Optimizing Glycemic Control: A Scientific Review of Injection Site Rotation for the Prevention of Insulin-Associated Lipodystrophy
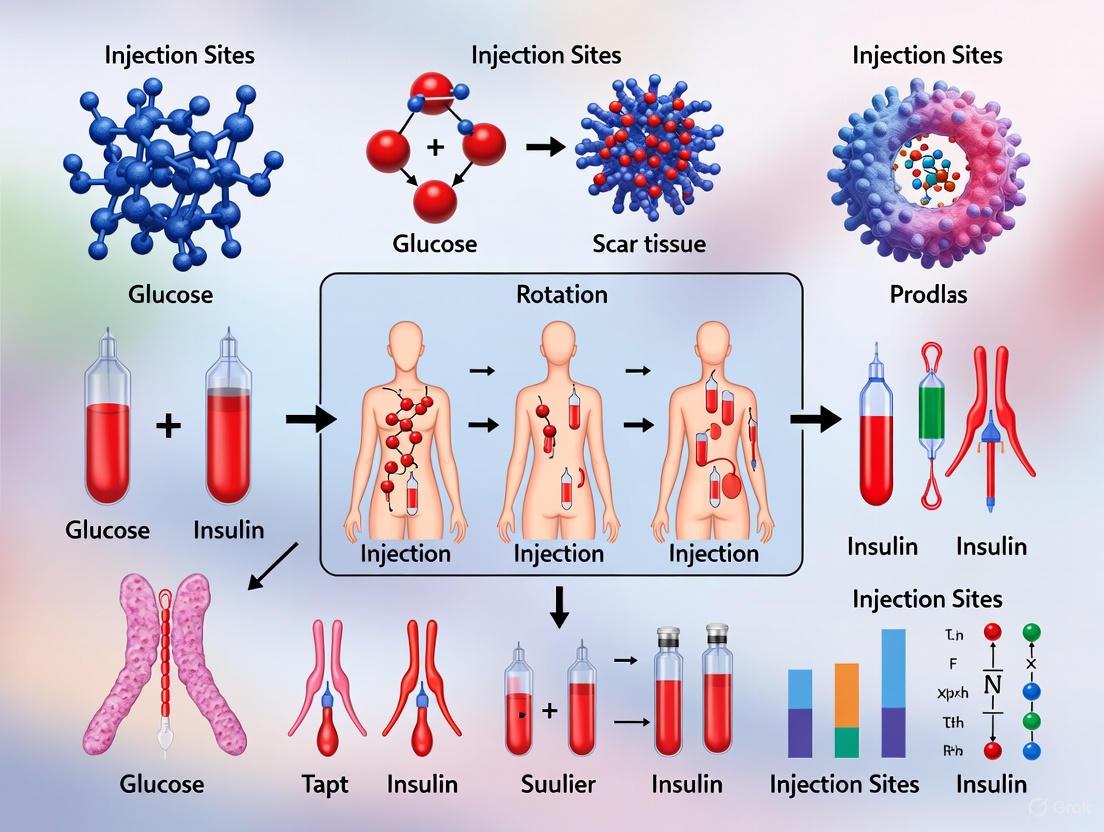
This article provides a comprehensive analysis for researchers and clinical scientists on the critical role of injection site rotation in preventing lipodystrophy, a common complication of insulin therapy.
Optimizing Glycemic Control: A Scientific Review of Injection Site Rotation for the Prevention of Insulin-Associated Lipodystrophy
Abstract
This article provides a comprehensive analysis for researchers and clinical scientists on the critical role of injection site rotation in preventing lipodystrophy, a common complication of insulin therapy. We explore the underlying pathophysiology of lipohypertrophy, its significant impact on glycemic variability and insulin pharmacokinetics, and the barriers to effective prevention. The content systematically reviews evidence-based injection protocols, advanced detection methodologies including ultrasound, and evaluates the efficacy of structured educational interventions. By synthesizing current evidence and identifying research gaps, this review aims to inform both clinical practice and the development of next-generation insulin delivery systems.
The Pathophysiology and Clinical Impact of Insulin-Associated Lipohypertrophy
Definition and Clinical Significance
Lipohypertrophy (LH) is defined as a tumor-like lump, visible and touchable, comprising swollen adipose tissue at the site of repeated insulin injection [1]. It represents the most prevalent local cutaneous complication of insulin therapy, with reported prevalence in insulin-treated individuals ranging from 11.1% to 73.4%; recent studies in China report rates from 53.1% to 73.4% [1]. This pathology is characterized by the proliferation of adipose tissue and manifests as subcutaneous nodular swelling due to adipose tissue proliferation at injection sites [2]. Histological examination reveals that LH tissue contains a significantly larger number of macro-adipocytes and fibrosis compared to normal adipose tissue [3].
The clinical impact of LH is profound. Injecting insulin into lipohypertrophic tissue significantly impairs insulin absorption, leading to marked hyperglycemia and substantial glycemic variability [2] [1]. This disrupted absorption results in a separation of post-meal blood glucose curves after 30 minutes, leading to significant differences in blood glucose levels from 2 hours onwards and in maximum postprandial blood glucose concentrations [1]. Conversely, when patients subsequently inject their usual insulin dose into unaffected tissue, the risk of unpredictable and severe hypoglycemia increases substantially [3] [1]. These glycemic excursions contribute to poor long-term metabolic control and increased risk of diabetes complications.
Table 1: Epidemiological and Clinical Characteristics of Lipohypertrophy
| Characteristic | Details |
|---|---|
| Global Prevalence in Insulin Users | 11.1% - 73.4% (average ~41.8%) [2] [1] |
| Reported Prevalence in China | 53.1% - 73.4% [1] |
| Primary Etiology | Repeated insulin exposure to subcutaneous tissue [2] [1] |
| Key Histological Features | Macro-adipocytes, fibrosis, dense fibrous texture [3] [1] |
| Impact on Insulin Pharmacokinetics | Slower, unpredictable absorption [1] |
| Key Clinical Consequences | Glycemic variability, unexplained hypoglycemia, hyperglycemia, increased insulin requirements [2] [3] [1] |
Troubleshooting Guides and FAQs for Researchers
Frequently Asked Questions
Q1: What are the primary cellular mechanisms driving lipohypertrophy development? The pathophysiology of insulin-related LH is not fully elucidated, but several mechanisms have been proposed. The predominant theory suggests insulin's anabolic effect on local adipocytes promotes the synthesis of fats and proteins, leading to adipose tissue expansion [1]. Some evidence suggests that anti-insulin antibody levels show a positive relationship with LH, indicating possible immunological factors [1]. Histological studies show that areas with insulin-induced LH contain a significantly larger number of macro-adipocytes and fibrosis compared to normal adipose tissue [3].
Q2: Why does insulin absorption become impaired in lipohypertrophic tissue? The structural properties of LH tissue, characterized by thickened, hard, elastic adipose tissue with large adipocytes and dense fibrous texture, create a physical barrier that makes insulin release slower and more unpredictable [1]. The fibrotic components likely disrupt normal capillary perfusion and create diffusion barriers, leading to blunted and more variable insulin absorption and action, ultimately impairing postprandial glucose control [1].
Q3: What are the key risk factors for lipohypertrophy development in clinical populations? Major risk factors include failure to rotate injection sites, concentrating injections in a small area, needle reuse, injection of cold insulin, high number of daily injections, large injection volumes, and using long and thick needles [3]. Patient behavior is particularly significant, as individuals often prefer reusing less painful tissue and more promptly accessible sites [1].
Q4: What detection methods are most sensitive for identifying early lipohypertrophy? While conventional diagnosis relies on visual inspection and palpation, these methods exhibit limited effectiveness in detecting flat LH lesions [2]. Ultrasound examination emerges as a superior diagnostic modality, offering approximately 30% greater sensitivity in detecting LH compared to palpation [3]. Ultrasound can reveal structural changes in deeper levels of subcutaneous tissue before any visual surface changes appear [3].
Q5: How can researchers differentiate lipohypertrophy from other injection site reactions? LH typically presents as a soft, spongy, or firm swelling at injection sites, unlike lipoatrophy which presents as dimpling or loss of subcutaneous fat [3] [4]. Histologically, LH demonstrates adipocyte hypertrophy and fibrosis rather than the inflammatory infiltrates or fat destruction seen in other conditions. Ultrasound characterization can precisely differentiate LH from other subcutaneous pathologies by revealing distinct echogenicity patterns and structural changes [3].
Table 2: Key Risk Factors for Lipohypertrophy Development
| Risk Factor Category | Specific Factors | Strength of Association |
|---|---|---|
| Injection Technique | Failure to rotate sites, needle reuse (>3 times), small rotation area | Strong [2] [3] [1] |
| Patient Factors | High BMI, long insulin therapy duration, high HbA1c, hypoglycemia history | Moderate [1] |
| Insulin Formulation | Use of regular insulin (3.2-fold risk vs. rapid-acting) [1] | Moderate |
| Device Factors | Longer/thicker needles, improper technique | Moderate [3] |
Experimental Models and Research Methodologies
Established Research Protocols
Protocol 1: Ultrasound Detection and Characterization of Lipohypertrophy
Ultrasound represents the gold standard for non-invasive LH detection in both clinical and research settings [1]. The protocol should utilize high-frequency linear array transducers (≥12 MHz) for optimal subcutaneous tissue resolution. Examination should include:
- B-mode imaging to assess subcutaneous tissue echogenicity and architechture
- Measurement of subcutaneous layer thickness at both affected and unaffected sites
- Doppler evaluation to assess vascularity within the lesion
- Elastography (where available) to evaluate tissue stiffness
LH typically appears as an increased echo of the subcutaneous tissue, with or without different sizes of definite nodules in the boundary area [1]. Researchers should document the size, shape, echogenicity, and vascularity of all identified lesions. This method is particularly valuable for identifying non-palpable "flat" LH that escapes detection by physical examination [2] [3].
Protocol 2: Histopathological Analysis of Lipohypertrophy
For studies utilizing animal models or human biopsy specimens, comprehensive histological characterization should include:
- Standard H&E staining to assess overall tissue architecture and adipocyte morphology
- Masson's Trichrome or Picrosirius Red staining to quantify collagen deposition and fibrosis
- Immunohistochemistry for adipocyte differentiation markers (PPAR-γ, C/EBP-α) and proliferation markers (Ki-67)
- Scanning electron microscopy to examine adipocyte ultrastructure and extracellular matrix organization
Histology images of LH obtained through scanning electron microscopy have shown that up to 75% of the subcutaneous tissue is composed of macro-adipocytes with significantly larger size than adjacent normal adipocytes, associated with increased fibrosis and apoptosis [3].
Protocol 3: Metabolic Characterization in Preclinical Models
To evaluate the metabolic consequences of LH in animal models:
- Inject insulin exclusively into induced-LH sites and compare pharmacokinetic/pharmacodynamic profiles with normal tissue
- Perform frequent glucose measurements following injection to assess absorption variability
- Conduct hyperinsulinemic-euglycemic clamps to quantify insulin sensitivity
- Measure adipokine profiles (leptin, adiponectin) in serum and tissue
Studies in humans have demonstrated that injection into LH sites results in significant differences in postprandial blood glucose from 2 hours onwards, and in maximum postprandial blood glucose concentrations compared to normal tissue [1].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for Lipohypertrophy Investigation
| Reagent/Material | Application in LH Research | Technical Notes |
|---|---|---|
| High-frequency Ultrasound Systems (≥12 MHz) | Non-invasive detection and monitoring of subcutaneous tissue changes | Enables precise measurement of lesion size, echogenicity, and evolution over time [3] |
| Collagenase Type I/II | Isolation of stromal vascular fraction (SVF) from adipose tissue | Critical for digesting extracellular matrix to release adipocytes and progenitor cells for in vitro studies [5] |
| Adipocyte Differentiation Media | In vitro modeling of adipogenesis | Typically contains insulin, dexamethasone, IBMX, and indomethacin to induce preadipocyte differentiation |
| Anti-PPAR-γ & C/EBP-α Antibodies | Immunohistochemical analysis of adipocyte differentiation | Key transcription factors regulating adipogenesis; expression patterns altered in LH [6] |
| Masson's Trichrome Stain | Histological quantification of fibrosis | Differentiates collagen (blue/green) from muscle/cytoplasm (red) in tissue sections [3] |
| Human Insulin Preparations | In vitro stimulation of adipocyte cultures | Used to model repeated insulin exposure; regular insulin shows 3.2-fold higher LH risk vs. rapid-acting [1] |
| GLUT4 Translocation Assays | Assessment of insulin signaling integrity | LH tissue demonstrates impaired insulin responsiveness and glucose uptake |
| Cytokine Profiling Arrays | Analysis of inflammatory mediators in LH tissue | LH may involve low-grade inflammation; panels should include TNF-α, IL-6, adiponectin, leptin [5] |
Pathophysiological Pathways and Molecular Mechanisms
The development of lipohypertrophy involves complex interactions between insulin's biological actions and the subcutaneous tissue response. Several interconnected pathways contribute to its pathogenesis:
Insulin's Anabolic Actions: Insulin exerts direct lipogenic effects on adipocytes, promoting the synthesis of fats and proteins, which drives adipocyte hypertrophy and tissue expansion [1]. This localized trophic effect is amplified by repeated insulin exposure in the same tissue areas.
Fibrotic Remodeling: Histological analysis reveals that LH tissue contains a significantly larger number of macro-adipocytes and fibrosis compared to normal adipose tissue [3]. This fibrotic component develops through the activation of profibrotic genes such as connective tissue growth factor (CTGF) and TGF-β signaling components, leading to extracellular matrix accumulation [6].
Mechanical Trauma and Tissue Repair: Repeated needle insertion creates microtrauma that initiates wound healing responses, potentially leading to excessive extracellular matrix deposition and fibrotic remodeling [2]. This process is exacerbated by needle reuse, which dulls needles and increases tissue damage.
Potential Immunological Factors: Some evidence suggests immunological involvement, with studies showing a positive relationship between anti-insulin antibody levels and LH development [1]. The role of immune cell infiltration and localized inflammation warrants further investigation.
Prevention and Management Strategies in Research Context
Understanding LH pathology directly informs prevention strategies, which are particularly relevant for longitudinal studies involving repeated injections in animal models or clinical trials.
Injection Site Rotation Protocols: Systematic rotation of injection sites is fundamental to preventing LH. Research protocols should implement standardized rotation patterns that ensure ≥1 cm spacing between consecutive injections [2]. The recommended anatomical sites include abdominal wall, lateral/posterior arms, anterolateral thighs, and buttocks [2] [7].
Needle Replacement Guidelines: Studies consistently show that needle reuse correlates with increased LH prevalence [3]. Research protocols should specify single-use of disposable needles to minimize tissue trauma [2]. The use of shorter needles (4 mm) is also recommended to reduce deep tissue injury while ensuring consistent subcutaneous delivery [2].
Educational Interventions: Research from clinical settings demonstrates that structured education significantly improves injection technique and reduces LH incidence [8]. In one study of Chinese community nurses, 47.7% had poor insulin injection knowledge, highlighting the need for comprehensive training even among healthcare professionals [8]. Research protocols should include standardized training and periodic reassessment of injection technique.
Monitoring and Early Detection: Regular monitoring of injection sites using standardized palpation techniques or ultrasound can detect early LH formation [2] [3]. The pinching maneuver can aid in identifying less visible, elastic nodules, though ultrasound examination remains the most sensitive detection method, particularly for non-palpable LH [2].
The reversibility of LH with proper injection technique underscores the importance of these preventive measures. With consistent site rotation and avoidance of affected areas, existing LH lesions can gradually resolve over time, restoring normal insulin absorption and metabolic control [1].
Lipohypertrophy (LH), the thickening of fatty tissue at insulin injection sites, represents a prevalent and significant complication in diabetes management. For researchers and drug development professionals, understanding its epidemiology and the underlying pathophysiology is crucial for developing advanced insulin formulations and delivery systems. This complication, often overlooked in clinical practice, directly impacts drug absorption kinetics, glycemic control, and therapeutic outcomes, making it a critical area of scientific inquiry within the context of injection site rotation and scar tissue research.
Epidemiology and Prevalence Data
Extensive clinical studies have quantified the significant burden of lipohypertrophy among insulin-treated patients. The table below summarizes key epidemiological findings:
Table 1: Documented Prevalence of Lipohypertrophy in Diabetes Populations
| Study / Population Context | Reported Prevalence | Key Risk Factors Identified |
|---|---|---|
| General diabetes population [9] | Up to 64% | Failure to rotate injection/infusion sites; Low BMI; Reuse of needles; Use of human (vs. analog) insulin |
| Patients with type 1 or type 2 diabetes [10] | Up to 62% | Continuous injections at the same site; Injection into areas of scar tissue |
| Global Injection Technique Questionnaire (ITQ) Survey [11] | Nearly 50% | Reusing injection sites for a whole day or even days; Injecting into lipohypertrophic areas (reported by 26% of respondents) |
The high prevalence is largely attributed to persistent suboptimal injection techniques among patients. A major global survey, the Forum for Injection Technique (FITTER) Injection Technique Questionnaire (ITQ), highlighted that nearly 50% of patients exhibit symptoms suggestive of LH, with 21% reporting repeated injections at the exact same site over multiple days [11]. This underscores a critical gap between established clinical guidelines and real-world patient practices.
Pathophysiology and Experimental Models
Underlying Biological Mechanisms
Lipohypertrophy results from the localized trophic effects of insulin repeated injections into the same subcutaneous site [12]. The condition is characterized by:
- Cellular Hypertrophy: Lipohypertrophic fat cells can be approximately twice the size of normal adipocytes, contributing to the visible and palpable lump [9].
- Tissue Composition: The lumps consist of a buildup of fat, protein, and scar tissue [9].
- Absorption Dysregulation: The altered architecture and vascularization of the tissue lead to erratic and unpredictable absorption of insulin [9] [10]. Depending on the injection, insulin release from these sites can be delayed or accelerated, causing glycemic excursions.
This pathophysiology can be conceptually mapped to guide research focus:
Standardized Clinical Assessment Protocol
For consistent evaluation in clinical trials or studies, researchers should employ a standardized diagnostic protocol.
- 1. Patient History: Systematically document injection habits, including duration of insulin use, frequency of site rotation, and needle reuse practices [9] [10].
- 2. Visual Inspection: Examine common injection sites (abdomen, thighs, arms, buttocks) for raised, swollen, or thickened areas of skin. LH can vary in size from a golf ball to a fist [9] [13].
- 3. Palpation: Methodically palpate all potential injection areas. LH typically feels firm, rubbery, or lumpy and is often characterized by reduced sensation or numbness compared to surrounding healthy tissue [9] [10].
- 4. Severity Grading: For facial lipoatrophy (a related condition), a 5-degree scale exists, ranging from discrete flattening to excessive indentation with protruding bone structures [14]. While a universally accepted grading scale for LH is not explicitly detailed in the sources, the principle of classifying severity based on physical characteristics is a key research methodology.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Methods for Lipohypertrophy Research
| Tool / Material | Research Function & Application |
|---|---|
| High-Frequency Ultrasound | High-resolution imaging to non-invasively measure skin thickness, subcutaneous tissue depth, and quantitatively characterize the internal structure of LH lesions [11]. |
| Insulin Analogs | Comparative studies to investigate the mitogenic potency and lipohypertrophic potential of different insulin formulations (e.g., glargine, detemir, degludec) versus human insulin [12]. |
| Histopathological Staining | Analysis of biopsy specimens from LH sites to identify key tissue changes: lobular panniculitis, lymphocytic infiltration, hyaline necrosis of fat lobules, and fibrosis [14]. |
| Patient Injection Technique Questionnaire (ITQ) | Validated survey tool to quantitatively assess patient behaviors related to site rotation, needle reuse, and injection into LH areas, correlating practices with clinical outcomes [11]. |
Technical Support & Troubleshooting Guides
FAQ for Research and Clinical Trial Design
Q1: In our clinical trials, we observe significant variability in insulin absorption. Could undiagnosed lipohypertrophy be a confounding factor, and how can we control for it? Yes, LH is a major source of pharmacokinetic variability. Insulin absorption from LH sites is erratic, leading to unpredictable glycemic excursions that can obscure trial results [9] [15].
- Troubleshooting Protocol: Implement a mandatory injection site examination for all trial participants at every study visit. This should include both visual inspection and systematic palpation of all potential injection areas by a trained healthcare professional [10]. Participants found to have LH should be instructed to strictly avoid injecting into affected areas for a minimum of 2-3 months to allow for tissue healing [9].
Q2: Our in-vitro models show differences in IGF-1 receptor affinity between insulin analogs. What is the clinical significance of this for long-term tissue effects like lipohypertrophy? While in-vitro studies indicated that insulin glargine had a higher mitogenic potency and IGF-1 receptor affinity, it is rapidly degraded to metabolites (M1) in the subcutaneous tissue with lower binding affinity [12]. Large-scale human epidemiologic studies and observational studies with up to 7 years of follow-up have not found conclusive evidence of an associated increased risk of malignancy or specific tissue complications like LH compared to other insulins [12]. The long-term clinical significance of differences in IGF-1 binding remains an area of active investigation, highlighting the necessity of robust post-marketing surveillance.
Q3: What are the most critical, evidence-based recommendations we can provide to patients in our studies to prevent lipohypertrophy? The cornerstone of prevention is proper injection technique, which can be standardized in clinical protocols [11]:
- Systematic Site Rotation: Establish and document a formal rotation plan that moves injections/system sites around the body (abdomen, thigh, buttocks, arms) [9] [16].
- Avoid Needle Reuse: Mandate the use of a new needle for every injection. Reused needles cause microtrauma that contributes to tissue damage [9] [17].
- Spatial Separation within a Site: Ensure successive injections in the same general area (e.g., the abdomen) are spaced at least one finger-width (approximately 1-2 cm) apart to prevent over-stimulating a single spot [9].
Q4: How can we objectively measure the resolution of lipohypertrophy in intervention studies? The primary method is the cessation of injections into the affected area and longitudinal monitoring.
- Methodology: Document the size and texture of the LH area via palpation and photography at baseline. Re-examine the area at regular intervals (e.g., monthly). Natural resolution can take months to years [9]. High-frequency ultrasound can be used as an objective tool to track changes in subcutaneous tissue thickness and echogenicity over time [11].
Core Molecular Mechanisms of Insulin
Insulin Synthesis, Structure, and Key Metabolic Functions
Insulin is a peptide hormone essential for energy conservation and utilization, produced by pancreatic beta cells. Its synthesis begins with preproinsulin, which is cleaved in the endoplasmic reticulum to form proinsulin. Further processing removes the C-peptide, yielding the bioactive hormone composed of 51 amino acids arranged in two chains (A and B) linked by disulfide bonds [18] [19]. The primary anabolic effects of insulin are mediated through its binding to the Insulin Receptor (INSR), a receptor tyrosine kinase expressed on the surface of target cells [19]. This interaction triggers a downstream signaling cascade that regulates glucose, lipid, and protein metabolism.
The table below summarizes insulin's key anabolic effects on different metabolic pathways [18].
| Metabolic Pathway | Insulin's Effect | Key Molecular Mechanisms |
|---|---|---|
| Glucose Metabolism | Stimulates glucose uptake; suppresses hepatic glucose production | Activates phosphatidylinositol-3-kinase (PI3K) pathway; promotes translocation of GLUT-4 transporters to cell membrane in muscle and adipose tissue [18]. |
| Glycogen Metabolism | Promotes glycogenesis (glycogen synthesis) | Activates Protein Phosphatase 1 (PP1), which dephosphorylates and activates glycogen synthase and inactivates glycogen-degrading enzymes [18]. |
| Lipid Metabolism | Stimulates lipogenesis; inhibits lipolysis | Increases expression of lipogenic enzymes (e.g., fatty acid synthase); dephosphorylates and inhibits hormone-sensitive lipase [18]. |
| Protein Metabolism | Stimulates protein synthesis; inhibits degradation | Increases cellular uptake of amino acids; upregulates expression of proteins like albumin and muscle myosin; downregulates proteases involved in degradation [18]. |
The Anti-Inflammatory Role of Insulin
Beyond its metabolic roles, insulin possesses significant anti-inflammatory properties. Within endothelial cells and macrophages, insulin suppresses the activity of the pro-inflammatory transcription factor nuclear factor-kappa B (NF-κB). This suppression reduces the expression of adhesion molecules and the production of pro-inflammatory cytokines such as TNF-α, IL-6, and IL-8. Insulin also stimulates the release of nitric oxide (NO) from the endothelium, promoting vasodilation, and suppresses the generation of reactive oxygen species (ROS) in macrophages [18]. In the context of obesity, the development of insulin resistance (IR) creates a vicious cycle by disrupting these anti-inflammatory actions and promoting a state of chronic, low-grade inflammation [19].
Cellular Pathology of Injection Site Trauma
Repeated insulin injections or infusion set placements can cause localized tissue injury, initiating a wound healing response that, when chronically activated, leads to pathological skin complications. The two most common sequelae are lipohypertrophy and fibrosis [20].
Lipohypertrophy
This condition is characterized by a local accumulation of fatty tissue at the injection site. It results from the direct stimulatory effect of insulin on adipocytes, leading to both hypertrophy and hyperplasia of fat cells [20]. It is incredibly common, with an estimated prevalence of between 14.5% and 88% of insulin-dependent people with diabetes [20].
Fibrosis
Fibrosis involves the accumulation of stiff, dense scar tissue at the injection site. It is a chronic process driven by repeated minor tissue trauma and the ensuing inflammatory response. This leads to the activation of fibroblasts, which deposit a pathological amount of extracellular matrix (ECM) proteins [20].
The table below compares these two primary complications.
| Feature | Lipohypertrophy | Fibrosis (Scarring) |
|---|---|---|
| Pathological Process | Local expansion of adipose tissue [20]. | Excessive deposition of dense, collagen-rich scar tissue [20]. |
| Primary Cellular Driver | Adipocytes (fat cells) [20]. | Fibroblasts [20]. |
| Key Stimulus | Direct anabolic effect of insulin on lipid metabolism [20]. | Repeated tissue trauma and inflammatory response [20]. |
| Palpable Feel | Soft, rubbery, or swollen mass [20]. | Firm, hard, dense nodule [20]. |
Insulin-Derived Amyloidosis
A less common but significant complication is insulin-derived amyloidosis (AIns), where insulin aggregates into amyloid fibrils at the injection site, forming palpable, hard subcutaneous masses. The formation of these cytotoxic fibrils, primarily from the insulin B-chain, fundamentally disrupts insulin absorption, leading to subcutaneous insulin resistance and poor glycemic control [21]. A key finding is that the average daily insulin dose can be reduced by 30 units when patients avoid injecting into amyloid sites [21].
The Role of Mechanical Forces and Experimental Pathways
Mechanopathology of Tissue Trauma
The role of mechanical forces in the development of injection site complications is a critical area of research.
- Fibrosis and Mechanical Tension: Fibroblasts are highly sensitive to mechanical stress. Increased skin tension stimulates them to produce excess ECM, a hallmark of fibrosis. Clinical studies have shown that tension-offloading of surgical wounds significantly reduces scarring, suggesting a similar approach could benefit injection-related fibrosis [20].
- Lipohypertrophy and Compression: Adipocytes also sense mechanical forces. Intriguingly, in vitro studies indicate that compressive force can inhibit adipocyte production and differentiation by downregulating key adipogenic genes. This suggests that applying controlled compression might counteract the processes driving lipohypertrophy [20].
Experimental Therapeutic Strategies
A proposed theoretical approach involves using a tension-offloading dressing (e.g., the embrace device) at insulin injection sites. This device applies a compressive, tension-reducing force across the skin. Based on existing evidence, this strategy could simultaneously target the mechanical drivers of both fibrosis (by reducing tension) and lipohypertrophy (by applying compression) [20]. Clinical trials are needed to validate this approach for preventing insulin injection site complications [20].
Mechanistic Pathways of Injection Site Trauma and a Theoretical Intervention
The Scientist's Toolkit: Key Research Reagents & Methodologies
The following table details essential materials and methods for investigating insulin's molecular biology and injection site pathologies.
| Tool/Reagent | Primary Function in Research |
|---|---|
| Ultrasonography | Used to non-invasively measure skin and subcutaneous tissue thickness, identify and characterize lesions like lipohypertrophy and amyloidosis, and guide needle length selection [11] [21]. |
| Tension-Offloading Dressings | An experimental device (e.g., embrace) applied to injection sites to apply compressive, tension-reducing forces; used to test the hypothesis that modulating mechanics prevents fibrosis and lipohypertrophy [20]. |
| Behavioral Insulin Administration Skills (BIAS) Rubric | A validated observational scoring tool used in clinical studies to systematically assess a patient's insulin injection technique and identify common errors [22]. |
| Injection Technique Questionnaire (ITQ) | A large-scale global survey tool used to collect data on patients' injection practices, knowledge, and the prevalence of skin complications [11]. |
| Histological Staining & Analysis | Essential for definitive diagnosis of tissue complications. Allows for visualization of amyloid deposits, fibrotic scar tissue, and adipocyte morphology in biopsy samples [20] [21]. |
| Cell Culture Models (Fibroblasts & Adipocytes) | In vitro systems used to study the direct effects of insulin and mechanical forces (tension/compression) on ECM production, fibroblast activation, and adipocyte differentiation/gene expression [20]. |
Frequently Asked Questions (FAQs) for Troubleshooting Experimental & Clinical Challenges
Q1: In our in vitro models, we see inconsistent results when studying insulin's effect on adipogenesis. What is a key mechanical factor we might be overlooking? A: The application of compressive force has been shown in vitro to inhibit adipocyte production and differentiation by down-regulating key adipogenic genes [20]. Standard cell culture methods may not account for this mechanical variable. Ensure your experimental setup controls for or investigates the role of physical force on adipocyte behavior.
Q2: Our clinical trial data shows high variability in insulin absorption rates among participants. What is a common, often overlooked, confounding variable we should control for? A: Injection into lipohypertrophic or fibrotic sites is a major source of erratic absorption. One study found that total daily insulin doses for patients with lipohypertrophy were, on average, 36% higher (an absolute difference of 15 IU/day) than for those without it, due to impaired and variable absorption [20] [22]. Protocol should include systematic palpation and visual inspection of all potential injection sites by a trained clinician to exclude these areas from the study.
Q3: When developing new insulin formulations, how can we pre-clinically assess the risk of inducing localized amyloidosis? A: The formation of amyloid fibrils is linked to the dissociation of insulin hexamers into monomers, with the B-chain being the principal amyloidogenic factor [21]. Pre-clinical assays should focus on the formulation's stability and its propensity for monomer aggregation under stress conditions. Techniques like electron microscopy and thioflavin T staining can be used to detect fibril formation in experimental models.
Q4: What is the most critical technique failure in patients with poorly controlled glucose despite high insulin doses? A: A failure to properly rotate injection sites is a primary cause. Repeated injections in the same spot lead to lipohypertrophy and fibrosis, which severely impair insulin absorption. Educating patients on structured rotation, using methods like a 4x4 grid on the abdomen and moving to different body parts, is crucial [23]. Studies show that simply educating patients on proper rotation can lead to significant improvements in glycemic control and a reduction in daily insulin requirements [11].
The Direct Link Between Lipohypertrophy and Unpredictable Insulin Pharmacokinetics
Frequently Asked Questions (FAQs)
Q1: What is the pathophysiological basis for altered insulin absorption in lipohypertrophic tissue?
A1: Lipohypertrophy (LH) is characterized by adipose tissue hyperplasia and hypertrophy, combined with fibrotic tissue deposition [3] [20]. Histological analysis reveals that approximately 75% of the subcutaneous tissue in LH lesions consists of macro-adipocytes that are significantly larger than normal adipocytes, alongside increased fibrosis and apoptosis [3]. This pathological remodeling creates a diffusion barrier and alters local blood flow. The fibrotic component impedes insulin diffusion, while the enlarged, insulin-stimulated adipocytes create an erratic reservoir effect. This combination results in non-linear and unpredictable absorption kinetics, manifesting as both delayed and sometimes accelerated insulin release into the systemic circulation [20] [24].
Q2: What is the prevalence of lipohypertrophy in research cohorts, and what are its primary risk factors?
A2: The prevalence of LH is substantially high but varies significantly with detection methodology. Clinical studies using visual inspection and palpation report prevalence rates between 37% and 64% in insulin-treated populations [3] [9]. When more sensitive ultrasound techniques are employed, detection rates can be even higher, as ultrasound identifies structural changes in deeper tissue layers before surface manifestations occur [3]. The key risk factors identified in clinical research are summarized in Table 1 below.
Table 1: Key Risk Factors for Lipohypertrophy Development
| Risk Factor | Experimental/Observational Evidence |
|---|---|
| Lack of Injection Site Rotation | Consistently identified as the primary modifiable risk factor; leads to concentrated micro-trauma and localized insulin action [3] [9] [25]. |
| Needle Reuse | Damages the needle tip (visible under microscopy), increasing tissue trauma and the risk of scarring and LH [3] [17] [24]. |
| High Number of Daily Injections | A higher frequency of injections per day correlates with an increased prevalence of LH [3]. |
| Large Injection Volumes | Single injections exceeding recommended volumes contribute to localized tissue stress and expansion [3]. |
| Longer/Thicker Needles | The use of longer and thicker needles is associated with a greater risk of developing LH [3]. |
Q3: What quantitative impact does lipohypertrophy have on insulin dosing and glycemic outcomes?
A3: LH has a demonstrable and significant impact on both pharmacokinetic and pharmacodynamic outcomes. Research indicates that total daily insulin doses for patients with LH are, on average, 36% higher than for those without LH, representing an absolute mean increase of 15 IU/day [20]. This suggests impaired and wasted insulin absorption. Glycemically, this translates to increased glycemic variability, a 2.7 times higher risk of unexplained hypoglycemia, and an increased risk of hyperglycemia and diabetic ketoacidosis (DKA) [20]. Case studies document patients with fluctuating blood glucose and unpredictable hypoglycemia resolving after avoiding LH sites, with HbA1c improvements of over 2% [24].
Q4: What are the standard and advanced experimental methods for detecting and quantifying lipohypertrophy in a research setting?
A4: The diagnostic and research methods for LH range from simple clinical techniques to advanced imaging, as outlined in the experimental protocol below.
Table 2: Methodologies for Lipohypertrophy Detection and Characterization
| Method | Protocol Description | Utility and Limitations |
|---|---|---|
| Visual Inspection & Palpation | Protocol: Visually assess for raised, swollen areas. Perform a pinching maneuver and deep palpation to detect elastic or firm nodules, even if not visible. Change body positioning to improve detectability [3]. | Utility: Low-cost, clinically feasible. Limitation: Low sensitivity for small or deep lesions; diagnostic accuracy highly dependent on examiner training (trained professionals are 45% better at detecting sub-4cm lesions) [3]. |
| High-Frequency Ultrasound | Protocol: Use a high-frequency linear array transducer. Measure dermal and subcutaneous echo-texture, thickness, and look for structural disorganization, hypoechoic areas (fat), and hyperechoic strands (fibrosis) [3]. | Utility: Gold standard for research. ~30% more sensitive than palpation. Allows objective quantification of tissue changes, including depth and fibrosis [3] [20]. |
| Histological Analysis | Protocol: Tissue biopsy of affected sites, followed by staining (e.g., H&E, Masson's Trichrome for collagen) and analysis via light or scanning electron microscopy [3]. | Utility: Reveals pathophysiological mechanisms: macro-adipocytes, fibrosis, and apoptosis. Limitation: Invasive; not for routine use [3] [20]. |
Experimental Protocols for Investigating Lipohypertrophy
Protocol for a Randomized Site-Rotation Intervention Study
Objective: To quantify the effect of a structured injection site rotation protocol on the incidence of new LH and glycemic variability.
Methodology:
- Cohort Recruitment: Recruit insulin-dependent participants with no existing LH, confirmed via baseline ultrasound.
- Randomization & Intervention: Randomize into two groups:
- Intervention Group: Follows a structured, timed site rotation schedule (e.g., consistent morning injections in the thigh, evening injections in the abdomen) with each injection spaced at least one finger-width apart [26] [25] [17]. Use of body maps and tracking apps is mandated.
- Control Group: Receives standard care with general advice to rotate sites.
- Blinding: Outcome assessors (e.g., ultrasound technicians) should be blinded to group allocation.
- Outcome Measures:
- Primary: Incidence of new LH at 6 and 12 months, diagnosed by ultrasound.
- Secondary: Change in HbA1c, Glucose Time-in-Range (TIR), hypoglycemia events, and total daily insulin dose.
Protocol for Assessing Insulin Pharmacokinetics/Pharmacodynamics (PK/PD)
Objective: To directly compare the absorption profile and action of insulin injected into healthy versus lipohypertrophic tissue.
Methodology:
- Participant Selection: Recruit participants with clearly demarcated LH areas and adjacent healthy tissue.
- Study Design: Cross-over design where each participant serves as their own control.
- Experimental Procedure: After an overnight fast and standardized basal insulin, administer an identical dose of rapid-acting insulin into both the LH site and a healthy control site on separate study days.
- Data Collection: Measure plasma insulin concentrations and blood glucose levels frequently over the subsequent 6-8 hours. Use euglycemic clamps if possible to precisely quantify glucose infusion rates (GIR).
- PK/PD Analysis: Calculate for both sites:
- T~max~: Time to maximum insulin concentration.
- C~max~: Maximum insulin concentration.
- AUC: Total area under the insulin concentration-time curve.
- GIR~AUC~: Total glucose infused to maintain euglycemia.
Signaling Pathways and Experimental Workflows
The following diagram illustrates the mechanistic pathway from repeated insulin injections to unpredictable pharmacokinetics, integrating the roles of mechanical force and insulin's biological action.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Lipohypertrophy Research
| Research Tool / Reagent | Function in Experimental Context |
|---|---|
| High-Frequency Ultrasound System | The primary non-invasive tool for objective quantification of subcutaneous tissue architecture, thickness, and echogenicity to characterize and monitor LH lesions [3]. |
| Human Insulin (Various Formulations) | To study the differential effects of human vs. analog insulin on adipocyte stimulation and LH development in experimental models [9] [24]. |
| Rapid-Acting Insulin Analog | The standard for PK/PD studies due to its widespread use in pumps and injections; allows for precise measurement of absorption kinetics from different tissue sites [27]. |
| Tension-Offloading Dressings | An investigational device (e.g., embrace) based on the hypothesis that reducing mechanical tension can mitigate injection-induced fibrosis and potentially LH, providing a mechanistic intervention [20]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | For precise and frequent measurement of serum/plasma insulin concentrations in PK studies, especially when high doses are involved that require sample dilution [28]. |
| Continuous Glucose Monitoring (CGM) Systems | To collect high-resolution glycemic data (Time-in-Range, variability) as a pharmacodynamic readout of insulin absorption efficiency from LH vs. healthy tissue [3] [27]. |
| Sterile Single-Use Needles (4-6mm) | The research standard to control for the confounding variable of needle reuse, ensuring that tissue trauma is consistent and not exacerbated by a damaged needle tip [3] [17]. |
Troubleshooting Guides and FAQs
Frequently Asked Questions for Researchers
Q1: What is the established clinical link between improper injection site rotation and glycemic variability?
A1: Research demonstrates a direct correlation. A 2018 study found that a poorer insulin injection technique score was negatively correlated with the Mean Amplitude of Glycemic Excursion (MAGE), a key metric for GV. Patients who self-injected had significantly higher MAGE than when injections were performed by a specialist nurse, who ensured proper technique including site rotation [29]. Furthermore, improper rotation leads to lipohypertrophy (LH), which results in erratic and unpredictable insulin absorption, directly driving glycemic fluctuations [30] [31].
Q2: How can a researcher experimentally confirm that lipohypertrophy is causing unexplained hypoglycemia in a study subject?
A2: A focused diagnostic approach is required [32].
- Clinical Examination: First, thoroughly inspect and palpate all potential injection sites (abdomen, thighs, arms) for rubbery or raised lumps [30] [31].
- Intervention: Instruct the subject to strictly avoid injecting into any suspected LH areas for a minimum of six months [33].
- Monitoring: Implement continuous glucose monitoring (CGM) to track hypoglycemic events (Time Below Range, TBR) and glycemic variability (Coefficient of Variation, CV) [34] [35].
- Outcome: A significant reduction in unexplained hypoglycemic events and improved GV after switching to healthy injection sites confirms the diagnosis. Concurrently, you may observe a reduction in total daily insulin requirements, as insulin absorption from healthy tissue is more efficient [31].
Q3: What are the core mechanisms by which scar tissue (lipohypertrophy) increases insulin requirements?
A3: Lipohypertrophy alters the pharmacokinetics of insulin via two primary mechanisms [31]:
- Impaired Absorption: The altered architecture of scarred and fatty tissue disrupts normal vascularization, leading to delayed, erratic, or sometimes trapped insulin absorption.
- Reduced Bioavailability: A portion of the injected insulin may become sequestered within the LH tissue, failing to enter the systemic circulation. This necessitates a higher administered dose to achieve the required therapeutic plasma insulin level. When the injection site is subsequently rotated to healthy tissue, the accumulated insulin can be released, leading to dangerous, unexplained hypoglycemia [33].
Q4: Which quantitative metrics from Continuous Glucose Monitoring (CGM) are most critical for assessing the impact of injection technique in a clinical trial?
A4: Beyond HbA1c, CGM provides dynamic data essential for this assessment. Key metrics include [34] [35]:
- Time in Range (TIR): Percentage of time glucose is between 70-180 mg/dL. A low TIR indicates poor control.
- Time Below Range (TBR): Percentage of time glucose is <70 mg/dL (<54 mg/dL is clinically significant). High TBR indicates hypoglycemia risk.
- Coefficient of Variation (CV): A measure of glycemic variability (standard deviation/mean glucose). A CV ≤ 36% indicates stable glucose, while a higher CV predicts hypoglycemia risk.
- Mean Amplitude of Glycemic Excursion (MAGE): A specific measure of major glucose swings, which has been directly linked to poor injection technique scores [29].
Troubleshooting Guide: Common Experimental Scenarios
Problem: Unexplained Hypoglycemia in a Study Cohort
- Potential Cause: Undiagnosed lipohypertrophy leading to erratic insulin release; surreptitious insulin use; pancreatic pathology (e.g., insulinoma); adrenal or pituitary insufficiency [32] [31].
- Action Plan:
- Inspect and Palpate all injection sites for LH [30].
- Implement Site Rotation and monitor hypoglycemia frequency [33].
- Conduct a focused lab workup during a hypoglycemic event: measure plasma glucose, insulin, C-peptide, and β-hydroxybutyrate. Inappropriately "normal" or high insulin and C-peptide with low glucose suggest excessive endogenous insulin (e.g., from sulfonylurea use or insulinoma), while suppressed insulin points to other causes [32].
Problem: High Glycemic Variability Despite Optimal HbA1c
- Potential Cause: Improper injection technique, including failure to rotate sites and needle reuse, leading to LH [30] [29].
- Action Plan:
- Audit Injection Technique using a validated skill-assessment scale [29].
- Analyze CGM Data for CV and MAGE. A high CV (>36%) confirms unstable control [34] [35].
- Educate on Site Rotation and proper technique. A study showed that correcting technique alone improved MAGE and overall glycemic control [29].
Problem: Consistently High Insulin Requirements with Poor Response
- Potential Cause: Injecting into lipohypertrophic sites with poor absorption, necessitating dose escalation [31].
- Action Plan:
- Systematically rotate to unaffected sites.
- Monitor and Log insulin doses and corresponding glucose responses.
- Expect a Dose Reduction: After switching to healthy sites, insulin requirements often decrease significantly due to restored absorption efficiency. Carefully monitor for hypoglycemia during this transition period [31].
Table 1: Prevalence of Improper Injection Techniques and Lipohypertrophy (Cross-Sectional Study, n=851) [30]
| Parameter | Type 1 Diabetes (n=298) | Type 2 Diabetes (n=553) |
|---|---|---|
| Performed Site Rotation | 66.8% | 69.4% |
| Needle Reuse (>3 times) | 36.6% | 50.5% |
| Lipohypertrophy Prevalence | 57.0% | 55.5% |
| Mean HbA1c (Uncontrolled, >7%) | 8.8% ± 1.8 | 7.6% ± 6.9 |
Table 2: Impact of Injection Technique on Glycemic Control (Self-Controlled Trial, n=52) [29]
| Glycemic Metric | Patient Self-Injection Period | Specialist Nurse Injection Period | P-value |
|---|---|---|---|
| Mean Amplitude of Glycemic Excursion (MAGE) | Significantly Higher | Significantly Lower | < 0.05 |
| Mean Injection Technique Score (out of 30) | 17.0 ± 4.4 | Optimal (30) | Not Applicable |
| Correlation | IT score negatively correlated with MAGE & HbA1c | < 0.05 |
Table 3: Key CGM Metrics for Assessing Glycemic Control and Variability [34] [35]
| Metric | Definition | Target (Most Adults with Diabetes) |
|---|---|---|
| Time in Range (TIR) | % of time glucose is between 70–180 mg/dL | >70% |
| Time Below Range (TBR) | % of time glucose is below 70 mg/dL | <4% |
| Time Above Range (TAR) | % of time glucose is above 180 mg/dL | <25% |
| Coefficient of Variation (CV) | (Standard Deviation / Mean Glucose) x 100; measures variability | ≤36% |
Experimental Protocols
Protocol 1: Assessing Injection Technique and Its Correlation with Glycemic Variability
Objective: To quantitatively evaluate the quality of insulin injection technique in study subjects and determine its correlation with short-term glycemic variability using Continuous Glucose Monitoring (CGM).
Methodology (Based on a published self-controlled trial) [29]:
- Subject Recruitment: Enroll patients with diabetes (Type 1 or 2) who have been on a stable regimen of premixed or basal-bolus insulin for at least three months.
- Study Design: A single-center, cross-sectional, self-controlled design.
- Intervention Phases:
- Phase 1 (Patient Injection - 2 days): Subjects self-inject insulin as per their usual technique.
- Phase 2 (Nurse Injection - 2 days): A specialist nurse administers the same type and dose of insulin using optimal technique.
- Data Collection:
- CGM: A CGM system (e.g., Medtronic CGM) is worn for 96 hours throughout both phases. Data from the second day of each phase is analyzed.
- Injection Technique Assessment: On the last day of Phase 1, two independent nurses assess the subject's technique using a validated 15-item skill scale. Each item is scored from 0-2 (maximum score 30). Key items include:
- Key Outcome Measures:
- Primary: Mean Amplitude of Glycemic Excursion (MAGE) during the patient injection period vs. the nurse injection period.
- Secondary: Correlation between the total injection technique score and MAGE; Correlation between the technique score and HbA1c.
Protocol 2: Investigating the Impact of Lipohypertrophy on Insulin Pharmacokinetics
Objective: To compare the absorption profile and glycemic response of insulin injected into lipohypertrophic (LH) sites versus healthy, rotation-managed control sites.
Methodology:
- Subject Selection: Recruit subjects with confirmed, palpable lipohypertrophy.
- Study Design: Randomized, cross-over study.
- Intervention:
- On two separate study days, subjects receive a standardized dose of fast-acting insulin.
- Day A: Injection into a documented LH site.
- Day B: Injection into a healthy, non-LH site (contralateral side or different anatomical area).
- Data Collection:
- Frequent Plasma Sampling: Measure serum insulin and glucose levels at regular intervals (e.g., every 15-30 minutes) for 4-6 hours post-injection.
- CGM: Use CGM to capture real-time glucose fluctuations and calculate TIR, TBR, and CV for each study day [34].
- Absorption Kinetics: Calculate the area under the curve (AUC) for insulin concentration, time to peak concentration (Cmax), and absorption half-life.
- Key Outcome Measures:
- Differences in insulin AUC and Cmax between LH and healthy sites.
- Differences in glucose AUC and the frequency of hypoglycemic events (TBR) between the two conditions.
- Documented delay in time to peak insulin action from LH sites.
Signaling Pathways and Workflows
Diagram 1: Pathophysiological pathway of poor injection technique consequences.
Diagram 2: Diagnostic workflow for unexplained hypoglycemia.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Materials and Tools for Investigating Injection Site Complications
| Tool / Reagent | Function in Research | Example / Specification |
|---|---|---|
| Continuous Glucose Monitoring (CGM) System | Provides high-frequency glucose data to calculate GV metrics (MAGE, TIR, TBR, CV) and assess glycemic control in real-world settings [34] [35]. | Medtronic CGM, Dexcom G6 [29]. |
| Validated Injection Technique Assessment Scale | Standardized tool to quantitatively evaluate and score a subject's adherence to proper injection protocols, allowing for correlation with outcomes [29]. | 15-item skill scale (score 0-30) assessing resuspension, site rotation, needle reuse, etc [29]. |
| High-Frequency Plasma Sampling Assays | To measure insulin pharmacokinetics (absorption rate, Cmax, Tmax, AUC) following injection into LH vs. healthy sites. | ELISA or Chemiluminescence assays for serum insulin. |
| Standardized Lipohypertrophy Palpation Protocol | Ensures consistent and objective identification and documentation of LH lesions across all study subjects. | Defined by size, texture (rubbery vs. hard), and location [30] [31]. |
| Ultrasound Imaging | Provides objective, quantitative measurement of subcutaneous tissue structure and can precisely characterize the size and depth of LH lesions. | High-frequency linear array probe. |
Economic and Quality of Life Burden on Patients and Healthcare Systems
Lipohypertrophy (LH), the most prevalent local complication of insulin therapy, presents as subcutaneous nodular swelling due to adipose tissue proliferation at injection sites. With an average occurrence rate of 41.8% among insulin users, LH represents a significant clinical and economic challenge in diabetes management. Insulin injection into LH-affected sites significantly impairs insulin absorption, leading to marked glycemic excursions including both hyperglycemia and hypoglycemia. These clinical consequences contribute to increased healthcare expenditures and represent a substantial quality of life burden for patients. This technical support document establishes a framework for researchers investigating injection site rotation protocols and their impact on preventing LH, thereby reducing the associated economic and quality of life burdens on patients and healthcare systems.
Key Research Gaps and Clinical Challenges
Quantitative Data on LH Prevalence and Risk Factors
Table 1: Epidemiological Data on Lipohypertrophy in Insulin-Treated Diabetes
| Parameter | Statistical Value | Context & Implications |
|---|---|---|
| Global Diabetes Prevalence | 537 million adults (20-79 years) | Represents 10.5% of global population; establishes population at risk [2] |
| China Diabetes Prevalence | 12.4% (over 140 million affected) | Exceeds global rates; highlights significant at-risk population [2] |
| LH Prevalence Average | 41.8% of insulin users | Indicates high frequency of this complication among insulin-dependent patients [2] |
| Common Insulin Regimen | 4 times per day (in studied cohort) | High injection frequency increases LH risk without proper site rotation [2] |
| Mean Insulin Therapy Duration | 7.2 ± 3.2 years (in studied cohort) | Longer therapy duration correlates with increased LH development risk [2] |
Identified Barriers to Effective Injection Site Rotation
Table 2: Barriers to LH Prevention in Diabetes Self-Management
| Theme Category | Specific Barriers | Representative Participant Quotations |
|---|---|---|
| Knowledge Deficits | Insufficient health education, Forgetfulness, Misconceptions | "When I was hospitalized before, they (HCPs) did not tell me about LH..." (P7) [2] |
| Implementation Challenges | Limitations in site rotation, Financial pressures in needle replacement, Failure to self-monitor flat LH | "The HCPs asked me to rotate the injection site, but they did not say how to do it clearly." (P10) [2] |
| Motivational Barriers | Low perceived severity, Low perceived susceptibility | No specific quotation provided in search results, but identified as key thematic barrier [2] |
Experimental Protocols and Methodologies
Qualitative Research Protocol for Barrier Identification
Research Design: Qualitative descriptive design using semi-structured interviews [2] Participant Selection:
- Inclusion Criteria: Diagnosis of diabetes mellitus receiving insulin therapy; LH confirmed by ultrasound examination; self-administered insulin at home prior to admission; volunteered for study participation [2]
- Exclusion Criteria: Medical record of severe psychiatric or cognitive disorders; inability to participate in interviews for any reason [2] Sample Characteristics: 17 participants (10 male, 7 female) with type 2 diabetes; mean age 56.1±8.3 years [2] Data Collection: Face-to-face interviews in quiet, separate room; 20-60 minute duration; audio recorded and transcribed verbatim within 24 hours; participants reviewed summaries for factual verification [2] Data Analysis: Thematic analysis following Braun and Clarke methodology; six-phase analytical process using NVivo 8 software; continued until data saturation achieved [2]
Ultrasound Detection Protocol for LH Assessment
Clinical Procedure: Ultrasound examination emerges as superior diagnostic modality compared to conventional palpation, offering enhanced sensitivity and specificity particularly for non-palpable LH [2] Technical Advantages: Facilitates precise identification of optimal injection sites in patients with LH concerns; enables detection of flat LH lesions that are challenging to identify through physical assessment alone [2] Implementation Gap: Lack of routine LH examinations for outpatient and hospitalized individuals with diabetes in hospitals in China highlights translational challenge between research and clinical practice [2]
Diagram 1: Qualitative Research Methodology Workflow for LH Barrier Identification
Technical Support: Troubleshooting Guides & FAQs
Frequently Asked Questions for Research Implementation
Q: What are the most significant methodological challenges in LH prevention research? A: The primary challenges include: (1) accurate detection of non-palpable "flat LH" without routine ultrasound screening; (2) participant adherence to complex site rotation protocols in real-world settings; (3) differentiation between knowledge deficits and implementation barriers; and (4) accounting for financial constraints that lead to needle reuse exceeding recommended limits [2].
Q: How can researchers effectively measure adherence to injection site rotation protocols? A: Recommended approaches include: (1) combining self-report interviews with visual inspection and ultrasound confirmation; (2) utilizing injection site mapping tools to track rotation patterns; (3) assessing needle reuse through prescription refill patterns and direct participant reporting; and (4) incorporating both qualitative and quantitative measures to capture the multifactorial nature of adherence barriers [2].
Q: What physiological mechanisms explain impaired insulin absorption at LH sites? A: While the complete mechanism requires further research, current evidence suggests that injection into LH-affected areas significantly alters insulin pharmacokinetics, resulting in impaired absorption and marked glycemic excursions. The anabolic effects of insulin on regional adipose tissue, combined with repeated injection-induced subcutaneous tissue trauma and subsequent repair processes, contribute to this phenomenon [2].
Q: How do financial barriers impact needle replacement practices? A: Economic constraints create significant pressure for patients to reuse needles beyond recommended limits. This cost-saving measure directly contradicts optimal injection technique guidelines which recommend single-use disposable needles, creating a tension between clinical recommendations and financial realities for many patients [2].
Troubleshooting Guide for LH Research Protocols
Problem: Low participant recognition of flat LH lesions during self-assessment. Solution: Implement standardized ultrasound screening protocols at study baseline to establish objective LH presence regardless of palpability. Develop visual aids and tactile training tools to enhance participant detection capabilities [2].
Problem: Inconsistent application of site rotation protocols among study participants. Solution: Utilize simplified rotation guides with clear visual mapping of appropriate sites (abdominal wall, lateral/posterior arms, anterolateral thighs, and buttocks). Emphasize the critical ≥1 cm spacing requirement between injections through practical demonstration and reinforcement [2].
Problem: High rates of needle reuse contradicting research protocols. Solution: Acknowledge financial pressures and incorporate needle provision into study design where feasible. Address cost-benefit perceptions through education about long-term consequences of LH development, including increased insulin requirements and healthcare utilization [2].
Problem: Underestimation of LH severity and susceptibility among participants. Solution: Develop targeted educational materials demonstrating the clinical and economic impact of LH, including its effects on glycemic control, insulin pharmacokinetics, and long-term diabetes outcomes [2].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Methodologies for LH Research
| Research Tool | Specifications & Applications | Research Utility |
|---|---|---|
| Ultrasound Imaging System | High-frequency linear array transducer (7-15 MHz) | Gold-standard detection of LH lesions, particularly non-palpable "flat LH"; enables precise characterization of subcutaneous tissue changes [2] |
| Semi-structured Interview Guide | Open-ended questions exploring knowledge, practices, and barriers | Qualitative data collection on patient experiences, perceptions, and implementation challenges regarding injection site rotation [2] |
| Site Rotation Mapping Tool | Anatomical diagrams with injection site documentation | Visual documentation of rotation practices; enables correlation of specific sites with LH development patterns [2] |
| Needle Use Assessment Protocol | Combination of self-report and prescription refill data | Objective measurement of needle replacement practices and identification of economic barriers to adherence [2] |
| Qualitative Data Analysis Software | NVivo, MAXQDA, or similar platforms | Systematic organization and thematic analysis of interview transcripts; facilitates identification of emergent themes and patterns [2] |
Diagram 2: Clinical Consequences Pathway of Lipohypertrophy Development
The economic and quality of life burden associated with lipohypertrophy represents a significant yet preventable challenge in diabetes management. The identified barriers—knowledge deficits, implementation challenges, and motivational factors—provide critical targets for intervention development. Future research should focus on translating these findings into practical, patient-centered solutions that address both the clinical and economic dimensions of LH prevention. By developing more effective injection site rotation protocols and addressing the systemic barriers to their implementation, researchers can contribute substantially to reducing the economic and quality of life burden on both patients and healthcare systems.
Evidence-Based Protocols for Optimal Injection Technique and Site Rotation
FAQs: Core Principles of the FITTER Forward Guidelines
Q1: What are the FITTER Forward recommendations and why were they developed?
Q2: How do proper injection techniques specifically prevent lipodystrophy in research models?
Lipodystrophy, particularly lipohypertrophy (LH), is a common complication of subcutaneous insulin injections, presenting as thickened, "rubbery" tissue swellings [37]. The pathophysiology involves both the growth-promoting properties of insulin and localized trauma from poor injection habits. Injecting into these lesions causes erratic insulin absorption, leading to wide glycemic oscillations including unexplained hypoglycemia and hyperglycemia, which are scarcely responsive to insulin dose adjustments [37]. Proper site rotation prevents this localized trauma. The FITTER Forward guidelines emphasize that correct technique is a more crucial factor in maintaining target blood glucose levels than many realize, directly impacting the predictability of insulin absorption and the prevention of LH [38].
Q3: What are the critical methodological steps for assessing injection sites in clinical research?
A key diagnostic methodology involves systematic palpation of all potential injection sites [37]. Researchers should visually inspect and palpate for areas that feel lumpy, firm, rubbery, or raised compared to surrounding tissue [9]. These areas often have reduced sensation. In research settings, accurate identification is crucial as LH can be easily missed in a standard examination. The use of ultrasound and radiological methods can provide objective confirmation, but structured palpation techniques have been validated for clinical and research identification of LH [37]. Unexplained variations in glucose levels and/or unexplained hypoglycemic episodes in study participants should prompt a thorough examination for LH [37].
Q4: What are the quantitative clinical impacts of improper injection technique?
Improper technique, particularly injection into lipohypertrophic tissue, has significant, measurable clinical consequences. The table below summarizes key quantitative findings from the literature.
Table 1: Quantitative Impacts of Improper Injection Technique and Lipohypertrophy (LH)
| Parameter | Impact | Source/Study Context |
|---|---|---|
| LH Prevalence | Affects up to 64% of people with diabetes; 46.2% in a study of 780 insulin-treated adults [37]. | Clinical observational studies [9] [37]. |
| Glycemic Control | Erratic absorption causes wide glucose oscillations, increased hypoglycemia, and hyperglycemia [9] [37]. | Clinical observation in patients with LH [9] [37]. |
| Hemoglobin A1c (HbA1c) | Can be reduced by 1.0% within 6 months by correcting technique errors like needle reuse and using proper needle length [39]. | Interventional study on injection technique [39]. |
| Insulin Dose | Increased requirements are common when injecting into LH sites; doses often normalize after switching to healthy sites [9] [37]. | Clinical observation [9] [37]. |
| Needle Reuse | 39% of participants in a Canadian survey reused pen needles, a major risk factor for LH [39]. | Survey of 230 Canadian participants [39]. |
| Injection into LH | 37% of survey participants injected insulin into lipohypertrophic tissue [39]. | Survey of 230 Canadian participants [39]. |
Troubleshooting Guides for Research and Clinical Practice
Guide 1: Managing and Reversing Lipohypertrophy in Study Cohorts
Problem: Persistent lipohypertrophy (LH) nodules in clinical trial participants, leading to unpredictable insulin pharmacokinetics and compromised study data.
Solution Protocol:
- Immediate Cessation: Instruct participants to completely avoid injecting into any identified LH areas. This is the single most critical step [9].
- Healing Period: Document a cessation period of a minimum of 2 to 3 months, and sometimes years, for the tissue to heal and return to normal [9] [23].
- Site Mapping: Implement a structured site rotation plan for the participant using a body map or chart to track used and unused sites, ensuring healed areas are not re-used prematurely [9] [17].
- Verification: Confirm tissue healing via palpation (and ultrasound if available) before the area is cleared for use again in the study [9] [37].
- Surgical Consideration (Severe Cases): For severe, persistent deposits that do not resolve with conservative management, a protocol deviation may be considered for surgical removal via liposuction [9].
Guide 2: Implementing a Structured Rotation Protocol
Problem: Inconsistent and inadequate site rotation, a primary cause of lipodystrophy.
Solution Protocol: Adopt the FITTER Forward-recommended structured rotation plan [40] [38], which can be visualized as the following workflow for research participants.
Key Procedural Steps:
- Site Selection: Valid regions include the abdomen (avoiding a 5 cm perimeter around the navel), thighs, buttocks, and upper arms [17] [23].
- Systematic Rotation: Within a region (e.g., abdomen), use a systematic pattern, moving injection sites at least 1-2 cm (one finger width) apart from the previous injection [9] [39]. For pump infusion sets, the minimum distance is 1 inch for 90-degree sets and 2 inches for angled sets [23].
- Needle Usage: Mandate the use of a new needle for every injection to prevent tissue trauma and ensure sterility [9] [39] [17].
- Documentation: Provide participants with a logbook, calendar, or smartphone app to meticulously track injection sites [9] [23].
Guide 3: Addressing Participant-Specific Barriers to Adherence
Problem: Low adherence to rotation protocols due to participant-reported barriers.
Solution Protocol: A survey of youth with Type 1 diabetes identified key barriers and offers targeted solutions [41].
Table 2: Common Barriers to Site Rotation and Proposed Mitigation Strategies
| Barrier | Proposed Mitigation Strategy for Researchers |
|---|---|
| Fear of Pain in New Sites [41] | Counsel on using room-temperature insulin and shorter needles (4-6 mm). Teach relaxation and distraction techniques. [41] [17] |
| Difficulty Reaching Sites (e.g., arms, buttocks) | Recommend the use of an insertion device for hard-to-reach sites. For self-injection, identify the most accessible body regions for the participant. [23] |
| Habit and Forgetfulness | Implement structured reminder systems: pump alarms, phone alerts, or calendar notations. Correlate site changes with a regular weekly activity. [23] |
| Belief that LH is Not Problematic | Educate on the direct link between LH, erratic insulin absorption, and unexplained hypoglycemia/hyperglycemia, using data from Table 1. [9] [37] |
The Scientist's Toolkit: Research Reagents and Materials
This table details essential materials for studies investigating injection techniques and lipodystrophy.
Table 3: Key Research Reagent Solutions for Injection Technique Studies
| Item | Function/Justification in Research |
|---|---|
| Short Pen Needles (4-6 mm) | Recommended for most adults to ensure subcutaneous delivery and minimize intramuscular injection, a key variable in pharmacokinetic studies. [39] [17] |
| Non-Posted (Contoured) Pen Needles | Research tool to control for and study the impact of unintended injection force, which can lead to intramuscular injection and variable results. [39] |
| High-Frequency Ultrasound System | Gold-standard for objective, quantitative measurement of subcutaneous fat thickness and the precise characterization of lipohypertrophic lesions. [37] |
| Structured Palpation Protocol | A validated, low-cost methodological tool for the systematic identification and documentation of lipohypertrophic skin lesions during clinical assessments. [37] |
| Patient Body Maps & Logbooks | Essential for tracking injection site history, correlating specific sites with local tissue reactions, and monitoring adherence to rotation protocols. [9] [23] |
Visualizing the Pathophysiology and Clinical Impact
The following diagram synthesizes the relationship between improper injection practices, the development of lipohypertrophy, and the subsequent clinical and research outcomes, as detailed in the literature [9] [39] [37].
FAQs and Troubleshooting Guides
What is injection site lipodystrophy and why should researchers be concerned about it?
Lipodystrophy (LD) is a disorder of adipose tissue and a common complication of subcutaneous insulin injections in research models. It presents in two primary forms [37]:
- Lipoatrophy (LA): Defined as large, often deep, retracted scars on the skin resulting from serious damage to subcutaneous fatty tissue. Its prevalence has dropped to only 1–2% with the use of purified insulin, and an immunological etiology is suggested [37].
- Lipohypertrophy (LH): Characterized by thickened, "rubbery" tissue swellings which may be firm or occasionally soft. The exact etiology is unclear but is associated with the insulin molecule's growth-promoting properties and repeated trauma from poor injection habits like infrequent site rotation and needle reuse [37].
Clinical/Experimental Consequences: Injecting into LD-affected sites causes wide glycemic oscillations, including inexplicably high glucose levels and unexplained hypoglycemic episodes. These fluctuations are poorly responsive to insulin dose adjustments and can compromise data integrity in studies involving insulin administration [37].
How can researchers systematically define anatomical rotation zones to prevent lipodystrophy?
A systematic approach involves dividing the body into standardized anatomical zones based on established terminology [42] [43] [44].
- Anterior and Posterior Trunk: Utilize the ventral (anterior) and dorsal (posterior) surfaces. The abdomen is a common injection site on the anterior trunk [43].
- Lateral Aspects of Trunk and Limbs: The lateral body surfaces, away from the midline, provide additional injection areas [43].
- Proximal and Distal Limb Segments: The limbs can be divided into proximal segments (closer to the torso, like the upper arm and thigh) and distal segments (further away, like the forearm) [43].
- Consistent Landmarks: Use fixed bony landmarks, such as the iliac crest or patella, to ensure consistent and reproducible zone delineation across multiple researchers and sessions [43].
What are the best practices for implementing a rotation scheme in a longitudinal study?
Implementing a successful rotation scheme requires planning and documentation.
- Structured Patterns: Employ fixed, predictable rotation patterns (e.g., Zone A → Zone B → Zone C) to ensure all sites are used equally and allow adequate time for tissue recovery between injections in the same zone [45].
- Detailed Documentation: Meticulously log the specific zone used for each injection for every subject. Visual aids and maps in animal records can enhance accuracy [37].
- Regular Palpation: Before each injection, palpate (feel) the intended site for any rubbery or thickened tissue (indicating LH) or retracted areas (indicating LA). Avoid injecting into these areas [37].
Troubleshooting: If subjects exhibit unexplained glycemic variability, check for undiagnosed LH at common injection sites. Implementing an educational program on proper rotation techniques has been shown to significantly reduce glucose oscillations [37].
What quantitative data supports the need for systematic site rotation?
The table below summarizes key findings from clinical studies on lipodystrophy prevalence and its impact [37].
| Parameter | Quantitative Finding | Study Context |
|---|---|---|
| LH Prevalence | 46.2% of patients | n=780 insulin-treated adults (Type 1 & 2) |
| Mean LH Lesion Diameter | 4.8 ± 3.1 cm | n=780 insulin-treated adults (Type 1 & 2) |
| LA Prevalence | 3.2% of patients | n=780 insulin-treated adults (Type 1 & 2) |
| Bruising Prevalence | 33.2% of patients | n=780 insulin-treated adults (Type 1 & 2) |
| Effect of Education | Significant reduction in glucose oscillations | Observed after patient education on injection technique |
Experimental Protocols for Monitoring Lipodystrophy
Protocol 1: Palpation and Visual Inspection for Lipohypertrophy and Lipoatrophy
Objective: To consistently identify and document LD in research subjects. Materials: Examination gloves, subject skin maps, calipers (for measuring lesion size), camera (for documentation). Methodology [37]:
- With the subject in a relaxed, standing or sitting position, expose the common injection sites (abdomen, thighs, upper arms).
- Visually inspect all sites for visible swellings, dimples, or skin retractions.
- Using the palmar surfaces of the fingers, systematically palpate all injection zones.
- Feel for abnormal tissue consistency—LH typically presents as a thickened, "rubbery" swelling, while LA feels like an indentation or loss of underlying tissue.
- If a lesion is found, measure its dimensions with calipers and document its location and characteristics on the subject's skin map. Photograph the lesion if possible for longitudinal tracking. Frequency: This inspection should be performed weekly during studies involving frequent subcutaneous injections.
Protocol 2: Ultrasound Assessment of Subcutaneous Tissue Thickness
Objective: To obtain quantitative, high-fidelity data on subcutaneous tissue changes. Materials: High-frequency linear array ultrasound system, ultrasound gel, measurement calipers (digital). Methodology [37]:
- Mark standard anatomical zones on the subject's skin with a surgical pen for consistent probe placement over time.
- Apply ultrasound gel to the transducer head to ensure acoustic coupling.
- Place the transducer perpendicular to the skin surface on the marked zone. Acquire a clear image showing the skin layer, subcutaneous tissue (hypodermis), and underlying muscle fascia.
- Use the machine's electronic calipers to measure the distance from the dermis-subcutaneous junction to the subcutaneous-muscle fascia junction.
- Record measurements from at least three different injection zones per subject during each session to establish a baseline and monitor for regional changes. Frequency: Baseline pre-study, then bi-weekly or monthly depending on study duration and injection frequency.
Research Reagent Solutions and Essential Materials
The table below details key materials used in the study and monitoring of injection site reactions [37].
| Item | Function/Application |
|---|---|
| Purified Insulin Preparations | To minimize immunogenic reactions that can contribute to Lipoatrophy. |
| Short, Thin-Gauge Pen Needles | To reduce trauma, pain, and bruising at the injection site. |
| High-Frequency Ultrasound System | For objective, quantitative measurement of subcutaneous tissue thickness and morphology. |
| 4% Cromolyn Sodium Topical Prep | An inhibitor of mast cells; used in research contexts to investigate and manage immune-mediated LA. |
Logical Workflow for Site Rotation and Complication Management
The following diagram outlines the logical decision process for implementing a systematic site rotation scheme and managing identified complications.
Site Rotation and Complication Management Workflow
For researchers investigating insulin delivery optimization, the choice of needle technology is a critical variable influencing both clinical outcomes and experimental data. Suboptimal injection techniques and needle reuse are significant confounding factors in studies related to subcutaneous drug delivery, often leading to complications such as lipodystrophy which can compromise research integrity. This technical support center provides a detailed framework for understanding the role of 4mm pen needles and single-use policies within the broader context of preventing adipose tissue pathology. The following guides and protocols are designed to support scientists and drug development professionals in standardizing methodologies and troubleshooting common experimental challenges.
Frequently Asked Questions (FAQs)
Q1: What is the clinical and research significance of standardizing 4mm pen needles for subcutaneous injections?
A1: Standardizing 4mm pen needles is significant for both clinical practice and experimental design for several reasons:
- Reduced Pain and Improved Adherence: Shorter, thinner needles decrease pain during injection, a key variable in patient-reported outcomes and adherence in long-term studies [11] [46].
- Consistent Subcutaneous Delivery: Ultrasonography studies confirm that the 4mm length is sufficient to penetrate the skin and deliver insulin into the subcutaneous tissue in most adult patients, regardless of Body Mass Index (BMI), without requiring a skin fold [11]. This minimizes the risk of erratic absorption due to intramuscular injection.
- Minimized Confounding Variables: The use of a standardized, short needle reduces variability in injection depth caused by different application forces. Technologies like contoured hub designs further ensure precise 4mm target penetration with less variability, enhancing data reproducibility [11].
Q2: How does the failure to rotate injection sites directly contribute to the development of lipohypertrophy (LH), and what are the implications for drug absorption?
A2: Lipohypertrophy is a thickened, "rubbery" tissue swelling resulting from local trauma and the growth-promoting properties of insulin [37].
- Pathophysiology: Repeated injections into the same site cause localized trauma. Combined with insulin's lipogenic effects, this stimulates hypertrophic growth of adipose cells [37].
- Impact on Drug Pharmacokinetics: Injecting into LH-affected areas leads to erratic and delayed insulin absorption [37]. This results in wide glycemic oscillations, including unexplained hypoglycemic episodes and rebound hyperglycemia [37]. For researchers, this means that the pharmacokinetic (PK) and pharmacodynamic (PD) data collected from subjects with LH are highly unreliable.
- Prevalence: Studies indicate that nearly 50% of insulin-treated patients have LH, with a mean lesion diameter of 4.8 cm [37]. This high prevalence underscores the risk of not controlling for this variable in clinical trials.
Q3: What is the evidence-based protocol for a proper injection technique that prevents complications?
A3: A proper technique is defined as one that successfully delivers the drug into the subcutaneous space with minimal pain and no leakage [11]. The "SAFETY" acronym summarizes key steps [47]:
- Secure the safety pen needle to the pen and prime it.
- Alternate injection sites to prevent lipohypertrophy.
- Firmly inject at a 90° angle.
- Ensure to hold for a full 10 seconds after full depression.
- Thoroughly remove the needle and discard it immediately.
- Your excellent technique benefits both therapeutic outcomes and clinician safety.
Q4: Why is a single-use policy for pen needles non-negotiable in a research setting?
A4: Enforcing a single-use policy is critical for methodological rigor.
- Prevention of Needlestick Injuries: Single-use policies, supported by safety-engineered devices, directly reduce needlestick injuries among research staff [47].
- Ensuring Dosing Accuracy: Reusing needles causes blunting and deformation, which can increase injection force and potentially lead to under-dosing or incomplete delivery, introducing significant error in dose-response studies [11] [48].
- Reducing Infection Risk and Lipohypertrophy: Needle reuse is a major contributing factor to the development of LH [37]. Using a sharp, sterile needle for every injection minimizes local tissue trauma and ensures consistent drug delivery.
Troubleshooting Guides
Problem: Unexplained Glycemic Variability in Study Subjects
- Potential Cause 1: Undetected Lipohypertrophy (LH) at injection sites.
- Solution: Implement a palpation protocol to systematically identify LH at all injection sites. Visually inspect and palpate sites for thickened, rubbery tissue. Educate subjects to avoid these areas entirely [37].
- Potential Cause 2: Inconsistent injection technique or needle reuse.
Problem: Subject Reports of Injection Pain or Bruising
- Potential Cause: Suboptimal needle gauge or length, or angled insertion/removal.
Experimental Protocols & Data
Protocol 1: Palpation and Documentation of Lipodystrophy
Objective: To systematically identify, classify, and document lipodystrophic lesions in clinical trial subjects. Methodology:
- Inspection and Palpation: Visually inspect and gently palpate all potential injection sites (abdomen, thighs, buttocks, upper arms). LH presents as a firm, rubbery swelling; Lipoatrophy (LA) presents as a retracted, atrophic area [37].
- Documentation: For each lesion, record:
- Location (e.g., periumbilical, right thigh).
- Type (LH or LA).
- Size (length x width in cm).
- Texture (graded on a scale from normal to severely thickened).
- Ultrasonography Confirmation: Use high-frequency ultrasonography on identified lesions to measure the exact depth and structural changes in the subcutaneous tissue layer for quantitative analysis [37].
Protocol 2: Assessing Injection Technique Compliance
Objective: To monitor and validate adherence to proper injection technique and single-use policies. Methodology:
- Direct Observation: Periodically observe subjects performing injections to assess compliance with the "SAFETY" protocol, focusing on site rotation, angle, and hold-time.
- Sharps Container Audit: Perform periodic checks of returned sharps containers to count used needles against the reported number of injections, providing objective data on needle reuse rates.
- Subject Diary Analysis: Review patient injection diaries for patterns of site rotation and any self-reported issues.
Table 1: Quantitative Data on Lipohypertrophy Prevalence and Impact
| Parameter | Finding | Research Implication |
|---|---|---|
| LH Prevalence | 46.2% of insulin-treated patients (n=780) [37] | A highly prevalent confounder that must be screened for in subject populations. |
| Mean LH Lesion Diameter | 4.8 ± 3.1 cm [37] | Lesions are large enough to significantly impact available injection site real estate. |
| Bruising Prevalence | 33.2% of patients (with or without LH) [37] | Indicates local trauma; a potential marker for suboptimal technique. |
| Impact of Injection into LH | Erratic absorption, unexplained hypoglycemia, rebound hyperglycemia [37] | Directly compromises PK/PD data and endpoint validity in clinical trials. |
Table 2: Technical Specifications of Modern Pen Needles
| Needle Length | Gauge (G) | Key Features & Research Applications |
|---|---|---|
| 4 mm | 31G, 32G | Recommended standard for most adults without pinching [11]. Minimizes pain, reduces intramuscular risk, ideal for PK studies requiring consistent SC delivery. |
| 5 mm | 31G, 32G | Often features safety mechanisms (e.g., DropSafe, AutoShield Duo) for protecting research staff [47] [46]. |
| 6 mm | 31G, 32G | A previously common size; may require a skin fold in non-obese subjects to ensure subcutaneous delivery [49]. |
| 8 mm | 31G | Longer needle; should be used with a skin fold to avoid intramuscular injection, adding a technique variable [11] [49]. |
Research Reagent Solutions
Table 3: Essential Materials for Injection Technique Research
| Item | Function in Research |
|---|---|
| 4mm Pen Needles (e.g., BD Nano, NovoFine, Nipro 4SURE) | The primary intervention device. Enables standardized, low-pain, subcutaneous delivery with minimal variability [11] [46] [50]. |
| Safety-Engineered Pen Needles (e.g., DropSafe, AutoShield) | Mitigates needlestick injury risk for research staff, a key consideration for workplace safety and protocol approval [47] [46]. |
| High-Frequency Ultrasound System | Provides objective, quantitative measurement of skin thickness and subcutaneous tissue structure to identify and monitor LH [37]. |
| Standardized Palpation Protocol | A low-cost, systematic method for screening and documenting lipodystrophic lesions across a study cohort [37]. |
| Sharps Containers | Essential for the safe disposal of single-use needles, allowing for audits of compliance. |
Visual Workflow: From Improper Technique to Experimental Confounding
The following diagram illustrates the logical sequence and causal relationships between improper injection practices, the development of tissue complications, and the resulting impact on research data.
Technical FAQs: Core Mechanisms and Clinical Significance
Q1: What are the primary pathophysiological mechanisms behind insulin-induced lipohypertrophy (LH)?
The development of LH involves two key interconnected processes:
- Adipocyte Hypertrophy and Hyperplasia: Insulin is a growth hormone with potent anabolic effects on lipid metabolism. Localized, repeated insulin stimulation at injection sites leads to both the excessive growth (hypertrophy) and proliferation (hyperplasia) of adipocytes [20]. Histological analysis reveals that LH tissue is composed of up to 75% macro-adipocytes, which are significantly larger than normal fat cells [3].
- Fibrosis and Tissue Remodeling: Repeated needle insertion causes minor tissue trauma, initiating a chronic inflammatory response and the deposition of fibrotic, scar tissue [20]. This fibrosis is mechanosensitive; increased mechanical tension at the injection site stimulates fibroblasts to produce more pathological extracellular matrix [20]. Consequently, LH areas often present as a complex mix of expanded adipose tissue and fibrotic strands [3] [20].
Q2: Why does injecting into lipohypertrophic lesions lead to unpredictable glycemic control?
Lipohypertrophic tissue exhibits fundamentally altered pharmacokinetic properties. The vascular network and normal architecture of the subcutaneous space are disrupted by the enlarged adipocytes and fibrotic tissue [3]. This leads to:
- Reduced and Erratic Absorption: Insulin absorption from LH sites is significantly impaired and highly variable [20] [51]. This results in unexpected blood glucose fluctuations, including both hyperglycemia and an increased risk of hypoglycemia [20].
- Increased Insulin Requirements: To overcome the poor absorption, patients often require higher insulin doses. One study found total daily doses were, on average, 36% higher in patients with LH, representing a major source of clinical inefficiency and cost [20].
Q3: What is the evidence-based gold standard for diagnosing lipohypertrophy in a clinical research setting?
A multi-modal approach is recommended, as visual inspection alone is insufficient.
- Palpation: The clinical standard, involving a systematic pinching maneuver to detect elastic or firm nodules beneath the skin [3] [51]. However, its accuracy is highly dependent on trained personnel, with trained professionals being 45% more likely to detect smaller LH lesions [3].
- Ultrasonography: A more sensitive and objective tool that is about 30% more effective than palpation. Ultrasound can identify structural changes in the deep subcutaneous tissue before they are visible or palpable and can differentiate between pure LH and mixed lesions with fibrotic components [3].
Experimental Protocols & Methodologies
Protocol 1: Ultrasonographic Assessment of Injection Sites
Objective: To quantitatively and qualitatively characterize subcutaneous tissue changes in response to repeated insulin injections.
Methodology:
- Equipment: Use a high-frequency linear array transducer (e.g., >12 MHz) for detailed superficial tissue resolution.
- Subject Positioning: Standardize patient positioning (e.g., supine for abdomen, sitting for arms) and mark a grid on the area of interest for systematic scanning [3].
- Image Acquisition: Apply ample gel to minimize transducer pressure, which can deform subcutaneous architecture. Capture images in both transverse and longitudinal planes.
- Key Metrics:
- Echogenicity: Compare the brightness of the subcutaneous layer to adjacent normal tissue. LH often appears as hypoechoic (darker) areas due to increased adiposity, while fibrosis is hyperechoic (brighter) [3].
- Layer Thickness: Measure the thickness of the dermis and subcutaneous fat layer.
- Structural Anomalies: Document the presence of nodules, cystic changes, or fibrous strands.
Protocol 2: Assessing the Impact of Injection Technique on Glycemic Outcomes
Objective: To evaluate the metabolic and economic impact of correcting improper injection techniques.
Methodology (based on a cited clinical study [52]):
- Baseline Assessment (Day 0):
- Recruit insulin-using patients (e.g., with >4 years of insulin therapy).
- Administer a detailed Injection Technique Questionnaire (ITQ).
- Perform a thorough clinical examination of all injection sites for LH via palpation and/or ultrasound.
- Record baseline HbA1c, Fasting Blood Glucose (FBG), and Total Daily Insulin Dose (TDD).
- Intervention:
- Conduct a standardized, individualized training session.
- Educate on proper site rotation (e.g., anti-clockwise pattern), avoiding LH areas [53].
- Switch all participants to 4mm pen needles with instruction to not reuse them [52].
- Teach correct injection without aspiration and with an adequate post-injection dwell time.
- Follow-up (3 and 6 months):
- Re-assess all metabolic parameters (HbA1c, FBG, TDD) and injection sites.
- Re-administer the ITQ to evaluate adherence to the new technique.
Expected Outcomes (based on [52] and [53]): Significant reductions in HbA1c (~0.6%), FBG, TDD (~2.0 IU), and LH prevalence after 3 months.
Quantitative Data Synthesis
Table 1: Economic and Clinical Impact of Lipohypertrophy (LH)
| Parameter | Findings | Source / Context |
|---|---|---|
| LH Prevalence | 37% - 64% of insulin-injecting patients (based on clinical examination); up to 48% in pediatric T1D cohorts. | [3] [51] |
| Increased Insulin Requirement | TDD is 36% higher (avg. +15 IU/day) in patients with LH vs. those without. | [20] |
| Glycemic Improvement Post-Training | Mean HbA1c reduction of 0.58% and TDD reduction of 2.0 IU after 3 months of proper technique. | [52] |
| LH Reduction Post-Training | Significant reduction in LH incidence and grade after 6 months of systematic site rotation. | [53] |
Table 2: Recommended Needle Specifications for Subcutaneous Delivery
| Parameter | Recommendation | Rationale | |
|---|---|---|---|
| Needle Length | 4 mm for all adults and children; 5-6 mm only if 4mm unavailable (with skinfold). | Minimizes risk of intramuscular (IM) injection; equivalent glycemic control to longer needles. | [11] [51] [52] |
| Injection Angle | 90° (perpendicular) for 4mm needles without a skinfold for most adults. | Ensures consistent subcutaneous deposition. A 45° angle is recommended only for longer needles when using a skinfold. | [51] [54] |
| Skinfold | Required for 4mm needles in very thin adults (BMI <19 kg/m²) and children ≤6 years. | Ensures the needle does not penetrate into muscle. | [51] |
Pathophysiological Workflow and Signaling
The following diagram illustrates the core pathways from insulin injection to the development of tissue complications.
Mechanisms of Insulin-Induced Lipohypertrophy
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for Investigating Insulin Injection Techniques
| Item / Solution | Function / Application in Research |
|---|---|
| High-Frequency Ultrasound System | Gold-standard for objective, quantitative measurement of subcutaneous tissue thickness, echogenicity, and early detection of LH lesions before clinical manifestation [3]. |
| Tension-Offloading Dressings | Investigational device (e.g., embrace) to apply compressive force and reduce mechanical tension at injection sites. Used to test the hypothesis that modulating mechanotransduction can prevent fibrosis and adipogenesis [20]. |
| 4mm Pen Needles | The recommended standard needle length for ensuring consistent subcutaneous deposition and minimizing intramuscular injection risk in clinical trials and practice [11] [51] [52]. |
| Injection Technique Questionnaire (ITQ) | Validated data collection tool (e.g., from FITTER workshop) to standardize the assessment of patient-reported injection practices, site rotation habits, and needle reuse across study populations [11] [51]. |
| Continuous Glucose Monitoring (CGM) | Provides high-resolution data on glycemic variability (e.g., time-in-range, hypoglycemia). Essential for quantifying the metabolic consequences of injecting into LH sites versus healthy tissue [3] [20]. |
FAQs: Addressing Core Challenges in Injection Site Research
Q1: What are the primary pathophysiological mechanisms of injection site lipohypertrophy (LH) and fibrosis?
Lipohypertrophy and fibrosis are common sequelae of repeated subcutaneous insulin injections. The mechanisms involve two interrelated processes [20]:
- Lipohypertrophy: Local accumulation of fatty tissue results from insulin's localized anabolic effect on adipocytes, stimulating both hypertrophy (cell enlargement) and hyperplasia (cell proliferation) of fat cells [20].
- Fibrosis: The mechanical trauma of repeated injections triggers a chronic inflammatory response and wound-healing process. This leads to the deposition of stiff, dense fibrotic scar tissue by fibroblasts, a process heavily influenced by mechanical forces on the skin [20].
Q2: What is the clinical and economic impact of these injection site complications?
These complications significantly impair diabetes management and increase costs [20] [51]:
- Impaired Glycemic Control: Insulin absorption from these sites becomes erratic and substantially reduced. This leads to marked hyperglycemia and increased glycemic variability [20] [51].
- Increased Insulin Requirements: Patients injecting into LH sites require, on average, 36% more insulin daily to achieve glycemic targets, representing a multi-billion dollar waste in the US alone [20].
- Heightened Complication Risk: Unpredictable absorption increases the risk of both hyperglycemia and hypoglycemia (a 2.7-fold increased risk) [20].
Q3: What are the key barriers to patient adherence with proper site rotation protocols?
Qualitative research identifies three major thematic barriers [2]:
- Lack of Knowledge: This includes insufficient health education from providers, patient forgetfulness, and misconceptions about the technique [2].
- Limited Feasibility: Patients report practical difficulties with site rotation, financial pressures leading to needle reuse, and an inability to self-monitor for flat, non-palpable LH lesions [2].
- Low Motivation: Patients often demonstrate low perceived severity and low perceived susceptibility to the risks of LH [2].
Q4: How can researchers accurately detect and quantify lipohypertrophy in clinical studies?
While physical examination (inspection and palpation) is common in clinical practice, it has significant limitations for research. Ultrasound examination emerges as a superior diagnostic modality, offering enhanced sensitivity and specificity, particularly for identifying non-palpable or "flat" lipohypertrophy. Ultrasound facilitates precise identification and measurement of affected areas [2].
Q5: What novel interventions are being explored to prevent these complications beyond patient education?
Beyond educational initiatives, a novel biomechanical approach is under investigation. Given the role of mechanical tension in driving fibrosis, tension-offloading devices (e.g., specific adhesive dressings) are being studied. These devices apply compressive force to the injection site, which has been shown in vitro to inhibit adipogenesis and, based on clinical evidence from surgery, to reduce skin scarring. Clinical trials are needed to validate this approach for insulin injection sites [20].
Table 1: Epidemiological and Clinical Impact Data of Injection Site Complications
| Metric | Value | Context / Source |
|---|---|---|
| LH Prevalence | 41.8% (average), range 14.5%-88% | Common local complication of insulin therapy [2] [20]. |
| Increase in Daily Insulin Dose | 36% higher (absolute +15 IU/day) | For patients injecting into LH sites versus those without LH [20]. |
| Hypoglycemia Risk | 2.7 times increased risk | Associated with the presence of lipohypertrophy [20]. |
| Needle Reuse | ≥3 times | Frequent needle reuse is a major risk factor for LH [2]. |
| Barrier: Lack of Knowledge | 100% of interviewed cohort | No patient knew all preventive measures for LH [2]. |
Table 2: Key Recommendations for Optimal Injection Technique in Research Protocols
| Parameter | Evidence-Based Recommendation | Rationale |
|---|---|---|
| Needle Length | 4-mm pen needles for all patients | Shortest needle available; minimizes risk of intramuscular injection and reduces pain; no need for skinfold pinches in most adults [51]. |
| Site Rotation | Systematic, clockwise pattern; ≥1 cm between consecutive injections | Prevents overuse of a single area, allowing tissue recovery and preventing LH [2] [23]. |
| Needle Reuse | Single-use only | Reuse blunts the needle, increases trauma, and is a primary risk factor for LH [2]. |
| Site Monitoring | Regular palpation and ultrasound confirmation | Essential for identifying early-stage or flat LH. Palpation can be supplemented with ultrasound for higher sensitivity in research settings [2]. |
Experimental Protocols for Adherence and Complication Research
Protocol 1: Assessing the Efficacy of a Structured Site Rotation Education Framework
This protocol is adapted from quasi-experimental and qualitative research methodologies [2] [53].
1. Objective: To evaluate the impact of a structured patient education framework on the incidence of lipohypertrophy and glycemic control.
2. Methodology:
- Design: Quasi-experimental, pre-test/post-test with a control group.
- Participants: Recruit adult participants with diabetes on insulin therapy. Exclude those with severe cognitive or psychiatric disorders.
- Intervention:
- Control Group: Receives standard care and education.
- Study Group: Receives a structured education intervention based on identified barriers [2]. This includes:
- Theoretical Component: Education on LH consequences and susceptibility.
- Practical Demonstration: Visual guides and hands-on training for systematic anti-clockwise site rotation.
- Feasibility Aids: Address needle cost concerns, provide guides for self-palpation.
- Data Collection:
- Analysis: Compare within-group and between-group changes in LH incidence and glycemic metrics.
Protocol 2: Evaluating a Novel Biomechanical Prevention Strategy
This protocol is based on theoretical and early clinical evidence for tension-offloading [20].
1. Objective: To determine if a tension-offloading dressing can reduce the histological severity of fibrosis and lipohypertrophy at insulin injection sites.
2. Methodology:
- Design: Randomized controlled trial, ideally double-blinded.
- Participants: Patients with type 1 or type 2 diabetes initiating insulin pump therapy or multiple daily injections.
- Intervention:
- Active Group: Applies a validated tension-offloading dressing (e.g., embrace device) immediately after needle removal at each injection/set change.
- Control Group: Uses standard care or a placebo dressing.
- Data Collection:
- Primary Outcome: Histological assessment of adipose tissue hyperplasia and fibrosis from 3mm punch biopsies of used injection sites after 6 months.
- Secondary Outcomes: Ultrasound-measured LH thickness, intra-patient variability in glucose levels, and insulin absorption kinetics measured by microdialysis.
- Analysis: Compare histological scores and secondary outcomes between groups using appropriate statistical tests (e.g., t-tests, ANOVA).
Signaling Pathways and Experimental Workflows
Mechanisms of Tissue Complication and Targeted Intervention
Workflow for Evaluating Adherence Frameworks
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Injection Technique Research
| Item / Solution | Function in Research Context |
|---|---|
| High-Frequency Ultrasound Systems | Gold-standard for objective, quantitative measurement of subcutaneous tissue thickness, lipohypertrophy lesion size, and density. Essential for validating palpation findings [2]. |
| 4mm Pen Needles | The standard needle recommended for all patients to ensure consistent subcutaneous deposition and minimize confounding from intramuscular injections in clinical trials [51]. |
| Tension-Offloading Dressings | An investigational device (e.g., embrace device) to test the biomechanical hypothesis of reducing fibrosis and lipohypertrophy through applied compressive force [20]. |
| Structured Interview Guides | Qualitative research tool (semi-structured) to identify nuanced patient barriers (knowledge, feasibility, motivation) to adherence, informing the design of targeted education frameworks [2]. |
| Injection Site Phantoms | Artificial skin and subcutaneous tissue models for training patients on proper rotation techniques and for standardizing injection force measurements across study participants. |
| Glucose Clamp Equipment | To precisely measure insulin pharmacodynamics (action) and pharmacokinetics (absorption) when comparing injections into healthy sites versus lipohypertrophic sites [20]. |
For researchers investigating insulin efficacy and complications such as lipodystrophy, proper storage and handling are critical variables that can significantly influence experimental outcomes. Inconsistent insulin potency, resulting from improper storage or injection techniques, introduces a major confounding variable in studies aiming to understand the pathogenesis of injection site reactions and optimize drug delivery. This guide provides detailed, actionable protocols to ensure insulin stability and proper administration throughout your research workflows.
Core Storage Protocols: Quantitative Stability Data
Adherence to precise storage conditions is fundamental to maintaining the chemical integrity and biological activity of insulin. The following table summarizes key stability parameters derived from manufacturer guidelines and empirical studies.
Table 1: Insulin Storage Stability Parameters
| Insulin State | Recommended Temperature Range | Maximum Storage Duration | Key Supporting Evidence |
|---|---|---|---|
| Unopened (Refrigerated) | 36°F to 46°F (2°C to 8°C) [55] [56] | Until expiration date [55] | Manufacturer guidelines; maintained potency in controlled cold-chain [57] |
| In-Use (Room Temperature) | 59°F to 86°F (15°C to 30°C) [55] [56] | 28 days for most formulations [55] [58] [59] | Standard practice; FDA and manufacturer recommendations [55] [56] |
| Opened Vials (Extreme Conditions) | Up to 37°C [57] | Up to 2 months (unopened) [57] | Cochrane review indicating no clinically relevant loss of potency for unopened SAI/IAI [57] |
| Insulin in Pump Infusion Set | Below 98.6°F (37°C) [55] | 48-72 hours [55] [56] | Manufacturer advisories; risk of degradation and contamination [55] |
Experimental Consideration: For studies simulating real-world conditions, note that data indicates unopened short-acting (SAI) and intermediate-acting (IAI) insulins can be stored at up to 25°C for six months and up to 37°C for two months without clinically relevant loss of potency [57]. This is a critical parameter for designing experiments related to insulin stability in resource-limited settings or climate-impacted scenarios.
Handling and Preparation: Best Practice Methodologies
Proper handling prior to injection is essential to ensure sterility and consistent pharmacological response.
Visual Inspection Protocol: Before use, visually inspect the insulin. Do not use if the solution is unclear, discolored, or cloudy (unless it is a formulation like NPH that is normally cloudy after mixing). Also discard insulin if it appears viscous, has crystallization, small lumps, or particles, or has an unusual odor [55] [59].
Mixing and Preparation:
- For cloudy insulins, mix by gently rolling the vial between your palms. Avoid shaking vigorously, as this can create air bubbles that affect dosing accuracy [55].
- If drawing from a multi-use vial, clean the rubber stopper with an alcohol swab before each use and allow it to air dry [55].
Essential Research Reagents and Materials
The following table details key materials required for studies involving insulin storage, handling, and injection site analysis.
Table 2: Key Research Reagent Solutions and Materials
| Item | Function/Application in Research |
|---|---|
| Domestic/Medical Refrigerator | Provides standard 2°C-8°C storage for unopened insulin stocks; requires internal thermometer due to potential temperature fluctuations [59]. |
| Temperature Data Logger | Critical for continuous monitoring and validation of storage temperature throughout the experimental supply chain [60]. |
| Ultrasound Imaging System | Gold-standard for identifying and characterizing subclinical lipohypertrophy (LH) lesions, which are often non-palpable [2]. |
| 4-mm Pen Needles | Standard for subcutaneous delivery in clinical and translational research; minimizes pain and intramuscular injection risk [11]. |
| Sharps Containers | Mandatory for safe disposal of used needles and syringes in accordance with biohazard safety protocols [55] [61]. |
| Alcohol Swabs | Used for skin asepsis and cleaning vial stoppers to maintain sterility and prevent microbial contamination [55]. |
Troubleshooting FAQs: Addressing Common Research Scenarios
Q1: An experimental batch of insulin was accidentally left at room temperature (22°C) for 48 hours in its original, unopened packaging. Is it still viable for our study? A: Yes, it is likely still viable. Unopened insulin is quite stable. Pharmaceutical data indicates that unopened vials and cartridges can be stored at temperatures up to 25°C for several months without a clinically relevant loss of potency [57]. You can proceed with its use, but for the integrity of your experiment, it is advisable to mark this batch and consider using it for non-critical assays or to confirm potency if possible.
Q2: What is the recommended protocol for administering multiple daily injections in an animal model to prevent site complications that could confound histological analysis? A: Implement a systematic site-rotation protocol within the same general anatomical area. Inject in a line about 1 cm away from the previous injection, moving to a new site with each dose [2]. This ensures consistent absorption kinetics for your pharmacokinetic studies while preventing lipohypertrophy (LH), a common complication that alters tissue morphology and insulin absorption, thereby introducing significant variability in your results [2] [11].
Q3: During a long-term study, we suspect lipohypertrophy at injection sites in our animal model. How can we confirm this and how does it impact our data on insulin absorption? A: Ultrasound examination is the most sensitive method to confirm LH, including non-palpable "flat" lesions [2]. Visually inspect and palpate sites for soft, rubbery swellings. Injecting into LH sites significantly impairs insulin absorption, leading to marked hyperglycemia and unpredictable glycemic responses [2]. This can invalidate pharmacokinetic data. If LH is confirmed, you must avoid injecting into those areas and note this variable in your analysis.
Q4: A power outage compromised the refrigeration for insulin vials designated for a critical assay. What are the stability thresholds under such emergency conditions? A: Pharmaceutical data provides guidance for these scenarios. Unopened vials of short-acting and intermediate-acting insulin can withstand temperatures up to 37°C for up to two months without a clinically relevant loss of potency [57]. If the temperature exceeded this threshold or the insulin was already opened, it is safer to discard the batch to ensure assay reliability. Always refer to the specific manufacturer's data for the insulin formulation you are using.
Experimental Protocols and Workflows
Protocol: Assessing the Impact of Storage Temperature on Insulin Potency
Objective: To determine the in vitro potency of insulin samples subjected to various storage conditions.
Methodology:
- Sample Preparation: Aliquot identical samples of a single insulin lot into multiple vials.
- Experimental Groups: Expose groups to different conditions:
- Control: Constant 4°C refrigeration.
- Room Temperature: Constant 25°C.
- Elevated Temperature: Constant 37°C.
- Cyclic Stress: Oscillating temperatures between 25°C and 37°C every 12 hours.
- Duration: Expose samples for periods of 28 days, 2 months, and 3 months.
- Analysis: Use High-Performance Liquid Chromatography (HPLC) to detect and quantify insulin transformation products and measure insulin content [57]. Compare results against control samples to calculate percentage potency loss.
Protocol: Correlating Injection Technique with Tissue Morphology
Objective: To investigate the relationship between injection site rotation practices and the development of lipohypertrophy.
Methodology:
- Subject Grouping: Establish a longitudinal study with appropriate animal or human subject cohorts.
- Intervention: Implement a standardized injection protocol, deliberately varying site rotation practices between groups (systematic rotation vs. repeated same-site injections).
- Monitoring: Regularly (e.g., monthly) examine all injection sites using high-frequency ultrasound and palpation to detect and characterize LH lesions [2].
- Histological Correlation: At defined endpoints, perform tissue biopsies for histological analysis to correlate ultrasound findings with adipose tissue hyperplasia and fibrosis.
- Functional Assessment: Concurrently, perform glucose clamp studies or similar assays to measure the pharmacodynamic response (e.g., rate of insulin absorption) when insulin is injected into healthy vs. LH-affected sites [2].
The following workflow diagram illustrates the logical relationship between improper handling, its consequences on insulin and tissue, and the resulting impact on research data.
Overcoming Implementation Barriers and Advanced Detection Strategies
Technical Support & FAQs: Troubleshooting Patient Barriers in Injection Site Rotation Research
FAQ 1: What are the primary patient-derived barriers to consistent insulin injection site rotation, and what is their relative prevalence? Research, particularly recent qualitative studies, identifies three core barrier themes. A 2024 study involving in-depth interviews with 17 patients with lipohypertrophy (LH) found that barriers cluster into lack of knowledge, limited feasibility, and low motivation [2]. The table below summarizes these themes and their underlying subthemes.
Table 1: Primary Patient Barriers to Injection Site Rotation
| Major Theme | Subthemes | Representative Patient Quote |
|---|---|---|
| Lack of Knowledge | Insufficient health education, forgetfulness, misconceptions | "The HCPs asked me to rotate the injection site, but they did not say how to do it clearly." [2] |
| Limited Feasibility | Limitations in site rotation, financial pressures for needle replacement, failure to self-monitor flat LH | Information not available in search results |
| Low Motivation | Low perceived severity of LH, low perceived susceptibility to developing LH | Information not available in search results |
FAQ 2: What quantitative evidence links lipohypertrophy to negative glycemic and economic outcomes? Lipohypertrophy has a significant and measurable impact on glycemic control and healthcare costs. The following table synthesizes key findings from large-scale observational studies and meta-analyses.
Table 2: Quantitative Impact of Lipohypertrophy on Glycemic and Economic Outcomes
| Outcome Metric | Findings with Lipohypertrophy (LH) | Comparative Data without LH | Source / Context |
|---|---|---|---|
| Prevalence | 37% - 64% of insulin-injecting patients [3]; up to 88% in some populations [20] | N/A | Multiple clinical examinations [3] [20] [51] |
| HbA1c | 8.85% (average in one large study) [62] | 8.30% (average) [62] | Injection Technique Questionnaire (ITQ) survey of >13,000 patients [62] |
| Total Daily Insulin Dose | 36% higher on average (+15 IU/day) [20]; ~10 more units per day [62] | Lower, more appropriate doses | Controlled studies comparing patients with and without LH [20] [62] |
| Hypoglycemia Risk | 2.7 times increased risk [20]; Higher frequency of unexpected hypoglycemia [62] | Lower, baseline risk | Patient surveys and clinical studies [20] [62] |
FAQ 3: What are the established and emerging experimental methodologies for investigating injection site pathology? Research into lipodystrophy employs a range of diagnostic and investigative protocols.
Established Clinical Diagnostic Protocol: Visual Inspection and Palpation
- Methodology: Diagnosis begins with visual inspection and systematic palpation of all potential injection sites (abdomen, thighs, arms, buttocks) [3] [9]. A pinching maneuver is critical for identifying less visible, elastic nodules [3] [2].
- Workflow: The patient should be in a relaxed state. The examiner visually scans the area for swelling or discoloration, then uses deep palpation with the fingertips to assess texture. The pinching maneuver helps determine the sides and full extent of a lipohypertrophic lesion [3]. Clinical training improves detection rates for lesions smaller than 4 cm by 45% [3].
Advanced Diagnostic Protocol: Ultrasonic Imaging
- Methodology: High-frequency ultrasound is used to visualize structural changes in the subcutaneous tissue [3] [2]. This method can identify dermal thickening, fibrotic tissue, and necrotic changes that are not detectable via palpation [3].
- Workflow: A linear array transducer is used on cleaned skin over the injection area. Ultrasound can reveal hypoechoic areas corresponding to adipocyte hypertrophy and hyperechoic strands indicating fibrosis [3]. It is about 30% more sensitive than palpation alone and is particularly useful for quantifying tissue changes in a research setting [3].
Experimental Research Model: Investigating Mechanical Force Modulation
- Background: Based on the established role of mechanical forces in fibrosis and adipogenesis, researchers are exploring tension-offloading as a preventive measure [20].
- Methodology: This involves applying a specialized, pre-tensioned dressing (e.g., the embrace device) to the injection site. The dressing applies a compressive, tension-reducing force across the skin and underlying tissue [20].
- Hypothesized Mechanism: Reduced mechanical tension is known to decrease fibroblast production of pathological extracellular matrix, thereby preventing fibrosis. Concurrently, compressive force has been shown in vitro to inhibit adipocyte differentiation and proliferation, targeting the hyperproliferation seen in lipohypertrophy [20]. Clinical trials are needed to validate this approach for insulin injection sites [20].
The following diagram illustrates the logical framework and hypothesized biological pathways for this experimental approach.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials and Tools for Injection Site Pathology Research
| Item | Function / Rationale in Research |
|---|---|
| High-Frequency Ultrasound System | The gold-standard for objective, quantitative measurement of subcutaneous tissue changes, including dermal thickness and early fibrotic formation before visual manifestation [3] [2]. |
| 4-mm Pen Needles / 6-mm Syringe Needles | The recommended needle length for all patients in clinical practice; using the shortest effective needle minimizes the variable of intramuscular injection and its confounding effect on insulin pharmacokinetics in studies [51] [62]. |
| Tension-Offloading Dressings | An investigational device (e.g., embrace Device) used in experimental models to apply controlled compressive force to an injection site, allowing for the study of mechanical force modulation in preventing fibrosis and lipohypertrophy [20]. |
| Continuous Glucose Monitoring (CGM) Systems | Provides high-resolution, objective data on glucose variability, hypoglycemia, and hyperglycemia. Essential for correlating the presence of lipohypertrophy with metrics like Time-in-Range and for measuring the glycemic consequences of injection site complications [3] [63]. |
Technical Support Center
Troubleshooting Guide: Common Ultrasonography Challenges
1. Problem: Inability to distinguish between lipohypertrophy (LH) types based on echo patterns.
- Question: During ultrasound imaging, the hyperechoic patterns of different LH types look similar. How can I accurately classify them?
- Solution: Focus on the combination of morphology, borders, and internal echogenicity. Nodular hyperechoic LH typically presents as a well-defined, focal mass. In contrast, diffuse hyperechoic LH has less defined borders and a more spread-out appearance. Utilize high-frequency linear array probes (e.g., >12 MHz) for superior spatial resolution to visualize these subtle differences [64].
2. Problem: Low detection rate for subclinical, non-palpable LH.
- Question: My study's detection rate for subclinical LH is lower than the 13-55% reported in literature. What am I missing?
- Solution: Ensure you are systematically scanning the entire recommended injection area (abdomen, thighs, arms), not just where lesions are visible. Subclinical LH lacks surface deformation. Apply a standardized scanning protocol with minimal probe pressure to avoid compressing subtle underlying structures. Ultrasound is 30% more sensitive than palpation, so persistence in technique is key [3].
3. Problem: Uncertainty in quantifying LH area for longitudinal studies.
- Question: I need to track the progression or regression of LH lesions over time. What is the most reliable method for measurement?
- Solution: Use the ultrasound machine's built-in electronic calipers to trace the lesion's perimeter in two perpendicular planes (longitudinal and transverse). Record the maximum length and width. For greater accuracy, capture the cross-sectional area. Ensure consistent patient positioning and anatomical landmarks across all follow-up scans to make measurements comparable [64].
4. Problem: Differentiating early LH from other subcutaneous structures.
- Question: How can I be sure that a subtle hypoechoic area is early LH and not normal fibrous tissue or a small vessel?
- Solution: Employ Color or Power Doppler mode. LH areas typically show reduced or absent blood flow, helping to distinguish them from vascular structures. Furthermore, LH lesions often feel firmer and less mobile under the probe compared to normal adipose tissue. Correlate your findings with the patient's injection history—lesions in common injection sites are highly suspect [64].
5. Problem: Inconsistent results when measuring the impact of LH on insulin pharmacodynamics.
- Question: My experimental data on insulin absorption variability from LH sites is inconsistent. What factors should I control for?
- Solution: Control for these key variables:
- LH Type: Different ultrasound patterns (nodular, diffuse, hypoechoic) may have different absorption kinetics [64].
- Injection Technique: Ensure consistent needle length, injection volume, and injection angle across experiments.
- Insulin Formulation: The absorption profile may differ between insulin analogs and human insulin. Standardizing these parameters will reduce experimental noise and yield more reliable data on insulin absorption variability.
Frequently Asked Questions (FAQs)
Q1: What is the definitive pathological feature of insulin-induced LH observed through advanced imaging? A1: Histological data from scanning electron microscopy reveals that approximately 75% of the subcutaneous tissue in LH areas is composed of macro-adipocytes. These adipocytes are significantly larger than those in adjacent healthy tissue and are often associated with increased fibrosis [3].
Q2: Why is ultrasonography considered superior to physical examination for LH screening in research settings? A2: Ultrasonography provides an objective, high-resolution assessment of subcutaneous tissue architecture. Quantitative data shows it has a significantly higher detection rate (57.6–100%) compared to physical examination (27.9–79.7%). It is uniquely capable of identifying subclinical, non-palpable LH, which can be present in 13.0–55% of cases [64].
Q3: Are there any emerging molecular pathways relevant to LH and skin fibrosis that could be investigative targets? A3: Yes, recent preclinical research highlights the Wnt/lipogenesis axis. Sustained Wnt signaling in dermal adipocytes downregulates key enzymes of de novo lipogenesis, such as Fatty Acid Synthase (FASN). This inhibition is mechanistically linked to both lipodystrophy (fat loss) and subsequent extracellular matrix (ECM) accumulation in skin fibrosis, presenting a potential therapeutic target [65].
Q4: From a technical perspective, what are the primary risk factors for LH development that our experimental models should replicate? A4: The main risk factors to incorporate into experimental design or screening protocols are [3]:
- Failure to rotate injection/site infusion sites.
- Reuse of needles.
- Injection of cold insulin.
- High daily number of injections.
- Large volume per injection.
- Use of longer, thicker needles.
Q5: What is the clinical and research significance of classifying LH into different ultrasonographic patterns? A5: Classification is prognostically significant. The three distinct patterns—nodular hyperechoic (65.5%), diffuse hyperechoic (27.5%), and hypoechoic (7.0%)—are believed to represent different stages or types of tissue remodeling. Each type demonstrates distinct progression patterns and varying degrees of metabolic improvement after intervention, which is crucial for designing targeted studies and interpreting outcomes [64].
Table 1: Comparison of Lipohypertrophy (LH) Detection Methods
| Method | Detection Rate Range | Key Advantages | Key Limitations |
|---|---|---|---|
| Physical Examination | 27.9% - 79.7% | Quick, low cost, no specialized equipment | Low sensitivity for subclinical LH, subjective |
| Ultrasonography | 57.6% - 100% | Detects subclinical LH, objective, allows for classification & measurement | Requires specialized equipment and trained operator |
Table 2: Ultrasonographic Classification of Lipohypertrophy (LH) and Prevalence
| Ultrasound Pattern | Prevalence | Key Sonographic Characteristics |
|---|---|---|
| Nodular Hyperechoic | 65.5% | Well-defined borders, hyperechoic internal pattern [64] |
| Diffuse Hyperechoic | 27.5% | Less defined borders, hyperechoic pattern [64] |
| Hypoechoic | 7.0% | darker, less reflective internal pattern [64] |
Experimental Protocol: Ultrasonographic Assessment of Lipohypertrophy
Title: Standardized Protocol for Longitudinal Ultrasound Imaging and Classification of Insulin-Induced Lipohypertrophy.
1. Objective: To systematically identify, classify, and measure LH lesions in subcutaneous tissue using high-resolution ultrasonography.
2. Materials and Equipment:
- High-frequency linear array ultrasound probe (≥12 MHz).
- Ultrasound gel.
- Examination table.
- Skin marker.
- Data recording sheet or electronic medical record system.
3. Methodology: 1. Patient Positioning: Position the patient supine for abdominal scans and seated for arm and thigh scans. Ensure the target area is relaxed and fully accessible. 2. Scanning Technique: * Apply a generous amount of ultrasound gel to the skin to ensure acoustic coupling. * Place the probe gently on the skin to avoid compressing the underlying tissue, which can alter the appearance of lesions. * Systematically scan the entire potential injection area (a 4-quadrant approach for the abdomen is recommended) in both longitudinal and transverse planes. 3. Image Acquisition and Analysis: * Identify any areas of altered subcutaneous echogenicity. Normal fat is moderately hyperechoic with a fine, homogeneous speckle pattern. * For any identified lesion, freeze the image and use electronic calipers to measure its maximum length and width in two perpendicular planes. * Classify the lesion according to the established ultrasound patterns (Nodular Hyperechoic, Diffuse Hyperechoic, Hypoechoic) based on its borders and internal echo pattern [64]. * Engage Color Doppler mode to assess vascularity within and around the lesion. LH typically exhibits reduced or absent blood flow. 4. Documentation: Save representative images for each lesion, noting the size, location, classification, and vascularity.
4. Data Interpretation:
- Correlate ultrasound findings with the patient's injection history and glycemic control metrics (e.g., HbA1c, glucose variability).
- In longitudinal studies, document changes in lesion size, echogenicity, and classification over time in response to intervention (e.g., proper site rotation).
Signaling Pathway and Experimental Workflow
Pathway from Insulin Stimulation to Skin Fibrosis
LH Ultrasound Study Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for LH and Skin Fibrosis Research
| Item / Reagent | Function / Application in Research |
|---|---|
| High-Frequency Linear Ultrasound | High-resolution imaging of subcutaneous tissue structure for LH detection and classification [64]. |
| Fatty Acid Synthase (FASN) Inhibitors | Pharmacological tools to investigate the role of de novo lipogenesis in the Wnt-mediated lipodystrophy and fibrosis pathway [65]. |
| Wnt Signaling Agonists/Antagonists | Molecular probes to manipulate the Wnt pathway in vitro and in vivo to establish its mechanistic role in adipocyte dysfunction [65]. |
| Histology Stains (e.g., H&E, Masson's Trichrome) | For visualizing tissue morphology, adipocyte size, and collagen deposition (fibrosis) in biopsy samples [3]. |
| Dedicated Injection Site Rotation Maps | Clinical tools used in interventional studies to educate patients and standardize the site rotation protocol, mitigating LH formation [3]. |
Table 1: Key Epidemiological and Clinical Data on Insulin-Induced Lipohypertrophy
| Metric | Value/Range | Context & Implications |
|---|---|---|
| Global Prevalence | 37% - 64% of insulin users [3] | Highlights the widespread nature of the problem among individuals with diabetes. |
| Reported Peak Prevalence | Up to 88% of insulin-dependent patients [20] | Indicates the severity of the issue in specific cohorts. |
| Affected Global Population | ~90 million people [3] | Estimates the vast scale of the issue based on nearly half of ~200 million insulin users. |
| Impact on Insulin Requirements | Increases by ~36% on average [20] | Patients with LH require significantly higher daily insulin doses (absolute difference of ~15 IU/day). |
| Economic Impact (US) | >$1 billion/year in unnecessary insulin costs [20] | Conservative estimate of the financial waste due to increased insulin requirements. |
| Risk of Hypoglycemia | 2.7 times increased risk [20] | Demonstrates a major safety consequence of unpredictable insulin absorption from LH sites. |
| Common Risk Factors | Failure to rotate sites, needle reuse, >1 injection/day, large injection volumes [3] | Identifies primary correctable behaviors leading to LH development. |
Troubleshooting Guide: Resolving Lipohypertrophy
Table 2: Troubleshooting Common Scenarios and Implementing Corrective Actions
| Scenario / Problem | Underlying Cause | Corrective Action & Protocol |
|---|---|---|
| Existing LH Lesions Identified | Repeated insulin injections/infusions into the same localized area, triggering adipocyte hyperplasia and local fibrosis [3] [20]. | 1. Immediate Cessation: Completely avoid injecting into any identified or suspected LH area [2].2. Site Transition: Switch to healthy, unaffected tissue following a structured rotation plan [53].3. Long-Term Monitoring: LH areas can resolve over time once insulin exposure ceases [17]. |
| Unpredictable Glycemic Swings | Altered and erratic insulin absorption pharmacokinetics from fibrotic and hypertrophic LH tissue [20] [66]. | 1. Site Audit: Systematically palpate and inspect all potential injection sites for LH [3].2. Correlate with Data: Review glucose monitoring data for patterns of unexplained variability coinciding with injections from specific areas [3].3. Re-educate on Technique: Retrain on comprehensive site rotation to prevent recurrence [11]. |
| Patient Non-Adherence to Site Rotation | Multi-factorial barriers including lack of knowledge, financial pressure to reuse needles, and low perceived severity of LH [2]. | 1. Structured Education: Implement and repeatedly reinforce standardized injection technique training, emphasizing the "how" and "why" of rotation [3] [11].2. Visual Aids: Provide clear diagrams and rotation schedules.3. Address Needle Cost: Acknowledge financial concerns and advocate for single-use needle policies to reduce reuse [2]. |
| Failure to Detect Non-Visible LH | Reliance solely on visual inspection; flat, nodular LH may not be visibly apparent [3] [2]. | 1. Implement Palpation: Train providers and patients in systematic palpation and the "pinching maneuver" to identify sub-surface lesions [3].2. Ultrasound Imaging: Utilize high-frequency ultrasound in clinical settings for objective, sensitive detection of structural changes in subcutaneous tissue [3] [2]. |
Experimental Protocols for LH Research
Protocol 1: Clinical Detection and Grading of Lipohypertrophy
Objective: To standardize the identification and classification of LH lesions in a clinical or research setting using palpation and visual inspection.
Materials: Examination table, disposable gloves, marking pen, camera (optional, for documentation).
Methodology:
- Positioning: Have the participant lie in a supine position. Rotating the body along its longitudinal axis can enhance the profile of the skin and improve detectability of smaller lesions [3].
- Systematic Palpation: Using a gloved hand, systematically palpate all recommended injection areas (abdomen, thighs, buttocks, arms). Employ a pinching maneuver to lift the skin and subcutaneous tissue. This is critical for identifying less visible, elastic nodules [3] [2].
- Assessment: Note the texture, size, and elasticity of any raised or hardened areas. Compare with adjacent normal tissue.
- Grading (Example Framework):
- Grade 0: No palpable or visual abnormality.
- Grade 1: Palpable nodularity or thickening without visual change.
- Grade 2: Visible and palpable soft, fatty swelling.
- Grade 3: Large, visible, and hard fibrous lump.
- Documentation: Mark the boundaries of any LH lesions and record their location, size, and grade. Photograph with consent.
Protocol 2: Ultrasonic Imaging of Subcutaneous Tissue Structure
Objective: To objectively quantify structural changes in the subcutaneous tissue associated with LH, including dermal thickening and adipocyte morphology.
Materials: High-frequency linear array ultrasound transducer (e.g., >15 MHz), ultrasonic gel, DICOM image analysis software.
Methodology:
- Preparation: Apply ultrasonic gel to the area of interest (a known LH site and a contralateral control site).
- Imaging: Using the high-frequency transducer, capture cross-sectional images of the skin and subcutaneous tissue. Ensure the image depth is sufficient to capture the full subcutaneous fat layer.
- Measurement: Use caliper tools within the ultrasound software to measure:
- Dermal Thickness: From the epidermis to the dermal-hypodermal junction.
- Subcutaneous Echoarchitecture: Note the presence of hyperechoic fibrous strands within the normally hypoechoic fat layer [3].
- Lesion Dimensions: Measure the depth and width of any distinct LH nodules.
- Analysis: Compare echoarchitecture and thickness measurements between LH and healthy control sites. Ultrasound has been shown to be about 30% more sensitive in detecting LH than palpation alone [3].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Models for Investigating Insulin Injection Site Pathophysiology
| Research Tool / Reagent | Function & Application in LH Research |
|---|---|
| High-Frequency Ultrasound System | Non-invasive in vivo imaging for longitudinal monitoring of subcutaneous tissue changes, fibrosis development, and lesion resolution in animal models or human participants [3]. |
| Tension-Offloading Dressings | Investigational device (e.g., embrace) for testing the hypothesis that modulating mechanical forces at the injection site can prevent both fibrosis and lipohypertrophy [20]. |
| Histology Reagents | Standard H&E staining plus specialized stains (e.g., Masson's Trichrome for collagen) to validate tissue morphology, quantify macro-adipocytes, and assess fibrosis in biopsy specimens [3]. |
| 4-mm Pen Needles | Standardized delivery device for preclinical studies aiming to replicate human injection techniques and assess the impact of needle geometry and injection depth on tissue trauma [11]. |
| In Vitro Adipocyte Models | Primary human pre-adipocytes or 3T3-L1 cell lines to study the direct anabolic effects of insulin and the impact of mechanical compressive forces on adipogenesis and hypertrophy [20]. |
FAQs on Lipohypertrophy Management and Research
Q1: What is the direct pathophysiological mechanism by which repeated insulin injections cause lipohypertrophy?
The mechanism is multifactorial. Histology shows that LH areas contain a significantly larger number of macro-adipocytes and regions of fibrosis [3] [20]. This is driven by:
- Local Anabolic Effect: Insulin acts as a growth factor, stimulating localized hypertrophy (enlargement) and hyperplasia (proliferation) of adipocytes [20].
- Mechanical Trauma & Repair: Repeated needle insertion causes minor tissue trauma, initiating an inflammatory response and subsequent repair processes that can lead to fibrotic tissue deposition [2] [20].
- Mechanical Force Sensing: Both fibroblasts and adipocytes are mechanosensitive. Increased skin tension promotes fibrosis, while compressive forces may inhibit adipogenesis [20].
Q2: How does injecting into LH tissue lead to unpredictable glycemic control and increased hypoglycemia risk?
LH significantly alters insulin pharmacokinetics. The fibrotic and hypertrophic tissue:
- Impairs Absorption: Reduces the rate and completeness of insulin absorption from the injection site, leading to marked hyperglycemia [2] [20].
- Increases Variability: Creates an unpredictable and erratic absorption profile [20]. When a patient injects a large dose intended for an LH site into normal tissue, the insulin is absorbed more fully and rapidly, substantially increasing the risk of hypoglycemia [2].
Q3: What are the most effective strategies for preventing LH in a clinical population?
Evidence-based prevention rests on a cornerstone of education and technique:
- Structured Site Rotation: Implementing a formal, systematic rotation plan (e.g., anti-clockwise within a quadrant) is critical. Injections should be spaced at least 1 cm apart [2] [53].
- Single-Use Needles: Strict avoidance of needle reuse prevents microscopic tip deformation that increases tissue trauma [3] [17].
- Regular Site Monitoring: Healthcare professionals should perform visual inspection and palpation of injection sites at least annually, and more frequently if issues arise [66] [17].
- Patient Re-education: Knowledge and technique wane over time. Regular retraining is essential for sustained prevention [3] [11].
Research Pathway and Tissue Response Diagram
Troubleshooting Guides and FAQs
This section addresses common experimental and clinical challenges in the management and prevention of injection site complications.
FAQ 1: What are the primary pathophysiological mechanisms behind injection-induced skin complications, and how can they be modeled in a laboratory setting? Lipohypertrophy and fibrosis are the two most common complications. Lipohypertrophy results from the local stimulating effect of insulin on adipocytes, leading to both hypertrophy and hyperplasia [20]. Fibrosis is a chronic process involving the accumulation of stiff, dense scar tissue due to repeated minor tissue trauma and a subsequent inflammatory response [20]. Histological analysis of biopsy specimens reveals that skin thickening is associated with slightly thickened and tight bundles of collagen in the dermis. Furthermore, amyloid deposits, which stain positively for insulin antibody, have been identified in the subcutaneous tissue and dermis of some patients [67].
FAQ 2: What quantitative imaging metrics can objectively assess the severity of injection site complications? Ultrasonography is a key non-invasive tool for objective assessment. Research studies frequently measure skin thickness and subcutaneous tissue thickness. The table below summarizes quantitative findings from one clinical study [67].
Table 1: Ultrasonographic Measurements of Skin and Subcutaneous Tissue
| Measurement Site | Skin Thickness (mm), Median (Q1, Q3) | Subcutaneous Tissue Thickness (mm), Median (Q1, Q3) |
|---|---|---|
| Normal Site (No injection) | 1.95 (1.60, 2.50) | 15.50 (12.00, 18.25) |
| Abnormal Site (With complications) | 2.80 (2.27, 3.30) | 11.70 (9.25, 14.80) |
FAQ 3: Beyond standard site rotation advice, what novel bioengineering approaches are being investigated to prevent these complications? Modulation of mechanical forces at the injection site is an emerging strategy. Evidence indicates that increased skin tension promotes fibrosis, while compressive force can inhibit adipogenesis [20]. A proposed intervention involves the use of a tension-offloading dressing, which applies a compressive force across the skin. This approach has been shown in randomized controlled trials to significantly reduce scarring after surgical incisions and is theorized to mitigate both fibrosis and lipohypertrophy from repeated injections, though clinical trials for this specific application are needed [20].
FAQ 4: How effective are structured educational interventions at improving injection practices, and what is the quantifiable impact? Structured education, particularly when led by pharmacists, significantly improves injection technique. A pre-post interventional study demonstrated that pharmacist-led training resulted in a dramatic improvement in overall injection technique scores [68]. The following table illustrates the improvement in specific practice metrics before and after the intervention [68] [69].
Table 2: Impact of Pharmacist-Led Intervention on Injection Practices
| Injection Practice | Pre-Intervention | Post-Intervention | 2-Week Follow-up |
|---|---|---|---|
| Correct Insulin Mixing | 7.8% | 100% | 81.1% |
| Proper Cartridge Storage | 77.8% | 91.4% | 88.6% |
| Correct Pen Storage at Room Temperature | 49.4% | 95.1% | 70.8% |
| Median Total Technique Score (0-16 scale) | 10 | 15 | 14 |
FAQ 5: What is the clinical and economic impact of injection site complications like lipohypertrophy? Lipohypertrophy has a direct, negative impact on glycemic control and healthcare costs. Insulin absorption from these sites is erratic and delayed, leading to increased glycemic variability and unexplained hypoglycemia and hyperglycemia [20]. Economically, one study found that patients with lipohypertrophy required, on average, 36% more insulin daily (an absolute difference of 15 IU/day) than those without, representing a significant and unnecessary cost burden to the healthcare system [20].
Experimental Protocols
This section provides detailed methodologies for key experiments and interventions cited in the literature.
Protocol for Ultrasonographic Evaluation of Injection Sites
This protocol is adapted from a study that objectively assessed skin and subcutaneous tissue properties [67].
- Objective: To quantitatively evaluate skin thickness and subcutaneous tissue structure at insulin injection sites and compare them to normal, non-injected control sites.
- Equipment:
- Ultrasonic diagnostic equipment with a linear probe (e.g., center frequency of 12 MHz).
- Coupling gel.
- Procedure:
- Position the participant in a recumbent position.
- Obtain cross-sectional B-mode images of the skin and subcutaneous tissue at a documented abnormal injection site and a control site (e.g., an area 5 cm from the navel with no history of injection).
- Set the depth of field to 3-3.5 cm.
- Measure the skin thickness as the combined thickness of the epidermis and dermis.
- Measure the subcutaneous tissue thickness as the distance from the deepest part of the dermis to the deepest part of the fascia.
- Evaluate the boundary between skin and subcutaneous tissue and the layered structure/echo brightness of the subcutaneous tissue.
- For additional data, perform tissue elasticity imaging (elastography) to assess tissue hardness.
- Analysis: Compare measurements between abnormal and normal sites using appropriate statistical tests (e.g., Wilcoxon signed-rank test).
Protocol for a Pharmacist-Led Injection Technique Intervention
This protocol is based on a pre-post interventional study that demonstrated significant improvements in patient practices [68] [69].
- Objective: To assess and improve insulin injection technique through structured, one-on-one pharmacist-led education.
- Materials:
- Semi-structured questionnaire for demographic and baseline data.
- Observational checklist assessing 16 key injection technique elements (e.g., site rotation, needle disposal).
- A placebo insulin pen device for patient demonstration.
- Procedure:
- Baseline Assessment: Have the patient complete the questionnaire. Use the observational checklist to assess the patient's current injection technique, potentially using the placebo device.
- Intervention: Conduct a one-on-one educational session. The pharmacist should:
- Provide structured education on proper injection technique.
- Demonstrate the correct technique using the placebo device.
- Address specific errors identified in the baseline assessment.
- Discuss the importance of site rotation and the consequences of lipohypertrophy.
- Immediate Re-assessment: Have the patient demonstrate the technique again immediately after training for post-intervention scoring.
- Follow-up: Re-assess the patient's technique after a set period (e.g., 2 weeks) to evaluate the sustainability of the improvement.
- Analysis: Calculate total technique scores and compare pre-, post-, and follow-up scores using non-parametric tests like the Friedman test.
Signaling Pathways and Experimental Workflows
This diagram illustrates the pathophysiological pathways leading to injection site complications and the points of intervention for novel strategies.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Injection Site Complication Research
| Item | Function/Application in Research |
|---|---|
| High-Frequency Linear Ultrasound Probe | Provides high-resolution, cross-sectional images for objectively measuring skin thickness and evaluating subcutaneous tissue structure and echogenicity [67]. |
| Tension-Offloading Dressings | Investigational devices used to apply compressive force and reduce mechanical tension at injection sites, allowing researchers to test the role of biomechanics in fibrosis and lipohypertrophy pathogenesis [20]. |
| Colored Pen Needle System | An educational tool where colors are linked to specific injection zones on a body map. Used in behavioral research to improve patient adherence to site rotation protocols and assess intervention efficacy [70]. |
| Placebo Insulin Pen Device | A training device that mimics a real insulin pen without administering medication. Essential for safely observing and assessing a patient's injection technique in interventional studies [68]. |
| Histological Stains (H&E, Congo Red) | Used on skin biopsy specimens to visualize tissue morphology (H&E) and detect the presence of amyloid deposits (Congo Red), a rare but documented complication at injection sites [67]. |
| Immunohistochemistry Antibodies (e.g., anti-insulin) | Used to confirm the identity of amyloid deposits found in tissue specimens, verifying their origin from injected insulin aggregates [67]. |
FAQs: Glucose Data and Insulin Absorption
Q1: How can glucose data indicate that insulin is being injected into lipohypertrophic (LH) sites?
A1: Injecting insulin into lipohypertrophic (LH) sites, areas of hardened or fatty tissue, significantly alters insulin absorption. This manifests in glucose data through several key patterns [2] [51]:
- Unexplained Hyperglycemia: Persistent high blood glucose levels post-injection, as insulin released from LH sites is slowed and erratic [51].
- Increased Glycemic Variability: Wide, unexplained swings between high and low blood glucose readings due to inconsistent insulin uptake [51] [20].
- Unexplained Hypoglycemia: If a dose accumulates in an LH site and is then suddenly released, or if a subsequent dose is injected into healthy tissue, it can cause a rapid drop in blood glucose [9].
- Elevated Glycated Hemoglobin (A1c): A trend of rising A1c levels despite appropriate insulin dosing [9].
- Dawn Phenomenon Mimicry: Morning hyperglycemia that is resistant to typical dose adjustments of basal insulin [51].
Q2: What are the primary research-identified barriers to proper injection site rotation that contribute to these absorption issues?
A2: A recent qualitative study identified three major thematic barriers [2]:
- Lack of Knowledge: This includes insufficient health education from providers, forgetfulness, and misconceptions about the importance of site rotation.
- Limited Feasibility: Patients report practical limitations in performing systematic site rotation, financial pressures leading to needle reuse, and an inability to self-monitor for "flat" LH that is not visible.
- Low Motivation: Patients often have a low perceived severity of LH and a low perceived susceptibility to developing it, reducing adherence to rotation protocols.
Q3: What quantitative metabolic impacts does lipohypertrophy have on insulin pharmacokinetics and pharmacodynamics?
A3: Research has quantified the significant effects of LH on insulin efficacy and cost. The table below summarizes key findings from clinical studies [51] [20].
Table 1: Quantitative Impact of Lipohypertrophy on Insulin Therapy
| Parameter | Impact of Injecting into LH Sites | Clinical Consequence |
|---|---|---|
| Insulin Absorption | Slower and highly erratic absorption profile [51]. | Increased postprandial glucose and glycemic variability [51]. |
| Total Daily Insulin Dose | Increases by an average of 36% (approx. 15 IU/day) [20]. | Higher treatment costs and increased risk of dosage errors [20]. |
| Risk of Hypoglycemia | Can increase the risk of hypoglycemia by 2.7 times [20]. | More frequent and dangerous low blood sugar events [20]. |
| Glycemic Control | Leads to poorer outcomes and elevated A1c [9] [51]. | Increased risk of long-term diabetic complications [9]. |
Q4: What advanced monitoring techniques are available for detecting subclinical lipohypertrophy in a research setting?
A4: Beyond visual inspection and palpation, which are ineffective for flat LH, ultrasound examination is the superior diagnostic modality [2]. It offers:
- Enhanced Sensitivity: Precisely identifies non-palpable LH lesions and measures subcutaneous tissue structure [2].
- Site Identification: Facilitates the precise identification of optimal injection sites in patients with LH concerns, improving research protocol accuracy [2].
Troubleshooting Guide: Investigating Absorption Anomalies
This guide provides a methodological workflow for researchers to systematically diagnose insulin absorption issues linked to injection sites.
Step 1: Analyze Continuous Glucose Monitor (CGM) Data
- Methodology: Download and analyze CGM or structured self-monitoring of blood glucose (SMBG) data. Calculate key metrics including Mean Glucose, Standard Deviation, and Coefficient of Variation. Visually inspect traces for specific patterns [51] [20].
- Key Indicators: Look for a high glucose level immediately after a meal that fails to decrease over the expected insulin action time, or a sudden, unexplained drop after a period of hyperglycemia.
Step 2: Correlate Glucose Excursions with Injection Logs
- Methodology: Cross-reference the timing and magnitude of glucose excursions with detailed patient logs of injection sites and timings. Use statistical analysis (e.g., regression) to identify correlations between specific anatomic sites and poor glycemic control [2].
- Key Indicators: A consistent pattern of hyperglycemia occurring specifically after injections administered in one region (e.g., left abdomen) but not others.
Step 3: Perform Systematic Physical Examination of Injection Sites
- Methodology: With patient consent, visually inspect and palpate all potential injection sites (abdomen, thighs, arms, buttocks). Use a standardized pinching maneuver to detect elastic, rubbery, or hardened nodules beneath the skin that may not be visible [2] [9].
- Documentation: Document the location, size, and texture of any suspected LH areas on a body map.
Step 4: Conduct Ultrasonographic Confirmation
- Methodology: For research-grade confirmation, use high-frequency ultrasound imaging on identified sites. Compare the echogenicity and structure of subcutaneous tissue at suspected sites to adjacent healthy tissue [2].
- Outcome: Precisely identify and measure the extent of LH lesions, including those not detectable by palpation (flat LH).
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Investigating Insulin Absorption Issues
| Item | Function in Research |
|---|---|
| Continuous Glucose Monitor (CGM) | Provides high-frequency, interstitial glucose data to visualize real-time absorption kinetics and glycemic variability [71]. |
| High-Frequency Ultrasound System | The gold-standard for objectively identifying and quantifying subclinical lipohypertrophy and assessing subcutaneous tissue structure [2]. |
| Standardized Injection Site Body Maps | Enables precise documentation and tracking of injection sites for correlation with metabolic and physical examination data [72]. |
| 4mm Pen Needles | The recommended needle length for consistent subcutaneous deposition, minimizing confounding variables from intramuscular injection [51] [11]. |
| Data Logging Software | For integrating and analyzing time-synchronized data from glucose monitors, insulin pumps, and patient-reported injection logs. |
Developing Patient-Centric Tools and Technologies to Simplify Adherence
Technical Support Center: Troubleshooting Guides and FAQs
This resource provides researchers and drug development professionals with targeted information on overcoming common experimental and clinical challenges related to insulin injection site management, specifically in the context of preventing lipohypertrophy (LH) and scar tissue formation.
Frequently Asked Questions (FAQs)
Q1: What is the clinical significance of lipohypertrophy in diabetes research? Lipohypertrophy is a localized accumulation of fatty tissue at insulin injection sites, with an estimated prevalence of between 14.5% and 88% of insulin-dependent people with diabetes [20]. Its significance lies in its impact on insulin pharmacokinetics; it causes erratic and unpredictable insulin absorption, leading to increased glycemic variability and a higher risk of both hypoglycemia and hyperglycemia [9] [20]. From a research perspective, this variability introduces significant noise into clinical trial data concerning insulin efficacy and dosing.
Q2: What are the primary cellular mechanisms underlying injection-induced fibrosis and lipohypertrophy? The two primary interrelated mechanisms are:
- Fibrosis: This involves the accumulation of stiff, dense scar tissue resulting from repeated minor tissue trauma (injections), which triggers a chronic inflammatory response and causes fibroblasts to produce excess extracellular matrix [20].
- Lipohypertrophy: This is a local accumulation of fatty tissue thought to result from local stimulation of adipocytes by insulin, which is a key hormone in lipid metabolism. This leads to both hypertrophy (enlargement) and hyperplasia (proliferation) of fat cells [20].
Q3: What is the evidence that mechanical forces influence these tissue changes? Research indicates that mechanical forces play a key role. Fibroblasts and adipocytes are mechanosensitive [20]. Increased skin tension is known to promote fibrosis, while in vitro studies show that compressive force can inhibit adipocyte production and differentiation [20]. This provides a theoretical basis for investigating tension-offloading dressings to prevent both fibrotic and lipohypertrophic changes at injection sites.
Q4: How does proper site rotation impact clinical and economic outcomes? Correct injection site rotation is the most critical preventive factor. One study found that of patients with LH, 98% either did not rotate sites or rotated incorrectly, whereas only 5% of those who correctly rotated sites developed LH [73]. Clinically, LH is linked to unexplained hypoglycemia and glycemic variability. Economically, patients with LH require higher daily insulin doses (on average 15 IU more per day), leading to annual costs amounting to hundreds of millions of dollars at a population level [73].
Troubleshooting Guide: Common Experimental and Clinical Challenges
Problem 1: High Glycemic Variability in Study Cohort
- Theory of Probable Cause: Participants are injecting insulin into sites with pre-existing or developing lipohypertrophy [9] [10].
- Plan of Action & Verification:
- Implement a standardized site examination protocol. This should include both visual inspection and palpation of all potential injection sites (abdomen, thighs, buttocks, upper arms) to identify areas that feel lumpy, firm, or rubbery [9] [10].
- Train participants on a structured rotation plan, such as moving systematically from the left to the right side of the abdomen and down the leg, spacing sites at least one finger-width apart [9].
- Verify by re-examining sites during follow-up visits and correlating A1c and glycemic variability data with adherence to the rotation protocol [73].
Problem 2: Inconsistent Insulin Absorption Data in Pre-Clinical Model
- Theory of Probable Cause: Repeated injections in the same localized area on an animal model are inducing localized tissue fibrosis and dysregulated absorption.
- Plan of Action & Verification:
- Establish a rigorous injection site rotation schedule for the animal model, using a shaving or mapping system to track sites accurately.
- Histologically analyze tissue from previous injection sites to confirm the presence of fibrotic scar tissue and adipocyte hypertrophy [20].
- Verify by comparing pharmacokinetic/pharmacodynamic (PK/PD) data, such as serum insulin levels and glucose infusion rates, from rotated sites versus non-rotated sites.
Problem 3: Participant Non-Adherence to Injection Site Rotation Protocol
- Theory of Probable Cause: Participants find rotating sites painful or inconvenient, or prefer lipohypertrophic sites because injections there are less painful [9] [10].
- Plan of Action & Verification:
- Technology Solution: Develop or utilize patient-centric tools like smartphone apps with visual calendars and reminders to track rotation [9].
- Device Optimization: Advocate for the use of modern, shorter (e.g., 4-mm) needles, which are associated with less pain and a lower risk of intramuscular injection, improving the injection experience [11].
- Education: Re-educate participants on the cost and health consequences of LH, framing proper technique as a critical component of their therapy [11] [10].
- Verify adherence through digital logs from the app and confirm via physical examination at study visits.
Summarized Quantitative Data
Table 1: Prevalence and Risk Factors for Lipohypertrophy (LH)
| Factor | Metric | Source |
|---|---|---|
| Overall Prevalence | 14.5% - 88% of insulin-dependent patients | [20] |
| Specific Study Prevalence | 64.4% of studied outpatients (n=430) | [73] |
| Key Risk Factor: Non-Rotation | 98% of patients with LH did not rotate or rotated incorrectly | [73] |
| Key Risk Factor: Needle Reuse | Risk increases significantly when needles are reused >5 times | [73] |
| Impact on Unexplained Hypoglycemia | 39.1% of patients with LH vs. 5.9% without LH | [73] |
| Impact on Glycemic Variability | 49.1% of patients with LH vs. 6.5% without LH | [73] |
Table 2: Economic and Dosing Impact of Lipohypertrophy
| Parameter | Finding | Source |
|---|---|---|
| Average Daily Insulin Dose (with LH) | 56 IU/day | [73] |
| Average Daily Insulin Dose (without LH) | 41 IU/day | [73] |
| Average Dose Increase due to LH | 15 IU/day (a 36% increase) | [73] [20] |
| Reported Insulin Cost Increase (US) | >$1 billion/year in unnecessary costs | [20] |
Detailed Experimental Protocols
Protocol 1: Clinical Identification and Characterization of Lipohypertrophy
- Objective: To systematically identify and document the presence and severity of lipohypertrophy in a clinical research population.
- Materials: Examination table, non-permanent skin marker, ultrasound machine with high-frequency linear probe (for detailed characterization) [73].
- Methodology:
- Inspection: Under good lighting, visually examine all standard insulin injection areas (abdomen, thighs, buttocks, upper arms) for raised, swollen, or thickened areas of skin.
- Palpation: Using the pads of the fingers, systematically palpate the entire area. Note any regions that feel lumpy, firm, rubbery, or hardened compared to the surrounding tissue [9] [10].
- Documentation: Mark the borders of any suspected LH areas with a skin marker. Document the size, location, and texture.
- Ultrasound Confirmation (Optional): Use ultrasonography to obtain an "echo signature" of the tissue. LH typically appears as a hyperechoic (brighter) region in the subcutaneous fat layer, allowing for objective measurement and tracking over time [73].
Protocol 2: Assessing the Impact of Tension-Offloading on Injection Site Pathology
- Objective: To evaluate the efficacy of a mechanical tension-offloading device in preventing fibrosis and lipohypertrophy in an insulin-injecting cohort.
- Materials: Tension-offloading dressing (e.g., embrace device), standard insulin injection supplies, ultrasound machine, patient-reported outcome surveys.
- Methodology:
- Study Design: Randomized controlled trial. Participants are randomized to a treatment group (using tension-offloading dressing on injection sites) or a control group (standard care).
- Intervention: The dressing is applied to active injection sites according to manufacturer instructions and left in place for the recommended duration, creating a compressive, tension-reducing force [20].
- Outcome Measures:
- Primary: Change in subcutaneous tissue thickness and echogenicity as measured by ultrasound at baseline, 3, 6, and 12 months.
- Secondary: Intra-patient variability in glycemic control (standard deviation of blood glucose), total daily insulin dose, and incidence of hypoglycemic events [20].
- Exploratory: Patient-reported satisfaction and skin comfort.
Signaling Pathways and Workflow Visualizations
Pathways of Injection Site Complications
Intervention Trial Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Injection Site Research
| Item | Function/Justification |
|---|---|
| High-Frequency Linear Ultrasound | Provides objective, quantitative measurement of subcutaneous tissue thickness and echogenicity for identifying and monitoring lipohypertrophy [73]. |
| 4mm Pen Needles | The current standard for subcutaneous insulin delivery in clinical research, minimizing pain and the risk of intramuscular injection, thus reducing a key confounding variable [11]. |
| Tension-Offloading Dressings | An investigational device (e.g., embrace) to test the hypothesis that modulating mechanical forces can prevent fibrosis and lipohypertrophy [20]. |
| Continuous Glucose Monitoring (CGM) | Essential for capturing the high-resolution data on glycemic variability (e.g., Standard Deviation) that is a key consequence of erratic insulin absorption from LH [73]. |
| Structured Patient Journals/Apps | Digital or paper-based tools for participants to log injection sites, doses, and hypoglycemic events, crucial for correlating technique with outcomes [9]. |
| Histology Stains (e.g., Masson's Trichrome, H&E) | For pre-clinical studies, these stains allow visualization of collagen deposition (fibrosis) and adipocyte morphology in tissue sections from biopsy or animal models [20]. |
Evaluating Intervention Efficacy and Comparative Outcomes in Lipohypertrophy Management
Experimental Protocols & Methodologies
Core Quasi-Experimental Design for Site Rotation Intervention
A pretest-posttest control group design is effective for evaluating the impact of structured injection site rotation on technique scores and clinical outcomes [53].
- Participant Allocation: Participants are divided into a study group (receiving the structured intervention) and a control group (continuing usual practice). A sample size of 30 per group has been utilized previously [53].
- Intervention Protocol: The study group is trained on a systematic, anti-clockwise site rotation technique within a defined injection area (e.g., the abdomen). The methodology emphasizes moving to a new injection site with each administration, ensuring a distance of at least 1 cm from the previous injection spot [51] [11].
- Data Collection Points: Lipohypertrophy (LH) incidence and grade, along with glycemic control markers (e.g., HbA1c, fasting blood glucose), are assessed at baseline and again after a 6-month intervention period [53].
Qualitative Investigation of Implementation Barriers
In-depth interviews are key to understanding the underlying reasons for poor injection techniques.
- Participant Selection: Purposive sampling of patients with diabetes who have confirmed LH, ideally identified via ultrasound examination for higher sensitivity [2].
- Data Collection: Conduct face-to-face, semi-structured interviews in a quiet setting until thematic saturation is achieved. An interview guide should explore knowledge, daily practices, and perceived barriers related to injection technique [2].
- Data Analysis: Employ qualitative content analysis or thematic analysis. Transcripts are coded, and codes are grouped into themes and subthemes that characterize the major barriers, such as knowledge gaps and motivational issues [2].
Data Presentation
Identified Barriers to Proper Injection Technique
Qualitative analysis of patient interviews reveals a framework of barriers that impede proper technique [2].
Table 1: Primary Themes and Subthemes of Injection Technique Barriers
| Major Theme | Subtheme | Characteristic Patient Statement |
|---|---|---|
| Lack of Knowledge | Insufficient health education | "The HCPs asked me to rotate the injection site, but they did not say how to do it clearly." [2] |
| Forgetfulness | (Implied through thematic analysis) [2] | |
| Misconceptions | (Implied through thematic analysis) [2] | |
| Limited Feasibility | Limitations in site rotation | (Identified as a key theme) [2] |
| Financial pressures in needle replacement | (Identified as a key theme) [2] | |
| Failure to self-monitor flat LH | (Identified as a key theme) [2] | |
| Low Motivation | Low perceived severity | (Identified as a key theme) [2] |
| Low perceived susceptibility | (Identified as a key theme) [2] |
Quantitative Outcomes of Site Rotation Intervention
Structured intervention shows significant positive effects on clinical outcomes.
Table 2: Pre-Post Intervention Clinical Outcomes
| Assessment Metric | Pre-Intervention (Baseline) | Post-Intervention (6-Month) | Key Findings |
|---|---|---|---|
| Lipohypertrophy (LH) Incidence | High prevalence in study and control groups | Significant reduction in study group | A marked reduction in the incidence and grade of LH was noted in the study group applying anti-clockwise rotation [53]. |
| Glycemic Control | Suboptimal / Variable | Improved in study group | Improved glycemic control was observed in the study group, indicating the clinical significance of proper rotation [53]. |
Visualization of Workflows
Research Evaluation Workflow
Injection Site Rotation Protocol
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Injection Technique Research
| Item | Function in Research Context |
|---|---|
| High-Frequency Ultrasound | A superior diagnostic modality for precise identification of non-palpable (flat) lipohypertrophy lesions and for measuring subcutaneous tissue thickness [2] [51]. |
| 4 mm Pen Needles | The recommended shortest needle for subcutaneous insulin delivery; reduces risk of intramuscular injection and pain, a key variable in device studies [51] [11]. |
| Lipohypertrophy Assessment Sheet | A standardized data collection instrument for consistently grading the presence and severity of LH nodules across study timepoints [53]. |
| Semi-Structured Interview Guide | A qualitative research tool to comprehensively explore patients' knowledge, practices, and barriers regarding injection technique, ensuring consistent data collection [2]. |
Troubleshooting Guides & FAQs
For Research Participants and Clinical Subjects
Q: Why do participants in my study keep injecting into lipohypertrophic areas even after education? A: This is a common challenge driven by three primary barriers. First, patients often have low perceived severity and susceptibility, meaning they don't believe the complications are serious or will happen to them [2]. Second, forgetfulness and a lack of automated habit play a major role [2]. Finally, injections into LH sites can be less painful than injections into healthy tissue, creating a perverse incentive for the patient [51].
Q: What is the most effective way to teach the systematic site rotation method? A: Effective education involves clear, visual, and simple instructions. Teach participants the "anti-clockwise" rotation pattern within a defined zone (like an abdominal quadrant), ensuring each new injection is at least 1 cm (about half the width of a thumb) from the last site [51] [53]. Use body charts and diagrams for demonstration and provide them as take-home aids to guide daily practice.
Q: How can we mitigate financial pressures that lead to needle reuse? A: While researchers cannot always control costs, they can emphasize that needle reuse is a false economy. It leads to dull, bent, and contaminated needles, increasing pain, skin trauma, and the risk of LH, which in turn degrades glycemic control and increases overall diabetes management costs [51] [11]. Counsel participants that needles are designed for single use only.
For Experimental Design and Data Analysis
Q: Our pre-post intervention data shows improved technique scores, but no significant change in HbA1c. Does this mean the intervention failed? A: Not necessarily. Glycemic control is multifactorial. An intervention can be successful by achieving important secondary endpoints, such as a reduced incidence or grade of lipohypertrophy, decreased daily insulin dose requirements, or lower glycemic variability (reduced hypoglycemia events) [51] [53]. LH itself impairs insulin absorption, so its reduction is a critical outcome that precedes long-term HbA1c changes.
Q: What is the most reliable method for detecting lipohypertrophy in a clinical trial? A: While visual inspection and palpation are common, they have limited effectiveness, especially for non-palpable, flat LH lesions [2]. Ultrasound examination emerges as a superior diagnostic modality with enhanced sensitivity and specificity, allowing for precise and objective measurement of lesion size and subcutaneous tissue structure [2] [51].
Q: How can we prevent mix-ups between different insulin pens in a device study? A: Implement strategies that enhance differentiation. Research shows that using pens with distinct full body colors, rather than just label differences, significantly reduces error rates [74]. Additional strategies include adding tactile markers (like rubber bands) to one pen and training participants to check the label before every single injection [74] [36].
FAQs: Glycemic Outcomes and Injection Site Research
Q1: What is the established clinical link between lipohypertrophy (LH) and impaired glycemic outcomes?
A1: Injecting insulin into sites of lipohypertrophy (LH), a common complication of improper injection site rotation, significantly impairs insulin absorption. This leads to marked and unpredictable hyperglycemia, resulting in a continuous deterioration of blood glucose levels. To compensate, the total daily insulin dose is often increased. If these larger doses are then inadvertently injected into normal tissue, the risk of hypoglycemia rises substantially, leading to high glycemic variability and poor overall control [2].
Q2: What are the primary barriers to effective insulin injection site rotation identified in patient studies?
A2: Qualitative research has systematically identified three major thematic barriers [2]:
- Lack of Knowledge: This includes insufficient health education from providers, forgetfulness, and misconceptions about the importance of rotation.
- Limited Feasibility: Patients report practical difficulties with site rotation, financial pressures that lead to reusing needles more than recommended, and an inability to self-monitor for "flat" LH that is not easily visible or palpable.
- Low Motivation: Patients often demonstrate a low perceived severity of LH consequences and a low perceived susceptibility to developing the condition.
Q3: How do Automated Insulin Delivery (AID) systems improve HbA1c and Time-in-Range (TIR) in clinical trials?
A3: AID systems, which combine continuous glucose monitoring (CGM) with insulin pumps that automate insulin delivery, have shown significant benefits in randomized controlled trials (RCTs). For example, the RADIANT study in type 1 diabetes (T1D) showed that transitioning from multiple daily injections (MDI) to the Omnipod 5 AID system reduced HbA1c from 8.1% to 7.2% and increased TIR from 39% to 65% (an improvement of 26 percentage points, or over 6 hours per day) over 13 weeks [75]. Similarly, the 2IQP study in insulin-treated type 2 diabetes (T2D) found that an AID system outperformed standard therapy, increasing TIR to 64% compared to 52% in the control group [75].
Q4: What glycemic improvements can be expected from Continuous Glucose Monitoring (CGM) use in both type 1 and type 2 diabetes?
A4: CGM acts as a foundational technology for glycemic management, providing real-time feedback that guides therapy adjustments. Clinical evidence and real-world data across diabetes types and treatment regimens consistently show [76] [77]:
- HbA1c Reductions: CGM use is associated with HbA1c reductions ranging from 0.25% to 3.0%, with typical between-group differences of 0.3% to 0.6% in RCTs.
- Time-in-Range Improvements: TIR can improve by 15% to 34%, equivalent to several more hours per day in the target glucose range.
- Hypoglycemia Reduction: CGM significantly reduces time spent in hypoglycemia, with some studies reporting over a 70% reduction in hypoglycemic events [76].
Quantitative Data on Glycemic Outcomes
The following tables summarize key glycemic outcome data from recent studies and guidelines.
Table 1: Glycemic Outcomes from Continuous Glucose Monitoring (CGM) Studies
| Study Population | Treatment Regimen | Key Glycemic Outcome (CGM vs. Control) | Study Details |
|---|---|---|---|
| Adults with T1D [77] | Multiple Daily Injections (MDI) | HbA1c reduction: -0.6% (7.7% vs. 8.2%) | RCT, 24 weeks |
| Adults with T2D [77] | Multiple Daily Injections (MDI) | HbA1c reduction: -0.3% (7.7% vs. 8.0%) | RCT, 6 months |
| Adults with T2D [77] | Basal Insulin Only | HbA1c reduction: -0.4% (8.0% vs. 8.4%) | RCT, 8 months |
| Adults with T2D [77] | Non-Insulin (OHA) | HbA1c reduction: -0.68% | RCT, 3 months |
| Large Retrospective Cohort (T1D & T2D) [77] | Any | HbA1c reduction: -0.4% (7.76% vs. 8.19%) | 12-month observation |
Table 2: Glycemic Outcomes from Automated Insulin Delivery (AID) System Trials
| Study (Population) | System | Baseline | Post-Intervention | Change |
|---|---|---|---|---|
| RADIANT (T1D) [75] | Omnipod 5 AID | HbA1c: 8.1%TIR: 39% | HbA1c: 7.2%TIR: 65% | HbA1c: -0.9%TIR: +26% |
| 2IQP Study (T2D) [75] | Control-IQ AID | HbA1c: Not SpecifiedTIR: Baseline not specified | HbA1c: Results shown as changeTIR: 64% (Control: 52%) | HbA1c: -0.9% (vs. -0.3% control)TIR: +12% (vs. control) |
| SECURE-T2D (T2D) [78] | Omnipod 5 AID | TIR: 45%HbA1c: 8.1%-8.4% | TIR: 66%HbA1c: 7.3%-7.5% | TIR: +21%HbA1c: -0.7% to -0.9% |
Experimental Protocols for Key Cited Studies
Protocol 1: Assessing Barriers to Injection Site Rotation (Qualitative Study) [2]
- Objective: To comprehensively identify barriers to preventing insulin injection-associated lipohypertrophy (LH) in patients with diabetes.
- Design: A qualitative descriptive design using face-to-face, semi-structured interviews.
- Participants: 17 individuals with type 2 diabetes and confirmed LH via ultrasound examination.
- Data Collection:
- Participants were recruited via purposive sampling from a hospital endocrinology department.
- Interviews were conducted in a quiet, separate room, audio-recorded, and ranged from 20 to 60 minutes.
- A semi-structured interview guide was used to explore knowledge, practices, and perceptions regarding insulin injections and LH.
- Verbatim transcription was completed within 24 hours, and participants were given summaries for factual verification.
- Data Analysis: Thematic analysis was performed following Braun and Clarke's methodology. This involved familiarization with data, generating initial codes, searching for themes, reviewing themes, defining themes, and producing the report. Data management was supported by NVivo 8 software, and analysis continued until data saturation was achieved.
Protocol 2: Randomized Controlled Trial (RCT) of AID vs. MDI in T1D (RADIANT Study) [75]
- Objective: To evaluate the efficacy of the Omnipod 5 Automated Insulin Delivery (AID) system compared to Multiple Daily Injections (MDI) in children and adults with type 1 diabetes.
- Design: A multinational, randomized, controlled, parallel-group trial.
- Participants: 188 participants (aged 4-70 years) with T1D for ≥1 year and screening HbA1c between 7.5% and 11%.
- Intervention & Control:
- Run-in Period: All participants used MDI with a FreeStyle Libre 2 CGM for a 2-week data collection period.
- Randomization: Participants were randomly assigned in a 2:1 ratio to either the intervention group (Omnipod 5 AID system) or the control group (continued MDI and CGM).
- Study Duration: The intervention period lasted for 13 weeks.
- Primary Outcome: Change in HbA1c from baseline to 13 weeks.
- Secondary Outcomes: CGM-based metrics including Time-in-Range (TIR) (70-180 mg/dL), time in hypoglycemia, and patient-reported outcomes.
Visualizing the Impact of Injection Practices on Glycemic Outcomes
The following diagram illustrates the logical pathway and consequences of improper insulin injection site rotation, and how technology interventions can help improve outcomes.
Impact of Injection Practices and Technology on Glycemic Outcomes
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Diabetes Injection Site and Glycemia Research
| Research Tool / Reagent | Function / Application in Research |
|---|---|
| High-Frequency Ultrasound | Precisely identifies and characterizes lipohypertrophy (LH) lesions, including non-palpable "flat" LH, serving as an objective outcome measure in intervention studies [2]. |
| Continuous Glucose Monitor (CGM) | The core tool for measuring glycemic outcomes. It provides high-resolution data on glucose Time-in-Range (TIR), variability, and hypoglycemia, essential for evaluating the impact of injection techniques or new therapies [76] [77]. |
| Automated Insulin Delivery (AID) System | An integrated technology used as an intervention in clinical trials to assess its superiority over standard injection therapy in achieving glycemic targets, particularly in populations with suboptimal control [78] [75]. |
| Validated Patient Surveys & Interview Guides | Qualitative and quantitative tools to assess patient-reported barriers, knowledge, and adherence related to injection site rotation, providing context for clinical findings [2] [41]. |
| HbA1c Point-of-Care Analyzer | Provides standardized, central lab-quality measurement of glycosylated hemoglobin (HbA1c), the key metric for long-term glycemic control in clinical trials [77] [75]. |
This technical support center provides resources for researchers and scientists investigating lipodystrophy, a common complication of subcutaneous insulin administration characterized by adipose tissue abnormalities (lipohypertrophy) or atrophy (lipoatrophy). The predictable absorption of insulin is significantly impaired when injected into these affected sites, leading to erratic glycemic control and compromising research outcomes on insulin pharmacokinetics and pharmacodynamics [79].
Proper injection technique, including systematic site rotation, is a critical intervention for preventing these complications. This guide offers comparative data on educational methodologies and detailed protocols to support the standardization of experimental procedures in preclinical and clinical research settings.
Frequently Asked Questions (FAQs) for Experimental Design
Q1: What are the primary quantitative outcomes used to measure the effectiveness of educational interventions on injection technique?
The table below summarizes key metrics from comparative studies, highlighting the enhanced performance of a pharmacist-led model.
Table 1: Key Quantitative Outcomes from Comparative Studies
| Outcome Measure | Standard Education Model | Pharmacist-Led Education Model | Study Details |
|---|---|---|---|
| HbA1c Reduction | -0.79% ± 0.24 [80] | -1.19% ± 0.10 [80] | Randomized Controlled Trial (RCT): 139 patients [80] |
| Injection Technique (IT) Score | Not specified (Improvement observed) [80] | +2.02 points vs. control [80] | RCT; 17-point checklist [80] |
| Medication Adherence Score | Not specified (Improvement observed) [80] | +1.48 points vs. control [80] | RCT; Measured via Medication Compliance Questionnaire (MCQ) [80] |
| Patient Perception (ITAS Score)* | Worsened (+0.55) [80] | Improved (-1.44) [80] | RCT; Lower ITAS score indicates more positive perception [80] |
| Lipohypertrophy (LH) Reduction | Supported by systematic review [81] | Supported by systematic review [81] | Systematic review of 11 studies [81] |
*ITAS: Insulin Treatment Appraisal Scale.
Q2: What are the core mechanistic barriers that prevent effective injection site rotation in patients?
A qualitative study identified three major thematic barriers, which should be considered as confounding variables in research protocols [2]:
- Lack of Knowledge: Includes insufficient health education, forgetfulness, and misconceptions about the need for rotation.
- Limited Feasibility: Encompasses physical limitations preventing self-rotation, financial pressure to reuse needles, and failure to self-monitor for flat lipohypertrophy.
- Low Motivation: Stemming from low perceived severity of lipohypertrophy and low perceived susceptibility to developing it [2].
Q3: How does improper injection technique confound research on insulin dosing and efficacy?
Injecting into lipohypertrophic tissue significantly alters insulin pharmacokinetics, leading to marked hyperglycemia [2]. Conversely, injecting a large dose intended for a lipohypertrophic site into normal tissue substantially increases the risk of hypoglycemia [2]. This variability in absorption can lead to significant noise and bias in studies measuring glycemic control, insulin bioavailability, and optimal dosing.
Troubleshooting Guides for Common Research Challenges
Problem: High Variability in Glycemic Response Data
- Potential Cause: Uncontrolled for injection technique and site selection in study participants.
- Solution: Implement a standardized injection technique training and certification protocol for all study participants. Regularly palpate injection sites to ensure avoidance of lipohypertrophic areas [79] [39].
Problem: Participant Non-Adherence to Site Rotation Protocol
- Potential Cause: Barriers identified in FAQ #2, such as lack of knowledge or physical limitations.
- Solution: Incorporate structured, repeated education sessions led by a clinical pharmacist. Provide participants with clear, visual guides for site rotation and supply an adequate quantity of needles to eliminate reuse [80] [39].
Experimental Protocols for Intervention Studies
Protocol: Evaluating the Impact of a Pharmacist-Led Educational Intervention
This methodology is adapted from a randomized controlled trial [80].
- Objective: To determine the effect of monthly, structured pharmacist-led re-education on insulin injection technique, lipohypertrophy incidence, and glycemic control compared to standard care.
- Population: Individuals with type 2 diabetes on insulin therapy with suboptimal glycemic control (e.g., HbA1c ≥ 8%) and/or unsatisfactory injection technique.
- Randomization: Assign participants to either Control or Intervention group using computer-generated sequences.
- Intervention Group:
- Schedule: Receive one-on-one counselling and injection technique re-education monthly for four months.
- Content: Based on a structured checklist (e.g., 17-point IT checklist) covering site rotation, needle reuse, lipohypertrophy inspection, and correct administration.
- Assessment: Injection sites should be palpated for lipohypertrophy by trained personnel at each visit [80].
- Control Group: Receive standard counselling at baseline and the fourth month only.
- Data Collection: Collect HbA1c, complete validated questionnaires (ITAS, MCQ), perform injection technique assessment, and conduct physical examination for lipohypertrophy at baseline and study end.
Signaling Pathways and Workflow Diagrams
The diagram below illustrates the proposed mechanism through which pharmacist-led education improves glycemic outcomes, by addressing key barriers and promoting proper injection technique.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for Injection Technique Research
| Item | Function/Application in Research |
|---|---|
| High-Frequency Ultrasound | A superior diagnostic modality for precise identification of non-palpable (flat) lipohypertrophy lesions and measuring their size in clinical studies [2]. |
| Validated Questionnaires | Tools like the Insulin Treatment Appraisal Scale (ITAS) and Medication Compliance Questionnaire (MCQ) to quantitatively measure patient perception and adherence as secondary outcomes [80]. |
| Structured Injection Technique (IT) Checklist | A standardized tool (e.g., 17-point checklist) to ensure consistent assessment and training of proper injection technique across all study participants and personnel [80]. |
| 4-6 mm Pen Needles | The recommended needle length for subcutaneous administration in most adults, minimizing the risk of unintentional intramuscular injection, a key variable in insulin absorption studies [39]. |
Cost-Benefit Analysis of Structured Training Programs and Routine Ultrasound Screening
Frequently Asked Questions (FAQs): Technical Troubleshooting
FAQ 1: What are the most common experimental confounders when quantifying the economic impact of injection site complications, and how can they be controlled?
- Confounder: Inconsistent detection and classification of lipohypertrophy (LH) lesions. Studies report widely varying LH prevalence rates, from 14.5% to over 60%, often due to non-standardized palpation techniques [20] [82] [37]. This variability undermines the reliability of cost calculations.
- Control Method: Implement a standardized, documented palpation protocol across all study personnel. This should include a specific sequence for manual skin search at all potential injection sites (e.g., abdomen, thighs, arms) to identify "thickened, rubbery" tissue swellings [37]. Supplement with high-frequency ultrasound (HFUS) for objective, quantitative measurement of subcutaneous tissue density and structure to validate palpation findings [37].
FAQ 2: Our cost-benefit model for a structured training program shows high sensitivity to the "reduction in daily insulin dose" parameter. How can this reduction be accurately measured in a clinical trial?
- Issue: Insulin dose requirements are influenced by multiple factors (diet, exercise, stress), making it difficult to isolate the effect of improved injection technique.
- Solution: Design a controlled trial where the primary endpoint is the change in total daily insulin dose (TDD) after patients with confirmed LH are retrained to inject exclusively into healthy tissue. To isolate the variable, aim to keep other factors like diet and exercise stable during the observation period. Prior research indicates that TDD can be reduced by an average of 36% (approximately 15 International Units per day) after correcting injection technique, providing a benchmark for your model [20] [82].
FAQ 3: When designing a cost-effectiveness analysis for routine ultrasound screening of injection sites, what is the most appropriate primary economic endpoint?
- Endpoint Recommendation: The primary endpoint should be the cost per quality-adjusted life year (QALY) gained or the incremental cost-effectiveness ratio (ICER). This is the standard for health economic evaluations and allows for comparison with other healthcare interventions [83].
- Justification: A successful intervention reduces LH, leading to better glycemic control, fewer diabetic complications (e.g., hypoglycemia, hyperglycemia), and improved quality of life. The QALY captures these clinical and patient-centered benefits in a single metric. A secondary endpoint could be a simple cost-benefit ratio, calculating the monetary value of insulin savings and averted complications against the cost of the screening and training program [20].
Experimental Protocols for Key Investigations
Protocol for Clinical Identification and Documentation of Lipohypertrophy
Objective: To standardize the detection, classification, and documentation of injection site lipohypertrophy in a study cohort.
Materials:
- Examination table
- Disposable gloves
- Skin marker (surgical, non-permanent)
- Digital camera
- Data collection form (including body map diagram)
- High-frequency ultrasound system (e.g., 18-20 MHz transducer) - Optional, for validation [37]
Methodology:
- Patient Preparation: The patient should disrobe sufficiently to expose all potential injection sites (abdomen, thighs, upper arms, buttocks). Ensure adequate lighting.
- Systematic Palpation:
- Visually inspect all areas for visible swellings, dimples, or discoloration.
- Using the pads of the fingers, palpate each site systematically. Apply light, then firm pressure in a circular motion.
- Identify LH as a thickened, "rubbery," or firm swelling within the subcutaneous tissue [37].
- Documentation:
- Mapping: On a body map diagram, outline the borders of any identified LH lesion.
- Characteristics: Record the lesion's consistency (soft/firm), approximate diameter in centimeters, and tenderness upon palpation.
- Photography: Take standardized photographs of the lesions with a scale and patient identifier.
- Ultrasound Confirmation (Optional): Use HFUS to measure the exact depth and echogenicity of the lesion, providing an objective baseline for monitoring change [37].
Protocol for Cost-Benefit Analysis of a Structured Injection Training Program
Objective: To evaluate the economic return on investment for implementing a structured patient education program on correct insulin injection technique.
Framework: This analysis should be conducted from a healthcare system or societal perspective [84].
Data Collection and Calculation Steps:
Table: Key Parameters for Cost-Benefit Analysis of a Training Program
| Parameter | Description | Data Source |
|---|---|---|
| Cost of Program (C) | Sum of trainer time, educational materials, facility costs, and patient time. | Program budgeting and micro-costing. |
| Reduction in TDD | The mean percentage and absolute reduction in total daily insulin dose post-training. | Clinical trial data (see FAQ 2) [20] [82]. |
| Annual Insulin Cost per IU | The average cost per International Unit of insulin. | Pharmacy acquisition costs or national drug pricing databases. |
| Reduction in Hypoglycemia Events | The frequency of severe hypoglycemic events requiring medical assistance before and after training. | Patient diaries, electronic health records. |
| Cost per Hypoglycemia Event | The average cost of treating a severe hypoglycemia event (e.g., ambulance, ER visit, hospitalization). | Published literature or hospital billing data. |
Calculation:
- Annual Benefit from Insulin Savings (B_insulin):
- (Mean Reduction in TDD in IU) × (365 days) × (Cost per IU)
- Annual Benefit from Averted Complications (B_complications):
- (Reduction in hypoglycemia events per year) × (Cost per event)
- Total Annual Benefit (Btotal): Binsulin + B_complications
- Net Annual Benefit: B_total - C (if C is an annualized cost)
- Benefit-Cost Ratio (BCR): B_total / C. A BCR > 1 indicates the program is economically beneficial.
Table: Economic and Clinical Impact of Injection Site Complications and Screening Programs
| Metric | Value or Range | Context / Source |
|---|---|---|
| Prevalence of Lipohypertrophy (LH) | 14.5% to >60% of insulin-treated patients [20] [82] [37] | Highlights the scale of the problem and potential variability in detection. |
| Excess Insulin Use due to LH | ~36% increase in Total Daily Dose (TDD) [20] [82] | A key driver for cost calculations in a cost-benefit model. |
| Estimated Annual U.S. Cost of Unnecessary Insulin | > $1 Billion USD [20] | Illustrates the massive economic burden at a population level. |
| Cost-Effectiveness Threshold (for reference) | EUR 3,000 - 8,000 per QALY [83] | Benchmark for cost-effective healthcare interventions (e.g., mammography screening). A similar threshold can be applied to ultrasound screening. |
Signaling Pathways and Experimental Workflows
Diagram 1: Pathogenesis of Injection Site Complications
Diagram 2: Clinical Trial Workflow for Training Program Evaluation
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Investigating Injection Site Pathophysiology
| Item / Reagent | Function in Research |
|---|---|
| High-Frequency Ultrasound (HFUS) | Provides non-invasive, objective quantification of subcutaneous tissue structure, allowing for precise measurement of LH lesion size and density changes over time [37]. |
| Tension-Offloading Dressings | An investigational device (e.g., embrace device) used to apply compressive force at injection sites. Based on mechanobiology principles, it is theorized to reduce mechanical stress, potentially preventing both fibrosis and lipohypertrophy in preclinical and clinical models [20]. |
| Standardized Palpation Protocol | A critical low-tech "tool" comprising a defined checklist and body map. It ensures consistent, reproducible identification and documentation of LH lesions across different clinicians in a multi-center study, reducing detection bias [37]. |
| Short Pen Needles (4mm/32G or 3.5mm/34G) | The standard needle recommended for correct subcutaneous injection. Used in interventional studies to ensure that technique improvements are not confounded by inappropriate needle length [82]. |
| Patient Injection Diaries | Used to collect real-world data on injection habits, needle reuse frequency, and site rotation adherence, which are key behavioral variables correlated with LH development [82] [37]. |
Lipohypertrophy (LH), a localized thickening of fatty tissue at insulin injection sites, represents a significant and prevalent complication of insulin therapy, with reported prevalence rates of up to 64% in insulin-injecting patients with diabetes [73]. This condition, along with fibrotic scarring, arises from repeated minor tissue trauma and the growth-promoting properties of insulin, leading to both pathological skin changes and erratic insulin absorption [20] [85]. For researchers and drug development professionals, LH is not merely a patient compliance issue; it is a complex biomechanical and biochemical response that undermines the efficacy and predictability of subcutaneous insulin delivery. The associated increased intra-patient variability in insulin absorption and effect complicates clinical trials and the assessment of new insulin formulations, as injection site health becomes a critical, and often unmeasured, confounding variable [20]. The financial implications are equally staggering, with one study noting a 15 IU/day average increase in insulin dose for patients with LH, translating to over €122 million in annual costs in Spain alone, and similarly, over $1 billion in unnecessary insulin costs annually in the United States [20] [73]. Sustaining proper injection technique, specifically consistent site rotation, is therefore not just a matter of patient care but a fundamental prerequisite for reliable pharmacological research and development in diabetes therapeutics.
Quantitative Evidence: The Scale and Impact of the Problem
The table below summarizes key quantitative findings from the literature, highlighting the high prevalence of lipohypertrophy and its significant clinical and economic consequences.
Table 1: Quantitative Evidence on Lipohypertrophy Prevalence and Impact
| Metric | Finding | Source/Study Context |
|---|---|---|
| LH Prevalence | 64.4% of insulin-injecting patients (n=430) [73] | Multicenter study examining injection sites [73] |
| LH & Site Rotation | 98% of patients with LH did not rotate sites or rotated incorrectly [73] | Association between non-rotation and LH presence [73] |
| Unexplained Hypoglycemia | 39.1% in patients with LH vs. 5.9% in those without [73] | Link between LH and glycemic variability [73] |
| Glycemic Variability | 49.1% in patients with LH vs. 6.5% in those without [73] | Patient reports of erratic glucose levels [73] |
| Increased Insulin Dose | 15 IU/day average increase (56 vs. 41 IU/day) [20] [73] | Direct result of impaired absorption at LH sites [20] [73] |
| Subclinical LH | 19.9% of patients (n=316) after one year of insulin use [86] | LH detectable only via ultrasound, not palpation [86] |
The data underscores that lipohypertrophy is the norm rather than the exception among long-term insulin users, with faulty injection technique being a primary driver. The high rate of subclinical LH is particularly relevant for researchers, as it indicates that even visually normal injection sites may have underlying tissue pathology that could interfere with the pharmacokinetic (PK) and pharmacodynamic (PD) profiles of experimental insulins.
Pathophysiology and Experimental Models
Understanding the mechanistic pathways leading to LH and fibrosis is essential for developing preventive strategies and accurate experimental models.
Key Pathological Pathways
The development of injection site complications is driven by two interrelated processes:
- Fibrosis: Repeated needle trauma induces a chronic inflammatory response and mechanical tension on the skin. Fibroblasts, sensitive to these mechanical forces, are stimulated to produce excess extracellular matrix, leading to the accumulation of stiff, dense scar tissue [20].
- Lipohypertrophy: Insulin itself acts as a local growth factor for adipocytes, leading to both hypertrophy (enlargement) and hyperplasia (proliferation) of fat cells. These lipohypertrophic fat cells can be up to twice the size of normal fat cells [20] [9].
The diagram below illustrates the logical sequence of events from repeated injection trauma to the two primary complications.
Diagram 1: Pathogenesis of injection site complications. The pathway shows how repeated injections trigger two distinct but concurrent pathological processes leading to fibrosis and lipohypertrophy.
The Role of Mechanical Forces
Emerging research points to the critical role of mechanical forces in modulating these pathways. Increased skin tension is known to promote fibrosis, while compressive force has been shown to inhibit adipogenesis (the formation of fat cells) in vitro [20]. This biomechanical insight provides a novel target for interventions, suggesting that modulating forces at the injection site could simultaneously address both fibrotic and lipohypertrophic changes.
The Scientist's Toolkit: Key Research Reagents and Methodologies
To systematically study injection site complications and adherence, researchers require a specific toolkit for assessment, intervention, and measurement.
Table 2: Essential Research Tools for Studying Injection Site Complications
| Tool/Reagent | Function/Explanation in Research |
|---|---|
| High-Frequency Ultrasound | Gold-standard for objective identification and measurement of subclinical lipohypertrophy; provides an "echo signature" of affected tissue that palpation misses [73] [85]. |
| Standardized Palpation Protocol | A systematic, documented method for physical examination of injection sites to ensure consistent identification of LH across different study raters and sites [85]. |
| Tension-Offloading Dressings | Investigational device (e.g., embrace) used to apply compressive force to injection sites; a biomechanical intervention to test the hypothesis that reducing tissue tension prevents fibrosis and LH [20]. |
| Glycemic Variability Metrics | Key outcome measures (e.g., standard deviation of glucose, coefficient of variation, Low/High Blood Glucose Index) to quantify the clinical impact of LH on insulin absorption erraticism [73]. |
| Structured Site Rotation Maps | Visual tools and educational protocols provided to study participants to standardize and track the "correct rotation" intervention arm in clinical trials [73] [17] [87]. |
| Needle Gauge/Length Variants | To investigate the relationship between needle physical properties (diameter, length) and the degree of tissue trauma, inflammation, and subsequent complication rates. |
Experimental Protocols for Adherence and Complication Research
For researchers designing studies to evaluate long-term adherence or test novel interventions, the following protocols provide a methodological foundation.
Protocol 1: Validating a Standardized Palpation and Ultrasound Assessment for LH
This protocol is designed to systematically identify and characterize LH in study participants.
- Patient History: Prior to physical examination, document the patient's injection habits via a detailed questionnaire. Key data points include: duration of insulin therapy, injection device (syringe/pen/pump), frequency of needle reuse, and self-reported site rotation practices [73].
- Visual Inspection: Under good lighting, examine all potential injection sites (abdomen, thighs, arms, buttocks) with the patient in both standing and sitting positions. Look for visible swellings, indentations, or skin discoloration [9] [17].
- Systematic Palpation:
- Use the pads of the fingers (not the tips) to gently palpate the entire injection area.
- Compare the texture and resilience of the tissue to adjacent non-injected areas and to contralateral body sites.
- Note any areas that feel firmer, harder, lumpy, rubbery, or thickened compared to normal tissue. Also, check for reduced sensation, as LH areas are often somewhat numb [9] [85].
- Measure and record the diameter of any identified lesions.
- Ultrasound Confirmation: Perform a high-frequency ultrasound scan (e.g., using a >15 MHz transducer) of all injection sites, including those that appeared normal on palpation. Measure the thickness of the subcutaneous fat layer and document any architectural disruptions or characteristic "echo signatures" of LH [73] [85].
- Data Correlation: Correlate the palpation and ultrasound findings with the patient's historical data on glycemic variability and unexplained hypoglycemic episodes.
Protocol 2: Testing a Biomechanical Intervention (Tension-Offloading)
This protocol outlines a clinical trial to evaluate a novel, mechanics-based approach to preventing injection site complications.
- Hypothesis: Application of a continuous, compressive, tension-offloading dressing to active insulin injection sites will reduce the incidence and severity of both fibrosis and lipohypertrophy by modulating mechanobiological pathways.
- Study Design: Randomized, controlled, within-subject trial. Each participant uses two designated abdominal injection areas for a 6-month period.
- Intervention Area: Insulin injections are performed through a tension-offloading dressing (e.g., embrace device), which is changed according to manufacturer instructions.
- Control Area: Insulin injections are performed using standard care, with routine site rotation within the designated area.
- Blinded Outcome Assessment:
- Primary Endpoint: Change in subcutaneous tissue thickness and architecture from baseline to 6 months, as measured by high-frequency ultrasound, comparing the intervention and control areas.
- Secondary Endpoints:
- Difference in insulin dose requirement (IU/kg) between areas to maintain equivalent glycemic control.
- Intra-patient variability in glucose levels (measured by continuous glucose monitor) linked to injections in each area.
- Histological assessment of tissue biomarkers for fibrosis and inflammation from optional biopsy samples at the end of the study.
- Mechanistic Analysis: In vitro models can be run in parallel, applying controlled compressive forces to adipocyte and fibroblast cell cultures to elucidate the molecular pathways involved (e.g., down-regulation of adipogenic genes) [20].
The workflow for this experimental approach is detailed below.
Diagram 2: Experimental workflow for testing a tension-offloading intervention. The within-subject design controls for inter-individual variation, allowing direct comparison of the intervention against standard care.
Troubleshooting Guides and FAQs for Research Implementation
Q1: In our clinical trial, participants' self-reported site rotation logs are often incomplete or inaccurate. How can we objectively monitor adherence to the injection site rotation protocol?
- A: Self-reporting is notoriously unreliable. Implement one or more of the following objective measures:
- Photographic Documentation: Regularly take standardized, high-resolution photos of injection areas (with participant consent) to track visual changes and infer rotation patterns.
- Structured Site Mapping: Provide participants with body maps and require them to mark every injection site. Combine this with regular (e.g., weekly) photo uploads of their marked map.
- Device Data Logs: For insulin pen users, some "smart" pens can log the time and dose of injections. While they don't track location, correlating injection frequency with site maps can improve accuracy.
- Ultrasound Surveillance: Schedule periodic ultrasounds of common injection sites to detect subclinical LH, which serves as an objective biological marker of poor rotation adherence [73] [86].
Q2: We are testing a new long-acting insulin analog. How can we determine if erratic PK/PD results in a participant are due to the drug's properties or an underlying injection site complication?
- A: Proactively screen for and monitor injection site health to eliminate this confounder.
- Baseline Screening: Enroll participants only after a thorough palpation and ultrasound examination of all intended injection sites confirms the absence of significant LH or fibrosis.
- Designated Injection Areas: In the trial protocol, strictly define and document the injection areas to be used. Prohibit injections outside these areas.
- Continuous Monitoring: Incorporate brief palpation checks at every study visit. If erratic PK/PD is observed, immediately perform a targeted ultrasound of the injection sites used. If pathology is found, the data point may need to be excluded and the participant re-trained on injection technique [20] [85].
Q3: Our in vitro models of fibrosis and adipogenesis are not fully recapitulating the complex tissue environment of a chronic injection site. What are more physiologically relevant approaches?
- A: Move towards more advanced 3D and mechano-biological models.
- 3D Bioprinted Tissues: Use bioprinted constructs containing human fibroblasts and adipocytes in a collagenous matrix to simulate the subcutaneous layer.
- Application of Cyclic Strain: Utilize bioreactors that apply controlled, cyclic mechanical strain to these 3D tissues, mimicking the repeated stress of injections, and observe fibrotic responses [20].
- Co-culture Models: Establish co-cultures of adipocytes and fibroblasts to study the paracrine signaling between these cell types in response to both insulin and mechanical stimulation.
- Micro-Needle Arrays: Use micro-needle arrays to deliver insulin in a more physiologically relevant manner to these advanced tissue models, simulating the actual delivery method.
Sustaining proper insulin injection technique is a critical, yet often overlooked, variable in both clinical management and pharmaceutical research. The high prevalence of lipohypertrophy represents a significant failure in long-term patient adherence and a major source of noise and bias in clinical trials for insulin therapies. The research community must move beyond merely educating patients and begin developing and validating objective monitoring tools, novel biomechanical interventions, and more physiologically relevant experimental models. Integrating standardized injection site assessments into the core protocol of every insulin trial is no longer optional but essential for generating clean, interpretable, and generalizable data. The future of optimizing insulin therapy lies not only in designing better molecules but also in ensuring the integrity of the delivery platform—the subcutaneous tissue itself.
FAQs: Novel Formulations and Lipodystrophy Risk
Q1: How do novel insulin formulations fundamentally aim to reduce the risk of lipohypertrophy (LH)? Novel formulations target the root causes of LH, which include the localized anabolic effect of insulin on adipocytes and tissue trauma from frequent injections. Key strategies include reducing injection frequency and improving bioavailability. For instance, once-weekly basal insulins like insulin icodec decrease the number of subcutaneous injections from 365 to 52 per year, significantly reducing localized tissue trauma and insulin exposure at a single site [88]. Concurrently, ultra-rapid-acting insulins are designed for more complete and predictable absorption, minimizing the prolonged exposure of local tissue to high insulin concentrations that can stimulate adipocyte growth [89].
Q2: What are the critical pharmacokinetic parameters to monitor when evaluating new insulin formulations for their potential to cause LH? Researchers should focus on parameters that indicate the duration and consistency of insulin presence at the injection site. The table below summarizes key parameters:
Table: Key Pharmacokinetic Parameters for LH Risk Assessment
| Parameter | Description | Significance for LH Risk |
|---|---|---|
| Half-life | Time for insulin concentration to reduce by half. | A very long half-life (e.g., 196 hours for icodec) reduces injection frequency [88]. |
| Time to Steady State | Number of doses required to achieve stable plasma concentration. | Icodec requires 3-4 weekly doses; unstable levels may prompt site repetition [88]. |
| Day-to-Day Variability | Fluctuation in glucose-lowering effect between doses. | High variability (e.g., with some daily insulins) is linked to poor glycemic control and potentially injurious injection habits [89]. |
Q3: Which emerging delivery technologies show promise for completely bypassing subcutaneous injection site complications? Several advanced technologies aim to eliminate subcutaneous complications:
- Encapsulated Cell Therapies: Devices like the O2Line platform encapsulate insulin-producing cells, protecting them from immune rejection and providing continuous, physiologic insulin delivery, thereby eliminating the need for exogenous insulin injections [90].
- Implantable Emergency Drug Reservoirs: These devices, such as the MIT-developed glucagon implant, store a stable powdered drug subcutaneously for remote-activated release during hypoglycemic events. This technology demonstrates a paradigm for on-demand delivery that could be adapted for insulin [91].
- Glucose-Responsive "Smart Insulins": These formulations remain inactive in the circulation until activated by rising blood glucose levels. This system-wide approach removes the variable of subcutaneous absorption and the problem of localized insulin buildup [89].
- Inhaled Insulin (Afrezza): As a prandial insulin, Afrezza bypasses the subcutaneous space entirely, offering a non-injectable option for mealtime coverage and reducing the overall burden on injection sites [92].
Q4: What are the primary barriers to patient adherence to proper injection site rotation, and how can new technologies address them? Recent qualitative research identifies three major barrier themes [2]:
- Lack of Knowledge: Insufficient education from healthcare professionals on LH and proper rotation techniques.
- Limited Feasibility: Practical difficulties in site rotation, financial pressure to reuse needles, and an inability to self-monitor for flat LH lesions.
- Low Motivation: Low perceived severity and susceptibility to LH. New technologies address these by reducing the cognitive and physical burden. Smart pens with Bluetooth connectivity (e.g., tracking dose amount and timing) prevent "insulin stacking" and automate dose logging, while integrated digital platforms help patients and providers monitor rotation patterns [89]. Automated insulin delivery (AID) systems further automate insulin delivery, centralizing the infusion site and reducing the decision-making burden on the user [92].
Troubleshooting Guides for Pre-Clinical Research
Guide 1: Inconsistent Glycemic Response in Animal Models of Established Lipohypertrophy
Problem: High variability in blood glucose measurements following insulin administration in animal models with pre-existing LH, making efficacy data for new formulations unreliable.
Investigation & Resolution:
- Step 1: Verify Injection Site Accuracy. Utilize high-frequency ultrasound (e.g., >20 MHz) to precisely map LH lesion boundaries and ensure injections for the test formulation and control are administered within the same lesioned tissue. Palpation alone is insufficient for non-visible LH [3].
- Step 2: Standardize the LH Model. Ensure the model induction protocol is consistent regarding insulin type, injection volume, frequency, and site. Histological analysis (e.g., H&E staining) of a sample of lesions should confirm increased macro-adipocytes and fibrosis [3] [20].
- Step 3: Employ Continuous Glucose Monitoring (CGM). Use CGM to capture comprehensive glycemic data, including time-in-range and glycemic variability, which are more sensitive indicators of erratic absorption than single-point glucose measurements [3] [89].
Guide 2: Differentiating Formulation Effects from Device Effects
Problem: An observed reduction in LH in a pre-clinical study is ambiguous; it could be due to the novel insulin formulation or the new delivery device (e.g., a smart pen or jet injector).
Investigation & Resolution:
- Step 1: Design a Factorial Study. Implement a 2x2 study design that tests both the novel formulation and the standard of care using both the new device and a standard syringe/pen needle. This isolates the effect of the device from the effect of the formulation.
- Step 2: Quantitate Tissue Response. Use objective, quantifiable endpoints. Ultrasound can measure lesion volume, while histomorphometric analysis of tissue biopsies can quantify adipocyte size and fibrosis area [3] [20]. This provides more robust data than subjective visual scores.
- Step 3: Control for Known Confounders. Strictly control and document needle reuse policies, injection volumes, and site rotation schedules across all experimental groups to prevent these factors from skewing the results [2] [63].
Experimental Protocols
Protocol 1: Assessing the Impact of a Novel Insulin Formulation on Lipohypertrophy Development in a Rodent Model
Objective: To evaluate the potential of a novel weekly basal insulin analog to reduce the incidence and severity of LH compared to a daily basal insulin.
Materials:
- Animal Model: Diabetic rodents (e.g., streptozotocin-induced or db/db mice).
- Test Articles: Novel weekly insulin (e.g., Insulin Icodec), control daily insulin (e.g., Insulin Glargine U-100), vehicle control.
- Key Equipment: High-frequency ultrasound system (e.g., 40-70 MHz probe), CGM systems, micro-syringes with fixed needles.
- Histology Reagents: Formalin, paraffin, Hematoxylin and Eosin (H&E) stain, Masson's Trichrome stain for collagen/fibrosis.
Methodology:
- Acclimatization & Baseline: Acclimatize animals for one week. Collect baseline body weight, blood glucose, and perform baseline ultrasound scan of the intended injection area (typically the dorsum for rodents).
- Randomization & Dosing: Randomize animals into three groups (Weekly Insulin, Daily Insulin, Vehicle). Administer subcutaneous injections in a confined, non-rotated area to induce LH.
- Weekly Insulin Group: Single weekly injection.
- Daily Insulin Group: Daily injections (7x per week).
- Vehicle Group: Daily or weekly vehicle injection (scheme matching the weekly group).
- In-Life Monitoring: Weigh animals and measure blood glucose daily. Use CGM for one week at the study's start, middle, and end to assess glycemic variability. Perform ultrasound imaging weekly to monitor subcutaneous tissue changes and measure lesion thickness/diameter.
- Terminal Analysis: At the end of the study period (e.g., 8-12 weeks), euthanize animals and excise the injection site tissue.
- Histopathological Examination: Fix tissue in formalin, process, and embed in paraffin. Section and stain with H&E (for adipocyte morphology) and Masson's Trichrome (for fibrosis). Perform blinded scoring for LH severity and quantitative image analysis for adipocyte size and fibrotic area [3] [20].
Visualization of Experimental Workflow:
Protocol 2: Evaluating a Tension-Offloading Dressing for Prevention of Injection Site Fibrosis
Objective: To determine if mechanical offloading of skin tension at insulin injection sites can prevent fibrosis, a key component of LH.
Materials:
- Animal Model: A suitable rodent or porcine model.
- Test Device: Tension-offloading dressing (e.g., embrace device).
- Control: Standard transparent film dressing.
- Insulin: A standard commercial insulin formulation.
- Key Equipment: Tensile tester, tools for histology.
Methodology:
- Study Setup: Identify two symmetrical injection areas on the animal (e.g., both flanks). Randomly assign one site to the test device and the other to the control dressing.
- Device Application & Dosing: Apply the test and control dressings to their respective sites according to manufacturer instructions. Perform daily insulin injections through the center of each dressing for a set period (e.g., 4 weeks).
- Tissue Harvest & Mechanical Testing: After the treatment period, euthanize the animal and harvest the tissue from beneath the dressings. Cut standardized tissue strips and use a tensile tester to measure the ultimate tensile strength and stiffness of the tissue—stiffer tissue indicates higher fibrosis [20].
- Histological Confirmation: Process the tissue for histology (as in Protocol 1). Stain for collagen (Masson's Trichrome) and quantify the collagen density to confirm the mechanical testing results [20].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Investigating Insulin Injection Site Complications
| Item | Function/Brief Explanation |
|---|---|
| High-Frequency Ultrasound System | High-resolution imaging for non-invasive, longitudinal monitoring of subcutaneous tissue structural changes (e.g., early LH, dermal thickening). More sensitive than palpation [3]. |
| Tension-Offloading Dressing | A research tool to test the hypothesis that reducing mechanical forces at the injection site can inhibit both fibrotic tissue deposition and adipocyte hyperplasia [20]. |
| Smart Insulin Pens | Used in clinical or translational research to objectively monitor and analyze patient injection habits (dose, timing, rotation) and correlate them with LH development [89]. |
| Stable Insulin Analogs (e.g., Icodec) | A key experimental variable to test the impact of reduced injection frequency and improved pharmacokinetic stability on LH incidence [88]. |
| Glucose-Responsive Insulin Prototypes | Investigational reagents to study a paradigm where insulin action is decoupled from subcutaneous absorption kinetics, potentially eliminating localized tissue growth [89]. |
| Histology Stains (H&E, Masson's Trichrome) | Essential for endpoint analysis to quantify adipocyte size/number and fibrotic area, providing definitive evidence of tissue-level changes [3] [20]. |
Signaling Pathways in Lipohypertrophy Pathogenesis
Visualization of Key Signaling Pathways:
Conclusion
Effective prevention of insulin-associated lipodystrophy through proper injection site rotation is not merely a technical skill but a critical component of diabetes management that directly influences pharmacokinetic predictability and glycemic outcomes. The synthesis of evidence presented confirms that structured, multidisciplinary education significantly improves technique and metabolic results, yet sustained adherence requires addressing pervasive barriers including knowledge gaps, financial constraints, and low perceived risk. For the research and drug development community, these findings highlight urgent priorities: the need for standardized, scalable training protocols integrated into routine care; the development of more sensitive, accessible detection technologies; and the innovation of insulin formulations and delivery devices inherently designed to minimize localized tissue complications. Future clinical success depends on translating this comprehensive understanding into practical interventions that empower both patients and providers.
References
- 1. Lipohypertrophy: prevalence, clinical consequence, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7862817/]
- 2. Barriers to the Prevention of Insulin Injection-Associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619546/]
- 3. Lipohypertrophy and Insulin: An Update From the Diabetes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10658672/]
- 4. Lipodystrophy Syndromes: One Name but Many Diseases ... [https://link.springer.com/article/10.1007/s11892-025-01602-5]
- 5. Evolution of cell therapies derived from adipose tissue [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382222/]
- 6. Wnt Activation in Mature Dermal Adipocytes Leads to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12240021/]
- 7. Best insulin injection sites: Absorption time and rotation [https://www.medicalnewstoday.com/articles/316618]
- 8. Insulin injection knowledge, attitude, and practice of ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1501992/full]
- 9. Lipohypertrophy: Symptoms, Causes, Treatment & ... [https://my.clevelandclinic.org/health/diseases/22928-lipohypertrophy]
- 10. Lipohypertrophy: A Forgotten Problem [https://www.adces.org/practice/practice-resources/perspectives-on-diabetes-care/adces-perspectives-on-diabetes-care/2020/01/28/lipohypertrophy-a-forgotten-problem]
- 11. Optimising Insulin Injection Techniques to Improve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10570228/]
- 12. Insulin- Pharmacology, Therapeutic Regimens and Principles ... [https://www.ncbi.nlm.nih.gov/books/NBK278938/]
- 13. Insulin Injection Sites: Where and How to Inject [https://www.healthline.com/health/diabetes/insulin-injection]
- 14. Acquired facial lipoatrophy: pathogenesis and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4436232/]
- 15. Skin-related complications of insulin therapy: epidemiology ... [https://pubmed.ncbi.nlm.nih.gov/14507228/]
- 16. Insulin Routines | ADA [https://diabetes.org/health-wellness/medication/insulin-routines]
- 17. Site selection, site rotation and tips for injecting insulin [https://www.diabetesvic.org.au/insulin-injections-site-selection-site-rotation-and-tips-for-injecting-insulin/]
- 18. Biochemistry, Insulin Metabolic Effects - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK525983/]
- 19. Molecular Mechanisms for the Vicious Cycle between ... [https://www.mdpi.com/1422-0067/24/12/9818]
- 20. Leveraging Mechanical Forces to Target Insulin Injection– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8387605/]
- 21. Comprehensive investigation of insulin-induced ... [https://www.sciencedirect.com/science/article/abs/pii/S1871402124001449]
- 22. Incorrect Insulin Administration: A Problem That Warrants ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4714726/]
- 23. Insulin Pumps l Infusion Set Site Rotation l danatech [https://www.adces.org/education/danatech/insulin-pumps/pumps-in-professional-practice/insulin-infusion-set-site-rotation-toolkit]
- 24. Insulin lipodystrophy and lipohypertrophy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3743397/]
- 25. Learning About Preventing Lipohypertrophy [https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=acd5155]
- 26. Diabetes Injection Site Rotation- Pediatric Endocrinology [https://www.urmc.rochester.edu/childrens-hospital/endocrinology/injection-site.aspx]
- 27. Insulin Pumps l Troubleshooting Hyperglycemia l danatech [https://www.adces.org/education/danatech/insulin-pumps/troubleshooting-pumps/troubleshooting-unexplained-hyperglycemia]
- 28. Variability in insulin pharmacokinetics following high-dose ... [https://pubmed.ncbi.nlm.nih.gov/34521309/]
- 29. Insulin Injection Technique is Associated with Glycemic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6250622/]
- 30. Effect of Insulin Injection Techniques on Glycemic Control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9762765/]
- 31. What Is Lipohypertrophy? Symptoms, Treatments, and More [https://www.webmd.com/diabetes/what-is-lipohypertrophy]
- 32. Unexplained Hypoglycemia: A Focused Approach to ... [https://www.consultant360.com/articles/unexplained-hypoglycemia-focused-approach-finding-cause]
- 33. (1) | PDF Rotating injection sites [https://www.slideshare.net/slideshow/rotating-injection-sites-1/63466663]
- 34. How to Measure Glycemic Variability? A Literature Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC10818970/]
- 35. Core Glycemic Metrics Explained. TIR, TBR, TAR, GMI, CV, ... [https://www.adces.org/education/danatech/glucose-monitoring/continuous-glucose-monitors-(cgm)/glycemic-metrics--an-overview]
- 36. Insulin Pen Overview & FAQs [https://www.adces.org/education/danatech/insulin-medicine-delivery/insulin-medicine-delivery-101/insulin-pen-overview-faqs]
- 37. Lipodystrophy in Insulin-Treated Subjects and Other Injection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5014793/]
- 38. Mayo Clinic Proceedings Publishes New Global Insulin ... [https://investors.embecta.com/news-releases/news-release-details/mayo-clinic-proceedings-publishes-new-global-insulin-injection]
- 39. Troubleshooting Your Patient's Injection Technique [https://www.opatoday.com/troubleshooting-your-patients-injection-technique-a-guide-for-pharmacists/]
- 40. Advance Insulin Injection Technique and Education With ... [https://pubmed.ncbi.nlm.nih.gov/40180487/]
- 41. Survey of Insulin Site Rotation in Youth with Type 1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3298887/]
- 42. Anatomical Terms of Movement - Flexion - Rotation [https://teachmeanatomy.info/the-basics/anatomical-terminology/terms-of-movement/]
- 43. Anatomical terms of location [https://en.wikipedia.org/wiki/Anatomical_terms_of_location]
- 44. The 3 Anatomical Body Planes and The Movements In Each [https://www.healthline.com/health/body-planes]
- 45. Multi-Site Rotation Scheduling: Ultimate Shift Planning Guide [https://www.myshyft.com/blog/rotation-scheduling-across-sites/]
- 46. Comparing Insulin Pen Needles [https://www.healthline.com/diabetesmine/all-about-insulin-pen-needles]
- 47. DropSafe® Safety Pen Needles | DropSafe® [https://dropsafe.info/products/dropsafe-safety-pen-needles/]
- 48. Easy Comfort Insulin Pen Needles - 32G 4mm 100/BX [https://www.diabeticwarehouse.org/products/easy-comfort-insulin-pen-needles-32g-4mm-100ct]
- 49. 4 Needle Sizes & Their Effects on Diabetes Control [https://us.ukmedi.co.uk/blogs/articles/4-needle-sizes-their-effects-on-diabetes-control]
- 50. 4SURE Pen Needles | Nipro [https://www.nipro-group.com/en/our-offer/products-services/4sure-pen-needles]
- 51. The Injection Technique Factor: What You Don't Know or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6640874/]
- 52. Optimizing insulin injection technique and its effect on ... [https://www.sciencedirect.com/science/article/pii/S2214623714000271]
- 53. Ameliorating Insulin Injection Site Rotation and its Impact ... [https://www.sciencedirect.com/org/science/article/pii/S0250688224000033]
- 54. How to Give a Subcutaneous Injection [https://www.hopkinsarthritis.org/patient-corner/how-to-give-a-subcutaneous-injection/]
- 55. Insulin and syringes - storage and safety Information [https://www.mountsinai.org/health-library/special-topic/insulin-and-syringes-storage-and-safety]
- 56. Information Regarding Insulin Storage and Switching ... [https://www.fda.gov/drugs/emergency-preparedness-drugs/information-regarding-insulin-storage-and-switching-between-products-emergency]
- 57. Thermal stability and storage of human insulin [https://pubmed.ncbi.nlm.nih.gov/37930742/]
- 58. Storing Insulin - IDDT [https://www.iddt.org/about/living-with-diabetes/storing-insulin/]
- 59. Safe and effective use of insulin requires proper storage [https://www.health.harvard.edu/blog/safe-and-effective-use-of-insulin-requires-proper-storage-2018120415486]
- 60. Investigating Real-World Stability and Sterility of in-Use Insulin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12390779/]
- 61. Considerations for Blood Glucose Monitoring and Insulin ... [https://www.cdc.gov/injection-safety/hcp/infection-control/index.html]
- 62. Optimizing Insulin Injection – Expert Recommendations ... [https://diatribe.org/diabetes-medications/optimizing-insulin-injection-expert-recommendations-fitter]
- 63. Lipodystrophy with an uncommon clinical presentation in a ... [https://www.openaccessjournals.com/articles/lipodystrophy-with-an-uncommon-clinical-presentation-in-a-patient-with-type-2-diabetes-on-insulin-therapy-18559.html]
- 64. The Distinct Ultrasound Characteristics and Prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11963818/]
- 65. Lipodystrophy and recovery are mediated by the Wnt ... [https://pubmed.ncbi.nlm.nih.gov/41040283/]
- 66. Comment on Lombardo et al. The Impact of Insulin-Induced ... [https://www.mdpi.com/2227-9067/12/2/111]
- 67. Repeated insulin injection without site rotation affects skin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9153835/]
- 68. Assessment of insulin pen injection practices and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12556281/]
- 69. Assessment of insulin pen injection practices and the ... [https://www.sciencedirect.com/science/article/pii/S266727662500112X]
- 70. A Coloured Pen Needle Education System Improves Insulin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7644732/]
- 71. The American Diabetes Association Releases Standards of ... [https://diabetes.org/newsroom/press-releases/american-diabetes-association-releases-standards-care-diabetes-2025]
- 72. Lumps and Bumps Around Insulin Injection Sites [https://www.medtronicdiabetes.com/loop-blog/lumps-and-bumps-from-insulin-therapy]
- 73. Prevalence and risk factors of lipohypertrophy in insulin - injecting ... [https://pubmed.ncbi.nlm.nih.gov/23886784/]
- 74. Do Different Body Colors and Labels of Insulin Pens ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3045242/]
- 75. ATTD 2025: Key Breakthroughs in Diabetes Technology ... [https://touchendocrinology.com/insight/attd-2025-key-breakthroughs-in-diabetes-technology-and-treatment/]
- 76. Advances in Continuous Glucose Monitoring: Clinical ... [https://www.e-enm.org/journal/view.php?doi=10.3803/EnM.2025.2370]
- 77. Advances in Continuous Glucose Monitoring: Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12061739/]
- 78. 2025 American Diabetes Association's (ADA) Standards of ... [https://www.omnipod.com/hcp/blog/tips-guidelines/2025-ada-standards-of-care]
- 79. Troubleshooting Acute Infusion Set/Site Issues [https://www.adces.org/education/danatech/insulin-pumps/troubleshooting-pumps/troubleshooting-acute-infusion-set-site-issues]
- 80. Impact of pharmacist insulin injection re-education on ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8347656/]
- 81. Educational Interventions for Individuals with Insulin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11389829/]
- 82. A Neglected Complication of Insulin Therapy Due to Errors ... [https://www.mdpi.com/2673-4540/6/3/22]
- 83. A Systematic Review of the Cost-Effectiveness of Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12606780/]
- 84. Routine second-trimester ultrasonography in the United ... [https://www.sciencedirect.com/science/article/abs/pii/S0002937800800320]
- 85. in Lipodystrophy -Treated Subjects and Other Insulin - Injection ... Site [https://link.springer.com/article/10.1007/s13300-016-0187-6]
- 86. Why We Rotate Insulin Injections [https://childrenwithdiabetes.com/clinical-director/why-we-rotate-insulin-injections/]
- 87. Tips for Insulin Injection Site Rotation [https://www.healthxchange.sg/how-to-manage/type-2-diabetes-mellitus/tips-insulin-injection-site-rotation]
- 88. Insulin icodec: A novel once-weekly formulation for the ... [https://link.springer.com/article/10.1007/s11154-025-09960-x]
- 89. Newer Advancements in Insulin Therapy [https://globalrph.com/2024/12/6442846/]
- 90. Ithaca startup aims to free diabetes patients from daily burden [https://news.cornell.edu/stories/2025/10/ithaca-startup-aims-free-diabetes-patients-daily-burden]
- 91. Implantable device could save diabetes patients from ... [https://news.mit.edu/2025/implantable-device-could-save-diabetes-patients-low-blood-sugar-0709]
- 92. With Expanded Research, Mount Sinai Teams Aim to ... [https://reports.mountsinai.org/article/endo2025-_4_diabetes]