Model Predictive Control for Blood Glucose Regulation: Algorithm Design, Clinical Validation, and Future Directions
This comprehensive review examines Model Predictive Control (MPC) algorithms for automated blood glucose regulation in type 1 diabetes.
Model Predictive Control for Blood Glucose Regulation: Algorithm Design, Clinical Validation, and Future Directions
Abstract
This comprehensive review examines Model Predictive Control (MPC) algorithms for automated blood glucose regulation in type 1 diabetes. We explore foundational MPC principles and their application in artificial pancreas systems, detailing methodological advances including adaptive tuning strategies and data-driven predictors using LSTM networks. The analysis covers troubleshooting challenges like model inaccuracies and optimization techniques, alongside rigorous clinical validation through comparative trials against PID control and conventional insulin therapy. Synthesizing evidence from recent clinical studies and meta-analyses, this article provides researchers and drug development professionals with a thorough technical foundation and critical assessment of MPC performance, safety considerations, and future research trajectories in closed-loop glucose management.
Fundamental Principles and Clinical Rationale for MPC in Glucose Regulation
The artificial pancreas (AP), or automated insulin delivery (AID) system, represents a landmark achievement in the treatment of Type 1 Diabetes (T1D), transforming a once-disputed concept into the modern standard of care [1]. This technology aims to mimic the glucose-regulatory function of a healthy pancreas by automating insulin delivery. At its core, the artificial pancreas is a closed-loop control system that integrates continuous glucose monitoring with automated insulin infusion [2]. The development of these systems has been largely driven by advances in control algorithms, with Model Predictive Control (MPC) emerging as a predominant strategy due to its ability to handle system delays, constraints, and disturbances [3] [4]. This document details the core components of the AP system, analyzes the specific challenges in glucose control, and provides structured experimental protocols for evaluating MPC algorithms in both simulation and clinical settings, framed within the context of blood glucose regulation research.
System Components of the Artificial Pancreas
An artificial pancreas system is composed of three interconnected hardware components that work in concert with a control algorithm.
Core Components
- Continuous Glucose Monitor (CGM): This sensor measures glucose concentrations in the interstitial fluid subcutaneously, transmitting data to the control algorithm nearly in real-time. Modern CGMs have been pivotal for AP development, though they introduce challenges such as a physiological time lag (typically 5-15 minutes) between blood and interstitial glucose levels and require periodic calibration [5].
- Control Algorithm: This is the "brain" of the AP system. Residing on a dedicated controller or a smartphone, the algorithm processes CGM data and determines the appropriate insulin infusion rate. Model Predictive Control (MPC) is particularly prominent because it uses a model of the patient's glucose-insulin dynamics to predict future glucose levels and computes optimal insulin deliveries while respecting safety constraints on insulin delivery and glucose levels [3] [4].
- Insulin Pump: This device delivers rapid-acting insulin subcutaneously based on commands from the control algorithm. Most systems use conventional pumps with infusion sets, while patch pumps that adhere directly to the skin are also available [5].
The Research Toolkit: Essential Components and Reagents
Table 1: Key Research Reagents and Solutions for AP Development
| Item | Function in Research |
|---|---|
| In Silico Simulator | A computer model of the human metabolic system in T1D, accepted by regulatory bodies as a substitute for animal trials in early algorithm testing [1]. |
| Universal Research Platform (e.g., APS) | A software platform that enables automated communication between various CGMs, pumps, and control algorithms, powering early inpatient clinical trials [1]. |
| Rapid-Acting Insulin Analogue | The manipulated input in the control system; its pharmacodynamic variability and slow absorption kinetics are major challenges for controller design [5]. |
| Metabolic Challenge Meals | Standardized meals used in clinical trials to create a consistent and significant disturbance (glucose excursion) to evaluate controller performance [3]. |
| Continuous Glucose Monitor | Provides the primary feedback signal for the closed-loop system; its accuracy, delay, and reliability are critical for safe operation [5]. |
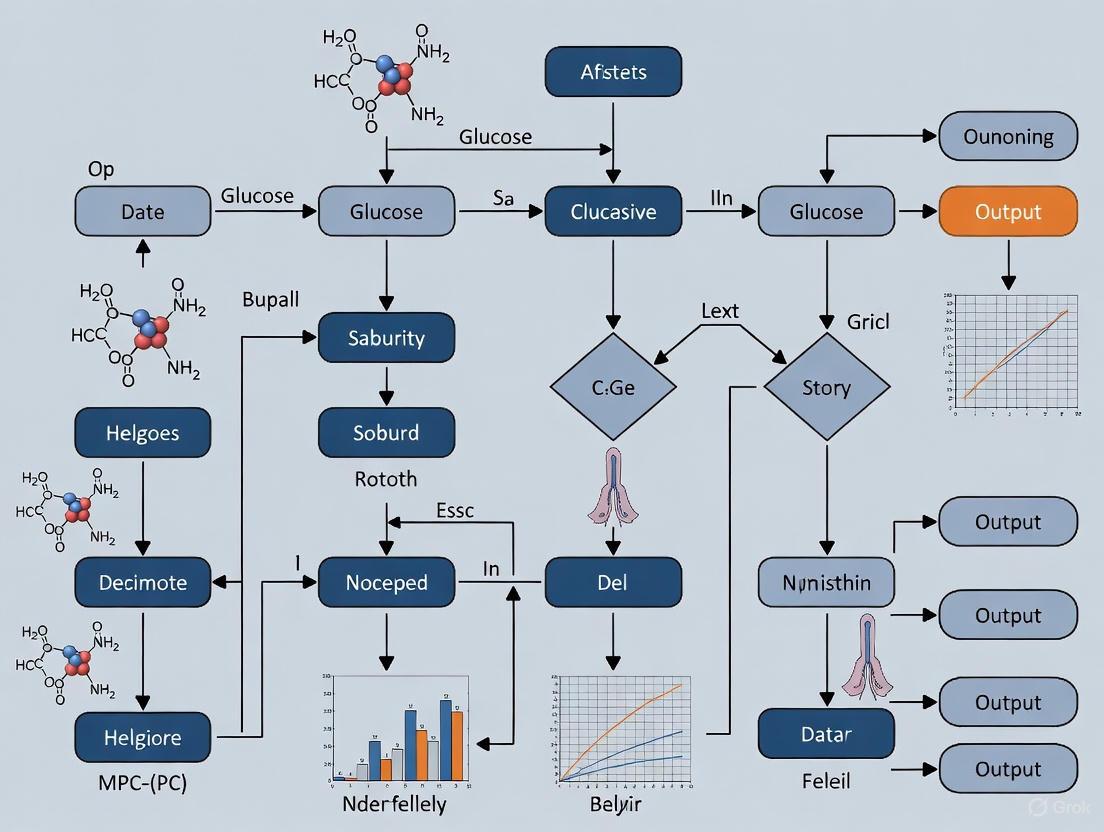
The interaction of these components forms a closed-loop control system, visually summarized in the workflow below.
Control Challenges and the Role of MPC
The primary challenge in closing the glucose control loop stems from the complex, nonlinear, and highly variable physiology of glucose-insulin dynamics. MPC has become a leading algorithmic approach due to its inherent ability to address several of these fundamental challenges.
Primary Control Challenges
- Significant Time Delays: The system is affected by multiple delays, including the slow absorption of subcutaneously administered insulin, the lag between blood and interstitial glucose measured by the CGM, and the delayed action of insulin on glucose uptake [5] [3].
- Meal Disturbances: Carbohydrate intake represents a large, rapid, and often uncertain disturbance. Accurately estimating the carbohydrate content of a meal is difficult, and the rate of glucose appearance in the blood is variable [5] [6].
- Inter- and Intra-Patient Variability: An individual's insulin sensitivity changes throughout the day and is influenced by factors like exercise, stress, and hormonal cycles. Furthermore, there is significant variability in insulin pharmacodynamics between different patients [5] [7].
- Actuator and Sensor Limitations: Insulin pumps can experience infusion set failures, while CGM sensors can suffer from signal dropouts or calibration errors, requiring the control algorithm to be robust to such device-related faults [5] [6].
- Safety Constraints: The controller must strictly avoid hypoglycemia while simultaneously minimizing hyperglycemia, creating a narrow therapeutic window for operation [8].
How MPC Addresses These Challenges
MPC is well-suited to this problem because it uses an internal model to predict future glucose trajectories over a defined horizon. This allows it to anticipate and proactively counteract glycemic events [3]. Key advantages include:
- Constraint Handling: MPC can explicitly incorporate constraints on maximum insulin delivery and minimum glucose levels, enhancing safety [3] [8].
- Delay Compensation: By forecasting future states, MPC can account for the system's inherent delays [3].
- Meal Announcement: MPC can effectively utilize feedforward action from meal announcements to improve postprandial control, though it must also handle unannounced meals robustly [3].
Quantitative Performance of MPC Algorithms
The effectiveness of MPC-based AID systems has been validated in numerous clinical trials. The table below summarizes key glycemic outcomes from a systematic review and meta-analysis.
Table 2: Glycemic Outcomes of MPC-based Artificial Pancreas vs. Conventional Therapy [4]
| Outcome Measure | Intervention Scenario | Mean Difference (MPC vs. Control) | Statistical Significance (p-value) |
|---|---|---|---|
| Time in Target Range (3.9-10 mmol/L) | Overnight Use | +10.03% (95% CI: 7.50, 12.56) | < 0.00001 |
| Time in Hypoglycemia (< 3.9 mmol/L) | Overnight Use (Long-term: >1 month) | -1.34% (95% CI: -1.87, -0.81) | < 0.00001 |
Experimental Protocols for AP Research
Protocol 1: In Silico Closed-Loop Validation
This protocol uses a computer simulator to test and refine MPC algorithms prior to clinical studies [3].
- Objective: To assess the performance, robustness, and safety of a novel MPC algorithm under controlled conditions with a large virtual population.
- Materials:
- Simulator: FDA-accepted T1D simulation platform (e.g., UVa/Padova Simulator) [3].
- Algorithm: The MPC algorithm to be tested.
- Virtual Cohort: A population of
n(e.g., 100) adult, pediatric, and adolescent simulators with varying insulin sensitivities.
- Procedure:
- Day 1: Run a 24-hour simulation with a standard meal protocol (e.g., 45g breakfast, 70g lunch, 60g dinner) with 50% of meals announced to the algorithm.
- Day 2-4: Introduce realistic meal variations using a stochastic meal generator and include a period of moderate-intensity exercise (e.g., 45 minutes) on one day [9].
- Day 5: Test robustness by simulating a 30% over-estimation of carbohydrate content for all meals and a temporary CGM signal dropout.
- Data Analysis:
- Calculate primary outcomes: Percentage of Time in Range (3.9-10.0 mmol/L), time in hypoglycemia (<3.9 mmol/L), and time in hyperglycemia (>10.0 mmol/L).
- Calculate secondary outcomes: Mean glucose, glucose standard deviation, and LBGI/HBGI (Low/High Blood Glucose Indices) [8].
The following diagram illustrates the iterative process of an in silico trial using MPC.
Protocol 2: Clinical Outpatient Trial
After successful in silico testing, the algorithm progresses to a clinical trial in a free-living environment.
- Objective: To evaluate the safety and efficacy of the MPC-based AP system in real-world conditions over an extended period.
- Materials:
- AID System: The integrated system comprising CGM, insulin pump, and handheld controller running the MPC algorithm.
- Study Cohort:
n(e.g., 30-50) adult participants with T1D. - Comparator: Sensor-augmented pump (SAP) therapy as the control intervention.
- Procedure:
- Design: Randomized, crossover trial where each participant undergoes both AID and control periods.
- Run-in Phase: A 1-2 week period where all participants use SAP therapy to collect baseline data and individualize pump settings.
- Intervention Phase: A 3-month period where the participant uses the MPC-based AID system. Users are instructed to announce meals but are not forced to, allowing for assessment of algorithm performance with unannounced meals.
- Control Phase: A 3-month period where the participant uses SAP therapy.
- Data Collection and Analysis:
Advanced MPC Formulations and Future Directions
Research continues to address the limitations of linear MPC. Recent advances explored in the literature include:
- Nonlinear Explicit MPC (NEMPC): This approach uses Taylor series expansion to create an analytical solution to the nonlinear MPC problem, significantly reducing computational burden and avoiding the need for iterative online optimization, which is beneficial for portable devices [8].
- Data-Driven and LSTM-Augmented MPC: To improve long-term prediction accuracy, studies are incorporating Long Short-Term Memory (LSTM) neural networks to learn the nonlinear glucose dynamics from data. The predictor is structured to be affine in the future control inputs, allowing the MPC problem to remain a tractable quadratic program [9].
- Adaptive and Fault-Tolerant Control: Research into adaptive backstepping and other nonlinear methods aims to compensate for unannounced meals and actuator faults, providing robustness in cases of pump failures or mis-estimated meal sizes [6].
Model Predictive Control (MPC) is an advanced, model-based control strategy that uses a dynamic model of a system to predict its future behavior and compute optimal control actions through online optimization [10] [11]. Unlike reactive control strategies such as PID control, MPC operates on a proactive principle, anticipating future system behavior and disturbances to make informed decisions [10] [11]. This capability is particularly valuable for complex, multivariable systems with constraints, such as blood glucose regulation in artificial pancreas systems [12] [13].
The core architecture of MPC rests on three fundamental pillars: (1) a prediction model that forecasts system behavior, (2) an optimization process that computes control actions by minimizing a cost function, and (3) a receding horizon implementation that provides feedback and robustness [10] [11]. This architecture enables MPC to handle constraints directly, manage multivariable interactions, and compensate for delays—properties that make it exceptionally suitable for biomedical applications like glucose regulation [13].
In the context of blood glucose regulation for Type 1 Diabetes (T1D) patients, MPC has emerged as a leading control algorithm for artificial pancreas systems [12] [13]. Its predictive capability allows it to anticipate glycemic fluctuations and calculate appropriate insulin doses while respecting safety constraints on both insulin delivery and glucose concentrations [12]. This application note explores the core architectural components of MPC and their specific implementation in glucose regulation research.
Core Architectural Components of MPC
Prediction Models
The prediction model forms the foundation of any MPC implementation, serving as the mathematical representation of the system dynamics used to forecast future behavior [10] [11]. The choice of model significantly impacts the controller's performance, robustness, and computational requirements.
For discrete-time systems, which are common in digital control implementations including artificial pancreas systems, the state-space representation is typically used:
[ x{k+1} = f(xk, uk, pk) ] [ yk = h(xk, uk, pk) ]
Where (xk) represents the system states, (uk) the control inputs, (pk) the parameters, and (yk) the system outputs [11]. In glucose regulation applications, the states may include plasma glucose, subcutaneous glucose, insulin concentrations, and other physiological variables; the control input is typically insulin infusion rate; and the output is often the continuous glucose monitor (CGM) measurement [12] [13].
Table: Common Model Types in MPC for Glucose Regulation
| Model Type | Description | Advantages | Limitations | Representative Uses in Glucose Regulation |
|---|---|---|---|---|
| Physiological (Sorensen) | Comprehensive 19-state model representing organ-level glucose-insulin dynamics [13] | High physiological fidelity, accounts for glucagon | High complexity, computationally intensive | Dual-hormone (insulin & glucagon) control [13] |
| Compartmental (Hovorka) | 6-state nonlinear model with glucose compartments, insulin action, and plasma insulin [13] | Balanced complexity and accuracy, validated in clinical studies | Limited individualization | Single-hormone MPC implementations |
| Data-Driven (CHoKI) | Nonparametric learning method using patient data [12] | Customized per patient, no need for physiological model | Requires extensive training data | Learning-based MPC for inter-patient variability [12] |
| Minimal (Bergman) | 3-state model with plasma glucose, remote insulin, plasma insulin [13] | Simple structure, rapid computation | Limited accuracy, especially during meals | Early artificial pancreas prototypes |
For complex physiological systems like glucose metabolism, two main modeling approaches prevail: first-principles models derived from mass balance and physiological knowledge (e.g., Sorensen model), and data-driven models learned from patient data (e.g., CHoKI - Componentwise Hölder Kinky Inference) [12] [13]. The Sorensen model, with its 19 differential equations, offers comprehensive representation of glucose-insulin-glucagon dynamics but presents significant computational challenges [13]. In contrast, data-driven approaches like CHoKI create customized models for individual patients, potentially enhancing performance despite inter- and intra-patient variability in diabetes [12].
Optimization Framework
The optimization component is the computational engine of MPC, responsible for calculating control actions that minimize a defined cost function while satisfying operational constraints [10] [11]. The general finite-horizon optimal control problem solved at each sampling instant can be formulated as:
[ \min{\mathbf{u}{0:N}} J = \sum{k=0}^{N-1} l(xk, uk, pk) + m(xN) ] Subject to: [ x{k+1} = f(xk, uk, pk), \quad k = 0,\dots,N-1 ] [ u{lb} \leq uk \leq u{ub}, \quad k = 0,\dots,N-1 ] [ x{lb} \leq xk \leq x{ub}, \quad k = 0,\dots,N ] [ g(xk, u_k) \leq 0, \quad k = 0,\dots,N ]
Where (N) is the prediction horizon, (l(\cdot)) is the stage cost function, (m(\cdot)) is the terminal cost function, and the constraints represent input limits, state boundaries, and general nonlinear constraints [11].
In glucose regulation, the cost function typically penalizes deviations from the target glucose range (70-180 mg/dL) while minimizing excessive insulin delivery [12] [13]. For example:
[ J = \sum{k=1}^{N} wg(Gk - G{target})^2 + \sum{k=0}^{N-1} wI(Ik - I{basal})^2 ]
Where (Gk) is the predicted glucose level, (Ik) is the insulin infusion rate, and (wg), (wI) are weighting factors that balance the competing objectives of glucose control and insulin conservation [12].
Table: Optimization Considerations in Glucose Regulation MPC
| Aspect | Considerations in Glucose Regulation | Typical Values/Approaches |
|---|---|---|
| Cost Function Terms | Glucose deviation from target, insulin delivery amount, constraint violation penalties | Quadratic terms for glucose error ((wg = 1.0)), smaller weights for insulin ((wI = 0.01)) [13] |
| Constraints | Hypoglycemia prevention (<70 mg/dL), hyperglycemia mitigation (>180 mg/dL), maximum insulin delivery, insulin on board (IOB) limits [12] | Hard constraints at 70 mg/dL and 250 mg/dL, IOB constraints based on patient-specific factors [12] |
| Optimization Algorithm | Computational efficiency, handling of nonlinearities, guarantee of feasible solution | Quadratic programming (linearized models), nonlinear programming (SQP, interior-point), explicit MPC [14] |
| Horizon Selection | Long enough to capture meal response, short enough for computational tractability | Prediction horizon: 2-6 hours; Control horizon: 30-120 minutes [12] |
A critical safety consideration in glucose regulation MPC is the incorporation of Insulin on Board (IOB) constraints [12]. These constraints dynamically limit insulin delivery based on previously administered insulin that remains active in the body, thereby reducing hypoglycemia risk:
[ uk \leq u{max} - IOB_k ]
Where (IOB_k) represents the estimated active insulin at time (k) [12]. This constraint prevents excessive insulin stacking, particularly following correction boluses or during periods of increasing insulin sensitivity.
Receding Horizon Principle
The receding horizon principle implements feedback in MPC and distinguishes it from traditional optimal control [10] [11]. This mechanism involves:
- At each sampling instant (k), measuring or estimating the current system state (x_k)
- Solving an optimization problem over a finite prediction horizon (N) to determine a sequence of optimal control moves (\mathbf{u}_{k:k+N-1}^*)
- Implementing only the first control action (u_k^*) from the optimized sequence
- Advancing to the next sampling instant (k+1), measuring the new state, and repeating the entire process
This "plan-and-execute-one-step" approach introduces feedback that compensates for model inaccuracies, measurement noise, and unmeasured disturbances [10]. In glucose regulation, this means the MPC can continuously adjust to unexpected glucose fluctuations, changes in insulin sensitivity, or unannounced meals [13].
The following diagram illustrates the receding horizon principle in the context of an artificial pancreas system:
Diagram: Receding Horizon Principle in Artificial Pancreas
The selection of appropriate horizons represents a critical design trade-off. The prediction horizon must be sufficiently long to capture the dominant dynamics—typically 2-6 hours in glucose regulation to account for meal responses and insulin pharmacokinetics [12]. The control horizon is often shorter (30-120 minutes) to reduce computational complexity while maintaining adequate degrees of freedom [10]. The sampling time (typically 5-10 minutes) balances responsiveness to rapid glucose changes with computational burden and CGM measurement frequency [13].
MPC Implementation Protocols for Glucose Regulation
Experimental Setup and Reagent Solutions
Robust experimental protocols are essential for developing and validating MPC systems for glucose regulation. The following table details key research components and their functions:
Table: Research Reagent Solutions for Glucose Regulation MPC
| Component | Function | Implementation Example |
|---|---|---|
| In Silico Simulator | Provides validated virtual patient population for testing and development | UVA/Padova T1D Simulator (FDA-accepted substitute for preclinical trials) [12] |
| Physiological Model | Represents glucose-insulin dynamics for prediction | Sorensen Model (19 states), Hovorka Model (6 states), Bergman Minimal Model (3 states) [13] |
| Learning Method | Customizes controller to individual patient characteristics | Componentwise Hölder Kinky Inference (CHoKI) - nonparametric learning [12] |
| Performance Metrics | Quantifies controller efficacy and safety | Time-in-Range (70-180 mg/dL), Time-in-Hypoglycemia (<70 mg/dL), Time-in-Hyperglycemia (>180 mg/dL) [12] |
| Constraint Formulation | Ensures patient safety despite disturbances | Insulin-on-Board (IOB) constraints, maximum basal rate limits, hypoglycemia prediction constraints [12] |
The UVA/Padova simulator has emerged as a critical tool in artificial pancreas research, providing a population of virtual T1D patients with realistic physiological variability [12]. This simulator enables controlled, reproducible testing of MPC algorithms without risking patient safety, and its FDA acceptance for preclinical studies underscores its validity [12].
Detailed Protocol: CHoKI-Based MPC Implementation
The following protocol outlines the implementation procedure for a data-driven MPC using the CHoKI learning method, as presented in recent research [12]:
Objective: Implement a personalized MPC for basal insulin delivery in T1D patients that maintains blood glucose in the safe range (70-180 mg/dL) while minimizing hypoglycemia risk through IOB constraints.
Materials:
- UVA/Padova T1D Simulator (10 adult patients)
- Historical data collection: CGM measurements, insulin delivery records, meal announcements (if available)
- MATLAB/Python implementation environment with optimization toolbox
- CHoKI learning method code implementation
Procedure:
Data Collection Phase (2 weeks per virtual patient):
- Collect CGM measurements at 5-minute intervals
- Record basal insulin delivery rates
- Log meal carbohydrate content and timing (if available)
- Include various daily patterns to capture inter-day variability
Model Identification Phase:
- Apply CHoKI nonparametric learning to historical data
- Identify input-output relationship: ( G{k+1} = f(Gk, G{k-1}, ..., Ik, I_{k-1}, ...) )
- Validate model prediction accuracy on withheld data (10% of dataset)
- Require minimum prediction accuracy: CVGA A/B zone > 90%
MPC Configuration:
- Prediction horizon: 3 hours (N = 36 steps at 5-minute intervals)
- Control horizon: 1 hour (M = 12 steps)
- Cost function weights: ( wg = 1.0 ) (glucose error), ( wI = 0.01 ) (insulin change)
- Safety constraints:
- Hard glucose constraint: 70 mg/dL (lower bound)
- IOB-dependent insulin constraint: ( uk \leq u{max} - IOB_k )
- Maximum basal rate: patient-specific based on total daily dose
Closed-Loop Evaluation:
- Implement 7-day in-silico trial for each virtual patient
- Include unannounced meals (50% of meals) to test robustness
- Introduce ±30% insulin sensitivity variations to test adaptation
- Compare against standard constant basal therapy (control)
Performance Analysis:
- Calculate percentage time in target range (70-180 mg/dL)
- Quantify time in hypoglycemia (<70 mg/dL) and hyperglycemia (>180 mg/dL)
- Compute average glucose and glucose variability (coefficient of variation)
- Perform statistical analysis (paired t-tests) against control condition
The following workflow diagram illustrates the CHoKI-based MPC development process:
Diagram: CHoKI-Based MPC Development Workflow
Performance Metrics and Validation
Rigorous performance validation is essential for evaluating glucose regulation MPC. Recent studies have demonstrated promising results with the CHoKI-based approach:
Table: Quantitative Performance of CHoKI-MPC in Glucose Regulation
| Metric | Standard Basal Therapy | CHoKI-MPC | Improvement | Validation Method |
|---|---|---|---|---|
| Time-in-Range (70-180 mg/dL) | 65.2% | 78.9% | +13.7% | 7-day in-silico trial (n=10 adults) [12] |
| Time-in-Hypoglycemia (<70 mg/dL) | 4.8% | 1.2% | -3.6% (75% reduction) | UVA/Padova simulator [12] |
| Time-in-Hyperglycemia (>180 mg/dL) | 30.0% | 19.9% | -10.1% | With ±30% insulin sensitivity variation [12] |
| Average Tracking Error | 14.3 mg/dL | 4.4 mg/dL | -9.9 mg/dL | Compared to setpoint of 90 mg/dL [13] |
The significant reduction in hypoglycemia time (75% reduction) demonstrates the particular strength of MPC with IOB constraints in mitigating the most acute safety risk in glucose regulation [12]. The improved time-in-range (+13.7%) while simultaneously reducing hyperglycemia confirms the multi-objective optimization capability of MPC [12].
Advanced MPC Architectures for Enhanced Robustness
Multi-Stage MPC for Uncertainty Management
Multi-stage MPC extends the basic architecture to explicitly handle system uncertainties through a scenario-tree formulation [11]. This approach is particularly valuable in glucose regulation due to significant inter- and intra-patient variability in insulin sensitivity and meal responses.
The multi-stage approach:
- Approximates the uncertainty space with discrete samples
- Constructs a tree of possible future scenarios
- Optimizes control actions that are feasible for all considered scenarios
- Incorporates feedback information through non-anticipativity constraints
For a system with (np) uncertain parameters and (vi) possible values for each parameter, the number of scenarios grows as (Ns = (\prod{i=1}^{np} vi)^{N{robust}}) [11]. To maintain computational tractability, branching is typically limited to a robust horizon ((N{robust})) shorter than the prediction horizon.
In glucose regulation applications, key uncertainties include:
- Meal absorption rates and timing
- Insulin sensitivity variations
- Physical activity effects
- Stress and illness impacts
Hybrid MPC for Dual-Hormone Control
Advanced artificial pancreas systems may employ dual-hormone control using both insulin (to lower glucose) and glucagon (to raise glucose) [13]. This requires hybrid MPC architectures capable of managing multiple manipulated variables with different constraints and dynamics.
The MPC formulation for dual-hormone control extends the cost function:
[ J = \sum{k=1}^{N} wg(Gk - G{target})^2 + \sum{k=0}^{N-1} [wI(Ik - I{basal})^2 + w{GL}(GLk)^2] ]
Where (GL_k) represents glucagon delivery, with appropriate constraints on both hormone delivery rates [13]. The Sorensen model, with its explicit representation of glucagon dynamics, is particularly suited for such applications [13].
The core architecture of Model Predictive Control—encompassing prediction models, optimization, and receding horizon implementation—provides a powerful framework for blood glucose regulation in artificial pancreas systems. The predictive capability enables anticipation of glycemic fluctuations, while the optimization framework permits explicit handling of safety constraints and competing control objectives.
The integration of data-driven learning methods like CHoKI with traditional MPC represents a promising direction for personalized glucose control, adapting to individual patient characteristics and varying insulin sensitivity [12]. Furthermore, robust MPC formulations, such as multi-stage approaches, enhance safety despite significant uncertainties in meal absorption, metabolism, and daily activities.
For researchers and drug development professionals, implementing the protocols and architectures described herein requires careful attention to model selection, constraint formulation, and validation methodologies. The use of FDA-accepted simulation platforms like the UVA/Padova simulator provides a critical foundation for preclinical development, while rigorous performance metrics ensure meaningful evaluation of controller efficacy and safety.
As artificial pancreas technology evolves, MPC continues to offer a flexible, robust control paradigm capable of incorporating increasingly sophisticated physiological models, adaptive learning mechanisms, and enhanced safety constraints—ultimately improving the quality of life for individuals with Type 1 Diabetes.
Model Predictive Control (MPC) algorithms represent a significant evolution in automated insulin delivery (AiDS) for blood glucose regulation, directly addressing two persistent challenges in conventional diabetes therapy: high glycemic variability and postprandial hyperglycemia. Conventional methods, such as multiple daily injections (MDI) or traditional insulin pump therapy, often rely on predefined, static insulin regimens. These approaches struggle to adapt to dynamic physiological conditions, leading to suboptimal glucose control, particularly after meals. MPC, a advanced model-based control strategy, utilizes a dynamic model of the patient's glucose-insulin metabolism to predict future glucose levels and proactively compute optimal insulin doses. This enables the system to manage glycemic variability and respond to unannounced meals more effectively than reactive conventional therapies. This document details the quantitative advantages, experimental protocols, and core components of MPC-based systems for researchers and drug development professionals.
Table 1: Comparative Performance of MPC-based Systems vs. Conventional Therapy
| Metric | Conventional Therapy (Typical Performance) | MPC-based AiDS (Reported Performance) | Citation |
|---|---|---|---|
| Overall Time in Range (TIR: 70-180 mg/dL) | ~60-65% (varies widely) | 75.97% - 91.08% (in-silico) / 83.4% (preclinical) | [15] [16] |
| Time in Hypoglycemia (<70 mg/dL) | ~3-5% | 0.0% - 3.62% (mild events, no severe hypoglycemia) | [17] [16] |
| Mean Blood Glucose Level | Often >154 mg/dL | 132 - 159 mg/dL | [18] |
| Postprandial Hyperglycemia Control | Frequent excursions | Rapid regulation (e.g., peak of 320 mg/dL regulated within 50 min) | [16] |
| Performance with Unannounced Meals | Poor without manual bolus | Maintains TIR >83% via meal detection and adaptive control | [18] [16] |
Core MPC Algorithm Components and Workflow
The efficacy of MPC in managing glycemic variability stems from its structured, multi-component architecture. The following diagram illustrates the integrated workflow of a modern MPC system for an AiDS.
Diagram 1: Integrated MPC Workflow for AiDS. The system uses a model to predict future glucose levels and an optimizer to compute insulin doses, enhanced by meal detection and state estimation.
Key Component Functions
- Continuous Glucose Monitor (CGM): Provides real-time, noisy glucose measurements to the controller [15] [19].
- State & Disturbance Estimator: A Kalman filter is typically used to reduce sensor noise and provide an optimal estimate of the current metabolic state (e.g., glucose levels, insulin on board) and unmeasured disturbances, which is critical for the controller's accuracy [18] [15].
- Glucose-Insulin Model: A mathematical model (e.g., based on the Bergman minimal model or identified from population data) that predicts future glucose trajectories over a defined horizon based on the current state and potential insulin inputs [6] [15] [19].
- MPC Optimizer: The core algorithm that solves a constrained optimization problem at each control cycle. It calculates the sequence of insulin doses that minimizes a cost function (penalizing hyperglycemia, hypoglycemia, and excessive insulin use) over the prediction horizon, subject to safety constraints [19].
- Meal Detection Algorithm: A supervisory module that analyzes the rate of change of CGM readings to detect unannounced meals and trigger a feed-forward bolus or adjust controller aggressiveness [18].
Detailed Experimental Protocols
Protocol 1: In-Silico Validation of Adaptive MPC with RLS Estimation
This protocol evaluates the enhancement of MPC through real-time parameter adaptation [15].
1. Objective: To determine if integrating a Recursive Least Squares (RLS) estimator for insulin sensitivity (( \theta_1 )) improves glycemic regulation and if an event-triggered (ET) MPC strategy reduces energy consumption.
2. Materials & Setup:
- Simulator: UVA/Padova T1DM Simulator (FDA-approved) with 10 virtual adult subjects.
- Hardware-in-the-Loop (HIL): Raspberry Pi 3B, integrated with a custom low-cost insulin pump and battery driver.
- Control Strategies:
- Time-Triggered (TT-MPC): Standard MPC with 5-minute control cycles.
- TT-MPC with RLS: Enhanced with RLS for real-time ( \theta_1 ) estimation.
- Event-Triggered MPC (ET-MPC): Control actions computed only when a triggering condition (e.g., predicted glucose deviation) is met.
3. Procedure:
- Model Identification: Identify the prediction model (Eq. 1 in [15]) from the 10 adult subjects in the simulator.
- Controller Tuning: Tune the MPC and RLS parameters (forgetting factor, initial covariance).
- HIL Emulation: Run three-day simulations for each control strategy. Introduce unannounced carbohydrate meals and realistic CGM noise (Eq. 2 in [15]).
- Data Collection: Record Time in Range (TIR), hypoglycemia events, total insulin delivered, and energy consumption of the HIL setup.
4. Key Analysis & Outcomes:
- Glycemic Control: Compare TIR and hypoglycemia events between TT-MPC and TT-MPC+RLS.
- Energy Efficiency: Compare the number of control actions and total energy consumption between TT-MPC and ET-MPC.
- Conclusion: The study confirmed that RLS integration significantly improved TIR. The ET strategy reduced control actions by up to 60%, extending device operational time threefold with minimal performance loss [15].
Protocol 2: Preclinical Validation of Offset-Free Zone MPC in a Diabetic Rat Model
This protocol outlines the in vivo validation of an MPC algorithm, a critical step before human trials [16].
1. Objective: To validate the safety and efficacy of an impulsive, offset-free zone MPC (OF-ZMPC) in managing unannounced meals and plant-model mismatch in a live animal model.
2. Materials & Setup:
- Subjects: 14 male Wistar rats with streptozotocin (STZ)-induced diabetes.
- Devices: Commercial CGM sensor and a customized, low-cost insulin pump.
- Controller: OF-ZMPC, which uses a disturbance model to eliminate steady-state error.
3. Procedure:
- Day 0 - Induction & Device Installation: Induce diabetes via STZ. After stabilization, surgically implant the CGM and connect the insulin pump.
- Day 1 - Parameter Estimation:
- Administer a manual insulin bolus via the pump.
- Record the glucose response with the CGM.
- Perform off-line parameter estimation for the rat-specific glucose-insulin model.
- Day 2 - Controller Tuning:
- Use the estimated parameters to perform simulations for initial tuning of the OF-ZMPC and its state estimator.
- Conduct short in vivo tests to fine-tune controller parameters.
- Day 3-5 - Autonomous Trial:
- Initiate a 72-hour continuous, closed-loop operation of the i-AiDS.
- Provide food ad libitum (unannounced to the controller).
- Monitor and record glucose levels, insulin delivery, and animal health (e.g., body weight).
4. Key Analysis & Outcomes:
- Primary Endpoint: Percent Time in Range (80-180 mg/dL).
- Safety Metrics: Number of hypoglycemic events (<70 mg/dL) and severe hyperglycemic events.
- Model Fidelity: Median Absolute Relative Difference (MARD) between model predictions and CGM data.
- Conclusion: The controller achieved 83.4% TIR with no severe hypoglycemia, effectively handling unannounced meals and plant-model mismatch (MARD 24.66%), demonstrating robust preclinical performance [16].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for AiDS Research
| Item | Function/Description | Example/Citation |
|---|---|---|
| UVA/Padova T1DM Simulator | FDA-approved simulation platform for in-silico testing and validation of control algorithms without initial animal use. | [15] [16] |
| Hardware-in-the-Loop (HIL) Platform | Embedded system (e.g., Raspberry Pi) used to test control algorithms in a realistic hardware environment, measuring computational load and energy consumption. | [15] |
| Recursive Least Squares (RLS) Estimator | An adaptive algorithm used to estimate critical, time-varying patient parameters (e.g., insulin sensitivity) in real-time, improving controller personalization. | [15] |
| Offset-Free MPC Framework | An MPC formulation that incorporates a disturbance model to eliminate steady-state glucose errors caused by plant-model mismatch. | [16] |
| Meal Detection & Size Estimation Algorithm | A feed-forward component that identifies the occurrence and approximate carbohydrate content of unannounced meals, allowing for corrective bolusing. | [18] |
| Neural Network (NN) for MPC | A method to replicate complex MPC behavior using a lightweight, easy-to-deploy neural network, enabling implementation on resource-constrained devices. | [19] |
| Insulin-on-Board (IOB) Constraints | Safety constraints within the MPC optimizer that account for the active insulin from previous doses to prevent stacking and hypoglycemia. | [18] |
Advanced MPC Architecture: Meal Detection and IOB Safety
A critical advantage of MPC lies in its integration of safety modules and feed-forward mechanisms. The following diagram details the logic of the meal detection and IOB safety supervision system.
Diagram 2: Meal Detection and Safety Supervision Logic. This supervisory layer enhances the core MPC by adding feed-forward meal compensation and critical safety shut-offs to mitigate hypoglycemia risk.
The development of effective Model Predictive Control (MPC) algorithms for automated blood glucose regulation requires confronting significant physiological challenges that disrupt glucose homeostasis. Meal disturbances, physical activity, psychological and physical stress, and substantial inter-patient variability represent core obstacles that can compromise the performance and safety of artificial pancreas systems [3] [9]. This document details these challenges and provides structured experimental protocols to facilitate their systematic investigation, enabling the development of more robust, adaptive MPC frameworks capable of maintaining glycemic control amidst real-world variability.
Meal Disturbances
Physiological Impact and Quantitative Effects
Carbohydrate intake represents one of the most significant postprandial glycemic disturbances. The concept of Glycemic Load (GL) quantifies the glycemic impact of a meal by considering both the quality (Glycemic Index) and quantity of carbohydrates. A controlled study investigating the effects of high and low GL meals on individuals with different Body Mass Index (BMI) revealed critical data for modeling postprandial glucose dynamics [20].
Table 1: Blood Glucose Response to High vs. Low Glycemic Load Meals [20]
| BMI Group | Meal Type | Energy (kcal) | Peak BG Increase (Time) | BG Stability | P-value |
|---|---|---|---|---|---|
| Normal (BMI 18.5-24.9) | High GL (≥20) | 482 kcal | Significant at 60 min | Less Stable | < 0.05 |
| Normal (BMI 18.5-24.9) | Low GL (≤10) | 483 kcal | Lower increase | More Stable | < 0.05 |
| Overweight (BMI 25.0-29.9) | High GL (≥20) | 482 kcal | Significant at 90-120 min | Less Stable | < 0.05 |
| Overweight (BMI 25.0-29.9) | Low GL (≤10) | 483 kcal | Lower increase | More Stable | < 0.05 |
The study demonstrated that high GL meals produce a more pronounced and prolonged blood glucose elevation, particularly in overweight individuals, highlighting the interaction between meal composition and metabolic phenotype [20]. Furthermore, meal timing relative to circadian rhythms significantly influences glycemic control. Research shows that late-evening meals coinciding with elevated melatonin levels impair insulin secretion and glucose control, an effect exacerbated in carriers of the MTNR1B gene variant [21].
Experimental Protocol: Meal Challenge Studies
Objective: To characterize individual postprandial glycemic responses to standardized meals for personalizing MPC model parameters.
Methodology:
- Subject Preparation: Recruit subjects spanning different glycaemic statuses (normal, prediabetic, type 1 and type 2 diabetic). Instruct subjects to fast for 10-12 hours overnight.
- Test Meals: Prepare isocaloric meals (providing 25% of estimated daily energy requirement) with low (≤10) and high (≥20) Glycemic Load. Macronutrient composition should be standardized: Low GL meal (66% CHO, 17% protein, 17% fat); High GL meal (60% CHO, 10% protein, 30% fat) [20].
- Blood Sampling: Insert an intravenous catheter for frequent sampling. Collect baseline (0 min) capillary or venous blood samples. Administer the test meal and ensure consumption within 15 minutes. Collect subsequent blood samples at 15, 30, 45, 60, 90, and 120 minutes postprandial [20].
- Meal Timing Studies: For chronobiology studies, conduct identical protocols with early dinner (≥4 hours before bedtime) and late dinner (close to bedtime) conditions, measuring concomitant melatonin levels [21].
- Data Analysis: Plot glucose-time curves and calculate area under the curve (AUC). Model the glucose rise kinetics and identify time-to-peak for each subject group.
Exercise
Physiological Impact and Quantitative Effects
Physical activity influences glucose homeostasis through multiple, intensity-dependent mechanisms. Exercise enhances insulin sensitivity and stimulates insulin-independent glucose uptake via muscle contractions [22]. The effects, however, vary significantly with exercise modality and duration.
Table 2: Blood Glucose Responses to Different Exercise Modalities
| Exercise Modality | Intensity | Duration | Acute BG Effect (During) | BG Effect (Post-Exercise) | Key Physiological Mechanisms |
|---|---|---|---|---|---|
| Continuous Aerobic | Moderate (50-70% HRmax) | 30-60 min | Gradual decrease [22] | Increased insulin sensitivity for 24-72 hours [22] [23] | Increased GLUT4 translocation, enhanced insulin signaling [23] |
| High-Intensity Interval Training (HIIT) | Vigorous (≥80% VO₂max) | Brief bursts (e.g., 30s sprints) | Increase or stability [23] | Improved BG control for 24 hours (T2D) [23] | Catecholamine-driven hepatic glucose production, significant glycogen depletion [23] |
| Resistance Training | Variable | 60 min | Potential increase [24] | Improved long-term glycemic control (HbA1c) | Muscle mass development, transient hormonal responses |
High-Intensity Exercise (HIE) requires special consideration in MPC design. While it can cause transient hyperglycemia during and immediately after activity, it significantly improves glucose control for 24-72 hours post-exercise and carries a lower immediate risk of hypoglycemia compared to moderate-intensity exercise [23].
Experimental Protocol: Exercise Challenge Studies
Objective: To quantify the impact of various exercise modalities on glucose dynamics to inform disturbance models in MPC.
Methodology:
- Subject Preparation: Recruit subjects with diabetes (type 1 and type 2). Standardize meal timing and insulin administration prior to testing.
- Pre-Exercise Assessment: Check blood glucose 15-30 minutes before exercise. Do not exercise if BG >270 mg/dL with ketosis or <90 mg/dL; instead, administer 15-30g carbohydrates for low BG [24].
- Exercise Protocols:
- Moderate Aerobic: Cycle ergometry at 60-70% of maximum heart rate for 45 minutes.
- High-Intensity Interval Training (HIIT): Perform 4-6 cycles of 30-second "all-out" Wingate sprints on a cycle ergometer, separated by 4 minutes of rest [23].
- Resistance Training: Conduct a circuit of 8 exercises (e.g., leg press, chest press), 3 sets of 8-12 repetitions at 70-80% of one-repetition maximum.
- Monitoring: Measure blood glucose immediately before, every 15-30 minutes during, immediately after, and then hourly for 6-12 hours post-exercise. Use continuous glucose monitors (CGM) for dense data capture [24].
- Safety Measures: Have fast-acting carbohydrates (glucose tablets, juice) available to treat hypoglycemia (BG <70 mg/dL). Follow the 15-15 rule: consume 15g carbohydrates, wait 15 minutes, and recheck BG [22].
Figure 1: Exercise-Mediated Glucose Regulation Pathway
Stress
Physiological Impact and Quantitative Effects
Stress-Induced Hyperglycemia (SIH) is a common phenomenon in critically ill patients and during psychological stress, driven by neuroendocrine activation. SIH is defined as blood glucose >180 mg/dL in individuals without pre-existing diabetes and is associated with increased mortality, longer hospital stays, and higher complication rates [25].
The underlying pathophysiology involves two major systems:
- The Hypothalamic-Pituitary-Adrenal (HPA) Axis: Activation leads to increased cortisol secretion, which promotes gluconeogenesis and induces insulin resistance in peripheral tissues [26] [25].
- The Sympathoadrenal System: Releases catecholamines (epinephrine and norepinephrine), which further stimulate glycogenolysis and gluconeogenesis while suppressing insulin secretion [26].
Chronic stress perpetuates a vicious cycle of insulin resistance and β-cell dysfunction, significantly increasing the risk for developing type 2 diabetes [26]. Counter-regulatory hormones and pro-inflammatory cytokines (e.g., IL-6, TNF-α) work in concert to disturb glucose homeostasis by impairing insulin signaling and GLUT-4 translocation [25].
Experimental Protocol: Characterizing Stress-Induced Hyperglycemia
Objective: To quantify the glycemic and metabolic response to physiologic stress for integration into MPC stress models.
Methodology:
- Study Population: Include critically ill patients (e.g., post-cardiac surgery, severe infection) and/or healthy subjects under controlled psychological stress tests.
- Biomarker Assessment: On admission and at 24-hour intervals, collect blood samples for:
- Glucose (point-of-care and central lab)
- Counter-regulatory hormones: Cortisol, Catecholamines
- Inflammatory cytokines: IL-6, TNF-α
- Monitoring: Implement continuous glucose monitoring (CGM) or frequent capillary glucose checks (e.g., every 4-6 hours) to assess glycemic variability and identify hyperglycemic episodes [25].
- Insulin Sensitivity Assessment: Use validated methods like the Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) or hyperinsulinemic-euglycemic clamps in research settings to quantify insulin resistance.
- Data Correlation: Statistically correlate the magnitude and duration of hyperglycemia with the levels of stress biomarkers and clinical outcomes (e.g., length of stay, infection rates).
Figure 2: Stress-Induced Hyperglycemia Pathway
Inter-patient Variability
Inter-patient variability presents a fundamental challenge for "one-size-fits-all" MPC algorithms. This variability stems from a complex interplay of factors:
- Genetic Factors: Gene variants, such as the G-allele in the melatonin receptor-1b gene (MTNR1B), significantly affect glycemic responses to meal timing [21].
- Diabetes Type and Pathophysiology: Type 1 diabetes is characterized by absolute insulin deficiency, whereas type 2 diabetes is defined by insulin resistance and progressive β-cell dysfunction [26].
- Clinical Phenotype: Factors such as BMI, body composition, duration of diabetes, presence of diabetes-related complications, and beta-cell reserve capacity contribute to significant differences in insulin sensitivity and carbohydrate metabolism [20].
- Drug Therapies: Different medications (e.g., metformin, sulfonylureas, insulin) profoundly alter underlying physiology and glycemic responses [26].
The performance of personalized dosing strategies compared to clinician management is shown in the GLUCOSE study, where a distributional reinforcement learning algorithm achieved significantly higher Time in Range (TIR) when its recommendations were followed [27].
Experimental Protocol: Assessing Inter-patient Variability
Objective: To identify key sources of inter-patient variability and create patient stratification strategies for personalized MPC.
Methodology:
- Comprehensive Phenotyping:
- Clinical: Document age, sex, BMI, diabetes type and duration, body composition (DEXA scan).
- Metabolic: Perform Oral Glucose Tolerance Tests (OGTT) and hyperinsulinemic-euglycemic clamps to measure insulin sensitivity and secretion.
- Genetic: Sequence or genotype known variants associated with glycemic control (e.g., MTNR1B [21]).
- Lifestyle: Assess dietary patterns, physical activity levels, and sleep-wake cycles.
- Cluster Analysis: Use unsupervised machine learning (e.g., k-means clustering) on the phenotyping data to identify distinct subgroups of patients with similar physiological profiles.
- Model Personalization: For each cluster, identify individualized model parameters for MPC algorithms. Techniques may include Bayesian estimation or transfer learning to adapt a base model to individual patient data.
- In-silico Validation: Use a validated simulation platform (e.g., the UVA/Padova T1D Simulator) populated with virtual patients representing the identified clusters to test the robustness of MPC algorithms [3] [9].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Glucose Regulation Research
| Item | Function/Application | Example Use in Protocol |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Provides real-time, interstitial glucose readings at 1-5 minute intervals. | Dense glucose monitoring during meal, exercise, and stress challenges [27]. |
| Glucometer & Test Strips | Provides point-of-care capillary blood glucose measurements. | Calibration of CGM; backup glucose measurement during exercise [20] [24]. |
| Intravenous Insulin Infusion System | Precisely delivers regular insulin under controlled rates. | Implementation of MPC-derived insulin doses in closed-loop studies [3] [9]. |
| ELISA Kits (Cortisol, Catecholamines, Cytokines) | Quantifies specific biomarkers in serum/plasma. | Measuring stress hormones (cortisol, epinephrine) and inflammatory markers (IL-6, TNF-α) [26] [25]. |
| Standardized Meal Tests | Provides a consistent nutritional challenge to assess postprandial glucose metabolism. | Meal challenge studies with defined macronutrient composition and Glycemic Load [20]. |
| Cycle Ergometer / Treadmill | Provides a standardized and quantifiable exercise workload. | Conducting aerobic and high-intensity interval exercise protocols [23]. |
| Hyperinsulinemic-Euglycemic Clamp Equipment | The gold-standard method for quantifying insulin sensitivity in vivo. | Detailed metabolic phenotyping for inter-patient variability studies. |
| In-silico Patient Simulator | A computer model of the glucose-insulin system for testing algorithms. | Pre-clinical validation of MPC algorithms in a virtual population before human trials [3]. |
Addressing the physiological challenges of meal disturbances, exercise, stress, and inter-patient variability is paramount for the advancement of MPC in blood glucose regulation. The experimental protocols and data outlined herein provide a framework for systematically quantifying these disturbances and incorporating them into adaptive, personalized control models. Future research should focus on integrating real-time detection of these states (e.g., exercise, stress) and developing MPC frameworks that can automatically adapt to an individual's unique and dynamic physiology.
The global diabetes epidemic represents one of the most significant public health challenges of the 21st century, creating an urgent clinical imperative for advanced management strategies. For researchers developing blood glucose regulation algorithms, understanding the scale of this burden and the specific challenges in achieving glycemic control is fundamental. The growing prevalence of diabetes worldwide, coupled with persistent issues in treatment adherence and glucose management, provides a powerful justification for technological innovations such as model predictive control (MPC) systems. This application note synthesizes the most current global statistics on diabetes prevalence and analyzes the factors contributing to suboptimal glycemic control, with particular relevance to the development of automated insulin delivery systems.
Global Diabetes Burden: Quantitative Analysis
Current Prevalence and Projections
The global diabetes burden has reached alarming proportions, with recent estimates indicating a rapid acceleration in prevalence across both developed and developing nations. The data reveals a consistent upward trajectory that shows no signs of abating without significant intervention.
Table 1: Global Diabetes Prevalence Estimates and Projections
| Metric | 1995 | 2024/2025 | 2050 | Source |
|---|---|---|---|---|
| Global Adult Prevalence | 4.0% [28] | 11.1% (1 in 9 adults) [29] | 12.2% (1 in 8 adults) [29] | IDF Diabetes Atlas |
| Total Cases (Adults) | 135 million [28] | 589-590 million [29] | 853 million [29] | IDF Diabetes Atlas |
| Type 1 Diabetes Cases | - | 9.5 million (2025) [30] | 14.7 million (2040 projection) [30] | IDF/T1D Index |
| Undiagnosed Cases | - | 252 million (4 in 10 adults) [29] | - | IDF Diabetes Atlas |
The historical context reveals the dramatic scale of this increase, with global adult diabetes prevalence rising from 7% to 14% between 1990 and 2022—a doubling within just three decades [31]. This trend is particularly pronounced in low- and middle-income countries (LMICs), where 81% of people with diabetes now reside [29]. The analysis of untreated diabetes reveals even starker disparities, with approximately 450 million adults (59% of all cases) remaining untreated in 2022, 90% of whom live in LMICs [31].
Regional Variations and Risk Factors
The distribution of diabetes burden demonstrates significant geographical heterogeneity, with important implications for targeted intervention strategies. The WHO South-East Asia and Eastern Mediterranean Regions report the highest prevalence rates at approximately 20% among adults [31]. Type 2 diabetes, which constitutes over 90% of all cases, is driven by complex interactions between multiple factors including urbanization, aging populations, decreasing physical activity, and increasing overweight and obesity prevalence [29]. The structural determinants include socioeconomic transitions, marketing of unhealthy foods, and economic hardships that create barriers to healthy lifestyle choices [31].
Suboptimal Glycemic Control: Measurement and Contributing Factors
The Scope of Insulin Dosing Irregularities
For researchers developing MPC algorithms, understanding the very specific failures in current insulin administration protocols provides critical insight into the clinical problems requiring technological solutions. Recent empirical evidence demonstrates that suboptimal insulin dosing represents a significant barrier to glycemic control.
Table 2: Insulin Dosing Irregularities Among People with Diabetes (30-Day Recall)
| Dosing Irregularity | Basal Insulin | Bolus Insulin | Reported By |
|---|---|---|---|
| Missed Doses | 47.3% of patients (mean 3.5 ± 2.9 doses) [32] | 58.0% of patients (mean 5.0 ± 10.1 doses) [32] | Patient Report |
| Mistimed Doses | 47.3% of patients (mean 3.9 ± 4.3 doses) [32] | 51.0% of patients (mean 5.0 ± 7.1 doses) [32] | Patient Report |
| Miscalculated Doses | 47.5% of patients (mean 4.5 ± 5.0 doses) [32] | 63.3% of patients (mean 5.5 ± 7.5 doses) [32] | Patient Report |
This data from a 2025 study of German patients using analogue insulin pens reveals that nearly half of all patients experience significant deviations from their prescribed insulin regimens across multiple dimensions [32]. Healthcare professionals corroborate these findings, with ≥67% indicating that up to 30% of their patients miss, forget, skip, mistime, or miscalculate insulin doses within a 30-day period [32].
Underlying Causes and Consequences
The reasons for these dosing irregularities are multifaceted, including forgetting doses, disruptions to normal routines, being too busy or distracted, and uncertainty about appropriate dosing amounts [32]. These adherence challenges contribute directly to failure to achieve glycemic targets, with studies showing that over half of German type 2 diabetes patients fail to attain their HbA1c goals [32]. The consequences extend beyond suboptimal glucose control to include increased risks of hypoglycemia, heightened healthcare costs, and potentially all-cause mortality [32].
Experimental Protocol: Assessing Insulin Dosing Behaviors
Study Design and Methodology
To systematically investigate the scope and nature of insulin dosing irregularities, researchers can employ the following protocol adapted from contemporary studies in this domain:
Objective: To quantify the prevalence, frequency, and underlying reasons for suboptimal insulin dosing behaviors among people with diabetes using insulin pen devices.
Participant Recruitment:
- Target Population: 400 adults with diabetes (Type 1: n=100; Type 2: n=300) using analogue insulin pens
- Inclusion Criteria: Age ≥18 years; clinician-confirmed T1D or T2D diagnosis; current use of analogue insulin pens (basal-only or basal-bolus regimens)
- Exclusion Criteria: Current use of connection-enabled pen systems, caps, or sleeves
- Recruitment Quotas: Apply soft quotas for HbA1c levels (<7%: ≤25%; unknown HbA1c: ≤25%; recent diagnosis <6 months: ≤25%; pen use <6 months: ≤25%) to enhance generalizability
Healthcare Professional Cohort:
- Sample: 160 HCPs (general practitioners: n=80; specialists: n=80)
- Inclusion Criteria: ≥2 years experience; currently prescribing insulin for adults using insulin pens; actively seeing ≥5 such patients weekly
Assessment Instrument:
- Implement a 58-item questionnaire for people with diabetes and 53-item questionnaire for HCPs
- Develop questions through systematic literature review and consultation with diabetes advocates and key opinion leaders
- Pilot testing using virtual web-assisted telephone interviews followed by refinement
- Domains: Current treatment routines, insulin dosing behaviors, barriers to optimal dosing, potential solutions for dosing optimization
Data Collection:
- Modality: Cross-sectional, noninterventional, web-based survey
- Recall Period: 30 days for dosing behaviors
- Primary Metrics: Proportion reporting missed/mistimed/miscalculated doses; mean number of dosing errors; reasons for suboptimal dosing; suggested solutions
- Ethical Considerations: Secure approval from institutional review board; obtain electronic informed consent from all participants
Statistical Analysis Plan
- Descriptive Statistics: Calculate proportions, means, and standard deviations for dosing irregularities
- Stratified Analyses: Compare patterns between T1D and T2D populations; examine HCP versus patient perspectives
- Qualitative Analysis: Thematically analyze open-ended responses regarding barriers and solutions
Conceptual Framework: From Clinical Burden to Algorithmic Solutions
The relationship between the global diabetes burden and the imperative for advanced glucose control technologies can be visualized through the following conceptual workflow:
Figure 1: Conceptual workflow linking diabetes epidemiology to technological solutions. This diagram illustrates the pathway from the growing global diabetes burden to the clinical imperative for advanced glucose control technologies like MPC algorithms.
For investigators working at the intersection of diabetes epidemiology and glucose control algorithm development, the following resources represent essential components of the research toolkit:
Table 3: Research Reagent Solutions for Diabetes Investigation
| Resource Category | Specific Examples | Research Application |
|---|---|---|
| Data Resources | IDF Diabetes Atlas [29], T1D Index [30], NCD-RisC datasets [31] | Epidemiological analysis, burden quantification, trend projection |
| Assessment Tools | Insulin Dosing Questionnaires [32], HbA1c measurements, Continuous Glucose Monitoring [33] | Behavioral assessment, glycemic control evaluation, adherence measurement |
| Algorithm Development Platforms | MATLAB/Simulink [34], Model Predictive Control frameworks, Prescribed finite-time control systems [34] | Control algorithm design, simulation, validation |
| Clinical Validation Systems | Artificial Pancreas systems [34], Continuous Glucose Monitors [33], Connected insulin pens [32] | Algorithm testing, clinical trial implementation, performance verification |
These resources enable a comprehensive research approach that spans from understanding population-level disease patterns to implementing and testing precise interventional technologies. The integration of epidemiological data with engineering solutions represents the cutting edge of diabetes management research.
The compelling statistics on global diabetes prevalence and the documented challenges in achieving optimal glycemic control create an undeniable clinical imperative for advanced management solutions. For researchers developing MPC algorithms, these epidemiological realities provide both justification for their work and specific clinical problems requiring resolution. The integration of robust global burden data with precise understanding of insulin dosing failures enables the creation of targeted technological interventions that address the most pressing challenges in diabetes care today. Future research directions should focus on validating MPC systems in real-world settings, particularly in populations experiencing the greatest disparities in care and outcomes.
Algorithm Design Strategies and Implementation Frameworks
Model Predictive Control (MPC) has emerged as a dominant control strategy for Artificial Pancreas (AP) systems to automate insulin delivery for people with Type 1 Diabetes (T1D). Zone-MPC represents a significant advancement over setpoint-based MPC by regulating blood glucose to a safe target zone rather than a single value, acknowledging that all glucose levels within a clinically defined interval are equally acceptable [35]. This approach inherently provides robustness to plant-model mismatch, model bias, and Continuous Glucose Monitor (CGM) sensor errors because the controller intervenes only when glucose predictions indicate excursions outside the safe zone, reducing unnecessary control actions and hypoglycemia risk [35] [36].
The incorporation of asymmetric input costs represents a fundamental innovation in zone-MPC formulation, directly addressing the critical clinical challenge of the inherent asymmetry in diabetes management [35] [37]. This control strategy recognizes that the consequences of hypoglycemia are immediate and potentially severe (including seizures, coma, and death), while the effects of temporary hyperglycemia, though undesirable, are less acutely dangerous [36]. The asymmetric penalty structure enables independent tuning of the controller's response to hyperglycemia (through insulin delivery above basal rate) and hypoglycemia (through insulin reduction or suspension), facilitating a safety-first approach essential for outpatient AP deployment [35] [37].
Mathematical Formulation of Zone-MPC with Asymmetric Penalties
Core Optimization Problem
The zone-MPC algorithm computes the optimal insulin correction dose ( u_k ) at each discrete time step by solving a constrained optimization problem. The cost function penalizes both predicted glucose excursions from the target zone and control efforts, with the distinctive feature of asymmetric penalties on insulin delivery [35] [37] [38].
The standard formulation is:
[ J(xi, u{0:Nu-1}) := \sum{k=1}^{Np} zk^2 + \sum{k=0}^{Nu-1} (\hat{R}\hat{u}k^2 + \check{R}\check{u}k^2) ]
Subject to: System dynamics and safety constraints.
Where:
- ( Np ) and ( Nu ) represent the prediction and control horizons, respectively
- ( z_k ) represents the distance of the predicted glucose from the target zone
- ( \hat{u}k := \max(uk, 0) ) (insulin delivery above basal rate)
- ( \check{u}k := \min(uk, 0) ) (insulin reduction below basal rate)
- ( \hat{R} ) and ( \check{R} ) are the asymmetric penalty weights on positive and negative insulin deviations, respectively [37]
Asymmetric Input Cost Structure
The separation of insulin input costs into positive (( \hat{R} )) and negative (( \check{R} )) components enables independent controller tuning for hyperglycemia correction versus hypoglycemia prevention [37].
Table 1: Interpretation of Asymmetric Penalty Parameters in Zone-MPC
| Parameter | Mathematical Expression | Physiological Effect | Clinical Impact |
|---|---|---|---|
| Positive Input Penalty (( \hat{R} )) | Penalizes ( \hat{u}k = \max(uk, 0) ) | Modulates insulin delivery above basal rate | Higher values make the controller less aggressive in correcting hyperglycemia |
| Negative Input Penalty (( \check{R} )) | Penalizes ( \check{u}k = \min(uk, 0) ) | Modulates insulin reduction below basal rate | Higher values make the controller less likely to suspend insulin delivery when glucose is falling |
This formulation allows the control system to perform predictive pump suspension when hypoglycemia is imminent (by favoring negative ( u_k ) values when glucose is predicted to fall below the target zone) and subsequent predictive pump resumption once the hypoglycemia risk subsides [35].
Figure 1: Zone-MPC with asymmetric penalties logical workflow. The controller executes every 5 minutes, using state estimation and glucose prediction to solve an optimization problem that incorporates asymmetric penalties on insulin delivery above and below basal rate.
Quantitative Parameter Configurations and Performance Metrics
Controller Tuning Strategies
The asymmetric penalty parameters (( \hat{R} ), ( \check{R} )) can be configured to achieve different controller aggressiveness profiles, allowing customization based on patient needs and safety requirements [37].
Table 2: Zone-MPC Tuning Configurations with Asymmetric Penalties
| Controller Profile | ( \hat{R} ) Value | ( \check{R} ) Value | Hyperglycemia Response | Hypoglycemia Response | Clinical Scenario |
|---|---|---|---|---|---|
| Aggressive | 800 | 500 | Fast correction | Slow to suspend insulin | Conservative hypoglycemia prevention strategy |
| Moderate (Default) | 7,000 | 100 | Balanced correction | Moderately responsive suspension | General outpatient use |
| Conservative | 50,000 | 10 | Slow correction | Fast pump suspension | High hypoglycemia risk patients |
Advanced Adaptive Tuning Strategies
Recent research has introduced glucose- and velocity-dependent control penalties that dynamically adjust ( \hat{R} ) and ( \check{R} ) based on predicted glucose values (( yk )) and their rate of change (( \muk )) [38]. The modified cost function becomes:
[ J(\cdot) := \sum{k=1}^{Np} (\check{z}k^2 + Q(vk)\hat{z}k^2 + \hat{D}\hat{v}k^2) + \sum{k=0}^{Nu-1} (\hat{R}(\muk,yk)\hat{u}k^2 + \check{R}(\muk,yk)\check{u}k^2) ]
This adaptive approach enables more aggressive hyperglycemia correction when glucose levels are high and rising, while implementing more conservative responses when glucose is falling or near the hypoglycemia threshold [38]. Clinical evaluations demonstrate that this method significantly improves mean glucose (153.8 mg/dL vs. 159.0 mg/dL; p < 0.001) and time in target range [70, 180] mg/dL (70.5% vs. 66.3%; p < 0.001) without increasing hypoglycemia risk [38].
Experimental Protocols and Validation Methodologies
In Silico Testing Protocol
The UVA/Padova T1D Simulator, accepted by the FDA as a substitute for animal trials, provides the standard platform for preclinical validation of zone-MPC algorithms [35] [37] [39].
Protocol 1: Comprehensive In Silico Validation
- Subject Cohort: Utilize all 100 adult in-silico subjects of the UVA/Padova simulator to capture inter-subject variability [38]
- Meal Scenarios:
- 3 meals per day with increasing carbohydrate loads (50g, 75g, 100g)
- Test both announced and unannounced meal conditions
- Include meal-bolus mismatches (±30%, ±50%) to simulate real-world estimation errors [38]
- Controller Configurations: Compare asymmetric zone-MPC against:
- Performance Metrics:
Clinical Trial Protocol
Following successful in-silico testing, the zone-MPC with asymmetric penalties has been validated in FDA-approved clinical trials [35] [36].
Protocol 2: Clinical Validation Study
- Subject Recruitment: 32 adults with T1D, each completing two 25-hour closed-loop sessions [35]
- System Configuration:
- Portable Artificial Pancreas System (pAPS) running zone-MPC algorithm
- Diurnal target zone: [80, 140] mg/dL (day), [110, 170] mg/dL (night)
- Diurnal input constraint: Nighttime insulin limited to 1.8× basal rate [35]
- Meal Management:
- Mixed meal conditions (announced and unannounced)
- Option for meal-bolusing based on standard insulin-to-carbohydrate ratio [35]
- Safety Monitoring:
- Continuous clinical supervision
- Protocol for hypoglycemia rescue (carbohydrate administration or intravenous glucose)
- Pump suspension and resumption logging [35]
Figure 2: Experimental validation pathway for Zone-MPC with asymmetric penalties, showing the progression from in-silico testing to clinical trials.
Table 3: Key Research Reagents and Computational Tools for Zone-MPC Development
| Resource Category | Specific Tool/Platform | Function in Research | Key Features/Parameters |
|---|---|---|---|
| Metabolic Simulator | UVA/Padova T1D Simulator | Preclinical algorithm validation | 100-adult cohort; FDA-accepted; meal and exercise scenarios [37] [39] |
| Control Algorithm | Zone-MPC with asymmetric costs | Core control logic | ( \hat{R} ), ( \check{R} ) parameters; diurnal zones; velocity-weighting [35] [38] |
| State Estimation | Luenberger Observer | State variable estimation | Recursive formulation; tuning parameters Q, R [35] |
| CGM Model | Integrated CGM Simulator | Glucose measurement simulation | MARD <10%; realistic sensor noise [37] |
| Performance Analysis | Custom MATLAB Scripts | Statistical analysis and visualization | Time-in-range; hypoglycemia events; control variability [37] |
Performance Outcomes and Clinical Implications
The zone-MPC formulation with asymmetric penalties demonstrates significant clinical advantages in both in-silico and clinical settings. The adaptive version shows statistically significant improvements in mean glucose (153.8 mg/dL vs. 159.0 mg/dL; p < 0.001) and time in range [70, 180] mg/dL (70.5% vs. 66.3%; p < 0.001) compared to standard zone-MPC, without increasing hypoglycemia risk [38].
The algorithm's capability for predictive pump suspension before impending hypoglycemia and subsequent predictive resumption addresses a critical safety requirement for outpatient AP systems, particularly during nighttime when patients cannot respond to alarms [35]. Furthermore, the independent tuning of hyperglycemia and hypoglycemia responses enables personalized therapy adaptations for specific patient populations, as demonstrated in pregnancy-specific zone-MPC implementations with tighter target zones (80-110 mg/dL daytime; 80-100 mg/dL overnight) [40].
The robustness of the control strategy has been verified under challenging conditions including meal-bolus mismatches, basal-rate inaccuracies, and unannounced exercise, maintaining safety across a broad spectrum of real-world scenarios [38]. This performance profile makes zone-MPC with asymmetric penalties a promising foundation for fully automated insulin delivery systems that minimize user burden while maximizing safety.
Model Predictive Control (MPC) has emerged as a leading control strategy for artificial pancreas (AP) systems in the management of Type 1 Diabetes (T1D). A fundamental challenge in MPC performance is the inherent plant-model mismatch caused by complex, time-varying patient physiology. Adaptive MPC strategies that dynamically adjust controller parameters based on real-time model accuracy offer a promising solution to this problem. This Application Note details a specific adaptive methodology that uses prediction residual analysis and a computed Trust Index to automatically modulate controller aggressiveness, enhancing both safety and effectiveness in blood glucose regulation. This approach is situated within a broader thesis that posits adaptive control is essential for achieving robust, personalized glucose control in free-living conditions.
Core Methodology
The adaptive algorithm quantifies the accuracy of the glucose prediction model by analyzing the history of prediction residuals and translates this accuracy into a dynamic tuning parameter for the MPC's cost function.
Prediction Residual Analysis
The first step involves the systematic collection and weighting of prediction residuals. For a current time ( t ), the residual for a prediction made ( k ) steps earlier is defined as: [ resk^t = y{t|t-k} - Gt ] where ( y{t|t-k} ) is the glucose prediction made at time ( t-k ) for the current time ( t ), and ( G_t ) is the current measured glucose value [37].
A pool of the most recent ( Nf ) residuals (e.g., ( Nf = 60 )) is maintained for each prediction step ( k ) across the prediction horizon ( Np ). To prioritize recent data, these residuals are penalized using a logarithmic forgetting function: [ \widetilde{res}{k,i}^{\,t} = resk^{\,t-i} \cdot \frac{\log(Nf - i + 1)}{\log Nf} ] where ( i ) indexes the historical data, making older residuals progressively less significant [37]. This creates a time-varying matrix of penalized residuals, ( \widetilde{res}{k,i}^{\,t} ), which serves as an empirical sample of the error distribution for the prediction model.
Trust Index and Confidence Interval Estimation
The Trust Index is derived empirically from the distribution of the penalized residuals. For each prediction step ( k ), the 5th and 95th percentiles of the penalized residual sample are calculated to establish a confidence interval for the prediction error: [ \breve{B}k = \min(\text{percentile}{5}(\widetilde{res}{k}^{\,t}), 0) \quad \text{and} \quad \widehat{B}k = \max(\text{percentile}{95}(\widetilde{res}{k}^{\,t}), 0) ] Here, ( \breve{B}k ) and ( \widehat{B}k ) represent the lower and upper bounds of the confidence interval, respectively [37]. A narrow confidence interval indicates high confidence in the model's predictions, whereas a wide interval indicates low confidence.
Dynamic MPC Tuning
In a Zone-MPC framework, the cost function typically penalizes glucose deviations from a target zone and insulin delivery deviations from a basal rate. The adaptive strategy dynamically adjusts the insulin penalties, ( \hat{R} ) (penalizing insulin delivery above basal) and ( \breve{R} ) (penalizing insulin suspension below basal), based on the Trust Index [37] [41].
- High Trust (Accurate Predictions): The controller is allowed to be more aggressive. The penalties ( \hat{R} ) and ( \breve{R} ) are decreased, enabling the controller to respond more vigorously to correct hyperglycemia and be less quick to suspend insulin, thereby improving overall glycemic control.
- Low Trust (Inaccurate Predictions): The controller becomes more conservative. The penalties ( \hat{R} ) and ( \breve{R} ) are increased. This results in less insulin delivery to counter hyperglycemia and a faster suspension of insulin to prevent hypoglycemia, prioritizing patient safety.
This dynamic adjustment creates a feedback loop where the controller's aggressiveness is continuously optimized based on its recent performance [37].
Experimental Protocol and Validation
In-Silico Validation Setup
- Simulator: The University of Virginia/Padova T1D Metabolic Simulator, accepted by the FDA for pre-clinical trials, is the standard for in-silico validation. It incorporates 10 virtual subjects representing inter-patient variability [37] [9].
- Simulation Scenario: Simulations typically cover 24 hours or more, involving multiple meals of varying carbohydrate loads (e.g., 50 g, 75 g, 100 g). A 2-hour open-loop warm-up period precedes closed-loop operation [37].
- Meal Compensation Strategies:
- Announced Meals: The patient enters the carbohydrate count, and the system delivers a meal bolus based on the patient's insulin-to-carbohydrate ratio [37].
- Unannounced Meals: The controller relies on a meal detection algorithm (e.g., a Glucose Rate Increase Detector - GRID) to trigger a compensation bolus [37].
- Comparative Controllers: The adaptive MPC should be compared against non-adaptive MPCs with fixed aggressive (e.g., ( \hat{R}=800, \breve{R}=500 )) and conservative (e.g., ( \hat{R}=500, \breve{R}=50000 )) tunings [37].
Performance Metrics and Outcomes
Key glycemic outcomes must be evaluated to assess the algorithm's performance. The following table summarizes expected outcomes based on published studies, demonstrating the adaptive controller's ability to maintain efficacy while significantly enhancing safety [37] [4].
Table 1: Expected Glycemic Outcomes for Adaptive vs. Non-Adaptive MPC (24-hour in-silico study)
| Performance Metric | Target Range | Adaptive MPC | Aggressive MPC | Conservative MPC |
|---|---|---|---|---|
| Time in Range (TIR) | 70-180 mg/dL | Similar high performance (~75%) | High | Lower |
| Time in Hypoglycemia | <70 mg/dL | Significantly Reduced (~71.7% reduction) | Higher risk | Lowest |
| Time in Hyperglycemia | >180 mg/dL | Similar reduction to aggressive | Lower | Higher |
| Average Glucose | ~130 mg/dL | Similar | Similar | Potentially higher |
| Insulin Delivery | Patient-specific | Similar or reduced | Higher | Lower |
| Controller-Induced Hypoglycemia | N/A | Minimal | Present | Absent |
The Scientist's Toolkit: Research Reagent Solutions
The following table lists essential components for developing and testing an adaptive MPC system for an artificial pancreas.
Table 2: Essential Research Materials and Tools
| Item | Function/Description | Example/Note |
|---|---|---|
| UVa/Padova T1D Simulator | A widely accepted platform for in-silico testing and validation of control algorithms using a cohort of virtual patients. | FDA-approved substitute for animal trials [37]. |
| Continuous Glucose Monitor (CGM) | Provides real-time, subcutaneous glucose measurements, the primary input for the MPC algorithm. | Models with time lag and measurement noise should be used for realistic simulation [37] [5]. |
| Zone-MPC Algorithm | The core control algorithm that calculates optimal insulin delivery to maintain glucose in a target zone. | Asymmetric cost function allows independent tuning of responses to high and low glucose [37]. |
| Logarithmic Forgetting Function | A mathematical operator to weight recent prediction residuals more heavily than older ones for the Trust Index calculation. | Implementation choice: ( \frac{\log(Nf - i + 1)}{\log Nf} ) [37]. |
| Meal Detection Algorithm | A safety module that detects rapid glucose rises indicative of an unannounced meal to trigger a corrective bolus. | e.g., Glucose Rate Increase Detector (GRID) [37]. |
| Insulin Sensitivity Adaptation | A complementary run-to-run algorithm that updates the patient's insulin sensitivity factor in the MPC model. | Further reduces model-patient mismatch over a longer timescale (days) [41]. |
Workflow and System Diagrams
The following diagram illustrates the logical flow and integration of the Trust Index analysis within the adaptive MPC framework.
Figure 1: Adaptive MPC Workflow with Trust Index Analysis. The core adaptive loop (red/blue) analyzes past prediction performance to dynamically tune the MPC's aggressiveness before computing the next insulin dose.
The second diagram details the data structure and process for calculating the Trust Index from the history of prediction residuals.
Figure 2: Trust Index Calculation from Residual History. Historical prediction residuals are weighted and analyzed to compute a confidence interval, the width of which defines the Trust Index.
Within artificial pancreas systems, Model Predictive Control (MPC) has emerged as a dominant strategy for automated insulin delivery. The core principle of MPC relies on using an internal model to predict future glucose trajectories and compute optimal insulin doses [39]. The performance of these systems is therefore inherently dependent on the accuracy of their glucose forecasts. Long Short-Term Memory (LSTM) networks, a class of recurrent neural networks, are particularly suited for this task due to their ability to model complex, nonlinear temporal dependencies in physiological data, offering a significant advantage over traditional physiological and linear time-series models [42] [43]. These data-driven models can learn individual glucose patterns from historical data, leading to more personalized and adaptive predictions crucial for effective and safe MPC operation [42] [44]. This protocol details the application of LSTM networks for multi-step-ahead glucose prediction, providing a framework for researchers to develop robust prediction engines for next-generation MPC algorithms.
LSTM Performance & Comparative Analysis
Evaluating LSTM performance against other data-driven approaches and established benchmarks is critical for model selection in MPC research. The following tables summarize key quantitative findings from recent studies.
Table 1: Comparative Performance of LSTM vs. Other Models for Glucose Prediction (Type 1 Diabetes)
| Model | Prediction Horizon (PH) | RMSE (mg/dL) | Key Dataset | Context/Notes |
|---|---|---|---|---|
| LSTM (Personalized) | 60 min | 22.52 ± 6.38 | HUPA UCM | Trained on individual data only [42] |
| LSTM (Aggregated) | 60 min | 20.50 ± 5.66 | HUPA UCM | Trained on pooled population data [42] |
| LSTM-XGBoost Fusion | 30 min | 6.45 | OhioT1DM | Integrated temporal features [43] |
| LSTM-XGBoost Fusion | 60 min | 17.24 | OhioT1DM | Integrated temporal features [43] |
| Traditional ML | 30-60 min | Best Overall | OhioT1DM | Outperformed CTF and DNN in a comprehensive analysis [44] |
| Neural Network Model (NNM) | 45 min | 21.27 ± 5.17 | Multiple (Meta-analysis) | Highest relative performance in network meta-analysis [45] |
Table 2: Impact of Input Features and Conditions on Prediction Accuracy
| Factor | Impact on Prediction Performance (RMSE) | Citation |
|---|---|---|
| Multivariate Input (Carbs, Insulin, Activity) | Mixed results; can improve accuracy but not universally. Data fusion techniques may be needed to effectively leverage information. | [44] |
| Free-Living Exercise | 30-min PH RMSE: Median 16.85 mg/dL, Mean 17.74 mg/dL (Best model per patient). Errors remained in clinically safe zones. | [46] |
| Personalized vs. Aggregated Training | Personalized models achieved comparable accuracy to aggregated models despite using less data (e.g., 22.52 vs. 20.50 mg/dL at 60-min PH). | [42] |
| Increasing Prediction Horizon | RMSE increases with longer PH (e.g., 18.88 mg/dL at 15 min vs. 30.01 mg/dL at 60 min in meta-analysis). | [45] |
Experimental Protocol: LSTM Model Development for MPC
This protocol provides a step-by-step methodology for developing a personalized LSTM model for multi-step-ahead glucose prediction, suitable for integration into an MPC framework.
Data Acquisition and Preprocessing
- Data Sources: Utilize publicly available datasets such as the OhioT1DM Dataset [44] or the HUPA UCM Dataset [42]. These typically contain CGM readings, insulin doses (basal and bolus), carbohydrate intake, and sometimes physical activity metrics, all recorded at 5-minute intervals.
- Data Preprocessing:
- Imputation and Alignment: Address missing CGM values using linear interpolation for training data and extrapolation for testing data. Align all temporal data (e.g., physical activity, meals) to the 5-minute CGM timestamps. Assign zero to carbohydrates and insulin for timestamps with no reported data [44].
- Normalization: Normalize all input features (e.g., CGM, carbs, insulin) to a common scale, typically [0, 1], using min-max scaling or Z-score standardization. This stabilizes and accelerates LSTM training.
- Supervised Learning Reframing: Structure the time-series data into input-output pairs for supervised learning. For a 180-minute lookback window and a 60-minute (12-step) prediction horizon, each input sample is a matrix of shape
(36, N_features)and the corresponding output is a vector of shape(12,)representing the future 12 glucose values [42].
LSTM Model Architecture and Training
- Model Formulation: Frame the task as a sequence-to-sequence regression problem. The model maps a historical sequence of physiological data to a future sequence of glucose values.
- Architecture Specification:
- Input Layer: Accepts a sequence of 36 time steps (180 minutes) with
N_features(e.g., 4 for glucose, carbs, bolus insulin, basal insulin). - LSTM Layer: A single LSTM layer with 50 hidden units and
tanhactivation is a recommended starting point, balancing performance and computational cost [42]. - Output Layer: A fully connected (Dense) layer with 12 units and a linear activation function to output the 12 predicted glucose values (60-minute horizon) [42].
- Input Layer: Accepts a sequence of 36 time steps (180 minutes) with
- Training Procedure:
- Data Splitting: Chronologically split each patient's data into training (60%), validation (20%), and testing (20%) sets.
- Loss Function and Optimizer: Use Mean Squared Error (MSE) as the loss function and the Adam optimizer with a learning rate of 0.001 [42].
- Training Regimen: Train for 50 epochs with a batch size of 32. Employ a validation-based early stopping callback to halt training if validation loss does not improve for a set number of epochs, preventing overfitting.
- Training Strategy: For personalized models, train one model per patient on their own data. For aggregated models, combine training data from all patients before training a single model [42].
Model Evaluation and Integration with MPC
- Performance Metrics:
- Primary Metric: Root Mean Square Error (RMSE) in mg/dL. Calculate this for the entire test set and for specific prediction horizons (e.g., 30-min, 60-min) [42] [44].
- Clinical Metric: Use the Clarke Error Grid (CEG) analysis to categorize predictions into clinically accurate (Zones A & B) versus erroneous (Zones C, D, E) zones [46] [42].
- Integration into MPC: The trained LSTM model serves as the internal prediction model within the MPC's cost function. At each control cycle (e.g., every 5 minutes), the MPC uses the LSTM's predicted glucose trajectory over the prediction horizon to compute the insulin dose that minimizes future glucose deviations from the target range while respecting safety constraints [39].
Schematic Workflows
LSTM-Based MPC Control Loop
This diagram illustrates the closed-loop integration of the LSTM predictor within an MPC algorithm for automated insulin delivery.
LSTM Model Training Strategy
This diagram outlines the two primary training strategies for LSTM glucose prediction models: personalized and aggregated.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for LSTM-Based Glucose Prediction Research
| Resource / Reagent | Type | Function in Research | Exemplar / Standard |
|---|---|---|---|
| Continuous Glucose Monitoring (CGM) Data | Data Source | Primary time-series input for model training and prediction; reflects subcutaneous glucose concentrations. | Medtronic Enlite Sensor [44], Dexcom G-series |
| Insulin Pump Records | Data Source | Provides history of insulin delivery (basal & bolus), a critical exogenous input for the model. | Tandem t:slim X2, OmniPod [39] |
| In Silico T1D Simulator | Software Tool | Enables cost-effective, large-scale, and safe testing of LSTM-MPC algorithms on virtual patient cohorts. | FDA-approved UVA/Padova T1D Simulator [39] [17] |
| Public Clinical Datasets | Data Source | Provides standardized, annotated real-world data for model training, benchmarking, and validation. | OhioT1DM Dataset [44], HUPA UCM Dataset [42] |
| Deep Learning Framework | Software Library | Provides the programming environment for building, training, and evaluating LSTM neural networks. | TensorFlow/Keras [42], PyTorch |
| Federated Learning Platform | Software Framework | Enables training of models across decentralized data sources (e.g., multiple patient devices) while preserving data privacy [17]. | PySyft, TensorFlow Federated |
The management of blood glucose concentration in individuals with Type 1 Diabetes (T1D) is a complex challenge, characterized by significant inter- and intra-individual variability in physiological responses. Model Predictive Control (MPC) has emerged as a leading algorithm for automated insulin delivery in Artificial Pancreas (AP) systems. The core principle of MPC is to use a model of the glucose-insulin dynamics to proactively compute optimal insulin doses that will maintain glycemia within a safe target range. The performance and safety of these systems are profoundly dependent on the ability of the underlying model to capture individual patient characteristics. Personalization is, therefore, not an enhancement but a necessity for effective glucose regulation. This document details application notes and protocols for incorporating two critical personalization elements into MPC algorithms: individual basal insulin profiles and insulin sensitivity. These techniques address the fundamental sources of variability among patients, moving from a one-size-fits-all approach to a tailored therapeutic strategy that can improve time-in-range and reduce hypoglycemic events [47] [48].
Personalizing Basal Insulin Profiles
Basal insulin secretion in healthy individuals is not constant but exhibits diurnal variations, with characteristic peaks such as the "dawn" and "dusk" phenomena. Replicating this pattern is a cornerstone of physiological insulin replacement in T1D.
Quantitative Foundations of Basal Rate Variability
Data from studies of patients with T1D on insulin pump therapy reveal substantial heterogeneity in basal rate requirements. The following table summarizes key findings from a study that developed a model to predict individual basal rate profiles based on clinical characteristics [49].
Table 1: Key Findings from Basal Rate Profiling Study
| Parameter | Value / Finding | Context and Significance |
|---|---|---|
| Overall Basal Insulin Dose | 0.27 ± 0.01 IU∙d⁻¹∙kg⁻¹ | Mean daily basal insulin requirement per kilogram of body weight. |
| Circadian Variations | Peaks corresponding to "dawn" and "dusk" phenomena. | Confirms the non-constant nature of insulin needs throughout the day. |
| Key Predictive Variables | Age, gender, duration of pump treatment, body-mass-index (BMI), HbA1c, triacylglycerol concentrations. | Clinical parameters that explain a significant portion of the variability in basal demand. |
| Model Performance (r²) | 0.518 (P < .0001) | The multivariate regression model explained 51.8% of the variation in individual basal insulin demand per day. |
| Model Validation | No significant difference between model-predicted and actual basal rates in exploratory (Δ 0.1 IU/d) or confirmatory (Δ -0.5 IU/d) cohorts. | Demonstrates the model's accuracy and generalizability to new patient populations. |
Protocol for Deriving and Validating a Personalized Basal Profile
The following workflow outlines the process for generating and validating a patient-specific basal profile, suitable for initializing an MPC algorithm.
Title: Personalized Basal Profile Derivation
Protocol Steps:
Patient Cohort Selection:
- Inclusion Criteria: Patients with T1D, aged 16-80 years, on continuous subcutaneous insulin infusion (CSII) therapy [49].
- Exclusion Criteria: Non-type 1 diabetes, pregnancy, inability to perform a 24-hour fasting test.
Data Collection and Clinical Characterization:
- Extract and record patient characteristics identified as key predictive variables (see Table 1) [49].
Empirical Basal Rate Determination via 24-Hour Basal Rate Test (BRT):
- Procedure: Initiate a supervised 24-hour fasting period, typically starting at 6:00 PM. Omit dinner, breakfast, lunch, and all snacks.
- Safety Monitoring: Plasma glucose is monitored continuously. Fasting is interrupted only if carbohydrate intake is required to treat hypoglycemia (plasma glucose < 3.9 mmol/L) [49].
- Outcome: The individual's hourly basal insulin infusion rates are carefully adjusted to maintain stable euglycemia throughout the fast, thereby establishing a validated, patient-specific 24-hour basal profile.
Predictive Model Generation and Validation:
- Exploratory Phase: Randomly assign a subset of the cohort (e.g., 170 patients). Perform a multivariate regression analysis to relate the clinical characteristics from Step 2 to the empirically determined basal rates from Step 3.
- Validation Phase: Apply the generated mathematical algorithm to a separate, confirmatory cohort (e.g., 169 patients). Compare the model-predicted basal profiles to the actual BRT-validated profiles to confirm accuracy [49].
Integration into MPC:
- The finalized personalized basal profile is not used as a static delivery schedule but is incorporated into the MPC's internal model. It serves as the nominal baseline insulin infusion rate around which the controller makes dynamic adjustments based on real-time glucose predictions.
Integrating Insulin Sensitivity and Pharmacokinetic/Pharmacodynamic Profiles
Insulin sensitivity (IS) defines the responsiveness of tissues to the glucose-lowering effect of insulin. It is a major source of inter-individual variability and can fluctuate within an individual over time. Similarly, the pharmacokinetic (PK; absorption, distribution, metabolism) and pharmacodynamic (PD; physiological effect) profiles of subcutaneously administered insulin introduce critical delays that the controller must account for.
Modeling Insulin Time-Action Profiles
Model-based simulations of insulin PK/PD profiles are essential for understanding and predicting the time course of insulin action. Population PK models can be developed using data from euglycemic clamp studies to characterize various insulin formulations [50].
Table 2: Examples of Insulin Formulations and Their Characteristics
| Insulin Formulation | Type / Onset | Primary Clinical Use | Relevant PK/PD Model Inputs |
|---|---|---|---|
| Insulin Glargine [50] | Long-Acting / Slow | Basal insulin replacement | Dose (U or U/kg), body weight, timing of administration. |
| Neutral Protamine Hagedorn (NPH) [50] | Intermediate-Acting / Moderate | Basal insulin replacement | Dose (U or U/kg), body weight. |
| Insulin Lispro [50] | Rapid-Acting / Fast | Prandial (mealtime) bolus | Dose (U or U/kg), time of administration relative to a meal. |
| Human Regular Insulin [50] | Short-Acting / Slower | Prandial (mealtime) bolus | Dose (U or U/kg), time of administration relative to a meal. |
| Premixed Formulations (e.g., Mix 70/30, Mix 75/25) [50] | Biphasic / Dual | Combined basal and prandial coverage | Total dose (U or U/kg), component ratios. |
Protocol for Adaptive MPC with Personalized Models and Rules
Advanced MPC formulations go beyond static models by incorporating adaptive mechanisms that personalize the controller itself in response to changing patient dynamics.
Title: Adaptive MPC Control Cycle
Protocol Steps:
Model Personalization:
- Technique: Employ a Regularized Partial Least Squares (rPLS) model. This is a latent variable model that is particularly effective for handling highly correlated data from multiple variables (e.g., historical glucose, insulin, meal data) [48].
- Incorporating Prior Knowledge: Explicitly encode physiological knowledge, such as the exponential stability of the glycemic system, into the rPLS model. This improves prediction reliability by ensuring model weights decrease exponentially over the past data window, balancing complexity and flexibility [48].
Robustness to Real-World Data Issues:
- Missing Data Framework: Implement a prediction framework that allows the model to generate glucose forecasts even during short-term dropouts in CGM data (e.g., up to 30 minutes), preventing controller failure during signal loss [48].
Adaptive Control Tuning:
- Evaluation: Continuously assess the recent performance of the controller, using metrics like percentage of time in the target range (70-180 mg/dL) and glycemic variability [48].
- Adaptive Laws: Develop personalized rules to automatically adjust the hyperparameters of the MPC. For example:
- If the patient is trending towards hyperglycemia with low variability, the controller can become more aggressive by increasing the penalty on glucose deviations in the cost function.
- If the patient is trending towards hypoglycemia or exhibits high glucose variability, the controller can become more conservative by tightening constraints on the maximum allowable insulin infusion rate [48].
- This adaptive strategy allows the MPC to respond proactively to time-varying changes in insulin sensitivity caused by factors like stress, hormones, or physical activity.
Experimental Validation Protocols
In-Silico Validation Using the UVa/Padova T1D Simulator
The UVa/Padova T1D Simulator is a widely accepted platform for the pre-clinical testing of AP algorithms.
- Objective: To compare the performance of different personalization strategies for MPC in a controlled, virtual environment [47].
- Procedure:
- Cohort Selection: Simulate a large cohort of virtual patients (e.g., 100 subjects) representing a broad population with T1D.
- Algorithm Testing: Test the following MPC configurations:
- Non-personalized MPC: Uses a generic, average population model.
- Cost-Function Personalized MPC: Uses a generic model but with a personalized cost function.
- Model-Personalized MPC: Uses a model personalized to each virtual subject (e.g., based on the techniques in Sections 2 and 3).
- Fully Personalized MPC: Uses both a personalized model and a personalized cost function [47].
- Scenario Simulation: Run simulations with standardized meal challenges, varying insulin sensitivities, and potentially unannounced meals.
- Outcome Measures:
- Primary: Mean glucose; Percentage of time in target range (70-180 mg/dL); Percentage of time in hypoglycemia (<70 mg/dL) and hyperglycemia (>180 mg/dL).
- Secondary: Total daily insulin dose; Glucose variability (Standard Deviation).
Clinical Validation in a Randomized Controlled Trial (RCT)
Following successful in-silico testing, clinical trials are essential for validation.
- Objective: To compare the efficacy and safety of a personalized MPC algorithm against a routine glucose management protocol in a patient population [51].
- Design: A randomized, controlled, parallel-group study.
- Participants: 60 elective cardiac surgery patients with T1D (or stress-induced hyperglycemia) [51].
- Intervention:
- Experimental Group (n=30): Glucose control managed by the personalized MPC algorithm with a variable blood glucose sampling rate.
- Control Group (n=30): Glucose control managed by a routine glucose management protocol (e.g., sliding scale insulin with fixed sampling) [51].
- Outcome Measures:
- Efficacy: Mean blood glucose; Percentage of time in the target range (e.g., 4.4-6.1 mmol/L).
- Safety: Number of hypoglycemic events (e.g., blood glucose < 2.9 mmol/L); Total insulin infusion rate [51].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for MPC Personalization Research
| Item / Reagent | Function / Description | Example / Reference |
|---|---|---|
| UVa/Padova T1D Simulator | A mathematical simulator of the glucose-insulin system that provides a virtual patient population for in-silico testing and validation of control algorithms. | Accepted by the FDA as a substitute for animal trials in pre-clinical testing [47]. |
| Insulin Formulations | Various rapid-, short-, intermediate-, and long-acting insulins with distinct PK/PD profiles used to model and mimic physiological secretion. | Insulin Glargine, Lispro, NPH, Human Regular [50]. |
| Continuous Glucose Monitor (CGM) | A device that measures subcutaneous glucose concentrations at regular intervals (e.g., every 5 minutes), providing the essential feedback signal for the MPC. | Data used for recursive model updating and adaptive control [48]. |
| Population PK/PD Modeling Software | Software tools used to develop and validate mathematical models that describe the time course and effect of insulin in the body. | NONMEM (Nonlinear Mixed Effects Modeling) [50]. |
| Euglycemic Clamp Study Data | The "gold standard" method for assessing insulin sensitivity and beta-cell function. Data from these studies are used to build and validate PK/PD models. | Provides critical data on insulin time-action profiles [50] [52]. |
| Statistical Software (R with Shiny) | An open-source programming environment for statistical computing and graphics. The Shiny package can be used to build interactive web applications for visualizing insulin PK profiles. | Enables model-based simulations and informative visualization of insulin time-action profiles [50]. |
Hybrid Closed-Loop (HCL) systems represent a transformative advancement in type 1 diabetes (T1D) management, combining automated basal insulin delivery with meal announcement functionalities. The integration of sophisticated model predictive control (MPC) algorithms has enabled these systems to dynamically adjust insulin in response to real-time glucose readings while managing postprandial glycemic excursions. This protocol examines the operational framework of advanced HCL systems, with specific emphasis on meal announcement strategies and their optimization through MPC algorithms. Evidence from clinical studies demonstrates that simplified meal announcement approaches can achieve glycemic outcomes comparable to traditional carbohydrate counting, potentially reducing user burden while maintaining safety standards. The following application notes provide detailed methodologies for implementing and evaluating these systems in both research and clinical settings.
Model Predictive Control in Glucose Regulation
Model Predictive Control (MPC) has emerged as a dominant control strategy in artificial pancreas systems due to its ability to handle complex, dynamic systems with constraints. The MPC algorithm utilizes a mathematical model of the glucose-insulin regulatory system to predict future glucose values and compute optimal insulin delivery rates that maintain glycemic targets while minimizing hypoglycemia risk [4]. This predictive capability is particularly valuable for managing postprandial glucose excursions, where traditional control strategies often struggle.
The fundamental operation of MPC involves solving a finite-horizon optimal control problem at each sampling period (typically 5-minute intervals) based on current continuous glucose monitor (CGM) readings [33]. The algorithm incorporates constraints on maximum insulin delivery, insulin-on-board calculations, and personalized glucose targets to ensure safety. Clinical validations demonstrate that MPC-based systems significantly increase time-in-range (TIR, 70-180 mg/dL) compared to conventional insulin therapy, with one meta-analysis reporting an additional 10.03% TIR during overnight periods [4].
Advanced Hybrid Closed-Loop Systems
Advanced Hybrid Closed-Loop (AHCL) systems represent the current state-of-the-art in automated insulin delivery, combining fully automated basal rate adjustments with meal-responsive features. The MiniMed 780G system exemplifies this technology, incorporating both automated basal adjustments every five minutes and automatic correction boluses for hyperglycemia [53]. Unlike earlier systems, AHCL technology allows personalization of glucose targets, with settings as low as 100 mg/dL (5.5 mmol/L), enabling tighter glycemic control while maintaining safety through hypoglycemia protection algorithms [53].
The "hybrid" nature of these systems acknowledges the continued importance of meal announcement for optimal postprandial glucose control, though emerging evidence suggests simplified approaches may be effective. Real-world performance data from Egyptian patients across age groups (3-71 years) demonstrates that the MiniMed 780G system significantly increases TIR from 63.48% to 81.54% while reducing time-above-range and time-below-range across all age groups [53].
Meal Annunciation Strategies: Protocols and Performance
Comparative Framework: Precise vs. Simplified Meal Announcement
Experimental Protocol: A structured crossover study design was implemented to evaluate meal announcement strategies in adults with T1D using the MiniMed 780G system [54]. Fourteen participants (mean age 45.7±12.4 years, 71% male) with baseline HbA1c of 6.8%±1.2% and TIR of 67.5%±16.7% underwent three distinct study phases:
- Precise Phase (13 weeks): Traditional precise carbohydrate counting with meal announcement
- Fixed One-Step Phase (3-4 weeks): Simplified announcement using one personalized fixed carbohydrate amount regardless of actual meal size
- Multistep Phase (3-4 weeks): Simplified announcement using multiples (1x, 2x, or 3x) of a personalized fixed carbohydrate amount based on meal size estimation
Participants were instructed to maintain consistent meal timing and composition across study phases. CGM metrics, insulin delivery data, and safety parameters were collected throughout the study period. Statistical analysis employed paired t-tests with significance defined as p<0.05.
Table 1: Glycemic Outcomes by Meal Announcement Strategy
| Parameter | Precise CHO Counting | Fixed One-Step | Multistep |
|---|---|---|---|
| Time-in-Range (%) | 77.7 ± 9 | 75.4 ± 13 (p=0.12) | 80.5 ± 10 (p=0.02) |
| Glucose Management Indicator | 6.6% | 6.8% (p=0.01) | 6.6% |
| Level 1 Hypoglycemia (<70 mg/dL) | 2.8 ± 2% | 1.6 ± 1% (p=0.03) | 1.9 ± 1% (p=0.01) |
| Level 2 Hypoglycemia (<54 mg/dL) | 0.65 ± 1% | 0.3 ± 5% (p=0.08) | 0.4 ± 0.7% (p=0.08) |
| Level 1 Hyperglycemia (>180 mg/dL) | 15.0 ± 7% | 17.1 ± 8% (p=0.05) | - |
| Level 2 Hyperglycemia (>250 mg/dL) | 3.6 ± 3% | 5.5 ± 5% (p=0.04) | - |
MPC Performance in Diverse Populations
Implementation Protocol: Real-world performance of AHCL systems with integrated MPC algorithms was evaluated across age groups in a prospective, single-arm, open-label study involving 107 Egyptian patients with T1D (ages 3-71 years) [53]. Participants transitioned from multiple daily injections (73.8%) or sensor-augmented pump therapy (26.2%) to the MiniMed 780G system. Data collection occurred over six months, with comprehensive CGM metrics analyzed before and after AHCL initiation.
Key methodological considerations included:
- Insulin Aspart (NovoRapid) used in all patients
- Standardized meal announcement with carbohydrate counting and pre-meal bolusing
- Personalization of glucose targets (100-120 mg/dL) and active insulin time settings
- Analysis included only patients with ≥14 days of sensor glucose data
Table 2: Age-Stratified Performance of AHCL System with MPC Algorithm
| Age Group | Pre-AHCL TIR | Post-AHCL TIR | Time in Auto Mode | GMI Reduction |
|---|---|---|---|---|
| Children (<11 years) | 63.48 ± 10.14% | 82.29 ± 7.22% | 85.31 ± 22.04% | 7.9% to 6.95% |
| Adolescents (11-18 years) | 63.48 ± 10.14% | 78.4 ± 7.34% | 85.31 ± 22.04% | 7.9% to 6.95% |
| Adults (>18 years) | 63.48 ± 10.14% | 83.86 ± 9.24% | 85.31 ± 22.04% | 7.9% to 6.95% |
The study demonstrated significant improvements in all glycemic metrics post-AHCL initiation (p<0.001), with no serious adverse events reported. The total daily insulin dose increased across all age groups, primarily due to system-initiated insulin delivery including auto-correction boluses and adaptive basal insulin [53].
Technical Implementation of MPC in AHCL Systems
Algorithm Architecture and Workflow
The MPC algorithm in modern AHCL systems operates through a sophisticated integration of prediction, optimization, and safety modules. The following diagram illustrates the continuous workflow of the MPC algorithm within the AHCL system:
Meal Integration Logic
The meal announcement interface with the MPC algorithm involves specialized handling of postprandial glucose dynamics. The following diagram details the meal information processing pathway:
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for HCL System Investigation
| Research Tool | Specification/Function | Application in HCL Research |
|---|---|---|
| Advanced HCL System | MiniMed 780G with SmartGuard algorithm | Provides automated basal insulin and auto-correction boluses; enables meal announcement strategies [54] [53] |
| Continuous Glucose Monitor | Real-time CGM (e.g., Dexcom G7, Medtronic Guardian) | Provides glucose data at 5-minute intervals to MPC algorithm [33] |
| Insulin Pump | Automated insulin delivery system | Executes commands from MPC algorithm; delivers micro-boluses every 5 minutes [53] |
| Model Predictive Control Algorithm | Customizable MPC software | Core control system that predicts glucose trends and computes insulin doses [55] [4] |
| Carbohydrate Reference Database | Standardized CHO values | Enables consistent meal announcement in clinical trials [54] |
| Glycemic Analysis Software | CareLink Personal or similar | Aggregates and analyzes CGM metrics, insulin delivery data, and system performance [53] |
Discussion and Clinical Implications
The integration of meal announcement with automated basal control represents a significant advancement in HCL technology. Evidence indicates that simplified meal announcement strategies, particularly the multistep approach using multiples of a fixed carbohydrate amount, can achieve glycemic outcomes comparable to or better than traditional precise carbohydrate counting [54]. This finding has important implications for reducing user burden and potentially improving adherence to meal announcement protocols.
The MPC algorithm's ability to handle unannounced meals and physiological disturbances has been validated in preclinical models. Research in diabetic rats demonstrated that an offset-free impulsive zone MPC controller achieved 83.4% time-in-range (80-180 mg/dL) with no severe hypoglycemic or hyperglycemic events, despite unannounced carbohydrate intake [56]. This robustness is attributed to the algorithm's disturbance rejection capabilities and adaptive tuning mechanisms.
Future developments in MPC-based HCL systems should focus on further reducing meal announcement burden through improved glucose prediction models and integration of additional physiological signals. The emerging understanding of individualized glycemic responses to different carbohydrates [57] suggests opportunities for personalizing meal announcement protocols based on metabolic phenotypes.
Hybrid Closed-Loop systems with integrated MPC algorithms represent a sophisticated solution for automated glucose regulation that successfully balances automated basal control with meal-responsive features. The documented performance of simplified meal announcement strategies indicates potential for reducing user burden while maintaining glycemic targets. Continued refinement of MPC algorithms, particularly in handling meal-related disturbances and adapting to individual metabolic profiles, will further enhance the effectiveness and usability of these systems in diverse populations with type 1 diabetes.
Addressing Implementation Challenges and Performance Optimization
Model Predictive Control (MPC) has emerged as a leading algorithm for Automated Insulin Delivery (AID) systems, demonstrating significant potential in enhancing glycemic control for people with diabetes [56] [19]. These controllers utilize an internal model of glucose-insulin dynamics to forecast blood glucose levels and compute optimal insulin infusion rates. However, a critical challenge impeding their performance is the inherent presence of model inaccuracies stemming from parameter mismatches and inter-/intra-individual physiological variations.
This application note, framed within broader thesis research on MPC for blood glucose regulation, details the primary sources of these inaccuracies and provides validated experimental protocols to quantify and mitigate their impact. By implementing the outlined strategies, researchers can develop more robust AID systems capable of maintaining safe glycemic control despite physiological uncertainties and plant-model mismatches.
Quantifying the Impact of Model Inaccuracies
Model inaccuracies can significantly degrade controller performance. The table below summarizes quantitative evidence from recent preclinical and methodological studies demonstrating this impact and the efficacy of proposed mitigation strategies.
Table 1: Documented Impacts of Model Inaccuracies and Performance of Mitigation Strategies
| Source of Inaccuracy / Mitigation Strategy | Experimental Context | Key Performance Metric | Reported Value |
|---|---|---|---|
| Unmitigated Plant-Model Mismatch [56] | Impulsive MPC in Diabetic Rats (n=14) | MARD between model predictions and sensor data | 24.66% |
| Offset-Free Impulsive Zone MPC [56] | Same cohort with disturbance handling | Time in Target Range (80-180 mg/dL) | 83.4% |
| Neural Network MPC (OSD-trained) [19] | Replication of UVA MPC Algorithm | Final NN Accuracy Improvement | Four-fold vs. conventional training |
| Deep Learning for Parameter Inference [58] | Inference from FSIGT Test Data | Trajectory Reconstruction Accuracy | High R² values, low P-values |
Protocols for Characterizing Physiological Variations
A major source of parameter mismatch is individual variation in metabolic responses. The following protocol, derived from a Stanford Medicine-led study, provides a methodology for characterizing these variations, which can inform personalized model parameterization [57].
Protocol: Metabolic Response Profiling to Carbohydrates
Objective: To identify individual-specific blood glucose response patterns to different carbohydrates and associate them with underlying metabolic dysfunctions (e.g., insulin resistance, beta-cell dysfunction).
Materials:
- Continuous Glucose Monitors (CGM)
- Standardized portions of test foods: Jasmine rice, buttermilk bread, shredded potato, pasta, canned black beans, grapes, berry mix.
- Metabolic testing kits for insulin resistance and beta-cell function.
- Multi-omics profiling resources (optional): Plasma triglyceride levels, metabolite panels, gut microbiome analysis.
Procedure:
- Participant Preparation: Recruit subjects (with and without prediabetes). Participants fast for 10-12 hours overnight.
- Baseline Testing: Conduct initial metabolic testing for insulin resistance and beta-cell dysfunction.
- Food Challenge: Each morning, participants consume a single test food item. Each food type is tested twice in random order to ensure reproducibility.
- Monitoring: CGM data is collected for 3 hours post-prandial. Blood samples may be taken at intervals for multi-omics profiling.
- Data Analysis: Correlate the magnitude of glucose spikes (ΔBG) for each food with the participant's metabolic subtype (e.g., insulin resistance, beta-cell dysfunction).
Key Findings for Model Personalization:
- High glucose spikes after pasta are strongly associated with insulin resistance.
- High glucose spikes after potatoes are linked to either insulin resistance or beta-cell dysfunction.
- The ratio of glucose responses to potatoes vs. grapes can serve as a potential biomarker for insulin resistance.
- Pre-meal protein/fiber supplementation was effective only in metabolically healthy participants, highlighting a limitation for generalized mitigation strategies [57].
Protocols for Mitigating Parameter Mismatch
Strategy: Advanced Parameter Inference using Deep Learning
Traditional parameter optimization for nonlinear physiological models is often slow and difficult to constrain within biological ranges. The protocol below uses a deep learning framework for accurate and efficient parameter inference [58].
Objective: To train a Convolutional Neural Network (CNN) to infer physiological parameters from time-series data (e.g., from Frequently Sampled Intravenous Glucose Tolerance Tests - FSIGT), overcoming limitations of iterative optimizers.
Materials:
- Physiological time-course data (e.g., Glucose, Insulin, FFA from FSIGT).
- A defined physiological model (e.g., lipolysis models of glucose, insulin, and FFA dynamics).
- Computational resources for model simulation and CNN training (e.g., Python, TensorFlow/PyTorch).
Procedure:
- Model Optimization: Perform initial parameter optimization from limited clinical data using traditional methods to establish baseline parameter distributions.
- Data Generation: Generate a large, synthetic training dataset by sampling parameters within physiological ranges and integrating the model to produce corresponding glucose, insulin, and FFA time courses.
- Feature Engineering (Critical): Preprocess the raw simulated data. Apply nonlinear transformations informed by the model's structure to create enhanced input features, helping the network learn underlying relationships more efficiently.
- Network Training: Train a CNN (or a hybrid CNN-LSTM-Attention network) using the simulated time courses as input and the corresponding parameter sets as the output.
- Validation: Evaluate the trained network's performance on a held-out test dataset, optimized model-fitting curves, and real physiological data, assessing both parameter inference accuracy and trajectory reconstruction fidelity.
Strategy: Neural Network-based MPC with Optimally-Sampled Datasets
Implementing MPC on resource-constrained devices is challenging. This protocol describes training a Neural Network (NN) to replicate a complex MPC, using a curated dataset to ensure accuracy and safety [19].
Objective: To create a lightweight, on-chip NN that reliably replicates a full-scale MPC algorithm's behavior, robust to state variations.
Materials:
- The target MPC algorithm to be replicated.
- A data generation environment to simulate the controlled system.
- Resources for NN training and validation.
Procedure:
- Data Generation: Run the original MPC algorithm over a wide range of possible system states ( xi ) to collect a large dataset of input-output pairs ( {xi, ui} ), where ( ui = \text{MPC}(x_i) ).
- Create an Optimally-Sampled Dataset (OSD): Process the raw data to construct a training set with three key properties:
- No duplicates: Remove repeated or near-duplicate states to avoid biasing the NN.
- Adaptive granularity: Ensure the dataset covers the state space with a resolution appropriate to the MPC's cost function.
- Saturation: Verify the dataset is complete and no additional data points would improve NN performance.
- NN Training and Validation: Train a ReLU-based NN on the OSD. Rigorously validate the NN's output ( u_{NN} ) against the original MPC's output ( u^* ) across the entire operating envelope to certify its performance.
Table 2: Research Reagent Solutions for Robust MPC Development
| Reagent / Tool | Function in Research | Application Context |
|---|---|---|
| Frequently Sampled IVGTT (FSIGT) Data [58] | Provides high-resolution time-course data for model identification and parameter inference. | Building and validating physiological models of glucose-insulin-FFA dynamics. |
| Continuous Glucose Monitor (CGM) [56] [19] | Provides real-time, subcutaneous glucose measurements for state feedback in closed-loop control. | Core sensor in AID systems; used for MPC state estimation and NN input. |
| Optimally-Sampled Dataset (OSD) [19] | An ideal training set for NN-MPCs, ensuring coverage, non-redundancy, and certified performance. | Deploying certified, high-fidelity NN-based controllers on embedded medical devices. |
| Convolutional Neural Network (CNN) [58] [59] | Infers parameters from complex time-series data or replicates MPC control laws. | Parameter inference from physiological data; on-chip MPC implementation. |
| Offset-Free State Estimator [56] | Estimates unmeasured disturbances and model mismatches to correct the internal state. | Handling plant-model mismatch and external disturbances like meals in MPC. |
Integrated Workflow for Robust MPC Development
The following diagram illustrates a comprehensive workflow integrating the protocols and strategies discussed to develop an MPC algorithm robust to model inaccuracies.
Achieving robustness against model inaccuracies is not a single-step solution but a systems-level approach. As demonstrated, this involves:
- Systematic Characterization of physiological variations to inform model personalization [57].
- Advanced Computational Techniques like deep learning for accurate and efficient parameter inference from limited data [58].
- Innovative Control Implementation strategies, such as NN-based controllers trained on optimally-sampled datasets [19] and offset-free MPC formulations [56], to actively compensate for plant-model mismatch and disturbances.
The integrated workflow and detailed protocols provided herein offer a structured pathway for researchers to develop next-generation AID systems that are safer, more effective, and adaptable to the unique physiology of each individual.
Hypoglycemia remains a common and serious complication of insulin therapy for individuals with diabetes, posing significant health risks including cardiac arrhythmias, seizures, and brain damage [60]. The advent of automated insulin delivery (AID) systems, particularly those utilizing model predictive control (MPC), has transformed hypoglycemia prevention strategies. This application note examines the safety constraints and insulin suspension logic embedded within these systems, focusing on their implementation in clinical practice and research settings. We frame this discussion within the broader context of MPC algorithm development for blood glucose regulation, highlighting how predictive models and control strategies integrate safety mechanisms to prevent hypoglycemic events while maintaining overall glycemic control.
Clinical Evidence and Quantitative Outcomes
Low-Glucose Suspend System Performance
The implementation of low-glucose suspend (LGS) functionality in sensor-augmented pump therapy represents a significant advancement in hypoglycemia prevention. Clinical studies have demonstrated the safety and efficacy of automated insulin suspension in response to impending hypoglycemia. A study of 24 participants with type 1 diabetes and impaired hypoglycemia awareness evaluated the Paradigm Veo System with LGS function set to suspend insulin delivery when sensor glucose values fell below 60 mg/dL [61].
Table 1: Performance Metrics of Low-Glucose Suspend System
| Parameter | Result | Context/Details |
|---|---|---|
| Total LGS Events | 3,128 events | Over 2,493 days of evaluation [61] |
| Event Frequency | 1.3 events per day | Median duration: 11.2 minutes [61] |
| Overnight Events | 36% of all events | Defined as between 10:00 p.m. and 6:00 a.m. [61] |
| Full 2-Hour Suspensions | 406 events (13%) | 80% occurred overnight [61] |
| Glucose at End of 2-Hour Suspend | 99 ± 6 mg/dL | Mean sensor glucose ± SE (5.5 ± 0.3 mmol/L) [61] |
| Glucose 2 Hours After Resume | 155 ± 10 mg/dL | Mean sensor glucose ± SE (8.6 ± 0.6 mmol/L) [61] |
| Next Morning Meter Glucose | 185 ± 9 mg/dL | Mean value entered at median time of 7:26 a.m. [61] |
| Severe Hypoglycemia Events | 0 | No episodes during study period [61] |
| Diabetic Ketoacidosis | 0 | No episodes during study period [61] |
Analysis of 126 overnight suspend events with no patient response revealed a characteristic glucose pattern: the decline in sensor glucose was promptly arrested after insulin suspension, followed by a steady rise during the 2-hour suspension period [61]. This pattern demonstrates the effectiveness of automated suspension in preventing progressive hypoglycemia without resulting in excessive rebound hyperglycemia.
Hypoglycemia Prevention in Hospital Settings
Inpatient hypoglycemia prevention requires specialized protocols, particularly for patients with ongoing hypoglycemia risk. A quality improvement project developed and implemented a proactive carbohydrate protocol to address recurrent hypoglycemia, shifting from reactive treatment to preventive management [60].
Table 2: Hypoglycemia Precipitating Factors in Hospital Settings
| Precipitating Factor | Blood Glucose Values <50 mg/dL in 2009 (%) | Blood Glucose Values <50 mg/dL in 2014 (%) | Rate per 1,000 Patient-Days in 2009 | Rate per 1,000 Patient-Days in 2014 |
|---|---|---|---|---|
| Long-acting or mixed insulin | 44.1% | 37.6% | 5.02 | 1.96 |
| IV regular insulin for high potassium | 0% | 18.3% | 0 | 0.89 |
| Rapid-acting analog insulin | 2.2% | 11.8% | 0.24 | 0.61 |
| Sulfonylurea | 31.2% | 12.9% | 3.55 | 0.67 |
| Organ failure and/or sepsis | 4.3% | 9.7% | 0.49 | 0.50 |
| Titratable IV insulin or insulin pump | 14.0% | 8.6% | 1.59 | 0.45 |
| Other, no exogenous agent | 4.3% | 2.2% | 0.49 | 0.22 |
| Total | 100% | 100% | 11.38 | 5.20 |
The protocol included provision of proactive carbohydrates and a standardized process for intravenous dextrose titration with the goal of maintaining blood glucose levels between 100-150 mg/dL (5.5-8.3 mmol/L) [60]. Implementation resulted in a significant reduction in hypoglycemia rates, from 11.38 to 5.20 events per 1,000 patient-days for blood glucose values <50 mg/dL [60].
Integration with Model Predictive Control Systems
MPC in Artificial Pancreas Systems
Model predictive control has emerged as the dominant control strategy for artificial pancreas (AP) systems, with insulin suspension logic serving as a critical safety constraint within these algorithms. MPC algorithms for blood glucose regulation typically utilize linear models to predict future glucose values and optimize insulin delivery, though recent advances incorporate data-driven learning approaches for improved accuracy [9].
The fundamental MPC optimization problem for AP systems can be formulated as:
[ J(xk, U{T-1}, \bar{Y}T, \bar{U}{T-1}) = (\hat{Y}T(xk) - \bar{Y}T)'Q(\hat{Y}T(xk) - \bar{Y}T) + (U{T-1}' - \bar{U}{T-1})R(U{T-1} - \bar{U}{T-1}) ]
Where ( \hat{Y}T ) represents the predicted glucose values, ( \bar{Y}T ) is the glucose setpoint, ( U{T-1} ) is the insulin delivery rate, ( \bar{U}{T-1} ) is the basal insulin rate, and Q and R are tuning parameters [9].
Recent innovations in MPC for AP systems include the development of multi-step-ahead predictors using Long Short-Term Memory (LSTM) networks, which improve prediction accuracy for longer horizons while maintaining the affine structure in control inputs that enables efficient solution via quadratic programming [9].
Safety Constraints in Control Algorithms
MPC algorithms incorporate multiple safety constraints to prevent hypoglycemia:
- Hard Constraints on Insulin Delivery: Minimum insulin delivery rates (often zero) to prevent over-delivery [9]
- Predictive Low Glucose Suspend: Preemptive reduction or suspension of insulin based on predicted future hypoglycemia [61] [9]
- Velocity Weighting: Penalizing rapid decreases in glucose levels to anticipate and prevent hypoglycemia [9]
- Asymmetric Cost Functions: Heavier weighting of hypoglycemic deviations compared to hyperglycemic excursions [9]
These constraints are particularly important given the limitations of linear models in capturing the full complexity of glucose metabolism, especially during periods of rapid change following meals, exercise, or other disturbances [9].
Figure 1: MPC Safety Logic Flow. This diagram illustrates the integration of safety constraints within the model predictive control framework for hypoglycemia prevention.
Experimental Protocols
Protocol for Evaluating LGS System Performance
Objective: To assess the safety and efficacy of low-glucose suspend functionality in preventing hypoglycemia without causing excessive rebound hyperglycemia.
Materials:
- Sensor-augmented insulin pump with LGS capability (e.g., Medtronic Paradigm Veo)
- Continuous glucose monitoring system
- Data upload capability (e.g., CareLink Therapy Management System)
- Blood ketone testing supplies
Methodology:
- Participant Selection: Recruit participants with type 1 diabetes and impaired hypoglycemia awareness (Clarke's questionnaire score ≥4) [61]
- Device Configuration:
- Set LGS threshold to 60 mg/dL (3.3 mmol/L)
- Configure low glucose alert at 70 mg/dL (3.9 mmol/L)
- Set high glucose alert at 324 mg/dL (18.0 mmol/L)
- Data Collection Period: Conduct study over 6-month intervention period
- Data Analysis:
- Identify all LGS events (insulin suspension triggered by glucose <60 mg/dL)
- Categorize events by duration (<10 min, 10-30 min, 30-60 min, 1-2 h, full 2 h)
- Differentiate between events with and without patient response
- Analyze glucose patterns before, during, and after suspension events
- Document any adverse events (severe hypoglycemia, ketoacidosis)
Outcome Measures:
- Frequency and duration of LGS events
- Sensor glucose values at suspension initiation, end of suspension, and 2 hours post-reactivation
- Percentage of time in target range (70-180 mg/dL)
- Incidence of severe hypoglycemia and ketoacidosis
Protocol for Inpatient Hypoglycemia Prevention
Objective: To implement and evaluate a proactive protocol for preventing recurrent hypoglycemia in hospitalized patients.
Materials:
- Point-of-care blood glucose testing equipment
- Intravenous dextrose solutions (D10W, D5W)
- Oral carbohydrate sources
- Blood glucose tracking system with alert functionality
Methodology:
- Baseline Assessment:
- Retrospectively review hypoglycemic events (blood glucose <50 mg/dL)
- Identify precipitating factors using standardized checklist
- Establish baseline hypoglycemia rate per 1,000 patient-days
- Protocol Development:
- Create nurse-driven protocol for recurrent hypoglycemia management
- Include oral carbohydrate administration guidelines
- Establish IV dextrose titration protocol (Table 1)
- Staff Education:
- Train healthcare providers on hypoglycemia risk factors
- Educate on protocol implementation and adjustment parameters
- Implementation:
- Deploy protocol hospital-wide
- Place printed protocols in all nursing units
- Evaluation:
- Conduct follow-up retrospective examination using same criteria as baseline
- Compare hypoglycemia rates and precipitating factors
IV Dextrose Titration Protocol:
- Initiate D10W at 50-100 mL/hour (5-10 g dextrose/hour) for blood glucose <70 mg/dL with ongoing risk factors
- Titrate rate based on blood glucose levels:
- Increase by 25 mL/hour if glucose <80 mg/dL
- Decrease by 25 mL/hour if glucose >150 mg/dL
- Discontinue when blood glucose remains 100-150 mg/dL for 4 hours without IV dextrose
- Monitor blood glucose every 30-60 minutes during titration [60]
Protocol for Validating MPC Algorithms with Hypoglycemia Prevention
Objective: To evaluate the performance of model predictive control algorithms in preventing hypoglycemia while maintaining glycemic control.
Materials:
- Continuous glucose monitor
- Insulin pump with automated suspension capability
- MPC algorithm implementation platform
- UVa-Padova T1D Simulator or equivalent [39]
Methodology:
- In Silico Testing:
- Utilize FDA-accepted T1D simulator with virtual patient cohort
- Test control algorithm under various meal and disturbance scenarios
- Evaluate performance across different patient profiles (adults, adolescents, children)
- Controller Formulation:
- Implement cost function with asymmetric weights for hypo- vs hyperglycemia
- Incorporate insulin suspension constraints based on predicted glucose values
- Set time-dependent glucose targets (e.g., 110 mg/dL daytime, 125 mg/dL nighttime) [9]
- Performance Metrics:
- Percentage time in target range (70-180 mg/dL)
- Percentage time in hypoglycemia (<70 mg/dL)
- Low Blood Glucose Index (LBGI)
- Controller effort and insulin delivery patterns
- Preclinical Validation:
- Conduct animal studies using diabetic rat model [56]
- Implement fully automated insulin delivery system
- Challenge system with unannounced meals and disturbances
Figure 2: MPC Validation Workflow. This diagram outlines the sequential process for developing and validating MPC algorithms with hypoglycemia prevention capabilities.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for Hypoglycemia Prevention Studies
| Category | Specific Examples | Research Application | Key Characteristics |
|---|---|---|---|
| Continuous Glucose Monitors | Medtronic Guardian, Dexcom G6, Abbott Freestyle Libre | Real-time glucose monitoring for algorithm input [61] [39] | MARD <10%, factory calibration, 10-14 day wear [39] |
| Insulin Pumps | Medtronic Paradigm Veo, Tandem t:slim, Insulet OmniPod | Precise insulin delivery with suspension capability [61] [39] | Tube/patch designs, automated suspension, connectivity [39] |
| Control Algorithms | Model Predictive Control, Proportional-Integral-Derivative, Fuzzy Logic | Core intelligence for automated insulin delivery [39] [9] | Prediction horizon, safety constraints, individualization [9] |
| Simulation Platforms | UVa-Padova T1D Simulator | Preclinical testing of control strategies [39] | 100 virtual adults, 100 adolescents, 100 children [39] |
| Insulin Formulations | Rapid-acting (aspart, lispro, glulisine), Long-acting (glargine, detemir) | Physiologic insulin replacement [62] | Altered absorption kinetics, duration of action [62] |
| Data Analysis Tools | CareLink, Tidepool, DIY APS | Therapy management and algorithm refinement [61] | Retrospective analysis, pattern identification [61] |
The integration of safety constraints and insulin suspension logic within MPC-based artificial pancreas systems represents a significant advancement in hypoglycemia prevention. Clinical evidence demonstrates that automated insulin suspension effectively arrests declining glucose trends without resulting in excessive rebound hyperglycemia or ketosis. The ongoing refinement of predictive models, particularly through data-driven approaches like LSTM networks, continues to enhance the ability of these systems to anticipate and prevent hypoglycemic events while maintaining overall glycemic control. As these technologies evolve, the focus remains on developing more sophisticated safety constraints that can adapt to individual patient characteristics and varying physiological conditions, ultimately working toward fully automated glycemic management that minimizes hypoglycemia risk while maximizing time in target range.
In the development of Model Predictive Control (MPC) algorithms for blood glucose regulation, a critical challenge lies in balancing computational efficiency with controller performance. The prediction horizon, a key MPC parameter defining how far into the future the controller predicts system behavior, directly influences this balance. Excessively long horizons can make real-time implementation computationally infeasible, while overly short horizons may compromise stability and performance [63] [64]. This application note provides a structured framework for selecting the prediction horizon and associated parameters to achieve computationally efficient and clinically effective glucose control.
Core Concepts and Quantitative Relationships
Fundamental MPC Parameters
Three parameters form the core of MPC design: sample time (Ts), prediction horizon (p), and control horizon (m).
- Sample Time (Ts): The interval between controller executions. A shorter Ts generally improves disturbance rejection but increases computational load. A longer Ts reduces computations but may miss critical dynamics [63].
- Prediction Horizon (p): The number of future sample intervals over which the system's output is predicted. This is the primary focus for balancing performance and computational load.
- Control Horizon (m): The number of future moves for the manipulated variables (e.g., insulin infusion rate) that are optimized. Typically, m < p to reduce computational complexity and ensure problem feasibility [63].
The following table summarizes the qualitative effects of varying these parameters:
Table 1: Effects of MPC Parameter Adjustments on System Performance and Computational Load
| Parameter | Increase | Decrease |
|---|---|---|
| Prediction Horizon (p) | Pros: Improved stability, anticipates constraints earlier.Cons: Increased memory, longer QP solution time [63]. | Pros: Reduced computation, faster QP solution.Cons: Risk of internal instability, poor long-term performance [63]. |
| Sample Time (Ts) | Pros: Lower computational burden per time unit.Cons: Potential for degraded disturbance rejection [63]. | Pros: Often improves disturbance rejection.Cons: Dramatically increased computational effort [63]. |
| Control Horizon (m) | Pros: Potentially better performance.Cons: More QP variables, slower computation, risk of singularities [63]. | Pros: Faster computations, promotes stability.Cons: May limit controller agility [63]. |
Quantitative Guidelines for Parameter Selection
Based on established practices, the following quantitative relationships provide a starting point for parameter selection:
- Sample Time (Ts): Set Ts to be between 10% and 25% of the desired closed-loop response time, T [63].
- Prediction Horizon (p): Choose p such that the product pTs approximates the desired closed-loop response time, T (i.e., T ≈ pTs) [63].
- Control Horizon (m): A control horizon of m=2 is often an effective default. For plants with significant delays, m should be strictly less than p (m < p) [63].
Experimental Protocols for Horizon Selection
Protocol 1: In Silico Testing of Horizon Length
Objective: To empirically determine the optimal prediction horizon (p) that balances glycemic performance and computational load using a accepted simulator.
Background: The University of Virginia-Padova (UVa-Padova) T1D Simulator is a widely recognized platform accepted by regulatory bodies for preclinical testing of glucose control strategies [39]. It contains virtual populations (adults, adolescents, children) with realistic inter-subject variability, enabling robust algorithm testing.
Materials:
- Simulator: UVa-Padova T1D Simulator.
- Controller: The MPC algorithm under development.
- Virtual Cohort: A representative group of virtual subjects (e.g., n=10 adults).
- Performance Metrics: Root Mean Square Error (RMSE), Time In Range (TIR: 70-180 mg/dL), computational time per control step.
Procedure:
- Baseline Setup: Fix the sample time (Ts) and control horizon (m) based on initial guidelines (e.g., Ts=5 minutes, m=2).
- Horizon Sweep: Perform closed-loop simulations for each virtual subject across a range of prediction horizons (e.g., p = 6, 9, 12, 15, 18, corresponding to 30, 45, 60, 75, and 90 minutes with Ts=5).
- Data Collection: For each (subject, p) pair, record:
- Glycemic control performance (RMSE, %TIR).
- Average and maximum computation time required to solve the optimization problem at each step.
- Analysis: Identify the point of diminishing returns where increasing p no longer yields significant glycemic improvement but computational time shows a marked increase.
Table 2: Exemplar In Silico Results for Prediction Horizon Tuning (Ts = 5 min)
| Prediction Horizon (p) | Horizon Duration (mins) | Mean RMSE (mg/dL) | Time in Range (%) | Mean Comp. Time (s) |
|---|---|---|---|---|
| 6 | 30 | 45.2 | 65.1 | 0.08 |
| 9 | 45 | 38.7 | 72.5 | 0.21 |
| 12 | 60 | 35.1 | 76.8 | 0.45 |
| 15 | 75 | 33.8 | 77.5 | 0.82 |
| 18 | 90 | 33.5 | 77.6 | 1.34 |
Note: Data is illustrative. Actual results will vary based on the MPC formulation and simulator settings.
Protocol 2: Sample Time and Disturbance Rejection
Objective: To evaluate if the initially chosen sample time provides adequate rejection of unmeasured disturbances (e.g., unannounced meals, stress).
Procedure:
- Select a fixed, suitably long prediction horizon (p) based on Protocol 1 results.
- Run a simulation with a challenging but realistic disturbance profile.
- Halve the sample time (Ts) and double the prediction horizon (p) to keep the horizon duration (p*Ts) constant. Re-run the simulation.
- Compare glycemic outcomes (e.g., post-prandial peaks, hypoglycemia events) and computational load between the two Ts values. If performance improves significantly with the smaller Ts, consider revising the initial choice, provided computational resources allow [63].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for MPC Algorithm Development in Glucose Regulation
| Item | Function in Research | Example |
|---|---|---|
| Metabolic Simulator | Provides a safe, cost-effective environment for preclinical testing of MPC algorithms on a virtual population with T1D [39]. | UVa-Padova T1D Simulator |
| Continuous Glucose Monitoring (CGM) Data | Serves as the primary input signal for the MPC model. High-accuracy CGM (low MARD) is critical for reliable performance [39]. | Dexcom G-series, Medtronic Guardian |
| Control Hardware Platform | The embedded system (e.g., smartphone, dedicated device) that runs the MPC algorithm in real-time. Must meet computational deadlines [39]. | Android-based platforms (e.g., DiAs), Embedded microcontrollers |
| In Silico Clinical Trial Framework | Enables large-scale, statistically powerful assessment of controller performance and safety across diverse virtual cohorts before human trials [39]. | Custom frameworks built around the UVa-Padova simulator |
| Performance Validation Metrics | Standardized measures to quantitatively evaluate and compare different MPC configurations [65]. | RMSE, MAE, Clarke Error Grid Analysis, Time In Range |
Logical Workflow and Decision Pathways
The following diagram illustrates the integrated decision process for tuning MPC parameters to achieve computational efficiency and control performance in a blood glucose regulation context.
In the development of a fully automated artificial pancreas (AP) for type 1 diabetes management, handling unannounced meals represents one of the most significant challenges. While hybrid closed-loop systems have substantially improved glycemic control, they remain dependent on user-initiated meal announcements to administer prandial insulin boluses. This manual component introduces substantial limitations, as missed meal boluses are strongly correlated with poor glycemic outcomes [66] [67]. Research indicates that even two missed boluses per week can elevate hemoglobin A1c values by approximately 0.3% [18] [66]. Consequently, developing robust meal detection algorithms and compensation strategies has become a critical research focus in the pursuit of a fully autonomous AP system.
This application note examines meal detection and compensation methodologies within the broader context of model predictive control (MPC) for blood glucose regulation. We provide a comprehensive technical overview of detection algorithms, quantitative performance comparisons, experimental protocols for validation, and integration strategies with MPC frameworks. The content is structured to assist researchers, scientists, and drug development professionals in implementing and evaluating these advanced techniques in both clinical and preclinical settings.
The Challenge of Unannounced Meals
Meals present a particular challenge for automated insulin delivery systems due to the rapid increase in blood glucose concentrations following carbohydrate ingestion, combined with the delayed pharmacokinetic and pharmacodynamic profiles of subcutaneously administered insulin. The slow absorption of insulin from the subcutaneous tissue creates a fundamental mismatch between the timing of glucose appearance and insulin action [66]. In healthy individuals, the pancreatic beta cells respond almost instantaneously to rising glucose levels, but in AP systems, this response is hampered by physiological delays.
MPC-based AP systems utilize predictive models to compute optimal insulin dosing, but these models require accurate disturbance information, including meal intake. Without meal announcement, the controller operates in a purely reactive mode, allowing significant postprandial hyperglycemia to occur before sufficient insulin can be delivered. This limitation has driven the development of meal detection algorithms that can identify carbohydrate intake based on its early effects on glucose dynamics, enabling faster insulin responses and improved postprandial glucose control [68] [66].
Meal Detection Algorithm Approaches
Technical Classifications and Methodologies
Multiple algorithmic approaches have been investigated for meal detection, each with distinct operating principles and implementation considerations:
Fuzzy Logic-Based Detection: This approach uses qualitative analysis of continuous glucose monitoring (CGM) trends to detect meals. The algorithm computes an "increase of glucose trend" (IGT) variable derived from the first and second derivatives of CGM readings. When IGT exceeds specific thresholds, a "meal flag" is activated, triggering carbohydrate estimation and potential insulin compensation [68]. The fuzzy system leverages qualitative variables that categorize glucose trends into patterns such as "accelerating increase," "decelerating increase," or "constant increase" based on the signs of the first and second derivatives of CGM values.
Model-Based Detection with Unscented Kalman Filter (UKF): This method employs an augmented minimal model of glucose-insulin dynamics. A UKF estimates a disturbance parameter that represents unmeasured inputs affecting glucose concentrations, such as meals. The detection algorithm computes the normalized cross-covariance between measured glucose and the forward difference of the estimated disturbance over sliding windows. When this cross-covariance exceeds predetermined thresholds, a meal is detected [66]. Different tuning strategies can prioritize high sensitivity (99% detection rate) or low false positives (47% detection rate) depending on safety considerations.
Probabilistic and Multi-Model Approaches: These methods use predefined meal shapes or multiple models to estimate the probability of meal consumption based on CGM patterns. The Variable State Dimension method switches between models with different state dimensions to detect meals and estimate meal size [66]. Probabilistic approaches compare real-time CGM data with libraries of meal response patterns to identify matches.
Neural Network Detection: Recent advances utilize machine learning models, particularly neural networks, for meal detection. These models are trained on historical CGM and insulin delivery data to recognize patterns indicative of meal consumption. One clinical implementation demonstrated 83.3% sensitivity with a mean detection time of 25.9 minutes and a false discovery rate of 16.6% [67].
Performance Comparison of Detection Methods
Table 1: Quantitative Performance Comparison of Meal Detection Algorithms
| Algorithm Type | Sensitivity (%) | False Positive Rate (%) | Mean Detection Time (min) | Validation Setting |
|---|---|---|---|---|
| Fuzzy Logic [68] | 93.5 (meals), 68.0 (snacks) | 20.8 | Not specified | Clinical (11 subjects) |
| UKF-Based [66] | 99.0 (high sensitivity), 93.0 (balanced), 47.0 (low FP) | Not specified | Not specified | In silico (10 adults) |
| Neural Network [67] | 83.3 | 16.6 | 25.9 | Clinical (13 adults) |
| Glucose Rate Increase Detector [37] | Not specified | Not specified | Not specified | In silico (100 adolescents/adults) |
Meal Size Estimation Techniques
Once a meal is detected, accurately estimating its carbohydrate content is essential for determining the appropriate insulin bolus. Two primary estimation approaches have emerged:
Fuzzy Estimation Systems: These systems use CGM data and insulin delivery history to estimate carbohydrate content gradually during the active meal detection period. The algorithm calculates the ratio of glucose increase and compares it to modeled effective insulin action, using a fuzzy logic framework to account for uncertainty and individual variability [68].
Model-Based Estimation: Physiological models of glucose appearance can be inverted to estimate meal size based on the observed glucose excursion. The UKF approach estimates disturbance parameters that correlate with carbohydrate absorption, enabling quantitative meal size assessment [66].
Table 2: Meal Size Estimation Performance
| Estimation Method | Input Data | Key Features | Validation |
|---|---|---|---|
| Fuzzy System [68] | CGM, insulin delivery (CSII) | Incremental estimation during active meal flag; uses FIR model for effective insulin | 117 meals/snacks from 11 subjects |
| Model-Based [18] | CGM, insulin delivery, patient parameters | Pharmacodynamic model of insulin action; IOB constraints | 100 in silico adolescents/adults |
| Neural Network [67] | CGM, insulin delivery, contextual data | Machine learning model; integrated with detection | 24 meals in clinical trial |
Integration with Model Predictive Control
MPC Framework Enhancements
Integrating meal detection with MPC requires specific architectural considerations to maintain safety and effectiveness. Two primary integration strategies have emerged:
Bolus Compensation: When a meal is detected, the system administers a meal insulin bolus equivalent to what would typically be delivered in a hybrid closed-loop system. The bolus amount is calculated using the patient's insulin-to-carbohydrate ratio based on the estimated meal size [37] [67]. The MPC then continues to operate, making fine adjustments to basal insulin delivery to address residual glucose excursions.
Adaptive MPC Tuning: This approach modifies the MPC cost function or constraints based on meal detection. Zone-MPC can implement asymmetric tuning parameters (R̂ and Ř) that penalize insulin delivery above or below basal rates differently. During meal periods, these parameters can be adjusted to allow more aggressive insulin delivery while maintaining safety constraints [37].
Safety Considerations and Constraints
Safety mechanisms are critical when integrating meal detection with MPC due to the risk of insulin stacking and hypoglycemia:
Insulin-on-Board (IOB) Constraints: IOB calculations prevent excessive insulin administration by accounting for the lingering effects of previously delivered insulin. Maximum IOB constraints can be individualized based on total daily insulin requirements and real-time glucose trends [18]. Adaptive IOB limits that adjust based on glucose levels and rates of change provide additional safety.
Trust Index and Residual Analysis: Several advanced MPC implementations incorporate prediction accuracy assessment through residual analysis. A "trust index" quantifies confidence in model predictions based on recent prediction errors. When confidence is low (high residuals), the controller becomes more conservative, while high confidence permits more aggressive control actions [37].
Pump Shut-Off Protocols: Safety modules can suspend insulin delivery when glucose levels are predicted to fall below threshold values (e.g., 100 mg/dL within 60 minutes) [18]. These predictive low-glucose suspend features provide critical protection against over-delivery following meal compensation.
Diagram 1: Integrated meal detection and MPC control architecture. The system combines continuous glucose monitoring, meal detection modules, and safety constraints within an MPC framework for automated insulin delivery.
Experimental Protocols and Validation
In Silico Validation Protocols
Computer simulation using FDA-accepted metabolic simulators provides a critical foundation for algorithm validation before human trials:
Simulation Environment: The University of Virginia/Padova T1D Simulator has been widely adopted for preclinical testing of AP algorithms [37]. This simulator incorporates a comprehensive model of glucose-insulin dynamics and includes 10 virtual adult subjects representing interindividual variability.
Protocol Design: Standard meal challenges typically include three meals of increasing carbohydrate content (e.g., 50g, 75g, 100g) over a 24-hour period. Simulations should be repeated multiple times (e.g., 100 repetitions) to account for CGM measurement noise and other stochastic elements [37].
Performance Metrics: Key evaluation metrics include:
- Mean glucose concentration
- Percentage time in target range (70-180 mg/dL)
- Percentage time in hypoglycemia (<70 mg/dL) and hyperglycemia (>180 mg/dL)
- Postprandial glucose excursion analysis
- Meal detection sensitivity and specificity
Clinical Validation Protocols
Study Design: Randomized crossover trials comparing the integrated meal detection/MPC system against standard MPC with meal announcement provide the most robust clinical evidence. Studies typically involve 12-24 participants with type 1 diabetes [67].
Meal Challenges: Standardized meals with varying carbohydrate content (typically 40-80g) are administered without announcement to the system. The timing and composition should reflect real-world eating patterns.
Outcome Measures: Primary outcomes focus on postprandial glucose control during the 4-hour period following meal ingestion:
- Incremental area under the curve (iAUC) of glucose
- Time in target range (70-180 mg/dL)
- Time above range (>180 mg/dL) and below range (<70 mg/dL)
- Meal detection performance (sensitivity, false positive rate, detection time)
Diagram 2: Clinical validation protocol for meal detection systems. The crossover design compares MPC performance with and without meal announcement following standardized meal challenges.
Research Reagent Solutions
Table 3: Essential Research Tools for Meal Detection Algorithm Development
| Research Tool | Function/Purpose | Example Implementation |
|---|---|---|
| UVA/Padova T1D Simulator | Preclinical algorithm validation | FDA-accepted metabolic simulator with 10 virtual subjects [37] |
| Continuous Glucose Monitor | Glucose data acquisition | Real-time glucose values at 5-minute intervals [68] |
| Insulin Pump | Insulin delivery implementation | Continuous subcutaneous insulin infusion (CSII) [68] |
| Meal Detection Algorithm | Unannounced meal identification | Fuzzy logic, UKF, or neural network approaches [68] [66] [67] |
| Model Predictive Control | Glucose regulation algorithm | Zone-MPC with asymmetric tuning parameters [37] |
| Insulin-on-Board Calculation | Safety constraint module | Pharmacodynamic model of insulin action [18] |
| Statistical Analysis Package | Performance quantification | RMSE, time-in-range, Clarke Error Grid analysis [65] |
Meal detection algorithms and compensation strategies represent a critical advancement toward fully automated insulin delivery systems. Current approaches demonstrate promising performance, with sensitivity rates exceeding 90% for some algorithms and significant improvements in postprandial glucose control when integrated with MPC frameworks. The combination of detection algorithms with robust safety constraints enables effective mitigation of unannounced meals while minimizing hypoglycemia risk.
Future research directions include the incorporation of additional signals such as physical activity and stress monitoring, the development of personalized detection thresholds based on individual glucose patterns, and the implementation of multi-hormone systems that combine insulin with amylin analogs or glucagon. As these technologies mature, fully automated insulin delivery systems without meal announcement will become increasingly feasible, substantially reducing the management burden for people with type 1 diabetes while improving glycemic outcomes.
In Model Predictive Control (MPC) for blood glucose regulation, the cost function is the central element that determines controller performance by quantifying the balance between multiple, often competing, control objectives. The general formulation of this finite-horizon optimization problem can be expressed as:
$$\min{uk, ..., u{k+N-1}} \sum{i=k}^{k+N-1} ||ri - yi||^2 + \sum{i=k}^{k+N-1} ||ui - u{i-1}||^2$$
subject to:
$$x{k+1} = f(xk, uk)$$
$$gj(xi, ui) \leq 0 \quad (j=1,2,...,m)$$
where u_k,\ldots, u_{k+N-1} are the control inputs, ri is the reference signal, yi is the system output, and f(xk, u_k) is the model prediction [69].
For Artificial Pancreas (AP) systems, the critical challenge lies in appropriately weighting these competing terms—primarily blood glucose tracking error versus control effort (hormone delivery)—to achieve safe and efficient glycemic control without excessive insulin or glucagon administration [70] [19]. The weighting factors associated with each term directly influence key performance metrics including time-in-range (TIR), hypoglycemia events, and controller aggressiveness [71] [70].
Quantitative Analysis of Weighting Factor Impacts
Table 1: Performance metrics influenced by cost function weighting factors in MPC for blood glucose regulation
| Control Objective | Performance Metric | Impact of Increased Weighting | Clinical Significance |
|---|---|---|---|
| Blood Glucose Tracking | Time in Range (TIR: 70-180 mg/dL) | Increases TIR | Primary efficacy measure; reduces long-term complications |
| Time Above Range (TAR: >180 mg/dL) | Decreases TAR | Reduces hyperglycemia symptoms & complications | |
| Time Below Range (TBR: <70 mg/dL) | May increase if over-weighted | Critical safety parameter; hypoglycemia prevention | |
| Control Effort (Insulin) | Total Daily Insulin Dose | Generally increases | Affects patient weight, cost, and hypoglycemia risk |
| Insulin Delivery Variability | Increases variability | May reduce insulin resistance but increase hypoglycemia risk | |
| Hormone Switching Frequency | Increases frequency | Particularly relevant in dual-hormone systems [70] | |
| Controller Performance | Computational Load | Increases with complexity | Critical for embedded implementations [19] |
| Postprandial Control | Improves with appropriate weighting | Addresses meal response challenges [70] | |
| Overnight Control | More stable with balanced weights | Prevents nocturnal hypoglycemia [70] |
Table 2: Comparison of weighting factor optimization methodologies for MPC in glucose regulation
| Optimization Method | Implementation Approach | Computational Burden | Adaptive Capability | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Manual Tuning | Offline, empirical | Low | None | Simple to implement; intuitive | Time-consuming; suboptimal; non-adaptive [71] |
| Genetic Algorithm (GA) | Offline optimization | High | None | Systematic; Pareto-optimal solutions | Computationally expensive; requires extensive simulations [71] |
| Deep Reinforcement Learning (DRL) | Online learning | Moderate to High (training); Low (deployment) | High | Adapts to individual patient dynamics; handles nonlinearities | Complex implementation; requires extensive training data [71] |
| Neural Network Approximation | Offline training; online execution | Low (deployment) | Moderate via retraining | Fast online execution; suitable for embedded systems | Limited to trained operating conditions; data quality critical [19] |
| Ensemble Data Assimilation (EnMPC) | Online optimization | Moderate | High | Handles uncertainty well; suitable for nonlinear systems | Emerging method; less validated in clinical applications [72] |
Experimental Protocols for Weighting Factor Optimization
Protocol 1: Generating Optimally-Sampled Datasets (OSD) for Neural Network Training
This protocol enables the creation of optimized training datasets for approximating MPC behavior with neural networks, facilitating implementation in resource-constrained embedded devices like insulin pumps [19].
Research Reagent Solutions:
- T1DiabetesGranada Dataset: Comprehensive longitudinal dataset with glucose measurements every 15 minutes for 736 patients with Type 1 Diabetes [70].
- Bergman Minimal Model (BMM): Fundamental physiological model of glucose-insulin dynamics used for controller design and simulation [70].
- Matlab/Simulink with MPCTools: Software environment for MPC design, simulation, and code generation.
- Arduino UNO with Continuous Glucose Monitor (CGM) Interface: Hardware platform for prototyping embedded control systems [70].
Procedure:
- Data Collection Phase:
- Generate synthetic state-control pairs {xi, ui} through extensive closed-loop simulations using the MPC controller and physiological model (e.g., BMM).
- Ensure coverage of the entire operational state space, including various glycemic states (hypo-, hyper-, and normoglycemia) and disturbance conditions (meals, exercise, stress).
Dataset Optimization Phase:
- Apply the OSD algorithm to eliminate duplicate or near-duplicate states while preserving numerical resolution and MPC information.
- Achieve dataset saturation where additional samples provide diminishing returns for NN accuracy.
- Validate dataset completeness through cross-validation with unseen test scenarios.
Neural Network Training Phase:
- Train ReLU-based neural networks using the optimized dataset to approximate the MPC control law.
- Employ standard deep learning frameworks (TensorFlow, PyTorch) for training.
- Validate NN performance against original MPC across the entire operational envelope.
Embedded Implementation Phase:
- Deploy the trained NN on target embedded hardware (Arduino, insulin pump processor).
- Verify real-time performance and memory footprint meet device constraints.
OSD Generation Workflow: Method for creating optimized training datasets to implement MPC via neural networks in embedded medical devices [19].
Protocol 2: Event-Triggered Dual-Hormone Control with Adaptive Weighting
This protocol describes the implementation of a Smart Dual Hormone Artificial Pancreas (SDHAP) with event-triggered feedback-feedforward control, which dynamically adjusts controller behavior based on predicted glycemic states [70].
Research Reagent Solutions:
- Support Vector Machine (SVM) / k-Nearest Neighbor (kNN): Machine learning classifiers for hypoglycemia and hyperglycemia event detection [70].
- ARIMA / GRU Models: Time-series prediction models for future blood glucose level forecasting [70].
- Event-Triggered Control Framework: Software architecture for reducing unnecessary control computations and hormone administrations.
- Dual-Hormone Delivery System: Hardware setup with separate insulin and glucagon reservoirs and precision pumping mechanisms.
Procedure:
- Glycemic Event Classification:
- Extract relevant features from CGM data including Time in Range (TIR), Time Below Range (TBR), Time Above Range (TAR), and spectral characteristics.
- Train SVM and kNN classifiers to identify hypoglycemic and hyperglycemic events using the T1DiabetesGranada dataset.
- Validate classification accuracy using standard metrics (precision, recall, F1-score).
Blood Glucose Prediction:
- Implement ARIMA and Gated Recurrent Unit (GRU) models to predict future glucose trends.
- Compare prediction performance using Root Mean Square Error (RMSE) and Mean Absolute Error (MAE).
- Establish prediction horizons appropriate for MPC (typically 30-120 minutes).
Event-Triggered Controller Design:
- Design a dual-hormone MPC based on the Bergman Minimal Model for both insulin and glucagon delivery.
- Implement feedforward control for meal disturbance rejection.
- Develop event-triggering logic to activate controller updates only when needed, reducing computational load and preventing simultaneous hormone infusion.
Hardware Implementation:
- Prototype using Arduino UNO, NEMA 17 stepper motors with TB6560 drivers, and 10ml syringes.
- Coordinate control logic between MATLAB and Arduino IDE.
- Validate system response to glycemic events in simulated and clinical environments.
SDHAP Control Architecture: Event-triggered framework for dual-hormone delivery that activates control actions based on predicted glycemic events [70].
Advanced Tuning Methodologies
Deep Reinforcement Learning for Adaptive Weighting
Recent advances have demonstrated the efficacy of Deep Reinforcement Learning (DRL) for online optimization of weighting factors in complex MPC applications. The Twin Delayed Deep Deterministic Policy Gradient (TD3) algorithm can be adapted for blood glucose regulation to formulate an optimal policy for weighting factor selection [71].
Implementation Framework:
- State Space Definition: Include current glucose level, rate of change, time of day, meal announcements, and recent insulin delivery.
- Action Space: Continuous adjustment of weighting factors for glucose tracking error, insulin delivery, and glucagon delivery terms in the cost function.
- Reward Function: Design to maximize time-in-range while minimizing hypoglycemia events and excessive control action.
- Training Environment: Use high-fidelity physiological simulators (e.g., UVa/Padova T1D Simulator) that incorporate meal and exercise disturbances.
Ensemble-Based MPC with Integrated Data Assimilation
The Ensemble MPC (EnMPC) framework combines MPC with ensemble data assimilation techniques to directly solve the cost function using ensemble smoother methods, including 4DEnsembleVariational (4DEnVar) and Ensemble Kalman Smoother (EnKS) [72].
Key Advantages for Glucose Regulation:
- Naturally handles uncertainty in glucose measurements and model predictions
- Uses analysis error covariance from ensemble data assimilation to determine optimal weights for control inputs
- Provides two approaches for control objectives: penalty term approach and trajectory-tracking approach
- Reduces computational burden through ensemble approximations compared to conventional MPC
Table 3: Comparison of optimization algorithms for MPC implementation in embedded glucose regulation devices
| Algorithm Characteristic | Conventional MPC Solver | Neural Network Approximation | Explicit MPC |
|---|---|---|---|
| Computational Complexity | High (iterative optimization) | Low (single forward pass) | Moderate (piecewise affine evaluation) |
| Memory Requirements | Low to Moderate | Moderate to High (network weights) | High (region coefficients) |
| Implementation Platform | Powerful processors | Embedded microcontrollers | Specialized hardware |
| Regulatory Certification | Well-established pathway | Emerging methodology (recently approved for clinical trials) | Established for smaller problems |
| Adaptability to Individual Patients | High (online adaptation possible) | Requires retraining | Fixed after design |
| Performance Guarantees | Convergence certifications available | Dependent on training data quality and coverage | Exact within regions |
The optimization of weighting factors and cost function formulations represents a critical advancement in MPC for blood glucose regulation. Through methodologies ranging from neural network approximation and deep reinforcement learning to ensemble-based control, researchers can now achieve more personalized and adaptive glycemic control while addressing the computational constraints of embedded medical devices.
The experimental protocols presented provide systematic approaches for implementing these advanced tuning methodologies, with the Optimally-Sampled Dataset method offering a pathway to certified implementations for clinical use. As these technologies continue to evolve, the integration of adaptive weighting factors tuned to individual patient dynamics and contextual factors (meals, exercise, stress) will further enhance the safety and efficacy of artificial pancreas systems.
For practical implementation, researchers should consider the trade-offs between computational complexity, adaptation capability, and certification requirements when selecting appropriate tuning methodologies for their specific application constraints and performance objectives.
Clinical Evidence, Safety Profiles, and Comparative Effectiveness
The artificial pancreas (AP) represents a revolutionary advancement in the management of Type 1 Diabetes (T1D), automating insulin delivery through a combination of continuous glucose monitors (CGMs), insulin pumps, and control algorithms [4]. At the heart of these systems lies the control algorithm, which determines the appropriate insulin infusion rates in response to dynamically changing glucose levels. For years, two primary control strategies have emerged as front-runners: Model Predictive Control (MPC) and Proportional-Integral-Derivative (PID) control [73]. The debate over which algorithm offers superior performance has persisted due to the difficulty of comparing results across studies with differing conditions, such as patient populations, device types, and trial protocols [74].
This application note synthesizes findings from the first comprehensive, head-to-head randomized crossover evaluation of MPC and PID controllers under identical clinical conditions. Such a design eliminates inter-trial variability, providing a clear, comparative analysis of their efficacy and safety in blood glucose regulation [74] [75]. Framed within broader research on MPC algorithms, this document details the experimental protocols, presents quantitative outcomes, and offers insights for researchers and drug development professionals working on advanced insulin delivery systems.
Algorithmic Foundations: MPC vs. PID
Core Operational Principles
The fundamental difference between the algorithms lies in their operational philosophy.
Proportional-Integral-Derivative (PID) Control: A reactive controller, the PID algorithm adjusts the insulin infusion rate based on the present error (the deviation of the current glucose level from the target setpoint), the integral of past errors, and the derivative (rate of change) of the error [73]. It functions similarly to a home thermostat, reacting to changes as they occur.
Model Predictive Control (MPC): A proactive controller, MPC utilizes an internal model of the patient's glucose-insulin dynamics to predict future glucose trajectories. It computes insulin deliveries by optimizing a cost function over a finite prediction horizon, enabling it to anticipate and prevent future hypo- or hyperglycemic events [73]. This predictive capability is a key differentiator.
As summarized in the literature, "MPC is proactive, allowing the system to think multiple steps ahead, predicting when the body may need more or less insulin and planning in advance" [73]. In contrast, a PID-based system is reactive.
Visualizing the Conceptual Workflow
The diagram below illustrates the core logical difference in how each algorithm determines an insulin dose.
Experimental Protocol: The Head-to-Head Crossover Trial
Study Design and Participant Profile
The foundational study for this analysis was a single-center, randomized, crossover trial conducted at the William Sansum Diabetes Center [76] [74].
- Design: Randomized, two-period crossover.
- Participants: 20 adults with T1D (completed the main study, following a pilot safety study of n=10).
- Inclusion Criteria: Age 21-65 years, clinical diagnosis of T1D for ≥1 year, use of an insulin pump for ≥6 months, HbA1c between 5-10% [76] [74].
- Interventions: Each subject underwent two 27.5-hour supervised closed-loop sessions, one governed by a personalized MPC algorithm and the other by a PID algorithm, separated by 5-14 days [74].
Closed-Loop System and Procedures
The portable Artificial Pancreas System (pAPS) integrated commercial devices with research algorithms.
- System Components:
- Sensors: Two Dexcom G4 Platinum CGM sensors.
- Pump: Animas OneTouch Ping insulin pump.
- Controller: A portable artificial pancreas system (pAPS v1.9.8.1) running on a Windows tablet, which housed the control algorithms [74].
- Meal Challenges: The protocol was designed to test the algorithms under non-ideal, realistic conditions:
- Announced Meals: A 65g carbohydrate (CHO) dinner and a 50g CHO breakfast, both preceded by a manual insulin bolus given at mealtime (100% based on the subject's insulin-to-carbohydrate ratio).
- Unannounced Meal: A 65g CHO lunch with no pre-meal bolus, simulating a common real-world scenario where a patient forgets to bolus [74].
- Safety: An independent Health Monitoring System (HMS) provided an additional safety layer by alerting for confirmed hypoglycemia, requiring carbohydrate intervention [74].
Visualizing the Trial Workflow
The following diagram outlines the sequential flow of the clinical trial, from participant recruitment through data analysis.
Quantitative Outcomes and Performance Metrics
Primary and Secondary Endpoint Results
The primary outcome was the percentage of time the sensor glucose was maintained in the target range of 70-180 mg/dL. Secondary outcomes included mean glucose, time in hypoglycemic and hyperglycemic ranges, and performance after the unannounced meal.
Table 1: Key Glycemic Outcomes from the Randomized Crossover Trial
| Outcome Measure | MPC Performance | PID Performance | P-value |
|---|---|---|---|
| Time in Range (70–180 mg/dL) | 74.4% | 63.7% | 0.020 |
| Mean Glucose (entire trial) | 138 mg/dL | 160 mg/dL | 0.012 |
| Time in Hypoglycemia (<70 mg/dL) | No significant difference | No significant difference | N/S |
| Mean Glucose (5h post-unannounced meal) | 181 mg/dL | 220 mg/dL | 0.019 |
The results demonstrate that the MPC algorithm achieved a statistically significant 10.7% absolute increase in time in range compared to PID. This superiority was particularly evident following the unannounced meal challenge, where MPC's predictive capabilities led to significantly better glucose handling [74] [75].
Broader Context: Meta-Analysis and Real-World Evidence
A 2022 systematic review and meta-analysis of 41 studies further corroborates the effectiveness of MPC-based systems, showing a statistically significant improvement in time in range during overnight use compared to conventional therapy [4]. Furthermore, real-world studies comparing commercial AHCL systems reveal nuanced performance differences.
Table 2: Real-World Nocturnal Performance of Commercial AHCL Systems
| CGM Metric (Nighttime) | Minimed 780G (PID-based) | Tandem t:slim X2 (MPC-based) | DBLG1 (MPC-based) |
|---|---|---|---|
| Time in Range (70–180 mg/dL) | 73.9% | 74.1% | 71.7% |
| Tight Time in Range (70–140 mg/dL) | 42.1% | 51.5% | 40.1% |
| Time in Hypoglycemia (<70 mg/dL) | 0.9% | 1.1% | 1.4% |
| Coefficient of Variation (CV) | 29.0% | 34.5% | 32.4% |
Data adapted from [77]. All systems achieved recommended targets, but the MPC-based Control-IQ system delivered a higher tight time in range.
The Scientist's Toolkit: Research Reagents and Materials
For researchers aiming to replicate or build upon such clinical trials, a core set of reliable components is essential. The following table details key materials used in the featured study.
Table 3: Essential Research Materials for Artificial Pancreas Trials
| Component | Example Product/Model | Function in the Experimental System |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Dexcom G4 Platinum [74] | Measures interstitial glucose concentrations at 5-minute intervals, providing real-time data to the control algorithm. |
| Insulin Pump | Animas OneTouch Ping [74] | Delivers subcutaneous rapid-acting insulin infusions (both basal and bolus) as commanded by the control algorithm. |
| Control Algorithm Platform | Portable AP System (pAPS) [74] | The software platform (e.g., on a tablet computer) that hosts the MPC or PID control algorithm and coordinates communication between system components. |
| Health Monitoring System (HMS) | UCSB Health Monitoring System [74] | An independent safety algorithm that monitors for impending hypoglycemia and alerts for confirmatory fingerstick checks and carbohydrate intervention. |
| Reference Glucose Analyzer | YSI 2300 Stat [74] | Provides laboratory-grade blood glucose measurements for point-of-care calibration and validation of CGM accuracy during in-clinic studies. |
Discussion and Research Implications
The direct, head-to-head comparison confirms that while both MPC and PID controllers provide safe and effective automated glucose management, the MPC algorithm performs as well as or better than PID across all key metrics [74] [75]. Its principal advantage lies in its predictive nature, which allows it to proactively mitigate glycemic excursions, especially after unannounced meals—a common stressor in everyday life [73].
From a research perspective, the flexibility of the MPC framework is a significant asset. As noted by researchers, "This is the first real head-to-head clinical study that compares the two lead controllers in identical conditions... we showed that there are scenarios in which MPC is superior, due to the flexibility of that design" [73]. This flexibility allows for the incorporation of more complex patient models, adaptation to individual time-varying insulin sensitivities, and integration of additional disturbances like exercise or stress [74] [78].
Future research directions should focus on long-term, fully outpatient trials to validate these findings in unsupervised environments. Furthermore, the development of adaptive MPC algorithms that can learn from individual patient data over time promises to further enhance personalization and performance, moving closer to the goal of a fully autonomous artificial pancreas [73] [4].
Model Predictive Control (MPC) has emerged as a leading algorithm for the artificial pancreas (AP), an automated system designed to regulate blood glucose levels in individuals with Type 1 Diabetes (T1D). The core strength of MPC lies in its predictive capability; it uses a model of the patient's glucose-insulin dynamics to forecast future glucose levels and preemptively calculates insulin doses to maintain glucose within a target range (typically 70-180 mg/dL or 3.9-10.0 mmol/L) [79] [9]. This is particularly valuable for mitigating the inherent delays in subcutaneous insulin absorption and glucose sensing.
Time-in-Range (TIR), the percentage of time a patient spends in the target glycaemic range, has become a critical endpoint for evaluating diabetes therapies. This application note synthesizes recent clinical evidence and experimental protocols to analyze the performance of MPC-based AP systems across different intervention periods, specifically comparing overnight versus 24-hour control. The analysis is framed within the broader thesis that MPC is a superior control strategy for T1D, offering enhanced safety and effectiveness by proactively managing glycaemic excursions.
Quantitative Analysis of MPC Performance
A comprehensive meta-analysis of 41 randomized controlled trials provides robust, quantitative evidence for the efficacy of MPC-based AP systems compared to conventional insulin therapy (such as sensor-augmented pumps [SAP] and continuous subcutaneous insulin infusion [CSII]) [79]. The performance is best understood by separating the outcomes based on the duration of intervention.
Table 1: MPC Performance vs. Conventional Therapy (Overnight Use) [79]
| Outcome Measure | Mean Difference (MD) | 95% Confidence Interval (CI) | P-value |
|---|---|---|---|
| Time in Target Range | +10.03% | [7.50, 12.56] | < 0.00001 |
| Time in Hypoglycaemia (< 3.9 mmol/L) | -1.34% | [-1.87, -0.81] | < 0.00001 |
The data reveals that overnight use of an MPC-based AP significantly improves glycaemic control by substantially increasing TIR while simultaneously reducing the risk of hypoglycaemia, a primary safety concern [79]. This performance is maintained over the long term, with the hypoglycaemia reduction being statistically significant in follow-up periods exceeding one month.
When comparing MPC against other control algorithms under identical, challenging conditions, its advantages become even more pronounced. A randomized crossover trial directly compared MPC with a Proportional-Integral-Derivative (PID) algorithm [74].
Table 2: MPC vs. PID Algorithm Performance in a 27.5-Hour Trial [74]
| Outcome Measure | MPC Performance | PID Performance | P-value |
|---|---|---|---|
| Overall Time in Range (70–180 mg/dL) | 74.4% | 63.7% | 0.020 |
| Mean Glucose (entire trial) | 138 mg/dL | 160 mg/dL | 0.012 |
| Mean Glucose (post-unannounced meal) | 181 mg/dL | 220 mg/dL | 0.019 |
| Time in Hypoglycaemia (< 70 mg/dL) | No significant difference | No significant difference | N/S |
This study demonstrates that MPC performs as well as or better than PID in all metrics, particularly in managing the challenging scenario of an unannounced meal, a common real-world stressor [74]. The ability to handle such unmeasured disturbances is a key feature of advanced MPC implementations [13].
Experimental Protocols for MPC Evaluation
To ensure reproducible and comparable results in AP research, standardized experimental protocols are essential. The following details a key clinical trial design that has yielded significant insights into MPC performance.
Randomized Crossover Comparison of MPC and PID
This protocol is designed to rigorously compare two control algorithms under identical, non-ideal conditions to simulate realistic use [74].
- Objective: To evaluate the effectiveness and safety of personalized MPC and PID control algorithms for an AP under challenging, realistic conditions.
- Subjects: Adults (21-65 years) with T1D for >1 year, using an insulin pump for ≥6 months.
- Study Design: A randomized, crossover trial where each subject undergoes two separate 27.5-hour supervised closed-loop sessions, one with MPC and one with PID, in a randomized order.
- System Components:
- Continuous Glucose Monitors (CGM): Two Dexcom G4 Platinum sensors.
- Insulin Pump: Animas OneTouch Ping.
- Control Platform: Portable Artificial Pancreas System (pAPS) running on a Windows tablet.
- Intervention & Challenges:
- Session Duration: 27.5 hours of closed-loop control.
- Announced Meals: A 65-g dinner (∼7:00 p.m.) and a 50-g breakfast (∼7:00 a.m.), with boluses given at mealtime (not pre-bolused).
- Unannounced Meal: A 65-g lunch (∼1:00 p.m.) with no bolus, testing the system's response to a missed meal scenario.
- Overnight Period: Control is assessed from midnight to 7:00 a.m. following the announced dinner.
- Primary Outcome: Percentage of time in glucose range (70–180 mg/dL).
- Safety: An independent Health Monitoring System (HMS) algorithm provides alerts for impending hypoglycaemia, requiring a fingerstick confirmation and carbohydrate intervention if necessary [74].
In Silico Validation Protocol
Before clinical trials, in silico (simulation) trials are crucial for validating and tuning MPC algorithms. The following workflow is adapted from a foundational study [3].
Technical Implementation of an MPC Algorithm
The core of an AP system is its control algorithm. This section outlines the key components and a recent advancement in implementing MPC for blood glucose regulation.
The MPC Control Loop
The following diagram illustrates the core structure and data flow of a typical MPC-based artificial pancreas system, incorporating elements from the described protocols and technical papers [79] [9] [13].
Enhancing Prediction with Data-Driven Models
A limitation of traditional MPC is its reliance on linear models, which can struggle with the body's non-linear response to events like meals. A novel approach involves using Long Short-Term Memory (LSTM) networks, a type of recurrent neural network, to learn more accurate multi-step-ahead predictors of blood glucose from data [9].
- Predictor Structure: The predictor is constructed as the superposition of a non-linear function (the LSTM) of past inputs and outputs and an affine function of future control moves (insulin doses). This structure maintains the convexity of the MPC optimization problem, allowing it to be solved efficiently via Quadratic Programming (QP) [9].
- Advantage: This data-driven LSTM predictor significantly increases the accuracy of long-term predictions compared to standard linear autoregressive (ARX) models, leading to improved post-meal glucose control and reduced risk of controller-induced hypoglycaemia [9].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for AP Research
| Item | Function & Application in Research |
|---|---|
| Dexcom G4 Platinum CGM | A continuous glucose monitoring system used to provide real-time, subcutaneous glucose measurements to the control algorithm every 5 minutes [74]. |
| Animas OneTouch Ping Pump | An insulin infusion pump used in clinical trials to deliver subcutaneously the insulin doses commanded by the AP control algorithm [74]. |
| Portable AP System (pAPS) | A software platform, often running on a tablet computer, that integrates the CGM data, runs the control algorithm (MPC/PID), and commands the insulin pump [74]. |
| Health Monitoring System (HMS) | An independent safety software layer that monitors for impending hypoglycaemia and alerts for carbohydrate intervention, adding a critical safety backup to the primary controller [74]. |
| UVa/Padova T1D Simulator | A widely accepted metabolic model of glucose metabolism equipped with a cohort of in-silico adult subjects. It is a vital tool for the preliminary design, testing, and validation of MPC algorithms before clinical trials [9] [3]. |
| LSTM Network Predictor | A data-driven modelling approach used to enhance the prediction accuracy of MPC, leading to better handling of non-linearities and long-term predictions after meals [9]. |
| Stochastic Meal Generator | A software tool designed to create realistic meal ingestion patterns based on the eating habits of a cohort of subjects with T1D, used for robust in-silico testing [9]. |
Maintaining optimal blood glucose levels is a fundamental challenge in diabetes management, with hypoglycemia representing a significant and potentially dangerous complication. This document synthesizes findings from recent meta-analyses and clinical studies to provide a comprehensive overview of evidence-based strategies for hypoglycemia risk reduction. The content is specifically framed within ongoing research into Model Predictive Control (MPC) algorithms for automated blood glucose regulation systems. For researchers and drug development professionals, this analysis provides critical insights into comparative safety profiles of various interventions and methodological approaches for evaluating hypoglycemia outcomes in clinical studies.
The progressive nature of diabetes often necessitates intensified treatment regimens over time, which inherently increases hypoglycemia risk [80]. Technological advancements in continuous glucose monitoring (CGM) and automated insulin delivery systems have created new opportunities for hypoglycemia prevention through predictive algorithms and optimized titration strategies. This review systematically examines the efficacy of these approaches through the lens of recent meta-analytical findings, with particular emphasis on safety superiority.
Quantitative Meta-Analysis Findings on Hypoglycemia Risk
Recent systematic reviews and meta-analyses have provided robust quantitative assessments of hypoglycemia risk across various diabetes management strategies. The table below summarizes key findings from recent studies:
Table 1: Hypoglycemia Risk Outcomes from Recent Meta-Analyses
| Intervention | Comparator | Risk Ratio for Hypoglycemia | Confidence Interval | References |
|---|---|---|---|---|
| IcoSema (once-weekly) | Basal-bolus insulin | Reduced risk | Significant reduction (P-value reported) | [81] |
| IDegLira | Insulin degludec | Comparable risk | No significant difference | [80] |
| Self-titration with HCP support | Other titration strategies | No significant increase | No significant difference | [82] |
| MPC-based Artificial Pancreas | Conventional insulin therapy | Reduced time in hypoglycemic range | -1.34% [-1.87, -0.81] (p<0.00001) | [79] |
The quantitative synthesis demonstrates that structured self-titration protocols with healthcare provider (HCP) support achieved superior glycemic control (HbA1c reduction) without increasing severe hypoglycemia risk compared to other titration methods [82]. Meanwhile, advanced insulin formulations like IcoSema showed improved glycemic control with lower hypoglycemia risk compared to traditional basal-bolus regimens [81].
For artificial pancreas systems, MPC algorithms demonstrated statistically significant reduction in hypoglycemia exposure, particularly during overnight use with longer follow-up periods (>1 month), reducing time in hypoglycemic range by -1.34% (95% CI [-1.87, -0.81]) compared to conventional insulin therapy [79].
Model Predictive Control: A Superior Framework for Hypoglycemia Prevention
MPC Mechanism of Action for Hypoglycemia Risk Reduction
Model Predictive Control algorithms represent a transformative approach to automated insulin delivery by employing a proactive, predictive methodology rather than reactive glucose management. The fundamental advantage of MPC lies in its ability to forecast future glucose levels and make preemptive adjustments to insulin delivery, thereby preventing both hyperglycemic and hypoglycemic events before they occur [73] [9].
The core differentiator between MPC and traditional control algorithms is this predictive capability. As noted in clinical comparisons, "MPC is proactive, allowing the system to think multiple steps ahead, predicting when the body may need more or less insulin and planning in advance" [73]. This contrasts with proportional-integral-derivative (PID) controllers, which operate reactively based on current glucose levels without anticipating future trends.
Clinical Evidence for MPC Superiority
Head-to-head clinical trials have demonstrated the superiority of MPC frameworks for hypoglycemia prevention. In the first randomized crossover evaluation comparing MPC with PID controllers under identical conditions, MPC maintained participants within safe glucose range 74% of the time compared to 64% for PID when challenged with unannounced meals [73]. This 10-percentage point improvement in time-in-range represents a significant clinical advancement for hypoglycemia prevention.
A comprehensive meta-analysis of 41 randomized controlled trials further confirmed these findings, showing that MPC-based artificial pancreas systems used overnight produced a statistically significant reduction in time spent in hypoglycemic range (-1.34%, 95% CI [-1.87, -0.81], p<0.00001) over longer follow-up periods (>1 month) [79]. The analysis noted that this improvement occurred while simultaneously increasing time in target range, demonstrating that MPC enhances overall glycemic control without the traditional trade-off of increased hypoglycemia risk.
Experimental Protocols for Hypoglycemia Risk Assessment
Protocol: MPC Algorithm Validation for Nocturnal Hypoglycemia Prevention
Table 2: Key Research Reagent Solutions for MPC Algorithm Development
| Reagent/Technology | Function | Application Example |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Provides real-time interstitial glucose measurements | Dexcom G5/G6, Medtronic Guardian [83] |
| Insulin Pump | Subcutaneous insulin infusion with precise dosing control | Tandem t:slim X2, Medtronic 670G [79] |
| UVA/Padova T1D Simulator | Academic simulator with 10 in-silico adult subjects for preclinical testing | Validation of MPC algorithms in controlled virtual environment [9] |
| Stochastic Meal Generator | Reproduces realistic eating patterns for algorithm testing | Creates identification and validation scenarios for predictor development [9] |
| Long Short-Term Memory (LSTM) Networks | Neural network architecture for glucose prediction | Multi-step ahead blood glucose predictors in data-driven MPC [9] |
Objective: To evaluate the efficacy of MPC algorithms in preventing nocturnal hypoglycemia events in adults with type 1 diabetes over a 4-week intervention period.
Study Design: Randomized crossover trial comparing MPC-based automated insulin delivery against sensor-augmented pump (SAP) therapy.
Participants:
- Inclusion: Adults (18-65 years) with T1D duration >1 year, HbA1c 7.0-9.0%
- Exclusion: History of severe hypoglycemia in past 6 months, pregnancy, renal impairment
- Sample Size: 30 participants providing 80% power to detect 30% reduction in nocturnal hypoglycemia events
Intervention Protocol:
- Run-in period: 1 week of CGM wear with current therapy
- Randomization: Participants receive either MPC system or SAP therapy for 4 weeks
- Washout: 1-week period with usual therapy
- Crossover: Switch to opposite intervention for 4 weeks
MPC System Configuration:
- Control Algorithm: Linear time-varying MPC with 90-minute prediction horizon
- Model Adaptation: Data-driven individualized model tuning based on first 3 days of CGM data
- Safety Constraints: Hypoglycemia early alert system with insulin suspension threshold at 80 mg/dL and predicted threshold of 70 mg/dL within 45 minutes
- Meal Announcement: Partial meal announcement to simulate real-world conditions
Primary Outcome:
- Percentage of time spent <70 mg/dL between 0000-0600 hours measured by CGM
Secondary Outcomes:
- Number of nocturnal hypoglycemia events (<54 mg/dL for >15 minutes)
- Mean nocturnal glucose value
- Time-in-range (70-180 mg/dL) during nocturnal period
- Total daily insulin dose
Statistical Analysis:
- Paired t-tests for continuous variables (or non-parametric equivalents)
- Generalized linear mixed models for repeated measures
- Significance threshold: p<0.05
This protocol design reflects methodology employed in recent meta-analyses demonstrating MPC efficacy for nocturnal hypoglycemia prevention [79].
Protocol: Hypoglycemia Prediction Algorithm Validation
Objective: To develop and validate machine learning algorithms for predicting hypoglycemia events 30-120 minutes before occurrence.
Data Collection:
- CGM Data: Continuous glucose monitoring at 5-minute intervals
- Additional Inputs: Heart rate, step count, calories burned (from wearable devices)
- Demographic Data: Age, diabetes duration, HbA1c, insulin regimen
- Outcome Definition: Hypoglycemia event (confirmed glucose <70 mg/dL within prediction horizon)
Feature Engineering:
- Short-term features (1-hour window): Current reading, rate of change, variability metrics
- Medium-term features (24-hour window): Time-in-range, glucose standard deviation, fasting glucose
- Long-term features (1-week window): Mean glucose, coefficient of variation, hypoglycemia pattern analysis
Algorithm Development:
- Comparative Models: Random Forest, XGBoost, Structured Grammatical Evolution, LSTM networks
- Interpretability Framework: SHAP (SHapley Additive exPlanations) for feature importance
- Validation Approach: 5-fold cross-validation with stratified sampling
Performance Metrics:
- Area Under Receiver Operating Curve (AUROC)
- Sensitivity (True Positive Rate)
- Specificity (True Negative Rate)
- Average Precision
- Alert Fatigue Assessment: False alerts per day
Recent studies have demonstrated excellent prediction performance with AUROC scores of 0.998 for hypoglycemia and 0.989 for hyperglycemia using XGBoost models with comprehensive feature engineering [83]. Structured Grammatical Evolution approaches have generated interpretable models with True Positive and True Negative Rates above 0.90 for 30-minute predictions [84].
The meta-analysis findings presented in this document consistently demonstrate that structured approaches to diabetes management significantly reduce hypoglycemia risk while maintaining or improving glycemic control. Key strategies with established safety superiority include:
- MPC-based automated insulin delivery systems that proactively prevent hypoglycemia through predictive modeling
- Structured self-titration protocols with healthcare provider support that balance efficacy and safety
- Advanced insulin formulations that offer improved therapeutic profiles
- Machine learning prediction algorithms that enable early intervention before hypoglycemia occurs
For researchers and drug development professionals, these findings highlight the critical importance of algorithmic approaches to hypoglycemia prevention rather than solely focusing on pharmaceutical interventions. The integration of advanced control algorithms with optimized therapeutic agents represents the most promising pathway for further reducing hypoglycemia risk in diabetes management.
Future research should focus on personalized MPC algorithms that adapt to individual physiological responses and explainable hypoglycemia prediction models that provide actionable insights to both patients and clinicians. As these technologies evolve, the integration of multi-hormonal control systems and expanded input parameters from wearable devices will likely further enhance hypoglycemia prevention capabilities.
Model Predictive Control (MPC) has emerged as a dominant control strategy for automated insulin delivery (AID) in the management of Type 1 Diabetes (T1D). Its ability to forecast future glucose levels and proactively determine optimal insulin doses makes it particularly suited for handling the complex, dynamic physiology of glucose regulation. The performance of these algorithms is quantified using a standard set of clinical metrics that assess safety and efficacy. This Application Note provides a structured overview of these key performance metrics, summarizes quantitative data from established and research-grade AID systems, and details experimental protocols for their pre-clinical evaluation, framed within the context of MPC algorithm development.
Key Performance Metrics for AID Systems
The performance of AID systems utilizing MPC is evaluated against a suite of standardized metrics derived from continuous glucose monitoring (CGM) data and insulin delivery logs [85] [16]. Table 1 defines the core metrics used to assess glycemic control, while Table 2 outlines metrics specific to insulin delivery and system operation.
Table 1: Primary Glycemic Control Metrics for AID System Evaluation
| Metric | Definition | Clinical/Research Significance |
|---|---|---|
| Time in Range (TIR) | Percentage of time CGM values are within 70–180 mg/dL [85] [86]. | Primary efficacy endpoint; higher TIR correlates with reduced complication risk [85]. |
| Time in Tight Range (TITR) | Percentage of time CGM values are within 70–140 mg/dL. | Indicator of tighter glycemic control. |
| Time in Hyperglycemia | Percentage of time CGM values are >180 mg/dL [86]. | Safety endpoint; indicates insufficient insulin delivery. |
| Time in Hypoglycemia | Percentage of time CGM values are <70 mg/dL [86]. | Critical safety endpoint; indicates excessive insulin delivery. |
| Mean Glucose | Arithmetic mean of all CGM values (mg/dL) [85]. | Provides a central tendency measure of glycemia. |
| Glucose Management Indicator (GMI) | Estimated HbA1c (%) calculated from mean CGM glucose [85]. | Standardized reporting of estimated long-term control. |
| Average Tracking Error (ATE) | Average deviation of blood glucose from a setpoint (e.g., 90 mg/dl) [13]. | Metric for controller performance in research simulations [13]. |
Table 2: Insulin Delivery and System Performance Metrics
| Metric | Definition | Clinical/Research Significance |
|---|---|---|
| Total Daily Insulin (TDI) | Total insulin (units) delivered by the system over 24 hours [87]. | Measures overall insulin consumption. |
| Basal-Bolus Split | Proportion of TDI delivered as basal vs. bolus insulin. | Insights into controller behavior (e.g., meal response). |
| Insulin-on-Board (IOB) Constraint | A safety constraint that limits insulin infusion based on estimated active insulin in the body [88] [86]. | Critical for mitigating hypoglycemia risk [86]. |
| Controller Updates | Number of times the control algorithm is invoked per hour [88]. | Key for evaluating computational efficiency of embedded systems [88]. |
| Processor Runtime | Total time the processor is active computing control actions [88]. | Directly impacts energy consumption in wearable devices [88]. |
Performance Data of Established and Research AID Systems
Table 3 consolidates performance data from commercial systems and research algorithms, illustrating the current state of the field. Note that sensor performance can influence CGM-derived metrics, and comparisons across systems using different sensors should be interpreted with caution [85].
Table 3: Comparative Performance of AID Systems in Clinical and Pre-clinical Studies
| System / Algorithm | TIR (%) | Mean Glucose (mg/dL) | Time <70 mg/dL (%) | Time >180 mg/dL (%) | Study Context |
|---|---|---|---|---|---|
| Tandem Control-IQ | 67.0 - 74.99 [85] | ~160 (8.9 mmol/L) [85] | Not Specified | Not Specified | Clinical Study (Real-world) |
| Minimed 780G | 73.77 - 77.38 [85] | ~150 (8.3 mmol/L) [85] | Not Specified | Not Specified | Clinical Study (Real-world) |
| MPC with Pramlintide | 91.6 [89] | Not Specified | Not Specified | Not Specified | In-silico Trial |
| Insulin-Only MPC | 64.1 [89] | Not Specified | Not Specified | Not Specified | In-silico Trial |
| Offset-free MPC (Rat Model) | 83.4 [16] | Not Specified | Mild events: 3.62 ± 1.8 cases [16] | Peak at 320 mg/dL (regulated in 50 min) [16] | Pre-clinical (In-vivo) |
| Single MPC (Insulin & Glucagon) | Not Specified | ATE: 4.4 mg/dl [13] | Hypoglycemia risk lowered [13] | Not Specified | In-silico Simulation |
Experimental Protocols for Pre-clinical AID Evaluation
A standardized, multi-stage testing protocol is essential for the rigorous development of MPC-based AID systems. The following workflow, detailed in the diagram below, outlines the progression from simulation to in-vivo validation, as demonstrated in recent studies [16].
Protocol 1: In-silico Evaluation Using the UVA/Padova T1D Simulator
Objective: To initially validate the safety and efficacy of the MPC algorithm in a simulated population under controlled challenges.
Materials:
- Simulation Environment: FDA-accepted UVA/Padova T1D Metabolic Simulator (100-adult cohort) [87] [86].
- Controller Platform: Hardware-in-the-loop embedded system or computational software (e.g., MATLAB/Simulink) [88].
- Challenge Scenarios: Meal library (varying carbohydrate content, timing), unannounced meals, and simulated exercise sessions [86].
Methodology:
- Baseline Run: Simulate the virtual cohort over 24-72 hours with standard meal challenges and the MPC algorithm active. Record all CGM traces and insulin delivery profiles.
- Robustness Testing: Introduce plant-model mismatch by modifying simulator parameters (e.g., insulin sensitivity scaling factor α ∈ [0.3, 2.5]) without informing the controller [87].
- Meal Challenge: Test with large, unannounced meals (e.g., 80g carbohydrates) to evaluate the postprandial glucose excursion and the controller's ability to mitigate hyperglycemia without causing late-onset hypoglycemia [87] [86].
- Data Analysis: Calculate all metrics from Table 1 and Table 2. The primary outcome is often TIR, with key safety outcomes being time in hypoglycemia and ATE [13].
Protocol 2: In-vivo Validation in a Diabetic Rat Model
Objective: To assess the performance of the MPC algorithm in a living organism with full physiological complexity and unmodeled disturbances [16].
Materials:
- Animal Model: Diabetic rats (e.g., male Wistar rats induced with streptozotocin) [16].
- Devices: Implantable CGM sensor and a customized, low-cost insulin infusion pump [16].
- Data Acquisition System: Interface for recording CGM data and controlling the pump.
Methodology:
- Post-Induction:
- Render rats diabetic.
- On Day 1, administer a manual insulin bolus via the pump and record the glucose response.
- Perform off-line parametric estimation from this data to personalize the model for the MPC [16].
- Controller Tuning (Day 2):
- Implement the initial MPC parameters based on the estimated model.
- Conduct a short test run and adjust controller parameters as necessary [16].
- Closed-Loop Trial (Day 3):
- Initiate a prolonged (e.g., 72-hour) fully autonomous closed-loop experiment.
- Provide food ad libitum without meal announcements to the controller.
- Continuously monitor animal health and weight [16].
- Data Analysis:
- Calculate TIR, hyperglycemia, and hypoglycemia metrics.
- Report the number of hypoglycemic events per subject.
- Calculate the Median Absolute Relative Difference (MARD) between model predictions and actual sensor data to quantify plant-model mismatch [16].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Tools for AID Research
| Item | Function in Research |
|---|---|
| UVA/Padova T1D Simulator | The FDA-accepted platform for in-silico testing of AID algorithms, providing a virtual cohort of adults, adolescents, and children with T1D for pre-clinical validation [87] [86]. |
| Sorensen Model | A comprehensive 19-state physiological model of glucose-insulin-glucagon dynamics; used for high-fidelity simulations and controller design [13]. |
| Continuous Glucose Monitor (CGM) | Provides real-time, interstitial glucose measurements; the primary input for the control algorithm. Performance (e.g., MARD) can vary between brands and affect outcomes [85] [16]. |
| Subcutaneous Insulin Pump | Deloys micro-boluses of insulin as determined by the MPC algorithm. Research often uses customized or commercial pumps capable of receiving external commands [16]. |
| Insulin Sensitivity (SI) Estimator | An algorithm (e.g., based on a mixed meal tolerance test) to estimate the subject's current SI. Informing the MPC with accurate SI estimates can improve glycemic outcomes and provide protection against hyper- and hypoglycemia [87]. |
| Offset-Free Disturbance Model | An augmented model within the MPC that estimates and compensates for unmeasured disturbances and plant-model mismatch, crucial for handling real-world variability [16]. |
| Event-Triggered MPC Framework | A control scheme that reduces computational load by invoking the MPC algorithm only when specific events occur (e.g., glucose deviating from a zone), thereby saving energy in embedded systems [88]. |
The management of blood glucose levels in individuals with diabetes, particularly type 1 diabetes (T1D), represents a complex physiological control challenge. The artificial pancreas (AP), or closed-loop control system, has emerged as a transformative technology for automating insulin delivery. While numerous control algorithms have been developed, Model Predictive Control (MPC) has demonstrated particular promise for long-term glycemic management. This application note synthesizes current evidence on the sustained efficacy of MPC-based systems, providing structured data and experimental protocols to support research and development activities.
MPC's superiority stems from its proactive control mechanism; unlike reactive algorithms such as Proportional-Integral-Derivative (PID), MPC utilizes a physiological model to predict future glucose levels and adjust insulin delivery preemptively [73]. This capability is critical for managing slow-acting insulin dynamics and anticipating disturbances such as meals. Clinical evidence confirms that this predictive capability enables MPC to maintain glucose levels within the target range for a significantly higher percentage of time compared to both conventional therapy and alternative control algorithms during extended use [79] [73].
Quantitative Evidence of Long-Term Efficacy
Clinical Outcomes: MPC vs. Conventional Therapy
A comprehensive meta-analysis of 41 randomized controlled trials provides robust evidence for the sustained effectiveness of MPC-based systems in outpatient settings. The table below summarizes key glycemic outcomes, demonstrating significant improvements over conventional insulin therapy.
Table 1: Glycemic Outcomes of MPC-Based Artificial Pancreas vs. Conventional Therapy
| Outcome Measure | Intervention Scenario | Result (Mean Difference, 95% CI) | P-value |
|---|---|---|---|
| Time in Target Range (3.9-10 mmol/L) | Overnight Use | +10.03% (7.50, 12.56) | < 0.00001 [79] |
| Time in Hypoglycemia (<3.9 mmol/L) | Overnight Use with >1 month follow-up | -1.34% (-1.87, -0.81) | < 0.00001 [79] |
Head-to-Headed Head Algorithm Comparison
The first randomized, crossover clinical trial directly comparing MPC and PID under identical conditions clearly established MPC's superiority. The study involved 30 adults with T1D and introduced challenges such as unannounced meals to simulate real-world conditions [73].
Table 2: MPC vs. PID Controller Performance in a Crossover Study
| Performance Metric | MPC Algorithm | PID Algorithm |
|---|---|---|
| Time in Safe Glucose Range | 74% | 64% (with unannounced meal) [73] |
| Mean Glucose Values | Statistically significantly lower | Higher [73] |
| Key Differentiator | Proactive prediction of highs/lows | Reactive to glucose deviations |
Experimental Protocols for Long-Term Validation
Protocol: Outpatient Evaluation of MPC Efficacy
This protocol is designed for long-term, real-world assessment of an MPC-based AP system.
1. Objective: To evaluate the long-term effectiveness and safety of an MPC-based artificial pancreas in maintaining glycemic control in outpatient adults with T1D, compared to sensor-augmented pump (SAP) therapy.
2. Study Design:
- Design: Randomized, controlled, crossover trial.
- Participants: Adults with T1D.
- Intervention: MPC-based closed-loop system.
- Comparator: Conventional insulin therapy (e.g., SAP or insulin pump).
- Duration: Each intervention arm should be a minimum of 4 weeks, with a washout period between arms to mitigate carryover effects [79].
3. Primary Endpoint:
- Percentage of time spent in the target glucose range (3.9–10.0 mmol/L or 70–180 mg/dL) over the study period [79].
4. Secondary Endpoints:
- Percentage of time in hypoglycemia (<3.9 mmol/L or <70 mg/dL).
- Percentage of time in hyperglycemia (>10.0 mmol/L or >180 mg/dL).
- Glucose variability (Standard Deviation).
- Total daily insulin dose.
- Safety endpoints (e.g., severe hypoglycemia events).
5. Data Collection:
- Continuous glucose monitoring (CGM) data collected throughout the study.
- Insulin delivery logs.
- Patient-reported events (meals, exercise, symptoms).
Protocol: Preclinical Validation of an MPC System
This protocol outlines the in vivo validation of a novel MPC algorithm in an animal model, a critical step before human trials.
1. Objective: To validate the efficacy and safety of a fully automated insulin delivery system using an impulsive offset-free MPC strategy in a diabetic rat model.
2. Animal Model:
- Subjects: Male Wistar rats (e.g., n=14) with diabetes induced by streptozotocin [56].
- Devices: Customized low-cost insulin pump and continuous glucose monitor.
3. Experimental Timeline:
- Day 1: Model Identification. Manual insulin injections are administered via the pump, and the glucose response is recorded. An offline parametric estimation is performed to create a patient-specific model for the MPC [56].
- Day 2: Controller Tuning. The estimated model parameters are used in simulations for the initial tuning of the MPC controller. The parameters are then tested and adjusted in the live animal model [56].
- Day 3-5: Autonomous Operation. A 72-hour test of the impulsive automated insulin delivery system (i-AiDS) is conducted in full autonomous mode, managing unannounced carbohydrate intake and other disturbances [56].
4. Outcome Measures:
- Primary: Percentage of time in target range (80-180 mg/dL).
- Safety: Number of hypoglycemic events (<70 mg/dL) and severe hyperglycemic events.
- Controller Performance: Median Absolute Relative Difference (MARD) between model predictions and actual sensor data.
Research Workflow and Logical Framework
The following diagram illustrates the structured workflow from preclinical development to the clinical validation of an MPC-based artificial pancreas system, integrating the protocols described above.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for MPC Algorithm Research
| Item | Function/Application | Example/Note |
|---|---|---|
| FDA-approved Metabolic Simulator | In-silico testing and initial algorithm validation in a virtual population. | UVA/Padova T1D Simulator [90]. |
| Continuous Glucose Monitor (CGM) | Provides real-time, interstitial glucose measurements for feedback control. | A primary component of the closed-loop system [79]. |
| Insulin Pump | Subcutaneous delivery device actuated by control algorithm commands. | A primary component of the closed-loop system [79]. |
| MPC Control Algorithm | The core software that predicts future glucose and computes optimal insulin doses. | Can be based on the Bergman Minimal Model or other physiological models [6]. |
| Streptozotocin (STZ) | Chemical for inducing insulin-deficient diabetes in preclinical animal models. | Used in diabetic rat models for in vivo validation [56]. |
| Federated Learning Framework | Enables privacy-preserving, collaborative model training across decentralized data sources. | Key for developing personalized models without centralizing sensitive data (e.g., PRIMO-FRL) [90]. |
Future Directions: Next-Generation Intelligent Control
While traditional MPC has proven effective, research is advancing towards more adaptive and personalized systems. Federated Reinforcement Learning (FRL) represents a cutting-edge frontier. The PRIMO-FRL framework, for instance, integrates multi-objective reward shaping to balance time-in-range, insulin efficiency, and hypoglycemia prevention [90]. By leveraging decentralized learning, it enhances personalization and scalability while preserving patient data privacy—a significant limitation of traditional centralized AI models [90].
Furthermore, Distributional Reinforcement Learning models like GLUCOSE have demonstrated superior performance in complex clinical settings, such as postoperative glucose management, by characterizing the full distribution of potential outcomes rather than just the expected reward, leading to safer and more nuanced decision-making [27].
These intelligent systems represent the natural evolution of MPC, building upon its predictive foundation to create fully adaptive, personalized, and secure solutions for long-term glycemic management.
Conclusion
Model Predictive Control represents a sophisticated and clinically validated approach for automated blood glucose regulation, demonstrating significant advantages over conventional insulin therapy and alternative control strategies like PID. Key takeaways include MPC's proven ability to increase time-in-range while reducing hypoglycemia risk, particularly through adaptive tuning and zone-based formulations that proactively manage glycemic excursions. The integration of data-driven predictors, such as LSTM networks, addresses fundamental limitations in linear prediction models, enabling more accurate long-horizon forecasting. Future directions should focus on developing fully adaptive personalized algorithms that automatically adjust to long-term physiological changes, incorporating multi-hormonal control systems, advancing robustness to extreme conditions and inter-patient variability, and conducting large-scale long-term outpatient studies to establish real-world efficacy and cost-effectiveness. These advances will accelerate the development of more intelligent, autonomous artificial pancreas systems that minimize patient burden while optimizing glycemic outcomes.
References
- 1. Artificial Pancreas: The First 20 Years [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213539/]
- 2. Automated Insulin Delivery Systems and Insulin Pumps [https://www.breakthrought1d.org/daily-management/t1d-technology/aid-insulin-pumps/]
- 3. Model Predictive Control of Type 1 Diabetes: An in Silico Trial [https://pmc.ncbi.nlm.nih.gov/articles/PMC2769684/]
- 4. Effectiveness and safety of a model predictive control (MPC ... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-022-00962-2]
- 5. Challenges and Recent Progress in the Development of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3501007/]
- 6. Control of blood glucose induced by meals for type-1 ... [https://www.nature.com/articles/s41598-022-16535-2]
- 7. Edward Damiano's Bold Bet on a Bionic Cure [https://www.scientificamerican.com/article/why-building-an-artificial-pancreas-for-people-with-diabetes-is-so-hard-and/]
- 8. An efficient nonlinear explicit model predictive control to ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809421007631]
- 9. Model Predictive Control (MPC) of an artificial pancreas ... [https://www.sciencedirect.com/science/article/pii/S0967066123003799?via=ihub]
- 10. Introduction to Model Predictive Control [https://imperix.com/doc/implementation/model-predictive-control]
- 11. Basics of model predictive control [https://www.do-mpc.com/en/latest/theory_mpc.html]
- 12. CHoKI-based MPC for blood in Artificial Pancreas glucose regulation [https://arxiv.org/html/2401.17157v1]
- 13. and control of insulin and glucagon infusion... Blood glucose regulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC8687336/]
- 14. Model predictive control [https://en.wikipedia.org/wiki/Model_predictive_control]
- 15. Efficient AiDS Through Real-Time Insulin Sensitivity ... [https://link.springer.com/article/10.1007/s42979-025-03846-0]
- 16. Validation in diabetic rats of a fully automated insulin delivery ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0330121]
- 17. Privacy-Preserving Glycemic Management in Type 1 Diabetes [https://diabetes.jmir.org/2025/1/e72874]
- 18. A Closed-Loop Artificial Pancreas Using Model Predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2769914/]
- 19. Neural Networks for on-chip Model Predictive Control [https://arxiv.org/html/2504.11355v1]
- 20. The effects of meal glycemic load on blood glucose levels ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5240084/]
- 21. How timing of dinner and genetics affect blood sugar level ... [https://saxena.mgh.harvard.edu/news/how-timing-of-dinner-and-genetics-affect-blood-sugar-level-control/]
- 22. Understanding Blood Glucose and Exercise | ADA [https://diabetes.org/health-wellness/fitness/blood-glucose-and-exercise]
- 23. The impact of brief high-intensity exercise on blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3587394/]
- 24. Diabetes and exercise: When to monitor your blood sugar [https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetes-and-exercise/art-20045697]
- 25. Stress-Induced Hyperglycemia: Consequences and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9360912/]
- 26. Stress-Induced Diabetes: A Review - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9561544/]
- 27. A distributional reinforcement learning model for optimal ... [https://www.nature.com/articles/s41746-025-01709-9]
- 28. Global burden of diabetes, 1995-2025: prevalence, ... [https://pubmed.ncbi.nlm.nih.gov/9727886/]
- 29. Diabetes Facts and Figures [https://idf.org/about-diabetes/diabetes-facts-figures/]
- 30. Global type 1 diabetes prevalence, incidence, and mortality ... [https://www.sciencedirect.com/science/article/pii/S0168822725002918]
- 31. Urgent action needed as global diabetes cases increase ... [https://www.who.int/news/item/13-11-2024-urgent-action-needed-as-global-diabetes-cases-increase-four-fold-over-past-decades]
- 32. Perceptions of Suboptimal Insulin Dosing from People with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317930/]
- 33. Global research trends in AI-assisted blood glucose ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1579640/full]
- 34. Prescribed finite-time backstepping control for blood ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482525010881]
- 35. Periodic zone-MPC with asymmetric costs for outpatient-ready safety of an artificial pancreas to treat type 1 diabetes* - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5040369/]
- 36. Periodic zone-MPC with asymmetric costs for outpatient-ready safety of an artificial pancreas to treat type 1 diabetes - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0005109816301388]
- 37. An Enhanced Model Predictive Control for the Artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5505428/]
- 38. Adaptive Zone Model Predictive Control of Artificial Pancreas Based on Glucose- and Velocity-Dependent Control Penalties - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6760658/]
- 39. Metabolic Models, in Silico Trials, and Algorithms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213549/]
- 40. Zone-MPC Automated Insulin Delivery Algorithm Tuned for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8982146/]
- 41. Adaptive Control of an Artificial Pancreas Using Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6835177/]
- 42. Data-Efficiency with Comparable Accuracy [https://www.mdpi.com/2673-4540/6/10/115]
- 43. Optimization of blood glucose prediction with LSTM ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809425003258]
- 44. Data-driven blood glucose level prediction in type 1 diabetes [https://www.nature.com/articles/s41598-024-70277-x]
- 45. Machine Learning Models for Blood Glucose Level ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10696506/]
- 46. A data-driven personalized approach to predict blood ... [https://pubmed.ncbi.nlm.nih.gov/40164029/]
- 47. Comparing individualization strategies of Model Predictive ... [https://www.sciencedirect.com/science/article/pii/S2405896325003118]
- 48. Adaptive Personalized Prior-Knowledge-Informed Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9730892/]
- 49. Prediction of Individual Basal Rate Profiles From Patient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8655298/]
- 50. Modeling Pharmacokinetic Profiles of Insulin Regimens to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5573917/]
- 51. Blood glucose control by a model predictive ... [https://pubmed.ncbi.nlm.nih.gov/17550955/]
- 52. Pharmacokinetic/Pharmacodynamic Modeling of Glucose ... [https://www.sciencedirect.com/science/article/pii/S1347436715300525]
- 53. MiniMed 780G™ advanced hybrid - closed performance... loop system [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-023-01184-w]
- 54. Simplified Meal Management in Adults Using an Advanced Hybrid ... [https://pubmed.ncbi.nlm.nih.gov/39115922/]
- 55. Multicentric, randomized, controlled trial to evaluate blood ... [https://pubmed.ncbi.nlm.nih.gov/16443872/]
- 56. Validation in diabetic rats of a fully automated insulin ... [https://pubmed.ncbi.nlm.nih.gov/40906706/]
- 57. Blood sugar response to various carbohydrates can point to ... [https://med.stanford.edu/news/all-news/2025/06/carb-sugar-spikes.html]
- 58. Deep learning approach to parameter optimization for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553359/]
- 59. A 1-Dimensional Physiological Signal Prediction Method ... [https://www.mdpi.com/1424-8220/25/21/6726]
- 60. Hypoglycemia Prevention in Hospital Patients: A Quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5070586/]
- 61. Analysis of Glucose Responses to Automated Insulin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3379608/]
- 62. Insulin- Pharmacology, Therapeutic Regimens and Principles ... [https://www.ncbi.nlm.nih.gov/books/NBK278938/]
- 63. Choose Sample Time and Horizons - MATLAB & Simulink [https://www.mathworks.com/help/mpc/ug/choosing-sample-time-and-horizons.html]
- 64. What is the Prediction Horizon in Model Predictive Control? [https://picontrolsolutions.wixsite.com/picontrol-solutions/post/what-is-the-prediction-horizon-in-model-predictive-control]
- 65. Multi-step ahead predictive model for blood glucose ... [https://www.nature.com/articles/s41598-021-03341-5]
- 66. Unannounced Meals in the Artificial Pancreas: Detection ... [https://www.mdpi.com/1424-8220/18/3/884]
- 67. Enabling fully automated insulin delivery through meal ... [https://www.nature.com/articles/s41746-023-00783-1]
- 68. Automatic Detection and Estimation of Unannounced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5867514/]
- 69. Model Predictive Control — Dynamic Optimization [https://apmonitor.com/do/index.php/Main/ControlTypes]
- 70. Event-triggered smart dual hormone artificial pancreas for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12402495/]
- 71. Optimal Weighting Factors Design for Model Predictive ... [https://www.mdpi.com/2076-3417/15/11/5874]
- 72. Ensemble-based model predictive control using data ... - NPG [https://npg.copernicus.org/articles/32/293/2025/]
- 73. In the fight to control glucose levels, this control algorithm ... [https://seas.harvard.edu/news/2016/06/fight-control-glucose-levels-control-algorithm-comes-out-top]
- 74. Randomized Crossover Comparison of Personalized MPC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4915560/]
- 75. Randomized Crossover Comparison of Personalized MPC ... [https://pubmed.ncbi.nlm.nih.gov/27289127/]
- 76. MPC Versus PID for Closed Loop Insulin Delivery | MedPath [https://trial.medpath.com/clinical-trial/d2bb686e53ffe3b3/nct02438670-pid-vs-mpc-controller-insulin-delivery]
- 77. Comparison of the night-time effectiveness in achieving ... [https://link.springer.com/article/10.1007/s00592-024-02397-9]
- 78. A habituating blood glucose control strategy for the ... [https://www.sciencedirect.com/science/article/abs/pii/S0959152412001825]
- 79. Effectiveness and safety of a model predictive control (MPC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9733359/]
- 80. IDeglira vs insulin degludec for type 2 diabetes [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1643386/full]
- 81. Efficacy and Safety of Once-Weekly IcoSema in Adults With ... [https://www.sciencedirect.com/science/article/pii/S3050915725000700]
- 82. Comparison of Insulin Titration Strategies for Glycemic ... [https://pubmed.ncbi.nlm.nih.gov/40273351/]
- 83. Explainable Machine Learning for Real-Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10899844/]
- 84. Explainable hypoglycemia prediction models through ... [https://www.nature.com/articles/s41598-024-63187-5]
- 85. How to compare algorithms for automated insulin delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11965003/]
- 86. Prior-knowledge-embedded model predictive control for blood glucose regulation: Towards efficient and safe artificial pancreas - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1746809422010059]
- 87. Performance Effect of Adjusting Insulin Sensitivity for Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10658700/]
- 88. Event-Triggered Model Predictive Control For Embedded Artificial Pancreas Systems - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5839516/]
- 89. An AI-enabled dual-hormone model predictive control ... [https://www.sciencedirect.com/science/article/pii/S2405896325003155]
- 90. Privacy-Preserving Glycemic Management in Type 1 Diabetes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12248133/]