Mastering the Caco-2/TC7 Glucose Uptake Assay: A Comprehensive Guide from Foundations to Advanced Applications
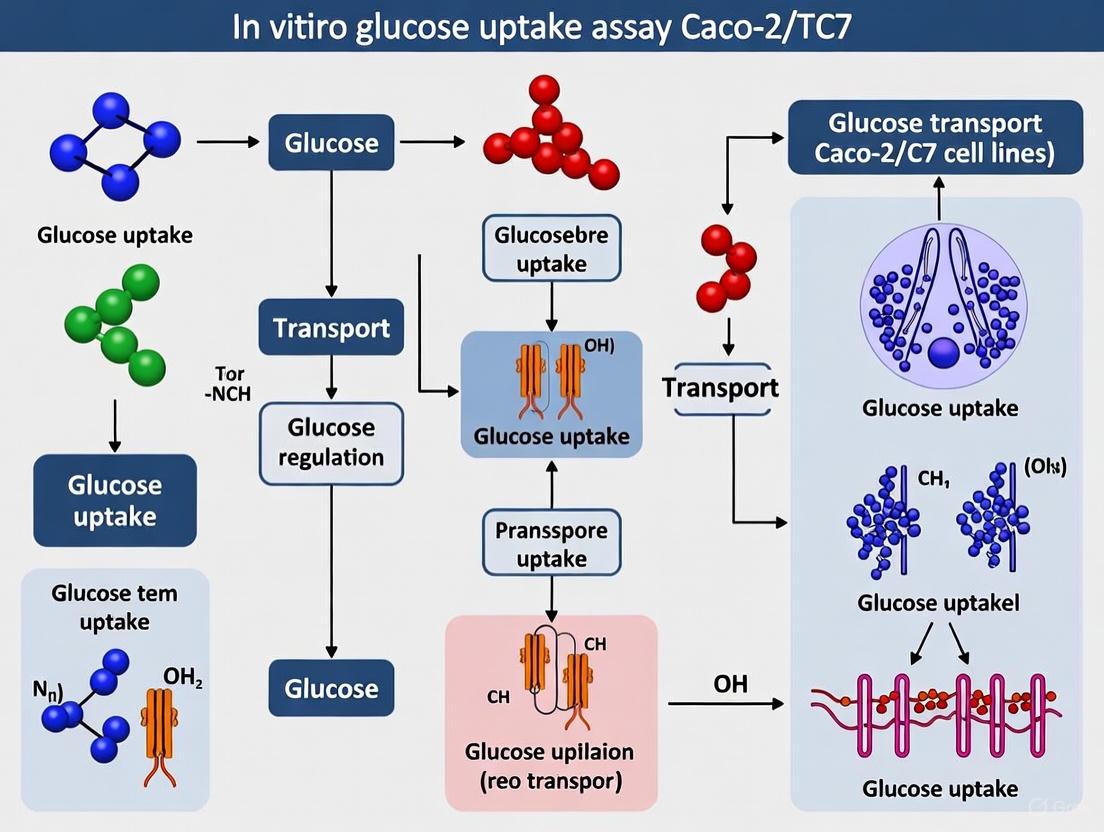
This article provides a definitive guide to conducting in vitro glucose uptake assays using the human intestinal Caco-2/TC7 cell model.
Mastering the Caco-2/TC7 Glucose Uptake Assay: A Comprehensive Guide from Foundations to Advanced Applications
Abstract
This article provides a definitive guide to conducting in vitro glucose uptake assays using the human intestinal Caco-2/TC7 cell model. Tailored for researchers and drug development professionals, it covers the foundational biology of intestinal glucose transporters, established and emerging methodological protocols, critical troubleshooting strategies, and advanced validation techniques. By synthesizing current research, this resource aims to equip scientists with the knowledge to reliably employ this model for investigating nutrient absorption, screening therapeutic compounds for metabolic diseases, and studying gut barrier function, thereby enhancing the translational value of their preclinical research.
Understanding Intestinal Glucose Transport: The Biological Basis of the Caco-2/TC7 Model
The absorption of dietary monosaccharides in the small intestine is a critical process for systemic energy homeostasis, primarily mediated by three key transporter proteins: SGLT1, GLUT2, and GLUT5. In vitro research utilizing the human-derived Caco-2/TC7 cell line, which undergoes enterocyte-like differentiation upon confluence, provides a robust model for investigating the function and regulation of these transporters [1] [2]. Understanding their distinct roles, kinetics, and regulatory mechanisms is fundamental to research in nutrient absorption, metabolic diseases, and drug development. This document outlines the core principles and detailed protocols for studying these transporters within the context of Caco-2/TC7 cell assays.
Transporter Characteristics and Functional Roles
Glucose absorption is a two-step process where monosaccharides are taken up across the apical membrane into the enterocyte and subsequently exported across the basolateral membrane into the circulation. The transporters involved have distinct functions, substrate specificities, and kinetic properties, summarized in the table below.
Table 1: Functional Properties of Key Intestinal Glucose Transporters
| Transporter | Gene | Transport Mechanism & Stoichiometry | Primary Substrates | Apparent Km (mM) | Cellular Localization | Inhibitors |
|---|---|---|---|---|---|---|
| SGLT1 | SLC5A1 | Sodium-gradient secondary active (2 Na⁺:1 Glucose) [3] [4] | D-Glucose, D-Galactose [3] | D-Glucose: ~0.5 mM [3] | Apical Membrane (BBM) [3] | Phlorizin [3] |
| GLUT2 | SLC2A2 | Facilitated diffusion [3] | D-Glucose, D-Galactose, D-Fructose [3] | D-Glucose: ~17 mM [3] | Basolateral Membrane (BLM); Apical under high glucose [3] [5] | Phloretin [3] |
| GLUT5 | SLC2A5 | Facilitated diffusion [3] | D-Fructose [3] | D-Fructose: ~6 mM [3] | Apical Membrane (BBM) [3] | Not specified in search results |
The collaborative work of these transporters ensures efficient sugar assimilation. At low luminal glucose concentrations (< 30 mM), absorption is dominated by high-affinity SGLT1 on the apical membrane, with GLUT2 facilitating exit across the basolateral membrane [5]. However, at high luminal concentrations, GLUT2 is rapidly recruited to the apical membrane, providing a high-capacity absorption pathway [3] [1]. GLUT5 is specialized for fructose uptake across the apical membrane, and this fructose may subsequently exit the cell via the broad-specificity GLUT2 transporter on the basolateral side [3].
Diagram 1: Collaborative glucose transport in enterocytes. SGLT1 and GLUT5 are constitutive apical transporters. GLUT2 is constitutively basolateral but is recruited to the apical membrane under high glucose conditions [3] [5]. The Na⁺/K⁺ ATPase maintains the sodium gradient that drives SGLT1 activity.
Research Reagent Solutions
The following table lists key reagents essential for conducting in vitro assays to investigate the function and inhibition of intestinal glucose transporters.
Table 2: Essential Research Reagents for Glucose Transport Studies
| Reagent / Tool | Function / Target | Key Characteristics & Experimental Use |
|---|---|---|
| Phlorizin | SGLT1 Inhibitor [3] | Competitive inhibitor of SGLT1. Used to isolate the SGLT1-mediated component of glucose uptake in uptake assays [4]. |
| Phloretin | GLUT2 Inhibitor [3] | Inhibits facilitative glucose transporters, including GLUT2. Used to distinguish GLUT-mediated from SGLT-mediated uptake [1]. |
| Radio-labelled Sugars (e.g., [³H]-D-Glucose, [¹⁴C]-D-Glucose) | Transporter Substrates | Enable quantitative measurement of sugar uptake. Used in tracer concentrations in uptake buffer to assay transport activity [1] [2]. |
| Sodium-free Buffer | Experimental Control | Replaces NaCl with equimolar Choline-Cl or NMDG. Eliminates the Na⁺ gradient, thereby abolishing SGLT1 activity and allowing measurement of the facilitative (GLUT-mediated) uptake component [1]. |
| Berry Extract (Polyphenol-rich) | Transporter Modulator | Shown to acutely inhibit glucose uptake and chronically downregulate SGLT1 and GLUT2 mRNA expression in Caco-2 cells [1]. A tool for studying dietary modulation. |
| Artificial Sweeteners (e.g., Lactisole) | Sweet Taste Receptor (T1R2/3) Antagonists | Used to investigate the role of sweet taste sensing pathways in the acute regulation of intestinal glucose transporter activity [2]. |
Detailed Experimental Protocols
Protocol: Acute Glucose Uptake Assay in Caco-2/TC7 Cells
This protocol measures the real-time transport activity of SGLT1 and GLUT2 in differentiated Caco-2/TC7 cell monolayers, adapted from published methodologies [1] [2].
Workflow Overview:
Diagram 2: Workflow for acute glucose uptake assay in Caco-2/TC7 cells.
Materials:
- Differentiated Caco-2/TC7 cell monolayers (19-21 days post-confluence)
- Uptake Buffer: Kreb's Bicarbonate Buffer or Kreb's Buffered Saline (KBS), pH 7.4 [2]
- Uptake Buffer, Sodium-free: NaCl replaced isotonically with Choline-Cl or N-Methyl-D-Glucamine (NMDG-Cl) [1]
- Radiolabelled Substrate: e.g., [³H]-D-Glucose or [¹⁴C]-D-Glucose
- Inhibitors/Compounds: e.g., Phlorizin (0.5-1.0 mM), Phloretin (0.5 mM), berry extract, artificial sweeteners
- Lysis Buffer: 0.2% (w/v) SDS
- Equipment: Scintillation counter, cell culture multi-well plates
Procedure:
- Cell Preparation: Culture Caco-2/TC7 cells in 24-well plates at a density of 10,000 cells/cm² and maintain for at least 19 days post-confluence to ensure full differentiation and transporter expression [2]. Change the medium every other day.
- Pre-incubation: On the day of the experiment, wash cell monolayers once with pre-warmed KBS (pH 7.4). Pre-incubate for 15 minutes at 37°C in KBS containing the desired test compounds (e.g., inhibitors, polyphenols, artificial sweeteners) or vehicle control [1] [2].
- Uptake Initiation: Remove the pre-incubation buffer and immediately add the uptake buffer (with or without sodium) containing the radiolabelled D-Glucose tracer (e.g., 0.1 μCi/mL). A non-transportable radiolabelled sugar like L-Glucose should be used in parallel to correct for simple diffusion and non-specific binding [2].
- Uptake Termination: After a short incubation (typically 2-5 minutes), rapidly terminate uptake by removing the radioactive buffer and immediately washing the monolayers three times with ice-cold PBS.
- Cell Lysis and Analysis: Lyse the cells with 0.2% SDS for 60 minutes at 37°C. Transfer the lysate to scintillation vials, add scintillation fluid, and measure radioactivity. Determine the protein content of the lysate using a standard assay (e.g., BCA) to normalize uptake values (nmol/mg protein/time) [1].
Data Interpretation:
- Total Glucose Uptake: Measured in sodium-containing buffer.
- Facilitated Uptake (GLUT-mediated): Measured in sodium-free buffer.
- SGLT1-mediated Uptake: Calculated as the difference between Total and Facilitated uptake.
Protocol: Investigating Chronic Regulation of Transporter Expression
This protocol assesses long-term changes in transporter mRNA and protein expression in response to dietary components or other stimuli.
Materials:
- Differentiated Caco-2/TC7 cells
- Treatment medium (e.g., serum-free medium containing test compounds like berry extract [0.125% w/v]) [1]
- TRIzol reagent for RNA isolation
- DNase I (RNase-free)
- cDNA synthesis kit
- Real-time PCR system and reagents (e.g., Power SYBR Green)
- Specific primers for SGLT1 (SLC5A1), GLUT2 (SLC2A2), GLUT5 (SLC2A5), and a housekeeping gene (e.g., GAPDH)
- RIPA buffer for protein extraction
- SDS-PAGE and Western Blotting equipment
- Primary antibodies against SGLT1, GLUT2, and a loading control (e.g., Actin)
Procedure:
- Cell Treatment: Expose differentiated Caco-2/TC7 cell monolayers to the treatment medium for a defined period (e.g., 16 hours) [1].
- RNA Extraction and qPCR:
- Isolate total RNA using TRIzol according to the manufacturer's instructions.
- Treat RNA with DNase I to remove genomic DNA contamination.
- Synthesize cDNA using a reverse transcription kit.
- Perform quantitative PCR (qPCR) using gene-specific primers. Calculate relative gene expression using the 2^(-ΔΔCt) method, normalizing to the housekeeping gene [1].
- Protein Extraction and Western Blotting:
- Lyse cells in RIPA buffer to extract total protein.
- Separate proteins (e.g., 40 μg per lane) by SDS-PAGE and transfer to a nitrocellulose membrane.
- Probe the membrane with specific primary antibodies against SGLT1, GLUT2, and Actin, followed by appropriate HRP-conjugated secondary antibodies.
- Detect immunoreactive bands using chemiluminescence and perform semi-quantitative analysis via densitometry, normalizing to Actin [1].
Application in Research: Inhibitory Studies
The Caco-2/TC7 model is widely used to screen for natural compounds and drugs that modulate glucose absorption. For instance, polyphenol-rich berry extracts and specific mulberry leaf phenolics like chlorogenic acid and rutin have been shown to acutely inhibit glucose uptake and chronically downregulate SGLT1 and GLUT2 mRNA expression [1] [6]. These findings highlight the potential of dietary compounds in managing postprandial glycemia. When conducting such inhibitory studies, it is critical to include both acute uptake assays and chronic expression analyses to fully characterize the mechanism of action, and to use specific pharmacological inhibitors (e.g., phlorizin for SGLT1) as experimental controls to validate the findings.
Why Caco-2/TC7 Cells? Mimicking Human Enterocyte Physiology and Differentiation
Within the field of intestinal physiology and drug discovery, the Caco-2/TC7 cell line has emerged as a premier in vitro tool for investigating human enterocyte function, particularly for glucose uptake and transport studies. As a subclone of the parental Caco-2 line, itself derived from human colorectal adenocarcinoma, the TC7 variant was isolated to provide a more homogeneous cell population that consistently exhibits characteristic functions of small intestinal enterocytes [7] [8]. When cultured under specific conditions, these cells undergo spontaneous differentiation and polarization, developing a phenotype that closely resembles the enterocytes lining the small intestine [7]. This transformation includes the formation of functional tight junctions, a well-defined brush border with microvilli, and the expression of key intestinal enzymes and transporters, making them an indispensable model for studying intestinal glucose absorption mechanisms within broader thesis research on metabolic diseases and drug development [7] [9].
Table 1: Key Advantages of Caco-2/TC7 Cells for Glucose Uptake Research
| Feature | Physiological Relevance | Application in Glucose Research |
|---|---|---|
| Enterocyte-like Differentiation [7] [8] | Develops polarized monolayer with apical brush border and microvilli | Provides authentic cellular context for studying apical glucose transporters |
| Expression of Key Transporters [10] [11] | Endogenously expresses SGLT1 and GLUT2 glucose transporters | Enables functional investigation of sodium-dependent and facilitative glucose transport |
| Well-developed Tight Junctions [9] | Forms physiologically relevant barrier with regulated paracellular transport | Allows measurement of transepithelial glucose flux and barrier integrity |
| High Degree of Homogeneity [8] | More uniform population compared to parental Caco-2 line | Improves experimental reproducibility for high-quality, quantifiable data |
Characterizing the Caco-2/TC7 Model for Glucose Transport Studies
Quantitative Expression of Glucose Transport Systems
The Caco-2/TC7 model is particularly valuable for glucose transport studies due to its robust expression of the primary intestinal glucose transporters. Research has demonstrated that these cells functionally express sodium-dependent glucose cotransporter 1 (SGLT1) and glucose transporter 2 (GLUT2) [10] [11]. The expression levels of these transporters are modifiable by various stimuli, making the model ideal for mechanistic studies. For instance, dexamethasone treatment dose-dependently increases glucose transport capacity by upregulating SGLT1 mRNA expression [10]. Similarly, pro-inflammatory cytokines (IL-1β and TNF-α) significantly upregulate SGLT1 gene expression, while the phytochemical genistein can normalize these inflammation-induced increases [11].
Experimental Validation of Model Integrity
The utility of any in vitro model depends on rigorous validation of its differentiation status and barrier function. For Caco-2/TC7 monolayers, two principal methods are employed to confirm model integrity:
- Transepithelial Electrical Resistance (TEER): This non-invasive measurement quantifies the integrity of tight junctions within the cell monolayer. Fully differentiated Caco-2/TC7 monolayers typically achieve TEER values exceeding 250 Ω·cm² (for 24-well plates), indicating the formation of competent intercellular junctions [9] [12].
- Paracellular Marker Flux: The apparent permeability (Papp) of low-permeability markers like mannitol or lucifer yellow is measured. Differentiated monolayers should exhibit mannitol Papp values lower than 0.5 × 10⁻⁶ cm/s, confirming restricted paracellular diffusion [9] [12].
Table 2: Experimentally Measured Parameters in Differentiated Caco-2/TC7 Monolayers
| Parameter | Measured Value | Experimental Context | Citation |
|---|---|---|---|
| Dexamethasone Effect on SGLT1 | Dose-dependent increase | Differentiated human Caco-2/TC7 intestinal cell monolayers | [10] |
| TEER Value (Minimum) | >250 Ω·cm² | Integrity check for Caco-2 monolayers in 24-well format | [9] |
| Mannitol Permeability (Papp) | <0.5 × 10⁻⁶ cm/s | Integrity check for validated Caco-2 monolayers | [9] |
| Cell Seeding Density | 0.1 × 10⁵ cells/cm² | Standard protocol for differentiation on Transwell filters | [10] [11] |
| Differentiation Time | 14-21 days | Time required to form fully differentiated monolayer | [10] [9] [11] |
Detailed Protocol: Establishing Differentiated Caco-2/TC7 Monolayers for Glucose Uptake
Materials and Reagent Solutions
Table 3: Essential Research Reagents for Caco-2/TC7 Culture and Differentiation
| Reagent / Kit | Function / Application | Example Specification |
|---|---|---|
| Dulbecco's Modified Eagle Medium (DMEM) | Standard culture medium for cell growth and maintenance | High glucose (4.5 g/L or 25 mM) [10] [11] |
| Fetal Bovine Serum (FBS) | Essential source of growth factors and hormones | 10-20% (v/v) heat-inactivated [10] [11] |
| Non-Essential Amino Acids (NEAA) | Supports cellular growth and protein synthesis | 1-2% (v/v) [10] [11] |
| Transwell Plates | Provide permeable support for polarization and differentiation | Polyester filters, 0.4 µm pore size [10] [11] |
| Trypsin-EDTA Solution | Enzymatic detachment of cells for subculturing and seeding | 0.25% (v/v) [10] [11] |
| Transepithelial Electrical Resistance (TEER) Meter | Measures monolayer integrity and tight junction formation | Epithelial voltohmmeter or equivalent system [9] |
Step-by-Step Differentiation Protocol
- Cell Seeding: Seed Caco-2/TC7 cells at a density of 0.1 × 10⁵ cells/cm² onto the apical chamber of Transwell plates containing polyester filters (0.4 µm pore size). Use complete DMEM medium (25 mM glucose) supplemented with 20% (v/v) FBS in both apical and basolateral compartments [10] [11].
- Initial Culture Period: Culture the cells until they reach 100% confluence, designated as Day 0. Continue differentiation in the same medium for the first 7 days, changing the medium three times per week [10].
- Serum Reduction for Polarization: From day 7 post-confluence, replace the apical compartment medium with FBS-free DMEM. The basolateral chamber should receive complete DMEM containing 10% (v/v) FBS to establish a growth factor gradient that promotes polarization [11].
- Monolayer Maturation: Allow cells to differentiate for a total of 14-21 days, with regular medium changes three times per week. The extended culture time is critical for the full expression of digestive hydrolases and transporter systems [10] [9].
- Quality Control: Before initiating experiments, validate monolayer integrity by measuring TEER. Use only monolayers with TEER values >250 Ω·cm² (for 24-well format) [9]. Confirm low paracellular leakage using a marker molecule like mannitol (Papp < 0.5 × 10⁻⁶ cm/s) [9].
The diagram below illustrates the cellular differentiation process and the key functional elements that make the Caco-2/TC7 model physiologically relevant.
Application Protocol: Glucose Uptake and Transport Assay
Experimental Workflow for Compound Screening
This protocol measures changes in glucose transporter activity and expression in response to experimental treatments, such as pharmaceutical compounds or phytochemicals.
- Treatment Application: Following differentiation and quality control, apply the test compound (e.g., dexamethasone, genistein) to the monolayer. Prepare test concentrations in FBS-free DMEM. Incubation times may vary; for example, dexamethasone effects are measurable after 60 hours of treatment [10].
- Glucose Uptake Measurement: Replace the treatment medium with a glucose-free buffer (e.g., HBSS). Add a non-metabolizable glucose analog, such as 2-deoxy-D-glucose, to the apical compartment to initiate the uptake phase. Incubate for a defined period (typically 15-60 minutes) at 37°C [10].
- Sample Collection and Analysis: Terminate uptake by removing the apical solution and washing the cells with ice-cold PBS. Lyse the cells and quantify the accumulated radiolabeled or fluorescent tracer using a scintillation counter or plate reader. Normalize the results to total cellular protein content.
- Gene Expression Analysis (qPCR/ddPCR): In parallel, isolate total RNA from treated monolayers. Use reverse transcription followed by droplet digital PCR (ddPCR) or quantitative PCR (qPCR) with TaqMan primers specific for SGLT1 (Hs01573793m1) and GLUT2 (Hs01096908m1) to quantify transporter mRNA expression [10] [11].
- Data Interpretation: Calculate the apparent permeability (Papp) coefficient for transport studies using the formula: Papp = VR / (A × C0) × (dC/dt) where VR is the receiver chamber volume (mL), A is the filter surface area (cm²), C0 is the initial donor concentration (µg/mL), and dC/dt is the slope of cumulative concentration in the receiver chamber over time (µg/mL/s) [9].
The following diagram outlines the key stages of a glucose uptake assay, from preparation to data analysis.
The Caco-2/TC7 cell line represents a robust, well-characterized, and physiologically relevant in vitro model for investigating the complex mechanisms of intestinal glucose absorption. Its capacity to form a polarized monolayer with authentic enterocyte features, including functional tight junctions and the regulated expression of key glucose transporters SGLT1 and GLUT2, makes it an invaluable tool for metabolic research and pharmaceutical development. The detailed protocols provided herein for cell differentiation, model validation, and functional glucose uptake assays offer a solid foundation for generating reliable, high-quality data within a thesis focused on understanding nutrient transport and screening potential therapeutic compounds.
Expression Profiles of SGLT1 and GLUT2 in Differentiated Caco-2/TC7 Monolayers
The Caco-2/TC7 cell line, a well-characterized clone of the human colorectal adenocarcinoma cell line, has emerged as a valuable in vitro model for studying intestinal glucose transport mechanisms. Upon differentiation, these cells form polarized monolayers that express key intestinal glucose transporters, including the sodium-glucose cotransporter 1 (SGLT1) and the facilitative glucose transporter 2 (GLUT2). Within the context of a broader thesis on in vitro glucose uptake assays, understanding the expression profiles and regulatory mechanisms of these transporters in Caco-2/TC7 monolayers is fundamental for research in nutrient absorption, drug development, and metabolic disorders. This application note synthesizes current data on SGLT1 and GLUT2 expression and function in this model system, providing standardized protocols and analytical tools to support research reproducibility.
Expression and Localization Profiles
In differentiated Caco-2/TC7 monolayers, SGLT1 and GLUT2 demonstrate distinct expression patterns, localization, and functional roles that can be modulated by various experimental conditions.
Table 1: Baseline Expression and Characteristics of SGLT1 and GLUT2 in Caco-2/TC7 Monolayers
| Feature | SGLT1 (SLC5A1) | GLUT2 (SLC2A2) |
|---|---|---|
| Primary Role | Apical, sodium-dependent glucose uptake [13] | Basolateral (and apical under high glucose), facilitative glucose/fructose transport [1] [2] |
| Localization | Apical membrane [13] | Basolateral membrane; can translocate to apical membrane under specific conditions [14] |
| Expression Confirmation | Protein confirmed by Western blot [15] | mRNA and protein detected [1] |
| Model Limitation | Lower expression compared to human enterocytes; lacks certain in vivo regulatory responses [13] | Expression is subject to regulation by metabolic and dietary factors [1] [14] |
Key Regulatory Mechanisms
The expression and activity of these transporters are influenced by multiple factors:
- Hormonal Regulation: Thyroid hormone (T3) treatment induces a 10-fold increase in SGLT1 mRNA abundance and a 6-fold increase in the Vmax of α-methylglucose transport [16]. Insulin internalizes GLUT2 from the brush border membrane, thereby reducing sugar absorption, a mechanism that is lost in insulin-resistant states [14]. Dexamethasone dose-dependently upregulates SGLT1 mRNA and increases functional glucose transport [10].
- Dietary Compounds: Polyphenol-rich berry extracts significantly decrease mRNA expression of both SGLT1 and GLUT2 in chronic treatments [1]. Acute exposure to certain flavonoids directly inhibits glucose uptake via these transporters [1] [17].
- Pathophysiological Context: In pro-inflammatory conditions, dexamethasone treatment further modulates the expression of these transporters and associated viral entry receptors, highlighting the model's relevance for studying metabolic inflammation [10].
Experimental Protocols for Transport Studies
Below are detailed methodologies for key experiments assessing glucose transporter function and expression in Caco-2/TC7 monolayers.
Cell Culture and Differentiation
- Cell Line: Caco-2/TC7 cells (passages 32-50 are commonly used [10] [2]).
- Culture Medium: Dulbecco's Modified Eagle Medium (DMEM) with high glucose (4.5 g/L or 25 mM), supplemented with 10-20% fetal bovine serum, 1% non-essential amino acids, 2 mM L-glutamine, and antibiotics [10] [2].
- Differentiation for Monolayers: Seed cells on permeable transwell filters (e.g., 0.4 µm pore size) at a density of 0.1 × 10⁵ cells/cm². Culture for at least 14-21 days post-confluence, with regular medium changes three times per week, to allow full differentiation and polarization [10]. The integrity of monolayers can be monitored by measuring Trans-Epithelial Electrical Resistance (TEER).
Glucose Uptake Assay
This protocol measures apical glucose uptake, adapted from published studies [1] [2].
Reagents:
- Uptake Buffer (Krebs-Ringer HEPES buffer): 130 mM NaCl, 4 mM KH₂PO₄, 1 mM MgSO₄, 1 mM CaCl₂, 30 mM HEPES, pH 7.4. For sodium-free buffer, replace NaCl with an equimolar amount of KCl or N-Methyl-D-glucamine.
- Radiolabeled Sugars: D-[¹⁴C(U)]-glucose or D-[³H]-glucose.
- Treatment Solutions: Compounds of interest (e.g., hormones, polyphenols) prepared in uptake buffer or culture medium.
- Wash Buffer: Ice-cold phosphate-buffered saline (PBS).
- Lysis Buffer: 0.1% SDS or 1% Triton X-100.
Procedure:
- Pre-treatment: Wash differentiated monolayers with uptake buffer. For acute inhibition studies, pre-incubate with the test compound for 15-30 minutes.
- Uptake Phase: Replace the apical buffer with uptake buffer containing the radiolabeled glucose tracer (e.g., 10 mM D-Glucose with 0.1 μCi/mL [¹⁴C]-glucose) with or without the test compound. Incubate for a defined period (typically 2-10 minutes) at 37°C.
- Termination: Quickly remove the uptake solution and wash the monolayers three times with ice-cold PBS to stop the reaction.
- Lysis and Analysis: Lyse cells with 0.2% SDS for 60 minutes at 37°C. Collect the lysate for scintillation counting to determine intracellular radioactivity. Normalize uptake data to total cellular protein content.
Data Analysis:
- Total Glucose Uptake: Measured in sodium-containing buffer.
- SGLT1-mediated Uptake: Calculated as the difference between total uptake and uptake in sodium-free buffer.
- Facilitated Uptake (GLUT-mediated): Measured directly in sodium-free buffer.
Gene Expression Analysis (RT-qPCR)
- RNA Isolation: Extract total RNA from monolayers using TRIzol reagent or similar, following the manufacturer's protocol [1] [2].
- cDNA Synthesis: Use 1 μg of DNase-treated RNA for reverse transcription with a High-Capacity cDNA kit.
- Quantitative PCR: Perform real-time PCR using TaqMan or SYBR Green chemistry. Use primer/probe sets specific for human genes:
- Data Analysis: Calculate relative gene expression using the 2^(-ΔΔCt) method.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagent Solutions for Studying Glucose Transporters in Caco-2/TC7 Models
| Reagent / Kit | Function / Application | Example Use / Note |
|---|---|---|
| Caco-2/TC7 Cell Line | Differentiates into enterocyte-like monolayers expressing SGLT1 and GLUT2. | Obtain from recognized cell banks; passage number should be carefully controlled [15]. |
| Transwell Permeable Filters | Provide a polarized environment for cell growth and differentiation. | Polyester filters, 0.4 µm pore size, various diameters (e.g., 12 mm, 24 mm) [10]. |
| D-[¹⁴C(U)]-Glucose | Radiolabeled tracer for measuring glucose uptake kinetics. | Used at ~0.1 μCi/mL in uptake buffer [1] [2]. |
| Phloridzin | Specific, competitive inhibitor of SGLT1. | Tool for isolating SGLT1-mediated transport component [17]. |
| Phloretin | Potent inhibitor of facilitative glucose transporters (GLUT2). | Tool for isolating GLUT-mediated transport component [1]. |
| Anti-SGLT1 / Anti-GLUT2 Antibodies | Protein detection and localization via Western blot or immunofluorescence. | Commercial antibodies available (e.g., Millipore) [1] [15]. |
| TRIzol Reagent | Total RNA isolation for gene expression studies. | Standard method for extracting high-quality RNA from monolayers [1] [2]. |
| Dexamethasone | Synthetic glucocorticoid that upregulates SGLT1 expression. | Used at 5-20 µM in treatment media to study hormonal regulation [10]. |
| OptiBerry / Walnut Polyphenols | Polyphenol-rich extracts that modulate transporter expression and activity. | Used to study dietary inhibition of glucose absorption (e.g., 0.125% w/v) [1] [18]. |
Signaling Pathways and Experimental Workflows
Diagram 1: Regulatory pathways and experimental analysis of glucose transporters in Caco-2/TC7 monolayers. External stimuli (red) trigger intracellular regulatory pathways (blue) that alter transporter expression or localization (blue), leading to functional outcomes (green) that are measured by specific experimental endpoints (green).
The Caco-2/TC7 cell model provides a robust and well-characterized platform for investigating the regulation of SGLT1 and GLUT2 in an intestinal context. Its responsiveness to hormonal, dietary, and pharmacological stimuli makes it particularly valuable for pre-clinical screening of compounds aimed at modulating intestinal glucose absorption for metabolic disease management. Researchers should remain cognizant of the model's limitations, including its cancerous origin and differences in regulatory responses compared to in vivo intestine. Standardization of culture conditions, differentiation protocols, and assay parameters, as outlined in this document, is critical for generating reproducible and physiologically relevant data.
Intestinal glucose transporters, primarily Sodium-dependent Glucose Transporter 1 (SGLT1) and Glucose Transporter 2 (GLUT2), serve as critical gatekeepers for dietary glucose absorption into the bloodstream [1]. Their dysregulation represents a significant contributing factor to postprandial hyperglycaemia, a key feature of metabolic syndrome and type 2 diabetes [19]. Furthermore, these transporters interact with various drugs and natural compounds, influencing drug absorption and efficacy [20]. The Caco-2/TC7 cell line, a well-established in vitro model of the human intestinal epithelium, provides a robust platform for investigating transporter activity and its implications for human health [21]. These cells spontaneously differentiate into enterocyte-like cells expressing functional brush border enzymes and nutrient transporters, including SGLT1 and GLUT2, making them indispensable for screening compounds that modulate glucose absorption and for assessing drug-nutrient interactions [2] [21]. This Application Note details protocols and findings from Caco-2/TC7-based research, providing a framework for exploring transporter function in health and disease.
Key Findings from Caco-2/TC7 Research
Research utilizing the Caco-2/TC7 model has yielded significant insights into the regulation of intestinal glucose transporters by pharmaceuticals, dietary compounds, and in pathological conditions. The quantitative effects of various modulators on glucose transporter expression and function, as established in this model system, provide a critical foundation for understanding their potential impact on human health.
Table 1: Quantified Effects of Pharmacologic Agents on Glucose Transporters in Caco-2/TC7 Models
| Modulator | Target / Class | Effect on SGLT1 | Effect on GLUT2 | Experimental Context |
|---|---|---|---|---|
| Dexamethasone [10] | Corticosteroid | ↑ mRNA (Dose-dependent) | ↓ mRNA (In cells); ↑ mRNA (In mice) | Differentiated Caco-2/TC7 monolayers; 5-20 µM dose range |
| Berry Extract [1] | Polyphenol / Anthocyanin | ↓ mRNA (Time & dose-dependent); Protein | ↓ mRNA & Protein (Time & dose-dependent) | Caco-2/TC7 cells; 0.125% (w/v) extract; 16h exposure |
| Mulberry Leaf Extract [6] | Phenolic Compounds | Inhibited activity (Functional assay) | Inhibited activity (Functional assay) | Digested extract on Caco-2 monolayers & IR-HepG2 co-culture |
| Genistein [19] | Phytochemical / Isoflavone | Normalized inflammation-induced ↑ | Not specified | Differentiated Caco-2/TC7 with IL-1β/TNF-α-induced inflammation |
| Digested Dietary Proteins [22] | Protein Hydrolysates | Not specified | ↓ mRNA | Caco-2/TC7 cells; 5 mg/mL for 1h (Casein, Fish Gelatin, etc.) |
Table 2: Effects of Inflammation and Natural Compounds on Viral Entry Receptors
| Condition / Modulator | Effect on ACE2 | Effect on TMPRSS2 | Experimental Context |
|---|---|---|---|
| Dexamethasone [10] | ↓ mRNA & Protein | ↑ mRNA | Differentiated Caco-2/TC7 monolayers |
| Pro-inflammatory Cytokines (IL-1β, TNF-α) [19] | ↑ Gene Expression | ↑ Gene Expression | Differentiated Caco-2/TC7; association with SGLT1 pattern |
| Genistein [19] | Not specified | ↓ Inflammation-induced increase | Differentiated Caco-2/TC7 with IL-1β/TNF-α-induced inflammation |
Detailed Experimental Protocols
Protocol 1: Measuring Glucose Uptake in Differentiated Caco-2/TC7 Monolayers
This protocol outlines the procedure for assessing active glucose transport using radio-labelled glucose analogs across differentiated Caco-2/TC7 cell monolayers, a standard method for evaluating transporter function [10] [22].
Key Research Reagent Solutions:
- Caco-2/TC7 Cells: Human colon carcinoma-derived cells that differentiate into enterocyte-like cells [10] [19].
- Dulbecco's Modified Eagle Medium (DMEM): High glucose (4.5 g/L or 25 mM) for cell culture and differentiation [10] [2].
- Fetal Bovine Serum (FBS): Heat-inactivated, used at 10-20% (v/v) for cell culture [10].
- Transwell Plates: Permeable supports with polyester filters (0.4 µm pore size) for monolayer growth [10] [19].
- 2-Deoxy-D-Glucose or α-Methyl-D-Glucopyranoside (AMG): Non-metabolizable glucose analogs used with radio-labelled tracers (e.g., 14C-AMG) to measure specific uptake [10] [22].
- Phlorizin: A specific SGLT1 inhibitor used to confirm sodium-dependent uptake and stop reactions [22].
Procedure:
- Cell Seeding and Differentiation: Seed Caco-2/TC7 cells at a density of 0.1 × 10^5 cells/cm² on the apical chamber of Transwell plates. Culture in complete DMEM (25 mM glucose) with 20% FBS. Upon reaching 100% confluence (designated Day 0), differentiate cells for 14-21 days. After the first 7 days, replace the apical medium with FBS-free DMEM, while the basolateral compartment should receive DMEM with 10-20% FBS. Change the medium three times per week [10] [19].
- Treatment with Test Compounds: Prior to the assay, pre-incubate cell monolayers with the compound of interest (e.g., digested proteins, phytochemicals, or pharmaceuticals) diluted in non-supplemented DMEM. For instance, incubate with digested proteins at 5 mg/mL for 1 hour in the apical compartment [22].
- Glucose Uptake Assay: Prepare an uptake buffer, such as Krebs' buffered saline (KBS). Replace the apical medium with buffer containing the radio-labelled glucose analog (e.g., 2 mM AMG with 0.2 μCi/mL 14C-AMG) and the test compound. Incubate for a defined period (e.g., 40 minutes) to allow for glucose transport [2] [22].
- Termination of Uptake and Analysis: Stop the uptake by washing the monolayers with cold phosphate-buffered saline (PBS) containing 0.5 mM phlorizin. Solubilize the cells, and measure the radioactivity in the cellular lysate using a scintillation counter. Normalize the results to the total protein content in the lysate, determined by a protein assay (e.g., BCA assay) [22].
Experimental workflow for measuring glucose uptake in Caco-2/TC7 monolayers.
Protocol 2: Evaluating Gene Expression of Transporters and Receptors
This protocol describes the process of quantifying mRNA expression of key targets like SGLT1, GLUT2, ACE2, and TMPRSS2 in Caco-2/TC7 cells following experimental treatments.
Procedure:
- Cell Treatment and RNA Isolation: Differentiate Caco-2/TC7 cells as described in Protocol 1. Treat the differentiated monolayers with the compound of interest (e.g., cytokines for inflammation models or phytochemicals). After treatment, wash the cells with ice-cold PBS and lyse them using a reagent like TRIzol. Extract total RNA using a commercial kit according to the manufacturer's instructions [1] [19].
- cDNA Synthesis: Treat the extracted RNA with DNase to remove genomic contamination. Perform reverse transcription using a High-Capacity cDNA reverse transcription kit to generate complementary DNA (cDNA) [1] [19].
- Gene Expression Analysis: Analyze the cDNA using quantitative methods such as droplet digital PCR (ddPCR) or real-time quantitative PCR (qPCR). Use TaqMan primers and probes specific for the genes of interest (e.g., SGLT1: Hs01573793m1; GLUT2: Hs01096908m1; ACE2: Hs01085333m1; TMPRSS2: Hs01122322m1). Normalize the expression of target genes to a housekeeping gene, such as TATA-box binding protein (TBP) [10] [19].
Signaling Pathways and Transporter Regulation
The regulation of intestinal glucose transporters is interconnected with inflammatory pathways and other receptor systems. The Caco-2/TC7 model has been instrumental in elucidating these connections, particularly the link between inflammation, the renin-angiotensin system, and glucose absorption.
Signaling pathway linking inflammation to glucose transporter regulation.
Pro-inflammatory cytokines such as IL-1β and TNF-α activate the NF-κB pathway, which can lead to a downregulation of ACE2 in the intestine [19]. As ACE2 is a negative regulator of SGLT1 and GLUT2 expression via the ACE2/Ang-(1-7)/Mas axis, its downregulation results in increased expression and activity of these glucose transporters, thereby enhancing intestinal glucose absorption and contributing to postprandial hyperglycemia [19]. Furthermore, inflammation induces a correlated upregulation of SGLT1 and TMPRSS2, suggesting a shared regulatory mechanism [19]. This pathway identifies a potential link between gut inflammation, dysregulated glucose metabolism, and modulations in SARS-CoV-2 viral entry receptors. Research using Caco-2/TC7 cells shows that phytochemicals like the isoflavone genistein can normalize the inflammation-induced increases in SGLT1 and TMPRSS2 [19].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Caco-2/TC7 Transporter Studies
| Reagent / Tool | Function / Application | Specific Examples |
|---|---|---|
| Caco-2/TC7 Cell Line | Differentiates into enterocyte-like cells; expresses relevant transporters and enzymes for intestinal absorption studies. | Donated from Rousset Lab (U178 INSERM, Villejuif, France) [10] [19]. |
| Transwell Inserts | Permeable supports for growing differentiated, polarized cell monolayers with distinct apical and basolateral compartments. | Polyester filters, 0.4 µm pore size, various diameters (e.g., 12 mm, 24 mm) [10]. |
| Radio-labelled Glucose Analogs | Tracers for measuring specific, transporter-mediated glucose uptake in functional assays. | 14C-α-Methyl-D-Glucopyranoside (14C-AMG) [22]; 3H-D-Glucose [1]. |
| SGLT1 Inhibitor | Pharmacologic tool to confirm SGLT1-specific component of glucose uptake. | Phlorizin (used in wash buffer to terminate uptake) [22]. |
| TaqMan Primers for qPCR/ddPCR | Target-specific probes for precise quantification of gene expression levels. | SGLT1 (Hs01573793m1), GLUT2 (Hs01096908m1), ACE2 (Hs01085333m1), TMPRSS2 (Hs01122322m1) [10] [19]. |
| Pro-inflammatory Cytokines | To establish in vitro models of intestinal inflammation for studying its impact on transporter expression. | Human IL-1β and TNF-α proteins [19]. |
Protocols and Applications: Establishing a Robust Glucose Uptake Assay
Standard Cell Culture and Differentiation Protocols for Reproducible Monolayers
The Caco-2/TC7 cell line, a clone derived from the original human colorectal adenocarcinoma Caco-2 cells, has become a premier in vitro model for studying intestinal barrier function, nutrient transport, and drug permeability [23]. When cultured under specific conditions, these cells spontaneously differentiate into polarized enterocyte-like cells that form tight junctions and express functional brush border enzymes and transporters characteristic of the human small intestine [23] [24]. This application note provides detailed, standardized protocols for cultivating and differentiating Caco-2/TC7 cells to generate reproducible, high-quality monolayers specifically optimized for glucose uptake assays and related transport studies. Implementation of these standardized methods ensures experimental consistency and reliability, which is crucial for generating physiologically relevant data in pharmaceutical development and basic research.
Cell Culture Maintenance
Proper maintenance of stock cultures is fundamental to obtaining consistent differentiation results in subsequent experiments.
Basic Culture Conditions
Growth Medium Composition:
- Base Medium: Dulbecco's Modified Eagle Medium (DMEM) with high glucose (4.5 g/L or 25 mM) [19] [25]
- Serum Supplement: 20% (v/v) heat-inactivated fetal bovine serum (FBS) [19] [26]
- Additional Supplements:
Culture Environment:
- Temperature: 37°C [26]
- Gas Phase: 10% CO₂/90% air [19] or 5% CO₂ [26]
- Vessel: 75 cm² culture flasks [19]
Table 1: Standard Culture Conditions for Caco-2/TC7 Cells
| Parameter | Specification | Reference |
|---|---|---|
| Seeding Density | 0.2 × 10⁵ cells/cm² | [19] |
| Subculturing Confluence | ~60% | [19] |
| Passage Ratio | 1:2 to 1:4 | [26] |
| Medium Change Frequency | Every 2-3 days | [26] |
| Typical Passage Range for Experiments | 32-50 | [19] [2] |
Practical Culture Tips
- Cell Adhesion: Caco-2/TC7 cells adhere slowly after thawing or passaging. Avoid changing the medium within the first 48 hours to facilitate attachment [26].
- Cell Morphology: The cells typically grow in island-like patterns and may contain large vacuoles and black granules in the cytoplasm, which is considered normal [26].
- Digestion Control: Carefully control trypsinization time (5-10 minutes) to ensure cells dissociate into single cells without damage [26].
- Serum Quality: Use high-quality FBS, as serum concentration below 20% can prolong adhesion time and potentially prevent proper attachment [26].
Monolayer Differentiation on Filter Inserts
Cultivation on permeable filter supports enables polarization and functional differentiation that closely mimics the intestinal epithelium.
Differentiation Protocol
Seeding and Initial Culture:
- Filter Selection: Use polyester Transwell filters (0.4 μm pore size) in 6-well (24 mm diameter) or 12-well (12 mm diameter) plates [19] [25].
- Seeding Density: Seed cells at 0.1 × 10⁵ cells/cm² in complete DMEM medium (25 mM glucose) supplemented with 20% FBS in both apical and basolateral compartments [19] [25].
- Confluence Monitoring: Examine cells daily until they reach 100% confluence, marked as Day 0 of differentiation [19].
Differentiation Timeline:
- Days 0-7: Maintain cells in complete DMEM (25 mM glucose, 20% FBS) on both apical and basolateral sides [19] [25].
- Day 7 Onward: Replace apical compartment medium with FBS-free DMEM, while the basolateral chamber receives complete DMEM with either 10% or 20% FBS [19] [25].
- Medium Changes: Change medium regularly three times per week [19].
- Differentiation Duration: Culture for 14-21 days total to allow full differentiation [19] [24].
Critical Parameters for Reproducible Monolayers
- Seeding Density Impact: Higher seeding densities (>0.2 × 10⁶ per cm²) may cause earlier confluence but increase risk of detachment after 16 days [24].
- Optimal Differentiation Period: 19-21 days of cultivation leads to optimal enzymatic properties and uniform cell density [24].
- Extended Culture Caution: Cultivation periods over 21 days increase the likelihood of cell detachment, as indicated by rapid decreases in TEER values [24].
Quality Control of Differentiated Monolayers
Rigorous quality assessment is essential before utilizing monolayers for experimental applications.
Transepithelial Electrical Resistance (TEER) Measurement
TEER measures the integrity of tight junctions in cell monolayers [23].
- Acceptance Criteria: TEER values ≥200 Ω·cm² at 37°C indicate acceptable monolayer integrity [24].
- Measurement Frequency: Measure at least once weekly during differentiation and before starting experiments [24].
- Typical Pattern: TEER values typically increase throughout the differentiation period, forming a characteristic curve as the tight junctions mature [24].
Paracellular Permeability Assay
This assay validates the barrier function by measuring the passage of non-absorbable markers.
- Common Markers: Dextran Blue or [¹⁴C]-mannitol [24].
- Typical Values: Apparent permeability (Papp) for [¹⁴C]-mannitol should be approximately 1.30 ± 0.77 × 10⁻⁶ cm/s [24].
- Experimental Setup: Monitor paracellular transit of Dextran Blue every hour over 6 hours or [¹⁴C]-mannitol over 2 hours [24].
Confocal Microscopy Validation
Visual confirmation of monolayer integrity and tight junction formation.
- Staining Protocol: Use fluorescently labelled antibody against zonula occludens (ZO)-1 tight junction protein (e.g., Alexa Fluor 594 conjugated anti-ZO-1 antibody, 1 μg/mL) with DAPI nuclear counterstain [24].
- Expected Outcome: A single, continuous cell layer with well-defined tight junctions between adjacent cells in both top view and cross-section [24].
Table 2: Quality Control Parameters for Differentiated Caco-2/TC7 Monolayers
| Parameter | Method | Acceptance Criteria | Typical Values |
|---|---|---|---|
| Barrier Integrity | TEER Measurement | ≥200 Ω·cm² | Increases with differentiation [24] |
| Paracellular Permeability | [¹⁴C]-mannitol transport | Papp ~1.30 ± 0.77 × 10⁻⁶ cm/s | Low values indicate tight junctions [24] |
| Tight Junction Formation | ZO-1 immunofluorescence | Continuous junctional staining | Visual confirmation of barrier [24] |
| Cell Viability | CCK-8 assay | ≥80% for transport studies | Concentration-dependent [6] |
Application: Glucose Uptake Assay Protocol
The following protocol has been specifically optimized for measuring glucose transport in differentiated Caco-2/TC7 monolayers.
Experimental Setup
Pre-experiment Conditions (Day 19-21):
- On day 19 of differentiation, begin treatment with experimental compounds (e.g., dexamethasone, phytochemicals) or vehicle control twice daily for total treatment duration of 60 hours [25].
- During the last 24 hours before the experiment, use FBS-free DMEM medium (with appropriate glucose concentration) on both apical and basolateral compartments [25].
Glucose Starvation and Uptake Measurement:
- On day 21, starve cells for 4 hours using glucose- and FBS-free DMEM medium in the presence of test compounds or vehicle control [25].
- After starvation, remove all media and add fresh FBS- and glucose-free medium to the basolateral side [25].
- Add fresh FBS- and glucose-free medium supplemented with 5 mM 2-deoxy-D-glucose (non-metabolizable glucose analog) to the apical side [25].
- Measure 2-deoxy-D-glucose transport across the monolayer to quantify glucose uptake capacity [25].
Key Assay Considerations
- Glucose Concentration: Culture cells in either 5.5 mM (normal) or 25 mM (high) glucose-containing medium from day 7 of differentiation to model different metabolic conditions [25].
- Inflammation Models: To study inflammatory conditions, co-stimulate with pro-inflammatory cytokines (e.g., IL-1β and TNF-α) for up to 168 hours to induce inflammation and examine its effects on glucose transporter expression [19].
- Compound Screening: This system effectively screens phytochemicals (e.g., genistein, apigenin) and pharmaceuticals for their effects on glucose transporters (SGLT1, GLUT2) and related pathways [19].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Caco-2/TC7 Culture and Experiments
| Reagent Category | Specific Examples | Function/Application | References |
|---|---|---|---|
| Cell Culture Medium | High-glucose DMEM (4.5 g/L) | Base nutrient medium supporting cell growth and differentiation | [19] [25] |
| Serum Supplement | Heat-inactivated Fetal Bovine Serum (FBS), 16-20% | Provides essential growth factors and adhesion factors | [19] [27] |
| Differentiation Supplements | Non-essential amino acids, GlutaMAX | Supports polarized growth and tight junction formation | [19] [2] |
| Permeability Markers | [¹⁴C]-mannitol, Dextran Blue | Quality control of monolayer integrity | [24] |
| Glucose Uptake Tracers | 2-deoxy-D-glucose, [¹⁴C] radio-labelled sugars | Measurement of glucose transport functionality | [2] [25] |
| Pro-inflammatory Cytokines | IL-1β, TNF-α | Modeling inflammatory conditions in gut epithelium | [19] |
| Transporter Modulators | Genistein, Apigenin, Dexamethasone | Research tools for modulating glucose transporter expression | [19] [25] |
| Molecular Biology Kits | TaqMan primers for SGLT1, GLUT2, ACE2, TMPRSS2 | Quantifying gene expression of relevant transporters | [19] [25] |
Troubleshooting Common Challenges
- Poor Cell Adhesion: Ensure FBS concentration is at least 20% and use high-quality serum batches. Avoid disturbing cultures immediately after seeding [26].
- Low TEER Values: Check passage number (use passages 32-50), verify seeding density, and confirm proper medium changes. Low TEER may indicate inadequate differentiation [19] [24].
- Cellular Senescence: Use lower passage cells, adjust seeding density to avoid over-confluence, and ensure regular medium changes to prevent nutrient depletion [26].
- High Experimental Variability: Standardize passage numbers, maintain consistent differentiation timelines, and implement rigorous quality control checks for each experiment [28] [24].
Standardized culture and differentiation protocols are essential for generating reproducible Caco-2/TC7 monolayers that reliably model intestinal epithelial function. The detailed methods outlined in this application note provide researchers with a robust framework for establishing high-quality intestinal barriers optimized for glucose uptake studies and related transport assays. Consistent implementation of these protocols, coupled with rigorous quality control measures, ensures the generation of reliable, physiologically relevant data for both basic research and drug development applications.
Within the field of intestinal biology and drug development, the Caco-2/TC7 cell line is a well-characterized and physiologically relevant in vitro model of the human enterocyte. These cells, upon differentiation, form polarized monolayers that express functional digestive enzymes, membrane peptidases, and nutrient transporters characteristic of the small intestinal epithelium, making them indispensable for studying intestinal glucose absorption [28] [11]. Accurate assessment of glucose transporter activity is fundamental to research on nutrient metabolism, drug discovery for metabolic diseases, and toxicology studies. This application note details three core assay techniques—using radio-labelled sugars, non-metabolizable analogs, and inhibition controls—within the context of a broader thesis on glucose uptake assays in Caco-2/TC7 cell research.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table catalogues essential reagents and their specific functions in conducting glucose uptake assays with Caco-2/TC7 cells.
Table 1: Essential Reagents for Glucose Uptake Assays
| Reagent / Assay Kit | Primary Function in Assay | Key Features & Considerations |
|---|---|---|
| ²H- or ¹⁴C-labelled D-Glucose | Tracer for measuring total glucose uptake via scintillation counting [1]. | Requires handling and disposal of radioactive materials; multiple wash steps are needed [29]. |
| ¹⁴C-α-methyl-D-glucopyranoside (AMG) | Non-metabolizable SGLT1-specific substrate; trapped inside cell after transport [22]. | Resistant to metabolism; used with scintillation counting [22]. |
| 2-Deoxy-D-Glucose (2-DG) | Non-metabolizable glucose analog; phosphorylated and accumulated as 2DG6P [10] [29]. | Can be radiolabelled (³H-2DG) or detected enzymatically in non-radioactive kits [29]. |
| 2-NBDG | Fluorescently tagged glucose analog for imaging glucose uptake [29]. | Ideal for real-time, single-cell imaging; its larger molecular size may not perfectly reflect native glucose transporter kinetics [29]. |
| Glucose Uptake-Glo Assay | Luminescent, non-radioactive method to detect accumulated 2DG6P [29]. | No wash steps; high-throughput compatible; sensitive detection with a large signal window [29]. |
| Phlorizin | Potent and specific inhibitor of the SGLT1 transporter [1] [22]. | Used in inhibition controls to isolate SGLT1-mediated uptake from facilitative diffusion/GLUT transport. |
| Phloretin | Inhibitor of facilitative glucose transporters (GLUTs) [1]. | Used in inhibition controls to isolate GLUT-mediated uptake from SGLT1 activity. |
| Sodium-Free Buffers | Replaces sodium ions with choline or other cations in uptake buffers [1]. | Functionally inhibits sodium-dependent SGLT1 activity, allowing measurement of the sodium-independent (GLUT-mediated) uptake component. |
Core Techniques & Quantitative Comparison
Selecting the appropriate assay technique is critical for experimental success. The table below provides a comparative overview of the primary methods.
Table 2: Core Assay Techniques for Measuring Glucose Uptake
| Assay Technique | Principle of Detection | Key Advantages | Key Disadvantages / Considerations |
|---|---|---|---|
| Radio-Labelled Sugars (e.g., ³H-/¹⁴C-D-Glucose) | Scintillation counting of intracellular accumulated radiolabel [30] [1]. | High sensitivity; considered a gold standard [29]. | Radioactive handling/disposal; multiple wash steps [29]. |
| Non-Metabolizable Analogs (e.g., 2-DG, AMG) | Analog is transported and phosphorylated, but not further metabolized, leading to intracellular accumulation [10] [29] [22]. | Distinguishes transport from metabolism; versatile detection methods (radioactive, luminescent) [29]. | 2-NBDG may have altered transport kinetics [29]. |
| Luminescent Detection (e.g., Glucose Uptake-Glo) | Enzymatic conversion of accumulated 2DG6P to generate a luminescent signal [29]. | No radioactivity; simple "add-and-read" with no wash steps; high-throughput; sensitive [29]. | Not suitable for cell imaging [29]. |
Detailed Experimental Protocols
Protocol 1: Radio-Labelled Sugar Uptake Assay
This protocol is adapted from studies investigating the acute effects of sugars and phytochemicals on glucose transport [30] [1] [2].
Key Applications:
- Measuring acute changes in total glucose uptake capacity.
- Studying the effects of drugs, nutrients, or inflammatory stimuli on transporter activity.
Procedure:
- Cell Culture & Differentiation: Seed Caco-2/TC7 cells at a density of 250,000 cells per 4.2 cm² transwell insert or 10,000 cells/cm² in multi-well plates [30] [22]. Culture for at least 14-21 days post-confluence to ensure full differentiation, with regular media changes three times per week [10] [11].
- Pre-incubation (Optional): Pre-treat cell monolayers with compounds of interest (e.g., test compounds, cytokines) for a defined period. For acute inhibitor studies, a 15-minute pre-incubation is often used [1].
- Uptake Phase:
- Aspirate the culture medium and wash cell monolayers once with pre-warmed Krebs' Buffered Saline (KBS) or a similar physiological buffer (e.g., 30 mM HEPES, 130 mM NaCl, 4 mM KH₂PO₄, 1 mM MgSO₄, 1 mM CaCl₂, pH 7.4) [30] [2].
- Add the uptake buffer containing the radiolabelled tracer. A typical final concentration is 10 mM D-Glucose spiked with 0.1 μCi/mL [¹⁴C] D-Glucose [30] [2].
- Incubate for a short, defined period (e.g., 2-10 minutes) at 37°C to ensure initial uptake rates are measured.
- Termination & Lysis:
- Scintillation Counting & Analysis:
- Transfer the lysate to scintillation vials, add scintillation fluid, and measure radioactivity with a scintillation counter [30] [2].
- Normalize the accumulated radioactivity to the total protein content of each sample (e.g., using a BCA or Bradford assay) [1] [22]. Correct for simple diffusion by performing parallel assays with a non-transportable analog like [¹⁴C] L-Glucose [30].
Protocol 2: Uptake Assay Using Non-Metabolizable Analogs (2-DG/AMG)
This protocol is commonly used to specifically measure transporter activity without interference from subsequent metabolic pathways [10] [22].
Key Applications:
- Specific measurement of SGLT1 activity (using AMG).
- General assessment of hexose kinase activity in conjunction with transport.
- High-throughput screening of transporter inhibitors.
Procedure:
- Cell Preparation: Differentiate Caco-2/TC7 cells on transwell or multi-well plates as described in Protocol 1, steps 1-2.
- Uptake Initiation:
- For 2-DG uptake, replace the medium with buffer containing 2 mM 2-DG (or a similar concentration) along with a tracer amount of radiolabelled ¹⁴C-2-DG [10]. Alternatively, use a non-radioactive detection kit.
- For SGLT1-specific uptake, use 2 mM α-methyl-D-glucopyranoside (AMG) with 0.2 μCi/mL ¹⁴C-AMG [22].
- Incubate for a defined time (e.g., 10-40 minutes) at 37°C [10] [22].
- Termination & Detection:
- For radioactive analogs: Follow the same termination, washing, and lysis steps as in Protocol 1, followed by scintillation counting [22].
- For non-radioactive detection (e.g., Glucose Uptake-Glo):
- After the uptake incubation, simply aspirate the uptake buffer.
- Add the proprietary detection reagent directly to the cells without washing. The subsequent enzymatic reaction generates a luminescent signal proportional to the intracellular 2DG6P concentration [29].
Protocol 3: Implementing Inhibition Controls
Inhibition controls are essential for deconvoluting the specific contributions of different transporter types to the total observed glucose uptake [1].
Key Applications:
- Distinguishing SGLT1-mediated vs. GLUT-mediated glucose uptake.
- Validating the mechanism of action of novel transport inhibitors.
- Isolating specific transport components in mechanistic studies.
Procedure:
- Experimental Groups: Differentiated Caco-2/TC7 monolayers should be divided into the following experimental groups for a single uptake experiment:
- Total Uptake: Uptake measured in sodium-containing buffer.
- SGLT1-Inhibited / GLUT Component: Uptake measured in sodium-containing buffer with 0.5 mM Phlorizin [22] OR in a sodium-free buffer (where NaCl is replaced isotonically with Choline-Cl or N-Methyl-D-glucamine) [1].
- GLUT-Inhibited / SGLT1 Component: Uptake measured in sodium-containing buffer with 0.5 mM Phloretin [1].
- Non-specific Diffusion / Background: Uptake of a non-transportable analog like L-Glucose.
- Assay Execution: Perform the uptake assay as outlined in Protocol 1 or 2 for all groups simultaneously.
- Data Calculation:
- SGLT1-mediated Uptake = (Total Uptake) - (Uptake in presence of Phlorizin or in Na⁺-free buffer)
- GLUT-mediated Uptake = (Total Uptake) - (Uptake in presence of Phloretin)
- Facilitated Uptake (Sodium-independent) = (Uptake in Na⁺-free buffer) - (Non-specific Diffusion)
Workflow Visualization & Data Interpretation
Experimental Workflow for Glucose Uptake Studies
The following diagram illustrates the logical flow for designing and executing a glucose uptake study in Caco-2/TC7 cells.
Data Interpretation and Normalization
Robust data analysis is critical for drawing meaningful conclusions. The table below outlines key parameters and normalization methods.
Table 3: Key Parameters for Data Analysis in Glucose Uptake Assays
| Parameter | Description & Calculation | Application & Significance |
|---|---|---|
| Absolute Uptake (nmol/mg protein) | (Measured radioactivity or 2DG6P) / (Total protein per well). Corrected for non-specific diffusion (L-Glucose uptake) [1]. | Provides a direct measure of glucose transporter activity under the tested conditions. |
| Apparent Permeability Coefficient (Papp) | Papp = (dQ/dt) / (A × C₀), where dQ/dt is the transport rate, A is the membrane surface area, and C₀ is the initial donor concentration [28]. | Standardizes transport rates for comparisons between different experimental setups; used for BCS classification of drugs [28]. |
| Fractional Uptake Components | SGLT1% = (SGLT1-mediated Uptake / Total Uptake) × 100. GLUT% = (GLUT-mediated Uptake / Total Uptake) × 100 [1]. | Quantifies the relative contribution of each transporter system, revealing specific regulatory mechanisms. |
The techniques outlined herein—radio-labelled sugars, non-metabolizable analogs, and inhibition controls—form the cornerstone of robust and interpretable glucose uptake studies in Caco-2/TC7 intestinal models. The choice of assay depends critically on the research question, required sensitivity, throughput, and safety considerations. Adherence to detailed protocols for cell culture, differentiation, and assay execution, coupled with the appropriate use of pharmacological controls, ensures the generation of reliable and mechanistically insightful data. These protocols provide a solid foundation for advanced research in nutrient absorption, drug transport, and the development of therapeutic interventions for metabolic disorders.
The Caco-2 cell line, particularly the TC7 clone, serves as a well-established in vitro model of the human intestinal epithelial barrier for studying glucose absorption and screening potential modulators [31]. Upon differentiation, these cells develop a polarized morphology, functional tight junctions, and a brush border, expressing key intestinal glucose transporters including SGLT1 (Sodium-Glucose Cotransporter 1) and GLUT2 (Glucose Transporter 2) [13] [32]. This model is instrumental in the early screening of pharmaceuticals, plant extracts, and dietary compounds for their ability to modulate postprandial glycaemia by affecting intestinal glucose transport mechanisms [33] [32]. The predictability of this model for human intestinal absorption, especially for compounds absorbed via passive diffusion, has been validated, though researchers must be mindful of its limitations concerning highly lipophilic compounds, transporter-mediated routes, and first-pass metabolism [31].
Key Experimental Protocols
This section details the core methodologies for culturing Caco-2/TC7 cells and performing glucose uptake assays to screen for transport modulators.
Cell Culture and Differentiation on Filter Inserts
The formation of a tight, differentiated monolayer is critical for reproducible and physiologically relevant results.
- Seeding and Differentiation: Seed Caco-2/TC7 cells (passages 40-50) onto filter inserts (e.g., PET or polycarbonate) at a density of approximately 0.2 × 10^6 per cm² [24]. Culture the cells for 19-21 days post-confluence to allow for full differentiation, refreshing the culture medium every other day. The standard culture medium is Dulbecco's Modified Eagle Medium (DMEM) with high glucose, supplemented with 20% (v/v) Fetal Bovine Serum (FBS), 0.1 mM non-essential amino acids, 10 mM HEPES buffer, 2 μM L-glutamine, and 100 U/mL Penicillin/Streptomycin [34] [32].
- Quality Control: Monitor monolayer integrity by regularly measuring Transepithelial Electrical Resistance (TEER). Use only monolayers with TEER values ≥200 Ω·cm² for experiments [24]. Confirm integrity and the presence of tight junctions by staining for Zonula Occludens-1 (ZO-1) [33] [24]. Paracellular permeability can be assessed using markers like [¹⁴C]-mannitol, with typical apparent permeability (P_app) values of ~1.30 ± 0.77 × 10⁻⁶ cm·s⁻¹ indicating an intact barrier [24].
Glucose Uptake Assay Protocol
This protocol measures the acute effects of test compounds on glucose transport.
- Pre-equilibration: Pre-equilibrate differentiated Caco-2/TC7 monolayers with the test compound (e.g., plant extract, pharmaceutical) dissolved in uptake buffer for 15 minutes [32]. A suitable positive control for inhibition is phloretin (a GLUT inhibitor) or phloridzin (an SGLT1 inhibitor).
- Uptake Initiation: Initiate glucose uptake by adding uptake buffer containing a traceable form of glucose (e.g., [³H]-D-glucose or a fluorescent glucose analog) and the test compound. For mechanistic studies, perform parallel assays in sodium-free buffer (e.g., with choline chloride replacing NaCl) to isolate the facilitative GLUT-mediated transport from the sodium-dependent SGLT1-mediated uptake [32].
- Incubation and Termination: Incubate for a short, defined period (e.g., 2-15 minutes) to ensure initial uptake rates are measured. Terminate the uptake by removing the solution and washing the monolayer thoroughly with ice-cold phosphate-buffered saline [32].
- Analysis: Analyze the accumulated radiolabel or fluorescence in the cells using a scintillation counter or plate reader, respectively. Normalize uptake data to the total protein content per well [32]. The apparent permeability coefficient (P_app) can be extrapolated from the passage of the test compound from the donor to the receiver compartment over time [31].
Chronic Treatment and Transporter Expression Analysis
To assess long-term effects of modulators on transporter expression.
- Treatment: Expose differentiated Caco-2/TC7 monolayers to the test compound for 16-24 hours in serum-free culture medium [32].
- Gene Expression Analysis: Isolate total RNA and analyze the expression levels of SGLT1 and GLUT2 mRNA via real-time quantitative PCR (qPCR), using GAPDH as a housekeeping gene [32].
- Protein Expression Analysis: Isolate total protein and evaluate SGLT1 and GLUT2 protein levels by Western blotting, normalizing to a housekeeping protein like actin [32].
Key Research Findings and Data
Research using the Caco-2/TC7 model has yielded significant quantitative data on the effects of various compounds on glucose transport and transporter expression.
Table 1: Effects of Bioactive Compounds on Glucose Uptake and Transporter Expression in Caco-2/TC7 Cells
| Compound/Extract | Concentration | Exposure Time | Effect on Glucose Uptake | Effect on Transporter Expression/Levels | Citation |
|---|---|---|---|---|---|
| Berry Extract (Anthocyanin-rich) | 0.125% (w/v) | 15 minutes (Acute) | ↓ Total uptake by ~40%↓ Facilitated (GLUT) uptake by ~40% | Not assessed (acute) | [32] |
| Berry Extract (Anthocyanin-rich) | 0.125% (w/v) | 16 hours (Chronic) | Not directly measured | ↓ GLUT2 mRNA↓ GLUT2 protein | [32] |
| Posidonia oceanica Leaf Extract (POE) | 15 μg GAE/mL | 24 hours | ↓ Transport (Na+ conditions)↓ Transport (Na+-free conditions) | ↓ GLUT2 protein (to 68% of control)→ SGLT1 protein (no change) | [33] |
| Cyanidin Aglycone | 100 μM | 15 minutes | ↓ Total uptake↓ Facilitated uptake | Not assessed (acute) | [32] |
| Cyanidin-3-glucoside | 100 μM | 15 minutes | ↓ Total uptake↓ Facilitated uptake | Not assessed (acute) | [32] |
Table 2: Key Characteristics and Limitations of the Caco-2/TC7 Model for Glucose Transport Studies
| Aspect | Characteristic/Limitation | Implication for Screening | Citation |
|---|---|---|---|
| Predictive Reliability | Reliable for predicting passive diffusion of compounds. | Excellent for initial screening of passively absorbed modulators. | [31] |
| SGLT1 Function | SGLT1-mediated transport is present but lower than in human enterocytes; lacks sugar-induced apical translocation. | May underestimate the potency of SGLT1-specific inhibitors. | [13] [31] |
| Major Limitations | Not suitable for highly lipophilic compounds, when transporter-mediated routes are involved, or when first-pass metabolism is significant. | Compounds excluded by these criteria may require alternative models for validation. | [31] |
| Barrier Integrity | Forms a tight monolayer with TEER ≥200 Ω·cm² and low paracellular permeability. | Essential to verify before each experiment to ensure valid transport data. | [24] |
The Scientist's Toolkit: Essential Research Reagents
A successful screening campaign requires a set of well-defined reagents and tools.
Table 3: Essential Research Reagent Solutions for Caco-2/TC7 Glucose Uptake Assays
| Reagent/Material | Function/Application | Example & Notes |
|---|---|---|
| Caco-2/TC7 Cells | The intestinal epithelial model system. | TC7 clone provides a homogeneous population with well-developed intercellular junctions [31] [32]. |
| Filter Inserts | Support for polarized cell growth and differentiation, allowing access to apical and basolateral compartments. | Polycarbonate or PET membranes in 6-, 12-, or 24-well formats [24] [34]. |
| DMEM (High Glucose) | Base cell culture medium for maintenance and differentiation. | Typically supplemented with 20% FBS, NEAA, HEPES, and Glutamine [34] [13]. |
| [³H]-D-Glucose / Fluorescent Glucose Analog | Tracer for quantifying glucose uptake. | Fluorescent analogs (e.g., 2-NBDG) are non-radioactive alternatives [35] [36]. |
| Phloridzin / Phloretin | Pharmacological controls for inhibition. | Phloridzin inhibits SGLT1; Phloretin inhibits GLUTs [32]. |
| Sodium-Free Buffer | To isolate facilitative GLUT-mediated transport from total uptake. | NaCl is replaced with equimolar Choline Chloride or N-Methyl-D-glucamine [32]. |
| Antibodies (ZO-1, SGLT1, GLUT2) | For quality control (ZO-1) and mechanistic analysis of transporter expression. | Used in Western blotting and immunofluorescence [33] [24] [32]. |
Visualizing Experimental Workflows and Mechanisms
The following diagrams illustrate the core experimental workflow and the molecular mechanisms targeted during screening.
Glucose Uptake Assay Workflow
Glucose Transport and Modulation Mechanisms
The Caco-2/TC7 cell line, a well-characterized subclone of the human colorectal adenocarcinoma, represents a gold-standard in vitro model for studying intestinal permeability and nutrient transport [31] [28]. When differentiated, these cells exhibit a polarized monolayer with tight junctions, apical brush borders, and functional expression of digestive enzymes and membrane transporters characteristic of human enterocytes [28]. This model is particularly valuable for investigating glucose metabolism, transporter regulation, and the impact of bioactive compounds, providing critical insights for pharmaceutical development and nutritional science.
Advanced functional readouts combining droplet digital PCR (ddPCR), enzyme-linked immunosorbent assay (ELISA), and transport kinetics offer unprecedented resolution in understanding complex biological processes. This integrated approach enables researchers to correlate gene expression changes with protein-level modifications and functional transport outcomes, creating a comprehensive dataset from a single biological model. Within the context of a broader thesis on in vitro glucose uptake assays, these methodologies provide a robust framework for investigating regulation of intestinal glucose transporters and their implications for metabolic health and disease.
Biological Context: Glucose Transporters and Inflammatory Regulation
Intestinal glucose absorption is primarily mediated by the coordinated action of sodium-dependent glucose cotransporter 1 (SGLT1) on the apical membrane and facilitative glucose transporter 2 (GLUT2) on the basolateral membrane [11]. Recent evidence demonstrates that inflammation significantly modulates the expression of these transporters alongside viral entry receptors such as ACE2 and TMPRSS2, suggesting interconnected regulatory pathways [11]. Pro-inflammatory cytokines including interleukin-1 beta (IL-1β) and tumor necrosis factor-alpha (TNF-α) have been shown to upregulate ACE2, TMPRSS2, and SGLT1 gene expression in differentiated Caco-2/TC7 cells [11].
This inflammatory signaling creates a complex network where glucose transporter expression can be altered, potentially contributing to postprandial hyperglycemia—a significant risk factor for type 2 diabetes [11]. Furthermore, the association between TMPRSS2 and SGLT1 gene expression under inflammatory conditions implies a common regulatory mechanism that can be exploited for therapeutic interventions [11]. Phytochemicals such as genistein, apigenin, artemisinin, and sulforaphane have demonstrated potential to modulate these pathways, normalizing inflammation-induced increases in SGLT1 and TMPRSS2 [11].
Table 1: Key Glucose Transporters in Caco-2/TC7 Cells
| Transporter | Type | Location | Primary Function | Regulatory Factors |
|---|---|---|---|---|
| SGLT1 | Sodium-glucose cotransporter | Apical membrane | Active glucose uptake against concentration gradient | Dietary carbohydrates, IL-1β, TNF-α, genistein [11] |
| GLUT2 | Facilitative glucose transporter | Basolateral membrane | Passive glucose efflux into circulation | Glucose concentration, ACE2/Ang-(1-7)/Mas axis [11] |
| GLUT1 | Facilitative glucose transporter | Basolateral membrane | Basal glucose uptake | AMPK, GPCR signaling, cellular stress [37] [38] |
Integrated Methodological Framework
Cell Culture and Differentiation
The Caco-2/TC7 cells require specific culture conditions to ensure proper differentiation and development of intestinal characteristics. Cells should be cultured in high-glucose Dulbecco's Modified Eagle Medium (DMEM) supplemented with 20% (v/v) heat-inactivated fetal bovine serum, 2% (v/v) non-essential amino acids, 2% (v/v) Glutamax, and 1% (v/v) penicillin-streptomycin [11]. For differentiation, seed cells on Transwell plates with polyester filters (0.4 µm pore size) at a density of 0.1 × 10⁵ cells/cm² [11]. Maintain cells at 37°C in a humidified 10% CO₂/90% air atmosphere, with medium changes every 2-3 days. Cellular differentiation occurs over 21-28 days, during which time cells form tight junctions and develop apical microvilli [28].
Monitor differentiation by measuring transepithelial electrical resistance (TEER) using an epithelial voltohmmeter. TEER values should exceed 300 Ω·cm² for reliable monolayer integrity [28]. Validate monolayer integrity further using zero-permeability markers like FITC-dextran or mannitol, with apparent permeability coefficient (Papp) values < 1.0 × 10⁻⁶ cm/s indicating appropriate tight junction formation [28].
Treatment and Inflammation Induction
For inflammation studies, stimulate differentiated Caco-2/TC7 monolayers with pro-inflammatory cytokines interleukin-1 beta (IL-1β) and tumor necrosis factor-alpha (TNF-α) for periods up to 168 hours [11]. Optimal cytokine concentrations typically range from 10-100 ng/mL, though dose-response experiments should be conducted for specific research contexts. To investigate potential therapeutic interventions, co-treat with phytochemicals of interest such as genistein (10-100 µM), apigenin (5-50 µM), artemisinin (1-10 µM), or sulforaphane (1-10 µM) [11]. Include appropriate vehicle controls (e.g., DMSO at concentrations ≤0.1%) for all treatment conditions.
Gene Expression Analysis via ddPCR
ddPCR provides absolute quantification of gene expression with high precision, making it ideal for detecting subtle transcriptional changes in limited sample material.
Protocol:
- RNA Extraction: Extract total RNA from differentiated Caco-2/TC7 monolayers using a commercial kit (e.g., Aurum Total RNA Mini Kit). Include DNase treatment to remove genomic DNA contamination. Quantify RNA purity and concentration using spectrophotometry (A260/A280 ratio ~2.0) [11].
- cDNA Synthesis: Convert 500-1000 ng of total RNA to cDNA using a high-capacity RNA-to-cDNA kit with random primers [11].
- ddPCR Reaction Setup: Prepare 20 µL reactions using ddPCR Supermix for Probes (no dUTP). Use FAM-labeled TaqMan primers for target genes (ACE2, SGLT1, GLUT2, TMPRSS2) and VIC-labeled primers for reference genes (TBP, GAPDH, or β-actin) [11]. Recommended primer/probe sets include:
- ACE2: Hs01085333m1
- SGLT1: Hs01573793m1
- GLUT2: Hs01096908m1
- TMPRSS2: Hs01122322m1
- TBP: Hs00427620_m1 [11]
- Droplet Generation and PCR: Generate droplets using a QX200 Droplet Generator. Perform PCR amplification with the following cycling conditions: 95°C for 10 min (enzyme activation), followed by 40 cycles of 94°C for 30 s (denaturation) and 60°C for 60 s (annealing/extension), with a final 98°C for 10 min (enzyme deactivation) [11].
- Quantification: Analyze plates using a QX200 Droplet Reader and QuantaSoft software. Express results as copies/μL of cDNA or normalize to reference genes for relative expression analysis [11].
Table 2: Key Gene Targets for Glucose Metabolism and Inflammation Studies
| Target Gene | Assay ID | Biological Function | Expected Change with Inflammation |
|---|---|---|---|
| ACE2 | Hs01085333_m1 | Viral receptor, regulates glucose transport via SGLT1/GLUT2 | Upregulated [11] |
| TMPRSS2 | Hs01122322_m1 | Serine protease, viral priming | Upregulated [11] |
| SGLT1 | Hs01573793_m1 | Apimal sodium-glucose cotransporter | Upregulated [11] |
| GLUT2 | Hs01096908_m1 | Basolateral facilitative glucose transporter | Variable regulation [11] |
| GLUT1 | Custom assay | Basal glucose transport | Context-dependent regulation [37] |
| TBP | Hs00427620_m1 | Reference gene (TATA-box binding protein) | Stable [11] |
Protein Quantification via ELISA
ELISA provides sensitive quantification of specific proteins in cell lysates or culture supernatants, complementing gene expression data.
Protocol:
- Sample Collection: Collect cell culture supernatants or prepare cell lysates using RIPA buffer supplemented with protease inhibitors. Centrifuge at 12,000×g for 15 minutes at 4°C to remove debris [11].
- Protein Assay: Determine protein concentration using a colorimetric assay (e.g., Coomassie Plus Bradford assay) with bovine serum albumin standards [11].
- ELISA Procedure: Following manufacturer instructions for specific ELISA kits (e.g., human ACE2 ab235649, human IL-8 ab100575):
- Add 100 μL of standards or samples to appropriate wells.
- Incubate for specified time (typically 2.5 hours) with detection antibody.
- Wash plates thoroughly between incubations.
- Add substrate solution and incubate for 30 minutes in darkness.
- Stop reaction and read absorbance at appropriate wavelength [11].
- Data Analysis: Generate standard curves using reference standards and interpolate sample concentrations. Normalize cell lysate values to total protein concentration.
Glucose Transport Kinetics
Functional glucose transport assays provide critical validation of transcriptional and translational findings.
Protocol:
- Experimental Setup: Differentiate Caco-2/TC7 cells on Transwell filters for 21-28 days until TEER values indicate complete monolayer formation [28].
- Transport Assay: Prepare glucose transport solution containing radiolabeled or fluorescent glucose analogs (e.g., ¹⁴C-glucose or 2-NBDG) in transport buffer (e.g., Hank's Balanced Salt Solution). Add solution to the apical chamber for uptake studies or basolateral chamber for efflux studies [6].
- Sampling: Collect samples from the receiving chamber at predetermined time points (e.g., 15, 30, 60, 90, 120 minutes). Replace with fresh buffer to maintain sink conditions [28].
- Analysis: Quantify transported compound using liquid scintillation counting (for radiolabeled compounds) or fluorescence measurement. Calculate apparent permeability coefficient (Papp) using the formula: Papp = (dQ/dt) × (1/(A × C₀)) where dQ/dt is the transport rate, A is the membrane surface area, and C₀ is the initial donor concentration [28].
- Data Interpretation: Classify compounds according to Papp values: high-permeability (Papp > 10 × 10⁻⁶ cm/s), moderate-permeability (Papp 1-10 × 10⁻⁶ cm/s), and low-permeability (Papp < 1.0 × 10⁻⁶ cm/s) [28].
Integrated Data Analysis and Interpretation
The power of this methodological approach lies in correlating data across transcriptional, translational, and functional levels. For example, inflammation-induced upregulation of SGLT1 mRNA (measured by ddPCR) should correlate with increased SGLT1 protein and enhanced glucose transport kinetics. Similarly, therapeutic interventions with phytochemicals like genistein should demonstrate coordinated downregulation at all three levels [11].
Statistical analysis should include appropriate tests for significance (e.g., ANOVA with post-hoc tests for multiple comparisons) and correlation analyses (e.g., Pearson correlation) to establish relationships between variables. The strong negative correlation between ACE2 and IL-8 (r = -0.77, p < 0.01) exemplifies the important relationships that can be uncovered through this integrated approach [11].
Research Reagent Solutions
Table 3: Essential Research Reagents for Integrated Caco-2/TC7 Studies
| Reagent/Category | Specific Examples | Function/Application | References |
|---|---|---|---|
| Cell Culture | Caco-2/TC7 cells | In vitro intestinal model | [31] [11] |
| High-glucose DMEM | Culture medium | [38] [11] | |
| Transwell filters (0.4 µm) | Cell differentiation support | [11] [28] | |
| Molecular Biology | TaqMan ddPCR assays | Gene expression quantification | [11] |
| RNA extraction kit | Nucleic acid isolation | [11] | |
| Reverse transcription kit | cDNA synthesis | [11] | |
| Protein Analysis | ACE2 ELISA kit | Protein quantification | [11] |
| IL-8 ELISA kit | Cytokine measurement | [11] | |
| RIPA buffer | Cell lysis | [38] [11] | |
| Transport Studies | ¹⁴C-glucose/2-NBDG | Glucose transport tracer | [6] |
| HBSS | Transport buffer | [6] | |
| Treatment Compounds | IL-1β, TNF-α | Inflammation induction | [11] |
| Genistein, Apigenin | Phytochemical interventions | [11] |
Signaling Pathways and Experimental Workflow
The signaling pathways regulating glucose transporter expression in Caco-2/TC7 cells involve complex interactions between inflammatory cytokines, glucose transporters, and viral entry receptors. The following diagrams visualize these pathways and the integrated experimental workflow.
Figure 1: Inflammatory Regulation of Glucose Transporters. This pathway illustrates how pro-inflammatory cytokines modulate glucose transporter expression through NF-κB signaling, and the potential inhibitory effects of phytochemicals [11].
Figure 2: Experimental Workflow. This diagram outlines the sequential steps for conducting integrated studies using Caco-2/TC7 cells, from culture and treatment to multi-modal analysis [11] [28].
The integration of ddPCR, ELISA, and transport kinetics in Caco-2/TC7 models provides a powerful methodological framework for advanced nutrient transport studies. This multi-modal approach enables researchers to establish comprehensive correlations between gene expression, protein translation, and functional outcomes under various physiological and therapeutic conditions. The protocols and analytical frameworks presented here offer a standardized yet flexible foundation for investigating complex questions in intestinal biology, metabolic regulation, and therapeutic development.
Within the scope of a broader thesis on intestinal glucose absorption, this application note provides detailed protocols for using the human colon adenocarcinoma Caco-2/TC7 cell line to investigate the modulation of glucose transport. This model is particularly valuable for studying the interplay between inflammation, glucose transporters, and potential therapeutic agents [19]. Chronic low-grade inflammation, characterized by elevated pro-inflammatory cytokines such as IL-1β and TNF-α, is a hallmark of metabolic disorders like type 2 diabetes and can directly alter the expression of intestinal glucose transporters [19]. This document outlines specific case studies demonstrating how this in vitro system can be employed to evaluate the effects of the phytochemicals genistein and apigenin on inflammation-induced glucose transporter expression.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs key reagents and their critical functions for establishing the Caco-2/TC7 in vitro model and conducting the described assays.
Table 1: Essential Research Reagents and Materials for Caco-2/TC7 Glucose Uptake Studies
| Reagent/Material | Function/Application | Example or Note |
|---|---|---|
| Caco-2/TC7 Cells | Differentiate into enterocyte-like cells; model for human intestinal epithelium [19]. | Forms polarized monolayers with tight junctions. |
| Transwell Plates | Culture cells on permeable supports to create apical (AP) & basolateral (BL) compartments [19]. | Enables study of polarized transport. |
| Pro-inflammatory Cytokines (IL-1β, TNF-α) | Induce a chronic inflammatory state to study its effect on transporter expression [19]. | Used at 1-10 ng/mL for ≤168 hours [19]. |
| Phytochemicals (Genistein, Apigenin) | Investigated for potential to normalize inflammation-induced changes in transporter expression [19]. | Genistein (soy isoflavone), Apigenin (found in vegetables). |
| Droplet Digital PCR (ddPCR) | Precisely quantify target gene expression (e.g., ACE2, TMPRSS2, SGLT1, GLUT2) [19]. | Offers high precision for absolute quantification. |
| ELISA Kits | Measure protein levels of cytokines (e.g., IL-8) or targets (e.g., ACE2) [19]. | Abcam kits for human ACE2 and IL-8 [19]. |
| GLUT1 Inhibitor (STF-31) | Pharmacological tool to investigate GLUT1 involvement in substrate uptake [39]. | Validates transporter-specific mechanisms. |
| Cell Culture Medium (DMEM, high glucose) | Standard medium for cell growth and maintenance [19]. | Typically supplemented with FBS, NEAA, and Glutamax [19]. |
Case Study: Investigating Genistein and Apigenin in an Inflammatory Model
Background and Rationale
Inflammation can significantly disrupt intestinal glucose homeostasis. Studies show that treatment of Caco-2/TC7 cells with IL-1β and TNF-α upregulates the gene expression of ACE2, TMPRSS2, and the sodium-dependent glucose transporter SGLT1 [19]. This upregulation may contribute to postprandial hyperglycaemia, a key risk factor for type 2 diabetes [19] [5]. Furthermore, a strong association between the regulation of SGLT1 and TMPRSS2 gene expression has been observed, suggesting a common regulatory pathway during inflammation [19]. Dietary phytochemicals like genistein and apigenin have demonstrated anti-inflammatory and glucose-lowering properties in various tissues, but their precise effects on inflamed intestinal epithelium are less clear [19]. This case study details a protocol to assess their potential to normalize these inflammation-induced changes.
Experimental Workflow and Signaling Pathways
The following diagram illustrates the core experimental workflow and the key molecular pathways investigated in this case study.
Detailed Experimental Protocol
Cell Culture and Differentiation
- Culture Maintenance: Grow Caco-2/TC7 cells in 75 cm² flasks with complete high-glucose (25 mM) DMEM, supplemented with 20% (v/v) heat-inactivated FBS, 1% NEAA, 1% Glutamax, and 1% penicillin-streptomycin. Maintain at 37°C in a 10% CO₂ atmosphere. Use cell passages between 32 and 40 [19].
- Differentiation on Transwells: Seed cells onto the apical chamber of 6- or 12-well Transwell plates (0.4 µm pore polyester filters) at a density of 0.1 × 10⁵ cells/cm². Culture with complete medium in both apical and basolateral chambers until 100% confluence (designated Day 0). On day 7 post-confluence, replace the apical compartment medium with FBS-free medium. Continue differentiation for a total of 14-21 days, changing the medium three times per week [19].
Inflammation Induction and Phytochemical Treatment
- Inflammation Model: Differentiated Caco-2/TC7 monolayers are stimulated with a combination of human IL-1β and TNF-α (typically at concentrations of 1-10 ng/mL each) added to the culture medium. The cytokine treatment can be applied for up to 168 hours to model chronic inflammation [19].
- Phytochemical Intervention: Co-treat the inflamed cells with the phytochemicals of interest. In the referenced study, genistein, apigenin, artemisinin, and sulforaphane were identified as promising candidates. These compounds are typically dissolved in DMSO (final concentration ≤0.1%) and applied concurrently with the cytokines for the duration of the experiment [19].
Downstream Analysis and Data Collection
- Gene Expression Analysis (ddPCR): Harvest cells and extract total RNA using a kit (e.g., Aurum Total RNA Mini Kit). Convert RNA to cDNA using a high-capacity RNA-to-cDNA kit. Perform droplet digital PCR using FAM- or VIC-labeled TaqMan primers for target genes (e.g., ACE2, TMPRSS2, SGLT1, GLUT2) and a housekeeping gene (e.g., TBP). This provides absolute quantification of transcript copy numbers [19].
- Protein Quantification (ELISA): Collect cell culture supernatants or cell lysates. Use commercial ELISA kits (e.g., for human IL-8 or ACE2) according to the manufacturer's instructions to measure secreted or cellular protein levels [19].
- Data Interpretation: Analyze the data to determine if phytochemical treatment normalizes the inflammation-induced upregulation of SGLT1 and TMPRSS2 gene expression. For example, genistein was found to significantly downregulate the inflammation-induced increase in both SGLT1 and TMPRSS2 [19].
Key Quantitative Findings
The table below summarizes exemplary quantitative data from experiments investigating the effects of inflammation and phytochemicals on gene expression in Caco-2/TC7 cells.
Table 2: Exemplary Data from Caco-2/TC7 Studies on Inflammation and Phytochemical Effects
| Experimental Condition | Target | Observed Change | Biological Significance |
|---|---|---|---|
| IL-1β + TNF-α | ACE2 Gene Expression | Upregulated [19] | Links inflammation to glucose metabolism & SARS-CoV-2 entry. |
| IL-1β + TNF-α | TMPRSS2 Gene Expression | Upregulated [19] | Suggests common regulation with SGLT1 during inflammation. |
| IL-1β + TNF-α | SGLT1 Gene Expression | Upregulated [19] | May increase intestinal glucose absorption, contributing to hyperglycaemia. |
| Genistein in Inflamed Cells | SGLT1 & TMPRSS2 Expression | Downregulated (normalized) [19] | May lower postprandial glycaemic response and COVID-19 risk. |
| Correlation in Inflamed Cells | ACE2 increase vs. IL-8 decrease | Strong Negative (r = -0.77) [19] | Suggests a novel inverse relationship between anti-inflammatory response and ACE2. |
Advanced Technical Notes
Investigating Transporter-Mediated Uptake Mechanisms
For studies focusing on the direct uptake of compounds rather than transporter expression, a modified approach is required. The following diagram outlines a general workflow for investigating transporter-mediated uptake, for instance, via GLUT1.
Key Methodological Steps:
- Inhibitor/Knockdown Studies: To confirm the involvement of a specific transporter like GLUT1, pre-treat cells with a pharmacological inhibitor (e.g., STF-31) or use siRNA to knock down the transporter gene. A significant reduction in uptake or transport in treated groups confirms the transporter's role [39].
- Uptake and Transport Assays: After applying the test compound (e.g., resveratrol, 6AzGal), measure both the amount accumulated inside the cells (uptake) and the amount passed through the monolayer to the opposite chamber (transport). This should be done bidirectionally (AP→BL and BL→AP) to identify active transport processes [39].
- Temperature Dependence: Conduct uptake/transport assays at both 37°C and 4°C. A significant reduction at 4°C indicates an energy-dependent, transporter-mediated process, as low temperature affects membrane fluidity and active transport [39].
- Apparent Permeability (Papp): Calculate the Papp value using the formula:
Papp = (dQ/dt) / (A × C₀), wheredQ/dtis the transport rate,Ais the membrane surface area, andC₀is the initial donor concentration. A higher Papp value in the BL→AP direction than AP→BL suggests active efflux [39].
The Caco-2/TC7 cell model is a robust and well-characterized in vitro system for investigating the complex relationships between intestinal inflammation, glucose transporter dynamics, and potential therapeutic interventions. The case studies and protocols detailed herein provide a framework for researchers to reliably assess the efficacy of phytochemicals like genistein and apigenin in modulating glucose absorption under inflammatory conditions. The application of ddPCR, ELISA, and specific pharmacological inhibitors allows for a comprehensive, mechanistic understanding of compound effects, contributing valuable data for drug development and nutritional science focused on metabolic diseases.
Troubleshooting and Optimization: Ensuring Assay Reproducibility and Accuracy
Critical Pitfalls in Cell Differentiation and Achieving Tight Junction Integrity
Within the context of in vitro glucose uptake assays using Caco-2/TC7 cell lines, the integrity of the intestinal epithelial barrier model is paramount. The functional assessment of glucose transport and the screening of potential modulators rely exclusively on the proper formation of a differentiated cell monolayer with robust tight junctions (TJs). These dynamic, multi-protein complexes regulate paracellular permeability and are critical for maintaining the polarity of nutrient transporters, such as SGLT1 and GLUT2 [40] [33]. This Application Note details the predominant pitfalls encountered during cell differentiation and TJ formation and provides validated protocols to overcome these challenges, thereby ensuring the generation of reliable and physiologically relevant data for drug development research.
Major Pitfalls and Quantitative Impact on Barrier Integrity
The following table summarizes the key critical pitfalls, their consequences on the model system, and quantitative data on their impact from published studies.
Table 1: Critical Pitfalls in Caco-2/TC7 Model Development and Their Impact on Barrier Integrity
| Pitfall Category | Specific Challenge | Impact on Model & Key Quantitative Findings |
|---|---|---|
| Differentiation Timeline | Standard 21-day protocol is labor-intensive and high-cost [12]. | Increased contamination risk, low throughput, and significant resource commitment without guaranteeing quality. |
| Accelerated Model Integrity | Use of leaky, abbreviated (e.g., 3-day) models with improper optimization [12]. | Low TEER values (~250 Ω·cm² in suboptimal models) and compromised TJ protein expression compared to robust 21-day monolayers [12]. |
| Culture Medium Composition | Suboptimal serum conditions and lack of differentiation-promoting agents [12]. | Serum starvation can aid barrier formation, but requires precise control. Sodium valerate significantly increases TEER (from ~250 to >300 Ω·cm²) and promotes transporter expression [12]. |
| Tight Junction Protein Regulation | Inadequate understanding of molecular mechanisms for de novo TJ formation and repair [41] [42]. | Failure to rapidly form new TJs during cell turnover, leading to barrier breaches. Rho-ROCK pathway activation is crucial for supplying polymerizable claudin via EpCAM/TROP2 cleavage [41] [42]. |
| Oxidative Stress | Exposure to high glucose concentrations or pro-oxidants [33]. | Induces oxidative stress, increasing intracellular ROS (e.g., ~2.0 A.U. vs. ~1.0 A.U. in controls) and decreasing cell viability by ~40%, thereby disrupting barrier function [33]. |
Detailed Experimental Protocols
Protocol 1: Establishing a High-Integrity, Abbreviated 3-Day Caco-2 Model
This protocol, adapted from Rehman et al., uses sodium valerate to induce rapid differentiation and enhance tight junction integrity [12].
3.1.1 Reagents and Materials
- Caco-2 or Caco-2/TC7 cells
- Dulbecco's Modified Eagle's Medium (DMEM)
- Fetal Bovine Serum (FBS)
- Insulin-Transferrin-Selenium (ITS) supplement
- Sodium valerate (VA)
- Hanks' Balanced Salt Solution (HBSS)
- HEPES buffer
- Transwell permeable supports (e.g., 12-well, 1.12 cm² surface area, 0.4 µm pore size)
- Triton X-100
3.1.2 Procedure
- Cell Seeding: Seed Caco-2 cells onto Transwell inserts at a high density of (1.5 \times 10^5) cells/cm².
- Initial Attachment Medium: Culture the cells for 24 hours in DMEM supplemented with 5% FBS and 1% ITS.
- Differentiation Induction: After 24 hours, replace the medium with a differentiation-inducing medium composed of DMEM supplemented with 1% FBS, 1% ITS, and 5 mM sodium valerate.
- Monitoring: Culture the cells for an additional 48 hours (3 days total). Monitor Transepithelial Electrical Resistance (TEER) daily.
- Validation: Validate monolayer integrity via TEER measurement and paracellular marker flux (e.g., Lucifer Yellow) before initiating glucose uptake assays. A TEER value >300 Ω·cm² indicates acceptable integrity [12].
3.1.3 Quality Control
- TEER Measurement: Measure TEER using an epithelial voltohmmeter. Calculate the net resistance by subtracting the value of a blank insert and multiplying by the membrane surface area.
- Paracellular Flux Assay: Apically add a non-absorbable marker like Lucifer Yellow (100 µM). Sample from the basolateral chamber over 1-2 hours and quantify fluorescence to ensure minimal leakage.
Protocol 2: Assessing Glucose Transporter Activity via a Novel Post-Click Labeling Method
This protocol leverages a click chemistry-based approach for highly accurate, single-cell resolution measurement of GLUT-mediated glucose uptake, overcoming limitations of traditional fluorescent analogs like 2NBDG [43].
3.2.1 Reagents and Materials
- 6-azido-6-deoxy-D-galactose (6AzGal)
- BDP-DBCO fluorescent dye (cell-permeable, copper-free)
- Cytochalasin B (GLUT inhibitor)
- D-Glucose
- Phosphate Buffered Saline (PBS)
- Flow cytometry staining buffer
3.2.2 Procedure
- Azido-Sugar Uptake: Wash differentiated Caco-2 monolayers with PBS. Incubate cells with 100 µM 6AzGal in HBSS/HEPES buffer for 30 minutes at 37°C.
- Inhibition Control: Include control wells pre-treated with 50 µM Cytochalasin B for 20 minutes prior to and during 6AzGal incubation.
- Click Labeling: After incubation, wash cells thoroughly to remove extracellular 6AzGal. Incubate with 5 µM BDP-DBCO in PBS for 30 minutes at room temperature, protected from light.
- Analysis: Wash cells to remove unbound dye. Analyze fluorescence intensity via flow cytometry or confocal microscopy. Co-staining with surface markers allows for immunophenotyping.
- Validation: Confirm GLUT-specific uptake by effective competition with excess D-glucose and inhibition by Cytochalasin B, which should reduce signal by >70% [43].
Protocol 3: Tight Junction Reinforcement with Micronutrients
This protocol outlines the application of TJ-enhancing micronutrients, which can be used to fortify the barrier prior to glucose uptake assays or to test the protective effects of novel compounds [44].
3.2.1 Reagents and Materials
- Sodium butyrate
- Berberine
- Quercetin
- Zinc sulfate
- Indole
- (^{14})C-D-mannitol or Fluorescein isothiocyanate (FITC)-dextran
3.2.2 Procedure
- Treatment: Apply the micronutrient to both the apical and basolateral compartments of differentiated Caco-2 monolayers. Example concentrations for a 48-hour treatment are:
- Sodium butyrate: 2-5 mM
- Berberine: 50-150 µM
- Quercetin: 50-200 µM
- Zinc: 50-100 µM
- TEER Monitoring: Measure TEER at 24 and 48 hours post-treatment. Expect an increase of up to 200% of control values for effective agents like berberine [44].
- Permeability Assessment: After TEER measurement, perform a paracellular flux assay using (^{14})C-D-mannitol or FITC-dextran to confirm functional improvement in barrier tightness.
Molecular Pathways and Workflows
Signaling Pathway for Rapid De Novo Tight Junction Formation
The following diagram illustrates the molecular mechanism that supplies claudin for the rapid formation of new tight junctions, a critical process for maintaining barrier integrity during cell turnover.
Experimental Workflow for Glucose Uptake and Barrier Assessment
This workflow integrates the culture, validation, and application of the Caco-2 model for a comprehensive glucose uptake study.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Differentiating and Assessing Caco-2/TC7 Monolayers
| Reagent | Function/Application in Model | Key Consideration |
|---|---|---|
| Sodium Valerate (VA) | Safe, effective differentiation-promoting agent for accelerated (3-day) models. Enhances TEER and transporter expression [12]. | Superior safety profile compared to sodium butyrate; use at 5 mM. |
| Insulin-Transferrin-Selenium (ITS) | Serum replacement supplement that enhances initial cell attachment and monolayer integrity in abbreviated models [12]. | Optimal concentration is 1% for seeding and differentiation phases. |
| 6AzGal & BDP-DBCO | Click chemistry pair for highly accurate, single-cell analysis of GLUT-mediated glucose uptake with low background [43]. | Superior to 2NBDG; requires flow cytometer or confocal microscope for detection. |
| Sodium Butyrate / Berberine | Micronutrients for reinforcing existing TJs and increasing TEER; useful for protective/intervention studies [44]. | Butyrate may induce cytotoxicity at high doses; Berberine also reduces mannitol flux. |
| Cytochalasin B | Potent endofacial inhibitor of GLUTs. Essential as a control to confirm GLUT-specific activity in uptake assays [43]. | Validates specificity of glucose uptake probes; expect >70% signal reduction. |
| Lucifer Yellow (LY) | Fluorescent paracellular tracer for quantitatively assessing tight junction integrity and monolayer leakiness [12]. | Standard for measuring permeability; use a low molecular weight, non-absorbable marker. |
Optimizing Pro-Inflammatory Cytokine Treatment (IL-1β, TNF-α) for Inflammation Models
The use of pro-inflammatory cytokines, particularly Interleukin-1β (IL-1β) and Tumor Necrosis Factor-α (TNF-α), is fundamental for establishing reliable in vitro inflammation models using human intestinal Caco-2/TC7 cell lines. These models are crucial for investigating the interplay between inflammation, intestinal glucose absorption, and the potential therapeutic effects of novel compounds [11]. IL-1β and TNF-α are master pro-inflammatory cytokines primarily produced by activated macrophages and are key players in orchestrating the inflammatory cascade in chronic diseases, including metabolic disorders [45] [46] [47]. In the context of Caco-2/TC7 research, which is a well-established model for a homogenous population of human enterocytes, these cytokines are used to mimic a low-grade inflammatory environment. This simulated inflammation has been shown to significantly upregulate the expression of key genes, including intestinal glucose transporters (SGLT1, GLUT2) and SARS-CoV-2 viral entry receptors (ACE2, TMPRSS2), thereby providing a robust platform for studying metabolic and infectious disease pathophysiology [11].
Cytokine Treatment Optimization Parameters
Optimizing cytokine treatment involves careful consideration of concentration, exposure time, and the synergistic effects of cytokine combinations to ensure a physiologically relevant and reproducible inflammatory response.
Cytokine Concentrations and Exposure Times
The following table summarizes key parameters for inducing inflammation in Caco-2/TC7 cell models, as supported by recent literature.
Table 1: Optimized Cytokine Treatment Parameters for Caco-2/TC7 Inflammation Models
| Cytokine | Effective Concentration | Treatment Duration | Key Cellular Effects | Source Model |
|---|---|---|---|---|
| IL-1β & TNF-α (Combination) | 10 ng/mL each | 24 - 168 hours (up to 7 days) | Significant upregulation of ACE2, TMPRSS2, and SGLT1 gene expression. ACE2 increase is duration-dependent. [11] | Differentiated Caco-2/TC7 monolayers [11] |
| IL-1β | 10 ng/mL | 24 hours | Used in combination with TNF-α to stimulate IL-6 and IL-8 secretion and activate NF-κB signaling pathways. [11] | Differentiated Caco-2/TC7 monolayers [11] |
| TNF-α | 10 ng/mL | 24 hours | Used in combination with IL-1β. A key orchestrator of the pro-inflammatory cytokine cascade. [47] [11] | Differentiated Caco-2/TC7 monolayers [11] |
Rationale for Combination Therapy
Using IL-1β and TNF-α in combination is a strategic approach to induce a robust and synergistic inflammatory response. Scientific evidence shows that a pro-inflammatory cytokine overexpression leads to a state of "metabolic infection" and systemic inflammation [45]. These cytokines are generated in a cascade manner, with one cytokine stimulating the further release of others, creating a redundant pro-inflammatory action [45]. Furthermore, a synergistic interaction between IL-1β and TNF-α in regulating IL-6 expression has been demonstrated in other cell types, and this alliance is likely a key contributor to the high inflammatory burden observed in vitro and in vivo [45]. This combination effectively activates the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) pathway, a primary signaling route leading to the expression of a broad set of genes involved in inflammation [46] [11].
Detailed Experimental Protocol for Cytokine-Induced Inflammation in Caco-2/TC7 Cells
Pre-Treatment: Cell Culture and Differentiation
Objective: To establish a fully differentiated monolayer of Caco-2/TC7 cells that mimics the human intestinal epithelium. Materials:
- Caco-2/TC7 cells (passages 32-40) [11]
- Complete Dulbecco's Modified Eagle Medium (DMEM) with high glucose (4.5 g/L or 25 mM), supplemented with 20% (v/v) heat-inactivated Fetal Bovine Serum (FBS), 2% (v/v) Non-Essential Amino Acids (NEAAs), 2% (v/v) Glutamax, and 1% (v/v) penicillin-streptomycin [11]
- Tissue culture flasks and Transwell plates (e.g., 12-well format, polyester filters, 0.4 µm pore size) [11]
- Humidified incubator at 37°C with 10% CO₂ [11]
Method:
- Maintenance: Culture Caco-2/TC7 cells in 75 cm² flasks until ~60% confluence. Sub-culture using a 0.25% (v/v) trypsin-EDTA solution [11].
- Seeding for Differentiation: Seed cells onto the apical chamber of Transwell plates at a density of 0.1 × 10⁵ cells/cm² in complete DMEM with 20% FBS in both apical and basolateral compartments [11].
- Monitoring: Examine cells daily until they reach 100% confluence. Mark this day as Day 0 of differentiation.
- Differentiation Period: Continue culturing the cells for at least 21 days to allow for full differentiation and polarization, with media changes three times per week. From day 7 onwards, the apical compartment can be switched to FBS-free medium, while the basolateral side receives medium with 10-20% FBS [11].
- Validation: Confirm monolayer integrity by measuring Trans-Epithelial Electrical Resistance (TEER) prior to experimentation.
Cytokine Treatment Phase
Objective: To induce a consistent and reproducible state of inflammation in the differentiated Caco-2/TC7 monolayers. Materials:
- Recombinant human IL-1β protein [11]
- Recombinant human TNF-α protein [11]
- Serum-free DMEM (or appropriate treatment medium)
Method:
- Preparation of Cytokine Stock Solutions: Reconstitute lyophilized cytokines according to the manufacturer's instructions to create concentrated stock solutions. Prepare aliquots to avoid freeze-thaw cycles.
- Working Solution Preparation: Dilute the cytokine stocks in serum-free DMEM to create a 2X working solution with a final desired concentration of 10 ng/mL for each cytokine (IL-1β and TNF-α) [11].
- Treatment Application:
- Carefully aspirate the medium from both the apical and basolateral compartments.
- Add the prepared cytokine working solution to the basolateral compartment. Add an equal volume of fresh serum-free DMEM to the apical compartment to maintain osmotic balance.
- For control groups, treat with serum-free DMEM containing the same volume of cytokine diluent (e.g., PBS with BSA).
- Incubation: Return the Transwell plates to the incubator (37°C, 10% CO₂) for the desired treatment period (e.g., 24 hours for acute studies, or up to 168 hours for chronic exposure models) [11].
- Post-Treatment Sample Collection:
- Gene Expression Analysis: After incubation, wash the cell monolayers with cold PBS and lysate the cells directly on the Transwell membrane for RNA extraction using a kit such as the Aurum Total RNA Mini Kit. Subsequent gene expression analysis for targets like ACE2, TMPRSS2, SGLT1, and GLUT2 can be performed via droplet digital PCR (ddPCR) using TaqMan primers [11].
- Protein Secretion Analysis: Collect conditioned media from the basolateral compartment. Analyze the secretion of inflammatory markers like IL-8 and IL-6 using multiplex ELISA kits [11].
- Functional Assays: The inflamed monolayers are now ready for downstream functional assays, such as glucose uptake studies.
Signaling Pathways and Experimental Workflow
The following diagrams illustrate the core signaling pathway activated by the cytokine treatment and the sequential workflow of the protocol.
Diagram 1: Inflammatory signaling pathway activated by IL-1β and TNF-α cytokine treatment, showing the downstream gene expression changes relevant to Caco-2/TC7 research.
Diagram 2: Step-by-step experimental workflow for establishing a cytokine-induced inflammation model using differentiated Caco-2/TC7 cell monolayers.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table lists essential reagents and their specific functions for successfully implementing this inflammation model.
Table 2: Essential Reagents for Cytokine Treatment in Caco-2/TC7 Models
| Reagent / Kit | Specific Function / Application | Example Product / Citation |
|---|---|---|
| Recombinant Human IL-1β | Induction of pro-inflammatory signaling; used in combination with TNF-α. | Merck Life Science [11] |
| Recombinant Human TNF-α | Induction of pro-inflammatory signaling; used in combination with IL-1β. | Merck Life Science [11] |
| Caco-2/TC7 Cell Line | Human intestinal epithelial cell model that forms homogeneous, differentiated enterocyte monolayers. | Rousset Lab (U178 INSERM, Villejuif, France) [11] |
| Droplet Digital PCR (ddPCR) | Absolute quantification of gene expression changes (e.g., ACE2, TMPRSS2, SGLT1, GLUT2). | Bio-Rad QX200 System; TaqMan primers (Thermo Fisher) [11] |
| Multiplex ELISA Kits | Quantification of secreted inflammatory markers (e.g., IL-6, IL-8) in conditioned media. | EMD Millipore IL-6/IL-8 panel; Abcam IL-8 kit [11] |
| RNA Extraction Kit | High-quality total RNA isolation from differentiated Caco-2/TC7 monolayers. | Bio-Rad Aurum Total RNA Mini Kit [11] |
| Transwell Plates | Physical support for growing polarized, differentiated intestinal cell monolayers. | Polyester filter, 0.4 µm pore size (e.g., Falcon, Corning) [11] |
The Caco-2/TC7 cell line, a clonal derivative of the human colorectal adenocarcinoma Caco-2 cell line, has emerged as a premier in vitro model for studying intestinal glucose absorption and nutrient transport. These cells spontaneously differentiate under standard culture conditions to exhibit a polarized enterocyte-like phenotype with well-developed brush border enzymes and intercellular junctions, closely mimicking the human small intestinal epithelium. Within the context of glucose uptake assays, standardization of culture parameters is paramount for generating reproducible, physiologically relevant data. This Application Note addresses two critical sources of experimental variability: passage number effects and culture medium composition, providing validated protocols to enhance research reliability in drug development and nutritional science.
Key Experimental Parameters and Their Standardization
Passage Number and Cell Culture History
The passage number of Caco-2/TC7 cells significantly influences their differentiation capacity and transporter expression profile. Consistent passage practices are essential for experimental reproducibility.
Table 1: Standardized Passage Parameters for Caco-2/TC7 Cells
| Parameter | Specification | Rationale & Reference |
|---|---|---|
| Recommended Passage Range | Passages 32–40 [10] [11] [19] | Ensures a homogeneous cell population with stable, representative intestinal enterocyte functions. |
| Seeding Density for Maintenance | 0.2 × 10⁵ cells/cm² [10] [11] | Prevents overcrowding and maintains consistent growth rates between passages. |
| Sub-culturing Confluence | ~60% confluence [11] [19] | Avoids over-confluence, which can trigger premature differentiation and phenotypic drift. |
| Dissociation Reagent | 0.25% (v/v) trypsin-EDTA solution [10] [11] | Standardizes the process of cell detachment for sub-culturing. |
Culture Medium Composition and Differentiation Protocol
The composition of the culture medium, particularly during the post-confluence differentiation phase, directly modulates the development of the mature enterocyte phenotype, including the expression of glucose transporters like SGLT1 and GLUT2.
Table 2: Standardized Culture Medium Formulation for Differentiation
| Component | Proliferation Phase (Pre-confluence) | Differentiation Phase (Post-confluence) | Function |
|---|---|---|---|
| Basal Medium | Dulbecco's Modified Eagle Medium (DMEM) [10] [11] [27] | Dulbecco's Modified Eagle Medium (DMEM) [10] [11] [27] | Provides essential nutrients and vitamins. |
| Glucose Concentration | 4.5 g/L (25 mM) - "High Glucose" [10] [11] [27] | 5.5 mM or 25 mM (context-dependent) [10] | Energy source; concentration can be adjusted experimentally to mimic different conditions. |
| Fetal Bovine Serum (FBS) | 20% (v/v) [10] [11] [19] | Apical: FBS-free after day 7 [10] [19]. Basolateral: 10-20% (v/v) [10] [19] | Provides growth factors and hormones essential for differentiation. Removing apical FBS promotes polarization. |
| Non-Essential Amino Acids (NEAAs) | 1-2% (v/v) [10] [11] | 1-2% (v/v) [10] [11] | Improves cell viability and growth in rapidly dividing cells. |
| Glutamine Supplement | 2% (v/v) GlutaMAX [10] [11] | 2% (v/v) GlutaMAX [10] [11] | Stable dipeptide source of L-Glutamine, crucial for energy metabolism. |
| Antibiotics | 1% (v/v) Penicillin-Streptomycin [10] [11] | 1% (v/v) Penicillin-Streptomycin [10] [11] | Prevents bacterial contamination. |
| Atmosphere | 10% CO₂ / 90% air [10] [11] [19] | 10% CO₂ / 90% air [10] [11] [19] | Maintains physiological pH. |
Detailed Experimental Protocols
Protocol 1: Seeding and Differentiation of Caco-2/TC7 Monolayers
This protocol outlines the process for establishing differentiated, polarized cell monolayers on semi-permeable filters, which are critical for vectorial transport studies like glucose uptake assays.
Workflow Title: Caco-2/TC7 Seeding & Differentiation (47 chars)
Procedure:
- Seeding: Seed Caco-2/TC7 cells (passages 32-40) onto the apical chamber of Transwell plates (e.g., polyester filters, 0.4 µm pore size) at a density of 0.1 × 10⁵ cells/cm² in complete DMEM (25 mM glucose) supplemented with 20% (v/v) FBS in both the apical and basolateral compartments [10] [11].
- Initial Differentiation (Days 0-7): Monitor cells daily until they reach 100% confluence, designated as Day 0. Continue culturing the cells in the same complete medium (with 20% FBS on both sides) for the first 7 days post-confluence, changing the medium three times per week [10] [19].
- Advanced Differentiation (Days 7-21): From day 7 onwards, replace the apical compartment medium with FBS-free DMEM. The basolateral compartment should continue to receive complete DMEM containing 10% or 20% (v/v) FBS [10] [19]. Maintain this configuration with regular medium changes three times a week until the monolayers are fully differentiated, typically by day 21 [10].
- Pre-assay Conditioning: For specific experimental setups, such as glucose transport assays, a final conditioning step may be applied. For example, 24 hours before the experiment, both compartments can be switched to FBS-free, low-glucose (5.5 mM) DMEM [10].
Protocol 2: Assessing Impact of Culture Conditions on Gene Expression
This protocol describes how to treat differentiated Caco-2/TC7 monolayers with experimental compounds and subsequently analyze gene expression of key targets like glucose transporters and viral entry receptors.
Workflow Title: Treatment & Gene Expression Analysis (48 chars)
Procedure:
- Treatment: On day 19 or 20 of differentiation, treat the differentiated Caco-2/TC7 monolayers with the test compound (e.g., dexamethasone, pro-inflammatory cytokines like IL-1β and TNF-α, or phytochemicals like genistein). For soluble compounds, prepare them in FBS-free DMEM. Include vehicle control groups (e.g., 0.1% DMSO) [10] [11].
- Incubation: Incubate the cells with the treatment for the desired duration. For instance, studies have treated cells with dexamethasone (5-20 µM) twice daily for a total of 60 hours [10], or with a cytokine mix (e.g., IL-1β and TNF-α) for up to 168 hours to model chronic inflammation [11] [19].
- RNA Extraction: At the end of the treatment period, extract total RNA from the cell monolayers using a commercial mini kit (e.g., Aurum Total RNA Mini Kit) [11] [19].
- cDNA Synthesis: Reverse transcribe the purified RNA into complementary DNA (cDNA) using a high-capacity RNA-to-cDNA kit [10] [11].
- Gene Expression Analysis: Quantify the expression of genes of interest (e.g., SGLT1, GLUT2, ACE2, TMPRSS2) using highly sensitive methods such as droplet digital PCR (ddPCR) or quantitative real-time PCR (qPCR) with specific TaqMan probes [10] [11] [19]. Normalize expression data to a housekeeping gene like TATA-box binding protein (TBP).
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Caco-2/TC7 Glucose Uptake Research
| Reagent / Kit | Function / Application | Specific Example |
|---|---|---|
| Caco-2/TC7 Cell Line | In vitro model of the human intestinal epithelium. | Clone derived from parental Caco-2 cells, forms a homogeneous enterocyte population [11] [31]. |
| Transwell Plates | Semi-permeable supports for culturing polarized cell monolayers for transport studies. | Polyester filters, 0.4 µm pore size, various diameters (e.g., 12 mm, 24 mm) [10] [11]. |
| Droplet Digital PCR (ddPCR) | Absolute quantification of gene expression with high precision. | Bio-Rad QX200 system with specific TaqMan probes for SGLT1 (Hs01573793_m1), etc. [10] [11]. |
| ELISA Kits | Quantification of protein secretion or expression. | Human ACE2, IL-8, IL-6 ELISA kits for validating gene expression data at the protein level [11] [19]. |
| Pro-inflammatory Cytokines | To induce an in vitro model of intestinal inflammation. | Human IL-1β and TNF-α proteins [11] [19]. |
| Dexamethasone | Synthetic glucocorticoid used to study steroid-induced effects on glucose transport and viral receptor expression [10]. | Prepared from a 20 mM stock in DMSO, used at 5-20 µM [10]. |
| Phytochemicals | Natural compounds to study modulation of glucose transport and inflammation. | Genistein, Apigenin, Sulforaphane (from Merck Life Science) [11] [19]. |
Concluding Remarks
Meticulous attention to passage number and culture medium composition is non-negotiable for achieving reliable and interpretable results in Caco-2/TC7-based glucose uptake assays. Adherence to the standardized protocols outlined in this document will significantly reduce experimental variability, thereby enhancing the predictive power of this robust in vitro model for intestinal research. This standardization is fundamental for accurate investigations into nutrient transport, drug absorption, and the complex interplay between metabolism and inflammation in the human gut.
Validating Transporter-Specific Inhibition with Pharmacological Agents (Phlorizin, Cytochalasin B)
Within the framework of in vitro glucose uptake assays using the human intestinal Caco-2/TC7 cell model, the precise identification of transport pathways is fundamental for investigating nutrient absorption, drug permeability, and the mechanisms of action for potential therapeutic compounds. This application note provides a detailed protocol for the pharmacological validation of the key intestinal glucose transporters, SGLT1 (Sodium-dependent Glucose Cotransporter 1) and GLUT2 (Glucose Transporter 2), using the specific inhibitors phlorizin and cytochalasin B, respectively. The Caco-2/TC7 cell line, a well-established model of the human intestinal epithelium, expresses these critical transporters upon differentiation, making it an ideal system for such investigations [10] [11]. The use of these inhibitors allows researchers to dissect the relative contributions of active, sodium-coupled transport versus facilitative diffusion to the overall glucose absorption process, a crucial distinction in metabolic and pharmacological studies [48].
Experimental Design and Principles
The experimental design capitalizes on the distinct mechanisms of action and specificities of two pharmacological agents.
- Phlorizin is a competitive and high-affinity inhibitor of SGLT1. It acts by binding to the external glucose-binding site of the transporter, thereby blocking the active, sodium-dependent uptake of glucose from the intestinal lumen into the enterocyte [48].
- Cytochalasin B is a potent inhibitor of facilitative glucose transporters (GLUTs), including GLUT2. It binds to the inner surface of the transporter, preventing the conformational changes required for the facilitative diffusion of glucose across the plasma membrane [48].
By applying these inhibitors individually and in combination during glucose uptake assays, the specific transport activity mediated by SGLT1, GLUT2, and non-specific diffusion can be quantitatively resolved. The typical workflow for this validation is outlined in the diagram below.
Key Reagents and Materials
The following table details the essential research reagent solutions required for the successful execution of this protocol.
Table 1: Research Reagent Solutions for Transporter Inhibition Studies
| Reagent / Material | Function / Role in the Protocol | Key Specifications / Notes |
|---|---|---|
| Caco-2/TC7 Cells | Differentiated human intestinal epithelial cell model. | Forms polarized monolayers with apical brush border and functional expression of SGLT1 and GLUT2 [10] [11]. |
| Phlorizin | Specific, competitive inhibitor of SGLT1. | Used at a final concentration of 10 μM to block sodium-dependent glucose co-transport [48]. |
| Cytochalasin B | Potent inhibitor of facilitative GLUT transporters (GLUT2). | Used at a final concentration of 5 μM to block sodium-independent glucose transport [48]. |
| 2-Deoxy-D-Glucose (2-DG) | Non-metabolizable glucose analog. | Used as a tracer to measure glucose uptake specifically; not a substrate for SGLT1 [10]. |
| α-Methyl-D-Glucopyranoside (AMG) | Non-metabolizable glucose analog. | Used as a tracer; is a substrate for SGLT1 and is transported but not metabolized [22]. |
| Hank's Balanced Salt Solution (HBSS) | Physiological buffer for transport assays. | Maintains ion gradients and pH; can be prepared with or without sodium ions to isolate sodium-dependent transport [33] [6]. |
| Transwell Plates | Permeable supports for cell culture. | Enables the formation of polarized cell monolayers and separate access to apical and basolateral compartments (e.g., 0.4 μm pore size, polyester filters) [10]. |
Detailed Experimental Protocol
Cell Culture and Differentiation
- Culture Maintenance: Grow Caco-2/TC7 cells in high-glucose (25 mM) Dulbecco's Modified Eagle Medium (DMEM), supplemented with 20% (v/v) heat-inactivated fetal bovine serum, 1% non-essential amino acids, 2% Glutamax, and 1% penicillin-streptomycin. Maintain cells in a humidified atmosphere of 10% CO₂ at 37°C [10] [11].
- Monolayer Differentiation: Seed cells onto apical chambers of Transwell plates (e.g., 0.1 × 10⁵ cells/cm²) and allow them to differentiate for at least 21 days. Change the medium three times per week. Monitor the integrity of the monolayers by measuring the Transepithelial Electrical Resistance (TEER) regularly [10] [49]. Differentiated monolayers typically achieve TEER values > 300 Ω∙cm².
Inhibitor Preparation and Pre-incubation
- Stock Solutions: Prepare a 10 mM stock of phlorizin and a 5 mM stock of cytochalasin B in DMSO. Aliquot and store at -20°C.
- Working Solutions: On the day of the experiment, dilute the stock solutions in pre-warmed, serum-free assay buffer (e.g., HBSS, pH 7.4) to achieve the final working concentrations. The final DMSO concentration should not exceed 0.1% (v/v) in all treatment groups, including the vehicle control.
- Vehicle Control: Assay buffer + 0.1% DMSO.
- Phlorizin Treatment: Assay buffer + 10 μM phlorizin.
- Cytochalasin B Treatment: Assay buffer + 5 μM cytochalasin B.
- Combination Treatment: Assay buffer + 10 μM phlorizin + 5 μM cytochalasin B.
- Pre-incubation: Aspirate the culture medium from both apical and basolateral compartments. Gently wash the cell monolayers with pre-warmed HBSS. Add the respective inhibitor or vehicle solutions to the apical compartment and incubate for 30-60 minutes at 37°C [48].
Glucose Uptake Assay
- Tracer Solution: Prepare the uptake solution in HBSS containing a physiological concentration of cold D-glucose (e.g., 5-10 mM) spiked with a radiolabeled (e.g., 14C-AMG) or fluorescent glucose tracer. For 2-DG uptake, a colorimetric or fluorometric glucose assay kit can be used to quantify uptake [22].
- Uptake Procedure: After pre-incubation, aspirate the inhibitor solutions. Add the tracer-containing uptake solution to the apical compartment and fresh HBSS to the basolateral compartment. Incubate for a defined period (e.g., 20-40 minutes) at 37°C [48].
- Termination: Stop the uptake by promptly removing the uptake solution and washing the monolayers three times with ice-cold phosphate-buffered saline (PBS) containing 0.5 mM phlorizin to halt all SGLT1 activity [22].
- Sample Collection: Lysate the cells with an appropriate lysis buffer (e.g., RIPA buffer or 0.1% SDS). Determine the protein concentration of the lysates using a standard assay (e.g., BCA assay). Quantify the tracer accumulation in the lysates via scintillation counting (for radiolabeled tracers) or a plate reader (for colorimetric/fluorometric assays).
Expected Results and Data Interpretation
A successful validation experiment will yield quantitative data that clearly delineates the contributions of each transporter. The expected outcomes and calculation logic for data interpretation are summarized below and in the following table.
Table 2: Quantification of Transporter-Specific Contributions to Glucose Uptake
| Experimental Condition | Measured Uptake (nmol/min/mg protein) | Calculated Transport Component | Interpretation |
|---|---|---|---|
| A. Vehicle Control | 4.50 ± 0.30 | Total Glucose Uptake | Represents the sum of all uptake pathways. |
| B. + Phlorizin (10 μM) | 2.90 ± 0.20 | Residual Uptake (primarily GLUT2) | Uptake remaining after SGLT1 blockade. |
| C. + Cytochalasin B (5 μM) | 2.10 ± 0.15 | Residual Uptake (primarily SGLT1) | Uptake remaining after GLUT blockade. |
| D. + Both Inhibitors | 0.50 ± 0.10 | Non-Specific/Diffusive Uptake | Represents transporter-independent uptake. |
| Calculation | Result | Definition | Biological Meaning |
| A - B | 1.60 | SGLT1-Specific Uptake | Phlorizin-sensitive, sodium-dependent transport. |
| B - D | 2.40 | GLUT2-Specific Uptake | Cytochalasin B-sensitive, facilitative transport. |
| C - D | 1.60 | Alternative SGLT1 Calculation | Confirms the primary calculation. |
| D | 0.50 | Non-Specific Component | Background level of uptake. |
Application in Research
This validated protocol serves as a critical tool in several research contexts:
- Mechanism of Action Studies: Screening natural compounds, plant extracts (e.g., Posidonia oceanica, mulberry leaf phenolics, fruit juice extracts), or drugs to determine if their hypoglycemic effect involves direct inhibition of intestinal glucose transporters [33] [6] [50].
- Pathophysiological Investigations: Studying the regulation of glucose transporters under inflammatory conditions or in metabolic diseases, where cytokine exposure can modulate the expression of SGLT1 and GLUT2 [11].
- Drug Transport Studies: While focused on glucose, the Caco-2/TC7 model and inhibitor principles are applicable to studying the permeability of pharmaceutical drugs, distinguishing between passive diffusion and carrier-mediated transport [51].
By implementing this detailed protocol, researchers can robustly and quantitatively validate the specific contributions of SGLT1 and GLUT2 in their Caco-2/TC7 glucose uptake assays, thereby strengthening the mechanistic conclusions of their research.
The study of intestinal glucose absorption is a cornerstone of metabolic research and drug development. The human colon carcinoma cell line Caco-2, particularly the TC7 clone, upon differentiation, spontaneously exhibits a polarized enterocyte-like phenotype with well-defined tight junctions and expresses key intestinal glucose transporters, including SGLT1 and GLUT2 [33]. This makes it a quintessential in vitro model for investigating glucose uptake and transport across the intestinal barrier.
Traditional assays for quantifying glucose uptake or transport often rely on fluorescently labeled glucose analogs, radiolabeled tracers, or enzymatic colorimetric reactions. While useful, these methods are inherently label-dependent, potentially perturbing natural glucose transport kinetics, and often require complex sample preparation, cell lysis, or the use of hazardous materials. Fourier-Transform Infrared (FTIR) Spectroscopy emerges as a powerful, label-free alternative that directly probes molecular vibrations, providing a non-destructive and reagent-free method for quantifying glucose in complex biological media [52] [53]. This application note details the use of FTIR spectroscopy for monitoring glucose transport in Caco-2/TC7 transwell systems, providing a robust protocol for researchers in drug discovery and metabolic disease research.
Principles of FTIR Spectroscopy for Glucose Detection
FTIR spectroscopy measures the absorption of infrared light by molecular bonds within a sample. Different functional groups absorb light at characteristic wavelengths, creating a unique molecular "fingerprint." The mid-infrared (MIR) region (4000 cm⁻¹ to 400 cm⁻¹) is particularly informative for glucose, as it contains strong fundamental vibrational modes [54].
- Key Absorption Bands for Glucose: Glucose exhibits distinctive absorption peaks in the MIR region, notably around 1030 cm⁻¹ (primarily C-O stretching vibrations) and 1080 cm⁻¹ (C-O-H bending) [52] [53]. The intensity of these absorption bands is directly proportional to the concentration of glucose in the sample path.
- Attenuated Total Reflection (ATR) Mode: For liquid samples like cell culture media, the ATR sampling technique is ideal. It involves pressing a small volume of the sample against a high-refractive-index crystal. The infrared beam undergoes total internal reflection within the crystal, generating an evanescent wave that penetrates the sample a few micrometers, thereby recording its absorption spectrum [52] [53]. This method requires minimal sample preparation and is highly reproducible.
When glucose is transported from the apical to the basolateral compartment in a Transwell system, the changing glucose concentration in either chamber can be tracked quantitatively by monitoring the intensity of its characteristic IR absorption bands [52].
Research Reagent Solutions Toolkit
The following table summarizes the essential materials and reagents required to establish the FTIR-based glucose transport assay.
Table 1: Key Research Reagents and Materials for FTIR-based Glucose Uptake Assay
| Item | Function/Description | Example/Reference |
|---|---|---|
| Caco-2/TC7 Cell Line | A well-characterized in vitro model of the human intestinal barrier. | [52] [33] |
| Transwell Inserts | Permeable supports for growing differentiated, polarized cell monolayers. | [52] |
| Cell Culture Medium | High-glucose DMEM is often used for cell maintenance. For transport assays, a defined buffer like PBS or HBSS is recommended. | [52] [33] |
| FTIR Spectrometer | Instrument equipped with an ATR accessory (e.g., diamond crystal). | [52] [55] |
| Transport Inhibitors | Pharmacological agents to validate the assay, e.g., Cytochalasin B (GLUT inhibitor) or Phloretin (SGLT/GLUT inhibitor). | [52] |
| Software | For spectral acquisition, preprocessing (e.g., baseline correction, normalization), and multivariate data analysis (e.g., PCA, PLS). | [55] [53] |
Detailed Experimental Protocol
Cell Culture and Differentiation
- Culture Caco-2/TC7 cells in high-glucose Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% Fetal Bovine Serum (FBS), 1% Non-Essential Amino Acids (NEAA), and 1% penicillin/streptomycin in a humidified incubator at 37°C and 5% CO₂ [52] [33].
- Seed cells on Transwell inserts (e.g., 12-well format, 1.12 cm² surface area, 0.4 µm pore size) at a density of ~1 x 10⁵ cells/cm².
- Differentiate the monolayers for 18-21 days, renewing the culture medium in both the apical and basolateral compartments every 2-3 days.
- Monitor barrier integrity regularly by measuring the Transepithelial Electrical Resistance (TEER) using an epithelial voltohmmeter. A TEER value exceeding 300 Ω·cm² typically indicates the formation of a tight, confluent monolayer suitable for transport studies [52] [33].
Sample Preparation for Glucose Transport Assay
- Pre-incubation: Prior to the assay, wash the differentiated Caco-2/TC7 monolayers twice with pre-warmed transport buffer (e.g., PBS or HBSS). Incubate the inserts for 20 minutes in the buffer to deplete residual glucose.
- Glucose Transport:
- Replace the apical chamber with a defined volume (e.g., 0.5 mL) of transport buffer containing a known initial concentration of D-glucose (e.g., 10 mM).
- Replace the basolateral chamber with a defined volume (e.g., 1.5 mL) of glucose-free transport buffer.
- Return the plate to the 37°C incubator.
- Sampling: At designated time intervals (e.g., 0, 30, 60, 90, 120 minutes), collect a small aliquot (e.g., 50 µL) from the basolateral compartment for FTIR analysis. Replace the removed volume with fresh, pre-warmed glucose-free buffer to maintain hydrostatic pressure.
- Inhibition Studies: To confirm the specificity of the assay, include control inserts where cells are pre-treated with transport inhibitors (e.g., 50 µM Cytochalasin B) for 30 minutes before and during the transport assay [52].
FTIR Spectral Acquisition and Analysis
- Instrument Setup: Turn on the FTIR spectrometer and allow it to stabilize. Clean the ATR crystal thoroughly with ethanol and water, and acquire a background spectrum of the clean, dry crystal.
- Data Acquisition: Place a 5-10 µL droplet of each collected basolateral sample directly onto the ATR crystal. Acquire spectra over the MIR range (e.g., 4000-800 cm⁻¹) with a resolution of 4 cm⁻¹ and 32-64 scans per spectrum. Clean the crystal between samples to prevent cross-contamination.
- Spectral Preprocessing: Process all acquired spectra using the instrument's software or specialized analysis tools. Standard steps include:
- Quantitative Analysis:
- The most straightforward approach is to monitor the intensity or area under the peak in the C-O stretching region (1030-1000 cm⁻¹).
- Construct a calibration curve by measuring the FTIR spectra of transport buffer spiked with known concentrations of glucose (e.g., 0-20 mM).
- Plot the peak area (or intensity) at ~1030 cm⁻¹ against the known glucose concentrations to generate a linear standard curve.
- Use this calibration model to convert the spectral data from the basolateral samples into glucose concentrations.
The following workflow diagram illustrates the key experimental steps from cell culture to data analysis:
Expected Results and Data Interpretation
Successful application of this protocol will yield time-dependent FTIR spectra showing a progressive increase in the characteristic glucose absorption bands in the basolateral compartment. The following table presents a summary of quantitative data that can be expected from such an experiment.
Table 2: Example Quantitative Data from a FTIR-based Glucose Transport Assay
| Time (minutes) | Basolateral Glucose Peak Area (a.u.) | Calculated Glucose Concentration (mM) | Apparent Permeability (Papp) (x10⁻⁶ cm/s) |
|---|---|---|---|
| 0 | 0.05 ± 0.01 | 0.10 ± 0.05 | - |
| 30 | 0.18 ± 0.03 | 0.85 ± 0.15 | 1.45 ± 0.25 |
| 60 | 0.35 ± 0.04 | 1.75 ± 0.20 | 1.52 ± 0.18 |
| 90 | 0.52 ± 0.05 | 2.65 ± 0.25 | 1.55 ± 0.15 |
| 120 | 0.68 ± 0.06 | 3.50 ± 0.30 | 1.58 ± 0.14 |
| 120 (with Cytochalasin B) | 0.25 ± 0.04 | 1.15 ± 0.20 | 0.58 ± 0.10 |
Data are presented as mean ± standard deviation (n≥3). Peak area is for the ~1030 cm⁻¹ band. Concentration calculated from a standard curve. Papp calculated using standard formulas.
- Data Interpretation: The increase in glucose concentration over time, as quantified by FTIR, directly reflects the transport activity across the Caco-2/TC7 monolayer. The significant reduction in both the final glucose concentration and the calculated apparent permeability (Papp) in the presence of Cytochalasin B confirms that the measured signal is due to specific, transporter-mediated glucose uptake and not passive diffusion or paracellular leakage [52]. This validates the biological relevance of the assay.
The mechanistic pathway below illustrates how FTIR detection and pharmacological inhibition integrate into the study of glucose transport biology.
Advantages and Technical Considerations
Key Advantages of the FTIR Method
- Label-Free and Non-Destructive: Avoids the use of fluorescent or radioactive labels, eliminating potential interference with natural transporter function [52] [53].
- Minimal Sample Preparation: The ATR technique requires only a small volume of sample without the need for derivatization or complex processing.
- Rapid and Cost-Effective: Spectral acquisition takes seconds to minutes, and the method does not require expensive enzyme-based assay kits or radioactive materials [52].
- Rich Information Content: A single spectrum provides information on not only glucose but also other biomolecules present, allowing for quality control and detection of potential contaminants or cellular metabolites.
Critical Technical Considerations
- Water Subtraction: As cell culture media and buffers are aqueous, the strong, broad absorption band of water dominates the IR spectrum. Sophisticated subtraction algorithms are crucial to reveal the analytic bands of glucose clearly [53].
- Sensitivity and Limit of Detection: While sufficient for monitoring transport in this system, the sensitivity of standard FTIR may be lower than enzymatic assays. Recent advancements, such as coupling FTIR with Multi-pass ATR (MATR) and Quantum Cascade Lasers (QCL), can significantly boost the signal-to-noise ratio and detection sensitivity for future applications [55].
- Data Analysis Expertise: While simple peak analysis is straightforward, leveraging the full potential of the multidimensional spectral data may require familiarity with multivariate data analysis techniques like Principal Component Analysis (PCA) or Partial Least Squares (PLS) regression [55] [53].
This application note establishes FTIR spectroscopy as a robust, label-free analytical tool for investigating glucose transport in Caco-2/TC7 intestinal barrier models. The provided detailed protocol enables researchers to directly quantify glucose concentrations in transport media, offering a compelling alternative to traditional label-dependent methods. Its non-destructive nature, speed, and reagent-free operation make it particularly suitable for high-throughput screening in drug discovery, especially for identifying compounds that modulate intestinal glucose absorption for the management of metabolic disorders like diabetes and obesity.
Validation and Comparative Analysis: Confirming Physiological Relevance
Within the context of in vitro glucose uptake assay research using Caco-2/TC7 cell lines, a critical challenge remains the validation and correlation of experimental findings with more complex biological systems. Research utilizing intestinal epithelial models operates within a critical methodological framework, where the ultimate physiological relevance depends on rigorous benchmarking against ex vivo and in vivo data [56]. This protocol details established methodologies and correlation strategies to enhance the translational validity of in vitro glucose uptake studies, with a specific focus on the Caco-2/TC7 intestinal barrier model. The integration of these approaches provides a robust scaffold for researchers in drug development and functional food science to generate predictive and physiologically relevant data on glucose metabolism and transport.
Foundational Concepts and Validation Strategies
The process of correlating in vitro findings with higher-order systems relies on understanding the capabilities and limitations of each model. The Caco-2 cell line, when differentiated into a monolayer, expresses key intestinal glucose transporters (SGLT1 and GLUT2) and forms tight junctions, making it a valuable surrogate for the human intestinal epithelium [33] [56]. However, to confirm the physiological relevance of findings from this system, a multi-faceted validation strategy is essential.
Key validation approaches include:
- Transport Mechanism Identification: Differentiating between sodium-dependent (SGLT1) and sodium-independent (GLUT2) glucose uptake pathways by manipulating buffer conditions [33].
- Barrier Integrity Assessment: Correlating transporter activity with epithelial barrier function via Transepithelial Electrical Resistance (TEER) and tight junction protein (e.g., ZO-1) quantification [33].
- Functional Redundancy Checks: Acknowledging that in vivo systems possess compensatory mechanisms absent in vitro, necessitating orthogonal validation [56].
- Spatial Resolution: Employing techniques like tissue slice cultures to map glucose uptake heterogeneity within intact tissue architectures, providing an ex vivo benchmark for in vitro findings [57].
Table 1: Core Validation Benchmarks for In Vitro Glucose Uptake Assays
| Validation Parameter | In Vitro Metric (Caco-2) | Ex Vivo / In Vivo Correlation | Key Assessment Method |
|---|---|---|---|
| GLUT2 Activity | Glucose uptake in Na+-free buffer [33] | 2-NBDG uptake in tissue slices [57] | Inhibitor studies, transporter expression (WB) |
| SGLT1 Activity | Glucose uptake in Na+-containing buffer [33] | Not directly measured in standard ex vivo models | Phlorizin inhibition, expression (WB) |
| Barrier Integrity | TEER, ZO-1 protein levels [33] | Histology, permeability assays in live tissue [56] | TEER monitoring, immunofluorescence |
| Functional Outcome | Reduced apical-to-basolateral glucose flux | Lowered post-prandial blood glucose in vivo [33] | Radio-/fluorescent-labeled tracer transport |
Experimental Protocols for Correlation
In Vitro Glucose Uptake Assay in Caco-2 Cells
This protocol is adapted from studies investigating the modulation of glucose transporters by natural extracts [33].
Key Reagents & Materials
- Differentiated Caco-2/TC7 cell monolayers (21 days post-seeding on transwell inserts)
- Krebs-Ringer Bicarbonate Buffer (KRB, pH 7.4)
- Sodium-containing and sodium-free (e.g., choline chloride substitution) uptake buffers
- 2-Deoxy-D-[3H]-glucose or cold 2-Deoxy-D-Glucose (2-DG)
- Test compounds (e.g., Posidonia oceanica extract, POE)
- Cell lysis buffer (e.g., RIPA buffer)
- Scintillation cocktail (for radiolabeled glucose) or commercial glucose uptake assay kit
Procedure
- Preparation: Differentiate Caco-2 cells on semi-permeable membrane inserts for 21 days. Confirm monolayer integrity by measuring TEER (>300 Ω×cm²).
- Pre-treatment: Serum-starve cells for 2-4 hours. Pre-incubate with the test compound (e.g., POE at 15 µg GAE/mL) or vehicle control in the appropriate buffer for a predetermined time (e.g., 4-24 hours) [33].
- Uptake Phase:
- Aspirate the treatment medium.
- Wash cell monolayers gently with pre-warmed (37°C) sodium-containing or sodium-free KRB buffer.
- Add uptake buffer containing the labeled glucose tracer (e.g., 1 µCi/mL 2-Deoxy-D-[3H]-glucose) or a fixed concentration of cold 2-DG.
- Incubate for a defined, short period (e.g., 5-15 minutes) at 37°C to ensure initial rate conditions.
- Termination:
- Rapidly aspirate the uptake solution.
- Immediately wash the monolayers 3-4 times with ice-cold PBS to terminate uptake and remove extracellular tracer.
- Sample Collection:
- Lyse cells in an appropriate lysis buffer for 30-60 minutes.
- Transfer lysate to a microcentrifuge tube and centrifuge to remove insoluble debris.
- Quantification:
- For radiolabeled tracers: Mix an aliquot of the supernatant with scintillation fluid and measure radioactivity with a scintillation counter.
- For cold tracers: Use a commercial glucose uptake colorimetric/fluorometric kit to quantify the accumulated 2-DG-6-phosphate in the lysate.
- Normalization: Normalize the glucose uptake counts to the total protein content of the lysate (determined by BCA or Bradford assay).
Ex Vivo Validation Using Live Tissue Slices
This protocol leverages the spatial and functional preservation of intact tissue to validate findings from cell lines [57].
Key Reagents & Materials
- Freshly harvested murine intestinal tissue (e.g., jejunum) or lymph nodes
- Vibratome or compresstome for slice preparation (200-300 µm thickness)
- Oxygenated slice culture media (e.g., ACSF or RPMI-based)
- Fluorescent glucose analogue: 2-NBDG (2-[N-(7-Nitrobenz-2-oxa-1,3-diazol-4-yl)amino]-2-deoxyglucose)
- Live-cell imaging setup (confocal or widefield microscope with environmental chamber)
- Optional: Live-cell immunofluorescence markers (e.g., anti-CD3 for T-cells)
Procedure
- Tslice Preparation: Immediately after euthanasia, harvest the target tissue. Embed in low-melting-point agarose and section 300 µm thick slices using a vibratome in ice-cold, oxygenated buffer.
- Recovery & Culture: Allow tissue slices to recover in oxygenated culture media for 1-2 hours at 37°C in a tissue culture incubator.
- 2-NBDG Incubation:
- Prepare a working solution of 2-NBDG (e.g., 100-200 µM) in pre-warmed "starve media" (e.g., PBS with 10% FBS) from a DMSO stock [57].
- Incubate tissue slices in the 2-NBDG solution for 30-45 minutes at 37°C, protected from light.
- Washing & Imaging:
- Gently wash slices 2-3 times with fresh, pre-warmed media to remove excess extracellular 2-NBDG.
- Transfer slices to an imaging chamber. Image immediately using a confocal microscope to capture spatially resolved fluorescence.
- Stimulation & Dynamic Imaging (Optional):
- For repeated-measures design, perform a baseline 2-NBDG incubation and imaging step.
- Then, treat slices with a stimulant (e.g., T-cell activator) for several hours.
- Perform a second, identical 2-NBDG incubation and imaging sequence to quantify dynamic changes in glucose uptake within the same sample [57].
- Image Analysis: Quantify mean fluorescence intensity (MFI) in specific regions of interest (ROIs) corresponding to different tissue structures (e.g., villi, crypts, T-cell zones) using image analysis software (e.g., ImageJ/Fiji).
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Glucose Uptake and Validation Studies
| Reagent / Material | Function / Application | Example Usage & Notes |
|---|---|---|
| Caco-2/TC7 Cell Line | In vitro model of the human intestinal epithelium. | Forms polarized monolayers with enterocyte-like properties for transport studies [33]. |
| 2-Deoxy-D-Glucose (2-DG) | Non-metabolizable glucose analog for uptake measurement. | Trapped in cells after phosphorylation; measured via colorimetric/fluorometric kits or radiolabeled forms [33]. |
| 2-NBDG | Fluorescent glucose analog for real-time, spatial uptake analysis. | Used for imaging glucose uptake in live cells and ex vivo tissue slices [57]. |
| Transwell Inserts | Permeable supports for growing polarized cell monolayers. | Critical for proper differentiation of Caco-2 cells and TEER measurement [33]. |
| Transepithelial Electrical Resistance (TEER) Meter | Instrument to measure integrity and tight junction formation in cell monolayers. | A key quality control metric for Caco-2 studies; values >300 Ω×cm² indicate good barrier integrity [33]. |
| SGLT/GLUT Inhibitors | Pharmacological tools to dissect transporter-specific contributions. | Phlorizin (SGLT inhibitor) or Phloretin (GLUT inhibitor) used in mechanistic studies. |
| Live Tissue Slice Culture System | Ex vivo platform that preserves tissue architecture and cellular heterogeneity. | Used for validating in vitro findings in a more physiologically relevant context [57]. |
| Antibodies for Western Blot | Protein level analysis of glucose transporters and junctional proteins. | Used to quantify changes in GLUT2, SGLT1, or ZO-1 expression in response to treatments [33]. |
Workflow and Pathway Visualization
The following diagram illustrates the integrated experimental workflow for conducting and validating in vitro glucose uptake assays, from initial screening to mechanistic and functional correlation.
Integrated Workflow for Validating Glucose Uptake Mechanisms
The molecular signaling pathways through which active compounds modulate glucose transport and barrier function are complex. The following diagram summarizes the key mechanistic pathways identified in foundational studies, such as those involving Posidonia oceanica extract (POE).
Key Molecular Pathways of Glucose Uptake Modulation
The Caco-2/TC7 cell line, a well-established in vitro model of the human intestinal epithelium, serves as a cornerstone for studying nutrient transport, drug absorption, and metabolic diseases [58] [59] [24]. These cells spontaneously differentiate into polarized enterocyte-like monolayers, expressing functional characteristics of mature small intestinal cells, including key glucose transporters [58] [22]. This protocol details the use of CRISPR/Cas9-mediated knockout (KO) of the MTTP and SAR1B genes in Caco-2/TC7 cells to create mechanistically informative models for investigating intestinal glucose absorption and lipid metabolism. These genes are critical for lipoprotein assembly and secretion; their disruption recapitulates features of rare lipid malabsorption disorders (Chylomicron Retention Disease, CRD) and provides a powerful tool for dissecting the crosstalk between lipid and glucose metabolic pathways [60] [61].
Application Notes
Utility of MTTP and SAR1B Knockout Models
MTTP (Microsomal Triglyceride Transfer Protein) is essential for the assembly of apolipoprotein B-containing lipoproteins, including chylomicrons [61]. SAR1B (Secretion-Associated Ras-related GTPase 1B) is a key component of the COPII coat complex, mediating the vesicular transport of pre-chylomicrons from the endoplasmic reticulum to the Golgi apparatus [60] [61]. Biallelic mutations in these genes in humans lead to impaired fat-soluble vitamin absorption and defective chylomicron secretion [60] [61].
- Mechanistic Insights: KO clones allow researchers to probe the direct molecular consequences of blocked lipoprotein secretion, such as the accumulation of intracellular lipid droplets, alterations in triglyceride and cholesterol efflux, and subsequent compensatory changes in cellular metabolism [61].
- Therapeutic Screening: These isogenic cell lines provide a robust platform for screening therapeutic compounds, including different pharmaceutical forms of fat-soluble vitamins like vitamin E (e.g., tocopherol acetate and tocofersolan), to overcome the absorption defect characteristic of CRD [61].
- Glucose Metabolism Interplay: Although primarily affecting lipid transport, these models are invaluable in a broader thesis context to investigate how disrupted lipid metabolism influences intestinal glucose uptake mechanisms, a relevant area of research for conditions like metabolic syndrome and type 2 diabetes [22].
Quantitative Characterization of Knockout Clones
The following table summarizes key phenotypic changes observed in validated MTTP and SAR1B KO Caco-2/TC7 clones compared to wild-type cells.
Table 1: Characteristic Phenotypes of MTTP and SAR1B KO Caco-2/TC7 Clones
| Parameter | Wild-Type (Control) | MTTP KO Clones | SAR1B KO Clones | Measurement Method |
|---|---|---|---|---|
| MTP / Sar1b Protein | Normal expression | Undetectable [61] | Undetectable [61] | Western Blot [61] |
| Intracellular Lipid Droplets | Normal distribution | Significant accumulation [61] | Significant accumulation [61] Microscopy [61] | |
| Triglyceride Secretion | Normal secretion | ↓ 57.0% to 83.9% [61] | Impaired [60] | Secretion assay [61] |
| Cholesterol Secretion | Normal secretion | ↓ 35.3% to 60.6% [61] | Impaired [60] | Secretion assay [61] |
| α-Tocopherol (Vitamin E) Secretion | Normal secretion | ↓ 41.5% to 97.2% [61] | Impaired [61] | HPLC analysis [61] |
| Phenotype Severity | N/A | More severe [61] | Less severe [61] | Comparative analysis of secretion deficits [61] |
Experimental Protocols
Protocol #1: Generation of MTTP and SAR1B KO Caco-2/TC7 Clones Using CRISPR/Cas9
This protocol is adapted from the work of Le Grand et al. (2023) [61].
3.1.1 Research Reagent Solutions
Table 2: Essential Reagents for CRISPR/Cas9 Knockout
| Reagent / Material | Function / Application | Example Source / Identifier |
|---|---|---|
| TrueCut Cas9 Protein v2 | RNA-guided endonuclease for targeted DNA cleavage. | Thermo Fisher Scientific [61] |
| Lipofectamine CRISPRMAX | Transfection reagent for complexing Cas9-gRNA ribonucleoproteins. | Thermo Fisher Scientific [61] |
| MTTP-gRNA1 & gRNA2 | Guide RNAs targeting coding sequences of the MTTP gene. | Synthego; Sequences: 5′-ACGCUCCUUCAUCUAAUCCA-3′, 5′-UACACGGCCAUUCCCAUUGU-3′ [61] |
| SAR1B-gRNA1 & gRNA2 | Guide RNAs targeting coding sequences of the SAR1B gene. | Synthego; Sequences: 5′-UUGACUCUAACAGCCUUUCG-3′, 5′-UCCGAAGAACUGACCAUGC-3′ [61] |
| Caco-2/TC7 Cell Line | Human intestinal epithelial model for differentiation into enterocytes. | ATCC or Rousset Lab [10] [22] |
| Anti-MTP / Anti-Sar1b Antibodies | Validation of protein knockout by Western Blot. | Santa Cruz Biotechnology (clones C-1 and AT1C7) [61] |
3.1.2 Workflow Diagram
3.1.3 Step-by-Step Procedure
- gRNA Design and Complexation: Design and synthesize two gRNAs for your target gene (MTTP or SAR1B) to increase knockout efficiency. Complex the purified Cas9 protein with the gRNAs to form ribonucleoproteins (RNPs) according to the manufacturer's instructions [61].
- Cell Culture: Maintain Caco-2/TC7 cells in Dulbecco’s Modified Eagle Medium (DMEM) supplemented with 16% fetal bovine serum (FBS), 1% non-essential amino acids, and 1% penicillin/streptomycin. Culture cells in a humidified atmosphere of 10% CO₂ at 37°C [61] [22].
- Transfection: Seed cells in a standard culture flask or plate so they are 60-80% confluent at the time of transfection. Using Lipofectamine CRISPRMAX, transfert the cells with the pre-formed RNP complexes. A positive control (e.g., gRNA targeting HPRT1) and a negative control (untransfected or mock-transfected) should be included [61].
- Clone Isolation: 48-72 hours post-transfection, trypsinize the cells and seed them at very low density (e.g., 1-5 cells/cm²) in large culture dishes or multi-well plates to facilitate the isolation of single-cell-derived colonies. Allow individual clones to expand for 2-3 weeks, monitoring colony growth microscopically [61].
- Validation: Once clones have expanded sufficiently, validate the knockout.
- Genomic DNA: Isolate genomic DNA and sequence the target regions to confirm the presence of indels (insertions or deletions) [61].
- mRNA: Perform RT-qPCR on total RNA to confirm a significant reduction in target gene mRNA levels [61].
- Protein: Confirm the absence of the target protein by Western Blot analysis using specific antibodies against MTP or Sar1b. β-actin should be used as a loading control [61].
Protocol #2: Functional Validation Using an In Vitro Glucose Uptake Assay
This protocol assesses the functional impact of gene knockouts and can be adapted from general glucose uptake methods [62] and specific applications in Caco-2/TC7 cells [22].
3.2.1 Workflow Diagram
3.2.2 Step-by-Step Procedure
- Monolayer Differentiation: Seed wild-type and validated KO Caco-2/TC7 cells at a density of 3 × 10⁴ cells/cm² on permeable polyester filter inserts (e.g., 1 μm pore size, 24 mm diameter). Differentiate the cells for 19-21 days, changing the medium every 2-3 days. For the first 7-14 days, use medium supplemented with 10-20% FBS on the basolateral side. Subsequently, reduce to serum-free or low-serum medium to induce final differentiation [61] [24].
- Quality Control: Monitor monolayer integrity by regularly measuring the Transepithelial Electrical Resistance (TEER). Use only monolayers with TEER values ≥ 200 Ω·cm² for experiments. Confirm low paracellular permeability using tracers like [¹⁴C]-mannitol [24].
- Glucose Uptake Assay:
- Pre-incubation (Optional): The apical side of the monolayers can be pre-incubated for 1 hour with compounds of interest (e.g., digested dietary proteins at 5 mg/mL) dissolved in unsupplemented DMEM [22].
- Uptake Phase: Replace the apical medium with a solution containing a non-metabolizable glucose analogue, such as 2 mM α-methyl-D-glucopyranoside (AMG) spiked with 0.2 μCi/mL of ¹⁴C-AMG, with or without the test compounds. Incubate for 40 minutes at 37°C [22].
- Termination: Stop the uptake by removing the radioactive solution and washing the apical side three times with ice-cold phosphate-buffered saline (PBS) containing 0.5 mM phlorizin (a specific SGLT1 inhibitor) to block further transporter activity.
- Quantification: Solubilize the cell monolayer with a suitable lysis buffer (e.g., 0.1 M NaOH or commercial solubilizer). Measure the radioactivity in the cell lysate using a scintillation counter. Determine the protein concentration of the lysate using a BCA or Bradford assay. Express glucose uptake as pmol or nmol of AMG taken up per mg of cellular protein per unit time [22] [62].
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for Caco-2/TC7 CRISPR and Functional Studies
| Category | Reagent | Function / Application |
|---|---|---|
| CRISPR Components | TrueCut Cas9 Protein v2 | Catalytic enzyme for precise DNA cleavage. |
| Gene-specific gRNAs (e.g., MTTP-gRNA1) | Guides Cas9 to the specific genomic target site. | |
| Lipofectamine CRISPRMAX | Transfection reagent for efficient RNP delivery. | |
| Cell Culture | Caco-2/TC7 Cell Line | A well-differentiated subclone of Caco-2 ideal for transport studies. |
| Polyester Filter Inserts | Permeable supports for polarization and differentiation. | |
| DMEM with High Glucose (4.5 g/L) | Standard culture medium. | |
| Validation & Assay | Anti-MTP / Anti-Sar1b Antibodies | Confirm protein knockout via Western Blot. |
| [¹⁴C]-α-Methyl-D-Glucopyranoside | Radiolabeled, non-metabolizable glucose analogue for uptake studies. | |
| Phlorizin | SGLT1 transporter inhibitor to stop uptake and validate specificity. | |
| Scintillation Counter | Instrument to quantify radioactivity in cell lysates. |
The investigation of intestinal glucose absorption mechanisms is fundamental to understanding nutrient metabolism and developing therapeutic strategies for metabolic disorders. In vitro models of the intestinal epithelium serve as indispensable tools for such research, allowing scientists to study transporter dynamics and regulatory pathways in controlled environments. Among these models, the Caco-2/TC7 cell line, derived from human colorectal adenocarcinoma, has emerged as a gold standard due to its ability to spontaneously differentiate into enterocyte-like cells. However, the quest for more physiologically relevant systems has led to the development of advanced models, including co-cultures with mucus-producing HT29-MTX cells and primary cell-derived systems. This application note provides a comprehensive comparison of these intestinal models, with a specific focus on their applications in glucose uptake assays, to guide researchers in selecting the most appropriate system for their experimental objectives.
Model Characteristics and Comparative Analysis
Key Features of Prominent Intestinal Models
Table 1: Characteristics of Intestinal Cell Models for Glucose Uptake Studies
| Model Type | Key Cellular Components | Differentiation Time | Glucose Transporters Expressed | Mucus Production | Physiological Relevance | Primary Applications |
|---|---|---|---|---|---|---|
| Caco-2/TC7 Monoculture | Differentiated enterocyte-like cells [50] | 15-21 days [63] | SGLT1, GLUT2, GLUT1 [50] [63] | None or minimal [64] | Medium - Represents absorptive epithelium | Drug permeability, transporter studies, nutrient absorption [40] |
| Caco-2/HT29-MTX Co-culture | Enterocytes (Caco-2) & Goblet-like cells (HT29-MTX) [65] | 15-21 days [65] | SGLT1, GLUT2 [50] | Yes (from HT29-MTX cells) [65] | High - Mimics cellular diversity and mucus barrier | Compound absorption, host-microbe interactions, toxin studies [65] [66] |
| Caco-2 ALI-VIP Model | Differentiated Caco-2 with induced mucus production [64] | ~21 days (including ALI phase) [64] | Information not specified in search results | Robust (induced by ALI conditions & VIP) [64] | High - Features functional mucus layer without co-culture complexity | Mucus-barrier interactions, pathogen invasion studies [64] |
| Primary Cell Systems (e.g., Organoids) | All native intestinal epithelial cell types [40] [67] | Variable (days to weeks) [67] | Native transporter profile | Yes (native goblet cells) [40] | Very High - Closest to in vivo physiology | Disease modeling, host-pathogen interactions, personalized medicine [67] |
Functional Performance in Glucose Uptake Studies
Table 2: Functional Performance Metrics of Intestinal Models
| Model Type | Transepithelial Electrical Resistance (TEER, Ω×cm²) | Glucose Uptake Mechanisms | Response to Polyphenol Inhibition | Key Advantages | Inherent Limitations |
|---|---|---|---|---|---|
| Caco-2/TC7 Monoculture | High (exact values context-dependent) | SGLT1 (active, low [Glucose]), GLUT2 (facilitated, high [Glucose]) [63] | Yes (e.g., by fruit juice polyphenols) [50] | Well-characterized, reproducible, high throughput | Lacks mucus layer, does not represent cellular heterogeneity [40] |
| Caco-2/HT29-MTX Co-culture | High, can be modulated [65] | SGLT1 and GLUT2, responsive to biochemical cues [50] | Effective reduction of GLUT2 transcription shown [50] | Mucus barrier, more predictive absorption data, suitable for toxin studies [65] [66] | Seeding ratio optimization required, longer setup than monoculture [65] |
| Caco-2 ALI-VIP Model | Altered junction protein expression increases small molecule permeability [64] | Information not specified in search results | Information not specified in search results | Robust inducible mucus production without complex co-culture | Requires specific culture conditions (ALI, VIP supplementation) [64] |
| Primary Cell Systems | Variable, depends on origin and culture method [67] | Native physiology including potential apical GLUT2 translocation [63] | Information not specified in search results | Highest physiological relevance, patient-specific responses | Technically challenging, high cost, donor-to-donor variability [40] [67] |
Detailed Experimental Protocols
Protocol 1: Establishing Caco-2/HT29-MTX Co-culture for Glucose Transport Studies
Principle: This protocol creates a more physiologically relevant intestinal barrier model by co-culturing absorptive enterocyte-like Caco-2 cells with mucus-producing HT29-MTX cells in a 9:1 ratio [65]. The resulting epithelium expresses functional glucose transporters and is protected by a mucus layer.
Materials:
- Cell Lines: Caco-2 cells (e.g., ATCC HTB-37) and HT29-MTX cells (e.g., from ECACC) [65] [34]
- Culture Vessel: Permeable Snapwell or Transwell inserts (e.g., 12 mm diameter, 0.4 µm pore size) [65]
- Culture Medium: Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% Fetal Bovine Serum (FBS), 1% Non-Essential Amino Acids (NEAA), 2 mM L-glutamine, 100 U/mL penicillin, and 100 µg/mL streptomycin [65] [34]
- Differentiation: The cells require 15-21 days to form a fully differentiated monolayer capable of supporting a mucus layer and expressing key transporters like SGLT1 and GLUT2 [50] [65].
Procedure:
- Cell Seeding:
- Harvest and count Caco-2 and HT29-MTX cells separately.
- Mix the cell suspensions at a 9:1 ratio (Caco-2:HT29-MTX) to achieve a final combined density of (1 \times 10^5) cells per insert [65].
- Seed the cell mixture onto the apical side of the pre-hydrated Transwell insert.
- Add culture medium to both the apical (0.5 mL) and basolateral (1.5 mL) compartments.
Culture and Differentiation:
- Maintain cultures at 37°C in a 5% CO₂ atmosphere for 21-28 days to allow for complete differentiation and polarization [65].
- Change the culture medium every 2-3 days.
Quality Control:
- Transepithelial Electrical Resistance (TEER): Monitor barrier integrity regularly using an epithelial voltohmmeter. Stable, high TEER values indicate the formation of tight junctions [65] [64].
- Permeability Assay: Validate barrier function using a marker like Lucifer Yellow (100 µM). Add to the apical compartment and measure its appearance in the basolateral compartment over time; low flux indicates an intact barrier [65] [66].
Protocol 2: Glucose Uptake Assay Using Radiolabeled Glucose
Principle: This assay quantitatively measures the capacity of the intestinal model to absorb glucose by using a traceable radiolabel. It allows for the dissection of specific transporter contributions through the use of pharmacological inhibitors.
Materials:
- Uptake Buffer: Krebs buffer (e.g., 30 mM HEPES, 130 mM NaCl, 4 mM KH₂PO₄, 1 mM MgSO₄, 1 mM CaCl₂, pH 7.4) [63].
- Tracers: ¹⁴C-labeled D-glucose (to measure total uptake) and ³H-labeled L-glucose (a non-metabolizable stereoisomer to measure passive diffusion) [63].
- Inhibitors: Phlorizin (a specific SGLT1 inhibitor) and Phloretin (a GLUT2 inhibitor) [63].
- Equipment: Cell culture plates with inserts, water bath, scintillation counter.
Procedure:
- Pre-equilibration: Wash the differentiated cell monolayers twice with pre-warmed (37°C) uptake buffer.
- Inhibition (Optional): To study specific transporter contributions, pre-incubate cells for a short period (e.g., 15-30 minutes) with uptake buffer containing phlorizin (for SGLT1) or phloretin (for GLUT2) [63].
- Uptake Phase:
- Prepare the uptake solution in pre-warmed Krebs buffer, containing the desired concentration of D-glucose (e.g., 0.5-50 mM) and the radioactive tracers (¹⁴C-D-glucose and ³H-L-glucose) [63].
- Rapidly replace the apical buffer with the uptake solution and incubate for a defined period (e.g., 30 seconds to 10 minutes).
- Termination:
- Quickly stop the uptake by removing the solution and washing the cells twice with ice-cold phosphate-buffered saline (PBS).
- Solubilize the cell monolayer with 0.1N NaOH for 30 minutes at 37°C [63].
- Analysis:
- Measure the radioactivity in the cell lysates using a scintillation counter.
- Calculate protein content in the lysate for normalization (e.g., using a BCA assay).
- Carrier-mediated (active) uptake is calculated as the difference between total D-glucose uptake (¹⁴C) and passive uptake (³H).
Signaling Pathways and Data Visualization
Glucose Transporter Dynamics in Enterocytes
The cellular uptake of glucose is a tightly regulated process mediated by specific transporters on the apical and basolateral membranes. The classic paradigm involves active transport via SGLT1 at low luminal glucose concentrations and facilitated diffusion via GLUT2 at high concentrations. However, evidence suggests a more dynamic model where GLUT2 can be recruited to the apical membrane in response to high glucose, significantly increasing uptake capacity [63]. This process may involve Protein Kinase C βII (PKCβII) activation and cytoskeletal elements [63]. The following diagram illustrates these key pathways and their modulation.
Experimental Workflow for Model Comparison
The systematic evaluation of different intestinal models for glucose uptake studies involves a multi-step process, from model establishment to functional assay and data analysis. The following diagram outlines a standardized workflow that can be applied to compare the performance of Caco-2/TC7 monocultures with more complex models like Caco-2/HT29-MTX co-cultures.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Intestinal Glucose Uptake Studies
| Reagent / Kit | Function / Application | Example Usage in Protocols |
|---|---|---|
| Caco-2 Cells | Forms differentiated, enterocyte-like monolayer for absorption studies [34] | Parental line for monoculture; base for co-culture with HT29-MTX [50] [65] |
| HT29-MTX Cells | Provides mucus-producing goblet cell phenotype in co-culture models [65] | Mixed with Caco-2 cells (e.g., 9:1 ratio) to create a mucus barrier [65] |
| Transwell/Snapwell Inserts | Permeable supports for culturing polarized epithelial cell layers [65] [34] | Platform for growing differentiated monolayers for transport and TEER assays [65] [64] |
| Phlorizin | Specific, competitive inhibitor of the SGLT1 transporter [63] | Used to pharmacologically dissect the contribution of SGLT1 to total glucose uptake [63] |
| Phloretin | Potent inhibitor of the GLUT2 (and GLUT1) facilitated glucose transporters [63] | Used to inhibit GLUT2-mediated glucose transport in uptake assays [63] |
| ¹⁴C-D-Glucose & ³H-L-Glucose | Radiolabeled tracers for quantifying total and passive glucose uptake, respectively [63] | Added to uptake buffer to measure carrier-mediated and passive diffusion components [63] |
| Glucose Colorimetric Assay Kit | Enables quantification of glucose concentration without radioactivity [50] | Can be used to measure glucose depletion from media or appearance in basolateral compartment [50] |
| Vasointestinal Peptide (VIP) | Induces mucus production and differentiation in Caco-2 cells under Air-Liquid Interface (ALI) [64] | Added to basolateral compartment of ALI cultures to create a robust mucus layer [64] |
Within the framework of a broader thesis on in vitro models for metabolic research, this application note provides a detailed protocol for a multi-parametric assessment of glucose handling using the human intestinal Caco-2/TC7 cell line. The absorption of glucose in the small intestine is a critical process in maintaining systemic glucose homeostasis, and its dysregulation is a key feature of metabolic diseases [49] [68]. This process is not isolated; it is intrinsically linked to the integrity of the intestinal barrier [69]. A robust in vitro model that can simultaneously evaluate glucose uptake, barrier integrity (via Transepithelial Electrical Resistance, TEER), and the molecular underpinnings (gene and protein expression) is therefore essential for a comprehensive understanding of nutrient absorption and for the development of therapeutic interventions.
The Caco-2/TC7 subclone, used in these protocols, is particularly suited for such studies as it exhibits a more homogeneous and functional differentiation compared to the parental Caco-2 line, forming a polarized monolayer with a well-developed brush border that mimics the intestinal epithelium [70] [71]. This note outlines standardized methodologies for culturing and differentiating Caco-2/TC7 cells, and for conducting correlated assays to generate a holistic dataset on glucose transport and intestinal barrier function.
Experimental Principles and Workflow
The following diagram illustrates the integrated experimental workflow, from cell culture to multi-assay data correlation, as detailed in the subsequent protocols.
Materials and Reagents
Research Reagent Solutions
The following table lists the essential materials and reagents required to perform the experiments described in this application note.
Table 1: Essential Research Reagents and Materials
| Item | Function/Description | Example/Catalog Reference |
|---|---|---|
| Caco-2/TC7 Cells | Human intestinal epithelial cell model; upon differentiation, forms polarized monolayer with enterocyte-like properties. | [70] [71] |
| Transwell Inserts | Permeable supports for cell culture enabling apical and basolateral compartment access, essential for TEER and transport studies. | Polycarbonate or PET filters, 0.4-3.0 µm pore size [72] |
| DMEM, High Glucose | Cell culture medium providing nutrients and a high-glucose environment for cell growth and differentiation. | With 4.5 g/L D-Glucose [49] |
| Fetal Bovine Serum (FBS) | Essential supplement for cell culture media, providing growth factors and nutrients for cell proliferation and differentiation. | Heat-inactivated [73] |
| TEER Measurement System | Instrument for measuring Transepithelial Electrical Resistance to quantify monolayer integrity and tight junction formation. | e.g., Millicell ERS-2 Volt-Ohm Meter [49] [74] |
| D-Glucose | Primary substrate for glucose uptake assays. | |
| GLUT2 Antibody | For detection of the facilitative glucose transporter GLUT2 protein levels via Western Blot. | [49] [68] |
| SGLT1 Antibody | For detection of the sodium-dependent glucose transporter SGLT1 protein levels via Western Blot. | [49] |
| ZO-1 Antibody | For detection of the tight junction protein Zonula Occludens-1 via immunofluorescence or Western Blot. | [72] [68] |
| Occludin Antibody | For detection of the tight junction protein Occludin via immunofluorescence or Western Blot. | [49] [69] |
Detailed Experimental Protocols
Protocol 1: Cell Culture and Differentiation on Transwell Inserts
The formation of a consistent, fully differentiated monolayer is the foundational step for all subsequent assays.
- Cell Seeding: Culture Caco-2/TC7 cells in complete DMEM (high glucose, supplemented with FBS, NEAA, L-Glutamine, and antibiotics). Harvest cells at 80-90% confluence and seed onto collagen-coated Transwell inserts at a density of (1 \times 10^5) cells/cm² (e.g., (2.5 \times 10^5) cells/well for a 12-well insert) [49] [71].
- Differentiation: Change the medium in both the apical and basolateral compartments every 48 hours for the first week, and daily thereafter. Allow cells to differentiate for 14-21 days post-confluence. The Caco-2/TC7 subclone has been demonstrated to reach a stable, functional differentiation state as early as 14 days [71].
- Quality Control (QC): Monitor monolayer integrity regularly by measuring TEER. A TEER value of ≥200 Ω·cm² at 37°C indicates a tight, confluent monolayer suitable for experiments [72]. Confocal microscopy staining for ZO-1 can be used to visually confirm tight junction formation [72].
Table 2: Key Parameters for Caco-2/TC7 Cell Differentiation
| Parameter | Specification | Rationale & Reference |
|---|---|---|
| Seeding Density | (1 \times 10^5) cells/cm² | Optimal for forming a uniform monolayer without over-confluence [49]. |
| Differentiation Time | 14 - 21 days | Caco-2/TC7 cells are functionally differentiated by day 14 [71]. |
| QC: TEER Value | ≥ 200 Ω·cm² | Validated indicator of monolayer integrity and tight junction formation [72] [49]. |
| QC: Paracellular Marker | e.g., [14C]-Mannitol permeability < (2.0 \times 10^{-6}) cm/s | Confirms low paracellular leakage [72]. |
Protocol 2: Glucose Uptake Assay
This protocol measures the cellular capacity to absorb glucose, which can be modulated by various treatments.
- Preparation: Differentiate Caco-2/TC7 cells on Transwell inserts as in Protocol 1. Serum-starve the cells for a few hours prior to the assay to reduce background interference.
- Treatment: Apply the test compound (e.g., 6-shogaol, plant extracts) to the apical compartment for a predetermined incubation period (e.g., 24 hours) [49] [68].
- Uptake Measurement:
- Wash the cell monolayers with a warm buffer (e.g., HBSS).
- Add a solution containing D-glucose to the apical compartment. To distinguish between SGLT1 and GLUT2 activity, perform the assay under both sodium-containing and sodium-free (e.g., choline chloride substitution) conditions [68].
- Incubate at 37°C for a specified time (e.g., 30-60 minutes).
- Collect samples from the basolateral compartment or lyse the cells to measure glucose content using a standard glucose assay kit [49]. A significant decrease in glucose uptake under sodium-free conditions indicates a primary role for SGLT1, while uptake persisting in sodium-free conditions is mediated by GLUT2.
Protocol 3: TEER Measurement for Barrier Integrity
TEER is a non-invasive, quantitative measure of the integrity of the intestinal epithelial barrier.
- Measurement: Using a volt-ohm meter with "chopstick" electrodes, measure the resistance across the cell monolayer on the Transwell insert. Ensure the electrodes are placed correctly in the apical and basolateral compartments without touching the membrane.
- Calculation: Subtract the resistance of a cell-free insert (background) from the measured value. Multiply this value by the surface area of the Transwell filter (e.g., 1.1 cm² for a 12-well insert) to obtain the TEER in Ω·cm² [49].
- Application: Measure TEER before and after experimental treatments to assess their impact on barrier function. An increase in TEER suggests enhanced barrier integrity (e.g., via upregulation of tight junction proteins), while a decrease indicates barrier disruption [49] [68].
Protocol 4: Molecular Analysis of Transporters and Tight Junctions
This protocol provides the molecular context for the functional data obtained from the glucose uptake and TEER assays.
- Sample Collection: After functional assays, wash the cell monolayers with PBS and lyse the cells directly on the Transwell membrane to extract total RNA for gene expression analysis or protein for Western Blot analysis.
- Gene Expression (qRT-PCR):
- Synthesize cDNA from the extracted RNA.
- Perform quantitative real-time PCR (qRT-PCR) using primers for genes of interest:
- Glucose Transporters: SGLT1 (SLC5A1), GLUT2 (SLC2A2)
- Tight Junction Proteins: ZO-1 (TJP1), Occludin (OCLN), Claudins (e.g., CLDN1)
- Normalize expression data to a stable housekeeping gene (e.g., GAPDH, β-actin) [49] [69].
- Protein Analysis (Western Blot):
- Separate proteins by SDS-PAGE and transfer to a membrane.
- Probe the membrane with specific primary antibodies against GLUT2, SGLT1, ZO-1, and Occludin.
- Use fluorescent or HRP-conjugated secondary antibodies for detection. Normalize protein levels to a loading control (e.g., Vinculin, β-actin) [49] [68].
Data Integration and Correlation Analysis
The power of this multi-assay approach lies in the integration of the generated data. The following diagram conceptualizes the key relationships and correlations that can be investigated.
The following table provides an example of how quantitative data from the different assays can be compiled and interpreted in a correlated manner.
Table 3: Example of Correlated Multi-Assay Data Output
| Experimental Group | Glucose Uptake (nmol/mg protein) | GLUT2 Protein Level (% of Control) | TEER (Ω·cm²) | ZO-1 Protein Level (% of Control) | Integrated Interpretation |
|---|---|---|---|---|---|
| Control | 100.0 ± 5.0 | 100 ± 5 | 350 ± 25 | 100 ± 8 | Baseline function and expression. |
| 6-Shogaol [49] | 65.0 ± 4.5 * | 68 ± 2 * | 118 ± 5 * | 200 ± 10 * | Compound inhibits glucose uptake, likely by downregulating GLUT2, while simultaneously enhancing barrier integrity by upregulating ZO-1. |
| POE Extract [68] | 75.0 ± 3.0 * | 70 ± 3 * | 118 ± 3 * | 200 ± 15 * | Natural extract reduces glucose transport via GLUT2 downregulation and strengthens the epithelial barrier. |
| High Glucose [69] | [Expected Increase] | [Expected Increase] | ~50 ± 10 * | [Expected Decrease] | High glucose environment increases permeability and is associated with barrier dysfunction, despite potential increases in transporter expression. |
Note: Data are illustrative examples based on literature. * indicates a significant difference compared to the control group.
The integrated methodological approach detailed in this application note—combining functional glucose uptake assays, real-time monitoring of barrier integrity (TEER), and molecular analyses—provides a powerful and robust framework for studying intestinal glucose metabolism and barrier function in the Caco-2/TC7 model. The correlation of data across these assays, as exemplified in the results section, offers profound mechanistic insights that are not attainable through single-assay approaches. This multi-parametric strategy is highly relevant for research in drug discovery, nutraceutical development, and toxicology, enabling a more predictive in vitro assessment of compound effects on critical intestinal functions.
The Caco-2/TC7 intestinal epithelial cell model serves as a powerful platform for investigating the complex interplay between metabolic diseases, inflammation, and viral infection pathogenesis. This application note details established protocols for utilizing this in vitro system to study the regulation of intestinal glucose transporters and SARS-CoV-2 viral entry receptors, which share common regulatory pathways in response to inflammatory stimuli and pharmacological agents. The documented methodologies support research into the mechanisms underlying steroid-induced hyperglycemia, post-COVID metabolic sequelae, and the screening of therapeutic compounds for metabolic and infectious diseases.
Key Experimental Findings and Quantitative Data
Table 1: Summary of Key Experimental Effects on Gene Expression in Caco-2/TC7 Cells
| Experimental Treatment | SGLT1 | GLUT2 | ACE2 | TMPRSS2 | Primary Functional Outcome | Citation |
|---|---|---|---|---|---|---|
| Dexamethasone (5-20 µM) | ↑ mRNA (Dose-dependent) | ↓ mRNA (In cells); ↑ mRNA (In mice) | ↓ mRNA & Protein | ↑ mRNA | Enhanced intestinal glucose uptake; Modulated viral receptor availability | [10] |
| Pro-inflammatory Cytokines (IL-1β & TNF-α) | ↑ mRNA | ↓ mRNA | ↑ mRNA | ↑ mRNA | Increased glucose absorption potential; Altered viral entry site expression | [75] [19] |
| Phytochemical: Genistein | Normalized inflammation-induced ↑ | Information Missing | Not Significant | Normalized inflammation-induced ↑ | Reduced inflammation-driven SGLT1/TMPRSS2 upregulation; Potential to lower postprandial glycaemia and COVID-19 risk | [75] [19] |
| Dietary Protein Digests (e.g., Casein, Fish Gelatin) | Information Missing | ↓ mRNA | Not Studied | Not Studied | Decreased intestinal glucose absorption; Improved glucose tolerance in vivo | [22] |
Table 2: Key Research Reagent Solutions for Caco-2/TC7-Based Disease Modeling
| Reagent / Kit | Function / Target | Example Application in Protocol |
|---|---|---|
| Differentiated Caco-2/TC7 Cells | Human intestinal epithelial model with enterocyte-like properties | Core model for all studies of glucose transport and viral receptor expression [10] [22] [19]. |
| Dexamethasone | Synthetic glucocorticoid receptor agonist | Used to model steroid-induced diabetes and its effects on glucose transporters and ACE2/TMPRSS2 [10]. |
| Recombinant Human IL-1β & TNF-α | Pro-inflammatory cytokines | Applied to induce a chronic low-grade inflammation model relevant to diabetes and COVID-19 [75] [19]. |
| Phytochemicals (Genistein, Apigenin, etc.) | Natural compounds with potential anti-inflammatory and glucose-modulating effects | Screened for ability to normalize inflammation-induced changes in SGLT1 and TMPRSS2 [75] [19]. |
| TaqMan ddPCR Primers/Probes | Quantitative digital PCR for gene expression analysis | Target genes: ACE2, TMPRSS2, SGLT1, GLUT2, and housekeeping genes (e.g., TBP) [10] [19]. |
| ELISA Kits (e.g., ACE2, IL-8) | Protein-level quantification | Validation of gene expression results and measurement of inflammatory markers [10] [19]. |
| 2-deoxy-D-glucose / α-methyl-D-glucopyranoside | Non-metabolizable glucose analogs | Used in transport assays to specifically measure glucose uptake activity [10] [22]. |
Detailed Experimental Protocols
Protocol 1: Modeling Dexamethasone-Induced Dysregulation of Glucose Transport and Viral Receptors
Objective: To investigate the direct effects of the corticosteroid dexamethasone on the expression of intestinal glucose transporters (SGLT1, GLUT2) and SARS-CoV-2 viral entry receptors (ACE2, TMPRSS2) [10].
Materials:
- Differentiated Caco-2/TC7 cell monolayers (21-day culture)
- Dexamethasone (e.g., Merck Life Science), prepared as a 20 mM stock in DMSO
- Serum-free DMEM culture media (with 5.5 mM or 25 mM glucose)
- RNA extraction kit (e.g., Aurum Total RNA Mini Kit, Bio-Rad)
- Droplet Digital PCR (ddPCR) system and TaqMan assays for SGLT1, GLUT2, ACE2, TMPRSS2, and a housekeeping gene (e.g., TBP)
- ACE2 ELISA kit (e.g., Abcam ab235649)
Procedure:
- Cell Culture and Differentiation: Culture Caco-2/TC7 cells in high-glucose (25 mM) DMEM supplemented with 20% FBS, 2% non-essential amino acids, 2% Glutamax, and 1% penicillin-streptomycin. For experiments, seed cells on Transwell inserts (0.4 µm pore size) and differentiate for 21 days. In the final week, consider using media with different glucose concentrations (e.g., 5.5 mM vs. 25 mM) to model different glycemic conditions [10].
- Dexamethasone Treatment: On day 19 of differentiation, replace the medium in both apical and basolateral compartments with serum-free medium containing dexamethasone at final concentrations of 5, 10, or 20 µM (from the DMSO stock, ensuring final DMSO concentration is 0.1% v/v). Include a vehicle control (0.1% DMSO). Refresh the treatment medium every 12 hours for a total treatment duration of 60 hours [10].
- Gene Expression Analysis (ddPCR):
- Protein Analysis (ELISA):
- Functional Glucose Uptake Assay (Optional):
- Following treatment, assay glucose transport using a non-metabolizable analog like 2-deoxy-D-glucose.
- Incubate cells with the glucose analog in Krebs-Ringer buffer.
- Stop uptake with ice-cold PBS containing phlorizin (an SGLT1 inhibitor). Measure accumulated radiolabel or analog concentration via scintillation counting or other detection methods [10] [22].
Protocol 2: Investigating the Impact of Inflammation and Phytochemical Intervention
Objective: To model inflammation-driven co-regulation of glucose transporters and viral entry factors and to screen for phytochemicals that can normalize these changes [75] [19].
Materials:
- Differentiated Caco-2/TC7 cell monolayers (14-day culture)
- Recombinant Human IL-1β and TNF-α (e.g., Merck Life Science)
- Phytochemicals: Genistein, Apigenin, Artemisinin, Sulforaphane (e.g., Merck Life Science), dissolved in DMSO or as recommended
- ddPCR reagents and TaqMan assays (as in Protocol 1)
- ELISA kits for IL-8 and/or IL-6 (e.g., Abcam, EMD Millipore)
Procedure:
- Inflammation Model Optimization:
- Differentiate Caco-2/TC7 cells on Transwell plates for 14 days.
- To establish an inflammation model, stimulate cells by adding a combination of IL-1β (e.g., 10 ng/mL) and TNF-α (e.g., 50 ng/mL) to the basolateral compartment. Treat for durations ranging from 4 to 168 hours, refreshing cytokines every 48 hours [19].
- Monitor inflammatory response by measuring secreted IL-8 via ELISA.
- Phytochemical Screening:
- Gene and Protein Expression Analysis:
- Data Correlation: Perform statistical analysis (e.g., Pearson correlation) to investigate relationships between changes in inflammatory markers (IL-8), glucose transporters, and viral receptors [75] [19].
Signaling Pathways and Mechanistic Workflows
The following diagrams illustrate the core mechanistic insights and experimental workflows derived from the cited research.
Diagram 1: Proposed coregulation of SGLT1 and TMPRSS2. This diagram summarizes experimental evidence suggesting that inflammation and dexamethasone trigger an unknown common regulatory pathway leading to the simultaneous upregulation of the glucose transporter SGLT1 and the viral entry protease TMPRSS2, while downregulating the ACE2 receptor. The phytochemical genistein appears to normalize these changes [10] [75] [19].
Diagram 2: Two-phase workflow for disease modeling and compound screening. This standardized workflow shows the process of first establishing a disease model (inflammation or dexamethasone-induced) and then using that validated model to screen for therapeutic compounds that can normalize the observed pathophysiological changes [10] [75] [19].
Conclusion
The Caco-2/TC7 cell model remains an indispensable and physiologically relevant tool for studying intestinal glucose transport. Mastering its use—from foundational biology and robust protocol establishment to sophisticated troubleshooting and validation—is paramount for generating reliable, translatable data in metabolic research and drug discovery. Future directions will likely see increased integration of genetic engineering, complex co-culture systems, and novel analytical techniques like FTIR spectroscopy to further enhance the model's predictive power for human absorption and disease mechanisms, ultimately accelerating the development of novel therapeutics for diabetes and related metabolic disorders.
References
- 1. Regulation of Glucose Transporter Expression in Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3827299/]
- 2. A Study Using CaCo-2 Cells As an In Vitro Model of the ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0167785]
- 3. Glucose transporters in the small intestine in health and disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC7462918/]
- 4. Sodium Glucose Cotransporter 1 - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/sodium-glucose-cotransporter-1]
- 5. Mechanisms of Glucose Absorption in the Small Intestine ... [https://www.mdpi.com/2072-6643/13/7/2474]
- 6. Hypoglycemic effect and intestinal transport of phenolics ... [https://www.sciencedirect.com/science/article/abs/pii/S0963996923012371]
- 7. Caco-2 - Wikipedia [https://en.wikipedia.org/wiki/Caco-2]
- 8. Caco-2/TC-7 Human Colon Adenocarcinoma Cell Line [https://www.sigmaaldrich.com/US/en/product/mm/scc209?srsltid=AfmBOop64SSf6ugFMl9bimvD-V_GLaQ2K6BdnIoAU6eba7stlWVZ5UZw]
- 9. Caco-2 Cell Line - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/medicine-and-dentistry/caco-2-cell-line]
- 10. Dexamethasone enhances intestinal glucose absorption and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12583508/]
- 11. Impact of Glucose, Inflammation and Phytochemicals on ... [https://www.mdpi.com/2076-3921/14/3/253]
- 12. Short Caco-2 model for evaluation of drug permeability [https://www.sciencedirect.com/science/article/abs/pii/S0378517324006495]
- 13. Characterization of SGLT1-mediated glucose transport in ... [https://www.sciencedirect.com/science/article/abs/pii/S0014299921000789]
- 14. Insulin internalizes GLUT2 in the enterocytes of healthy but ... [https://pubmed.ncbi.nlm.nih.gov/18057092/]
- 15. Relevance of sodium/glucose cotransporter-1 (SGLT1) to ... [https://www.sciencedirect.com/science/article/abs/pii/S0739724013000088]
- 16. Thyroid hormone regulation of the Na+/glucose ... [https://pubmed.ncbi.nlm.nih.gov/9729472/]
- 17. Attenuation of glucose transport across Caco-2 cell ... [https://pubmed.ncbi.nlm.nih.gov/23361943/]
- 18. Inhibition of human starch digesting enzymes and intestinal ... [https://www.sciencedirect.com/science/article/pii/S0963996924006422]
- 19. Impact of Glucose, Inflammation and Phytochemicals on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11939507/]
- 20. Editorial: Diverse functions of drug transporters - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535901/]
- 21. Transport, metabolism and remedial potential of functional ... [https://www.sciencedirect.com/science/article/abs/pii/S0963996920302659]
- 22. An Exploratory Study of the Role of Dietary Proteins in ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2021.769773/full]
- 23. The third dimension: new developments in cell culture models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11108567/]
- 24. Caco-2 Cells for Measuring Intestinal Cholesterol Transport [https://biologicalproceduresonline.biomedcentral.com/articles/10.1186/s12575-020-00120-w]
- 25. Dexamethasone enhances intestinal glucose absorption ... [https://www.nature.com/articles/s41598-025-22312-8]
- 26. Caco-2 Cell Culture & Gene Editing Tips [https://www.ubigene.us/application/caco-2-cells-tips.html]
- 27. Validation of Knock-Out Caco-2 TC7 Cells as Models ... [https://www.mdpi.com/2072-6643/15/3/505]
- 28. Caco-2 Cell Line Standardization with Pharmaceutical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10674574/]
- 29. Comparison of Glucose Uptake Assay Methods [https://www.promega.com/resources/pubhub/comparison-of-glucose-uptake-assay-methods/]
- 30. Acute Effects of Sugars and Artificial Sweeteners on Small ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5161324/]
- 31. Caco-2/TC7 cell line characterization for intestinal absorption: how reliable is this in vitro model for the prediction of the oral dose fraction absorbed in human? - PubMed [https://pubmed.ncbi.nlm.nih.gov/20732406/]
- 32. Regulation of Glucose Transporter Expression in Human ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0078932]
- 33. Glucose Uptake and Oxidative Stress in Caco-2 Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC9319946/]
- 34. Alvetex Scaffold Protocol: Caco-2 Cell Line (Inserts & Plates) [https://www.reprocell.com/resources/protocols/alvetex-scaffold/d015-caco-2-cell-line]
- 35. High Throughput Screening to Identify Glut1 Modulators [https://www.g1dfoundation.org/high-throughput-screening-to-identify-glut1-activators/]
- 36. Identification of glucose transport modulators in vitro and ... [https://pubmed.ncbi.nlm.nih.gov/36635085/]
- 37. Impact of Delta SARS-CoV-2 Infection on Glucose Metabolism [https://pmc.ncbi.nlm.nih.gov/articles/PMC10893195/]
- 38. An arrayed CRISPR knockout screen identifies genetic ... [https://www.nature.com/articles/s41598-023-48361-5]
- 39. The Transport and Uptake of Resveratrol Mediated via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10301264/]
- 40. Complexification of In Vitro Models of Intestinal Barriers, A ... [https://www.mdpi.com/1422-0067/24/4/3595]
- 41. Rho-ROCK liberates sequestered claudin for rapid de novo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289309/]
- 42. Rho-ROCK liberates sequestered claudin for rapid de novo ... [https://elifesciences.org/articles/102794]
- 43. Post-click labeling enables highly accurate single cell ... [https://www.nature.com/articles/s42003-024-06164-y]
- 44. Remodeling of Tight Junctions and Enhancement of Barrier ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4520484/]
- 45. Rapid Reduction of Pro-Inflammatory Cytokines with an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12112298/]
- 46. IL-1 family cytokines in inflammation and immunity [https://www.nature.com/articles/s41423-025-01358-8]
- 47. New natural pro-inflammatory cytokines (TNF-α, IL-6 and ... [https://www.sciencedirect.com/science/article/abs/pii/S1567576923002606]
- 48. Functional expression of SGLTs in rat brain - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3006325/]
- 49. Effects of 6-Shogaol on Glucose Uptake and Intestinal ... [https://www.mdpi.com/2304-8158/12/3/503]
- 50. The influence of fruit juice extracts on glucose intestinal ... [https://pubs.rsc.org/en/content/articlehtml/2025/fo/d4fo03950e]
- 51. Applications of the Caco-2 model in the design and ... [https://www.sciencedirect.com/science/article/pii/S0169409X96004279]
- 52. FTIR spectroscopy as a novel analytical approach for ... [https://www.sciencedirect.com/science/article/abs/pii/S1386142520303668]
- 53. Advances in Fourier infrared spectroscopy for noninvasive ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X24018769]
- 54. Analysis of glucose concentrations in blood solutions using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12265447/]
- 55. Precision Signal Boost for Non-Invasive Blood-Glucose ... [https://www.spectroscopyonline.com/view/precision-signal-boost-for-non-invasive-blood-glucose-tests-with-advanced-ft-ir-and-machine-learning]
- 56. Upgrading In Vitro Digestion Protocols with Absorption ... [https://www.mdpi.com/2076-3417/14/18/8320]
- 57. Spatially Resolved Measurement of Dynamic Glucose Uptake ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7701360/]
- 58. Caco-2 cell monolayers as a model for drug transport ... [https://pubmed.ncbi.nlm.nih.gov/2235888/]
- 59. Caco-2 monolayers in experimental and theoretical ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X12002657]
- 60. Sar1b mutant mice recapitulate gastrointestinal abnormalities ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8175419/]
- 61. Validation of Knock-Out Caco-2 TC7 Cells as Models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9921550/]
- 62. In vitro glucose uptake assay [https://bio-protocol.org/exchange/minidetail?id=6683060&type=30]
- 63. Mechanisms of Glucose Uptake in Intestinal Cell Lines [https://pmc.ncbi.nlm.nih.gov/articles/PMC3237888/]
- 64. Development of a Caco-2-based intestinal mucosal model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11702969/]
- 65. Caco-2/HT29-MTX co-cultured cells as a model for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8496855/]
- 66. Caco-2/HT29-MTX co-cultured cells as a model for studying ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0257824]
- 67. In vitro models replicating the human intestinal epithelium ... [https://www.sciencedirect.com/science/article/pii/S0168365921002522]
- 68. Glucose Uptake and Oxidative Stress in Caco-2 Cells [https://www.mdpi.com/1660-3397/20/7/457]
- 69. Glucose but Not Fructose Alters the Intestinal Paracellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8744209/]
- 70. A Shared Perspective on in Vitro and in Vivo Models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10723066/]
- 71. Multiparametric temporal analysis of the Caco-2/TC7 ... [https://www.ovid.com/journals/ejops/pdf/10.1016/j.ejps.2015.02.013~multiparametric-temporal-analysis-of-the-caco-2tc7]
- 72. Caco-2 Cells for Measuring Intestinal Cholesterol Transport [https://pmc.ncbi.nlm.nih.gov/articles/PMC7149936/]
- 73. Good Caco-2 cell culture practices [https://www.sciencedirect.com/science/article/abs/pii/S0887233312000707]
- 74. Evaluation of Caco-2 and human intestinal epithelial cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9304606/]
- 75. Impact of Glucose, Inflammation and Phytochemicals on ... [https://pubmed.ncbi.nlm.nih.gov/40227199/]