Insulin's Multimeric Blueprint: A Structural Guide to Monomers, Dimers, and Therapeutic Hexamers
This comprehensive review dissects the structural architecture of insulin across its monomeric, dimeric, and hexameric states, detailing their biological relevance and therapeutic implications.
Insulin's Multimeric Blueprint: A Structural Guide to Monomers, Dimers, and Therapeutic Hexamers
Abstract
This comprehensive review dissects the structural architecture of insulin across its monomeric, dimeric, and hexameric states, detailing their biological relevance and therapeutic implications. Targeting researchers and drug developers, the article explores foundational biophysical principles, modern analytical methodologies for studying assembly, common challenges in formulation stability, and comparative validation of novel insulin analogs. The synthesis provides a roadmap for leveraging structural knowledge to design next-generation insulin therapies with optimized pharmacokinetic profiles.
From Chain to Complex: Decoding the Structural Hierarchy of Insulin
Within the broader architectural research of insulin monomers, dimers, and hexamers, the primary structure—the linear amino acid sequence and its invariant disulfide bonds—serves as the fundamental blueprint. This covalent framework dictates all higher-order folding, assembly, and ultimately, the hormone's biological activity and stability. For researchers and drug development professionals, a precise understanding of this foundation is critical for rational design of insulin analogs and formulations.
The Canonical Primary Structure of Human Insulin
Human insulin is synthesized as preproinsulin. The mature, active hormone consists of two polypeptide chains: the A-chain (21 amino acids) and the B-chain (30 amino acids). These chains are covalently linked by two interchain disulfide bonds. An additional intrachain disulfide bond stabilizes the A-chain fold.
Table 1: Primary Structure and Disulfide Bonds of Human Insulin
| Feature | A-Chain | B-Chain | Linkage |
|---|---|---|---|
| Residue Count | 21 aa | 30 aa | — |
| Disulfide Bonds | CysA6-CysA11 (intrachain) | — | — |
| Interchain Disulfide Bonds | CysA7 ←→ CysB7 | CysB7 ←→ CysA7 | Covalent (S-S) |
| CysA20 ←→ CysB19 | CysB19 ←→ CysA20 | Covalent (S-S) | |
| Isoelectric Point (pI) | ~5.3 – 5.4 (monomer) |
The Role of Primary Structure in Quaternary Architecture
The specific amino acid sequence, particularly at dimer and hexamer contact surfaces, directly enables the assembly of insulin monomers into higher-order structures. Key residues involved in dimerization (mostly B-chain) and zinc-mediated hexamer formation (B10, B14, B17) are invariant or conservatively substituted, underscoring their structural importance.
Table 2: Key Residues Governing Insulin Self-Assembly
| Assembly State | Critical Residues | Role | Experimental Perturbation Effect |
|---|---|---|---|
| Dimer Interface | PheB24, TyrB26, ProB28, PheB25 | Hydrophobic core & van der Waals contacts | Mutation disrupts dimerization, alters pharmacokinetics. |
| Hexamer Interface (Zinc binding) | HisB10 (Critical), GluB13, HisB5, HisB14 | Coordinate Zn²⁺ ions at hexamer axis | Substitution abolishes Zn²⁺ binding, prevents hexamer formation. |
| Monomer Stability | Cys residues (A6-A11, A7-B7, A20-B19) | Maintain native fold | Reduction of disulfides leads to irreversible unfolding & loss of activity. |
Experimental Protocols for Primary Structure Analysis
Protocol: Determination of Disulfide Bond Connectivity via Peptide Mapping
- Objective: To experimentally verify the canonical disulfide pairings (A6-A11, A7-B7, A20-B19) in a purified insulin sample.
- Materials: Lyophilized human insulin or analog, trypsin/chymotrypsin (sequencing grade), trifluoroacetic acid (TFA), HPLC system with C18 column, mass spectrometry (MALDI-TOF or ESI-MS).
- Method:
- Denaturation & Proteolysis: Dissolve 1 mg insulin in 100 µL of 6 M guanidine HCl, pH 8.0. Dilute 10-fold with 50 mM ammonium bicarbonate to reduce denaturant concentration. Add protease (enzyme:substrate 1:50 w/w) and incubate at 37°C for 4-16 hours.
- HPLC Separation: Quench digestion with 1% TFA. Separate peptide fragments by reverse-phase HPLC using a 0-60% acetonitrile gradient in 0.1% TFA.
- Mass Spectrometry Analysis: Collect individual peaks. Analyze by mass spectrometry to determine molecular weights of disulfide-linked peptide pairs (e.g., A-chain peptide containing Cys7 linked to B-chain peptide containing Cys7).
- Confirmation: Compare experimental masses to theoretical digests. Confirm linkages by comparing reduced vs. non-reduced digests.
Protocol: Assessing Oligomeric State via Size-Exclusion Chromatography (SEC)
- Objective: To separate and quantify insulin monomers, dimers, and hexamers based on solution conditions.
- Materials: HPLC/FPLC system, Superdex 75 Increase column, mobile phases (e.g., 100 mM sodium phosphate, pH 7.4 with/without 0.1 mM ZnCl₂), insulin sample.
- Method:
- Condition Equilibration: Equilibrate SEC column with ≥2 column volumes of desired mobile phase (without Zn²⁺ for monomer/dimer, with 0.1 mM ZnCl₂ for hexamer stabilization).
- Sample Preparation: Dissolve insulin at 1 mg/mL in the corresponding mobile phase. Centrifuge to remove particulates.
- Chromatography: Inject 50 µL sample. Run isocratic elution at 0.5 mL/min. Monitor absorbance at 280 nm.
- Analysis: Identify peaks using molecular weight standards. Hexamers (~36 kDa) elute first, followed by dimers (~12 kDa), then monomers (~6 kDa).
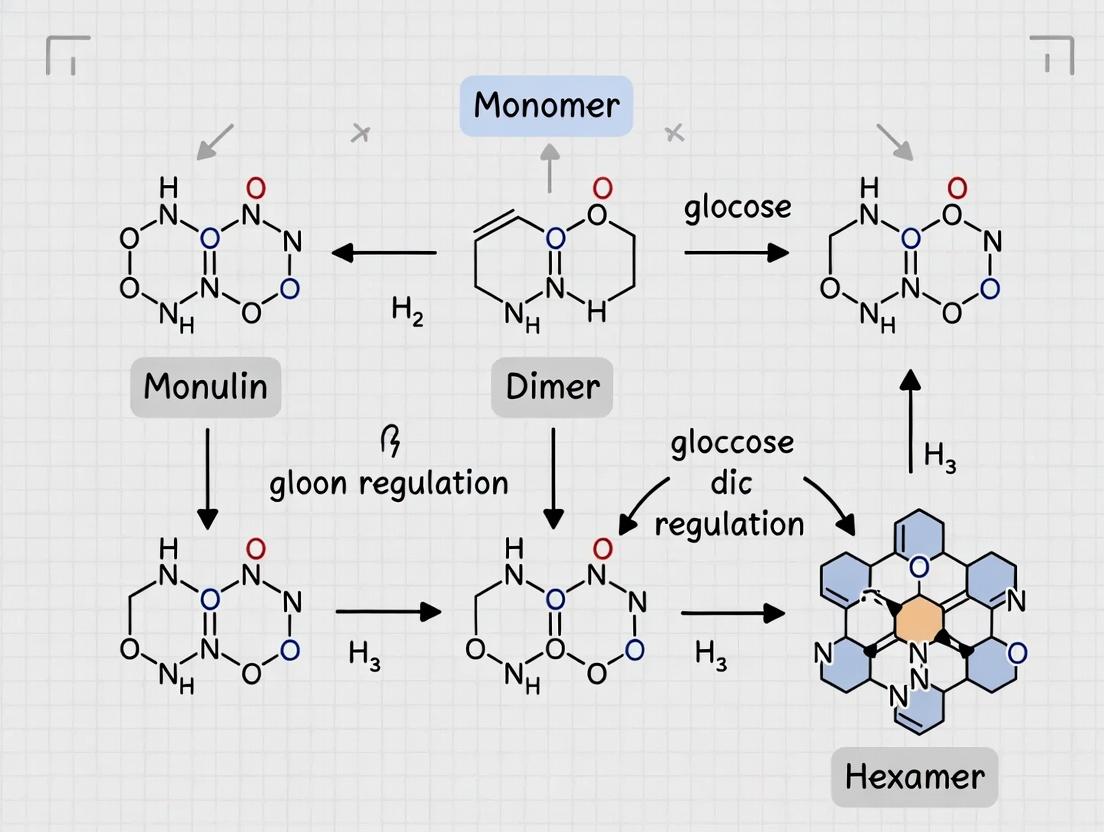
Visualization of Structural Determinants
Diagram Title: Insulin Assembly Pathway from Sequence
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Insulin Primary & Quaternary Structure Research
| Reagent/Material | Function/Application | Key Consideration |
|---|---|---|
| Recombinant Human Insulin (Std.) | Gold-standard control for comparative studies of analogs. | Ensure high purity (>99%) and documented disulfide integrity. |
| Zinc Chloride (ZnCl₂) | Essential for hexamer stabilization in formulations & crystallography. | Concentration critical (typically 0.01-0.1 mM per hexamer). |
| Phenol or m-Cresol | Hexamer-stabilizing ligand & antimicrobial preservative. | Used in commercial formulations; affects assembly kinetics. |
| Dithiothreitol (DTT) / TCEP | Reducing agents for disulfide bond cleavage (control experiments). | Use under denaturing conditions to ensure complete reduction. |
| Guanidine HCl / Urea | Chaotropic agents for denaturation prior to refolding or digestion studies. | High purity grade required to avoid carbamylation (urea). |
| Trypsin (Sequencing Grade) | Proteolytic digestion for peptide mapping & disulfide analysis. | Modified trypsin prevents autolysis, improves specificity. |
| SEC Column (e.g., Superdex 75) | Separation of insulin oligomers based on hydrodynamic radius. | Run at 4°C to minimize on-column association/dissociation. |
| NMR isotopes (¹⁵N, ¹³C-labeled Insulin) | For high-resolution solution structure & dynamics studies. | Requires bacterial expression system for cost-effective labeling. |
Within the broader architectural study of insulin monomers, dimers, and hexamers, defining the active monomeric conformation is a fundamental challenge. The insulin receptor (IR) is activated by insulin in its monomeric state, yet the hormone is stored as hexamers and circulates as dimers. This whitepaper details the current understanding of the insulin monomer's bioactive conformation and the critical surfaces mediating IR binding, synthesizing recent structural and biophysical data.
The Active Monomeric Conformation
The active monomer is characterized by a conformational shift from its T-state (tense, hexamer-associated) to an R-state (relaxed). Key changes involve the B-chain C-terminus (B24-B30), which swings away from the hormone's core, exposing residues critical for receptor engagement.
Table 1: Key Structural Parameters of Insulin Conformations
| Parameter | T-state (Hexamer) | R-state (Monomer, Receptor-Bound) | Measurement Technique |
|---|---|---|---|
| B24-B30 Conformation | Extended β-strand | Disordered/α-helical | X-ray Crystallography, NMR |
| Distance between α-carbons of B12 Val & B24 Phe | ~12 Å | ~16 Å | Molecular Dynamics Simulation |
| TyrB26 Side Chain Orientation | Buried in dimer interface | Exposed to solvent | HDX-MS, Fluorescence |
| Insulin pKa (HisB10) | ~7.0 | ~6.4 | NMR Titration |
Receptor-Binding Surfaces
IR binding is mediated by two primary surfaces on the insulin monomer.
Table 2: Key Insulin Residues in IR Binding Surfaces
| Binding Surface | Critical Residues (Human Insulin) | Proposed Role in IR Engagement | ΔΔG upon Ala Mutation (kcal/mol)* |
|---|---|---|---|
| Classic Binding Site 1 | GlyA1, GlnA5, TyrA19, AsnA21, ValB12, TyrB16, PheB24, PheB25, TyrB26 | High-affinity interaction with IR L1 domain | -1.5 to -3.2 |
| Novel Binding Site 2 | SerA12, LeuA13, GluA17, HisB10, GluB13 | Secondary interaction with IR FnIII-1 domain | -0.8 to -1.7 |
| Allosteric "Switch" Region | GlyB8, SerB9, HisB10, GluB13 | Stabilizes active monomer conformation | N/A |
*Representative data from recent site-directed mutagenesis and isothermal titration calorimetry (ITC) studies.
Experimental Protocols
Generating Stable Monomers for Study
Protocol: Preparation of Monomeric Insulin via Site-Directed Mutagenesis (B9-B9′ Ser→Asp)
- Gene Cloning: Clone the human insulin gene with a B9 Ser→Asp (S9D) mutation into an E. coli expression vector (e.g., pET-3a) for recombinant production.
- Expression & Inclusion Body Isolation: Express the proinsulin-S9D analog in E. coli BL21(DE3). Harvest cells, lyse, and pellet inclusion bodies.
- Refolding & Purification: Solubilize inclusion bodies in 8M urea, 0.1M Tris, pH 10.7. Refold by rapid dilution into 0.1M Tris, 0.5M Arg-HCl, 2mM EDTA, 0.1mM oxidized glutathione, 1mM reduced glutathione, pH 10.7. Purify folded proinsulin analog via anion-exchange chromatography.
- Enzymatic Cleavage & Final Purification: Digest with trypsin and carboxypeptidase B to yield insulin-S9D. Purify the monomeric analog via reverse-phase HPLC (C18 column, acetonitrile/0.1% TFA gradient).
- Validation: Confirm monomeric state via analytical ultracentrifugation (AUC) at 50 µM in PBS, pH 7.4.
Determining Receptor-Binding Kinetics
Protocol: Surface Plasmon Resonance (SPR) for Insulin-IR Affinity Measurement
- Sensor Chip Preparation: Immobilize the purified soluble insulin receptor extracellular domain (sIR-ECD) on a CMS Series S chip using amine coupling chemistry to achieve ~5000 Response Units (RU).
- Running Buffer: HBS-EP+ (10mM HEPES, 150mM NaCl, 3mM EDTA, 0.05% v/v Surfactant P20, pH 7.4).
- Kinetic Analysis: Inject insulin monomer analogs in a 2-fold dilution series (0.78 nM to 100 nM) over the sIR-ECD surface at 30 µL/min. Association phase: 180 sec. Dissociation phase: 600 sec in buffer.
- Data Processing: Reference flow cell data is subtracted. Fit sensograms to a 1:1 Langmuir binding model using Biacore Evaluation Software to derive association (ka) and dissociation (kd) rate constants. Calculate equilibrium dissociation constant KD = kd/ka.
Probing Conformational Dynamics
Protocol: Hydrogen-Deuterium Exchange Mass Spectrometry (HDX-MS)
- Labeling: Dilute insulin (monomeric analog vs. wild-type zinc hexamer) 10-fold into D2O-based labeling buffer (PBS, pD 7.4). Incubate at 25°C for 10 sec to 4 hours.
- Quenching: Lower pH to 2.5 with pre-chilled quench buffer (0.1 M phosphate, 0.5 M TCEP, pH 2.2).
- Digestion & Analysis: Inject onto an immobilized pepsin column at 0°C. Trap peptides on a C18 UPLC column, separate with a 5-40% acetonitrile gradient, and analyze by high-resolution MS.
- Data Interpretation: Calculate deuterium uptake for identified peptides. Regions with decreased uptake in the monomer vs. hexamer indicate protection due to structural stabilization or new interactions.
Visualizations
Diagram 1: Path from Storage Hexamer to Active Monomer
Diagram 2: Insulin Monomer Binding Surfaces Engage Distinct IR Domains
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Function & Rationale |
|---|---|
| Monomeric Insulin Analogs (e.g., S9D, B28 Asp) | Engineered to prevent dimer/hexamer formation; essential for studying the true receptor-binding species. |
| Soluble IR Extracellular Domain (sIR-ECD) | Purified recombinant protein for in vitro binding assays (SPR, ITC) without full receptor transmembrane complications. |
| Site-Directed Mutagenesis Kits | For systematic alanine scanning of putative binding surface residues to map functional epitopes. |
| Hydrogen-Deuterium Exchange (HDX) Buffers | High-purity D2O and quench buffers are critical for reproducible HDX-MS conformational dynamics studies. |
| Biacore Series S CMS Sensor Chip | Gold-standard SPR surface for covalent immobilization of sIR-ECD for kinetic binding analyses. |
| Analytical Ultracentrifugation (AUC) Cells | Equipped with sapphire windows for high-speed sedimentation equilibrium experiments to definitively quantify oligomeric state. |
| C18 Reverse-Phase HPLC Columns | For high-resolution purification of insulin analogs, separating closely related conformational variants. |
This whitepaper examines the molecular architecture driving insulin dimerization, with a specific focus on the contribution of hydrophobic interactions and the central role of the B-chain β-sheet. Framed within the broader thesis on the architecture of insulin monomers, dimers, and hexamers, this guide provides a technical dissection of the forces governing this initial quaternary association. The dimer interface, primarily mediated by the B-chain, serves as the foundational module for subsequent hexamer formation, a critical consideration in therapeutic insulin formulation and stability engineering.
Insulin function and stability are inextricably linked to its quaternary structure. The dimer represents the fundamental protein-protein interaction unit, preceding zinc-mediated hexamer formation. Dimerization is primarily driven by hydrophobic forces, with the B-chain β-sheet (residues B24-B28) forming a central, antiparallel interface. This association reduces the solvent-accessible hydrophobic surface area and creates the structural template necessary for hexamer assembly. Understanding this dimeric architecture is paramount for research aimed at modulating insulin pharmacokinetics, stability, and design of novel analogs.
Structural Basis of the Dimer Interface
The insulin dimer is formed by the reciprocal association of two monomers. The core interaction involves the formation of a four-stranded, antiparallel β-sheet comprised of the B24-B28 strands from each monomer. This sheet is stabilized by main-chain hydrogen bonds and reinforced by extensive van der Waals contacts between hydrophobic side chains.
Key Structural Features:
- Antiparallel β-Sheet: Strands B24-B28 (sequence: FFYTP) from each monomer pair to form the sheet's core.
- Hydrophobic Core: Side chains of Phe B24, Tyr B26, and Pro B28 are deeply buried at the interface.
- Peripheral Interactions: Residues from the B-chain C-terminus (B29-B30) and the A-chain also contribute to stabilizing the dimer.
Table 1: Key Residues in the Insulin Dimer Interface
| Residue | Chain | Role in Dimerization | Interaction Type |
|---|---|---|---|
| Phe B24 | B | Primary hydrophobic contact | π-π stacking & van der Waals |
| Tyr B26 | B | Hydrophobic & hydrogen bonding | van der Waals, potential OH interaction |
| Pro B28 | B | Structural constraint; hydrophobic | van der Waals |
| Thr B27 | B | Sidechain orientation; moderate contribution | Hydrogen bonding to solvent/backbone |
| Lys B29 | B | Peripheral electrostatic stabilization | Salt bridge (in some conformations) |
| C-terminal Carboxylate | B30 | Electrostatic & hydrogen bonding | Intermolecular H-bonds |
The Dominant Role of Hydrophobic Forces
Quantitative analyses confirm that hydrophobic desolvation provides the major thermodynamic driving force for dimerization. The association constant (K_dimer) for human insulin is typically in the range of 10^4 to 10^5 M^-1, corresponding to a ΔG of approximately -6 to -7 kcal/mol at physiological pH and low ionic strength. Experimental mutagenesis of interfacial hydrophobic residues (e.g., B24 Phe → Ala) can reduce dimer stability by 2-3 orders of magnitude.
Table 2: Thermodynamic and Kinetic Parameters of Insulin Dimerization
| Parameter | Value (Human Insulin, pH 7-8, 25°C) | Method | Implication |
|---|---|---|---|
| K_dimer (Association Constant) | ~1 × 10^5 M^-1 | Analytical Ultracentrifugation (AUC) | Moderately strong monomer-dimer equilibrium |
| ΔG° (kcal/mol) | -6.8 ± 0.5 | Isothermal Titration Calorimetry (ITC) | Spontaneous association |
| ΔH° (kcal/mol) | Slightly exothermic or near zero | ITC | Driven largely by entropy (hydrophobic effect) |
| -TΔS° (kcal/mol) | Major favorable contribution | ITC calculated | Highlights hydrophobic driving force |
| k_on (M^-1 s^-1) | ~10^4 | Stopped-flow Fluorescence | Diffusion-limited encounter facilitated |
| k_off (s^-1) | ~0.1 | Stopped-flow Fluorescence | Moderately stable complex |
Experimental Protocols for Studying Dimerization
Analytical Ultracentrifugation (AUC) – Sedimentation Equilibrium
Purpose: To determine the absolute molecular weight and association constant of the insulin dimer in solution. Protocol:
- Sample Preparation: Dialyze insulin solution (0.1-0.5 mg/mL) against a chosen buffer (e.g., 20 mM phosphate, 100 mM NaCl, pH 7.4). Use matching buffer for reference.
- Instrument Setup: Load sample into a 12 mm double-sector centerpiece. Use an 8-cell rotor (e.g., An-50 Ti). Set temperature to 20°C or 25°C.
- Data Acquisition: Conduct runs at multiple speeds (e.g., 18,000, 24,000, and 30,000 rpm) until equilibrium is reached (16-24 hours). Monitor absorbance at 280 nm or interference.
- Data Analysis: Fit the equilibrium concentration vs. radial position data to a monomer-dimer equilibrium model using software such as SEDPHAT or UltraScan. Extract K_dimer.
Isothermal Titration Calorimetry (ITC)
Purpose: To measure the enthalpy change (ΔH), binding constant (K_a), and stoichiometry (N) of dimerization. Protocol:
- Sample Preparation: Exhaustively dialyze insulin monomer (in syringe) and dimer (in cell) solutions against identical buffer. Degas before use.
- Instrument Setup: Fill the sample cell (typically 200 µL) with a solution expected to be predominantly dimer (e.g., 50-100 µM). Load the syringe with a concentrated monomer solution (10x higher concentration).
- Titration: Perform a series of injections (e.g., 20 injections of 2 µL) with 180-second intervals. Stir at 1000 rpm. Temperature set to 25°C.
- Data Analysis: Integrate heat peaks, subtract dilution heat, and fit the binding isotherm to a "dimerization" or "self-association" model in the instrument software to obtain ΔH, Ka (1/Kdimer), and N.
Mutagenesis & Stability Assays
Purpose: To probe the role of specific B-chain β-sheet residues. Protocol:
- Site-Directed Mutagenesis: Engineer point mutations in the human insulin gene (e.g., B24 Phe→Ala, B26 Tyr→Glu). Express and purify the analog from E. coli or yeast.
- Circular Dichroism (CD) Spectroscopy: Measure far-UV CD spectra (190-260 nm) to confirm native secondary structure is retained.
- Size-Exclusion Chromatography (SEC): Compare elution volumes of wild-type and mutant insulins on a calibrated Superdex 75 column to assess dimer/monomer distribution.
- Cross-linking Analysis: Treat insulin samples with a low concentration of a homobifunctional cross-linker (e.g., BS3). Analyze by SDS-PAGE under non-reducing conditions to visualize dimer bands.
Visualizing the Dimerization Pathway and Analysis
Diagram Title: Insulin Dimerization Pathway from Monomers
Diagram Title: Workflow for Analyzing Insulin Dimer Formation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Insulin Dimer Research
| Item | Function & Specification | Key Consideration |
|---|---|---|
| Recombinant Human Insulin | High-purity (>99%) standard for benchmarking. Source: E. coli or yeast expression. | Ensure zinc-free preparation for studying dimer-specific (not hexamer) interactions. |
| Site-Directed Mutagenesis Kit (e.g., QuikChange) | To create B-chain β-sheet mutants (e.g., B24, B26, B28). | Verify sequence and ensure proper folding of analog via CD spectroscopy. |
| Analytical Ultracentrifuge with AUC cells | Gold-standard for determining absolute molecular weights and association constants in solution. | Requires precise buffer matching and clean optics. Use charcoal-filled Epon centerpieces. |
| Isothermal Titration Calorimeter (ITC) | Measures heat of binding for direct thermodynamic profiling of dimerization. | Demands high-purity, exhaustively dialyzed samples. Optimal concentration range is critical. |
| Size-Exclusion Chromatography Column (e.g., Superdex 75 Increase 10/300 GL) | Fast, qualitative assessment of monomer/dimer/hexamer distribution. | Calibrate with known standards. Buffer conditions (pH, ionic strength) dramatically affect equilibrium. |
| Circular Dichroism Spectrophotometer | Confirms secondary structure integrity of wild-type and mutant insulins. | Use short pathlength cuvettes (0.1 cm) for far-UV scans. High signal-to-noise is essential. |
| Cross-linking Reagent (e.g., Bis(sulfosuccinimidyl)suberate - BS3) | Chemical "snapshot" of oligomeric state in solution via SDS-PAGE. | Use fresh reagent and optimize concentration/time to avoid higher-order aggregates. |
| Phosphate & Tris Buffer Systems | Maintain precise pH (7.0-8.5) for controlling ionization states of key residues. | Avoid amines in Tris for cross-linking or labeling experiments. Include NaCl to modulate ionic strength. |
The dimerization of insulin, anchored by the hydrophobic collapse of the B-chain β-sheet, is a paradigmatic example of a specific, weak protein-protein interaction with profound biological and therapeutic consequences. Within the architectural hierarchy of insulin assembly, the dimer is the critical intermediate. Modern drug development leverages this knowledge: rapid-acting insulin analogs are engineered with disrupted dimer interfaces (e.g., via charge repulsion at B28 or B29), while stable basal formulations rely on promoting dimer and hexamer formation. Future research directions include the precise mapping of dimerization dynamics in vivo and the design of novel dimer-stabilizing agents for improved insulin storage and delivery.
Within the architectural hierarchy of insulin—monomers → dimers → hexamers—the formation of the hexamer is a critical step governing the hormone's pharmacokinetics and stability. This assembly is not spontaneous but is driven by the coordination of zinc ions (Zn²⁺) and modulated by allosteric effectors. This whitepaper provides an in-depth technical analysis of the mechanisms underpinning zinc-mediated hexamerization, the resultant allosteric transitions, and the application of this knowledge in therapeutic stabilization.
Structural Architecture and Zinc Coordination
The insulin hexamer is a symmetric assembly of three insulin dimers arranged around a central axis. The coordination of divalent zinc ions is the cornerstone of this quaternary structure.
- Primary Coordination Sites: Two zinc ions are located on the hexamer's central axis, approximately 16.4 Å apart, within a cavity formed by the three symmetry-related B10 His residues (HisB10).
- Coordination Sphere: Each Zn²⁺ is octahedrally coordinated by three B10 His imidazole nitrogens (from three different monomers) and three water molecules.
- Allosteric States: The presence of anions, most notably phenol or its derivatives, induces a conformational shift from the T-state (tense) to the R-state (relaxed) hexamer, which has higher affinity for Zn²⁺ and greater stability.
Table 1: Key Structural Parameters of Insulin Hexamer States
| Parameter | T-State (Zn²⁺ only) | R-State (Zn²⁺ + Phenol) | Reference / PDB Code |
|---|---|---|---|
| Zn²⁺-Zn²⁺ Distance | ~16.4 Å | ~16.0 Å | 4INS (T), 1EV3 (R) |
| B10 His Geometry | Slightly distorted octahedral | Regular octahedral | |
| Monomer Conformation | More extended | More compact, C-terminal B-chain α-helix stabilized | |
| Central Cavity Diameter | Larger | Smaller, more hydrophobic | |
| Thermodynamic Stability (ΔG) | Lower | Higher (by ~10-15 kJ/mol) | Recent calorimetry studies |
Allosteric Regulation of Assembly
Hexamer formation is a classic model of allosteric regulation. The binding of ligands (Zn²⁺, anions, phenolic compounds) at distinct sites communicates conformational changes across the oligomer.
- Positive Cooperativity: Zn²⁺ binding facilitates the recruitment of dimers into the hexameric complex.
- Anion-Driven Transition: Phenol derivatives bind at symmetry-related sites between monomers, stabilizing the R6 state. This closure of the B-chain C-terminal helix enhances Zn²⁺ coordination and dimer-dimer contacts.
- Pharmacological Relevance: This allosteric mechanism is exploited in formulation. Protamine (in NPH insulin) and synthetic polymers act as exogenous allosteric effectors to control hexamer dissociation kinetics post-injection.
Experimental Protocols for Studying Hexamer Assembly
Isothermal Titration Calorimetry (ITC) for Zn²⁺ Binding Affinity
Objective: Determine the stoichiometry (n), binding constant (Kd), and thermodynamic parameters (ΔH, ΔS) of Zn²⁺ binding to insulin dimers. Protocol:
- Sample Preparation: Purified recombinant human insulin (0.05-0.1 mM) in Chelex-treated buffer (e.g., 20 mM HEPES, 100 mM NaCl, pH 7.4) to remove trace metals.
- Titrant: ZnCl₂ solution (5-10 mM) in identical buffer.
- Instrument Settings: Cell temperature at 25°C. Stirring speed at 750 rpm.
- Titration: Perform 25-30 injections of 1-2 µL of ZnCl₂ into the insulin solution.
- Data Analysis: Fit corrected heat data to a "Two Sets of Sites" model to account for high-affinity hexamer coordination and lower-affinity non-specific binding.
X-ray Crystallography of Allosteric States
Objective: Obtain high-resolution structures of T- and R-state hexamers. Protocol:
- Crystallization:
- T-state: 10 mg/mL insulin, 0.05 M ZnCl₂, 0.1 M Tris-HCl pH 8.0, 20% (w/v) PEG 4000. Hanging drop vapor diffusion at 20°C.
- R-state: As above, with addition of 1-2% (v/v) m-cresol or phenol to the reservoir.
- Data Collection: Collect diffraction data at a synchrotron source (λ ~1.0 Å). Cryo-cool crystals in mother liquor with 25% glycerol.
- Structure Solution: Solve by molecular replacement using a known insulin monomer (PDB: 1TRZ). Refine with iterative cycles in PHENIX and Coot.
Analytical Ultracentrifugation (AUC) for Assembly Monitoring
Objective: Quantify the distribution of monomers, dimers, and hexamers under varying conditions. Protocol:
- Sample: Insulin at 0.5 mg/mL in desired buffer (±Zn²⁺, ±phenol).
- Run Conditions: Use a Beckman Optima AUC. Equilibrate at 20°C. Sedimentation velocity run at 50,000 rpm.
- Analysis: Use SEDFIT to model continuous c(s) distribution, identifying species by their sedimentation coefficients (~1 S for monomer, ~2 S for dimer, ~5 S for hexamer).
Visualization of Mechanisms and Workflows
Diagram Title: Zinc & Phenol-Driven Hexamer Allostery
Diagram Title: ITC Workflow for Zn²⁺ Binding
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Insulin Hexamer Research
| Reagent / Material | Function / Purpose in Research | Key Considerations |
|---|---|---|
| Recombinant Human Insulin | Primary protein for in vitro studies. Ensures absence of animal-source variants. | High purity (>99%) required for biophysics; source from reliable vendors (e.g., Sigma-Aldrich, Novo Nordisk). |
| Zinc Chloride (ZnCl₂) | Source of Zn²⁺ ions for coordination studies. | Prepare fresh stock in metal-free, acidic water (pH ~4) to prevent hydrolysis and precipitation. |
| Phenol / m-Cresol | Allosteric effector to induce and stabilize the R-state hexamer. | Handle with caution in fume hood. Used in crystallization and stability assays. |
| Chelex 100 Resin | Removes trace contaminating metal ions from buffers to ensure defined Zn²⁺ concentrations. | Must treat all buffers prior to adding protein or Zn²⁺. |
| HEPES or Tris Buffer | Maintains physiological pH (7.0-8.5) for assembly studies. | HEPES is non-coordinating; Tris can weakly bind metals. Use consistently. |
| Size-Exclusion Chromatography (SEC) Column (e.g., Superdex 75) | Separates and analyzes oligomeric states (mono/di/hexamer). | Calibrate with standards. Run with Zn²⁺/phenol in mobile phase if analyzing stabilized hexamer. |
| Crystallization Screen Kits (e.g., Hampton Research) | Initial screening for obtaining hexamer crystals under various conditions. | PEG-based screens at pH 7-9 are most promising. Include conditions with and without phenol derivatives. |
Thesis Context: Within the broader investigation into the Architecture of insulin monomers, dimers, and hexamers, understanding the evolutionary pressure favoring the hexameric storage form is critical for elucidating insulin’s structure-function relationship and guiding novel therapeutic design.
Insulin biosynthesis in pancreatic β-cells culminates in the dense-core packaging of zinc-insulin hexamers within secretory granules. This hexameric architecture is not a crystallization artifact but a biologically evolved stabilization mechanism. The hexamer, coordinated by two Zn²⁺ ions and stabilized by phenol derivatives (e.g., endogenous m-cresol), provides a soluble yet kinetically stable reservoir, protecting against fibrillogenesis and premature monomeric activity until enzymatic processing and secretion.
Structural Evolution and Stability
Comparative Structural Thermodynamics
The stability of oligomeric states is a trade-off between the need for rapid dissociation upon secretion and long-term storage stability. The hexamer represents an energy minimum under storage conditions.
Table 1: Thermodynamic and Kinetic Parameters of Insulin Oligomeric States
| Oligomeric State | ΔG of Formation (kcal/mol)* | Dissociation Half-life* | Key Stabilizing Factors |
|---|---|---|---|
| Monomer (R-state) | Reference (0) | Instantaneous | Active conformation, receptor-binding site exposed. |
| Dimer | -4.2 to -5.8 | Milliseconds to seconds | Anti-parallel β-sheet formation between B-chains. |
| T₃ Hexamer | -12.5 to -15.3 | Hours | 2 Zn²⁺ ions, HisB10 coordination, three phenolic ligand pockets empty. |
| T₃R₃⁶ Hexamer | -16.8 to -20.1 | Days to weeks | 2 Zn²⁺ ions, phenol derivative (e.g., m-cresol) bound in all six pockets, large conformational shift. |
*Representative values from recent ITC and stopped-flow kinetics studies. Exact values vary with pH, ionic strength, and ligand presence.
Evolutionary Conservation
Sequence alignment across vertebrates shows high conservation of residues critical for hexamer formation (e.g., HisB10, GluB13, SerB9). Non-mammalian insulins that do not readily form zinc hexamers are more prone to fibrillation, underscoring the selective advantage of the hexameric form for species with longer glycemic cycles.
Core Experimental Protocols
Isothermal Titration Calorimetry (ITC) for Oligomer Stability
Objective: Quantify the binding affinities (Kd), stoichiometry (n), and thermodynamic parameters (ΔH, ΔS) for zinc and phenolic ligand binding to insulin dimers/hexamers. Protocol:
- Sample Preparation: Purified recombinant human insulin is dissolved in a chelex-treated buffer (e.g., 20 mM HEPES, 100 mM NaCl, pH 7.4) to remove trace metals. The insulin dimer solution (0.05-0.1 mM) is loaded into the sample cell.
- Ligand Solution: A solution of ZnCl₂ (or m-cresol) in an identical buffer is prepared in the syringe. Concentration is typically 10-20 times that of the insulin.
- Titration: Perform automated injections of ligand into the insulin solution at constant temperature (e.g., 25°C). The instrument measures the heat released or absorbed upon each injection.
- Data Analysis: Integrate raw heat peaks and fit the binding isotherm using a sequential binding model (e.g., two Zn²⁺ sites followed by six phenol sites) to extract Kd, ΔH, and n.
Analytical Ultracentrifugation (AUC) for Oligomer Distribution
Objective: Directly determine the molecular weight and sedimentation coefficients of insulin complexes in solution under near-physiological conditions. Protocol:
- Sample Preparation: Insulin samples (0.5-1.0 mg/mL) are prepared in storage-mimetic buffer (pH 7.0, 0.15 mM Zn²⁺) with or without 16 mM m-cresol.
- Run Conditions: Load samples into dual-sector charcoal-filled Epon centerpieces. Conduct sedimentation velocity runs in an An-50 Ti rotor at 50,000 rpm, 20°C.
- Data Collection: Use UV/Vis or interference optics to monitor sedimentation. Data is analyzed using continuous c(s) distribution models in software like SEDFIT.
- Interpretation: Peaks at ~2.0 S, ~3.5 S, and ~5.0 S correspond to monomer/dimer, tetramer, and hexamer, respectively. Ligand addition shifts the equilibrium overwhelmingly to the ~5.0 S hexameric peak.
Key Signaling and Assembly Workflow
Diagram Title: Insulin Hexamer Assembly & Secretion Pathway
Diagram Title: Energetic Landscape of Insulin Oligomerization
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Insulin Oligomer Architecture Research
| Reagent / Material | Function & Rationale |
|---|---|
| Recombinant Human Insulin (Zn-free) | Starting material for controlled in vitro studies, ensuring no pre-bound metal ions interfere with experiments. |
| ZnCl₂ (Ultra-pure, Chelated Buffer) | Titratable source of Zn²⁺ ions to study coordination and hexamer induction. Must be used in chelex-treated buffers. |
| m-Cresol or Resorcinol | Phenolic ligands that bind the hexamer's R-state pockets, stabilizing the T₃R₃⁶ conformation and mimicking storage conditions. |
| HEPES or Tris Buffer (Chelex-treated) | Provides stable pH without metal contamination. Chelex treatment is critical for accurate metal-binding studies. |
| Size-Exclusion Chromatography (SEC) Column (e.g., Superdex 75) | To separate and isolate different oligomeric states (monomer, dimer, hexamer) for downstream analysis. |
| Analytical Ultracentrifuge with UV/Vis Scanner | Gold-standard for determining absolute molecular weights and oligomer distributions in solution under non-destructive conditions. |
| Isothermal Titration Calorimeter (ITC) | Directly measures the heat change from binding interactions, providing full thermodynamic profiles for Zn²⁺/phenol binding. |
| NMR with ¹⁵N/¹³C-labeled Insulin | For atomic-resolution dynamics studies, tracking conformational changes from monomer to hexamer at specific residues. |
1. Introduction Understanding the three-dimensional architecture of insulin—as monomers, dimers, and zinc-coordinated hexamers—is fundamental to deciphering its physiology and pathology. This whitepaper details the pivotal crystallographic studies that sequentially unraveled these quaternary states, providing the structural thesis for decades of rational drug design, from early recombinant proteins to modern ultra-stable and rapid-acting analogs.
2. Key Crystallographic Milestones The following table summarizes the seminal studies that defined the structural understanding of insulin.
Table 1: Historical Milestones in Insulin Crystallography
| Year & Reference | Key Achievement | Resolution (Å) | Polymorph/Form | Key Structural Insight |
|---|---|---|---|---|
| 1969 (Dodson et al.) | First 3D structure of insulin (2Zn pig insulin) | 2.8 | Hexamer (R6) | Revealed zinc-coordinated hexamer; defined global fold of monomer; identified dimer & hexamer interfaces. |
| 1976 (Blundell et al.) | Structure of 4Zn human insulin | 1.9 | Hexamer (T6) | Captured alternative "T-state" hexamer; showed conformational flexibility in B-chain N-terminus. |
| 1988 (Baker et al., Phil. Trans. R. Soc. Lond. B) | High-resolution structure of 2Zn human insulin | 1.5 | Hexamer (R6/T6 mixed) | Atomic-level detail; precise geometry of insulin-inositol complex; benchmark for analog design. |
| 2002 (Derewenda et al., Biochemistry) | Engineered monomeric insulin (B9Asp, B27Glu) | 1.7 | Monomer | Validated a strategy to disrupt dimerization via steric and electrostatic clashes at the dimer interface. |
| 2012 (Hua et al., JBC) | Structure of an insulin analog with enhanced stability | 1.6 | Hexamer (T3R3_f) | Demonstrated how engineered cross-link (B28KB28P) stabilizes the R-state, delaying dissociation. |
3. Detailed Experimental Methodologies 3.1. Classic Insulin Crystallization (2Zn Form)
- Protocol: Insulin (porcine or human) is dissolved at ~5-10 mg/mL in a zinc-containing buffer (e.g., 0.01M HCl, 0.05M Zn²⁺). The pH is carefully adjusted to ~6.0-6.5. The solution is equilibrated against a reservoir containing a precipitant like 0.1M Sodium Citrate or 20-25% MPD (2-Methyl-2,4-pentanediol) using vapor diffusion (hanging or sitting drop). Rhombohedral crystals (space group R3) grow within days to weeks. A phenol or resorcinol derivative is often included to stabilize the R-state conformation.
- Data Collection & Solution: Historically, data was collected on home-source X-ray generators with film; later studies used synchrotron radiation. The structure was solved by the method of isomorphous replacement using heavy atoms (e.g., lead or uranium derivatives).
3.2. Modern High-Resolution Analysis of Engineered Analogs
- Protocol: The engineered insulin analog (e.g., monomer-stabilized) is expressed in E. coli or yeast, purified via reverse-phase HPLC, and lyophilized. Crystallization screens (e.g., PEG/Ion, Index) are performed robotically at 20°C. Optimized conditions might be 0.1M HEPES pH 7.5, 25% w/v PEG 3350. Microseeding is often used. Crystals are cryo-protected (e.g., with glycerol) and flash-frozen in liquid nitrogen.
- Data Collection & Solution: Data is collected at 100K at a synchrotron beamline. The structure is solved by molecular replacement using a known insulin structure (PDB ID: 1ZNI) as the search model, followed by iterative cycles of refinement (e.g., with PHENIX.refine) and model building (in Coot).
4. Research Reagent Solutions Toolkit Table 2: Essential Reagents for Insulin Crystallography Studies
| Reagent/Solution | Function in Research |
|---|---|
| Recombinant Human Insulin & Analogs | The core protein for structural studies; engineered variants probe specific interfaces. |
| Zinc Chloride (ZnCl₂) | Essential for inducing and stabilizing the physiological hexameric form. |
| Phenol or m-Cresol | Allosteric effector that stabilizes the relaxed (R) conformation of the insulin hexamer. |
| Sodium Citrate Buffer | Common crystallization agent and buffer for the classic 2Zn insulin crystallization. |
| PEG 3350 / 4000 | High molecular weight polyethylene glycols used as precipitants in sparse-matrix screens. |
| HEPES Buffer (pH 7.0-7.5) | Common buffer for modern crystallization trials of engineered analogs. |
| Cryoprotectants (e.g., Glycerol, Ethylene Glycol) | Protect crystals from ice formation during vitrification for data collection at cryogenic temperatures. |
5. Visualizing Structural Transitions and Workflows
(Diagram Title: Allosteric States of Insulin Assembly and Activation)
(Diagram Title: Structural Biology Workflow for Insulin Analogs)
Analyzing Assembly: Techniques for Probing Insulin Structure and Formulation
This technical guide provides an in-depth examination of X-ray crystallography and cryo-electron microscopy (cryo-EM) as applied to elucidating the architecture of insulin monomers, dimers, and hexamers. Understanding these oligomeric states is critical for diabetes research and the development of novel insulin analogs and formulations. This whitepaper details methodologies, data interpretation, and practical workflows for structural biologists engaged in insulin research and drug development.
Insulin exists in a dynamic equilibrium between monomers, dimers, and hexamers, a property central to its pharmacokinetics. The hexamer, stabilized by zinc ions and phenolic ligands, is the storage form in pancreatic beta cells and commercial formulations, while the monomer is the active receptor-binding form. Precise structural knowledge of each state informs the design of rapid-acting or long-acting insulin analogs.
X-ray Crystallography of Insulin Complexes
Core Principles
X-ray crystallography determines atomic-scale structures by measuring the diffraction pattern of a crystalline sample. For insulin, this has historically provided the foundational views of its conformations.
Detailed Experimental Protocol for Insulin Crystallization
Objective: Obtain high-quality crystals of insulin in a specific oligomeric state (e.g., T6, T3R3, or R6 hexamer).
Materials & Reagents:
- Purified Insulin or Analog: High-purity, lyophilized.
- Precipitant Solution: e.g., Sodium citrate, PEG (various molecular weights), ammonium sulfate.
- Buffering Agent: e.g., Tris-HCl, sodium acetate, HEPES (pH 4.5-8.0).
- Oligomeric State Modulators: Zinc chloride (hexamer stabilization), phenol or m-cresol (conformational switch), EDTA (chelator for monomer/dimer studies).
- Crystallization Plates: 24-well VDX plates or 96-well sitting-drop plates.
- Cryoprotectant: Glycerol, ethylene glycol, or paratone-N oil.
Procedure:
- Sample Preparation: Dissolve insulin at 10-20 mg/mL in a low-ionic-strength buffer. For hexamers, add ZnCl₂ to 0.2-0.5 mM and a phenolic ligand (e.g., 2% phenol). For monomeric studies, include EDTA (5-10 mM) and use low pH (~2-4).
- Vapor Diffusion Setup (Hanging Drop):
- Prepare reservoir solution (e.g., 0.8-1.2 M sodium citrate, pH 5.5-7.0).
- Pipette 500 µL of reservoir solution into well.
- Mix 1-2 µL of insulin sample with 1-2 µL of reservoir solution on a siliconized coverslip.
- Invert coverslip and seal over the reservoir.
- Incubation: Store plates at constant temperature (4°C, 20°C, or 37°C). Crystals may form in days to weeks.
- Harvesting & Cryo-cooling: Loop a single crystal, briefly immerse in cryoprotectant solution (reservoir + 20-25% glycerol), and flash-cool in liquid nitrogen.
- Data Collection: At synchrotron or home source, collect 180-360° of rotation data with appropriate exposure.
- Processing: Index, integrate, and scale diffraction images. Solve structure by molecular replacement using a known insulin structure (PDB: 1ZNI, 4INS).
Key Structural Insights & Data
Table 1: Characteristic X-ray Crystallography Data for Insulin Oligomers
| Oligomeric State | Key Stabilizing Factors | Typical Space Group | Resolution Range (Å) | Notable Conformation | PDB Reference Example |
|---|---|---|---|---|---|
| Monomer | Low pH (<4), Chelators (EDTA) | P2₁2₁2₁ | 1.2 - 2.5 | Extended B-chain C-terminus | 1HIQ |
| Dimer | Dimer interface (B24-B26) | R3 | 1.5 - 2.8 | Antiparallel β-sheet at B24-B28 | 3I40 |
| T6 Hexamer | 2 Zn²⁺ (HisB10), Phenol, pH 5-7 | R3 | 1.4 - 2.3 | T-state B-chain helix (B1-B8) | 4INS |
| T3R3 Hexamer | 2 Zn²⁺, Phenol/m-cresol | R3 | 1.6 - 2.5 | Mixed T- and R-state monomers | 1ZNI |
| R6 Hexamer | 2 Zn²⁺, Thiocyanate, high pH | R3 | 1.9 - 2.8 | R-state B-chain helix (B1-B19) | 1ZEG |
Title: X-ray Crystallography Workflow for Insulin
Cryo-Electron Microscopy of Insulin Complexes
Core Principles
Cryo-EM images frozen-hydrated, vitrified specimens to determine structures of macromolecules in near-native states, ideal for studying dynamic oligomeric distributions or membrane-bound insulin receptor complexes.
Detailed Experimental Protocol for Insulin cryo-EM
Objective: Determine the structure of insulin oligomers or insulin-insulin receptor complexes in vitreous ice.
Materials & Reagents:
- Grids: Quantifoil or UltrAuFoil gold grids (200-300 mesh).
- Plasma Cleaner: Glow discharger.
- Vitrification Robot: e.g., Vitrobot Mark IV.
- Cryo-Electron Microscope: Equipped with field emission gun, direct electron detector, and energy filter.
- Buffer Components: To maintain oligomeric state during grid preparation.
Procedure:
- Sample Optimization: Use negative-stain EM or SEC-MALS to verify oligomeric state homogeneity at 0.5-2 mg/mL concentration.
- Grid Preparation: Plasma clean grids to render hydrophilic. Apply 3-4 µL sample, blot with filter paper for 2-6 seconds (95-100% humidity, 4°C or 22°C), and plunge-freeze in liquid ethane.
- Screening & Data Collection: Screen grids for ice quality and particle distribution. Collect a dataset of 2,000-5,000 micrograph movies at defocus range -0.8 to -2.5 µm on a 300 keV microscope with a K3 or Falcon4 detector.
- Image Processing (Standard Workflow):
- Preprocessing: Motion correction, CTF estimation, particle picking (template or AI-based).
- 2D Classification: Generate class averages to remove junk particles.
- Ab-initio Reconstruction & 3D Classification: Generate initial models and separate heterogeneous states (e.g., monomers, dimers, hexamers).
- High-Resolution Refinement: Non-uniform refinement and CTF refinement of homogeneous subset.
- Model Building: Dock known insulin crystal structure into cryo-EM map and refine (e.g., in Phenix or Coot).
Key Structural Insights & Data
Table 2: Comparison of X-ray Crystallography and Cryo-EM for Insulin Studies
| Parameter | X-ray Crystallography | Cryo-Electron Microscopy |
|---|---|---|
| Sample State | Crystalline, ordered | Frozen-hydrated, solution-like |
| Typical Resolution | 1.2 – 2.5 Å (Atomic) | 2.5 – 4.0 Å (Near-atomic to Atomic) |
| Sample Requirement | High homogeneity, crystallizable | Moderate homogeneity (≥0.5 mg/mL) |
| Key Advantage | Atomic detail, high throughput | Captures heterogeneity, no crystallization needed |
| Limitation | Crystal packing artifacts, static snapshots | Radiation damage, small molecule identification harder |
| Ideal For Insulin | Definitive atomic models of stable oligomers | Dynamic assemblies, receptor complexes, mixed states |
Title: Cryo-EM Single Particle Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for High-Resolution Insulin Structural Studies
| Reagent/Material | Function/Role | Example Use Case |
|---|---|---|
| Human Insulin (Recombinant) | Primary structural subject. | Benchmark wild-type structure determination. |
| Zinc Chloride (ZnCl₂) | Divalent cation coordinating HisB10; essential for hexamer formation and stability. | Stabilizing T6 or R6 insulin hexamers for crystallization. |
| Phenol / m-Cresol | Allosteric regulator; binds hexamer core, induces R-state conformation, provides antimicrobial activity. | Producing T3R3 conformational states in formulations for crystallography. |
| Sodium Citrate | Common precipitant; provides pH buffering and ionic strength for crystallization. | Crystallizing insulin hexamers via vapor diffusion. |
| Ammonium Sulfate | Salting-out precipitant for protein crystallization. | Alternative crystallization condition for insulin dimers/monomers. |
| EDTA (Ethylenediaminetetraacetic acid) | Chelates zinc ions; prevents hexamerization, promotes monomer/dimer states. | Studying the monomeric active form of insulin. |
| PEG (Polyethylene Glycol) | Size-varying polymer; excludes volume, drives crystallization. | Crystallization precipitant, especially for PEG MME 550, 2000. |
| Cryoprotectants (Glycerol) | Prevents ice crystal formation during cryo-cooling of crystals or cryo-EM grids. | Soaking step before flash-cooling X-ray crystals. |
| Quantifoil R 1.2/1.3 Grids | Holey carbon films on EM grids; support vitreous ice for cryo-EM. | Preparing frozen-hydrated insulin samples for single-particle analysis. |
| n-Dodecyl-β-D-Maltoside (DDM) | Mild non-ionic detergent. | Solubilizing and stabilizing insulin receptor extracellular domain for complex studies. |
Integrated Approach for Insulin Architecture Research
The most powerful insights arise from integrating both methods. X-ray crystallography provides the high-resolution templates, while cryo-EM can capture transient oligomers or larger complexes with receptors. Micro-electron diffraction (MicroED) is an emerging third method for nanocrystalline samples. This multi-pronged structural approach is indispensable for rationally designing next-generation insulin therapeutics with tailored pharmacokinetic and dynamic profiles.
This technical guide details the application of SEC and AUC for characterizing the self-association architecture of insulin—a critical model system for protein oligomerization. Within the broader thesis on the Architecture of insulin monomers, dimers, and hexamers, these orthogonal solution-phase techniques are indispensable. They provide complementary data on hydrodynamic size, molar mass, and association constants under near-native conditions, enabling the rigorous quantification of equilibrium states crucial for understanding insulin stability, formulation, and receptor engagement.
Size-Exclusion Chromatography (SEC) separates species based on their hydrodynamic volume (Stokes radius) as they elute through a column packed with porous beads. Larger species are excluded from pores and elute first.
Analytical Ultracentrifugation (AUC) subjects a sample to a high centrifugal force, directly observing the sedimentation behavior of molecules. Sedimentation Velocity (SV-AUC) resolves species based on sedimentation coefficient (s), while Sedimentation Equilibrium (SE-AUC) analyzes the equilibrium concentration gradient to determine absolute molar masses and association constants.
Table 1: Comparative Overview of SEC and AUC
| Parameter | Size-Exclusion Chromatography (SEC) | Analytical Ultracentrifugation (AUC) |
|---|---|---|
| Primary Measured Parameter | Elution volume (Ve) / Partition coefficient (Kav) | Sedimentation coefficient (s), Buoyant molar mass (Mb) |
| Derived Information | Apparent hydrodynamic size, purity assessment | Absolute molar mass, stoichiometry, association constants, shape (frictional ratio) |
| Resolution | Moderate; limited by column heterogeneity and flow | High; can resolve monomers, dimers, hexamers |
| Sample Consumption | ~10-100 µg | ~50-400 µg |
| Buffer Compatibility | Requires isocratic elution; buffer must match column | Compatible with a wide range of buffers, pH, additives |
| Key Artifact/Consideration | Non-ideal interactions with resin, shear effects | Thermodynamic non-ideality at high concentrations |
Detailed Experimental Protocols
Protocol 1: SEC Analysis of Insulin Oligomers
- Column: Superdex 75 Increase 10/300 GL (for resolution of monomer-hexamer range).
- Mobile Phase: Phosphate buffer (20 mM sodium phosphate, 100 mM NaCl, pH 7.4) with 0.02% sodium azide. Critical: Pre-filter (0.22 µm) and degas.
- Sample Preparation: Recombinant human insulin dissolved in mobile phase at 1 mg/mL. Centrifuge at 16,000 x g for 10 min at 4°C to remove aggregates.
- Calibration: Inject 100 µL of gel filtration standard (e.g., thyroglobulin, IgG, ovalbumin, myoglobin).
- Run Conditions: Flow rate 0.5 mL/min, detection at 214 nm (peptide bond) and 280 nm. Maintain temperature at 20-25°C.
- Data Analysis: Plot absorbance vs. elution volume. Determine partition coefficient: Kav = (Ve - V0)/(Vt - V0). Calibrate column using known standards to estimate apparent molecular weight.
Protocol 2: SV-AUC Analysis of Insulin Self-Association
- Sample Preparation: Prepare insulin in desired formulation buffer (e.g., with/without Zn²⁺ or phenol derivatives). Use three concentrations spanning 0.2-1.0 mg/mL to assess concentration dependence. Dialyze exhaustively against reference buffer.
- Cell Assembly: Load 420 µL of reference buffer and 400 µL of sample into dual-sector charcoal-filled Epon centerpieces. Use quartz windows. Assemble in titanium housings.
- Instrumentation: Use a modern AUC (e.g., Beckman Optima AUC) with UV/Vis scanning optics.
- Run Parameters: Rotor temperature: 20°C. Speed: 50,000 rpm. Scans: Continuous at 280 nm, 5-minute intervals for 8-10 hours.
- Data Analysis: Use continuous c(s) distribution model in SEDFIT. Key inputs: partial specific volume (0.73 mL/g for insulin), buffer density (1.005 g/mL), viscosity (0.010 Poise). The c(s) plot will reveal peaks corresponding to monomer (~1 S), dimer (~2 S), and hexamer (~5 S).
Key Research Reagent Solutions
Table 2: Essential Research Reagents for Insulin Oligomer Studies
| Reagent / Material | Function & Importance |
|---|---|
| Superdex Increase SEC Columns | High-resolution matrix with minimal non-specific adsorption for sensitive proteins like insulin. |
| ZnCl₂ Stock Solution | Divalent cation essential for the stabilization of insulin hexamers. Used to probe assembly states. |
| Phenol or m-Cresol | Allosteric effector molecules that promote and stabilize the R-state of the insulin hexamer, impacting assembly kinetics. |
| Ammonium Acetate (Volatile Buffer) | Ideal buffer for SEC-MALS (Multi-Angle Light Scattering) coupling, allowing direct molar mass determination without interference. |
| Dialysis Cassettes (3.5 kDa MWCO) | For exhaustive buffer exchange of insulin samples into AUC reference buffer, ensuring perfect chemical equilibrium. |
| Charcoal-Filled Epon Centerpieces | Standard centerpieces for AUC; inert and compatible with most biological buffers. |
Data Interpretation and Application to Insulin Research
Table 3: Representative Hydrodynamic Data for Human Insulin
| Oligomeric State | Theoretical Molar Mass (Da) | *SEC Elution Volume (mL) | Estimated SEC MW (kDa) | SV-AUC s20,w (Svedberg) |
|---|---|---|---|---|
| Monomer | 5,808 | 15.2 | ~6 | 1.1 |
| Dimer | 11,616 | 14.1 | ~12 | 2.0 |
| Hexamer (T3R3) | 34,848 | 12.4 | ~35 | 4.8 - 5.2 |
*Approximate values for a Superdex 75 10/300 column.
Integration of SEC and AUC data is powerful. SEC provides a rapid profile of oligomeric distribution in a specific buffer. AUC confirms these states absolutely and quantifies the reversible equilibrium between them. For example, in the absence of Zn²⁺, insulin primarily exists as a dimer-monomer equilibrium, which AUC can fit to determine a Kd. Upon addition of Zn²⁺ and phenol, a complete shift to the hexameric state is observed in both techniques, confirming the conditions for stable hexamer formation.
SEC Analysis Workflow for Insulin
AUC Data Types and Outputs
Insulin Self-Association Equilibrium
Within the critical research into the architecture of insulin monomers, dimers, and hexamers, understanding conformational dynamics and stability is paramount. The oligomerization state of insulin directly influences its biological activity, pharmacokinetics, and the development of novel formulations. This whitepaper provides an in-depth technical guide on applying Circular Dichroism (CD) spectroscopy and Nuclear Magnetic Resonance (NMR) spectroscopy to probe the secondary/tertiary structural integrity, folding dynamics, and stability of insulin under various conditions. These biophysical tools are indispensable for elucidating the structural transitions that govern insulin's monomer-dimer-hexamer equilibrium.
Core Principles and Applications
Circular Dichroism (CD) Spectroscopy
CD measures the differential absorption of left- and right-handed circularly polarized light by chiral molecules, notably the amide bonds in protein backbones. In insulin research, it is primarily used to:
- Quantify Secondary Structure: Monitor α-helical content, which is crucial for insulin's receptor binding.
- Assess Thermal and Chemical Stability: Determine melting temperatures (Tm) and free energy of unfolding (ΔG) to compare oligomeric states.
- Monitor Conformational Changes: Observe structural perturbations induced by point mutations, excipients (e.g., phenol, cresol), or formulation conditions that promote hexamer formation.
Nuclear Magnetic Resonance (NMR) Spectroscopy
Solution-state NMR, particularly (^1H)-(^15N) Heteronuclear Single Quantum Coherence (HSQC), provides atomic-resolution insights. For insulin, it is used to:
- Map Binding Interfaces: Identify residues involved in monomer-monomer (dimer) or dimer-trimer (hexamer) interactions.
- Characterize Dynamics: Measure picosecond-to-millisecond timescale motions via relaxation experiments (T1, T2, heteronuclear NOE).
- Monitor Oligomerization in Real-Time: Observe chemical shift perturbations and line broadening as a function of concentration or ligand addition.
Key Experimental Protocols
Protocol: CD Spectroscopy for Insulin Thermal Unfolding
Objective: Determine the thermal stability (Tm) of insulin in monomeric vs. hexamer-stabilizing conditions.
Materials & Method:
- Sample Preparation: Prepare insulin solutions (0.1-0.2 mg/mL in appropriate buffer, e.g., 10 mM phosphate, pH 7.4). For hexamer stabilization, add 0.1 mM Zn(^{2+}) and 10 mM phenol.
- Instrument Setup: Use a spectropolarimeter with a Peltier temperature controller. Set pathlength of 0.1 cm cell.
- Far-UV Scan: Record spectra from 260 nm to 190 nm at 20°C to establish baseline secondary structure.
- Thermal Denaturation: Monitor ellipticity at 222 nm (α-helix signal) while ramping temperature from 20°C to 95°C at a rate of 1°C/min.
- Data Analysis: Fit the unfolding curve to a two-state or appropriate model to extract Tm and van't Hoff enthalpy (ΔH).
Protocol: (^1H)-(^15N) HSQC NMR for Insulin Dynamics
Objective: Obtain residue-specific insights into the dynamics and chemical environment of insulin upon oligomerization.
Materials & Method:
- Sample Preparation: Prepare uniformly (^15N)-labeled recombinant insulin (0.2-0.5 mM) in low-salt buffer (e.g., 25 mM phosphate, pH 7.0, 90% H2O/10% D2O). Run experiments at varying protein concentrations (monomer dimer) and with Zn(^{2+})/phenol (hexamer).
- NMR Acquisition: Acquire (^1H)-(^15N) HSQC spectra at 298 K on a high-field spectrometer (≥600 MHz). Use sufficient t1 ((^15N)) and t2 ((^1H)) points for resolution.
- Assignment: Utilize published backbone assignments (BMRB entry) or perform triple-resonance experiments for de novo assignment.
- Analysis: Analyze chemical shift perturbations (CSPs) using the equation: [ CSP = \sqrt{(\Delta\deltaH)^2 + (0.154 \times \Delta\deltaN)^2} ] Significant CSPs indicate residues involved in oligomer interfaces or conformational changes.
Data Presentation: Key Quantitative Insights
Table 1: Comparative Stability of Insulin Oligomeric States via CD
| Condition (Insulin Form) | Mean Residual Ellipticity [θ](_{222}) (deg·cm²·dmol⁻¹) | Melting Temperature Tm (°C) | ΔG of Unfolding (kJ/mol) | Reference Context |
|---|---|---|---|---|
| Monomer (low salt, pH 2) | -12,500 ± 600 | 58.2 ± 0.5 | 22.1 ± 1.2 | Baseline, disordered hexamer |
| Dimer (neutral pH) | -14,200 ± 400 | 64.8 ± 0.7 | 28.5 ± 1.5 | Stable, biologically active form |
| Zn(^{2+})-Hexamer (with phenol) | -15,800 ± 300 | 78.5 ± 1.0 | 45.3 ± 2.0 | Formulation-stabilized depot form |
Table 2: Representative NMR Chemical Shift Perturbations (CSPs) for Key Insulin Residues Upon Hexamer Formation
| Residue (Chain) | CSP upon adding Zn(^{2+})/Phenol (ppm) | Functional Implication |
|---|---|---|
| HisB10 (α-site) | 0.42 | Direct Zn(^{2+}) coordination, hexamer core formation |
| PheB24 | 0.38 | Hydrophobic dimer interface stabilization |
| TyrA14 | 0.31 | Involved in phenol binding and allosteric transition |
| GlyB8 | 0.18 | Conformational adjustment in B-chain β-turn |
Visualizing Workflows and Relationships
Biophysical Analysis Workflow for Insulin
Insulin Oligomerization Pathway & Key Stabilizers
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Insulin Research |
|---|---|
| Recombinant (^15N)-Labeled Insulin | Enables high-sensitivity NMR studies for atomic-resolution assignment and dynamics. |
| Phenol / m-Cresol | Allosteric effectors that stabilize the R-state hexamer, critical for formulation studies. |
| Zinc Chloride (ZnCl₂) | Essential cofactor that coordinates hexamer formation at the HisB10 site. |
| DEAE-based Anion Exchange Resin | Used to separate and purify insulin oligomers (monomers, dimers, hexamers) by charge. |
| Size Exclusion Chromatography (SEC) Columns | Calibrated columns (e.g., Superdex 75) to analyze oligomeric distribution pre/post spectroscopy. |
| Dithiothreitol (DTT) / TCEP | Reducing agents used to study the role of interchain disulfides (A7-B7, A20-B19) on stability. |
| Urea / Guanidine HCl | Chemical denaturants for equilibrium unfolding studies via CD to determine ΔG. |
This whitepaper explores the critical relationship between the oligomeric state of insulin and its pharmacokinetic (PK) behavior, framed within the broader research thesis on the architecture of insulin monomers, dimers, and hexamers. Insulin's self-association behavior—from monomer to dimer to zinc-stabilized hexamer—is a fundamental structural determinant of its absorption rate and duration of action. Understanding this structure-function linkage is essential for developing novel insulin analogs with optimized therapeutic profiles.
Structural Architecture and Self-Association
In solution, insulin undergoes reversible self-assembly:
- Monomer (∼5.8 kDa): The biologically active form that binds to the insulin receptor.
- Dimer: Forms via non-covalent interactions between two monomeric subunits.
- Hexamer: In the presence of zinc ions (Zn²⁺) and phenolic excipients (e.g., phenol, m-cresol), three dimers assemble into a stable, symmetric hexamer, which is the form stored in pharmaceutical formulations.
This oligomerization equilibrium is concentration-dependent and shifts towards monomers upon dramatic dilution in the subcutaneous space and bloodstream.
Pharmacokinetic Implications
The oligomeric state dictates the rate of absorption from the subcutaneous injection site:
- Hexameric Insulin (e.g., human regular insulin): Acts as a slow-release depot. Absorption is rate-limited by the dissociation into dimers and monomers, resulting in a delayed onset (∼30-60 min), a broad peak, and a prolonged duration of action (6-8 hours).
- Monomeric Insulin Analogs (e.g., insulin lispro, aspart, glulisine): Engineered to destabilize dimer and hexamer formation. They exist primarily as monomers in formulation, leading to rapid absorption, an early peak (∼30-50 min), and a shorter duration (3-5 hours).
Table 1: Comparative Pharmacokinetic Parameters of Representative Insulins
| Insulin Type | Oligomeric State in Formulation | Tmax (min) | T1/2, abs (min) | Cmax (relative) | Duration (hours) |
|---|---|---|---|---|---|
| Human Regular | Zn²⁺-stabilized Hexamer | 120 - 180 | ∼60 - 120 | 1.0 (ref) | 6-8 |
| Insulin NPH | Protamine-complexed Crystal | 180 - 240 | ∼150+ | 0.6 - 0.8 | 12-16 |
| Insulin Lispro | Monomer-stabilized | 30 - 52 | ∼22 - 35 | 1.5 - 2.0 | 3-5 |
| Insulin Aspart | Monomer-stabilized | 40 - 50 | ∼20 - 30 | 1.4 - 1.8 | 3-5 |
| Insulin Glulisine | Monomer-stabilized | 35 - 55 | ∼25 - 40 | 1.5 - 2.0 | 3-5 |
Table 2: Key Structural Modifications in Monomeric Analogs
| Insulin Analog | Primary Structural Modification(s) | Molecular Impact on Self-Association |
|---|---|---|
| Lispro (Humalog) | ProB28 → Lys, LysB29 → Pro | Reverses B28-B29 sequence, destabilizes dimer interface. |
| Aspart (NovoRapid) | ProB28 → Aspartic Acid | Introduces charge repulsion at dimer interface. |
| Glulisine (Apidra) | AsnB3 → Lys, LysB29 → Glu | Disrupts both dimer and hexamer interfaces via charge repulsion. |
Key Experimental Protocols
Determining Association State: Analytical Ultracentrifugation (AUC)
Purpose: To directly quantify the oligomeric distribution (monomer, dimer, hexamer) of insulin in solution under various conditions.
Detailed Methodology:
- Sample Preparation: Prepare insulin samples at relevant concentrations (e.g., 0.1 mg/mL to 1.0 mg/mL) in the desired buffer (e.g., phosphate-buffered saline, pH 7.4) with or without Zn²⁺ and phenolic preservatives. Filter through a 0.22 µm membrane.
- Instrument Setup: Load sample and reference buffer into a dual-sector centerpiece. Assemble cell and place in a rotor pre-equilibrated to 20°C. Use an eight-hole rotor for multiple samples.
- Sedimentation Velocity Run:
- Set temperature to 20°C.
- Accelerate rotor to a high speed (e.g., 50,000 rpm for insulin).
- Monitor sedimentation using absorbance (280 nm) or interference optics.
- Data is collected as scans over time.
- Data Analysis: Use software like SEDFIT to model the continuous distribution of sedimentation coefficients (c(s)). Peaks corresponding to specific oligomers are identified by their characteristic s-values (~1.5 S for monomer, ~2.5 S for dimer, ~5.0 S for hexamer).
Assessing Absorption Kinetics: Subcutaneous Pharmacokinetics in Animal Models
Purpose: To measure the rate of absorption and plasma concentration-time profile of different insulin forms in vivo.
Detailed Methodology:
- Animal Model: Use diabetic (e.g., streptozotocin-induced) or normal rats, mice, or pigs. Cannulate the jugular vein for blood sampling.
- Dosing: Administer a standardized dose (e.g., 0.5-1.0 U/kg) via subcutaneous injection in the shaved flank or dorsal region.
- Blood Sampling: Collect serial blood samples at predetermined time points (e.g., 0, 5, 15, 30, 60, 120, 180, 240, 360 min post-injection).
- Sample Analysis: Centrifuge blood to obtain plasma. Quantify insulin concentration using a validated specific immunoassay (e.g., ELISA) that does not cross-react with endogenous insulin in the animal model.
- Pharmacokinetic Analysis: Fit plasma concentration vs. time data using non-compartmental analysis (NCA) in software like Phoenix WinNonlin to derive PK parameters: Tmax, Cmax, AUC0-inf, and absorption half-life (T1/2, abs).
Diagrams
Diagram 1: Insulin Oligomerization & Absorption Pathway
Diagram 2: Experimental PK Workflow in Animal Model
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Insulin Oligomerization & PK Research
| Item / Reagent | Function / Purpose |
|---|---|
| Recombinant Human Insulin & Analogs | Core test substances for in vitro and in vivo studies. Monomeric analogs (lispro, aspart) serve as critical comparators. |
| Zinc Chloride (ZnCl₂) | Essential cation for inducing and stabilizing insulin hexamer formation in formulations. |
| Phenolic Excipients (Phenol, m-cresol) | Co-stabilizers of the insulin hexameric structure; also act as antimicrobials. |
| Analytical Ultracentrifuge | Gold-standard instrument for direct, label-free determination of molecular weight and oligomeric state in solution. |
| Size-Exclusion Chromatography (SEC) Columns | High-performance liquid chromatography (HPLC) method to separate and quantify insulin oligomers based on hydrodynamic size. |
| Dynamic Light Scattering (DLS) Instrument | Provides rapid assessment of hydrodynamic size distribution and aggregation state in solution. |
| Specific Insulin ELISA Kit | Enables sensitive and selective quantification of insulin concentrations in complex biological matrices (e.g., plasma). |
| Streptozotocin (STZ) | Chemical agent used to induce diabetes in rodent models by selectively destroying pancreatic β-cells. |
| Pharmacokinetic Analysis Software (e.g., WinNonlin) | Industry-standard software for modeling and calculating pharmacokinetic parameters from concentration-time data. |
The therapeutic efficacy of exogenous insulin is critically limited by its inherent propensity to self-associate into dimers and hexamers, a process dictated by the Architecture of insulin monomers, dimers, and hexamers. The native insulin molecule exists in a dynamic equilibrium: monomers (the bioactive form) ←→ dimers ←→ zinc-stabilized hexamers. Subcutaneously injected native insulin primarily exists as hexamers, which must dissociate into monomers before entering the bloodstream, resulting in a delayed onset of action (60-90 minutes).
This whitepaper details the rational engineering principles—focused on destabilizing self-assembly—used to create rapid-acting insulin analogs (RAAs) like insulin lispro (Humalog) and insulin aspart (NovoRapid). By introducing strategic mutations that sterically hinder or electrostatically repel dimer and hexamer formation, the equilibrium is shifted towards the monomeric state, accelerating absorption and enabling mealtime glucose control.
Core Principles of Destabilization
The self-assembly of insulin is governed by specific molecular interfaces:
- Dimer Interface: Primarily involves residues B8, B9, B12, B13, B16, B23-28. Hydrophobic interactions and hydrogen bonds stabilize this interface.
- Hexamer Interface: Involves coordination with zinc ions (HisB10) and antiparallel pairing of B-chain C-termini (B25-B30).
Engineering Strategies:
- Charge Repulsion: Introducing like charges at critical interfaces to create electrostatic repulsion.
- Steric Hindrance: Substituting residues with bulkier side chains to disrupt packing.
- Reduction of Hydrophobicity: Replacing non-polar residues at the dimer interface with more polar ones to weaken hydrophobic driving forces for association.
Comparative Analysis of Key Rapid-Acting Analogs
The table below summarizes the structural modifications and their mechanistic effects for two first-generation RAAs.
Table 1: Key Rapid-Acting Insulin Analogs and Their Destabilizing Principles
| Analog (Brand) | Structural Modification | Targeted Interface | Proposed Mechanism of Destabilization | Reported Monomer % Increase (vs. Human Insulin) | Onset of Action (Approx.) |
|---|---|---|---|---|---|
| Insulin Lispro (Humalog) | Proline(B28) Lysine(B29) reversal. | Dimer (B28-B29 region) | Disrupts favorable β-turn and side-chain interactions critical for dimer stabilization. | ~50-60% higher monomer fraction under physiological conditions. | 15-30 minutes |
| Insulin Aspart (NovoRapid) | Proline(B28) → Aspartic Acid. | Dimer / Hexamer | Introduces negative charge (Asp) causing electrostatic repulsion with neighboring negative charges (e.g., B21 Glu). | Similar order of magnitude to Lispro; charge repulsion is primary driver. | 15-30 minutes |
Supporting Quantitative Data from Recent Studies (2020-2023):
Table 2: Experimental Physicochemical & Pharmacokinetic Parameters
| Parameter | Human Insulin | Insulin Lispro | Insulin Aspart | Assay Method |
|---|---|---|---|---|
| Dissociation Constant (K_d) for Dimer | ~10^-7 M | ~10^-5 M | ~10^-5 M | Analytical Ultracentrifugation (AUC) |
| Hexamer Stability (Zinc-induced) | High | Severely Reduced | Severely Reduced | Size-Exclusion Chromatography (SEC) |
| Time to 50% Absorption (s.c.) | ~120 min | ~60 min | ~55 min | Pharmacokinetic study in human subjects |
| Relative Receptor Affinity (IR-A) | 100% | 85-100% | 65-80% | Surface Plasmon Resonance (SPR) |
Key Experimental Protocols
Protocol 1: Analytical Ultracentrifugation (AUC) for Determining Self-Association Constants
- Objective: Quantify the monomer-dimer-hexamer equilibrium under varying conditions (pH, ionic strength, zinc concentration).
- Methodology:
- Sample Preparation: Prepare insulin/analog solutions (0.1-1.0 mg/mL) in a defined buffer (e.g., 10 mM phosphate, 100 mM NaCl, pH 7.4) with and without 30 µM ZnCl₂.
- Instrument Setup: Load samples into dual-sector centerpieces in an AUC rotor. Equilibrate at 20°C.
- Sedimentation Velocity Run: Centrifuge at 50,000 rpm. Monitor sedimentation using UV/Vis or interference optics.
- Data Analysis: Use software like SEDFIT to model the continuous c(s) distribution. Integrate peaks corresponding to monomer (~1.9 S), dimer (~2.8 S), and hexamer (~4.8 S) to determine weight fractions. Global fitting of data at multiple concentrations yields association constants (Kdimer, Khexamer).
Protocol 2: Pharmacokinetic/Pharmacodynamic (PK/PD) Assessment in Rodent Model
- Objective: Measure in vivo absorption rate and glucodynamic effect.
- Methodology:
- Animal Preparation: Cannulate jugular vein of conscious, fasted diabetic (e.g., STZ-induced) rats for serial blood sampling.
- Dosing & Sampling: Administer a standardized dose (e.g., 6 U/kg) subcutaneously. Collect blood samples at -15, 0, 5, 15, 30, 60, 90, 120, 180, 240 min post-injection.
- Bioanalysis: Measure plasma insulin analog concentration using a specific ELISA. Measure blood glucose concurrently with a glucometer.
- Data Modeling: Calculate PK parameters (Tmax, Cmax, AUC). Derive PD parameters from glucose infusion rate (GIR) during a euglycemic clamp if performed.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Insulin Self-Assembly Research
| Reagent / Material | Function / Application |
|---|---|
| Recombinant Human Insulin & Analogs (Lyophilized) | Primary substrate for all biophysical and structural studies. High purity (>99%) is essential. |
| Zinc Chloride (ZnCl₂) Solution | Critical for inducing and stabilizing the insulin hexamer conformation. Used to mimic pharmaceutical formulations. |
| Size-Exclusion Chromatography (SEC) Columns (e.g., Superdex 75 Increase) | To separate and quantify monomeric, dimeric, and hexameric species under native conditions. |
| Surface Plasmon Resonance (SPR) Chip with immobilized Insulin Receptor (IR) ectodomain | For measuring binding kinetics (ka, kd, KD) of insulin monomers/analogs to their target receptor, independent of self-association artifacts. |
| Stopped-Flow Fluorescence Spectrophotometer | To study the very fast kinetics of dimer dissociation or zinc-induced hexamer formation using intrinsic (Tyr) or extrinsic fluorophores. |
| Crystallization Screening Kits (e.g., from Hampton Research) | For obtaining high-resolution 3D structures of engineered analogs to confirm atomic-level disruption of interfaces. |
Visualizations
Diagram 1: Insulin Self-Assembly Equilibrium & Rate-Limiting Step
Diagram 2: Rational Design Workflow for Rapid-Acting Analogs
This whitepaper explores the rational design of long-acting basal insulins, a direct application of foundational research into the Architecture of insulin monomers, dimers, and hexamers. Native insulin exists in a dynamic equilibrium: monomers (the bioactive form) <-> dimers <-> hexamers (stabilized by Zn²⁺). The hexamer is too large for efficient capillary absorption. The core thesis posits that by engineering this self-assembly architecture, one can control the subcutaneous dissociation kinetics, thereby creating stable, depot-like formulations that provide slow, steady monomer release over 24+ hours. This document details the strategies, experimental validation, and tools central to this endeavor.
Core Engineering Strategies for Protraction
Two primary strategies have been successfully commercialized, both relying on modifying the hexamer stability and its post-injection dissociation profile.
| Strategy | Molecular Mechanism | Key Insulin Analog(s) | Protraction Outcome |
|---|---|---|---|
| Isoelectric Point (pI) Shift | Engineering substitutions that raise the insulin's pI from ~5.4 to near-neutral (~6.8-7.0). At the acidic pH of formulation (pH ~4), the molecule is soluble. Upon SC injection (pH ~7.4), reduced solubility causes microprecipitates to form. | Insulin Glargine (Gly⁺²¹, Arg⁺³¹, Arg⁺³²) | Slow dissolution from precipitate provides ~24-hour action. |
| Acylation & Albumin Binding | Attaching a fatty diacid chain via a linker to the insulin molecule. This enables reversible, non-covalent binding to serum albumin. The acyl chain also promotes stable, reversible multi-hexamer formation upon injection. | Insulin Degludec (Thr⁺²⁹, 16-C fatty diacid) | Ultra-long, >42-hour action from soluble multi-hexamer chains. |
| Enhanced Zinc-Hexamer Stability | Modifying residues at the monomer-monomer or hexamer interfaces to strengthen zinc-coordinated hexamer stability, delaying dissociation into absorbable monomers. | Not used alone; combined with other strategies (e.g., in Degludec's phenol-less formulation). | Contributes to delayed monomer release. |
Table 1: Pharmacokinetic/Pharmacodynamic Parameters of Key Long-Acting Analogs
| Parameter | Insulin Glargine U100 | Insulin Degludec U100 | Human NPH Insulin |
|---|---|---|---|
| Time to Onset (h) | 1-2 | 1-2 | 1-2 |
| Time to Peak (h) | No pronounced peak | No pronounced peak | 4-8 |
| Duration of Action (h) | ~24 | >42 (ultra-long) | 12-18 |
| Half-life (SC, h) | ~12 | ~25 | ~7 |
| Coefficient of Variation (PK, %) | ~40-50 | ~20 | ~60-70 |
| pI | ~6.8 | ~5.4 (native) | ~5.4 |
| Formulation State | Clear, acidic (pH 4) | Clear, neutral (pH 7.4) | Cloudy, suspension |
Table 2: Key Structural Modifications and Their Architectural Impact
| Analog | B-Chain Substitution(s) | A-Chain Substitution | Acylation | Impact on Quaternary Structure |
|---|---|---|---|---|
| Glargine | Arg⁺³¹, Arg⁺³² | Gly⁺²¹ | None | Raises pI; promotes hexamer stability at acidic pH but precipitation at neutral pH. |
| Detemir | None | None | Myristic acid (C14) at B²⁹ | Di-hexamer formation & albumin binding. |
| Degludec | Thr⁺²⁹ (removes B³⁰) | None | Hexadecanedioic acid (C16) via γ-L-Glu linker at B²⁹ | Forms soluble, stable multi-hexamers; strong albumin binding. |
Experimental Protocols for Characterization
Protocol: Analyzing Hexamer Stability via Size-Exclusion Chromatography (SEC)
Objective: To determine the oligomeric state (monomer/dimer/hexamer/multi-hexamer) of insulin analogs in formulation and under physiological conditions.
- Column: Equilibrate a Superdex 75 Increase 10/300 GL column with relevant buffer (e.g., phosphate buffer, pH 7.4, with 0.01% Zn²⁺).
- Sample Preparation: Dilute insulin analog to 1 mg/mL in formulation buffer and in simulated physiological buffer (pH 7.4, 140 mM NaCl, 30 μM ZnAc₂, 0.01% phenol if relevant).
- Run: Inject 100 μL sample at 0.5 mL/min. Monitor absorbance at 280 nm.
- Calibration: Use a standard protein mixture (e.g., thyroglobulin, albumin, ovalbumin, ribonuclease A) to establish elution volumes for different molecular weights.
- Analysis: Compare elution peaks of analogs vs. human insulin to identify shifts indicating larger (multi-hexamer) or more stable oligomers.
Protocol: Determining Dissociation Kinetics via Fluorescence Spectroscopy
Objective: To measure the rate of hexamer dissociation into monomers upon dilution, simulating subcutaneous diffusion.
- Labeling: Label insulin analogs with a environmentally sensitive fluorophore (e.g., ANS, 1-anilinonaphthalene-8-sulfonate) that fluoresces upon binding to hydrophobic patches exposed during dissociation.
- Kinetic Setup: Rapidly dilute a concentrated, labeled hexamer solution (in formulation buffer) 100-fold into a cuvette containing phosphate buffer (pH 7.4, 37°C) in a fluorometer.
- Measurement: Monitor fluorescence intensity (ex: 350 nm, em: 480 nm) over time (0-600 seconds).
- Data Fitting: Fit the resulting time-course curve to a first-order or multi-exponential dissociation model to derive dissociation rate constants (k_off).
Protocol: Assessing Albumin Binding Affinity via Surface Plasmon Resonance (SPR)
Objective: To quantify the binding strength (KD) between acylated insulin analogs and human serum albumin (HSA).
- Immobilization: Covalently immobilize HSA on a CM5 sensor chip via amine coupling to ~5000 Response Units (RU).
- Running Buffer: Use HBS-EP+ (pH 7.4) as running buffer.
- Analytes: Prepare serial dilutions of acylated insulin analog (e.g., Degludec) and native insulin (negative control) in running buffer.
- Cycle: Inject analytes at 30 μL/min for 120s association, followed by 300s dissociation. Regenerate with a short pulse of 10 mM glycine, pH 2.0.
- Analysis: Subtract the reference cell and buffer blank sensorgrams. Fit the concentration series data to a 1:1 binding model to determine association (ka), dissociation (kd) rates, and equilibrium dissociation constant (KD).
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Insulin Hexamer Architecture Research
| Reagent / Material | Function & Rationale |
|---|---|
| Recombinant Human Insulin & Analogs | The core substrates for structural and kinetic studies. Must be highly purified (>99%). |
| Zinc Chloride (ZnCl₂) | Essential for stabilizing the native R6 hexamer. Used at micromolar concentrations in buffers. |
| m-Cresol / Phenol | Hexamer-stabilizing excipients used in formulations. Their presence or absence critically impacts dissociation kinetics. |
| Human Serum Albumin (Fatty Acid Free) | Critical for studying the binding and protraction mechanism of acylated analogs (Detemir, Degludec). |
| Size-Exclusion Chromatography (SEC) Columns (e.g., Superdex 75 Increase) | For separating and identifying insulin oligomeric states under native conditions. |
| Surface Plasmon Resonance (SPR) System (e.g., Biacore) | For label-free, real-time quantification of albumin-insulin analog binding kinetics and affinity. |
| Fluorescent Probes (e.g., ANS, TNS) | Environment-sensitive dyes used to monitor conformational changes during hexamer dissociation. |
| Dynamic Light Scattering (DLS) Instrument | To measure the hydrodynamic size distribution of insulin formulations, detecting aggregates or multi-hexamers. |
Visualization of Strategies and Workflows
Title: Design Strategies for Long-Acting Insulin Analogs
Title: Key Experimental Workflow for Protraction Mechanism Study
Solving Stability and Aggregation Challenges in Insulin Product Development
An in-depth technical guide framed within the broader thesis on the Architecture of insulin monomers, dimers, and hexamers
The architectural equilibrium of insulin—monomers, dimers, and hexamers—is fundamental to its stability, bioavailability, and therapeutic efficacy. This delicate balance is critically threatened by three interrelated pitfalls: non-native aggregation, fibrillation, and surface adsorption. These phenomena represent major hurdles in the development of stable insulin formulations and novel insulin analogs, directly impacting drug shelf-life, delivery, and patient safety. This guide delves into the mechanistic underpinnings of these pitfalls, providing detailed experimental methodologies for their study, and offering a toolkit for mitigation strategies relevant to researchers and drug development professionals.
Non-Native Aggregation
Non-native aggregation involves the irreversible association of insulin molecules into disordered, polydisperse oligomers and higher-order species, distinct from the native dimeric and hexameric states. It is often triggered by partial unfolding or exposure of hydrophobic regions.
Key Drivers: Stresses such as thermal denaturation, pH shifts away from the isoelectric point (pI ~5.3), mechanical agitation, or exposure to hydrophobic interfaces.
Experimental Protocol: Monitoring Aggregation via Size-Exclusion Chromatography coupled with Multi-Angle Light Scattering (SEC-MALS)
Objective: To quantify soluble oligomeric species in a stressed insulin sample.
- Sample Preparation: Prepare insulin solution (1 mg/mL) in desired buffer (e.g., 20 mM phosphate, pH 7.4). Subject an aliquot to stress (e.g., 40°C for 24 hours). Keep a control aliquot at 4°C.
- Chromatography: Use an HPLC system with a SEC column (e.g., TSKgel G2000SWxl). Isocratically elute samples at 0.5 mL/min with a mobile phase of 100 mM Na₂SO₄, 20 mM NaH₂PO₄, pH 6.8, to suppress non-specific interactions.
- Detection: The effluent passes through in-line detectors: a UV/Vis detector (280 nm), a MALS detector, and a differential refractometer (dRI).
- Data Analysis: The MALS detector measures absolute molecular weight (MW) at each elution slice, independent of elution volume. Use ASTRA or similar software to derive weight-average molar mass (Mw) and polydispersity index (Đ) for each peak. Integrate peak areas to quantify the percentage of monomer/dimer vs. higher oligomers.
Table 1: Representative SEC-MALS Data of Stressed Insulin (1 mg/mL, pH 7.4, 40°C, 24h)
| Sample Condition | % Monomer/Dimer (by mass) | % Soluble Oligomers (by mass) | Weight-Avg. Mw of Oligomer Peak (kDa) |
|---|---|---|---|
| Control (4°C) | 98.5 ± 0.5 | 1.5 ± 0.5 | ~12 (dimer/hexamer) |
| Thermal Stress (40°C) | 82.3 ± 2.1 | 17.7 ± 2.1 | 85 - 350 (polydisperse) |
Diagram 1: Pathway of non-native aggregation from native insulin.
Fibrillation (Amyloidogenesis)
Insulin fibrillation is a specific, well-ordered aggregation pathway leading to cross-β-sheet amyloid fibrils. It occurs under destabilizing conditions where the monomeric form is predominant, such as low pH and elevated temperature.
Key Mechanism: Nucleation-dependent polymerization, where a rate-limiting nucleus forms, followed by rapid elongation. Agitation introduces shear forces and increases air-water interface, dramatically accelerating fibrillation.
Experimental Protocol: Quantifying Fibrillation Kinetics using Thioflavin T (ThT) Fluorescence
Objective: To monitor the real-time kinetics of fibril formation.
- Sample & Plate Setup: Prepare insulin solution (2 mg/mL) in 20 mM HCl, 100 mM NaCl (pH 1.6). Add ThT dye to a final concentration of 20 µM. Pipette 100 µL into multiple wells of a black, clear-bottom 96-well plate. Include negative controls (buffer + ThT).
- Instrument Settings: Use a plate reader capable of fluorescence top-reading. Set excitation to 440 nm and emission to 485 nm. Set the temperature to 37°C.
- Kinetic Measurement: Perform cyclic agitation (e.g., orbital shaking for 60 seconds every 5 minutes). Measure fluorescence immediately after each agitation period. Run the experiment for 24-48 hours.
- Data Analysis: Plot fluorescence intensity vs. time. Fit the sigmoidal curve to determine the lag time (nucleation phase), apparent growth rate, and final fluorescence plateau.
Table 2: ThT Fluorescence Assay Parameters for Insulin Fibrillation (2 mg/mL, pH 1.6, 37°C)
| Condition | Lag Time (hours) | Apparent Growth Rate (a.u./hour) | Final ThT Fluorescence (a.u.) |
|---|---|---|---|
| Quiescent (No Agitation) | 15.2 ± 1.8 | 12.5 ± 2.1 | 850 ± 75 |
| With Agitation (1 min/5 min) | 1.5 ± 0.3 | 105.3 ± 10.4 | 1200 ± 90 |
Surface Adsorption
Insulin readily adsorbs to a wide variety of surfaces (glass, plastics, tubing, air-water interfaces), leading to loss from solution, potential conformational changes, and nucleation of aggregates or fibrils. This is a critical concern in manufacturing, storage, and delivery (e.g., insulin pumps, infusion sets).
Key Mechanism: Driven by hydrophobic and electrostatic interactions. Adsorption is often maximal near the protein's pI, where net charge is minimal.
Experimental Protocol: Quantifying Adsorption Loss using Radiolabeled Insulin
Objective: To precisely measure insulin loss to container surfaces.
- Labeled Solution: Prepare a trace solution of ¹²⁵I-labeled insulin (or fluorescently labeled insulin) in a physiologically relevant buffer (e.g., PBS, pH 7.4).
- Incubation: Aliquot the solution into the test material vials (e.g., glass, polypropylene, silicone-coated). Also fill vials pre-treated with a blocking agent (e.g., 1% BSA, 0.1% Tween-20). Incubate under gentle rotation at 25°C.
- Sampling: At defined time points (e.g., 1h, 4h, 24h), carefully remove an aliquot from the center of the vial without touching the walls.
- Measurement: Quantify the remaining radioactivity (using a gamma counter) or fluorescence in the aliquot.
- Calculation: The percentage adsorbed is calculated relative to the concentration at time zero (measured from a control vial sacrificed immediately).
Table 3: Adsorption of Insulin (0.1 mg/mL in PBS) to Various Surfaces after 24h Incubation
| Surface Material | % Insulin Adsorbed (± SD) | Mitigation Strategy |
|---|---|---|
| Untreated Glass | 45.2 ± 5.1 | Silanization |
| Polypropylene | 22.7 ± 3.3 | Pre-treatment with BSA |
| Polystyrene | 30.5 ± 4.2 | Pre-treatment with Tween-20 |
| Silicone (Tubing) | 38.8 ± 4.8 | Use of specialized coatings |
| BSA-Blocked Surface | 2.1 ± 0.5 | (Reference) |
Diagram 2: Consequences of surface adsorption on insulin stability.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Materials for Studying Insulin Stability Pitfalls
| Reagent/Material | Function & Purpose | Example Product/Catalog |
|---|---|---|
| Human Recombinant Insulin | Primary substrate for all stability studies. Ensure high purity (>99%). | Sigma-Aldrich I2643 |
| Thioflavin T (ThT) | Fluorescent dye that binds specifically to cross-β-sheet amyloid structures; essential for fibrillation kinetics. | Sigma-Aldrich T3516 |
| Size-Exclusion Chromatography Column | High-resolution separation of monomers, dimers, hexamers, and soluble aggregates. | Tosoh Bioscience TSKgel G2000SWxl |
| Multi-Angle Light Scattering (MALS) Detector | Provides absolute molecular weight measurement for eluting species from SEC. | Wyatt Technology miniDAWN TREOS |
| ¹²⁵I-labeled Insulin or Fluorescent Dye (e.g., Alexa Fluor 488) | Tracer for sensitive quantification of adsorption and low-level aggregation. | PerkinElmer NEX420 |
| BSA (Bovine Serum Albumin) or Tween-20 | Used as blocking agents to passivate surfaces and prevent non-specific adsorption in experiments. | Sigma-Aldrich A7906 / P9416 |
| Quartz Cuvettes or Low-Binding Microplates | Minimize adsorption artifacts during spectroscopic measurements (UV, fluorescence). | BrandTech 759150 (Quartz) / Corning 4515 (Plate) |
| Silanizing Agent (e.g., Sigmacote) | Hydrophobically coats glass surfaces to reduce insulin adsorption. | Sigma-Aldrich SL2 |
This whitepaper addresses a pivotal, applied challenge within the broader thesis on the Architecture of insulin monomers, dimers, and hexamers. A fundamental understanding of insulin's oligomeric states—from the rapid-acting monomer to the stable, protracted hexamer—is essential for designing therapeutic formulations. The strategic application of specific excipients (Zn²⁺, phenol, m-cresol, polysorbates) is not merely a matter of stability or preservation; it is a direct exercise in controlling this oligomeric equilibrium. Formulation optimization, therefore, represents the translational bridge between structural biophysics and clinically efficacious drug products, enabling precise pharmacokinetic profiles.
Excipient Roles: Mechanisms and Quantitative Effects
Each excipient exerts a specific, quantifiable effect on insulin's oligomeric state, stability, and delivery.
Zinc (Zn²⁺)
- Primary Role: Hexamer stabilization.
- Mechanism: Zn²⁺ ions bind at the center of the insulin hexamer, coordinating with His(B10) residues, which is critical for maintaining the R6 (T6) conformation. This stabilizes the hexamer, delaying dissociation and absorption post-injection.
- Key Data: Typically used at a stoichiometry of 2 Zn²⁺ per hexamer (~0.4-0.8 mg/100 IU, or ~0.015-0.025% w/v in formulations).
Phenol and m-Cresol
- Primary Roles: Antimicrobial preservation and allosteric hexamer stabilization.
- Mechanism: These phenolic compounds bind to specific sites on the insulin hexamer (e.g., at the dimer-dimer interface), inducing a conformational shift from the T6 to the R6 state. This further stabilizes the hexamer and modulates its dissociation kinetics.
- Synergy: Phenol and cresol are often used in combination, as they may exhibit synergistic stabilizing and antimicrobial effects.
Polysorbates (20/80)
- Primary Role: Surface-active stabilizer against aggregation.
- Mechanism: Polysorbates competitively adsorb at interfaces (air-liquid, solid-liquid), preventing surface-induced denaturation and fibrillation of insulin. They also directly shield hydrophobic patches on insulin monomers/oligomers in solution.
- Criticality: Essential in modern insulin analog formulations, especially in pump use, to prevent fibrillation at the infusion set.
Table 1: Quantitative Excipient Roles in Insulin Formulation
| Excipient | Typical Concentration Range | Primary Function | Molecular Target & Effect |
|---|---|---|---|
| Zinc (Zn²⁺) | 0.015 - 0.025% w/v (or ~0.4-0.8 mg/100 IU) | Hexamer Stabilization | Binds His(B10); nucleates & stabilizes hexamer structure. |
| Phenol | 0.1 - 0.3% w/v | Antimicrobial / Conformational Modifier | Binds hexamer, induces T6→R6 transition; delays dissociation. |
| m-Cresol | 0.1 - 0.3% w/v | Antimicrobial / Conformational Modifier | Similar to phenol; often used in combination for synergy. |
| Polysorbate 20/80 | 0.005 - 0.02% w/v | Anti-aggregation / Surfactant | Competes for interfaces; shields hydrophobic protein patches. |
| Glycerol | 1.6% w/v | Tonicity Adjuster | Provides isotonicity; mild stabilizing effect. |
Experimental Protocols for Formulation Analysis
Protocol: Size-Exclusion Chromatography (SEC) for Oligomeric Distribution
Objective: Quantify the proportion of insulin monomers, dimers, and hexamers in a formulated solution. Methodology:
- Column: Use a high-resolution SEC column (e.g., TSKgel G2000SWxl).
- Mobile Phase: 50 mM sodium phosphate, 100 mM sodium sulfate, 0.02% sodium azide, pH 7.4. The sulfate suppresses non-size-based interactions.
- Standardization: Run purified insulin monomer, dimer (cross-linked), and hexamer (Zn²⁺-stabilized) standards.
- Sample Preparation: Dilute formulation to ~1 mg/mL in mobile phase. Do not filter if assessing aggregation.
- Analysis: Run at 0.5 mL/min, detect at 214 nm or 280 nm. Integrate peak areas to determine percent distribution.
Protocol: Forced Degregation (Agitation) Study with Polysorbate Efficacy
Objective: Assess the protective effect of polysorbate against surface-induced aggregation. Methodology:
- Sample Prep: Prepare 5 mL aliquots of insulin formulation (100 IU/mL) with and without polysorbate 80 (0.01% w/v) in glass vials.
- Agitation: Place vials on a horizontal shaker platform at 300 rpm, 25°C.
- Time Points: Withdraw samples at 0, 1, 2, 4, 8, 12, and 24 hours.
- Analysis:
- Visual: Inspect for particles/cloudiness.
- Turbidity: Measure optical density at 350 nm or 600 nm.
- SEC: Analyze soluble monomer/oligomer loss and high-molecular-weight aggregate formation.
Protocol: Isothermal Calorimetry (ITC) for Phenol/Zn²⁺ Binding
Objective: Determine binding stoichiometry (n) and affinity (Kd) of phenolic compounds to zinc insulin. Methodology:
- Sample Preparation: Exhaustively dialyze zinc insulin hexamer into a standard buffer (e.g., 20 mM Tris, pH 7.4).
- Cell: Load insulin solution (~0.05 mM hexamer) into the sample cell.
- Syringe: Prepare a solution of phenol or m-cresol (~1.0 mM) in the identical dialysis buffer.
- Experiment: Perform sequential injections of phenol into the insulin cell at constant temperature (25°C).
- Analysis: Fit the integrated heat data to a binding model to derive n, Kd, and ΔH.
Visualizing Formulation Control Pathways
Diagram 1: Excipient Control of Insulin Oligomer & Stability Pathways
Diagram 2: Formulation Optimization Experimental Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Insulin Formulation Research
| Reagent / Material | Function & Rationale | Example / Specification |
|---|---|---|
| Human Insulin or Analog Standards | Primary substrate for formulation studies. High purity is critical. | USP Reference Standards; recombinant, >99% purity. |
| Zinc Chloride (ZnCl₂) | Source of Zn²⁺ ions for hexamer stabilization. | ACS grade, prepared in sterile water for injection (WFI). |
| m-Cresol & Phenol | Antimicrobial preservatives and conformational modifiers. | Pharmaceutical grade, USP/EP compliance. |
| Polysorbate 20 & 80 | Surfactants to mitigate interfacial aggregation. | Low peroxide grade, specified for biopharmaceuticals. |
| Size-Exclusion Chromatography (SEC) System | Gold-standard for quantifying oligomeric/aggregate distribution. | HPLC system with UV detector; TSKgel G2000SWxl or equivalent column. |
| Dynamic Light Scattering (DLS) | Rapid assessment of hydrodynamic size and particle formation. | Instrument with capability to measure sizes from 1 nm to 10 µm. |
| Isothermal Titration Calorimetry (ITC) | Label-free measurement of excipient binding affinity and thermodynamics. | MicroCal PEAQ-ITC or equivalent. |
| Forced Degradation Stations | Controlled stress testing (agitation, temperature). | Horizontal shaker, controlled temperature incubators. |
| Stability Indicating Assay Buffers | For sample dilution and analysis without altering equilibrium. | Phosphate buffers with ionic strength modifiers (e.g., Na₂SO₄). |
1. Introduction: Stability within the Architecture of Insulin Oligomers
The therapeutic efficacy of insulin, a critical life-saving drug for diabetes, is intrinsically linked to its structural integrity. Insulin exists in a dynamic equilibrium of monomers, dimers, and zinc-coordinated hexamers, a structural architecture fundamental to its pharmacokinetics and formulation stability. This oligomeric state directly influences the susceptibility of the protein to primary chemical degradation pathways, notably deamidation and hydrolysis. Deamidation, primarily at AsnB3, and hydrolysis, particularly at Aspartate (Asp) residues, lead to loss of bioactive potency, increased immunogenicity, and the generation of potentially toxic aggregates. This whitepaper provides a technical guide on mitigating these pathways, framed within the context of insulin oligomer architecture, to preserve bioactivity from discovery through formulation.
2. Degradation Pathways: Mechanisms and Impact on Oligomeric States
- Deamidation: A non-enzymatic reaction where the side-chain amide of asparagine (or glutamine) undergoes hydrolysis to form a carboxylic acid. In insulin, AsnB3 is highly labile. The reaction proceeds via a succinimide intermediate, yielding both iso-aspartate (major) and aspartate (minor) products. This modification disrupts the local conformation critical for receptor binding and can alter the monomer-dimer equilibrium.
- Hydrolysis (Peptide Bond Cleavage): Acidic hydrolysis can occur at the C-terminal side of Asp residues (Asp-Pro bonds are exceptionally labile). In insulin, the AspB10-HisB11 bond is a known site. Cleavage severs the polypeptide chain, irrevocably destroying the native structure and bioactivity.
The propensity for these reactions is modulated by the insulin oligomeric state. The hexamer, stabilized by zinc and phenolic ligands (e.g., phenol, cresol), buries susceptible residues like AsnB3 at the dimer-dimer interface, significantly reducing its deamidation rate compared to the more exposed monomeric or dimeric forms.
3. Quantitative Data Summary: Degradation Kinetics
Table 1: Comparative Degradation Half-lives (t₁/₂) of Insulin Oligomeric Forms at pH 7.4, 37°C
| Oligomeric State | Stabilizing Condition | Deamidation (AsnB3) t₁/₂ | Hydrolysis (AspB10-HisB11) t₁/₂ | Primary Assay Method |
|---|---|---|---|---|
| Monomer | Low concentration, no Zn²⁺ | ~10 days | >100 days | RP-HPLC, LC-MS |
| Dimer | Moderate concentration, no Zn²⁺ | ~30 days | >100 days | Size-Exclusion Chromatography |
| Hexamer | 0.33% Phenol, 2 Zn²⁺/hexamer | >2 years | >2 years | X-ray Crystallography, Ion-Exchange HPLC |
Table 2: Impact of Formulation Excipients on Degradation Rates
| Excipient | Concentration | Primary Role | Effect on Deamidation Rate vs. Buffer | Effect on Hydrolysis Rate vs. Buffer |
|---|---|---|---|---|
| Phenol / m-Cresol | 0.1-0.3% (w/v) | Hexamer stabilization, antimicrobial | Decrease by >90% | No significant effect |
| Glycerol | 16% (v/v) | Torsional stabilizer, reduces water activity | Decrease by ~60% | Decrease by ~40% |
| Zn²⁺ ions | 20-80 µg/mL | Hexamer coordination | Decrease by ~95% | No significant effect |
| Polysorbate 20 | 0.01-0.05% (w/v) | Surface tension reduction | Slight increase (exposes monomer) | No significant effect |
4. Experimental Protocols for Assessing Degradation
Protocol 4.1: Forced Deamidation Study (pH/ Temperature Stress)
- Preparation: Prepare insulin samples (1 mg/mL) in 0.05 M phosphate buffers at target pH (7.0, 7.4, 8.0) with and without hexamer-stabilizing excipients (0.3% phenol, 40 µg/mL Zn²⁺).
- Stress Incubation: Aliquot samples into sterile HPLC vials. Incubate in controlled temperature ovens or water baths at 37°C and 45°C. Withdraw triplicate samples at time points (e.g., 0, 1, 2, 4, 8 weeks).
- Analysis: Quench samples by immediate acidification (pH 2.5) and cooling. Analyze by Reversed-Phase High-Performance Liquid Chromatography (RP-HPLC) using a C18 column and a water/acetonitrile gradient with 0.1% TFA. Quantify intact insulin and deamidated variants (eluting earlier). Confirm identity of peaks using in-line Electrospray Ionization Mass Spectrometry (ESI-MS).
- Kinetics: Plot Ln(% intact) vs. time. The slope provides the apparent first-order rate constant (kobs). Calculate t₁/₂ = Ln(2)/kobs.
Protocol 4.2: Peptide Mapping for Site-Specific Hydrolysis Analysis
- Reduction and Alkylation: Denature stressed insulin sample (100 µg) in 6 M Guanidine HCl, reduce with DTT, and alkylate with iodoacetamide.
- Digestion: Desalt and digest with a site-specific protease (e.g., Glu-C) in ammonium bicarbonate buffer, pH 7.8, overnight at 25°C.
- LC-MS/MS Analysis: Separate peptides using nano-flow LC on a C18 column. Analyze eluting peptides with a high-resolution tandem mass spectrometer (e.g., Q-TOF, Orbitrap).
- Data Processing: Use proteomics software (e.g., Mascot, MaxQuant) to identify peptides. Search for non-tryptic cleavages, specifically at Asp residues. The relative abundance of hydrolysis products is quantified by integrating extracted ion chromatograms (XICs) for the precursor and cleaved peptides.
5. Visualization of Concepts and Workflows
Diagram Title: Insulin Oligomer Stability Influences Degradation
Diagram Title: Forced Degradation & Analysis Workflow
6. The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Insulin Stability Research
| Reagent / Material | Function & Rationale |
|---|---|
| Human Recombinant Insulin (Monomeric Analog) | Reference standard for monomeric state studies (e.g., Insulin Lispro, Aspart). Provides baseline degradation kinetics without hexamer stabilization. |
| Zinc Chloride (ZnCl₂), USP Grade | Essential for hexamer formation. Used to study the protective effect of oligomerization against deamidation. |
| Phenol & m-Cresol, Pharmaceutical Grade | Phenolic ligands that allosterically stabilize the insulin hexamer conformation, shielding labile sites. Also act as antimicrobials. |
| Stability-Indicating RP-HPLC Column (C18, 300Å, 3.5µm) | Core analytical tool for separating intact insulin from its deamidated, hydrolyzed, and aggregated variants based on hydrophobicity. |
| Glu-C (Endoproteinase Glu-C) | Protease that cleaves C-terminal to glutamate and aspartate residues. Used in peptide mapping to generate fragments containing labile Asn/Asp sites for detailed MS analysis. |
| Deamidation-Sensitive ELISA Kit | Immunoassay for quantitative detection of iso-aspartate (isoAsp) formation, a direct product of deamidation, in formulation samples. |
| Size-Exclusion Chromatography (SEC) Columns with LC-MS compatibility | For monitoring oligomeric state distribution (monomer/dimer/hexamer/aggregate) under various formulation conditions pre- and post-stress. |
| Stable Isotope-Labeled Amino Acids (¹³C, ¹⁵N) | Used in metabolic labeling during recombinant expression to produce insulin for advanced NMR studies, allowing atomic-level monitoring of degradation-induced conformational dynamics. |
7. Mitigation Strategies Rooted in Oligomer Architecture
Effective preservation of insulin bioactivity requires strategic exploitation of its oligomeric architecture:
- Formulate for the Hexamer: Utilize Zn²⁺ and phenolic ligands at optimal ratios to maximize hexamer population in the vial, minimizing exposure of AsnB3 and other labile sites.
- Optimize pH and Ionic Strength: Maintain formulation pH in the slightly acidic range (pH 7.0-7.4) to balance deamidation rate (minimized at lower pH) and physical stability. Adjust ionic strength to support hexamer integrity.
- Employ Torsional Stabilizers: Incorporate excipients like glycerol or sucrose to reduce solvent-accessible water activity, thereby slowing both hydrolytic and deamidation reactions.
- Engineer Stabilized Analogs: Implement rational protein engineering to substitute labile residues (e.g., AsnB3 to Ser, Gln, or His) or introduce stabilizing mutations that favor the hexameric state without compromising receptor binding affinity.
8. Conclusion
The preservation of insulin's bioactivity is a direct function of controlling its oligomeric state to chemically "lock" the molecule in its less reactive hexameric form. A deep understanding of the architecture of insulin monomers, dimers, and hexamers provides the blueprint for devising rational mitigation strategies against deamidation and hydrolysis. By combining formulation science guided by this structural knowledge, rigorous forced degradation studies, and advanced analytical techniques, researchers can ensure the delivery of stable, potent, and safe insulin therapeutics.
Within the critical research on the architecture of insulin monomers, dimers, and hexamers, analytical techniques like Size Exclusion Chromatography (SEC), High-Performance Liquid Chromatography (HPLC), and Dynamic Light Scattering (DLS) are fundamental. They assess purity, stability, and oligomeric distribution. However, aberrations in data from these methods are not merely noise; they are red flags signaling underlying sample or methodological issues. This guide interprets common aberrations within the context of insulin self-assembly research, providing protocols and tools for robust analysis.
SEC Aberrations in Insulin Oligomer Analysis
Size Exclusion Chromatography is pivotal for separating insulin monomers (~5.8 kDa), dimers (~11.6 kDa), and hexamers (~34.9 kDa). Deviations from expected elution profiles indicate potential problems.
Common Red Flags and Interpretations:
- Premature/Early Elution: Indicates non-ideal interactions with the column matrix (e.g., hydrophobic or ionic interactions), often due to inappropriate mobile phase (pH, ionic strength). For insulin, this can mimic a larger oligomeric state.
- Broadened or Tailing Peaks: Suggests sample heterogeneity, column overloading, or slow exchange between oligomeric states during separation.
- Extra Peaks: Can signal aggregation (high molecular weight), fragmentation (low molecular weight), or excipient/interferent presence.
- Shift in Expected Elution Volume: Between runs, this may indicate column degradation or inconsistent run conditions.
Table 1: SEC Aberrations in Insulin Analysis
| Aberration | Potential Cause | Implication for Insulin Architecture |
|---|---|---|
| Additional peak > Hexamer void | Soluble aggregate formation | Incipient fibrillation or misfolded oligomers. |
| Peak broadening at dimer position | Dynamic monomer-dimer equilibrium | Fast exchange kinetics on chromatographic timescale. |
| Retention time shift vs. standard | Change in mobile phase pH/ionic strength | Altered net charge affecting interaction with resin. |
| Loss of resolution | Column degradation or overloading | Inability to monitor critical monomer-hexamer transition. |
Detailed SEC Protocol for Insulin Oligomer Separation
- Column: Use a high-resolution silica- or polymer-based SEC column with separation range of 1-100 kDa.
- Mobile Phase: 50 mM Sodium Phosphate, 100 mM Sodium Sulfate, pH 7.4. The sulfate suppresses non-specific insulin-column interactions.
- Flow Rate: 0.5 mL/min.
- Detection: UV at 214 nm (peptide bond) and 280 nm.
- Sample Preparation: Dissolve human insulin at 1 mg/mL in the mobile phase. Incubate at defined temperature (e.g., 4°C favors monomers, 37°C favors hexamers) for 2 hours prior to injection.
- Injection Volume: 20 µL.
- Calibration: Perform with a native protein molecular weight marker kit.
HPLC Aberrations (Reverse-Phase)
Reverse-Phase HPLC (RP-HPLC) assesses insulin purity and chemical stability by separating variants based on hydrophobicity.
Common Red Flags and Interpretations:
- Peak Splitting: Often indicates the presence of diastereomers or conformational isomers.
- Peak Tailing: Can suggest secondary interactions with residual silanols on the column stationary phase.
- New/Shouldering Peaks: Primary indicators of chemical degradation (e.g., deamidation at AsnA21/B3, hydrolysis, oxidation of Met).
- Changing Retention Time: Column aging or temperature/eluent gradient inconsistencies.
Table 2: RP-HPLC Aberrations in Insulin Analysis
| Aberration | Potential Cause | Chemical Degradation Implication |
|---|---|---|
| Earlier eluting shoulder | Deamidation (formation of acidic variant) | Common degradation pathway affecting potency. |
| Later eluting minor peak | Covalent dimer/aggregate | Disulfide scrambling or cross-linking. |
| Multiple small peaks post-main peak | Oxidation products | Methionine sulfoxide formation. |
| General peak broadening | Column damage or suboptimal pH | Masks detection of critical degradants. |
Detailed RP-HPLC Protocol for Insulin Purity
- Column: C8 or C18 column, 150 x 4.6 mm, 3.5 µm particle size.
- Mobile Phase A: 0.1% Trifluoroacetic Acid (TFA) in water.
- Mobile Phase B: 0.1% TFA in acetonitrile.
- Gradient: 30% B to 50% B over 25 minutes.
- Flow Rate: 1.0 mL/min.
- Column Temperature: 40°C.
- Detection: UV at 214 nm.
- Sample: Dissolve insulin at 0.5 mg/mL in 0.01 M HCl to favor monomeric state for analysis.
Dynamic Light Scattering (DLS) Aberrations
DLS measures hydrodynamic diameter and polydispersity, critical for assessing insulin oligomerization and aggregation in solution.
Common Red Flags and Interpretations:
- High Polydispersity Index (PDI >0.2): Indicates a heterogeneous mixture of sizes (e.g., monomers, hexamers, and aggregates coexisting).
- Multiple Peaks in Size Distribution: Direct evidence of a polydisperse system. A small peak at >100 nm can signal early aggregation.
- Intensity vs. Volume Discrepancies: A large aggregate peak in intensity distribution that nearly vanishes in volume/mass distribution indicates trace amounts of large, highly scattering particles (critical early warning).
- Changing Size with Concentration or Temperature: Expected for insulin's associative equilibrium, but erratic changes suggest instability.
Table 3: DLS Aberrations in Insulin Analysis
| Aberration | Potential Cause | Implication for Solution State |
|---|---|---|
| High PDI (>0.3) at neutral pH | Coexistence of multiple oligomeric states | Sample is in dynamic equilibrium or contaminated. |
| Large peak in intensity, not volume | Few large aggregates/scatterers | Onset of fibrillation; a critical red flag. |
| Mean size drifting over time | Time-dependent aggregation/assembly | Sample instability under measurement conditions. |
| Poor correlation function fit | Too many large aggregates or dust | Sample preparation failure. |
Detailed DLS Protocol for Insulin Hydrodynamic Size
- Instrument: Standard DLS instrument with 633 nm laser and detector at 173° (non-invasive backscatter).
- Sample Preparation: Filter all buffers (0.02 µm filter) and centrifuge insulin samples at 15,000 x g for 10 minutes at 4°C to remove dust.
- Concentration: 1 mg/mL insulin in a defined buffer (e.g., 20 mM phosphate, pH 7.4, with/without Zn²⁺).
- Equilibration: Equilibrate sample in cuvette at measurement temperature (e.g., 25°C) for 5 minutes.
- Measurement: Perform a minimum of 10-12 measurements per sample, 10 seconds each.
- Analysis: Use intensity-based distribution for detecting aggregates. Report Z-average size and PDI from cumulants analysis, and peak sizes from distribution analysis.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Insulin Oligomer Architecture Studies
| Reagent/Material | Function in Analysis | Key Consideration |
|---|---|---|
| SEC Column (e.g., Superdex 75 Increase) | High-resolution separation of monomers, dimers, hexamers. | Choice of mobile phase additives (e.g., Na₂SO₄) is critical to suppress adsorption. |
| RP-HPLC Column (C8 or C18) | Assessment of chemical purity and degradation products. | Requires acidic mobile phases (TFA) for good peak shape. |
| Zinc Chloride (ZnCl₂) | Essential for hexamer stabilization. | Concentration directly controls hexamer population. |
| Phenol/M-Cresol | Pharmaceutical stabilizers; affect self-assembly kinetics. | Can interfere with UV detection if not dialyzed out. |
| High-Purity Buffer Salts | Maintain precise pH and ionic strength for reproducibility. | Contaminants can catalyze deamidation or oxidation. |
| 0.02 µm Anotop Filters | Critical for dust-free DLS samples. | Syringe filters compatible with protein samples. |
| Certified Molecular Weight Markers | SEC calibration for accurate size assignment. | Must be analyzed under identical buffer conditions. |
Visualizing Analytical Workflows and Data Interpretation
Title: SEC Anomaly Investigation Workflow
Title: Multi-Method Triangulation of an Anomaly
Title: Insulin Assembly Pathway & Red Flag
This whitepaper is framed within a broader research thesis investigating the Architecture of Insulin Monomers, Dimers, and Hexamers. Insulin's stability and shelf-life in therapeutic formulations are intrinsically linked to its dynamic equilibrium between these multimeric states. Monomeric insulin is the pharmacologically active form, yet the dimeric and, particularly, the zinc-coordinated hexameric states confer critical stability against aggregation and chemical degradation during storage. Accelerated stability studies that monitor shifts in this equilibrium provide a powerful predictive tool for real-time shelf-life determination. This guide details the methodologies and analytical frameworks for leveraging multimeric state changes as key stability-indicating parameters.
Quantitative Data on Insulin Multimeric States & Stability
Table 1: Properties of Insulin Multimeric States Relevant to Stability
| Multimeric State | Molecular Weight (kDa) | Typical Conditions for Prevalence | Key Stabilizing Interactions | Role in Formulation Stability |
|---|---|---|---|---|
| Monomer | ~5.8 | Very low concentration (<0.1 µM), neutral pH, no Zn²⁺ | N/A (active form) | Prone to fibrillation; target for bioavailability. |
| Dimer | ~11.6 | Low concentration, moderate pH, no Zn²⁺ | Hydrophobic (B-chain) & H-bonding | Intermediate state; less stable than hexamer. |
| Hexamer | ~34.8 | Pharmaceutical formulations (≥0.1 mM), presence of Zn²⁺, phenolic excipients (e.g., m-cresol) | Coordinated by 2 Zn²⁺ ions, H-bonding, phenolic ligand binding | Provides maximal physical & chemical stability; resists aggregation. |
Table 2: Impact of Stress Conditions on Multimeric Equilibrium & Degradation
| Accelerated Stress Condition | Typical Protocol | Observed Shift in Multimeric State | Associated Degradation Pathways |
|---|---|---|---|
| Elevated Temperature | 25°C, 40°C, 50°C for 0, 1, 3, 6 months | Hexamer → Dimer → Monomer (with time/temp) | Deamidation (Asn A21), Hydrolysis, Aggregation |
| Agitation/Shear | Orbital shaking, vortexing, pumping | Surface-induced denaturation & dimer dissociation | Fibrillation, Subvisible particle formation |
| pH Extremes | pH 3.0 & pH 8.0 buffers, 25°C | Monomer favored at low pH; dissociation at high pH | Covalent dimerization (pH 3), Deamidation (pH > 6) |
| Freeze-Thaw Cycling | Multiple cycles (-20°C to 25°C) | Local concentration effects disrupt equilibrium | Precipitation, Insulin loss at container interface |
Experimental Protocols for Multimeric State Analysis
Protocol 3.1: Size-Exclusion Chromatography (SEC) with Multi-Angle Light Scattering (MALS)
Objective: Quantify absolute molecular weights and relative populations of monomers, dimers, and hexamers in stressed samples. Materials: HPLC system, SEC column (e.g., TSKgel G2000SWXL), MALS detector, refractive index (RI) detector. Procedure:
- Buffer Preparation: Use 100 mM sodium phosphate, 100 mM sodium sulfate, 0.05% sodium azide, pH 7.4. Filter (0.22 µm) and degas.
- Sample Prep: Dilute insulin formulation to 1 mg/mL in running buffer. Centrifuge at 14,000g for 10 min to remove particulates.
- Chromatography: Inject 50 µL. Isocratic elution at 0.5 mL/min. Column temperature: 25°C.
- Data Analysis: Use MALS/RI data with dn/dc=0.185 mL/g to calculate absolute molar mass across the elution peak. Deconvolute peaks corresponding to hexamer (~35 kDa), dimer (~12 kDa), and monomer (~6 kDa). Report % area under the curve for each species.
Protocol 3.2: Native Mass Spectrometry (Native MS)
Objective: Directly observe and quantify non-covalent multimeric complexes under near-physiological conditions. Materials: Q-TOF or Orbitrap mass spectrometer with nano-electrospray ionization source. Procedure:
- Buffer Exchange: Desalt insulin sample into 100 mM ammonium acetate, pH 6.8, using centrifugal filters (10 kDa MWCO).
- Sample Loading: Load into gold-coated nano-ESI capillaries.
- Instrument Parameters: Use low collision energy (20-50 eV) in the source region to preserve non-covalent interactions. Capillary voltage: 1.2 kV. Backing pressure increased to 6-8 mbar.
- Data Acquisition & Analysis: Acquire spectra in positive ion mode over m/z 2000-8000. Deconvolute charge state series to obtain zero-charge mass spectra. Integrate peak intensities for each multimer to determine relative abundances.
Protocol 3.3: Kinetics of Dissociation via Stopped-Flow Fluorescence
Objective: Measure the kinetics of Zn²⁺-induced hexamer dissociation under dilution, a critical parameter for stability modeling. Materials: Stopped-flow instrument, fluorescence detector. Insulin labeled with environmentally sensitive fluorophore (e.g., ANS). Procedure:
- Labeling: Incubate insulin with 8-Anilino-1-naphthalenesulfonate (ANS).
- Rapid Dilution: Mix equal volumes of concentrated insulin hexamer (1 mM in Zn²⁺) and chelating buffer (EDTA) in the stopped-flow apparatus. Final dilution >100-fold.
- Monitoring: Record fluorescence change (ex 360 nm, em 480 nm) over time (milliseconds to seconds).
- Kinetic Analysis: Fit the fluorescence transient to a multi-exponential model to extract dissociation rate constants (k_off) for hexamer → dimer → monomer.
Visualizations
Diagram 1: Insulin Multimerization Equilibrium & Stability Relationships
Diagram 2: Workflow for Shelf-Life Prediction from Multimeric State
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Insulin Multimer Stability Studies
| Item | Function & Relevance | Example Product/ Specification |
|---|---|---|
| Human Insulin (rDNA) | Primary analyte for stability studies. High purity (>99%) is essential. | USP Reference Standard, or in-house purified bulk. |
| Zinc Chloride (ZnCl₂) | Critical for hexamer formation. Concentration ratio (Zn²⁺:Insulin) must be controlled. | Molecular biology grade, trace metal analyzed. |
| Phenolic Excipients (m-cresol, phenol) | Act as allosteric ligands, stabilizing the hexameric R-state and providing antimicrobial activity. | Pharmaceutical grade, USP. |
| Ammonium Acetate (MS Grade) | Volatile buffer for native mass spectrometry, preserving non-covalent interactions. | LC-MS grade, 99.99% purity. |
| SEC-MALS Buffer Salts | High ionic strength phosphate/sulfate buffers to minimize non-size exclusion interactions during SEC. | HPLC grade Na₂HPO₄, NaH₂PO₄, Na₂SO₄. |
| Size-Exclusion Chromatography Column | High-resolution separation of insulin multimers based on hydrodynamic radius. | TSKgel G2000SWXL (7.8 mm ID x 30 cm). |
| Fluorescent Probe (ANS) | Hydrophobic dye used in stopped-flow to monitor conformational changes during dissociation. | 8-Anilino-1-naphthalenesulfonic acid, ammonium salt. |
| Stability Study Vials | Chemically inert containers to prevent adsorptive losses. | Type I glass vials with fluoropolymer-coated stoppers. |
This case study is framed within the critical context of ongoing research into the architecture of insulin monomers, dimers, and hexamers. Understanding these quaternary structures is paramount for developing stable, safe, and efficacious therapeutic formulations. A common challenge in the development of pre-filled syringe (PFS) formulations of protein therapeutics, including insulin analogs, is the unexpected appearance of high-molecular-weight species (HMWS), primarily aggregates, during stability studies. This guide details a systematic, technical approach to investigating the root cause of such an event.
Background: Insulin Oligomerization Dynamics
Insulin's propensity to self-associate into dimers and, in the presence of zinc, hexamers, is a fundamental aspect of its biochemistry. This equilibrium is sensitive to formulation conditions (pH, ionic strength, excipients), mechanical stress, and interfacial interactions. HMWS formation in a PFS represents a shift in this equilibrium towards irreversible aggregation, posing potential risks to product safety (immunogenicity) and efficacy.
Initial Observation and Problem Statement
A candidate insulin analog formulation, filled into siliconized glass PFS, showed an increase in HMWS from <0.5% at initial time point to 3.2% after 3 months of storage at 5°C. The specification limit is ≤2.0%. No significant change was observed in vials.
Table 1: Stability Data Summary for HMWS by SEC-HPLC
| Time Point | Storage Condition | Primary Packaging | HMWS (%) | Monomer (%) |
|---|---|---|---|---|
| T0 | NA | PFS & Vial | 0.4 | 99.1 |
| 1 Month | 5°C | Vial | 0.5 | 98.9 |
| 1 Month | 5°C | PFS | 1.8 | 97.6 |
| 3 Months | 5°C | Vial | 0.6 | 98.8 |
| 3 Months | 5°C | PFS | 3.2 | 96.2 |
Hypothesis Generation
Based on the differential outcome between PFS and vial, hypotheses center on interactions unique to the syringe system:
- Silicon Oil-Induced Aggregation: Shear during shipping or piston movement destabilizes the protein-silicone interface.
- Leachates: Tungsten (from syringe barrel manufacturing) or silicone oil components leach into the formulation.
- Surface-Induced Denaturation: Increased air-liquid interface during plunger movement or headspace formation.
- Stopper Interaction: Leachates from the syringe plunger (elastomer components).
Experimental Investigation Protocols
Experiment 1: Analysis of Silicone Oil and Interfacial Stress
Objective: To assess the role of silicone oil-induced aggregation. Protocol:
- Empty 1 mL of formulation into a clean glass vial.
- Add 10 µL of the silicone oil used for syringe lubrication.
- Subject the vial to controlled agitation on an orbital shaker (200 rpm, 24 hours, 25°C).
- Carefully extract the aqueous phase, avoiding the oil layer.
- Analyze for sub-visible particles (micro-flow imaging) and HMWS (SEC-HPLC).
- Compare against a non-agitated control and a sample agitated without silicone oil.
Experiment 2: ICP-MS Analysis for Tungsten and Other Metals
Objective: To quantify leached tungsten and other metals from the syringe barrel. Protocol:
- Recover liquid from stability PFS units (n=5) and control vials.
- Digest 1 mL of each sample with concentrated nitric acid (trace metal grade) using a microwave digestion system.
- Dilute digested samples appropriately with deionized water.
- Analyze via Inductively Coupled Plasma Mass Spectrometry (ICP-MS).
- Compare against a freshly prepared formulation sample and the known formulation buffer.
Experiment 3: Forced Degradation at the Air-Water Interface
Objective: To evaluate sensitivity to interfacial denaturation. Protocol:
- Place 1 mL of formulation in a 2 mL glass vial.
- Create a high air-water interface by horizontal shaking (100 cycles/min, 37°C).
- Sample at 0, 24, 48, and 72 hours.
- Analyze for HMWS (SEC-HPLC) and measure turbidity at 350 nm.
Experiment 4: Plunger Elastomer Extractables Study
Objective: To identify organic leachates from the plunger. Protocol:
- Prepare extracts by incubating plunger components in formulation buffer at 40°C for 10 days.
- Analyze the extracts using Liquid Chromatography-Mass Spectrometry (LC-MS) for non-volatile organics and Headspace Gas Chromatography-Mass Spectrometry (HS-GC-MS) for volatiles.
- Spike formulation with identified leachates at 10x the detected level and monitor HMWS formation upon temperature stress (40°C/1 week).
Results and Root Cause Analysis
Table 2: Summary of Investigational Experiment Results
| Experiment | Key Finding | Implication for HMWS |
|---|---|---|
| 1: Silicone Oil Agitation | HMWS increased to 2.1% in oil-agitated sample vs. 0.5% in control. | Silicone oil-water interface is a contributor. |
| 2: ICP-MS for Metals | Tungsten levels in PFS: 120 ppb. Vial: <5 ppb. Specification: ≤50 ppb. | Root Cause Identified. Tungsten catalyzes oxidation and aggregation. |
| 3: Air-Water Interface | HMWS reached 1.5% after 72h shaking. | Interfacial stress is a moderate contributor. |
| 4: Plunger Extractables | No significant organic leachates identified above safety thresholds. | Plunger is not the primary contributor. |
The primary root cause was identified as tungsten leaching from the syringe barrel. Tungsten residues, left from the pin used to form the syringe barrel during manufacturing, can catalyze the oxidation of protein side chains and promote aggregation. This finding directly connects to insulin architecture research: perturbations like metal-catalyzed oxidation can destabilize the delicate monomer-dimer-hexamer equilibrium, favoring aberrant association pathways.
Workflow Diagram of Investigation
Title: HMWS Investigation Workflow from Observation to Root Cause
Proposed Mitigation Strategies and Confirmation
- Source Alternative Syringes: Switch to PFS manufactured using a tungsten-free process (e.g., ceramic pin).
- Formulation Optimization: Add a chelating agent (e.g., EDTA) to sequester trace metals. Note: Must confirm no impact on insulin zinc hexamer stability.
- Process Change: Implement a syringe washing step before filling to remove residual tungsten.
Table 3: Mitigation Strategy Confirmation Study Design
| Strategy | Study Arms | Storage Conditions | Key Analytics |
|---|---|---|---|
| Tungsten-Free PFS | New PFS vs. Original PFS vs. Vial | 5°C, 25°C/60%RH | HMWS (SEC), Tungsten (ICP-MS) |
| Chelator Addition | Formulation ± 0.05% EDTA in Original PFS | 40°C (Accelerated) | HMWS, Monomer Purity, Zn²⁺ Content |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Materials for Investigating Protein Aggregation in PFS
| Item | Function/Benefit | Example/Note |
|---|---|---|
| Tungsten-Free Pre-filled Syringes | Control for tungsten-induced aggregation; critical for metal-sensitive biologics. | Supplied by specialty manufacturers (e.g., SiO2 Materials Science, Schott). |
| Silicone Oil (Highly Purified) | For spiking studies to model interfacial shear and adsorption. | Dow Corning 360, 1000 cSt. |
| ICP-MS Standard Solutions | For quantitative calibration in leachate testing of metals (W, Si, Al, etc.). | Multi-element standards from accredited suppliers (e.g., Inorganic Ventures). |
| Recombinant Human Insulin & Analogs | Well-characterized model proteins for studying oligomer dynamics. | Commercially available for research (e.g., Sigma-Aldrich). |
| Size-Exclusion HPLC Columns | High-resolution separation of monomers, dimers, and HMWS. | TSKgel G3000SWxl, AdvanceBio SEC 300Å. |
| Micro-Flow Imaging (MFI) System | Quantifies and characterizes sub-visible particles (2-100 µm). | ProteinSimple MFI 5200. |
| Stable Isotope-Labeled Amino Acids | For mechanistic studies on aggregation pathways using MS. | Used in SILAC or pulse-labeling experiments. |
This case study underscores that troubleshooting aggregation in PFS requires a holistic understanding of both protein science (insulin architecture) and the drug product system (primary packaging). The identification of tungsten as a root cause highlights a critical interface between manufacturing processes and protein stability. Solutions must be evaluated not only for their mitigation of HMWS but also for their potential impact on the intended therapeutic protein structure and pharmacokinetics. This systematic approach provides a template for resolving similar challenges in biotherapeutic development.
Benchmarking Innovation: Structural and Clinical Comparison of Modern Insulin Analogs
1. Introduction
This guide provides a technical framework for the comparative structural analysis of insulin analogs, situated within the broader thesis research on the architecture of insulin monomers, dimers, and hexamers. Understanding the precise conformational changes induced by amino acid substitutions in therapeutic analogs is critical for rational drug design, enabling the modulation of pharmacokinetic profiles and receptor binding affinities. Overlaying high-resolution crystal structures is the principal method for visualizing these subtle yet functionally significant differences.
2. Key Structural States and Therapeutic Analogs
The functional architecture of insulin exists in an equilibrium of oligomeric states. Monomers are the bioactive form. Dimers form via antiparallel β-sheet hydrogen bonding between B24-B26 chains. Hexamers, stabilized by two central Zn²⁺ ions and phenolic ligands (e.g., phenol, m-cresol) in commercial formulations, consist of a trimer of dimers. Therapeutic analogs are engineered to perturb this equilibrium to achieve desired absorption profiles.
Table 1: Representative Insulin Analogs and Key Modifications
| Analog Name (Commercial) | Key Structural Modification(s) | Primary Designed Effect on Oligomerization/Pharmacokinetics |
|---|---|---|
| Insulin Lispro (Humalog) | Pro(B28) Lys(B28), Lys(B29) → Pro(B29) | Reduces dimer stability, accelerates dissociation into monomers. |
| Insulin Aspart (NovoRapid) | Pro(B28) → Asp(B28) | Disrupts B28-Pro interaction, weakening dimer formation. |
| Insulin Glargine (Lantus) | Gly(A21) → Asn, Arg(B31)-Arg(B32) extension | Shifts isoelectric point, causing precipitation at injection site for prolonged action. |
| Insulin Degludec (Tresiba) | Dele-Thr(B30), Lys(B29) → Nε-hexadecandioyl-γ-Glu | Multi-hexamer formation upon subcutaneous injection, creating a depot. |
| Fast-Acting (Monomeric) | Various (e.g., omitted Zn²⁺, specific mutations) | Engineered to remain predominantly monomeric in formulation. |
3. Experimental Protocol: Structural Overlay and Analysis
3.1. Data Acquisition and Preprocessing
- Source: Retrieve crystal structures from the Protein Data Bank (PDB). Current, relevant entries (as of 2023-2024) include: 1TRZ (Human insulin), 1LPH (Lispro), 1ZEG (Aspart), 3I3Z (Glargine), 4LRM (Degludec in hexameric form).
- Software: Molecular visualization and analysis suites such as PyMOL (Schrödinger) or UCSF ChimeraX.
- Protocol:
- Load all structures into the analysis software.
- Structural Alignment: Superimpose the analog structure onto the native insulin structure using a least-squares fitting algorithm. Typically, alignment is performed on a conserved core (e.g., all Cα atoms of residues A1-A21 and B1-B29, excluding modified regions).
- Root Mean Square Deviation (RMSD) Calculation: Quantify the global structural difference by calculating the RMSD (in Ångströms) of the aligned Cα atoms.
- Local Deviation Analysis: Identify regions of high conformational divergence by visualizing per-residue Cα displacement or calculating local RMSD for specific segments (e.g., B-chain C-terminus, critical dimer/hexamer interface residues B8, B12, B16, B23-28).
3.2. Quantitative Comparison of Oligomer Interfaces
- Method: Analyze intermolecular contacts within dimer and hexamer interfaces.
- Metrics:
- Interface Area: Calculate the buried surface area (Ų) upon oligomer formation using tools like PISA (Protein Interfaces, Surfaces and Assemblies).
- Hydrogen Bonds/Salt Bridges: Identify and count specific polar interactions stabilizing the interface.
- Non-bonded Contacts: Map van der Waals interactions.
Table 2: Hypothetical Comparative Analysis of Hexamer Interfaces
| Metric | Native Insulin (PDB: 1TRZ) | Insulin Lispro (PDB: 1LPH) | Insulin Degludec (PDB: 4LRM) |
|---|---|---|---|
| Global Cα RMSD vs. Native (Å) | 0.00 | 0.20 | 0.85 |
| Dimer-Dimer Interface Area (Ų) | 1250 | 1180 | 1350* |
| Key Dimer Interface H-bonds | B24 C=O...N B26 (antiparallel β-sheet) | Weakened/Disrupted | Modified/Extended |
| Zn²⁺ Coordination Geometry | Tetrahedral (His B10) | Tetrahedral | Tetrahedral |
| Phenol Binding Site Occupancy | Yes | Yes | Yes, with acyl chain modifications |
Note: Increased in Degludec due to hexamer-stabilizing dihexamer formation.
4. The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Insulin Structural Biology
| Reagent/Material | Function in Research |
|---|---|
| High-Purity Insulin/ Analog | (>99%) Starting material for crystallization to ensure homogeneity. |
| Crystallization Screen Kits (e.g., Hampton Research, Jena Bioscience) | Matrices of pH, precipitant, and salt conditions to identify initial crystal leads. |
| Zinc Chloride (ZnCl₂) | Essential divalent cation for promoting and stabilizing the T6 hexameric state. |
| Phenol or m-Cresol | Allosteric effector that stabilizes the R6 hexameric conformation; also acts as preservative. |
| Size-Exclusion Chromatography (SEC) Columns | To separate and analyze oligomeric states (monomer, dimer, hexamer) in solution prior to crystallization. |
| Synchrotron Beamtime | Access to high-intensity X-ray source for collecting diffraction data from small, weakly diffracting crystals. |
5. Visualizing the Analysis Workflow and Structural Consequences
Diagram 1: Structural Overlay & Analysis Workflow (89 chars)
Diagram 2: Insulin Oligomer Equilibrium & Action (86 chars)
Within the thesis context of "Architecture of insulin monomers, dimers, and hexamers research," validating the mechanism of action (MoA) is paramount. A critical step is establishing a quantitative bridge between the in vitro self-assembly kinetics of insulin oligomers and the observed in vivo pharmacokinetic/pharmacodynamic (PK/PD) profile. This guide details the technical approach for this correlation, essential for rational formulation design and developing novel insulin analogs.
The Oligomeric State Landscape: Architecture and Implications
Insulin's oligomerization is concentration-dependent and dictates its absorption and bioavailability. The equilibrium is formulated as:
Monomer (M) ⇌ Dimer (D) ⇌ Hexamer (H) + Zn²⁺
Hexamers are stabilized by Zn²⁺ and phenolic ligands (e.g., m-cresol in formulations). The monomer is the bioactive form absorbed from subcutaneous tissue and binding to the insulin receptor.
Table 1: Key Properties of Insulin Oligomeric States
| Oligomeric State | Molecular Weight (kDa) | Approx. Radius (nm) | Relative Receptor Affinity | Primary Role in PK |
|---|---|---|---|---|
| Hexamer (Zn²⁺-bound) | ~36 | ~2.5 | Very Low | Depot form in formulation and SC tissue |
| Dimer | ~12 | ~1.8 | Low | Transient state during dissociation |
| Monomer | ~6 | ~1.2 | High | Absorbable, bioactive form |
Experimental Protocols
In VitroSelf-Assembly Kinetics Measurement
Objective: Quantify the rates of hexamer dissociation and monomer formation under physiologically mimetic conditions.
Protocol: Stopped-Flow Fluorescence Spectroscopy
- Principle: Rapid mixing of a diluted insulin formulation (pre-dominantly hexameric) with a dissociation buffer, monitoring intrinsic tryptophan fluorescence or extrinsic dye (e.g., ANS) emission shift over milliseconds to seconds.
- Reagents:
- Test insulin formulation (e.g., 100 µM in presence of Zn²⁺ and phenol).
- Dissociation Buffer: 50 mM Tris-HCl, 100 mM NaCl, pH 7.4, 1 mM EDTA (chelates Zn²⁺), 37°C.
- Procedure: a. Load one syringe with insulin formulation (diluted to 10 µM final hexamer concentration). b. Load second syringe with dissociation buffer. c. Rapidly mix at 1:1 ratio in the stopped-flow chamber. d. Record fluorescence emission at 350 nm (excitation at 280 nm) over 0.001 to 1000 seconds. e. Fit the kinetic trace to a multi-exponential model to derive rate constants (k_off) for dissociation steps (e.g., Hexamer→Tetramer+Dimer, Dimer→2 Monomers).
In VivoPharmacokinetic Study in Animal Model
Objective: Measure the time-concentration profile of insulin in plasma after subcutaneous administration.
Protocol: Rat Subcutaneous PK Study
- Animal Preparation: Cannulate jugular vein of Sprague-Dawley rats (n=6/group) for serial blood sampling.
- Dosing: Administer a single subcutaneous bolus of insulin formulation (0.5 U/kg) in the flank.
- Sampling: Collect blood samples at pre-dose, 5, 15, 30, 60, 120, 180, and 240 minutes post-dose.
- Bioanalysis: Quantify plasma insulin concentration using a validated ELISA specific for insulin, not cross-reactive with C-peptide.
- PK Analysis: Non-compartmental analysis to determine Cmax, Tmax, and AUC. Use compartmental modeling (e.g., two-compartment with SC absorption) to derive the absorption rate constant (k_a).
Data Correlation and MoA Validation
The core validation lies in correlating the in vitro dissociation rate constant (kdiss, hexamer→monomer) with the *in vivo* absorption rate constant (ka). A strong positive correlation confirms that subcutaneous absorption is rate-limited by hexamer dissociation.
Table 2: Example Correlation Data for Insulin Analogs/Formulations
| Formulation | In Vitro t½ Dissociation (min) | In Vitro k_diss (min⁻¹) | In Vivo T_max (min) | In Vivo k_a (min⁻¹) | Relative Bioavailability (%) |
|---|---|---|---|---|---|
| Regular Human Insulin (Zn²⁺/phenol) | 45.0 | 0.0154 | 120 | 0.025 | 100 (Reference) |
| Rapid-Acting Analog A (Zn²⁺-free) | 2.5 | 0.277 | 50 | 0.055 | 98 |
| Rapid-Acting Analog B (engineered monomer) | 0.1 | 6.93 | 30 | 0.090 | 95 |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function/Explanation |
|---|---|
| Recombinant Human Insulin (various analogs) | Primary substrate for oligomerization studies. Analog mutations (e.g., Lispro, Aspart) destabilize hexamers. |
| Zinc Chloride (ZnCl₂) | Stabilizes insulin hexamers. Critical for studying formulation effects. |
| m-Cresol / Phenol | Formulation preservatives that also allosterically stabilize the hexameric R-state. |
| EDTA / EGTA | Chelating agents used in vitro to sequester Zn²⁺ and trigger controlled hexamer dissociation. |
| Stopped-Flow Spectrofluorimeter | Instrument for measuring rapid kinetic events (ms-s) like oligomer dissociation. |
| Size-Exclusion Chromatography (SEC) with MALS | To characterize oligomeric distribution (monomer/dimer/hexamer) in formulation pre- and post-experiment. |
| Analytical Ultracentrifugation (AUC) | Gold-standard for determining absolute molecular weights and equilibrium constants of self-association. |
| Insulin-Specific ELISA Kit | For sensitive and specific quantification of insulin in complex biological matrices (plasma). |
| Physiologic Buffer Systems (e.g., PBS, Tris at pH 7.4, 37°C) | To mimic subcutaneous interstitial fluid conditions during in vitro kinetics. |
Title: Linking Insulin Oligomer Dissociation to PK/PD
Title: MoA Validation Workflow for Insulin
Within the critical research framework of the architecture of insulin monomers, dimers, and hexamers, establishing biosimilarity represents a foundational scientific and regulatory challenge. A biosimilar is a biological product highly similar to an already approved reference product, notwithstanding minor differences in clinically inactive components. For insulin and its complex quaternary structures, demonstrating structural equivalence is the primary pillar of biosimilarity assessment. This technical guide details the core analytical methodologies employed to prove that a biosimilar insulin's structural architecture matches that of its reference product, ensuring identical primary, secondary, tertiary, and quaternary states that dictate pharmacological activity and safety.
Hierarchical Structure of Insulin
Insulin's biological function is intrinsically linked to its self-association states. The monomer is the active, receptor-binding form. Under physiological conditions, insulin reversibly associates into dimers and, in the presence of zinc, into hexamers—the stable storage form. Any alteration in this dynamic equilibrium due to structural variances can impact pharmacokinetics, stability, and immunogenicity. Therefore, biosimilar assessment must interrogate each level of this architectural hierarchy.
Table 1: Key Structural Attributes of Insulin States
| Structural Level | Description | Critical Analytical Method |
|---|---|---|
| Primary Structure | Amino acid sequence (51 amino acids; A and B chains). | Peptide Mapping, Mass Spectrometry |
| Secondary Structure | Local folding (α-helices, β-sheets, turns). Insulin monomer contains three α-helices. | Circular Dichroism (Far-UV), FTIR |
| Tertiary Structure | 3D folding of a single chain; disulfide bond network (A6-A11, A7-B7, A20-B19). | X-ray Crystallography, NMR, Disulfide Bond Mapping |
| Quaternary Structure | Association states (Monomer Dimer Zinc-bound Hexamer). | Analytical Ultracentrifugation (AUC), Size-Exclusion Chromatography with Multi-Angle Light Scattering (SEC-MALS) |
Core Analytical Methodologies for Structural Equivalence
Primary Structure Analysis
Experimental Protocol: Peptide Mapping with LC-MS/MS
- Objective: Confirm identical amino acid sequence and verify post-translational modifications (e.g., deamidation).
- Procedure:
- Denaturation & Reduction: Incubate reference and biosimilar insulin samples (~100 µg) in 6 M guanidine HCl, 10 mM DTT, pH 8.0, at 37°C for 1 hour.
- Alkylation: Add iodoacetamide to a final concentration of 20 mM. Incubate in the dark at 25°C for 30 minutes.
- Digestion: Desalt samples. Digest with trypsin (enzyme-to-protein ratio 1:50) in 50 mM ammonium bicarbonate, pH 7.8, at 37°C for 4 hours.
- LC-MS/MS Analysis: Separate peptides using reversed-phase C18 nano-LC coupled to a high-resolution tandem mass spectrometer.
- Data Analysis: Compare the total ion chromatograms and MS/MS spectra. Use software to confirm sequence coverage >95% and match retention times and fragmentation patterns for all peptides.
Higher-Order Structure Analysis
Experimental Protocol: Circular Dichroism (CD) Spectroscopy
- Objective: Compare secondary and tertiary structure in solution.
- Procedure:
- Sample Preparation: Prepare reference and biosimilar insulin in the same buffer (e.g., 10 mM phosphate, pH 7.4) at a concentration of 0.2 mg/mL. Filter through 0.22 µm membrane.
- Far-UV CD Scan: Use a 0.1 cm pathlength quartz cuvette. Scan from 260 nm to 190 nm at 20 nm/min, 1 nm bandwidth, 4-second response time. Perform 3 accumulations. Subtract buffer baseline.
- Near-UV CD Scan: Use a 1.0 cm pathlength cuvette. Scan from 320 nm to 250 nm with insulin at 0.5-1.0 mg/mL. This probes tertiary structure via aromatic amino acid environment.
- Data Analysis: Calculate mean residue ellipticity. Overlay spectra for reference and biosimilar. Use statistical similarity tests (e.g., wavelength-by-wavelength equivalence testing).
Quaternary Structure and Aggregation Analysis
Experimental Protocol: Analytical Ultracentrifugation (Sedimentation Velocity)
- Objective: Quantitatively determine the distribution of monomers, dimers, hexamers, and higher-order aggregates under formulated conditions.
- Procedure:
- Sample & Buffer Preparation: Dialyze both insulin products extensively against the desired formulation buffer (e.g., zinc-containing formulation buffer). Use dialysate as the reference buffer.
- Loading: Load ~400 µL of sample and reference buffer into a double-sector centerpiece. Use protein concentrations of 0.5 and 1.0 mg/mL to assess concentration-dependent association.
- Centrifugation: Run in an ultracentrifuge with an optical detection system (absorbance at 280 nm) at 50,000 rpm, 20°C.
- Data Analysis: Use software like SEDFIT to model the continuous sedimentation coefficient distribution [c(s)]. Identify peaks corresponding to monomer (~2 S), dimer (~3 S), and hexamer (~5 S).
Table 2: Example AUC Data for Insulin Biosimilarity Assessment
| Sample | % Monomer | % Dimer | % Hexamer | % High-MW Aggregates | Weight-Average Sedimentation Coefficient (sw,20) |
|---|---|---|---|---|---|
| Reference Product | 15.2 ± 1.1 | 24.8 ± 1.5 | 59.5 ± 2.0 | 0.5 ± 0.1 | 4.21 ± 0.05 |
| Proposed Biosimilar | 16.0 ± 0.9 | 25.1 ± 1.3 | 58.4 ± 1.8 | 0.5 ± 0.2 | 4.18 ± 0.04 |
Workflow for Comprehensive Structural Assessment
Diagram Title: Comprehensive Insulin Structural Biosimilarity Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Insulin Structural Analysis
| Reagent / Material | Function in Biosimilarity Assessment |
|---|---|
| Reference Insulin Product | The approved biological product used as the benchmark for all comparative structural analyses. Critical for side-by-side testing. |
| High-Purity Trypsin/Lys-C | Protease for enzymatic digestion in peptide mapping. Must be sequencing grade to ensure specific cleavage and avoid autolysis. |
| MS-Grade Solvents (ACN, FA) | Acetonitrile and formic acid for LC-MS mobile phases. High purity is essential for sensitivity and reproducibility in mass spectrometry. |
| CD Spectroscopy Buffer Salts | Ultrapure phosphate or other buffer salts free from UV-absorbing impurities, crucial for obtaining accurate CD spectra in the far-UV region. |
| AUC Cell Assemblies | Charcoal-filled Epon double-sector centerpieces and quartz windows for sedimentation velocity experiments. Requires precise manufacturing for leak-free runs. |
| SEC-MALS Columns | High-resolution size-exclusion chromatography columns (e.g., silica-based) calibrated for separating proteins in the 1-100 kDa range, compatible with MALS detection. |
| Stability-Indicating Assay Buffers | Buffers for forced degradation studies (e.g., oxidative, thermal stress) to compare degradation profiles of reference and biosimilar. |
Demonstrating structural equivalence in insulin biosimilars requires a rigorous, multi-parametric analytical approach that deconstructs and compares the molecule at every architectural level—from its linear amino acid sequence to its dynamic quaternary hexameric assembly. The integration of orthogonal techniques like mass spectrometry, circular dichroism, and analytical ultracentrifugation provides a holistic comparison that forms the cornerstone of the "totality of evidence" required for biosimilar approval. In the context of insulin monomer-dimer-hexamer architecture research, these assessments confirm that the biosimilar shares not just the blueprint but the identical three-dimensional construction and dynamic behavior of the reference product, ensuring equivalent safety and efficacy.
The functional and storage forms of insulin—monomers, dimers, and hexamers—are governed by non-covalent interactions at specific surfaces. This architecture is not merely a structural curiosity but a fundamental determinant of pharmacokinetics and pharmacodynamics. Traditional insulin engineering has focused on modulating these self-association properties through point mutations. The next-generation frontier moves beyond this paradigm by designing fundamentally new polypeptide architectures: Single-Chain Insulins (SCIs) and Covalent Insulin Dimers (CIDs). These constructs decouple self-assembly from receptor binding via covalent linkages, offering unprecedented control over oligomeric state and dynamic behavior. This whitepaper provides a technical evaluation of these novel constructs within the established thesis of insulin oligomer research.
Architectural Principles and Design
The Canonical Oligomerization Landscape
Insulin's oligomerization is a concentration-dependent equilibrium:
- Monomer: The biologically active form that binds the insulin receptor (IR).
- Dimer: Forms via anti-parallel β-sheet hydrogen bonding between monomers (mainly B24-B26 residues).
- Hexamer: A trimer of dimers, stabilized by Zn²⁺ ions and conformational changes (T6 <-> R6 transition).
Novel Constructs: A Covalent Override
Single-Chain Insulins (SCIs): The A- and B-chains are connected by a synthetic linker peptide (typically 35-40 Å in length), replacing the native disulfide bonds. This enforces a permanent monomeric state. Covalent Insulin Dimers (CIDs): Two insulin monomers are linked covalently, typically via disulfide bridges or peptide linkers at designed positions (e.g., B29-B29'), creating a permanent, non-dissociating dimer.
Diagram 1: Insulin Construct Architectural Evolution
Quantitative Comparative Analysis
Table 1: Biophysical & Functional Properties of Novel vs. Native Constructs
| Property | Native Human Insulin | Single-Chain Insulin (SCI) | Covalent Dimer (B29-B29' CID) | Measurement Method |
|---|---|---|---|---|
| Molecular Weight (kDa) | 5.8 | ~6.1 (varies by linker) | ~11.6 | Mass Spectrometry |
| Oligomeric State | MonomerDimerHexamer | Monomer (enforced) | Dimer (enforced) | Analytical Ultracentrifugation (AUC) |
| Receptor Binding (IR-A) Relative Potency | 100% | 80-120% | 50-80% per monomer | Surface Plasmon Resonance (SPR) |
| EC₅₀ for Akt Phosphorylation | 1.0 nM (reference) | 0.8 - 1.5 nM | 2.0 - 4.0 nM | Cell-Based ELISA (pAkt) |
| Plasma Half-Life (in murine model) | ~5 min | ~15-25 min | ~35-60 min | Radiolabeled Pharmacokinetics |
| Stability (Aggregation Onset) | High (hexamer stabilizes) | Moderate; linker-dependent | Very High; resists fibrillation | Turbidity at 37°C (A350 nm) |
Table 2: Key Experimental Protocols for Characterization
| Protocol | Objective | Detailed Methodology Summary |
|---|---|---|
| Forced Degradation Stability Assay | Compare fibrillation resistance. | 1. Prepare 1 mg/mL solutions in pH 7.4 buffer. 2. Agitate continuously at 37°C in quartz cuvettes. 3. Monitor turbidity by absorbance at 350 nm every hour for 72h. 4. Determine time to reach an absorbance of 0.1. |
| Surface Plasmon Resonance (SPR) Kinetics | Measure IR binding affinity (KD). | 1. Immobilize recombinant IR ectodomain on CMS chip via amine coupling. 2. Use HBS-EP+ as running buffer. 3. Inject insulin constructs (0.1-100 nM) for 180s association, then dissociate for 600s. 4. Fit sensorgrams to a 1:1 Langmuir binding model. |
| Pharmacokinetic (PK) Profile in Rodents | Determine in vivo clearance rates. | 1. Administer a 0.5 U/kg IV bolus to fasted, conscious mice (n=6/group). 2. Collect serial blood samples via tail vein at 2, 5, 10, 20, 30, 45, 60, 90 min. 3. Measure serum insulin concentration using a specific ELISA (cross-reactivity validated). 4. Fit data to a two-compartment model. |
| Analytical Ultracentrifugation (AUC) | Confirm oligomeric state. | 1. Dialyze samples into PBS, pH 7.4. 2. Load into dual-sector cells and equilibrate at 20°C in an XL-A/I centrifuge. 3. Run at 50,000 rpm, scanning absorbance at 280 nm. 4. Analyze sedimentation velocity data using the c(s) distribution model in SEDFIT. |
Signaling Pathway Implications
The covalent linkage in CIDs creates a bivalent ligand, potentially enabling novel receptor engagement modes (e.g., cross-linking two IR subunits). SCIs, as pure monomers, may exhibit altered endocytic trafficking.
Diagram 2: Proposed Receptor Engagement & Signaling Modes
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Construct Evaluation
| Reagent / Material | Supplier Examples | Critical Function in Research |
|---|---|---|
| Recombinant Insulin Receptor Ectodomain | Sino Biological, R&D Systems | Essential for in vitro binding studies (SPR, ITC) to determine affinity independent of cellular context. |
| Phospho-Akt (Ser473) ELISA Kit | Cell Signaling Technology, Abcam | Quantifies canonical insulin signaling pathway activation in cell-based experiments. |
| Human Insulin-Specific ELISA | Mercodia, Alpco | Measures pharmacokinetic profiles without cross-reactivity to endogenous rodent insulin or C-peptide. |
| Stable CHO-K1 Cell Line Overexpressing Human IR-A | ATCC, generated in-house | Provides a consistent cellular model for potency (EC₅₀) and signaling studies. |
| HPSEC Columns (e.g., TSKgel G2000SWxl) | Tosoh Bioscience | Assesses aggregation state and purity of constructs under native conditions. |
| Reference Standard: Human Insulin | USP, NIBSC | Provides the essential benchmark for all comparative biophysical and biological assays. |
Synthesis and Future Directions
The covalent engineering of insulin's oligomeric architecture represents a paradigm shift. SCIs offer rapid-onset profiles due to the elimination of the dissociation lag from hexamers, while CIDs promise ultra-long action through decreased renal clearance and potential Fc fusion compatibility. Future research must address:
- Linker Optimization: Systematic exploration of linker composition, length, and flexibility on SCI folding and CID geometry.
- Structural Validation: High-resolution cryo-EM structures of CID-bound insulin receptors to confirm engagement modes.
- In Vivo Efficacy: Long-term toxicology and glucodynamic studies in diabetic large animal models.
These novel constructs are not mere analogues but are fundamentally new molecular entities that test and expand the core thesis of insulin oligomer architecture, paving the way for a next-generation therapeutic arsenal.
The therapeutic utility of insulin and its analogs is governed by the critical balance between glycemic efficacy and safety, with mitogenic potential being a primary concern. This balance is quantified by the therapeutic index (TI). The intrinsic mitogenic signaling and receptor specificity of insulin are inextricably linked to its structural dynamics, which are rooted in the equilibrium between monomers, dimers, and hexamers. Insulin must dissociate from its stable hexameric formulation state into dimers and, ultimately, monomers to activate the insulin receptor (IR). This dissociation pathway, a core focus of modern "Architecture of insulin monomers, dimers, and hexamers" research, provides the structural handle for engineering analogs with optimized pharmacokinetics. However, modifications that alter this equilibrium or directly affect receptor binding interfaces can inadvertently increase affinity for the Insulin-like Growth Factor-1 Receptor (IGF-1R), a key driver of cell proliferation. This whitepaper details how specific structural modulations impact receptor specificity and mitogenicity, thereby defining the therapeutic index.
Structural Modulations and Their Biochemical Consequences
The following table summarizes key structural modifications, their targets within the insulin oligomer architecture, and their primary biochemical effects.
Table 1: Structural Modifications in Insulin Analogs and Their Effects
| Modification (Example Analog) | Target Oligomeric State | Primary Structural Effect | IR Affinity (Relative to Human Insulin) | IGF-1R Affinity (Relative to Human Insulin) | Mitogenic Potential |
|---|---|---|---|---|---|
| B28 Pro → Asp (Insulin Lispro) | Dimer/Hexamer | Destabilizes hexamer, accelerates dissociation to monomer. | ~1x | ~1x | Low (comparable to HI) |
| B31 Arg, B32 Arg → Lys, Pro (Insulin Glulisine) | Dimer/Hexamer | Electrostatic repulsion reduces dimer stability. | ~1x | ~0.3x | Low |
| A21 Asn → Gly, B31 Arg, B32 Arg → Arg, Lys (Insulin Degludec) | Multi-hexamer (after injection) | Promotes multi-hexamer formation via fatty acid side chain, creating a soluble depot. | ~0.7x | ~0.01x | Very Low |
| B28 Pro → Lys, B29 Lys → Pro (Insulin Aspart) | Dimer/Hexamer | Similar to Lispro, reduces hexamer stability. | ~0.9x | ~1x | Low |
| B10 His → Asp (Historical X10) | Monomer/Dimer | Increases monomer stability; alters receptor interface. | ~2.5x | ~8x | High (Withdrawn) |
| DesB30 (Insulin Detemir) | Hexamer/Albumin Binding | Fatty acid acylation promotes albumin binding and hexamer stability. | ~0.2x | ~0.1x | Very Low |
Key Experimental Protocols for Assessing Mitogenicity & Specificity
3.1. Receptor Binding Affinity Assay (Radioligand Displacement)
- Objective: Quantify the relative affinity of an insulin analog for the IR-A/IR-B and IGF-1R.
- Protocol:
- Cell Preparation: Use cell lines overexpressing human IR (e.g., CHO-IR) or IGF-1R (e.g., MCF-7).
- Membrane Preparation: Harvest cells, lyse, and isolate crude plasma membrane fractions via differential centrifugation.
- Binding Reaction: Incubate membrane preparations (25-50 µg protein) with a fixed concentration of radioiodinated ([¹²⁵I]) insulin or IGF-1 in increasing concentrations of unlabeled test analog (10⁻¹¹ to 10⁻⁶ M) in binding buffer (e.g., HEPES, pH 7.8, with BSA).
- Separation & Measurement: After equilibrium (overnight, 4°C), separate bound from free radioligand by rapid filtration through GF/C filters. Wash filters and measure bound radioactivity via gamma counter.
- Data Analysis: Calculate IC₅₀ values. The ratio of IC₅₀(Insulin)/IC₅₀(Analog) for IR and IGF-1R yields relative affinity. The IGF-1R:IR affinity ratio is a critical safety indicator.
3.2. Cell Proliferation (Mitogenicity) Assay
- Objective: Measure the direct mitogenic potency of analogs via DNA synthesis.
- Protocol:
- Cell Culture: Use IGF-1R-responsive cell lines (e.g., MCF-7 breast cancer cells or R- fibroblasts).
- Serum Starvation: Plate cells and starve in serum-free medium for 24 hours to synchronize in G₀/G₁ phase.
- Stimulation: Treat cells with a concentration range (0.1 nM - 1 µM) of human insulin, IGF-1, or test analog for 18-24 hours.
- Proliferation Measurement: Add bromodeoxyuridine (BrdU) for the final 2-4 hours. Fix cells and detect incorporated BrdU using an anti-BrdU antibody conjugated with a colorimetric or fluorometric readout.
- Analysis: Determine EC₅₀ values for stimulation. A lower EC₅₀ and a higher maximal response relative to insulin indicate increased mitogenic potency.
3.3. Receptor Autophosphorylation & Downstream Signaling
- Objective: Profile the potency and temporal dynamics of receptor activation and key pathway engagement.
- Protocol:
- Stimulation: Serum-starve IR/IGF-1R-expressing cells (e.g., L6 myoblasts). Stimulate with ligands for defined times (e.g., 0, 5, 10, 30 min).
- Cell Lysis: Lyse cells in RIPA buffer containing protease and phosphatase inhibitors.
- Immunoprecipitation/Western Blot: For receptor phosphorylation, immunoprecipitate the IR or IGF-1R, then perform SDS-PAGE and Western blot with anti-phosphotyrosine (pTyr) antibodies. For downstream effectors (e.g., Akt, MAPK), analyze total cell lysates directly.
- Detection: Use phospho-specific antibodies (e.g., pAkt-Ser473, pERK1/2) to assess pathway activation. Normalize to total protein levels.
- Analysis: Compare the intensity, duration, and bias (Akt vs. ERK pathway) of signaling induced by analogs versus native insulin.
Visualization of Key Signaling Pathways & Experimental Workflow
(Diagram 1: Insulin/IGF-1 Receptor Cross-Activation and Signaling)
(Diagram 2: Key Experimental Assessment Workflow)
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents for Insulin Mitogenicity & Specificity Research
| Item / Reagent | Function & Purpose in Research |
|---|---|
| Recombinant Human Insulin Analogs | Test articles for binding, signaling, and proliferation studies. Must be highly purified and characterized. |
| [¹²⁵I]-Labeled Insulin & IGF-1 | Tracers for quantitative radioligand binding displacement assays to determine receptor affinity. |
| Cell Lines: CHO-IR, L6 (IR-high); MCF-7, R- (IGF-1R-high) | Engineered or selected cell systems for isolating IR- vs. IGF-1R-specific effects. |
| Phospho-Specific Antibodies (anti-pTyr, pIR-β, pIGF-1R-β, pAkt-Ser473, pERK1/2) | Essential tools for Western blot analysis to quantify and compare pathway activation potency and bias. |
| BrdU Cell Proliferation ELISA Kit | Standardized assay to measure DNA synthesis as a direct readout of mitogenic potency. |
| IR & IGF-1R Extracellular Domain (ECD) Proteins | For surface plasmon resonance (SPR) or ELISA-based kinetic binding studies without cellular complexity. |
| Insulin Hexamer-Stabilizing Agents (Phenol, Cresol, Zn²⁺) | To study the formulation-to-monomer dissociation kinetics critical to pharmacokinetics. |
| Molecular Modelling & Dynamics Software (e.g., Schrödinger Suite, GROMACS) | To predict the structural impact of amino acid substitutions on oligomer stability and receptor docking. |
The development of glucose-responsive "smart" insulins represents a paradigm shift in diabetes therapy, aiming to mimic the dynamic secretory function of pancreatic β-cells. This pursuit is fundamentally rooted in the structural architecture of insulin—its monomeric, dimeric, and hexameric states. The hexamer, stabilized by zinc ions and phenolic excipients, serves as a crucial depot form in contemporary formulations. Smart insulin strategies exploit this inherent structural plasticity, engineering molecular systems where insulin bioavailability is modulated by the glucose concentration. This whitepaper examines these future directions through a structural lens, detailing experimental approaches and the requisite toolkit for advancing this transformative field.
Structural Foundations: Insulin Quaternary Dynamics
The pharmacodynamic profile of any insulin formulation is dictated by its dissociation kinetics from oligomeric states into the active monomer. This dissociation is governed by key structural elements:
- Monomer: The bioactive form, characterized by the receptor-binding surface involving the A-chain N-terminus, A8-A10, B1-B3, and B22-B30 residues.
- Dimer Interface: Primarily mediated by antiparallel β-sheet hydrogen bonding between B24-B28 strands.
- Hexamer Assembly: A zinc-coordinated trimer of dimers, with coordination spheres involving His(B10). The allosteric binding sites for phenolic derivatives (e.g., phenol, m-cresol) at the dimer-dimer interface further stabilize this state.
The design of glucose-responsive insulins requires precise manipulation of these equilibrium constants (Kdimer, Khexamer) in a glucose-dependent manner.
Table 1: Quantitative Parameters of Insulin Oligomeric States
| Oligomeric State | Key Stabilizing Interactions | Approximate Kd for Dissociation | Functional Role |
|---|---|---|---|
| Hexamer | Zn2+ coordination, phenolic ligand binding, dimer-dimer hydrophobic contacts | ~10-9 to 10-12 M (for Zn2+) | Depot form in subcutis; slow dissociation. |
| Dimer | Anti-parallel β-sheet (B24-B28), side-chain hydrophobic interactions (B12, B16) | ~10-6 M | Intermediate; dominant in dilution prior to monomer formation. |
| Monomer | Intramolecular disulfide bonds, native folding. | N/A | Bioactive form binding Insulin Receptor (IR). |
Strategic Frameworks for Smart Insulin Design
Current research focuses on three primary structural-architectural strategies:
- Molecular Conjugation (Glucose-Binding Moieties): Insulin is conjugated via cleavable linkers to glucose-binding proteins (e.g., Concanavalin A) or synthetic ligands (e.g., phenylboronic acid, PBA). Glucose competition triggers insulin release.
- Competitive Displacement Systems: Insulin is non-covalently complexed within a glucose-binding polymer hydrogel (e.g., PBA-containing polymer). Glucose influx swells or dissolves the matrix, releasing insulin via competitive binding.
- Allosteric Switching Proteins: De novo engineered proteins or insulins modified with glucose-sensitive domains undergo glucose-induced conformational changes that modulate receptor affinity or oligomerization state.
Key Experimental Protocols
Protocol 1: Assessing Glucose-Dependent Dissociation Kinetics via Analytical Ultracentrifugation (AUC)
Objective: Quantify the shift in oligomeric state distribution of a smart insulin candidate in response to varying glucose concentrations. Methodology:
- Prepare samples of the candidate smart insulin (e.g., PBA-insulin conjugate) at 0.1 mg/mL in phosphate buffer (pH 7.4) with 0, 5, 10, and 20 mM D-glucose. Include 0.02% sodium azide.
- Load samples into dual-sector charcoal-filled Epon centerpieces and assemble cells with quartz windows.
- Equilibrate in an XL-A/XL-I analytical ultracentrifuge at 20°C.
- Perform sedimentation velocity experiments at 50,000 rpm, monitoring absorbance at 280 nm.
- Analyze data using continuous c(s) distribution models in SEDFIT to determine the sedimentation coefficients (S-values) for monomeric, dimeric, and hexameric species.
- Plot the relative concentration of monomeric insulin against glucose concentration to generate a response curve.
Protocol 2: In Vitro Activity Profiling using Adipocyte Glucose Uptake Assay
Objective: Measure the glucose-dependent bioactivity of smart insulin candidates. Methodology:
- Differentiate 3T3-L1 murine fibroblasts into adipocytes over 10-14 days.
- Serum-starve differentiated adipocytes for 4 hours in low-glucose (5.5 mM) DMEM.
- Incubate cells for 20 minutes in Krebs-Ringer HEPES buffer containing 0, 10, or 100 nM smart insulin candidate, across a range of glucose concentrations (0, 5.6, 11.1, 16.7 mM).
- Add 2-deoxy-D-[1,2-3H]glucose (0.5 µCi/well) for 10 minutes.
- Terminate uptake by washing with ice-cold PBS containing 10 µM cytochalasin B.
- Lyse cells with 0.1% SDS and measure incorporated radioactivity via scintillation counting.
- Normalize data to basal (no insulin) uptake at each glucose level to calculate fold-stimulation.
Visualizing Key Mechanisms and Workflows
Diagram Title: Smart Insulin Release & Dissociation Pathways (89 chars)
Diagram Title: Key Experimental Validation Workflow (61 chars)
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Research Reagent Solutions for Smart Insulin Development
| Item | Function & Application |
|---|---|
| Recombinant Human Insulin (Monomer Standard) | Gold-standard control for structural (AUC, NMR) and activity (IR binding, cell assays) studies. |
| ZnCl2 & m-Cresol | Formulation excipients to stabilize the insulin hexamer; controls for dissociation kinetics experiments. |
| Phenylboronic Acid (PBA) Derivatives (e.g., 3-Fluoro-4-carboxy-PBA) | Key synthetic moiety for constructing glucose-sensitive linkers and polymer matrices. |
| Concanavalin A (Con A) Tetramer | Plant lectin serving as a classic glucose-binding protein for competitive displacement systems. |
| Photo-Crosslinkable Polymers (e.g., PEG-Diacrylate with PBA side chains) | For fabricating glucose-responsive hydrogel depots for sustained, stimulus-driven release studies. |
| Differentiated 3T3-L1 Adipocytes | Standard cell line for in vitro evaluation of insulin-stimulated glucose uptake. |
| STZ-Induced Diabetic Rodent Model | Animal model for in vivo pharmacokinetic/pharmacodynamic (PK/PD) profiling of smart insulin candidates. |
| Sensitive Glucose Oxidase Assay Kit | For precise, high-throughput measurement of glucose concentrations in cell media and serum samples. |
The path to clinically viable glucose-responsive insulins necessitates a deep integration of structural biology with materials science and pharmacokinetics. Success hinges on engineering molecules or systems where the architectural principles of insulin assembly are reversibly governed by physiological glucose signals. Future research must focus on optimizing response kinetics, biocompatibility, and scalable manufacture, all while maintaining the intrinsic structural fidelity required for receptor engagement. The continued elucidation of insulin's oligomerization dynamics remains the foundational blueprint for this next generation of autonomous diabetes therapeutics.
Conclusion
The intricate architecture of insulin monomers, dimers, and hexamers is not merely an academic curiosity but the central framework for rational therapeutic design. From foundational biophysics to troubleshooting aggregation, each structural state dictates critical pharmacological properties. The comparative validation of modern analogs underscores how targeted disruptions or stabilizations of self-assembly directly translate to clinical benefits. Future research, leveraging advanced structural biology and computational modeling, must focus on further refining this blueprint to develop insulins with unprecedented precision, responsiveness, and safety profiles, ultimately moving closer to a physiological cure for diabetes management.