Insulin, Glucagon, and Beyond: Molecular Mechanisms and Therapeutic Innovations in Blood Glucose Regulation
This article provides a comprehensive analysis of the hormonal regulation of blood glucose, synthesizing foundational physiology with cutting-edge research and therapeutic applications.
Insulin, Glucagon, and Beyond: Molecular Mechanisms and Therapeutic Innovations in Blood Glucose Regulation
Abstract
This article provides a comprehensive analysis of the hormonal regulation of blood glucose, synthesizing foundational physiology with cutting-edge research and therapeutic applications. Tailored for researchers, scientists, and drug development professionals, it explores the intricate balance between insulin and glucagon, delving into molecular signaling pathways, secretory mechanisms, and the emerging role of α-cell plasticity. It further evaluates state-of-the-art methodological approaches for hormone and biomarker analysis, examines pathophysiological disruptions in diabetes, and critically assesses current and emerging therapeutic strategies, including dual and triple agonists. The review aims to bridge foundational knowledge with translational innovation, offering a roadmap for future diabetes and metabolic disease research.
The Core Duet: Foundational Physiology of Insulin and Glucagon in Glucose Homeostasis
The pancreatic islets of Langerhans represent a complex endocrine micro-organ essential for systemic metabolic homeostasis, primarily through the regulated secretion of glucagon and insulin [1] [2]. These two counter-regulatory hormones are produced in close proximity by alpha (α) and beta (β) cells, respectively, enabling a sophisticated feedback system that maintains blood glucose concentrations within a narrow physiological range [3] [1]. Disruption of this delicate equilibrium is a hallmark of diabetes mellitus, a group of metabolic diseases affecting hundreds of millions worldwide [2]. While traditional pathophysiological models of diabetes have predominantly focused on insulin deficiency and resistance, emerging research underscores the critical role of alpha cell dysfunction and inappropriate glucagon secretion in disease pathogenesis [4] [5]. This whitepaper synthesizes current knowledge of the cellular origins, secretory triggers, and functional interplay between pancreatic alpha and beta cells, providing a technical foundation for researchers and drug development professionals working within the framework of hormonal blood glucose regulation.
Cellular Origins and Islet Architecture
The pancreatic islets contain multiple endocrine cell types strategically organized to facilitate metabolic regulation [2]. Beta cells, which produce insulin, constitute the majority (approximately 60-80%) of the islet cell population and are predominantly located at the core of human islets [2]. Alpha cells, which produce glucagon, account for approximately 30-40% of the islet population and typically form a mantle surrounding the beta cell core in rodent islets, though this architecture shows species-specific variations [1] [2]. Other endocrine cell types include delta (δ) cells that produce somatostatin, epsilon (ε) cells that produce ghrelin, and PP cells that produce pancreatic polypeptide, each playing modulatory roles in islet function [2].
This spatial arrangement is crucial for the paracrine interactions that fine-tune hormone secretion [1] [2]. The close proximity allows secretory products from one cell type to directly influence the function of neighboring cells, creating a robust regulatory network that enables precise response to metabolic demands [1].
Beta Cell Function: Insulin Synthesis and Secretion
Insulin Structure and Biosynthesis
Insulin is synthesized as preproinsulin and processed to proinsulin through cleavage of the signal peptide [6]. Proinsulin is then converted to insulin and C-peptide via proteolytic cleavage and stored in secretory granules awaiting release [6]. The crystal structure of insulin reveals a complex organization where the active monomer consists of a 21-amino acid A-chain and a 30-amino acid B-chain linked by two disulfide bonds [6]. Insulin stored in β-cells is packed into densely clustered granules as insoluble crystalline hexamers coordinated with zinc atoms, reaching concentrations of approximately 40 mM [6]. The hexamer serves as the storage form, while the monomer is the active form that dissociates upon secretion into the bloodstream [6].
Table 1: Key Structural Features of Insulin
| Structural Component | Characteristics | Functional Significance |
|---|---|---|
| Primary Structure | 51 amino acids; A-chain (21 aa) and B-chain (30 aa) | Determines receptor binding affinity |
| Disulfide Linkages | Two interchain (A7-B7, A20-B19); one intrachain (A7-A11) | Stabilizes tertiary structure |
| Storage Form | Zinc-coordinated hexamer (≈40 mM concentration in granules) | Stable packaging within secretory granules |
| Active Form | Monomer (dissociates upon secretion) | Binds insulin receptor |
| Critical Binding Regions | N-terminus of A-chain, C-terminus of both chains | Mutation causes reduced receptor affinity (e.g., insulin Wakayama, Chicago) |
Glucose-Stimulated Insulin Secretion (GSIS)
Glucose-stimulated insulin secretion involves a sequence of events in β-cells that lead to fusion of secretory granules with the plasma membrane [6]. The process occurs through two complementary pathways: the triggering pathway and the metabolic amplifying pathway [1] [2].
The triggering pathway begins with glucose uptake into β-cells through glucose transporters (GLUT1 and GLUT3 in humans; GLUT2 in rodents) [1] [2]. Following uptake, glucose is phosphorylated by glucokinase, which serves as the rate-limiting step for glucose entry into the glycolytic pathway [2]. Subsequent glucose metabolism through glycolysis and the tricarboxylic acid (TCA) cycle generates ATP, increasing the ATP/ADP ratio [1] [2]. This elevated ATP/ADP ratio causes closure of ATP-sensitive potassium (KATP) channels, leading to membrane depolarization [2]. Subsequently, voltage-gated calcium channels open, allowing influx of extracellular Ca2+ [1] [2]. The resulting sharp increase in intracellular Ca2+ concentration ([Ca2+]i) triggers the exocytosis of insulin secretory granules [1] [2].
The metabolic amplifying pathway operates in parallel to enhance insulin secretion independently of further KATP channel activity, primarily through mechanisms that facilitate the recruitment and priming of insulin granules for release [2]. Mitochondria play a crucial role in this process by serving as metabolic and redox centers, establishing connections with plasma membrane channels, insulin granule vesicles, and cellular redox balance [2]. Additionally, metabolic signals such as NADPH production contribute to the amplification of insulin secretion [2].
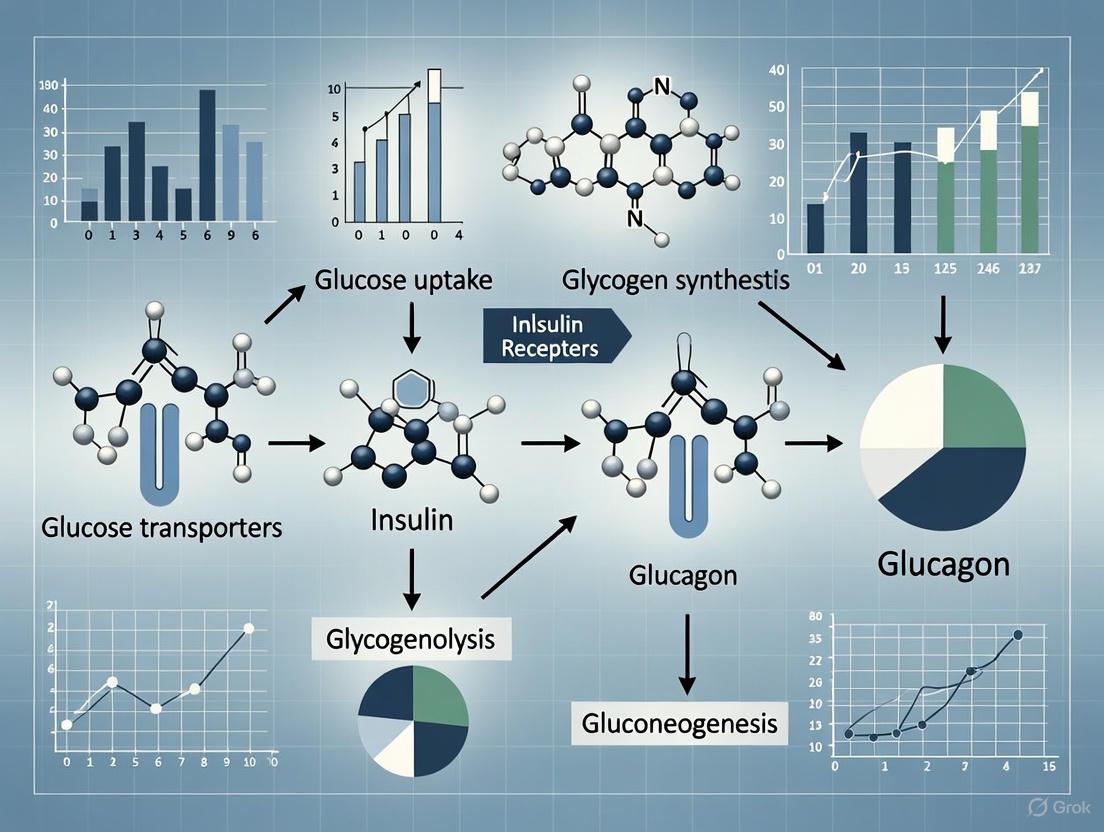
Diagram 1: Beta Cell Glucose-Stimulated Insulin Secretion Pathway. This diagram illustrates the key steps in the triggering pathway of GSIS, from glucose uptake to calcium-triggered exocytosis of insulin granules.
Additional Regulators of Insulin Secretion
Beyond glucose, various nutrients, hormones, and neural inputs modulate insulin secretion. Free fatty acids and amino acids can augment glucose-induced insulin secretion [6]. Hormonal regulators include melatonin, estrogen, leptin, growth hormone, and glucagon-like peptide-1 (GLP-1) [6]. The cAMP/protein kinase A (PKA)/exchange protein directly activated by cAMP (EPAC) system serves as a critical signaling hub for many hormonal modulators [1] [6]. When activated by stimuli such as GLP-1 or glucagon receptor engagement, cAMP signaling potentiates GSIS without triggering insulin secretion independently [1].
Recent research has identified additional regulatory mechanisms that constrain insulin secretion to prevent excessive release. The nutrient sensor mTORC1 is rapidly activated by glucose in β-cells and acts as an intrinsic feedback regulator that restrains insulin secretion via RhoA-dependent actin remodeling, limiting vesicle movement and dampening the second phase of insulin secretion [7].
Alpha Cell Function: Glucagon Synthesis and Secretion
Glucagon Biosynthesis and Structure
Glucagon is a 29-amino acid peptide hormone derived from the preproglucagon gene (GCG) [1]. In pancreatic alpha cells, proglucagon is processed by prohormone convertase 2 (PC2), resulting in the generation of glucagon and the major proglucagon fragment [1]. This processing differs from that in intestinal L cells, where prohormone convertase PC1/3 generates GLP-1 and other products from the same precursor [1]. The crystal structure of glucagon was solved in the 1950s, following its identification as a pancreatic hormone that elevates blood glucose levels [5].
Regulation of Glucagon Secretion
Glucagon secretion is tightly regulated by nutrients, endocrine factors, and neural inputs [5]. The primary stimulus for glucagon release is low blood glucose concentration, which directly affects alpha cell electrical activity [5]. During hypoglycemia, reduced glucose metabolism decreases the ATP/ADP ratio, promoting the opening of KATP channels and membrane hyperpolarization, which ultimately triggers action potentials and calcium influx that stimulate glucagon exocytosis [5].
Table 2: Primary Regulators of Glucagon Secretion
| Regulatory Factor | Effect on Secretion | Mechanism of Action |
|---|---|---|
| Hypoglycemia | Stimulates | ↓ ATP/ADP ratio; KATP channel opening; Ca2+ influx |
| Amino Acids | Stimulates | Direct nutrient signaling; cAMP elevation |
| Somatostatin | Inhibits | SSTR2 activation; ↓ cAMP & Ca2+ levels |
| Insulin | Inhibits | PI3K-Akt pathway; inhibition of exocytosis |
| GABA | Inhibits | GABAA receptor activation; membrane hyperpolarization |
| Zn2+ | Inhibits | KATP channel modulation; membrane hyperpolarization |
| Sympathetic Nervous System | Stimulates | β-adrenergic receptor activation; ↑ cAMP |
| GLP-1 | Inhibits | GLP-1 receptor signaling; paracrine/neural pathways |
| GIP | Stimulates | GIP receptor activation; cAMP signaling |
Intracellular cAMP signaling serves as the primary trigger for glucagon secretion, with calcium acting as a secondary messenger [5]. During stress or fasting, sympathetic activation increases cAMP levels, triggering glucagon release through PKA and EPAC activation, which enhances calcium channel activity and vesicle trafficking [5]. Additional GPCR pathways, including Gq-coupled receptors such as the vasopressin 1b receptor (V1bR), activate phospholipase C (PLC) and generate inositol trisphosphate (IP3), leading to increased intracellular calcium and enhanced glucagon release [5].
Paracrine inhibition from neighboring islet cells represents a crucial regulatory layer. Insulin, somatostatin, γ-aminobutyric acid (GABA), and zinc (co-secreted with insulin) all suppress glucagon secretion through distinct mechanisms [5]. Insulin activates its receptor on alpha cells, inhibiting exocytosis through PI3K-Akt-dependent pathways [5]. Somatostatin binds to somatostatin receptor subtype 2 (SSTR2), reducing cAMP and calcium levels [5]. GABA activates GABAA receptors, leading to chloride influx and membrane hyperpolarization, while zinc influences KATP channels to promote hyperpolarization [5]. Disruption of these inhibitory pathways in type 2 diabetes contributes to paradoxical hyperglucagonemia and impaired glycemic control [5].
Diagram 2: Alpha Cell Glucagon Secretion Regulation. This diagram illustrates the complex regulation of glucagon secretion, highlighting cAMP as the primary intracellular trigger and the modulatory role of paracrine inhibition from other islet cells.
Paracrine and Endocrine Crosstalk in Islet Function
Alpha to Beta Cell Communication
Alpha cells significantly influence beta cell function through paracrine signaling. The most well-established paracrine factor is glucagon itself, which binds to glucagon receptors on beta cells and activates the cAMP/PKA/EPAC system, thereby potentiating GSIS [1]. This stimulatory effect was first documented in 1965 and has since been confirmed in multiple model systems [1]. Isolated beta cells exhibit reduced cAMP content and impaired GSIS, both of which are restored by the presence of alpha cells or exogenous glucagon [1]. Interestingly, glucagon can also activate the GLP-1 receptor on beta cells, triggering similar downstream signaling events [1].
Beyond glucagon, alpha cells secrete additional factors that modulate beta cell function. Glutamate, co-released with glucagon, may influence beta cells through NMDA receptors, though its effects appear context-dependent [1]. In humans, alpha cells can produce and release acetylcholine, which functions as a paracrine signal to sensitize beta cells to prevailing glucose concentrations [1]. This acetylcholine activates muscarinic receptors on beta cells, initiating the phospholipase C (PLC)/diacylglycerol (DAG)/protein kinase C (PKC) cascade that enhances GSIS [1].
Beta to Alpha Cell Communication
Beta cells reciprocally regulate alpha cell function through several inhibitory pathways. Insulin itself acts on insulin receptors present on alpha cells to suppress glucagon secretion through PI3K-Akt-dependent pathways [5]. Zinc, co-packaged with insulin in secretory granules and co-secreted upon glucose stimulation, promotes alpha cell hyperpolarization by modulating KATP channels [5]. GABA, synthesized from glutamate by the enzyme glutamic acid decarboxylase in beta cells, activates GABAA receptors on alpha cells, leading to chloride influx and membrane hyperpolarization that inhibits glucagon release [1] [5]. These multifaceted inhibitory mechanisms ensure appropriate suppression of glucagon secretion during hyperglycemia.
Emerging Concepts: Intra-islet GLP-1 and Oxytocin
Recent research has revealed that pancreatic alpha cells can produce and release glucagon-like peptide-1 (GLP-1) under certain conditions, creating an intra-islet incretin system [8]. This intra-islet GLP-1 acts locally to potentiate insulin secretion in a glucose-dependent manner [8]. A newly discovered hormonal pathway links oxytocin to this intra-islet GLP-1 system. Oxytocin stimulates GLP-1 release from pancreatic alpha cells, which subsequently enhances insulin secretion, particularly under high glucose conditions [8]. This indirect action—oxytocin triggering alpha cells to release GLP-1, which then acts on beta cells—represents a novel mechanism for controlling insulin release that is glucose-dependent, making it a potentially safe option for regulating blood sugar [8].
Experimental Methodologies for Islet Cell Research
Key Research Models and Approaches
The study of alpha and beta cell function employs a range of sophisticated experimental models and approaches. Isolated pancreatic islets from various species (particularly rodents and humans) serve as a primary ex vivo model for investigating secretory function and paracrine interactions [1]. These islets can be studied in static incubation systems or more dynamic perifusion assays that provide temporal resolution of hormone secretion [9]. Isolated islets can be further dissociated into individual cells for fluorescence-activated cell sorting (FACS) to obtain purified populations of alpha and beta cells [1].
Genetic mouse models with tissue-specific ablation or overexpression of key genes involved in hormone secretion have been instrumental in delineating signaling pathways in vivo [1] [9]. For instance, mice with beta cell-specific ablation of the GLP-1 receptor revealed that the physiological effects of GLP-1 may involve non-endocrine mechanisms, possibly neuronal relay systems between the intestine and endocrine pancreas [9].
Advanced imaging techniques, including live-cell imaging of intracellular calcium dynamics and vesicle trafficking, provide real-time visualization of stimulus-secretion coupling events [1]. These approaches can be complemented by electrophysiological methods such as patch clamping to characterize ion channel activity and membrane potential changes in response to secretagogues [2].
Assessment of Hormone Secretion and Cell Function
Table 3: Key Methodologies for Assessing Alpha and Beta Cell Function
| Methodology | Application | Key Measured Parameters |
|---|---|---|
| Islet Perifusion | Dynamic hormone secretion | Temporal pattern of insulin/glucagon release; pulsatility |
| Static Insulin/Glucagon Secretion Assay | Batch sampling of hormone output | Total hormone secreted under defined conditions |
| Patch Clamp Electrophysiology | Ion channel function | KATP channel activity; membrane potential; Ca2+ currents |
| Live-cell Calcium Imaging | Intracellular Ca2+ dynamics | [Ca2+]i oscillations; response to secretagogues |
| Immunofluorescence Microscopy | Islet architecture; hormone co-localization | Cellular composition; receptor distribution |
| cAMP FRET Sensors | Real-time cAMP dynamics | Spatiotemporal cAMP signaling in live cells |
| Single-cell RNA sequencing | Transcriptomic profiling | Cell-type specific gene expression; heterogeneity |
For quantitative assessment of hormone secretion, radioimmunoassays (RIA) and enzyme-linked immunosorbent assays (ELISA) remain standard techniques for measuring insulin and glucagon concentrations in experimental samples and clinical specimens [5]. These assays can be applied to both in vitro systems and in vivo during metabolic tests such as the oral glucose tolerance test (OGTT) and intraperitoneal glucose tolerance test (IPGTT) [9].
To investigate intracellular signaling pathways, researchers employ phosphoproteomic profiling to identify phosphorylation changes in proteins involved in processes such as actin remodeling and vesicle trafficking [7]. This approach revealed that mTORC1 modulates the phosphorylation of proteins in the RhoA-GTPase pathway, providing mechanistic insight into how this nutrient sensor constrains insulin exocytosis [7].
Research Reagent Solutions
Table 4: Essential Research Reagents for Islet Cell Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Hormone Receptor Agonists | Exendin-4 (GLP-1R); Glucagon | Receptor activation; cAMP signaling studies |
| Hormone Receptor Antagonists | Exendin(9-39) (GLP-1R) | Receptor blockade; pathway dissection |
| Ion Channel Modulators | Diazoxide (KATP opener); Tolbutamide (KATP closer) | Electrophysiology; GSIS mechanism studies |
| Metabolic Inhibitors | 2-deoxyglucose; Oligomycin | Metabolic pathway dissection |
| Signaling Pathway Inhibitors | Rapamycin (mTORC1); H-89 (PKA) | Specific pathway inhibition; mechanism studies |
| Cell Isolation Enzymes | Collagenase P; Liberase | Islet isolation for ex vivo studies |
| Fluorescent Indicators | Fura-2 (Ca2+); cAMP FRET sensors | Live-cell imaging of second messengers |
Pathophysiological Implications and Therapeutic Perspectives
Dysregulation of alpha and beta cell function is central to diabetes pathogenesis. In type 1 diabetes, autoimmune destruction of beta cells leads to absolute insulin deficiency, while also eliminating the paracrine inhibition of alpha cells, resulting in inappropriate glucagon secretion that exacerbates hyperglycemia [3] [5]. In type 2 diabetes, progressive beta cell dysfunction occurs alongside peripheral insulin resistance, while alpha cells develop resistance to the suppressive effects of insulin and glucose, leading to fasting and postprandial hyperglucagonemia [3] [5].
Therapeutic strategies increasingly target both alpha and beta cell dysfunction. GLP-1 receptor agonists enhance glucose-dependent insulin secretion while suppressing glucagon release, addressing both hormonal defects [10]. Emerging approaches include dual and triple agonists that target multiple related receptors (GLP-1R, GIPR, GCGR) to achieve superior metabolic outcomes [10]. Glucagon receptor antagonists have shown efficacy in lowering blood glucose in diabetic patients, supporting the "glucagonocentric hypothesis" of diabetes [5]. Additionally, research into alpha-to-beta cell conversion offers potential regenerative approaches for restoring functional beta cell mass [4].
The intricate partnership between alpha and beta cells exemplifies the sophistication of metabolic regulation. Continued research into their cellular origins, secretory triggers, and functional interplay will undoubtedly yield novel therapeutic insights for diabetes and related metabolic disorders.
This technical guide provides a comprehensive analysis of the molecular mechanisms underlying insulin and glucagon receptor signaling and their integrated regulation of metabolic homeostasis. We examine the intricate signaling cascades, downstream metabolic effects, and experimental approaches used to investigate these pathways. With the growing therapeutic importance of multi-agonist drugs targeting incretin receptors, this review synthesizes current understanding of receptor crosstalk, pathway integration, and metabolic outcomes relevant to conditions including obesity, type 2 diabetes, and metabolic dysfunction-associated steatotic liver disease. The content is structured to serve researchers, scientists, and drug development professionals working in metabolic disease therapeutics.
The maintenance of systemic glucose homeostasis is primarily governed by the counter-regulatory hormones insulin and glucagon, which orchestrate complex molecular interactions across multiple tissues. These hormones activate specific receptor-mediated signaling pathways that coordinate anabolic and catabolic processes to ensure metabolic stability. Recent research has revealed substantial complexity in these signaling systems, including pathway crosstalk, feedback mechanisms, and opportunities for therapeutic intervention through multi-receptor targeting [11] [10]. The development of glucagon-like peptide-1 (GLP-1) receptor agonists and emerging multi-agonists represents a paradigm shift in metabolic disease treatment, leveraging our growing understanding of these interconnected pathways [10] [12]. This review examines the molecular architecture of insulin and glucagon signaling systems, their integration in metabolic regulation, and the experimental approaches driving discovery in this field.
Insulin Signaling: Molecular Architecture and Metabolic Regulation
Insulin Receptor Activation and Downstream Cascades
Insulin signaling initiates with hormone binding to the transmembrane insulin receptor (IR), triggering receptor autophosphorylation and activation of its intrinsic tyrosine kinase activity. This activation recruits and phosphorylates insulin receptor substrate (IRS) proteins, which serve as docking platforms for downstream signaling components. The primary metabolic pathway involves IRS recruitment of phosphoinositide 3-kinase (PI3K), which generates phosphatidylinositol (3,4,5)-trisphosphate (PIP3) at the membrane, facilitating phosphorylation and activation of AKT (protein kinase B) [13].
Activated AKT serves as a central signaling node, translocating to various cellular compartments to regulate multiple metabolic processes including glucose uptake, glycogen synthesis, and lipid metabolism. AKT phosphorylates and inhibits glycogen synthase kinase 3 (GSK3), relieving inhibition of glycogen synthase and promoting glycogen storage. Simultaneously, AKT activation stimulates translocation of glucose transporter 4 (GLUT4) to the plasma membrane through additional downstream effectors, enhancing cellular glucose uptake [13]. The insulin signaling network exhibits emergent properties including bistability, where the activation threshold for AKT phosphorylation differs from its deactivation threshold, creating a hysteretic response that maintains metabolic state stability despite fluctuating glucose levels [14].
Insulin Signaling Disruption in Metabolic Disease
Insulin resistance represents a state of diminished cellular responsiveness to insulin stimulation, characterized by disruptions at multiple points in the signaling cascade. Molecular mechanisms underlying insulin resistance include serine phosphorylation of IRS proteins that inhibits their function, reduced PI3K/AKT pathway activation, and inflammatory signaling through pathways such as JNK and IKKβ that interfere with insulin signal transduction [13]. These disruptions lead to impaired glucose uptake in peripheral tissues, uncontrolled hepatic glucose production, and aberrant lipid metabolism, collectively contributing to the pathogenesis of type 2 diabetes and related metabolic disorders.
Table 1: Key Components of Insulin Signaling Pathway and Functional Roles
| Signaling Component | Activation Mechanism | Primary Metabolic Functions | Dysregulation Consequences |
|---|---|---|---|
| Insulin Receptor (IR) | Insulin binding, autophosphorylation | Initial signal transduction | Impaired insulin sensitivity |
| IRS proteins | Tyrosine phosphorylation by IR | Scaffold for signaling complex | Serine phosphorylation inhibits function |
| PI3K | Recruitment to IRS | PIP3 generation | Reduced AKT activation |
| AKT | Phosphorylation by PDK1/2 | GLUT4 translocation, glycogen synthesis | Impaired glucose disposal |
| GSK3β | Inhibition by AKT phosphorylation | Regulation of glycogen synthase | Increased glycogen synthase inhibition |
Glucagon Signaling: Mechanisms and Metabolic Effects
Glucagon Receptor Signaling Cascade
Glucagon exerts its effects through binding to the glucagon receptor (GCGR), a class B G protein-coupled receptor primarily expressed in the liver, with lower expression in kidney, adipose tissue, and other organs [11]. GCGR activation stimulates dissociation of heterotrimeric G proteins into Gαs and Gβγ subunits. Gαs activates adenylate cyclase, increasing intracellular cyclic AMP (cAMP) levels, which in turn activates protein kinase A (PKA) [15]. Additionally, glucagon receptor signaling can activate the IP3-AMPK signaling pathway, providing an alternative mechanism for metabolic regulation [15].
Activated PKA phosphorylates numerous downstream targets including transcription factors, enzymes, and other regulatory proteins. In the liver, PKA-mediated phosphorylation activates key enzymes in gluconeogenesis and glycogenolysis while inhibiting glycogen synthase. PKA also phosphorylates cAMP response element-binding protein (CREB), which translocates to the nucleus and activates transcription of gluconeogenic enzymes including phosphoenolpyruvate carboxykinase (PEPCK) and glucose-6-phosphatase (G6Pase) [11]. Recent evidence indicates that glucagon signaling also regulates amino acid metabolism through a liver-pancreatic alpha cell axis, stimulates lipolysis and mitochondrial fat oxidation, reduces caloric intake, and increases energy expenditure, at least in animal models [11].
Emerging Roles of Glucagon in Metabolic Regulation
Beyond its classical hyperglycemic effects, glucagon signaling has demonstrated importance in broader metabolic processes. Global elimination of glucagon receptor signaling in mice decreases median lifespan by 35% in lean animals and renders mice unresponsive to the metabolic benefits of caloric restriction, including reduced liver fat and improved serum lipids [15]. Glucagon signaling appears indispensable for activation of key nutrient-sensing pathways including AMPK and for appropriate regulation of mTOR activity in response to dietary interventions [15]. These findings position glucagon as a crucial regulator of metabolic health beyond its glucose-elevating effects.
Table 2: Metabolic Processes Regulated by Glucagon Signaling
| Metabolic Process | Mechanism of Regulation | Primary Tissues | Therapeutic Implications |
|---|---|---|---|
| Glucose production | PKA-mediated enzyme phosphorylation | Liver | Hyperglycemic effect limits therapeutic use |
| Lipid metabolism | Stimulation of lipolysis, fat oxidation | Liver, adipose tissue | Potential for treating MASLD/NAFLD |
| Energy expenditure | Unclear; possibly CNS-mediated | CNS, peripheral tissues | Obesity treatment |
| Amino acid metabolism | Liver-pancreatic alpha cell axis | Liver, pancreas | Relationship with gluconeogenesis |
| Longevity pathways | AMPK activation, mTOR inhibition | Multiple | Healthspan extension |
Signaling Pathway Integration and Crosstalk
Insulin-Glucagon Reciprocal Regulation
The insulin and glucagon signaling systems function as an integrated network rather than independent pathways, with multiple points of crosstalk and reciprocal regulation. Insulin not only stimulates glucose uptake and lipid synthesis but also inhibits glucagon secretion from pancreatic alpha cells and antagonizes many catabolic processes activated by glucagon [14]. Conversely, glucagon signaling can modulate insulin sensitivity through effects on substrate competition and direct signaling interference. Computational modeling of this integrated network reveals bistable behavior in the anabolic zone (glucose >5.5 mmol/L), where the positive feedback of AKT on IRS creates hysteresis in the system response [14].
This bistability provides a buffering mechanism that maintains metabolic state stability despite fluctuations in nutrient availability. The modeling further indicates that the positive feedback of calcium on cAMP is responsible for ensuring ultrasensitive response in the catabolic zone (glucose <4.5 mmol/L), while crosstalk between AKT and phosphodiesterase 3 (PDE3) enables efficient catabolic response under low glucose conditions [14]. These emergent properties of the integrated signaling network illustrate how insulin and glucagon cooperatively maintain metabolic homeostasis through complex nonlinear interactions.
Incretin Hormones and Multi-Agonist Therapeutics
The incretin hormones GIP and GLP-1 have emerged as crucial regulators of insulin and glucagon secretion with important therapeutic implications. GLP-1 receptor agonists enhance glucose-dependent insulin secretion, suppress glucagon secretion, delay gastric emptying, and reduce food intake through central appetite suppression [10] [12]. GIP exerts complementary effects, stimulating insulin secretion during hyperglycemia while having glucagonotropic effects during hypoglycemia, and directly promoting lipogenesis in adipose tissue [12].
The development of multi-agonists that simultaneously target multiple receptors represents a significant advancement in metabolic therapeutics. Several GCGR-based multi-agonists (mazdutide, survodutide, retatrutide) have demonstrated substantial efficacy for weight loss in people with obesity while improving liver health in those with metabolic dysfunction-associated steatotic liver disease (MASLD) [11]. These unimolecular compounds typically incorporate moieties that activate both GLP-1 and glucagon receptors, with GLP-1 receptor activation mitigating the hyperglycemic effects of glucagon receptor activation [11]. The success of these agents underscores the therapeutic potential of targeting multiple interconnected hormonal pathways simultaneously.
Experimental Approaches and Methodologies
Computational Analysis of Signaling Networks
Computational approaches provide powerful tools for analyzing the complex behaviors emerging from insulin-glucagon signaling interactions. Mathematical modeling of the integrated network enables simulation of system responses to various perturbations and prediction of behaviors difficult to observe experimentally [14]. A representative modeling approach involves:
Network Construction: Define all molecular species and interactions based on established literature, including receptors, secondary messengers, enzymes, and transcription factors. Key interactions should include insulin-mediated AKT activation, glucagon-mediated PKA activation, and crosstalk mechanisms such as AKT-mediated PDE3 activation and calcium-mediated cAMP modulation [14].
Parameter Estimation: Determine kinetic parameters from experimental data where available, using optimization algorithms to estimate unknown parameters. Validation should include comparison to experimental data such as IRS and AKT activation profiles in adipocytes [14].
System Perturbation: Simulate the network response to varying concentrations of insulin, glucagon, glucose, amino acids, and fatty acids. Analyze steady-state profiles for key signaling nodes (AKT phosphorylation, PKA activation) and defined output indices such as phosphorylation state (Ps) [14].
Bifurcation Analysis: Identify parameter regions exhibiting bistability or other nonlinear behaviors. Determine how feedback loops and crosstalk mechanisms shape these emergent properties [14].
This computational framework has revealed that certain macronutrient compositions may be more conducive to homeostasis than others and identified network perturbations that may contribute to disease states such as diabetes, obesity, and cancer [14].
Genetic and Pharmacological Manipulation
Genetic manipulation approaches provide crucial insights into signaling pathway functions:
Global and Tissue-Specific Knockout Models: Global glucagon receptor knockout (Gcgr KO) mice demonstrate the essential role of glucagon signaling in metabolic responses to caloric restriction [15]. Liver-specific knockout models (Gcgrhep−/−) enable dissection of tissue-specific functions, revealing that hepatic glucagon receptor signaling is necessary for CR-induced changes in AMPK and mTOR activity [15].
Pharmacological Activation: Acute and chronic administration of glucagon analogues (e.g., NNC9204-0043) allows investigation of glucagon receptor signaling effects on downstream pathways including cAMP production, AMPK activation, and mTOR inhibition [15]. Dosing regimens typically involve single injections for acute effects (e.g., 1.5 nmol/kg BW subcutaneous) or prolonged administration for chronic effects.
Metabolic Phenotyping: Comprehensive assessment includes body composition analysis (NMR), indirect calorimetry for energy expenditure and respiratory quotient, oral glucose tolerance tests (OGTT), insulin tolerance tests (ITT), and tissue collection for molecular analysis of signaling pathway activation [15].
Diagram 1: Glucagon receptor signaling pathway and downstream metabolic effects
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating Insulin-Glucagon Signaling
| Reagent/Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Genetic Models | Gcgr KO, Gcgrhep−/−, IRS KO mice | Pathway necessity studies | Determine tissue-specific functions |
| Receptor Agonists | NNC9204-0043, dual/tri-agonists | Pharmacological activation | Pathway-specific effects |
| Antibodies | Phospho-AKT, phospho-PKA, total proteins | Western blot, IHC | Detect pathway activation |
| Metabolic Assays | OGTT, ITT, indirect calorimetry | Physiological assessment | Whole-body metabolic phenotyping |
| cAMP Assays | ELISA, FRET-based biosensors | Second messenger measurement | Quantify GCGR activation |
| Hormone Analytics | GLP-1, GIP, insulin ELISAs | Hormone level quantification | Correlate with signaling states |
Visualization of Integrated Metabolic Signaling
Diagram 2: Integrated insulin and glucagon signaling network with key regulatory nodes
The molecular mechanisms of insulin and glucagon receptor signaling represent a complex, integrated system for maintaining metabolic homeostasis. Understanding these pathways at a detailed level provides crucial insights for developing novel therapeutic approaches for metabolic diseases. The emergence of multi-agonists that simultaneously target multiple receptors highlights the translational importance of this basic research. Continued investigation using the experimental approaches outlined in this review will further elucidate the intricate regulation of these pathways and their potential as therapeutic targets for obesity, diabetes, MASLD, and other cardio-kidney-metabolic conditions.
The precise regulation of blood glucose is a fundamental physiological process, essential for survival and metabolic health. While insulin serves as the primary hypoglycemic hormone, a sophisticated counter-regulatory system exists to antagonize its effects and prevent dangerous drops in blood glucose. This system comprises several hormones—glucagon, adrenaline, cortisol, and growth hormone—that work in concert to maintain glucose homeostasis, particularly during fasting, stress, and exercise [16] [5]. Understanding the dynamics of these hormones is crucial for researchers and drug development professionals seeking to address metabolic diseases such as diabetes mellitus.
The "glucagonocentric hypothesis" represents a paradigm shift in our understanding of metabolic regulation, positing that glucagon is not merely insulin's counter-regulatory counterpart but a central driver of metabolic physiology and pathophysiology [5]. This framework is vital for interpreting the complex hormonal interactions that govern systemic energy balance. Disruptions in this delicate equilibrium are hallmarks of diabetes and other metabolic disorders, making the counter-regulatory system a prime target for therapeutic intervention. This review synthesizes current evidence on the mechanisms, interactions, and experimental approaches for studying these critical hormonal regulators.
Core Counter-Regulatory Hormones and Their Mechanisms
The counter-regulatory response involves a coordinated sequence of hormonal actions with distinct temporal characteristics and mechanisms.
Glucagon: The Primary Rapid Responder
Glucagon, a 29-amino-acid peptide secreted by pancreatic α-cells, is the most critical hormone for acute glucose counter-regulation [16] [5]. Its secretion is stimulated by hypoglycemia, protein-rich meals, and sympathetic activation [5]. Glucagon primarily acts on the liver, where it activates hepatic glucose output through two key processes: glycogenolysis (breakdown of glycogen to glucose) and gluconeogenesis (synthesis of glucose from non-carbohydrate precursors) [17] [3] [5]. The onset of glucagon's insulin-antagonistic effect is rapid, making it the first line of defense against falling blood glucose levels [16].
The molecular mechanism of glucagon action involves binding to a specific G-protein-coupled receptor (GPCR) on hepatocytes, which activates adenylate cyclase to increase intracellular cyclic adenosine monophosphate (cAMP) levels [18] [5]. This cascade activates protein kinase A (PKA), which in turn phosphorylates key enzymes that promote glycogen breakdown and gluconeogenic pathways [5]. Recent research has revealed that glucagon's role extends beyond glucose regulation to include modulation of amino acid metabolism, lipid oxidation, and appetite control [5].
Adrenaline: The Secondary Messenger
Adrenaline (epinephrine) is released from the adrenal medulla in response to hypoglycemia and other stress conditions [16]. When glucagon secretion is deficient, as in patients with insulin-dependent diabetes, adrenaline becomes the most important hormone for glucose recovery during hypoglycemia [16]. Adrenaline contributes to glucose elevation through multiple mechanisms: directly stimulating hepatic glucose output, promoting glycogenolysis in muscle, enhancing gluconeogenesis, and inhibiting glucose uptake by peripheral tissues [16].
Adrenaline induces early post-hypoglycemic insulin resistance, which can persist for several hours after glucose normalization [16]. Its effects are mediated through β-adrenergic receptors that activate cAMP-dependent pathways similar to glucagon, as well as α-adrenergic receptors that utilize calcium and inositol phosphate signaling systems [5].
Cortisol and Growth Hormone: Delayed Regulators
Cortisol and growth hormone exhibit counter-regulatory effects that manifest after a lag period of several hours [16]. These hormones are particularly important during prolonged hypoglycemia, where they help sustain glucose levels by inducing insulin resistance in peripheral tissues and promoting alternative fuel utilization [16] [3].
Growth hormone reduces glucose utilization by cells and increases fat mobilization, thereby conserving glucose for glucose-dependent tissues [3]. The pronounced insulin-antagonistic effect of growth hormone suggests it plays a key role in regulating diurnal rhythms of glucose metabolism, including the dawn phenomenon [16]. Cortisol promotes gluconeogenesis, antagonizes insulin action in peripheral tissues, and synergizes with other counter-regulatory hormones to maintain fasting glucose levels [16].
Table 1: Characteristics of Major Counter-Regulatory Hormones
| Hormone | Site of Secretion | Primary Stimulus | Onset of Action | Major Metabolic Effects |
|---|---|---|---|---|
| Glucagon | Pancreatic α-cells | Hypoglycemia, protein meals, sympathetic activation | Rapid (minutes) | ↑ Hepatic glycogenolysis & gluconeogenesis, ↑ amino acid catabolism, ↑ lipid oxidation |
| Adrenaline | Adrenal medulla | Hypoglycemia, stress | Rapid (minutes) | ↑ Hepatic glucose output, ↑ muscle glycogenolysis, ↓ peripheral glucose uptake |
| Cortisol | Adrenal cortex | Prolonged hypoglycemia, stress | Slow (hours) | ↑ Gluconeogenesis, ↑ peripheral insulin resistance, ↑ protein catabolism |
| Growth Hormone | Anterior pituitary | Prolonged hypoglycemia, stress | Slow (hours) | ↑ Peripheral insulin resistance, ↑ lipolysis, ↓ glucose utilization |
Quantitative Hormone Dynamics and Pancreatic Stores
Understanding the quantitative aspects of hormone secretion and pancreatic reserves provides critical insights for metabolic disease research.
Hormonal Dynamics in Glucose Regulation
In healthy individuals, fasting blood glucose concentrations typically range between 80-90 mg/dL, with postprandial levels rising to 120-140 mg/dL before returning to baseline within 2 hours [3]. This stability is maintained through the pulsatile secretion of insulin and precisely timed counter-regulatory responses [18] [3]. During hypoglycemia, glucagon secretion increases dramatically, with adrenaline becoming significant if hypoglycemia persists or when glucagon is deficient [16].
The insulin-antagonistic effects of these hormones occur at different potencies and time courses. Glucagon and adrenaline exert their effects within minutes, while cortisol and growth hormone require several hours to manifest their full impact [16]. The hierarchy of importance varies with context: glucagon is paramount for acute counter-regulation, while adrenaline serves as a critical backup, and cortisol/growth hormone contribute to prolonged responses [16].
Pancreatic Hormone Content in Health and Disease
Post-mortem analyses of pancreatic tissue reveal significant differences in hormone stores between non-diabetic and type 2 diabetic (T2D) subjects. A study of 20 lean non-diabetic, 19 obese non-diabetic, and 18 T2D subjects found that pancreatic insulin content was 35% lower in T2D subjects (7.4 mg versus 11.3 mg in non-diabetic subjects) [19]. In contrast, pancreatic glucagon content was similar between T2D and non-diabetic subjects (0.76 mg versus 0.81 mg) [19]. This disparity resulted in a significantly higher glucagon/insulin ratio in T2D subjects (17.4% versus 11.7% in non-diabetic subjects) [19].
Notably, pancreatic somatostatin content was 29% lower in T2D subjects, though the ratios of somatostatin to both insulin and glucagon were not significantly different [19]. These findings indicate that the secretory abnormalities characteristic of T2D cannot be attributed solely to alterations in pancreatic hormone reserves, suggesting instead functional dysregulation in secretion control [19].
Table 2: Pancreatic Hormone Content in Non-Diabetic and Type 2 Diabetic Subjects
| Parameter | Lean Non-Diabetic (n=20) | Obese Non-Diabetic (n=19) | All Non-Diabetic (n=39) | Type 2 Diabetic (n=18) |
|---|---|---|---|---|
| Insulin Content (mg) | 10.2 ± 3.7 | 12.5 ± 3.9 | 11.3 ± 3.9 | 7.4 ± 3.9* |
| Glucagon Content (mg) | 0.92 ± 0.49 | 0.70 ± 0.33 | 0.81 ± 0.43 | 0.76 ± 0.45 |
| Somatostatin Content (mg) | 0.036 ± 0.017 | 0.040 ± 0.018 | 0.038 ± 0.017 | 0.027 ± 0.015* |
| Glucagon/Insulin Ratio (%) | 13.5 ± 6.6 | 9.8 ± 4.3 | 11.7 ± 5.8 | 17.4 ± 7.7* |
Note: Data presented as mean ± SD; *P < 0.05 compared to All Non-Diabetic group
Experimental Models and Methodologies
Key Experimental Protocols
Several sophisticated methodologies have been developed to study counter-regulatory hormone dynamics:
Pancreatic Hormone Extraction and Quantification: Human pancreatic tissue obtained at autopsy can be processed for hormone measurement. Tissue samples are homogenized in acid-ethanol solution for hormone extraction, followed by centrifugation and collection of supernatants [19]. Hormone concentrations are determined using specific radioimmunoassays (RIAs) or enzyme-linked immunosorbent assays (ELISAs) for insulin, glucagon, and somatostatin [19]. Total pancreatic hormone content is calculated by multiplying hormone concentration by pancreas weight, accounting for regional variations in islet distribution (higher density in tail vs. head/body) [19].
Perfused Mouse Pancreas Model: This ex vivo system allows precise control of the pancreatic microenvironment. The pancreas is isolated with intact vascular supply and perfused with oxygenated buffer containing specific nutrient or pharmacologic stimuli [20]. Efficient blockage of glucagon signaling can be achieved using specific glucagon receptor (GCGR) antagonists like des-His¹-Glu⁹-glucagon amide, while GLP-1 receptor (GLP-1R) blockade utilizes exendin(9-39) [20]. Effluent samples are collected at timed intervals for hormone measurement by RIA to assess dynamic secretion patterns [20].
Intra-islet Paracrine Signaling Studies: To investigate communication between α- and β-cells, researchers employ specific receptor antagonists and genetic models. The impact of glucagon signaling on insulin secretion is studied using GCGR blockers in perfused pancreas systems and isolated islets [20]. Similarly, the effects of insulin on α-cells are examined using insulin receptor antagonists and β-cell-specific insulin receptor knockout models [5]. These approaches have revealed that insulin normally suppresses glucagon secretion through PI3K-Akt-dependent pathways, a mechanism impaired in T2D [5].
Mass Spectrometry for Bioactive GLP-1 Detection: Duke researchers developed a high-specificity mass spectrometry assay to detect only the bioactive form of GLP-1, avoiding interference from inactive fragments that often confound traditional measurements [21]. This methodology revealed that pancreatic α-cells produce substantial bioactive GLP-1, particularly when glucagon production is blocked, demonstrating remarkable α-cell plasticity [21].
Signaling Pathway Visualization
Glucagon and GLP-1 Signaling Pathways
Emerging Concepts and Therapeutic Implications
Alpha Cell Plasticity and GLP-1 Production
Recent research has uncovered remarkable flexibility in pancreatic α-cell function. Duke University studies demonstrate that when glucagon production is blocked by inhibiting the prohormone convertase PC2, α-cells increase production of GLP-1 via the enzyme PC1 [21]. This shift improves glucose control and enhances insulin secretion, suggesting GLP-1 is a more powerful insulin stimulator than glucagon [21]. This plasticity represents a potential endogenous mechanism for maintaining glucose homeostasis that could be therapeutically harnessed.
The discovery that pancreatic α-cells, not just intestinal L-cells, produce significant amounts of bioactive GLP-1 challenges traditional paradigms [21]. Using mass spectrometry, researchers found that human pancreatic tissue produces much higher levels of bioactive GLP-1 than previously believed, with production directly linked to insulin secretion [21]. This finding is particularly relevant for diabetes drug development, as GLP-1 receptor agonists are already established therapies.
Intra-islet Paracrine Communication
The pancreatic islet functions as a micro-organ with sophisticated cell-to-cell communication. Insulin, zinc, GABA, and somatostatin secreted by β- and δ-cells provide paracrine inhibition of glucagon release from α-cells [5]. In type 2 diabetes, resistance to insulin's suppressive effect on α-cells contributes to hyperglucagonemia and impaired glycemic control [5]. Understanding these paracrine interactions is essential for developing therapies that restore normal islet function rather than simply replacing individual hormones.
Research using perfused mouse pancreas models demonstrates that insulin secretion depends on intra-islet glucagon signaling [20]. Blocking glucagon receptors impairs insulin secretion, revealing that the glucagon receptor plays a physiological role in maintaining insulin secretion, likely through the cAMP signaling pathway [20]. This challenges the simplistic view of glucagon solely as an insulin antagonist and highlights the complexity of islet cross-talk.
Glucagon-Centric View of Metabolic Disease
The "glucagonocentric hypothesis" positions glucagon as a central driver of diabetic hyperglycemia, not merely a counter-regulatory hormone [5]. Hyperglucagonemia is present in both type 1 and type 2 diabetes and contributes significantly to fasting and postprandial hyperglycemia [5]. In T1DM, lack of insulin removes its inhibitory effect on α-cells, leading to inappropriate glucagon secretion even during hyperglycemia [5]. In T2DM, α-cells become resistant to insulin-mediated suppression [5].
Glucagon's role extends beyond glycemic control to include regulation of amino acid metabolism, lipid oxidation, bile acid turnover, and thermogenesis [5]. Disruptions in these pathways contribute to the pathogenesis of NAFLD, CKD, and cardiovascular complications, suggesting glucagon dysregulation may be an upstream factor driving diabetic complications across multiple organ systems [5].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Counter-Regulatory Hormone Studies
| Reagent / Method | Function / Application | Research Context |
|---|---|---|
| GCGR Antagonists (e.g., des-His¹-Glu⁹-glucagon amide) | Competitive blockade of glucagon receptors to study glucagon signaling pathways | Used in perfused pancreas and isolated islet studies to demonstrate intra-islet glucagon dependency for insulin secretion [20] |
| GLP-1R Antagonists (e.g., exendin(9-39)) | Specific inhibition of GLP-1 receptors to delineate GLP-1-mediated effects | Employed to distinguish GLP-1 signaling from glucagon signaling in α-cell studies [20] |
| Mass Spectrometry Assay | High-specificity detection of bioactive GLP-1, excluding inactive fragments | Enabled discovery of substantial GLP-1 production in human pancreatic α-cells [21] |
| Prohormone Convertase Inhibitors (PC1/PC2 blockade) | Selective inhibition of hormone processing enzymes to study α-cell plasticity | Demonstrates α-cell switch from glucagon to GLP-1 production when PC2 is blocked [21] |
| Specific RIAs/ELISAs | Precise quantification of hormone concentrations in tissues and fluids | Used to measure insulin, glucagon, and somatostatin in pancreatic extracts from diabetic and non-diabetic subjects [19] |
| Perfused Pancreas System | Ex vivo model maintaining intact vascular and paracrine signaling | Allows precise control of pancreatic microenvironment and dynamic assessment of hormone secretion [20] |
The counter-regulatory hormone system represents a complex, multi-layered network that maintains glucose homeostasis through precisely coordinated interactions. The traditional view of glucagon as merely insulin's counter-regulatory hormone has evolved to recognize its central role as a master regulator of nutrient metabolism and a significant contributor to the pathophysiology of diabetes and related metabolic disorders. Emerging concepts of α-cell plasticity, intra-islet paracrine communication, and multi-organ glucagon signaling provide new frameworks for understanding metabolic disease.
For researchers and drug development professionals, these advances open promising therapeutic avenues. Targeting α-cell plasticity, restoring normal paracrine signaling within islets, and developing balanced multi-agonist molecules that engage both insulin and glucagon pathways represent frontier areas in metabolic disease therapeutics. As our understanding of counter-regulatory dynamics continues to deepen, so too will opportunities to develop more effective treatments for diabetes and related metabolic disorders that address the root causes of hormonal dysregulation rather than merely compensating for its consequences.
For decades, the prevailing model of hormonal blood glucose regulation placed insulin deficiency and resistance as the central pathophysiologic drivers of diabetes mellitus. Within this framework, glucagon was viewed primarily as insulin's counter-regulatory hormone, tasked with preventing hypoglycemia by stimulating hepatic glucose production [5] [22]. However, recent research has catalyzed a conceptual shift toward the "glucagonocentric hypothesis," which posits that glucagon is not merely a counter-regulatory hormone but a key systemic regulator of energy balance with multifaceted roles beyond glycemic control [5] [22]. This whitepaper synthesizes current evidence demonstrating glucagon's critical involvement in amino acid metabolism, lipid oxidation, appetite control, and energy expenditure, thereby reframing our understanding of its pathophysiological significance in cardiometabolic diseases.
Disruptions in glucagon signaling pathways contribute significantly to the pathogenesis of type 1 and type 2 diabetes (T1DM, T2DM), non-alcoholic fatty liver disease (NAFLD)/metabolic dysfunction-associated steatotic liver disease (MASLD), chronic kidney disease (CKD), and obesity [5] [11]. These conditions often manifest as hyperglucagonemia and hepatic glucagon resistance, states whose broader systemic effects are still being elucidated [22]. This expanded understanding is now driving the development of novel therapeutic agents that incorporate glucagon receptor activity alongside other incretin hormones, representing a frontier in metabolic disease pharmacotherapy [11] [23].
Expanded Metabolic Roles of Glucagon
Glucagon in Amino Acid Metabolism
The liver-α-cell axis represents a crucial feedback loop maintaining systemic amino acid homeostasis. Glucagon directly stimulates hepatic amino acid uptake and catabolism, while also promoting ureagenesis—the conversion of ammonia into urea for safe excretion [5] [22]. This process is vital for detoxifying ammonia generated from protein catabolism. When hepatic glucagon signaling is impaired, as occurs in glucagon resistance, it disrupts this axis, leading to hyperaminoacidemia (elevated blood amino acid levels) [5]. This elevated amino acid concentration subsequently triggers excessive glucagon secretion from pancreatic α-cells, creating a pathological cycle [5] [22].
Notably, glucagon-induced amino acid catabolism may have detrimental consequences in chronic metabolic diseases. By increasing the breakdown of amino acids, particularly from skeletal muscle, glucagon can potentially contribute to muscle wasting, thereby supplying substrates for hepatic gluconeogenesis and perpetuating hyperglycemia [5] [22]. This catabolic pathway illustrates how glucagon's amino acid-regulating functions can indirectly sustain elevated blood glucose levels in diabetes.
Glucagon in Lipid Metabolism and Energy Balance
Beyond its classical roles, glucagon exerts significant effects on lipid homeostasis and overall energy balance through multiple mechanisms:
Hepatic Lipid Metabolism: Glucagon promotes hepatic lipolysis and fatty acid oxidation while facilitating cholesterol clearance [5] [22]. Recent research has identified that the RNA-binding protein ALKBH5 regulates the glucagon receptor (GCGR) and mTORC1 signaling through distinct mechanisms, integrating control of both glucose and lipid metabolism [23]. Specifically, ALKBH5 regulates the EGFR-mTORC1 signaling cascade independently of its demethylase activity, thereby influencing lipid homeostasis [23].
Appetite Regulation: Glucagon acts as a satiety signal through the liver–vagal nerve–hypothalamic axis. Studies demonstrate that glucagon decreases food intake in rodent models, while glucagon antibodies have been associated with increased food consumption, highlighting its anorexigenic effect [5].
Thermogenesis: Glucagon encourages heat production by activating brown adipose tissue (BAT), thereby increasing energy expenditure and potentially aiding weight loss [5]. This thermogenic effect, combined with appetite suppression, positions glucagon as a significant regulator of whole-body energy balance.
Table 1: Glucagon's Multi-Organ Metabolic Effects
| Target Organ/Tissue | Primary Metabolic Effects | Signaling Pathways |
|---|---|---|
| Liver | Stimulates gluconeogenesis, glycogenolysis; Enhances amino acid uptake/catabolism, ureagenesis; Promotes lipolysis, fatty acid oxidation, cholesterol clearance | cAMP-PKA, ALKBH5-GCGR, ALKBH5-EGFR-mTORC1 |
| Brain | Decreases food intake; Regulates blood glucose via central nervous system | Liver-vagal nerve-hypothalamic axis |
| Brown Adipose Tissue | Activates thermogenesis; Increases energy expenditure | Sympathetic nervous system activation |
| Pancreas | Paracrine regulation of β-cells; Potential GLP-1 production | cAMP-PKA, intra-islet signaling |
Signaling Pathways and Molecular Mechanisms
Canonical and Emerging Signaling Cascades
Glucagon signaling is primarily mediated through the glucagon receptor (GCGR), a G protein-coupled receptor (GPCR) highly expressed in the liver, kidney, and various other tissues [11]. Upon glucagon binding, GCGR activates adenylate cyclase, leading to increased intracellular cyclic adenosine monophosphate (cAMP) levels. This second messenger then activates protein kinase A (PKA) and exchange protein directly activated by cAMP (Epac), which in turn regulate downstream effectors including calcium channels and vesicle trafficking proteins [5] [22].
Recent research has uncovered novel signaling intermediaries, particularly the RNA-binding protein ALKBH5, which integrates glucagon's effects on both glucose and lipid metabolism through two distinct mechanisms [23]:
Glucose Homeostasis: Glucagon-PKA signaling phosphorylates ALKBH5 at Ser362, promoting its translocation from the nucleus to the cytoplasm, where it binds to and stabilizes Gcgr mRNA via m6A demethylation, sustaining GCGR signaling.
Lipid Homeostasis: ALKBH5 independently activates Egfr transcription through demethylase-independent enhancer binding, subsequently upregulating the EGFR-PI3K-mTORC1-SREBP1 pathway to regulate lipid synthesis.
Central Nervous System Integration
The central nervous system (CNS), particularly hypothalamic and brainstem regions, plays a vital role in glucagon-mediated systemic metabolism. Specific neuronal populations in the arcuate nucleus (ARH), ventromedial hypothalamus (VMH), and dorsal vagal complex (DVC) sense metabolic signals including glucose, insulin, and likely glucagon itself to regulate autonomic outflow and endocrine function [24] [25]. Glucagon receptors in the hypothalamus coordinate hepatic glucose production via neural pathways that help sustain overall metabolic balance [5] [22].
Notably, AgRP/NPY neurons in the ARH regulate hepatic glucose production and systemic insulin sensitivity, while POMC neurons mediate glucose-lowering effects and influence renal glucose reabsorption [25]. The VMH is particularly important for counterregulatory hormone responses during hypoglycemia, with SF-1 neurons essential for recovery from insulin-induced hypoglycemia through glucagon and corticosterone secretion [25]. These central regulatory circuits demonstrate the sophisticated integration of glucagon signaling within broader neuroendocrine networks maintaining metabolic homeostasis.
Experimental Approaches and Methodologies
Key Research Models and Techniques
Investigating glucagon's expanded metabolic roles requires sophisticated experimental approaches spanning molecular, cellular, and whole-organism levels. The following methodologies represent cutting-edge techniques in the field:
Table 2: Experimental Approaches for Studying Glucagon Biology
| Methodology | Application | Key Findings |
|---|---|---|
| Genetic lineage tracing & indelible marking | Tracking β-cell and α-cell subtypes over time; Studying cellular plasticity | Revealed β-cell subtypes with varying fitness; Maternal diet effects on offspring β-cell populations [26] |
| High-specificity mass spectrometry | Detecting bioactive GLP-1 (not inactive fragments) | Discovered alpha cells produce significant bioactive GLP-1, especially when glucagon blocked [21] |
| Chemogenetics & Optogenetics | Controlling specific neuronal population activity in live animals | Identified AgRP neurons decrease insulin sensitivity; VMH SF-1 neurons crucial for hypoglycemia recovery [25] |
| Hepatocyte-specific knockout models | Tissue-specific gene function analysis (e.g., Alkbh5-HKO mice) | ALKBH5 regulates GCGR (glucose) and EGFR-mTORC1 (lipid) via distinct mechanisms [23] |
| Enzyme manipulation (PC1/PC2 inhibition) | Studying hormone production pathways in alpha cells | Blocking PC2 (glucagon production) boosted PC1 (GLP-1 production), improving glucose control [21] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Glucagon Signaling Studies
| Reagent / Tool | Function / Application | Research Context |
|---|---|---|
| Alkbh5-HKO mice | Liver-specific ALKBH5 knockout model | Studying tissue-specific regulation of glucose (GCGR) and lipid (EGFR-mTORC1) homeostasis [23] |
| GCGR antagonists | Blocking glucagon receptor signaling | Validating glucagon's role in hyperglycemia; GCGR antagonism lowers blood glucose but increases body weight, hepatic fat [11] |
| PC2 inhibitors | Blocking prohormone convertase 2 enzyme | Inhibiting glucagon production from alpha cells; Surprisingly increases GLP-1 production [21] |
| GalNAc-siRNA technology | Liver-specific gene knockdown therapeutic approach | Hepatic Alkbh5 knockdown reversed hyperglycemia, hyperlipidemia, and MAFLD in db/db mice [23] |
| Insulin-glucagon fusion proteins | Single molecule combining insulin and glucagon activities | Exploits endogenous hepatic switch: insulin dominates at high glucose, glucagon at low glucose [27] |
Therapeutic Implications and Future Directions
Emerging Pharmacological Approaches
The expanding understanding of glucagon biology has catalyzed the development of novel therapeutic agents for metabolic diseases. Unlike earlier strategies that focused solely on glucagon receptor antagonism, contemporary approaches leverage glucagon's beneficial metabolic effects while mitigating its hyperglycemic potential:
Multi-Agonist Therapies: Unimolecular compounds incorporating glucagon receptor activation alongside GLP-1 receptor (GLP-1R) and/or glucose-dependent insulinotropic polypeptide receptor (GIPR) agonism have demonstrated substantial efficacy. Retatrutide (GCGR/GIPR/GLP-1R triple agonist), mazdutide, and survodutide (both GCGR/GLP-1R dual agonists) have advanced to Phase III clinical trials, showing promising results for weight loss and MASLD/MASH improvement [11] [23].
Stabilized Glucagon Analogs: Research on ultrastable insulin-glucagon fusion proteins demonstrates the potential for exploiting endogenous hepatic switches where "insulin wins" at high glucose levels, while "glucagon wins" at low glucose levels, thereby mitigating hypoglycemic risk [27].
RNA-Targeted Therapies: The identification of ALKBH5 as a coordinator of glucose and lipid metabolism through distinct mechanisms highlights the potential of targeting RNA-binding proteins for metabolic disease treatment [23].
Future Research Directions
Despite significant advances, critical questions remain regarding glucagon's expanded metabolic roles. Future research should focus on:
Glucagon Resistance Mechanisms: Delineating the molecular pathways underlying hepatic and extra-hepatic glucagon resistance across different metabolic diseases [5] [22].
Alpha Cell Plasticity: Further exploration of alpha cell reprogramming capabilities, including the physiological and therapeutic relevance of their GLP-1 production capacity [21].
Central Glucagon Signaling: Elucidating the precise neural circuits and mechanisms through which central glucagon signaling influences peripheral metabolism [24] [25].
Tissue-Specific Effects: Understanding how glucagon signaling is regulated in different tissues (skeletal muscle, adipose tissue, kidney) and its contribution to whole-body metabolic homeostasis [5] [23].
The ongoing clinical development of GCGR-based multi-agonists and continued basic research into glucagon biology will further clarify its role in energy regulation and lipid metabolism, potentially yielding new therapeutic options for obesity, MASLD, and other cardio-kidney-metabolic conditions [11]. As these data emerge, the glucagon-centric perspective on metabolic disease will continue to evolve, potentially transforming our approach to treating these prevalent conditions.
The traditional paradigm of pancreatic islet function delineates a strict division of labor: α-cells produce glucagon to elevate blood glucose, while β-cells secrete insulin to lower it. However, a transformative shift is underway, fueled by the discovery that pancreatic α-cells exhibit significant plasticity, including the capacity to co-produce glucagon-like peptide-1 (GLP-1). This whitepaper synthesizes recent advances revealing that α-cells can dynamically alter their hormonal output, upregulating the production of bioactive GLP-1 via the enzyme PC1/3. This review details the molecular mechanisms, quantitative assessments, and experimental methodologies defining this phenomenon, and discusses its profound implications for understanding systemic glucose homeostasis and developing next-generation therapeutics for diabetes.
For decades, the hormonal regulation of blood glucose has been modeled on the opposing actions of insulin and glucagon. Insulin, secreted by pancreatic β-cells in response to elevated blood glucose, promotes glucose uptake and storage. In contrast, glucagon, released from pancreatic α-cells during fasting or hypoglycemia, stimulates hepatic glucose production [2] [5]. This binary model is now recognized as incomplete.
Alpha cell plasticity challenges this conventional view. Emerging evidence demonstrates that α-cells are not terminally differentiated but possess the remarkable ability to adapt their function and hormone profile in response to metabolic cues and disease states [21] [28]. A cornerstone of this plasticity is the co-production of GLP-1, a potent incretin hormone that enhances glucose-stimulated insulin secretion, inhibits glucagon release, and slows gastric emptying [29]. While GLP-1 was traditionally considered a gut-derived hormone, produced and secreted by intestinal L-cells [30], its synthesis within pancreatic islets, particularly by α-cells, is now established as a functionally significant source [21] [31].
This whitepaper explores the molecular basis and functional consequences of α-cell GLP-1 production, framing it within the broader context of islet cell transdifferentiation and hormonal crosstalk. It is intended to equip researchers and drug development professionals with a detailed technical overview of this emerging paradigm.
Molecular Mechanisms of Proglucagon Processing
The production of both glucagon and GLP-1 from a single precursor, proglucagon, is a classic example of tissue-specific post-translational processing.
The Proglucagon Gene and Protein
The proglucagon gene (Gcg) encodes a 160-amino acid precursor polypeptide that contains the sequences for several biologically active peptides, including glucagon, GLP-1, and GLP-2 [29]. The fate of this prohormone is determined by the specific prohormone convertase (PC) enzymes expressed in different tissues.
Tissue-Specific Cleavage
The differential processing of proglucagon in pancreatic α-cells and intestinal L-cells is summarized in the table below.
Table 1: Tissue-Specific Processing of Proglucagon
| Tissue/Cell Type | Key Processing Enzyme | Primary Peptide Products |
|---|---|---|
| Pancreatic α-cell | Prohormone Convertase 2 (PC2) | Glucagon, Major Proglucagon Fragment (MPGF) [29] [30] |
| Intestinal L-cell | Prohormone Convertase 1/3 (PC1/3) | Glicentin, GLP-1, GLP-2, Oxyntomodulin [29] [30] |
The historical view held that pancreatic α-cells exclusively express PC2, thus producing glucagon but not mature GLP-1. This view has been overturned. Recent studies confirm that α-cells can co-express PC1/3, allowing them to process proglucagon into bioactive GLP-1(7-36)NH₂ [21] [31]. This plasticity in processing enzyme usage is a fundamental mechanism enabling α-cells to switch their hormonal output.
The following diagram illustrates the differential processing of proglucagon and the key experimental manipulation of the convertase enzymes.
Enzymatic Switching and Functional Consequences
Research utilizing transgenic mouse models with α-cell-specific inducible deletion of Pcsk2 (encoding PC2) has been pivotal. Campbell et al. demonstrated that blocking PC2 and thus glucagon production did not impair insulin secretion as expected. Instead, α-cells upregulated PC1/3, increased GLP-1 production, and improved glucose tolerance [21] [31]. This "enzymatic switch" from PC2 to PC1/3 represents a built-in rescue mechanism for maintaining insulin secretion and blood glucose control.
Quantitative Evidence and Functional Impact
The physiological relevance of α-cell-derived GLP-1 is supported by robust quantitative data. The table below summarizes key findings from recent studies quantifying GLP-1 in pancreatic tissue and its functional correlation.
Table 2: Quantitative Evidence for α-Cell-Derived GLP-1
| Experimental Model | Key Quantitative Finding | Functional Correlation | Source |
|---|---|---|---|
| Human pancreatic tissue (various ages, weights, diabetes statuses) | Human islets contain substantially higher levels of bioactive GLP-1(7-36)NH₂ than mouse islets. | GLP-1 levels positively correlated with rates of insulin secretion. | [21] [31] |
| Mouse model with α-cell-specific PC2 knockout | Upregulation of PC1/3 and a significant increase in GLP-1 production. | Improved glucose tolerance and enhanced insulin secretion. | [21] [31] |
| Single-cell RNA-seq of human non-diabetic and T2D islets | Identification of a distinct α-cell subpopulation ("AB cells") co-expressing GCG (glucagon) and INS (insulin). | AB cells comprised 2.2-6.9% of insulin-positive cells, increasing in T2D; suggests bihormonal potential and transdifferentiation. | [28] |
These data confirm that GLP-1 production in the human pancreas is not a mere artifact but a quantifiable and functionally significant phenomenon. The presence of bioactive GLP-1 in islets and its positive correlation with insulin secretion underscores its role in a paracrine α-to-β cell signaling axis.
Experimental Protocols for Key Investigations
This section outlines detailed methodologies for key experiments that have been instrumental in elucidating α-cell GLP-1 co-production.
Mass Spectrometry Assay for Bioactive GLP-1
Objective: To accurately detect and quantify levels of the bioactive form of GLP-1 (GLP-1(7-36)NH₂) in pancreatic tissue or islet lysates, avoiding cross-reactivity with inactive fragments [21].
Workflow:
- Tissue Preparation: Isolate pancreatic islets from human or mouse donors. Homogenize islets in a buffer containing protease inhibitors to prevent peptide degradation.
- Peptide Extraction: Use acid-ethanol extraction or solid-phase extraction to isolate peptides from the homogenate.
- Immunoaffinity Enrichment: Incubate the peptide extract with antibodies specific for the N-terminus of GLP-1(7-36)NH₂. This step is critical for excluding other proglucagon-derived peptides and inactive C-terminal fragments (e.g., GLP-1(9-36)NH₂).
- Liquid Chromatography (LC): Separate the enriched peptides using reverse-phase high-performance liquid chromatography (HPLC).
- Mass Spectrometry (MS) Analysis: Analyze the eluent using a high-sensitivity mass spectrometer (e.g., tandem MS). Quantify GLP-1(7-36)NH₂ by comparing its signal to a known concentration of a stable isotope-labeled internal standard.
This method's high specificity, achieved through immunoaffinity and mass spectrometry, was crucial for the definitive discovery of bioactive GLP-1 in human islets [21].
α-Cell-Specific Prohormone Convertase Knockout Model
Objective: To determine the specific roles of PC1/3 and PC2 in α-cell proglucagon processing and islet function in vivo [21] [31].
Workflow:
- Genetic Model Generation: Generate transgenic mouse lines with loxP sites flanking critical exons of the Pcsk1 (PC1/3) and Pcsk2 (PC2) genes. Cross these mice with a mouse line expressing Cre recombinase under the control of an α-cell-specific promoter (e.g., Gcg-Cre or Pax6-CreER for inducible systems).
- Induction and Validation: For inducible models, administer tamoxifen to adult mice to activate Cre recombinase and delete the target genes. Validate gene deletion and protein loss using qPCR, immunohistochemistry, and Western blot on isolated islets.
- Phenotypic Characterization:
- Metabolic Phenotyping: Perform glucose tolerance tests (GTT) and insulin tolerance tests (ITT) on knockout and control mice.
- Hormone Secretion Assays: Use isolated islet perfusion or static incubation to measure glucose-stimulated insulin secretion (GSIS) and glucagon secretion.
- Hormone Level Quantification: Apply the mass spectrometry protocol (4.1) to measure GLP-1 and glucagon levels in knockout islets.
- Data Interpretation: The key finding from this approach was that PC2 knockout improved glucose tolerance via GLP-1, while double knockout of PC1/3 and PC2 abrogated this effect, confirming the critical role of PC1/3 in the compensatory GLP-1 production [21] [31].
Single-Cell RNA Sequencing for α-Cell Heterogeneity
Objective: To identify transcriptomically distinct subpopulations of α-cells and infer cell trajectories in non-diabetic and T2D islets [28].
Workflow:
- Islet Dissociation and Cell Sorting: Dissociate human islets into single-cell suspensions. Use fluorescent cell sorting if specific markers are available.
- Library Preparation and Sequencing: Use a platform like 10x Genomics to capture single cells, barcode RNA, and prepare sequencing libraries. Perform both single-cell RNA-seq (scRNA-seq) and single-nucleus RNA-seq (snRNA-seq) to capture cytoplasmic and nuclear transcripts.
- Bioinformatic Analysis:
- Data Integration and Clustering: Integrate scRNA-seq and snRNA-seq datasets. Perform unsupervised clustering (e.g., Louvain algorithm) to identify cell clusters.
- Subcluster Analysis: Subset the α-cell cluster (GCG+ cells) and re-cluster at high resolution to identify α-cell subtypes.
- Differential Expression and Trajectory Inference: Identify differentially expressed genes (DEGs) between subclusters. Use RNA velocity and PAGA (Partition-based Graph Abstraction) algorithms to infer potential developmental trajectories and transitions between β-cell and α-cell states.
- Validation: Validate key findings from bioinformatic analysis using RNAscope (in situ hybridization) or immunohistochemistry on pancreatic sections. For example, the discovery of the SMOC1 gene as a marker of β-cell dedifferentiation towards an α-cell-like phenotype was validated in this manner [28].
The following diagram illustrates the integrated experimental and computational workflow for single-cell analysis.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs key reagents and tools essential for investigating α-cell plasticity and GLP-1 biology.
Table 3: Research Reagent Solutions for Alpha Cell Plasticity Studies
| Reagent / Tool | Function / Application | Example / Note |
|---|---|---|
| α-Cell-Specific Cre Mouse Models | Enables cell-type-specific gene manipulation (knockout, overexpression) in α-cells in vivo. | Gcg-Cre, Pax6-CreER (tamoxifen-inducible). Critical for studying PC1/3 and PC2 function [31]. |
| High-Specificity GLP-1 Antibodies | Immunoaffinity enrichment for MS, immunohistochemistry (IHC), and immunofluorescence (IF). | Must be specific for N-terminal epitope of GLP-1(7-36)NH₂ to avoid cross-reactivity [21]. |
| Prohormone Convertase Inhibitors | Pharmacological inhibition of PC1/3 or PC2 to validate their roles in proglucagon processing in isolated islet studies. | e.g., PC1/3-specific inhibitors to block GLP-1 production. |
| Single-Cell RNA-seq Kits | Profiling the transcriptome of individual cells to uncover heterogeneity and identify novel subpopulations. | 10x Genomics Chromium platform. Used to identify α-cell subtypes and bihormonal AB cells [28]. |
| Human Pancreatic Islets | Direct ex vivo study of human α-cell biology. Sourced from organ donors (non-diabetic, T2D). | Essential for translational validation of findings from mouse models. Available via programs like HIRN-HPAP [28]. |
| GLP-1 Receptor Agonists (GLP-1RAs) & Antagonists | To probe the functional effects of GLP-1 receptor signaling on β-cells and islet function. | Exendin-9-39 is a common GLP-1R antagonist. |
Discussion and Future Directions
The recognition of α-cells as plastic, multifunctional endocrine cells that can co-produce GLP-1 has fundamentally altered our understanding of islet biology and its dysregulation in diabetes. This paradigm reveals a previously underappreciated layer of intra-islet paracrine control, where α-cells can directly support β-cell function via GLP-1 signaling, especially under metabolic stress [21]. This discovery also provides a potential explanation for the efficacy of GLP-1-based therapies, suggesting they may augment an endogenous compensatory pathway.
The phenomenon of α-cell plasticity is closely linked to transdifferentiation, the conversion of one differentiated cell type into another. Single-cell sequencing studies provide strong evidence for β-cell dedifferentiation and conversion towards an α-cell-like fate in T2D, a process characterized by specific signature genes like SMOC1 [28]. Conversely, targeted inhibition of α-cell identity factors like Arx can promote transdifferentiation into functional β-like cells, offering a promising therapeutic strategy for diabetes [32].
Future research should focus on:
- Identifying Triggers: Precisely defining the metabolic and molecular signals that initiate the switch to GLP-1 production in α-cells.
- Therapeutic Harnessing: Developing safe pharmacological or gene-editing approaches (e.g., CRISPR) to selectively enhance endogenous α-cell GLP-1 production or to promote α-to-β cell transdifferentiation [32] [33].
- Functional Heterogeneity: Understanding the specific physiological roles of the newly identified α-cell subpopulations, particularly the bihormonal AB cells, in health and disease [28].
- Human Specificity: Deepening investigations in human islets, given the quantitively greater production of GLP-1 in human versus mouse α-cells [31].
In conclusion, the co-production of GLP-1 by pancreatic α-cells is a robust and physiologically relevant component of islet hormone regulation. Harnessing this innate plasticity holds immense potential for creating novel, regenerative therapies that go beyond current standards of care for diabetes.
Advanced Analytical and Translational Methods in Hormone Research
The precise quantification of bioactive hormones is fundamental to advancing research in metabolic diseases, particularly in understanding the hormonal regulation of blood glucose by insulin and glucagon. Traditional immunoassays, while widely used, are often limited by cross-reactivity and insufficient sensitivity for detecting low hormone concentrations in complex biological matrices [34]. Liquid chromatography–mass spectrometry (LC–MS) has emerged as the gold-standard technology for hormone analysis, offering unparalleled specificity, sensitivity, and multiplexing capabilities [35] [34]. This technical guide details how modern LC–MS methodologies are empowering researchers and drug development professionals to obtain highly reliable data on hormone dynamics, thereby accelerating discovery in diabetes research and related fields.
The transformation from immunoassays to mass spectrometry-based platforms represents a paradigm shift in endocrine research. LC–MS enables the specific measurement of insulin, glucagon, and other glycemic regulators alongside their precursors, metabolites, and synthetic analogs, providing a comprehensive view of hormonal status [36]. This capability is crucial for investigating complex endocrine pathways, identifying novel biomarkers, and validating the mechanisms of action for new therapeutic compounds.
Technological Foundations of Mass Spectrometry for Hormone Analysis
Core Principles and Historical Development
The integration of liquid chromatography with mass spectrometry (LC–MS) was first conceptualized in the mid-20th century, culminating in the first commercial systems in the 1970s [35]. This combination leverages the superior separation power of LC with the exquisite detection specificity of MS. A pivotal advancement came with the development of soft ionization techniques, notably electrospray ionization (ESI) and atmospheric pressure chemical ionization (APCI), which enabled the efficient ionization and analysis of large, polar biomolecules like peptides and proteins without extensive fragmentation [35]. For hormone analysis, this was revolutionary, allowing researchers to study intact protein hormones such as insulin and glucagon, as well as smaller steroid hormones, within their physiological contexts.
The evolution of mass analyzer technology has been equally critical. Modern hormone analysis platforms commonly employ triple quadrupole (QQQ), quadrupole time-of-flight (Q-TOF), and Orbitrap instruments, often in hybrid configurations [35]. QQQ systems, operating in Multiple Reaction Monitoring (MRM) mode, are the workhorse for targeted, quantitative analysis due to their exceptional sensitivity and wide dynamic range [37]. In contrast, Q-TOF and Orbitrap systems provide high-resolution and accurate mass (HRAM) measurements, making them ideal for untargeted discovery, structural elucidation, and distinguishing between hormones with similar masses [35].
Enhancing Sensitivity and Specificity: MS3 and Advanced Fragmentation
A significant challenge in hormone bioanalysis is detecting ultra-trace concentrations (often pg/mL) within complex sample matrices like serum or plasma. While MS/MS (MRM) is highly effective, background interference can persist. Recent innovations utilize multistage fragmentation (MS3) on ion trap-based instruments to achieve a new level of specificity [37].
In this approach, a precursor ion is isolated and fragmented to produce a primary product ion. This product ion is then isolated and fragmented again, generating a secondary product ion (MS3 spectrum). This additional stage of isolation and fragmentation dramatically reduces chemical noise. Research has demonstrated that MS3 can improve the signal-to-noise ratio (S/N) by an order of magnitude for steroid hormones like cortisol and 17α-hydroxyprogesterone, enabling precise quantification at sub-ng/mL levels with recovery rates of 85–110% [37]. This approach is particularly valuable for differentiating hormones with subtle structural variations and for analyzing samples with severe matrix effects.
Application to Glucose-Regulating Hormones
Analyzing Pancreatic Peptide Hormones: Insulin and Glucagon
The detection and quantification of pancreatic peptide hormones represent a prime application for LC–MS in metabolic research. Insulin and glucagon are crucial counter-regulatory hormones that maintain blood glucose homeostasis [17] [38]. Glucagon, secreted by pancreatic alpha cells, prevents hypoglycemia by stimulating hepatic glycogenolysis and gluconeogenesis, thereby increasing blood sugar levels [38] [39]. Insulin, produced by beta cells, has the opposite effect, promoting glucose uptake into cells and reducing blood sugar [39].
LC–MS methods for these hormones involve careful sample preparation to extract peptides from biological fluids, followed by high-resolution separation and detection [36]. The technology allows researchers to confidently distinguish between the active hormones, their inactive precursors, synthetic analogs used in therapeutics, and degradation products [36]. This is critical for drug development, as LC–MS can monitor the pharmacokinetics of administered hormone therapeutics and differentiate them from endogenous molecules. Furthermore, the speed of modern LC–MS methods, which can be completed in just a few minutes, facilitates high-throughput screening of candidate molecules in preclinical studies [36].
Diagram 1: Insulin and Glucagon in Glucose Regulation. This diagram illustrates the counter-regulatory relationship between insulin and glucagon in maintaining blood glucose homeostasis.
Assaying Steroid Hormones in Metabolic Research
While not direct regulators like insulin, steroid hormones such as cortisol significantly influence glucose metabolism. Cortisol, a glucocorticoid released from the adrenal cortex, increases blood sugar levels by promoting gluconeogenesis and antagonizing insulin [39]. Accurate measurement of these steroids is therefore essential for a holistic understanding of glycemic control. LC–MS has proven vastly superior to immunoassays for this purpose, due to its ability to precisely quantify low-abundance steroids without cross-reactivity from structurally similar molecules [40] [34].
This high specificity is indispensable in pediatric endocrinology and for diagnosing conditions like Cushing's syndrome or congenital adrenal hyperplasia (CAH), which can profoundly disrupt glucose metabolism [40]. For example, in managing CAH, LC–MS is recommended by professional societies for quantifying key adrenal steroids like 17-hydroxyprogesterone, providing greater diagnostic accuracy and enabling more precise monitoring of treatment efficacy [40].
Table 1: Performance of Mass Spectrometry vs. Immunoassay for Hormone Quantification
| Analyte | Typical Clinical Context | Key Challenge | LC-MS/MS Advantage | Reported Performance |
|---|---|---|---|---|
| Testosterone | PCOS, Pediatric Disorders | Overestimation by IA at low concentrations [34] | High specificity in female and pediatric samples [34] | LC-MS/MS median 37 ng/dL vs. CDC RMP 36.7 ng/dL; IA medians 21-51 ng/dL [34] |
| Estradiol (E2) | Postmenopausal BC, Pediatrics | Inaccurate IA measurement at <2 pg/mL [34] | Accurate quantification at ultra-low levels [41] [34] | GC-MS/MS showed good agreement with RIA; sensitive enough for prepubertal children [41] |
| 17-Hydroxyprogesterone | Congenital Adrenal Hyperplasia | Immunoassay false positives [40] | Reduced false-positive rates, superior specificity [40] | Recommended by Endocrine Society over immunoassays [40] |
| Glucagon | Diabetes Research | Specificity against precursors/metabolites [36] | Distinguishes hormone from analogs and degradation products [36] | Enables multi-hormone panels (insulin, glucagon, somatostatin) [36] |
Experimental Protocols and Methodologies
A Representative Workflow for Serum Steroid Hormone Profiling by LC-MS3
The following protocol, adapted from Yi et al. (2025), outlines a highly sensitive and specific method for quantifying five steroid hormones in human serum using an LC-MS3 approach on a quadrupole-linear ion trap (Q-LIT) system [37].
1. Sample Preparation:
- Chemicals: Hydrocortisone (CORT), 4-androstenedione (4AD), 11-deoxycortisol (11D), 21-deoxycortisol (21D), 17α-hydroxyprogesterone (17OHP), and their corresponding isotopically labeled internal standards (e.g., d4-CORT, C3-4AD).
- Procedure:
- Spike 500 µL of human serum with isotopic internal standards.
- Perform liquid-liquid extraction with 2 mL of ethyl acetate/hexane (6:4, v/v).
- Vortex for 2 minutes and centrifuge at 12,000 rpm for 10 minutes.
- Transfer the organic layer and evaporate to dryness under a gentle nitrogen stream.
- Reconstitute the dry residue in 100 µL of methanol/water (70:30, v/v) for LC-MS analysis.
2. Liquid Chromatography:
- Column: Reversed-phase C18 column (e.g., 2.1 mm x 100 mm, 1.8 µm).
- Mobile Phase: A) 0.1% Formic acid in water, B) 0.1% Formic acid in methanol.
- Gradient: Start at 40% B, increase to 95% B over 8 minutes, hold for 3 minutes, then re-equilibrate.
- Flow Rate: 0.3 mL/min.
- Column Temperature: 40 °C.
3. Mass Spectrometric Detection (MS3 on Q-LIT):
- Ionization: Positive electrospray ionization (ESI+).
- Detection Mode: Multistage fragmentation (MS3).
- Process:
- Step 1 (MS1): Select the protonated precursor ion ([M+H]⁺) of the target hormone.
- Step 2 (MS2): Isolate and fragment the precursor ion (e.g., using CID) to generate primary product ions.
- Step 3 (MS3): Select a characteristic primary product ion and fragment it again to generate secondary product ions for quantification.
- Key Advantage: This two-stage fragmentation process significantly reduces background noise, enhancing the signal-to-noise ratio and lowering the limit of detection (LOD). For the five steroids analyzed, LODs were below 0.06 ng/mL, and limits of quantification (LOQ) were below 0.20 ng/mL [37].
Diagram 2: LC-MS3 Experimental Workflow. This diagram outlines the key steps in a multistage fragmentation mass spectrometry assay for high-sensitivity hormone quantification.
Discovery Workflow for Novel Bioactive Peptides
Beyond targeted quantification, LC–MS is a powerful tool for discovering novel bioactive peptides. A large-scale peptidomics study analyzed seven tissues from four mouse strains, identifying over 150,000 unique peptide sequences [42]. The key challenge was distinguishing the few truly bioactive peptides from a vast background of inactive degradation products.
Machine Learning-Enhanced Discovery:
- Data Acquisition: Tissues were heat-stabilized to minimize post-mortem degradation. Peptides were separated from proteins using molecular weight cut-off filters and analyzed by nano-LC-MS/MS with high-resolution fragmentation.
- Data Analysis: A machine learning model was trained on the massive peptidomics dataset. The algorithm learned to predict bioactive peptides based on patterns in the MS data, such as clustering of peptide sequences around known cleavage motifs (e.g., dibasic KR, RR sites) on protein precursors.
- Validation: The model successfully identified known bioactive peptides and predicted new candidates. In-silico and experimental validation (via in-vitro and in-vivo diabetes models) confirmed the bioactivity of several predicted peptides, demonstrating the utility of this integrated approach for therapeutic discovery [42].
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of LC–MS hormone assays requires specific, high-quality reagents and materials. The following table details key components for a robust analytical workflow.
Table 2: Essential Research Reagent Solutions for LC-MS Hormone Analysis
| Reagent/Material | Function/Application | Technical Notes |
|---|---|---|
| Isotopically Labeled Internal Standards (e.g., d4-CORT, d8-17OHP) [41] [37] | Corrects for matrix effects and losses during sample preparation; essential for accurate quantification. | Should be added at the very beginning of the sample preparation process. |
| Chromatography Solvents (LC-MS Grade Methanol, Water, Formic Acid) [37] | Mobile phase components for high-resolution LC separation. Minimizes background noise and ion suppression. | Using high-purity grades is critical to reduce system contamination and maintain sensitivity. |
| Solid-Phase Extraction (SPE) Cartridges or Liquid-Liquid Extraction Solvents (e.g., Ethyl Acetate/Hexane) [37] | Purifies and pre-concentrates target analytes from complex biological matrices like serum or plasma. | Removes proteins, salts, and phospholipids that cause ion suppression. |
| Stable Reference Standards (Certified Hormones: Cortisol, Testosterone, Glucagon, etc.) [41] [37] [36] | Used for instrument calibration and method development. | Sourced as certified reference materials to ensure data accuracy and traceability. |
| Specialized Derivatization Reagents (e.g., Pentafluorobenzyl bromide for GC-MS) [41] | Enhances ionization efficiency and detectability, particularly for steroids in GC-MS and some LC-MS applications. | Can improve sensitivity and lower limits of detection by several orders of magnitude. |
Mass spectrometry has unequivocally established itself as the leading technology for the high-specificity detection of bioactive hormones. Its ability to deliver precise, multiplexed, and sensitive quantification of molecules like insulin, glucagon, and related steroid hormones is transforming basic research and drug development focused on glycemic control. As the technology continues to evolve with advancements in automation, miniaturization, and data analysis—including integration with machine learning—its role in deciphering complex endocrine pathways and delivering novel therapeutics is poised to grow even further [35] [42] [40]. For researchers demanding the highest data quality, leveraging the protocols and tools outlined in this guide provides a robust foundation for generating reliable and impactful results in the field of hormonal regulation.
In Vivo and In Vitro Models for Studying Islet Cell Function and Signaling
The pancreatic islet of Langerhans is a complex micro-organ containing multiple endocrine cell types that collectively maintain blood glucose homeostasis. β-cells secrete insulin to lower blood glucose, while α-cells release glucagon to raise it, with δ-cells (somatostatin) and γ-cells (pancreatic polypeptide) providing additional paracrine regulation [43] [44]. Understanding islet cell function requires sophisticated experimental models that preserve the physiological context while enabling precise experimental manipulation. This technical guide provides a comprehensive overview of established and emerging models for studying islet cell function and signaling, with particular emphasis on their applications in investigating the hormonal regulation of blood glucose by insulin and glucagon.
Model Systems for Islet Research
Researchers employ complementary model systems ranging from reduced in vitro preparations to intact in vivo models, each offering distinct advantages and limitations for investigating specific aspects of islet biology.
1In VitroModels
In vitro systems provide controlled environments for mechanistic studies while maintaining key physiological features of islet function.
Table 1: Comparison of In Vitro Islet Model Systems
| Model System | Key Features | Applications | Limitations |
|---|---|---|---|
| Intact Isolated Islets | Maintains native cell-cell contacts and paracrine signaling; available from rodent and human sources [43] | Hormone secretion assays (static & perifusion); calcium imaging; electrophysiology [43] [45] | Limited culture duration (degranulation over time); hypoxia in large islets; removed from physiological environment [43] |
| Dispersed Islet Cells | Enables study of individual cells; facilitates cell sorting and purification [45] | Single-cell electrophysiology; heterogeneity studies; high-content screening [45] | Loss of native paracrine interactions; altered cell function after dispersion [45] |
| β-cell Pseudoislets | Human primary β-cells only; self-assembled structures [46] | Studying intrinsic β-cell function without non-β-cell influences; transplantation studies [46] | Absence of paracrine regulation from other endocrine cell types [46] |
Isolated intact islets represent the most commonly used in vitro system, preserving the native architecture and paracrine signaling among α-, β-, and δ-cells [43]. Mouse or rat islets can be routinely isolated using established protocols, while human islets have become increasingly available through programs such as the Integrated Islet Distribution Program (IIDP) and European Consortium for Islet Transplantation (ECIT) [43]. For functional studies, islets are typically cultured overnight post-isolation to recover from collagenase digestion, with rodent islets maintained in RPMI 1640 medium (11 mM glucose) and human islets in CMRL medium (5.5 mM glucose) [43].
2In VivoandIn SituModels
These models preserve the physiological context of islet function within the intact organism or tissue environment.
Table 2: In Vivo and In Situ Models for Islet Research
| Model System | Key Features | Applications | Unique Advantages |
|---|---|---|---|
| Zebrafish Embryos | Optical transparency; conserved islet development; amenable to genetic manipulation [47] | In vivo calcium imaging; developmental studies; vascular interactions [47] | High-resolution imaging of every β-cell in live animals; direct observation of functional heterogeneity [47] |
| Pancreatic Slice Preparation | Preserves islet structure within native exocrine tissue [48] | Cellular imaging in near-native environment; study of islet-exocrine interactions [48] | Maintains three-dimensional architecture and local signaling environment |
| Genetically Engineered Mouse Models | Cell-type-specific ablation; expression of sensors or actuators [46] | Role of specific cell types in glucose homeostasis; longitudinal studies [46] | Enables determination of necessity of non-β-cells for glucose regulation [46] |
The zebrafish model has emerged as particularly valuable for in vivo functional imaging due to its optical transparency and conserved islet development. Using transgenic zebrafish expressing the red fluorescent calcium indicator Rcamp1.07 under the insulin promoter (Tg(ins:Rcamp1.07)), researchers have visualized glucose-stimulated Ca²⁺ responses in individual β-cells in vivo with high-resolution two-photon, three-axis, digital scanning light-sheet microscopy (2P3A-DSLM) [47]. This approach revealed that β-cells acquire function in two waves propagating from the islet mantle to the core, coordinated by islet vascularization [47].
For mammalian systems, innovative mouse models enable specific manipulation of islet cell populations. The "non-βDTR" mouse model allows inducible diphtheria toxin-mediated ablation of adult α-, δ-, and γ-cells while preserving β-cells, creating "β-only" islets [46]. Surprisingly, these mice maintain proper glucose homeostasis and even show improved glucose tolerance and insulin sensitivity under high-fat diet conditions, challenging assumptions about the essential role of non-β-cells in insulin secretion regulation [46].
Methodologies for Functional Analysis
Hormone Secretion Assays
Static Incubation: This straightforward approach evaluates accumulated hormone release over time. Small groups of islets (10-20) are incubated with secretagogues, after which supernatant is collected for hormone measurement. Using cell strainers with mesh bottoms facilitates liquid transfer while retaining islet cells [43].
Dynamic Perifusion: This method provides superior temporal resolution of secretion kinetics, revealing the characteristic biphasic pattern of insulin secretion in response to glucose. Systems can be custom-built or commercial (e.g., Biorep Technologies) [43].
Imaging Approaches
Hormone Secretion Imaging: Three primary fluorescent sensors enable direct visualization of secretion events:
- pHluorin: A pH-sensitive GFP targeted to secretory granules; fluorescence increases during exocytosis due to luminal alkalinization [43]
- Sulforhodamine B (SRB): A fluid-phase tracer taken up during activity-dependent endocytosis; reveals Ω-shaped profiles during granule fusion using two-photon microscopy [43]
- ZIMIR: A synthetic Zn²⁺ indicator that anchors to the cell membrane; fluorescence increases upon binding Zn²⁺ co-released with insulin, revealing heterogeneous secretion patterns among β-cells [43]
Calcium Imaging: Ca²⁺ serves as a key messenger in stimulus-secretion coupling, with imaging approaches utilizing:
- Small synthetic indicators (Fluo-3, Fluo-4, Oregon Green 488 BAPTA-1) loaded as AM esters, though limited to superficial islet cells [43]
- Genetically encoded Ca²⁺ indicators (GECIs) with improved sensitivity and dynamic range, enabling long-term expression in specific cell types [43]
Diagram: Experimental Workflow for Comprehensive Islet Functional Analysis
Electrophysiological Characterization
Whole-cell patch-clamp recording in intact islets enables detailed investigation of the electrical properties that underlie hormone secretion. Using a logistic regression model incorporating 15 electrophysiological variables, researchers can identify islet cell types (α, β, or δ) with 94% accuracy without requiring genetic labeling [45]. Key distinguishing characteristics include:
- β-cells: Larger size; non-inactivating K⁺ currents; voltage-gated Na⁺ current that inactivates at hyperpolarized potentials [45]
- Non-β-cells: A-type transient K⁺ current; Na⁺ current with depolarized inactivation properties; T-type Ca²⁺ channels [45]
Signaling Pathways in Islet Cell Function
GLP-1/GIP/GCG Triagonist Signaling
Recent research has investigated unimolecular peptides targeting multiple incretin receptors simultaneously. The GLP-1/GIP/GCG receptor triagonist IUB447 enhances glucose-stimulated insulin secretion (GSIS) beyond what is achieved by co-administration of individual mono-agonists [49]. Mechanistic studies using knockout models reveal that this enhancement primarily depends on GLP-1 receptor activation and subsequent Gαq-TRPM5 signaling, rather than GIP or GCG receptor activation [49].
Diagram: GLP-1/GIP/GCG Triagonist Signaling Mechanism
Calcium Signaling in Functional Maturation
In vivo imaging in zebrafish has revealed that glucose-mediated heterogeneity of β-cell functional development occurs through calcineurin/NFAT signaling activation [47]. Increasing glucose concentrations induce functional acquisition and enhancement of β-cells via this pathway, which is conserved in mammalian systems [47]. This mechanism represents a potential strategy for promoting functional maturation of stem cell-derived β-like cells in vitro.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Islet Cell Function Studies
| Reagent Category | Specific Examples | Application/Function | Technical Notes |
|---|---|---|---|
| Calcium Indicators | Fluo-4, Oregon Green 488 BAPTA-1, Rcamp1.07 [43] [47] | Monitoring cytosolic Ca²⁺ dynamics as proxy for cell activation | Synthetic dyes for acute studies; genetically encoded for long-term expression |
| Hormone Secretion Reporters | pHluorin, ZIMIR, Sulforhodamine B [43] | Direct visualization of exocytotic events | pHluorin requires viral expression; ZIMIR labels cell surface |
| Cell Identification Markers | Anti-insulin, anti-glucagon, anti-somatostatin antibodies [45] | Immunocytochemical identification of cell types | Essential for validating functional identity post-recording |
| Receptor Agonists/Antagonists | Exendin-3(9-39) (GLP-1R antagonist), YM254890 (Gαq inhibitor) [49] | Pathway dissection and mechanistic studies | Critical for determining signaling requirements |
| Genetic Tools | Cell-specific Cre drivers, DTR expression, CRISPR/Cas9 [46] | Cell-type-specific manipulation and ablation | Enables precise functional dissection in complex tissues |
| Culture Media | RPMI 1640 (rodent), CMRL (human) [43] | Maintaining islet viability and function | Glucose concentration optimization critical for specific applications |
The comprehensive analysis of islet cell function requires integration of multiple model systems and methodological approaches. In vitro models using isolated islets provide controlled environments for detailed mechanistic studies, while in vivo models preserve the physiological context necessary for understanding systemic regulation. Advanced imaging technologies, particularly high-resolution calcium imaging in transparent zebrafish models, have revealed previously unappreciated heterogeneity in β-cell functional development and its regulation by glucose through calcineurin/NFAT signaling. Simultaneously, innovative genetic mouse models have challenged conventional wisdom about the essential role of non-β-cells in regulating insulin secretion. Together, these approaches provide complementary insights into the complex mechanisms governing hormonal regulation of blood glucose by insulin and glucagon, offering powerful tools for developing novel therapeutic strategies for diabetes.
The precise hormonal regulation of blood glucose is a cornerstone of metabolic health, primarily governed by the counterbalancing actions of insulin and glucagon. Insulin resistance and hyperglucagonemia represent two fundamental pathophysiological pillars underlying Type 2 Diabetes Mellitus (T2DM) and related metabolic disorders. Insulin resistance describes a state of reduced responsiveness of target tissues—primarily liver, skeletal muscle, and adipose tissue—to circulating insulin, necessitating compensatory hyperinsulinemia to maintain euglycemia [50]. Concurrently, hyperglucagonemia, or elevated circulating glucagon levels, inappropriately stimulates hepatic glucose production, further exacerbating hyperglycemia [51]. This dysregulation disrupts the delicate insulin-glucagon axis, leading to a progressive metabolic imbalance. The identification and validation of robust biomarkers for these conditions are therefore critical for early diagnosis, precise patient stratification, and the development of targeted therapies. This technical guide synthesizes current advances in biomarker technologies, framing them within the broader context of hormonal blood glucose regulation for a research and drug development audience.
Established and Emerging Biomarker Classes
The biomarker landscape for insulin resistance and hyperglucagonemia is rapidly evolving, moving beyond traditional measures to include sophisticated omics-derived and imaging-based signatures.
Biomarkers for Insulin Resistance
Table 1: Biomarker Classes for Assessing Insulin Resistance
| Biomarker Class | Specific Biomarker/Technique | Key Findings/Association | Performance/Accuracy |
|---|---|---|---|
| Functional Assay (Gold Standard) | Hyperinsulinemic-Euglycemic Clamp | Directly measures whole-body glucose disposal rate in response to insulin infusion. | High accuracy, but invasive, laborious, and expensive [52]. |
| Imaging Biomarkers | MRI-derived Intramyocellular Lipid (IMCL) in psoas/erector muscles | T2DM-IR associated with higher IMCL/muscle ratio in paravertebral muscles [52]. | Shows promise for non-invasive diagnosis; requires further validation [52]. |
| Epigenetic Biomarkers | Blood-based DNA methylation at 540 specific CpG sites | Classifies brain insulin resistance; many sites associated with elevated T2D risk [53]. | High accuracy (83-94%) in independent cohorts, independent of age or BMI [53]. |
| Biochemical Ratios | Triglyceride/HDL-Cholesterol Ratio | Surrogate marker of systemic IR, linked to atherosclerosis [52]. | Accessible but moderate specificity. |
| Molecular Signatures | Postprandial Multi-omics Profiling | Better predicts IR than fasting state, with hepatic enrichment; protein load strongly associated with hepatic/muscular IR [54]. | Provides a dynamic and tissue-specific assessment. |
Biomarkers for Hyperglucagonemia and Glucagon Signaling
Direct measurement of circulating glucagon is challenging due to assay variability and its rapid degradation. Therefore, research often focuses on functional assessments of glucagon action and associated molecular signatures.
- Glucagon Receptor (GCGR) Signaling Analysis: Hepatic GCGR engagement activates dual intracellular cascades: the canonical Gs/cAMP/PKA pathway and the Gq/Ca2+ pathway, leading to increased glycogenolysis and gluconeogenesis [51]. Dysregulation in this signaling network is a marker of glucagon pathway dysfunction.
- Amino Acid Levels: Hyperglucagonemia is closely linked to amino acid metabolism. Elevated circulating levels of certain amino acids, particularly alanine and arginine, can stimulate glucagon secretion. Conversely, hyperaminoacidemia is observed when hepatic glucagon signaling is inhibited, forming a liver-α-cell axis [51].
- Islet and Gut Hormone Dynamics: Dynamic multi-omics profiling after varied nutritional challenges reveals distinct secretion patterns for glucagon, insulin, GLP-1, and GIP. The interplay between these hormones and other postprandial biomolecules provides a rich signature for identifying dysregulation, such as the inappropriate glucagon secretion after glucose ingestion seen in T2DM [54].
Experimental Methodologies for Biomarker Investigation
Protocol: Hyperinsulinemic-Euglycemic Clamp
The clamp technique is the reference method for quantifying whole-body insulin sensitivity in vivo [52].
- Principle: Co-administration of a fixed, continuous insulin infusion and a variable glucose infusion to maintain basal plasma glucose levels at euglycemia.
- Procedure:
- After an overnight fast, an intravenous catheter is inserted for insulin and glucose infusion. A second catheter is placed in a contralateral vein for frequent blood sampling.
- A primed, continuous intravenous infusion of insulin (e.g., 40 mU/m²/min) is initiated to raise plasma insulin to a predetermined super-physiological level.
- Simultaneously, a variable 20% glucose infusion is started and adjusted every 5-10 minutes based on frequent (e.g., every 5 min) plasma glucose measurements to "clamp" the glucose level at the fasting concentration (~5.0 mmol/L).
- The clamp is maintained for a minimum of 120 minutes until a steady state is achieved.
- Data Analysis: The glucose infusion rate (GIR) required to maintain euglycemia during the final 30 minutes of the clamp is calculated. The GIR is a direct measure of whole-body insulin sensitivity; a lower GIR indicates greater insulin resistance.
Protocol: Multiparametric MRI for Ectopic Lipid Quantification
This non-invasive method quantifies ectopic fat deposition in skeletal muscle as a proxy for insulin resistance [52].
- Principle: Uses quantitative Dixon (Q-Dixon) and diffusion MRI protocols to differentiate and quantify fat and water signals within tissues.
- Procedure:
- Participants are positioned in an MRI scanner (e.g., 3T). The region of interest (e.g., L4-L5 paravertebral muscles) is identified.
- A Q-Dixon sequence is acquired. This technique acquires multiple echoes, allowing for the precise separation of fat and water signals and the calculation of a fat fraction map.
- The data is processed to segment the specific muscles (psoas, erector spinae, multifidus).
- Data Analysis: For each muscle, the following are quantified:
- Intramyocellular Lipid (IMCL): Fat stored within muscle cells.
- Extramyocellular Lipid (EMCL): Fat stored between muscle cells.
- Total Fat Content/Muscle Ratio: The overall fat fraction within the muscle region. Higher IMCL and total fat ratios are correlated with insulin resistance [52].
Protocol: Epigenetic Signature Analysis for Brain Insulin Resistance
This methodology identifies blood-based DNA methylation signatures reflective of central insulin resistance [53].
- Principle: Machine learning is used to correlate DNA methylation patterns in blood with brain insulin sensitivity, measured via functional neuroimaging.
- Procedure:
- Cohort Selection: Study participants without T2D, stratified by brain insulin response but with similar peripheral insulin sensitivity.
- Data Acquisition:
- Blood Collection: Blood samples are drawn for DNA extraction.
- Brain Imaging: Functional Magnetic Resonance Spectroscopy (fMRS) or Positron Emission Tomography (PET) is used to quantify brain insulin sensitivity.
- DNA Methylation Analysis: DNA is treated with bisulfite, which converts unmethylated cytosines to uracils. Genome-wide methylation analysis is performed (e.g., using microarrays or sequencing).
- Data Analysis:
- Methylation data from the discovery cohort is integrated with imaging and metabolic data using a machine learning workflow.
- Specific CpG sites with differential methylation patterns between individuals with and without brain insulin resistance are identified.
- The signature is validated for accuracy in independent replication cohorts [53].
Signaling Pathways and Experimental Workflows
Insulin and Glucagon Receptor Signaling Crosstalk
This diagram illustrates the antagonistic signaling pathways of insulin and glucagon in a hepatocyte. Insulin promotes anabolic processes via the AKT pathway, leading to increased glucose uptake and glycogen synthesis [50]. Glucagon triggers catabolic processes primarily through the Gs/cAMP/PKA pathway, stimulating gluconeogenesis and glycogenolysis [51]. Dysregulation of these pathways is central to insulin resistance and hyperglucagonemia.
Multi-omics Profiling Workflow for Hormonal Dysregulation
This workflow outlines a dynamic multi-omics approach to study postprandial hormonal responses and identify biomarkers [54]. Participants undergo nutritional challenges, followed by serial blood collection. The resulting samples are subjected to comprehensive molecular profiling, and the integrated data is analyzed using machine learning to elucidate hormone-metabolite interactions and their relationship with tissue-specific insulin resistance.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 2: Essential Research Reagents for Investigating Insulin Resistance and Hyperglucagonemia
| Research Reagent / Material | Function and Application in Research |
|---|---|
| Stable Isotope Tracers | Enable precise tracking of glucose flux, gluconeogenesis, and lipid kinetics in vivo during clamp studies or meal tests. |
| ELISA/Multiplex Immunoassay Kits | For the specific and quantitative measurement of hormones (Insulin, Glucagon, GLP-1, GIP, etc.) and cytokines in plasma/serum. |
| DNA Methylation Analysis Kits | For bisulfite conversion of DNA and subsequent genome-wide (e.g., EPIC array) or targeted (e.g., pyrosequencing) methylation analysis [53]. |
| GLP-1 Receptor Agonists (GLP-1RAs) & GCGR Agonists/Antagonists | Pharmacological tools (e.g., Exenatide, Liraglutide, synthetic glucagon) to probe receptor function and signaling in cellular and animal models [51] [10]. |
| PCR and qRT-PCR Reagents | For gene expression analysis of key targets in insulin and glucagon signaling pathways (e.g., Pck1, G6pc, IRS1, PPARGC1A) [51]. |
| Cell Culture Models | Primary hepatocytes, myocytes, adipocytes, and immortalized cell lines (e.g., HepG2, L6, 3T3-L1) for in vitro studies of insulin/glucagon action. |
| Animal Models | Genetically modified mice (e.g., ob/ob, db/db, GCGR-/-) and diet-induced obese (DIO) mice to study disease pathophysiology and therapeutic efficacy. |
The field of biomarker discovery for insulin resistance and hyperglucagonemia is advancing rapidly, driven by sophisticated technologies that move beyond static, single-analyte measurements. The integration of dynamic functional assessments like the clamp, non-invasive imaging of ectopic fat, and high-dimensional molecular data from epigenomics and multi-omics profiling provides a more holistic and granular view of dysregulation in the insulin-glucagon axis. These biomarkers are not merely diagnostic; they offer profound insights into the underlying pathophysiology, enabling patient stratification and paving the way for personalized therapeutic interventions. As these tools are refined and validated in larger, diverse cohorts, they hold the promise of transforming the management of T2DM and related metabolic disorders by targeting the specific molecular drivers of disease in individual patients.
The precise hormonal regulation of blood glucose is a cornerstone of metabolic health, primarily governed by the counter-balancing actions of insulin and glucagon. For decades, the therapeutic focus for conditions like diabetes centered on insulin replacement or sensitization. However, a profound shift has occurred with the recognition that glucagon and glucagon-related peptides offer equally potent therapeutic avenues. This whitepaper provides an in-depth technical review of two critical and expanding classes of therapeutics: emergency glucagon for acute hypoglycemia and glucagon-like peptide-1 receptor agonists (GLP-1RAs) for chronic metabolic diseases. Framed within the context of the "glucagonocentric hypothesis" of metabolic disease, this review details the molecular mechanisms, clinical applications, and experimental methodologies underpinning these therapies, providing a essential resource for researchers and drug development professionals [5] [10].
Glucagon: From Emergency Hormone to Therapeutic Agent
Molecular Mechanisms and Physiological Roles
Glucagon is a 29-amino acid polypeptide hormone secreted by pancreatic α-cells. Its primary role is to counteract hypoglycemia by promoting hepatic glucose production [55] [5].
- Mechanism of Action: Glucagon binds to a specific G-protein–coupled surface receptor (GCGR), predominantly expressed in the liver. This binding activates adenylate cyclase, increasing intracellular cyclic adenosine monophosphate (cAMP) levels. Elevated cAMP stimulates protein kinase A (PKA), which in turn triggers the activation of enzymes critical for glycogenolysis and gluconeogenesis, resulting in the release of glucose into the bloodstream [55].
- Beyond Glycemic Control: Emerging research highlights glucagon's role in systemic energy balance. It suppresses appetite via the liver–vagal nerve–hypothalamic axis, promotes lipolysis and fat oxidation, stimulates hepatic amino acid catabolism and ureagenesis, and induces thermogenesis in brown adipose tissue [5].
The following diagram illustrates the core signaling pathway of glucagon and the opposing pathway of GLP-1R agonism.
FDA-Approved and Emerging Therapeutic Applications
Glucagon's therapeutic use is bifurcated into established emergency applications and novel diagnostic/off-label uses.
Table 1: Glucagon Formulations and Approved Indications
| Formulation | Route of Administration | Strength | Primary Indication | Dosing Guidelines |
|---|---|---|---|---|
| Glucagon Emergency Kit | IM, SC, IV (after reconstitution) | 1 mg | Severe Hypoglycemia | 1 mg (≥25 kg); 0.5 mg (<25 kg or young children); repeat after 15 min if needed [55] [56] |
| Gvoke (pre-filled syringe/auto-injector) | SC | 0.5 mg/0.1 mL, 1 mg/0.2 mL | Severe Hypoglycemia | 1 mg (adults & children ≥12 yrs); 0.5 mg (children 2-<12 yrs & <45 kg) [56] [57] |
| BAQSIMI (nasal powder) | Intranasal | 3 mg | Severe Hypoglycemia | Single 3 mg dose administered into one nostril [55] [57] |
| Glucagon (Diagnostic) | IV, IM | 0.25 - 2 mg | Radiologic Examinations | IV: 0.25-2 mg; IM: 1-2 mg to induce gastrointestinal hypotonia [55] |
- Severe Hypoglycemia: Glucagon is a life-saving intervention for severe hypoglycemia in individuals with diabetes who cannot safely consume oral carbohydrates. Its key advantage is the ability to be administered without patent IV access, making it suitable for layperson use in community settings [55] [57]. Per Memorial Sloan Kettering guidelines, after administration, the patient should be positioned on their side and, upon regaining consciousness, should consume oral carbohydrates to stabilize blood glucose levels [57].
- Off-Label and Emerging Uses:
- Beta-Blocker and Calcium Channel Blocker Overdose: High-dose glucagon infusion serves as an inotropic and chronotropic agent in overdoses that are refractory to standard therapies, due to its ability to increase cardiac cAMP [55].
- Esophageal Food Impaction: Glucagon's smooth muscle relaxant properties can facilitate the passage of an obstructed food bolus [55].
- Metabolic Diseases: Research is exploring glucagon's potential in treating conditions like Non-Alcoholic Fatty Liver Disease (NAFLD) and obesity, leveraging its effects on lipid oxidation and energy expenditure [5].
GLP-1 Receptor Agonists: Rewriting the Treatment of Metabolic Disease
From Incretin Hormone to Blockbuster Therapeutics
Glucagon-like peptide-1 (GLP-1) is an incretin hormone derived from the post-translational processing of proglucagon, primarily synthesized in intestinal L-cells. Its primary physiological actions include glucose-dependent insulin secretion, suppression of glucagon release, slowing of gastric emptying, and promotion of satiety [58] [10]. The native hormone has an extremely short half-life (~1-2 minutes) due to rapid degradation by dipeptidyl peptidase-IV (DPP-4) [10]. GLP-1 receptor agonists (GLP-1RAs) are engineered analogs that resist DPP-4 degradation, providing a prolonged and potent pharmacological effect [58].
Table 2: Select GLP-1 Receptor Agonists in Clinical Use
| Drug (Brand Name) | Mechanism | Dosing Frequency | Key Indications | Notable Efficacy Data |
|---|---|---|---|---|
| Liraglutide (Victoza) | GLP-1RA | Once Daily | T2D, Obesity | Significant weight loss and glycemic improvement [58]. |
| Semaglutide (Ozempic, Wegovy) | GLP-1RA | Once Weekly | T2D, Obesity | In a meta-analysis, 2.4 mg weekly demonstrated -12.4% body weight vs -1.2% with placebo [59]. |
| Tirzepatide (Mounjaro) | GLP-1/GIP Dual Agonist | Once Weekly | T2D | In a meta-analysis, 15 mg weekly achieved -11.09% body weight in T2D patients and superior HbA1c reduction vs. all GLP-1RAs [59]. |
| Retatrutide (In development) | GLP-1/GCG/GIP Triple Agonist | Once Weekly | Obesity (Phase 3) | In a meta-analysis, 12 mg weekly demonstrated -26.56% body weight, the most pronounced effect reported [59]. |
Multi-System Therapeutic Applications and Mechanisms
The therapeutic impact of GLP-1RAs extends far beyond glycemic and weight control, demonstrating pleiotropic effects across multiple organ systems.
- Cardiovascular Benefits: GLP-1RAs have demonstrated significant cardioprotective effects in large cardiovascular outcome trials (CVOTs). They reduce major adverse cardiovascular events (MACE), improve endothelial function, and have been shown to reduce risks of heart failure, atherosclerosis, and hypertension [58] [10]. The proposed mechanisms include direct effects on the vascular endothelium, reduction of systemic inflammation, and improvement in lipid profiles.
- Neuroprotection: GLP-1 receptors are expressed in the brain, and GLP-1RAs show promise in slowing the progression of neurodegenerative diseases like Alzheimer's and Parkinson's. Mechanisms involve reducing neuroinflammation, attenuating oxidative stress, promoting synaptic plasticity, and mitigating amyloid-beta and tau pathology in Alzheimer's models [10].
- Renal and Hepatic Benefits: Clinical trials indicate that GLP-1RAs can delay the progression of diabetic kidney disease by reducing albuminuria. Furthermore, through their effects on weight loss and insulin sensitization, they are being actively investigated for the treatment of Non-Alcoholic Fatty Liver Disease (NAFLD) and its more severe form, non-alcoholic steatohepatitis (NASH) [58] [10].
The diagram below maps the multi-organ signaling and physiological effects of GLP-1 receptor activation.
Experimental Protocols and Research Methodologies
In Vivo Protocol for Assessing a Novel "Smart Insulin" in a Rodent Model
The following protocol is adapted from recent research on a glucose-responsive fusion protein combining insulin and glucagon actions, evaluated in a Type 1 diabetic rat model [60].
- Objective: To evaluate the efficacy and stability of a novel insulin-glucagon fusion protein in maintaining euglycemia and reducing hypoglycemic events in a chemically-induced (e.g., streptozotocin, STZ) Type 1 diabetic rat model.
- Materials:
- Animals: Adult Sprague-Dawley rats.
- Disease Model Induction: Streptozotocin (STZ) dissolved in citrate buffer, injected intraperitoneally to ablate pancreatic β-cells.
- Test Article: Lyophilized powder of the insulin-glucagon fusion protein, reconstituted in sterile solvent.
- Control Articles: Conventional insulin (e.g., human insulin), vehicle control.
- Equipment: Subcutaneous infusion pumps, blood glucose monitoring system, refrigeration for standard insulin storage.
- Methodology:
- Induction and Confirmation of Diabetes: Administer STZ. Monitor blood glucose for 72-96 hours. Confirm diabetes with sustained hyperglycemia (blood glucose >250 mg/dL).
- Treatment Administration:
- Randomize diabetic rats into treatment groups: Fusion Protein, Conventional Insulin, and Vehicle.
- Administer treatments via a single subcutaneous injection or continuous infusion via pump.
- For the stability assessment, pre-reconstitute the fusion protein and store it at room temperature for several weeks prior to administration to a subgroup of animals.
- Glucose Monitoring:
- Measure blood glucose levels at frequent intervals (e.g., every 15-30 minutes initially, then hourly) over a 12-24 hour period.
- Perform an insulin tolerance test by fasting animals and administering a standard insulin dose to challenge the system and assess the counter-regulatory (hypoglycemia-protective) effect of the glucagon component.
- Endpoint Analysis:
- Primary: Percentage of time in euglycemic range (e.g., 70-180 mg/dL).
- Secondary: Incidence of hypoglycemia (blood glucose <70 mg/dL), area under the curve (AUC) for glucose levels, and stability of the fusion protein as determined by HPLC post-recovery from storage.
- Data Interpretation: The fusion protein is considered superior if it demonstrates a significant reduction in hypoglycemic events and a greater percentage of time in the euglycemic range compared to conventional insulin, without compromising overall glycemic control.
In Vitro Protocol for GLP-1RA Signaling and Satiety Pathway Analysis
This protocol outlines the methodology for investigating the molecular pathways of GLP-1RAs in neuronal models of satiety.
- Objective: To delineate the cAMP-dependent and -independent signaling pathways activated by GLP-1RAs in a hypothalamic neuronal cell line and their link to expression of satiety neurotransmitters.
- Materials:
- Cell Line: Immortalized mouse hypothalamic neurons (e.g., mHypoA-2/10).
- Test Compounds: GLP-1RAs (e.g., Liraglutide, Semaglutide), GLP-1R antagonist (e.g., Exendin(9-39)), PKA inhibitor (e.g., H-89), Epac inhibitor (e.g., ESI-09).
- Assay Kits: cAMP ELISA kit, Western Blot reagents for p-CREB and c-Fos, qPCR reagents for POMC and CART.
- Methodology:
- Cell Culture and Treatment: Maintain cells in high-glucose DMEM. Serum-starve cells before treatment. Pre-treat cells with inhibitors for 1 hour before adding GLP-1RAs for defined durations (e.g., 15 min for phosphorylation studies, 4-6 hours for gene expression).
- cAMP Measurement: Lyse cells after 15-minute GLP-1RA exposure. Quantify intracellular cAMP levels using a competitive ELISA kit according to the manufacturer's protocol.
- Western Blot Analysis: Resolve proteins from cell lysates via SDS-PAGE. Transfer to membranes and probe with antibodies against p-CREB (Ser133), total CREB, c-Fos, and β-actin (loading control).
- Gene Expression Analysis (qPCR): Extract total RNA after 4 hours of GLP-1RA treatment. Synthesize cDNA and perform qPCR with primers for POMC and CART, using GAPDH as a housekeeping gene.
- Data Interpretation: A successful GLP-1RA response will show a significant, dose-dependent increase in cAMP, phosphorylation of CREB, and upregulation of POMC and CART mRNA. The use of pathway-specific inhibitors will determine the relative contributions of PKA and Epac to these effects.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Hormone and GLP-1RA Research
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| Streptozotocin (STZ) | Chemical agent for selective ablation of pancreatic β-cells. | Induction of experimental Type 1 diabetes in rodent models to test efficacy of new insulins or glucagon formulations [60]. |
| cAMP ELISA Kit | Quantifies intracellular cyclic AMP (cAMP) concentrations. | Measuring proximal GLP-1R or GCGR activation in cell-based assays after agonist stimulation [55] [5]. |
| GLP-1R Antagonists (e.g., Exendin(9-39)) | Competitively blocks the GLP-1 receptor. | Confirming that observed effects of a test compound are specifically mediated through the GLP-1 receptor (mechanism confirmation) [10]. |
| Phospho-Specific Antibodies (e.g., p-CREB) | Detects activated, phosphorylated forms of signaling proteins. | Analyzing downstream signaling pathway activation (e.g., cAMP/PKA/CREB) via Western Blot or immunohistochemistry. |
| Hypothalamic Neuronal Cell Lines | In vitro model of central appetite regulation. | Investigating the molecular mechanisms of GLP-1RA-induced satiety and gene expression changes (POMC, CART) [5] [10]. |
| Dipeptidyl Peptidase-4 (DPP-4) | Proteolytic enzyme that degrades native GLP-1. | Testing the stability and half-life of novel GLP-1 analogs in plasma or buffer solutions [10]. |
The therapeutic landscape of hormonal blood glucose regulation has evolved from the singular focus on insulin replacement to a sophisticated, multi-targeted approach. Emergency glucagon remains an irreplaceable, life-saving tool for acute hypoglycemia, with new formulations improving its usability and accessibility. Concurrently, the rise of GLP-1 receptor agonists represents a paradigm shift, offering multi-system benefits for chronic metabolic, cardiovascular, and potentially neurodegenerative diseases. The frontier continues to expand with the development of dual and triple agonists that co-target the receptors for GLP-1, GIP, and glucagon, promising unprecedented efficacy. For researchers and drug developers, this field offers rich opportunities to build upon these mechanisms, innovate in drug design and delivery, and translate these advances into novel therapies for a growing global patient population.
The precise regulation of blood glucose is a fundamental physiological process, centrally governed by the counterbalancing actions of insulin and glucagon. While insulin's role in facilitating glucose clearance is well-established, glucagon—a 29-amino-acid peptide hormone secreted by pancreatic alpha cells—serves as the primary hyperglycemic hormone, opposing insulin's effects [61] [62]. Its discovery in the 1920s identified a pancreatic factor capable of raising blood sugar, leading to its naming as a "GLUCose-AGONist" [62]. Glucagon exerts its biological actions primarily by binding to the glucagon receptor (GCGR), a class B G protein-coupled receptor (GPCR) predominantly expressed on the surface of liver cells [62] [63]. Activation of hepatic GCGR signaling is a key driver of gluconeogenesis and glycogenolysis, especially during fasting or hypoglycemic conditions [61] [63]. Consequently, the GCGR has emerged as a compelling therapeutic target for metabolic diseases, with strategies exploring both receptor antagonism to suppress excessive hepatic glucose production and receptor agonism to exploit other beneficial metabolic effects.
Glucagon Receptor Antagonism for Hyperglycemia Management
Mechanism of Action and Therapeutic Rationale
In type 2 diabetes mellitus (T2DM), a pathological hypersecretion of glucagon is frequently observed, which contributes significantly to fasting and postprandial hyperglycemia through an unchecked increase in hepatic glucose output [61] [62] [64]. This understanding forms the basis of the "bihormonal hypothesis" of diabetes [62]. Glucagon receptor antagonists (GRAs) are small-molecule compounds designed to bind to the GCGR without activating it, thereby blocking the binding of native glucagon and its subsequent signal transduction pathway [61] [64]. By inhibiting GCGR activation, these antagonists directly reduce the rate of glycogenolysis and gluconeogenesis in the liver, leading to a decrease in endogenous glucose production and a consequent lowering of blood glucose concentrations [61] [64].
Table 1: Selected Glucagon Receptor Antagonists in Clinical Development
| Compound Name | Clinical Stage (as of 2024) | Reported HbA1c Reduction | Key Findings and Adverse Effects |
|---|---|---|---|
| LY2409021 | Phase 2 (Development ceased) | ~1.5% after 12 weeks [61] | Lowered fasting & postprandial glucose; associated with elevated liver enzymes (ALT), increased hepatic fat, hyperglucagonemia, and elevated blood pressure & cholesterol [61]. |
| MK-0893 | Phase 2 | ~1.5% at 80 mg dose for 12 weeks [65] | Effective in reducing hyperglycemia; dose-dependent elevation of LDL-cholesterol linked to increased cholesterol absorption [65]. |
| LGD-6972 | Phase 2 | Not Specified in Sources | Similar to other GRAs, associated with increased hepatic lipid content and hyperglucagonemia [61]. |
Experimental Protocols for GRA Investigation
In Vivo Efficacy and Safety Assessment: A standard protocol for evaluating GRA efficacy involves randomized, placebo-controlled trials in patients with T2DM over 12 to 24 weeks. Key measurements include changes from baseline in hemoglobin A1c (HbA1c), fasting plasma glucose, and postprandial glucose levels [61] [65]. Safety monitoring is critical and must include regular measurement of liver enzymes (alanine aminotransferase, ALT, and aspartate aminotransferase, AST), assessment of hepatic fat fraction via imaging (e.g., MRI-PDFF), and monitoring of lipid panels (especially LDL-cholesterol) [61]. For instance, a study with LY2409021 demonstrated significant HbA1c reduction over 6 months but was halted due to consistent, albeit transient, elevations in ALT and hepatic fat [61].
Mechanistic Study on LDL-Cholesterol Elevation: To investigate the mechanism behind GRA-induced dyslipidemia, as seen with MK-0893, a mouse model can be employed. The protocol involves [65]:
- Treatment: Administer the GRA to diabetic or diet-induced obese mice.
- Measurement: Track plasma LDL-cholesterol levels over time.
- Pathway Analysis: Measure plasma levels of glucagon-like peptide-2 (GLP-2), a hormone known to increase cholesterol absorption.
- Co-administration: To confirm the mechanism, co-administer ezetimibe, a cholesterol absorption inhibitor, with the GRA. The abrogation of the LDL-c increase by ezetimibe supports the hypothesis that the effect is mediated via increased cholesterol absorption [65].
Glucagon Receptor Agonism and the Promise of Multi-Agonists
The Dual and Triple Agonism Approach
Paradoxically, while blocking glucagon action is beneficial for glucose control, activating the GCGR pathway is also being therapeutically exploited, particularly in the context of energy expenditure and weight loss. This strategy often involves co-activating the GCGR with other related receptors to create a balanced and synergistic metabolic effect. The development of unimolecular dual and triple agonists represents a significant advancement in pharmacotherapy for obesity and T2DM [66] [10]. These agents are engineered to activate multiple hormone receptors simultaneously, harnessing the benefits of each.
- GLP-1/Glucagon Co-agonists: Glucagon activation is leveraged to promote significant weight loss through increased energy expenditure and satiety, while the GLP-1 component counteracts glucagon's hyperglycemic effect by improving glycemia and stimulating insulin secretion [66].
- GLP-1/GIP/Glucagon Tri-agonists: Adding glucose-dependent insulinotropic polypeptide (GIP) receptor activation to GLP-1 and glucagon agonism has shown unprecedented efficacy in preclinical models. The triple agonist retatrutide (targeting GLP-1R, GIPR, and GCGR) has demonstrated profound weight loss effects in phase 2 trials [10].
Table 2: Properties of Glucagon-Containing Multi-Agonists
| Agent Type | Targeted Receptors | Primary Therapeutic Goal | Key Metabolic Effects |
|---|---|---|---|
| GLP-1/Glucagon Co-agonist | GLP-1R, GCGR | Weight loss, improved glycemic control | ↑ Satiety (GLP-1), ↑ Energy expenditure (Glucagon), ↑ Insulin secretion (GLP-1), ↓ Hyperglycemia (GLP-1 counteracts Glucagon) [66]. |
| GLP-1/GIP/Glucagon Tri-agonist | GLP-1R, GIPR, GCGR | Superior weight loss and metabolic improvement | Enhanced weight loss beyond dual agonists, improved insulin secretion, dysglycemia, satiety, and energy expenditure [66] [10]. |
Signaling Pathways of Glucagon and Related Receptors
The glucagon receptor signals primarily through the Gs protein pathway. Upon binding, the activated Gs alpha subunit stimulates adenylate cyclase, which catalyzes the conversion of ATP to cyclic adenosine monophosphate (cAMP). The resulting elevated cAMP levels activate protein kinase A (PKA), which in turn phosphorylates key enzymes [66] [63]. This cascade leads to the activation of glycogen phosphorylase (promoting glycogenolysis) and the inhibition of glycogen synthase, ultimately increasing hepatic glucose output [63]. A secondary, cAMP-independent pathway involving Gq protein activation and intracellular calcium release can also contribute to regulating gluconeogenic genes [63]. In contrast, the GLP-1 receptor, while also a Gs-coupled GPCR, exhibits a unique resistance to desensitization, enabling it to produce robust and prolonged cAMP signals, which is a key feature for its therapeutic success [66].
Diagram 1: Core signaling of glucagon receptors.
Experimental Protocol for Evaluating Agonists in Aging
Emerging research links glucagon signaling to healthy aging. A protocol to test the effect of a long-acting glucagon agonist in aging mice involves [67]:
- Animal Model: Utilize aged mice (e.g., 20 months old).
- Intervention: Treat mice with a long-acting glucagon agonist versus a vehicle control over a defined period.
- Outcome Measures:
- Molecular: Analyze liver and muscle tissues to measure the suppression of established aging-related pathways (e.g., using RNA sequencing or Western blot).
- Functional: Conduct metabolic tests (e.g., glucose tolerance tests) to assess overall metabolic health.
- Lifespan: In long-term studies, track survival to determine if treatment extends lifespan compared to controls [67].
Challenges and Future Directions
The therapeutic targeting of the GCGR is not without significant challenges. For antagonists, the most prominent hurdles include hepatic steatosis (increased liver fat) and elevated transaminase levels, as observed with multiple compounds like LY2409021 and PF-06291874 [61]. Furthermore, hyperglucagonemia due to feedback mechanisms, alpha-cell hyperplasia in preclinical models, and dyslipidemia (increased LDL-cholesterol) present serious clinical obstacles [61] [65]. The latter has been mechanistically linked to increased cholesterol absorption mediated via elevated GLP-2 [65].
Future work must focus on elucidating the precise mechanisms underlying these adverse effects, potentially through the development of biased agonists that selectively activate beneficial downstream pathways (e.g., those governing amino acid metabolism) while avoiding those leading to steatosis and dyslipidemia [62]. The concept of hepatic glucagon resistance, a state where the liver becomes less responsive to glucagon's action, also requires further delineation for its role in metabolic disease [62]. Finally, the promising applications of glucagon agonism in multi-agonist therapies for obesity and potentially even in slowing the aging process will continue to be an area of intense research and clinical interest [66] [67].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Glucagon Receptor Research
| Reagent / Tool | Function and Application | Example Use-Case |
|---|---|---|
| Small-Molecule GCGR Antagonists (e.g., MK-0893, LY2409021) | Pharmacologically inhibit glucagon receptor signaling to study glucose homeostasis and lipid metabolism. | In vivo proof-of-concept studies in diabetic rodent models to assess efficacy and side effects like LDL-c elevation [61] [65]. |
| Glucagon Receptor Knockout (Gcgr-/-) Mice | Genetic model to study the systemic physiological role of glucagon signaling absent of developmental compensation. | Investigating the necessity of glucagon signaling for calorie restriction-induced healthspan improvements [67]. |
| GLP-1/Glucagon Co-Agonists & Tri-Agonists | Unimolecular peptides that activate multiple incretin receptors to study synergistic metabolic effects. | Preclinical evaluation of weight loss, glycemic control, and energy expenditure in metabolic syndrome models [66] [10]. |
| DPP-4 Inhibitors | Inhibit the dipeptidyl peptidase-4 enzyme, which rapidly degrades native glucagon and GLP-1, prolonging their half-life. | Used in mechanistic studies to stabilize endogenous glucagon and observe prolonged effects [68]. |
| Ezetimibe | Potent inhibitor of cholesterol absorption in the gut. | Mechanistic tool to confirm if GRA-induced LDL-c elevation is mediated via increased cholesterol absorption [65]. |
| Glucagon ELISA Kits | Accurately measure plasma glucagon levels via immunoassay. | Essential for documenting hyperglucagonemia in disease models or in response to GRA treatment [61] [62]. |
Pathophysiology and Management of Hormonal Dysregulation in Metabolic Disease
Type 2 diabetes (T2D) represents a complex endocrine disorder characterized by dysfunctional hormonal regulation beyond the traditional insulin-centric model. This technical review deconstructs the pathophysiology of T2D through the integrated lens of insulin deficiency, insulin resistance, and the paradoxical state of hyperglucagonemia. We examine the molecular mechanisms through which glucagon excess contributes to hyperglycemia, the failure of normal feedback inhibition on pancreatic α-cells, and the emerging therapeutic strategies targeting glucagon signaling. The evidence supports a bihormonal or "glucagonocentric" hypothesis, wherein glucagon plays an indispensable role in the metabolic manifestations of diabetes. This synthesis provides researchers and drug development professionals with a refined framework for understanding disease pathogenesis and developing targeted interventions.
The understanding of diabetes mellitus has evolved substantially from early models focused exclusively on insulin deficiency. The traditional insulinocentric theory posited that a lack of insulin secretion was solely responsible for all metabolic derangements in diabetes [69]. While this framework successfully explained the pathophysiology of type 1 diabetes (T1D), it provided an incomplete picture of T2D, where insulin levels may be normal or even elevated [70].
The bihormonal abnormality theory, first comprehensively proposed by Unger et al. in the 1970s, introduced glucagon as a key counter-regulatory hormone whose dysregulation is fundamental to the diabetic state [69] [71]. This model recognizes that both absolute insulin deficiency and relative glucagon excess drive the metabolic disruptions characteristic of diabetes. More recently, evidence from genetic and pharmacological studies has led to the glucagonocentric hypothesis, which suggests that hyperglucagonemia is not merely a consequence but a primary driver of diabetic hyperglycemia, essential for the development of both T1D and T2D [69] [5].
Pathophysiological Framework: The Triad of Dysfunction
Insulin Deficiency and β-Cell Dysfunction
In T2D, insulin deficiency results from both functional impairment and potential reduction in β-cell mass [72]. The progression typically begins with compensatory hyperinsulinemia in response to insulin resistance, where β-cells increase insulin output to maintain normoglycemia [73] [74]. Over time, this compensatory mechanism fails due to:
- Glucolipotoxicity: Chronic exposure to elevated glucose and free fatty acids impairs β-cell function and induces apoptosis [74].
- β-Cell Dedifferentiation: Evidence suggests that β-cells may lose their mature identity under metabolic stress, reverting to progenitor-like states with reduced insulin production [72].
- Transcription Factor Alterations: Changes in the expression of key transcription factors (e.g., FOXO1) disrupt the regulatory networks maintaining β-cell identity and function [72].
Table 1: Stages of β-Cell Decline in Type 2 Diabetes
| Stage | β-Cell Function | Insulin Secretion | Glucose Homeostasis |
|---|---|---|---|
| Compensation | Normal or enhanced | Hyperinsulinemia | Normal |
| Adaptation | Early dysfunction | Elevated but inadequate | Prediabetes |
| Decompensation | Significant dysfunction | Insufficient | Overt diabetes |
Insulin Resistance: Systemic Metabolic Dysregulation
Insulin resistance represents an impaired biological response to insulin stimulation in target tissues, primarily liver, skeletal muscle, and adipose tissue [74]. The etiology includes both acquired factors (e.g., obesity, physical inactivity) and genetic predispositions [73] [74].
The pathophysiology involves:
- Skeletal Muscle: Intramyocellular accumulation of diacylglycerol activates protein kinase C theta (PKC-θ), impairing proximal insulin signaling and reducing GLUT4-mediated glucose uptake [74].
- Liver: Hepatic diacylglycerol activates protein kinase C epsilon (PKC-ε), disrupting insulin receptor signaling and resulting in uncontrolled gluconeogenesis and de novo lipogenesis [74].
- Adipose Tissue: Insulin-resistant adipose tissue exhibits reduced suppression of lipolysis, increasing circulating free fatty acids (FFAs) that further exacerbate hepatic and muscle insulin resistance [74].
Table 2: Tissue-Specific Manifestations of Insulin Resistance
| Tissue | Primary Defect | Metabolic Consequences |
|---|---|---|
| Skeletal Muscle | Reduced GLUT4 translocation | Decreased glucose disposal (~70% of postprandial glucose uptake) |
| Liver | Unsuppressed gluconeogenesis & glycogenolysis | Increased hepatic glucose output |
| Adipose Tissue | Increased lipolysis | Elevated circulating FFAs, ectopic fat deposition |
Paradoxical Hyperglucagonemia: The Alpha Cell Dysregulation
Despite hyperglycemia, individuals with T2D exhibit paradoxical hyperglucagonemia - inappropriately elevated glucagon levels that contribute significantly to fasting and postprandial hyperglycemia [71]. This phenomenon represents a fundamental breakdown in the normal feedback regulation of α-cells.
The mechanisms underlying α-cell dysregulation include:
- Impaired Paracrine Signaling: Loss of insulin's inhibitory effect on α-cells is a primary defect. In T2D, insulin resistance extends to α-cells, diminishing their ability to suppress glucagon secretion in response to hyperglycemia [5] [71].
- Somatostatin Deficiency: Reduced δ-cell secretion of somatostatin, a potent inhibitor of glucagon release, further contributes to α-cell overactivity [71].
- Intraislet Defects: Altered levels of other paracrine factors (e.g., zinc, GABA) normally co-secreted with insulin may disrupt the delicate balance of islet cell cross-talk [5] [71].
- Nutrient Sensing Dysregulation: α-cells in diabetic states show altered response to glucose and amino acids, failing to appropriately adjust secretion to metabolic needs [5].
Molecular Signaling Pathways
Insulin Signaling and Resistance Mechanisms
The following diagram illustrates the normal insulin signaling pathway and the key points of disruption in insulin resistance:
Diagram 1: Insulin signaling pathway and resistance mechanisms.
Glucagon Signaling and Hepatic Glucose Production
The molecular pathway through which glucagon regulates hepatic glucose metabolism involves:
Diagram 2: Glucagon signaling and hepatic glucose production pathway.
Experimental Models and Methodologies
Key Experimental Evidence
Critical insights into the role of glucagon in diabetes pathogenesis come from well-defined experimental models:
Glucagon Receptor Knockout (Gcgr⁻/⁻) Studies:
- Methodology: Global knockout mice lacking functional glucagon receptors are generated using CRISPR-Cas9 or traditional homologous recombination techniques [69].
- Key Findings: Gcgr⁻/⁻ mice exhibit:
- Interpretation: The absence of glucagon signaling prevents hyperglycemia even under conditions of severe insulin deficiency, supporting the essential role of glucagon in diabetes pathogenesis.
Hyperinsulinemic-Euglycemic Clamp Technique:
- Purpose: Considered the gold standard for assessing insulin resistance in vivo [74] [75].
- Protocol:
- Continuous intravenous infusion of insulin at a constant rate (e.g., 120 mU/m²/min)
- Simultaneous variable glucose infusion to maintain euglycemia (~90-100 mg/dL)
- Frequent blood glucose monitoring (every 5-10 minutes)
- Calculation of glucose infusion rate (GIR) as an index of insulin sensitivity
- Interpretation: Lower GIR indicates greater insulin resistance; the technique permits assessment of whole-body and tissue-specific glucose disposal [74].
Assessment Tools for Insulin Resistance and β-Cell Function
Table 3: Methodologies for Assessing Metabolic Parameters in Research
| Method/Index | Measurement Principle | Application | Advantages/Limitations |
|---|---|---|---|
| HOMA-IR | Fasting glucose × insulin / 22.5 | Population studies, large cohorts | Simple but only estimates basal state |
| Hyperinsulinemic-Euglycemic Clamp | Glucose infusion rate during fixed hyperinsulinemia | Gold standard for insulin sensitivity | Resource-intensive, not for clinical practice |
| Oral Glucose Tolerance Test (OGTT) | Glucose & insulin response to oral glucose load | β-cell function & peripheral sensitivity | Physiological, incorporates incretin effect |
| Intravenous Glucose Tolerance Test (IVGTT) | Acute insulin response to IV glucose | First-phase insulin secretion | Avoids gastrointestinal confounders |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Investigating Glucose Homeostasis
| Reagent/Category | Research Application | Key Function/Mechanism |
|---|---|---|
| Streptozotocin (STZ) | β-cell ablation model | DNA alkylating agent selectively toxic to β-cells |
| Glucagon Receptor Antagonists | Proof-of-concept for glucagon-centric therapy | Competitive inhibition of GCGR signaling |
| GLP-1 Receptor Agonists | Study incretin effects & therapeutic potential | Enhance glucose-dependent insulin secretion, suppress glucagon |
| Somatostatin Analogs | Paracrine regulation studies | Inhibit both insulin and glucagon secretion |
| GCGR Knockout Models | Elucidate glucagon pathophysiology | Genetic elimination of glucagon signaling |
| Hyperpolarization-activated Cyclic Nucleotide-gated (HCN) Channel Blockers | α-cell electrophysiology | Modulate glucagon secretion patterns |
Therapeutic Implications and Future Directions
The reconceptualization of diabetes as a bihormonal disorder has significant implications for therapeutic development:
Current Glucagon-Targeting Approaches:
- GLP-1 Receptor Agonists: Indirectly suppress glucagon secretion while stimulating insulin release [69] [5].
- Dual and Triple Agonists: Molecules combining GLP-1, GIP, and glucagon receptor agonism to optimize metabolic outcomes [5].
- Glucagon Receptor Antagonists: Despite theoretical promise, development has been challenging due to compensatory hyperglucagonemia and α-cell hyperplasia [69].
Emerging Research Frontiers:
- Hepatic-Glucagon Signaling Specificity: Developing tissue-specific glucagon receptor modulators to avoid systemic side effects [5].
- α-Cell Directed Therapies: Targeting the intrinsic defects in diabetic α-cells to restore normal glucose sensing and secretion patterns [71].
- Combination Therapies: Addressing insulin resistance and hyperglucagonemia simultaneously through multi-target agents [69] [5].
The deconstruction of diabetes reveals a complex pathophysiology involving the interplay between insulin deficiency, insulin resistance, and paradoxical hyperglucagonemia. The evidence from experimental models and clinical studies strongly supports a bihormonal abnormality framework where glucagon excess plays a fundamental role in the hyperglycemia of diabetes. For researchers and drug development professionals, this refined understanding highlights the importance of targeting both insulin and glucagon pathways for more effective diabetes management. Future therapeutic innovation should focus on correcting the dysregulation in both β-cell and α-cell function, potentially through combination approaches that address the multifaceted hormonal imbalance characterizing this metabolic disorder.
Diabetes pathophysiology has historically been dominated by a beta-cell-centric perspective, focusing on insulin deficiency and resistance. However, emerging evidence firmly establishes pancreatic α-cell dysregulation as a critical contributor to the disease process. The inappropriate secretion of glucagon exacerbates both fasting and postprandial hyperglycemia, creating a pathological state that accelerates metabolic decline [5]. This whitepaper examines the molecular mechanisms underlying α-cell dysfunction, details experimental models for its investigation, and evaluates emerging therapeutic strategies for its correction. α-Cell dysregulation represents not merely a consequence of beta-cell failure but an active driver of diabetes progression, characterized by glucagon hypersecretion, defective proglucagon processing, and significant transcriptional alterations [76] [77]. Understanding and addressing these defects is paramount for developing more comprehensive diabetes therapies that move beyond glucocentric models to encompass the full complexity of islet dysfunction.
Molecular Mechanisms of α-Cell Dysregulation
Defects in Glucagon Secretion Dynamics
In type 2 diabetes, α-cells lose their ability to appropriately regulate glucagon release in response to glycemic cues. This dysregulation manifests as fasting and postprandial hyperglucagonemia, which significantly contributes to elevated hepatic glucose production [77] [5]. The normal suppression of glucagon secretion by hyperglycemia is impaired, while hypoglycemic stimulation remains intact, creating a dangerous asymmetry in regulatory control. This dysfunction arises from multiple interconnected defects:
- Paracrine Signaling Failure: Loss of insulin-mediated suppression from neighboring β-cells removes a crucial inhibitory signal [5].
- Intrinsic α-Cell Glucose Sensing: Alterations in KATP channel activity and calcium signaling disrupt the core mechanism for glucose-responsive hormone release [5].
- Neural and Hormonal Input Imbalances: Disrupted somatostatin signaling from δ-cells and altered autonomic nervous system input further dysregulate secretion patterns [5].
Transcriptional Reprogramming and Identity Loss
Single-cell transcriptomic analyses reveal profound alterations in the α-cell transcriptional landscape in diabetes. Key identity-maintaining transcription factors, including MAFB and ARX, are significantly downregulated, destabilizing the mature α-cell phenotype [76]. This transcriptional shift facilitates a pathological plasticity where α-cells begin expressing genes typically associated with other endocrine lineages. A recent landmark study identified five distinct α-cell subpopulations in human islets, with one "AB cell" subpopulation co-expressing insulin and glucagon [28]. In diabetic islets, trajectory inference analyses demonstrate a unidirectional shift from β-cells to α-like cells, suggesting dedifferentiation and transdifferentiation events contribute to the altered cellular composition observed in diabetes [28].
Table 1: Key Transcription Factors in α-Cell Identity and Dysregulation
| Transcription Factor | Normal Function | Change in Diabetes | Functional Consequence |
|---|---|---|---|
| MAFB | Maintains mature α-cell identity | Downregulated [76] | Loss of secretory granule organization, altered hormone processing |
| ARX | Specifies α-cell fate | Downregulated [76] | Potential conversion to β-like cells; reduced GCG expression |
| SMOC1 | Limited expression in normal α-cells | Upregulated in β-cells [28] | Promotes β-cell dedifferentiation; reduces insulin expression |
Altered Proglucagon Processing and Hormone Production
In healthy α-cells, the proglucagon precursor is primarily cleaved by prohormone convertase 2 (PC2) to produce glucagon [76]. Under diabetic conditions, this processing pathway is disrupted, with increased expression of prohormone convertase 1 (PC1/3) that favors production of alternative peptides including glicentin and GLP-1 [76]. This abnormal processing results in:
- Altered Hormone Ratios: Increased secretion of glicentin and intra-islet GLP-1
- Paracrine Signaling Disruption: Aberrant GLP-1 signaling within the islet microenvironment
- Reduced Bioactive Glucagon: Diminished production of fully processed, bioactive glucagon
Endoplasmic reticulum (ER) stress has been identified as a key driver of this processing defect, establishing a direct link between cellular stress and hormone misprocessing in diabetic α-cells [76].
Experimental Models and Methodologies
Stem Cell-Derived Alpha (SC-α) Cell Models
The development of SC-α cells through directed differentiation of human pluripotent stem cells provides a reproducible, human-derived model system that closely mirrors primary α-cell biology [76]. These cells demonstrate key α-cell characteristics, including expression of glucagon and appropriate processing enzymes, making them suitable for diabetes modeling and therapeutic screening.
Table 2: Experimental Models for Studying α-Cell Dysregulation
| Model System | Key Features | Applications | Limitations |
|---|---|---|---|
| Stem Cell-Derived α-Cells (SC-α) [76] | ~68% glucagon-positive; recapitulate human α-cell transcriptome and proglucagon processing | ER stress studies; high-throughput drug screening; transcriptional profiling | Immature phenotype compared to primary cells; heterogeneous populations |
| Primary Human Islets [28] | Fully mature α-cells with authentic tissue context; multiple subpopulations | Single-cell RNA sequencing; trajectory analysis; transdifferentiation studies | Limited availability; donor-to-donor variability |
| Mathematical Modeling [77] | Integrates glucose, insulin, glucagon dynamics with β-cell functional mass | Simulating disease progression; predicting therapeutic interventions | Dependent on accurate parameter estimation; validation required |
Protocol: Modeling Diabetic Dysfunction with ER Stress in SC-α Cells
Purpose: To induce diabetes-like α-cell dysfunction in vitro for mechanistic studies and therapeutic screening.
Materials:
- SC-α cells (generated via 6-stage differentiation protocol) [76]
- ER stress inducers: Tunicamycin (1-5 µg/mL) or Thapsigargin (100-500 nM)
- Control solution: DMSO (vehicle)
- Sunitinib (tyrosine kinase inhibitor, 1-10 µM for protection studies)
- Glucagon ELISA kit
- RNA extraction kit and qPCR reagents
- Immunostaining reagents: anti-glucagon, anti-PC1/3, anti-PC2 antibodies
Methodology:
- Cell Culture: Maintain SC-α cells in appropriate maturation medium.
- ER Stress Induction: Treat cells with tunicamycin or thapsigargin for 6-24 hours.
- Therapeutic Intervention: Co-incubate with sunitinib during ER stress induction.
- Outcome Assessment:
- Hormone Secretion: Measure glucagon, glicentin, and GLP-1 secretion via ELISA
- Transcriptional Analysis: Quantify expression of MAFB, ARX, and metabolic pathway genes via qPCR
- Protein Localization: Assess prohormone convertase expression and localization via immunostaining
Validation: Confirm diabetic phenotype by demonstrating glucagon hypersecretion, increased glicentin release, and downregulation of MAFB and oxidative phosphorylation genes [76].
Single-Cell RNA Sequencing for α-Cell Heterogeneity Analysis
Purpose: To identify α-cell subpopulations and transcriptional trajectories in diabetic islets.
Experimental Workflow:
Key Analytical Steps:
- Cell Clustering: Subset α-cells and apply Louvain clustering at resolution 0.8 to identify subpopulations [28].
- Trajectory Inference: Utilize RNA velocity and PAGA to map potential differentiation paths between clusters.
- Signature Gene Identification: Identify genes consistently altered along β-to-α cell trajectories (e.g., SMOC1, PLCE1) [28].
- Functional Validation: Overexpress candidate genes (e.g., SMOC1) in β-cells to assess impact on identity and function.
Signaling Pathways in α-Cell Dysregulation
The regulation of glucagon secretion involves complex intracellular signaling networks that become dysregulated in diabetes. The following diagram illustrates key pathways controlling α-cell function:
This integrated signaling network demonstrates how nutrient, hormonal, and neural inputs converge to regulate glucagon production and secretion. In diabetes, multiple nodes in this network become dysregulated, including:
- cAMP Overproduction: Leads to excessive glucagon secretion despite hyperglycemia [5].
- KATP Channel Dysregulation: Impairs glucose sensing and appropriate secretion responses.
- ER Stress Activation: Shifts proglucagon processing toward PC1/3 and alternative peptides [76].
- Transcription Factor Dysregulation: Reduced MAFB and ARX expression destabilizes α-cell identity [76].
Quantitative Assessment of α-Cell Dysregulation
Mathematical modeling provides a systems-level understanding of how α-cell dysregulation contributes to diabetes progression. The following table summarizes key parameters from a recently published model that simulates 20-year disease progression:
Table 3: Mathematical Modeling Parameters for α-Cell Dysregulation in Diabetes Progression [77]
| Parameter | Normoglycemic Value | T2D Value | Impact on Disease Trajectory |
|---|---|---|---|
| Basal Glucagon Secretion | Reference (1.0x) | 1.3-1.5x increased | Increases fasting glucose; drives initial β-cell compensation |
| Glucagon Suppression by Glucose | Normal (100%) | 40-60% impaired | Contributes to postprandial hyperglycemia |
| Hepatic Glucagon Sensitivity | Normal (100%) | 70-80% reduced (glucagon resistance) | Reduces glycemic stability; increases glucagon levels |
| β-Cell Functional Mass Response | Appropriate compensation | Initial enhancement then accelerated decline | Mild dysregulation enhances then exhausts compensation |
| Time to Diabetes Onset | N/A | 10-15 years with moderate dysregulation | Moderate dysregulation accelerates onset by 5+ years |
This model demonstrates that α-cell dysregulation initially stimulates β-cell compensation through elevated fasting glucose but eventually accelerates functional decline when glucagon secretion becomes severely dysregulated, creating a vicious cycle of metabolic deterioration [77].
Therapeutic Correction Strategies
Small Molecule Approaches
Targeting cellular stress pathways represents a promising approach for correcting α-cell dysfunction. The tyrosine kinase inhibitor sunitinib has demonstrated efficacy in protecting SC-α cells from ER stress-induced dysregulation, preventing glucagon hypersecretion and preserving normal transcriptional profiles [76]. Additional small molecule strategies include:
- Glucagon Receptor Antagonists: Effectively lower blood glucose and HbA1c but risk adverse lipid profiles and α-cell hyperplasia [78] [5].
- Dual GLP-1/Glucagon Receptor Agonists: Leverage glucagon's energy expenditure effects while maintaining GLP-1-mediated glucose control [78] [5].
- ER Stress Reducers: Compounds that alleviate protein misfolding stress may restore normal proglucagon processing.
Cell Reprogramming and Transdifferentiation
Forcing transcriptional reprogramming of α-cells to β-cells represents a novel regenerative approach. Key strategies include:
- ARX Inhibition: Suppressing this key α-cell fate transcription factor promotes conversion to β-like cells [32].
- MAFA Induction: Enforcing expression of this β-cell maturity factor stabilizes the converted phenotype.
- PDX1/NKX6.1 Co-expression: Activates β-cell genetic programs while suppressing α-cell identity.
This approach not only increases β-cell mass but also reduces the glucagon-producing α-cell population, addressing both hormonal imbalances simultaneously [32].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Investigating α-Cell Dysregulation
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Cell Models | SC-α cells (stem cell-derived) [76]; EndoC-βH1 cells | In vitro disease modeling; transcriptional studies | Provide human-relevant systems for mechanistic studies |
| ER Stress Inducers | Tunicamycin; Thapsigargin [76] | Inducing diabetic phenotype in α-cells | Disrupt protein folding; model cellular stress in diabetes |
| Signaling Modulators | Sunitinib (tyrosine kinase inhibitor) [76] | Testing therapeutic protection | Protects against ER stress-induced dysfunction |
| Gene Expression Analysis | scRNA-seq/snRNA-seq platforms [28]; qPCR assays | Identifying cell subpopulations; transcriptional changes | Reveal heterogeneity and trajectory changes in diabetes |
| Key Antibodies | Anti-glucagon; Anti-PC1/3; Anti-PC2 [76] | Immunostaining; protein localization | Assess hormone production and processing enzyme distribution |
Addressing α-cell dysregulation represents a paradigm shift in diabetes therapeutics, moving beyond glucocentric approaches to embrace the full complexity of islet dysfunction. The mechanisms outlined—defective secretion control, transcriptional identity loss, and aberrant hormone processing—provide multiple intervention points for novel therapies. The experimental models and methodologies detailed enable systematic investigation of these mechanisms, while the therapeutic strategies offer promising avenues for clinical translation.
Future research should prioritize understanding the temporal sequence of α-cell dysfunction relative to β-cell decline, identifying biomarkers for different α-cell subpopulations, and developing targeted delivery systems for α-cell-specific therapeutics. As single-cell technologies continue to reveal the remarkable heterogeneity and plasticity of pancreatic islet cells, the potential grows for precisely correcting the dysfunctional α-cell phenotype that so significantly contributes to diabetic hyperglycemia.
Managing Glycemic Variability and Metabolic Stress in Complex Patients
Glycemic variability (GV) has emerged as a critical dimension in assessing glycemic control beyond traditional hemoglobin A1c (HbA1c) measurements. This technical review examines GV as a phenomenon of blood glucose oscillations that induces significant metabolic stress and contributes to diabetes-related complications. Within the framework of hormonal regulation by insulin and glucagon, we analyze the pathophysiological mechanisms linking GV to oxidative stress, endothelial dysfunction, and cardiovascular risk. For researchers and drug development professionals, this article provides standardized methodologies for GV quantification, comprehensive experimental protocols, and visualization of key signaling pathways. The synthesized evidence positions GV management as an essential therapeutic target in complex diabetic patients, particularly those with type 1 diabetes or advanced type 2 diabetes with compromised beta-cell function.
Glycemic variability represents the magnitude of glucose oscillations occurring within defined time intervals, encompassing both short-term (within-day) and long-term (day-to-day) fluctuations [79]. While HbA1c has traditionally served as the gold standard for glycemic assessment, it cannot capture these glucose excursions, creating a critical gap in understanding overall glycemic control [80]. The clinical significance of GV extends beyond mere measurement limitations; evidence demonstrates that GV exerts more detrimental effects than sustained hyperglycemia through multiple pathophysiological pathways, including excessive oxidative stress, heightened inflammatory responses, and endothelial dysfunction [81].
The hormonal regulation of glucose homeostasis primarily involves insulin and glucagon, creating a delicate balance that GV profoundly disrupts. In complex patients with compromised pancreatic function, this disruption becomes particularly pronounced, leading to both hyperglycemic excursions and dangerous hypoglycemic episodes [3]. For pharmaceutical researchers, understanding these mechanisms is essential for developing targeted therapies that address not only overall glycemic control but specifically the fluctuations that drive diabetes complications.
Quantitative Assessment of Glycemic Variability
Core Metrics and Their Clinical Significance
Continuous glucose monitoring (CGM) systems have enabled the precise quantification of GV through multiple metrics, each capturing different aspects of glucose fluctuations [79]. The international consensus recommends specific target values for these metrics to optimize glycemic control while minimizing complication risks.
Table 1: Key Glycemic Variability Metrics and Target Values
| Metric | Formula/Calculation | Clinical Significance | Target Value |
|---|---|---|---|
| Coefficient of Variation (CV) | CV = (SD/mean glucose) × 100 [79] | Measures relative variability; superior to SD for hypoglycemia risk assessment [80] | <36% [81] |
| Time in Range (TIR) | Percentage of readings within 70-180 mg/dL [81] | Direct measure of quality of glycemic control; associated with complication risk | >70% [81] |
| Standard Deviation (SD) | √[Σ(xi - x̄)²/(n-1)] [79] | Measures absolute glucose fluctuations around mean | Individualized; lower values indicate stability |
| Mean Amplitude of Glycemic Excursions (MAGE) | Mean of glucose excursions >1 SD from mean [80] | Captures major glucose swings while filtering minor fluctuations | Not established; lower values preferred |
The coefficient of variation (CV) has emerged as the most clinically valuable metric due to its ability to contextualize glucose fluctuations relative to mean glucose levels, providing a more accurate assessment of hypoglycemia risk than standard deviation alone [80]. International guidelines now recommend a composite target for optimal diabetes management: HbA1c <7.0%, CV <36%, and TIR >70% [81]. However, real-world data reveals that only 28.6% of type 1 diabetes patients achieve all three targets simultaneously, highlighting the clinical challenge and research opportunity in addressing GV [81].
Research Methodologies for GV Assessment
Experimental Protocol: CGM Data Collection and Analysis
Objective: To quantify glycemic variability in a study population using continuous glucose monitoring.
Materials:
- Certified continuous glucose monitoring system (e.g., Dexcom G6, FreeStyle Libre 2/3)
- Data extraction software and validation algorithms
- Statistical package for comprehensive GV analysis (e.g., R with appropriate packages, EasyGV platform)
- Standardized data collection forms for clinical parameters
Procedure:
- Sensor Placement: Apply CGM sensors according to manufacturer specifications in appropriate anatomical locations (typically abdominal region or upper arm).
- Monitoring Period: Maintain continuous monitoring for minimum 14 days to capture both intra-day and inter-day variability, with at least 70% data capture required for valid analysis [79].
- Calibration: If required by device, calibrate according to manufacturer guidelines using capillary blood glucose measurements.
- Data Extraction: Download raw glucose values at 5-minute intervals (288 measurements per day) from CGM platform.
- Data Cleaning: Remove artifacts and erroneous values using validated algorithms (e.g., removing values <40 mg/dL or >400 mg/dL without clinical correlation).
- Metric Calculation: Compute all key GV parameters (CV, SD, TIR, MAGE) using standardized formulas.
- Statistical Analysis: Perform correlation analysis between GV metrics and clinical parameters (HbA1c, hypoglycemia events, complication markers).
Validation Measures: Ensure consistent device operation throughout study period; document any sensor failures or signal losses; correlate with periodic capillary glucose measurements when clinical validation required.
GV and Hormonal Regulation Framework
The regulation of blood glucose occurs through a complex interplay of hormones, primarily insulin and glucagon, which GV profoundly disrupts. In healthy physiology, insulin facilitates glucose transport into cells and inhibits hepatic glucose production, while glucagon counterregulates by stimulating glycogenolysis and gluconeogenesis during fasting states [3]. This delicate balance becomes severely compromised in diabetic states, particularly in type 1 diabetes where absolute insulin deficiency creates dramatic glucose fluctuations [81].
Diagram 1: Pathophysiological Pathways of Glycemic Variability-Induced Complications
GV triggers excessive mitochondrial reactive oxygen species production, overwhelming endogenous antioxidant defenses more effectively than sustained hyperglycemia [81]. This oxidative stress cascade, combined with activated inflammatory pathways, leads to widespread endothelial dysfunction and subsequent microvascular and macrovascular complications [81] [79]. The diagram illustrates how these pathways interconnect to drive diabetes-related complications.
Clinical Implications and Complications
Microvascular and Macrovascular Complications
Evidence consistently demonstrates that increased GV independently predicts the development and progression of diabetes complications, even in patients with apparently well-controlled HbA1c levels [79].
Table 2: GV-Associated Complication Risks and Underlying Mechanisms
| Complication | Epidemiological Association | Proposed Mechanism | Research Evidence |
|---|---|---|---|
| Cardiovascular Disease | 4-10× higher risk in T1D [81] | Endothelial dysfunction, oxidative stress, inflammation [81] | Predicts mortality in T2D with MI [80] |
| Retinopathy | ~80% prevalence after 5 years in T1D [81] | Intermittent hypoxia, oxidative damage | DCCT: >50% reduction with stable control [81] |
| Nephropathy | 20-50% develop within 20 years [81] | Glomerular hyperfiltration, inflammation | Association with albuminuria [79] |
| Neuropathy | 20-40% incidence in T1D [81] | Polyol pathway activation, oxidative damage | Correlation with GV metrics [79] |
| Cognitive Impairment | Significant association [80] | Cerebrovascular damage, direct neuronal impact | Protective effect with GV-reducing drugs [80] |
The relationship between GV and cardiovascular disease is particularly well-established. In patients with type 2 diabetes and acute myocardial infarction, GV predicts mortality, with increased visit-to-visit GV associated with elevated mortality risk [80]. The FLAT-SUGAR trial demonstrated that different treatment approaches achieving similar HbA1c reductions had markedly different effects on GV and potentially cardiovascular outcomes [80].
Mortality and Quality of Life Impacts
Beyond specific complications, GV directly impacts mortality risk and quality of life measures. Analyses from the DEVOTE trial revealed that patients with doubled day-to-day fasting GV had significantly increased risks of severe hypoglycemia and all-cause mortality [80]. Those experiencing severe hypoglycemia had more than two-fold higher risk of all-cause and cardiovascular mortality, even after adjusting for confounding factors [80].
Quality of life measures are significantly compromised by high GV, with studies demonstrating particular impairment in treatment-related and diabetes-specific emotional domains [80]. The perception of reduced GV through optimized treatment correlates with improved work productivity, reduced absenteeism, and enhanced treatment satisfaction [80].
Research Reagent Solutions Toolkit
Table 3: Essential Research Materials for GV Investigation
| Reagent/Technology | Specification | Research Application | Functional Role |
|---|---|---|---|
| Continuous Glucose Monitors | 5-minute sampling frequency; 14-day duration [79] | Continuous glucose profiling | Primary GV data acquisition |
| HbA1c Assay Kits | HPLC-standardized; NGSP-certified | Chronic glycemic control assessment | Reference metric correlation |
| Oxidative Stress Markers | 8-iso-PGF2α, 8-OHdG, nitrotyrosine kits | Oxidative damage quantification | Pathophysiological mechanism studies |
| Inflammatory Cytokine Panels | Multiplex assays for IL-6, TNF-α, CRP | Inflammation pathway analysis | Mechanistic biomarker assessment |
| Endothelial Function Assays | ET-1, VCAM-1, ICAM-1, E-selectin kits | Vascular damage evaluation | Cardiovascular risk correlation |
| Data Analysis Platforms | EasyGV, R packages (cgmanalysis) | GV metric calculation | Standardized parameter derivation |
Therapeutic Approaches and Experimental Models
Pharmacological Interventions
Different therapeutic classes exhibit varying effects on GV, independent of their HbA1c-lowering capabilities. The FLAT-SUGAR trial demonstrated that basal insulin plus GLP-1 receptor agonists reduced GV significantly more effectively than basal-bolus insulin regimens despite similar HbA1c outcomes [80]. This highlights the importance of selecting therapeutic agents based on their GV modulation properties, particularly for high-risk patients.
Diagram 2: Therapeutic Mechanisms for Glycemic Variability Reduction
GLP-1 receptor agonists and SGLT2 inhibitors have demonstrated particularly favorable effects on GV, possibly contributing to their cardiovascular benefits observed in outcome trials [80]. These drug classes not only reduce postprandial glucose excursions but also appear to directly address the underlying pathophysiological mechanisms linking GV to cardiovascular damage.
Experimental Protocol: Assessing Therapeutic Efficacy on GV
Objective: To evaluate the effect of investigational compounds on glycemic variability in preclinical models.
Materials:
- Animal model of diabetes (e.g., streptozotocin-induced diabetic rodents, db/db mice)
- Miniaturized CGM systems for animal research
- Investigational compound and appropriate vehicle control
- Standard reference therapeutic agent (e.g., GLP-1 analog, insulin)
- Metabolic cages for controlled environment
- Tissue collection and preservation reagents
Procedure:
- Model Development: Induce diabetes or utilize genetic model with confirmation of diabetic state (fasting glucose >250 mg/dL).
- Baseline Assessment: Implant CGM and record 72-hour glucose profile before treatment initiation.
- Randomization: Assign animals to treatment groups (investigational compound, reference agent, vehicle control).
- Dosing Protocol: Administer treatments according to established schedule (once-daily or continuous infusion).
- Monitoring Phase: Collect continuous glucose data throughout treatment period (minimum 7 days).
- Endpoint Analyses: Calculate all GV parameters from CGM data; collect plasma for oxidative stress biomarkers; harvest tissues for histological examination.
- Statistical Comparison: Compare GV metrics between treatment groups using appropriate statistical methods (ANOVA with post-hoc tests).
Outcome Measures: Primary: Coefficient of variation, MAGE; Secondary: TIR, oxidative stress markers, endothelial function parameters.
Future Research Directions
While significant progress has been made in understanding GV, several research gaps remain. Prospective studies investigating the predictive power of GV for incident disease in non-diabetic populations are warranted [82]. The relationship between GV and cognitive impairment requires further elaboration, as does the potential for GV-reducing therapies to provide neuroprotective effects [80]. From a drug development perspective, the specific mechanisms by which various therapeutic classes differentially affect GV need deeper characterization to enable more targeted drug design.
Future research should prioritize standardized GV assessment protocols, validation of novel GV metrics against hard clinical endpoints, and exploration of personalized GV targets based on individual patient characteristics and complication risks. The integration of GV parameters into regulatory endpoints for antidiabetic therapies represents an important frontier for clinical trial design.
Glycemic variability has established itself as a critical dimension in diabetes management, particularly for complex patients with heightened vulnerability to glucose fluctuations. Within the framework of insulin and glucagon regulation, GV emerges as both a consequence of hormonal dysregulation and a contributor to further metabolic deterioration through oxidative stress and inflammatory pathways. For researchers and drug development professionals, comprehensive GV assessment requires sophisticated CGM methodologies and specialized analytical approaches. The development of therapeutics specifically targeting GV reduction, rather than solely HbA1c lowering, represents a promising direction for reducing diabetes-related complications and improving patient quality of life. As evidence continues to accumulate, GV management deserves integration into both clinical practice paradigms and pharmaceutical development strategies.
The management of blood glucose presents a fundamental therapeutic paradox: the very medications essential for controlling hyperglycemia in diabetes, particularly insulin and insulin secretagogues, frequently induce hypoglycemia, a dangerous and potentially fatal side effect [83] [84]. This risk underscores a critical limitation in current pharmacologic strategies, which often operate unidirectionally. The body's exquisite natural glucose homeostasis is maintained by the counter-regulatory actions of insulin and glucagon [5]. Insulin, secreted by pancreatic β-cells, lowers blood glucose by facilitating cellular uptake and suppressing hepatic glucose production. Conversely, glucagon, secreted by pancreatic α-cells, elevates blood glucose during fasting states by stimulating hepatic glycogenolysis and gluconeogenesis [5]. In diabetes, this balance is disrupted, and traditional treatments that aggressively replace or stimulate insulin can overwhelm the system's natural defenses, leading to hypoglycemia. This whitepaper examines the pathophysiological basis of this challenge and explores emerging scientific approaches that seek to restore physiological balance, thereby mitigating the pervasive risk of hypoglycemia.
Core Pathophysiology: Hormonal Dysregulation in Diabetes
The pathogenesis of both Type 1 (T1DM) and Type 2 Diabetes Mellitus (T2DM) involves significant dysregulation of pancreatic α-cell function, which critically contributes to hypoglycemia risk. In a healthy physiological state, declining blood glucose levels suppress insulin secretion and stimulate glucagon release, which mobilizes glucose from hepatic stores [5]. However, in diabetes, this counter-regulatory response is profoundly impaired.
In T1DM, the absolute lack of endogenous insulin eliminates its paracrine inhibitory effect on neighboring pancreatic α-cells. This loss of intra-islet insulin signaling results in inappropriately elevated glucagon secretion, even during hyperglycemia [85] [5]. Consequently, patients are entirely dependent on exogenous insulin administration, which lacks the fine-tuned, feedback-controlled precision of endogenous secretion. In T2DM, a state of α-cell resistance to insulin develops; insulin loses its ability to suppress glucagon secretion, leading to elevated basal and postprandial glucagon levels (hyperglucagonemia) that exacerbate hyperglycemia [85] [5]. When patients with T2DM are treated with insulin or sulfonylureas, the glucagon response to hypoglycemia becomes blunted and inadequate, mirroring the defect in T1DM and increasing vulnerability to low blood glucose.
Table 1: Drugs Associated with Hypoglycemia Risk
| Drug Class | Specific Agents | Primary Mechanism | Risk Context |
|---|---|---|---|
| Insulin | All types (short- & long-acting) | Directly lowers blood glucose | Overdose, missed meals, increased activity [83] [84] |
| Sulfonylureas | Glipizide, Glimepiride, Glyburide | Stimulates insulin secretion from β-cells | Prolonged duration of action, renal impairment [83] |
| Glinides | Nateglinide, Repaglinide | Stimulates rapid insulin secretion | Dosing too close to meals, variable food intake [83] |
| SGLT2 Inhibitors | Canagliflozin, Dapagliflozin | Increases urinary glucose excretion | When used concomitantly with insulin/sulfonylureas [83] |
| Non-Diabetes Drugs | Quinine, Pentamidine, Beta-blockers* | Varied (e.g., pancreatic toxicity) | Accidental ingestion, overdose [83] [84] |
*Note: Beta-blockers can mask tachycardia, a key symptom of hypoglycemia.
The clinical symptoms of hypoglycemia range from autonomic signs (shakiness, sweating, palpitations) to neuroglycopenic symptoms (confusion, difficulty concentrating, seizures, and coma) [84]. Repeated episodes can lead to hypoglycemia unawareness, a dangerous condition where the autonomic warning signals of low blood glucose fail, significantly increasing the risk of severe events [84].
Emerging Research and Novel Therapeutic Targets
Recent research has moved beyond simple glucose lowering to focus on therapies that mimic or harness the body's innate regulatory logic. Key advances highlight the potential of the α-cell and dual-hormone approaches to create safer treatment paradigms.
Alpha Cell Plasticity and Endogenous GLP-1 Production
A groundbreaking discovery from Duke University has revealed significant plasticity in pancreatic α-cell function. Contrary to the long-standing belief that α-cells solely produce glucagon, research demonstrates that human alpha cells can naturally produce and secrete significant quantities of bioactive glucagon-like peptide-1 (GLP-1) [21]. GLP-1 is a potent incretin hormone that glucose-dependently stimulates insulin secretion while suppressing glucagon release.
Using mass spectrometry-based assays specifically designed to detect the bioactive form of GLP-1, researchers found that when glucagon production was genetically or pharmacologically blocked (e.g., by inhibiting the Prohormone Convertase 2 (PC2) enzyme), α-cells markedly increased their production of GLP-1 (via the PC1 enzyme) [21]. This hormonal "switch" resulted in improved glucose tolerance and enhanced insulin secretion in mouse models. This discovery positions the α-cell as a built-in source of a powerful, glucose-responsive insulin secretagogue, opening a new therapeutic avenue: pharmacologically modulating α-cell fate to boost endogenous GLP-1 production as a more physiological way to support β-cell function in T2DM [21].
Smart Insulins and Dual-Hormone Systems
To address the unidirectional action of conventional insulin, researchers are developing "smart" molecular and system-based solutions.
Molecular Solutions: Investigators at Indiana University School of Medicine have designed a novel fusion protein that combines insulin and glucagon into a single molecule [60]. This "smart insulin" exploits the liver's natural signaling network, where the relative actions of insulin and glucagon compete. The hybrid molecule is engineered so that its net effect is context-dependent: at high glucose concentrations, the insulin signal dominates, lowering blood sugar; at low glucose concentrations, the glucagon signal wins, raising blood sugar and preventing hypoglycemia [60]. In preclinical rat studies, this molecule maintained stability for weeks without refrigeration, offering a potential future of more robust and safer glucose-regulating therapeutics.
System Solutions: The Artificial Pancreas: The Dual Hormone Artificial Pancreas (DHAP) represents the pinnacle of technological integration for managing T1DM. This closed-loop system consists of a continuous glucose monitor (CGM), a control algorithm, and two pumps that administer both insulin and glucagon [85] [86]. Recent advances focus on making these systems smarter and more patient-specific. For instance, research published in 2025 describes a Smart DHAP (SDHAP) that uses machine learning models (K-Nearest Neighbor and Support Vector Machine) to classify and predict glycemic events from CGM data [86]. An event-triggered feedback-feedforward controller then delivers precise, personalized doses of insulin or glucagon only when needed, minimizing hormone infusion and reducing the risk of hypoglycemia, particularly after meals or exercise [86].
The LEAP2-Ghrelin Axis
Beyond insulin and glucagon, other hormonal systems offer additional leverage for metabolic control. Liver-expressed antimicrobial peptide 2 (LEAP2) is an endogenous antagonist of the ghrelin receptor, countering ghrelin's appetite-stimulating and growth hormone-releasing effects [87]. Recent research has elucidated that LEAP2 is regulated by insulin and glucagon [87]. During somatostatin clamps in humans, glucagon infusion was shown to significantly decrease plasma LEAP2 levels. Furthermore, insulin receptor antagonism in mice blocked the postprandial rise in LEAP2, indicating insulin is a key postprandial regulator [87]. This newly described endocrine axis suggests that manipulating LEAP2 could provide a new method to modulate appetite and energy balance in metabolic diseases, potentially influencing body weight—a key comorbidity in T2DM.
Table 2: Quantitative Outcomes of Novel Hypoglycemia Mitigation Strategies
| Strategy | Experimental Model | Key Quantitative Outcome | Significance |
|---|---|---|---|
| CGM in Long-Term Care [88] | 38 LTC residents with diabetes | 12-fold increase in hypoglycemia detection (88 to 1049 events); 40% reduction in nursing time per test. | Enables data-driven deprescribing and reduces clinical burden. |
| Smart Insulin Fusion Protein [60] | Rat model of T1D | Stable for >2 weeks at room temperature; prevented hypoglycemia while controlling hyperglycemia. | Offers a molecular-level, glucose-responsive solution with practical storage benefits. |
| Smart Dual-Hormone AP [86] | In-silico trial using the T1DiabetesGranada dataset (736 patients) | Event-triggered control with ML prediction improved glucose time-in-range and reduced hypoglycemic events. | Moves towards personalized, predictive, and pre-emptive hormone delivery. |
Experimental Methodologies for Key Findings
Protocol: Assessing Alpha Cell GLP-1 Production
Objective: To quantify the production of bioactive GLP-1 from human pancreatic alpha cells and investigate its functional role [21].
Materials & Reagents:
- Human and mouse pancreatic tissue from donors of varying age, weight, and diabetes status.
- High-specificity mass spectrometry assay to detect bioactive GLP-1 (7-36 amide and 7-37) and avoid cross-reaction with inactive metabolites.
- Enzyme inhibitors: Specific inhibitors for PC2 (to block glucagon production) and PC1 (to block GLP-1 production).
- Glucose tolerance tests to assess physiological impact.
Methodology:
- Tissue Analysis: Pancreatic tissue samples were homogenized, and peptides were extracted. The extracts were analyzed using the custom mass spectrometry assay to precisely quantify levels of bioactive GLP-1 and glucagon.
- Genetic/Pharmacologic Manipulation: In mouse models, the genes for enzymes PC2 and PC1 were selectively knocked out in α-cells, or their activity was pharmacologically inhibited.
- Functional Secretion Assays: Isolated human islets or α-cell lines were perfused with low- and high-glucose solutions. Effluent was collected and analyzed via mass spectrometry to measure dynamic GLP-1 and glucagon secretion.
- In-Vivo Validation: Treated and control mice underwent glucose tolerance tests. Blood glucose and serum insulin levels were measured to determine the metabolic consequence of shifting α-cell output from glucagon to GLP-1.
Protocol: Regulation of LEAP2 by Insulin and Glucagon
Objective: To define the roles of insulin and glucagon in the endocrine regulation of LEAP2 in mice and humans [87].
Materials & Reagents:
- Human participants, including individuals with obesity and T2DM, and mouse models.
- Somatostatin clamp technique to suppress endogenous insulin and glucagon secretion, allowing for controlled hormone infusion.
- Glucagon and insulin infusions at fixed, controlled rates.
- Insulin receptor antagonists (e.g., S961) for murine studies.
- ELISA or MS-based assays for measuring plasma LEAP2 and ghrelin concentrations.
Methodology:
- Human Clamp Studies: Participants underwent a somatostatin clamp with co-infusion of insulin and glucagon at basal rates. Following a baseline period, glucagon was infused at a higher, pharmacological rate while maintaining insulin at a basal level. Plasma samples were collected throughout for LEAP2 measurement.
- Murine Studies:
- Insulin Antagonism: Mice were treated with an insulin receptor antagonist before and during an oral glucose tolerance test to assess its effect on the postprandial LEAP2 response.
- Genetic Tracing: Insulin and glucagon receptor-expressing hepatocytes were identified using lineage-tracing techniques to confirm the liver as the primary source of LEAP2.
- Data Analysis: LEAP2 levels under different hormonal milieus were compared to establish insulin as a stimulator and glucagon as a suppressor of LEAP2 secretion.
Diagram 1: Alpha cell GLP-1 pathway.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Investigating Glucose-Regulatory Hormones
| Research Reagent | Function in Experimental Design |
|---|---|
| High-Specificity Mass Spectrometry | Precisely measures bioactive peptide hormones (GLP-1, LEAP2) without cross-reactivity from inactive fragments or related prohormones [21] [87]. |
| Somatostatin Clamp | A gold-standard physiological technique to suppress endogenous insulin and glucagon secretion, allowing researchers to study the isolated effects of infused hormones [87]. |
| Prohormone Convertase Inhibitors (PC1/PC2) | Pharmacologic tools to selectively block the enzymatic conversion of prohormones into their active products (e.g., blocking glucagon production with a PC2 inhibitor) [21]. |
| Lineage-Tracing Mouse Models | Genetically engineered models that allow for the specific labeling and fate-tracking of distinct cell types (e.g., insulin- or glucagon-receptor-expressing hepatocytes) [87]. |
| Continuous Glucose Monitor (CGM) | A clinical and research device that measures interstitial glucose levels at regular intervals (e.g., every 5-15 minutes), providing rich time-series data for glycemic variability analysis [88] [86]. |
| Machine Learning Classifiers (SVM, KNN) | Algorithms used to analyze complex datasets (e.g., CGM data) to classify glycemic states (hypo-/hyper-glycemia) and predict future glucose trends for pre-emptive intervention [86]. |
Diagram 2: Smart dual-hormone artificial pancreas.
The challenge of hypoglycemia is an intrinsic flaw in our current dominant paradigm of diabetes management. The future of diabetes therapy lies in moving beyond simple, unidirectional glucose-lowering agents toward treatments that recapitulate the body's innate intelligence. The most promising strategies—harnessing α-cell plasticity, developing smart molecules with context-dependent actions, and deploying intelligent closed-loop systems—all share a common principle: restoring dynamic, bi-directional control over blood glucose.
For researchers and drug development professionals, this shift necessitates a focus on systems biology and complex therapeutic modalities. The tools of machine learning for glucose prediction, advanced mass spectrometry for hormone quantification, and sophisticated control theory for algorithm design are becoming as crucial as traditional molecular pharmacology. The convergence of these disciplines promises a new generation of therapies that not only control hyperglycemia but also respect the physiological imperative to avoid hypoglycemia, ultimately delivering safer and more effective care for people with diabetes.
For decades, the hormonal regulation of blood glucose has been conceptualized through a simple binary model: insulin lowers blood glucose, while glucagon raises it. While this framework remains foundational, recent research has revealed far greater complexity in the cross-talk between organs and hormone systems. The liver-α-cell axis represents a critical bidirectional communication network between the pancreas and liver that extends beyond glucose homeostasis to encompass amino acid and lipid metabolism [89]. Simultaneously, the incretin system, particularly glucagon-like peptide-1 (GLP-1), has emerged as a powerful therapeutic pathway with multi-organ effects [90] [10]. This whitepaper examines the integrated physiology of these systems and explores how their therapeutic manipulation is generating novel treatment strategies for diabetes, obesity, and related metabolic disorders for research and drug development professionals.
The Liver-α-Cell Axis: From Glucose Stat to Nutrient Integrator
Core Physiology and Regulatory Mechanisms
The liver-α-cell axis functions as a sophisticated feedback loop wherein hepatocytes and pancreatic α-cells communicate to maintain metabolic homeostasis. Glucagon, secreted from pancreatic α-cells, acts primarily on hepatocytes through the glucagon receptor (GCGR), a class B G protein-coupled receptor (GPCR) [5] [22]. Beyond its classical role in stimulating hepatic glucose output via glycogenolysis and gluconeogenesis, glucagon regulates amino acid catabolism and lipid metabolism [89].
The axis operates on a principle of nutrient sensing: elevated amino acids stimulate glucagon secretion, which in turn enhances hepatic amino acid uptake and catabolism via ureagenesis [89]. This creates a closed-loop system where glucagon functions as both a regulator of glucose and a controller of amino acid clearance. Disruption of this axis contributes to the pathophysiology of multiple metabolic diseases, including type 2 diabetes (T2D) and non-alcoholic fatty liver disease (NAFLD) [5] [22].
The following diagram illustrates the key components and signaling pathways of the liver-α-cell axis:
Figure 1: The Liver-α-Cell Axis Signaling Pathway. This diagram illustrates the bidirectional feedback between pancreatic α-cells and hepatocytes, highlighting glucagon secretion stimulated by amino acids and subsequent hepatic signaling through the GCGR-cAMP-PKA pathway.
Pathophysiological Implications in Metabolic Disease
Dysregulation of the liver-α-cell axis manifests as two primary pathological states: hyperglucagonemia and hepatic glucagon resistance. In type 2 diabetes, α-cells develop resistance to the paracrine inhibitory effects of insulin and somatostatin, leading to fasted and postprandial hyperglucagonemia that drives excessive hepatic glucose production [5] [22]. More recently, the concept of "glucagon resistance" has emerged, describing a state where the liver becomes selectively resistant to glucagon's effects on amino acid and lipid metabolism while maintaining sensitivity to its hyperglycemic actions [89]. This selective resistance may explain the observed hyperaminoacidemia in diabetic states and contribute to the lipid accumulation characteristic of NAFLD [89].
Table 1: Key Regulators of Glucagon Secretion in Pancreatic α-Cells
| Regulator | Source | Receptor/Pathway | Key Signaling Molecules | Effect on Glucagon Secretion |
|---|---|---|---|---|
| Low Glucose | Hypoglycemia | Sympathetic activation | ↑ cAMP, ↑ PKA, ↑ Epac2, ↑ Ca²⁺ | Stimulation [22] |
| Amino Acids | Protein intake/catabolism | GCGR feedback, amino acid sensors | mTORC1, AMPK | Stimulation [89] |
| Insulin | β-cell | Insulin receptor (IR) | PI3K-Akt signaling | Inhibition [22] |
| Somatostatin | δ-cell | SSTR2 | ↓ cAMP, ↓ Ca²⁺ | Inhibition [22] |
| GLP-1 | Gut (incretin) | GLP-1R (direct or indirect) | ↓ cAMP, ↑ Insulin | Inhibition [90] [22] |
| GIP | Gut (incretin) | GIP receptor | ↑ cAMP | Stimulation [22] |
| Epinephrine | Stress response | β-adrenergic receptor | ↑ cAMP → ↑ PKA, Epac2 | Stimulation [5] |
Incretin Systems: Beyond Glucose-Dependent Insulin Secretion
GLP-1 Biology and Signaling Mechanisms
GLP-1 is a 30-amino-acid peptide derived from proglucagon, primarily synthesized in intestinal L-cells, pancreatic α-cells, and neurons in the nucleus of the solitary tract [10]. As an incretin hormone, GLP-1 exerts its effects through binding to the GLP-1 receptor (GLP-1R), a G protein-coupled receptor widely expressed on pancreatic β-cells, lung, stomach, intestine, kidney, heart, and brain tissues [90] [10].
The intracellular signaling cascade initiated by GLP-1R activation begins with adenylate cyclase activation and cyclic adenosine monophosphate (cAMP) production [90]. Downstream of cAMP, two primary pathways mediate the metabolic effects of GLP-1: protein kinase A (PKA)-dependent signaling and exchange protein directly activated by cAMP (Epac2)-dependent pathways [90]. The PKA-independent pathway requires approximately 5-fold higher cAMP concentrations for activation compared to the PKA-dependent pathway [90].
The following diagram illustrates the GLP-1 receptor signaling pathway:
Figure 2: GLP-1 Receptor Signaling and Physiological Effects. This diagram illustrates the GLP-1 receptor activation and downstream signaling through both PKA and Epac2 pathways, resulting in multiple metabolic benefits.
Therapeutic Applications of Incretin-Based Therapies
GLP-1 receptor agonists (GLP-1RAs) represent a cornerstone of modern diabetes and obesity treatment. These agents are categorized as either human GLP-1 derivatives (liraglutide, semaglutide, dulaglutide, albiglutide) or exendin-4-based compounds (exenatide, lixisenatide) with varying administration frequencies (daily or weekly) and routes (subcutaneous or oral) [90]. Beyond their glucose-lowering effects via stimulation of glucose-dependent insulin secretion and suppression of glucagon release, GLP-1RAs delay gastric emptying, reduce food intake through central appetite suppression, and demonstrate significant cardiorenal benefits [90] [10].
Table 2: GLP-1 Receptor Agonists: Pharmacological Properties and Clinical Effects
| Agent | Structure Base | Dosing Frequency | Administration Route | Key Clinical Effects Beyond Glycemic Control |
|---|---|---|---|---|
| Liraglutide | Human GLP-1 | Daily | Subcutaneous | Weight loss, cardiovascular risk reduction [90] |
| Semaglutide | Human GLP-1 | Weekly/Oral | Subcutaneous/Oral | Significant weight loss, cardiovascular benefits [90] [10] |
| Dulaglutide | Human GLP-1 | Weekly | Subcutaneous | Cardiovascular risk reduction, low hypoglycemia risk [90] |
| Exenatide | Exendin-4 | Twice daily/Weekly | Subcutaneous | Weight loss, sustainable HbA1c reduction [90] |
| Lixisenatide | Exendin-4 | Daily | Subcutaneous | Anti-inflammatory effects, potential neuroprotection [10] |
Integrated Therapeutic Approaches: Targeting Multiple Pathways
Dual and Triple Agonists: Next-Generation Therapeutics
The most significant advancement in metabolic therapeutics has been the development of unimolecular multi-agonists that simultaneously target multiple hormone receptors. These innovative molecules leverage the synergistic effects of complementary metabolic pathways:
Dual GLP-1/GIP Receptor Agonists: Tirzepatide represents the first-in-class dual GLP-1/GIP receptor agonist, demonstrating superior glycemic control and weight loss compared to selective GLP-1RAs in phase 3 clinical trials [10]. The addition of GIP receptor agonism is believed to enhance insulin sensitivity and adipose tissue metabolism while mitigating gastrointestinal side effects.
Dual GLP-1/Glucagon Receptor Agonists: These agents combine the anorectic and insulinotropic effects of GLP-1 with glucagon's energy expenditure and lipid oxidation properties [10]. The glucagon component promotes hepatic lipid oxidation and reduces hepatic steatosis, while GLP-1 activity ensures glucose homeostasis is maintained.
GLP-1/GIP/Glucagon Receptor Tri-Agonists: Agents like Retatrutide represent the cutting edge of multi-agonist development, simultaneously targeting three key metabolic receptors [10]. In phase 2 trials, triple agonists have demonstrated unprecedented weight loss effects, hypothesized to result from combined appetite suppression (GLP-1), enhanced energy expenditure (glucagon), and improved insulin sensitivity (GIP) [10].
Table 3: Multi-Agonist Therapies: Mechanisms and Therapeutic Profiles
| Therapy Class | Receptor Targets | Primary Mechanisms | Metabolic Benefits | Development Status |
|---|---|---|---|---|
| GLP-1R Agonists | GLP-1R | ↑ Glucose-dependent insulin secretion, ↓ glucagon, ↓ appetite | HbA1c reduction, weight loss, cardiorenal protection | Marketed [90] |
| GLP-1/GIP Dual Agonists | GLP-1R, GIPR | Enhanced insulin secretion, adipose tissue modulation, appetite regulation | Superior HbA1c reduction vs. GLP-1RAs, significant weight loss | Marketed (tirzepatide) [10] |
| GLP-1/Glucagon Dual Agonists | GLP-1R, GCGR | Appetite suppression, ↑ energy expenditure, ↑ lipid oxidation | Weight loss, hepatic steatosis reduction, glycemic control | Clinical development [10] |
| GLP-1/GIP/Glucagon Tri-Agonists | GLP-1R, GIPR, GCGR | Comprehensive metabolic enhancement via three complementary pathways | Unprecedented weight loss, glycemic control, lipid improvement | Phase 3 trials [10] |
Experimental Approaches and Research Methodologies
Key Experimental Protocols for Investigating the Liver-α-Cell Axis
1. Hyperinsulinemic-Euglycemic Clamp with Stable Isotope Tracing:
- Purpose: To assess hepatic glucose production and glucagon sensitivity under controlled conditions.
- Methodology: Subjects receive a primed, continuous infusion of insulin to suppress endogenous insulin production, while glucose is infused to maintain euglycemia (∼5.0-5.5 mmol/L). Stable isotopes ([6,6-²H₂]glucose or [U-¹³C]glucose) are co-infused to quantify rates of endogenous glucose production, gluconeogenesis, and glycogenolysis. Glucagon infusion can be superimposed to assess hepatic responsiveness [89].
- Key Measurements: Glucose infusion rate (GIR), endogenous glucose production (EGP), gluconeogenic flux.
2. Pancreatic Islet Perfusion Studies:
- Purpose: To characterize dynamic glucagon secretion patterns from α-cells in response to nutrient and hormonal stimuli.
- Methodology: Isolated islets or perfused pancreas preparations are subjected to controlled perfusion with physiological buffers while systematically varying nutrient (glucose, amino acids) and hormone (insulin, GLP-1) concentrations. Effluent is collected at timed intervals for glucagon quantification via ELISA or RIA [89].
- Key Measurements: Glucagon secretion kinetics, dose-response relationships, paracrine interactions.
3. Hepatic Amino Acid Flux Assessment:
- Purpose: To quantify glucagon's effects on amino acid turnover and ureagenesis.
- Methodology: Subjects receive continuous infusion of stable isotope-labeled amino acids (e.g., [¹⁵N]alanine, [²H₅]phenylalanine) with and without glucagon infusion. Arteriovenous difference across the liver can be measured via catheterization to assess hepatic amino acid extraction [89].
- Key Measurements: Amino acid appearance and disposal rates, ureagenesis flux, hepatic extraction efficiency.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Investigating Liver-α-Cell Axis and Incretin Biology
| Reagent/Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Receptor Agonists/Antagonists | GCGR agonists (GLP-1/glucagon co-agonists), GCGR antagonists (LY2409021), GLP-1R antagonists (exendin(9-39)) | Target validation, mechanism studies, signaling pathway analysis | Selective modulation of specific receptor pathways to dissect their physiological contributions [89] [10] |
| Stable Isotopes | [6,6-²H₂]glucose, [U-¹³C]glucose, [¹⁵N]alanine, [²H₅]phenylalanine | Metabolic flux studies, substrate utilization assessment, kinetic analysis | Safe tracing of metabolic pathways in vivo; quantification of substrate fluxes through gluconeogenesis, ureagenesis [89] |
| Hormone Assays | Glucagon ELISA/RIA (Mercodia, Millipore), GLP-1 ELISA (total/active), Multiplex panels | Hormone quantification, secretion dynamics, correlation with metabolic parameters | Precise measurement of hormone concentrations in plasma, perfusate, cell culture media [5] [89] |
| Cell Models | Primary hepatocytes, α-cell lines (αTC1, InR1G9), primary human islets, stem cell-derived islet cells | In vitro signaling studies, secretion assays, drug screening | Physiologically relevant systems for mechanistic studies without in vivo complexity [89] |
| Genetic Models | GCGR knockout mice, α-cell specific GLP-1R knockout, Glucagon-Cre models | Target validation, tissue-specific function analysis, pathway necessity testing | Determination of physiological roles of specific genes/receptors in controlled genetic backgrounds [89] [10] |
The emerging understanding of the liver-α-cell axis and incretin systems represents a paradigm shift in metabolic disease therapeutics. Moving beyond the traditional glucocentric view, contemporary approaches recognize the integrated nature of nutrient metabolism and the therapeutic potential of simultaneously targeting multiple hormonal pathways. The development of dual and triple agonists demonstrates the promising clinical translation of these physiological insights, offering unprecedented efficacy for complex metabolic diseases.
Future research directions should focus on delineating the precise molecular mechanisms underlying tissue-specific glucagon resistance, developing organ-specific modulators of GCGR signaling, and identifying biomarkers that can predict individual responses to multi-agonist therapies. Additionally, the exploration of gut-liver-brain axis connections may reveal further therapeutic opportunities for holistic metabolic regulation. As these innovative approaches mature, they hold the potential to fundamentally transform our management of diabetes, obesity, NAFLD, and related cardiometabolic disorders.
Comparative Efficacy and Future Directions in Diabetes Therapeutics
The strategic selection between monotherapy and combination therapy represents a fundamental challenge in therapeutic drug development, particularly in the management of complex endocrine disorders such as diabetes mellitus. This paradigm is acutely observed in the realm of blood glucose regulation, where the counterbalancing hormones insulin and glucagon maintain homeostasis through a sophisticated feedback system. Insulin, secreted by pancreatic beta cells, facilitates cellular glucose uptake and inhibits hepatic glucose production, thereby reducing blood glucose levels. Conversely, glucagon, released from pancreatic alpha cells, elevates blood glucose by stimulating glycogenolysis and gluconeogenesis in the liver [17] [91]. Dysregulation of this intricate system necessitates pharmacological intervention, where the choice between targeting a single pathway versus employing multi-target approaches carries significant implications for efficacy, safety, and personalized treatment outcomes.
Therapeutic decisions must account for multiple factors including disease pathophysiology, patient-specific characteristics, and the mechanistic complementarity of available agents. This review provides a comprehensive technical analysis of the monotherapy versus combination therapy paradigm, with specific focus on blood glucose regulation, to inform researchers and drug development professionals in their pursuit of optimized treatment strategies. We present quantitative comparative analyses, detailed experimental methodologies, and visualizations of core biological pathways to equip the scientific community with tools for advanced therapeutic development.
Core Physiological Mechanisms: Insulin and Glucagon Interplay
The regulatory system governing blood glucose represents a classic endocrine feedback loop. In the fed state, rising blood glucose levels stimulate pancreatic beta cells to secrete insulin. Insulin then promotes glucose uptake in muscle and adipose tissue via GLUT4 transporter translocation, stimulates glycogenesis in the liver, and inhibits hepatic glucose production. Simultaneously, insulin secretion suppresses glucagon release from alpha cells, further reducing endogenous glucose production [91] [92].
During fasting or periods of increased energy demand, declining blood glucose levels trigger glucagon secretion. Glucagon activates hepatic glycogenolysis and gluconeogenesis, releasing glucose into the bloodstream. This glucagon-mediated response is suppressed by insulin, establishing a tightly regulated bi-hormonal system that maintains blood glucose within a narrow range of approximately 70-110 mg/dL [93] [91]. The failure of this system—through autoimmune beta-cell destruction (Type 1 Diabetes), insulin resistance (Type 2 Diabetes), or other pathological mechanisms—creates the therapeutic necessity for exogenous intervention.
Signaling Pathway Diagram
Diagram 1: Core regulatory pathways of insulin and glucagon in blood glucose homeostasis. The diagram illustrates the bi-hormonal feedback system that maintains glucose equilibrium, highlighting the opposing actions on target tissues and mutual inhibition between pancreatic alpha and beta cells.
Comparative Clinical Efficacy: Quantitative Analysis
The therapeutic efficacy of monotherapy versus combination approaches varies significantly across disease contexts and patient populations. Recent meta-analyses in diabetes treatment demonstrate that combination therapies often provide superior glycemic control compared to monotherapies, particularly in patients with elevated baseline HbA1c.
Table 1: Efficacy Outcomes of Monotherapy vs. Combination Therapy for Type 2 Diabetes
| Therapy Regimen | HbA1c Reduction (%) | Weight Change (kg) | Patient Population | Reference Study |
|---|---|---|---|---|
| DPP4i Monotherapy | Baseline | Baseline | Asian & Non-Asian | [94] |
| SGLT2i Monotherapy | Baseline | -1.57 to -2.10 | Asian & Non-Asian | [94] |
| SGLT2i/DPP4i Combination | -0.57 vs DPP4i-0.46 vs SGLT2i | -1.57 vs DPP4iNSD vs SGLT2i | Overall Population | [94] |
| SGLT2i/DPP4i Combination (Asian) | -0.55 | Similar to overall | Asian Subpopulation | [94] |
| SGLT2i/DPP4i Combination (Non-Asian) | -0.38 | Similar to overall | Non-Asian Subpopulation | [94] |
Similar comparative patterns emerge across other therapeutic areas. In oncology, a retrospective study of older patients (≥75 years) with advanced biliary tract cancer found that while combination therapy (gemcitabine + cisplatin) showed a trend toward improved median overall survival (16.4 months vs. 12.8 months) compared to monotherapy, this advantage was not statistically significant in multivariable analysis (HR 1.05, 95% CI 0.66-1.68) [95]. The therapeutic context significantly influences outcomes, as demonstrated in infectious disease, where vancomycin combination therapy (VCT) for central nervous system infections following neurosurgery demonstrated significantly higher clinical cure rates (90% vs. 76%, p=0.007) compared to single-drug therapy (SDT) [96].
Experimental Design and Methodologies
Randomized Controlled Trial Design for Glucose-Lowering Therapies
The gold standard for comparing therapeutic efficacy is the randomized controlled trial (RCT). A recent meta-analysis investigating SGLT2i/DPP4i combination therapy provides a robust methodological framework [94]:
Study Population: Adults with Type 2 Diabetes inadequately controlled on metformin monotherapy or other background therapy. Trials typically exclude patients with type 1 diabetes, severe renal impairment, or history of diabetic ketoacidosis.
Intervention Groups:
- Combination Therapy Arm: SGLT2i (e.g., dapagliflozin 10mg daily) + DPP4i (e.g., saxagliptin 5mg daily)
- Active Comparator Arm 1: SGLT2i monotherapy + placebo
- Active Comparator Arm 2: DPP4i monotherapy + placebo
Outcome Measures:
- Primary Efficacy Endpoint: Change in HbA1c from baseline to study endpoint (typically 24-52 weeks)
- Secondary Efficacy Endpoints: Change in fasting plasma glucose, body weight, systolic blood pressure
- Safety Endpoints: Incidence of hypoglycemic events, genital and urinary tract infections, other adverse events
Statistical Analysis: Utilizing mixed-model repeated measures or analysis of covariance to assess least-squares mean differences between treatment groups, with multiple imputation for missing data. Subgroup analyses by baseline HbA1c (<8.5% vs ≥8.5%) and racial group (Asian vs. non-Asian) provide insights into personalized treatment approaches.
Artificial Pancreas Control Algorithm Development
For Type 1 Diabetes research, the development of bi-hormonal artificial pancreas systems represents a sophisticated combination approach utilizing both insulin and glucagon:
System Components:
- Continuous Glucose Monitor (CGM) providing real-time interstitial glucose measurements every 5 minutes
- Insulin pump with rapid-acting insulin analog
- Glucagon delivery system with stable glucagon formulation
- Model Predictive Control (MPC) algorithm
Control Algorithm: The MPC approach uses a comprehensive physiological model (e.g., Sorensen model with 19 differential equations) to predict future glucose levels based on current measurements, meal announcements (feed-forward control), and physical activity. The algorithm simultaneously optimizes both insulin and glucagon delivery rates to maintain glucose within target range (70-180 mg/dL), employing constraints to prevent over-delivery of either hormone and including safety modules to mitigate hypoglycemia risk [93].
Performance Metrics:
- Percentage time in target glucose range (70-180 mg/dL)
- Percentage time in hypoglycemia (<70 mg/dL) and severe hypoglycemia (<54 mg/dL)
- Percentage time in hyperglycemia (>180 mg/dL)
- Average tracking error (ATE) relative to target glucose (e.g., 90 mg/dL)
Experimental Workflow Diagram
Diagram 2: Generalized workflow for comparative therapy trials. The schematic outlines key phases from patient recruitment through statistical analysis, highlighting parallel intervention arms and outcome assessment procedures common to randomized controlled trials.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents for Glucose Regulation Studies
| Reagent/Material | Function/Application | Technical Specifications |
|---|---|---|
| Human Insulin Analogs | In vitro and in vivo studies of insulin signaling | Rapid-acting (Lispro, Aspart); Long-acting (Glargine, Detemir); >95% purity |
| Glucagon Formulations | Research on counter-regulatory responses | Lyophilized powder requiring reconstitution; stable liquid formulations recently developed |
| SGLT2 Inhibitors | Investigation of renal glucose excretion | Canagliflozin, Dapagliflozin, Empagliflozin; selective against SGLT1 |
| DPP4 Inhibitors | Studies of incretin hormone enhancement | Sitagliptin, Saxagliptin, Linagliptin; enzyme inhibition IC50 < 10 nM |
| Continuous Glucose Monitors | Real-time glucose monitoring in animal and human studies | Electrochemical sensing; 1-5 minute measurement intervals; MARD < 10% |
| Pancreatic Cell Lines | In vitro screening of beta and alpha cell function | Beta-TC-6, INS-1E (beta cells); Alpha-TC-1 (alpha cells) |
| GLUT4 Translocation Assays | Assessment of insulin sensitivity | Immunofluorescence, photobleaching; Myc-GLUT4-GFP transfected cells |
The strategic selection between monotherapy and combination approaches remains context-dependent, requiring careful consideration of therapeutic goals, patient characteristics, and mechanistic synergies. In blood glucose regulation, the emerging evidence supports combination therapies for patients requiring substantial glycemic improvement or those with specific phenotypic characteristics, while monotherapy may suffice for early-stage disease or mild hyperglycemia.
Future research directions should focus on identifying predictive biomarkers for treatment response, developing more sophisticated drug combinations with complementary mechanisms of action, and creating adaptive treatment algorithms that can dynamically adjust therapeutic intensity based on individual patient needs. The integration of continuous glucose monitoring with automated insulin and glucagon delivery systems represents the cutting edge of combination approaches, potentially revolutionizing management for people with diabetes.
As therapeutic science advances, the dichotomy between monotherapy and combination approaches will likely evolve into a more nuanced paradigm of personalized, dynamic treatment optimization, leveraging insights from ongoing research into the complex hormonal regulation of metabolism.
The relentless global increase in metabolic diseases such as type 2 diabetes (T2DM) and obesity has necessitated the development of therapeutic strategies that move beyond single-target approaches. This whitepaper examines the scientific rationale and emerging evidence for the simultaneous activation of the glucagon-like peptide-1 (GLP-1) and glucagon (GCG) receptors as a transformative therapeutic pathway. Building upon the established framework of hormonal blood glucose regulation by insulin and glucagon, we detail the complementary mechanisms of GLP-1 and glucagon receptor co-stimulation. The document provides a comprehensive analysis of preclinical and clinical data, delineates the intricate signaling pathways involved, and offers detailed experimental methodologies for validating this dual-agonist approach. The synthesis of evidence indicates that GLP-1/glucagon co-agonism effectively leverages the anorexigenic and insulinotropic effects of GLP-1 with the energy-expending and lipid-clearing properties of glucagon, resulting in superior metabolic outcomes including robust weight loss, improved glycemic control, and reduced hepatic steatosis.
Systemic blood glucose homeostasis in humans is predominantly governed by the counter-regulatory actions of insulin and glucagon [97] [5]. For decades, the pathophysiology of diabetes has been viewed primarily through the lens of insulin deficiency or resistance. However, the pivotal role of glucagon, a hormone secreted from pancreatic α-cells, is now fully recognized. Glucagon's primary function is to stimulate hepatic glucose output during fasting states via glycogenolysis and gluconeogenesis, thereby preventing hypoglycemia [5]. In T2DM, dysregulation of both insulin and glucagon secretion contributes to fasted and postprandial hyperglycemia [5].
The "incretin effect," whereby oral glucose elicits a more robust insulin response than intravenous glucose, led to the discovery and therapeutic harnessing of glucagon-like peptide-1 (GLP-1) [98]. GLP-1 is a peptide hormone secreted from intestinal L-cells that enhances glucose-stimulated insulin secretion, suppresses glucagon release, slows gastric emptying, and promotes satiety [97] [10]. The success of GLP-1 receptor agonists (GLP-1RAs) like semaglutide marked a paradigm shift in T2DM and obesity treatment [99] [100].
Despite this success, limitations remain. Not all patients achieve sufficient glycemic control or weight loss, and some experience gastrointestinal side effects. This has spurred investigation into multi-receptor agonists. The GLP-1/glucagon co-agonist approach represents a logical evolution, seeking to balance the glucose-lowering and anorexigenic effects of GLP-1 with the unique metabolic benefits of glucagon, such as increased energy expenditure and lipid oxidation [99]. This whitepaper validates this pathway by synthesizing current evidence and providing a technical framework for its continued investigation.
Mechanistic Rationale and Signaling Pathways
The therapeutic efficacy of GLP-1/glucagon co-stimulation arises from the distinct yet complementary actions of each hormone. The following diagram illustrates the integrated signaling pathways activated by a GLP-1/Glucagon co-agonist and their resulting metabolic effects.
Diagram 1. Integrated Signaling Pathways of GLP-1/Glucagon Co-stimulation. Activation of GLP-1R (green) and GCGR (blue) by a co-agonist triggers a synergistic intracellular signaling cascade, primarily via the cAMP/PKA pathway, leading to coordinated metabolic effects across multiple tissues [97] [5] [101].
Key Receptor Activation and Downstream Effects
Table 1: Tissue-Specific Actions of GLP-1 and Glucagon Receptor Activation
| Target Tissue | GLP-1 Receptor (GLP-1R) Action | Glucagon Receptor (GCGR) Action | Integrated Co-agonist Effect |
|---|---|---|---|
| Pancreatic β-cells | Enhances glucose-dependent insulin secretion; promotes β-cell proliferation and survival [97] [101]. | Minimal direct effect. | Potent insulinotropic effect, improving glycemia without hypoglycemia risk. |
| Pancreatic α-cells | Suppresses postprandial glucagon secretion [97]. | - | Counters hyperglucagonemia, contributing to reduced hepatic glucose output. |
| Liver | Minimal direct effect. | Stimulates glycogenolysis & gluconeogenesis; promotes lipid oxidation & clearance [5] [99]. | GLP-1-mediated insulin rise and glucagon suppression offsets glucagon's hyperglycemic action, allowing lipid-clearing benefits to dominate. |
| Brain | Activates hypothalamic satiety centers; modulates food reward pathways [102]. | Suppresses appetite via hepatic-vagal-brain axis; may promote thermogenesis [5] [99]. | Additive or synergistic reduction in food intake. |
| Adipose Tissue | Indirect lipolysis via central sympathetic activation [12]. | Potential indirect effects on lipid mobilization. | Enhanced lipid turnover and reduction in fat mass. |
The synergy is particularly evident in the liver. While glucagon receptor agonism acutely raises blood glucose, the concurrent GLP-1-mediated insulin secretion and glucagon suppression in the postprandial state mitigates this effect. Meanwhile, glucagon's ability to stimulate hepatic lipid oxidation and reduce intrahepatic triglyceride content is preserved, offering a significant benefit for conditions like non-alcoholic fatty liver disease (NAFLD) [99].
Quantitative Preclinical and Clinical Evidence
The validation of this pathway is supported by a growing body of quantitative data from animal models and human trials, summarized in the table below.
Table 2: Summary of Key Preclinical and Clinical Outcomes with GLP-1/Glucagon Co-agonists
| Study Model / Agent | Weight Loss | Glycemic Control | Other Metabolic Parameters | Source / Citation |
|---|---|---|---|---|
| Diet-Induced Obese Mice | ~25-30% (greater than GLP-1RA alone) | Significant improvement in glucose tolerance | ↑ Energy expenditure; ↑ lipid oxidation; reduced hepatic steatosis | [99] |
| Human Phase 2 Trial (Cotadutide) | ~5-10% (placebo-subtracted) | HbA1c reduction: ~0.5-1.0% | Significant improvement in liver enzymes (ALT), markers of fibrosis | [99] |
| Triple Agonist (GLP-1/GIP/Glucagon) | Up to ~25% in preclinical models | Superior to single GLP-1RAs | Profound reduction in liver fat; improved lipid profile | [10] [99] |
The data consistently demonstrate that co-agonists produce superior weight loss compared to selective GLP-1RAs. For example, in a landmark study, the triple agonist retatrutide (GLP-1/GIP/Glucagon) achieved an unprecedented ~24% weight loss in a phase 2 trial [10]. This supports the concept that adding glucagon receptor activity augments the catabolic and anorexigenic effects of GLP-1.
Experimental Protocols for Pathway Validation
To empirically validate the efficacy and mechanism of action of a GLP-1/glucagon co-agonist, the following experimental workflows are recommended.
In Vitro Receptor Signaling and Functional Assays
Objective: To confirm dual-receptor activation and measure downstream signaling potency and efficacy.
Detailed Methodology:
- Cell Culture: Maintain recombinant cell lines stably expressing human GLP-1R, GCGR, or both (e.g., HEK-293 or CHO cells).
- cAMP Accumulation Assay: Seed cells in 96-well plates. Treat with a concentration range of the co-agonist, reference agonists (e.g., native GLP-1 and glucagon), and vehicle control. After incubation, lyse cells and quantify intracellular cAMP levels using a commercial HTRF (Homogeneous Time-Resolved Fluorescence) or ELISA kit. This is the primary readout for receptor activation [101].
- β-Arrestin Recruitment Assay: Use a Tango or PathHunter β-arrestin recruitment assay format to determine if the co-agonist has a biased signaling profile compared to native hormones.
- Data Analysis: Generate concentration-response curves for each receptor. Calculate EC₅₀ values to determine potency and Eₘₐₓ values for efficacy relative to the native hormones.
In Vivo Efficacy Study in Rodent Models of Obesity and Diabetes
Objective: To evaluate the metabolic effects of chronic co-agonist treatment.
Detailed Methodology:
- Animal Model: Utilize 8-10 week old male C57BL/6J mice with diet-induced obesity (DIO), fed a 60% high-fat diet for 12-16 weeks.
- Study Design:
- Randomize DIO mice into groups (n=10-12/group) based on body weight and fasting blood glucose.
- Treatment groups: Vehicle control; GLP-1RA reference (e.g., liraglutide, 0.2 mg/kg); GCGR agonist reference; co-agonist (at low, mid, and high doses).
- Administer compounds via once-daily subcutaneous injection for 4-6 weeks.
- Key Outcome Measures:
- Body Weight & Food Intake: Measure and record daily.
- Glycemic Control: Perform weekly fasting glucose measurements. Conduct an oral glucose tolerance test (OGTT) and insulin tolerance test (ITT) at baseline and study end.
- Metabolic Phenotyping: In a separate cohort, use comprehensive lab animal monitoring system (CLAMS) cages in the final treatment week to measure energy expenditure (indirect calorimetry), respiratory exchange ratio (RER), and locomotor activity.
- Terminal Analysis: Collect plasma for insulin, glucagon, lipid profile, and liver enzymes. Harvest tissues (liver, fat, pancreas) for histology (H&E, Oil Red O staining) and gene/protein expression analysis (e.g., qPCR for gluconeogenic and lipid metabolism genes) [99].
The following diagram outlines the core in vivo experimental workflow.
Diagram 2. In Vivo Efficacy Study Workflow. The standardized protocol for evaluating the metabolic effects of a co-agonist in a diet-induced obese murine model, from induction and treatment to comprehensive phenotypic analysis [99].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for GLP-1/Glucagon Co-agonist Research
| Research Reagent | Function and Application | Example Vendor/Catalog Note |
|---|---|---|
| Recombinant Co-agonist Peptides | The core investigational molecules for in vitro and in vivo studies. Available as native sequences or with modifications (e.g., acylations, PEGylations) for extended half-life. | Custom synthesis from peptide manufacturers (e.g., Bachem, Peptide Institute). |
| cAMP Assay Kits | Quantify intracellular cAMP levels as a direct measure of GLP-1R and GCGR activation in cell-based assays. | HTRF cAMP kits (Cisbio) or AlphaLISA (PerkinElmer). |
| Phospho-Specific Antibodies | Detect phosphorylation of downstream signaling nodes (e.g., CREB, Akt) via Western blot to map activated pathways. | Cell Signaling Technology (e.g., pCREB Ser133 #9198). |
| Disease-Relevant Cell Lines | Engineered cell lines for receptor-specific signaling studies. | Ready-made GLP-1R/GCGR-expressing HEK-293 cells (e.g., Eurofins DiscoverX). |
| Specialized Animal Diets | Induce obesity and insulin resistance in rodent models to create a clinically relevant disease state. | Research Diets, Inc. (e.g., D12492, 60% fat). |
| Metabolic Phenotyping Systems (CLAMS) | Integrated systems to simultaneously measure energy expenditure, food intake, and locomotor activity in live rodents. | Columbus Instruments or Sable Systems. |
| Multiplex Metabolic Hormone Panels | Simultaneously measure key hormones (Insulin, Glucagon, GLP-1, GIP) from small-volume plasma samples. | Luminex xMAP or Meso Scale Discovery (MSD) panels. |
The strategic co-stimulation of GLP-1 and glucagon receptors represents a validated and highly promising therapeutic pathway for treating complex metabolic diseases. The mechanistic synergy between the anorexigenic and insulin-sensitizing effects of GLP-1 and the energy-expending and lipid-catabolic properties of glucagon translates into superior efficacy for weight loss and metabolic improvement compared to single-receptor agonists. While the initial clinical results with dual and triple agonists are compelling, the field is now advancing towards optimizing the balance of receptor activity to maximize therapeutic benefits and minimize side effects. Future research will focus on identifying biased agonists that selectively activate beneficial signaling pathways, developing oral and long-acting formulations to improve patient adherence, and expanding clinical trials to confirm long-term cardiovascular and renal safety. The GLP-1/glucagon co-agonist paradigm firmly establishes that the future of metabolic therapeutics lies in intelligently designed polypharmacology.
The management of type 2 diabetes (T2D) has evolved from a primary focus on glycemic control to a comprehensive strategy aimed at reducing macro- and microvascular complications. This paradigm shift is anchored in the understanding that dysregulation of the insulin-glucagon axis extends beyond hyperglycemia to directly contribute to cardiovascular and renal pathophysiology. Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) have emerged as pivotal therapeutic agents that not only improve glycemic control but also offer significant cardiorenal protection. This review synthesizes current evidence on the cardiovascular and renal outcomes associated with GLP-1 RAs, framed within the context of hormonal glucose regulation, and provides technical insights for research and drug development professionals.
The inherent relationship between pancreatic hormones and end-organ damage provides the mechanistic foundation for this analysis. Insulin and glucagon work in a delicate balance to maintain glucose homeostasis; insulin facilitates cellular glucose uptake and storage, while glucagon promotes hepatic glucose production during fasting states [17] [103]. In T2D, this balance is disrupted, resulting in both hyperglycemia and a cascade of metabolic disturbances that accelerate cardiovascular disease and chronic kidney disease. GLP-1 RAs, through their glucose-dependent insulinotropic and glucagon-suppressing effects, represent a pharmacologic restoration of this hormonal equilibrium with demonstrable benefits beyond glycemic control.
Molecular Mechanisms: Integrating Hormonal Signaling with End-Organ Protection
Foundation of Glucose Homeostasis
The hormonal regulation of blood glucose centers on the counterbalancing actions of insulin and glucagon. Insulin, secreted by pancreatic β-cells in response to elevated blood glucose, promotes glucose uptake in peripheral tissues (e.g., muscle and adipose) and inhibits hepatic glucose production [17] [103]. Conversely, glucagon, secreted by pancreatic α-cells during hypoglycemia or fasting, triggers hepatic glycogenolysis and gluconeogenesis to increase blood glucose levels [104]. This feedback loop maintains plasma glucose within a narrow range (80-140 mg/dL) in healthy individuals [3]. In T2D, insulin resistance and relative glucagon excess disrupt this equilibrium, leading to persistent hyperglycemia and increased cardiovascular risk.
GLP-1 Receptor Agonism: Mechanisms of Action
GLP-1 RAs mimic the action of endogenous glucagon-like peptide-1, an incretin hormone that enhances glucose-dependent insulin secretion, suppresses glucagon release, delays gastric emptying, and promotes satiety [105]. The cardiorenal benefits of GLP-1 RAs, however, extend beyond these glucose-regulating effects through multiple proposed mechanisms:
- Direct Cardiovascular Effects: GLP-1 receptors are expressed in the heart and vasculature. Activation leads to improved endothelial function, reduced oxidative stress, and enhanced nitric oxide bioavailability, which collectively improve vascular compliance and reduce atherosclerosis progression.
- Anti-inflammatory Actions: GLP-1 RAs reduce circulating levels of C-reactive protein and other inflammatory cytokines, attenuating the chronic inflammatory state associated with diabetes and its cardiovascular complications [105].
- Renal Protection: GLP-1 receptors are present in renal tissue. Agonism reduces renal inflammation, fibrosis, and oxidative stress. Additionally, GLP-1 RAs have been shown to reduce hyperfiltration and albuminuria, key drivers of diabetic kidney disease progression [106] [107].
Figure 1: Multimodal Mechanisms of GLP-1 Receptor Agonists. GLP-1 RAs exert cardiorenal benefits through direct receptor-mediated actions and secondary metabolic improvements.
Quantitative Outcomes Analysis: Comparative Efficacy Across Populations
Cardiovascular Outcomes
Evidence from randomized controlled trials and meta-analyses demonstrates consistent cardiovascular benefits with GLP-1 RA therapy, though with notable variations between specific agents and patient populations.
Table 1: Cardiovascular Outcomes of GLP-1 RAs Versus Active Comparators
| Outcome Measure | Comparison | Hazard Ratio (95% CI) | Certainty of Evidence | Key Studies |
|---|---|---|---|---|
| Composite Cardiovascular Outcomes | GLP-1 RAs vs. DPP-4 inhibitors | 0.77 (0.69-0.87) | Moderate | [108] [107] |
| Composite Cardiovascular Outcomes | GLP-1 RAs vs. basal insulin | 0.62 (0.48-0.79) | High | [108] [107] |
| Major Adverse Cardiovascular Events (MACE) | GLP-1 RAs vs. placebo in CKD | OR: 0.86 (0.74-0.99) | Moderate | [106] |
| Cardiovascular Mortality | GLP-1 RAs vs. DPP-4 inhibitors | 0.76 (0.68-0.85) | High | [108] [107] |
| Hospitalization for Heart Failure | GLP-1 RAs vs. DPP-4 inhibitors (BMI ≥25) | subdistribution HR: 0.77 (0.62-0.94) | Moderate | [109] |
| Stroke | GLP-1 RAs vs. DPP-4 inhibitors | 0.83 (0.74-0.93) | High | [108] [107] |
| Myocardial Infarction | GLP-1 RAs vs. DPP-4 inhibitors | 0.82 (0.69-0.97) | Moderate | [108] [107] |
The cardiovascular benefits of GLP-1 RAs exhibit significant modification by body mass index (BMI). A large cohort study of 97,156 patients with T2D found that GLP-1 RAs were associated with significantly lower risks of major adverse cardiovascular events, cardiovascular death, and hospitalization for heart failure specifically among patients with BMI ≥25 [109]. Restricted cubic spline analysis revealed increasing cardiovascular benefit associated with GLP-1 RAs among patients with higher BMI, suggesting a weight-dependent effect on cardiovascular outcomes.
Renal Outcomes
GLP-1 RAs consistently demonstrate renal protective effects across various patient populations and stages of chronic kidney disease.
Table 2: Renal Outcomes of GLP-1 RAs in Type 2 Diabetes
| Outcome Measure | Population | Effect Size (95% CI) | Certainty of Evidence | References |
|---|---|---|---|---|
| Composite Kidney Outcome | Baseline eGFR <60 mL/min/1.73m² | OR: 0.85 (0.77-0.94) | Moderate | [106] |
| eGFR decline >40% | Chronic kidney disease | OR: 0.76 (P=0.01) | Moderate | [106] |
| eGFR decline >50% | Chronic kidney disease | OR: 0.72 (P<0.001) | Moderate | [106] |
| Composite Kidney Outcomes | Across BMI categories | Consistent benefit | High | [109] |
| Albuminuria | Type 2 diabetes | Risk reduction | Low | [105] |
Unlike cardiovascular outcomes, the renal benefits of GLP-1 RAs appear consistent regardless of BMI status [109]. A systematic review focusing on patients with chronic kidney disease (baseline eGFR <60 mL/min/1.73m²) confirmed that GLP-1 RAs significantly reduce the risk of composite kidney outcomes with low heterogeneity, supporting their use in this vulnerable population [106].
Comparative Effectiveness Against Other Drug Classes
Network meta-analyses provide insights into the relative effectiveness of GLP-1 RAs compared to other antidiabetic agents.
Table 3: Comparative Effectiveness for Cardiorenal Outcomes in T2DM with CKD
| Therapy Class | MACE | Heart Failure | Stroke | Composite Renal Outcomes | All-Cause Mortality |
|---|---|---|---|---|---|
| SGLT2 Inhibitors | P-score: 0.93 | P-score: 1.00 | P-score: <0.83 | P-score: 0.94 | P-score: 0.83 |
| GLP-1 RAs | P-score: <0.93 | P-score: <1.00 | P-score: 0.83 | P-score: <0.94 | P-score: 0.83 |
| DPP-4 Inhibitors | Limited benefit | Limited benefit | Limited benefit | Limited benefit | Limited benefit |
SGLT2 inhibitors demonstrate superior benefit over GLP-1 RAs for heart failure and renal outcomes, while GLP-1 RAs are particularly effective for reducing myocardial infarction, macroalbuminuria, and stroke risk [110]. Both classes show similar effectiveness for reducing all-cause mortality.
Methodological Approaches in Outcome Studies
Cohort Study Design (BMI-Stratified Analysis)
Data Source and Population: The recent large-scale cohort study investigating BMI-specific outcomes utilized the Chang Gung Research Database, a multi-institutional electronic medical record database covering multiple hospitals in Taiwan [109]. The study identified 97,156 adults with T2D who initiated GLP-1 RAs or DPP-4 inhibitors between 2011 and 2022.
Inclusion/Exclusion Criteria: Key exclusion criteria included age <20 years, type 1 diabetes, heart failure with reduced ejection fraction (<40%), bariatric surgery history, prior use of SGLT2 inhibitors, missing baseline hemoglobin A1c or BMI, follow-up <90 days, and treatment switching within 90 days [109].
Propensity Score Matching: To address confounding, researchers performed 1:1 propensity score matching separately within BMI categories (<25 and ≥25) using a comprehensive set of demographic, clinical, and biochemical variables. Matching employed a nearest-neighbor algorithm with a caliper of 0.2, and covariate balance was assessed using standardized mean differences [109].
Outcome Assessment: Patients were followed from the initial dispensation date until outcome occurrence, drug switch, death, or end of the database (December 31, 2022), whichever came first. Mortality data were linked to the national death registry. Outcomes were analyzed using Cox proportional hazards models for mortality and Fine-Gray subdistribution models for nonfatal events, accounting for the competing risk of death [109].
Figure 2: Cohort Study Methodology for BMI-Stratified Analysis. The study design employed propensity score matching within BMI categories to minimize confounding.
Meta-Analysis Methodology
Search Strategy and Study Selection: The umbrella review of GLP-1 RA outcomes across health domains identified 3,145 records through systematic searches of Embase, CINAHL, Google Scholar, PubMed, and MEDLINE [105]. After screening, 17 meta-analyses of 432 randomized controlled trials were included, covering 65 outcomes across cardiovascular, metabolic, oncologic, renal, gastrointestinal, and other clinical domains.
Data Extraction and Quality Assessment: Two independent reviewers extracted data on study characteristics, outcomes, and effect sizes. Methodological quality was assessed using AMSTAR 2, and certainty of evidence was evaluated using the GRADE methodology [105].
Statistical Analysis: Individual estimates from included meta-analyses were re-analyzed using fixed-effect and random-effects models. Heterogeneity was quantified with the I-squared statistic, and evidence was synthesized across multiple outcomes to provide a comprehensive assessment of GLP-1 RA effects [105].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents for Investigating GLP-1 RA Mechanisms and Outcomes
| Reagent/Material | Application in GLP-1 RA Research | Research Context |
|---|---|---|
| GLP-1 RA Compounds (liraglutide, semaglutide, dulaglutide, exenatide) | Investigate drug-specific effects on cardiorenal outcomes | In vitro, animal models, clinical trials [109] [105] |
| Dipeptidyl Peptidase-4 (DPP-4) Inhibitors | Active comparator for cardiovascular and renal safety studies | Clinical trials, cohort studies [109] [108] |
| Propensity Score Matching Algorithms | Minimize confounding in observational studies of treatment effects | Retrospective cohort studies [109] |
| GRADE Methodology Framework | Assess certainty of evidence across multiple studies | Systematic reviews and meta-analyses [105] |
| AMSTAR 2 Tool | Evaluate methodological quality of systematic reviews | Evidence synthesis studies [105] |
| Restricted Cubic Splines | Model continuous variable relationships (e.g., BMI and outcomes) | Statistical analysis of cohort data [109] |
| Cox Proportional Hazards Models | Analyze time-to-event data for mortality outcomes | Clinical trials, cohort studies [109] |
| Fine-Gray Subdistribution Models | Analyze nonfatal events with competing risk of death | Cardiovascular outcome studies [109] |
The evidence synthesized in this review firmly establishes GLP-1 receptor agonists as foundational therapies in type 2 diabetes management with proven benefits extending beyond glycemic control to encompass significant cardiovascular and renal protection. The molecular mechanisms underlying these benefits integrate with fundamental insulin and glucagon physiology, representing a pharmacologic restoration of disrupted hormonal balance.
Future research should prioritize personalized treatment approaches that consider individual patient characteristics such as BMI, cardiovascular risk profile, and renal function. The demonstrated variation in drug-specific effects underscores the importance of agent selection based on the desired outcome profile. Additionally, long-term safety monitoring and comparative effectiveness research against emerging therapies will further refine the role of GLP-1 RAs in the evolving landscape of diabetes management. For drug development professionals, these findings highlight the importance of targeting multiple pathways within the glucose regulatory system to achieve comprehensive cardiorenal protection.
For nearly a century, diabetes management and research have been dominated by an insulinocentric perspective, which attributes the pathophysiology of diabetes primarily to insulin deficiency or resistance [5] [111]. This framework has guided therapeutic development toward insulin replacement and insulin-sensitizing approaches. However, accumulating evidence now compellingly demonstrates that this view is incomplete. The glucagonocentric hypothesis proposes that dysregulated glucagon secretion is not merely a consequence but a fundamental driver of the diabetic phenotype [111] [22]. This paradigm shift recognizes glucagon excess—rather than insulin deficiency alone—as the sine qua non of diabetes, fundamentally restructuring our understanding of disease mechanisms and opening new avenues for therapeutic intervention [111].
This re-evaluation is supported by several critical observations: (a) glucagon increases hepatic glucose and ketone production, catabolic features present in insulin deficiency; (b) hyperglucagonemia is present in every form of poorly controlled diabetes; (c) glucagon suppressors can ameliorate catabolic manifestations even during total insulin deficiency; (d) total β cell destruction in glucagon receptor–null mice does not cause diabetes; and (e) anti-insulin serum perfusion directly triggers hyperglucagonemia [111]. This evidence collectively positions α-cell dysfunction and glucagon signaling as central players in metabolic disease pathogenesis.
Glucagon Physiology and Regulatory Mechanisms
Historical Context and Fundamental Biology
Glucagon was first identified in 1922 by Charles Kimball and John Murlin as a pancreatic hyperglycemic factor and named "glucose agonist" or simply "glucagon" [5] [22]. The hormone was purified and crystallized in 1953, with its 29-amino-acid sequence identified in 1957 [5]. A critical advancement came in 1959 with Roger Unger's development of a radioimmunoassay (RIA) for glucagon, enabling precise measurement of circulating concentrations and facilitating detailed physiological studies [5] [22].
Glucagon is primarily secreted from pancreatic α-cells and acts as a key regulator of systemic energy homeostasis [5]. Its most well-characterized function involves stimulating hepatic glucose output through glycogenolysis and gluconeogenesis to maintain euglycemia during fasting states [5] [78]. Beyond glucoregulation, glucagon influences multiple metabolic pathways, including amino acid metabolism (enhancing hepatic uptake and breakdown of amino acids and ureagenesis), lipid oxidation (facilitating hepatic lipolysis and ketogenesis), appetite control, and thermogenesis [5] [22].
Molecular Regulation of Glucagon Secretion
Glucagon secretion is tightly regulated by nutrient availability, neural inputs, and paracrine factors within pancreatic islets [5] [22]. The intricate control mechanisms ensure appropriate metabolic responses to changing physiological conditions.
Table 1: Key Regulators of Glucagon Secretion
| Regulator | Source | Receptor/Pathway | Key Signaling Molecules | Effect on Glucagon |
|---|---|---|---|---|
| High Glucose | Postprandial state | β-/δ-cell paracrine signaling | ↑ Insulin, ↑ Somatostatin → ↓ cAMP, ↓ Ca²⁺ | Inhibition |
| Low Glucose | Hypoglycemia | Sympathetic activation | ↑ cAMP, ↑ PKA, ↑ Epac2, ↑ Ca²⁺ | Stimulation |
| Amino Acids | Protein intake/catabolism | GCGR feedback, amino acid sensors | mTORC1, AMPK (context-dependent) | Stimulation |
| Insulin | β-cell | Insulin receptor (IR) | PI3K-Akt signaling | Inhibition |
| Somatostatin | δ-cell | SSTR2 (on α-cell) | ↓ cAMP, ↓ Ca²⁺ | Inhibition |
| GABA | β-cell | GABAA receptor | Cl⁻ influx → Hyperpolarization | Inhibition |
| Epinephrine | Stress response | β-adrenergic receptor | ↑ cAMP → ↑ PKA, Epac2 | Stimulation |
| GLP-1 | Gut (incretin) | GLP-1R | ↓ cAMP, ↑ Insulin | Inhibition |
| GIP | Gut (incretin) | GIP receptor | ↑ cAMP | Stimulation |
| Famsin | Gut | OLFR796/OR10P1 | ER calcium release | Stimulation |
During hyperglycemic conditions, somatostatin released from pancreatic δ-cells inhibits glucagon secretion through reduced cAMP and calcium signaling [5] [22]. In contrast, hypoglycemia promotes glucagon secretion through sympathetic nervous system activation and elevated circulating amino acids [5]. The intracellular second messenger cyclic adenosine monophosphate (cAMP) serves as the primary trigger for glucagon secretion, with calcium acting as a secondary messenger [5]. During stress or exercise, sympathetic activation increases cAMP levels, triggering glucagon release by activating protein kinase A (PKA) and exchange protein directly activated by cAMP (Epac), which subsequently activate calcium channels and vesicle trafficking [5].
Intra-islet paracrine regulation represents a crucial control mechanism, with insulin, somatostatin, γ-aminobutyric acid (GABA), and zinc (co-secreted with insulin) all providing inhibitory signals to α-cells [5] [22]. Insulin interacts with its receptor on α-cells to inhibit exocytosis through PI3K–Akt–dependent pathways, while somatostatin binds to somatostatin receptor subtype 2 (SSTR2), reducing cAMP and calcium levels [5]. GABA activates GABAA receptors, leading to chloride influx and membrane hyperpolarization, while zinc influences KATP channels to promote hyperpolarization [5]. Disruption of these inhibitory pathways—common in type 2 diabetes mellitus (T2DM)—leads to paradoxical hyperglucagonemia and impaired glycemic control [5].
Signaling Pathways and Multi-Organ Effects
Figure 1: Glucagon Signaling Pathways in Hepatic and Pancreatic α-Cells. The diagram illustrates core glucagon signal transduction mechanisms, including the cAMP-PKA-Epac and PLC-IP3 pathways, along with key regulatory inputs from famsin, epinephrine, insulin, and somatostatin.
Glucagon's metabolic effects extend beyond hepatic glucose production to include multi-organ regulation of energy balance [5]. In the liver, glucagon binding to its receptor activates Gs proteins, stimulating adenylate cyclase to produce cAMP, which then activates PKA and Epac pathways, ultimately increasing hepatic glucose production [5]. Additionally, Gq-coupled receptor activation can stimulate phospholipase C (PLC), producing inositol trisphosphate (IP3) that mobilizes intracellular calcium [5].
Beyond traditional targets, glucagon affects cardiovascular function by modulating cardiac contractility, heart rate, and conduction [5]. It also acts on the brain to decrease food intake via the liver–vagal nerve–hypothalamic axis and stimulates thermogenesis through brown adipose tissue activation [5]. These diverse actions position glucagon as a systemic regulator of energy homeostasis rather than merely a counter-regulatory hormone to insulin.
Evidence Supporting the Glucagonocentric Hypothesis
Pathophysiological Evidence in Diabetes
The glucagonocentric hypothesis is substantiated by robust pathophysiological observations across diabetes spectrum. Hyperglucagonemia is a consistent feature in both type 1 (T1DM) and type 2 diabetes (T2DM), contributing significantly to fasting and postprandial hyperglycemia [5] [111]. In T1DM, the absence of endogenous insulin eliminates its paracrine inhibitory effect on α-cells, resulting in inappropriate glucagon secretion even during hyperglycemia [5] [111]. In T2DM, α-cells develop resistance to insulin-mediated suppression, leading to elevated basal and postprandial glucagon levels [5].
The liver-α-cell axis represents a crucial feedback loop that becomes dysregulated in diabetes [5]. Under physiological conditions, glucagon stimulates hepatic amino acid catabolism and ureagenesis, while amino acids subsequently stimulate glucagon secretion [5]. In diabetes, disruption of this axis can lead to hyperaminoacidemia, which further triggers excessive glucagon secretion, creating a vicious cycle that perpetuates hyperglycemia [5]. Glucagon-induced amino acid catabolism may also contribute to muscle wasting, supplying substrates for gluconeogenesis and further exacerbating hyperglycemia [5].
The profound significance of glucagon signaling is demonstrated by the remarkable finding that total β-cell destruction in glucagon receptor–null mice does not cause diabetes [111]. This compelling evidence suggests that the absence of glucagon signaling can prevent the development of diabetic phenotypes even in the complete absence of insulin, strongly supporting the central role of glucagon in diabetes pathophysiology.
Emerging Endocrine Axes: Famsin-Glucagon Signaling
Recent research has identified novel endocrine regulators of glucagon secretion, further expanding our understanding of glucagon-centric physiology. Famsin, a gut-secreted hormone, has been identified as a key regulator of fasting-induced glucagon secretion through its receptor OLFR796 (human OR10P1) [112]. This famsin-glucagon axis represents an important gut-islet-liver endocrine circuit that mediates glucose homeostasis [112].
Mechanistically, famsin binds to its receptor on pancreatic α-cells and triggers endoplasmic reticulum calcium release, thereby stimulating glucagon secretion and subsequently promoting hepatic gluconeogenesis [112]. Human genetic evidence supports the physiological relevance of this pathway, as individuals with predicted loss-of-function mutations in OR10P1 demonstrate attenuated glucagon secretion and reduced blood glucose levels [112]. This newly discovered endocrine axis provides additional evidence for the multi-organ regulatory networks centered on glucagon physiology and offers potential novel therapeutic targets for metabolic disease.
Alpha Cell Plasticity and GLP-1 Production
The traditional view of pancreatic islet cell function as strictly fixed has been challenged by the discovery of α-cell plasticity. Recent research demonstrates that α-cells can produce glucagon-like peptide-1 (GLP-1), a powerful insulinotropic hormone [21]. Using high-specificity mass spectrometry, researchers found that human α-cells produce substantial amounts of bioactive GLP-1, with production directly linked to insulin secretion [21].
In experimental models, when glucagon production was blocked, α-cells unexpectedly switched to increasing GLP-1 production, resulting in improved glucose control and enhanced insulin secretion [21]. This adaptive response reveals a built-in backup system wherein α-cells can modulate their hormonal output to maintain metabolic homeostasis. The discovery that α-cells can function as "secret GLP-1 factories" suggests they play a more dynamic role in glucose regulation than previously appreciated and represent a potential endogenous target for diabetes therapy [21].
Table 2: Experimental Evidence Supporting the Glucagonocentric Hypothesis
| Experimental Approach | Key Findings | Implications |
|---|---|---|
| Glucagon Receptor Knockout Mice | Total β-cell destruction does not cause diabetes in the absence of glucagon signaling [111] | Demonstrates glucagon signaling is essential for diabetic phenotype development |
| Glucagon Receptor Antagonists | Effectively lower blood glucose and HbA1c in diabetic patients [5] | Supports therapeutic potential of glucagon signaling inhibition |
| Famsin-OR10P1 Pathway Analysis | Human OR10P1 loss-of-function mutations associated with reduced glucagon and blood glucose [112] | Reveals novel endocrine regulator of glucagon secretion |
| Alpha Cell GLP-1 Production | Human α-cells produce bioactive GLP-1; blocking glucagon boosts GLP-1 and improves glucose control [21] | Demonstrates α-cell plasticity and alternative pathway for insulin secretion |
| Paracrine Regulation Studies | Insulin inhibits glucagon via PI3K-Akt; disruption leads to hyperglucagonemia in T2DM [5] | Elucidates intra-islet mechanisms underlying glucagon dysregulation |
Therapeutic Implications and Emerging Approaches
Glucagon-Targeted Therapies
The glucagonocentric hypothesis has stimulated development of novel therapeutic strategies targeting glucagon signaling:
Glucagon Receptor Antagonists: These agents have demonstrated efficacy in lowering blood glucose and HbA1c levels in patients with diabetes, validating the therapeutic potential of glucagon signaling inhibition [5]. However, some approaches have been associated with α-cell hyperplasia and abnormal lipid metabolism, making direct α-cell inhibition potentially more appealing [111].
Dual and Multi-Agonists: Innovative approaches include dual GLP-1/glucagon receptor agonists that simultaneously enhance insulin secretion while modulating glucagon activity [78]. The combination of insulin degludec with liraglutide (iDegLira) has demonstrated improved glycemic control compared to premixed insulin, with lower hypoglycemia risk and beneficial effects on body weight [113].
Smart Insulin Designs: Novel fusion proteins combining insulin and glucagon into a single molecule exploit the liver's natural ability to adjust hormonal responses based on glucose levels [60]. This approach creates a glucose-responsive system where "too high, insulin wins; too low, glucagon wins," potentially reducing hypoglycemia risk [60].
Alpha Cell-Directed Strategies
Rather than targeting glucagon receptors directly, alternative approaches focus on modulating α-cell function:
GLP-1-Based Therapies: Utilizing the natural inhibitory effect of GLP-1 on glucagon secretion [5]. Real-world studies demonstrate that adding GLP-1 receptor agonists to basal insulin regimens reduces diabetes complications and mortality [114].
Alpha Cell Plasticity Exploitation: Strategies to enhance the natural shift from glucagon to GLP-1 production in α-cells could leverage the body's inherent backup system for maintaining glucose control [21].
Intraislet Paracrine Signaling: Restoring normal insulin-mediated suppression of α-cells or enhancing somatostatin signaling could address fundamental defects in T2DM [5].
Research Methods and Experimental Approaches
Essential Research Reagents and Methodologies
Table 3: Research Reagent Solutions for Glucagon-Centric Investigations
| Research Tool Category | Specific Examples | Research Applications |
|---|---|---|
| Hormone Measurement Assays | High-specificity mass spectrometry for bioactive GLP-1 [21]; Radioimmunoassay (RIA) for glucagon [5] | Precise quantification of hormone levels and processing intermediates |
| Genetic Models | Glucagon receptor-null mice [111]; OLFR796/OR10P1 knockout models [112] | Determination of signaling pathway necessity and physiological functions |
| Signaling Pathway Modulators | PC2 inhibitors (blocks glucagon production); PC1 activators (enhances GLP-1 production) [21] | Investigation of hormone processing and secretion mechanisms |
| Cell Biology Tools | α-Cell lines; Primary human islet cultures; Calcium mobilization assays [112] | Study of cellular responses and secretory mechanisms |
| Receptor Binding Assays | OLFR796/OR10P1 binding assays; Glucagon receptor activation assays [112] | Characterization of ligand-receptor interactions and signaling |
Experimental Workflow for Glucagon Signaling Studies
Figure 2: Experimental Workflow for Glucagon-Centric Research. The diagram outlines an integrated approach combining genetic models, hormone measurements, signaling studies, and metabolic phenotyping to comprehensively investigate glucagon biology and therapeutic applications.
A comprehensive approach to glucagon research incorporates multiple methodological dimensions:
Genetic and Molecular Analyses: Investigation of loss-of-function mutations in human populations (e.g., OR10P1 mutations) [112] and creation of targeted genetic models to establish necessity and sufficiency of specific pathway components.
Hormone Secretion Studies: Precise measurement of glucagon and related peptides (GLP-1, GIP) using high-specificity assays under controlled nutrient conditions (fasting, feeding, hypoglycemia) [21] [22].
Signaling Pathway Characterization: Detailed mapping of intracellular cascades (cAMP, PKA, Epac, calcium mobilization) using pharmacological inhibitors, activators, and measurement of second messengers [5] [22].
Metabolic Phenotyping: Assessment of whole-body glucose homeostasis (glucose tolerance, insulin sensitivity), tissue-specific glucose flux, and hepatic glucose production using tracer methodologies [113] [111].
Therapeutic Validation: Preclinical testing of glucagon-targeted therapies in relevant disease models followed by clinical validation using continuous glucose monitoring, HbA1c, and comprehensive metabolic assessments [113] [60].
The glucagonocentric hypothesis represents a fundamental restructuring of diabetes pathophysiology that emphasizes the primary role of α-cell dysfunction and glucagon excess in driving metabolic disease [111]. This paradigm shift from traditional insulinocentric models has profound implications for both basic research and therapeutic development.
Future research directions should focus on several critical areas: (1) elucidating the precise mechanisms of α-cell dysfunction in different forms of diabetes; (2) exploring the therapeutic potential of modulating newly identified endocrine axes such as the famsin-glucagon pathway [112]; (3) leveraging α-cell plasticity to develop strategies that enhance beneficial hormone production (e.g., GLP-1) while suppressing detrimental outputs (e.g., excess glucagon) [21]; and (4) developing smarter therapeutic systems that dynamically respond to metabolic needs, such as glucose-responsive insulins with built-in glucagon counter-regulation [60].
The glucagonocentric framework provides a more comprehensive understanding of metabolic regulation that extends beyond glycemic control to include multi-organ effects on lipid metabolism, protein homeostasis, appetite regulation, and cardiovascular function [5] [22]. As research continues to unravel the complexities of glucagon biology, this paradigm will likely yield innovative approaches to diabetes management that more effectively address the fundamental pathophysiological processes driving disease progression and complications.
The regulation of blood glucose is a complex process orchestrated primarily by the counter-balancing hormones insulin and glucagon. Insulin, secreted by pancreatic β-cells, facilitates cellular glucose uptake and storage, thereby lowering blood sugar levels. In contrast, glucagon, released from pancreatic α-cells, elevates blood glucose by stimulating hepatic glycogenolysis and gluconeogenesis [17] [38]. For decades, therapeutic strategies for diabetes focused on supplementing insulin or enhancing its secretion. However, a paradigm shift is underway, moving beyond single-hormone manipulation towards multi-receptor agonism. The success of Glucagon-Like Peptide-1 Receptor Agonists (GLP-1 RAs), which enhance glucose-dependent insulin secretion and suppress glucagon release, paved the way for this new era [10] [98]. This whitepaper provides a critical appraisal of the emerging drug classes of dual and triple agonists, which harness the complementary physiology of multiple entero-pancreatic hormones—GLP-1, Glucose-dependent Insulinotropic Polypeptide (GIP), and glucagon—to achieve superior metabolic outcomes [115] [116].
Scientific Foundation of Hormonal Blood Glucose Regulation
The Insulin-Glucagon Axis
The pancreas maintains glucose homeostasis through the coordinated secretion of insulin and glucagon. When blood glucose levels rise, such as after a meal, insulin is released. It promotes the uptake of glucose into muscle and adipose tissue, stimulates glycogenesis in the liver, and inhibits gluconeogenesis [17] [3]. Conversely, during fasting or hypoglycemia, glucagon secretion increases. Its primary target is the liver, where it binds to glucagon receptors (GCGR) and activates signaling pathways that break down glycogen into glucose (glycogenolysis) and create new glucose from precursors like amino acids (gluconeogenesis) [38] [5]. This delicate balance is dysregulated in type 2 diabetes (T2DM), often characterized by insulin resistance and inappropriately elevated glucagon levels, contributing to hyperglycemia [5].
The Incretin Effect and GLP-1
The incretin effect describes the phenomenon where oral glucose administration elicits a more robust insulin response than intravenous glucose, due to the action of gut-derived hormones [98]. The two primary incretin hormones are GLP-1 and GIP. Both are secreted in response to nutrient intake and augment glucose-stimulated insulin secretion [116]. GLP-1, secreted from intestinal L-cells, has become a cornerstone of modern metabolic therapy. Its actions are mediated through the GLP-1 receptor (GLP-1R), a G protein-coupled receptor (GPCR) widely expressed in the pancreas, brain, heart, and gastrointestinal tract [10]. Activation of GLP-1R results in a cascade of beneficial effects:
- Glucose-Dependent Insulin Secretion: Increases intracellular cyclic AMP (cAMP) in pancreatic β-cells, potentiating insulin release in a glucose-dependent manner, which minimizes the risk of hypoglycemia [10] [116].
- Glucagon Suppression: Inhibits glucagon secretion from pancreatic α-cells, reducing hepatic glucose output [98].
- Appetite and Gastric Emptying: Acts on central nervous system receptors to promote satiety and delays gastric emptying, contributing to weight loss [10] [115].
Despite their efficacy, native GLP-1 has a very short half-life (<2 minutes) due to rapid degradation by the enzyme dipeptidyl peptidase-4 (DPP-4) [10]. This led to the development of degradation-resistant GLP-1 receptor agonists (GLP-1 RAs), such as liraglutide and semaglutide, which marked a significant therapeutic advance [10] [98].
Diagram 1: Hormonal regulation of blood glucose. This diagram illustrates the core regulatory network involving insulin and glucagon, and the modulatory role of incretin hormones (GLP-1 and GIP) secreted in response to food intake.
The Evolution from Single to Multi-Target Agonists
The limitations of single-target GLP-1 RAs, including variable patient response and a weight loss efficacy plateau below that of bariatric surgery, spurred the development of multi-agonists [115]. The rationale is to harness the synergistic or complementary actions of multiple hormonal pathways to achieve enhanced efficacy. This approach was inspired by the profound metabolic improvements and elevated levels of multiple gut hormones observed after bariatric surgery [115]. Two primary dual agonist classes and a nascent triple agonist class have emerged, each with a distinct pharmacological profile.
Dual GLP-1/GIP Agonists
Tirzepatide is the first-in-class dual GLP-1/GIP receptor agonist approved for T2DM and obesity. GIP is an incretin hormone secreted from K-cells in the duodenum and jejunum. While its role in T2DM pathogenesis was once debated, co-activation with GLP-1R has proven highly effective [115] [116].
Mechanism and Synergistic Effects: The precise mechanism for GIP's contribution is under investigation but is believed to include:
- Enhanced Insulin Secretion: GIP provides an additive insulinotropic effect to GLP-1 [116].
- Appetite Regulation: Preclinical data suggests GIP receptor agonism may enhance the anorectic effect of GLP-1 RAs and mitigate nausea, potentially improving tolerability [115].
- Adipose Tissue Metabolism: GIP may promote energy storage in adipose tissue, but its net effect in a dual-agonist framework appears to be catabolic, enhancing weight loss [116].
Clinical Efficacy: In the SURPASS clinical trial program, tirzepatide demonstrated superior glycemic control and weight reduction compared to selective GLP-1 RAs, including semaglutide 1 mg. In the SURMOUNT-1 trial for obesity, tirzepatide (15 mg) achieved a mean weight reduction of 20.9% at 72 weeks, a landmark outcome for pharmacotherapy [115].
Dual GLP-1/Glucagon Agonists
Agonists like survodutide and mazdutide target the receptors for GLP-1 and glucagon. This combination may seem counterintuitive given glucagon's hyperglycemic action, but the GLP-1 component effectively counterbalances potential glucose elevation while leveraging other beneficial effects of glucagon receptor activation [115] [116].
Mechanism and Synergistic Effects:
- Energy Expenditure and Thermogenesis: Glucagon activation increases energy expenditure and promotes thermogenesis in brown adipose tissue [5].
- Appetite Suppression: Glucagon exerts anorectic effects via the liver-vagal nerve-hypothalamic axis [115] [5].
- Hepatic Fat Reduction: Glucagon agonism has potent effects on reducing hepatic lipid accumulation. Phase 2 data for efinopegdutide showed a 72.7% reduction in liver fat, significantly greater than that achieved with semaglutide, even after accounting for weight loss [115]. This suggests a weight-independent benefit for metabolic dysfunction-associated steatotic liver disease (MASLD) [115].
Clinical Efficacy: Phase 2 results for survodutide (4.8 mg) demonstrated an 18.7% reduction in body weight after 46 weeks [115].
Triple GLP-1/GIP/Glucagon Agonists
Retatrutide is the most advanced triple agonist, currently in Phase 3 trials. It simultaneously activates GLP-1R, GIPR, and GCGR, aiming to deliver the full spectrum of benefits from all three pathways [115] [116].
Mechanism and Synergistic Effects: The triple agonism strategy is predicated on preclinical studies showing that activating all three receptors produces greater weight loss than mono- or dual-agonists [115]. The mechanisms are integrated:
- GLP-1 provides a strong foundation for glucose control, insulin secretion, and satiety.
- GIP is theorized to improve efficacy and potentially dampen side effects.
- Glucagon adds to weight loss by boosting energy expenditure and lipid oxidation, while its hyperglycemic potential is checked by the other two incretins.
Clinical Efficacy: Phase 2 trial data for retatrutide has been remarkable. In individuals with obesity, it achieved up to 24.2% mean weight loss after 48 weeks. In a study with T2DM patients, it resulted in 16.9% weight loss and a 2.2% reduction in HbA1c over 36 weeks. It also showed profound benefits on cardiometabolic parameters, including an 82% reduction in hepatic steatosis [115].
Table 1: Clinical Efficacy of Leading Dual and Triple Agonists vs. GLP-1 RAs
| Drug (Class) | Mechanism of Action | Weight Loss (Mean) | HbA1c Reduction | Key Clinical Trial |
|---|---|---|---|---|
| Semaglutide (GLP-1 RA) | GLP-1R Agonist | ~14.9% (68 weeks) [115] | ~1.8% [116] | STEP Program |
| Tirzepatide (Dual) | GLP-1R/GIPR Agonist | ~20.9% (72 weeks) [115] | ~2.0-2.6% [116] | SURMOUNT-1 |
| Survodutide (Dual) | GLP-1R/GCGR Agonist | ~18.7% (46 weeks) [115] | Data not specified | Phase 2 [115] |
| Retatrutide (Triple) | GLP-1R/GIPR/GCGR Agonist | ~24.2% (48 weeks) [115] | ~2.2% (36 weeks) [115] | Phase 2 [115] |
Diagram 2: Unified signaling pathway of multi-receptor agonists. Agonist binding to Class B GPCRs (GLP-1R, GIPR, GCGR) activates a common Gαs protein, triggering a cAMP-PKA signaling cascade that drives diverse metabolic effects.
Experimental Protocols for Preclinical and Clinical Evaluation
The development of dual and triple agonists requires a multi-layered experimental approach to validate mechanism of action, efficacy, and safety.
In Vitro Receptor Activation Assays
Objective: To quantify the potency and efficacy of a candidate molecule at each target receptor (e.g., GLP-1R, GIPR, GCGR). Methodology:
- Cell Line Engineering: Utilize engineered cell lines (e.g., HEK-293) stably expressing a single human GPCR of interest along with a cAMP-sensitive reporter gene (e.g., pCRE-luciferase).
- Dose-Response Treatment: Cells are treated with a serial dilution of the candidate agonist, a native hormone reference (e.g., GLP-1 for GLP-1R), and a vehicle control.
- cAMP Measurement: After incubation, cAMP production is measured indirectly via luminescence from the reporter gene or directly using ELISA/HTRF assays.
- Data Analysis: Data is used to generate dose-response curves and calculate EC₅₀ values (potency) and Eₘₐₓ values (efficacy) for the candidate molecule at each receptor, confirming its multi-target profile [116].
In Vivo Efficacy Studies in Rodent Models
Objective: To evaluate the metabolic effects of the agonist in a living organism. Methodology:
- Animal Models: Use established mouse models of obesity and diabetes (e.g., diet-induced obese (DIO) mice, ob/ob mice, or Zucker diabetic fatty (ZDF) rats).
- Dosing Regimen: Animals are randomly assigned to treatment groups: vehicle control, candidate agonist (at various doses), and a reference control (e.g., a selective GLP-1 RA). Compounds are administered daily via subcutaneous injection.
- Endpoint Monitoring: Over a study period of 4-8 weeks, track:
- Body weight and food intake daily/every other day.
- Fasting blood glucose regularly.
- An oral glucose tolerance test (OGTT) is performed at baseline and study end to assess glycemic control.
- Tissue Collection: At terminal endpoint, collect blood for HbA1c, insulin, and lipid panel analysis, and harvest tissues (liver, fat, pancreas) for histology and molecular analysis (e.g., gene expression of metabolic markers) [115] [116].
Clinical Trial Phase 2 Protocol (Weight Loss and Glycemic Control)
Objective: To establish proof-of-concept for efficacy and safety in humans. Methodology:
- Study Design: Randomized, double-blind, placebo-controlled, parallel-group trial.
- Participant Population: Adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one comorbidity, or adults with T2DM.
- Intervention: Participants are randomized to receive subcutaneous injections of placebo, the candidate agonist (at multiple dose levels), or sometimes an active comparator (e.g., semaglutide or tirzepatide). The dose is typically escalated weekly to mitigate gastrointestinal side effects.
- Primary Endpoints:
- Percent change in body weight from baseline to week 48 (or similar timepoint).
- Change in HbA1c from baseline for T2DM cohorts.
- Secondary Endpoints: Include changes in waist circumference, fasting glucose, blood pressure, lipid profile, liver fat fraction (measured by MRI-PDFF), and incidence of adverse events [115].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Investigating Multi-Agonists
| Reagent / Material | Function in Research |
|---|---|
| GPCR-Expressing Cell Lines (e.g., CHO or HEK-293 with hGLP-1R, hGIPR, hGCGR) | In vitro screening to determine a compound's potency (EC₅₀) and efficacy (Eₘₐₓ) at each target receptor [116]. |
| cAMP Detection Kits (e.g., HTRF, ELISA, or reporter gene assays) | To quantify the intracellular cAMP levels, the primary second messenger for Class B GPCR signaling, following receptor activation [116]. |
| Diet-Induced Obese (DIO) Mouse Model | A standard preclinical in vivo model for evaluating the effects of candidate drugs on body weight, food intake, and glucose metabolism in a context of obesity and insulin resistance [115]. |
| Liquid Chromatography-Mass Spectrometry (LC-MS) | Used for the bioanalysis of drug candidate concentrations in plasma and tissues, providing critical data on pharmacokinetics (half-life, exposure) [10]. |
| Magnetic Resonance Imaging-Proton Density Fat Fraction (MRI-PDFF) | A non-invasive, imaging-based biomarker to accurately quantify the percentage of fat in the liver, used to assess efficacy in treating MASLD/MASH in clinical trials [115]. |
The emergence of dual and triple agonists represents a transformative advance in the therapeutic landscape for metabolic diseases. By moving beyond single-target pharmacology, these agents leverage the synergistic biology of GLP-1, GIP, and glucagon to achieve unprecedented levels of glycemic control and weight reduction, edging closer to the efficacy of bariatric surgery. Retatrutide's phase 2 results, demonstrating over 24% weight loss, underscore the immense potential of this approach. Ongoing and future research will focus on optimizing receptor activity ratios, managing side effects (primarily gastrointestinal), and exploring the full scope of their pleiotropic benefits on the cardiovascular system, liver, and kidneys. As these sophisticated molecules progress through clinical development, they cement the principle of multi-target agonism as a cornerstone of next-generation metabolic therapy.
Conclusion
The regulation of blood glucose by insulin and glucagon is a dynamic and highly integrated process, the understanding of which has evolved from a simple counter-regulatory model to a complex network involving α-cell plasticity, multi-organ crosstalk, and systemic energy balance. Key takeaways include the validation of glucagon as a central driver of diabetic hyperglycemia and the therapeutic promise of leveraging the body's innate regulatory mechanisms, such as α-cell production of GLP-1. Future research must focus on deciphering the precise molecular switches that control hormone secretion and cell identity, developing more sophisticated biomarkers to predict disease progression, and advancing next-generation poly-agonists that optimally balance metabolic benefits. For biomedical and clinical research, this implies a continued shift towards a 'glucagonocentric' perspective and the development of personalized therapies that target the unique hormonal signature of an individual's disease, ultimately moving beyond glucose-centricity to improve comprehensive cardiometabolic outcomes.
References
- 1. Alpha cell regulation of beta cell function - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7476996/]
- 2. Pancreatic Islet Cell Hormones: Secretion, Function, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12413566/]
- 3. Physiology, Glucose Metabolism - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK560599/]
- 4. Pancreatic alpha cells and glucagon secretion [https://www.sciencedirect.com/science/article/pii/S147148922200025X]
- 5. Glucagon in metabolic disease: a mini-review of emerging ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1645041/full]
- 6. Regulation of Insulin Synthesis and Secretion and Pancreatic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3934755/]
- 7. Beta cells intrinsically sense and limit their secretory ... [https://www.sciencedirect.com/science/article/pii/S2211124725004188]
- 8. New Hormonal Pathway Links Oxytocin to Insulin Secretion ... [https://www.aging-us.com/news-room/new-hormonal-pathway-links-oxytocin-to-insulin-secretion-in-the-pancreas]
- 9. Inter-organ communication and regulation of beta cell function [https://pmc.ncbi.nlm.nih.gov/articles/PMC4801104/]
- 10. Glucagon-like peptide-1 receptor: mechanisms and ... [https://www.nature.com/articles/s41392-024-01931-z]
- 11. Shared mechanistic pathways of glucagon signalling [https://pubmed.ncbi.nlm.nih.gov/41025406/]
- 12. Mechanisms of action and therapeutic applications of GLP ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1431292/full]
- 13. Advances in Insulin Resistance—Molecular Mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11942056/]
- 14. Computational Analysis of Insulin-Glucagon Signalling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6814820/]
- 15. Glucagon receptor signaling is indispensable for the ... [https://link.springer.com/article/10.1007/s11357-025-01899-w]
- 16. The insulin-antagonistic effect of the counterregulatory ... [https://pubmed.ncbi.nlm.nih.gov/2043222/]
- 17. Insulin and glucagon: How they regulate blood sugar levels [https://www.medicalnewstoday.com/articles/316427]
- 18. Current perspective on the role of insulin and glucagon in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6515536/]
- 19. Insulin, glucagon and somatostatin stores in the pancreas ... [https://www.nature.com/articles/s41598-017-10296-z]
- 20. Insulin Secretion Depends on Intra-islet Glucagon Signaling [https://www.sciencedirect.com/science/article/pii/S2211124718315948]
- 21. Alpha Cells Moonlight as Secret GLP-1 Factories [https://medschool.duke.edu/news/alpha-cells-moonlight-secret-glp-1-factories]
- 22. Glucagon in metabolic disease: a mini-review of emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12350081/]
- 23. a novel target for modulating glucose and lipid metabolism [https://www.nature.com/articles/s41392-025-02236-5]
- 24. Neuroendocrine control of glucose homeostasis [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1731725/full]
- 25. Homeostatic Regulation of Glucose Metabolism by the ... [https://www.e-enm.org/journal/view.php?number=2263]
- 26. New research points to cell subtypes that increase risk of ... [https://medschool.vanderbilt.edu/basic-sciences/2025/07/23/new-research-points-to-cell-subtypes-that-increase-risk-of-diabetes/]
- 27. Using a lab-designed protein to regulate blood glucose ... [https://www.news-medical.net/news/20251009/Using-a-lab-designed-protein-to-regulate-blood-glucose-levels.aspx]
- 28. Human pancreatic α-cell heterogeneity and trajectory ... [https://www.nature.com/articles/s41467-025-62670-5]
- 29. Glucagon-like peptide 1 (GLP-1) - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6812410/]
- 30. What Is an L-Cell and How Do We Study the Secretory ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2021.694284/full]
- 31. α cells use both PC1/3 and PC2 to process proglucagon ... [https://pubmed.ncbi.nlm.nih.gov/40971442/]
- 32. Recent advances in pancreatic α-cell transdifferentiation ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1551372/full]
- 33. A perfect islet: reviewing recent protocol developments and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11959787/]
- 34. Clinical utility of laboratory developed mass spectrometry ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9900367/]
- 35. Recent Advances in Liquid Chromatography–Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12204688/]
- 36. Liquid chromatography mass spectrometry-based ... [https://www.sciencedirect.com/science/article/pii/S2772391724000306]
- 37. Multistage fragmentation (MS 3 ) detection enhances ... [https://www.sciencedirect.com/science/article/abs/pii/S0039914025006885]
- 38. Glucagon: What It Is, Function & Related Conditions [https://my.clevelandclinic.org/health/articles/22283-glucagon]
- 39. Physiology, Glucose - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK545201/]
- 40. Leveraging mass spectrometry for pediatric endocrine ... [https://diagnostics.roche.com/global/en/article-listing/lab-leaders/article/pediatric-endocrine-disorders-mass-spectrometry.html]
- 41. High-sensitivity quantification of serum androstenedione, ... [https://www.sciencedirect.com/science/article/abs/pii/S0960076018303236]
- 42. Combining mass spectrometry and machine learning to ... [https://www.nature.com/articles/s41467-022-34031-z]
- 43. Functional analysis of islet cells in vitro, in situ, and in vivo [https://pmc.ncbi.nlm.nih.gov/articles/PMC8155742/]
- 44. Generation of human islet cell type-specific identity genesets [https://www.nature.com/articles/s41467-022-29588-8]
- 45. Functional identification of islet cell types by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5378133/]
- 46. Regulated and adaptive in vivo insulin secretion from islets ... [https://www.nature.com/articles/s42255-024-01114-8]
- 47. In vivo imaging of β-cell function reveals glucose-mediated ... [https://elifesciences.org/articles/41540]
- 48. Functional analysis of islet cells in vitro, in situ, and in vivo [https://www.sciencedirect.com/science/article/abs/pii/S1084952118303070]
- 49. GLP-1/GIP/GCG receptor triagonist (IUB447) enhances insulin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12534261/]
- 50. Targeting the root cause of obesity-related comorbidities ... [https://www.sciencedirect.com/science/article/pii/S0753332225005827]
- 51. Cross Talk Between Insulin and Glucagon Receptor Signaling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9450567/]
- 52. Potentially novel surrogate biomarker for diagnosing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12635711/]
- 53. Biomarkers for Brain Insulin Resistance Discovered in the ... [https://www.dzd-ev.de/en/article/biomarker-fuer-insulinresistenz-des-gehirns-im-blut-entdeckt]
- 54. Dynamic multi-omics profiling of islet and gut hormonal ... [https://www.sciencedirect.com/science/article/pii/S2666379125004008]
- 55. Glucagon - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK559195/]
- 56. Glucagon (injection route) - Side effects & dosage [https://www.mayoclinic.org/drugs-supplements/glucagon-injection-route/description/drg-20064089]
- 57. About Emergency Glucagon Treatments [https://www.mskcc.org/cancer-care/patient-education/about-emergency-glucagon-treatments]
- 58. GLP-1 Agonists [https://my.clevelandclinic.org/health/treatments/13901-glp-1-agonists]
- 59. A Systematic Review and Model-Based Meta-Analysis [https://pubmed.ncbi.nlm.nih.gov/39911047/]
- 60. New 'smart insulin' shows promise in reducing low blood ... [https://medicine.iu.edu/news/2025/10/type-1-diabetes-fusion-protein]
- 61. Glucagon Receptor Antagonist - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/glucagon-receptor-antagonist]
- 62. Glucagon Receptor Signaling and Glucagon Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC6651628/]
- 63. Glucagon Signaling Pathway [https://www.cusabio.com/pathway/Glucagon-signaling-pathway.html?srsltid=AfmBOoq7tDRFCuIW6D_diL1hyBaKseGd-Gk_Oiei2E4OX8yF-VjxYfpV]
- 64. What are GCGR antagonists and how do they work? [https://synapse.patsnap.com/article/what-are-gcgr-antagonists-and-how-do-they-work]
- 65. Glucagon receptor antagonism induces increased ... [https://pubmed.ncbi.nlm.nih.gov/26373568/]
- 66. Glucagon-like Peptide-1 Receptor (GLP-1R) Signaling [https://pmc.ncbi.nlm.nih.gov/articles/PMC12347461/]
- 67. U of A scientists link calorie restriction, glucagon, healthy aging [https://research.arizona.edu/news/u-scientists-link-calorie-restriction-glucagon-healthy-aging]
- 68. Glucagon-Like Peptide-1 Receptor Agonists - StatPearls - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK551568/]
- 69. Role of Glucagon and Its Receptor in the Pathogenesis ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2022.928016/full]
- 70. Current Insights and New Perspectives on the Roles of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3810031/]
- 71. Glucagon, a key factor in the pathophysiology of type 2 ... [https://www.sciencedirect.com/science/article/abs/pii/S0300908417302468]
- 72. Q&A: insulin secretion and type 2 diabetes: why do β-cells fail? [https://pmc.ncbi.nlm.nih.gov/articles/PMC4435650/]
- 73. Insulin Resistance: What It Is, Causes, Symptoms ... [https://my.clevelandclinic.org/health/diseases/22206-insulin-resistance]
- 74. Insulin Resistance - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK507839/]
- 75. Insulin Resistance and Diabetes | ADA [https://diabetes.org/health-wellness/insulin-resistance]
- 76. Modeling diabetic alpha cell dysfunction using stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181959/]
- 77. Evaluating the role of alpha cell dysregulation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12534288/]
- 78. Glucagon in glucose homeostasis and metabolic disease [https://pubmed.ncbi.nlm.nih.gov/40314189/]
- 79. How to Measure Glycemic Variability? A Literature Review [https://www.mdpi.com/1648-9144/60/1/61]
- 80. Glycemic Variability: How to Measure and Its Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6709582/]
- 81. Glycemic Variability and Its Association with Traditional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11989622/]
- 82. Glycemic variability assessed using continuous glucose ... [https://www.sciencedirect.com/science/article/pii/S0261561424000566]
- 83. Drug-induced low blood sugar [https://medlineplus.gov/ency/article/000310.htm]
- 84. Hypoglycemia - Symptoms and causes [https://www.mayoclinic.org/diseases-conditions/hypoglycemia/symptoms-causes/syc-20373685]
- 85. Diabetes treatment in 2025: can scientific advances keep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3498849/]
- 86. Event-triggered smart dual hormone artificial pancreas for ... [https://www.nature.com/articles/s41598-025-18085-9]
- 87. Regulation of LEAP2 by insulin and glucagon in mice and ... [https://pubmed.ncbi.nlm.nih.gov/40056903/]
- 88. Revolutionizing Hypoglycemia Management in Long-Term Care [https://diabetes.jmir.org/2025/1/e73485]
- 89. The Liver–α-Cell Axis in Health and in Disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9862287/]
- 90. Insights into the Roles of GLP-1, DPP-4, and SGLT2 at the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11898734/]
- 91. Pancreas Hormones [https://www.endocrine.org/patient-engagement/endocrine-library/hormones-and-endocrine-function/pancreas-hormones]
- 92. How Do Insulin and Glucagon Regulate Blood Sugar Levels? [https://www.tandemclinicalresearch.com/blog/how-does-insulin-work/]
- 93. Blood glucose regulation and control of insulin and glucagon ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8687336/]
- 94. Efficacy and safety of combination therapy using SGLT2 ... [https://pubmed.ncbi.nlm.nih.gov/40555695/]
- 95. Comparison of monotherapy and combination therapy for ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14014-1]
- 96. a retrospective cohort study - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12046949/]
- 97. Regulation of Glucose Homeostasis by GLP-1 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4159612/]
- 98. Current Perspectives on GLP-1 Agonists in Contemporary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511252/]
- 99. GLP-1, GIP and glucagon receptor poly-agonists [https://pmc.ncbi.nlm.nih.gov/articles/PMC9420816/]
- 100. Review The expanding role of GLP-1 receptor agonists [https://www.sciencedirect.com/science/article/pii/S2589537025002950]
- 101. GLP-1R in diabetes mellitus: from basic discovery to ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1610512/full]
- 102. Glucagon-Like Peptide-1 and Hypothalamic Regulation of ... [http://e-dmj.org/journal/view.php?doi=10.4093/dmj.2025.0106]
- 103. Insulin and Glucagon: How Do They Work? [https://www.healthline.com/health/diabetes/insulin-and-glucagon]
- 104. Glucagon Physiology - Endotext - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK279127/]
- 105. Study compares GLP-1 drug benefits and finds substantial ... [https://www.news-medical.net/news/20251120/Study-compares-GLP-1-drug-benefits-and-finds-substantial-variation-in-clinical-effects.aspx]
- 106. Kidney and Cardiovascular Outcomes Among Patients ... [https://www.sciencedirect.com/science/article/pii/S0272638625000423]
- 107. Cardiovascular and renal outcomes of GLP-1 receptor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10734357/]
- 108. Cardiovascular and renal outcomes of GLP-1 receptor ... [https://pubmed.ncbi.nlm.nih.gov/38111352/]
- 109. GLP-1 RAs and Cardiovascular and Kidney Outcomes by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12418133/]
- 110. Comparative analysis on renal and cardiovascular ... [https://pubmed.ncbi.nlm.nih.gov/40798873/]
- 111. Glucagonocentric restructuring of diabetes - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3248306/]
- 112. A famsin-glucagon axis mediates glucose homeostasis [https://www.sciencedirect.com/science/article/abs/pii/S1550413124004546]
- 113. Switch from premixed insulin analogue to degludec ... [https://pubmed.ncbi.nlm.nih.gov/41268167/]
- 114. Effectiveness of adding glucagon-like peptide-1 receptor ... [https://www.sciencedirect.com/science/article/pii/S1056872725000364]
- 115. Triple Agonism Based Therapies for Obesity - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12304053/]
- 116. Next generation dual GLP-1/GIP, GLP-1/glucagon, and ... [https://www.sciencedirect.com/science/article/abs/pii/S0939475325003679]