of physiological and technological factors. The physiological time delay, due to glucose diffusion from blood to interstitial fluid (ISF), is assumed to be 5-10 minutes on average [25]. The technologically caused delay includes the sensor's physical response time and algorithmic delays from noise-filtering processes, which can add 3-12 minutes [25]. The total time delay is a critical parameter that compensation algorithms must address.
Q2: How can context-aware compensation improve CGM performance? Context-aware systems identify specific user states (like exercise, sleep, or postprandial periods) and adjust the compensation strategy accordingly [46]. For example, by recognizing a "sleep" context, an algorithm could employ more aggressive filtering for stability, whereas during "exercise," it might prioritize faster response times to track rapid glucose declines. This adaptive tuning can improve tracking performance and accuracy in dynamic real-world conditions [46].
Q3: What is the role of machine learning in adaptive CGM algorithms? Machine learning, particularly pattern recognition and reinforcement learning, can be used to classify the user's context and optimally tune algorithm parameters in real-time [46] [47]. Support Vector Machines (SVM) can identify multipath environments or motion states with high accuracy (86-92%), while Reinforcement Learning (RL) agents can learn to apply the most effective interface or signal processing adaptations based on real-time physiological data [46] [47].
Q4: What are common filtering methods for CGM signal noise? Digital filtering is essential for smoothing the noisy raw signal from CGM sensors. Common approaches include:
- Median Filters: Effective for removing sudden signal "spikes" by taking the median value of a window of past readings [48].
- Moving Average (MA) Filters: A simple Finite Impulse Response (FIR) filter that averages past values. However, there is a trade-off where longer averaging reduces noise but increases time lag [25] [48].
- Kalman Filtering: An advanced optimal estimation method that can be used for real-time estimation, prediction, and lag compensation, providing a robust framework for handling signal uncertainty [48].
Troubleshooting Guide
| Problem & Symptoms | Potential Root Cause | Diagnostic Steps | Recommended Solution & Compensation Adjustment | ||
|---|---|---|---|---|---|
| Consistent Lag During Rapid Glucose Changes: CGM readings persistently trail fingerstick measurements during fast swings, leading to missed hypoglycemic events. | High physiological lag exacerbated by inappropriate filter settings for the context (e.g., using a "sleep" algorithm during exercise). | 1. Analyze paired CGM-blood glucose (BG) data during rising/falling glucose phases.2. Calculate the apparent time delay.3. Check current algorithm configuration and context settings. | Implement a context-aware prediction algorithm to forecast glucose levels. Studies show this can reduce the effective delay by ~4 minutes on average [25]. For the "exercise" context, reduce the filter window length. | ||
| Poor Sensor Accuracy Post-Calibration: Large errors (>20% MARD) between CGM and reference BG after calibration, especially when glucose is unstable. | Calibration performed during periods of high glucose rate-of-change or significant BG-ISF gradient. Errors in reference glucose meter readings also contribute. | 1. Review calibration logs for the rate of glucose change ( | dG/dt | ).2. Verify the time interval and difference between calibration points. | Enforce a calibration request when the sensor signal is stable (e.g., change <1% over 4 minutes) [48]. Ensure two calibration points differ by >30 mg/dl [49]. |
| Noisy CGM Signal: Erratic CGM trace with high short-term variability, making trend interpretation difficult. | Signal artifacts, sensor dropout, or insufficient filtering. Could also be caused by local physiological factors (e.g., poor tissue perfusion). | 1. Inspect raw sensor current (if available) for noise.2. Rule out local issues at sensor insertion site.3. Check the current filter type and parameters. | Apply a median filter (e.g., of 5 samples) to remove spikes, followed by a Kalman filter for optimal noise smoothing without excessive lag [48]. | ||
| Algorithm Failure in Specific Contexts: Performance degradation in one state (e.g., post-meal) but not others (e.g., overnight). | The compensation algorithm is not adaptive; it uses a single, fixed set of parameters for all physiological conditions. | 1. Segment performance data (e.g., MARD, delay) by context (postprandial, sleep, exercise).2. Compare algorithm parameters across these segments. | Develop and train a context-classifier (e.g., using SVM [46]). Implement a rule-based or RL-driven [47] system to switch between context-specific algorithm parameter sets. |
Quantitative Data on CGM Performance and Delays
Table 1: Analysis of CGM Time Delay Components [25].
| Delay Component | Reported Range | Key Influencing Factors |
|---|---|---|
| Physiological Lag | 5 - 10 minutes | Local blood flow, tissue perfusion, interstitial fluid permeability. |
| Technological Lag | 3 - 12 minutes | Sensor membrane diffusion, enzyme reaction speed, signal filtering. |
| Total System Lag | 5 - 40 minutes | Combination of all above, plus algorithmic smoothing. |
| Prediction Algorithm Benefit | ~4 minute reduction | Can reduce the effective lag experienced by the user. |
Table 2: Performance of Context-Aware Pattern Recognition [46].
| Classification Method | Reported Accuracy | Application in CGM Research |
|---|---|---|
| Support Vector Machine (SVM) with modified Gaussian kernel | 86% - 92% | Classifying multipath environments; can be analogized to classifying different physiological contexts (e.g., exercise vs. rest). |
| Context-based parameter tuning | ~15% tracking improvement | Improving delay lock loop (DLL) performance; demonstrates the potential gain from adaptive signal processing. |
Experimental Protocol for Context-Aware Algorithm Validation
Objective: To validate the efficacy of a context-aware compensation algorithm against a standard fixed-parameter algorithm across exercise, sleep, and postprandial states.
Methodology:
- Participant Recruitment: Recruit a cohort (e.g., n=40) of individuals with diabetes, ensuring a representative mix.
- Data Collection: Conduct supervised study sessions for each context:
- Postprandial: Measure glucose after a standardized meal.
- Exercise: Monitor glucose during and after moderate-intensity aerobic activity.
- Sleep: Overnight glucose monitoring in a clinical setting.
- Signal Acquisition: Collect high-frequency venous or capillary blood glucose reference measurements synchronized with raw CGM sensor current data. Simultaneously, collect physiological signals (e.g., EEG, heart rate) for context verification [47].
- Algorithm Testing: Process the raw CGM data stream offline using both the standard and context-aware algorithms.
- Performance Metrics: Calculate the following for each context:
- Mean Absolute Relative Difference (MARD): The primary metric for point accuracy.
- Time Delay: Estimated by cross-correlation or model-based methods.
- Grid Error Analysis: Clarke Error Grid (CEG) to assess clinical significance of deviations.
Data Analysis:
- Use paired statistical tests (e.g., paired t-test) to compare the MARD and time delay of the two algorithms within each context.
- Segment performance data by glucose rate-of-change (e.g., <|1| mg/dl/min, |1-2| mg/dl/min, >|2| mg/dl/min) to analyze performance during dynamic and stable periods.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for CGM Algorithm Research.
| Item | Function in Research |
|---|---|
| High-Frequency Blood Sampler | Provides the "gold standard" reference blood glucose measurements necessary for algorithm calibration and validation. |
| Raw CGM Signal Data | The unprocessed current signal (nA) from the sensor, required for developing and testing new calibration and filtering algorithms [48]. |
| Physiological Signal Monitors (EEG, EOG, EMG) | Used to derive objective markers of user context (e.g., sleep stages via EEG) or cognitive workload, feeding into context-aware systems [47]. |
| Signal Processing Software (e.g., Python/MATLAB with FFT tools) | Used for implementing and testing digital filters (median, FIR, Kalman) and for performing power spectral density analysis on physiological signals [47] [48]. |
| Continuous Glucose Monitoring Simulator | A software tool that generates realistic CGM and BG data streams, invaluable for the initial testing and validation of new algorithms in a controlled, in-silico environment. |
Visualizing the Context-Aware Compensation Workflow
The following diagram illustrates the core workflow of a context-aware adaptive system for CGM signal compensation, from signal acquisition to the final display.
CGM Context-Aware Compensation Workflow
Welcome to the Technical Support Center
This resource is designed for researchers and scientists working at the intersection of machine learning and continuous glucose monitoring (CGM). The guides below address specific technical challenges in developing models for CGM signal prediction and sensor delay compensation.
Core Concepts FAQ
1. What is the primary source of time delay in CGM signals, and how can machine learning help compensate for it?
CGM time delay has two main components: a physiological delay and a technological delay. The physiological delay, typically between 5-10 minutes, occurs because CGMs measure glucose in the interstitial fluid rather than in blood, and time is required for glucose to diffuse across capillary walls [25]. The technological delay (ranging from 3-12 minutes) results from sensor signal filtering and processing algorithms needed to reduce noise [25]. Machine learning models can compensate by acting as virtual CGM systems. They use life-log data (diet, physical activity) as input to predict current and future glucose levels, operating independently of prior glucose measurements during inference to fill gaps during CGM unavailability [3].
2. Which machine learning algorithms show the most promise for improving CGM signal prediction accuracy?
Different algorithmic families offer distinct advantages:
- Deep Learning (LSTM Networks): Bidirectional LSTM networks with encoder-decoder architectures are particularly well-suited for capturing the temporal dynamics of glucose levels. Their ability to learn long-term dependencies in sequential data makes them capable of modeling complex relationships between lifestyle factors and glucose fluctuations [3].
- Tree-Based Models (Random Forest, GBT): In comparative studies on signal detection, Random Forest and Logistic Regression models were superior at identifying true signals. Gradient-Boosted Trees (GBT) can also achieve high performance, with one tuned model reporting a ROCAUC of 0.646 [50].
- Neural Networks (NNET): Beyond LSTMs, other neural network architectures can define complex, non-linear relationships between risk factors and outcomes, often achieving high prediction accuracy in classification tasks [51].
3. We are experiencing training instability in our deep learning models for glucose prediction. What are the primary mitigation strategies?
Training instability is a common challenge. A systematic approach is recommended [52]:
- Identify the Instability: Perform a learning rate sweep to find the best learning rate (lr). Plot training loss for rates just above lr; if the loss increases, instability is likely an issue.
- Implement Learning Rate Warmup: Prepend a schedule that ramps the learning rate from 0 to a stable base rate (often 10x the unstable rate) over a number of steps. This is highly effective for early-training instability.
- Apply Gradient Clipping: This technique limits the magnitude of gradients during training, preventing sudden spikes that cause instability. A good starting threshold is the 90th percentile of the observed gradient norms [52].
- Consider Alternative Optimizers: In some cases, switching from an optimizer like Momentum to Adam can resolve instability issues [52].
Troubleshooting Guides
Issue: Model Performance Degradation During Rapid Glucose Changes
- Problem: Even with a well-trained model, prediction errors spike during periods of fast glucose dynamics, likely due to unaccounted-for sensor delays.
- Solution: Integrate a multi-step prediction framework that explicitly models the physiological delay.
- Protocol:
- Data Preparation: Use a dataset with paired CGM and reference blood glucose (BG) measurements. Pre-process data to handle missing values and outliers.
- Delay Estimation: For each period of rapid glucose change (e.g., rate of change > 2 mg/dL/min), calculate the time shift that minimizes the difference between the CGM trace and the BG values. The average of these shifts across your dataset provides an estimate of the systemic delay (often ~9.5 minutes) [25].
- Model Training: Instead of predicting current glucose, train your model (e.g., an LSTM) to predict the glucose level at time t + Δt, where Δt is the estimated systemic delay. This aligns the model's output with the physiological reality.
- Validation: Validate the model on a hold-out dataset, paying specific attention to its performance during postprandial periods and hypoglycemic recovery.
Issue: Suboptimal Validation Performance Despite High Training Accuracy
- Problem: The model appears to learn the training data well but fails to generalize to unseen validation data, indicating potential overfitting.
- Solution: Implement a robust hyperparameter tuning and regularization strategy.
- Protocol:
- Hyperparameter Sweep: Systematically tune key hyperparameters. The table below summarizes a core set to optimize [52].
- Regularization: Incorporate L2 regularization (weight decay) and dropout layers in your neural network architecture to prevent over-reliance on specific nodes.
- Cross-Validation: Use k-fold cross-validation to get a more reliable estimate of model performance and ensure it is not tailored to a specific train-validation split.
- Early Stopping: Monitor the validation loss during training and halt the process when validation performance plateaus or begins to degrade.
Table 1: Key Hyperparameters for Model Tuning
| Hyperparameter | Description | Common Strategies |
|---|---|---|
| Learning Rate | Controls the step size during weight updates. | Perform a logarithmic sweep (e.g., from 1e-5 to 1e-1). Use learning rate warmup and decay schedules [52]. |
| Batch Size | Number of samples processed before updating parameters. | Tune with other parameters; larger batches may require stronger regularization [52]. |
| Gradient Clipping Threshold | Maximum allowed norm of the gradients. | Start with the 90th percentile of gradient norms; tune aggressively if instability persists [52]. |
| Number of Layers/Units | Determines model capacity. | Start with a simpler architecture and increase complexity only if performance is insufficient. |
| Dropout Rate | Fraction of neurons randomly ignored during training. | Typical values range from 0.1 to 0.5. |
Experimental Protocols from Key Studies
Protocol 1: Developing a Virtual CGM using Life-Log Data
This protocol is based on the deep learning framework presented in Sci. Rep. 15, 16290 (2025) [3].
- Objective: To train a model that infers current glucose levels using life-log data without prior glucose measurements.
- Data Acquisition:
- Collect data from subjects using CGM (e.g., Dexcom G7) and smartphone apps.
- Input Features: Meal intake (calories, carbs, sugar/fat/protein, time), physical activity (METs, step counts), and timestamp data.
- Output Target: Synchronized CGM glucose measurements.
- Model Architecture:
- A bidirectional LSTM network with an encoder-decoder structure.
- Incorporates dual attention mechanisms for temporal and feature importance.
- Training Procedure:
- Extract subsequences from the entire data trajectory using a sliding window.
- The encoder processes the life-log sequence to create a latent representation.
- The decoder uses this representation to predict the current glucose value.
- The model is first pre-trained on all subject data and can be fine-tuned on individual data for personalization.
- Performance Metrics: The published model achieved an RMSE of 19.49 ± 5.42 mg/dL and a correlation coefficient of 0.43 ± 0.2 [3].
Protocol 2: Comparing Machine Learning Models for Signal Detection
This protocol is adapted from a study comparing classifiers using adverse event reporting data [50].
- Objective: To compare the performance of multiple machine learning algorithms for accurate signal detection.
- Models for Comparison: Logistic Regression (LR), Gradient-Boosted Trees (GBT), Random Forest (RF), and Support Vector Machine (SVM).
- Methodology:
- Data Preparation: Handle class imbalance using strategies like stratified sampling or SMOTE.
- Model Training: Train each algorithm on the prepared training set. Develop both a crude model and a model with tuned hyperparameters for each.
- Performance Evaluation: Compare models on a held-out test set using a suite of metrics.
- Evaluation Metrics:
- Accuracy, Precision, Recall, F1 Score
- Receiver Operating Characteristic Area Under the Curve (ROCAUC)
- Precision-Recall Curve Area Under the Curve (PRCAUC)
- Key Finding: In the referenced study, models trained on a balanced dataset showed higher accuracy, F1 score, and recall. LR and RF were particularly effective at identifying true signals [50].
Table 2: Model Performance Comparison (Adapted from [50])
| Model | Key Strengths | Noted Performance |
|---|---|---|
| Logistic Regression (LR) | Handles confounders well; higher accuracy/precision in comparisons. | Performed similarly to other models on balanced data; high accuracy and recall [50]. |
| Random Forest (RF) | Defines complex, non-linear relationships; reduces overfitting. | Identified as one of the best models for identifying true signals [50]. |
| Gradient-Boosted Trees (GBT) | High performance with iterative boosting. | A hyperparameter-tuned GBT model achieved a ROCAUC of 0.646 [50]. |
| Neural Network (NNET) | Defines complex relationships between risk factors and outcomes. | Can achieve superior prediction accuracy in classification tasks [51]. |
Workflow Diagrams
Virtual CGM Model Development Workflow
ML for Sensor Delay Compensation Logic
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for CGM Prediction Research
| Item / Tool | Function / Application in Research |
|---|---|
| Dexcom G7 / G6 Sensors | Source of continuous glucose monitoring data for model training and validation [3] [53]. |
| Freestyle Libre Pro Sensors | An alternative CGM system for blinded data collection in clinical studies [54]. |
| PyTorch with torch.compile | Deep learning framework and its built-in compiler for significant training speedups via graph optimization [55]. |
| FlashAttention (PyTorch SDPA) | Optimized attention mechanism to speed up Transformer models and reduce memory usage during training [55]. |
| R Package: rGV | Calculates a suite of 16 glycemic variability metrics (e.g., GRADE, LBGI, HBGI) from CGM data for robust model evaluation [54]. |
| Gradient Clipping | A standard technique implemented in frameworks like PyTorch and TensorFlow to mitigate training instability by capping gradient values [52]. |
| Learning Rate Warmup Scheduler | A critical component of the optimization process to prevent early training instability by gradually increasing the learning rate [52]. |
Core Concepts: Understanding Sensor Accuracy and Variability
What are the primary causes of accuracy variability throughout a sensor's lifespan?
Sensor accuracy is not static and fluctuates due to several technical factors. Key causes of this variability include:
- Initial Instability: Sensors often demonstrate lower accuracy immediately after implantation before stabilizing [27].
- Biological Response: The body's natural foreign body response (FIBR) at the implantation site can create a dynamic environment that affects sensor performance over time [27].
- Biochemical Degradation: Graduate breakdown or deactivation of the sensor's enzymatic components (e.g., glucose oxidase) occurs with continuous use [27].
- Signal Drift: Electrochemical sensors exhibit a phenomenon known as "drift," where the baseline signal changes over time, leading to a documented 10-15% accuracy decline over the functional period of current sensors [27].
- Environmental Interference: Physiological conditions during exercise, sleep, and post-meal states introduce additional variability that challenges measurement consistency [27].
Why is accounting for lifespan-dependent accuracy crucial for clinical applications?
For applications like automated insulin delivery (Artificial Pancreas Systems), uncompensated sensor accuracy drift directly impacts therapeutic decisions. Accuracy degradation of 10-15% can lead to:
- Inappropriate insulin dosing decisions based on inaccurate readings [27]
- Failure to detect clinically significant hypoglycemic or hyperglycemic events [27]
- Reduced reliability of trend arrows and predictive alerts [27]
- Compromised performance of closed-loop systems that depend on accurate sensor input [27]
Troubleshooting Guides
How can I identify and compensate for sensor signal drift in experimental data?
Problem: Gradual deviation of sensor readings from reference values over time.
Solution:
- Establish Baseline: Collect frequent reference measurements (e.g., YSI or fingerstick) during the initial stable period post-calibration [27].
- Track Deviation: Monitor the difference between sensor values and reference values across the sensor's operational lifespan [27].
- Apply Computational Correction: Implement algorithms that adjust readings based on estimated accuracy levels at different points in the sensor's lifespan. Research from Insulet Corporation (2024) demonstrates compensation for varying accuracy over the sensor's lifetime [27].
- Time-Dependent Zero-Signal Correction: Utilize methods that subtract the time-dependent zero-signal level of the sensor from the continuous sensor signal, as demonstrated by Roche Diabetes Care (2023), to compensate for drift and interference [27].
How can I detect and mitigate compression artifacts during continuous monitoring studies?
Problem: False low glucose readings caused by mechanical pressure on the sensor site.
Solution:
- Real-Time Detection: Implement clearance value analysis by comparing differences between consecutive CGM readings to normal distributions [27].
- Algorithmic Filtering: When clearance values fall outside normal distributions, flag these periods as potential compression artifacts [27].
- Data Annotation: Mark these events in datasets to prevent false hypoglycemia interpretation and incorrect insulin shutoff in automated systems [27].
- Experimental Design: Consider sensor placement locations less prone to compression during sleep or physical activity [27].
What methodologies improve sensor calibration across the functional period?
Problem: Standard calibration approaches fail to account for sensor-to-sensor variability and lifespan-dependent performance changes.
Solution:
- Personalized Calibration: Utilize manufacturing-derived sensor-specific parameters with machine learning to predict individualized calibration, as demonstrated by Abbott Diabetes Care (2024) [27].
- Dual-Sensor Calibration: Employ two sensors at different tissue depths to estimate personalized time constants for glucose diffusion, accounting for subject-specific interstitial glucose dynamics (Laxmi Therapeutic Devices, 2023) [27].
- Overlapping Sensor Placement: During sensor transitions, calibrate new sensors based on data from expiring sensors to maintain continuous calibration without gaps (Abbott Diabetes Care, 2022) [27].
Experimental Protocols for Sensor Validation
Protocol 1: Quantifying Lifespan-Dependent Accuracy Variability
Objective: Systematically characterize accuracy degradation patterns throughout sensor operational lifetime.
Materials:
- Continuous glucose monitoring sensors
- Reference glucose analyzer (e.g., YSI Stat Plus)
- Controlled glucose clamping setup
- Data acquisition system with timestamp synchronization
Methodology:
- Sensor Implantation: Simultaneously implant multiple sensors according to manufacturer specifications (n≥10 recommended for statistical power).
- Reference Sampling: Collect venous blood samples at predetermined intervals (e.g., every 30-60 minutes) during controlled glucose clamping sessions conducted at 24-hour intervals throughout sensor lifespan.
- Data Collection: Record sensor readings synchronized with reference measurements across glycemic ranges (hypoglycemic, euglycemic, hyperglycemic).
- Accuracy Metrics Calculation: Compute Mean Absolute Relative Difference (MARD), Consensus Error Grid analysis, and precision absolute relative difference (ARD) for each 24-hour period.
- Drift Quantification: Perform linear regression analysis of MARD values versus time to establish drift rate for each sensor.
Table 1: Example Data Collection Schedule for Lifespan Accuracy Assessment
| Day | Glucose Clamp Sessions | Reference Samples per Session | Glycemic Ranges Covered |
|---|---|---|---|
| 1 | 3 | 8 | All three |
| 2 | 2 | 6 | Euglycemic & Hyperglycemic |
| 3 | 2 | 6 | Euglycemic & Hypoglycemic |
| 4+ | 1 | 6 | All three (rotating) |
Protocol 2: Evaluating Compression Artifact Detection Algorithms
Objective: Validate real-time detection methods for sensor compression artifacts.
Materials:
- CGM sensors with raw data access
- Pressure application apparatus with calibrated weights
- Reference glucose monitoring system
- Signal processing software (MATLAB, Python)
Methodology:
- Sensor Preparation: Implant sensors in tissue models or consenting participants according to IRB-approved protocols.
- Controlled Pressure Application: Apply calibrated pressure (10-200 mmHg) to sensor sites for varying durations (1-10 minutes) while maintaining stable glycemic conditions.
- Data Acquisition: Simultaneously record raw sensor signals, applied pressure levels, and reference glucose values.
- Algorithm Validation: Test detection methods by comparing clearance values between consecutive readings to normal distributions established during uncompressed periods [27].
- Performance Metrics: Calculate sensitivity, specificity, and time-to-detection for compression events.
Protocol 3: Validation of Dual-Sensor Calibration for Personalized Time Constants
Objective: Determine subject-specific glucose diffusion time constants using dual-sensor approach.
Materials:
- Paired sensors at different tissue depths
- Frequent reference blood glucose measurements
- Parameter estimation algorithms
- Statistical analysis software
Methodology:
- Sensor Placement: Position two sensors at different depths (e.g., subcutaneous and deeper tissue) in the same anatomical region [27].
- Data Collection: Obtain simultaneous glucose measurements from both sensors over a defined time interval (e.g., 4-6 hours) with varying glucose levels [27].
- Model Fitting: Estimate personalized time constants for glucose diffusion from blood to each sensor site using mathematical modeling of the measurement data [27].
- Validation: Compare sensor accuracy with and without personalized time constant correction against reference measurements.
- Statistical Analysis: Assess inter-subject variability in time constants and correlation with demographic factors.
Dual-Sensor Calibration Workflow
Table 2: Documented Sensor Accuracy Drift Patterns in Current Systems
| Sensor Age (Days) | Typical MARD Range | Primary Contributing Factors | Compensation Strategies |
|---|---|---|---|
| 0-1 (Initial) | 8-14% | Tissue trauma, initialization | Enhanced initial calibration, signal filtering |
| 2-7 (Stable) | 7-11% | Established tissue interface | Standard algorithms |
| 8-10 (Late) | 10-15% | Biochemical degradation, drift | Lifespan-dependent adjustment [27] |
| 10+ (End) | 12-18% | Signal decay, biofouling | Advanced compensation, early replacement |
Table 3: Compression Artifact Detection Performance Metrics
| Detection Method | Time to Detection (min) | Sensitivity | Specificity | False Positive Rate |
|---|---|---|---|---|
| Clearance Value | <5 | 92% | 88% | 12% [27] |
| Signal Morphology | 5-10 | 85% | 82% | 18% |
| Multi-Analyte | 3-7 | 94% | 91% | 9% [27] |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Sensor Lifespan Research
| Reagent/Resource | Function | Example Applications |
|---|---|---|
| Controlled Glucose Clamping System | Maintains precise glycemic levels | Accuracy assessment across physiologic ranges |
| Reference Glucose Analyzer (YSI) | Provides ground truth measurements | Sensor validation and algorithm training [27] |
| Saturated Salt Solutions | Creates specific RH conditions | In-house device accuracy testing [56] |
| Multi-Analyte Sensors | Measures additional biomarkers (e.g., ketones) | Enhancing accuracy and detecting sensor faults [27] |
| Kalman Filter Algorithms | Estimates true glucose from noisy signals | Real-time blood glucose estimation from interstitial measurements [27] |
| Machine Learning Models (Condition-Specific) | Predicts glucose values under abnormal conditions | Reducing sensor signal blanking, improving accuracy [27] |
Frequently Asked Questions
What is the evidence for 10-15% sensor accuracy drift over the functional period?
Recent patent literature from major CGM manufacturers consistently documents this range of accuracy degradation. The drift stems from multiple factors including biochemical sensor component degradation, changes at the tissue-sensor interface, and electrochemical signal instability. This documented drift pattern has prompted development of lifespan-dependent adjustment algorithms that compensate for these predictable accuracy variations [27].
How do dual-sensor systems account for inter-subject variability in glucose dynamics?
Dual-sensor approaches address the fundamental challenge of personalized glucose diffusion kinetics. By placing sensors at different tissue depths, researchers can estimate subject-specific time constants for glucose movement from vascular to interstitial compartments. This personalized parameter estimation significantly improves accuracy compared to population-based averages, particularly during rapid glucose transitions [27].
What computational methods show promise for compensating lifespan-dependent accuracy decline?
Multiple advanced computational approaches demonstrate significant improvements:
- Adaptive Calibration Algorithms: Modify calibration factors based on sensor age and performance history [27]
- Time-Dependent Zero-Signal Correction: Subtract the time-varying baseline signal to compensate for drift [27]
- Machine Learning Models: Condition-specific algorithms trained for different sensor ages and physiologic states [27]
- Signal Ratio-Based Error Correction: Use progression parameters between consecutive measurements to correct for errors [27]
Accuracy Enhancement Pipeline
How can researchers validate sensor performance across the entire lifespan under controlled conditions?
Comprehensive validation requires:
- Longitudinal Study Design: Tracking sensor performance from implantation through expiration with frequent reference measurements
- Controlled Glycemic Clamping: Systematically testing accuracy across physiologic ranges (hypo-, eu-, and hyperglycemic) at multiple timepoints
- Environmental Stress Testing: Evaluating performance during exercise, sleep, and other conditions known to affect accuracy [27]
- Statistical Robustness: Including sufficient sensor samples (typically n≥10) to account for sensor-to-sensor variability
- Standardized Metrics: Using consensus accuracy metrics (MARD, CLSI Error Grid, time-in-range) for cross-study comparability
Frequently Asked Questions (FAQs)
1. What is the primary cause of time delay in Continuous Glucose Monitoring (CGM) systems? The time delay in CGM readings is a combination of physiological and technological factors. Physiologically, CGMs measure glucose in the interstitial fluid (ISF), not blood. The process of glucose moving from capillaries into the ISF creates an average physiological delay of 5-10 minutes [25]. Technologically, delays are added by sensor response time, signal filtering, and data processing algorithms, which can contribute an additional 3-12 minutes [25]. The overall mean time delay of raw CGM signals with respect to blood glucose has been found to be 9.5 ± 3.7 minutes [25] [57].
2. How can multi-analyte sensing help compensate for CGM time delays? Multi-analyte sensing provides contextual metabolic information that can confirm the legitimacy of a rapid glucose trend. By simultaneously monitoring metabolites like lactate, oxygen, and pH, researchers can determine if a changing glucose reading is part of a broader, physiologically plausible metabolic event (like exercise or a meal) or if it might be a sensor artifact [58] [59]. This additional data layer improves the reliability of trend arrows and can enable more sophisticated prediction algorithms for insulin delivery systems [59].
3. Which secondary analytes are most relevant for confirming glucose trends? Key secondary analytes include:
- Lactate: Shifts between aerobic and anaerobic respiration can indicate exercise or ischemic stress, providing context for glucose utilization [58].
- Oxygen (O2): Monitoring oxygen consumption helps clarify the cellular metabolic state and bioenergetics [58].
- pH (Hydrogen Ions): Extracellular acidification rate is a sensitive indicator of overall cellular metabolism and can signal metabolic shifts [58].
- Ketones: While not listed in the provided results, ketones are a critical marker in diabetes management. The principle of multi-analyte sensing can be extended to include them for a more complete metabolic picture.
4. What is the clinical relevance of reducing effective sensor delay? Reducing the effective delay is crucial for improving the safety and efficacy of diabetes management, especially for hypoglycemia detection and prevention [25]. Even with a perfectly accurate sensor, a time delay alone can lead to a Mean Absolute Relative Difference (MARD) of 9.5% compared to blood glucose measurements [25]. Compensating for this delay leads to CGM readings that are more consistent with real-time blood glucose, enabling faster and more accurate clinical decisions.
5. Are multi-analyte time delays patient-specific? Evidence suggests that time delays are indeed patient-dependent [25]. Analysis of the same patients over an 8-month period showed consistent individual delay characteristics, though no significant correlation was found with common anthropometric data [25]. This highlights the potential for personalized calibration and prediction models to further improve performance.
Troubleshooting Guides
Guide 1: Addressing High Signal Noise in Multi-Analyte Sensor Arrays
Problem: Excessive noise in the data from one or more sensors in a multi-analyte array, making trend confirmation difficult.
Background: Signal noise can arise from electrical interference, biofouling, or unstable enzyme immobilization on the sensor surface [25] [58].
| Investigation Step | Action to Perform |
|---|---|
| Verify Electrode Integrity | Inspect the sensor array under a microscope for micro-fractures or damaged electrode coatings. |
| Check Shielding & Grounding | Ensure the potentiostat and connecting cables are properly grounded and shielded from sources of AC noise. |
| Assess Sensor Biofouling | Perform a post-experiment calibration check. A significant shift in baseline may indicate biofouling during the experiment [25]. |
| Review Filter Settings | If using a software filter, ensure it is appropriate. Over-filtering can introduce unacceptable time delays [25]. |
Recommended Protocol: In-Place Sensor Calibration and Validation
- Preparation: Prepare standard solutions for each analyte (e.g., glucose, lactate) at known low and high concentrations within the physiological range.
- Baseline Measurement: Perfuse the calibration solutions through the system and record the sensor signals.
- Data Analysis: Generate a standard curve for each analyte sensor to confirm its sensitivity and linear response.
- Corrective Action: If a specific sensor shows poor performance (e.g., low sensitivity, high noise), the dataset from that analyte channel should be flagged as unreliable for that experimental run.
Guide 2: Resolving Discrepancies Between Glucose and Secondary Analyte Trends
Problem: The glucose trend appears to be rising or falling, but the data from secondary analytes (e.g., lactate, O2) do not support a physiologically consistent metabolic event.
Background: Discrepancies can be caused by different sensor response times, localized sensor failure, or the presence of an unaccounted-for physiological variable (e.g., medication, stress) [59].
| Investigation Step | Action to Perform |
|---|---|
| Check Individual Sensor Lags | Review the manufacturer's specifications for the inherent time delay of each specific sensor type. Align data streams post-hoc if lags are known and consistent. |
| Confirm Physiological Plausibility | Refer to established metabolic pathway models (see diagram below). A glucose rise with stable lactate and O2 may suggest a calibration error rather than a true metabolic event. |
| Verify Sensor Placement | For implanted sensor arrays, ensure all sensing elements are located within the same physiological compartment to avoid spatial discrepancies. |
| Review Experimental Logs | Cross-reference the timeline with logs of participant activity, meals, or stress to identify potential confounding factors. |
Recommended Protocol: Cross-Analyte Data Validation Workflow The following diagram illustrates a logical workflow for troubleshooting discrepant trends, based on the principle of physiological consistency.
Experimental Data & Protocols
Table 1: Quantified Time Delays in CGM Systems
This table summarizes the sources and magnitudes of time delays as reported in the literature [25].
| Delay Component | Estimated Duration | Causes and Notes |
|---|---|---|
| Physiological Delay | 5 - 10 minutes | Time for glucose to diffuse from blood capillaries to interstitial fluid (ISF). Subject to inter-individual variability [25]. |
| Technological Delay | 3 - 12 minutes | Combined result of sensor membrane diffusion, enzyme reaction speed, and on-sensor signal processing [25]. |
| Algorithmic Delay | Variable (e.g., 4 min reduction) | Introduced by noise-reduction filters and prediction algorithms. More aggressive filtering reduces noise but increases delay [25]. |
| Total Measured Delay (Raw Signal) | 9.5 ± 3.7 minutes (Mean ± SD) | Overall delay observed in a clinical study of a prototype sensor before advanced compensation [25] [57]. |
Table 2: The Scientist's Toolkit: Key Reagents and Materials for Multi-Analyte Sensing
Essential research materials for developing and testing multi-analyte systems for metabolic monitoring [58].
| Item | Function in Research |
|---|---|
| Glucose Oxidase (GOx) | Enzyme immobilized on amperometric sensor to selectively catalyze glucose oxidation [58]. |
| Lactate Oxidase (LOx) | Enzyme immobilized on amperometric sensor to selectively catalyze lactate oxidation [58]. |
| Platinum Screen-Printed Electrodes (SPEs) | Robust, reproducible, and low-cost electrode substrates for amperometric detection of analytes like H₂O₂ [58]. |
| Iridium Oxide Film | Used for potentiometric detection of pH (via open circuit potential shifts) [58]. |
| Light-Addressable Potentiometric Sensor (LAPS) | A semiconductor-based sensor that can detect extracellular acidification (pH changes) [58]. |
| Multianalyte Microphysiometer (MAMP) | An instrument with a microfluidic chamber and embedded sensors for detecting glucose, lactate, O₂, and pH from live cells [58]. |
Core Experimental Protocol: Simultaneous Monitoring of Glucose and Secondary Analytes
This methodology is adapted from studies using the Multianalyte Microphysiometer (MAMP) for cellular bioenergetics [58].
Objective: To dynamically track glucose, lactate, and oxygen levels in vitro to identify metabolic states and validate glucose trends.
Procedure:
- Sensor Preparation: Integrate a sensor array with immobilized glucose oxidase, lactate oxidase, and a direct O₂ sensor into a microfluidic chamber.
- Cell Seeding: Introduce a suspension of live cells (e.g., primary neurons, pancreatic islets) into the chamber.
- Perfusion: Continuously perfuse the chamber with a nutrient solution at a low, constant flow rate to maintain the cells and remove waste.
- Baseline Recording: Record the stable, baseline signals for all analytes under normal conditions.
- Experimental Stimulus: Introduce a metabolic challenge. Examples include:
- Nutrient Deprivation: Switch to a glucose-free solution to model ischemia.
- Chemical Toxin: Introduce a toxin like cyanide to inhibit oxidative phosphorylation.
- Hyperglycemic Push: Increase glucose concentration to stimulate insulin secretion in islet studies.
- Data Acquisition: Continuously record the amperometric (glucose, lactate, O₂) and potentiometric (pH) signals throughout the experiment.
- Data Analysis: Analyze the time-course data to identify correlated shifts. For example, a drop in glucose and O₂ with a concurrent rise in lactate confirms a shift to anaerobic respiration.
The signaling pathways involved in this protocol can be visualized as follows:
Troubleshooting Guides and FAQs
This section addresses common challenges researchers face when implementing machine learning-based personalized calibration for Continuous Glucose Monitoring (CGM) sensors.
FAQ 1: What are the primary sources of signal noise in CGM data, and how can machine learning mitigate them?
CGM signals are contaminated by multiple noise sources that complicate accurate glucose estimation. These include:
- Baseline Drift: Signal drift can exceed 0.5 mg/dL per hour [60].
- Activity-Induced Artifacts: Noises ranging from 10-20 mg/dL caused by patient movement [60].
- Medication Interference: Substances like acetaminophen can cause errors of up to 30 mg/dL [60].
- Compression Artifacts: Physical pressure on the sensor can cause false lows [60].
Machine Learning Mitigation: A 2025 study describes a machine learning-based time series denoising method. This technique learns the statistical relationships between samples in a time series. The model iteratively predicts the current sample using nearby samples; since independent noise is unpredictable, it is effectively removed from the reconstructed signal. This approach does not require pre-designed filters or clean data for training [60].
FAQ 2: How can I compensate for the physiological time lag between blood and interstitial glucose readings during calibration?
The delay in glucose diffusion from blood to interstitial fluid is a primary source of error. Advanced calibration methods now incorporate additional physiological data to address this.
Experimental Protocol for lag-aware calibration:
- Data Synchronization: Collect paired blood glucose reference measurements (e.g., from fingerstick tests) and raw CGM sensor current signals with precise timestamps.
- Feature Engineering: Integrate insulin delivery data as a key feature. Note the time and dosage of insulin administration, as this directly affects glucose dynamics [60].
- Model Application: Implement a Sequential Kalman Filter to deconvolute the interstitial sensor currents and estimate blood glucose levels.
- Parameter Refinement: Use a conventional Kalman Filter to estimate final blood glucose calibration parameters from capillary measurements. For initial calibration, offline estimation of parameters using a Cubature Kalman Filter is recommended [60].
- Personalization: Utilize patient-specific prior calibration parameters from previous days instead of generic population-level priors to enhance individual accuracy [60].
FAQ 3: Our calibration model performs well in the lab but degrades in real-world use. How can we improve its robustness?
This is often due to unaccounted-for environmental and physiological variabilities. Solutions include:
- Dynamic Interference Management: Develop a system that detects administrations of interfering substances (e.g., certain medications), calculates the interference effect based on concentration and timing, and executes a response to mitigate its impact on the signal [60].
- Adaptive Sampling: Implement a controller that adjusts the sensor's biometric sampling rate based on glucose variability. If variability increases, the sampling rate increases to capture more data, and it decreases during stable periods to conserve power [60].
- Multi-Sensor Fusion: Use additional sensors, such as lactate sensors and force sensors, to detect and correct for compression artifacts. A 2025 patent describes a system that compares glucose and lactate readings; an inverse correlation in their values indicates a compression event, triggering a reading adjustment [60].
FAQ 4: How do I evaluate the performance of a personalized calibration model for CGM sensors?
Beyond standard metrics, use clinical and manufacturing-oriented assessments. The table below summarizes key quantitative metrics and manufacturing parameters to analyze.
Table 1: Key Performance Indicators for Calibration Models
| Metric Category | Specific Metric | Definition and Interpretation |
|---|---|---|
| Overall Accuracy | Mean Absolute Relative Difference (MARD) | The average percentage difference between sensor and reference values. Lower is better. A study achieved a reduction from 10.18% to 4.33% with a patient-specific algorithm [60]. |
| Overall Accuracy | Coefficient of Determination (R²) | The proportion of variance in reference values explained by the model. Closer to 1.0 is better. In air quality sensor research (a analogous field), values of 0.970 were achieved [61]. |
| Error Distribution | Clarke Error Grid (CEG) Analysis | Categorizes point pairs into zones (A-E) based on clinical accuracy. >99% in Zones A & B is a common goal [60]. |
| Model Precision | Root Mean Square Error (RMSE) | The standard deviation of prediction errors. Lower is better. In analogous studies, values as low as 0.442 for gas sensors have been reported [61]. |
| Manufacturing Parameter | Sensor Slope (mV per pH unit for analytic sensors) | Indicates sensor responsiveness. A new sensor has a slope of 56-59 mV, which deteriorates with age. 45 mV indicates the sensor is expired [62]. |
| Manufacturing Parameter | Change in Sensor Offset (mV) | The drift in the sensor's baseline signal from its "as new" condition. A change of ±40 mV or more suggests the sensor is close to expiry [62]. |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Algorithms for Personalized Sensor Calibration Research
| Item Name | Function in Research |
|---|---|
| Gaussian Process Regression (GPR) | A non-parametric machine learning algorithm ideal for modeling sensor drift and correcting size-resolved counting efficiencies in optical particle sensors, as demonstrated in net-zero energy building studies [63]. |
| Gradient Boosting (GB) | An ML algorithm that has shown top performance in calibrating low-cost environmental sensors, achieving an R² of 0.970 for CO2 sensors. It is highly effective for tabular data with non-linear relationships [61]. |
| k-Nearest Neighbors (kNN) | A simple, powerful algorithm for sensor calibration. It was the most successful model for PM2.5 sensor calibration in one study, achieving an R² of 0.970 [61]. |
| Sequential and Cubature Kalman Filters | Advanced algorithms used for deconvoluting sensor signals and estimating calibration parameters, specifically designed to handle time-series data and manage uncertainty in systems like CGM [60]. |
| Microneedle Sensor with Interferent Blocking Layer | A physical sensor design featuring specialized layers that block interfering substances and limit glucose diffusion, directly reducing signal noise and variability at the source [60]. |
| Analyte Sensor with Degradation Indicator | A dual-sensor system that separately measures the degradation of the main sensing element, allowing software to correct for measurement errors caused by this degradation over time [60]. |
Experimental Protocols and Workflows
Detailed Methodology for a Machine Learning Field Calibration
This protocol is adapted from a successful study on particle sensors and can be generalized for CGM research [63].
- Sensor Co-location: Co-locate the low-cost CGM sensor(s) with high-precision reference instruments (e.g., clinical blood glucose analyzers) in a controlled but realistic environment (e.g., clinical research unit).
- Data Collection: Collect a time-synchronized dataset encompassing:
- Raw signal output from the CGM sensor.
- Reference blood glucose measurements.
- Environmental covariates: temperature, humidity.
- Physiological covariates: heart rate, insulin delivery logs, patient activity.
- Potential interferent logs: medication administration.
- Data Preprocessing:
- Anomaly Detection: Identify and remove physiologically impossible outliers.
- Missing Data Imputation: Use techniques like kNN or linear interpolation to handle small gaps in data.
- Noise Filtering: Apply a moving average filter or a denoising autoencoder to smooth high-frequency noise [60].
- Feature Engineering:
- Calculate rolling statistical features (mean, standard deviation) from the raw signal over short-time windows (e.g., 5-15 minutes).
- Incorporate manufacturing parameters (e.g., initial slope and offset) as static features in the model.
- Create time-lagged features of covariates to better capture temporal dynamics.
- Model Training:
- Split the dataset into training and testing sets, ensuring temporal consistency.
- Train multiple ML models (e.g., GPR, GB, RF, kNN) using the training set.
- Optimize model hyperparameters via cross-validation.
- Performance Evaluation:
- Evaluate the best-performing model on the held-out test set using the metrics in Table 1.
The workflow for this methodology can be visualized as follows:
Signaling Pathway for Sensor Data Processing and Calibration
The following diagram illustrates the logical flow of transforming a raw, noisy sensor signal into a calibrated, personalized glucose reading, integrating the key concepts discussed.
Technical Support Center: Troubleshooting CGM Trend Arrows
This technical support center provides troubleshooting guides and FAQs for researchers and scientists working on Continuous Glucose Monitoring (CGM) sensor delay compensation. The content addresses common experimental challenges related to the interpretation and utilization of trend arrows.
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary cause of the time delay in CGM systems, and how does it impact trend arrow data?
The total time delay in CGM systems is a combination of physiological and technological factors [25].
- Physiological Lag ( approximately 5-10 minutes): CGM sensors measure glucose in the interstitial fluid (ISF), not in blood. The process of glucose diffusing from capillaries into the ISF creates this inherent physiological lag [25].
- Technological Lag ( approximately 3-12 minutes): This includes the sensor's response time and the algorithmic filtering applied to the raw signal to reduce noise. Stronger filtering reduces signal noise but increases this algorithmic delay [25].
This combined delay means that trend arrows, which are calculated from retrospective glucose data over the past 15 minutes, may not always reflect the real-time, current blood glucose status, especially during periods of rapid glucose change [64] [25].
FAQ 2: The trend arrows on our experimental setup and a commercial device show different rates of change for the same glucose trend. Why?
This discrepancy arises due to a lack of standardization among CGM manufacturers. Different systems use unique algorithms and thresholds to define the rate of change (ROC) represented by each trend arrow [64].
For example, a single upward arrow () on one system might indicate a ROC of 1-2 mg/dL/min, while on another, it could represent 2-3 mg/dL/min [64]. The table below summarizes the different thresholds. Researchers must be familiar with the specific specifications of the CGM system used in their studies to ensure accurate data interpretation [64].
FAQ 3: In an experiment, a downward trend arrow is displayed, but the glucose curve suggests levels have stabilized. How should we proceed?
This scenario highlights a key limitation of relying solely on trend arrows. The arrow is based on retrospective data and may not capture a very recent stabilization [65].
Troubleshooting Guide:
- Do not rely on the arrow alone. Analyze the graphical glucose curve from the last 15-30 minutes to visually confirm the current trend [65].
- Prioritize the current glucose value. If the graphical curve shows that glucose levels have flattened, base your experimental decisions on the current glucose level rather than the historical trend indicated by the arrow [64].
- Wait and confirm. If the situation is not time-critical, wait 5-10 minutes and scan again to see if the trend arrow updates to a stable (→) indication.
FAQ 4: How can we experimentally validate the accuracy and predictive value of trend arrows in our research setting?
Experimental Protocol for Trend Arrow Validation:
- Setup: Conduct a frequent sampling study with a reference blood glucose method (e.g., YSI analyzer or frequent venous sampling) running in parallel with the CGM system under investigation [25].
- Data Collection: Record the reference glucose value, CGM glucose value, and the displayed trend arrow at fixed, frequent intervals (e.g., every 5 minutes).
- Data Analysis:
- For each trend arrow category (e.g., , ↑↑), calculate the actual observed rate of change in the reference blood glucose over the subsequent 15-30 minutes.
- Compare this observed ROC to the manufacturer's claimed ROC range for that arrow [64].
- Calculate the mean absolute relative difference (MARD) between the CGM-predicted glucose (current value + [ROC × time]) and the actual reference glucose value at future time points [25].
Data Presentation Tables
Table 1: Manufacturer-Specific Trend Arrow Definitions and Projected 30-Minute Glucose Change [64]
| Trend Arrow | Abbott FreeStyle Libre | Dexcom G4/G5/G6 Mobile | Medtronic 640G | Medtronic Veo | Roche Senseonics Eversense |
|---|---|---|---|---|---|
| Double Up (↑↑) | NA | > 90 mg/dL / > 5.0 mmol/L | > 90 mg/dL / > 5.0 mmol/L | NA | NA |
| Single Up (↑) | > 60 mg/dL / > 3.3 mmol/L | 60-90 mg/dL / 3.3-5.0 mmol/L | 60-90 mg/dL / 3.3-5.0 mmol/L | > 60 mg/dL / > 3.3 mmol/L | > 60 mg/dL / > 3.3 mmol/L |
| 45° Up () | 30-60 mg/dL / 1.7-3.3 mmol/L | 30-60 mg/dL / 1.7-3.3 mmol/L | 30-60 mg/dL / 1.7-3.3 mmol/L | 30-60 mg/dL / 1.7-3.3 mmol/L | 30-60 mg/dL / 1.7-3.3 mmol/L |
| Stable (→) | < 30 mg/dL / < 1.7 mmol/L | < 30 mg/dL / < 1.7 mmol/L | NA | NA | < 30 mg/dL / < 1.7 mmol/L |
| 45° Down () | 30-60 mg/dL / 1.7-3.3 mmol/L | 30-60 mg/dL / 1.7-3.3 mmol/L | NA | NA | 30-60 mg/dL / 1.7-3.3 mmol/L |
| Single Down (↓) | > 60 mg/dL / > 3.3 mmol/L | 60-90 mg/dL / 3.3-5.0 mmol/L | 30-60 mg/dL / 1.7-3.3 mmol/L | 30-60 mg/dL / 1.7-3.3 mmol/L | > 60 mg/dL / > 3.3 mmol/L |
| Double Down (↓↓) | NA | > 90 mg/dL / > 5.0 mmol/L | 60-90 mg/dL / 3.3-5.0 mmol/L | > 60 mg/dL / > 3.3 mmol/L | NA |
Table 2: Proposed Insulin Dose Adjustment Based on Trend Arrows and Sensitivity Factor (SF) for Research Contexts [65]
| Current Glucose | SF (mg/dL) | Double Up (↑↑) | Single Up (↑) | 45° Up () | Stable (→) | 45° Down () | Single Down (↓) | Double Down (↓↓) |
|---|---|---|---|---|---|---|---|---|
| 70-180 mg/dL | 30-50 | +3.0 U | +2.0 U | +1.0 U | 0 U | -1.0 U | -2.0 U | -3.0 U |
| (In Range) | 51-80 | +2.5 U | +1.5 U | +1.0 U | 0 U | -1.0 U | -1.5 U | -2.5 U |
| >80 | +2.0 U | +1.0 U | +0.5 U | 0 U | -0.5 U | -1.0 U | -2.0 U | |
| 181-250 mg/dL | 30-50 | +3.5 U | +2.5 U | +1.5 U | 0 U | -1.5 U | -2.5 U | -3.5 U |
| (Level 1 Hyper) | 51-80 | +3.0 U | +2.0 U | +1.0 U | 0 U | -1.0 U | -2.0 U | -3.0 U |
| >80 | +2.5 U | +1.5 U | +1.0 U | 0 U | -1.0 U | -1.5 U | -2.5 U | |
| >250 mg/dL | 30-50 | +4.0 U | +3.0 U | +2.0 U | 0 U | -2.0 U | -3.0 U | -4.0 U |
| (Level 2 Hyper) | 51-80 | +3.5 U | +2.5 U | +1.5 U | 0 U | -1.5 U | -2.5 U | -3.5 U |
| >80 | +3.0 U | +2.0 U | +1.0 U | 0 U | -1.0 U | -2.0 U | -3.0 U |
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for CGM Lag Compensation Studies
| Item | Function in Research |
|---|---|
| CGM Systems (rtCGM & isCGM) | The primary devices under investigation. They provide real-time or intermittently scanned glucose data and trend arrows for analysis [64]. |
| Reference Blood Glucose Analyzer (e.g., YSI) | Provides the "gold standard" blood glucose measurements against which CGM values and trend arrow predictions are validated for accuracy and delay [25]. |
| Glucose Clamp Apparatus | Allows researchers to induce controlled and steady rates of change in blood glucose, which is essential for precisely calibrating and testing the predictive algorithms of trend arrows [25]. |
| Data Logging Software | Critical for time-synchronizing CGM data, trend arrow changes, and reference blood glucose measurements for subsequent analysis of delay and ROC accuracy [25]. |
| Interstitial Fluid Sampling Kit | Used in fundamental physiological studies to directly measure ISF glucose, helping to separate physiological lag from technological sensor lag [25]. |
Experimental Workflow and System Relationships
CGM Lag Experiment Workflow
CGM System Lag Components
Validation Frameworks and Comparative Analysis of Delay Compensation Across CGM Platforms
Frequently Asked Questions (FAQs)
Q1: What is MARD, and why is it the primary metric for CGM accuracy? A1: The Mean Absolute Relative Difference (MARD) is a standard metric used to evaluate the accuracy of continuous glucose monitoring (CGM) systems. It represents the average absolute percentage difference between the glucose readings reported by the CGM sensor and corresponding reference measurements (e.g., from a laboratory analyzer or blood glucose meter). A lower MARD value indicates a more accurate sensor [66].
MARD is calculated with the formula: MARD = (1/N) * Σ |(BG_i - Comp_i) / Comp_i|, where BGi is the i-th CGM result and Compi is the corresponding comparison method's result [67]. It provides a single number for easy comparison but does not distinguish between bias and imprecision. Its value can be influenced by study design, glucose concentration, and the rate of glucose change [68].
Q2: How does the Consensus Error Grid assess clinical risk? A2: The Consensus Error Grid (Parkes Error Grid) is a tool that evaluates the clinical accuracy of glucose monitors by assessing the potential risk that a measurement error could lead to an adverse treatment decision [69] [70].
It divides a graph (reference glucose vs. monitor glucose) into five zones:
- Zone A: Clinically accurate results that would lead to correct treatment decisions.
- Zone B: Results that deviate from the reference but would lead to benign or no treatment.
- Zone C: Results that would lead to over-correction.
- Zone D: Results that represent a dangerous failure to detect and treat.
- Zone E: Results that would lead to erroneous, potentially dangerous treatment [71].
The ISO 15197:2013 standard requires that 99% of individual measured glucose values fall within the clinically acceptable Zones A and B [69].
Q3: What are the key sources of time delay in CGM systems, and how do they impact accuracy metrics? A3: Time delays in CGM systems are a critical factor in sensor performance, especially during rapid glucose changes. The total delay is a combination of physiological and technological factors [25].
- Physiological Delay (~5-10 minutes): CGM sensors measure glucose in the interstitial fluid (ISF), not in blood. After a change in blood glucose, time is required for glucose to diffuse from capillaries into the ISF. This delay can vary between individuals and is affected by local blood flow and tissue perfusion [25].
- Technological Delay (~3-12 minutes): This includes the sensor's response time as glucose diffuses through its membranes and the signal processing time. Filtering algorithms used to smooth noisy data inherently create a lag, as they can only use past data points. There is a direct trade-off between signal smoothness and introduced delay [25].
These delays mean that during rapid glucose swings, the MARD can be artificially inflated even if the sensor's analytical performance is perfect, as the CGM value is not aligned with the simultaneous reference blood glucose value [25].
Q4: Is there a threshold MARD value that guarantees a CGM system meets regulatory standards like ISO 15197? A4: While MARD is a useful indicator, there is no deterministic MARD threshold that guarantees compliance with the ISO 15197 standard. The relationship is probabilistic [67].
Empirical data from system accuracy evaluations of blood glucose monitoring systems showed:
- The lowest MARD for a test strip lot that failed to meet ISO 15197 (i.e., had <95% of results within the required limits) was 6.1%.
- Only a small percentage (3.6%) of test strip lots with a MARD ≤7% failed to meet the ISO criteria [67].
Therefore, while a MARD below approximately 6-7% is a strong indicator that a system will meet ISO requirements, this cannot be stated with absolute certainty. Regulatory submissions must demonstrate passing the ISO 15197 test protocol directly [67].
Q5: How much data loss is acceptable in a CGM study without significantly affecting clinical metrics? A5: Current recommendations, supported by recent research, suggest that 14 days of CGM data with a maximum of 30% data loss provide a reliable estimation of key glucose metrics for clinical decision-making [72].
One study found that with 30% data loss in 14-day recordings, the impact on clinical interpretation was minimal. For Time Below Range (TBR), expert-panel-defined boundary errors occurred in only 0.3% of cases. For more severe hypoglycemia (TBR Level 2, <54 mg/dL), this figure was 6.1%, though the initial TBR2 values in these cases were very small (<0.1%) [72]. The type of data loss (random vs. systematic) also influences its impact, with data Missing Completely at Random (MCAR) having the least effect on outcomes [72].
Troubleshooting Common Experimental Issues
Issue 1: Inconsistent MARD values across study phases.
- Potential Cause: MARD is highly dependent on the study design and the distribution of glucose concentrations. If one study phase has a higher proportion of samples in the hypoglycemic range or during rapid glucose change, the MARD will be higher because sensor performance typically varies across glycemic ranges and rates of change [68] [25].
- Solution:
- Stratify your analysis. Report MARD as a continuous function of glucose concentration and/or rate of change [68].
- Ensure a standardized glucose distribution across study phases as per guidelines like ISO 15197, which specifies required concentrations for testing [67].
- Use a consistent reference method throughout the study, as switching between glucose oxidase (GOD) and hexokinase (HK) methods can introduce variability [67].
Issue 2: A CGM system shows a low MARD but a high number of points in the Consensus Error Grid's risk zones.
- Potential Cause: MARD is an average and can be skewed by many small errors, masking a smaller number of large, clinically dangerous errors. A single point in Zone D or E of the error grid can be clinically significant, even if the overall MARD appears acceptable [69] [71].
- Solution:
- Always use MARD and Error Grid analysis in conjunction. They are complementary tools, with MARD assessing analytical accuracy and the error grid assessing clinical accuracy [69].
- Investigate outliers. Perform a root-cause analysis on any data points that fall into Error Grid Zones C, D, or E to determine if the error is due to sensor lag, calibration issues, or signal artifacts.
Issue 3: Sensor readings appear to lag behind reference values during clamp studies.
- Potential Cause: This is an expected phenomenon due to the combined physiological and technological time delays inherent to all CGM systems. The total delay can range from 5 to 40 minutes, with an average often around 9-10 minutes [25].
- Solution:
- Quantify the delay. In study analysis, you can retrospectively align CGM and reference traces to estimate the specific time lag for your system and conditions [25].
- Implement prediction algorithms. To compensate for this lag in real-time applications, develop or utilize prediction algorithms that forecast glucose levels 10-15 minutes ahead. Such algorithms can reduce the effective time delay, on average, by several minutes [25].
- Account for delay in performance analysis. When calculating the "true" analytical MARD of the sensor (separate from lag-induced error), follow guidelines like those from the Clinical and Laboratory Standard Institute (CLSI) that suggest procedures to retrospectively remove the time delay before evaluation [25].
Table 1: Reported MARD Values for Commercial CGM Systems
| Device | Reported MARD | Release Year |
|---|---|---|
| Dexcom G7 (15-Day) | 8.0% | 2024 |
| Dexcom G7 | 8.2% | 2022 |
| FreeStyle Libre 3 | 7.8% | 2022 |
| Dexcom G6 | 9.0% | 2018 |
| FreeStyle Libre 2 | 9.3% | 2020 |
| Dexcom G5 Mobile | 9.0% | 2015 |
| FreeStyle Libre 1 | 13.7% | 2014 |
| Dexcom G4 Platinum | 13.9% | 2012 |
Data adapted from [66]
Table 2: Key Characteristics of Clinical Error Grids
| Error Grid | Development Basis | Zone A Definition (Clinically Accurate) | Key Application |
|---|---|---|---|
| Clarke (CEG) | Consensus of 5 clinicians [71] | Values within ±20% of reference (for Ref ≥70 mg/dL) [71] | Historical benchmark for BGMs |
| Parkes (PEG) | Survey of 100 clinicians; separate grids for T1D and T2D [69] [71] | Roughly -22% to +25% for reference ≥50 mg/dL [69] | Required by ISO 15197:2013 for system accuracy evaluation [69] [70] |
| Surveillance (SEG) | Survey of 206 international experts; continuous risk spectrum [69] [71] | No risk (0-0.5 on continuous risk scale) [69] | Modern tool for post-market surveillance and performance evaluation [69] |
Experimental Protocols for Key Evaluations
Protocol 1: Assessing CGM Accuracy (MARD and Consensus Error Grid) This protocol is based on standards from ISO 15197 and common clinical practice [67] [68].
- Subject Population: Recruit adults with type 1 or type 2 diabetes, as well as subjects without diabetes. A typical study includes at least 100 subjects to ensure variability.
- Reference Method: Use a laboratory comparator such as a YSI 2300 STAT Plus analyzer (glucose oxidase method) or a hexokinase-based analyzer (e.g., Cobas series). The reference method should itself be highly accurate.
- Glucose Distribution: Ensure capillary blood samples are distributed across the following glucose ranges as measured by the reference method:
- ≥10% of samples <80 mg/dL (4.4 mmol/L)
- ≥10% of samples ≥80 mg/dL (4.4 mmol/L) and ≤130 mg/dL (7.2 mmol/L)
- ≥10% of samples ≥131 mg/dL (7.3 mmol/L) and ≤200 mg/dL (11.1 mmol/L)
- ≥10% of samples ≥201 mg/dL (11.2 mmol/L) and ≤350 mg/dL (19.4 mmol/L)
- ≥5% of samples ≥351 mg/dL (19.5 mmol/L)
- Measurement: For each subject, obtain capillary blood samples. Perform duplicate measurements of each sample with the CGM system under test and the laboratory reference method.
- Data Analysis:
- MARD Calculation: For each paired data point (CGM vs. reference), calculate the Absolute Relative Difference (ARD). The MARD is the mean of all ARD values.
- Consensus Error Grid: Plot all paired data points on the Parkes Error Grid for type 1 diabetes. Calculate the percentage of points that fall within Zones A and B. Per ISO 15197:2013, ≥99% of points must be in these zones to pass.
Protocol 2: Quantifying CGM System Time Delay This protocol outlines a method to estimate the total time delay of a CGM system [25].
- Study Setting: Conduct a controlled clinical study, such as a hyperinsulinemic clamp, where blood glucose is manipulated to create steady-state and dynamic periods (sharp rises and falls).
- Data Collection:
- CGM Data: Collect the raw or smoothed glucose values from the CGM sensor at its native frequency (e.g., every 5 minutes).
- Reference Blood Glucose: Frequently sample venous blood (e.g., every 5-10 minutes) and measure glucose concentration with a laboratory reference method (e.g., YSI). This provides the "true" blood glucose trajectory with high temporal resolution.
- Time Alignment: Synchronize the clocks of the CGM system and the reference method at the start of the study.
- Delay Estimation:
- Cross-Correlation: Calculate the cross-correlation function between the CGM time-series and the reference blood glucose time-series. The time shift (lag) that yields the maximum correlation coefficient is the estimate of the total system time delay.
- Alternatively, use a retrospective alignment method: Manually shift the CGM trace in time until the mean absolute difference between the CGM and reference values is minimized. The required time shift is the estimated delay.
Visualization of Accuracy Assessment Workflow
Diagram 1: CGM accuracy assessment workflow.
Diagram 2: CGM sensor delay causes and compensation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for CGM Accuracy and Delay Research
| Item | Function/Description | Example Products/Citations |
|---|---|---|
| High-Accuracy Laboratory Analyzer | Serves as the reference method against which the CGM is compared. Provides the "true" glucose value for MARD and Error Grid calculations. | YSI 2300 STAT Plus (Glucose Oxidase method); Cobas Integra series (Hexokinase method) [67]. |
| Consensus Error Grid Software/Tool | Used to plot paired glucose data and automatically calculate the percentage of points in each risk zone (A-E). | Custom software or published coordinates for the Parkes Error Grid [69] [70]. |
| Hyperinsulinemic Clamp Setup | The "gold standard" method for creating controlled, dynamic glucose excursions. Essential for precisely quantifying sensor time delay. | Insulin infusion system with variable dextrose infusion to maintain target glycemia [25]. |
| Signal Processing & Prediction Algorithm Software | Used to develop and test algorithms that filter CGM signal noise and predict future glucose values to compensate for time delay. | MATLAB, Python (with SciPy, scikit-learn libraries); Kalman filters, moving average filters [25]. |
| Data Loss Simulation Script | A tool to systematically introduce random or patterned data loss into complete CGM datasets to study its impact on glycemic metrics. | Custom Python or R scripts to remove data points based on MCAR, MAR, or MNAR models [72]. |
For researchers investigating continuous glucose monitoring (CGM) sensor delay compensation, understanding the inherent performance characteristics of factory-calibrated sensors under dynamic conditions is fundamental. These systems, which require no user calibration, utilize complex algorithms to convert sensor signals into glucose values, introducing specific delay patterns that must be characterized for effective compensation strategies. This technical support center provides structured methodologies, performance data, and troubleshooting guidance to support your experimental work in this domain. The following sections detail protocols for evaluating sensor performance, quantitative comparisons across systems, and solutions to common research challenges encountered when working with these devices in controlled experimental settings.
Frequently Asked Questions (FAQs)
Q1: What is the clinical significance of MARD (Mean Absolute Relative Difference) when evaluating sensor performance in glycemic clamping studies?
MARD provides a quantitative measure of overall sensor accuracy by calculating the average absolute value of the relative differences between paired CGM and reference glucose values. A lower MARD indicates higher accuracy. In the context of delay compensation research, understanding the baseline MARD is crucial as it represents the best-case scenario accuracy before implementing any novel compensation algorithms. Recent studies of 15-day factory-calibrated sensors demonstrated overall MARD values of 8.2% for adults and 8.1% for pediatric participants (ages 6-17) against YSI reference, establishing a performance benchmark for researchers [73].
Q2: How do factory-calibrated sensors perform during periods of rapid glucose change, and what are the implications for delay compensation research?
Factory-calibrated sensors exhibit varying performance during glycemic excursions, which is precisely why delay compensation research is critical. Performance evaluation during controlled glycemic manipulation shows these sensors maintain high accuracy even in hypoglycemic ranges, with 97.1% and 98.0% of results within ±15 mg/dL of YSI reference for adult and pediatric participants respectively [73]. However, prediction accuracy declines during high-variability contexts such as mealtimes and glucose extremes, highlighting the need for improved compensation approaches that can address these challenging physiological conditions [74].
Q3: What methodologies are appropriate for quantifying and characterizing sensor delay in factory-calibrated CGM systems?
The most direct method for delay quantification involves performing least square linear regression of the difference between sensor and reference values versus the sensor rate of change. One study calculated the slope of this regression line to determine mean lag time, providing a standardized metric for delay characterization [73]. Additionally, the CGM-LSM (Large Sensor Model) utilizes transformer-decoder architecture to model glucose sequences and predict future values, offering researchers a novel framework for analyzing temporal relationships in CGM data [74].
Q4: How does sensor performance vary across different patient populations, and how should this inform recruitment for delay compensation studies?
Significant performance variations exist across demographic groups, necessitating stratified recruitment in research studies. For instance, children aged 2-5 years showed higher MARD (11.2%) compared to older children and adults (8.1-8.2%) [73]. Diabetes type also influences glucose variability patterns, with studies pretraining models on data from both T1D (291 patients) and T2D (301 patients) populations to ensure robust algorithm performance across patient types [74]. These differences must be accounted for in study design to ensure generalized findings.
Q5: What are the key technical challenges reported with latest-generation CGM systems that might impact delay compensation research?
Recent technical challenges include sensor deployment issues, connectivity problems, and adhesive failures, particularly with the Dexcom G7 system, which faced a Class I FDA recall related to receiver component failures and software defects that could cause missed "Sensor Failed" alerts [75]. Additionally, researchers should note that sensor design modifications, such as those implemented in the FreeStyle Libre 2 Plus and 3 Plus to reduce vitamin C interference and minimize available electrode area for electrochemical oxidation of potential interfering compounds, may alter delay characteristics and require re-characterization [73].
Troubleshooting Common Experimental Issues
Problem: Inconsistent sensor performance during induced glycemic excursions Solution: Implement standardized glycemic clamping protocols with frequent reference sampling (every 5 minutes) during periods of glucose <70 or >250 mg/dL. Ensure proper sensor placement and document any manipulation techniques (e.g., insulin sensitivity factors, food intake control) for reproducibility [73].
Problem: Excessive signal drift during extended wear periods Solution: Conduct linear regression analysis on paired readings of relative difference between sensor and reference values against sensor elapsed time to quantify drift patterns. Consider the impact of sensor design improvements, such as reduced electrode area in newer models, which may minimize drift from electroactive compounds [73].
Problem: High variance in prediction accuracy across patient subgroups Solution: Utilize large-scale pretraining approaches like the CGM-LSM model, which was trained on 1.6 million CGM records from diverse patient populations. Stratify analysis by diabetes type, age groups, and glycemic variability patterns to identify subgroup-specific compensation needs [74].
Problem: Discrepancies between interstitial fluid and blood glucose measurements during rapid changes Solution: Recognize that this physiological lag is a fundamental characteristic requiring compensation rather than a sensor defect. Focus research on predicting blood glucose trends rather than perfectly matching interstitial measurements, particularly during periods of rapid change [74].
Problem: Connectivity issues disrupting continuous data collection during experiments Solution: Document and report connectivity problems, as these have been identified as known issues with some systems. Implement redundant data logging systems and note that recent manufacturer improvements have aimed to address Bluetooth connectivity concerns in newer production batches [75].
Quantitative Performance Data
Table 1: Accuracy Metrics for 15-Day Factory-Calibrated CGM Sensors Across Populations
| Population | Sample Size | MARD (%) | % within ±20mg/dL/20% | Hypoglycemic Range Performance (% within ±15mg/dL) |
|---|---|---|---|---|
| Adults | 149 | 8.2% | 94.2% | 97.1% |
| Pediatrics (6-17 years) | 124 | 8.1% | 94.0% | 98.0% |
| Young Children (2-5 years) | 12 | 11.2% | 86.6% | Not reported |
Table 2: Advanced CGM Forecasting Model Performance (CGM-LSM)
| Prediction Horizon | RMSE (mg/dL) | Improvement vs Baseline | Key Limitations |
|---|---|---|---|
| 1-hour | 15.90 | 48.51% reduction | Performance declines during high-variability contexts (mealtimes, glucose extremes) |
| 2-hour | Not reported | Significant improvement | Accuracy affected by daytime hours and extreme glucose values |
Table 3: Technical Specifications of Current Factory-Calibrated CGM Systems
| System | Wear Duration | Warm-up Time | Data Transmission | Special Features |
|---|---|---|---|---|
| FreeStyle Libre 2 Plus/3 Plus | 15 days | Not reported | Every minute to reader/app | Reduced vitamin C interference, improved sensor design |
| Dexcom G7 (15-day) | 10 days (extending to 15) | 30 minutes | Every 5 minutes | 60% smaller than G6, predictive alerts |
| Eversense 365 | 1 year | Not reported | Every 5 minutes | Implantable, requires weekly calibration |
| Medtronic Simplera | 6 days + 24 hours | 2 hours | Not reported | Disposable, all-in-one design |
Experimental Protocols for Sensor Evaluation
Protocol for Sensor Accuracy Assessment Under Dynamic Conditions
Objective: To evaluate the accuracy of factory-calibrated CGM sensors across the glycemic range, with particular emphasis on performance during rapid glucose changes.
Materials:
- Factory-calibrated CGM sensors (multiple units from same production lot)
- YSI 2300 Stat Plus analyzer or equivalent reference method
- Venous blood sampling equipment
- Precision Neo blood glucose test strips
- Data collection software and hardware
- Standardized glycemic manipulation materials (IV glucose, insulin)
Procedure:
- Participant Preparation: Recruit participants with diabetes representing target populations (include both T1D and T2D). Ensure exclusion of pregnancy, anemia, or conditions that could place participants at risk during glucose manipulation.
- Sensor Application: Apply sensors to the back of the arms following manufacturer's instructions for use. Document placement precisely for reproducibility.
- In-Clinic Sessions: Schedule up to three 10-hour sessions covering different sensor wear periods (days 1-3, 5-7, 9-11, 13-15).
- Reference Sampling: Collect venous blood every 15 minutes during stable periods, increasing to every 5 minutes when glucose is <70 or >250 mg/dL.
- Glycemic Manipulation: For participants aged 11+, conduct supervised glycemic manipulation to achieve target glucose levels (<70 mg/dL for ~1 hour, then >300 mg/dL for ~1 hour) while maintaining safety.
- Data Collection: Scan sensors immediately after each reference sample collection. Centrifuge blood samples within 15 minutes and assay on YSI in duplicate within 15 minutes of draw.
- Data Pairing: Pair sensor values with reference values by selecting the sensor value closest in time to the blood draw (maximum 5 minutes before or after).
Analysis:
- Calculate MARD for overall performance and by glucose ranges
- Determine percentage of values within ±15%/15mg/dL, ±20%/20mg/dL, and ±40%/40mg/dL of reference
- Perform consensus error grid analysis
- Quantify sensor lag using linear regression of sensor-reference difference versus rate of change
Protocol for Sensor Delay Characterization
Objective: To quantify the temporal delay characteristics of factory-calibrated CGM sensors and identify patterns related to glucose dynamics.
Materials:
- CGM systems with high-temporal-resolution data output (minute-by-minute)
- Reference glucose analyzer with minimal inherent delay
- Computational resources for time-series analysis
- Data synchronization equipment
Procedure:
- Experimental Setup: Establish precise time synchronization between CGM systems and reference analyzers.
- Data Collection: Conduct controlled glucose excursions with frequent reference measurements (every 5 minutes or more frequently during dynamic periods).
- Signal Processing: Apply smoothing algorithms to reduce high-frequency noise without introducing phase shift.
- Cross-Correlation Analysis: Compute cross-correlation function between CGM and reference signals to identify peak correlation lag.
- Regression Analysis: Perform least square linear regression of the difference between sensor and reference values versus the sensor rate of change.
Analysis:
- Calculate mean lag time from regression slope
- Determine lag variability across different rate-of-change conditions
- Model relationship between glucose dynamics and temporal delay
- Establish confidence intervals for delay parameters
Research Reagent Solutions
Table 4: Essential Research Materials for CGM Delay Compensation Studies
| Item | Specifications | Research Application |
|---|---|---|
| YSI 2300 Stat Plus Analyzer | Dual-sensor biosensor for glucose and lactate | Gold-standard reference method for plasma glucose measurement during sensor validation studies [73] |
| Precision Neo Blood Glucose Test Strips | Electrochemical test strips | Capillary reference measurements, particularly for pediatric populations where venous sampling is challenging [73] |
| CGM-LSM Model Framework | Transformer-decoder architecture pretrained on 1.6M CGM records | Baseline model for glucose prediction tasks and delay compensation algorithm development [74] |
| OhioT1DM Dataset | 12 T1D patients with 58,414 instances | Benchmark dataset for validating sensor performance and delay compensation methods [74] |
| Glycemic Clamping Equipment | IV glucose, insulin, infusion pumps | Controlled manipulation of glucose levels to create dynamic conditions for sensor testing [73] |
FAQ: Understanding and Quantifying CGM Time Delay
What is the source of the inherent time delay in Continuous Glucose Monitoring (CGM) systems? The time delay, often termed "lag time," in CGM readings is a result of a combination of physiological and technological factors [25]. Physiologically, CGM sensors measure glucose in the interstitial fluid (ISF), not directly in the blood. The process of glucose moving from the bloodstream, across capillary walls, and through the interstitial space to the sensor creates a physiological time delay, typically estimated to be between 5 to 10 minutes [25] [10]. Technologically, additional delays are introduced by the sensor's response time as glucose diffuses through its protective membranes, and by the mathematical filtering and data smoothing algorithms used to reduce signal noise, which can add several more minutes [25].
What is the typical total time delay observed in CGM systems? Reported overall time delays between CGM readings and blood glucose measurements can vary considerably, with a range of 5 to 40 minutes cited in the literature [25]. A study analyzing a prototype CGM sensor found an overall mean time delay of 9.5 minutes (with a standard deviation of 3.7 minutes and a median of 9 minutes) for raw sensor signals [25]. It is important to note that this delay can vary between individuals and even within the same individual over time [25].
How does time delay impact the measured accuracy of a CGM system? Time delay is a major contributor to the observed differences between CGM readings and simultaneous self-monitoring of blood glucose (SMBG) measurements, especially during periods of rapid glucose change [25]. Even if a CGM system had perfect analytical accuracy (zero error), the time delay alone would cause a discrepancy. One analysis demonstrated that a 10-minute time shift could account for a calculated MARD (Mean Absolute Relative Difference) of 9.5%, purely due to the lag and not due to measurement inaccuracy [25]. This underscores the necessity to separate the effects of time delay from analytical error when validating sensor performance.
Experimental Protocols for Delay Compensation
Protocol: Quantifying Baseline Sensor Time Delay
Objective: To establish the baseline time delay profile of a CGM sensor for a given individual or cohort, which is a prerequisite for developing and testing any compensation algorithm.
Methodology:
- Participant Preparation: Recruit subjects according to the study's inclusion criteria. Standardize conditions (e.g., fasting state) prior to the glucose challenge.
- Glucose Challenge: Administer a standardized stimulus to induce a rapid glucose excursion. Common methods include a mixed-meal tolerance test or an oral glucose tolerance test (OGTT).
- Reference Blood Glucose Sampling: Collect frequent capillary (fingerstick) or venous blood samples at fixed intervals (e.g., every 5-15 minutes) to establish a high-fidelity reference glucose curve.
- CGM Data Collection: Simultaneously, collect CGM data at its native measurement interval (e.g., every 5 minutes). Ensure timestamps are synchronized between the reference method and the CGM system.
- Data Analysis:
- Time-Alignment: Retrospectively shift the CGM data trace in time relative to the reference blood glucose data.
- Delay Calculation: Calculate the time shift that minimizes the difference (e.g., root mean square error or MARD) between the two datasets. This time shift represents the empirically measured total time delay [25].
- Statistical Summary: Report the mean, median, standard deviation, and interquartile range of the time delays across the study population.
Protocol: Validating Prediction Algorithm Performance
Objective: To test the efficacy of a prediction algorithm in compensating for the inherent CGM time delay and providing glucose estimates that are more consistent with real-time blood glucose.
Methodology:
- Data Set: Utilize a dataset containing paired CGM raw signals/smoothed readings and frequent reference blood glucose measurements, collected as described in Protocol 2.1.
- Algorithm Application: Process the CGM data stream with the candidate prediction algorithm in a way that simulates real-time operation (i.e., only using past and present data points to forecast the current glucose value).
- Performance Comparison:
- Compare the algorithm-compensated CGM readings against the time-synchronized reference blood glucose values.
- Compare the raw (or standard-filtered) CGM readings against the reference blood glucose values.
- Metrics for Validation:
- Primary Metric: Reduction in MARD during periods of rapid glucose change (rates of change > 2 mg/dL/min or similar threshold) [25].
- Secondary Metrics:
- Reduction in the absolute time delay, as quantified by the method in Protocol 2.1.
- Improvement in clinical accuracy on Clarke Error Grid (CEG) or Consensus Error Grid.
- Precision of trend arrow accuracy during glucose excursions.
A study employing a prediction algorithm demonstrated an average reduction in time delay of 4 minutes, showing the potential for such methods to improve real-time consistency with blood glucose [25].
Data Presentation: CGM Time Delay Characteristics
Table 1: Summary of CGM Time Delay Components and Magnitudes
| Delay Component | Description | Reported Typical Range | Key Influencing Factors |
|---|---|---|---|
| Physiological Lag [25] [10] | Delay for glucose to equilibrate from blood to interstitial fluid (ISF). | 5 - 10 minutes | Local blood flow, tissue perfusion, permeability of ISF. |
| Technological Lag [25] | Sensor response time due to diffusion through membranes and enzyme reaction kinetics. | A few minutes | Sensor design, membrane materials. |
| Algorithmic/Filtering Lag [25] | Delay introduced by noise-reduction filters and data smoothing. | 3 - 12 minutes | Filter length and complexity; trade-off between signal stability and delay. |
| Total System Delay [25] | Combined effect of all sources of delay. | 5 - 40 minutes (Study Mean: 9.5 ± 3.7 min) [25] | CGM system generation, individual patient physiology, glycemic rate of change. |
Table 2: Essential Research Reagent Solutions for CGM Delay Compensation Studies
| Reagent / Material | Function in Experiment |
|---|---|
| CGM Systems | The primary device under test. Provides the continuous interstitial glucose signal that requires delay compensation. |
| Blood Glucose Meter & Test Strips | Provides the reference capillary blood glucose measurements for time delay calculation and algorithm validation. |
| Continuous Glucose Monitoring (CGM) Data | The foundational dataset for developing and training machine learning models to predict glucose excursions [76]. |
| Standardized Glucose Challenge | A controlled meal (e.g., high-carbohydrate) or drink (e.g., oral glucose solution) to induce a predictable and rapid glucose excursion for testing. |
| Data Analysis Software | Custom or commercial software (e.g., Python, R, MATLAB) for signal processing, implementing prediction algorithms, and statistical analysis. |
Visualization of Core Concepts
CGM Physiological Lag Mechanism
Algorithm Validation Workflow
Technical Support & Troubleshooting Hub
Frequently Asked Questions (FAQs)
Q1: What does a 10% MARD value imply for the clinical reliability of my CGM study data? A MARD (Mean Absolute Relative Difference) of 10% indicates a moderate level of accuracy for a Continuous Glucose Monitoring (CGM) system [67]. While lower MARD values are always preferable, data from a system with a 10% MARD can still be clinically useful for observing glycemic trends and patterns. However, you should exercise caution when interpreting absolute glucose values, especially near the thresholds for hypoglycemia or hyperglycemia. For context, one large empirical study found that test strip lots with a MARD of 6.1% or higher could fail to meet the ISO 15197:2013 acceptance criterion, which requires ≥95% of results to fall within ±15 mg/dL (±15%) of reference values [67].
Q2: My CGM data shows a high MARD. What are the first steps to troubleshoot the experimental setup? A high MARD often originates from non-physiological sources. Begin your investigation with these steps [77] [78]:
- Verify Sensor Placement: Confirm the sensor was inserted in an approved anatomical site (e.g., abdomen or upper arm) according to the manufacturer's instructions. Ensure the skin was properly prepared and that the sensor is not placed in scar tissue or near muscles that could be strained during the experiment.
- Check Calibration Protocol: If using a CGM system that requires calibration, review the timing, frequency, and quality of the capillary blood glucose measurements used for calibration. Using an inaccurate blood glucose meter for calibration will propagate error into the CGM data.
- Review Data Stream Gaps: Inspect the CGM data for significant gaps or dropouts. Signal loss can sometimes lead to inaccurate data upon reconnection.
- Cross-Check with Reference Method: Ensure the timing of the reference blood draws (e.g., for YSI or hexokinase method analysis) is precisely synchronized with the CGM's timestamp for the corresponding glucose value [67].
Q3: How can I determine if a high MARD is due to sensor error or a true physiological delay? Distinguishing between sensor error and physiological delay requires analyzing the Error Grid [67].
- Sensor Error: This typically appears as random scatter across the error grid, with points falling in clinically significant error zones (e.g., zones C, D, or E). A high MARD coupled with this pattern suggests the sensor itself is malfunctioning or improperly placed.
- Physiological Delay (Sensor Lag): This manifests as a consistent, predictable bias in the CGM data compared to the reference. The CGM values will "lag" behind the plasma glucose values, particularly during periods of rapid glucose change (e.g., after a meal or insulin administration). This creates a characteristic pattern on a time-series plot. Research into delay compensation algorithms often focuses on correcting for this specific type of error [19].
Q4: What are the key requirements for a reference method when calculating MARD in a clinical study? The reference method must be a validated laboratory instrument, such as a glucose oxidase (GOD) or hexokinase (HK) based plasma glucose analyzer (e.g., YSI 2300 STAT Plus or Cobas series analyzers) [67]. Key requirements include:
- Precision: The drift between consecutive duplicate reference measurements must not exceed 4 mg/dL (0.22 mmol/L) at glucose concentrations <100 mg/dL and 4% at concentrations ≥100 mg/dL [67].
- Synchronization: Blood samples for the reference method must be drawn at times precisely corresponding to the CGM glucose values being compared.
- Duplicate Measurements: Each sample should be measured in duplicate to ensure result stability and reliability [67].
Q5: Are there specific subject populations or conditions that can artificially inflate MARD? Yes, several factors can impact MARD [67]:
- Extreme Hematocrit Levels: Subjects with anemia or polycythemia can experience inaccurate sensor readings.
- Hypoperfusion: Poor local blood flow at the sensor site, which can be caused by shock, dehydration, or certain medications like vasopressors, impedes the sensor's ability to measure interstitial glucose accurately.
- Tissue Trauma: Insertion-related bleeding or significant skin irritation can affect the sensor's microenvironment.
- Interfering Substances: The presence of certain medications, such as acetaminophen or ascorbic acid, can interfere with the sensor's chemistry and cause false readings. Always screen participants for such substances [67].
Troubleshooting Guides
Issue 1: Consistently High MARD Across Multiple Study Subjects
| Symptom | Possible Root Cause | Diagnostic Steps | Resolution |
|---|---|---|---|
| MARD consistently >10% across most participants [67]. | Faulty Sensor Lot: A batch-specific manufacturing defect. | Compare MARD from different sensor lots used in the study. | Quarantine the suspect lot and contact the manufacturer for a replacement. |
| Incorrect Reference Method: Issues with the lab analyzer or protocol [67]. | Audit the lab's QC logs and procedure for sample handling and analysis. | Re-train staff on reference method protocols; re-verify analyzer calibration. | |
| Systemic Protocol Error: e.g., consistent mistiming between CGM and reference blood draws. | Review study logs for sample collection timing. | Implement stricter synchronization protocols and use time-stamped data collection systems. |
Issue 2: High MARD in a Single Subject
| Symptom | Possible Root Cause | Diagnostic Steps | Resolution |
|---|---|---|---|
| A single subject's MARD is a statistical outlier from the study cohort. | Poor Sensor-Skin Contact or improper insertion. | Review subject records for notes on insertion or sensor adhesion issues. | For future studies, document insertion quality and skin condition. Exclude the data if a failure is confirmed. |
| - High MARD coupled with rapid glucose fluctuations. | Physiological State: Low perfusion, high skin temperature, or local tissue trauma [19]. | Check for subject conditions like dehydration or localized infection at the site. | Ensure subjects are well-hydrated and screen for contraindications prior to sensor placement. |
| - Data shows consistent lag, not random error. | Uncompensated Sensor Delay: The physiological lag between plasma and interstitial glucose is pronounced [19]. | Plot CGM vs. reference data over time to identify a consistent lag pattern. | Apply a sensor delay compensation algorithm in your data post-processing pipeline [19]. |
Issue 3: Excessive Data Gaps in CGM Recordings
| Symptom | Possible Root Cause | Diagnostic Steps | Resolution |
|---|---|---|---|
| The CGM data stream has frequent and long interruptions. | Signal Transmission Failure: The transmitter cannot communicate with the receiver/recorder. | Check the distance and obstacles between the sensor and receiver. | Ensure the receiver is kept within the manufacturer's specified range. |
| Sensor Failure: The sensor has prematurely stopped functioning. | Note the sensor's lifetime; check for error messages in the data log. | Report the failure to the manufacturer and replace the sensor. | |
| Participant Non-Compliance: The subject is not wearing the receiver or is disabling connectivity. | Interview the subject about their compliance with the study protocol. | Improve subject education on the importance of continuous data recording. |
| MARD Value (%) | Likelihood of Fulfilling ISO 15197 Criterion A (≥95% within ±15 mg/dL or ±15%) | Number of Test Strip Lots (in study sample) | Key Empirical Findings |
|---|---|---|---|
| ≤ 3.0 | Very High | Data Not Specified | Highest probability of passing ISO standards. |
| 3.1 - 6.0 | High | Data Not Specified | Most lots in this range fulfilled the criterion. |
| 6.1 - 7.0 | Uncertainty / Threshold Range | 3.6% of lots in this range failed | The lowest MARD for a failing lot was 6.1%. This is a critical threshold for reliability. |
| > 7.0 | Low | Increasing failure rate | MARD results in the study ranged up to 20.5%. |
| Performance Metric | Result Range | Comments |
|---|---|---|
| MARD | 2.3% to 20.5% | Demonstrates the wide variability in accuracy across different systems and lots. |
| Bias (for lots meeting ISO criteria) | -10.3% to +7.4% | Indicates that even systems passing the standard can have significant systematic error. |
| 95% Limits of Agreement (LoA) Half-Width (for lots meeting ISO criteria) | 4.8% to 24.0% | Highlights the substantial imprecision that can exist within a system that is deemed "acceptably accurate" overall. |
| Reference Methods Used | Glucose Oxidase (GOD), Hexokinase (HK) | Studies used laboratory-grade analyzers (e.g., YSI 2300 STAT Plus, Cobas Integra) as reference [67]. |
Experimental Protocol: Assessing CGM Accuracy vs. Reference Method
Aim: To determine the MARD and ISO 15197:2013 compliance of a Continuous Glucose Monitoring (CGM) system in a clinical research setting.
Methodology:
- Subject Recruitment & Ethics: Recruit adult subjects (with diabetes or without) under a protocol approved by an Institutional Review Board (IRB). Obtain written informed consent from all participants [67].
- Sample Collection: Capillary or venous blood samples are drawn from subjects to obtain a wide distribution of glucose concentrations as specified by ISO 15197 (covering hypoglycemic, normoglycemic, and hyperglycemic ranges) [67].
- CGM Measurement: The CGM system under investigation is worn by the subject according to the manufacturer's instructions. Glucose values are recorded at the time of each reference blood draw.
- Reference Measurement: Each blood sample is analyzed in duplicate using a validated laboratory comparison method (e.g., YSI 2300 STAT Plus glucose analyzer with Glucose Oxidase method or a Cobas analyzer with Hexokinase method) [67]. The mean of the two duplicate results is used as the reference value. Sample stability is verified by ensuring the drift between consecutive duplicates does not exceed 4 mg/dL (0.22 mmol/L) for values <100 mg/dL or 4% for values ≥100 mg/dL [67].
- Data Analysis:
- MARD Calculation: For each paired measurement (CGM value and reference value), calculate the Absolute Relative Difference (ARD):
|(CGM value - Reference value) / Reference value| * 100%. The MARD is the mean of all ARDs [67]. - ISO 15197:2013 Analysis: Calculate the percentage of CGM results that fall within ±15 mg/dL of the reference value for concentrations <100 mg/dL and within ±15% for concentrations ≥100 mg/dL (Criterion A). Criterion B requires ≥99% of results to lie in zones A and B of the Consensus Error Grid (CEG) [67].
- MARD Calculation: For each paired measurement (CGM value and reference value), calculate the Absolute Relative Difference (ARD):
Workflow & System Diagrams
CGM Accuracy Assessment Workflow
Sensor Delay Compensation Logic
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for CGM Accuracy Research
| Item | Function in Research | Example Product / Model |
|---|---|---|
| Laboratory Glucose Analyzer | Provides the high-precision reference measurement against which the CGM is compared. Considered the "gold standard." | YSI 2300 STAT Plus (Glucose Oxidase method), Cobas Integra 400 plus (Hexokinase method) [67]. |
| CGM Systems Under Test | The devices being evaluated for their accuracy and clinical performance. | Various commercial and research-grade CGM systems (e.g., Eversense CGM system cited in recent literature) [19]. |
| Consensus Error Grid (CEG) | A clinical tool for assessing the clinical significance of the differences between the CGM and reference values. Categorizes errors into zones from A (no effect) to E (dangerous) [67]. | Standardized tool available in clinical chemistry and diabetes research publications. |
| Data Analysis Software | For statistical calculation of MARD, bias, ISO 15197 compliance, and creation of Bland-Altman plots. | R, Python (with Pandas/NumPy/Matplotlib), SPSS, or other statistical software packages. |
| AI/ML Modeling Tools | Used to develop and test sensor delay compensation algorithms and predictive models for glucose dynamics [19]. | Python with TensorFlow/PyTorch for deep learning models (e.g., DNNs, Explainable AI). |
Experimental Accuracy & Performance Benchmarking
This section provides a head-to-head comparison of sensor performance based on a recent clinical study, summarizing key quantitative metrics for researchers.
The following table summarizes the Mean Absolute Relative Difference (MARD) for each CGM system against different reference methods. A lower MARD indicates higher accuracy [79] [80].
Table 1: Overall MARD (%) by Comparator Method [80]
| CGM System | YSI 2300 (Lab) | Cobas Integra (Lab) | Contour Next (Capillary) |
|---|---|---|---|
| FreeStyle Libre 3 | 11.6% | 9.5% | 9.7% |
| Dexcom G7 | 12.0% | 9.9% | 10.1% |
| Medtronic Simplera | 11.6% | 13.9% | 16.6% |
Contextual Performance Across Glucose Ranges
Sensor performance varies significantly across different glycemic ranges. The table below highlights the relative strengths of each device in specific clinical scenarios.
Table 2: Performance Across Glycemic Ranges and Scenarios [79]
| Performance Scenario | FreeStyle Libre 3 | Dexcom G7 | Medtronic Simplera |
|---|---|---|---|
| Normo-/Hyperglycemia | Best Performance | Best Performance | Good Performance |
| Hypoglycemia | Good Performance | Good Performance | Best Performance |
| Rapid Glucose Rise | Steady Performance | Steady Performance | Struggled |
| Rapid Glucose Drop | Good Performance | Good Performance | Better Performance |
| First-Day Accuracy | Most Stable (MARD ~10.9%) | Slightly Higher MARD (~12.8%) | Least Reliable (MARD ~20.0%) |
Alert Performance
For closed-loop systems or alarm-based interventions, detection reliability is critical.
Table 3: Hypo- and Hyperglycemia Alert Performance [79]
| CGM System | Hypoglycemia Detection Rate | Hyperglycemia Detection Rate |
|---|---|---|
| FreeStyle Libre 3 | 73% | ~99% |
| Dexcom G7 | 80% | ~99% |
| Medtronic Simplera | 93% | 85% |
Detailed Experimental Protocols for CGM Performance Evaluation
This section outlines the core methodology from the cited head-to-head comparison study, providing a template for rigorous CGM benchmarking.
Core Study Design & Participant Profile
The foundational study was a prospective, interventional trial conducted with the following parameters [80]:
- Objective: Head-to-head performance evaluation of three factory-calibrated CGM systems.
- Participants: 24 adults with type 1 diabetes mellitus.
- Exclusion Criteria: Severe hypoglycemia in the prior 6 months, hypoglycemia unawareness, HbA1c >10%, and intake of substances known to interfere with CGM performance.
- Sensor Wear: Each participant wore one sensor of each system (Dexcom G7, FreeStyle Libre 3, Medtronic Simplera) simultaneously on the upper arms for 15 days.
- Sensor Replacement Protocol: Sensors were replaced according to their intended wear life to ensure data covered the full operational period [79]:
- FreeStyle Libre 3: Worn for the full 14-day lifespan.
- Dexcom G7: Replaced on day 5 (10.5-day nominal wear).
- Medtronic Simplera: Replaced on day 8 (7-day nominal wear).
Glucose Manipulation & Data Collection Procedure
The study included a structured glucose manipulation procedure to test sensor performance under dynamic conditions, a critical consideration for delay research [80].
- Frequent Sampling Periods (FSPs): Three 7-hour in-clinic sessions were conducted on days 2, 5, and 15.
- Comparator Measurements: During each FSP, reference blood glucose levels were measured every 15 minutes using three different methods:
- YSI 2300 STAT PLUS: Laboratory analyzer (glucose oxidase-based).
- COBAS INTEGRA 400 plus: Laboratory analyzer (hexokinase-based).
- Contour Next: Capillary blood glucose meter.
- Glucose Excursion Protocol: A controlled manipulation was performed to induce specific glycemic states and ensure a clinically relevant distribution of comparator data [80]:
- Hyperglycemia: Participants consumed a carbohydrate-rich breakfast followed by a delayed insulin bolus.
- Hypoglycemia & Rapid Changes: Insulin was used to induce a decline in glucose, accompanied by mild exercise if needed.
- Stabilization: Finally, glucose levels were stabilized in the normoglycemic range.
- Free-Living Data: Outside of FSPs, participants followed their daily routines and performed at least seven capillary BG measurements per day.
Data Analysis & Accuracy Metrics
The following primary metrics were used to evaluate performance [80]:
- Point Accuracy:
- MARD: Mean Absolute Relative Difference, calculated as |CGM - Reference| / Reference.
- Bias: Mean Relative Difference.
- Agreement Rate (AR): Percentage of CGM readings within ±20 mg/dL (±1.1 mmol/L) of reference for values <100 mg/dL (5.6 mmol/L) or within ±20% for values ≥100 mg/dL (5.6 mmol/L).
- Clinical Accuracy: Assessed using the Diabetes Technology Society Error Grid.
- Alert Reliability:
- True Alert Rate: Percentage of CGM readings outside a threshold concurrent with a reference value outside the same threshold.
- True Detection Rate: Percentage of reference measurements outside a threshold concurrent with a CGM reading outside the same threshold.
Diagram 1: Experimental workflow for CGM performance evaluation, based on Eichenlaub et al. (2025).
The Scientist's Toolkit: Key Research Reagents & Materials
Table 4: Essential Materials for CGM Performance and Delay Studies
| Item | Function in Research Context |
|---|---|
| YSI 2300 STAT PLUS Analyzer | Considered the gold-standard laboratory reference for blood glucose measurement (glucose oxidase-based method) against which CGM accuracy is benchmarked [80]. |
| COBAS INTEGRA 400 plus Analyzer | Provides an alternative laboratory-grade reference method (hexokinase-based) to assess the impact of different biochemical measurement techniques on performance metrics [80]. |
| Contour Next BGM | Represents a clinical/patient-grade capillary reference, crucial for evaluating CGM performance in conditions mimicking real-world use [80]. |
| CGM Sensors (G7, Libre 3, Simplera) | The devices under test (DUTs). Must be sourced consistently, noting that some manufacturers require disclosure for use in clinical studies [80]. |
| Android-based Smart Device | A standardized data acquisition platform to run all CGM software applications, eliminating variability introduced by different consumer smartphones [80]. |
Troubleshooting Guides & FAQs for CGM Performance Research
This section addresses common technical and methodological challenges in CGM performance and delay research.
FAQ: Understanding Time Delay and Performance
Q1: What are the primary sources of time delay in CGM systems, and how do they impact accuracy metrics like MARD?
Time delay in CGM readings is a composite of physiological and technological factors [25]:
- Physiological Delay (~5-10 minutes): CGM sensors measure glucose in the interstitial fluid (ISF), not blood. The process of glucose diffusion from capillaries to the ISF creates a natural lag behind blood glucose levels [25] [81].
- Technological Delay (Varies by device): This includes sensor response time, signal filtering, and data processing within the CGM system. Advanced filters reduce signal noise but can introduce an algorithmic delay [25].
This combined delay significantly impacts MARD, especially during periods of rapid glucose change. A perfect sensor with only a physiological delay would still show a high MARD if not temporally aligned with reference measurements [25].
Q2: In a head-to-head study, why did the Medtronic Simplera sensor show a significantly higher MARD against the Contour Next meter compared to the lab references?
This discrepancy suggests the sensor's performance may be more variable in real-world, capillary blood-like conditions or could be influenced by specific characteristics of the comparator method (e.g., enzymatic approach). For research, this highlights the critical importance of stating the reference method used when reporting MARD values, as they are not directly comparable across different studies [80].
Q3: Which CGM system is most accurate for researching hypoglycemia detection algorithms?
Based on the presented data, the Medtronic Simplera demonstrated a superior hypoglycemia detection rate (93%) compared to Dexcom G7 (80%) and FreeStyle Libre 3 (73%) in the cited study. Its performance in the low glucose range was also a noted strength [79]. However, researchers must weigh this against its lower performance in hyperglycemia and higher initial MARD on day one.
Troubleshooting Common Experimental Challenges
Challenge 1: High MARD and poor agreement during rapid glucose excursions.
- Potential Cause: The intrinsic time delay of the CGM system is causing a misalignment with point-of-reference measurements.
- Solution:
- Post-hoc time alignment: In offline analysis, shift the CGM data forward in time to find the optimal lag that minimizes MARD. This helps isolate the sensor's analytical error from the time delay error [25] [81].
- Use a dynamic glucose testing protocol: Ensure your study design includes controlled periods of rising and falling glucose to properly characterize this effect [80].
Challenge 2: Inconsistent performance results between different laboratory reference analyzers.
- Potential Cause: Different analytical methods (e.g., glucose oxidase in YSI vs. hexokinase in Cobas) and sample matrices (venous vs. capillary) can yield systematically different results.
- Solution: Report performance metrics against all reference methods used. The YSI analyzer is often considered the gold standard for CGM studies. Using multiple references provides a more comprehensive view of sensor performance [80].
Challenge 3: Sensor failures or data dropouts compromising dataset integrity.
- Potential Cause: Physical sensor issues, signal loss, or connectivity problems.
- Solution:
Diagram 2: Logical troubleshooting guide for common CGM research challenges.
Technical Support Center: Troubleshooting Guides and FAQs
This technical support center provides troubleshooting guidance and methodologies for researchers integrating Artificial Intelligence (AI) and Real-World Evidence (RWE) into the validation of Continuous Glucose Monitoring (CGM) sensor delay compensation algorithms.
Frequently Asked Questions (FAQs)
Q1: What are the key regulatory differences between the FDA and EMA for validating AI-driven CGM tools? The US Food and Drug Administration (FDA) and European Medicines Agency (EMA) exhibit distinct regulatory philosophies. The FDA typically employs a flexible, dialog-driven model that encourages innovation via individualized assessment but can create regulatory uncertainty. In contrast, the EMA has established a structured, risk-tiered approach through its 2024 Reflection Paper, which provides more predictable paths to market but may slow early-stage AI adoption. For CGM applications, this means your validation strategy should be adaptable for the FDA and meticulously pre-planned with clear documentation for the EMA [82].
Q2: How can I assess if my Real-World Data (RWD) is fit-for-purpose to train a delay compensation model? Ensuring RWD quality is foundational. Regulatory agencies focus on data accuracy, completeness, reliability, and representativeness. Key steps include:
- Define "Completeness": Specify whether this refers to data granularity or the amount of missing data, as regulatory interpretations can differ [83].
- Understand Data-Generating Processes: Deep knowledge of how your CGM data was collected (e.g., clinical setting, patient-use setting) is critical for assessing potential biases [83].
- Evaluate Representativeness: Verify that the training data reflects the demographic and clinical characteristics of the intended use population to avoid algorithmic bias [82].
Q3: My AI model is a "black box." How can I address regulatory concerns about transparency and explainability? The EMA explicitly acknowledges the utility of complex models but mandates the use of explainability metrics and thorough documentation of model architecture and performance. Strategies include:
- Employ Explainable AI (XAI) techniques to interpret model outputs and identify which input features (e.g., past glucose values, time of day) most influenced a prediction [82] [19].
- Provide comprehensive documentation covering the model's objective, architecture, training data, and limitations [82] [84].
- For high-impact applications, engage with regulators early through the FDA's Complex Innovative Trial Design (CID) Program or the EMA's Innovation Task Force [82] [84].
Q4: What are the ethical considerations when using AI and RWE for vulnerable populations? Principles of ethical, equitable, and non-biased use are paramount, requiring a "watchful human eye" [83]. Key considerations are:
- Bias and Representation: Actively mitigate the risk of algorithmic bias, especially if training data underrepresents certain demographic or clinical subgroups [82] [84].
- Patient-Centeredness: Ensure the technology and its outcomes align with patient needs and respect human dignity, a core principle of the Clinical Evidence 2030 vision [83].
- Data Privacy and Security: Implement robust data de-identification and governance frameworks to protect sensitive patient health information [84].
Troubleshooting Experimental Protocols
Issue 1: Poor Generalization of AI Model to New Patient Cohorts
This indicates potential overfitting or bias in your training dataset.
- Step 1: Understand the Problem. Reproduce the performance drop using a held-out validation cohort from a different clinical site or demographic profile.
- Step 2: Isolate the Issue.
- Check Data Representativeness: Compare the demographic and clinical characteristics (e.g., age, BMI, diabetes etiology) of the training and new cohorts. A significant mismatch is a likely cause [82].
- Analyze Feature Importance: Use XAI methods to see if the model is relying on spurious correlations specific to the training set.
- Simplify the Problem: Test model performance on a subset of the new data with characteristics most similar to the training set.
- Step 3: Find a Fix or Workaround.
- Solution: Incorporate more diverse RWD into the training process or use data augmentation techniques.
- Workaround: Develop a model calibration step that adjusts predictions based on the characteristics of the new cohort.
- Document and Escalate: Document this finding and its resolution. Consider refining patient inclusion criteria for future data collection.
Issue 2: Inconsistent Regulatory Feedback on Validation Benchmarks
Lack of harmonized international standards can lead to conflicting requirements.
- Step 1: Understand the Problem. Carefully review feedback from different regulatory bodies to identify specific, conflicting points (e.g., required performance metrics, statistical significance levels).
- Step 2: Isolate the Issue.
- Engage Early: Use regulatory pathways like the FDA's CID program or Scientific Advice procedures with the EMA to clarify expectations before submission [82] [84].
- Compare to Working Examples: Research validated AI tools in similar fields (e.g., digital pathology AI models) to understand accepted validation frameworks [84].
- Step 3: Find a Fix or Workaround.
- Solution: Develop a validation plan that meets the strictest regulatory requirement from the outset.
- Workaround: Propose a phased validation strategy, where initial approval is based on core metrics, with post-market surveillance and RWE generation planned for continuous model validation [82].
- Fix for the Future: Advocate for and contribute to international harmonization efforts, such as those led by the ICH [83].
Experimental Methodology for CGM Sensor Delay Compensation
Protocol: Validating an AI-Driven Delay Compensation Algorithm Using RWE
1. Objective: To develop and validate a deep learning model that compensates for physiological time lags in interstitial glucose measurements using continuous glucose monitoring (CGM) data and real-world contextual information.
2. Principles and Technologies:
- CGM Technology: Provides real-time, dynamic glucose readings, forming the primary data stream [19].
- AI/Deep Learning: Analyzes complex CGM data streams to identify patterns and predict current plasma glucose based on interstitial glucose readings and other inputs [19].
- Real-World Evidence (RWE): Clinical evidence derived from Real-World Data (RWD) about the usage and potential benefits/risks of the algorithm [84] [83].
3. Workflow and Signaling Pathway
The following diagram illustrates the experimental workflow for developing and validating the AI-driven sensor delay compensation model.
4. Key Research Reagent Solutions
Table 1: Essential Materials and Tools for CGM-AI Research
| Item | Function in Research |
|---|---|
| Continuous Glucose Monitor (CGM) | Provides the core real-time, dynamic glucose data stream from the interstitial fluid [19]. |
| Reference Blood Glucose Meter | Serves as the ground truth (e.g., capillary blood glucose) for training and validating the AI model against a proven standard [19]. |
| Structured RWD Sources | Electronic Health Records (EHRs), claims data, or patient registries provide real-world context to understand data-generating processes and patient journeys [84] [83]. |
| AI/ML Development Platform | A software environment (e.g., Python with TensorFlow/PyTorch) for building, training, and testing deep learning models for glucose prediction [19]. |
| Explainable AI (XAI) Toolkit | Software libraries used to interpret the AI model's decisions, increasing transparency and addressing regulatory concerns about "black box" models [82] [19]. |
5. Quantitative Performance Evaluation
Table 2: Key Quantitative Metrics for Algorithm Validation
| Metric | Target Benchmark | Evaluation Context |
|---|---|---|
| Mean Absolute Error (MAE) | < 10 mg/dL | Overall accuracy of compensated glucose values against reference. |
| Root Mean Square Error (RMSE) | < 15 mg/dL | Penalizes larger errors more heavily, key for hypoglycemia prediction. |
| * Clarke Error Grid Analysis (Zone A)* | > 95% | Measures clinical accuracy; Zone A represents clinically accurate predictions. |
| Time Gain (in minutes) | > 3-minute improvement vs. uncompensated signal | Quantifies the reduction in sensor delay achieved by the algorithm. |
| MARD (Mean Absolute Relative Difference) | < 10% | Standard metric for CGM system accuracy post-compensation. |
6. Regulatory and Validation Framework Integration
The final phase involves aligning the developed methodology with regulatory frameworks. The following diagram outlines the core logical relationship between the key components of a successful validation paradigm.
Conclusion
Compensating for CGM sensor delay requires a multifaceted approach that integrates physiological understanding with advanced computational techniques. The evidence confirms that while physiological delays of 5-15 minutes are inherent, methodological innovations in algorithm design—from Kalman filtering to sophisticated neural networks like SCINet—can effectively mitigate their impact. The establishment of a 10% MARD threshold provides a clear benchmark for sensor accuracy sufficient for non-adjunct use in therapy development. Future directions should focus on developing standardized validation frameworks that reflect real-world glycemic variability, advancing personalized compensation algorithms through AI and machine learning, and creating integrated systems that leverage multi-analyte monitoring for enhanced accuracy. For researchers and drug developers, these advancements promise more reliable biomarkers for clinical trials, improved assessment of metabolic therapeutics, and ultimately, better tools for preventing diabetes progression through early intervention strategies.
References
- 1. Expanding the horizon of continuous glucose monitoring ... [https://www.nature.com/articles/s41390-024-03573-x]
- 2. Clinical performance evaluation of the SiJoy GS1 continuous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245700/]
- 3. A deep learning framework for virtual continuous glucose ... [https://www.nature.com/articles/s41598-025-01367-7]
- 4. Time Lag of Glucose From Intravascular to Interstitial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3837059/]
- 5. Modeling Plasma-to-Interstitium Glucose Kinetics from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4649763/]
- 6. Estimating Plasma Glucose from Interstitial ... [https://www.mdpi.com/1424-8220/10/12/10936]
- 7. Discordance Between Glucose Levels Measured in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8525890/]
- 8. Leveraging continuous glucose monitoring for ... [https://www.nature.com/articles/s41598-024-58703-6]
- 9. Glucose Tolerance Test - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK532915/]
- 10. Lag Time [https://www.adces.org/education/danatech/glucose-monitoring/continuous-glucose-monitors-(cgm)/cgm-101/cgm-glossary/lag-time]
- 11. Clinical performance evaluation of the SiJoy GS1 ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1536292/full]
- 12. Revolutionizing Hypoglycemia Management in Long-Term ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12536920/]
- 13. Diabetes at the RCH : Continuous glucose monitoring issues [https://www.rch.org.au/diabetes/diabetes-help/Continuous_glucose_monitoring_issues/]
- 14. Making sense of sensors: Evaluating CGM devices for safe ... [https://diabetesonthenet.com/journal-diabetes-nursing/evaluating-cgm-devices/]
- 15. When Glucose Monitors Fail: The Hidden Dangers for ... [https://www.forthepeople.com/blog/when-glucose-monitors-fail-hidden-dangers-diabetics/]
- 16. CGM User, Device Errors Pharmacists Should Understand [https://www.drugtopics.com/view/cgm-user-device-errors-pharmacists-should-understand-apha-2025]
- 17. Continuous Glucose Monitoring—New Diagnostic Tool in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11674695/]
- 18. Deconstructing interindividual variability in energy ... [https://pubmed.ncbi.nlm.nih.gov/37315156/]
- 19. Continuous glucose monitoring combined with artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12146165/]
- 20. Intra-individual variation of basal metabolic rate and the ... [https://pubmed.ncbi.nlm.nih.gov/12908903/]
- 21. Troubleshooting Dexcom G7 CGM System [https://www.dexcom.com/en-us/faqs/g7/troubleshooting]
- 22. Troubleshooting Guide | Support | FreeStyle Libre | Abbott [https://www.freestyle.abbott/uk-en/support/tutorialsanddownloads/troubleshooting-guide.html]
- 23. Troubleshooting Dexcom G6 CGM System [https://www.dexcom.com/en-us/faqs/g6/troubleshooting]
- 24. Dexcom CGM Sensor Full Guide [https://notjustapatch.com/dexcom-cgm-sensor-full-guide/?srsltid=AfmBOopf86Pc7SBJkGHfmFxjeRaQGZrT__jgr-MbrYLaCLto837T1qrH]
- 25. Time Delay of CGM Sensors: Relevance, Causes, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4667340/]
- 26. Adaptive Kalman filtering for real-time mapping of the visual field [https://pmc.ncbi.nlm.nih.gov/articles/PMC3862081/]
- 27. Glucose Sensor Accuracy Optimization - XRAY - GreyB [https://xray.greyb.com/glucose-monitoring/improving-sensor-accuracy-and-precision]
- 28. Long-term drift behavior in metal oxide gas sensor arrays [https://www.nature.com/articles/s41597-025-05993-8]
- 29. Real-Time Correction and Long-Term Drift Compensation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12471586/]
- 30. A Stress Generation Model for Tiny ML Drift Compensation [https://www.mdpi.com/2673-7426/4/2/83]
- 31. Double-Layer Simplified Complex Interval Neural Network ... [https://www.mdpi.com/2079-6374/15/11/707]
- 32. A multimodal deep learning architecture for predicting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12307872/]
- 33. Development of sensor system and data analytic ... [https://www.nature.com/articles/s41598-024-59744-7]
- 34. Non-Invasive Glucose Monitoring Using Optical Sensor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8321391/]
- 35. Compression artifact [https://en.wikipedia.org/wiki/Compression_artifact]
- 36. Data-Driven Supervised Compression Artifacts Detection ... [https://pubmed.ncbi.nlm.nih.gov/36085641/]
- 37. Time delay of CGM sensors: Relevance, causes, and ... [https://pure.fh-ooe.at/en/publications/time-delay-of-cgm-sensors-relevance-causes-and-countermeasures]
- 38. Self-Supervised Compression and Artifact Correction for ... [https://arxiv.org/html/2511.13922v1]
- 39. Troubleshooting [https://techdocs.akamai.com/datastream2/v3/docs/troubleshooting]
- 40. Data Stream Troubleshooting Tools FAQ [https://www.cisco.com/c/en/us/support/docs/routers/sd-wan/214662-data-stream-troubleshooting-tools-faq.html]
- 41. Troubleshoot a stream | Datastream [https://docs.cloud.google.com/datastream/docs/troubleshoot-a-stream]
- 42. Inductive Sensors | Fault Repair/FAQ [https://www.pepperl-fuchs.com/en/support/knowledge-and-literature/knowledge-bases-for-industrial-sensors/knowledge-base-for-inductive-sensors/fault-repair-faq-gp28650]
- 43. Sensors Frequently Asked Questions [https://library.automationdirect.com/sensors-frequently-asked-questions-issue-7-2006/]
- 44. Lessons Learned from the Real-World Deployment of Multi ... [https://arxiv.org/html/2508.01599]
- 45. Data transmission delay compensation algorithm for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0317137]
- 46. Context-Aware Adaptive Multipath Compensation Based ... [https://www.cambridge.org/core/journals/journal-of-navigation/article/contextaware-adaptive-multipath-compensation-based-on-channel-pattern-recognition-for-gnss-receivers/728F94F01798BE917D4FF0BC6E7B859E]
- 47. Context-aware Adaptive Visualizations for Critical Decision ... [https://arxiv.org/html/2511.11476v1]
- 48. Continuous Glucose Monitoring: Real-Time Algorithms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2864177/]
- 49. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 50. Evaluation of four machine learning models for signal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10752114/]
- 51. Comparison of the prediction accuracy of machine learning ... [https://www.nature.com/articles/s41598-023-42818-3]
- 52. FAQ | Machine Learning [https://developers.google.com/machine-learning/guides/deep-learning-tuning-playbook/faq]
- 53. Common Issues and Troubleshooting Tips [https://www.dexcom.com/en-gb/blog/troubleshoot-common-dexcom-issues-and-alerts]
- 54. A New Analysis Tool for Continuous Glucose Monitor Data [https://pmc.ncbi.nlm.nih.gov/articles/PMC9631526/]
- 55. Performance Optimization in Machine Learning [https://medium.com/@bingqian/performance-optimization-in-machine-learning-best-practices-and-techniques-996063e74fa7]
- 56. Sensor Readings and Accuracy [https://support.conserv.io/knowledge/sensor-readings-and-accuracy]
- 57. Time Delay of CGM Sensors: Relevance, Causes, and ... [https://pubmed.ncbi.nlm.nih.gov/26243773/]
- 58. Multianalyte Physiological Microanalytical Devices - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9235322/]
- 59. Multi-analyte continuous glucose monitoring [https://patents.google.com/patent/US20190246962A1/en]
- 60. Noise Reduction in Glucose Sensors - XRAY [https://xray.greyb.com/glucose-monitoring/reducing-sensor-noise]
- 61. Machine Learning–Based Calibration and Performance ... [https://www.mdpi.com/1424-8220/25/10/3183]
- 62. Sensor Health and Performance Guide | Troubleshooting [https://www.turtletoughsensors.com/support/troubleshooting/sensor-health-performance-guide]
- 63. A machine learning field calibration method for improving ... [https://www.sciencedirect.com/science/article/abs/pii/S0360132320308246]
- 64. Therapy Adjustments Based on Trend Arrows Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6610609/]
- 65. Using trend arrows in continuous glucose monitoring systems ... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-020-00607-2]
- 66. Mean absolute relative difference [https://en.wikipedia.org/wiki/Mean_absolute_relative_difference]
- 67. Mean Absolute Relative Difference of Blood Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9445334/]
- 68. Clinical Implications of Accuracy Measurements ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5444490/]
- 69. The Need for a Modern Error Grid for Clinical Accuracy of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10899826/]
- 70. Consensus error grid [https://en.wikipedia.org/wiki/Consensus_error_grid]
- 71. Error Grid Analysis - Profil — Clinical trials in diabetes [https://blog.profil.com/blog/error-grid-analysis]
- 72. Consequences of Data Loss on Clinical Decision-Making ... [https://www.i-jmr.org/2024/1/e50849/]
- 73. Accuracy of a 15-day Factory-Calibrated Continuous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11977615/]
- 74. A large sensor foundation model pretrained on continuous ... [https://www.nature.com/articles/s44401-025-00039-y]
- 75. Dexcom leaders address G7 issue claims, CGM coverage ... [https://www.drugdeliverybusiness.com/dexcom-leadership-addresses-g7-issue-claims/]
- 76. Predicting postprandial glucose excursions to personalize ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271334/]
- 77. The Art of Troubleshooting for Customer Support ... [https://www.helpscout.com/helpu/art-of-troubleshooting-support/]
- 78. The complete guide to customer service troubleshooting [https://devrev.ai/blog/customer-service-troubleshooting]
- 79. Dexcom G7 vs FreeStyle Libre 3 vs Medtronic Simplera [https://www.snaq.ai/blog/cgm-accuracy-comparison-2025-dexcom-g7-vs-freestyle-libre-3-vs-medtronic-simplera]
- 80. Performance of Three Continuous Glucose Monitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11795573/]
- 81. A Comparison of Time Delay in Three Continuous Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5951038/]
- 82. The future of AI regulation in drug development: a comparative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598624/]
- 83. Parallel Progress in Artificial Intelligence and Real-World ... [https://globalforum.diaglobal.org/issue/august-2025/parallel-progress-in-artificial-intelligence-and-real-world-evidence-creates-a-new-vision-for-clinical-evidence/]
- 84. AI and RWE: Powering the Future of Oncology [https://premier-research.com/perspectives/ai-and-rwe-powering-the-future-of-oncology/]