Optimizing Subcutaneous Insulin Delivery: Strategies to Prevent Intramuscular Injection and Reduce Absorption Variability in Diabetes Therapy
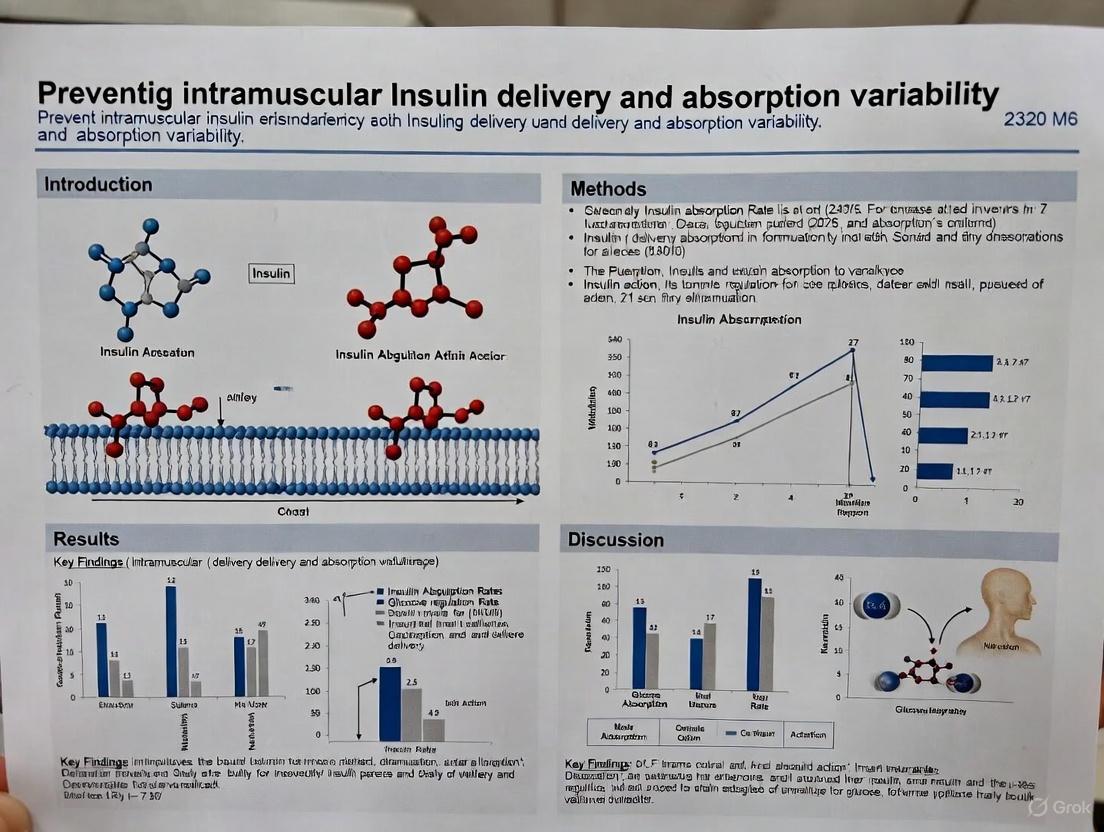
This article provides a comprehensive analysis of the factors contributing to unpredictable insulin absorption, with a specific focus on the risks and consequences of unintentional intramuscular (IM) delivery.
Optimizing Subcutaneous Insulin Delivery: Strategies to Prevent Intramuscular Injection and Reduce Absorption Variability in Diabetes Therapy
Abstract
This article provides a comprehensive analysis of the factors contributing to unpredictable insulin absorption, with a specific focus on the risks and consequences of unintentional intramuscular (IM) delivery. Aimed at researchers, scientists, and drug development professionals, it synthesizes foundational physiology, current injection methodologies, and troubleshooting strategies for lipohypertrophy. The content further explores validation techniques using continuous glucose monitoring and comparative analyses of insulin regimens, while also surveying the horizon of emerging technologies, including automated insulin delivery systems and smart injection devices, that promise to mitigate variability and enhance glycemic control.
The Science of Subcutaneous Absorption: Physiology and Pathophysiology of Insulin Variability
Frequently Asked Questions (FAQs)
Q1: Why is understanding skin and subcutaneous tissue thickness critical for intramuscular insulin delivery research?
Accurate understanding of these layers is essential to prevent inadvertent intramuscular (IM) injection, which can lead to unpredictable insulin absorption and affect glycemic control. Research shows that skin thickness (ST) is relatively consistent across populations and injection sites, while subcutaneous adipose layer thickness (SCT) varies significantly with body mass index (BMI), gender, and race. [1] Using a needle longer than the SCT at a given site, especially in lean individuals or certain body areas like the limbs, risks depositing insulin into muscle tissue. This can accelerate absorption into the bloodstream, potentially causing rapid glucose lowering and increasing hypoglycemia risk, thereby introducing significant variability in pharmacokinetic and pharmacodynamic studies. [1]
Q2: What are the key anatomical landmarks and risks associated with different injection sites?
The selection of an injection site must consider the underlying anatomy to avoid neurovascular injury. [2] The following table summarizes common sites:
| Injection Site | Anatomical Landmark Description | Key Neurovascular Structures to Avoid |
|---|---|---|
| Ventrogluteal | Triangle formed by placing the heel of the hand on the greater trochanter, index finger on the anterior superior iliac spine (ASIS), and middle finger along the iliac crest. Inject in the center of the triangle. [2] [3] | Superior and inferior gluteal arteries; Gluteal nerves. Considered the safest gluteal site with the thickest muscle and absence of major nerves. [2] [3] |
| Deltoid | Approximately 2.5 to 5 cm below the acromion process, in the middle of the muscle belly. [2] [3] | Axillary and radial nerves. The safe zone is approximately 7–13 cm below the mid-acromion, midway between the acromion and deltoid tuberosity. [2] |
| Vastus Lateralis | Middle third of the line joining the greater trochanter of the femur and the lateral femoral condyle of the knee. [2] | Femoral nerve and blood vessels. The middle of the muscle is considered safe. [2] |
| Dorsogluteal | Upper outer quadrant of the buttock. [2] | Sciatic nerve. This site is not routinely recommended due to its proximity to the sciatic nerve and major blood vessels, and inconsistent depth of adipose tissue. [2] [3] |
Q3: What experimental methodology is used to precisely measure skin and subcutaneous tissue thickness?
High-resolution ultrasonography is the standard, non-invasive method for obtaining precise measurements of skin thickness (ST) and subcutaneous adipose layer thickness (SCT) in vivo. [1]
Experimental Protocol:
- Subject Preparation: Recruit a diverse cohort of adults (e.g., by BMI, gender, race). Stabilize subjects in a relaxed, supine or sitting position for at least 5 minutes prior to measurement to ensure consistent muscle tone and blood flow.
- Site Selection and Marking: Clearly mark the four standard injection sites (abdomen, arm, thigh, buttock) using anatomical landmarks. Ensure consistency in the exact location measured across all subjects.
- Ultrasound Imaging: Use a high-frequency linear array ultrasound transducer (e.g., ≥10 MHz). Apply a generous amount of water-soluble transmission gel to the mark on the skin to ensure acoustic coupling. Place the transducer perpendicular to the skin surface without compressing the underlying tissues, as compression can artificially reduce SCT measurements.
- Image Capture and Measurement: Capture a static image. On the ultrasound image:
- Skin Thickness (ST): Measure the distance from the skin surface (entry echo) to the entrance of the dermis into the subcutaneous tissue.
- Subcutaneous Tissue Thickness (SCT): Measure the distance from the dermo-hypodermal junction to the surface of the muscle fascia. [1]
- Data Analysis: Perform multiple measurements per site per subject to ensure reliability. Analyze data using multivariate analyses to determine the statistical significance of factors like body site, gender, and BMI.
Q4: My research involves repeated injections in an animal model. What complications should I monitor for?
Common complications from IM injections include pain, bleeding, and inflammation. More serious complications to monitor for include:
- Nerve Injury: Resulting from direct needle trauma or compression from a hematoma. This can cause pain, paresthesia, or paralysis (e.g., foot drop from sciatic nerve injury). [2]
- Abscess Formation: Caused by bacterial introduction due to inadequate aseptic technique, or as a sterile aseptic abscess from insoluble or irritating drugs. [4] [2]
- Tissue Necrosis: Occurs from injecting substances contraindicated for IM administration, such as calcium chloride. [4]
- Intramuscular Hematoma: A particular risk in subjects with thrombocytopenia or coagulation defects. [2] [3]
Troubleshooting Guide
| Problem | Potential Cause | Solution / Preventive Action |
|---|---|---|
| High variability in insulin absorption data | Inadvertent intramuscular injection due to inappropriate needle length for the subject's SCT. | Use ultrasound to measure SCT at the study site. Select a needle length that ensures subcutaneous deposition without risk of IM injection. For most adults, a 4-5 mm needle inserted at 90° minimizes IM risk. [1] |
| Subject reports severe pain or neurological symptoms post-injection | Needle contact with or injury to a peripheral nerve. | Immediately suspend dosing. Perform a neurological assessment. Confirm injection technique and site landmarks. For subsequent injections, switch to a safer site (e.g., ventrogluteal over dorsogluteal) and ensure correct landmark identification. [2] |
| Induration, swelling, or redness at injection site | Sterile abscess from irritating drug formulation or infectious abscess from breached asepsis. | Ensure strict aseptic technique. For irritating drugs, use the Z-track technique to seal the medication in the muscle. Rotate injection sites frequently to prevent lipohypertrophy and allow tissue recovery. [4] [2] [3] |
| Unexpectedly rapid hypoglycemia following insulin administration | Insulin deposited directly into muscle tissue, leading to accelerated absorption. | Review and confirm the needle length and injection technique are appropriate for the subject's SCT. Aspirate before injection (if using the dorsogluteal site) to check for blood, though note this practice is debated for other sites. [1] [3] |
The following tables consolidate key quantitative findings from Gibney et al. (2010) on skin and subcutaneous tissue thickness in adults with diabetes. [1]
Table 1: Mean Skin Thickness (ST) and Subcutaneous Tissue Thickness (SCT) by Injection Site
| Injection Site | Mean Skin Thickness (mm) (± 95% CI) | Mean Subcutaneous Tissue Thickness (mm) (± 95% CI) |
|---|---|---|
| Abdomen | 2.2 (2.1, 2.2) | 13.9 (13.2, 17.7) |
| Arm | 2.2 (2.2, 2.3) | 10.8 (10.2, 11.3) |
| Thigh | 1.9 (1.8, 1.9) | 10.4 (9.8, 10.9) |
| Buttocks | 2.4 (2.4, 2.5) | 15.4 (14.7, 16.2) |
Table 2: Impact of Subject Factors on Tissue Thickness
| Factor | Impact on Skin Thickness (ST) | Impact on Subcutaneous Tissue (SCT) |
|---|---|---|
| Gender (Female vs. Male) | Statistically significant, but small effect. | Females had 5.1 mm greater mean SCT. [1] |
| BMI (Difference of 10 kg/m²) | Accounts for ~0.2 mm variation. [1] | Accounts for ~4.0 mm variation. [1] |
| Race | Statistically significant, but small effect. | Significant factor, with wider variation. [1] |
The Scientist's Toolkit: Key Research Reagents & Materials
| Item | Function in Research |
|---|---|
| High-Frequency Linear Ultrasound | Non-invasive measurement of skin and subcutaneous tissue thickness at designated injection sites with high precision. [1] |
| Anatomical Marking Pen | Precisely marks injection sites based on standardized anatomical landmarks to ensure consistency across measurements and injections. |
| Water-Soluble Ultrasound Gel | Provides acoustic coupling between the ultrasound transducer and the skin, enabling clear image acquisition without compressing the tissue. |
| Fixed-Capacity Insulin Syringes (Various Needle Lengths) | Allows for systematic investigation of how needle length (e.g., 4mm, 5mm, 8mm, 12.7mm) affects injection depth and insulin deposition. |
| Bioassay/Analytical Platform (e.g., ELISA, HPLC) | Measures serum insulin levels and/or glucose kinetics to quantify the pharmacokinetic and pharmacodynamic variability resulting from different injection depths. |
Anatomical and Experimental Visualization
Injection Site Anatomy and Needle Depth
Experimental Workflow for Tissue Measurement
Frequently Asked Questions (FAQs) for Researchers
FAQ 1: What are the primary physiological structures that form a barrier to insulin delivery in the subcutaneous tissue? The subcutaneous tissue is composed of adipose tissue separated by connective tissue septae. The extracellular matrix (ECM) within this connective tissue is the main physiological barrier. The ECM consists of proteins like collagen and elastin, as well as glycosaminoglycans (GAGs). Insulin must navigate this gel-like matrix before reaching the systemic circulation. Furthermore, insulin can bind to ECM proteins like collagen, which may act as temporary tissue reservoirs [5].
FAQ 2: How does the molecular state of insulin influence its absorption pathway? Upon injection, soluble insulin exists in an equilibrium of monomers, dimers, and hexamers. Monomers (6 kDa) and dimers (12 kDa) are small enough to be absorbed directly into the blood capillaries. Larger hexamers (36 kDa) are generally not absorbed into capillaries but can be taken up by the lymphatic system due to its more permeable structure. The absorption process involves the dissociation of injected hexamers into dimers and monomers at the injection site [5].
FAQ 3: How do injection parameters affect the formation and dispersion of a subcutaneous insulin depot? Recent high-resolution imaging studies show that injection parameters significantly influence depot morphology. Higher injection volumes lead to larger, less spherical depots with greater surface area. The formation of tissue "cracks" during injection can direct plume spread along specific pathways, influencing initial drug distribution. Faster initial flow rates, common in autoinjectors, can increase initial depot pressure but do not necessarily change the final shape [6].
FAQ 4: What is the role of the lymphatic system in insulin absorption? The lymphatic system plays a complementary role, particularly for larger insulin molecules or complexes. Lymphatic capillaries, located in a plexus between the dermis and subcutis, have endothelial cells that lack tight junctions, allowing the uptake of larger molecules. The composition of interstitial fluid is similar to plasma but with a much lower protein content, and fluid not recovered by blood venules is absorbed by the lymphatic system [5] [7].
Troubleshooting Common Experimental Challenges
Challenge 1: High Variability in Absorption Pharmacokinetics
- Potential Cause: Injection technique and site selection. Physiological factors such as local blood flow, skin temperature, and exercise can increase subcutaneous blood flow, thereby accelerating absorption.
- Solution: Standardize injection protocols across study subjects. Utilize imaging techniques like synchrotron CT or radiography to visualize and control for depot formation. Ensure consistent injection depth to avoid accidental intramuscular delivery, which has a faster absorption profile [5] [6].
Challenge 2: Unexpectedly Slow or Rapid Insulin Absorption Profile
- Potential Cause: Formulation-excipient interactions in the subcutaneous space. Excipients like phenol and meta-cresol stabilize insulin hexamers in the vial. Upon SC injection, their dispersion away from the depot shifts the equilibrium towards absorbable dimers and monomers. Issues with this dissociation can alter the absorption rate.
- Solution: Characterize the oligomer dissociation kinetics of your insulin formulation under simulated subcutaneous conditions. Consider the isoelectric point of the insulin preparation and its potential binding to ECM components [5].
Quantitative Data on Factors Influencing Insulin Absorption
Table 1: Molecular Oligomers of Insulin and Their Absorption Pathways
| Oligomer State | Molecular Weight | Primary Absorption Pathway | Notes |
|---|---|---|---|
| Monomer | 6 kDa | Blood Capillaries | Readily absorbed into circulation [5] |
| Dimer | 12 kDa | Blood Capillaries | Readily absorbed into circulation [5] |
| Hexamer | 36 kDa | Primarily Lymphatic System | Must dissociate into dimers/monomers for capillary uptake [5] |
Table 2: Impact of Autoinjector Delivery Volume on Depot Morphology (Ex-Vivo Data)
| Injection Volume | Depot Volume (mL) | Aspect Ratio | Sphericity | Surface Area (mm²) |
|---|---|---|---|---|
| 0.5 mL | 0.48 | 2.10 | 0.68 | 340 |
| 1.0 mL | 0.95 | 2.35 | 0.62 | 520 |
| 2.0 mL | 1.89 | 2.92 | 0.49 | 810 |
Data adapted from synchrotron CT analysis of injections into excised pork belly tissue [6].
Detailed Experimental Protocol: Synchrotron Imaging of SC Depot Formation
This protocol details the methodology for visualizing real-time subcutaneous depot formation and diffusion, as utilized in recent studies [6].
1. Objective: To characterize the impact of injection parameters (e.g., volume, flow rate) on the initial formation, morphology, and diffusion of a subcutaneous drug depot.
2. Materials and Reagents:
- Test Formulation: Iodine-based contrast solution (e.g., 30% w.t.) to simulate drug fluid with radiopaque properties.
- Biological Substrate: Excised pork belly tissue, used as a model for human subcutaneous tissue due to its structural similarity.
- Delivery Device: Autoinjectors with varying designed volumes (e.g., 0.5 mL, 1.0 mL, 2.0 mL).
- Imaging Equipment: Synchrotron facility for high-speed, high-resolution imaging.
- Synchrotron Radiography: For real-time 2D visualization of plume growth during injection (temporal resolution: ~1.02 seconds per frame).
- Synchrotron Computed Tomography (CT): For post-injection 3D reconstruction of final depot morphology.
3. Methodology: 1. Sample Preparation: Equilibrate autoinjectors and biological tissue to a standard room temperature (e.g., 20-25°C) to minimize temperature-induced variability. 2. Image Acquisition: - Radiography Setup: Position the autoinjector perpendicular to the tissue surface and the synchrotron X-ray beam. - Injection & Recording: Initiate the autoinjector and simultaneously begin high-speed radiography to capture the dynamic process of fluid ejection, tissue displacement, and plume formation. - Post-injection CT Scan: After needle retraction, perform a CT scan of the tissue sample to obtain a 3D model of the deposited depot. 3. Data Analysis: - Plume Growth Kinematics: From radiography sequences, analyze the rate and direction of plume expansion, noting the formation of tissue cracks. - Depot Morphometry: From CT data, calculate quantitative metrics for the final depot, including volume, surface area, aspect ratio, and sphericity. - Diffusion Analysis: Measure the mean gray value intensity in regions around the depot periphery over time to quantify the diffusion of the contrast solution into the surrounding tissue.
Pathway and Experimental Visualization
Insulin Absorption Pathway
SC Depot Imaging Workflow
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for SC Absorption and Depot Formation Studies
| Item / Reagent | Function in Experiment |
|---|---|
| Iodine Contrast Solution | Simulates the drug formulation, providing radiopacity for high-resolution X-ray imaging with synchrotron CT or radiography [6]. |
| Excised Pork Belly Tissue | Serves as an ex-vivo biological substrate that models the structural properties of human subcutaneous tissue for injection studies [6]. |
| Autoinjector Devices | Provides a standardized, clinically relevant method for administering subcutaneous injections with controlled parameters [6]. |
| Synchrotron Imaging Facility | Enables real-time, high-speed radiography and high-resolution CT imaging to visualize dynamic fluid-structure interactions during and after injection [6]. |
| Recombinant Human Insulin & Analogues | The active pharmaceutical ingredient for pharmacokinetic and pharmacodynamic studies. Includes rapid-, short-, intermediate-, and long-acting types [5]. |
| Stabilizing Excipients (Phenol, meta-cresol, Zinc) | Used in formulations to control insulin oligomerization (shifting equilibrium toward hexamers) and study their dissociation kinetics in the subcutaneous space [5]. |
FAQs: Intramuscular Delivery and Pharmacokinetics
Q1: What are the primary pharmacokinetic consequences of accidental intramuscular (IM) insulin delivery? Accidental IM delivery of insulin significantly alters its pharmacokinetic profile. Uptake from muscle tissue is markedly faster and more variable than from subcutaneous (SC) fat, leading to unpredictable blood glucose levels. This erratic absorption increases the risk of both hyperglycemia and hypoglycemia, compromising treatment safety and efficacy [8] [9]. The variability is further amplified if the muscle is exercised, accelerating uptake even more [8].
Q2: How can researchers ensure subcutaneous deposition in animal or human studies? The most effective strategy is to use the shortest needle possible. For most subjects, including adults and children, 4-mm needles are sufficient to reliably reach the SC tissue while minimizing the risk of IM injection. In very lean subjects, a skinfold lift is recommended, even with short needles. The use of longer needles (≥8 mm) substantially increases the risk of IM deposition and should be avoided [8] [10].
Q3: What is lipohypertrophy (LH) and how does it impact drug absorption? LH is a localized thickening of fatty tissue and a common complication of repeated SC injections, with a prevalence of over 50% in some studies. It is caused by improper injection site rotation and needle reuse. Injecting into LH lesions reduces and delays insulin absorption, increases pharmacokinetic variability, and leads to suboptimal glucose control [8] [9].
Q4: What are the best practices for injection site rotation to prevent tissue complications? A structured rotation schedule is crucial. The recommended practice is to use the same general area (e.g., abdomen) at the same time of day but rotate the exact injection spot within that site. The area should be divided into quadrants or halves, with daily injections administered at least 1-2 cm (about one finger's width) apart. This prevents repeated trauma to the same spot of tissue, reducing the risk of LH [10].
Troubleshooting Guide: Common Injection Technique Errors
| Error | Consequence | Solution |
|---|---|---|
| Using overly long needles [8] [10] | High risk of intramuscular injection, leading to faster, erratic drug uptake. | Switch to 4-mm pen needles for most subjects. Use 5-mm or 6-mm needles only with a skinfold or 45° angle if 4-mm is unavailable [8]. |
| Injecting into Lipohypertrophy (LH) [8] [9] | Unpredictable and reduced drug absorption, leading to poor glycemic control and unexplained glucose fluctuations. | Implement a structured site rotation plan. Visually inspect and palpate sites regularly. Avoid injecting into hardened or lumpy areas [10]. |
| Applying excessive injection force [10] | Increases the risk of depositing the drug intramuscularly. | Train on gentle needle insertion. If a dent is visible on the skin from force, pressure is too high. Consider contoured-needle designs [10]. |
| Reusing pen needles [8] [10] | Increases risk of LH, infection, pain, and bleeding. Compromises sterility and injection accuracy. | Counsel on "one needle, one injection" policy. Ensure an adequate supply of needles is provided to the patient/study subject [10]. |
| Incorrect skinfold technique with short needles [10] | Unnecessary complexity; for most adults, a skinfold is not required with 4-mm or 5-mm needles. | For 4-mm needles, a perpendicular (90°) injection without a skinfold is appropriate for most adults. Reserve skinfolds for very lean subjects and children [8]. |
Experimental Protocols for Investigating Delivery Kinetics
Protocol 1: Ultrasonography for Tissue Depth Measurement
Objective: To determine SC adipose tissue thickness at various injection sites to inform appropriate needle length selection.
- Subject Positioning: Position the subject supine for abdominal and thigh sites, or in a lateral decubitus position for ventrogluteal sites.
- Site Marking: Mark standard injection sites (abdomen, thigh, arm, buttocks) for consistent measurement.
- Imaging: Use a high-frequency linear array ultrasound probe. Apply a generous amount of water-soluble gel to the transducer head.
- Measurement: Place the transducer perpendicular to the skin surface without compressing the tissue. Capture images and measure the distance from the skin surface to the muscle fascia. Take multiple measurements per site.
- Data Analysis: Correlate SC thickness with subject demographics (BMI, sex, age) to identify risk factors for IM injection [8].
Protocol 2: Pharmacokinetic/Pharmacodynamic (PK/PD) Profiling of SC vs. IM Delivery
Objective: To quantitatively compare the absorption and action profiles of a drug delivered via SC and IM routes.
- Study Design: A controlled, crossover study is recommended.
- Dosing: Administer a standardized dose of the drug (e.g., insulin) via both SC and IM routes in the same subject, with an adequate washout period between interventions.
- Blood Sampling: Collect frequent serial blood samples over a period covering the drug's expected duration of action.
- SC Analysis: Measure serum drug concentrations (e.g., insulin levels) to generate PK parameters: Time to maximum concentration (T~max~), Maximum concentration (C~max~), and Area Under the Curve (AUC).
- PD Analysis: For insulin, measure blood glucose levels at the same time points to determine the glucose-lowering effect [8].
- Data Interpretation: Compare PK/PD parameters between SC and IM routes. IM injection is expected to show a significantly shorter T~max~, higher C~max~, and greater variability in both PK and PD measures, especially if the muscle is active [8].
Research Reagent Solutions
| Item | Function/Application |
|---|---|
| 4-mm Pen Needles | The recommended needle length for ensuring consistent subcutaneous deposition and minimizing the risk of intramuscular injection in most subjects, from children to obese adults [8] [9]. |
| High-Frequency Linear Ultrasound | Used to precisely measure skin and subcutaneous tissue thickness at potential injection sites, providing an evidence base for selecting appropriate needle lengths [8] [9]. |
| Contoured-Hub Needles | Pen needles with a redesigned hub that distributes insertion force over a larger area, reducing variability in penetration depth caused by differing application pressures [9]. |
| Vials and Syringes (for control) | Traditional delivery method used as a control in experiments comparing the pharmacokinetic profiles of different delivery systems (e.g., vs. pen devices) [9]. |
Diagrams of Pathways and Workflows
DOT Script for Drug Delivery Pathway
DOT Script for Experimental PK Workflow
Data presented as mean thickness in millimeters (mm) measured via ultrasonography.
| Body Site | BMI Category (kg/m²) | Skin Thickness (mm) | SC Tissue Thickness (mm) |
|---|---|---|---|
| Arm | < 23 | : 1.7 | : 3.6 |
| : 1.5 | : 6.5 | ||
| 23-25 | : 1.9 | : 7.6 | |
| : 1.8 | : 11.1 | ||
| > 25 | : 2.1 | : 12.5 | |
| : 2.1 | : 15.3 | ||
| Thigh | < 23 | : 1.7 | : 4.4 |
| : 1.5 | : 8.5 | ||
| 23-25 | : 1.9 | : 8.2 | |
| : 1.8 | : 13.3 | ||
| > 25 | : 2.1 | : 14.3 | |
| : 2.1 | : 19.2 | ||
| Abdomen | < 23 | : 1.6 | : 5.8 |
| : 1.6 | : 8.1 | ||
| 23-25 | : 1.8 | : 10.3 | |
| : 1.7 | : 13.9 | ||
| > 25 | : 1.9 | : 18.4 | |
| : 1.9 | : 19.1 |
Model-adjusted mean thickness (mm) in a diabetic population. Dermis thickness includes the epidermis.
| Cohort | Group | Abdominal Dermis (mm) | Abdominal Subcutis (mm) | Thigh Dermis (mm) | Thigh Subcutis (mm) |
|---|---|---|---|---|---|
| Children (Pre-pubertal) | Boys | 1.45 | 7.10 | 1.30 | 6.10 |
| Girls | 1.43 | 7.00 | 1.28 | 6.00 | |
| Children (Pubertal) | Boys | 1.89 | 9.25 | 1.60 | 7.78 |
| Girls | 1.83 | 16.70 | 1.57 | 16.70 | |
| Adults | Men | 2.10 | 17.90 | 1.89 | 9.80 |
| Women | 1.99 | 21.30 | 1.65 | 17.70 |
Detailed Experimental Protocols
Objective: To obtain accurate and reproducible measurements of skin and subcutaneous adipose tissue (SAT) thickness at key anatomical sites.
Key Materials and Equipment:
- Ultrasound System: B-mode ultrasound machine with a high-frequency linear array transducer (e.g., 12-17 MHz) for high-resolution imaging [11] [12].
- Coupling Gel: A thick layer of water-soluble gel is used to eliminate compression artifacts by ensuring no direct pressure is applied to the site by the transducer [13] [14].
- Anatomical Markers: For consistent site relocation.
Step-by-Step Workflow:
- Participant Preparation: Position the participant according to the study protocol (e.g., lying down, sitting). Ensure the anatomical site is relaxed and accessible.
- Site Identification and Marking: Identify and mark measurement sites using standardized bony landmarks to reduce inter-subject variability [11]:
- Abdomen: Midway between the umbilicus and the iliac crest.
- Thigh: Mid-section on the anterior thigh between the iliac crest and the top of the patella.
- Arm: Rear upper arm, mid-way between the acromion and olecranon processes.
- Image Acquisition: Apply a generous amount of coupling gel to the marked site. Place the transducer perpendicular to the skin surface without compressing the tissue. Capture a clear cross-sectional image showing the distinct layers: the epidermis/dermis (skin), the hypoechoic subcutaneous adipose tissue, and the underlying muscle fascia [15].
- Thickness Measurement: Using the ultrasound machine's calibrated caliper function:
- Data Recording: Record multiple measurements at each site to calculate a mean value and ensure reliability.
Objective: To evaluate structural changes in the skin and subcutaneous tissue resulting from repeated insulin injections without adequate site rotation.
Key Materials and Equipment:
- Ultrasound System (as described in Protocol 1).
- Skin Biopsy Kit for histological analysis (optional, for deep mechanistic studies).
- Staining Materials: Hematoxylin and Eosin (H&E) for general histology; Congo Red for amyloid detection; antibodies for immunohistochemical analysis (e.g., anti-insulin antibody) [16].
Step-by-Step Workflow:
- Cohort Selection: Recruit insulin-treated patients with and without palpable skin abnormalities (e.g., subcutaneous nodules, induration) at their injection sites [16].
- Site Examination: For each participant, perform ultrasonography on both the abnormal injection site and a contralateral or distant normal, non-injected control site using Protocol 1 [16].
- Image Analysis: Quantify and compare skin thickness and SAT thickness between the normal and affected sites. Note any changes in tissue layering structure and echo brightness [16].
- Histological Confirmation (Optional): In a subset of participants, perform a skin biopsy on the indurated site. Process and stain the tissue sections to identify pathological features such as thickened collagen bundles, amyloid deposits, and the presence of insulin-derived material [16].
Troubleshooting Guides & FAQs
Q1: Our ultrasound measurements of subcutaneous fat thickness are inconsistent. What are the primary sources of error and how can we mitigate them? [13] [15] [14]
- Problem: High variability in repeated measurements.
- Solution:
- Avoid Tissue Compression: This is a critical error. Use a thick layer of US gel as a standoff between the probe and skin to prevent deformation of the compressible fat layer, which can reduce thickness by 25-37% [14].
- Standardize Site Mapping: Use a systematic body mapping approach with precisely defined anatomical landmarks relative to body height to ensure consistency across measurements and studies [13].
- Operator Training: The technique is operator-dependent. Ensure all technicians undergo standardized training to achieve high inter- and intra-observer reliability, with target errors of less than 0.15 mm [13].
Q2: We observe unexplained variability in insulin absorption pharmacokinetics in our pre-clinical models. Could injection site characteristics be a factor? [17] [16] [18]
- Problem: Erratic insulin absorption profiles.
- Solution:
- Confirm SC Placement: Intramuscular injection leads to faster, more variable absorption. Use shorter needles (e.g., 4-5 mm) to minimize this risk [18].
- Screen for Lipohypertrophy: Visually inspect and palpate injection sites. Injecting into areas of lipohypertrophy (LH) significantly impairs and variates insulin absorption. Ensure systematic site rotation in study protocols to prevent LH [8].
- Account for SC Thickness: The inverse relationship between SC tissue thickness and insulin absorption rate is well-established. Stratify subjects or animal models by BMI and measure local SC thickness, as thicker adipose layers are associated with tempered insulin absorption [18].
Q3: How does the participant's posture during an injection study affect the relevance of our skin thickness measurements? [19]
- Problem: Measured skin thickness may not reflect real-world conditions.
- Solution:
- Simulate Actual Injection Conditions: Measure skin and SC thickness with the participant in their typical injection posture (e.g., sitting for abdominal injections). Evidence shows that average abdominal skin thickness measured while sitting (3.3 mm) is significantly greater than when measured lying down (2.2 mm), which could impact the risk of intradermal injection with shorter needles [19].
Pathway and Workflow Visualizations
SC Tissue Variation Factors
Tissue Change Assessment
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application in Research |
|---|---|
| High-Frequency Linear Ultrasound Probe (12-18 MHz) | Provides high-resolution imaging for accurate differentiation of skin, subcutaneous fat, and muscle layers. Essential for precise thickness measurements with technical accuracy as high as 0.1 mm [13] [15] [14]. |
| Agarose/Gelatin-Based Tissue Phantoms | Custom-fabricated phantoms with known layer thicknesses simulate skin, SAT, and muscle. Used to validate ultrasound measurement protocols, test new algorithms for automated boundary detection, and train technicians [14]. |
| Anti-Insulin Antibody (Monoclonal) | Used in immunohistochemical staining of biopsy specimens from injection sites to confirm the presence and localization of insulin-derived amyloid deposits, a key pathological finding in injection site reactions [16]. |
| Congo Red Stain | A histological dye used to detect amyloid deposits in tissue sections. Shows apple-green birefringence under polarized light, confirming the diagnosis of injection-localized amyloidosis [16]. |
| Standardized Site Mapping Chart | A template or digital tool based on relative body distances (e.g., percentages of height) to ensure consistent and reproducible identification of measurement sites across all subjects in a longitudinal study [13]. |
Frequently Asked Questions (FAQs)
Q1: How do formulation excipients like zinc and phenol directly influence insulin oligomerization kinetics? Zinc ions and phenolic compounds (e.g., metacresol) are critical excipients that stabilize the insulin hexamer, significantly altering its dissociation kinetics. Zinc coordinates with HisB10 on insulin dimers to form a toroidal hexamer structure [20]. Phenolic ligands, such as phenol or metacresol, induce a conformational change in the hexamer from the T-state (tense) to the R-state (relaxed), forming a markedly more stable complex (T3R3) [21] [20]. This stabilization can have a profound effect on disassembly rates; for instance, a single amino acid substitution (TyrB26→Trp) designed to enhance aromatic interactions at the dimer interface, when combined with these excipients, resulted in a 150-fold increase in hexamer half-life in vitro compared to the wild-type control [21].
Q2: What is the experimental evidence for alternative insulin assembly pathways beyond the classic monomer-dimer-hexamer model? Recent single-molecule studies have directly observed that insulin oligomerization can operate via multiple pathways, not just monomeric additions. The research quantified the existence and abundance of assembly and disassembly pathways involving the addition of monomeric, dimeric, or tetrameric insulin species [20]. The pathway taken is rerouted by solution conditions and excipients. For example, the presence of Zn²⁺ and phenol shifts the pathway to favor dimeric or tetrameric additions, thereby enhancing hexamer formation and stability. This direct evidence revises the oversimplified classical model and explains the high abundance of oligomers across a wide concentration range [20].
Q3: Why does intramuscular (IM) insulin injection lead to greater absorption variability compared to subcutaneous (SC) injection, and how does this impact research? Intramuscular injection leads to faster and more variable absorption because muscle tissue has a higher density of blood vessels and greater blood flow, especially during physical activity, compared to subcutaneous adipose tissue [22] [18]. One study found that the day-to-day (intrapatient) coefficient of variation for the absorption rate (T50%) of NPH insulin was significantly higher for IM injections (29.8%) than for SC injections (18.4%) [22]. For researchers, this highlights that inadvertent IM delivery is a major confounding variable in absorption studies. Ensuring true SC injection through validated techniques (e.g., using shorter needles, ultrasound guidance) is critical for obtaining reproducible pharmacokinetic data [22] [18] [23].
Q4: How can excipients be manipulated to create a stable, ultra-rapid acting insulin formulation rich in monomers? Creating a stable, monomer-rich formulation requires the strategic removal of excipients that promote oligomerization and their replacement with agents that stabilize the monomer. A proven strategy involves:
- Removing Zinc: Eliminating Zn²⁺ prevents the coordination that stabilizes hexamers [24].
- Replacing Phenolic Preservatives: Substituting metacresol with a non-phenolic antimicrobial agent like phenoxyethanol prevents stabilization of the R6 hexamer state [24].
- Adding a Stabilizing Polymer: Incorporating an amphiphilic acrylamide copolymer excipient (e.g., poly(acryloylmorpholine-co-N-isopropylacrylamide), or "MoNi") provides stability to the monomeric and dimeric forms [24]. This specific excipient combination has been shown to yield a formulation containing about 70% insulin monomers that is twice as stable as commercial rapid-acting analogs in stressed aging tests [24].
Troubleshooting Common Experimental Challenges
Problem: Variable Insulin Absorption Rates inIn VivoModels
Potential Causes and Solutions:
- Cause 1: Inconsistent Injection Depth. Intramuscular vs. subcutaneous delivery results in significantly different pharmacokinetics [18].
- Solution: Standardize injection protocols. Use shorter (e.g., 4-5 mm) needles to minimize risk of IM injection. For preclinical studies, consider ultrasound guidance to verify subcutaneous placement [18] [23].
- Cause 2: Site-to-Site Variability. Absorption rates differ between anatomical sites (abdomen > arm > thigh > buttock) due to variations in blood flow and subcutaneous tissue properties [25].
- Solution: Use a single, standardized injection site (e.g., abdomen) for a given study arm to reduce inter-injection variability.
- Cause 3: Local Tissue Status. Lipohypertrophy (fatty lumps from repeated injections) or local temperature changes can drastically alter absorption [18] [25].
- Solution: Rotate injection sites systematically within the approved anatomical area. Monitor and control ambient temperature at the injection site.
Problem: Unexpectedly Slow or Fast Hexamer Dissociation inIn VitroAssays
Potential Causes and Solutions:
- Cause 1: Unaccounted for Excipients. Trace amounts of zinc or phenolic preservatives in commercial insulin can profoundly skew oligomerization kinetics.
- Solution: Pre-treat insulin with chelating agents (e.g., EDTA) to remove zinc, and use size-exclusion chromatography to buffer exchange and remove preservatives prior to assay setup [24]. Precisely document and control all excipients in your experimental buffer.
- Cause 2: Assay Concentration Range. The oligomerization pathway is concentration-dependent. The abundance of different oligomers shifts across the nM to mM range [20].
- Solution: Use an assay appropriate for your target concentration. Single-molecule techniques (e.g., TIRF) are reliable at nM concentrations, while bulk assays (e.g., DLS, AUC) are better for µM-mM ranges [20].
Quantitative Data on Insulin Oligomerization
Table 1: Experimentally Determined Hexamer Dissociation Half-Lives
Data adapted from Brader et al., 2018 [21]
| Insulin Analog | Key Modification / Feature | Excipients Present | Half-life (t½, min ± S.D.) |
|---|---|---|---|
| Wildtype (WT) | Native human insulin | Zinc, Phenol | 7.7 (± 1.3) |
| Lispro | Weakened dimer interface | Zinc, Phenol | 4.6 (± 0.3) |
| OrnB29 | Semisynthesis-compatible control | Zinc, Phenol | 8.2 (± 0.8) |
| TrpB26, OrnB29 | Enhanced aromatic cluster | Zinc, Phenol | ~1200 (± 300) |
Table 2: Impact of Formulation Excipients on Insulin Association State
Data synthesized from Ma et al., 2022 [24]
| Formulation Base | Zinc | Phenolic Preservative (e.g., Metacresol) | Alternative Preservative | Stabilizing Polymer (MoNi) | Predominant Association State(s) |
|---|---|---|---|---|---|
| Commercial (e.g., Humalog) | Yes | Yes | No | No | Hexamer / Dimer |
| Zinc-Free Lispro-1 | No | Yes | No | Yes | Hexamer / Dimer |
| Zinc-Free Lispro-2 | No | Reduced | Phenoxyethanol | Yes | Mixed |
| Zinc-Free Lispro-3 | No | No | Phenoxyethanol | Yes | Monomer / Dimer |
| Zinc-Free RHI (Regular Human Insulin) | No | No | Phenoxyethanol | Yes | Hexamer |
Standard Experimental Protocols
Protocol 1: Determining Insulin Oligomerization State via Analytical Ultracentrifugation (AUC)
Objective: To determine the relative proportions of monomers, dimers, and hexamers in an insulin formulation. Methodology [24]:
- Sample Preparation: Prepare insulin samples at a standard concentration (e.g., 3.45 mg/mL or 100 U/mL) in the desired buffer with excipients.
- Instrument Setup: Use a preparative ultracentrifuge with an An-50 Ti analytical rotor. Set temperature to 20°C and speed to 45,000 rpm.
- Data Acquisition: Acquire data over 200 scans. Analyze data using software such as SEDFIT, employing the c(s) continuous size distribution model.
- Data Analysis: Identify oligomeric states based on their sedimentation coefficients (s). The stoichiometry (N) can be estimated from the monomer sedimentation coefficient (s1) using the relationship: (sN / s1)^(3/2). Typical ranges are:
- Monomer: s ~ 1.0-2.0 S
- Dimer: s ~ 2.5-3.5 S
- Hexamer: s > 5.0 S
Protocol 2: Measuring Hexamer Dissociation Kinetics via Size-Exclusion Chromatography (SEC)
Objective: To monitor the rate of dissociation of insulin hexamers into smaller oligomers under conditions that destabilize the hexamer. Methodology (adapted from [21]):
- Sample Formulation: Formulate insulin with ZnCl₂ (e.g., 2 Zn²⁺ ions per hexamer) and phenol to stabilize the R6 hexamer state.
- Chromatography: Inject the stabilized sample onto an SEC column pre-equilibrated with a zinc- and phenol-free mobile phase.
- Monitoring Dissociation: The change from the mobile phase triggers hexamer disassembly. Monitor the elution profile over time.
- Data Analysis: The chromatogram will show peaks corresponding to different oligomeric states (hexamers, dimers, monomers). The rate of disappearance of the hexamer peak and the appearance of smaller oligomer peaks can be used to calculate dissociation rate constants and half-lives.
Signaling Pathways and Experimental Workflows
Diagram: Insulin Oligomerization Pathways and Excipient Influence
Diagram: Experimental Workflow for Oligomer State Analysis
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Reagents for Investigating Insulin Oligomerization
Compiled from multiple sources [21] [24] [20]
| Reagent / Material | Function / Role in Research | Example Use Case |
|---|---|---|
| Zinc Chloride (ZnCl₂) | Stabilizes tetramer and hexamer formation via coordination with HisB10. | Creating pharmaceutical-like, stable hexameric insulin for baseline dissociation studies [20]. |
| Phenol / m-Cresol | Phenolic preservatives that induce T→R state transition, dramatically increasing hexamer stability. | Studying the R6 hexamer state and its dissociation kinetics [21] [24]. |
| Ethylenediaminetetraacetic acid (EDTA) | Chelating agent that binds Zn²⁺ and other divalent cations. | Removing zinc from commercial formulations to create zinc-free insulin for monomer/dimer studies [24]. |
| Phenoxyethanol | Non-phenolic antimicrobial agent. | Replacing m-cresol in formulations to prevent hexamer stabilization without compromising sterility [24]. |
| Amphiphilic Acrylamide Copolymer (MoNi) | Stabilizing excipient for monomeric/dimeric insulin. | Developing and studying ultra-rapid, stable monomeric insulin formulations [24]. |
| Fluorescent Dye (e.g., ATTO655) | Covalent label for single-molecule detection. | Labeling insulin at sites like LysB28 for real-time tracking of oligomerization via TIRF microscopy [20]. |
Best Practices in Injection Technique and Device Technology to Ensure Subcutaneous Deposition
FAQs: Needle Length and Intramuscular Injection Risk
Q1: What is the primary clinical risk of using a needle that is too long for subcutaneous insulin delivery?
The primary risk is unintentional intramuscular (IM) injection. Insulin delivered into muscle is absorbed more quickly and completely than from subcutaneous tissue, which can lead to unpredictable blood glucose levels and an increased risk of hypoglycemia. This absorption variability is a significant confounder in clinical trials aiming to study the pharmacokinetics of new insulin formulations [26].
Q2: Why is the 4mm pen needle recommended as the standard length for the vast majority of patients?
A 4mm needle is sufficient to reach the subcutaneous tissue in individuals of all body mass indices (BMIs) while minimizing the risk of intramuscular injection. This promotes consistent, predictable absorption and glycemic control. Longer needles do not provide additional therapeutic benefit for subcutaneous delivery and increase the risk of IM injection, especially in leaner individuals [26].
Q3: How does preventing intramuscular injection contribute to more robust research data in drug development?
Unintended IM injection introduces significant variability in insulin absorption rates. By standardizing the use of 4mm needles, researchers can minimize this procedural variable, leading to cleaner data and more accurate assessment of a new insulin product's true pharmacokinetic and pharmacodynamic profile [26].
Q4: What are the evidence-based techniques to further reduce injection pain and variability?
Systematic reviews and meta-analyses have identified several techniques that reduce IM injection pain, which can be applied to insulin injections. The evidence supports applying manual pressure or rhythmic (Helfer) tapping at the injection site before and during the injection. Furthermore, injections administered in the ventrogluteal site have been shown to be less painful than those in the dorsogluteal site [26].
Troubleshooting Guide for Researchers
Issue: Unexplained Variability in Insulin Absorption Data
This guide is designed to help researchers identify and correct for factors that introduce variability in insulin absorption data during clinical trials.
| Investigation Step | Purpose & Methodology | Interpretation of Findings |
|---|---|---|
| Verify Injection Technique | Ensure consistent subcutaneous delivery. Method: Train staff/participants on proper 4mm needle use with a 90-degree angle; utilize ultrasound imaging on a subset to confirm needle tip placement. | Ultrasound confirmation of IM placement identifies a major source of absorption variability and supports the need for technique re-training. |
| Analyze by Injection Site | Identify site-specific absorption differences. Method: In a controlled sub-study, systematically rotate and document injection sites (abdomen, thigh, arm) and compare pharmacokinetic (PK) curves. | Significant differences in PK parameters (e.g., T~max~, C~max~) between sites confirms site-specific absorption as a key variable. |
| Review Technique & Pain Metrics | Correlate procedure with patient-reported outcomes. Method: Implement standardized pain scales (e.g., Visual Analogue Scale) immediately post-injection and analyze against absorption data. | Reports of higher pain may correlate with quicker absorption, potentially indicating IM injection or nerve contact, highlighting the need for technique refinement [26]. |
| Control for Tissue Morphology | Account for the impact of subcutaneous fat thickness. Method: Use anthropometric measurements or imaging to categorize subjects and perform stratified analysis of PK data. | Increased variability in absorption for subjects with lower subcutaneous fat thickness provides strong evidence for the 4mm needle standard. |
Experimental Protocols
Protocol 1: Validating Needle Length Sufficiency via Ultrasound Imaging
Objective: To empirically verify that a 4mm pen needle consistently achieves subcutaneous deposition without risking intramuscular injection across a diverse patient population.
Methodology:
- Participant Recruitment: Recruit a cohort of participants with a wide range of BMIs.
- Imaging Setup: Mark potential injection sites (abdomen, thigh). Use a high-frequency linear ultrasound transducer to visualize the skin, subcutaneous tissue, and muscle layers. Measure the skin-to-muscle distance.
- Needle Insertion: Insert a 4mm pen needle adjacent to the transducer at a 90-degree angle.
- Data Collection: Capture ultrasound video and still images to document the final position of the needle tip relative to the muscle fascia.
- Data Analysis: Correlate BMI, subcutaneous tissue thickness, and the success rate of subcutaneous placement without muscle penetration.
Protocol 2: Quantifying Absorption Variability in a Crossover Study
Objective: To compare the pharmacokinetic variability of insulin after administration with 4mm needles versus longer needles (e.g., 8mm or 12mm).
Methodology:
- Study Design: A randomized, double-blind, crossover study where each participant receives standardized doses of insulin using both 4mm and longer needles in different study periods.
- Procedure: Administer insulin under fasting, standardized conditions. Injections should be performed by trained professionals at the same anatomical site.
- Blood Sampling: Conduct frequent serial blood sampling to measure serum insulin concentrations and/or glucose infusion rates (euglycemic clamp technique) over a period of 6-8 hours.
- Data Analysis: Calculate key PK parameters including Time to maximum concentration (T~max~), Maximum concentration (C~max~), and Area Under the Curve (AUC). The primary outcome is the coefficient of variation (CV) for these parameters between the two needle-length groups. A lower CV with the 4mm needle would demonstrate reduced variability [27].
Research Reagent Solutions
The following table details essential materials for conducting research on injection depth and insulin absorption.
| Item | Function & Application in Research |
|---|---|
| 4mm Insulin Pen Needles | The intervention being studied; the standard for ensuring consistent subcutaneous delivery and minimizing IM injection risk in all patients. |
| High-Frequency Ultrasound System | To objectively measure subcutaneous adipose tissue thickness and visually confirm needle tip placement (subcutaneous vs. intramuscular) during method validation. |
| Pharmacokinetic (PK) Assay Kits | (e.g., ELISA or similar) For measuring serial serum insulin concentrations to generate PK profiles and calculate variability metrics (AUC, C~max~, T~max~). |
| Visual Analogue Scale (VAS) | A standardized tool (typically a 100mm line) for subjects to quantitatively report injection-associated pain, allowing correlation with injection technique and depth. |
| Euglycemic Clamp Apparatus | The "gold standard" method for measuring insulin sensitivity and pharmacodynamics; involves controlled IV glucose infusion to maintain a fixed blood glucose level, providing a direct measure of insulin action. |
Research Methodology Visualization
ERS: Insulin Absorption Variability Study
ITV: Injection Technique Investigation
Frequently Asked Questions
Q1: Why is preventing intramuscular (IM) insulin injection a critical consideration in pharmacokinetic research? Intramuscular injection of insulin leads to faster and more erratic absorption compared to subcutaneous (SC) delivery [8]. This variability is a significant confounder in pharmacokinetic (PK) and pharmacodynamic (PD) studies, as it can precipitate hypoglycemia and result in inconsistent glucose control, thereby compromising the reliability of data on insulin action and bioavailability [8].
Q2: What is the evidence-based recommendation for insulin injection angle? Current expert consensus recommends a 90-degree (perpendicular) angle for the vast majority of injections using 4mm, 5mm, and 6mm needles [8]. This technique, when performed without a skinfold in appropriate patients, ensures consistent deposition into the subcutaneous tissue. Angled injections are generally not recommended with modern short needles.
Q3: How does needle length influence the decision to pinch a skinfold? Needle length is the primary determinant for the pinching technique. The following table summarizes the core recommendations:
| Needle Length | Recommended Technique | Key Rationale & Patient Demographics |
|---|---|---|
| 4 mm | Do not pinch for most adults [8]. | Sufficient to traverse skin, minimal IM risk. Suitable for all BMIs [8]. |
| Pinch for very thin adults (BMI <19 kg/m²) and children ≤6 years [8]. | Ensures SC delivery in individuals with reduced SC fat thickness [8]. | |
| 5 mm | Pinch is recommended [8]. | Provides an additional safety margin to avoid IM injection [8]. |
| 6 mm | Pinch and inject at a 45° angle [8]. | The angled injection effectively reduces the delivery depth to approximately 4 mm [8]. |
| 8 mm+ | Use is strongly discouraged; switch to a shorter needle [8]. | High risk of IM injection, more painful, and no glycemic benefit [8]. |
Q4: What are the most common errors in insulin injection technique that can introduce variability in research settings? The most prevalent errors that negatively impact insulin absorption and increase data variability are:
- Needle Reuse: Leads to lipohypertrophy (LH), increased pain, and inconsistent dosing [28] [8].
- Failure to Rotate Sites: The primary cause of LH, which alters insulin pharmacokinetics and can increase glucose variability [28] [8].
- Injecting into Lipohypertrophy: Insulin absorption from LH tissue is slowed and erratic, leading to unexplained hyperglycemia and higher insulin doses [28] [8].
Experimental Protocols for Technique Assessment
Protocol 1: Validating Injection Technique in a Clinical Cohort This methodology is adapted from a cross-sectional study designed to quantify the association between injection technique and glycemic outcomes [28].
- Objective: To determine the correlation between a standardized injection technique score and metabolic parameters (HbA1c, FBS, 2HPP).
- Patient Population: 301 adults with type 2 diabetes using insulin pens for at least 3 months.
- Technique Assessment: A 13-item, researcher-made questionnaire with a total score of 26. The tool's validity was confirmed by endocrinologist review, and reliability was established with a Cronbach’s alpha of 0.75 [28].
- Key Assessment Items:
- Needle reuse frequency
- Skin fold formation
- Site rotation practice
- Injection angle
- Needle hold time in skin
- Insulin resuspension (for NPH)
- Data Collection: Disease-related data (HbA1c, FBS) were extracted from medical records. Injection sites were physically examined for lipohypertrophy by a trained diabetes educator [28].
- Statistical Analysis: Data were analyzed using SPSS. Correlation between the total injection score and HbA1c was tested using regression analysis, revealing a significant negative correlation (β = -0.263, P < 0.001) [28].
Protocol 2: Point-of-Care Education and Follow-up (ITPR 2.0 Study) This protocol evaluates the effectiveness of immediate feedback on correcting injection errors [29].
- Objective: To explore the effectiveness of feedback and education at the point of care in improving patients’ insulin injection technique.
- Study Design: Physicians completed a baseline assessment survey for eligible patients. If an error was identified, a pop-up knowledge transfer (KT) prompt based on the Forum for Injection Technique (FITTER) recommendations was triggered, providing immediate, specific feedback [29].
- Intervention: The KT prompts provided verbal feedback and information on best practices related to the specific error identified (e.g., needle reuse, incorrect hold time).
- Follow-up: Patients completed a follow-up survey 1-3 months later (average 34.7 days) to identify changes in their technique [29].
- Outcome Measures: Reduction in the number of technique errors per patient. The study found a modest but significant improvement, with patients reducing an average of one error at follow-up [29].
The Scientist's Toolkit: Key Reagents and Materials
| Item | Function in Research Context |
|---|---|
| 4 mm Insulin Pen Needles | The recommended standard needle for minimizing IM injection risk across diverse patient demographics in clinical trials [8]. |
| Lipohypertrophy (LH) Palpation Protocol | A standardized method for identifying and documenting LH at injection sites, a key variable affecting insulin absorption kinetics [28] [8]. |
| Validated Injection Technique Questionnaire (ITQ) | A standardized tool (e.g., 13-item scale) to quantitatively assess participant adherence to proper injection protocols, allowing for correlation with PK/PD data [28]. |
| Structured Point-of-Care Feedback System | A protocol for delivering immediate, standardized education based on FITTER guidelines to correct technique errors during study visits, minimizing interventional variability [29]. |
Decision Pathway for Injection Technique
The following diagram outlines the logical decision process for selecting the correct insulin injection technique based on patient demographics and needle length, integrating evidence-based recommendations to minimize intramuscular delivery risk.
Troubleshooting Guide: Addressing Common Technique Errors
| Clinical or Research Observation | Probable Technique Error | Evidence-Based Correction |
|---|---|---|
| Unexplained hypoglycemia, especially post-injection [8]. | Intramuscular injection [8]. | Switch to a 4mm needle and inject at a 90-degree angle without pinching for most adults [8]. |
| Unexplained hyperglycemia & high glucose variability; presence of rubbery or swollen tissue at injection sites [28] [8]. | Lipohypertrophy (LH) from lack of site rotation and needle reuse [28] [8]. | 1. Avoid LH sites entirely. 2. Implement systematic site rotation. 3. Use needles only once. 4. Regularly inspect and palpate sites [28] [8]. |
| Reports of pain during injection; visible skin backflow [28]. | Needle reuse (blunting the needle) and/or incorrect injection angle [28] [8]. | 1. Educate on single-needle use. 2. Ensure a perpendicular (90°) angle with a 4mm or 5mm needle [28] [8]. |
| Inconsistent PK/PD profiles in a study cohort. | Lack of standardized technique training and validation among participants. | Incorporate a validated injection technique questionnaire and direct observation with immediate feedback at study initiation and follow-ups [28] [29]. |
Troubleshooting Guide: Frequent Infusion Set and Pen Needle Issues
Problem: Unexplained Hyperglycemia Following Infusion Set Change
- Question: After I change my infusion set, my blood glucose frequently spikes and does not respond to correction boluses. What could be causing this, and how can I prevent it?
- Answer: This is a common issue often linked to the infusion set. A spike in glucose after a set change can indicate that the new site is not delivering insulin effectively.
- Troubleshooting Steps:
- Prime the Set Properly: Ensure both the tubing and the catheter are fully primed with insulin after changing the set to eliminate any air gaps [30].
- Time the Change: Change the infusion set just before a meal and administer a full meal bolus immediately after inserting the new set. This helps verify the system is working and counteracts any initial absorption delay [30].
- Administer a Small Extra Bolus: Consider giving an additional small bolus (e.g., 0.5-1.0 unit) once the new infusion set is in place to account for potential undelivered insulin [30].
- Check for Bent Cannula: Upon removal, inspect the flexible cannula. If it is bent, it can impede insulin flow. To prevent this, choose insertion sites with ample subcutaneous fat, use a shorter cannula, or switch to a steel needle infusion set [30].
Problem: High Variability in Experimental Injection Depths
- Question: In our preclinical studies, we observe high variability in needle penetration depth (NPD) even when using needles of the same labeled length. What factors contribute to this, and how can we control for them?
- Answer: Variability in NPD is significantly influenced by two key factors: the hub design of the pen needle and the force applied against the skin during injection. A conventional "posted-hub" design offers less control over depth compared to a reengineered, flatter hub.
- Troubleshooting Steps:
- Select an Advanced Hub Design: Utilize a pen needle with a hub engineered to control depth. One study showed a reengineered hub achieved the target 4 mm depth with "significantly less variability" across a range of injection forces compared to posted-hub designs [31].
- Standardize Injection Force: In your experimental protocol, define and control the force applied during injection. Highly variable intra- and inter-operator applied skin forces are a major source of NPD inconsistency [31].
- Consider an Autoinjector Shield: Using a shield-triggered autoinjector can standardize the insertion and has been shown to reduce skin blood perfusion, a marker for tissue trauma, by controlling skin deflection [32].
Problem: Persistent Pain or Discomfort During Injection
- Question: Study participants or end-users report significant pain or discomfort during subcutaneous injection. What needle-related factors can we adjust to improve comfort?
- Answer: Pain can be mitigated through several design and technique modifications focused on the needle's physical characteristics and the injection process itself.
- Troubleshooting Steps:
- Use a Thinner, Shorter Needle: Research consistently shows that higher-gauge (thinner) needles result in lower reported pain levels. Similarly, using the shortest needle length appropriate for the subcutaneous tissue depth minimizes tissue trauma [33] [34].
- Evaluate the Hub Design: A hard polymer hub can minimize "flexing" during injection, which prevents leakage and potential tissue disturbance that can cause pain [35].
- Implement Cold Needle Technique: A prospective randomized controlled study found that using a needle chilled to 0-2 °C significantly reduced injection pain and increased patient satisfaction compared to a needle at room temperature [36].
- Ensure a Sharp, Multi-Beveled Tip: Needle tips with multiple bevels (e.g., 5 facets) are designed for smoother skin penetration, reducing insertion force and discomfort [34].
Frequently Asked Questions (FAQs)
FAQ 1: How does needle hub design physically influence the consistency of needle penetration depth?
The hub is the polymer base that connects the needle to the syringe or pen. Its geometry determines how it sits against the skin and interacts with tissue during insertion.
- Conventional Posted-Hub: This design features a small cylindrical post that extends from the hub base. This post can indent the skin upon application, allowing the needle to achieve a deeper-than-intended penetration, especially with higher injection forces. This leads to high variability in depth [31].
- Reengineered/Advanced Hub: These hubs are designed with a wider, flatter geometry that distributes pressure more evenly and limits skin indentation. This design effectively "bottoms out" on the skin surface, creating a more reliable stop that ensures the needle reaches the target subcutaneous tissue consistently, regardless of moderate variations in applied force [31].
FAQ 2: Beyond patient comfort, what is the critical research imperative for reducing intramuscular (IM) injection risk?
The primary research imperative is to control experimental variables and ensure accurate drug delivery. An unintended intramuscular injection represents a critical failure in subcutaneous dosing studies.
- Altered Pharmacokinetics/Pharmacodynamics (PK/PD): Insulin and many other drugs are absorbed much more rapidly from muscle tissue than from subcutaneous fat. An IM injection can cause a dangerously rapid onset of action and skew PK/PD data, leading to incorrect conclusions about a drug's profile [31].
- Increased Data Variability: Uncontrolled penetration depth is a major source of variability in absorption studies. By using hub designs that ensure consistent subcutaneous delivery, researchers can reduce noise in their data and achieve more reliable and reproducible results [31].
FAQ 3: Are there reusable or multi-use needle designs that are suitable for repeated preclinical testing?
Yes, novel robust needle designs are being developed for multi-use applications. Their suitability depends on the specific requirements of the test.
- Design Principle: These needles feature a reinforced tip geometry, such as larger bevel angles and a pre-bent design, to enhance durability and resist deformation (hooking) after multiple insertions [32].
- Preclinical Evidence: One study showed that a robust needle (EXP) required a force of 5.38 N to form a 33 µm hook, compared to only 0.92 N for a conventional single-use needle (NF30). When tested in a porcine model, this robust needle did not induce more tissue trauma than its single-use counterpart, especially when used with an autoinjector shield [32].
- Application: Such needles are ideal for repeated-dose studies or device durability testing, as they can reduce consumable costs and environmental impact while maintaining experimental integrity.
The following tables consolidate key quantitative findings from research on needle hubs and related technologies.
Table 1: Impact of Hub Design and Injection Force on Needle Penetration Depth (NPD) and IM Risk
| Hub Design Type | Applied Force (lbf [N]) | Mean Needle Penetration Depth (NPD) | Variability (vs. Target Depth) | Modeled IM Injection Risk (vs. Posted-Hub) |
|---|---|---|---|---|
| Reengineered Hub [31] | 0.25 lbf [1.1 N] | Closer to 4 mm target | Significantly less variability (P = 0.006) | ~2-8 times reduction |
| 0.75 lbf [3.3 N] | Closer to 4 mm target | Significantly less variability (P = 0.006) | ~2-8 times reduction | |
| 1.25 lbf [5.6 N] | Closer to 4 mm target | Significantly less variability (P = 0.006) | ~2-8 times reduction | |
| 2.00 lbf [8.9 N] | Closer to 4 mm target | Significantly less variability (P = 0.006) | ~2-8 times reduction | |
| Commercial Posted-Hub [31] | 0.25 lbf [1.1 N] | Deviated from 4 mm target | Higher variability | Baseline (Higher) |
| 0.75 lbf [3.3 N] | Deviated from 4 mm target | Higher variability | Baseline (Higher) | |
| 1.25 lbf [5.6 N] | Deviated from 4 mm target | Higher variability | Baseline (Higher) | |
| 2.00 lbf [8.9 N] | Deviated from 4 mm target | Higher variability | Baseline (Higher) |
Table 2: Efficacy of Pain Reduction and Needle Robustness Techniques
| Technique / Design | Metric | Result / Effect | Clinical / Research Implication |
|---|---|---|---|
| Cold Needle [36] | Pain Score (VAS) | 21.0 ± 14.46 (Cold) vs. 33.0 ± 18.03 (Room Temp) | Significant reduction in patient-reported pain. |
| Injection Satisfaction Score | 86.33 ± 11.29 (Cold) vs. 73.00 ± 17.04 (Room Temp) | Significant increase in patient satisfaction. | |
| Robust Needle (EXP) [32] | Force to form 33µm hook | 5.38 N (EXP) vs. 0.92 N (Control NF30) | Withstands significantly more mechanical stress, enabling multi-use. |
| Hard Polymer Hub (HPC) [35] | Pressure Resistance | Withstands up to 2.5x more pressure | Prevents hub flexing and leakage, ensuring dose accuracy. |
Experimental Protocols
Protocol 1: In Vivo Measurement of Needle Penetration Depth (NPD) Using Fluoroscopy
This protocol is adapted from a preclinical study that quantified the impact of hub design and injection force on penetration depth [31].
- Objective: To precisely measure the in vivo depth a needle reaches in subcutaneous tissue under controlled application forces.
- Materials:
- Animal Model: Yorkshire swine (35-40 kg). Swine skin is structurally and compositionally similar to human skin, providing a valid model [31] [32].
- Devices: Pen needles with different hub designs (e.g., reengineered vs. posted-hub). A standard pen injector (e.g., ClikSTAR).
- Instrumentation: Custom Insertion Force Measurement Tool (IFMT) with a donut load cell. Fluoroscope (e.g., Glenbrook Technologies LabScope).
- Injectate: Iodinated contrast agent (e.g., Omnipaque 350 mg Iodine/ml).
- Methodology:
- Anesthesia and Positioning: Anesthetize the animal and position it under the fluoroscope with the target flank area perpendicular to the X-ray beam path.
- Site Identification: Mark and number an array of injection sites on the flank.
- Force-Targeted Injection: Connect the IFMT between the pen and the needle. For each injection, the operator targets a specific application force (e.g., 0.25, 0.75, 1.25, 2.00 lbf). The IFMT acquires and displays force data in real-time.
- Contrast Administration: Administer a small, controlled volume (e.g., 20 µl) of contrast agent.
- Image Acquisition: Capture a fluoroscopic image immediately after injection to visualize the radio-opaque depot.
- Depth Measurement: Calculate the NPD from the 2D image against a radiopaque scale placed in the field of view, applying a parallax correction factor.
- Analysis: Statistically compare the mean NPD and variability for each hub design across the different force levels. Use an in silico probability model to estimate IM injection risk based on NPD data and human tissue thickness measurements.
Protocol 2: Assessing Injection Site Trauma via Skin Blood Perfusion (LASCA)
This protocol assesses tissue trauma, a proxy for pain and tissue damage, resulting from different needle designs [32].
- Objective: To quantify local tissue trauma induced by needle insertion by measuring changes in skin blood perfusion (SBP).
- Materials:
- Animal Model: Landrace, Yorkshire, and Duroc (LYD) pigs.
- Devices: Test needles (e.g., novel robust needle, conventional control needles), autoinjector shields.
- Instrumentation: Laser Speckle Contrast Analysis (LASCA) system. Handheld digital force gauge.
- Methodology:
- Site Preparation: Shave the pig's neck area one day before the experiment. On the day, mark a grid of insertion sites.
- Needle Insertion: Perform needle insertions according to the experimental plan (e.g., different needles, with/without shield, various applied forces). Use a force gauge to standardize shield pressure.
- LASCA Imaging: Use the LASCA system to scan the insertion area immediately after needle removal. The system measures microcirculatory blood flow by analyzing the speckle pattern of laser light.
- Blinding: The operator performing insertions and analysis should be blinded to the needle type to prevent bias.
- Analysis: Compare the SBP values between different needle groups. A higher SBP indicates greater tissue trauma and a stronger inflammatory response.
Experimental Workflow and Logical Diagrams
Diagram 1: NPD Evaluation Workflow
Diagram 2: Logic of Injection Variability
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Needle Hub and Injection Depth Research
| Item | Function / Application in Research | Key Specification / Rationale |
|---|---|---|
| Yorkshire Swine Model [31] | In vivo model for injection studies. | Skin structure, elasticity, and SC tissue thickness are highly analogous to humans. |
| Insertion Force Measurement Tool (IFMT) [31] | Precisely measures and controls the force applied against the skin during injection. | Critical for standardizing one of the most significant human factors (force) in injection depth studies. |
| Fluoroscope with Contrast Agent [31] | Enables real-time visualization and measurement of needle tip depth and injectate depot location. | Provides direct, quantitative data on Needle Penetration Depth (NPD). |
| Laser Speckle Contrast Analysis (LASCA) [32] | Quantifies local skin blood perfusion (SBP) as a non-invasive marker for needle-induced tissue trauma. | Offers an objective, preclinical measure of tissue damage and potential pain. |
| Reengineered Hub Pen Needles [31] | The independent variable in studies aiming to control injection depth. | Designed with a wider, flatter geometry to limit skin indentation and reduce NPD variability. |
| Autoinjector Shields [32] | Used to standardize the insertion angle and control skin deflection during automated injections. | Helps isolate the effect of needle design from user technique and can reduce tissue trauma. |
Systematic Site Rotation Protocols to Prevent Tissue Complications and Ensure Consistent Absorption
For researchers and drug development professionals, the subcutaneous (SC) space represents a critical interface for the delivery of biotherapeutics, particularly insulin. The integrity of this tissue is paramount for ensuring consistent pharmacokinetic (PK) and pharmacodynamic (PD) profiles of administered drugs. Lipohypertrophy (LH)—the localized hypertrophy of subcutaneous fat—is a frequent tissue complication that significantly alters drug absorption, leading to unpredictable glycemic outcomes in clinical trials and unreliable PK/PD data in pre-clinical studies [8] [37]. Systematic site rotation is a foundational methodology to preserve tissue health and ensure the reproducibility of absorption data. This guide provides troubleshooting and protocols to standardize this crucial aspect of preclinical and clinical research.
Understanding the Problem: Lipohypertrophy and Research Outcomes
The Impact of Lipohypertrophy on Drug Absorption
Lipohypertrophy is more than a clinical nuisance; it is a significant confounding variable in research settings. Injecting into LH tissue leads to:
- Erratic Absorption: Insulin absorption from LH sites is slowed and highly variable, increasing intrasubject variability and compromising data integrity [8] [37].
- Reduced Drug Action: The glucose-lowering effect of insulin is blunted and unpredictable when administered into LH [8] [38].
- Increased Resource Consumption: Studies note that subjects with LH may require a mean of over 10 IU more insulin per day to achieve glycemic control, directly impacting study dosing and cost calculations [38].
Pathophysiology and Histology
Histological analysis of LH tissue reveals a disrupted architecture, explaining the altered absorption kinetics. Affected areas show:
- Macro-adipocytes: Approximately 75% of the SC tissue is composed of enlarged fat cells compared to normal adjacent adipocytes [37].
- Fibrosis: Increased presence of fibrotic tissue, which may physically impede the diffusion and absorption of therapeutic agents [37].
- Altered Vascularization: The normal capillary network may be compromised, directly affecting the pathway of insulin into the bloodstream [18].
The following diagram illustrates the stark difference in insulin absorption pathways between healthy and lipohypertrophic subcutaneous tissue.
Technical Support Center: Troubleshooting Guides and FAQs
FAQ 1: What are the primary risk factors for lipohypertrophy in a research cohort?
Answer: The development of LH is primarily technique-dependent. Key risk factors identified in large surveys and clinical studies include [8] [37] [38]:
- Lack of Systematic Site Rotation: Failure to rotate injection sites is the most significant factor.
- Needle Reuse: Reusing pen or syringe needles causes increased tissue trauma and is strongly correlated with LH.
- High Injection Frequency: A greater number of daily injections into a limited area elevates risk.
- Large Injection Volumes: Administering large volumes per injection (>50 µL) may contribute to tissue trauma.
- Incorrect Needle Length: Using needles that are too long can increase the risk of intramuscular injection and deeper tissue damage.
FAQ 2: How can we accurately detect and monitor lipohypertrophy in study subjects?
Answer: A multi-modal approach is recommended for rigorous data collection.
Method 1: Visual Inspection and Palpation
- Protocol: Visually inspect and gently palpate the entire injection area with clean hands. Have the subject change body position (e.g., rotate torso) to make subtle LH more visible. A "pinching" maneuver helps identify elastic, non-visible nodules [37].
- Limitations: Subject to examiner experience. One study showed trained professionals are 45% more likely to correctly detect LH than untrained staff [37].
Method 2: High-Frequency Ultrasound
- Protocol: Utilize ultrasound imaging to obtain cross-sectional views of the subcutaneous tissue. LH appears as hyperechoic (brighter) regions with altered architecture [37].
- Advantages: Approximately 30% more sensitive than palpation. It can detect deeper structural changes before they are visible or palpable, providing objective, quantifiable data for longitudinal studies [37].
Troubleshooting Table: Common Injection Site Issues and Research Impact
| Problem | Underlying Mechanism | Impact on Research Data | Corrective Protocol |
|---|---|---|---|
| Lipohypertrophy (LH) | Repetitive trauma & anabolic effect of insulin causing macro-adipocytes & fibrosis [37]. | Highly variable PK/PD; increased insulin dose requirements; unreliable glucose response curves [8] [38]. | Implement strict site rotation; prohibit needle reuse; use ultrasound for detection; avoid injecting into affected areas. |
| Intramuscular (IM) Injection | Needle penetrates beyond SC tissue into muscle fascia. Risk is higher with longer needles (>6mm) and in lean subjects/children [8] [18]. | Faster, erratic insulin uptake; accelerated drug action; increased hypoglycemia risk in trials; confounds PK analysis [8] [18]. | Use shortest needle possible (4mm for pens, 6mm for syringes); utilize skinfolds in lean subjects; avoid high-risk sites (arms, thighs) in at-risk cohorts. |
| Inconsistent Absorption | Injection into LH, IM tissue, or sites with variable temperature or blood flow [18]. | High intra-subject variability; poor reproducibility of dose-response data; challenges in establishing therapeutic equivalence. | Standardize injection technique, sites, and needle length across all study participants and personnel. |
Experimental Protocols for Standardized Administration
Protocol: Systematic Injection Site Rotation
Objective: To prevent LH and ensure consistent drug absorption throughout a study period by implementing a structured, documented site rotation plan.
Materials:
- Standardized injection devices (pens or syringes) with specified needle length (e.g., 4mm or 6mm).
- Alcohol swabs.
- Study-specific documentation forms (e.g., body maps).
- Timer.
Methodology:
- Define Injection Zones: Divide the four recommended sites (abdomen, thighs, buttocks, upper arms) into smaller, manageable zones (e.g., abdominal quadrant divided into clock hours) [39] [38].
- Systematic Rotation: Instruct subjects to use one zone per injection and rotate to the next zone in a predetermined, systematic sequence (e.g., clockwise).
- Spatial Separation: Ensure each new injection is at least 1-2 cm (approximately the width of a finger) from the previous injection site [38].
- Documentation: For rigorous studies, provide subjects with body maps to log the precise location and time of each injection.
The following workflow provides a clear, standardized operating procedure for research subjects and staff.
Protocol: Optimized Injection Technique for Consistent SC Deposition
Objective: To ensure reliable and reproducible delivery of insulin into the subcutaneous tissue, avoiding intradermal or intramuscular deposition.
Materials:
- Insulin pen or syringe with needle.
- Alcohol swabs.
- Timer.
Methodology:
- Needle Selection: Based on anthropometric data, select the shortest needle that reliably reaches the SC tissue. The 4-mm pen needle is recommended for the vast majority of adults and children, as it minimizes IM injection risk while providing equivalent glycemic control to longer needles [8] [38].
- Skinfold Technique:
- Injection Angle:
- Injection and Wait Time: Inject the insulin slowly and deliberately. After the plunger is fully depressed, wait at least 10 seconds before removing the needle from the skin to prevent insulin leakage (backflow) which leads to dose inaccuracy [39].
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Research | Technical Notes |
|---|---|---|
| 4-mm Pen Needles | Standardized delivery to SC tissue; minimizes IM injection risk in most populations. | Considered the safest needle length for nearly all subjects; ensures consistent PK/PD data [8] [38]. |
| High-Frequency Ultrasound | Objective detection and monitoring of SC tissue health (LH, fibrosis). | Provides quantitative data on SC thickness and structural changes; essential for longitudinal studies [37]. |
| Structured Body Maps | Documentation and tracking of injection sites for systematic rotation. | Critical for protocol compliance and auditing; allows correlation of injection site with local tissue reactions or absorption data. |
| Alcohol Swabs | Aseptic site preparation. | Must be allowed to air dry completely to prevent stinging and potential irritation that could confound tissue response [39]. |
| Skinfold Simulators | Training tool for proper skinfold technique. | Ensures research staff and subjects can consistently perform correct injections in lean models or pediatric studies. |
Quantitative Data for Research Planning
| Needle Length | Overall Risk | Thigh | Arm | Abdomen | Buttock |
|---|---|---|---|---|---|
| 4 mm | 0.4% | 1.6% | 1.0% | 0.3% | 0.1% |
| 5 mm | 1.8% | 4.7% | 3.1% | 1.1% | 0.5% |
| 6 mm | 5.7% | 10.0% | 7.0% | 2.8% | 1.3% |
| 8 mm | 15.3% | 25.0% | 19.5% | 9.7% | 5.5% |
| 12.7 mm | 45.0% | 63.0% | 55.0% | 38.0% | 26.9% |
Note: Data highlights the dramatically lower risk of IM injection with 4-mm needles, supporting their use for standardized protocols.
| Metric | Effect in LH-Positive vs. LH-Negative Subjects | Research Implication |
|---|---|---|
| Daily Insulin Dose | ↑ >10 IU/day on average | Significantly higher drug consumption in trials. |
| Glycemic Control (HbA1c) | ↑ 0.55% on average | Masks true efficacy of the tested insulin or regimen. |
| Glycemic Variability | ↑ Increased | Introduces noise and reduces statistical power. |
| Unexplained Hypoglycemia | ↑ Increased | Compromises subject safety and data interpretability. |
The choice of insulin delivery system is a critical variable in metabolic research, directly influencing the pharmacokinetic (PK) and pharmacodynamic (PD) profiles of subcutaneous insulin. This analysis provides a technical resource for scientists investigating the core problem of absorption variability, with a specific focus on preventing the confounder of unintentional intramuscular injection. The fundamental principle underpinning this guide is that reproducible insulin absorption is contingent upon reliable delivery into the subcutaneous adipose tissue. Systems that ensure this consistency while minimizing tissue trauma are paramount for generating robust, interpretable experimental data. We frame this technical evaluation within the context of a broader thesis on mitigating absorption variability, providing troubleshooting guides and detailed experimental protocols to support preclinical and clinical research.
Quantitative Comparison of Delivery Systems
The following tables summarize the key technical and performance characteristics of insulin delivery systems, compiling data relevant to experimental design and variability assessment.
Table 1: Technical Specifications of Contemporary Insulin Delivery Systems
| Delivery System | Typical Needle/Cannula Length | Insulin Capacity (Units) | Wear Time / Use Life | Key Technological Features |
|---|---|---|---|---|
| Syringe | 4-8 mm (common for SC) [18] | Varies (e.g., 0.3-1 mL) | Single Use | Manual injection; depth control is user-dependent. |
| Insulin Pen | 4-8 mm [18] | 150-300 (prefilled) | Single Use (cartridge) | Semi-automated bolus; some with connected features (e.g., InPen) [40]. |
| Traditional Tubed Pump | 6-10 mm (cannula) | 180-300 | 2-3 days (infusion set) [41] [30] | Continuous SC infusion; variable basal & bolus rates. |
| Omnipod 5 (Patch Pump) | ~6 mm (cannula) | 200 | 80 hours (Pod) [42] | Tubeless; integrated with AID algorithm; smartphone-controlled [43] [42]. |
| Tandem Mobi | ~6 mm (cannula) | 200 | 2-3 days (infusion set) | Hybrid (pocketable with short tube); smartphone-controlled [44] [42]. |
| Medtronic MiniMed Fit (In Dev.) | Information Missing | 300 | 7 days (proposed) | Semi-durable patch pump; rechargeable battery [43] [45]. |
Table 2: Performance Characteristics and Research Considerations
| Delivery System | Reported PK/PD Variability | Primary Advantages for Research | Primary Limitations for Research |
|---|---|---|---|
| Syringe | High (injection depth & technique dependent) [18] | Low cost; simple to administer; full control over injection speed. | High risk of IM injection with longer needles; greatest user-dependent variability. |
| Insulin Pen | Moderate (technique dependent) | Standardized dose delivery; reduced user error vs. syringe; connected pens provide dose logging [40]. | Requires patient training for consistent SC delivery; potential for dose inaccuracy. |
| Traditional Tubed Pump | Moderate (infusion set dependent) [41] | Mimels continuous physiological delivery; stable basal platform. | Site inflammation & occlusion risk increase variability over >2 days [41]. |
| Patch Pumps (e.g., Omnipod 5) | Moderate (similar to tubed pumps) | Eliminates tubing as a variable; integrated AID allows for standardized response testing [43] [42]. | Fixed wear time; form factor may limit site selection; algorithm may confound pure PK studies. |
| Emerging Pumps (e.g., Mint, Sigi) | To be determined | New designs aim for simpler operation and reduced size [43] [45]. | Lacking real-world PK/PD data; timelines for commercial/research availability are uncertain. |
Mechanisms of Absorption Variability and Intramuscular Delivery
The Subcutaneous Insulin Pathway and Site of Delivery
Insulin absorption kinetics are determined by the formation of a subcutaneous depot and the subsequent diffusion of insulin to the vasculature. Unintentional intramuscular (IM) delivery bypasses this pathway, leading to rapid and erratic absorption.
The diagram above illustrates the standard subcutaneous pathway and the confounding effect of intramuscular delivery. Upon subcutaneous administration, insulin forms a depot where it must diffuse through the extracellular matrix, dissociate into monomers, and cross the capillary endothelium to reach systemic circulation [18]. This process is influenced by local blood flow, the composition of the subcutaneous tissue, and the insulin formulation itself [46] [18]. Intramuscular injection, a key confounder in absorption studies, creates a direct and highly variable pathway into the bloodstream or lymphatic system, bypassing the rate-limiting steps of subcutaneous absorption and leading to faster, less predictable pharmacokinetics [18].
The Inflammatory Response to Catheters
Continuous subcutaneous insulin infusion (CSII) presents a unique variability factor: the localized inflammatory response to the indwelling catheter. A porcine model study demonstrated that both Teflon and investigational catheters were surrounded by a layer of inflammatory tissue, the composition and thickness of which varied over time [41]. This inflammatory layer can act as a mechanical barrier to insulin flow, contributing to the high intra- and inter-subject variability in insulin absorption observed, particularly with increased catheter wear-time [41]. Catheter insertion method also plays a role, with manual insertion of a sharp-tipped catheter causing more tissue trauma and variability than an automated insertion of a 90° Teflon cannula [41].
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Materials for Investigating Insulin Absorption
| Item | Function in Research |
|---|---|
| Ultrasound Imaging | Gold standard for measuring subcutaneous adipose tissue thickness and verifying injection depth to prevent IM delivery [18]. |
| Short Pen Needles (4-6 mm) | Standardized research tool to consistently achieve subcutaneous delivery and minimize IM risk across study participants [18]. |
| Stable-Labeled Insulin (e.g., 125I) | Allows for precise, direct pharmacokinetic tracking of insulin absorption from the depot site in mechanistic studies [18]. |
| Continuous Glucose Monitor (CGM) | Provides high-resolution interstitial glucose data for calculating pharmacodynamic endpoints like Time-in-Range and hypoglycemic events [44]. |
| Electrochemically-Enabled Blood Ketone Meter | Critical for patient safety in pump failure studies; used to detect ketoacidosis resulting from infusion occlusions [30] [47]. |
| Liquid Chromatography-Mass Spectrometry (LC-MS) | Enables highly specific and sensitive measurement of plasma insulin concentrations for detailed pharmacokinetic analysis. |
| Teflon Catheters & Automated Inserters | Research-grade infusion sets designed to minimize tissue trauma and associated inflammatory response during CSII studies [41]. |
| Local Skin-Warming Device | Tool to experimentally manipulate and study the effect of local blood flow on the rate of insulin absorption [18]. |
Experimental Protocols for Absorption Variability Research
Protocol: Evaluating Insulin Pharmacokinetics in a Swine Model
This protocol is adapted from a pilot study investigating catheter-related variability [41].
Objective: To assess the intra- and inter-subject variability of insulin absorption pharmacokinetics (PK) and the local tissue response to different CSII catheter designs over a 5-day wear-time.
Materials:
- Animal model (e.g., swine, n=6)
- Commercial (CC) and Investigational (IC) CSII catheters
- Insulin pumps (e.g., Animas OneTouch Ping)
- Rapid-acting insulin (e.g., U-100 Insulin Lispro)
- Central Venous Catheters (CVC) for blood sampling
- YSI-style reference glucose analyzer
- ELISA kits for insulin assay (e.g., Mercodia Iso-insulin ELISA)
- Materials for histological analysis (fixative, stains)
Methodology:
- Surgical Preparation: Implant CVCs in the innominate vein/distal superior vena cava under general anesthesia and aseptic technique for centralized blood sampling.
- Catheter Implantation: Insert multiple CCs and ICs into the subcutaneous tissue of the abdomen using aseptic technique and manufacturer instructions. Secure catheters.
- Infusion Regimen: Connect catheters to pumps delivering a continuous low basal rate (e.g., 0.2 U/h/catheter) of insulin lispro or saline, using the same basal/bolus pattern.
- PK Studies: On Days 1, 3, and 5 of wear-time, administer a standardized 5-U bolus via specific catheters in a randomized order.
- Maintain euglycemia via a variable IV dextrose infusion.
- Collect frequent blood samples (e.g., every 10 min for ~2h, then every 15 min) via CVCs pre- and post-bolus.
- Sample Analysis: Centrifuge blood samples to plasma. Measure insulin concentration using a validated specific ELISA.
- Tissue Analysis: Excise tissue surrounding catheters after the 5-day period for histological staining (e.g., H&E) to visualize inflammation and tissue morphology.
- Data Analysis: Calculate PK parameters (Cmax, tmax, AUC, AUC60). Perform statistical analysis of PK variability and correlate with histopathological findings.
Protocol: Clinical Study of Exercise-Induced Absorption Variability
This protocol is based on factors reviewed in Frontiers in Endocrinology [18].
Objective: To quantify the effect of moderate-intensity exercise on the absorption kinetics of rapid-acting insulin analogs administered via different delivery systems (pen vs. pump) into different anatomic sites.
Materials:
- Human participants with T1D
- Insulin pens with 4mm/5mm needles and CSII pumps
- Rapid-acting insulin (e.g., Insulin Aspart, Lispro, Fiasp)
- Continuous Glucose Monitors (CGM)
- Treadmill or cycle ergometer
- Standardized meal kits
- Blood ketone meter
Methodology:
- Screening: Recruit participants and confirm subcutaneous fat thickness at proposed injection sites (abdomen, thigh) via ultrasound to exclude candidates at high risk for IM injection.
- Study Design: A randomized, crossover design where participants undergo different test conditions on separate days:
- Condition A (Pen-Rest): Insulin bolus via pen into thigh, resting period.
- Condition B (Pen-Exercise): Insulin bolus via pen into thigh, followed by moderate-intensity exercise.
- Condition C (Pump-Rest): Insulin bolus via pump (abdomen site), resting period.
- Condition D (Pump-Exercise): Insulin bolus via pump (abdomen site), followed by moderate-intensity exercise.
- Experimental Procedure:
- Participants present fasted and with baseline euglycemia.
- Administer a standardized insulin bolus dose.
- For exercise conditions, commence 45 minutes of moderate cycling (50-60% VO2max) 60 minutes post-bolus.
- Monitor glucose continuously via CGM and take periodic capillary blood samples for ketone and precise glucose measurement.
- Data Analysis: Compare CGM tracings and calculate PK parameters (Cmax, tmax) between conditions. Primary outcomes are the rate of glucose decline and the incidence of hypoglycemic events.
Troubleshooting Guides and FAQs
FAQ 1: What are the primary mechanical failure points in insulin pumps that can confound research data?
- Infusion Set Occlusion: A blocked or kinked cannula prevents insulin delivery, causing hyperglycemia. The pump's occlusion alarm may not always trigger immediately [30].
- Bent Cannula: During insertion of a flexible catheter, the cannula may bend upon hitting resistance (e.g., muscle fascia), partially or fully impeding flow [30].
- Insulin Degradation: Exposure of the insulin in the pump reservoir to high temperatures can cause partial degradation, reducing its biologic activity and leading to unexplained hyperglycemia [30].
- Patch Pump Adhesion Failure: Pods or patches can detach prematurely due to moisture, poor adhesion, or snagging, interrupting insulin delivery.
FAQ 2: In a clinical research setting, how should we manage unexplained hyperglycemia in a study participant using a pump?
Follow a systematic troubleshooting protocol to identify the source [30] [47]:
- Assess for Diabetic Ketoacidosis (DKA) Risk: If the participant is vomiting or showing signs of DKA, seek emergency medical care immediately.
- Check for Ketones: If no acute DKA signs are present, instruct the participant to check blood ketones.
- If ketones are elevated (≥ 0.6 mmol/L): This suggests a significant interruption of insulin flow. Instruct the participant to administer an immediate correction bolus via an insulin syringe or pen (not the pump), replace the entire infusion set, reservoir, and use a new insulin vial [30] [47].
- If ketones are negative/normal: The participant may attempt a correction via the pump. If glucose does not decline within 2 hours, treat as an infusion set failure and replace the set [30].
- Inspect the System: Check the pump history log for alarms, examine the infusion site for leakage or inflammation, and verify the insulin in the reservoir is not expired or exposed to extreme temperatures.
FAQ 3: What is the recommended procedure for a complete pump failure during a study?
Having a written backup plan is critical for participant safety and data integrity [47].
- Immediate Insulin Transition: Switch to multiple daily injections (MDI) using a basal-bolus regimen.
- Basal Insulin: Adminiate a dose of long-acting insulin (e.g., glargine, detemir). The daily basal dose can be estimated from the participant's total daily insulin dose (TDI) via pump (typically 40-50% of TDI) [47].
- Bolus Insulin: Use rapid-acting insulin injections to cover meals and correct hyperglycemia. Be cautious of "insulin-on-board" as the pump's active insulin calculator will be unavailable.
- Contact Pump Manufacturer: Report the failure and arrange for a replacement pump.
- Pump Reconnection: When the new pump arrives, it can be reconnected 24 hours after the last injection of long-acting insulin to avoid insulin stacking [47].
- Documentation: Meticulously document the failure, interventions taken, and all insulin doses administered for data analysis purposes.
Identifying and Correcting Clinical Complications like Lipohypertrophy and Erratic Glycemia
FAQs on Lipohypertrophy Fundamentals for Researchers
Q1: What is the precise pathological definition of lipohypertrophy (LH) in a research context? Lipohypertrophy is defined as a tumor-like lump of adipose tissue at the site of repeated insulin injection or infusion. Histologically, it is characterized by a significant increase in the number and size of macro-adipocytes and the presence of dense fibrous tissue, which alters the local architecture of the subcutaneous space [48] [37].
Q2: What is the estimated prevalence of LH in insulin-treated populations, and why do reported figures vary? Reported prevalence rates vary widely, from 11.1% to 73.4% in recent studies, with specific research in China indicating a range of 53.1% to 73.4% [48]. A meta-analysis of 26 studies involving 12,493 participants determined a pooled prevalence of 38% (95% CI 29–46%), with higher rates observed in patients with type 2 diabetes (49%) compared to those with type 1 diabetes (34%) [49]. This variability is attributed to differences in study populations, detection methods (palpation vs. ultrasound), and the experience of the examiners [48] [49].
Q3: What are the primary pathogenic mechanisms behind LH development? The pathogenesis is multifactorial and not fully elucidated. The dominant theory is the local anabolic effect of insulin, which promotes the synthesis of fats and proteins in adipocytes [48]. Other proposed mechanisms include:
- Immunological Factors: The role of anti-insulin antibodies (IgG or IgE) is under investigation, with one European study showing a positive relationship between antibody levels and LH [48].
- Mechanical Trauma: Repeated trauma from needle sticks, especially with needle reuse, is a significant contributor [50].
- Insulin Formulation: Some evidence suggests that regular insulin carries a 3.2-fold higher risk of LH compared to rapid-acting analogs, potentially due to the faster absorption and reduced local exposure time of the latter [48].
Q4: How does injecting insulin into LH tissue alter its pharmacokinetics (PK) and pharmacodynamics (PD)? Glucose clamp studies have quantified a statistically significant 26% reduction in insulin absorption and a 24% lower pharmacodynamic effect when insulin is injected into LH tissue compared to healthy subcutaneous tissue. Critically, the within-subject variability for insulin PK was up to 5-fold higher in LH tissue, leading to erratic and unpredictable absorption [51]. Meal tests confirm this, showing substantially higher postprandial blood glucose excursions following injection into LH sites [51].
Troubleshooting Guides for LH-Related Experimental Challenges
Guide 1: Troubleshooting Erratic Insulin Absorption Data
| Symptom | Possible Cause | Investigative Action | Corrective Action |
|---|---|---|---|
| High glycemic variability & unexplained hypoglycemia in study subjects | Insulin injection into LH tissue leading to unpredictable release [48] [37] | - Palpate all injection/infusion sites for lumps [48].- Confirm with ultrasound imaging for deeper structural changes [37]. | - Train subjects to avoid LH areas for injections [48] [37].- Implement and verify strict site rotation protocols [50]. |
| Significant, unexplained differences in postprandial glucose excursions between study cohorts | LH-induced blunted and variable insulin action [51] | - Standardize meal tests and compare PK/PD responses between injections in healthy vs. LH tissue. | - In study design, stratify subjects based on presence/absence of LH at baseline. |
| Rising HbA1c & increased insulin requirements in longitudinal studies | Impaired insulin absorption from LH sites, leading to apparent insulin resistance [48] [50] | - Track insulin doses and correlate with injection site health.- Use CGM to document glycemic variability. | - Re-educate subjects on proper injection technique and site rotation.- Audit and control for needle reuse. |
Guide 2: Troubleshooting LH Detection and Quantification In Vivo
| Symptom | Possible Cause | Investigative Action | Corrective Action |
|---|---|---|---|
| Inconsistent LH diagnosis between raters | Reliance on palpation without standardized technique [48] | - Implement a unified palpation protocol: apply pressure, compare skin thickness, perform vertical/horizontal fingertip movements, and use a pinching maneuver [48]. | - Train all research staff on the standardized technique.- Use high-frequency ultrasound as an objective, more sensitive measure (30% more sensitive than palpation) to resolve disputes [37]. |
| Failure to identify non-protruding LH lesions | LH nodules that are flat and not visible to the naked eye [37] | - Employ systematic palpation and pinching of all potential injection areas, changing the subject's body position to make subtle lesions more detectable [37]. | - Incorporate routine ultrasound screening into study check-ups to identify lesions before they are palpable [37]. |
| Subject non-compliance with injection site rotation | Pain reduction when injecting into LH tissue, leading to preference for these sites [48] [37] | - Interview subjects and directly observe their injection technique and site selection. | - Provide repeated, structured education on the impact of LH on insulin action and glucose control [37]. |
Experimental Protocols for LH Research
Protocol 1: Quantitative Assessment of Insulin PK/PD in LH vs. Non-LH Tissue
Objective: To quantify the differences in insulin absorption and action between lipohypertrophic and normal subcutaneous tissue.
Methodology:
- Subject Selection: Recruit insulin-treated subjects with and without clearly identified LH lesions.
- Study Design: A randomized, cross-over glucose clamp study.
- Intervention: Administer a standardized dose of rapid-acting insulin analog into both LH tissue and contralateral healthy tissue on separate study visits.
- Primary Outcomes:
- Pharmacokinetics: Serial measurements of serum insulin concentrations.
- Pharmacodynamics: Glucose infusion rate (GIR) required to maintain euglycemia during the clamp.
- Secondary Outcome: A standardized meal test to assess postprandial glucose excursions following injections into the different tissue types [51].
Key Measurements:
AUC_Insulin(Area Under the Curve for serum insulin concentration)T_Max_Insulin(Time to maximum insulin concentration)AUC_GIR(Area Under the Curve for Glucose Infusion Rate)CV_PK(Coefficient of Variation for PK parameters as a measure of variability)
Protocol 2: Histological and Ultrastructural Characterization of LH
Objective: To characterize the structural and cellular composition of LH tissue.
Methodology:
- Sample Acquisition: Obtain biopsy specimens from LH and adjacent healthy subcutaneous tissue (from consenting subjects undergoing relevant procedures).
- Histological Analysis:
- Stain tissue sections with Hematoxylin and Eosin (H&E) to assess general morphology and adipocyte size.
- Use Masson's Trichrome stain to identify and quantify collagen deposition (fibrosis).
- Advanced Imaging: Employ scanning electron microscopy (SEM) to examine the ultrastructural details of the adipose tissue and vasculature [37].
Key Measurements:
- Mean adipocyte diameter and size distribution.
- Percentage of tissue area occupied by fibrous matrix.
- Qualitative description of vascular density and integrity.
Signaling Pathways and Experimental Workflows
Diagram Title: Pathogenesis of Lipohypertrophy and Clinical Consequences
Diagram Title: Workflow for PK/PD Study in LH Tissue
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in LH Research |
|---|---|
| High-Frequency Ultrasound | Gold-standard for objective detection and quantification of subcutaneous tissue structural changes, including increased echo density and nodule formation [48] [37]. |
| Rapid-Acting Insulin Analogs (e.g., Insulin Aspart, Lispro) | The standard insulin formulation used in PK/PD studies to minimize confounding factors related to insulin absorption speed; shown to have a lower risk of inducing LH compared to regular insulin [48]. |
| Glucose Clamp Apparatus (Pumps, Glucose Analyzers) | Essential for conducting hyperinsulinemic-euglycemic clamps, the reference method for precisely quantifying insulin sensitivity and pharmacodynamic action [51]. |
| Continuous Glucose Monitoring (CGM) Systems | Used to document the real-world impact of LH on glycemic variability, time-in-range, and hypoglycemic events in outpatient studies [37] [52]. |
| Specific ELISA/EIA Kits | For measuring serum insulin levels (PK) and anti-insulin antibodies to investigate immunological contributions to pathogenesis [48]. |
| Histology Stains (H&E, Masson's Trichrome) | For characterizing adipocyte morphology and fibrosis levels in biopsied LH tissue samples [37]. |
In preclinical and clinical research involving subcutaneous drug delivery, the consistency of the injection process is a critical determinant of data reliability. For subcutaneously administered compounds, particularly insulin, the specific characteristics of the injection site profoundly influence absorption kinetics and pharmacodynamic response. Variability in absorption can introduce significant confounding effects, compromising the interpretation of experimental results. The physiological properties of the subcutaneous tissue are not uniform; factors such as local adipose tissue thickness, the presence of lipohypertrophy, and local blood flow can differ both between subjects and at different sites within the same subject. Routine visual inspection and palpation provide a simple, non-invasive methodology to standardize injection site selection, thereby reducing a major source of pharmacokinetic and pharmacodynamic variability. This practice is foundational for ensuring the integrity of data in studies investigating insulin action, insulin resistance, and the efficacy of new insulin formulations or delivery technologies.
FAQ: Addressing Key Researcher Questions
Q1: Why does injection site selection matter in a research setting? In a research context, inconsistent injection site selection directly introduces absorption variability, which can obscure true treatment effects. Insulin absorption rates differ anatomically; it is generally absorbed faster from the abdomen compared to other sites [17]. Furthermore, injection into areas of lipohypertrophy (LH)—localized swelling of adipose tissue from repeated injections—can delay insulin absorption and diminish its action, leading to unpredictable glucose-lowering effects [17]. For researchers, this variability increases data noise, necessitating larger sample sizes to achieve statistical power and potentially masking the physiological impact of an experimental intervention.
Q2: What is the clinical consequence of unintentional intramuscular (IM) insulin injection? Unintentional IM injection is a significant source of experimental error. Insulin absorption from an IM depot is more rapid and variable than from a subcutaneous depot. This effect is exacerbated when the injected muscle is exercised shortly after injection [18]. In a study with 125I-labeled insulin, moderate-intensity cycling significantly increased the rate of insulin absorption from an IM thigh injection but not from a subcutaneous one, resulting in a substantially greater fall in blood glucose [18]. This can lead to profound hypoglycemia in clinical settings and, in research, creates a severe confounding variable that disrupts the standardized assessment of an insulin's pharmacodynamic profile.
Q3: What are the best practices for ensuring a true subcutaneous injection? To ensure consistent subcutaneous delivery and avoid intramuscular deposition, researchers should adhere to the following protocols:
- Needle Length: Use shorter needles (4 mm or 5 mm) are recommended to minimize the risk of IM injection [18].
- Skin Fold Technique: If using longer needles, a skin fold should be lifted and the injection given at a 90-degree angle. The skin fold should be released before the needle is withdrawn.
- Site Rotation: Implement a systematic site rotation plan to prevent the development of lipohypertrophy, which alters local tissue properties and absorption [17].
- Palpation: Before injection, the proposed site must be palpated to check for pre-existing lumps, bruises, or areas of tissue hardness.
Q4: How do physiological factors at the injection site influence insulin absorption? Multiple physiological factors can alter absorption kinetics, and researchers must control for them:
- Local Temperature: Heat (e.g., sauna, hot bath) increases the rate of absorption, while cold slows it down [17] [18].
- Local Blood Flow: Factors that increase local capillary blood flow, such as massage or exercise of the nearby muscle, can accelerate insulin absorption [17].
- Tissue Thickness: An inverse relationship exists between subcutaneous adipose tissue thickness and the rate of insulin absorption [18].
Troubleshooting Guide: Injection Site Anomalies
Table 1: Identifying and Addressing Common Injection Site Issues
| Observation | Probable Cause | Impact on Research Data | Corrective Research Action |
|---|---|---|---|
| Lipohypertrophy (Rubbery or firm tissue swelling) | Repeated injection or infusion set placement in the same area. | Delayed and variable insulin absorption; reduced and unpredictable pharmacodynamic effect [17]. | Palpate sites pre-injection; exclude hypertrophied areas from study; implement strict site rotation. |
| Lipoatrophy (Localized loss of fat tissue) | Immune-mediated reaction, less common with modern human insulins. | Similar to LH, causes erratic absorption and unreliable data. | Same as for lipohypertrophy; document and report as an adverse event. |
| Bruising (Ecchymosis) | Hitting a capillary upon needle insertion. | Potential for localized micro-clotting, altering drug dispersion and absorption. | Apply gentle pressure post-injection; avoid the area for future injections until resolved. |
| Erythema (Redness) | Local inflammatory or allergic response. | Increased local blood flow may accelerate absorption; immune activation may degrade insulin. | Monitor and document; consider alternative insulin formulations if persistent. |
| Unintentional IM Injection | Needle is too long for the subject's tissue thickness or injection technique is incorrect. | Rapid, variable absorption leading to exaggerated and unpredictable early insulin action [18]. | Train staff on proper technique; use shorter needles; assess tissue thickness via ultrasound if needed. |
Essential Experimental Protocols for Standardization
Protocol for Routine Injection Site Assessment
Objective: To identify and document injection site characteristics prior to and during a research study to minimize absorption variability.
- Visual Inspection: Under good lighting, examine the entire potential injection area (abdomen, thighs, buttocks, upper arms) for erythema, bruising, swelling, depression, or skin discoloration.
- Systematic Palpation: Using the pads of the fingers, systematically palpate the same areas. Apply gentle pressure to feel for:
- Soft, uniform tissue: The ideal site for injection.
- Firm, rubbery, or thickened areas: Indicative of lipohypertrophy.
- Spongy or depressed areas: Indicative of lipoatrophy.
- Tenderness or pain: May indicate inflammation or early LH.
- Documentation: Map and document all abnormal findings in the subject's research record. A body diagram is highly recommended.
- Site Selection: Choose injection sites that are at least 1-2 cm away from any identified anomaly. Implement a formal rotation schedule.
Protocol for Assessing Subcutaneous Tissue Thickness
Objective: To objectively measure subcutaneous tissue depth to guide needle selection and prevent IM injection.
- Tool: High-frequency ultrasound scanner with a linear array transducer.
- Procedure:
- Position the subject supine for abdominal measurements or seated for arm and thigh measurements.
- Apply a copious amount of ultrasound gel to the transducer.
- Place the transducer gently on the skin without compressing the underlying tissue.
- Identify the hyperechoic (bright white) skin line, the hypoechoic (darker) subcutaneous fat layer beneath it, and the hyperechoic fascia of the underlying muscle.
- Use the device's caliper function to measure the vertical distance from the skin surface to the muscle fascia.
- Decision: Select a needle length that, when combined with the skin fold technique, ensures the tip remains within the subcutaneous layer and does not approach the muscle fascia. For subjects with limited subcutaneous tissue, 4 mm needles are strongly preferred.
Visualization of Key Concepts
Injection Site Assessment Workflow
The diagram below outlines the logical decision process for injection site assessment.
Insulin Absorption Pathway & Variability Factors
This diagram illustrates the journey of subcutaneously injected insulin and key factors that influence its absorption variability.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Materials for Injection Site and Absorption Research
| Item | Function in Research | Example Application |
|---|---|---|
| High-Frequency Ultrasound | Objectively measures subcutaneous tissue thickness to guide injection depth and classify subjects. | Standardizing subject populations by tissue depth; verifying SC placement [18]. |
| Alcohol Swabs | Standardizes skin preparation by disinfecting the injection site, removing oils and microbes that could interfere. | Essential pre-injection procedure to prevent infection and ensure clean tissue entry [53]. |
| Short Pen Needles (4mm, 5mm) | Minimizes risk of intramuscular injection, reducing a major source of pharmacokinetic variability. | Recommended for all SC injections in both adults and children to ensure consistent delivery [18]. |
| Radioisotope-Labeled Insulin (e.g., ¹²⁵I) | Allows direct tracking and quantification of insulin disappearance from the injection depot. | Gold-standard for measuring local insulin absorption rates under different conditions (e.g., exercise) [18]. |
| Hyperinsulinemic-Euglycemic Clamp | The gold-standard method for quantifying whole-body insulin sensitivity. | Assessing the metabolic consequences of altered absorption (e.g., from IM injection or LH) [54]. |
| Skin Marker & Body Diagrams | For mapping and tracking injection sites and tissue anomalies over time. | Enforcing systematic site rotation; avoiding areas of lipohypertrophy [17]. |
FAQs: Lipohypertrophy and Glycemic Variability
What is lipohypertrophy (LH) and how does it cause glycemic variability? Lipohypertrophy (LH) is the most frequent local complication of insulin injections, with prevalence rates of ≥50% in multiple studies [8]. It is characterized by raised, rubbery, and often painless areas of scar tissue at injection sites. Injecting into these areas substantially affects insulin uptake and action, leading to inconsistent absorption [8]. This erratic uptake raises postprandial glucose and greatly increases glycemic variability, causing unexplained high and low blood glucose readings [8].
What is the quantitative impact of LH on insulin absorption? Injecting into LH tissue can reduce the speed of insulin absorption by roughly 25–50% and cut overall uptake by half [55]. Clinical reports confirm that this leads to erratic, often delayed insulin uptake, while moving injections to healthy skin markedly smooths glucose fluctuations [55].
How does avoiding LH areas improve glycemic control? Simply rotating injection sites away from LH-affected areas can lead to a 30% reduction in unexplained hyperglycemia and a significant smoothing of glucose profiles [55]. This practice ensures insulin is deposited into healthy subcutaneous fat, allowing for more consistent and predictable absorption and action [8].
What are the best practices for site rotation to prevent LH? To break the lipohypertrophy cycle, move injection sites at least two finger-widths (or about 2 cm) from the last spot every time, and avoid re-using a specific spot for at least 4 weeks [55]. Using a body chart or map to track injections can help uncover and avoid patterns that lead to LH [55].
Table 1: Impact of Lipohypertrophy (LH) on Insulin Pharmacokinetics
| Parameter | Value in Healthy Tissue | Value in LH Tissue | Source/Context |
|---|---|---|---|
| LH Prevalence | — | ≥50% of injecting patients | [8] |
| Insulin Absorption Speed | Normal | 25–50% slower | [55] |
| Insulin Uptake (Potency) | ~70-80% of dose reaches circulation | ~50% reduction | [55] |
| Glucose Fluctuations | Controlled | Greatly increased | [8] |
| Time to Develop LH | — | 3–5 months of repeated injections within a 2-cm circle | [55] |
Table 2: Glycemic Outcomes from Injection Technique Interventions
| Intervention | Effect on Glycemic Control | Key Metric Improved |
|---|---|---|
| Avoiding LH areas | 30% reduction in unexplained highs | Postprandial glucose, GV |
| Using 4-mm needles | Equivalent control, reduced IM risk | Glycemic variability (SD, CoV) |
| Systematic site rotation | Marked smoothing of glucose profiles | Overall glucose stability |
Experimental Protocols
Protocol 1: Assessing the Impact of Injection Site on Glycemic Variability
Objective: To quantify the difference in glycemic variability (GV) when insulin is injected into lipohypertrophic (LH) sites versus healthy subcutaneous (SC) tissue.
Methodology:
- Participant Selection: Recruit insulin-using patients with clinically confirmed LH.
- Study Design: A crossover study where each participant serves as their own control.
- Intervention: Participants are instructed to use a specific LH site for one week, followed by a rigorously rotated healthy site for another week.
- Data Collection: Use Continuous Glucose Monitoring (CGM) to collect dense glucose measurements throughout the study period.
- GV Calculation: Calculate key GV metrics from CGM data for both phases [56]:
- Standard Deviation (SD): The standard deviation of mean glucose concentrations.
- Coefficient of Variation (CoV): The ratio of SD to mean glucose (%), which corrects for the mean glucose level.
- Mean Amplitude of Glycemic Excursions (MAGE): Measures the mean of ascending or descending glucose excursions that exceed one standard deviation.
Protocol 2: Establishing a Link Between GV and Ventricular Arrhythmias (VA)
Objective: To investigate whether GV-mediated adverse outcomes are partly mediated by cardiovascular events, specifically ventricular arrhythmias (VA).
Methodology:
- Data Source: Utilize a large clinical database like the Medical Information Mart for Intensive Care IV (MIMIC-IV) [57].
- Cohort Definition: Enroll intensive care unit (ICU) patients with multiple blood glucose measurements during their stay. Exclude patients with fewer than three measurements or those with pre-existing VA [57].
- Exposure Calculation: Calculate the Coefficient of Variation (CV) of blood glucose for each patient to represent GV [57].
- Outcome Assessment: Identify incidents of VA (e.g., frequent premature ventricular contractions, ventricular tachycardia) from heart rhythm records and in-hospital death from hospital records [57].
- Statistical Analysis: Use adjusted logistic regression models to determine the association between log-transformed CV and the risk of VA and in-hospital death. Employ mediation analysis (e.g., the KHB method) to determine the proportion of GV's effect on mortality that is mediated by VA [57].
Signaling Pathways and Experimental Workflows
Mechanistic Pathway from Injection Practice to Mortality
Crossover Study on LH and Glycemic Outcomes
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Investigating Insulin Absorption Variability
| Item | Function in Research |
|---|---|
| Continuous Glucose Monitor (CGM) | Provides high-frequency glucose measurements essential for calculating robust metrics of Glycemic Variability (GV) like SD, CoV, and MAGE [56]. |
| High-Frequency Ultrasound Probe | Used to objectively identify and grade the thickness of lipohypertrophic tissue at injection sites, providing a quantitative measure of the independent variable [55]. |
| 4-mm Pen Needles | Represents the current clinical best practice for ensuring consistent subcutaneous insulin delivery, minimizing the confounding risk of intramuscular injection in control groups [8]. |
| Standardized Injection Site Mapping Tool | A body chart or digital application to systematically track injection locations, ensuring proper rotation and accurate documentation of injection sites used in the study [55]. |
| Electronic Health Record (EHR) Database (e.g., MIMIC-IV) | A large, de-identified clinical database useful for conducting observational studies on the association between GV and hard clinical outcomes like arrhythmias and mortality [57]. |
Troubleshooting Guides
Troubleshooting Unexplained Hyperglycemia in Injection Research
Problem: Unexplained hyperglycemia and erratic insulin absorption profiles during clinical research on subcutaneous insulin delivery. Application: This guide assists researchers in systematically eliminating confounding variables introduced by patient injection techniques, thereby ensuring cleaner data on intrinsic insulin pharmacokinetics and pharmacodynamics.
| Consideration | Possible Causes Related to Injection Technique | Corrective/Preventative Research Actions |
|---|---|---|
| Insulin Delivery & Integrity | Interruption of delivery; Insulin spoilage due to improper storage by patient [30] | Verify participant compliance with insulin storage protocols. In stability studies, consider replacing the insulin vial used by the participant [30]. |
| Injection Site Status | Lipohypertrophy (LH) from poor rotation; Altered absorption from needle reuse [58] [59] | Physically examine and document injection sites for LH. Rotate sites for subsequent injections if LH is suspected. In study protocols, mandate site rotation and document reuse frequency [58]. |
| Injection Technique | Incorrect injection angle (IM vs. SC); Leakage; Reused/deformed needle [58] [59] | Re-educate participant on proper injection technique and use of new needle. For studies, standardize and verify needle length and injection angle to prevent intramuscular (IM) delivery [58]. |
| Physiologic & Lifestyle Factors | Illness, stress, changes in activity/sleep [30] | Screen for these variables during participant follow-up and account for them statistically in the analysis. |
Troubleshooting Lipohypertrophy and Variable Absorption
Problem: High rates of lipohypertrophy (LH) and high variability in insulin absorption metrics among study participants. Application: LH is a major confounder in absorption research. This guide helps identify and mitigate its causes to improve data quality.
| Symptom | Likely Technique-Related Cause | Research Intervention & Protocol Adjustment |
|---|---|---|
| Unexplained hypoglycemia & glycemic variability [58] | Insulin depot in LH tissue with erratic release [58]. | Implement protocol-mandated injection site examination before each study-administered injection. Avoid LH areas for research injections. |
| Rising HbA1c with increasing insulin doses [58] | Malabsorption from LH, requiring higher doses to achieve effect [58]. | In long-term studies, standardize and monitor injection technique continuously. Record all participant-administered injection sites. |
| Visible or palpable lumps at injection sites [59] | Poor site rotation and frequent needle reuse [59]. | Educate participants on the importance of site rotation for research integrity. Use a site rotation log as part of the study data collection. |
| Increased pain on injection reported by participant | Blunted, deformed needle from reuse causing tissue trauma [59]. | In studies, provide a surplus of needles to ensure single-use compliance and verify adherence. |
Frequently Asked Questions (FAQs)
Q1: How does needle reuse directly impact the parameters we measure in insulin absorption studies? A1: Reusing needles introduces significant variability. A deformed needle tip increases puncture force, causing micro-trauma and potential pain, which can stimulate local blood flow and alter absorption rates [59]. Furthermore, clogged or deformed needles can lead to incomplete dosing and leakage from the injection site, directly compromising the accuracy of dose-response and pharmacokinetic data [58] [59].
Q2: What is the evidence-based "safe" number of times a needle can be reused without affecting research outcomes? A2: From a research perspective, any reuse introduces an uncontrolled variable. One clinical study found that reuse beyond three times significantly reduced the probability of achieving target HbA1c (≤7.5%), and reuse more than six times was associated with a higher prevalence of lipodystrophy and local complications like redness and bleeding [59]. To minimize variability, research protocols should ideally mandate single-use of needles for all participant-administered injections during the study period.
Q3: Why is poor site rotation a critical confounder in our experiments? A3: Consistent injection into the same area causes lipohypertrophy (LH)—a thickening of the subcutaneous fat. Insulin absorption from LH tissue is erratic and unpredictable, leading to increased glycemic variability and unexplained hypoglycemia [58]. This directly obscures the true absorption profile of the insulin formulation you are studying. Proper rotation ensures consistent absorption from healthy adipose tissue.
Q4: We provide initial training on injection technique; why is continuous re-education necessary? A4: Initial training is often insufficient. Studies show that knowledge and compliance with proper technique decay over time without reinforcement [58]. Continuous re-education is a key process control to maintain protocol adherence. Evidence shows that educational interventions can improve knowledge and behaviors related to injection safety, which is analogous to proper technique compliance [60]. Re-education ensures that patient behavior does not become a source of error in your data.
Q5: What are the key components of an effective injection technique re-education program for a long-term study? A5: An effective program should be structured and ongoing. Key components include:
- Structured Guidelines: Base training on established guidelines (e.g., Indonesian Diabetes Educators Association/PEDI, FITTER recommendations) [58].
- Hands-on Demonstration: Use interactive demonstrations to teach proper injection angle, site rotation, and needle handling [60].
- Regular Verification: Periodically observe participants' injection techniques to identify and correct drift from the protocol.
- Reinforcement of Rationale: Continuously explain why proper technique is critical for the validity of the research results, linking participant behavior directly to data quality.
Impact of Needle Reuse on Clinical and Research Outcomes
Table: Correlation between needle reuse frequency and key study variables. [59]
| Frequency of Needle Reuse | Prevalence of Lipodystrophy | Correlation with Local Reactions (Redness, Bleeding) | Achievement of HbA1c ≤7.5% |
|---|---|---|---|
| ≤ 3 times | 75% | Lower | Significantly more likely |
| 4 - 6 times | 87.8% | Positive Correlation | Less likely |
| ≥ 10 times | 100% | Positive Correlation | Least likely |
Effectiveness of Educational Interventions
Table: Impact of education/training on sharps injury prevention, as a proxy for technique compliance. [60]
| Study Design | Follow-up Period | Effect on Injury Rate / Risk (RR = Risk Ratio) | Certainty of Evidence |
|---|---|---|---|
| Controlled Clinical Trials (CCTs) | 2 months | RR 0.68 (95% CI 0.48 to 0.95) | Very Low |
| Cluster-RCT (Self-reported) | 12 months | RR 0.41 (95% CI 0.14 to 1.21) | Low |
| Cluster-RCT (Registry-based) | 12 months | RR 0.46 (95% CI 0.16 to 1.30) | Low |
Experimental Protocols
Protocol: Assessing the Impact of Needle Reuse on Insulin Flow and Needle Integrity
Aim: To quantitatively evaluate the physical deformation of pen needles and insulin flow characteristics after multiple uses, simulating patient behavior. Background: Reusing pen needles can cause needle breakage in the skin, clogging of the needles, and inaccurate dosing, which are critical sources of error in drug delivery research [58].
Methodology:
- Apparatus: Insulin pen, compatible pen needles, sterile container, electron microscope, precision scale, timer, standardized insulin solution.
- Procedure: a. Simulated Injection: Conduct a series of simulated injections through a synthetic skin substitute or into a sterile vial, following a standardized protocol for force and angle. b. Needle Imaging: After 1, 3, 5, and 10 uses, randomly select needles (n=3 per group) for imaging under an electron microscope. Capture images at a standardized magnification to assess tip deformity (e.g., burring, bending). c. Flow Rate Test: Using a fresh insulin pen and cartridge, attach a new needle (control) and used needles (from steps a). Depress the plunger completely and collect the expressed insulin in a pre-weighed container. Measure the time to full dose delivery and weigh the expressed insulin to check for complete delivery. Calculate the effective flow rate. d. Leakage Assessment: Visually inspect the injection site for insulin leakage after each simulated injection.
- Data Analysis: Compare needle tip deformity scores and insulin flow rates across different reuse groups using ANOVA. Correlate the number of reuses with the incidence of leakage.
Protocol: Evaluating the Efficacy of a Re-education Program on Injection Technique
Aim: To measure the improvement and retention of proper injection technique following a structured re-education intervention in a study cohort. Background: Education and training interventions may lead to small reductions in errors and can create short-term improvements in knowledge and behaviors [60]. Continuous re-education is necessary to maintain proper technique [58].
Methodology:
- Design: Prospective, observational cohort study with a pre- and post-intervention assessment.
- Participants: Study participants who self-administer injectable drugs.
- Intervention: a. Baseline Assessment: Evaluate participants' injection technique using a standardized checklist (e.g., site rotation, angle, needle handling, duration) before any intervention. b. Structured Re-education: Conduct a single-session educational workshop combining a presentation and interactive demonstrations based on established guidelines (e.g., PEDI, FITTER) [58]. c. Follow-up Assessments: Re-evaluate injection technique using the same checklist at 1, 3, and 6 months post-intervention.
- Outcome Measures: Primary: Change in overall score on the injection technique checklist. Secondary: Incidence of lipohypertrophy, participant-reported pain scores.
- Data Analysis: Use paired t-tests to compare pre- and post-intervention checklist scores. Use regression analysis to examine the relationship between technique score and clinical outcomes like lipohypertrophy.
Logical Workflow and Pathway Diagrams
Patient Barriers to Research Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential materials and tools for controlling injection technique variables in research.
| Item | Function in Research | Protocol Application Note |
|---|---|---|
| Single-Use Pen Needles | Eliminates variability from needle deformation, clogging, and inconsistent flow. | Provide a surplus to study participants to ensure compliance and document lot numbers. |
| Injection Site Mapping Cards | Tracks and enforces systematic site rotation to prevent Lipohypertrophy (LH). | Issue to each participant. Use returned cards as source data for adherence monitoring. |
| Lipohypertrophy Palpation Guide | Standardizes the identification and documentation of LH at potential injection sites. | Train research nurses on grading scales (e.g., Grade 0-3) to ensure consistent data collection across sites. |
| Injection Technique Checklists | Quantifies and verifies adherence to proper injection protocol (angle, duration, etc.). | Use during periodic site visits for observational audits of participant technique. |
| Structured Education Kits | Provides standardized re-education materials (videos, guides) to all participants. | Ensures intervention consistency. Use pre/post-testing with the checklist to measure knowledge retention. |
Leveraging Continuous Glucose Monitoring (CGM) to Identify Patterns Suggestive of Improper Injection Technique
Continuous Glucose Monitoring (CGM) systems are wearable medical devices that estimate blood glucose levels by measuring glucose concentration in the interstitial fluid just under the skin. A typical CGM system consists of three primary components: (1) a subcutaneous sensor, (2) a transmitter, and (3) a receiver or smartphone app that displays the data [61] [62]. These devices take measurements as frequently as every 1 to 5 minutes, providing researchers with rich, high-frequency temporal data on glucose fluctuations [63]. For research on insulin delivery optimization, this granular data enables the detection of absorption anomalies and pharmacokinetic variability that would be impossible to identify with traditional intermittent fingerstick measurements.
The fundamental principle underlying CGM technology involves the physiological relationship between blood glucose and interstitial fluid glucose. Since glucose reaches the interstitial fluid after it appears in the bloodstream, there is an inherent physiological lag of several minutes between blood glucose levels and interstitial glucose readings [61]. Understanding this relationship is crucial when analyzing post-injection glucose patterns, as the timing of glucose changes must be interpreted within this context. For research focused on injection technique, CGM provides the temporal resolution necessary to identify aberrant absorption patterns characteristic of improper insulin delivery.
CGM-Detectable Patterns Associated with Improper Injection Technique
Intramuscular Injection Patterns
Intramuscular (IM) insulin delivery represents a significant failure of proper injection technique that substantially alters insulin pharmacokinetics. When insulin is inadvertently delivered into muscle tissue rather than subcutaneous fat, its absorption becomes faster and more variable, particularly if the muscle is exercised after injection [8]. CGM data can reveal this phenomenon through specific pattern signatures:
- Accelerated Glucose Reduction: Following a meal or glucose challenge, CGM trend arrows may show a steeper-than-expected downward slope immediately after insulin administration, indicating abnormally rapid insulin absorption [64].
- Unexplained Hypoglycemic Episodes: Particularly when occurring after mild to moderate physical activity that engages muscles near the injection site, as exercise further accelerates insulin absorption from muscle tissue [8].
- High Glucose Variability: Increased coefficient of variation in glucose levels between days despite similar insulin doses and dietary intake, reflecting the inconsistent absorption kinetics of intramuscular deposits [65].
The table below summarizes key CGM metrics and patterns suggestive of intramuscular injection:
Table 1: CGM Patterns Indicative of Intramuscular Insulin Delivery
| CGM Metric/Pattern | Manifestation in IM Injection | Physiological Basis |
|---|---|---|
| Rate of Change Arrows | Consistently double-down (↓↓) arrows appearing rapidly after injection | Accelerated insulin absorption from muscle tissue [64] |
| Time Below Range (TBR) | Increased hypoglycemia, particularly 1-3 hours post-injection | Faster peak insulin action and unpredictable pharmacokinetics [8] |
| Glucose Coefficient of Variation | Elevated day-to-day variability (>36%) despite consistent dosing | Erratic absorption dependent on muscle activity and injection depth [65] [8] |
| Nocturnal Hypoglycemia | Increased frequency when injecting in thigh/arm before evening | Prolonged muscle activity effects during sleep position changes [8] |
Lipohypertrophy-Related Absorption Variability
Lipohypertrophy (LH)—the thickening of subcutaneous fat tissue at frequently used injection sites—represents another common complication of improper injection technique that significantly impacts insulin absorption. Studies indicate that ≥50% of insulin-injecting patients develop LH, which substantially reduces and variably delays insulin absorption [8]. CGM signatures of LH include:
- Blunted Postprandial Response: Despite appropriate insulin dosing, CGM shows elevated postprandial glucose peaks that resolve more slowly than expected.
- Delayed Onset of Action: After insulin injection into LH tissue, the initial glucose-lowering effect may be delayed by 30-120 minutes compared to healthy tissue sites.
- "Stacking" Episodes: When additional correction doses are administered due to perceived ineffectiveness of the initial dose, followed by unexpected hypoglycemia as multiple doses eventually absorb simultaneously.
The table below contrasts CGM patterns between healthy injection sites and lipohypertrophic tissue:
Table 2: CGM Patterns Associated with Lipohypertrophy-Induced Absorption Variability
| Parameter | Normal Absorption | Lipohypertrophy-Affected Site |
|---|---|---|
| Time to Initial Glucose Reduction | 15-45 minutes | 60-120 minutes [8] |
| Postprandial Glucose Excursion | Consistent pattern with same meal/insulin dose | Unpredictable, often elevated [8] |
| Glucose Management Indicator (GMI) | Consistent with A1c | May show discrepancy (GMI lower than A1c) |
| Between-Day Variability | Low to moderate (CV <36%) | High (CV often >36%) [65] |
| Time In Range (TIR) | Stable with proper dosing | Unexplained reductions despite optimal dosing |
Experimental Protocols for Injection Technique Research
Controlled CGM Analysis of Injection Variables
To systematically investigate how injection technique factors influence glucose patterns, researchers can implement the following experimental protocol:
Study Population: Include participants with type 1 or insulin-requiring type 2 diabetes who regularly use multiple daily injections. Stratify by BMI, duration of diabetes, and injection experience [66].
Intervention Design:
- Site Rotation Analysis: Participants administer insulin in randomized order to (a) healthy tissue sites, (b) clinically confirmed lipohypertrophic areas, and (c) high-risk IM sites (e.g., deltoid with longer needles).
- Needle Length Comparison: Participants use different needle lengths (4mm, 8mm) in controlled alternating sequences with standardized insulin doses.
- Injection Angle Assessment: Compare perpendicular versus 45-degree angle injections with documentation of skin folding technique.
CGM Data Collection:
- Use real-time CGM systems with minimum 5-minute sampling frequency [63].
- Collect data for 14 days per intervention arm to ensure ≥70% data capture for reliable AGP analysis [67].
- Standardize meal challenges and physical activity during observation periods.
Outcome Measures:
- Primary: Time in Range (TIR) 70-180 mg/dL, Time Below Range (TBR) <70 mg/dL, and glucose coefficient of variation [67].
- Secondary: Postprandial glucose excursions, rate of change patterns, and hypoglycemia events.
Statistical Analysis:
- Use repeated measures ANOVA to compare CGM metrics across injection conditions.
- Apply Poincaré plot analysis (delay maps) to quantify pattern differences in glucose variability [63].
Protocol for Correlating CGM Patterns with Injection Site Assessment
This protocol establishes methodology for linking specific CGM patterns to physical examination findings of injection sites:
Physical Examination Component:
- Trained clinicians palpate all potential injection sites (abdomen, thighs, arms, buttocks) to identify lipohypertrophy.
- Document location, size, and texture of any LH areas using standardized classification.
- Measure skin and subcutaneous tissue thickness using ultrasound imaging at each site.
CGM Correlation Component:
- Participants record exact injection locations using body maps for all insulin doses.
- Analyze CGM data following injections into documented sites using the 3-step approach:
Data Integration:
- Create individual Ambulatory Glucose Profile (AGP) reports for each injection site category.
- Calculate time-above-range (TAR) and time-below-range (TBR) specifically for the 6-hour periods following injections at each site type.
Diagram 1: Experimental workflow for correlating CGM patterns with injection site pathology
Advanced CGM Data Visualization for Injection Technique Research
Density Delay Maps for Variability Analysis
The "glucose-at-a-glance" visualization method, based on colorized delay maps (Poincaré plots), provides researchers with a powerful tool for assessing the structure of glucose variability resulting from improper injection technique [63]. This methodology involves:
Construction Method:
- Plot each glucose value (G~i~) against the subsequent value (G~i+1~) from CGM time series data.
- Apply non-parametric density estimation to calculate the frequency of occurrence for each point pair.
- Color-code points according to density, typically from dark red-brown (high frequency) to dark blue (low frequency).
Interpretation in Injection Technique Context:
- Consistent Absorption: Healthy injection sites typically show a compact, elliptical distribution of high-density points along the diagonal.
- Erratic Absorption: IM injection or severe LH produces a more scattered, circular distribution pattern indicating unpredictable glucose transitions.
- Dual Absorption Rates: The presence of multiple high-density clusters may indicate alternating between proper and improper technique.
Diagram 2: CGM delay map analysis for injection technique assessment
The Researcher's Toolkit: Essential Materials and Reagents
Table 3: Essential Research Toolkit for CGM-Based Injection Technique Studies
| Tool/Reagent | Specifications | Research Application |
|---|---|---|
| Real-Time CGM Systems | Minimum 14-day wear, 5-minute sampling, API data access | Continuous glucose pattern capture with sufficient resolution for absorption kinetics [61] [62] |
| Ultrasound Imaging System | High-frequency (15-22MHz) linear array transducer | Precise measurement of skin and subcutaneous tissue thickness at injection sites [8] |
| Standardized Injection Grids | Body maps with coordinate system for all potential injection sites | Precise documentation and rotation of injection locations for correlation with CGM patterns |
| Multiple Needle Lengths | 4mm, 8mm pen needles; 6mm, 12mm syringes | Controlled comparison of injection depth variables on glucose patterns [8] |
| AGP Report Software | Compatible with CGM system, full metric export capability | Standardized analysis of Time in Range, variability, and hypoglycemia patterns [67] |
| Delay Map Visualization Algorithm | Colorized density plotting with point-and-click adjunct | Advanced analysis of glucose variability structure related to absorption anomalies [63] |
Frequently Asked Questions: Technical Support for Researchers
Q: What is the minimum CGM data capture percentage required for reliable injection technique analysis? A: The international consensus on time in range recommends at least 70% of data should be captured from 14 days of sensor wear for reliable pattern analysis. Lower data capture rates may miss critical post-injection glucose patterns [67].
Q: How can researchers distinguish between injection technique problems and other causes of glycemic variability? A: Implement controlled injection site protocols where participants use different techniques in randomized order while maintaining consistent diet, activity, and insulin types. The key is comparing CGM patterns following injections under different technique conditions within the same individual, which controls for confounding variables [8].
Q: What CGM metrics are most sensitive to detecting intramuscular injection? A: The most sensitive indicators include: (1) Rate of change arrows showing double-down (↓↓) patterns within 60 minutes post-injection, (2) Increased coefficient of variation (>36%) specifically in the 4-hour periods following injection, and (3) Unexplained hypoglycemia events within 3 hours of administration, particularly following physical activity [64] [65].
Q: How can researchers validate that observed CGM patterns actually result from injection technique issues? A: Use a multi-modal validation approach: (1) Correlate CGM patterns with ultrasound measurements of injection site tissue characteristics, (2) Conduct fingerstick blood glucose measurements at critical time points to confirm anomalous patterns, and (3) Implement blinded assessment of injection sites by trained clinicians [8].
Q: What statistical methods are most appropriate for analyzing CGM data in injection technique studies? A: Recommended approaches include: (1) Repeated measures ANOVA for comparing CGM metrics across different injection conditions, (2) Poincaré plot analysis (SD1/SD2 parameters) for quantifying pattern differences in glucose variability, and (3) Mixed-effects models to account for within-subject correlations across multiple injection observations [63] [65].
Troubleshooting Guide: Addressing Common Research Challenges
Challenge: Inconsistent injection documentation by study participants Solution: Implement automated digital tracking systems such as smartphone apps with photo documentation of injection sites. Provide structured injection journals with body maps and simple coordinate systems. Conduct regular verification checks during study visits [66].
Challenge: Confounding effects of diet and physical activity on CGM patterns Solution: Standardize meal challenges (e.g., identical mixed-meal tests) during critical observation periods. Use activity monitors (accelerometers) to quantify and control for physical activity effects. Implement crossover designs where each participant serves as their own control [67].
Challenge: Differentiating lipohypertrophy patterns from insulin resistance progression Solution: Conduct controlled injections into confirmed LH tissue versus healthy tissue in the same participant. LH-affected tissue typically shows delayed and blunted glucose responses compared to healthy tissue, while insulin resistance progression shows consistent elevation across all injection sites [8].
Challenge: Accounting for inter-individual differences in insulin pharmacokinetics Solution: Establish individual baselines using standardized injection protocols in optimal conditions before introducing technique variables. Express CGM metrics as change from baseline rather than absolute values to control for inherent metabolic differences [65].
Challenge: Managing large volumes of CGM data from longitudinal studies Solution: Implement automated data processing pipelines that extract relevant metrics (TIR, TBR, TAR, CV, rate of change) following each documented injection. Use the Ambulatory Glucose Profile (AGP) report as a standardized output format for pattern recognition [67].
Measuring Outcomes: From CGM Metrics to Comparative Analyses of Insulin Regimens and Future Tech
For researchers and scientists developing interventions to mitigate intramuscular insulin delivery and absorption variability, Continuous Glucose Monitoring (CGM) provides an unparalleled window into dynamic glycemic response. The core CGM-derived metrics—Time in Range (TIR), Time Below Range (TBR), Coefficient of Variation (CV), Standard Deviation (SD), and the Mean Amplitude of Glycemic Excursions (MAGE)—serve as critical quantitative endpoints for assessing the efficacy of new formulations, delivery systems, or protocols [68] [69]. These metrics move beyond the static picture provided by HbA1c, capturing the glucose fluctuations that are a direct consequence of inconsistent insulin absorption [69] [70]. Proper application of these tools allows for the precise quantification of whether an experimental intervention successfully stabilizes the glycemic landscape, thereby de-risking the drug and device development pipeline.
Essential CGM Metrics Reference Table
The following table summarizes the key CGM metrics, their definitions, and internationally recognized targets for most non-pregnant adults with diabetes, which serve as a baseline for designing preclinical and clinical studies [68] [69].
Table 1: Core CGM Metrics for Intervention Assessment
| Metric | Definition & Calculation | Primary Research Application & Target |
|---|---|---|
| Time in Range (TIR) | Percentage of time glucose is between 70 and 180 mg/dL [68]. | Primary Efficacy Endpoint: Strongly associated with complication risk. Target: ≥70% [68] [69]. |
| Time Below Range (TBR) | Percentage of time glucose is <70 mg/dL (Level 1) and <54 mg/dL (Level 2) [68]. | Key Safety Endpoint: Measures hypoglycemia risk. Target: <4% (<70 mg/dL) and <1% (<54 mg/dL) [68] [69]. |
| Coefficient of Variation (CV) | A normalized measure of variability: (Standard Deviation / Mean Glucose) × 100% [68]. | Predicts Hypoglycemia Risk: Indicator of overall glucose stability. Target: ≤36% [68] [71] [72]. |
| Standard Deviation (SD) | The absolute measure of dispersion around the mean glucose value [68]. | Variability Assessment: Describes absolute glucose swings. Lower values indicate greater stability [73]. |
| Mean Amplitude of Glycemic Excursions (MAGE) | The arithmetic mean of glucose increases (nadir to peak) or decreases (peak to nadir) that exceed one standard deviation of the 24-hour CGM data [74]. | Quantifies Acute Excursions: Captures major swings, often used in dietary studies; no universal target, but lower is better [74]. |
Standardized Experimental Protocol for CGM Data Collection
To ensure the reliability and reproducibility of your data, adherence to a standardized CGM data collection protocol is paramount. The following workflow outlines the critical steps from sensor deployment to data analysis.
Figure 1: Workflow for standardized CGM data collection and processing in clinical research.
Detailed Methodology
- Sensor Deployment & Calibration: Deploy FDA-/CE-approved CGM systems according to manufacturer instructions. Ensure proper sensor insertion and calibration with fingerstick blood glucose measurements as required by the device to minimize sensor noise and artifact [75].
- Data Collection Period: Collect data for a minimum of 14 days to ensure a representative sample of glycemic patterns. This duration has been shown to correlate strongly with longer-term mean glucose and hyperglycemia metrics [69].
- Data Completeness Check: Before analysis, verify that the CGM system was active for at least 70% of the data collection period (approximately 10 out of 14 days). Data failing this threshold may not be representative and should be treated with caution [69].
- Data Preprocessing & Signal Quality Control: Process raw CGM data to handle missing values. Common approaches include:
- Removal of Duplicates: Eliminate entries with identical timestamps.
- Gap Identification: Flag intervals where the time between consecutive readings exceeds the expected sampling interval (e.g., 5 minutes) by a defined tolerance.
- Interpolation: Reconstruct short, missing portions of the signal using methods like Piecewise Cubic Hermite Interpolating Polynomial (PCHIP) to maintain signal shape and smoothness. Alternatively, periods with excessive missing data can be excluded entirely [75].
- Metric Calculation & Statistical Analysis: Use the cleaned, continuous glucose signal to calculate the core metrics listed in Table 1. Employ specialized open-source tools (e.g.,
QoCGMfor MATLAB,cgmquantifyfor R/Python) for standardized and batch processing of multiple data files [75].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Analytical Tools for CGM Research
| Item | Function in Research |
|---|---|
| Real-time CGM (rtCGM) Systems | Provides continuous, real-time glucose data streams, essential for acute intervention studies and hypoglycemia alarm functionality. |
| Intermittently-scanned CGM (isCGM) Systems | Offers glucose data upon scanning; suitable for longer-term observational studies assessing overall glycemic stability. |
| Open-Source Analytical Suites (e.g., QoCGM, cgmquantify) | Software packages for standardized, batch calculation of CGM metrics (TIR, CV, MAGE, etc.) from raw data exports, ensuring reproducibility [75]. |
| Ambulatory Glucose Profile (AGP) | A standardized, visual report that consolidates CGM data into a single, 24-hour period, facilitating pattern recognition and presentation of group data [68] [69]. |
| Glycemia Risk Index (GRI) | An emerging composite metric that combines hypoglycemia and hyperglycemia risk into a single score, useful for a holistic safety and efficacy assessment [68]. |
Troubleshooting Guides & FAQs
FAQ 1: In our trial of a new insulin formulation, we observed a significant improvement in Mean Glucose but no change in TIR. How should this result be interpreted?
- Answer: This is a critical finding that highlights the superiority of multi-faceted CGM metrics over averages. An improved Mean Glucose without a corresponding increase in TIR suggests that while the intervention successfully lowered overall glycemia, it may have done so by concurrently increasing both high and low glucose excursions. These opposing excursions cancel each other out in the average but are captured by TAR and TBR.
- Troubleshooting Steps:
- Investigate TAR and TBR: Analyze the components of TIR. It is likely that Time Above Range (TAR) decreased, but Time Below Range (TBR) increased, resulting in a net zero change for TIR.
- Assess Glucose Variability: Examine the Coefficient of Variation (CV). A high CV (>36%) would confirm unstable glucose control, explaining the lack of TIR improvement despite a better average [68] [71].
- Re-evaluate Dosing: The data may indicate that the dosage is too aggressive, leading to iatrogenic hypoglycemia. A dose-titration sub-study may be warranted.
FAQ 2: Our study aims to prove that a new catheter design reduces absorption variability. Why is the Coefficient of Variation (CV) a more sensitive metric than Standard Deviation (SD) for this purpose?
- Answer: CV is normalized to the mean glucose, while SD is an absolute measure. This makes CV a more reliable indicator of relative variability, especially when comparing subjects or time periods with different mean glucose levels. A CV ≤ 36% is a globally accepted target because it strongly predicts a lower risk of hypoglycemia, a common consequence of erratic insulin absorption [71] [72]. A stable absorption profile should manifest as a lower, more predictable CV.
- Troubleshooting Steps:
- Report Both SD and CV: Always report both metrics. A significant reduction in SD alongside a CV that falls below the 36% threshold provides compelling evidence for improved stability.
- Correlate with TBR: Perform a correlation analysis between CV and TBR in your dataset. A positive correlation would strengthen the argument that your intervention, by lowering CV, directly reduces hypoglycemic risk [71].
FAQ 3: What is the mechanistic link between insulin absorption variability and the CGM metrics MAGE and CV?
- Answer: Inconsistent insulin absorption from the subcutaneous or intramuscular depot creates unpredictable plasma insulin levels, which in turn cause erratic glucose disposal [41] [18]. This manifests as significant glucose excursions.
- MAGE quantifies the magnitude of these major excursions (the "peaks and valleys").
- CV quantifies the overall dispersion and instability of the glucose signal around the mean.
- Factors such as local inflammation at the infusion site, tissue properties, and temperature can alter insulin pharmacokinetics, directly increasing MAGE and CV [41] [18]. The following diagram illustrates this cascade.
Figure 2: The mechanistic pathway linking infusion site physiology to measurable CGM metrics.
FAQ 4: We encountered significant missing CGM data in a pivotal cohort. What are the accepted procedures for data imputation, and when should subject data be excluded?
- Answer: The integrity of the dataset is paramount. The consensus recommends a minimum of 70% active CGM wear time over a 14-day period for reliable data interpretation [69] [75].
- Troubleshooting Steps:
- Exclusion First: As a primary rule, pre-specify in your statistical analysis plan that datasets with less than 70% completeness will be excluded from the primary analysis.
- Judicious Imputation: For datasets just above the threshold with small, isolated gaps (e.g., a few hours), interpolation methods like PCHIP can be used to create a continuous signal for analysis [75].
- Sensitivity Analysis: Perform a sensitivity analysis to determine if the results are robust. Compare the findings from the interpolated dataset with an analysis that uses only the raw, non-interpolated data. Significant differences may indicate that the missing data was not random and the results may be biased.
Comparative Efficacy Data: Basal Insulin+GLP-1 RA vs. Premixed Insulin
The following table summarizes key quantitative findings from a 24-week prospective study comparing a switch from premixed insulin to iDegLira (a fixed-ratio combination of insulin degludec and the GLP-1 receptor agonist liraglutide) in individuals with type 2 diabetes [76].
Table 1: Glycemic and Anthropometric Outcomes: iDegLira vs. Premixed Insulin
| Metric | Premixed Insulin (Baseline) | iDegLira (After 24 Weeks) | P-value |
|---|---|---|---|
| HbA1c (%) | 7.39 ± 0.7 | 7.10 ± 0.7 | 0.045 |
| Time in Range (TIR, %) | 64.3 ± 18.0 | 71.2 ± 17.2 | 0.027 |
| Fasting Glucose (mmol/L) | 8.25 ± 2.2 | 6.92 ± 1.64 | <0.031 |
| Total Daily Insulin Dose (units) | -- | ~21 units lower | <0.001 |
| Body Weight | Baseline | Modest reduction | Reported |
Note: Data presented as mean ± standard deviation. TIR is defined as the percentage of time glucose levels are between 3.9-10.0 mmol/L. The study involved 37 participants [76].
Hypoglycemia Outcomes: The switch to iDegLira resulted in numerical reductions in both overall and nocturnal Time Below Range (TBR), though these decreases did not reach statistical significance in this cohort. The study confirmed that iDegLira did not increase the risk of hypoglycemia [76].
Experimental Protocols for Key Studies
Protocol: CGM-Based Comparison of iDegLira and Premixed Insulin
This protocol details the methodology from the prospective study that generated the data in Table 1 [76].
- 1. Objective: To evaluate the impact of switching from premixed insulin to iDegLira on glycemic control, using Continuous Glucose Monitoring (CGM) metrics, HbA1c, and anthropometric measurements.
- 2. Participant Inclusion Criteria:
- Diagnosis of Type 2 Diabetes Mellitus for >6 months.
- Treatment with two daily doses of premixed insulin (aspart 30 or lispro 25).
- HbA1c < 10%.
- Total daily insulin dose < 70 units.
- 3. Exclusion Criteria: Poorly controlled diabetes (HbA1c >10%), end-stage renal disease, pregnancy, use of medications that significantly impact glycemia (e.g., glucocorticoids).
- 4. Study Design & Intervention:
- Baseline Phase: Participants underwent 10 days of blinded CGM (Dexcom G6) while on their existing premixed insulin regimen [76].
- Intervention Phase: Participants were switched to iDegLira. The starting dose was 16 dose steps, titrated to a fasting glucose target of 5–7 mmol/L [76].
- Endpoint Phase: After 6 months (24 weeks) on iDegLira, all baseline assessments (CGM, anthropometrics, lab tests) were repeated [76].
- 5. Data Collection & Primary Outcome:
- CGM Metrics: Time in Range (TIR), Time Below Range (TBR), Time Above Range (TAR), Coefficient of Variation (CV%), and Glucose Management Indicator (GMI) were analyzed using Dexcom Clarity software [76].
- Laboratory Measures: HbA1c and fasting glucose.
- Primary Outcome: Change in HbA1c from baseline to 6 months.
Protocol: Assessing the Impact of Injection Technique and Lipohypertrophy (LH)
This protocol outlines a methodology for investigating a key confounding variable in insulin therapy research: absorption variability due to poor injection technique [37].
- 1. Objective: To determine the prevalence of Lipohypertrophy (LH) and its impact on glycemic variability and insulin dose requirements in an insulin-treated cohort.
- 2. Participant Population: Patients with type 1 or type 2 diabetes who administer insulin via subcutaneous injection [37].
- 3. LH Detection Methods:
- Visual Inspection and Palpation: Systematic examination of all recommended injection sites (abdomen, thighs, buttocks, arms). A pinching maneuver is required to identify non-visible nodules. The ability to detect LH is significantly higher in trained professionals [37].
- Ultrasound Imaging (Higher Sensitivity): B-mode ultrasound can identify structural changes in subcutaneous tissue, such as dermal thickening and increased adipocyte size, before they are visible or palpable. Ultrasound is approximately 30% more sensitive than palpation alone for LH detection [37].
- 4. Data Correlation:
- Glycemic Data: Correlate the presence and severity of LH with CGM metrics, including increased glycemic variability (CV%), elevated HbA1c, and unexplained hypoglycemic events [37].
- Insulin Requirements: Document daily insulin dose (units/kg). LH often leads to unpredictable absorption, necessitating higher total daily doses to achieve glycemic control [37].
Signaling Pathways in Insulin Action and Resistance
The following diagram illustrates the core insulin signaling pathway and key points of disruption that contribute to insulin resistance, a fundamental concept when evaluating the metabolic effects of different insulin regimens [77].
Researcher's Toolkit: Essential Reagents and Materials
Table 2: Key Reagents and Tools for Insulin Regimen and Absorption Research
| Item | Function in Research |
|---|---|
| Continuous Glucose Monitor (CGM) | Provides high-resolution, real-time interstitial glucose measurements for calculating core metrics like TIR, TBR, and glycemic variability (CV%). Essential for outcome studies [76]. |
| Dexcom G6/G7 or Equivalent | A specific CGM system known for factory calibration and high accuracy. Can be used in blinded mode to eliminate participant bias [76]. |
| Ultrasound Imaging System | High-sensitivity tool for objective detection and monitoring of lipohypertrophy (LH), a major cause of absorption variability. More sensitive than palpation [37]. |
| Fixed-Ratio Combination (FRC) Insulin | Investigational product (e.g., iDegLira). Used to test hypotheses regarding simplified regimens, improved glycemic control, and reduced hypoglycemia risk compared to traditional therapies [76]. |
| Structured Injection Technique Assessment Form | Standardized checklist for consistent visual and palpation-based screening of injection sites for LH across all study participants [37]. |
Troubleshooting Guides & FAQs
Q1: In our study, we are observing high glycemic variability (CV > 36%) in both treatment arms, confounding the regimen comparison. What are the primary non-regimen factors we should investigate? A1: The most common factor is lipohypertrophy (LH) at injection sites.
- Action: Implement a standardized injection site examination protocol using both visual inspection and palpation by a trained professional. Consider confirming findings with ultrasound for higher sensitivity [37].
- Mitigation: Re-educate participants on proper injection technique, including systematic site rotation and strict avoidance of LH areas. Reuse of needles is a major risk factor and must be prohibited [37].
Q2: Our clinical trial of a new basal insulin analogue shows promising HbA1c reduction, but CGM data reveals a high rate of nocturnal hypoglycemia. What protocol adjustments can mitigate this risk? A2: Nocturnal hypoglycemia often indicates excessive basal insulin action.
- Protocol Adjustment: Review and adjust the titration algorithm for the basal insulin. Algorithms should be designed to be less aggressive as glucose levels approach the lower target limit [78].
- Data Analysis: Correlate nocturnal hypoglycemic events with insulin-on-board from previous doses and use CGM trend arrows to refine dosing rules. Incorporating a GLP-1 receptor agonist, as in an FRC, can provide glucose-dependent insulin action and lower hypoglycemia risk [76].
Q3: When comparing a once-daily basal regimen to twice-daily premixed insulin using CGM, how should we define and analyze "Time in Range" to ensure a fair comparison? A3: Use standardized, universally accepted TIR definitions, but consider a segmented analysis.
- Standard TIR: Define TIR as 3.9-10.0 mmol/L (70-180 mg/dL) for general populations [76].
- Segmented Analysis: Break down the 24-hour period into relevant segments: postprandial periods after breakfast, lunch, and dinner (to assess prandial coverage), overnight period (to assess basal stability), and fasting period. This reveals regimen-specific strengths and weaknesses that an overall TIR might obscure [76].
Q4: We are developing a new insulin delivery protocol and need to minimize the risk of intramuscular (IM) injection in our study participants. What are the critical guidance points? A4: Intramuscular injection increases the risk of painful injections and unpredictable absorption.
- Needle Length: Use the shortest needles possible (e.g., 4mm for adults, regardless of BMI) to reliably deliver insulin to the subcutaneous space [23].
- Injection Technique: Educate participants to give injections into a raised skin fold if using longer needles (≥6mm) and to use a 90-degree angle with shorter needles. Proper site rotation is critical to prevent LH, which can also alter tissue depth and increase IM risk [37].
The Role of HbA1c and Its Limitations in Capturing Day-to-Day Glucose Fluctuations
FAQs: Understanding HbA1c and Glucose Monitoring
Q1: What is the fundamental physiological reason HbA1c fails to reflect daily glucose swings? HbA1c measures the percentage of glycated hemoglobin in red blood cells, providing a 2-3 month average blood glucose level. It does not capture acute fluctuations because it is inherently a time-averaged metric [79]. It reflects the historical presence of glucose in the blood but lacks the temporal resolution to show the peaks and valleys that occur throughout the day. This is analogous to knowing the average annual temperature of a city without understanding the daily weather extremes.
Q2: What quantitative discrepancies exist between HbA1c and continuous glucose monitor (CGM)-derived metrics in clinical studies? Recent clinical studies show a consistent and significant discordance. A 2024 retrospective observational study concluded that the measured HbA1c was, on average, 0.34% (4 mmol/mol) higher than the glucose management indicator (GMI), an estimated HbA1c derived from CGM data [80]. Furthermore, other studies have shown a clinically significant discordance of ≥0.5% in 36-43% of patients, highlighting that this is not a rare occurrence [80].
Q3: Which non-glycemic patient factors can confound HbA1c measurements and lead to misinterpretation? Several conditions affect red blood cell (RBC) turnover or glycation kinetics, thereby distorting the relationship between average glucose and HbA1c. Key confounders include [80]:
- Anemias: Iron deficiency anemia can falsely elevate HbA1c, while hemolytic anemia can lower it.
- Chronic Diseases: Chronic kidney disease (CKD), cirrhosis of the liver, and metabolic dysfunction-associated steatohepatitis (MASH) can interfere with HbA1c accuracy.
- Other Factors: Pregnancy, racial background (e.g., African American), and conditions like polycythemia also alter HbA1c independent of glycemia [80].
Q4: From a research perspective, what are the primary sources of variability in subcutaneous insulin absorption that HbA1c would not capture? Variability in insulin absorption is a major source of day-to-day glucose fluctuations that HbA1c obscures. Key factors include [41] [18]:
- Injection Site & Tissue Properties: Insulin absorption is influenced by injection depth (subcutaneous vs. intramuscular), local adipose tissue thickness, and skin temperature. Thicker subcutaneous tissue is associated with a slower, more tempered absorption profile [18].
- Local Inflammation: The insertion of infusion catheters for insulin pumps causes an acute inflammatory response. The formation of a layer of inflammatory tissue around the cannula can act as a mechanical barrier to insulin flow, leading to high intra- and inter-subject absorption variability over time [41].
- Physiological Shifts: Physical exercise increases subcutaneous blood flow, which can accelerate insulin absorption and lead to exercise-induced hyperinsulinemia and hypoglycemia, a risk that is not discernible from an HbA1c value [18].
Troubleshooting Guides for Experimental Research
Guide 1: Investigating Inconsistent HbA1c and CGM Data
Problem: During a study, participant HbA1c values are inconsistent with GMI or other CGM metrics. Solution:
- Step 1: Verify CGM Data Integrity. Confirm the CGM device was active for at least 70-90% of the target period (e.g., 27 of 30 days). Scrutinize data for frequent sensor dropouts or calibration errors [80].
- Step 2: Screen for HbA1c-Confounding Conditions. For any participant with a significant HbA1c-GMI discrepancy (e.g., ≥0.5%), conduct laboratory tests to rule out anemia (CBC, iron studies), polycythemia, and chronic kidney disease (creatinine, eGFR) [80].
- Step 3: Analyze Glycemic Variability. Calculate the Coefficient of Variation (CV%) from the CGM data. A high CV (>36%) indicates significant glucose swings, which explains why an "average" like HbA1c is an insufficient descriptor of glycemic control [79].
Guide 2: Managing Variable Insulin Absorption in Preclinical Models
Problem: High variability in insulin pharmacokinetics/pharmacodynamics (PK/PD) in an animal model of subcutaneous insulin delivery. Solution:
- Step 1: Standardize the Injection/Infusion Protocol. Ensure consistent injection depth to avoid accidental intramuscular delivery, which has faster and more variable absorption [18]. Use automated insertion devices where possible, as manual insertion has been shown to cause more tissue trauma and variability [41].
- Step 2: Rotate Infusion/Injection Sites Systematically. To prevent local lipohypertrophy or inflammation from altering absorption, implement a strict site rotation schedule [41] [18].
- Step 3: Monitor Local Tissue Health. If using chronic infusion catheters, conduct histological analysis of the surrounding tissue after the study. Look for signs of inflammatory tissue encapsulation, which can act as a barrier to insulin absorption and explain PK variability [41].
- Step 4: Control Ambient and Local Temperature. Regulate the animal's environment, as local skin warming has been demonstrated to significantly accelerate insulin absorption kinetics [18].
Experimental Protocols
Protocol 1: Evaluating the Impact of Catheter-Induced Inflammation on Insulin PK
Objective: To quantify how acute inflammatory response to a subcutaneous catheter affects insulin absorption pharmacokinetics. Methodology:
- Catheter Implantation: Implant commercial (e.g., Teflon) and investigational catheters into the subcutaneous tissue of a preclinical model (e.g., swine) using aseptic technique [41].
- Insulin Infusion & PK Studies: Connect catheters to insulin pumps. On defined days post-implantation (e.g., Days 1, 3, and 5), administer a standardized bolus of rapid-acting insulin (e.g., 5 U). Collect frequent plasma samples to measure insulin concentration and calculate PK parameters (C~max~, t~max~, AUC) [41].
- Tissue Histology: Upon study termination, excise tissue surrounding each catheter. Process and stain with Hematoxylin and Eosin (H&E) to visualize and quantify the thickness and composition of the inflammatory tissue layer [41].
- Data Correlation: Correlate the PK parameters (e.g., a lower C~max~ or longer t~max~) with the degree of inflammatory encapsulation observed histologically.
Protocol 2: Correlating CGM-Derived Time-in-Range (TIR) with HbA1c
Objective: To establish the relationship between TIR and HbA1c in a defined cohort while controlling for confounding factors. Methodology:
- Cohort Selection: Recruit participants with diabetes (Type 1 or Type 2 on insulin therapy). Apply strict exclusion criteria: anemia, CKD, liver disease, pregnancy, and other conditions known to affect HbA1c reliability [80].
- CGM Data Collection: Participants wear a CGM device (e.g., Dexcom G6/G7, Freestyle Libre 3) for a minimum of 30 days, with a data capture requirement of ≥90% [80].
- HbA1c Measurement: Draw blood for HbA1c analysis via high-performance liquid chromatography (HPLC) within 30 days of the CGM monitoring period [80].
- Data Analysis: Calculate the participant's mean glucose, GMI, and TIR (percentage of time glucose is between 70-180 mg/dL) from CGM data. Perform linear regression analysis to correlate TIR with the measured HbA1c for the cohort.
Data Presentation
Table 1: Comparison of Key Glycemic Metrics for Research Assessment
| Metric | Definition | Method of Collection | Strengths | Key Limitations |
|---|---|---|---|---|
| HbA1c | Percentage of glycated hemoglobin reflecting average blood glucose over ~3 months [79]. | Phlebotomy; single blood draw. | Strong predictor of long-term complications; gold standard for population-level studies [79]. | Insensitive to acute hypoglycemia and hyperglycemia; confounded by RBC turnover issues [80] [79]. |
| Time-in-Range (TIR) | Percentage of time spent in target glucose range (typically 70-180 mg/dL) [79]. | Calculated from CGM data (interstitial fluid). | Captures daily glucose fluctuations; intuitive for patients; linked to microvascular risk [79]. | Requires CGM availability; does not describe hypoglycemia on its own [79]. |
| Glucose Management Indicator (GMI) | Estimated HbA1c calculated from mean CGM glucose [80]. | Derived from CGM data. | Provides an HbA1c-like value from CGM data; useful for trend analysis. | Often discordant from lab-measured HbA1c; is an estimate, not a direct measure [80]. |
| Time Below Range (TBR) | Percentage of time spent <70 mg/dL (Level 1) and <54 mg/dL (Level 2) [79]. | Calculated from CGM data. | Directly quantifies hypoglycemia exposure, a critical safety parameter. | Must be interpreted alongside TIR and Time Above Range for full context [79]. |
Table 2: Research Reagent Solutions for Insulin Absorption Studies
| Reagent / Material | Function in Research | Key Considerations |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Measures interstitial glucose concentrations nearly continuously (every 1-5 mins) to assess glycemic variability and calculate TIR [80] [79]. | Choose devices (e.g., Dexcom, Freestyle Libre) based on accuracy, form factor, and data accessibility for research. |
| Subcutaneous Infusion Catheters | Delivers insulin into the subcutaneous tissue for pump therapy studies; material and design influence inflammatory response [41]. | Teflon cannulas with automated insertion show less trauma vs. manual insertion with sharp tips [41]. |
| Rapid-Acting Insulin Analogs | Engineered insulin (e.g., Lispro, Aspart) with faster absorption profiles than human insulin; used to study PK variability [18]. | Excipients (e.g., niacinamide in Fiasp) can be used to further modify absorption kinetics [18]. |
| Bioimpedance Meter | A research tool to non-invasively monitor local impedance changes in tissue, potentially correlating with insulin bioavailability at the injection site [81]. | Can be prototyped with off-the-shelf components (e.g., ADuCM350 board); requires personalized calibration [81]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) | An invasive, high-latency method to quantitatively measure serum insulin concentrations for PK analysis [81]. | Considered a standard lab method but lacks the real-time capability for clinical decision support [81]. |
Signaling Pathways, Workflows, and Logical Diagrams
Insulin Absorption Pathway
HbA1c vs CGM Workflow
Automated Insulin Delivery (AID) systems, also known as artificial pancreas systems, represent the forefront of technological management for type 1 diabetes. These systems integrate three core components: a continuous glucose monitor (CGM) to track real-time glucose levels, an insulin pump for delivery, and a control algorithm that automatically adjusts insulin dosing based on CGM readings [82]. By mimicking the glucose-regulating function of a healthy pancreas, AID systems aim to reduce the cognitive burden of diabetes management while improving glycaemic outcomes.
The primary goal of AID systems is to maintain blood glucose within a target range (typically 3.9-10.0 mmol/L), thereby increasing Time in Range (TIR) while minimizing both hyperglycaemia and hypoglycaemia [83]. Recent systematic reviews and meta-analyses of randomized controlled trials provide robust evidence that these systems are associated with clinically meaningful improvements in multiple measures of glucose management, particularly during the nighttime, without increasing adverse events [83] [82].
Quantitative Evidence of AID System Efficacy
Clinical studies and meta-analyses provide substantial quantitative data demonstrating the efficacy of AID systems compared to standard care. The tables below summarize key findings from recent comprehensive reviews.
Table 1: Glycaemic Outcomes with AID Systems from Meta-Analyses
| Outcome Measure | Baseline with Standard Care | Improvement with AID Systems | Certainty of Evidence |
|---|---|---|---|
| Time in Range (TIR) | Mean 51% (SD 9%) [83] | +11.5% (95% CI: 9.3% to 13.7%) [83] | High |
| Nighttime TIR | Not specified | +19.7% (95% CI: 17.0% to 22.4%) [83] | Moderate |
| HbA1c | Mean 8.4% (SD 1.1%) [83] | -0.41% (95% CI: -0.58% to -0.25%) [83] | High |
| Time in Hyperglycaemia (>10 mmol/L) | Not specified | -10.8% (95% CI: -14.4% to -7.2%) [83] | Moderate |
| Time in Hypoglycaemia (≤3.9 mmol/L) | Not specified | -0.32% (95% CI: -0.60% to -0.03%) [83] | Moderate |
Table 2: Efficacy by AID System Type (Network Meta-Analysis) Data sourced from a systematic review of 46 RCTs with 4,113 participants [82]
| AID System Type | TIR Increase vs. Conventional Pump Therapy | HbA1c Improvement | Hypoglycaemia Reduction |
|---|---|---|---|
| Advanced Hybrid Closed-Loop (AHCL) | ~ +24% | Yes (magnitude not specified) | Low efficacy for <70 mg/dL and <54 mg/dL |
| Hybrid Closed-Loop (HCL) | Less than AHCL | Yes (magnitude not specified) | Low efficacy |
| Full Closed-Loop (FCL) | Less than AHCL | Yes (magnitude not specified) | Low efficacy |
The Critical Challenge of Subcutaneous Insulin Absorption Variability
AID systems administer insulin into the subcutaneous (SC) tissue, making the rate and extent of insulin absorption from this site a critical determinant of system performance. Variability in SC insulin absorption is a major source of glucose fluctuation in insulin therapy [5].
The Physiology of Subcutaneous Insulin Absorption
The absorption process involves multiple stages, each presenting opportunities for variability:
- Depot Formation: Upon injection, insulin forms a depot in the SC tissue, which consists primarily of adipocytes and an extracellular matrix (ECM) [5] [18].
- Oligomer Dissociation: Insulin molecules must dissociate from hexamers (too large for capillary absorption) into smaller dimers and monomers [5] [18].
- Capillary Absorption: Monomers and dimers are absorbed into the bloodstream through capillary walls [5].
- Lymphatic Absorption: Some larger hexamers may be absorbed via the lymphatic system [5].
Diagram: Pathway and Variability Factors in Subcutaneous Insulin Absorption
Key Factors Contributing to Absorption Variability
Table 3: Factors Influencing Subcutaneous Insulin Absorption
| Factor Category | Specific Factor | Impact on Absorption | Research Implications |
|---|---|---|---|
| Injection Technique | Injection Depth (IM vs SC) [84] [18] | Intramuscular (IM) injection increases absorption rate and variability, especially during exercise. | Need for shorter needles (4-5mm) and proper technique to minimize IM risk. |
| Site Rotation [30] | Failure to rotate sites leads to Lipohypertrophy (LH), impairing absorption. | Standardized protocols for site rotation and inspection are needed. | |
| Physiological | Local Blood Flow [18] | Increased flow (e.g., from heat, exercise) accelerates absorption. | AID algorithms must account for physiological states altering blood flow. |
| Ambient/Local Temperature [18] | Skin warming to 40°C significantly accelerates time to peak insulin action. | ||
| Subcutaneous Adipose Thickness [84] [18] | Thicker tissue is associated with slower, more tempered absorption. | Body site and individual adiposity are key variables in dosing models. | |
| Insulin Formulation | Molecular Structure (Monomer kinetics) [5] [18] | Analogues with faster disassociation rates (e.g., aspart, lispro) have more rapid onset. | Novel excipients (e.g., niacinamide) can further enhance absorption profiles. |
| Physical Activity | Exercise of Injected Muscle [18] | Dramatically increases absorption from IM injections; effect on SC is less pronounced. | Critical differentiator for activity-focused AID dosing strategies. |
Technical Support Center: Troubleshooting AID System Performance
For researchers validating AID performance or conducting clinical trials, identifying the root cause of glycaemic variability is essential. The following guide addresses common experimental challenges.
Frequently Asked Questions (FAQs) for Research Scenarios
Q1: During a closed-loop study, we observe unexpected hyperglycaemia in a participant. How should we systematically troubleshoot the cause?
A: Unexplained hyperglycaemia requires a structured investigation to determine if the cause is mechanical, physiological, or behavioural [30].
- Step 1 - Verify Insulin Delivery: Check for pump occlusions or infusion set failures. If ketones are present (≥ 0.6 mmol/L), the issue is likely interrupted delivery. Instruct to change the infusion set, tubing, and insulin vial [30].
- Step 2 - Interrogate the System: Review CGM data quality and cross-verify with blood glucose meter readings. Check for sensor skips or "???'' messages that disrupt the algorithm [85]. Examine pump settings (basal rates, correction factors) and clock accuracy [30].
- Step 3 - Consider Physiological Confounders: Inquire about stress, illness, menstrual cycle, or new medications (e.g., steroids) that induce insulin resistance [30].
- Step 4 - Assess Injection Site: Inspect for lipohypertrophy (LH) or signs of a bent cannula. Move the infusion site to an unaffected area [30].
Q2: What experimental protocols can minimize the risk of intramuscular (IM) injections and the associated absorption variability in clinical trials?
A: To standardize delivery and minimize IM risk, implement the following protocol:
- Needle Length: Mandate the use of shorter needles (4 mm or 5 mm) for all participants. An 8 mm needle has an estimated IM risk of 25% in the thigh and 9.7% in the abdomen when inserted at 90° without a pinch-up. This risk drops to 1.6% and 0.1% respectively with a 4 mm needle [84].
- Injection Angle: For individuals with lower Body Mass Index (BMI) or when using longer needles, recommend a 45-degree insertion angle to further reduce IM risk [84].
- Site Selection and Education: Train staff and participants on proper injection technique, including the use of a pinch-up where appropriate, and regular rotation of injection sites to prevent lipohypertrophy [30].
Q3: How does physical activity confound AID system performance, and how can this be managed in a study protocol?
A: Exercise poses a dual challenge: it can both increase insulin sensitivity and, under certain conditions, accelerate insulin absorption.
- Mechanism: Exercise increases local blood flow. If insulin is injected into or near an exercising muscle, its absorption can be significantly accelerated, potentially leading to hypoglycaemia [18]. This effect is most pronounced with intramuscular injections [18].
- Protocol Management:
- Standardization: In exercise studies, standardize the injection site (e.g., abdomen) away from active muscle groups.
- Site Documentation: Meticulously document the injection site and the type of exercise performed.
- Algorithm Suspension: For certain anaerobic or competitive activities that cause a sharp rise in blood glucose, the AID system's automated adjustments may be insufficient, and researchers may need to protocolize a manual "Exercise Mode" or a temporary suspension of automated corrections [30].
Q4: Our data shows consistent glucose spikes after infusion set changes. What is the underlying cause and solution?
A: This is a common phenomenon that can be addressed with procedural adjustments.
- Cause: The new tissue site may have different absorption kinetics, or there may be a minor local inflammatory response or interstitial fluid buildup that temporarily impedes insulin absorption.
- Solutions for Study Protocols: [30]
- Time the set change to occur just before a meal and administer the meal bolus after the new set is in place.
- Ensure the tubing and cannula are fully primed with insulin to eliminate any air gaps.
- Consider protocolizing a small additional bolus (e.g., 0.5-1.0 units) after inserting the new set to compensate for initial sub-optimal absorption.
Essential Research Reagents and Materials
Table 4: The Scientist's Toolkit for AID and Insulin Absorption Research
| Tool / Reagent | Function in Research | Application Example |
|---|---|---|
| Ultrasound Imaging | Precisely measures skin and subcutaneous fat thickness at injection sites. | Quantifying the distance from skin to muscle (D) to standardize injection depth and assess IM risk across different BMI groups and body sites [84]. |
| Stable Isotope-Labeled Insulins (e.g., 125I-labeled) | Allows for precise, direct tracking of insulin pharmacokinetics without confounding endogenous insulin measures. | Measuring the rate of absorption (e.g., %/min) of insulin from the injection depot under different conditions (rest, exercise, heat) in healthy and T1D populations [18]. |
| Local Skin-Warming Devices | Standardizes and manipulates local blood flow at the injection site. | Investigating the effect of increased cutaneous blood flow on the time to peak insulin concentration and the overall insulin action profile [18]. |
| Continuous Glucose Monitoring (CGM) Systems | Provides high-frequency, interstitial glucose measurements for calculating key endpoints like Time in Range (TIR) and glycaemic variability. | Serving as the primary glucose input for AID systems and evaluating the efficacy of different algorithms in outpatient RCTs [83] [82]. |
| Blood Ketone Monitors | Provides rapid, quantitative measurement of beta-hydroxybutyrate levels in blood. | A critical safety tool in troubleshooting hyperglycaemia to rapidly identify insulin deficiency and potential risk of Diabetic Ketoacidosis (DKA) during pump failure scenarios [30]. |
Diagram: Experimental Workflow for Investigating an AID-Related Hypothesis
Troubleshooting Guides and FAQs
This section addresses common technical challenges encountered during research and development in advanced insulin delivery systems.
Smart Insulin Pens and Data Connectivity
Q: During device testing, the smart pen fails to transmit dose data to the companion application. What are the initial diagnostic steps?
- A: Follow this systematic troubleshooting protocol:
- Bluetooth Verification: Confirm the smartphone's Bluetooth is enabled in the settings menu [86].
- Proximity Check: Ensure the smart pen and smart device are within 1 meter (3 feet) of each other to ensure a strong signal [86].
- Device Cycling: Power cycle the smartphone and restart the application [86].
- Connection Test: Dispense a 2-unit test dose (into the air) and check if it appears in the app's logbook. If it does, the connection is restored [86].
- Location Permissions (Android): For Android devices, the application requires location permissions to be set to "Allow all the time" for consistent Bluetooth communication. This is a standard Android requirement and does not mean the app tracks your location [86].
- A: Follow this systematic troubleshooting protocol:
Q: In a research setting, how should a prime be logged to avoid it being misinterpreted as a therapeutic dose in the dataset?
- A: The handling of primes is context-dependent:
- If you dose immediately after priming, the application algorithm should automatically detect and log the actions correctly [86].
- If too much time elapses between the prime and the dose, the prime may be logged as a dose. In this case, you must manually designate the entry as a prime within the application's logbook to ensure data integrity [86].
- A: The handling of primes is context-dependent:
Injection Technique and Absorption Variability
Q: What is the primary injection-related factor that causes high variability in insulin absorption, and how can it be mitigated in preclinical models?
- A: Intramuscular (IM) injection is a major source of erratic absorption. Insulin uptake from muscle is faster and more variable than from subcutaneous (SC) tissue, especially if the muscle is exercised [8]. The key mitigation strategy is to use the shortest needle possible that reliably delivers the dose to the SC space. A 4-mm needle inserted at a 90-degree angle is sufficient for most subjects, including those with high BMI, to deposit insulin into the SC tissue and minimize the risk of IM injection [8].
Q: How does lipohypertrophy (LH) at the injection site impact research data, and how can its effects be managed?
- A: Injecting into LH significantly alters absorption kinetics, leading to increased postprandial glucose and greater insulin uptake variability [8]. To prevent this confounder:
- Systematic Rotation: Implement and enforce a systematic injection site rotation protocol [8].
- Regular Inspection: Visually inspect and palpate injection sites at least annually, or more frequently, for signs of LH [8].
- Avoidance: Ensure all injections and catheter placements are performed outside of any identified LH areas [8].
- A: Injecting into LH significantly alters absorption kinetics, leading to increased postprandial glucose and greater insulin uptake variability [8]. To prevent this confounder:
Quantitative Data and Experimental Protocols
Pharmacokinetic Profiles of Ultra-Rapid-Acting Insulins
The table below summarizes key pharmacokinetic (PK) and pharmacodynamic (PD) data from clinical trials comparing ultra-rapid-acting insulins (URAA) to their conventional rapid-acting analogs [87].
Table 1: Comparison of Ultra-Rapid-Acting and Rapid-Acting Insulins
| Insulin Formulation | Key Excipients | Time to 50% Max Concentration (vs. Comparator) | Early Insulin Exposure (First 30 min) | Offset of Insulin Action |
|---|---|---|---|---|
| Faster Aspart (URAsp) | Niacinamide, L-arginine | 9.5 minutes earlier [87] | 2.0-fold greater [87] | 14.3 minutes earlier [87] |
| Insulin Lispro-aabc (URLi) | Citrate, Treprostinil | 14.0 minutes earlier [87] | 3.0-fold greater [87] | 37.9 minutes earlier [87] |
| Standard Insulin Aspart (IAsp) | - | Reference | Reference | Reference |
Experimental Protocol: Assessing Insulin Absorption Variability from Infusion Catheters
Objective: To evaluate the pharmacokinetic variability and local tissue response to continuous subcutaneous insulin infusion (CSII) catheters over a standard wear-time [41].
Materials:
- Animal Model: Non-diabetic, ambulatory female swine (e.g., ~68 kg) [41].
- Catheters: Commercial Teflon cannula (e.g., 6mm, 90° insertion) vs. Investigational Catheter [41].
- Insulin: Rapid-acting insulin (e.g., U-100 Insulin Lispro) [41].
- Pumps: Programmable insulin pumps to deliver basal and bolus doses [41].
- Analytical: Central venous catheters for blood sampling, YSI analyzer for blood glucose, ELISA kits for plasma insulin concentration measurement [41].
Methodology:
- Catheter Implantation: Aseptically implant multiple CSII catheters (e.g., 6 of each type per animal) into the SC tissue of the abdomen according to manufacturers' instructions [41].
- Insulin Infusion: Connect catheters to pumps primed with insulin lispro. Initiate a continuous basal infusion (e.g., 0.2 U/h per catheter) [41].
- Pharmacokinetic (PK) Studies: On days 1, 3, and 5 post-insertion, administer a standardized bolus (e.g., 5 U) through specific catheters in a randomized order [41].
- Data Analysis: Calculate PK parameters: Cmax (maximal plasma insulin concentration), tmax (time to Cmax), and AUC (Area Under the Curve for insulin concentration over time) [41].
- Histological Analysis: Upon study termination, excise tissue surrounding each catheter. Process and stain tissue sections (e.g., H&E) to visualize and score inflammation, tissue morphology, and vascularization [41].
Key Workflow Diagram: The following diagram illustrates the core experimental sequence for evaluating insulin absorption variability.
Visualizing Key Concepts and Pathways
The Impact of Injection Technique on Insulin Absorption
This diagram outlines the logical chain of events resulting from improper injection technique, leading to unreliable research data.
Mechanism of a Vascularizing Insulin Microchamber
This diagram depicts the structure and proposed mechanism of an implantable vascularizing microchamber designed to accelerate insulin absorption [88].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Investigating Insulin Delivery and Absorption
| Item / Reagent | Function / Research Application |
|---|---|
| 4-mm Pen Needles | The recommended standard for SC injection in research to minimize the risk of intramuscular (IM) delivery in subjects of all body types [8]. |
| Polytetrafluoroethylene (PTFE) Microchambers | Implantable devices with engineered pores to promote local vascularization; used to study and achieve accelerated insulin absorption in preclinical models [88]. |
| Continuous Glucose Monitors (CGM) | Wearable sensors that provide high-frequency, real-time interstitial glucose data essential for calculating glycemic outcomes like Time in Range (TIR) and variability [89] [90]. |
| Teflon SC Infusion Catheters | Standard catheters for continuous subcutaneous insulin infusion (CSII) studies; used to model insulin pump therapy and investigate catheter-related absorption variability [41]. |
| Niacinamide & Citrate/Treprostinil | Key excipients in ultra-rapid formulations (Faster Aspart & Lispro-aabc); used in mechanistic studies to understand and enhance the acceleration of insulin absorption [87]. |
| Lispro Insulin (U-100) | A rapid-acting insulin analog commonly used as the benchmark in PK/PD studies comparing new insulin formulations, devices, or delivery routes [41]. |
Conclusion
Preventing intramuscular insulin delivery and minimizing absorption variability is a critical, multi-faceted challenge in diabetes management. The evidence firmly establishes that adopting shorter needles (4mm) and proper injection techniques is fundamental to ensuring consistent subcutaneous deposition and avoiding the erratic pharmacokinetics of IM injections. Furthermore, vigilant management of injection sites to prevent lipohypertrophy is non-negotiable for stable glycemic control. Validation through CGM provides an objective means to quantify success. Looking forward, the field is moving beyond manual technique toward technological solutions. The integration of automated insulin delivery systems, smart connected devices, and advanced insulin formulations holds the promise of a future where glycemic variability is significantly reduced by design, ultimately improving outcomes and reducing the daily burden of diabetes management for patients. Future research should focus on personalized absorption profiles and the development of fully autonomous, adaptive delivery systems.
References
- 1. Skin and subcutaneous adipose layer thickness in adults ... [https://pubmed.ncbi.nlm.nih.gov/20429833/]
- 2. Intramuscular Injection - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK556121/]
- 3. Intramuscular injection [https://en.wikipedia.org/wiki/Intramuscular_injection]
- 4. Complications when administering intramuscular injections [https://www.vinmec.com/eng/blog/possible-complications-with-intramuscular-injection-en]
- 5. Factors Affecting the Absorption of Subcutaneously ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6079517/]
- 6. Subcutaneous depot formation and diffusion in autoinjector ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517325006416]
- 7. The Lymphatic System in Obesity, Insulin Resistance, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6868002/]
- 8. The Injection Technique Factor: What You Don't Know or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6640874/]
- 9. Optimising Insulin Injection Techniques to Improve ... [https://link.springer.com/article/10.1007/s13300-023-01460-y]
- 10. Troubleshooting Your Patient's Injection Technique [https://www.opatoday.com/troubleshooting-your-patients-injection-technique-a-guide-for-pharmacists/]
- 11. Evaluation of skin and subcutaneous tissue thickness at ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3784870/]
- 12. Effects of Age, Gender, BMI, and Anatomical Site on Skin ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0086637]
- 13. Measurement of mean subcutaneous fat thickness [https://www.nature.com/articles/s41598-018-34213-0]
- 14. Subcutaneous adipose tissue thickness determination ... [https://www.sciencedirect.com/science/article/abs/pii/S174680942200266X]
- 15. Measurement of subcutaneous fat tissue: reliability and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9500055/]
- 16. Repeated insulin injection without site rotation affects skin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9153835/]
- 17. Table 1. [Factors Affecting Insulin Absorption ()]. - Endotext [https://www.ncbi.nlm.nih.gov/books/NBK278938/table/insulin-pharmacology.T.factors_affecting/]
- 18. Factors Influencing Insulin Absorption Around Exercise in ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2020.573275/full]
- 19. Investigation of appropriate needle length considering skin ... [https://jphcs.biomedcentral.com/articles/10.1186/s40780-023-00288-9]
- 20. Enhanced hexamerization of insulin via assembly pathway ... [https://www.nature.com/articles/s42003-022-04386-6]
- 21. Structure-based stabilization of insulin as a therapeutic protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6052209/]
- 22. Variation in absorption of NPH insulin due to intramuscular ... [https://pubmed.ncbi.nlm.nih.gov/2404719/]
- 23. New Insulin Delivery Recommendations [https://www.sciencedirect.com/science/article/pii/S0025619616303214]
- 24. Formulation Excipients and Their Role in Insulin Stability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9633423/]
- 25. Insulin- Pharmacology, Therapeutic Regimens and ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK278938/]
- 26. The effect of intramuscular injection technique on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8092782/]
- 27. The high hourly overnight variability of insulin requirements ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12046452/]
- 28. Investigation of Association Between Insulin Injection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9871960/]
- 29. Addressing Insulin Injection Technique: A Follow-up Study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10597907/]
- 30. Insulin Pumps l Troubleshooting Hyperglycemia l danatech [https://www.adces.org/education/danatech/insulin-pumps/troubleshooting-pumps/troubleshooting-unexplained-hyperglycemia]
- 31. Evaluating the Impact of Human Factors and Pen Needle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6501541/]
- 32. Novel Robust Needle Tip Design Enables ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11874290/]
- 33. The Relationship Between Needle Size and Injection Pain [https://www.mycomedical.com/post/needle-size-and-injection-pain]
- 34. Influence of Insulin Pen Needle Geometry on Pain ... [https://www.mdpi.com/2227-7080/12/11/233]
- 35. HPC Advanced hub needle - 35% less extrusion force [https://www.tsklab.com/products/hpc-advanced-hub/]
- 36. The effect of cold needle on the development of pain and ... [https://pubmed.ncbi.nlm.nih.gov/40728686/]
- 37. Lipohypertrophy and Insulin: An Update From the Diabetes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10658672/]
- 38. Optimal Insulin Delivery [https://www.intechopen.com/chapters/60725]
- 39. Advance Insulin Injection Technique and Education with ... [https://www.guidelinecentral.com/insights/advance-insulin-injection-technique-guidelines-spotlight/]
- 40. Innovative Insulin Delivery Systems to Watch in 2025 [https://smilesmed.com/innovative-insulin-delivery-systems-to-watch-in-2025/]
- 41. Detailed Analysis of Insulin Absorption Variability and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5689134/]
- 42. Automated Insulin Delivery Systems: A Complete Guide [https://tcoyd.org/2025/04/automated-insulin-delivery-systems-comparison/]
- 43. The Most Exciting Diabetes Technology Updates [https://beyondtype1.org/top-diabetes-tech-ada-2025/]
- 44. Quarter 2 Diabetes Technology Update – August 2025 [https://www.diabetotech.com/blog/quarter-2-diabetes-technology-update-august-2025]
- 45. Diabetes tech firms preview new patch pumps, glucose ... [https://www.medtechdive.com/news/ada-conference-diabetes-new-pumps-cgms/751482/]
- 46. Bioavailability and variability of biphasic insulin mixtures [https://www.sciencedirect.com/science/article/abs/pii/S0928098711001722]
- 47. Insulin Pump Failure: A Guide for Families [https://pedsendo.org/patient-resource/insulin-pump-failure-a-guide-for-families/]
- 48. : prevalence, clinical consequence, and... Lipohypertrophy [https://pmc.ncbi.nlm.nih.gov/articles/PMC7862817/]
- 49. Prevalence of lipohypertrophy in insulin‐treated diabetes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5934253/]
- 50. Prevalence and risk factors of lipohypertrophy in insulin- ... [https://www.sciencedirect.com/science/article/abs/pii/S1262363613001213]
- 51. Lipohypertrophy – New insights into an old issue? [https://blog.profil.com/blog/lipohypertrophy-new-insights]
- 52. Research Gaps, Challenges, and Opportunities in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213545/]
- 53. Best practices for injection - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK138495/]
- 54. Injected Insulin Induces Insulin Insensitivity in Type 1 Diabetes [https://pmc.ncbi.nlm.nih.gov/articles/PMC7171956/]
- 55. Why isn't my rapid-acting insulin kicking in? Pinpointing ... [https://www.eurekahealth.com/resources/why-is-my-insulin-not-working-absorption-issues-t1d-en]
- 56. The clinical importance of measuring glycaemic variability : Utilising... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11646482/]
- 57. and in-hospital death of critically ill patients and... Glycemic variability [https://cardiab.biomedcentral.com/articles/10.1186/s12933-023-01861-0]
- 58. Expert Opinion on Addressing the Gap in Injection Technique ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10725793/]
- 59. Effect of Reuse of Insulin Needle on Glycaemic Control and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9302413/]
- 60. Education and training for preventing sharps injuries and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8094230/]
- 61. Continuous Glucose Monitoring (CGM): What It Is [https://my.clevelandclinic.org/health/articles/continuous-glucose-monitoring-cgm]
- 62. Continuous Glucose Monitoring - NIDDK [https://www.niddk.nih.gov/health-information/diabetes/overview/managing-diabetes/continuous-glucose-monitoring]
- 63. “Glucose-at-a-Glance”: New Method to Visualize the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4455408/]
- 64. Dexcom G7 Arrow Meanings for Better Treatment Decisions [https://www.dexcom.com/en-us/all-access/dexcom-cgm-explained/trend-arrow-and-treatment-decisions]
- 65. Trends in Total Daily Dose and Variability of Insulin ... [https://pubmed.ncbi.nlm.nih.gov/40803607/]
- 66. Incorrect Insulin Administration: A Problem That Warrants ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4714726/]
- 67. A Simple 3-Step Approach to CGM Data Interpretation | Dexcom [https://ca.provider.dexcom.com/articles/simple-3-step-approach-cgm-data-interpretation]
- 68. Core Glycemic Metrics Explained. TIR, TBR, TAR, GMI, CV, ... [https://www.adces.org/education/danatech/glucose-monitoring/continuous-glucose-monitors-(cgm)/glycemic-metrics--an-overview]
- 69. Clinical Targets for Continuous Glucose Monitoring Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6973648/]
- 70. Minimizing Glycemic Fluctuations in Patients with Type 2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5647495/]
- 71. Clinical significance of coefficient of variation in continuous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11527802/]
- 72. Prevent hypoglycaemia when using automated insulin ... [https://www.sciencedirect.com/science/article/abs/pii/S1262363624000818]
- 73. Applications of Variability Analysis Techniques for ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2018.01257/full]
- 74. Continuous Glucose Measurements for Diet Monitoring in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343543/]
- 75. From data to insights: a tool for comprehensive Quantification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12161138/]
- 76. Switch from premixed insulin analogue to degludec-liraglutide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12626799/]
- 77. Trends in insulin resistance: insights into mechanisms and ... [https://www.nature.com/articles/s41392-022-01073-0]
- 78. Optimizing Automated Insulin Delivery Systems for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12620746/]
- 79. Time-in-range for monitoring glucose control [https://www.sciencedirect.com/science/article/abs/pii/S0168822721002771]
- 80. The Discrepancy Between Hemoglobin A1c and Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11034459/]
- 81. A micro-bioimpedance meter for monitoring insulin ... [https://www.nature.com/articles/s41598-020-70376-5]
- 82. Type 1 Diabetes and AID Systems: Meta-Analysis Proves Eff [https://www.dzd-ev.de/en/press/press-releases/press-releases-2025/type-1-diabetes-and-aid-systems-meta-analysis-proves-eff]
- 83. Automated Insulin Delivery Systems and Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12418225/]
- 84. Intramuscular risk at insulin injection sites--measurement of ... [https://pubmed.ncbi.nlm.nih.gov/25329935/]
- 85. 4. Troubleshooting Your APS - Automated Insulin Delivery [https://www.artificialpancreasbook.com/4.-troubleshooting-your-aps]
- 86. Troubleshooting - InPen™ System Support [https://www.medtronicdiabetes.com/customer-support/inpen-system-support/troubleshooting]
- 87. The Role of Ultra-Rapid-Acting Insulin Analogs in Diabetes [https://pmc.ncbi.nlm.nih.gov/articles/PMC11874134/]
- 88. Accelerated absorption of regular insulin administered via a ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0278794]
- 89. Real-Time AI-Assisted Insulin Titration System for Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12059970/]
- 90. Integration of artificial intelligence and wearable ... [https://www.nature.com/articles/s41746-025-02036-9]