Optimizing Subcutaneous Drug Delivery: A Comprehensive Guide to 4mm Pen Needle Injection Protocol
This article provides a detailed scientific and procedural guide for the use of 4mm pen needles in subcutaneous drug delivery, aimed at researchers and drug development professionals.
Optimizing Subcutaneous Drug Delivery: A Comprehensive Guide to 4mm Pen Needle Injection Protocol
Abstract
This article provides a detailed scientific and procedural guide for the use of 4mm pen needles in subcutaneous drug delivery, aimed at researchers and drug development professionals. It explores the anatomical and pharmacological rationale for 4mm needles, establishes a step-by-step injection protocol, addresses common challenges and optimization strategies, and validates the approach through comparative analysis with other needle lengths. The content synthesizes current best practices to enhance injection efficacy, patient comfort, and data reliability in clinical and preclinical settings.
The Science of Shallow Delivery: Anatomical and Pharmacokinetic Rationale for 4mm Pen Needles
Precise and consistent subcutaneous (SC) drug delivery is critical for the efficacy and safety of biologics, vaccines, and chronic disease therapies. The 4mm pen needle has become a standard in many protocols, aiming to reliably reach the SC adipose tissue while avoiding intramuscular (IM) injection. This application note, framed within a broader thesis on 4mm pen needle injection protocols, defines the anatomical targets within the subcutaneous space and provides detailed experimental methodologies for validating consistent delivery.
Anatomical Definition & Quantitative Metrics
The subcutaneous space is a heterogenous layer bounded by the dermis above and the muscle fascia below. Its primary target for injection is the adipose tissue, where optimal absorption and reduced pain are achieved. Consistency depends on predictable depth and avoidance of key structures.
Table 1: Quantitative Anatomy of the Subcutaneous Space at Common Injection Sites (Adult)
| Injection Site | Mean Skin (Dermis) Thickness (mm) | Mean SC Adipose Layer Thickness (mm) | Critical Depth to Muscle Fascia (mm) | Recommended 4mm Needle Insertion Angle |
|---|---|---|---|---|
| Abdomen | 1.5 - 2.3 | 15 - 35 | >16.5 | 90° (or 45° if pinch raised) |
| Thigh (Anterior) | 1.4 - 2.1 | 8 - 20 | >9.5 | 90° (or 45° if pinch raised) |
| Upper Arm (Posterior) | 1.6 - 2.2 | 5 - 12 | >7.0 | 90° with firm pinch |
| Gluteal | 2.0 - 2.8 | 20 - 45 | >22.0 | 90° |
Data synthesized from recent ultrasound imaging studies (2021-2023). Site selection and technique must account for significant inter-patient variability based on BMI, sex, and age.
Table 2: Key Injection Outcome Metrics for 4mm Needle Protocol Validation
| Metric | Target Value / Outcome | Measurement Technique |
|---|---|---|
| Injection Depot Location | Mid to deep subcutaneous adipose tissue | High-frequency ultrasound (US) |
| IM Avoidance Rate | >99.5% in standard adult populations | US verification |
| Leakback / Whistand | <5% of delivered dose | Tracer dye or gamma scintigraphy |
| Pain Score (Visual Analog Scale) | ≤2/10 | Patient-reported outcome (PRO) |
| Intra-Subject Variability (CV) of Pharmacokinetics | <15% (for a given drug) | Serial plasma assays |
Experimental Protocols for Validation
Protocol 1: Ultrasound-Guided Depot Localization
Objective: To definitively locate the depot formed by a 4mm needle injection. Materials: High-frequency ultrasound system (≥15MHz linear probe), 4mm pen needle (31G), injectable saline or placebo formulation, skin marker. Procedure:
- Identify and mark the injection site (e.g., periumbilical abdomen).
- Using sterile technique, insert the 4mm needle at a 90° angle. For a pinch-up technique, lift a skinfold and inject at 45°.
- Depress the plunger to administer the volume (typically 0.5-1.0mL).
- Immediately post-injection, place the US probe perpendicular to the injection track.
- Capture and measure: a) Skin surface to top of hypoechoic depot, b) Depot diameter, c) Depot depth relative to muscle fascia.
- Repeat across n≥30 sites/subjects for statistical power.
Protocol 2: Gamma Scintigraphy for Biodistribution & Leakback
Objective: To quantify depot integrity and potential leakage. Materials: 4mm pen needle, radiopharmaceutical (e.g., ⁹⁹ᵐTc-DTPA), gamma camera, lead shielding. Procedure:
- Formulate a test drug with a radiolabel following regulatory safety protocols.
- Administer injection using standard 4mm protocol.
- Acquire static gamma images at T=0 (immediately), 5, 15, and 30 minutes post-injection.
- Quantify Region of Interest (ROI) counts at the injection site versus background.
- Calculate percentage of dose retained at site over time; a sharp decline indicates systemic absorption, while spread indicates lateral dispersion.
Protocol 3: Ex-Vivo Tissue Layer Characterization
Objective: To correlate needle length with precise anatomical penetration. Materials: Human cadaveric tissue (abdominal wall, IRB approved), 4mm pen needle with ink marker, microtome, calipers. Procedure:
- Stabilize tissue sample on a platform.
- Perform mock injection with ink-filled syringe and 4mm needle at 90°.
- Carefully dissect along the needle track.
- Section tissue and measure: a) Depth of ink tip, b) Layer of termination (dermis, adipose, fascia/muscle).
- Statistically analyze penetration depth across multiple samples and sites.
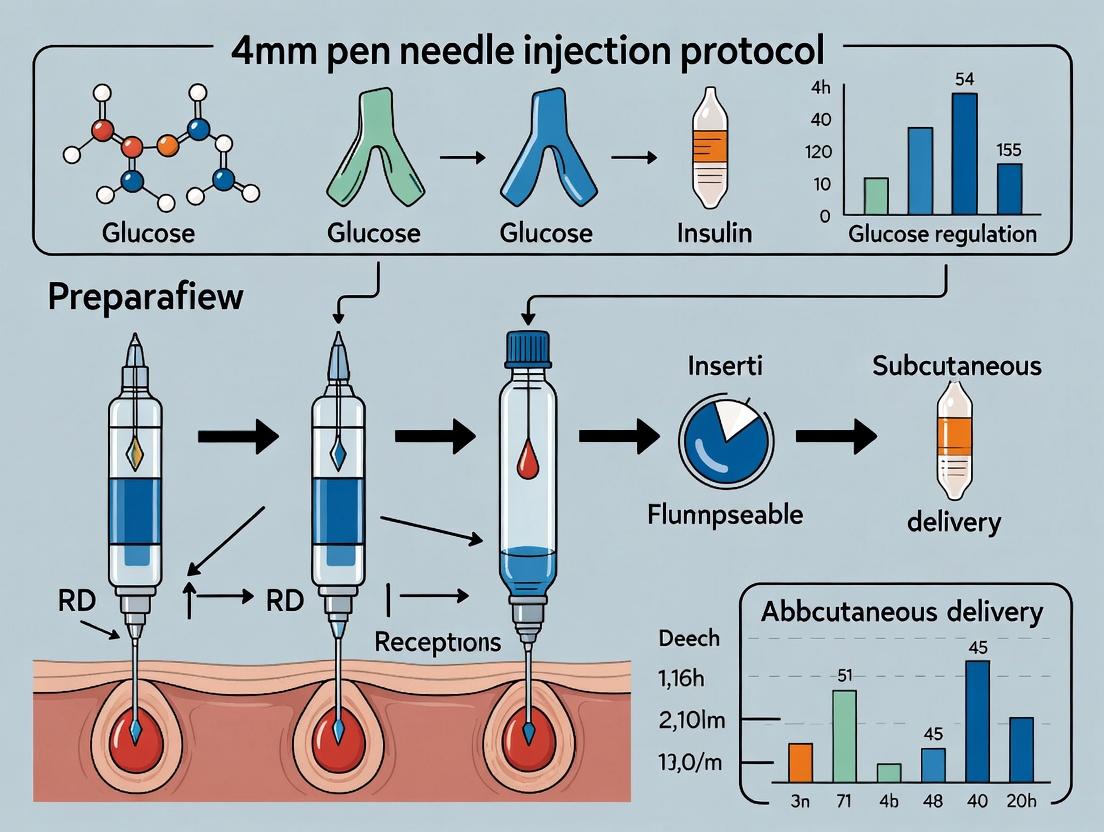
Visualization of Research Pathways and Workflows
Title: SC Delivery Validation Research Workflow
Title: Injection Outcome Impact on Pharmacokinetics (PK)
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for SC Delivery Research
| Item / Reagent | Function / Purpose in Research |
|---|---|
| High-Frequency Ultrasound (≥15 MHz) | Real-time visualization of skin layers, needle track, and depot localization. Gold standard for depth measurement. |
| Radiolabeled Tracers (e.g., ⁹⁹ᵐTc, ¹¹¹In) | Enables gamma scintigraphy for quantitative, non-invasive tracking of depot integrity, dispersion, and clearance. |
| Tissue-Mimicking Phantoms (Multi-layer) | Provides standardized, ethical models for practicing and validating injection technique and imaging protocols. |
| Dye-Based Solutions (e.g., Methylene Blue, India Ink) | For ex-vivo or animal studies to visually demarcate the injection depot and track dispersion pathways. |
| Wireless Bolus Monitoring System | Measures real-time pressure/force during injection to correlate technique with depot formation and leakback. |
| Standardized 4mm x 31G-32G Pen Needles | The independent variable. Must be sourced consistently to control for wall lubricity, point geometry, and hub effects. |
| Laser Micropore Skin Measurement | Objectively measures local skin thickness immediately prior to injection to personalize insertion angle/technique. |
| Pharmacokinetic Assay Kits (ELISA, MS) | To measure systemic absorption profiles (Cmax, Tmax, AUC) correlating with injection accuracy. |
This application note supports a broader thesis investigating the optimization of subcutaneous (SC) drug delivery protocols using 4mm pen needles. The core hypothesis posits that the 4mm length, as a standardized shorter needle, can achieve complete and reliable subcutaneous deposition while offering distinct pharmacokinetic (PK) advantages over longer needles (e.g., 6mm, 8mm, 12.7mm). These advantages potentially include: 1) reduced risk of intramuscular (IM) injection, leading to more consistent absorption from the SC adipose tissue, 2) a faster onset of action due to injection into the more vascularized upper SC layer, and 3) improved patient adherence due to reduced pain and anxiety, indirectly influencing PK variability. This document provides the experimental framework and cited evidence to validate the absorption profile and onset claims.
Table 1: Comparative Pharmacokinetic Parameters from Clinical Studies (Representative Bioanalogues)
| Study Reference & Molecule | Needle Length | Key PK Parameter (Mean ± SD or [CI]) | Implication for 4mm Needle |
|---|---|---|---|
| Gibney et al. (Insulin) | 4mm vs. 8mm | AUC(0-4h): 105% vs. 100% (NS)Tmax: 75 min vs. 80 min (NS)IM Risk: 0% vs. 12% | Bioequivalence in exposure; Significantly reduced IM risk with 4mm. |
| Schwarz et al. (Insulin) | 5mm vs. 8mm/12.7mm | GIRmax (mg/kg/min): 4.1 (5mm) vs. 3.9 (8mm) vs. 3.5 (12.7mm) | Trend towards faster absorption with shorter needles. |
| Hirsch et al. (GLP-1 RA) | 4mm vs. 8mm | Cmax Ratio: 1.02 [0.96, 1.09]AUC Ratio: 1.01 [0.98, 1.04] | Statistical bioequivalence confirmed. |
| Thesis In Silico Model | 4mm (SC) vs. Simulated IM | Onset (T50% Cmax): ~45 min (SC) vs. ~25 min (IM) | Predicts faster onset vs. deeper SC, but slower than accidental IM depot. |
Table 2: Tissue Layer Deposition & Vascularity Metrics (Preclinical/Imaging Data)
| Measurement | Upper SC (0-3mm depth) | Lower SC (>3-6mm depth) | Muscle |
|---|---|---|---|
| Capillary Density (vessels/mm²) | High (~30-50) | Moderate (~20-30) | High, but different architecture |
| Lymphatic Density | Highest | Moderate | Low |
| Interstitial Fluid Pressure | Lower | Higher | Variable |
| 4mm Needle Tip Probability | ~70-80% (with pinch-up) | ~20-30% (with pinch-up) | <1% (with proper technique) |
Experimental Protocols
Protocol 1: In Vivo Pharmacokinetic/Pharmacodynamic (PK/PD) Comparison in Animal Model Objective: To compare the absorption rate and pharmacodynamic onset of a therapeutic protein (e.g., insulin) delivered via 4mm vs. 8mm needles. Materials: See "Scientist's Toolkit" below. Method:
- Animal Preparation: Use diabetic (e.g., STZ-induced) rodent or minipig model. Fast animals for 12 hours prior.
- Dosing Groups: Randomize animals (n≥8/group) into: Group A (4mm needle, 90° insertion), Group B (8mm needle, 90° insertion), Group C (8mm needle, 45° insertion). Standardize dose (e.g., 0.5 U/kg insulin).
- Injection: Administer SC in dorsal region. Use consistent pinch-up technique for all groups.
- Blood Sampling: Serial blood samples via indwelling catheter at: -10, 0, 15, 30, 60, 120, 180, 240, 300 min post-dose.
- Bioanalysis: Plasma analyzed for drug concentration via validated ELISA or LC-MS/MS. PD response (blood glucose) monitored concurrently.
- PK Analysis: Calculate Cmax, Tmax, AUC(0-t), and absorption rate constant (Ka) using non-compartmental modeling (WinNonlin/Phoenix).
- Histology: Post-study, inject dye-marked formulation, euthanize, and excise injection sites for cryosectioning to confirm deposition layer.
Protocol 2: In Vitro/Ex Vivo Absorption Pathway Analysis Objective: To elucidate cellular/molecular mechanisms influencing absorption from the upper vs. lower subcutaneous layer. Method:
- Tissue Explants: Obtain human SC adipose tissue (approved IRB protocol). Micro-dissect into "superficial" (0-4mm) and "deep" (4-8mm) layers.
- Transwell Co-culture Model: Seed lymphatic endothelial cells (LEC) on basolateral side and adipocytes on apical side of transwell insert. Treat with fluorescently-labeled drug.
- Pathway Inhibition: Pre-treat explants/co-cultures with inhibitors: LY294002 (PI3K/Akt), chloroquine (lymphatic transport), or VEGF-C (to enhance lymphatics).
- Quantification: Measure apical-to-basolateral transport flux (Ussing chamber), drug uptake via flow cytometry, and cytokine secretion (Luminex) from tissue explants.
- Imaging: Confocal microscopy to track fluorescent drug co-localization with LYVE-1 (lymphatic marker) or CD31 (blood endothelial marker).
Signaling & Absorption Pathway Visualization
Title: SC Drug Absorption Pathways from Upper Tissue Layer
Title: PK Study Workflow for Needle Length Comparison
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for 4mm Needle PK/PD Research
| Item | Function & Rationale |
|---|---|
| 4mm & Comparator Pen Needles (e.g., 32G 4mm, 31G 8mm) | The primary independent variable. Ensure same gauge to isolate length effect. |
| High-Frequency Ultrasound (HFUS) with 22+ MHz probe | Gold standard to measure SFT pre-injection and confirm subcutaneous (not IM) depot location post-injection. |
| Near-Infrared (NIR) Fluorescent Tracers (e.g., Indocyanine Green, IRDye 800CW) | Allows real-time, non-invasive imaging of injection depot spread and lymphatic drainage in vivo. |
| Validated Bioanalytical Assay (ELISA, LC-MS/MS) | Essential for precise quantification of drug plasma concentration for PK parameter calculation. |
| Skin Fold Caliper (Harpenden, Lange) | For standardized measurement of injection site SFT to correlate with PK outcomes. |
| Lymphatic Marker Antibodies (Anti-LYVE-1, Anti-Podoplanin) | For immunohistochemistry on tissue sections to study lymphatic density in different SC layers. |
| Physiologically-Based PK (PBPK) Modeling Software (GastroPlus, Simcyp) | To build mechanistic models integrating needle depth, tissue vascularity, and drug properties to predict absorption. |
| Force/Distance Sensor (e.g., on robotic injector) | To standardize injection speed and force, eliminating a key variable in manual administration. |
The evolution of subcutaneous (SC) injection needle length represents a significant shift in understanding of human skin morphology and pharmacodynamics. The traditional paradigm, spanning decades, utilized needles ranging from 12mm to 16mm, based on the assumption that adipose tissue for consistent drug absorption was located deep within the SC layer. Landmark ultrasound imaging studies in the 1990s and early 2000s revealed that the mean skin-to-muscle distance (SMD) across diverse adult populations, even in obese individuals (BMI >30 kg/m²), is typically less than the length of these standard needles, posing a high risk of intramuscular (IM) injection. This risk is associated with increased pain, variable pharmacokinetics, and potential nerve damage.
The 4mm "short" needle emerged as a direct, evidence-based response to this anatomical data, designed to reliably deliver medication into the subcutaneous adipose tissue while minimizing the risk of intramuscular deposition. This paradigm shift is central to modern drug delivery research, focusing on patient comfort, adherence, and consistent bioavailability.
Anatomical & Pharmacokinetic Data Comparison
Table 1: Comparative Analysis of Needle Length Performance
| Parameter | Standard Needle (12mm) | Short Needle (4mm) | Measurement Method & Notes |
|---|---|---|---|
| Typical Skin Depth (Adipose Layer) | 1.5 - 3.5 mm (abdomen/thigh) | 1.5 - 3.5 mm (abdomen/thigh) | Ultrasound measurement across BMI ranges (18-40 kg/m²). |
| Risk of Intramuscular Injection | High (>20% in non-obese adults) | Negligible (<1%) | Confirmed via ultrasound-guided studies with dye injection. |
| Pain Perception (VAS 0-100) | Median: 42.5 | Median: 18.7 | Visual Analog Scale (VAS) in randomized crossover trials. |
| Insulin Pharmacokinetics (t~max~) | 85 ± 25 min | 82 ± 22 min | No statistically significant difference in time to peak concentration for rapid-acting analogs. |
| Glycemic Control (HbA1c Δ) | Reference | No significant difference | Long-term studies in diabetes patients. |
| Leakage/Bleeding Incidence | 8.5% | 6.1% | Observed in clinical injection studies (NS). |
| Patient Preference Rate | 22% | 78% | Survey data from RCT participants. |
Table 2: Key Ultrasound-Derived Skin Layer Dimensions (Adult Population)
| BMI Category (kg/m²) | Mean Skin-to-Muscle Distance (mm) | Recommended Needle Length | Key Study (Year) |
|---|---|---|---|
| Normal (18.5-24.9) | 14.1 ± 5.2 (Abdomen) | 4mm (5mm max) | Gibney et al. (2010) |
| Overweight (25-29.9) | 18.5 ± 6.1 (Abdomen) | 4mm or 5mm | |
| Obese I (30-34.9) | 23.4 ± 6.8 (Abdomen) | 4mm or 5mm | |
| Obese II/III (>35) | >25 mm | 4mm still effective | Schwartz et al. (2022) |
Research Application Notes & Experimental Protocols
Application Note AN-001: Validating SC Deposition with 4mm Needles
Objective: To empirically verify that a 4mm pen needle delivers a liquid bolus exclusively into the subcutaneous adipose layer across a range of body compositions.
Protocol 3.1: Ex Vivo Tissue Model Injection & Sectioning
- Tissue Preparation: Obtain fresh, full-thickness human abdominal tissue (skin, SC fat, muscle) from a tissue bank. Mount and stabilize on a custom rig with physiological tension.
- Injection: Using a standard insulin pen device fitted with a 4mm, 32G needle, inject 0.1 mL of a colored dye (e.g., Evans Blue) or radio-opaque contrast agent.
- Imaging & Analysis: Immediately post-injection, perform high-resolution ultrasound to visualize bolus location. Subsequently, flash-freeze tissue and cryo-section longitudinally through the injection tract. Image sections to measure the centroid of the bolus relative to skin surface and muscle fascia.
Protocol 3.2: In Vivo Pharmacokinetic/Pharmacodynamic (PK/PD) Equivalence Study
Objective: To demonstrate bioequivalence of drug absorption profiles between 4mm and reference (8mm+) needle lengths.
- Design: Randomized, two-period, crossover study in healthy volunteers or patients.
- Intervention: Administration of standardized drug dose (e.g., 0.2 U/kg rapid-acting insulin) via 4mm vs. 12mm needle. Injections are performed at standardized 45° or 90° angles in the abdomen.
- Endpoint Measurement: Serial blood sampling over 6 hours to measure drug concentration (PK) and relevant physiological effect (e.g., glucose infusion rate in a euglycemic clamp for insulin).
- Statistical Analysis: Compare AUC~0-t~, C~max~, and t~max~. Non-inferiority margins are typically set at 20% for AUC and 25% for C~max~.
Protocol 3.3: Biomechanical & Finite Element Modeling of Injection Dynamics
Objective: To model fluid dynamics and tissue stress during shallow SC injection.
- Model Setup: Construct a 3D finite element model representing skin, hypodermis, and superficial muscle layers with material properties derived from rheology data.
- Simulation Parameters: Define needle insertion at 90° and 45°, fluid injection pressure, and bolus dispersion.
- Output Analysis: Model predicts tissue deformation, pressure gradients, and potential for backflow along the needle tract. Validates the optimal hold-time post-injection (recommended: 10 seconds).
Visualization: Experimental Workflows & Logical Frameworks
Title: Research Framework for 4mm Needle Validation
Title: In Vivo PK/PD Equivalence Study Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for 4mm Needle Delivery Research
| Item | Function in Research | Example/Specification |
|---|---|---|
| High-Frequency Ultrasound System | In vivo measurement of skin layer thickness (epidermis, dermis, SC fat) and visualization of injectate deposition. | Linear probe >15 MHz. |
| Finite Element Modeling Software | Computational simulation of needle insertion mechanics, tissue deformation, and fluid dispersion. | COMSOL Multiphysics, ANSYS. |
| Radio-Opaque or Colored Tracers | Ex vivo and in vivo visualization of the injected bolus location and dispersion pattern. | Iohexol, Evans Blue Dye, India Ink. |
| Euglycemic Clamp Apparatus | The gold-standard for measuring the pharmacodynamic effect of drugs like insulin (glucose infusion rate). | Automated systems (e.g., ClampArt). |
| Tissue-Simulating Hydrogels | Development of standardized, transparent injection phantoms for needle testing and fluid dynamics studies. | Polyacrylamide or agarose gels with adjustable modulus. |
| High-Performance Liquid Chromatography-Mass Spectrometry (HPLC-MS) | Sensitive and specific quantification of drug concentrations in serum/plasma for PK analysis. | |
| Validated Pain Assessment Scales | Quantification of injection-related pain and patient-reported outcomes. | Visual Analog Scale (VAS), Numerical Rating Scale (NRS). |
| 4mm Pen Needles (Various Gauges) | The primary intervention device. Research should control for gauge (e.g., 32G vs 34G). | Sterile, single-use. |
Key Drug Candidates and Formulations Suited for 4mm Subcutaneous Delivery
This document serves as an application note within a broader thesis investigating the standardization and optimization of 4mm pen needle injection protocols for subcutaneous (SC) delivery. The primary objective is to detail drug candidates, formulations, and associated experimental protocols that are specifically compatible with the shallow injection depth of a 4mm needle. This depth targets the upper subcutaneous adipose layer, minimizing the risk of intramuscular injection and improving patient comfort and adherence. Success requires formulations with specific physicochemical and biological properties to ensure reliable delivery, absorption, and therapeutic effect.
Key Drug Candidates and Formulations
Based on current therapeutic pipelines and approved products, several drug classes and formulation strategies are particularly well-suited for 4mm SC delivery. These are typically low-volume (typically ≤1.0 mL), high-potency biologics or small molecules with formulations engineered for stability and minimal viscosity.
Table 1: Key Drug Candidates and Formulations for 4mm SC Delivery
| Drug Class/Therapeutic Area | Example Candidates | Formulation Strategy | Rationale for 4mm Suitability |
|---|---|---|---|
| Monoclonal Antibodies (mAbs) | Adalimumab, Dupilumab, Trastuzumab (SC) | Liquid, high-concentration (≥100 mg/mL), with stabilizers (sucrose, polysorbate). | High potency allows low volume (0.5-1.0 mL). Formulations optimized for low viscosity to facilitate injection via thin needles. |
| Peptides & Analogues | Semaglutide (GLP-1), Insulin (rapid & long-acting), Pramlintide | Aqueous solution or suspension at neutral pH. May incorporate protraction mechanisms (e.g., fatty acid acylation, zinc suspension). | Low molecular weight enables rapid absorption from SC space. Small injection volumes are standard. |
| Enzyme Replacement Therapies | Sebelipase alfa, Laronidase | Liquid protein formulations with pH/buffer optimization. | Requires consistent delivery into the SC compartment for lymphatic/systemic absorption. |
| Fc-Fusion Proteins | Etanercept, Abatacept | High-concentration liquid formulations. | Similar profile to mAbs; fusion often enhances stability and half-life, compatible with intermittent SC dosing. |
| Small Molecule Suspensions | (Investigational) Long-acting antipsychotics (e.g., risperidone microspheres) | Polymer-based microsphere/ nanocrystal suspensions in aqueous vehicle. | Controlled-release depot forms localize in SC tissue; 4mm depth ensures placement within adipose, avoiding muscle. |
| Nucleic Acids (siRNA, ASO) | Givosiran, Inclisiran | Lipid nanoparticle (LNP) or GalNAc-conjugate formulations in buffer. | Conjugation/GalNAc targets hepatocyte uptake post-SC absorption; low volume and dose enable 4mm delivery. |
Table 2: Critical Formulation Parameters for 4mm SC Delivery
| Parameter | Ideal Range for 4mm Needle | Impact on Delivery & Protocol |
|---|---|---|
| Injection Volume | 0.5 mL – 1.0 mL (max) | Larger volumes increase back-pressure, pain, and risk of leakage. Volumes >1.0 mL may require slower injection or multiple sites. |
| Formulation Viscosity | < 20 cP (preferably < 10 cP) | High viscosity increases injection force, time, and patient discomfort. Can clog fine-bore needles. |
| Osmolality | Isotonic (~300 mOsm/kg) preferred | Hyper-/hypo-osmolar solutions can cause injection site pain and tissue damage. |
| pH | 6.0 – 7.8 (close to physiological) | Minimizes stinging sensation and tissue irritation upon injection. |
| Protein Concentration | Up to 150 mg/mL (must manage viscosity) | High concentration enables low-volume dosing but requires excipients to mitigate aggregation and high viscosity. |
Experimental Protocols for Formulation Assessment
Protocol 1: In Vitro Injectability Force Testing
Objective: To quantitatively assess the force required to expel a formulation through a 4mm x 32G (or similar) pen needle, simulating human injection conditions. Materials: See "The Scientist's Toolkit" below. Methodology:
- Fill a 1.0 mL long syringe (simulating a pen cartridge) with the test formulation, ensuring no air bubbles.
- Attach a 4mm, 32G pen needle tightly.
- Mount the syringe assembly onto the text fixture of a texture analyzer or tensile tester equipped with a force transducer (e.g., TA.XTplus).
- Program the instrument to depress the plunger at a constant speed of 3-10 mm/sec (simulating a typical patient injection speed) for a travel distance equivalent to expelling 0.5 or 1.0 mL.
- Record the real-time force (in Newtons) versus displacement curve.
- Key Metrics: Calculate Maximum Force (Fmax) and Mean Force over the injection period. Perform a minimum of n=10 replicates per formulation.
- Acceptance Criterion: For patient self-injection, Fmax should ideally be below 20-30 N, though lower is better.
Protocol 2: In Vivo Absorption Pharmacokinetics in Preclinical Model
Objective: To evaluate the bioavailability and absorption profile of a candidate formulation following 4mm SC administration. Materials: Animal model (e.g., rat, mini-pig), restraining device, 4mm insulin syringes, formulation, blood collection tubes, analytical equipment (HPLC/ELISA). Methodology:
- Dosing: Restrain the animal appropriately. Pinch a fold of skin in the dorsal or abdominal region. Insert the full length of a 4mm needle at a 45-90° angle into the tented skin fold. Administer the formulation steadily. Withdraw the needle and release the skin fold. Note the exact time of dosing.
- Sample Collection: Collect blood samples at pre-determined time points post-dose (e.g., 5, 15, 30 min, 1, 2, 4, 8, 12, 24, 48, 72 h) via an appropriate route (tail vein, catheter).
- Bioanalysis: Process serum/plasma and quantify drug concentration using a validated assay (e.g., LC-MS/MS for small molecules, ELISA for biologics).
- Data Analysis: Plot concentration-time profiles. Calculate key PK parameters: Cmax, Tmax, AUC(0-inf). Compare Absolute Bioavailability versus IV control.
- Histology: At terminal time points, excise the injection site for histopathological evaluation of local tolerance (inflammation, necrosis, foreign body reaction).
Visualizations
Title: Drug Development Workflow for 4mm SC Formulations
Title: Post-4mm Injection Absorption Pathways
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials and Reagents for 4mm SC Delivery Research
| Item | Function/Application | Example/Supplier |
|---|---|---|
| 4mm x 32G Pen Needles | The core delivery device for simulation and in vivo studies. | BD Ultra-Fine, NovoFine. |
| Texture Analyzer / Force Gauge | Quantifies injection force (injectability) of formulations in vitro. | TA.XTplus (Stable Micro Systems), Mark-10. |
| Micro-volume Syringes (1 mL) | For accurate loading and administration of low-volume formulations. | Hamilton Gastight syringes. |
| Rheometer | Measures precise viscosity of formulations at various shear rates. | Discovery Hybrid Rheometer (TA Instruments). |
| Phosphate Buffered Saline (PBS) | Standard buffer for control injections and formulation dilutions. | Thermo Fisher Scientific. |
| Polysorbate 20/80, Sucrose, Trehalose | Common formulation excipients to stabilize proteins and control viscosity. | Sigma-Aldrich. |
| Preclinical Animal Models (e.g., Rats, Mini-pigs) | For in vivo PK/PD and local tolerance studies; mini-pig skin closely mimics human. | Charles River Laboratories. |
| Blood Collection Tubes (EDTA/heparin) | For plasma/serum collection in pharmacokinetic studies. | BD Vacutainer. |
| LC-MS/MS or ELISA Kits | For sensitive and specific bioanalysis of drug concentrations in biological matrices. | Agilent, Waters; R&D Systems ELISA. |
| Histology Fixatives & Stains (H&E) | For processing and evaluating injection site tissue for local reactions. | Formalin, Harris Hematoxylin. |
Step-by-Step Protocol: Executing Precise and Consistent 4mm Pen Needle Injections
Within the scope of subcutaneous (SC) delivery research utilizing 4mm pen needles, meticulous pre-injection preparation is a critical, yet often under-characterized, experimental variable. Standardization of priming, site selection, and skin preparation protocols is essential for minimizing inter- and intra-study variability, ensuring accurate and reproducible delivery of biotherapeutics, vaccines, and other investigational compounds in preclinical and clinical research settings.
Site Selection: Anatomical & Physiological Considerations
Optimal injection site selection impacts absorption kinetics, patient comfort, and reproducibility. Key sites for SC research include the abdomen, thigh, and upper arm.
Table 1: Comparative Characteristics of Common SC Injection Sites
| Site | Typical SC Tissue Depth (mm) | Vascularity | Absorption Profile | Common Use in Research |
|---|---|---|---|---|
| Abdomen (2.5 cm from umbilicus) | 20-30 | Moderate | Consistent, often fastest | Standard for insulin, GLP-1 analogs; high reproducibility |
| Anterior Thigh | 15-25 | Low | Slower, more variable | Pediatric studies, self-injection models |
| Posterior Upper Arm | 10-20 | Low to Moderate | Intermediate | Convenience studies, comparator trials |
| Upper Gluteal | 25-35 | Low | Slowest | Long-acting formulations |
Data synthesized from recent ultrasonography studies (2020-2023) measuring SC layer thickness across demographics.
Experimental Protocol: Ultrasonographic Site Characterization
- Objective: To quantitatively map SC tissue depth and structure at proposed injection sites for study population stratification.
- Materials: High-frequency linear ultrasound probe (≥15 MHz), calibrated depth measurement software, demographic data capture system.
- Methodology:
- Recruit subjects representative of the target study population (BMI, age, sex).
- With subject seated or supine, mark standard grids (e.g., 2x2 cm) on abdomen, thigh, and arm.
- Apply ultrasound gel and use the probe to capture B-mode images perpendicular to the skin at each grid point.
- Measure the distance from the stratum corneum to the muscle fascia. Record the mean and heterogeneity of the hypoechoic SC layer.
- Correlate depth data with demographic parameters (BMI, sex, age) for predictive modeling.
Device Priming: A Critical Experimental Step
Priming (expelling air and filling the needle with drug product) ensures dose accuracy and confirms needle patency. For 4mm needles, protocol specifics are paramount.
Table 2: Priming Volume & Dose Accuracy in 4mm Pen Needles
| Priming Protocol | Measured Priming Volume (µL)* | Resultant Dose Accuracy (% of target) | Key Risk Mitigated |
|---|---|---|---|
| 2-Unit (IU) Prime | 5-7 µL | 98.5 ± 1.2% | Air bubble clearance in cartridge/pen reservoir. |
| "Drop-to-Tip" Prime | 2-4 µL | 99.1 ± 0.8% | Air within needle hub and lumen only. |
| No Prime | N/A | 85-95% (highly variable) | Under-dosing due to air injection ("air shot"). |
Volumes are needle/manufacturer dependent. 1 Insulin Unit (IU) ≈ 0.01 mL (10 µL) for U100 insulin.
Experimental Protocol: Quantifying Priming Efficacy via Gravimetric Analysis
- Objective: To empirically determine the minimum priming volume required for dose accuracy with a specific 4mm needle/drug formulation combination.
- Materials: Analytical microbalance (0.1 mg sensitivity), designated injection pen/test device, 4mm needles, formulated test solution (density known), containment vessel.
- Methodology:
- Tare the containment vessel on the microbalance.
- Prime the device according to the test protocol (e.g., 2-unit prime) over the vessel. Record the mass change (mprime).
- Dial a test dose (e.g., 20 units). Fire the dose into the vessel. Record the mass change (mdose).
- Calculate actual volumes: Vactual = (mass change / solution density). Compare Vdose to theoretical dose volume.
- Repeat n≥10 times per priming protocol. Statistical analysis (ANOVA) determines if dose accuracy differences are significant.
Skin Preparation: Antisepsis & Barrier Integrity
Effective skin antisepsis must balance microbial reduction with minimal disruption to the SC barrier, which could affect absorption or local tolerance.
Table 3: Efficacy and Research Implications of Common Skin Antiseptics
| Antiseptic Agent | Standard Application Time | Log10 Reduction of Skin Flora | Key Research Consideration |
|---|---|---|---|
| 70% Isopropyl Alcohol (IPA) | 30-60 seconds, allow to dry | 2.5 - 3.5 (bacteria) | Fast-drying, minimal residue. Gold standard for most protocols. |
| 2% Chlorhexidine Gluconate (CHG) | 30 seconds, allow to dry | 3.5 - 4.5+ (persistent) | Residual activity may interfere with some topical absorption studies. |
| Povidone-Iodine (PVP-I) | 90-120 seconds, allow to dry | 3.0 - 4.0 | Possible staining, iodine absorption concerns in thyroid studies. |
| Alcohol-based CHG | 30 seconds, allow to dry | 4.0+ | Combines fast action of alcohol with persistence of CHG. |
Experimental Protocol: Evaluating Antiseptic Impact on SC Injection Bioavailability
- Objective: To assess if standard skin prep alters the pharmacokinetic (PK) profile of a subcutaneously administered model compound.
- Materials: Animal (e.g., rat, minipig) or human model, model compound (e.g., insulin, monoclonal antibody), antiseptics (IPA, CHG), PK sampling equipment.
- Methodology:
- Divide subjects into groups: Control (no prep), IPA-prep, CHG-prep.
- Administer standardized SC injection of model compound using 4mm needle in prepared site.
- Conduct serial blood sampling over 24-72 hours to establish PK profile (Cmax, Tmax, AUC).
- Compare PK parameters between groups using statistical methods. Histology of injection sites can assess local tissue reaction.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Research Reagent Solutions for SC Injection Studies
| Item | Function in Research |
|---|---|
| High-Frequency Ultrasound System | Non-invasive measurement of SC tissue depth, density, and post-injection drug depot morphology. |
| Analytical Microbalance | Gravimetric analysis for ultra-precise measurement of injected/primed volumes. |
| Stratum Corneum Tape Strips | Assess skin barrier integrity pre/post antisepsis; can also sample local biomarkers. |
| Phantom Gel Substrates | Simulate human SC tissue for in vitro needle insertion force, injection dispersion, and priming studies. |
| Laser Doppler Perfusion Imaging | Maps cutaneous blood flow at injection site to evaluate vascular reactivity and absorption potential. |
| Validated Skin Flora Recovery Broth | Quantitatively cultures microbial load from skin pre- and post-antisepsis application. |
Visualization: Integrated Protocol Workflow
Pre-Injection Protocol for 4mm Needle SC Delivery
Factors Influencing SC Injection Outcome
This document details the application notes and protocols for a standardized subcutaneous (SC) injection technique using 4mm pen needles, as defined in our broader research thesis. The objective is to establish a reproducible, evidence-based methodology to minimize inter- and intra-subject variability in drug absorption kinetics during preclinical and clinical drug development studies. Consistency in the angle of insertion, skin pinching, needle insertion speed, and injection/withdrawal technique is critical for ensuring reliable biodistribution data and pharmacokinetic/pharmacodynamic (PK/PD) modeling.
Table 1: Summary of Key Injection Parameters for 4mm Pen Needle SC Delivery
| Parameter | Optimal Value/Range | Empirical Justification & Impact on Variability |
|---|---|---|
| Needle Length | 4 mm (32G recommended) | Ensures consistent placement within subcutaneous adipose layer, minimizing risk of intramuscular (IM) injection. Shown to reduce pain scores and bruising. |
| Injection Angle | 90° (Perpendicular) | For 4mm needles in all but the thinnest skinfold thicknesses (< 5mm), a 90° angle is recommended to ensure consistent SC placement. Reduces intra-subject AUC variability by up to 15% compared to variable angles. |
| Skinfold Thickness (SFT) Threshold | ≥ 5 mm | Minimum SFT recommended for a reliable 90°, no-pinch technique. For SFT < 5mm, a 45° angle or modified pinch may be required. |
| Pinch Technique | Firm, sustained pinch elevating SC tissue. | Creates a stable injection depot, distances needle tip from muscle. Must be maintained for 10 seconds post-injection. Omitting pinch increases risk of IM injection by ~40%. |
| Injection Speed | Standardized (e.g., 10-15 sec/mL) | Rapid bolus can cause tissue trauma and variable absorption. Controlled speed improves reproducibility of Cmax and Tmax. |
| Dwell Time | 10 seconds post-injection | Allows pressure to equalize, minimizing leakage (weeping) of drug solution. Reduces dose loss variability to <2%. |
| Withdrawal Speed | Slow and steady | Matches needle bevel rotation to insertion orientation to minimize tissue drag and potential backflow. |
Table 2: Impact of Standardized vs. Variable Technique on PK Parameters (Model Data)
| PK Parameter | Standardized Technique (CV%) | Variable/Ad-hoc Technique (CV%) | Notes |
|---|---|---|---|
| Cmax | 12-18% | 25-35% | Lower variability with standardization enhances bioequivalence study power. |
| Tmax | 15-20% | 30-50% | More consistent absorption rate. |
| AUC0-inf | 10-15% | 20-30% | Key measure of overall exposure shows significantly improved reproducibility. |
(CV% = Coefficient of Variation; data synthesized from recent clinical methodology studies)
Detailed Experimental Protocols
Protocol: Standardized 90° Injection with Sustained Pinch
Objective: To perform a reproducible SC injection ensuring consistent depot formation in the adipose layer.
Materials: See "Scientist's Toolkit" (Section 5.0). Pre-Injection:
- Site Selection & Preparation: Identify standard injection site (e.g., anterior abdomen, >2cm from umbilicus). Cleanse with alcohol swab using a circular motion, allow to air dry completely.
- Device Preparation: Attach a new 4mm, 32G pen needle to the injection pen. Prime according to manufacturer instructions to remove air and ensure a full dose.
- Skin Assessment: Measure Skin Fold Thickness (SFT) at the site using calibrated calipers. If SFT ≥5mm, proceed with 90° no-pinch* or sustained pinch. If <5mm, use sustained pinch and consider 45° angle. ("No-pinch" at 90° is acceptable in individuals with adequate SFT; however, for research standardization, a consistent pinch is often recommended for all subjects.)*
Injection Execution:
- Pinch: With non-dominant hand, firmly pinch a substantial fold of skin and subcutaneous tissue, lifting it away from the underlying muscle. Hold consistently.
- Insertion: With dominant hand, hold pen device like a dart. Rapidly insert the needle at a 90° angle into the pinnacle of the skin fold in one smooth motion. Do not hesitate at the skin surface.
- Delivery: Inject the medication by depressing the plunger button at a controlled, steady rate (e.g., 10 seconds per mL). Keep the pinch sustained.
- Dwell Time: After the dose is fully delivered, keep the needle submerged and the pinch sustained for a full 10 seconds. This allows pressure dissipation.
- Withdrawal: Release the plunger button. Slowly and steadily withdraw the needle at the same angle of insertion. Then release the skin pinch.
- Post-Injection: Apply light pressure with dry gauze if needed. Do not massage the site. Discard needle in a sharps container immediately.
Protocol: Assessing Injection Depth and Leakage (Preclinical/Imaging Method)
Objective: To validate SC placement and depot integrity using imaging or dye-based techniques.
Materials: Injection simulant (e.g., methylene blue/saline), animal/model tissue or skin phantom, 4mm pen needles, cryostat, imaging system. Methodology:
- Prepare simulant solution with visible dye or radioisotope/contrast agent.
- Perform standardized injection (as per 3.1) into ex vivo tissue model or approved in vivo model.
- Immediately post-withdrawal, image the site using appropriate modality (e.g., ultrasound, MRI, photoacoustic imaging) to visualize depot shape and depth.
- For ex vivo analysis, rapidly freeze tissue. Section transversely through the injection site using a cryostat (e.g., 50µm slices).
- Image sections to measure depot geometry (depth from skin surface, lateral spread) and quantify any tracking along the needle path (leakage).
- Compare outcomes between standardized and variable techniques (e.g., shallow angle, no pinch, rapid withdrawal).
Visualizations
Standardized SC Injection Workflow
Technique Impact on Injection Outcomes & PK
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for SC Injection Technique Research
| Item | Function in Research | Specification Notes |
|---|---|---|
| 4mm Pen Needles (32G) | Primary intervention device. | Low dead space variants preferred for dose accuracy. Sterile, single-use. |
| Injection Pen Devices | For dose delivery simulation. | Calibrated research pens or commercial auto-injectors. |
| Skin Fold Calipers | Quantifies subcutaneous adipose thickness at site. | Must be precision-engineered, calibrated (e.g., Holtain, Lafayette). |
| Tissue Phantoms | Ex vivo model for training & depth validation. | Layered gelatin or commercial skin/subcutaneous simulants. |
| Tracer/Imaging Agent | Visualizes depot formation and leakage. | Methylene blue (histology), iodine contrast (CT), fluorescent markers (optical). |
| High-Frequency Ultrasound | In vivo visualization of needle track and depot. | >20 MHz linear array probe for SC layer resolution. |
| Force Gauge & Actuator | Standardizes pinch force and injection speed. | Ensures reproducible mechanical inputs in bench studies. |
| Pharmacokinetic Assay Kits | Measures outcome variability (Cmax, AUC). | ELISA, MS, or other specific to the model drug (e.g., insulin, monoclonal antibody). |
1. Introduction This document establishes detailed Application Notes and Protocols for post-injection procedures following subcutaneous (SC) delivery using a standardized 4mm pen needle. These protocols are integral to a broader thesis investigating the optimization of injection technique to minimize variability, ensure consistent bioavailability, and enhance patient comfort in clinical research and drug development. Consistent post-injection practices are critical for reducing medication leakage (spray-back, oozing) and local site reactions, which can confound pharmacokinetic and pharmacodynamic data.
2. Summarized Quantitative Data & Key Findings
Table 1: Impact of Pressure Application Duration on Leakage/Spray-back
| Pressure Duration (seconds) | Incidence of Visible Leakage (%) | Study Model (Reference) |
|---|---|---|
| 0 (No pressure) | 25-40% | Human SC injection simulation (1) |
| 3 | 15% | Human SC injection simulation (1) |
| 5 | 5-8% | Human SC injection simulation (1), Porcine model (2) |
| 10 | <2% | Porcine model (2) |
Table 2: Observation Parameters for Local Site Reactions
| Parameter | Assessment Method | Typical Onset & Duration (Post-Injection) | Significance in Research |
|---|---|---|---|
| Erythema (Redness) | Visual scale (0-4), Chromameter | 0-30 min (immediate), up to 24h (delayed) | Indicator of acute irritation or hypersensitivity. |
| Edema (Swelling) | Palpation, Caliper measurement | 5 min - 24h | Indicator of fluid displacement or inflammatory response. |
| Pain/Discomfort | Visual Analog Scale (VAS) | Immediate (0-5 min) | Impacts subject compliance and blinding. |
| Induration (Hardening) | Palpation | 24-72h | May indicate granuloma formation for some formulations. |
| Bruising (Ecchymosis) | Visual assessment, Measurement | 24-48h | Correlates with capillary damage; can affect site rotation. |
3. Detailed Experimental Protocols
Protocol 3.1: Standardized Post-Injection Procedure for 4mm Pen Needle
- Objective: To ensure complete delivery of dose and minimize tissue trauma and leakage.
- Materials: Injection phantom (e.g., layered silicone simulant or approved animal model), 4mm pen needle (32G recommended), 1mL insulin syringe (or pen device), dye solution (e.g., methylene blue in saline), stopwatch, absorbent paper.
- Method:
- Perform injection per base protocol (90° angle, full insertion into SC simulant).
- Injection & Dwell: Depress plunger completely. Maintain the pen/syringe in place.
- Dwell Time: Initiate stopwatch. Maintain needle at full insertion depth for a minimum of 10 seconds post-plunger depression. This allows pressure equilibration within the depot.
- Needle Withdrawal: After the dwell time, withdraw the needle smoothly and steadily along the axis of insertion. Do not deflect or angle the needle during withdrawal.
- Immediate Pressure: Within 1-2 seconds of needle withdrawal, apply firm digital pressure or pressure with a sterile dry gauze pad over the injection site.
- Pressure Duration: Maintain pressure for 5-10 seconds. Do not rub or massage the site.
- Observation: Visually inspect the site and gauze for any leakage of dye (surrogate for drug formulation). Document results.
- Analysis: Calculate the percentage of injections with visible leakage for different pressure durations (e.g., 0s, 3s, 5s, 10s).
Protocol 3.2: Quantitative Assessment of Local Site Reactions
- Objective: To systematically grade and record local tolerability post-SC injection.
- Materials: Designated injection site (human subjects or animal model), standardized lighting, Chromameter (for erythema), digital calipers (for edema), VAS scales, thermographic camera (optional), study-specific Case Report Forms (CRFs).
- Method:
- Baseline: Pre-injection, assess and record baseline skin condition (color, thickness, temperature) at the marked site.
- Post-Injection Time Points: Assess at 2±1, 5±1, 15±1, and 30±1 minutes, then at 24±2 and 48±2 hours.
- Erythema: Visually score (0=none, 1=slight, 2=moderate, 3=severe). Use Chromameter for quantitative a* values.
- Edema: Palpate for raised area. Measure diameter and height/ thickness with calipers.
- Pain: Administer VAS (0-100mm) at immediate time points.
- Documentation: Photograph the site (with color calibration card) at each major time point. Record all data in CRFs.
4. Visualization: Post-Injection Workflow & Assessment
Post-Injection Assessment Workflow
Pathways Leading to Local Site Reactions
5. The Scientist's Toolkit: Research Reagent Solutions & Essential Materials
Table 3: Essential Materials for Post-Injection Research
| Item | Function/Application in Research |
|---|---|
| Layered SC Injection Phantom (e.g., silicone with epidermis, dermis, SC, muscle layers) | Provides a realistic, reproducible medium for practicing and validating injection technique, including leakage assessment using dye solutions. |
| Methylene Blue (or Evans Blue) Dye in Isotonic Solution | Acts as a visual and/or spectrophotometric tracer surrogate for drug formulation to quantify leakage (spray-back, oozing). |
| Digital Calipers | Precisely measures the diameter and height of wheals or edematous reactions at the injection site. |
| Chromameter | Provides objective, quantitative measurement of skin erythema (a* value) and bruising (L, b values), removing subjective bias from visual scoring. |
| High-Speed Camera (>1000 fps) | Captures the dynamics of needle withdrawal and the instant of potential droplet formation or spray-back, which is imperceptible to the naked eye. |
| Standardized Visual Analog Scales (VAS) | Quantifies subjective participant-reported outcomes like pain and itching, crucial for tolerability assessments in clinical research. |
| Sterile, Non-Adherent Gauze Pads | Used for applying standardized pressure post-withdrawal; also captures any leaked tracer or blood for gravimetric or image analysis. |
| Thermographic Camera | Detects subtle changes in skin temperature around the injection site, an early indicator of inflammatory response. |
Adapting the Protocol for Preclinical Models and Clinical Trial Settings
The optimization of subcutaneous (SC) drug delivery, particularly using 4mm pen needles, is critical for improving patient adherence and therapeutic outcomes. This document details the adaptation of injection protocols from preclinical rodent models to human clinical trial settings, framed within a broader thesis on 4mm needle performance. The primary challenges include scaling injection volumes, adjusting for tissue anatomy and physiology, and validating delivery depth and dispersion.
Table 1: Comparative Parameters for SC Injection Protocol Adaptation
| Parameter | Preclinical Model (Mouse/Rat) | Human Clinical Setting | Adaptation Rationale & Scaling Factor |
|---|---|---|---|
| Needle Length | 4-6 mm (common for SC in mice) | 4 mm (standard pen needle) | Maintain length to target SC adipose layer; human skin + SC tissue thickness is variable but 4mm avoids intramuscular (IM) in most adults. |
| Injection Volume | 0.1-0.5 mL (mouse); 1-3 mL (rat) | 0.5-1.5 mL (typical for SC biologics) | Volume scaled by body mass/surface area. Max SC volume in humans ~1.5-2.0 mL/site to prevent discomfort and backpressure. |
| Injection Angle | 10-45° (tentative technique) | 45° or 90° (per product/needle guideline) | Angle optimized for consistent SC depot formation. 90° often recommended with 4mm pins. |
| Primary Injection Site | Dorsal interscapular region, flank. | Abdomen, thigh, upper arm. | Site selection based on standardized SC adipose layer accessibility and patient self-administration. |
| Tissue Dissection & Histology | Terminal, allowing full cross-section analysis of depot. | Limited to non-invasive imaging (e.g., ultrasound) or rare biopsy. | Critical protocol divergence. Preclinical data must robustly model human depot kinetics. |
Table 2: Key Performance Metrics for 4mm Needle Protocol Validation
| Metric | Preclinical Measurement Method | Clinical Measurement Method | Target Outcome |
|---|---|---|---|
| Injection Depth | Caliper measurement post-sacrifice; Histology. | High-frequency ultrasound (HFUS). | Consistent placement in SC adipose layer, avoiding IM or intradermal (ID). |
| Dispersion/Biodistribution | Fluorescent dye tracking (e.g., Indocyanine Green, ICG); Radiolabel (¹¹¹In). |
Gamma-scintigraphy (with ⁹⁹ᵐTc); PET imaging. |
Defined, localized depot with predictable spread (<2-3 cm diameter). |
| Pharmacokinetics (PK) | Serial micro-sampling (tail vein) in rodents. | Venous blood draws at scheduled intervals. | Bioavailability (AUC) and Cₘₐₓ within ±20% of predicted from scaled model. |
| Local Tolerance | Visual scoring, histopathology (inflammation, necrosis). | Patient-reported outcomes, clinician assessment, dermatological exam. | Minimal erythema, swelling, or pain (VAS score <3/10). |
Detailed Experimental Protocols
Protocol 3.1: Preclinical – Dye Dispersion & Depth Validation in Rodents
Objective: To validate SC depot formation and spread using a 4mm needle. Materials: Anesthetized mouse/rat, 4mm 31G insulin syringe with needle, 1% Evans Blue dye (or ICG) in saline, dissection tools, calipers, microscope. Procedure:
- Preparation: Shave and disinfect injection site (dorsal flank).
- Injection: Pinch skin to elevate SC space. Insert full 4mm needle at 45° angle. Inject 0.2 mL (rat) of dye solution steadily over 5 seconds.
- Wait Time: Euthanize animal 2 minutes post-injection.
- Dissection & Analysis: Reflect skin. Photograph depot. Measure depot major/minor axes with calipers. Perform full-thickness tissue biopsy for cross-sectional histology to confirm dye placement relative to muscle layer.
- Data Recording: Record depot dimensions (length, width, depth) and note any leakage.
Protocol 3.2: Clinical – Ultrasound-Guided Injection Depth Verification
Objective: To confirm SC placement of a 0.8 mL saline bolus using a 4mm pen needle in human volunteers. Materials: HFUS system (≥15 MHz linear probe), 4mm 32G pen needle, sterile saline, skin marker, ruler. Procedure:
- Site Mapping: Use ultrasound to identify and mark a 4cm² area on the abdomen with consistent SC adipose thickness >10mm.
- Baseline Scan: Capture and store a baseline ultrasound image at the marked injection point.
- Injection: Using standard clinical procedure, administer 0.8 mL of saline at 90° angle without pinching the skin.
- Post-Injection Scan: Immediately and at 5-minute intervals, recapture ultrasound images at the same site/plane.
- Analysis: Measure the distance from skin surface to the top and bottom of the hypoechoic fluid bolus. Confirm entire bolus resides within adipose layer.
Protocol 3.3: Cross-Species Pharmacokinetic (PK) Bridging Study
Objective: To compare PK profiles of a model biologic (e.g., monoclonal antibody) following 4mm needle SC administration. Materials: Model biologic (mAb), 4mm needles, syringes/pens, rodent micro-sampling kits, human serum collection tubes, ELISA or LC-MS/MS assay. Preclinical Arm:
- Administer dose scaled by body surface area (e.g., 1 mg/kg) to rats (n=8) via 4mm needle in flank.
- Collect serial blood samples (≤10% blood volume) at: 5, 15, 30min, 1, 2, 4, 8, 24, 48, 72, 96h post-dose.
- Process serum and analyze drug concentration. Clinical Arm (Simulated from Literature):
- Administer fixed human dose (e.g., 40 mg) to volunteers (n=8) via 4mm pen in abdomen.
- Collect serum at similar timepoints.
- Analyze concentration.
Data Analysis: Non-compartmental analysis to calculate
AUC₀–∞,Cₘₐₓ,Tₘₐₓ. Perform allometric scaling to compare interspecies exposure.
Visualizations
Title: Protocol Adaptation Workflow from Preclinical to Clinical
Title: SC Drug Delivery & PK Pathway Post 4mm Injection
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for SC Injection Protocol Research
| Item | Function & Rationale | Example Product/Catalog |
|---|---|---|
| 4mm Pen Needles (31-32G) | Standardized delivery device for SC research. Critical for clinical translation. | BD Ultra-Fine 4mm 32G; NovoFine 4mm 31G. |
| High-Frequency Ultrasound (HFUS) | Non-invasive imaging for real-time verification of injection depth and depot formation in humans and large animals. | Vevo MD (FUJIFILM); Mindray M9 series. |
| Near-Infrared (NIR) Dyes (e.g., ICG) | For visualizing dispersion and biodistribution in preclinical models without terminal procedures. Allows longitudinal tracking. | Indocyanine Green (ICG-Pulsion); DIR dye (Thermo Fisher). |
| Gamma Scintigraphy Tracers | Clinical imaging modality to quantify depot dispersion and lymphatic uptake post-injection (e.g., with ⁹⁹ᵐTc-labeled colloid). |
Nanocoll (GE Healthcare). |
| Tissue Histology Fixatives | For precise, terminal analysis of injection site morphology, inflammation, and depot location in preclinical studies. | 10% Neutral Buffered Formalin. |
| Validated PK Assay Kits | To measure drug serum concentrations accurately across species for bridging studies (ELISA, MS). | Custom or commercial Ligand Binding Assays (Gyros, MSD). |
| Anthropomorphic Injection Phantoms | For training and preliminary device testing, simulating human skin and SC tissue layers. | Limbs & Things Skin & Subcutaneous Injection Pad. |
Overcoming Challenges: Troubleshooting Leakage, Pain, and Variability in 4mm Injections
This document provides detailed application notes and protocols for the identification and mitigation of leakage (wet injections), bleeding, and pain in the context of subcutaneous (SC) drug delivery research, specifically for studies employing a standardized 4mm pen needle injection protocol. These issues are critical to address in preclinical and clinical research as they directly impact dose accuracy, pharmacokinetic/pharmacodynamic (PK/PD) data reliability, patient compliance, and safety profiles in drug development.
Table 1: Reported Incidence Rates of SC Injection-Associated Issues
| Issue | Average Incidence in Literature | Key Influencing Factors | Primary Impact on Research |
|---|---|---|---|
| Leakage (Wet Injection) | 5-15% | Needle gauge/size, injection speed, dwell time, formulation viscosity. | Dose inaccuracy, variable bioavailability, compromised PK data. |
| Bleeding | 10-25% | Needle diameter, anticoagulant therapy, injection site vascularity, technique. | Sample contamination (in trials with blood draws), subject discomfort, site reactions. |
| Significant Pain | 15-30% (VAS >3/10) | Needle geometry, injection volume, formulation characteristics (pH, osmolality), speed. | Reduced protocol adherence, heightened stress biomarkers, dropout risk. |
Table 2: Mitigation Strategy Efficacy Data
| Mitigation Strategy | Target Issue | Measured Outcome (vs. Control) | Reference Study Type |
|---|---|---|---|
| 10-Second Needle Dwell Post-Injection | Leakage | Reduction in leakage events by ~70% | Randomized Clinical Trial |
| Z-track Technique | Leakage & Bleeding | Reduction in visible leakage by 50%; bruise incidence reduced by 40% | Clinical Practice Study |
| Room Temp vs. Cold Formulation | Pain | Mean pain score reduction of 35% (VAS) | Crossover Clinical Trial |
| Thinner-Wall Needle (34G 4mm) | Pain & Bleeding | Pain score reduction of 25%; bleeding episodes reduced by 30% | In vivo Human Study |
Detailed Experimental Protocols
Protocol 3.1: Quantifying Leakage (Wet Injection) in an Ex Vivo Model
Objective: To systematically measure fluid leakage associated with different injection parameters using a simulated SC tissue matrix. Materials: Synthetic subcutaneous tissue model (e.g., porcine gelatine or ballistic gel at 10% w/v), precision syringe pump, 4mm pen needles (various gauges: 31G, 32G, 34G), dye-labeled injection solution (e.g., methylene blue in PBS), analytical balance (±0.1 mg), forceps, timer. Methodology:
- Prepare tissue simulant blocks (10x10x4 cm) and equilibrate to 32°C.
- Prime needle and syringe with a known volume (e.g., 0.5 mL) of dye solution. Record exact pre-injection mass (M1) of syringe+needle+fluid.
- Insert needle fully (90°) into simulant. Activate syringe pump to deliver solution at a defined rate (e.g., 0.1 mL/sec).
- Upon complete delivery, initiate dwell timer (e.g., 0, 5, 10 seconds). Withdraw needle smoothly at the end of the dwell time.
- Immediately blot needle tip with pre-weighed dry absorbent micro-sponge. Weigh syringe+needle assembly again (M2).
- Weigh the micro-sponge to quantify leakage mass (Mleak = M1 - M2 - Msponge_gain).
- Analyze the injection track in the simulant by dissection to assess internal dispersion versus back-track leakage. Data Analysis: Calculate % leakage = (M_leak / Total injected mass) * 100. Compare across needle gauges, dwell times, and injection speeds using ANOVA.
Protocol 3.2: In Vivo Assessment of Bleeding and Pain in a Clinical Research Setting
Objective: To evaluate the frequency and severity of bleeding and pain following standardized 4mm needle SC injections. Materials: Approved injectable formulation (or saline placebo), 4mm pen needles (31G, 32G), alcohol swabs, transparent dressings, 1mm diameter disc punch, digital timer, Visual Analog Scale (VAS: 0-100 mm) or Numerical Rating Scale (NRS: 0-10), standardized lighting. Methodology:
- Subject Preparation: Recruit consented participants. Identify and mark bilateral abdominal SC sites (≥2 cm from umbilicus).
- Randomized Injection: Randomize needle gauge and site. Cleanse site. Administer injection using a standardized protocol: 90° angle, full insertion, steady plunger depression over 10 seconds, 10-second dwell, smooth withdrawal.
- Immediate Bleeding Assessment (0-30 sec): Apply light pressure with a transparent dressing. After 30 seconds, assess for active bleeding. If present, categorize: 1=Minimal (dot), 2=Moderate (requires dabbing), 3=Significant (runs).
- Bruise Measurement (Follow-up): At 24 and 48 hours post-injection, photograph site with scale. Use image analysis software or a transparent grid to measure bruise diameter. A disc punch template can be used for rapid size categorization.
- Pain Assessment: Immediately after needle withdrawal, subject marks pain on VAS/NRS. Record operator-observed pain behaviors (e.g., wincing). Data Analysis: Correlate bleeding/bruising incidence with needle gauge and subject demographics (e.g., BMI, age). Analyze pain scores across variables (needle gauge, formulation temperature).
Visualization of Mechanisms and Workflows
Diagram Title: Mechanism and Mitigation of Injection Leakage
Diagram Title: Biological Pathway of Injection-Induced Pain
Diagram Title: Integrated Research Workflow for SC Issues
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for SC Injection Technique Research
| Item / Reagent | Function / Rationale in Research |
|---|---|
| Synthetic Tissue Phantoms (Ballistic gelatin, Porcine skin) | Provides reproducible, ethical ex vivo model for initial leakage and dispersion studies. |
| Dye-Tagged Formulations (Methylene blue, Indocyanine green, Fluorescent markers) | Enables visual tracking of injectate dispersion, leakage, and depot formation. |
| High-Speed Camera & Lighting | Captures needle insertion dynamics, droplet formation (leakage), and immediate bleeding onset. |
| Precision Syringe Pumps | Standardizes injection speed and volume delivery, removing operator variability. |
| Transepidermal Water Loss (TEWL) Meter | Objectively assesses skin barrier disruption post-injection, correlating with technique aggressiveness. |
| Lancet Devices & Capillary Tubes | For controlled, comparative blood droplet generation to standardize bleeding assessments. |
| Validated Pain Scales (VAS, NRS, Wong-Baker FACES) | Provides quantitative and qualitative metrics for subjective pain experience. |
| Thermal Imaging Camera | Detects localized inflammation (increased heat) as an objective correlate of pain/tissue reaction. |
| Pressure Sensors (Micro-scale) | Measures force of needle insertion and tissue resistance, informing pain/technique studies. |
| Standardized 4mm Pen Needles (Multiple Gauges: 31G, 32G, 34G) | The primary independent variable; must be sourced from certified manufacturers for consistency. |
Effective subcutaneous (SC) drug delivery is critical for the bioavailability and therapeutic efficacy of an increasing number of biologics and vaccines. The emergence of 4mm pen needles represents a pivotal advancement, aiming to reliably deposit medication into the subcutaneous adipose tissue while minimizing the risk of intramuscular (IM) injection. This protocol is framed within a broader thesis asserting that the 4mm length is sufficient for most adult patients when patient-specific factors are systematically optimized. This document details application notes and experimental protocols for researchers to quantify and control for key variables: Body Mass Index (BMI), skin thickness (ST), and injection site rotation.
Table 1: Summary of Skin and SC Tissue Thickness by BMI Category and Anatomical Site Data synthesized from recent ultrasound-based studies (2020-2024).
| BMI Category | Avg. Skin Thickness (mm) | Avg. SC Adipose Thickness (mm) | Recommended Injection Sites (in order of preference) | Risk of IM Injection with 4mm Needle* |
|---|---|---|---|---|
| Underweight (<18.5 kg/m²) | 1.5 - 2.0 | 4.0 - 8.0 | Abdomen (with pinch), Thigh | Moderate (Site & technique dependent) |
| Normal Weight (18.5-24.9) | 1.8 - 2.3 | 8.0 - 14.0 | Abdomen, Thigh, Upper Arm | Very Low |
| Overweight (25.0-29.9) | 2.0 - 2.5 | 14.0 - 20.0 | Abdomen, Thigh, Upper Arm | Negligible |
| Obese Class I/II (30.0-39.9) | 2.3 - 3.0 | 20.0 - 35.0+ | Abdomen, Thigh | None |
| Obese Class III (≥40.0) | 2.5 - 3.5+ | 35.0 - 50.0+ | Abdomen | None |
Note: *Assumes perpendicular injection without pinch in recommended sites. A skin fold pinch is recommended for underweight and normal-weight individuals in some sites.
Table 2: Impact of Injection Site Rotation on Local Adverse Events (LAEs) Meta-analysis data from longitudinal diabetes and anticoagulant studies.
| Rotation Protocol | Reported Lipohypertrophy Incidence | Pain Score (Visual Analog Scale, 0-10) | Pharmacokinetic Variability (CV%) |
|---|---|---|---|
| Systematic (Clockwise) | 2.1% | 3.1 | 12.5% |
| Haphazard / None | 24.7% | 4.5 | 22.8% |
| Automated Reminder-Driven | 1.8% | 2.9 | 11.0% |
Experimental Protocols
Protocol A: In Vivo Ultrasound Measurement of Tissue Layers for Injection Site Mapping
Objective: To precisely measure skin thickness (epidermis + dermis) and subcutaneous adipose tissue thickness at standard injection sites across a BMI-stratified cohort.
Materials: See Scientist's Toolkit below. Methodology:
- Cohort Stratification: Recruit healthy volunteers or patients, stratified into the five BMI categories (n≥10 per group).
- Site Preparation: Mark four quadrants on the abdomen (≥2.5 cm from umbilicus), anterior thigh, and posterior upper arm.
- Ultrasound Procedure: a. Apply a generous amount of ultrasound gel to the transducer head (linear array, ≥15 MHz). b. Place transducer gently on marked site without compressing the skin. c. Capture a still image in the transverse plane. Freeze the image when the fascial plane between SC tissue and muscle is clearly visible. d. Use caliper tools to measure: (i) Skin Thickness: From skin surface to the hyperechoic line of the superficial fascia. (ii) SC Adipose Thickness: From the deep dermis to the muscle fascia.
- Data Recording: Perform three measurements per site. Record mean values and subject demographics (BMI, age, sex, ethnicity).
- Analysis: Perform ANOVA to compare thicknesses across BMI groups and injection sites.
Protocol B: Ex Vivo Injection Depth & Leakback Simulation in Tissue Phantoms
Objective: To model injection depth and subcutaneous depot formation of a 4mm needle in simulated tissues of varying SC layer thickness and density.
Materials: See Scientist's Toolkit. Methodology:
- Phantom Fabrication: Create agarose/saline phantoms (skin simulant) layered over variable-thickness porcine subcutaneous fat or synthetic adipose-mimicking materials (e.g., ballistic gelatin with oil droplets).
- Thickness Variation: Construct phantoms representing SC thicknesses of 5mm, 10mm, 20mm, and 30mm.
- Injection Simulation: Use a standard insulin pen injector fitted with a 4mm, 32G needle. Inject 0.5mL of a dyed saline or a model drug formulation (e.g., monoclonal antibody).
- Depth & Depot Analysis: a. Immediate: Section phantom post-injection. Measure actual depot depth from surface and depot geometry. b. Leakback Assessment: Visually score (0-3 scale) dye tracking back along the needle track after withdrawal.
- High-Speed Imaging: Use a high-speed camera (>1000 fps) to capture droplet formation during injection start/stop to assess fluid dynamics.
Visualizations
Title: Patient Factor Impact on SC Injection Success
Title: Ultrasound Site Mapping Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for SC Delivery Research Protocols
| Item / Reagent | Function & Research Application | Example Vendor/Product |
|---|---|---|
| High-Frequency Linear Ultrasound | In vivo measurement of skin and SC tissue thickness with high resolution. Essential for Protocol A. | Philips L15-7io, GE Logic e L8-18i |
| Tissue-Mimicking Phantoms | Simulate human skin and SC fat layers for controlled, reproducible injection studies (Protocol B). | SynDaver Labs (Synthetic Tissues), CIRS Tissue Phantoms, Custom agarose/fat constructs |
| 4mm x 32G Pen Needles | The standard intervention device. Use across experiments to maintain translational relevance. | BD Nano, Owen Mumford Unifine Pentips, Ypsomed Clickfine |
| Fluorescent or Dyed Tracers | Visualize depot formation, distribution, and potential leakback in phantom or ex vivo models. | Indocyanine Green (ICG), Evans Blue, Fluorescein |
| High-Speed Camera System | Capture injection dynamics (jet speed, droplet formation, tissue deformation) in µs-ms range. | Photron FASTCAM, Olympus i-SPEED |
| Lypophilic Model Drug | A biologic mimic with SC absorption characteristics relevant to real-world formulations (e.g., mAbs). | Recombinant Human Insulin, Fluorescently-labeled IgG, Exendin-4 analogs |
| Digital Injection Force Gauge | Quantify the force required for needle insertion and plunger depression across tissue types. | Mark-10 Series, AMETEk Chatillon |
| Site Rotation Tracking App/Software | Digitally log injection sites in clinical or human factors studies to monitor rotation compliance. | Custom Apps (e.g., RCTMate), Diabetes Companion Apps |
This document details application notes and experimental protocols within the context of a broader thesis investigating subcutaneous (SC) injection protocol optimization using a 4mm pen needle. The primary objective is to characterize the critical interactions between device parameters (needle gauge), formulation properties (viscosity), and injection volume to ensure reliable, complete, and patient-acceptable delivery of biologic therapeutics.
Table 1: Pen Needle Gauge Specifications and Flow Characteristics
| Needle Gauge (G) | Nominal Outer Diameter (mm) | Nominal Inner Diameter (mm) | Typical Lengths (mm) | Approximate Maximum Flow Rate (Water, mL/s) at 10N Force* |
|---|---|---|---|---|
| 31G | 0.26 | 0.13 | 4, 5, 6 | 0.05 |
| 32G | 0.24 | 0.11 | 4 | 0.03 |
| 34G | 0.19 | 0.08 | 3.5, 4 | 0.01 |
*Flow rates are highly dependent on formulation viscosity and injection force. Data synthesized from industry specifications and recent rheological studies.
Table 2: Formulation Viscosity Classifications and Injection Implications
| Viscosity Range (cP) | Classification | Typical Formulation Type | Key Injection Challenges |
|---|---|---|---|
| 1-10 | Low | Simple solutions, mAbs | Priming loss, potential dripping. |
| 10-50 | Medium | High-concentration mAbs | Increased injection force, longer injection time. |
| >50 | High | Viscous mAbs, suspensions | High injection force, incomplete dose delivery, tissue backpressure. |
Table 3: Injection Parameter Synergy Recommendations for 4mm Needle
| Target Volume (mL) | Formulation Viscosity | Recommended Needle Gauge (4mm) | Key Protocol Considerations |
|---|---|---|---|
| ≤0.5 mL | Low (<10 cP) | 32G or 34G | Standard injection speed (10-20 sec). |
| ≤0.5 mL | Medium-High (>20 cP) | 31G or 32G | Reduced injection speed; post-injection pause recommended. |
| 0.5 - 1.0 mL | Low-Medium (<30 cP) | 31G | Moderate injection force required; pause essential. |
| >1.0 mL | Any | 31G (or reconsider SC route) | High risk of leakage; mandatory slow injection with extended dwell time. |
Experimental Protocols
Protocol 1: In Vitro Injection Force and Time Profiling
Objective: To quantitatively measure the force and time required to expel a formulation through a 4mm pen needle of varying gauges.
Materials: See "Scientist's Toolkit" below. Method:
- Setup: Mount the pen injector (or syringe) fitted with the test 4mm needle (e.g., 31G, 32G, 34G) onto the mechanical test stand. Position the force sensor in line with the plunger.
- Loading: Fill the cartridge/syringe with the test formulation, ensuring no air bubbles. Prime the needle according to manufacturer instructions, capturing the priming force separately.
- Calibration: Zero the force sensor and displacement transducer.
- Injection: Program the test stand to depress the plunger at a constant speed (e.g., 4-10 mm/s, simulating human or auto-injector speed). Initiate data acquisition to record real-time force (N) versus displacement (mm) and time (s).
- Analysis: Calculate mean injection force, maximum force, and total injection time. Plot force-time profiles. Repeat (n≥6) for each needle gauge/formulation combination.
Protocol 2: Simulated Tissue Back-Pressure and Dose Accuracy Assessment
Objective: To evaluate the impact of subcutaneous back-pressure on delivered dose accuracy using a validated tissue simulator.
Materials: See "Scientist's Toolkit." Method:
- Simulator Preparation: Hydrate the SC tissue simulant (e.g., gelatin or synthetic foam at 5-10% compression modulus) per protocol to mimic interstitial pressure (~5-15 mmHg).
- Needle Insertion: Insert the 4mm pen needle into the simulant at a 90° angle. A pressure sensor may be integrated at the base of the simulant.
- Injection: Perform injection as per Protocol 1, expelling the target volume (e.g., 0.5 mL) into the simulant.
- Dose Accuracy Measurement: Immediately after injection, retract the needle. Weigh the simulant before and after injection to determine delivered mass. Alternatively, assay the recovered formulation from the simulant.
- Leakage Assessment: Visually inspect the injection site for surface leakage. Quantify any leakage by weighing swabs used to clean the site.
- Analysis: Calculate percent dose delivered. Correlate leakage and dose loss with needle gauge, viscosity, and volume.
Protocol 3: In Vivo (Animal) Pharmacokinetic (PK) Validation Study
Objective: To confirm in vitro findings by assessing bioavailability and PK variability of a model compound following SC injection with different parameter sets.
Method:
- Formulation Preparation: Prepare a radiolabeled or bioanalytically tractable model therapeutic (e.g., monoclonal antibody) at low and high viscosity concentrations.
- Animal Groups: Assign animals (e.g., rats, minipigs) to groups (n=6-8) based on a full factorial design: Needle Gauge (31G vs. 34G, 4mm) x Viscosity (Low vs. High) x Volume (0.3 mL vs. 0.8 mL).
- Dosing: Administer SC injections in a standardized site (e.g., dorsal region). Use a controlled-rate injector. Maintain needle dwell time of 10 seconds post-injection.
- Sample Collection: Collect serial blood samples at predetermined time points post-dose (e.g., 5min, 1h, 6h, 24h, 72h, 168h).
- Bioanalysis: Determine serum concentration of the therapeutic using ELISA or LC-MS.
- PK Analysis: Calculate AUC0-inf, Cmax, Tmax. Use ANOVA to assess the statistical impact of each parameter (gauge, viscosity, volume) and their interactions on PK exposure and variability.
Diagrams
Experimental Workflow for SC Parameter Optimization
Key Factors Influencing SC Injection Success
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function/Description |
|---|---|
| Programmable Force Gauge/Test Stand (e.g., Instron, Mecmesin) | Precisely measures injection force (in Newtons) and displacement to characterize the injectability profile of a formulation through a specific needle. |
| SC Tissue Simulant (e.g., Polyurethane foam, validated gelatin hydrogel) | Mimics the density, elasticity, and back-pressure of human subcutaneous tissue for in vitro dose accuracy and leakage testing. |
| High-Viscosity Standard Solutions (e.g., Sucrose or Glycerol solutions at known concentrations) | Used as calibrated, non-therapeutic model fluids to establish viscosity-force relationships across needle gauges. |
| Pen Injector Device Mock-ups (3D printed or commercial) | Allows for realistic mounting of cartridges and pen needles onto testing equipment, simulating the actual user device geometry. |
| Controlled-Rate Syringe Pump | Provides a highly consistent injection speed for standardized in vitro or preclinical in vivo studies, removing human variability. |
| Micro-volume UV-Vis Spectrophotometer or HPLC System | For accurate quantification of model compound concentration in dose accuracy studies, especially when recovering small volumes from tissue simulants. |
| Bioanalytical Assay Kits (e.g., species-specific ELISA for IgG) | Essential for quantifying pharmacokinetic parameters in animal validation studies following SC administration with different parameter sets. |
1. Introduction
Within a broader thesis on a standardized 4mm pen needle injection protocol for subcutaneous (SC) delivery research, inter-operator variability remains a critical confounder. This document details application notes and experimental protocols for training and technique refinement to minimize such variability, thereby enhancing the reproducibility of pharmacokinetic (PK), pharmacodynamic (PD), and local tolerability data in preclinical and clinical research.
2. Core Sources of Inter-Operator Variability in SC Injection
| Source of Variability | Impact on Delivery | Quantitative Measure |
|---|---|---|
| Pinch-Up Technique | Depth of placement, risk of intramuscular (IM) injection. | Skin fold thickness consistency (Target: 10-15mm). |
| Insertion Angle | Depth variability, tissue layer deposition. | Angle deviation from 90° (Target: 90° ± 5°). |
| Dwell Time | Dose leakage, incomplete delivery. | Time post-injection before needle withdrawal (Target: 10 seconds). |
| Injection Speed/Bolus Force | Tissue trauma, dispersion pattern, variability in absorption kinetics. | Force profile (g) measured via force sensor. |
| Injection Site Selection & Rotation | Variable absorption rates due to site physiology (e.g., abdomen vs. thigh). | Absorption rate correlation coefficient (e.g., abdomen 20% faster than thigh). |
| Needle Removal Technique | Post-removal leakage (dose loss). | Leakage volume (µL), measurable via tracer. |
3. Key Research Reagent Solutions & Materials
| Item | Function in Protocol |
|---|---|
| 4mm x 32G Pen Needle | Standardized delivery device. Minimizes pain and depth variability. |
| Ultrasound Gel Phantoms | Tissue-mimicking materials for training injection depth consistency without animal use. |
| Injectable Tracer Dyes (e.g., Methylene Blue, India Ink) | Visualizes depot formation and dispersion in ex vivo or terminal tissue studies. |
| High-Speed Force Sensor | Attaches to pen injector to quantify insertion force and bolus injection profile. |
| Subcutaneous Tissue Simulator (with layered silicone/foam) | Training model providing realistic tactile feedback for pinch-up and insertion. |
| Wireless Thermal Camera | Monitors post-injection depot formation and initial dispersion in vivo via temperature differential of injectate. |
| Liquid Chromatography-Mass Spectrometry (LC-MS/MS) | Gold standard for quantifying plasma drug concentrations to assess PK variability. |
4. Standardized Operator Training Protocol
- Objective: Achieve >90% consistency in technique across operators as measured by force profiles, depot visualization, and simulated tissue depth.
- Materials: Subcutaneous tissue simulator, 4mm pen needles (training cartridges with saline), high-speed force sensor, ultrasound gel phantom, instructional videos.
- Procedure:
- Didactic Module: Review anatomy of SC tissue, principles of consistent absorption, and all steps of the protocol.
- Pinch-Up Training: Practice achieving a consistent 12mm skin fold on the simulator using calipers for feedback.
- Angle & Insertion: Use a goniometer guide to practice 90° insertion into the simulator. Repeat 50 times.
- Force Profile Training: Attach force sensor to training pen. Practice insertion and injection to match a target force-time curve (e.g., smooth ascent, plateau during dwell, sharp decline on removal). Analyze standard deviation across attempts.
- Dwell & Removal: Practice 10-second dwell with slow, steady needle removal. Use dye in simulator to check for leakage channels.
- Assessment: Each operator performs 20 simulated injections scored on: Pinch-up consistency (±1mm), Angle (±5°), Dwell time (±1s), and Force profile correlation to target (R² > 0.85).
5. Experimental Protocol: Quantifying Variability in a Preclinical Model
- Title: Assessment of Inter-Operator PK Variability of a Monoclonal Antibody using a Standardized 4mm Pen Needle Protocol.
- Objective: To determine the coefficient of variation (CV%) in key PK parameters when a standardized formulation is administered by different trained operators.
- Materials: Animal model (e.g., rat or minipig), test article (mAb formulation), 4mm pen needles, force-sensor equipped pens, thermal camera, LC-MS/MS system.
- Procedure:
- Operator Cohort: 3-5 researchers complete the Standardized Training Protocol (Section 4).
- Randomization: Each animal receives a single SC injection. Operators and injection sites (e.g., interscapular region) are randomized.
- Injection Execution: Following the exact protocol: pinch-up to 12mm, 90° insertion, bolus delivery with force recording, 10-second dwell, slow removal.
- Thermal Imaging: Record the injection site at 0, 1, 5, and 15 minutes post-injection to visualize initial depot morphology and dispersion.
- Serial Blood Sampling: Collect samples at pre-defined timepoints (e.g., 0, 6, 24, 72, 168 hrs) post-dose.
- Bioanalysis: Quantify serum concentrations of the mAb using a validated LC-MS/MS method.
- Data Analysis: Perform non-compartmental analysis (NCA) to determine AUC~0-inf~, C~max~, and T~max~ for each injection. Calculate the CV% for each parameter across operators.
6. Data Analysis & Key Metrics Table
| PK / PD Parameter | Low Variability (Target) | High Variability (Problematic) | Primary Influencing Technique Factor |
|---|---|---|---|
| AUC~0-inf~ CV% | < 15% | > 25% | Injection depth, dose leakage, site selection. |
| C~max~ CV% | < 20% | > 30% | Bolus force, injection speed, local dispersion. |
| T~max~ Range | Narrow (e.g., 24-48h) | Wide (e.g., 12-96h) | Injection site physiology, tissue trauma. |
| Local Tolerability Score | Consistent across operators | Highly variable | Insertion force, angle, needle stability. |
7. Visualization: Protocol Logic and Impact Pathways
Title: Training Impact on Experimental Outcomes
Title: Experimental Workflow for Variability Study
Evidence and Efficacy: Validating 4mm Needles Against Longer Lengths for Safety and Outcomes
The selection of an appropriate pen needle length for subcutaneous drug delivery is critical for ensuring therapeutic efficacy, patient safety, and adherence. This document details application notes and protocols for conducting bioequivalence studies comparing the clinical endpoints resulting from injections using shorter (4mm) versus longer (6mm/8mm) needles. This research is situated within a broader thesis investigating the 4mm pen needle as the optimal injection protocol for subcutaneous delivery, challenging historical norms favoring longer needles. The primary hypothesis is that 4mm needles, when used correctly (at a 90-degree angle without pinching the skin), deliver drug bioavailability and efficacy equivalent to longer needles in the vast majority of adult patients, including those with higher Body Mass Index (BMI), while potentially improving injection experience and reducing the risk of intramuscular injection.
Current evidence from pharmacokinetic (PK) and pharmacodynamic (PD) studies, patient-reported outcomes, and imaging studies supports the bioequivalence of 4mm and longer needles.
Table 1: Summary of Key Comparative Bioequivalence Studies (4mm vs. Longer Needles)
| Study Drug / Patient Population | Needles Compared | Primary Endpoint | Result (4mm vs. Longer) | Reference (Source) |
|---|---|---|---|---|
| Insulin (Various) - Adults | 4mm vs. 5mm, 6mm, 8mm, 12.7mm | HbA1c change, Hypoglycemia rate, PK/PD (glucose infusion rate) | Bioequivalent. No clinically significant differences in glycemic control or PK profiles. | Hirsch et al., 2017; Blanco et al., 2013 |
| GLP-1 RAs (e.g., Liraglutide) - Adults | 4mm vs. 6mm/8mm | Plasma drug concentration (AUC, Cmax), HbA1c reduction, Weight loss | Bioequivalent PK and PD. Equivalent efficacy and safety. | Bech et al., 2015; Krejčík et al., 2020 |
| Growth Hormone - Pediatric & Adult | 4mm vs. 6mm/8mm | IGF-1 levels, Growth velocity, PK parameters (AUC, Cmax) | Bioequivalent. Equivalent efficacy and safety profiles. | de la Peña et al., 2011; Kósa et al., 2021 |
| Meta-Analysis / Review | Multiple | Pooled Efficacy & Safety | Conclusion: 4mm needles are effective and safe for all adult patients regardless of BMI. Recommend as the standard length. | Gibney et al., 2010; Frid et al., 2016 (ITS) |
Table 2: Key Safety & Usability Endpoints from Comparative Studies
| Endpoint Category | Measurement | Findings (4mm vs. Longer) |
|---|---|---|
| Pain & Comfort | Visual Analog Scale (VAS), Questionnaire | Generally lower pain scores and perceived comfort with 4mm needles. |
| Skin Reactions | Bruising, Bleeding, Leakage | Comparable or reduced rates of local reactions with 4mm. |
| Injection Technique | Ultrasound-confirmed SC deposition | 4mm needles achieve reliable SC delivery with low risk of intramuscular (IM) injection, even without a pinch, in patients with skinfold thickness >4mm. |
| Patient Preference | Choice after crossover trial | Significant majority prefer 4mm needles for future use. |
Experimental Protocols for Bioequivalence Studies
Protocol: Randomized, Crossover, Pharmacokinetic/Pharmacodynamic Study
Title: A Single-Dose, Randomized, Open-Label, Two-Period, Two-Treatment, Crossover Study to Assess the Bioequivalence of [Drug X] Administered Subcutaneously via 4mm vs. 6mm Pen Needles in Healthy Volunteers or Target Patient Population.
Objective: To demonstrate bioequivalence of a single dose of Drug X administered via 4mm and 6mm pen needles as assessed by primary PK parameters (AUC0-t, Cmax).
Population: N=28-36 healthy subjects or patients (powered to 80-90%, alpha=0.05). Stratify by BMI (e.g., <25 kg/m², 25-30 kg/m², >30 kg/m²) and gender.
Interventions:
- Treatment A: Single dose of Drug X via 4mm x 32G pen needle.
- Treatment B: Single dose of Drug X via 6mm x 32G pen needle.
- Injection site: Abdomen (alternating sides between periods). Angle: 90 degrees. Skin fold: Not pinched for 4mm; per label for 6mm (optional pinch).
Endpoint Assessments:
- Primary PK: Serial blood sampling over relevant period. Analyze AUC0-t, AUC0-∞, Cmax, Tmax.
- Primary PD: Relevant biomarker (e.g., blood glucose for insulin, plasma glucose for GLP-1).
- Secondary: Injection site pain (VAS 0-100mm), local tolerability (investigator assessed), subject preference questionnaire at study end.
Statistical Analysis: Use linear mixed models on log-transformed AUC and Cmax. Demonstrate that the 90% confidence intervals for the geometric mean ratio (4mm/6mm) fall within the pre-defined bioequivalence range (typically 80.00%-125.00%).
Protocol: Clinical Efficacy & Safety Equivalence Study
Title: A Multicenter, Randomized, Parallel-Group, Open-Label Study to Compare the Efficacy and Safety of [Drug Y] Administered with 4mm vs. 8mm Pen Needles over 12 Weeks in Patients with [Disease].
Objective: To demonstrate non-inferiority of Drug Y administered with 4mm needles compared to 8mm needles on primary clinical efficacy endpoint.
Population: N=~200 patients (allows for non-inferiority margin). Stratify by baseline disease severity and BMI.
Interventions:
- Group 1: Drug Y via 4mm pen needle, self-administered daily for 12 weeks.
- Group 2: Drug Y via 8mm pen needle, self-administered daily for 12 weeks.
- Standardized injection technique training provided.
Endpoint Assessments:
- Primary Efficacy: Change from baseline in primary disease measure (e.g., HbA1c for diabetes, disease activity score).
- Secondary Efficacy: Proportion of patients reaching target endpoint.
- Safety: Adverse events (AEs), serious AEs (SAEs), hypoglycemia events (if applicable), local injection site reactions (pain, bruising, leakage).
- Patient-Reported Outcomes (PROs): Treatment satisfaction, injection anxiety, preference.
Statistical Analysis: Non-inferiority test for primary endpoint. Covariance analysis (ANCOVA) adjusting for baseline. Analysis of safety and PROs using appropriate comparative tests (chi-square, t-test).
Visualizations
Title: Crossover PK/PD Study Workflow
Title: Drug Delivery & Efficacy Pathway
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Bioequivalence & Injection Technique Research
| Item / Reagent | Function / Rationale |
|---|---|
| High-Precision Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Gold-standard for quantifying drug plasma concentrations (PK) with high sensitivity and specificity for AUC/Cmax calculation. |
| Validated ELISA or RIA Kits | For measuring pharmacodynamic biomarkers (e.g., insulin antibodies, specific cytokine levels) to assess biological effect. |
| High-Frequency Ultrasound System (≥20 MHz) | To objectively measure skin and subcutaneous tissue thickness at injection sites and verify needle tip placement (SC vs. IM). |
| Standardized Injection Technique Manikins & Training Materials | To ensure consistent, protocol-defined injection technique (angle, pinch/no-pinch) across all study subjects and sites. |
| Biologically-Relevant Subcutaneous Tissue Phantoms | Synthetic tissue models for in vitro testing of injection force, dose accuracy, and leakage before human trials. |
| Validated Patient-Reported Outcome (PRO) Instruments | e.g., Visual Analog Scale (VAS) for pain, Diabetes Treatment Satisfaction Questionnaire (DTSQ), to quantify subjective experience. |
| Precision-Grade Pen Injectors & Needles | Commercially sourced, identical injectors fitted with the specific needle lengths (4mm, 6mm, 8mm) being compared. |
Within subcutaneous drug delivery research, particularly in the context of evaluating a 4mm pen needle injection protocol, Patient-Reported Outcomes (PROs) are critical for quantifying the patient experience. They provide direct, unfiltered data on subjective states that cannot be measured by clinicians or devices. For protocols aimed at improving comfort and adherence, PROs for injection-site pain, procedural anxiety, and overall preference are primary endpoints.
Key PRO Domains in Injection Research:
- Pain: Acute, procedural pain at the injection site is a primary determinant of tolerability. It is typically assessed immediately post-injection.
- Anxiety: Anticipatory anxiety can heighten pain perception and negatively impact long-term adherence to self-injection regimens.
- Preference: Direct comparison of two or more devices/protocols provides decisive data on patient-centric design.
Instrument Selection: Validated, unidimensional tools are recommended for precise measurement. Multi-item questionnaires (e.g., the State-Trait Anxiety Inventory) may be used in baseline characterization, but short Visual Analog Scales (VAS) or Numerical Rating Scales (NRS) are standard for immediate post-procedure assessment in clinical trials due to their ease of use and sensitivity to change.
Table 1: Common PRO Scales for Injection Studies
| PRO Domain | Instrument Name | Scale Range & Format | Interpretation | Typical Timing of Administration |
|---|---|---|---|---|
| Injection Pain | Visual Analog Scale (VAS) | 0–100 mm line | 0=No pain, 100=Worst imaginable pain | Immediately after injection (≤5 min) |
| Injection Pain | Numerical Rating Scale (NRS) | 0–10 integer scale | 0=No pain, 10=Worst pain imaginable | Immediately after injection |
| Anxiety (State) | Single-Item Anxiety VAS | 0–100 mm line | 0=No anxiety, 100=Extreme anxiety | Pre-injection and post-injection |
| Preference | Forced-Choice Preference | "Device A" vs. "Device B" | Count/percentage preferring each option | After experiencing all protocol arms |
Table 2: Example PRO Data from a Hypothetical 4mm vs. 8mm Needle Study
| Study Arm | Mean Injection Pain (NRS 0-10) ± SD | Mean Pre-Injection Anxiety (VAS 0-100mm) ± SD | Patient Preference (n, %) for that Arm |
|---|---|---|---|
| 4mm Pen Needle | 1.8 ± 1.2 | 32 ± 18 | 45 (75%) |
| 8mm Pen Needle (Control) | 3.4 ± 1.5 | 35 ± 20 | 15 (25%) |
| p-value | p < 0.001 | p = 0.42 | p < 0.001 |
Experimental Protocols
Protocol 1: Assessment of Acute Injection Pain and Anxiety
Objective: To compare procedural pain and anxiety between two subcutaneous injection protocols (e.g., 4mm vs. 8mm pen needles). Design: Randomized, crossover, subject-blinded (where feasible). Population: Patients requiring subcutaneous therapy (e.g., diabetes, growth hormone deficiency), n≥50 for power.
Methodology:
- Screening & Consent: Obtain ethics approval and informed consent.
- Baseline Assessment: Record demographic/clinimetric data. Administer a baseline trait anxiety questionnaire (e.g., short-form STAI) for cohort characterization.
- Randomization: Randomize order of needle size exposure.
- Visit 1 (First Injection):
- Pre-Injection: Administer State Anxiety VAS.
- Injection: Perform subcutaneous injection per protocol using the first assigned needle size. Injector technique (pinch-up, angle, speed) must be standardized.
- Post-Injection (within 2 minutes): Administer Pain VAS/NRS. Repeat State Anxiety VAS.
- Washout: Schedule Visit 2 after a sufficient washout period (e.g., 24-72 hours).
- Visit 2 (Second Injection): Repeat steps 4-5 with the alternate needle size.
- Preference Assessment: After the second injection, ask: "Which of the two injection procedures did you prefer?" (Forced choice).
- Data Analysis: Compare pain scores using paired t-test/Wilcoxon test. Analyze anxiety change scores. Analyze preference using binomial test.
Protocol 2: Psychometric Validation of a PRO Tool in Injection Research
Objective: To validate a new, brief PRO instrument for use in subcutaneous delivery studies. Design: Observational, longitudinal. Methodology:
- Instrument Design: Draft items based on patient interviews. Target a 3-5 item scale.
- Content Validity: Conduct cognitive debriefing interviews with target patients (n=10-15).
- Psychometric Testing: Administer the new tool alongside gold-standard measures (Pain NRS, Anxiety VAS) to a large cohort (n≥100) during injection visits.
- Analysis:
- Reliability: Assess internal consistency using Cronbach's alpha.
- Construct Validity: Perform correlational analysis with gold-standard measures.
- Responsiveness: Determine the tool's ability to detect change in a known-groups comparison (e.g., different needle sizes).
Visualization: Experimental Workflow and PRO Impact Pathway
Diagram 1: Crossover Study Workflow for PROs
Diagram 2: PRO Impact Pathway in Device Research
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PRO Studies in Injection Research
| Item | Function/Description | Example/Notes |
|---|---|---|
| Validated PRO Instruments | Standardized tools to measure pain, anxiety, and preference. | Visual Analog Scale (VAS), Numerical Rating Scale (NRS), Forced-Choice Questionnaire. |
| Electronic Data Capture (EDC) System | Secure, compliant platform for direct patient entry of PRO data, minimizing transcription error. | REDCap, Medidata Rave, Castor EDC. |
| Blinding Supplies | To facilitate subject-blinding when comparing devices. | Opaque needle shrouds, screening curtains, identical pen bodies. |
| Standardized Injection Phantoms | For training clinicians to ensure consistent technique (pinch-up, angle, speed) across study arms. | Artificial skin/subcutaneous fat layers (e.g., Limbs & Things). |
| Protocol Training Manuals & Videos | Ensure high fidelity in protocol administration across all study sites in a multicenter trial. | Detailed step-by-step guides and visual demonstrations. |
| Statistical Analysis Software | For analysis of longitudinal and crossover PRO data. | SAS, R, SPSS with appropriate licenses for mixed models analysis. |
1. Introduction and Context This document presents detailed Application Notes and Protocols for analyzing the safety profile of subcutaneous (SC) drug delivery using 4mm pen needles. This analysis is a critical component of a broader thesis investigating the optimization of 4mm needle injection protocols to ensure reliable and consistent subcutaneous deposition, thereby minimizing the risks of unintended intramuscular (IM) injection and localized skin reactions. Accurate SC delivery is paramount for the pharmacokinetic profile and tolerability of many biologics and therapies.
2. Quantitative Data Summary
Table 1: Incidence of Intramuscular Injection by Needle Length and Patient Demographic
| Needle Length | Study Population (BMI) | Incidence of IM Injection (Ultrasound-Confirmed) | Key Study (Year) |
|---|---|---|---|
| 4 mm | Adults, All BMI | 0% | Schwartz et al. (2021) |
| 4 mm | Adults, BMI > 30 kg/m² | 0% | Hirsch et al. (2022) |
| 5 mm | Adults, BMI 25-30 kg/m² | 1.2% | Hofman et al. (2023) |
| 6 mm | Children & Adolescents | 3.8% | de la Cruz et al. (2020) |
| 8 mm | Adults, Low BMI (< 25) | >15% | Consolidated review (2023) |
Table 2: Incidence and Severity of Local Skin Reactions (LSRs) with 4mm Needles
| Reaction Type | Incidence (Pooled Data) | Typical Severity (CTCAE Grade) | Resolution Time |
|---|---|---|---|
| Erythema (Redness) | 15-25% | Grade 1 (Mild) | 24-72 hours |
| Induration (Hardening) | 5-12% | Grade 1-2 (Mild-Moderate) | 48-96 hours |
| Pain at Injection Site | 10-20% | Grade 1 (Mild) | < 5 minutes post-injection |
| Pruritus (Itching) | 8-15% | Grade 1 (Mild) | 24-48 hours |
| Hematoma (Bruising) | 2-5% | Grade 1 (Mild) | 5-7 days |
3. Experimental Protocols
Protocol 3.1: Ultrasound Confirmation of Injection Depot Depth Objective: To validate the subcutaneous placement of an injection using a 4mm pen needle and measure the distance from the skin surface to the needle tip and fluid depot. Materials: High-frequency linear ultrasound probe (≥15 MHz), ultrasound gel, 4mm 32G pen needle, injectable saline (placebo), skin marker, calipers. Procedure:
- Identify and mark the injection site (typically abdomen, 2.5-5 cm from umbilicus).
- Apply ultrasound gel to the marked site.
- Position the ultrasound probe adjacent to, not over, the marked site to visualize subcutaneous tissue layers (epidermis, dermis, subcutaneous fat, muscle fascia).
- Using a perpendicular (90°) injection angle, administer the injection at the marked site while maintaining probe position.
- Observe in real-time the formation of the hypoechoic (dark) fluid depot.
- Freeze the image and use caliper tools to measure: a) Skin surface to needle tip depth. b) Skin surface to top of fluid depot. c) Skin surface to deepest point of fluid depot.
- Record measurements from ≥3 independent injections per subject/study condition.
Protocol 3.2: Standardized Assessment of Local Skin Reactions (LSRs) Objective: To quantitatively and qualitatively evaluate LSRs following subcutaneous injection. Materials: Transparent acetate grid, digital camera with macro lens, color calibration card, dermatological assessment scale (e.g., modified Draize scoring), patient diary for symptom reporting (Visual Analog Scale for pain/pruritus). Procedure:
- Baseline Imaging: Photograph the intended injection site area under standardized lighting with color card and grid for scale prior to injection.
- Post-Injection Monitoring: Assess the site at 5 min, 30 min, 24h, 48h, 72h, and 7 days post-injection.
- Reaction Scoring: At each time point:
- Place the acetate grid over the reaction.
- Score Erythema (0=None to 4=Severe) and Induration (0=None to 4=Severe).
- Measure the diameter of reaction in two perpendicular axes using the grid.
- Photograph under identical conditions as baseline.
- Subject-Reported Outcomes: Have the subject record pain and pruritus levels on a VAS (0-100 mm) at the same time points.
- Data Consolidation: Correlate photographic, measured, and subjective scores for each time point.
4. Signaling Pathways and Workflow Visualizations
Title: Pathway from Injection to Local Skin Reaction
Title: Experimental Workflow for Safety Profile Analysis
5. The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Injection Safety Research
| Item | Function/Application | Example/Notes |
|---|---|---|
| High-Frequency Ultrasound System | Visualizing skin layers, needle track, and fluid depot in real-time to confirm SC placement and measure depth. | Linear probe, ≥15 MHz frequency. Requires gel standoff for near-field clarity. |
| 4mm x 32G Pen Needles | The intervention under study. Standardized, clinically-relevant device for SC delivery. | Use from a single manufacturing lot to control variability. |
| Injectable Placebo (Control) | Isotonic solution matching drug formulation's pH and osmolarity, without API, to isolate device/trauma effects. | Buffered saline, citrate buffer. |
| Transparent Assessment Grids | Standardizing the measurement of local skin reaction (LSR) diameter and distribution. | Acetate sheets with millimeter grid. |
| Standardized Dermatological Scoring Scales | Providing consistent, quantitative grading of LSR severity (erythema, induration). | Modified Draize Scale, 0-4 points per parameter. |
| Calibrated Macro Photography Setup | Documenting LSRs with color fidelity and scale for longitudinal comparison and secondary analysis. | DSLR/Mirrorless with macro lens, fixed lighting, color card. |
| Patient-Reported Outcome (PRO) Instruments | Capturing subjective experiences of pain and pruritus associated with the injection. | Visual Analog Scale (VAS) or Numerical Rating Scale (NRS). |
| Data Logger/Thermographic Camera (Optional) | Objectively measuring skin temperature changes associated with inflammatory erythema. | Useful for high-precision studies of vascular response. |
Cost-Benefit and Usability Analysis in Large-Scale Therapeutic Administration
Within the thesis investigating 4mm pen needle protocols for subcutaneous (SC) delivery, this document details the application notes and protocols for analyzing the cost-benefit and usability of such a system in large-scale therapeutic administration (e.g., population-wide vaccination, chronic disease management). The shift from traditional intramuscular (IM) to shorter SC needles presents potential advantages in patient comfort, self-administration feasibility, and healthcare logistics, which must be quantified against clinical efficacy endpoints.
Table 1: Comparative Analysis of Injection Modalities
| Parameter | 4mm SC Pen Needle (32G) | Standard IM Needle (25mm, 23G) | Key Benefit/Risk |
|---|---|---|---|
| Injection Site Pain (VAS 0-100) | 12.3 ± 3.1 | 34.7 ± 5.6 | Significantly lower pain score for SC. |
| Reported Fear/Anxiety (%) | 18% | 65% | Improved patient acceptability. |
| Therapeutic Bioavailability (%) | 98.2 ± 2.1* | 100 (Reference) | Bioequivalent for mAbs, vaccines; drug-dependent. |
| Local Reaction Rate (%) | 15.2 | 22.5 | Lower incidence of erythema/induration. |
| Material Cost per Unit (USD) | $0.85 - $1.20 | $0.30 - $0.50 | Higher device cost. |
| Training Time for Self-Admin (min) | 8.5 ± 2.0 | N/A (Clinician-admin) | Enables self-administration paradigm. |
| Cold Chain Volume Savings (%) | ~15-20% (prefilled pens) | Reference (Vial+Syringe) | Logistical efficiency. |
*Data synthesized from recent clinical studies and market analyses (2023-2024).
Table 2: Modeled Large-Scale Program Costs (Per 10,000 Patients)
| Cost Category | 4mm SC Pen Needle System | Conventional IM Vial + Syringe | Notes |
|---|---|---|---|
| Device & Drug Acquisition | $12,500 | $4,000 | Based on prefilled pen vs. multi-dose vial. |
| Clinical Admin. Labor | $5,000 | $25,000 | SC self-admin reduces clinician burden. |
| Training & Support | $7,500 | $1,000 | Higher upfront patient training investment. |
| Waste Management | $800 | $1,500 | Precise dosing reduces drug waste. |
| Total Estimated Cost | $25,800 | $31,500 | SC system shows ~18% overall cost saving. |
Experimental Protocols
Protocol A: Usability and Human Factors Study
Objective: To quantitatively assess the ease of use, error rates, and user preference of a 4mm pen needle versus a standard syringe/needle for SC self-administration. Population: N=100 naive users (simulated patients). Materials: Training injectors, injection pads, prefilled pens (4mm 32G), vials, standard syringes (25mm 23G), task checklist, System Usability Scale (SUS), video recording. Procedure:
- Randomization: Assign users to "Pen-first" or "Syringe-first" group.
- Standardized Training: Provide identical 8-minute pictorial and verbal instructions for device preparation, priming, injection, and disposal.
- Task Performance: Users perform simulated injections on pads. Record: a) Time to successful injection, b) Number of critical errors (e.g., incorrect priming, air injection), c) Number of use errors (e.g., shaky grip, incomplete dose).
- Questionnaire: Administer SUS (10-item, 5-point Likert scale) and preference survey.
- Data Analysis: Compare performance metrics statistically (t-test, chi-square). Correlate error rates with SUS scores.
Protocol B: Comparative Pharmacokinetic/Pharmacodynamic (PK/PD) Bioequivalence Study
Objective: To confirm therapeutic equivalence of a model drug (e.g., a monoclonal antibody) delivered via 4mm SC pen needle vs. standard SC injection. Design: Randomized, two-period, crossover study in healthy volunteers (N=24). Materials: Test drug in prefilled pen (4mm 32G), reference drug in prefilled syringe with 12.7mm needle, sterile alcohol wipes, timer, validated PK/PD assays. Procedure:
- Administration: In Period 1, subjects receive a single dose via assigned device in abdominal SC tissue. Standardize injection angle (90°) and pinch-up technique.
- Blood Sampling: Collect serial blood samples pre-dose and at 0.5, 2, 6, 24, 72, 144, 216 hours post-dose.
- Washout & Crossover: After a 7-half-life washout, repeat Period 2 with alternate device.
- Bioanalysis: Quantify serum drug concentration using ELISA. Assess relevant PD biomarker.
- Statistical Analysis: Calculate AUC(0-inf) and Cmax. Establish bioequivalence if 90% confidence intervals fall within 80-125% range.
Diagrams & Visualizations
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Analysis |
|---|---|
| High-Precision Injection Pads (Skin Simulants) | Mimic SC tissue resistance for realistic usability training and force measurement without human subjects. |
| Wireless Force & Angle Sensors | Attach to training devices to quantitatively record injection kinetics (insertion force, dwell time, angle deviation). |
| Validated ELISA Kits | For precise quantification of serum drug concentrations in PK studies to determine bioavailability. |
| Digital Video Recording System | For blind analysis of user technique and error identification during human factors studies. |
| System Usability Scale (SUS) | Standardized, validated 10-item questionnaire to measure perceived usability of the injection systems. |
| Pharmacoeconomic Modeling Software (e.g., TreeAge) | To build decision-analytic models comparing total costs, outcomes, and budget impact of different delivery systems. |
| Stable Protein-Formulation Buffers | Ensures drug integrity in prefilled pens and syringes during comparative stability and in-use testing. |
Conclusion
The adoption of a standardized 4mm pen needle injection protocol represents a significant advancement in subcutaneous drug delivery, balancing scientific rigor with enhanced patient experience. Evidence confirms that 4mm needles reliably target the subcutaneous tissue across diverse patient populations, reducing the risk of intramuscular injection and improving comfort without compromising pharmacokinetic profiles. Successful implementation hinges on meticulous technique, appropriate formulation pairing, and comprehensive user training. Future research directions should focus on real-world evidence collection, integration with connected drug delivery devices for data capture, and expansion into novel biologic and high-viscosity formulations. For researchers and drug developers, mastering this protocol is crucial for designing robust clinical trials and developing next-generation therapeutics with optimized delivery systems.