Insulin Analogs in Diabetes Management: A Comprehensive PK/PD Analysis for Drug Development
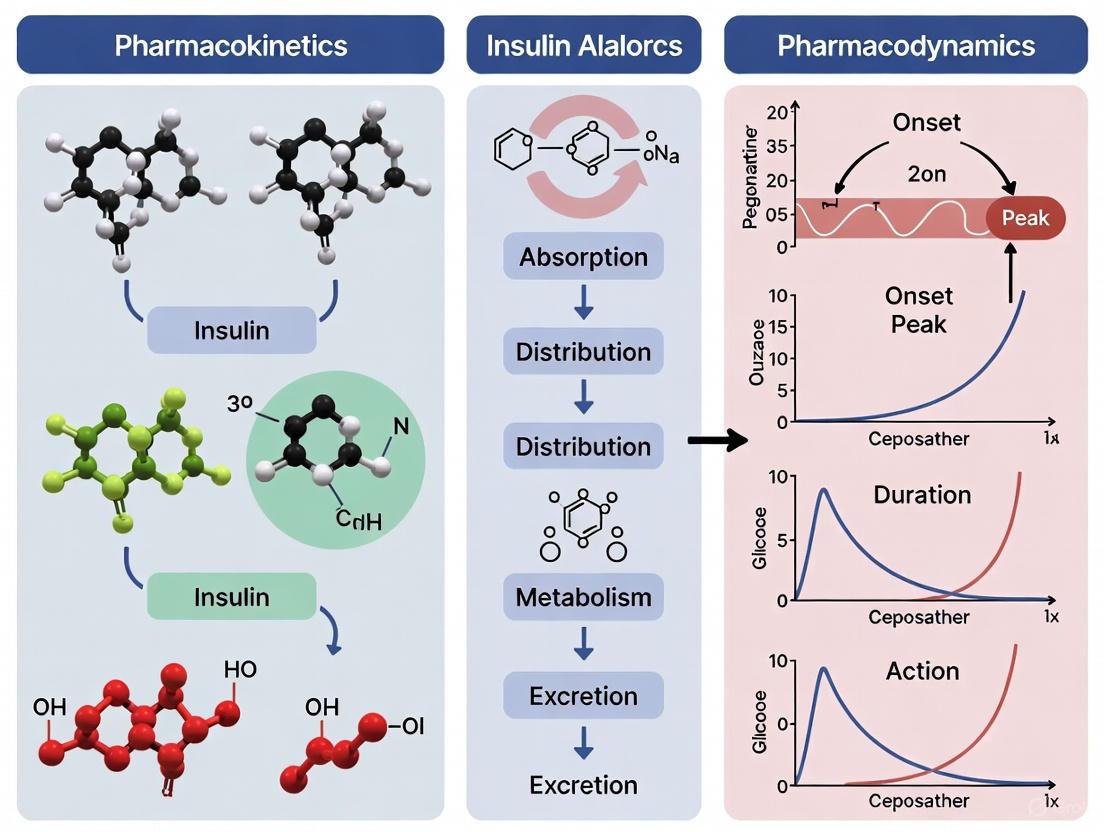
This article provides a comprehensive analysis of the pharmacokinetic (PK) and pharmacodynamic (PD) properties of modern insulin analogs, tailored for researchers and drug development professionals.
Insulin Analogs in Diabetes Management: A Comprehensive PK/PD Analysis for Drug Development
Abstract
This article provides a comprehensive analysis of the pharmacokinetic (PK) and pharmacodynamic (PD) properties of modern insulin analogs, tailored for researchers and drug development professionals. It explores the foundational principles of insulin analog design, from rapid-acting to ultra-long-acting formulations, and examines the advanced methodologies, including euglycemic clamp studies and mechanism-based PK/PD modeling, used to characterize their efficacy. The content addresses key challenges such as hypoglycemia risk, variability in drug response, and stability issues, while offering optimization strategies for clinical translation. Finally, it presents a comparative evaluation of existing and next-generation analogs, including once-weekly insulins, discussing their validation and implications for future therapeutic development and personalized diabetes treatment regimens.
Engineering Physiologic Profiles: The Structural Basis of Insulin Analog Design
The management of diabetes has been fundamentally shaped by the continuous pursuit of insulin formulations that more closely mimic the body's natural physiologic insulin secretion. Since its landmark discovery and first use in 1922, insulin therapy has evolved through remarkable scientific milestones—from animal-sourced insulins to recombinant human insulin and, most significantly, to the development of structurally engineered analogs with tailored pharmacokinetic properties. This evolution has been driven by the recognition that the pharmacokinetic and pharmacodynamic (PK/PD) profiles of traditional human insulin preparations do not adequately replicate the precise temporal pattern of endogenous insulin release, which consists of both basal background secretion and rapid prandial bursts.
The limitations of regular human insulin—characterized by a delayed onset and prolonged duration of action—created challenges in achieving optimal glycemic control without increasing hypoglycemia risk. The advent of recombinant DNA technology enabled protein engineering to modify the insulin molecule itself, leading to analogs designed to overcome these limitations. These designer analogs can be broadly categorized into rapid-acting formulations that accelerate subcutaneous absorption for mealtime coverage and long-acting formulations that provide a flat, stable basal insulin supply. This guide provides a comprehensive comparison of the performance characteristics of these insulin analogs, underpinned by experimental data and detailed methodologies essential for research and development professionals working at the forefront of metabolic therapeutics.
Comparative Pharmacokinetic and Pharmacodynamic Profiles
The clinical utility of any insulin preparation is determined by its absorption, distribution, and elimination characteristics, collectively known as pharmacokinetics (PK), and its subsequent glucose-lowering effects, or pharmacodynamics (PD). The following tables synthesize quantitative data from head-to-head comparative studies, euglycemic clamp experiments, and meta-analyses to provide a structured overview of the established and emerging insulin analogs.
Table 1: Pharmacokinetic Properties of Insulin Analogs and Formulations
| Insulin Type | Representative Products | Onset of Action | Peak Concentration (T~max~) | Effective Duration |
|---|---|---|---|---|
| Ultra-Rapid Analogs | Fast-acting insulin aspart (FIASP), Ultra-rapid lispro (URLi) | ~5-15 minutes | 30-60 minutes | 3-5 hours |
| Rapid-Acting Analogs | Insulin aspart, lispro, glulisine | 15-30 minutes | 1-2 hours | 3-5 hours |
| Short-Acting (Regular) | Human insulin | 30-60 minutes | 2-4 hours | 6-8 hours |
| Intermediate-Acting | NPH insulin | 1-3 hours | 5-8 hours | 13-18 hours |
| Long-Acting Analogs | Glargine U-100, Detemir, Degludec | 1-4 hours | Relatively flat | 18-24 hours (Detemir) to >42 hours (Degludec) |
| Once-Weekly Analog | Insulin Efsitora alfa (LY3209590) | ~1 day | Low peak-to-trough ratio (1.13) | ~7 days (Half-life: 15-16 days) |
The data in Table 1 illustrate how analog engineering has successfully modulated the absorption profile. Rapid-acting analogs achieve faster onset and higher peak concentrations by resisting hexamer formation, while long-acting analogs utilize strategies like albumin binding (detemir) and multi-hexamer formation (degludec, glargine) to create a stable, depot effect. The recent development of once-weekly insulin Efsitora alfa, with a half-life of 15-16 days and a low peak-to-trough ratio of 1.13, represents a significant advance in reducing dosing frequency and glycemic variability [1].
Table 2: Pharmacodynamic Outcomes from Comparative Clinical Studies
| Comparison | Study Design | Key Efficacy Endpoint (Mean Difference) | Key Safety Endpoint | Source |
|---|---|---|---|---|
| AID-URAI vs. AID-RAI | Meta-analysis of 16 RCTs (n=664, T1D) | TIR: +1.07% (95% CI: 0.11 to 2.02), p=0.029 | TBR (<3.9 mmol/L): -0.35% | [2] |
| URAIs (FIASP/URLi) vs. RAIs | Multiple RCTs in Automated Insulin Delivery (AID) | Improved postprandial glucose control | No increased risk of severe hypoglycemia or DKA | [2] |
| Generic vs. Brand Lispro 25 | Randomized crossover (n=52, healthy) | GIR~max~: 4.47 vs 4.12 mg/kg/min (T vs R) | No significant hypoglycemia or SAEs; Bioequivalence demonstrated | [3] |
| Oral ORMD-0801 (16 mg) vs. SC Insulin | Phase I clamp (n=20, healthy) | GIR~max~: 3.87 vs 3.51 mg/kg/minAUC~GIR0-11h~: 26.98 vs 23.74 h·mg/kg/min | SC-equivalent dose: 6.53 ± 3.97 IU | [4] |
| Once-Weekly Efsitora | Phase I/II in T2D (Japanese cohort) | Decreased fasting glucose with single doses (5-20 mg); Stable glycemic control with multi-dose | No severe hypoglycemic events; All AEs mild and unrelated | [1] |
The pharmacodynamic outcomes in Table 2 highlight subtle but meaningful clinical differences. Automated insulin delivery (AID) systems using ultra-rapid-acting analogs (URAIs) show a small but statistically significant improvement in Time-in-Range (TIR) without increasing hypoglycemia risk [2]. Bioequivalence studies confirm that generic insulin lispro products have nearly identical PK/PD profiles to their brand-name counterparts, supporting their interchangeability and potential to reduce healthcare costs [3]. Investigations into novel delivery routes, such as oral insulin ORMD-0801, demonstrate measurable pharmacodynamic effects, though with low relative bioavailability (0.53-0.94%) [4].
Experimental Protocols: The Gold Standard for Insulin Assessment
The Euglycemic Glucose Clamp Technique
The euglycemic glucose clamp remains the gold standard methodology for rigorously characterizing the PK/PD properties of insulin formulations. It allows for the precise quantification of insulin action by maintaining a constant plasma glucose level, thereby isolating the drug's effect from confounding metabolic variables.
Detailed Clamp Procedure: As implemented in a bioequivalence study of insulin lispro [3], the protocol involves:
- Subject Preparation: Healthy male volunteers (n=52) are fasted overnight. Baseline blood samples are collected for glucose and C-peptide measurement to confirm endogenous insulin suppression during the clamp.
- Insulin Administration: A single subcutaneous dose (0.3 IU/kg) of the test or reference insulin preparation is administered.
- Glucose Clamping: Blood glucose is measured frequently (e.g., every 5-120 minutes over 24 hours). A variable 20% glucose solution is infused intravenously at a rate adjusted to maintain the target blood glucose level (typically within ±10% of the baseline minus 0.28 mmol/L) [3].
- Pharmacokinetic Sampling: Blood is drawn at predetermined time points (e.g., -30 min to 24h post-dose) to measure plasma insulin analog concentration using high-performance liquid chromatography-mass spectrometry (HPLC-MS) [3].
- Data Analysis: The primary pharmacodynamic endpoint is the Glucose Infusion Rate (GIR) over time. Key parameters include:
- GIR~max~: The maximum glucose infusion rate, reflecting peak insulin action.
- AUC~GIR0-t~: The area under the GIR-time curve, reflecting the total glucose-lowering effect.
- PK parameters like C~max~ (maximum concentration) and AUC~Ins0-t~ (total exposure) are calculated from the plasma insulin concentration data.
Automated Insulin Delivery (AID) System Trials
For evaluating insulins in a clinically relevant setting, randomized controlled trials (RCTs) of AID systems (closed-loop systems) are employed.
Standard Protocol [2]:
- Participant Recruitment: Patients with type 1 diabetes are recruited and their existing insulin therapy is stabilized.
- Randomization & Intervention: Participants are randomized to use an AID system configured with either an ultra-rapid-acting insulin (URAI) or a standard rapid-acting insulin (RAI) for the trial duration.
- Outcome Measurement: The primary outcome is typically the percentage of Time-in-Range (TIR), defined as the duration spent in a glucose range of 3.9-10.0 mmol/L, as measured by continuous glucose monitoring (CGM). Key secondary outcomes include Time-Below-Range (TBR), Time-Above-Range (TAR), and the incidence of severe hypoglycemia or diabetic ketoacidosis (DKA).
- Meta-Analysis: Data from multiple RCTs are pooled in a meta-analysis to provide a higher level of evidence, as seen in the 2025 analysis that included 16 trials and 664 participants [2].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for Insulin PK/PD Research
| Item | Specific Example | Function in Research |
|---|---|---|
| Recombinant Insulin Analogs | Insulin aspart, lispro, glulisine, glargine, degludec | The active pharmaceutical ingredients under investigation for their PK/PD properties. |
| Euglycemic Clamp System | Variable IV glucose infusion pump, frequent glucose analyzer (e.g., glucose oxidase method) | The core experimental setup for measuring the pharmacodynamic effect of insulin via the Glucose Infusion Rate (GIR). |
| Analytical Chromatography | High-Performance Liquid Chromatography (HPLC) system with Mass Spectrometer (LC-MS/MS) | Gold standard for precise quantification of insulin analog concentrations in plasma for pharmacokinetic analysis [3]. |
| Immunoassays | Enzyme-Linked Immunosorbent Assay (ELISA) for C-peptide and insulin | Used to monitor endogenous insulin suppression (via C-peptide) and measure insulin levels in biological samples [3]. |
| Continuous Glucose Monitors (CGM) | Commercial CGM systems (e.g., Dexcom, Medtronic) | Provides high-resolution, real-world glycemic data (TIR, TBR, TAR) in outpatient clinical trials [2]. |
| Animal Models | Rats, Dogs, Pigs (non-diabetic and diabetic strains) | Used in pre-clinical studies to characterize initial PK/PD profiles and assess safety before human trials [5]. |
| PK/PD Modeling Software | MONOLIX, WinNonlin | Industry-standard software for non-linear mixed-effect modeling and bioequivalence analysis of complex PK/PD data [6] [3]. |
Molecular Mechanisms of Action and Signaling Pathways
Despite structural modifications, insulin analogs primarily exert their effects through the same fundamental mechanism as native human insulin: binding to and activating the insulin receptor (IR). The metabolic effects are mediated through downstream signaling pathways that promote glucose uptake and utilization.
Key Mechanistic Insights:
- Receptor Binding and Specificity: While engineered for altered pharmacokinetics, most analogs retain high specificity for the insulin receptor. However, minor structural changes can affect their binding affinity to the Insulin-like Growth Factor-1 Receptor (IGF-1R), a phenomenon investigated for its potential mitogenic implications. For instance, insulin glargine's metabolites exhibit a lower IGF-1R binding affinity compared to human insulin, whereas insulin detemir and degludec have a reduced affinity [7].
- Downstream Consequences: Activation of the PI3K/Akt pathway is responsible for the primary metabolic effects, including stimulation of glucose transporter (GLUT4) translocation to the cell membrane, enhancing cellular glucose uptake. Activation of the MAPK pathway can influence cell growth and proliferation [7].
- Mitogenic Potency: In vitro assessments are conducted to compare the mitogenic potency of analogs relative to human insulin. These studies have shown that insulin glargine has a higher mitogenic potency, attributed to its increased IGF-1R affinity, though its active metabolites (M1) exhibit a lower affinity. The long-term clinical significance of these in vitro findings remains unclear, as large epidemiological studies have not confirmed an associated increased cancer risk in patients [7].
The pursuit of physiologic insulin secretion has driven the development of a sophisticated arsenal of insulin analogs, each engineered with distinct PK/PD profiles to meet specific therapeutic needs. The experimental data clearly demonstrate that ultra-rapid analogs offer incremental improvements in postprandial glucose and time-in-range within AID systems, while long-acting and weekly analogs provide more stable basal coverage with reduced injection burden. The gold-standard euglycemic clamp methodology continues to be indispensable for the precise characterization of these properties during drug development.
Future innovation will likely focus on further optimizing the kinetic profiles of prandial insulins, extending the duration of basal insulins, and exploring non-invasive delivery systems like oral insulin. Furthermore, the integration of these advanced analogs with increasingly intelligent automated delivery systems represents the most promising path toward achieving fully physiologic insulin replacement, ultimately improving the quality of life for millions of people with diabetes worldwide.
The strategic engineering of insulin analogs through amino acid modifications represents a cornerstone of modern therapeutic development for diabetes mellitus. These deliberate structural alterations aim to optimize pharmacokinetic (PK) and pharmacodynamic (PD) profiles by fundamentally changing the self-association behavior of insulin molecules. This guide provides a comparative analysis of engineered insulin analogs, detailing how specific amino acid substitutions impact oligomerization, stability, and ultimately, clinical efficacy. We summarize critical experimental data and methodologies used to characterize these analogs, offering a resource for researchers and drug development professionals engaged in protein engineering and therapeutic design.
Insulin is a peptide hormone that exists in various states of self-assembly—monomers, dimers, and hexamers—with the monomer being the biologically active form capable of crossing the vascular endothelium [8]. In native human insulin, the propensity to form hexamers is a significant rate-limiting step for absorption after subcutaneous injection, leading to delays in its metabolic action [8]. Molecular engineering of insulin analogs focuses on introducing specific amino acid modifications to alter these self-association properties, thereby creating fast-acting or long-acting therapeutic profiles that more closely mimic physiological insulin secretion [9] [10].
The rationale for these structural changes is rooted in the thermodynamics of protein-protein interactions. By destabilizing dimer and hexamer formation, rapid-acting analogs are absorbed more quickly. Conversely, strategies that stabilize hexamers or promote precipitation at physiological pH lead to a prolonged release of insulin, forming the basis for long-acting basal analogs [11] [10]. This guide systematically compares these engineering strategies, their outcomes on self-association, and the experimental paradigms used to validate them.
Comparative Analysis of Insulin Analog Engineering
The following section provides a detailed comparison of how different amino acid modifications lead to distinct pharmacokinetic and pharmacodynamic outcomes.
Table 1: Comparison of Rapid-Acting Insulin Analogs and Their Engineering Strategies
| Analog Name | Amino Acid Modifications | Impact on Self-Association | Key Pharmacokinetic (PK) & Pharmacodynamic (PD) Outcomes | Primary Experimental Evidence |
|---|---|---|---|---|
| Insulin Lispro | Reversal of proline (B28) and lysine (B29) on the B-chain [8]. | Weakens self-association; reduces dimerization constant 200-300 fold vs. human insulin [8]. | PK: Peak serum concentration at ~42 min [10].PD: Time to peak action ~99 min; reduced postprandial glucose excursions [8]. | Euglycemic clamp studies in healthy subjects [10]. |
| Insulin Aspart | Proline at B28 replaced with aspartic acid [8]. | Reduces self-association of monomers; hexamers dissociate rapidly [8]. | PK: Absorbed twice as quickly as human insulin [10].PD: Time to peak action ~94 min [8]. | Double-blind, crossover euglycemic clamp trials [8]. |
| Insulin Glulisine | Asparagine at B3 replaced with lysine; lysine at B29 replaced with glutamic acid [9] [8]. | Introduces charge repulsion; decreases isoelectric point (pI) to 5.1, enhancing solubility and reducing hexamer formation [9] [11]. | PK: Onset of absorption 20-30 min earlier than human insulin [8].PD: Shorter duration of action [9]. | Euglycemic clamp studies comparing absorption rates [8]. |
Table 2: Comparison of Long-Acting Insulin Analogs and Their Engineering Strategies
| Analog Name | Amino Acid Modifications | Impact on Self-Association/Formulation | Key Pharmacokinetic (PK) & Pharmacodynamic (PD) Outcomes | Primary Experimental Evidence |
|---|---|---|---|---|
| Insulin Glargine | Glycine for asparagine at A21; two arginines added to B-chain C-terminus (B31 and B32) [9] [8]. | Shifts isoelectric point from pH 5.4 to 6.7, causing precipitation at physiological pH for prolonged release [8] [10]. | PK: Slow, consistent release over ~24 hours [8].PD: Relatively peakless, flat action profile [10]. | Clinical trials comparing time-action profiles vs. NPH insulin [8]. |
| Insulin Detemir | Threonine at B30 removed; lysine at B29 acylated with a myristic acid (C14) chain [9] [10]. | Promotes increased self-association and reversible albumin binding via the fatty acid chain, buffering plasma concentration [8] [10]. | PK: Protracted action via albumin binding [10].PD: Duration of action up to 24 hours; reduced within-subject variability [8]. | Euglycemic clamp studies and variability analyses [8]. |
| Insulin Icodec | (Not detailed in results, but mentioned as a once-weekly analog) [12]. | Engineered for strong albumin binding and stable depot formation for ultra-long action [12]. | PK: Once-weekly subcutaneous administration [12].PD: Sustained glycemic control over 7 days [12]. | PK/PD modeling analysis of phase 3a ONWARDS trials [12]. |
Experimental Protocols for Characterizing Self-Association and Efficacy
Robust experimental methodologies are critical for validating the engineered properties of insulin analogs. The following protocols are standards in the field.
Analytical Ultracentrifugation
- Purpose: To directly monitor the self-association properties of insulin analogs under various formulation conditions (e.g., with zinc ions or phenolic preservatives like m-cresol) [13].
- Protocol Details: Equilibrium and velocity analytical ultracentrifugation are employed. The process involves subjecting insulin samples to a high centrifugal force. Sedimentation velocity experiments measure the rate at which molecules move, providing the apparent sedimentation coefficient (s*). For instance, under formulation conditions with zinc and m-cresol, insulin analogs typically sediment at 2.9-3.1 S, corresponding to the hexameric form [13].
- Key Findings: Studies have demonstrated that despite mutations that destabilize self-assembly (e.g., in the B27-B29 region), the presence of both zinc and m-cresol can override these effects, stabilizing the hexameric structure necessary for formulation [13].
Euglycemic Glucose Clamp
- Purpose: Considered the gold standard for assessing the pharmacodynamic (PD) profile of insulin analogs by measuring the glucose infusion rate (GIR) required to maintain stable blood glucose levels after insulin administration [6] [3].
- Protocol Details: This is often conducted in healthy volunteers or patients in a clinical setting. After a subcutaneous injection of the test insulin analog, blood glucose levels are frequently monitored (e.g., every 5-10 minutes initially). A variable intravenous infusion of glucose is adjusted in real-time to maintain euglycemia. The GIR is recorded over time (e.g., 24 hours) to generate a time-action profile [3].
- Data Output: Key PD parameters include the maximum GIR (GIRmax) and the area under the GIR curve (GIRAUC), which reflect the potency and overall activity of the insulin, respectively. The time to peak GIR indicates the onset of action [6] [3]. This method was pivotal in showing that rapid-acting analogs like lispro and aspart have a significantly earlier and higher peak activity compared to regular human insulin [8] [10].
Pharmacokinetic/Pharmacodynamic (PK/PD) Modeling
- Purpose: To develop mechanistic models that link insulin pharmacokinetics (serum concentration over time) to its pharmacodynamic effects (glucose utilization) [6].
- Protocol Details: Data from euglycemic clamp studies are digitized and modeled using specialized software like MONOLIX. The PK model often describes subcutaneous absorption via sequential first-order processes and linear elimination. The PD component can use indirect response models to capture the maximum glucose stimulation (Smax) and the insulin concentration producing 50% of Smax (SC50) [6].
- Application: These models allow for the quantitative comparison of different insulin analogs and can predict outcomes in clinical scenarios, such as switching from daily basal insulin to once-weekly icodec [12].
Self-Association Interactions using Mass Spectrometry (SIMSTEX)
- Purpose: To determine self-association equilibrium constants for proteins and their analogs in solution [14].
- Protocol Details: SIMSTEX is a variation of the PLIMSTEX technique. It involves titrating a protein into a solution and using hydrogen/deuterium exchange (H/D exchange) mass spectrometry to monitor the kinetics of deuterium uptake. The changes in exchange rates are fit to a model to determine affinity constants for self-association [14].
- Key Findings: This method has shown that mutants like insulin lispro and AspB9 have a lower propensity for self-association, correlating with faster action in vivo, while others like GlnB13 have an increased tendency to associate, potentially slowing their action [14].
Visualization of Key Concepts
Insulin Signaling Pathway and Cellular Glucose Uptake
The following diagram illustrates the canonical insulin signaling pathway that is activated upon binding of insulin monomers to its receptor, culminating in glucose uptake.
(Diagram Title: Insulin Signaling and GLUT4 Translocation Pathway)
Experimental Workflow for Insulin Analog Characterization
This diagram outlines a logical workflow for the key experimental methods used in the development and characterization of engineered insulin analogs.
(Diagram Title: Insulin Analog R&D Experimental Workflow)
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists key reagents and their critical functions in insulin analog research, as derived from the experimental protocols cited.
Table 3: Key Research Reagent Solutions for Insulin Analog Studies
| Reagent / Material | Function in Research | Example Context from Literature |
|---|---|---|
| Zinc Ions (Zn²⁺) | Promotes and stabilizes the formation of insulin hexamers in formulations, which is crucial for the delayed absorption of certain analogs [13] [9]. | Used in formulations of insulin glargine and is a key component in ultracentrifugation studies to mimic formulation conditions [13] [8]. |
| Phenolic Preservatives (e.g., m-cresol) | Acts as a ligand that binds to insulin and stabilizes the hexameric conformation, overriding destabilizing mutations in rapid-acting analogs for shelf stability [13]. | Critical in analytical ultracentrifugation experiments to demonstrate hexamer formation under formulation conditions [13]. |
| Protamine | A protein used to complex with insulin, forming a suspension that delays absorption; used in NPH insulin and premixed analog formulations [3] [10]. | A key component in premixed analogs like insulin lispro protamine suspension [3]. |
| Recombinant Protein Expression Systems (e.g., E. coli) | Enable the large-scale production of recombinant human insulin and its engineered analogs, ensuring purity and consistency for research and therapy [11]. | The foundational technology that enabled the production of the first FDA-approved recombinant insulin, Humulin [11]. |
| Albumin | A serum protein used in in vitro assays to study the binding and protracted mechanism of action of albumin-binding analogs like insulin detemir [10]. | The binding of insulin detemir to albumin is a key part of its prolonged duration and reduced variability [8] [10]. |
The strategic application of amino acid modifications has enabled the rational design of insulin analogs with tailored dissociation kinetics and therapeutic profiles. As evidenced by the comparative data, single or double substitutions in the B-chain are sufficient to profoundly alter self-association, enabling either rapid postprandial coverage or sustained basal activity. The continued evolution of this field—exemplified by the emergence of once-weekly basal insulins and glucose-responsive analogs—relies on the sophisticated experimental toolkit outlined herein, including advanced biophysical characterization, clinical clamp studies, and mechanistic PK/PD modeling. Future engineering efforts will likely leverage these established principles to further enhance the stability, safety, and physiological fidelity of insulin replacement therapy.
The management of diabetes mellitus relies heavily on insulin therapy, with ongoing research focused on developing analogs that more closely mimic physiological insulin secretion. The fundamental goal of insulin analog design is to optimize pharmacokinetic (PK) profiles—how the body affects a drug—and pharmacodynamic (PD) responses—how the drug affects the body—to achieve superior glycaemic control while minimizing adverse effects, particularly hypoglycaemia [15]. Over the last two decades, significant developments in insulin pharmacology have produced analogs with improved PK and PD properties that better replicate physiological insulin patterns in the liver, skeletal muscle, and other tissues [15].
Insulin analogs are strategically engineered through molecular modifications of the native insulin structure, altering properties such as self-assembly, solubility, and receptor binding affinity [16]. These modifications yield formulations with tailored absorption rates and durations of action, classified primarily as rapid-acting, long-acting, and premixed analogs. Understanding the structural basis for these classifications, the experimental methodologies used to evaluate them, and their resulting clinical performance is essential for researchers, scientists, and drug development professionals working to advance diabetes therapeutics.
The primary structure of insulin, showing the A and B chains connected by disulfide bonds. Key modification sites for analog engineering are highlighted.
Classification and Molecular Engineering of Insulin Analogs
Structural Foundations and Design Principles
Insulin is a small peptide hormone with a molecular mass of approximately 5808 Daltons, consisting of two peptide chains—an A chain (21 amino acids) and a B chain (30 amino acids)—connected by two disulfide bonds [16]. The native form exists as hexamers that dissociate into active monomers upon subcutaneous injection. Analog design exploits this self-assembly behavior by introducing amino acid substitutions that either destabilize hexamer formation (for rapid-acting analogs) or promote stable depot formation (for long-acting analogs) [16]. These modifications alter the isoelectric point, solubility, and binding characteristics to achieve desired PK/PD profiles.
Categories of Insulin Analogs
| Insulin Category | Primary Mechanism of Action | Key Structural Modifications | Representative Agents |
|---|---|---|---|
| Rapid-Acting | Reduced self-assembly for faster absorption | Amino acid substitutions at B28, B29, or B3 to prevent hexamer formation | Insulin lispro, aspart, glulisine, faster aspart [16] [17] |
| Long-Acting | Enhanced hexamer stability or albumin binding for prolonged release | Addition of arginine residues, fatty acid side chains, or isoelectric point shift | Insulin glargine, detemir, degludec [16] |
| Premixed | Fixed combination of rapid- and intermediate-acting components | Biphasic formulation with different dissolution profiles | Insulin lispro 25/75, aspart 30/70 [3] |
Experimental Methodologies for Evaluating Insulin Analogs
The Euglycemic Clamp Technique
The euglycemic glucose clamp is considered the gold standard for assessing the pharmacodynamic properties of insulin formulations [3]. This procedure involves intravenous infusion of insulin while simultaneously administering a variable-rate glucose infusion to maintain blood glucose at a constant baseline level (typically within ±10% of target). The glucose infusion rate (GIR) required to maintain euglycemia serves as a direct measure of insulin action over time [3]. This method provides precise, reproducible data on the onset, peak, and duration of insulin action, making it indispensable for comparative studies of insulin analogs.
Experimental workflow for a euglycemic clamp study to assess insulin pharmacodynamics.
Pharmacokinetic and Pharmacodynamic Modeling
Mechanistic PK/PD modeling provides a quantitative framework for comparing insulin analogs. These models typically describe insulin absorption via sequential first-order processes, linear elimination, and effects on glucose utilization using biophase, indirect response, or receptor down-regulation components [6]. Key parameters include maximum glucose stimulation (Smax), sensitivity (SC50), and nonlinear clearance (Km) [6]. Modeling reveals that while PK parameters—particularly absorption rates—vary significantly between insulin types, many share common PD parameters related to receptor binding and glucose transporter activation [6] [18].
Comparative Analysis of Insulin Formulations
Rapid-Acting Insulin Analogs
Rapid-acting analogs are designed for prandial glucose control, with modifications that accelerate subcutaneous absorption. Faster aspart, an advanced rapid-acting formulation, contains niacinamide and L-arginine to further enhance absorption, providing earlier onset and greater early insulin exposure compared with traditional insulin aspart [17]. Real-world evidence from a large retrospective cohort study demonstrated that patients with type 1 diabetes switching to faster aspart experienced significant reductions in HbA1c and hypoglycaemia rates compared to those using other rapid-acting analogs [17].
Table 1: Pharmacokinetic/Pharmacodynamic Properties of Rapid-Acting Insulin Analogs
| Analog | Onset of Action | Peak Action | Duration | Key Structural Features | Clinical Advantages |
|---|---|---|---|---|---|
| Insulin Lispro | 15-30 min | 30-90 min | 3-5 hours | Pro(B28)→Lys, Lys(B29)→Pro [16] | Reduced postprandial glucose excursions |
| Insulin Aspart | 10-20 min | 60-90 min | 4-6 hours | Pro(B28)→Aspartic acid [17] | Improved PPG control |
| Insulin Glulisine | 10-15 min | 60-90 min | 3-5 hours | Lys(B3)→Glu, Glu(B29)→Lys [16] | Rapid dissociation into monomers |
| Faster Aspart | 5-10 min | 60-90 min | 4-6 hours | Niacinamide + L-arginine [17] | Superior HbA1c reduction, lower hypoglycaemia risk |
Long-Acting Insulin Analogs
Long-acting analogs provide basal insulin coverage, with modifications that delay absorption and extend duration. Insulin glargine incorporates two additional arginine residues and a shifted isoelectric point (from pH 5.4 to 6.7), causing precipitation at neutral subcutaneous tissue pH and forming a sustained-release depot [16]. Insulin degludec features a fatty acid side chain that promotes multi-hexamer formation, resulting in an ultra-long duration exceeding 42 hours [16]. Emerging once-weekly basal insulins like icodec and efsitora represent the next frontier in extended-duration therapy, potentially improving adherence through reduced injection frequency [16].
Table 2: Pharmacokinetic/Pharmacodynamic Properties of Long-Acting Insulin Analogs
| Analog | Onset of Action | Peak Action | Duration | Key Structural Features | Clinical Advantages |
|---|---|---|---|---|---|
| Insulin Glargine | 1-2 hours | Relatively flat | 20-24 hours | Arg(B31)-Arg(B32), IEP shift to 6.7 [16] | Stable basal coverage, reduced hypoglycaemia |
| Insulin Detemir | 1-2 hours | Relatively flat | 16-24 hours | Fatty acid chain (albumin binding) [16] | Weight-neutral profile |
| Insulin Degludec | 1-2 hours | Peakless | >42 hours | Fatty acid side chain, multi-hexamer formation [16] | Ultra-long duration, flexible dosing |
| Insulin Icodec | 1-2 hours | Peakless | ~7 days | Strong albumin binding, reduced receptor affinity [16] | Once-weekly dosing |
Premixed Insulin Analogs
Premixed analogs combine rapid- and intermediate-acting components in fixed ratios, simplifying regimen complexity. Insulin lispro 25 (25% insulin lispro, 75% insulin lispro protamine suspension) provides both prandial and basal coverage in a single injection [3]. Bioequivalence studies using euglycemic clamp methodology have demonstrated comparable PK/PD profiles between generic and brand-name premixed formulations, with 90% confidence intervals for AUC0-t, Cmax, GIRmax, and GIRAUC0–24h falling within 80%-125% equivalence boundaries [3]. This supports their interchangeability in clinical practice, potentially reducing treatment costs.
Emerging Innovations and Future Directions
Next-Generation Insulin Analogs
Research continues to address remaining challenges in insulin therapy through several innovative approaches. Glucose-responsive insulins represent a promising frontier, designed to modulate insulin release in response to blood glucose concentrations, thereby reducing hypoglycaemia risk [16]. Hepato-preferential analogs aim to restore the physiological insulin gradient that prioritizes hepatic delivery, potentially improving glucose homeostasis with reduced peripheral effects [16]. Additionally, ultra-stable analogs resistant to fibrillation and aggregation are under development to enhance thermal stability, eliminating refrigeration requirements and improving accessibility in resource-limited settings [16].
Advanced Delivery Systems
Technological advancements complement analog improvements, with hybrid closed-loop systems now becoming standard of care for type 1 diabetes in some regions [15]. These systems integrate continuous glucose monitoring with automated insulin delivery, optimizing glycemic control while reducing user burden. When paired with modern rapid-acting analogs like faster aspart, these systems demonstrate enhanced performance, though they require careful optimization of pump settings to account for the faster absorption profiles [17].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Key Research Reagents and Methodologies for Insulin Studies
| Reagent/Methodology | Primary Function | Research Application |
|---|---|---|
| Euglycemic Clamp System | Gold standard PD assessment | Quantifies glucose infusion rate (GIR) to maintain euglycemia during insulin infusion [3] |
| HPLC-Mass Spectrometry | High-sensitivity insulin quantification | Measures plasma concentration of insulin analogs for PK analysis [3] |
| ELISA for C-peptide | Endogenous insulin secretion assessment | Monitors residual pancreatic function and suppression during exogenous insulin studies [3] |
| MONOLIX/WinNonlin | PK/PD modeling software | Performs nonlinear mixed-effects modeling and bioequivalence testing [6] [3] |
| Glucose Oxidase Assay | Real-time glucose measurement | Provides immediate feedback for glucose clamp procedures [3] |
The insulin signaling pathway, from receptor binding to GLUT4 translocation and glucose uptake.
The systematic cataloging of insulin formulations through rigorous PK/PD analysis reveals a sophisticated landscape of molecular engineering tailored to specific therapeutic needs. Rapid-acting analogs prioritize accelerated absorption for prandial control, long-acting analogs focus on sustained release for basal coverage, and premixed formulations balance both needs in simplified regimens. The euglycemic clamp technique remains indispensable for comparative evaluation, while emerging innovations—including once-weekly formulations, glucose-responsive systems, and hepato-preferential analogs—promise to further transform diabetes management. For researchers and drug development professionals, understanding these principles and methodologies provides a foundation for advancing the next generation of insulin therapeutics.
The goal of insulin replacement therapy is to mimic the normal physiologic pattern of insulin secretion, which comprises a stable basal level with rapid prandial surges [19] [20]. Achieving this with exogenous insulin was historically limited by the pharmacokinetic properties of subcutaneously administered human insulin, which does not replicate this ideal profile [21]. The engineering of insulin analogues has been a pivotal advancement in diabetes treatment, designed specifically to alter the absorption kinetics following subcutaneous injection [22]. The mechanisms of protraction—the processes that extend the duration of action—are fundamental to developing effective basal insulins. This guide provides a detailed comparison of the three primary principles used to prolong the action of insulin analogues: albumin binding, precipitation at the injection site, and exploitation of altered isoelectric points. Aimed at researchers and drug development professionals, this document synthesizes pharmacokinetic and pharmacodynamic data and outlines key experimental methodologies used in this field.
Comparative Analysis of Protraction Mechanisms
The following table summarizes the core mechanisms, molecular modifications, and key pharmacokinetic profiles of the principal long-acting insulin analogues.
Table 1: Comparison of Protraction Mechanisms in Long-Acting Insulin Analogues
| Analogue (Trade Name) | Core Protraction Mechanism | Key Molecular Modifications | Reported Duration of Action (Hours) | Key PK/PD Characteristics |
|---|---|---|---|---|
| Insulin Detemir (Levemir) [20] [22] | Albumin Binding | B29 lysine coupled with a C14 fatty acid chain; B30 threonine omitted. | Up to 24 [21] | Predictable, flat profile; high degree of reversible albumin binding in tissue and circulation. |
| Insulin Glargine (Lantus) [16] [20] | Precipitation & Altered Isoelectric Point | A21 asparagine replaced by glycine; two arginines added to B-chain C-terminus (B31 & B32). | ~24 [21] | Precipitation at neutral pH creates a depot; isoelectric point shifted from 5.4 to 6.7. |
| Insulin Degludec (Tresiba) [16] | Multi-Hexamer Chain Formation | B29 lysine coupled with a C16 fatty diacid; B30 threonine omitted. | >24 (Ultra-long) [16] | Forms soluble multi-hexamer chains upon injection, resulting in a slow, continuous release. |
Detailed Mechanism Breakdown and Experimental Data
Mechanism 1: Albumin Binding
This approach prolongs insulin action by facilitating reversible binding to the abundant albumin protein in the subcutaneous tissue and plasma.
- Molecular Engineering: Insulin detemir is engineered with a C14 fatty acid (myristic acid) side chain covalently attached to the B29 lysine residue, and the terminal B30 threonine is removed [20] [22]. The fatty acid side chain enables the analogue to bind reversibly to albumin.
- Mechanism of Action: Upon subcutaneous injection, the fatty acid chain promotes self-association into di-hexamers [22]. More significantly, the fatty acid moiety allows for high-affinity binding to albumin at the injection site and in the bloodstream. This binding creates a large, stable circulating reservoir of insulin. Only the free, unbound fraction is pharmacologically active at the insulin receptor. The slow dissociation from albumin provides a steady, continuous release of insulin, resulting in a prolonged and predictable duration of action [20] [22].
- Experimental Data: Euglycemic clamp studies, the gold standard for assessing insulin pharmacodynamics, demonstrate that insulin detemir provides a relatively flat and stable time-action profile with low intra-patient variability [21] [22]. This predictable glucose-lowering effect is a key clinical advantage attributed to the albumin-binding mechanism.
Mechanism 2: Precipitation and Altered Isoelectric Point
This strategy involves formulating an insulin that is soluble in the vial but forms a precipitate upon injection, creating a subcutaneous depot.
- Molecular Engineering: Insulin glargine incorporates two key changes: a glycine substitution at position A21 and the addition of two arginine residues to the C-terminus of the B-chain [16] [20]. These modifications shift the isoelectric point of the molecule from pH 5.4 to 6.7 [20].
- Mechanism of Action: Insulin glargine is formulated in an acidic solution (pH 4) where it is fully soluble [16]. After subcutaneous injection into the neutral pH environment (~7.4) of the tissue, the insulin molecules precipitate into stable hexamers [20]. This precipitate forms a depot at the injection site. The prolonged duration of action is achieved through the slow dissolution of this precipitate and the subsequent enzymatic cleavage of the arginine residues in the circulation, which releases active insulin monomers over an extended period [16] [22].
- Experimental Data: Pharmacodynamic profiles from clamp studies confirm that insulin glargine provides a relatively peakless, 24-hour basal insulin supply [20] [21]. Its onset of action is approximately 1-2 hours, and its duration is close to 24 hours in most patients, making it suitable for once-daily dosing [21].
Emerging and Future Protraction Mechanisms
Research continues to develop insulins with even more optimized profiles.
- Multi-Hexamer Chain Formation: Insulin degludec utilizes a different mechanism. Its modification with a C16 fatty diacid leads to the formation of soluble multi-hexamer chains upon subcutaneous injection [16]. These chains slowly dissociate into monomers, providing an ultra-long and stable action profile exceeding 24 hours [16].
- Once-Weekly Insulins: The field is advancing towards once-weekly basal insulins, such as insulin Icodec and Efsitora [16]. These analogues represent the next frontier in protraction technology, though their specific molecular mechanisms were not detailed in the sourced results.
The following diagram illustrates the structural relationships and core mechanisms of the protraction strategies discussed.
Essential Experimental Protocols for Pharmacokinetic/Pharmacodynamic Profiling
A robust understanding of insulin analogue performance relies on standardized, high-fidelity experimental methods. The following section details key protocols.
The Euglycemic Clamp Technique
The euglycemic glucose clamp is the gold standard method for assessing the pharmacodynamics (glucose-lowering effect) of insulin [23].
- Objective: To quantify the time-action profile of an insulin formulation by measuring the glucose infusion rate (GIR) required to maintain a constant target blood glucose level despite the exogenous insulin administration.
- Detailed Workflow [23]:
- Baseline Period: After an overnight fast, baseline blood glucose and C-peptide levels are measured.
- Insulin Administration: A standardized dose (e.g., 0.3 U/kg) of the test insulin is administered subcutaneously.
- Clamp Initiation: A variable intravenous infusion of 20% glucose is started. The goal is to maintain blood glucose at a predetermined target level (e.g., baseline minus 0.28 mmol/L or 5 mg/dL) [23].
- Frequent Blood Sampling: Blood glucose is measured frequently (e.g., every 5-10 minutes initially, then at longer intervals) for a defined period, typically 24 hours.
- Real-Time Adjustment: The glucose infusion rate (GIR) is adjusted in real-time based on the frequent glucose measurements to maintain euglycemia.
- C-Peptide Monitoring: Serum C-peptide levels are periodically measured to confirm the suppression of endogenous insulin secretion, ensuring that the observed glucose-lowering effect is solely from the exogenous insulin.
- Key Output: The primary outcome is the Glucose Infusion Rate (GIR) over time. The area under the GIR curve (GIRAUC) and the maximum GIR (GIRmax) are critical PD parameters for comparing insulin formulations [23].
Pharmacokinetic (PK) Blood Sampling and Analysis
Concurrent PK profiling is essential to link the observed pharmacodynamic effect to the systemic concentration of the insulin analogue.
- Objective: To measure the plasma concentration of the insulin analogue over time following subcutaneous administration.
- Detailed Workflow [23]:
- Blood Collection: Serial blood samples are collected at predetermined time points (e.g., pre-dose, 10, 20, 30, 40, 60, 90, 120, 150, 180, 240, 300, 360, 480, 600, 720, 840, 960, 1200, and 1440 minutes post-dose).
- Sample Processing: Plasma is separated from blood cells via centrifugation.
- Analytical Method: The concentration of the specific insulin analogue is quantified using highly specific methods such as High-Performance Liquid Chromatography coupled with Mass Spectrometry (HPLC-MS/MS) [23]. This technique is necessary to distinguish the analogue from endogenous insulin and its metabolites.
- Key Output: The primary PK parameters are the maximum plasma concentration (Cmax), the time to Cmax (Tmax), and the area under the concentration-time curve (AUC). These parameters define the absorption and exposure profile of the insulin [23].
The workflow for a comprehensive PK/PD study integrating these protocols is depicted below.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 2: Essential Reagents and Materials for Insulin Pharmacology Research
| Item | Function/Application | Example from Search Results |
|---|---|---|
| Recombinant Insulin Analogues | The test articles for pharmacokinetic and pharmacodynamic comparison. | Insulin glargine, detemir, degludec, lispro, aspart [16] [20]. |
| HPLC-MS/MS System | The analytical platform for specific and sensitive quantification of insulin analogue concentrations in biological samples (plasma) [23]. | ACQUITY UPLC Protein BEH C4 Column coupled with a Triple Quad 6500+ Mass Spectrometer [23]. |
| Glucose Analyzer | To provide rapid and accurate blood glucose measurements essential for real-time adjustment of the glucose infusion during a euglycemic clamp. | Device using the glucose oxidase method [23]. |
| C-Peptide ELISA Kit | To measure serum C-peptide levels, confirming suppression of endogenous insulin secretion during clamp studies [23]. | Not specified by brand, but methodology is standard [23]. |
| Variable-Infusion Pump | To administer the 20% glucose solution at a precisely controlled and adjustable rate during the euglycemic clamp procedure [23]. | Not specified by brand, but essential for the procedure. |
| Stable Isotope-Labeled Insulin Internal Standards | Used in HPLC-MS/MS analysis to correct for sample matrix effects and improve quantitative accuracy. | Implied by the use of MS for bioanalysis, though not explicitly stated [23]. |
The development of long-acting insulin analogues through mechanisms of albumin binding, precipitation via isoelectric point shift, and multi-hexamer formation represents a triumph of rational drug design. Each strategy offers distinct molecular approaches to achieving a stable, protracted, and predictable basal insulin supply, closely mimicking physiological secretion. The euglycemic clamp technique, coupled with sophisticated analytical methods like HPLC-MS/MS, provides the critical experimental foundation for comparing these analogues. As research progresses, new mechanisms and ultra-long-acting formulations like once-weekly insulins continue to push the boundaries, promising even better tools for managing diabetes. For researchers, a deep understanding of these principles and methodologies is essential for driving the next wave of innovation in insulin therapeutics.
The development of ultra-long-acting insulin analogs represents a frontier in diabetes management, aiming to reduce injection frequency from daily to weekly administrations. A critical challenge in achieving this goal lies in overcoming the inherent thermodynamic instability of the native insulin molecule, which is susceptible to a previously overlooked clearance mechanism: redox-mediated disulfide bond cleavage [24] [25]. This process, insignificant for rapid-clearing native insulin, becomes a major determinant of the pharmacokinetic (PK) and pharmacodynamic (PD) profiles of analogs with prolonged circulation times. This guide provides a comparative analysis of how structural engineering, particularly in insulin icodec, mitigates this clearance pathway to enable a once-weekly dosing regimen, and outlines the essential experimental protocols for evaluating these properties in novel analogs.
Redox-Mediated Clearance: A Central Mechanism
The Redox Clearance Pathway
Native insulin is a heterodimeric protein comprising A and B chains linked by two disulfide bonds (B7-A7 and B19-A20) and one intra-chain bond (A6-A11) [25]. In the redox environment of plasma, these disulfide bonds, particularly the solvent-exposed A7-B7 bridge, are vulnerable to attack by small-molecule thiols like glutathione and cysteine [24] [25]. This thiol-disulfide exchange reaction can lead to the splitting of the insulin molecule into its separate A and B chains.
- Irreversible Inactivation: The separated chains are hormonally inactive. Given the low circulating concentrations of injected insulin, the reverse reaction is kinetically infeasible, making chain separation an irreversible inactivation and clearance pathway [24].
- Kinetic Trapping of Native Insulin: The rapid receptor-mediated clearance of native insulin (half-life of 4-6 minutes) means it is cleared from circulation before redox cleavage becomes significant [24] [16]. Ultra-long-acting analogs, by design, circulate for much longer periods (days to weeks), thus becoming highly susceptible to this degradation mechanism [25].
Table 1: Key Features of Redox-Mediated Insulin Clearance
| Feature | Description | Implication for Ultra-Long-Acting Analogs |
|---|---|---|
| Chemical Process | Thiol-disulfide exchange with plasma thiols (e.g., glutathione) [25] | A major non-receptor-mediated clearance pathway for analogs with long half-lives. |
| Resulting Products | Separated, cyclic A-chain and B-chain [24] [25] | Irreversible loss of hormonal activity and potency. |
| Dependence on Half-life | Significance increases with longer circulation time [25] | Must be addressed through molecular design to achieve once-weekly dosing. |
| Visualization of Pathway | The diagram below illustrates the redox-mediated cleavage process. |
Comparative Analysis of Insulin Analogs
Molecular Design Strategies for Stability
The molecular engineering of ultra-long-acting insulin analogs focuses on two primary strategies: enhancing albumin binding to create a circulating depot and increasing intrinsic structural stability to resist degradation.
- Albumin Binding: Fatty acid acylation (e.g., a C20 fatty diacid in icodec) promotes strong, reversible binding to human serum albumin (HSA). This binding shields the insulin molecule from receptor-mediated clearance and delays renal clearance, thereby prolonging its half-life [24] [26] [16].
- Amino Acid Substitutions for Stability: Key amino acid substitutions are introduced to increase the thermodynamic stability of the insulin monomer, reducing its flexibility and the solvent accessibility of its disulfide bonds, thereby directly countering redox-mediated cleavage [25].
Table 2: Comparative Structural Modifications of Long-Acting Insulins
| Insulin Analog | Dosing Frequency | Key Albumin-Binding Moieties | Key Stabilizing Amino Acid Substitutions | Primary Mechanism of Protraction |
|---|---|---|---|---|
| Insulin Detemir | Once- or twice-daily | C14 fatty acid chain (myristic acid) at LysB29 [16] | None | Albumin binding, increased self-association [16] |
| Insulin Degludec | Once-daily | C16 fatty diacid chain (hexadecandioic acid) at LysB29 [16] | Removal of ThrB30 [16] | Multi-hexamer formation at injection site, albumin binding [16] |
| Insulin Icodec | Once-weekly | C20 fatty diacid with linker (gGlu-2OEG) at LysB29 [25] [26] | A14E, B16H, B25H [24] [25] | Strong albumin binding, reduced receptor affinity, enhanced disulfide stability [24] |
| Novel Analog (TBE001-A-S033) | Once-weekly (preclinical) | C22 fatty diacid with modified linker/spacer [26] | A14E, B16H, B25H (icodec backbone) [26] | Optimized albumin binding and stability [26] |
Quantitative Pharmacokinetic and Pharmacodynamic Comparison
The structural modifications in insulin icodec translate into a significantly extended half-life, enabling once-weekly dosing. Clinical and modeling studies have confirmed its efficacy and safety profile in comparison to daily basal insulins.
- Half-life and Dosing: Insulin icodec has a half-life of approximately 196 hours (about 8 days) in humans, which is the foundation for its once-weekly administration [25]. A PK/PD modeling analysis of phase 3 trials (ONWARDS 2 and 4) confirmed that switching from daily basal insulin to icodec provides sustained glycemic control over 26 weeks without an increased rate of hypoglycemia [27].
- In Vitro Stability Data: The enhanced stability of icodec is quantifiable. In a redox stability assay, the combination of A14E, B16H, and B25H substitutions in the icodec backbone conferred significantly greater resistance to reductive cleavage compared to human insulin [25]. This was correlated with an increased midpoint of unfolding in chemical denaturation assays, indicating higher thermodynamic stability [25].
Table 3: Experimental Pharmacokinetic and Stability Data
| Parameter | Human Insulin | Insulin Icodec | Experimental Analog TBE001-A-S033 |
|---|---|---|---|
| Plasma Half-life | 4-6 minutes [16] | ~196 hours [25] | Slightly shorter than icodec in Beagle dogs [26] |
| Dosing Frequency | Multiple daily | Once-weekly [25] | Once-weekly (target, preclinical) [26] |
| GuHCl Unfolding Midpoint (Δ Stability) | 4.50 M [25] | 5.42 M [25] | Data not provided in search results |
| HSA Binding Affinity | Very low | High (via C20 diacid) [24] | Higher than icodec (via C22 diacid) [26] |
Experimental Protocols for Evaluation
Assessing Redox Stability
Objective: To evaluate the susceptibility of an insulin analog to thiol-disulfide exchange-mediated chain separation [25].
Protocol:
- Preparation: Incubate the insulin analog in a buffer system with a defined redox potential, typically using a gradient of reducing agents like glutathione or dithiothreitol (DTT).
- Analysis: Use reverse-phase high-performance liquid chromatography (RP-HPLC) to separate and quantify the intact insulin molecule and its degradation products over time.
- Identification: Confirm the identity of the degradation peaks as the separated A-chain and B-chain using mass spectrometry. The B-chain appears as a single peak, while the A-chain may present three isoforms due to disulfide bond isomerization [25].
- Quantification: The stability of the analog is expressed as the rate of degradation or the relative amount of intact insulin remaining after a fixed incubation period compared to a control (e.g., human insulin).
Measuring Thermodynamic Stability
Objective: To determine the thermodynamic folding stability of the insulin monomeric analog [25].
Protocol:
- Denaturation: Subject the insulin analog to increasing concentrations of a chemical denaturant, such as guanidine hydrochloride (GuHCl).
- Signal Monitoring: Monitor the unfolding process using far-UV circular dichroism (CD) spectroscopy, which detects changes in the protein's secondary structure.
- Data Fitting: Plot the CD signal as a function of denaturant concentration and fit the data to a unfolding model to calculate the midpoint of the transition (the [GuHCl]1/2 at which 50% of the molecules are unfolded).
- Interpretation: A higher [GuHCl]1/2 value indicates a more thermodynamically stable protein structure, which correlates with resistance to redox-mediated cleavage [25].
Determining Albumin Binding Affinity
Objective: To quantify the binding affinity of an insulin analog to Human Serum Albumin (HSA), a key driver of prolonged half-life.
Protocol:
- Immobilization: Immobilize HSA on a biosensor chip (e.g., for Surface Plasmon Resonance) or in a plate-based assay.
- Binding Kinetics: Expose the immobilized HSA to a range of concentrations of the insulin analog.
- Measurement: Measure the binding response in real-time to determine the association rate (kon) and dissociation rate (koff). The equilibrium dissociation constant (KD) is calculated as koff/k_on.
- Comparison: A lower K_D value signifies a higher binding affinity for HSA. This assay is crucial for screening novel fatty acid side chains, as demonstrated in the development of TBE001-A-S033 [26].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Studying Insulin Stability and Clearance
| Research Reagent / Method | Function in Experimental Protocol |
|---|---|
| Glutathione (Reduced/Oxided) | Creates a physiologically relevant redox environment to challenge insulin disulfide bonds in stability assays [25]. |
| Guanidine Hydrochloride (GuHCl) | A chemical denaturant used to unfold insulin in a controlled manner to measure its thermodynamic stability [25]. |
| Circular Dichroism (CD) Spectrophotometer | Measures changes in the secondary structure of insulin during unfolding induced by denaturants [25]. |
| RP-HPLC with Mass Spectrometry | Separates, detects, and identifies intact insulin and its degradation products (A-chain, B-chain) with high resolution and accuracy [25]. |
| Surface Plasmon Resonance (SPR) | A label-free technique for real-time analysis of the binding kinetics and affinity between insulin analogs and HSA [26]. |
| Human Serum Albumin (HSA) | The key plasma protein used in experiments to evaluate the albumin-binding capacity of long-acting insulin analogs [26]. |
The paradigm for developing ultra-long-acting insulin analogs has fundamentally shifted with the recognition of redox-mediated clearance as a critical factor. The success of once-weekly insulin icodec demonstrates that a dual-strategy approach—combining strong albumin binding with enhanced intrinsic stability through specific amino acid substitutions (A14E, B16H, B25H)—is effective in mitigating this pathway. Future innovations, such as single-chain insulin designs [24] or diselenide bridge substitutions [24], may further push the boundaries of stability and safety. For researchers, a standardized experimental workflow assessing redox stability, thermodynamic folding, and HSA binding is indispensable for the rational design and evaluation of the next generation of ultra-long-acting therapeutic proteins.
Quantifying Action and Efficacy: Advanced PK/PD Modeling and Clamp Methodologies
The hyperinsulinemic-euglycemic clamp (HEC) technique, developed in 1979, remains the undisputed gold standard for the in vivo assessment of insulin sensitivity and the pharmacodynamic (PD) properties of insulin formulations [28] [29]. This method provides a direct and quantitative measure of whole-body glucose disposal under standardized conditions, offering precision and accuracy unmatched by other techniques [28]. For researchers and pharmaceutical developers evaluating new insulin analogs or biosimilars, the clamp technique provides critical pharmacokinetic (PK) and PD data required by regulatory agencies for market approval [30] [31].
This objective comparison examines the performance of the euglycemic clamp against alternative methods and details its central role in advancing insulin pharmacotherapy. By synthesizing evidence from recent clinical trials and methodological studies, this guide serves as a comprehensive resource for scientists designing metabolic research or drug development programs.
Core Principle and Comparative Advantage
Fundamental Mechanism
The foundational principle of the HEC is to create an artificial steady state where plasma glucose is "clamped" at a predetermined target level (typically euglycemia) through a variable glucose infusion, while insulin is infused at a constant rate to achieve hyperinsulinemia [28]. During this procedure, the Glucose Infusion Rate (GIR) required to maintain euglycemia serves as the direct quantitative measure of insulin action—higher GIR values indicate greater insulin sensitivity [28] [32]. Since endogenous glucose production is largely suppressed under hyperinsulinemic conditions, the exogenous GIR essentially equals the total rate of glucose disposal by body tissues [28].
Advantages Over Alternative Methods
The table below compares the euglycemic clamp technique with other common methods for assessing insulin sensitivity.
Table 1: Comparison of Insulin Sensitivity Assessment Methods
| Method | Principle | Key Metrics | Advantages | Limitations |
|---|---|---|---|---|
| Euglycemic Clamp [28] | Variable glucose infusion maintains basal glucose during fixed insulin infusion. | Glucose Infusion Rate (GIR), M-value. | Gold standard; direct quantitative measure; can be combined with tracers and imaging. | Labor-intensive, complex, requires specialized equipment and personnel. |
| Frequently Sampled Intravenous Glucose Tolerance Test (FSIVGTT) [28] | Model-based analysis of glucose and insulin dynamics after IV glucose bolus. | Insulin Sensitivity Index (SI). | Less labor-intensive than clamp; provides data on insulin secretion. | Does not provide a steady state; less suitable for combination with other metabolic techniques. |
| Homeostasis Model Assessment (HOMA-IR) [28] | Mathematical model based on fasting glucose and insulin levels. | HOMA-IR score. | Simple, inexpensive, suitable for large-scale epidemiological studies. | High variability, theoretically limited to the fasting state, not reliable in diabetes. |
| Continuous Glucose Monitoring (CGM)-Derived Indices [33] | Statistical analysis of glucose time-series under physiological conditions. | ACVar, CGMStd. | Captures dynamic glucose regulation in free-living conditions; less invasive. | Indirect measure; validation against clamp required; performance in diabetic populations under investigation. |
The clamp's primary advantage is its ability to directly quantify insulin-mediated glucose disposal under controlled steady-state conditions, thereby eliminating the confounding effects of counter-regulatory hormone responses that plague other methods [28]. Furthermore, its versatility allows for combination with tracer methodologies, indirect calorimetry, and imaging techniques to dissect tissue-specific metabolic fluxes [28] [34].
Applications in Insulin Analog Development
The euglycemic clamp is indispensable for establishing bioequivalence between insulin formulations and characterizing the PK/PD profiles of new analogs. The following table summarizes key findings from recent clamp studies.
Table 2: Recent Euglycemic Clamp Studies in Insulin Analog Development
| Study Focus | Insulin Type & Dose | Clamp Duration & Design | Key PK/PD Findings (GMR, 90% CI) | Reference |
|---|---|---|---|---|
| Biosimilar Ultra-Rapid Lispro [31] | Ultra-rapid lispro in healthy volunteers. | 8-hour, double-blind, randomized, crossover clamp. | PK (AUC, Cmax) and PD profiles comparable; GMRs within 80-125%. | [31] |
| Biosimilar Insulin Glargine [35] | Insulin glargine (0.4 IU/kg) in healthy male volunteers. | 24-hour, randomized, open-label, crossover clamp. | GIR~max~: 42.75 (T) vs 45.28 (R) mg·kg⁻¹·min⁻¹. Bioequivalence demonstrated. | [35] |
| Biosimilar Premixed Lispro 25 [3] | Premixed insulin lispro (0.3 IU/kg) in healthy male volunteers. | 24-hour, randomized, open-label, crossover clamp. | GIR~max~: 4.47 (T) vs 4.12 (R) mg·kg⁻¹·min⁻¹. 90% CIs for PK/PD within bioequivalence range. | [3] |
| Long-Acting Insulin Degludec [32] | Insulin degludec (0.4 IU/kg) in healthy volunteers. | 24-hour clamp assessing test quality. | Established CV~BG~ ≤ 3.5% and C-peptide reduction ≥ 50% as key quality indicators. | [32] |
These studies consistently demonstrate the clamp technique's precision in detecting subtle differences in insulin onset, peak action, and duration. The robust PK/PD data generated underpin regulatory approvals for biosimilar and novel insulin products, ensuring their clinical performance matches reference products.
Detailed Experimental Protocol
Standardized Clamp Procedure
A typical HEC procedure for evaluating insulin preparations involves the following key steps, which can be adapted for specific study objectives and populations:
- Participant Preparation: After an overnight fast (>10 hours), participants rest in a supine position. Catheters are placed in a forearm vein for glucose/insulin infusion and in the contralateral arm (with a heating pad for arterialized venous blood) for frequent blood sampling [34] [32] [35].
- Baseline Period: Blood glucose (BG) is measured multiple times (e.g., at -30, -20, and -10 minutes) to establish a stable fasting baseline level [32] [35].
- Insulin Administration & Glucose Clamping:
- A subcutaneous injection of the test or reference insulin preparation is administered [3] [35].
- The target BG is typically set slightly below the baseline (e.g., baseline minus 0.3 mmol/L or 5%) to help suppress endogenous insulin secretion [30] [32].
- A variable 20% glucose solution is infused, and the GIR is adjusted based on frequent (e.g., every 5-10 minutes) BG measurements to maintain the BG at the target level [32] [3]. The entire process is often automated using systems like ClampArt for enhanced precision [29].
- Blood Sampling: Blood is collected at predefined intervals for PK analysis (measurement of plasma insulin concentration) and for monitoring C-peptide levels to confirm suppression of endogenous insulin secretion [32] [3].
Workflow Visualization
The following diagram illustrates the sequential flow and key decision points in a standard euglycemic clamp procedure.
Quality Control and Standardization
High-quality clamp data requires strict adherence to standardized protocols and rigorous quality control. Key performance indicators include:
- Blood Glucose Variability: The Coefficient of Variation of Blood Glucose (CV~BG~) is a primary metric. A CV~BG~ ≤ 3.5% is indicative of a high-quality clamp for long-acting insulin studies, ensuring stable experimental conditions [32].
- Endogenous Insulin Suppression: Effective suppression of the pancreas's own insulin secretion is confirmed by a reduction in C-peptide levels. A reduction of ≥ 50% from baseline is generally considered sufficient to exclude confounding effects from endogenous insulin [32].
- Additional Metrics: Other useful quality indices include the percentage of time BG is within the target range, the mean excursion from target BG, and the area under the curve of glucose excursion [32].
Advanced Research Applications
Tissue-Specific Insulin Sensitivity
The standard HEC measures whole-body insulin sensitivity. However, when combined with dynamic imaging techniques like [18F]FDG-PET/MRI, the method can quantify glucose uptake into specific tissues such as skeletal muscle, adipose tissue, and the brain [34]. This approach has revealed that individuals with Type 2 Diabetes (T2DM) exhibit impaired glucose uptake specifically in skeletal muscle and adipose tissue under insulin stimulation, highlighting the technique's power to elucidate tissue-level pathophysiology [34].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Equipment for Euglycemic Clamp Studies
| Item | Function/Application | Example/Specification |
|---|---|---|
| Insulin Formulation [31] [35] | The drug substance under investigation (prandial or basal). | Recombinant human insulin or analogs (e.g., Lispro, Glargine, Degludec). |
| 20% Glucose Solution [32] [35] | Variable infusion to maintain target blood glucose level. | Sterile, pharmaceutical grade for intravenous administration. |
| C-Peptide Assay [30] [32] | Monitor suppression of endogenous insulin secretion. | Validated ELISA or chemiluminescent immunoassay. |
| Glucose Analyzer [34] [32] | Rapid and accurate bedside measurement of blood glucose. | Glucose oxidase method (e.g., HemoCue, BIOSEN C_Line). |
| Automated Clamp System [29] | Integrates continuous glucose sensing and algorithm-driven glucose infusion. | CE-certified systems like ClampArt or Biostator. |
| Validated Bioanalytical Method [3] [35] | Quantify plasma concentrations of the insulin analog. | HPLC-MS/MS or specific immunoassays. |
| Indirect Calorimetry [28] [29] | Assess substrate utilization (glucose/lipid oxidation). | Metabolic cart for measuring O₂ consumption and CO₂ production. |
| Stable Isotope Tracers [29] | Measure endogenous glucose production and lipolysis. | [6,6-²H₂]-glucose, [¹³C]-oleate. |
The hyperinsulinemic-euglycemic clamp technique remains an indispensable tool in metabolic research and drug development. Its status as the gold standard is upheld by its direct quantitative nature, versatility, and unparalleled accuracy in characterizing the pharmacodynamic properties of insulin formulations. While emerging technologies like CGM offer promising, less invasive alternatives for population screening, the clamp is unlikely to be replaced for definitive proof-of-mechanism studies and regulatory submissions of new insulin products. Ongoing refinements in automation and standardization, as evidenced by recent studies, continue to enhance its precision and reliability, ensuring its central role in advancing the understanding and treatment of diabetes.
Mechanism-based pharmacodynamic (PD) modeling represents a quantitative discipline that integrates pharmacokinetics (PK), pharmacological systems, and pathophysiological processes to understand the intensity and time-course of drug effects on the body [36]. Unlike classical empirical approaches, mechanism-based models seek to separate drug-specific parameters from system-specific parameters, creating a platform that is more readily translatable across different experimental conditions and patient populations [36] [37]. The core value of these models lies in their ability to quantify and predict drug-system interactions for both therapeutic and adverse drug responses, thereby playing a critical role in drug discovery, development, and pharmacotherapy [36].
In the context of insulin therapy, mechanism-based PK/PD modeling has become indispensable. The goal of insulin therapy in patients with either type 1 diabetes mellitus (T1DM) or type 2 diabetes mellitus (T2DM) is to match as closely as possible normal physiologic insulin secretion to control fasting and postprandial plasma glucose [21]. The development of various insulin analogs with modified molecular structures has created a landscape where modeling can objectively compare their performance, guide formulation design, and optimize dosing regimens [21] [37]. This review will explore how different PK/PD modeling approaches—specifically integrating absorption, biophase, and indirect response models—provide a framework for comparing the pharmacokinetic and pharmacodynamic profiles of insulin analogs.
Theoretical Framework of Key PK/PD Models
Simple Direct Effect and Absorption Models
The most fundamental relationship in pharmacodynamics is described by the Hill equation (or Emax model), which assumes drug effects are directly proportional to receptor occupancy and that plasma drug concentrations are in rapid equilibrium with the effect site [36]:
This equation characterizes the concentration-effect relationship through a baseline effect (E₀), the maximum possible effect (E_max), and the drug concentration producing half maximal effect (EC₅₀) [36]. For drug administration via extravascular routes, absorption to the central compartment is typically described by either first-order or zero-order processes [37]. A one-compartment model with first-order absorption and elimination can be described by the following differential equations [37]:
Where A₁ represents the mass of drug at the administration site, ka is the absorption rate constant, A₂ denotes the mass of drug in the body, CL represents clearance, V represents volume of distribution, and Cp denotes plasma drug concentration [37].
Biophase Distribution Model
Often, a temporal disconnect exists between plasma drug concentrations and pharmacological effects, resulting in a hysteresis loop when plotting effect versus concentration [36]. Distribution to the site of action—the "biophase"—can represent a rate-limiting process accounting for this delay. The biophase model introduces a hypothetical effect compartment linked to the central compartment, with the rate of change of drug concentrations at the biophase (C_e) defined as [36]:
Where k_eo represents the equilibration rate constant between plasma and effect compartment [36]. This model effectively collapses the hysteresis loop, allowing characterization of the direct concentration-effect relationship.
Indirect Response Models
Many drug effects occur through indirect mechanisms where the drug stimulates or inhibits the production or loss of endogenous substances or mediators that subsequently drive the observed response [36]. Indirect response models capture these complex temporal dynamics by modeling the turnover of these response biomarkers, which often provides a more mechanistic representation of the drug's pharmacodynamic action compared to direct effect models.
Comparative PK/PD Analysis of Insulin Analogs
Rapid-Acting Insulin Analogs
Rapid-acting insulin analogs (aspart, lispro, glulisine) were designed to mimic the physiological first-phase insulin release in response to meals [21] [9]. Structural modifications, such as the paired amino acid substitution of proline and lysine at positions B28 and B29 in insulin lispro, reduce self-assembly tendencies, leading to faster absorption and shorter duration of action compared to regular human insulin [9].
Table 1: Pharmacokinetic Properties of Rapid-Acting Insulin Analogs
| Insulin Analog | Structural Modifications | Onset (minutes) | Peak (minutes) | Duration (hours) | T_max (minutes) | C_max (mU/mL) |
|---|---|---|---|---|---|---|
| Lispro [21] [9] | B28Pro→Lys, B29Lys→Pro | 5-15 | 30-60 | 3-4 | 30-90 | 116 |
| Aspart [21] | B28Pro→Asp | 10-20 | 40-50 | 3-5 | 40-50 | 82.1 |
| Glulisine [21] [9] | B3Lys→Glu, B29Lys→Glu | 20 | 60 | 4 | 30-90 | 82 |
| Regular Human Insulin [21] | - | 30 | 60-120 | 6-8 | 50-120 | 51 |
Long-Acting Insulin Analogs
Long-acting insulin analogs (glargine, detemir, degludec) provide basal insulin coverage with flatter time-action profiles and reduced peak-trough fluctuations compared to NPH insulin [21] [9]. These analogs employ different strategies to prolong their duration, including shifting the isoelectric point (glargine) or enhancing albumin binding (detemir, degludec) [9].
Table 2: Pharmacokinetic Properties of Long-Acting Insulin Analogs
| Insulin Analog | Structural Modifications | Mechanism of Prolongation | Onset (hours) | Peak | Duration (hours) |
|---|---|---|---|---|---|
| Glargine [21] [9] | A21Gly→Arg, B31Arg, B32Arg | Isoelectric point shift → precipitation at neutral pH | 1-2 | Flat | ~24 |
| Detemir [21] [9] | B30Thr deletion, B29Lys→myristic acid | Albumin binding via fatty acid acylation | 1.6 | Flat | Up to 24 |
| Degludec [9] | B30Thr deletion, B29Lys→hexadecandioic acid | Multi-hexamer formation & albumin binding | - | Flat | >24 |
| NPH Insulin [21] | Protamine complexation | Crystal formation | 1-2 | 3-8 hours | 12-15 |
Emerging Once-Weekly Insulin Analogs
The development of once-weekly insulin analogs represents the latest advancement in prolonged duration therapy. Insulin icodec incorporates three amino acid substitutions (A14E, B16H, and B25H) to enhance molecular stability and reduce insulin receptor (IR) binding, combined with a C20 fatty diacid-containing side chain that facilitates strong, reversible binding to human serum albumin (HSA) [9] [26]. Recent research has focused on further modifications to the fatty acid side chain of icodec to optimize HSA affinity and duration of action. One promising analog, TBE001-A-S033, features a C22 diacid-2γGlu-2OEG conjugation at the B29k position and has demonstrated superior HSA affinity and effective blood sugar reduction in murine models [26].
Experimental Protocols for Insulin Analog Evaluation
In Vitro Bioactivity and HSA Affinity Assays
The assessment of insulin analogs typically begins with in vitro characterization of receptor binding affinity and ability to activate downstream signaling pathways. The insulin signaling pathway can be visualized as follows:
Figure 1: Insulin Signaling Pathway for Glucose Uptake
For HSA affinity determination, researchers employ surface plasmon resonance (SPR) or similar biophysical techniques to quantify binding kinetics [26]. In recent studies, insulin analogs with varying fatty acid side chains were systematically evaluated, revealing that increasing carbon chain length (e.g., C22 diacid) generally enhances HSA affinity, while modifications to linker composition (γGlu content) and spacer elements (OEG units) further modulate binding characteristics [26].
In Vivo Pharmacokinetic Studies
Preclinical PK studies typically involve subcutaneous administration of insulin analogs to animal models (e.g., ICR mice, db/db mice, Beagle dogs) with serial blood sampling over extended periods [26]. Plasma insulin concentrations are quantified using validated immunoassays or LC-MS/MS methods, and PK parameters (Cmax, Tmax, half-life, AUC) are derived using noncompartmental or compartmental modeling approaches [37] [26].
The experimental workflow for evaluating novel insulin analogs integrates both in vitro and in vivo assessments:
Figure 2: Insulin Analog Evaluation Workflow
Pharmacodynamic Assessments in Diabetic Models
The hypoglycemic effects of insulin analogs are typically evaluated in rodent models of diabetes (e.g., streptozotocin-induced diabetic mice, db/db mice) [26]. Animals receive subcutaneous injections of test articles, and blood glucose levels are monitored periodically. The duration of action is determined as the time until blood glucose returns to baseline levels, with longer-lasting analogs maintaining glycemic control for extended periods [26]. For novel once-weekly candidates like TBE001-A-S033, studies have demonstrated blood glucose control comparable to insulin icodec in db/db mice, supporting their potential for weekly administration in humans [26].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Insulin Analog Studies
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Recombinant Insulin Analogs | Test articles for in vitro and in vivo studies | Insulin icodec main chain, TBE001-A-S033 [26] |
| Diabetic Rodent Models | In vivo PD assessment | ICR mice, db/db mice [26] |
| Human Serum Albumin (HSA) | In vitro binding affinity studies | Affinity determination via SPR [26] |
| Insulin Receptor Assays | In vitro bioactivity assessment | Cell-based phosphorylation assays [9] |
| LC-MS/MS Systems | Bioanalytical quantification | Insulin analog concentration measurement [26] |
| Glucose Assay Kits | PD endpoint measurement | Blood glucose monitoring systems [26] |
| Pichia pastoris Expression System | Recombinant production | Production of insulin analog main chains [26] |
Mechanism-based PK/PD modeling provides a powerful framework for comparing the performance of insulin analogs by integrating absorption characteristics, biophase distribution, and indirect response mechanisms. The continued evolution of insulin therapy—from rapid-acting analogs to once-weekly formulations—has been guided by these quantitative approaches, which enable researchers to understand how structural modifications translate to pharmacokinetic and pharmacodynamic differences. As emerging insulin analogs with enhanced thermostability, glucose responsiveness, and hepato-preferentiality advance through development, mechanism-based modeling will remain essential for optimizing their therapeutic profiles and translating preclinical findings to clinical practice [9] [37] [26].
Insulin therapy remains a cornerstone of diabetes management, and its efficacy is critically dependent on its pharmacokinetic (PK) and pharmacodynamic (PD) properties. For researchers and drug development professionals, a deep understanding of parameters such as the onset of action, peak effect, and duration of action is essential for designing new insulin analogs and optimizing therapeutic regimens. These parameters determine how well an insulin product can mimic the body's physiological insulin secretion, thereby influencing glycemic control and patient safety [7]. The evolution from animal insulins to recombinant human insulins and, more recently, to insulin analogs has been driven by the goal of improving these very properties to achieve more predictable and physiological insulin action profiles [7] [38]. This guide provides a comparative analysis of the key performance parameters of modern insulin analogs, supported by experimental data and methodologies relevant to preclinical and clinical research.
Comparative Pharmacokinetic and Pharmacodynamic Profiles of Insulin Analogs
The following tables summarize the key PK/PD parameters for the main categories of insulin analogs used in clinical practice. These parameters are crucial for predicting clinical performance and informing dosing schedules.
Table 1: Pharmacokinetic and Pharmacodynamic Parameters of Insulin Analogs
| Insulin Type | Onset of Action | Peak Effect | Duration of Action |
|---|---|---|---|
| Rapid-Acting(e.g., Insulin aspart, lispro, glulisine) | 10-15 minutes [39] | 30-90 minutes [39] | 3-5 hours [40] |
| Short-Acting(Regular human insulin) | 30 minutes [40] | 2-3 hours [39] | 6-8 hours [40] |
| Intermediate-Acting(NPH insulin) | 1-2 hours [40] | 4-10 hours [39] | 10-16 hours [40] |
| Long-Acting(e.g., Insulin glargine, detemir, degludec) | 1-2 hours [40] | Relatively flat, no pronounced peak [39] | 12-24 hours (detemir) to over 24 hours (glargine U-100, degludec) [40] |
Table 2: Ultra-Fast and Next-Generation Insulins in Research and Development
| Insulin Type / Candidate | Key Mechanism | Reported Onset & Peak | Research Status & Key Findings |
|---|---|---|---|
| Faster Aspart | Formulated with niacinamide and L-arginine to accelerate initial absorption [17]. | Provides an earlier onset of action and greater early insulin exposure compared with standard insulin aspart [17]. | Approved; real-world studies show numerically greater HbA1c reductions and higher treatment persistency in T1D vs. other rapid-acting analogs [17]. |
| Smart Insulins(e.g., Insulin-glucagon fusion protein) | A single molecule combining insulin and glucagon, designed to respond to endogenous glucose levels [41]. | Aims to automatically regulate blood sugar, reducing hypoglycemia risk [41]. | Preclinical (rat models); potential for weekly injection or pump use [41]. |
| Ultra-Fast Acting Analogs | Structural modifications for accelerated absorption and a more rapid, pronounced initial insulin peak [42]. | More rapid onset and earlier peak concentration vs. rapid-acting analogs [42]. | Research focus; shown to improve postprandial glucose and reduce glucose variability in T1D and T2D [42]. |
Experimental Protocols for Assessing Insulin Parameters
Robust and standardized experimental protocols are fundamental to generating reliable and comparable PK/PD data. The following methodologies are central to the evaluation of insulin analogs.
The Euglycemic Glucose Clamp Technique
The euglycemic glucose clamp is considered the gold standard for assessing the pharmacodynamics of insulin and its analogs [3].
- Objective: To measure the glucose-lowering effect (pharmacodynamics) of an insulin dose under steady-state blood glucose conditions.
- Procedure: After an overnight fast, subjects receive a subcutaneous injection of the test insulin. A variable-rate intravenous infusion of a glucose solution (e.g., 20%) is initiated and adjusted in real-time based on frequent (e.g., every 5-10 minutes) blood glucose measurements [3]. The primary goal is to maintain blood glucose at a predetermined target level, typically within ±10% of the baseline or a specific euglycemic value [3].
- Primary Outcome Measure: The Glucose Infusion Rate (GIR) is the key PD parameter. The GIR over time reflects the activity profile of the insulin under investigation. From the GIR curve, critical metrics such as the time to maximum effect (GIR~max~) and the total area under the curve (AUC~GIR0–t~) are derived to quantify onset, peak, and overall activity [3].
- Quality Control: The stability of the clamp is validated by maintaining steady blood glucose and suppressed endogenous C-peptide levels, confirming that the glucose infusion is solely compensating for the action of the exogenous insulin [3].
Bioequivalence and Pharmacokinetic Studies
For comparing formulations, randomized, crossover studies are employed to determine bioequivalence and detailed PK parameters.
- Study Design: A single-center, randomized, open-label, two-period, crossover design is commonly used. Healthy volunteers are randomized into two sequences to receive either the test (T) or reference (R) preparation in the first period, followed by a washout period and then the alternate preparation [3].
- Pharmacokinetic Blood Sampling: Blood samples are collected at frequent intervals before and after insulin administration (e.g., from -30 minutes up to 24 hours post-injection) [3].
- Analytical Methods: The plasma concentration of the insulin analog is typically quantified using high-performance liquid chromatography (HPLC) coupled with mass spectrometry (LC-MS/MS), which offers high specificity and sensitivity [3]. Serum C-peptide levels are often measured via enzyme-linked immunosorbent assay (ELISA) to monitor endogenous insulin secretion suppression [3].
- Statistical Analysis: Bioequivalence is concluded if the 90% confidence intervals for the geometric mean ratios (Test/Reference) of the primary PK parameters (AUC~0-t~ and C~max~) and PD parameters (GIR~max~ and AUC~GIR0–t~) fall entirely within the predefined acceptance range of 80%-125% [3].
Signaling Pathways and Experimental Workflows
The following diagrams illustrate the core experimental workflow for insulin assessment and the mechanism of a novel "smart insulin" approach.
Diagram 1: Euglycemic Clamp Workflow for Insulin PK/PD Profiling.
Diagram 2: Proposed Mechanism of a Novel Glucose-Responsive "Smart Insulin".
The Scientist's Toolkit: Key Research Reagents and Materials
This table details essential materials and their functions for conducting rigorous insulin pharmacokinetic and pharmacodynamic research.
Table 3: Essential Research Reagents and Materials for Insulin PK/PD Studies
| Research Reagent / Material | Function in Experimentation |
|---|---|
| Insulin Analogs (Test & Reference) | The active pharmaceutical ingredients being compared for their pharmacokinetic and pharmacodynamic properties. |
| High-Performance Liquid Chromatography with Mass Spectrometry (HPLC-MS/MS) | The analytical workhorse for the specific and sensitive quantification of insulin analog concentrations in plasma samples [3]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | Used for measuring biomarkers such as C-peptide, which indicates endogenous insulin secretion and helps validate clamp quality [3]. |
| Euglycemic Clamp System | An integrated setup including IV glucose, infusion pumps, and a protocol for real-time adjustment to maintain target blood glucose. |
| Glucose Oxidase Reagents | Used in bedside or lab analyzers for the rapid and precise measurement of blood glucose levels during clamp procedures [3]. |
| Continuous Glucose Monitors (CGM) | In clinical trials, CGMs provide high-resolution, real-time interstitial glucose data to complement clamp data and assess glycemic variability [17] [43]. |
| Automated Insulin Delivery (AID) Systems | Used in clinical research to evaluate the real-world performance of insulin analogs in a closed-loop context [43]. |
Pharmacokinetic (PK) and pharmacodynamic (PD) modeling represents a cornerstone of modern drug development, providing a critical framework for translating data from healthy volunteers to patient populations. For insulin analogs, this translation is particularly crucial as it directly informs dosing strategies that balance efficacy with safety, especially the risk of hypoglycemia. PK/PD modeling integrates data on a drug's absorption, distribution, metabolism, and excretion (PK) with its physiological and therapeutic effects (PD) to establish exposure-response relationships. These models enable researchers to simulate clinical outcomes under various dosing scenarios, optimizing therapeutic regimens before widespread clinical implementation [44]. The evolution of model-informed drug development (MIDD) approaches, including physiologically based pharmacokinetic (PBPK) modeling and population PK/PD analyses, has significantly enhanced our ability to predict drug behavior across diverse populations, ultimately supporting more personalized and effective diabetes management strategies [44].
Comparative PK/PD Profiles of Insulin Analogs
Quantitative Comparison of Insulin Pharmacokinetics
The pharmacokinetic properties of insulin analogs vary significantly based on their structural modifications and formulation technologies. These differences directly influence their onset of action, peak activity, and duration of effect, which in turn determines their clinical application as rapid-acting, intermediate-acting, or long-acting insulins.
Table 1: Comparative PK Parameters of Various Insulin Types from Glucose Clamp Studies
| Insulin Type | Tmax (hr) | Cmax (ng/mL) | AUC0-24h (ng·h/mL) | Absorption Rate Constant (hr⁻¹) |
|---|---|---|---|---|
| Insulin Lispro (Premixed) | 1.40 ± 0.45 | 1.36 ± 0.42 | 510 ± 86.2 | 1.92 ± 0.21 |
| Rapid-acting analogs | 0.5 - 1.5 | Variable | Variable | 2.5 - 3.2 |
| Long-acting analogs | 4 - 8 | Variable | Variable | 0.2 - 0.4 |
| Regular human insulin | 1.5 - 2.5 | Variable | Variable | 1.0 - 1.5 |
Data adapted from clinical studies comparing subcutaneously administered insulin analogs in healthy volunteers [6] [3]. The absorption rates varied significantly between insulin types, with rapid-acting analogs demonstrating the fastest absorption kinetics.
Pharmacodynamic Profiles and Clinical Efficacy
The pharmacodynamic responses to different insulin analogs, as measured by glucose utilization in euglycemic clamp studies, reflect their distinct PK profiles and directly correlate with their clinical efficacy in maintaining glycemic control.
Table 2: Pharmacodynamic Parameters of Insulin Analogs from Glucose Clamp Studies
| Insulin Type | GIRmax (mg·kg⁻¹·min⁻¹) | AUC-GIR0-24h (mg·h·kg⁻¹·min⁻¹) | Time to GIRmax (hr) | Duration of Action (hr) |
|---|---|---|---|---|
| Insulin Lispro (Premixed) | 4.12 ± 1.81 | 2,994 ± 941 | 2.5 - 3.5 | Up to 24 |
| Rapid-acting analogs | 5.8 - 7.2 | 3,500 - 4,200 | 1.5 - 2.5 | 3 - 5 |
| Long-acting analogs | 2.1 - 3.5 | 4,500 - 6,800 | 6 - 12 | 18 - 24+ |
| Once-weekly Insulin Icodec | N/A | N/A | N/A | 168+ |
Data synthesized from clinical studies including the ONWARDS trials [27] [6] [3]. GIR = Glucose Infusion Rate; N/A = Specific values not available in the searched literature.
Experimental Protocols for Insulin PK/PD Assessment
Euglycemic Clamp Methodology
The euglycemic glucose clamp technique remains the gold standard for assessing the pharmacodynamic properties of insulin analogs, providing precise measurements of glucose utilization under controlled conditions [3].
Protocol Details:
- Subject Preparation: Healthy volunteers or patients undergo screening for normal insulin secretion function and glucose tolerance. Participants typically fast overnight (10-12 hours) before the procedure.
- Baseline Period: Blood glucose levels are measured at -30, -20, and -10 minutes before insulin administration to establish baseline values.
- Insulin Administration: A standardized dose (e.g., 0.3 IU·kg⁻¹ for premixed insulin lispro) is administered subcutaneously.
- Glucose Monitoring and Infusion: Following insulin injection, blood glucose measurements are taken frequently (every 5 minutes initially, then at extended intervals) for 24 hours. A 20% glucose solution is infused intravenously at a variable rate to maintain blood glucose within ±10% of the target level (typically baseline minus 0.28 mmol·L⁻¹).
- Endpoint Measurement: The glucose infusion rate (GIR) required to maintain euglycemia is calculated and recorded throughout the study period, generating a time-action profile of the insulin's effect [3].
Blood Sampling and Analytical Methods
Comprehensive blood sampling protocols support both PK and PD assessments:
- PK Sampling: Blood samples for insulin concentration measurements are collected at predetermined intervals (-30 min, 0, 10, 20, 30, 40, 50, 60, 70, 80, 90, 100, 110, 120, 150, 180, 210, 240, 300, 360, 420, 480, 600, 720, 840, 960, 1200, and 1440 minutes post-dose).
- Analytical Methods: Plasma concentrations of insulin analogs are typically quantified using high-performance liquid chromatography (HPLC) coupled with mass spectrometry, providing high specificity and sensitivity [3].
- C-peptide Measurement: Serum C-peptide levels are assessed via ELISA to monitor endogenous insulin suppression, confirming the adequacy of exogenous insulin dosing during the clamp procedure.
Figure 1: Experimental workflow for insulin PK/PD assessment using euglycemic clamp methodology.
Advanced Modeling Approaches in Insulin Development
PK/PD Modeling for Novel Insulin Analogs
Mechanistic PK/PD modeling approaches have become increasingly sophisticated, enabling more accurate predictions of clinical dosing regimens. For novel analogs like once-weekly insulin icodec, these models integrate data from multiple sources to simulate real-world scenarios.
Model Structure and Application:
- PK Model Components: Typically describe insulin absorption via sequential first-order processes and linear elimination, with parameters varying between insulin types [6].
- PD Model Components: Often combine biophase, indirect response, and receptor down-regulation components to capture the complex relationship between insulin concentrations and glucose utilization.
- Clinical Translation: Models developed from healthy volunteer data are refined using patient population data to account for pathophysiological differences in type 2 diabetes, including insulin resistance and beta-cell dysfunction [6].
Recent modeling analyses from the ONWARDS trials demonstrated that switching from daily basal insulin to once-weekly icodec without a loading dose resulted in only mild, transient increases in prebreakfast glucose levels during the first 1-2 weeks, with no sustained differences in HbA1c reduction or hypoglycemia rates over 26 weeks [27] [12]. This type of modeling provides crucial evidence for simplifying transition protocols in clinical practice.
PBPK Modeling and AI Integration
Physiologically based pharmacokinetic (PBPK) modeling represents an advanced MIDD approach that integrates physiological parameters with drug-specific properties to predict pharmacokinetics across populations [44].
Recent Advances:
- AI-PBPK Integration: Emerging artificial intelligence-augmented PBPK models can predict PK/PD properties from molecular structures, potentially accelerating early-stage insulin analog development [45].
- Population Extrapolation: PBPK models facilitate dose selection for special populations, such as pediatric patients, by incorporating age-related physiological changes that affect drug disposition [44].
- Regulatory Applications: The FDA has incorporated PBPK modeling in regulatory submissions for biological products, including support for dosing strategies and clinical trial design [44].
Figure 2: AI-PBPK modeling workflow for predicting clinical dosing regimens.
Research Reagent Solutions for PK/PD Studies
Table 3: Essential Research Materials and Technologies for Insulin PK/PD Studies
| Reagent/Technology | Manufacturer/Example | Primary Function | Key Application in Insulin Studies |
|---|---|---|---|
| HPLC-MS/MS Systems | Shimadzu LC30AD with SCIEX Triple Quad 6500+ | High-sensitivity insulin quantification | Precise measurement of plasma insulin concentrations at low levels [3] |
| UPLC Columns | ACQUITY UPLC Protein BEH C4 Column | Chromatographic separation | Resolving insulin analogs from endogenous insulin and metabolites [3] |
| ELISA Kits | Commercial C-peptide ELISA | C-peptide measurement | Assessing endogenous insulin suppression during clamp studies [3] |
| Glucose Analyzers | Glucose oxidase-based systems | Real-time glucose measurement | Maintaining euglycemia during clamp procedures [3] |
| PBPK Modeling Platforms | GastroPlus, Simcyp Simulator | Predictive PK modeling | Simulating insulin disposition in virtual populations [44] [45] |
| AI-PBPK Platforms | B2O Simulator | Integrated AI and PBPK modeling | Predicting PK/PD properties from molecular structures [45] |
| Modeling Software | MONOLIX (Version 2024) | Nonlinear mixed-effects modeling | Population PK/PD analysis and parameter estimation [6] |
The translation of PK/PD data from healthy volunteers to patient populations represents a sophisticated process that integrates advanced experimental methodologies with computational modeling approaches. Euglycemic clamp studies provide the foundational PD data, while modern analytical technologies enable precise quantification of insulin pharmacokinetics. The emerging paradigm of AI-enhanced PBPK modeling holds particular promise for accelerating the development of novel insulin analogs like once-weekly icodec, potentially streamlining the path from initial discovery to clinical implementation. As these technologies continue to evolve, the translation of PK/PD data will increasingly support personalized dosing strategies that optimize both efficacy and safety for diverse patient populations with diabetes.
Leveraging Models for Regimen Visualization and Educational Tool Development
In the field of diabetes research and drug development, understanding the precise pharmacokinetic (PK) and pharmacodynamic (PD) properties of insulin analogs is fundamental to optimizing therapeutic regimens. The comparison of these properties across different insulin types provides critical insights for clinicians, researchers, and drug development professionals. This guide objectively compares the performance of various insulin analogs using experimental data derived from rigorous PK/PD modeling approaches, with a specific focus on how these models can be leveraged for regimen visualization and educational tool development. The application of mechanistic PK/PD models to data from controlled studies enables the quantification of parameters that directly influence clinical outcomes, forming a scientific basis for informed decision-making in both drug development and clinical practice [6].
Comparative Pharmacokinetic and Pharmacodynamic Profiles of Insulin Analogs
Structural and Functional Classification of Insulin Analogs
Insulin analogs are engineered modifications of human insulin designed to alter absorption kinetics and duration of action, thereby more closely mimicking physiological insulin secretion. They are broadly classified based on their onset and duration of action into rapid-acting, short-acting, intermediate-acting, and long-acting categories [46]. Premixed insulin analogs combine specific proportions of rapid- and intermediate-acting components to provide both prandial and basal glucose coverage in a single injection [3]. For instance, insulin lispro 25 contains 25% insulin lispro and 75% insulin lispro protamine suspension, offering a convenient option for managing postprandial and basal glucose requirements simultaneously [3].
The pharmacokinetic and pharmacodynamic properties of these analogs fundamentally determine their clinical application, dosing schedules, and therapeutic efficacy. Rapid-acting analogs like insulin lispro, aspart, and glulisine are characterized by a quick onset and short duration, making them ideal for mealtime glucose control [46]. Their PK/PD profile is closer to meal-time endogenous insulin secretion compared to human insulin, resulting in better control of postprandial glucose excursions [46].
Key Experimental Models and Methodologies
The gold standard for assessing insulin pharmacodynamics is the euglycemic glucose clamp technique [3] [47]. In this procedure, a fixed dose of insulin is administered subcutaneously to healthy volunteers or patients while intravenous glucose is infused at a variable rate to maintain blood glucose at a constant baseline level. The Glucose Infusion Rate (GIR) required to maintain euglycemia serves as a direct measure of insulin's pharmacodynamic effect [47]. The quality of a clamp study is validated by stable blood glucose maintenance and suppression of endogenous insulin secretion, as measured by C-peptide levels [3].
Pharmacokinetic modeling of insulin typically describes absorption via sequential first-order processes and linear elimination, while pharmacodynamic modeling often employs indirect response models combined with biophase distribution and receptor down-regulation components to capture the complex relationship between insulin concentration and glucose utilization effects [6]. Population PK/PD modeling approaches using software like MONOLIX and WinNonlin allow researchers to account for inter-individual variability and identify covariates that influence insulin exposure and response [6] [3] [48].
Table 1: Key Experimental Approaches in Insulin PK/PD Research
| Methodology | Key Measurements | Application in Insulin Research | References |
|---|---|---|---|
| Euglycemic Clamp | Glucose Infusion Rate (GIR), Blood Glucose Levels | Gold standard for assessing PD properties of insulin analogs | [3] [47] |
| Compartmental PK Modeling | Absorption rate, Clearance, Volume of Distribution | Quantifies absorption and elimination kinetics of different insulin formulations | [6] [49] |
| Indirect Response PD Modeling | SC₅₀, Sₘₐₓ, Effect Duration | Characterizes glucose utilization effects and dose-response relationships | [6] [48] |
| Population PK/PD Analysis | Inter-individual variability, Covariate effects | Identifies factors (e.g., body weight) influencing insulin exposure and response | [48] |
Quantitative Comparison of Insulin Analogs
Pharmacokinetic Parameters Across Insulin Types
Pharmacokinetic parameters vary significantly between insulin types, primarily due to differences in absorption rates from the subcutaneous tissue. Rapid-acting analogs exhibit faster absorption and earlier peak concentrations compared to regular human insulin or longer-acting formulations [46]. A comparative study of various subcutaneously dosed insulin analogs demonstrated that while PK parameters—especially absorption rates—varied between insulin types, researchers could identify a common set of nonlinear PD parameters to account for dose-related differences in glucose utilization [6].
For premixed insulin lispro 25, a bioequivalence study comparing test and reference formulations reported maximum concentration (Cmax) values of 1.40 ± 0.452 ng·mL⁻¹ and 1.36 ± 0.418 ng·mL⁻¹, respectively, with area under the curve (AUC₀–₂₄h) values of 497 ± 107 and 510 ± 86.2 ng·h·mL⁻¹ [3]. The 90% confidence intervals for the geometric mean ratios of the main PK parameters fell within the bioequivalence range of 80%-125%, supporting the interchangeability of these formulations [3].
Pharmacodynamic Profiles and Clinical Implications
The pharmacodynamic differences between insulin analogs have direct clinical consequences. Rapid-acting analogs control postprandial glucose excursions more effectively than human insulin due to their more physiological PK/PD profile [46]. Studies comparing the three marketed rapid-acting analogs—insulin lispro, insulin aspart, and insulin glulisine—suggest they are equally efficacious and safe, though some research indicates insulin glulisine may have a slightly faster onset of action [46].
For premixed insulin lispro 25, pharmacodynamic parameters measured by euglycemic clamp include GIRmax values of 4.47 ± 2.12 and 4.12 ± 1.81 mg·kg⁻¹·min⁻¹ for test and reference formulations, respectively, with AUCGIR₀–₂₄h values of 2,994 ± 1,232 and 2,994 ± 941 mg·h·kg⁻¹·min⁻¹ [3]. The duration of insulin action varies considerably between analogs, with rapid-acting formulations typically lasting 3-5 hours while long-acting analogs provide basal coverage for up to 24 hours or more [6].
Table 2: Comparative PK/PD Parameters of Insulin Analogs
| Insulin Type | Tmax (hr) | Cmax (ng·mL⁻¹) | AUC (ng·h·mL⁻¹) | GIRmax (mg·kg⁻¹·min⁻¹) | AUCGIR (mg·h·kg⁻¹·min⁻¹) | Clinical Applications | |
|---|---|---|---|---|---|---|---|
| Premixed Lispro 25 (Test) | Not specified | 1.40 ± 0.452 | 497 ± 107 | 4.47 ± 2.12 | 2,994 ± 1,232 | Prandial and basal coverage in single injection | [3] |
| Premixed Lispro 25 (Reference) | Not specified | 1.36 ± 0.418 | 510 ± 86.2 | 4.12 ± 1.81 | 2,994 ± 941 | Prandial and basal coverage in single injection | [3] |
| Rapid-acting Analogs (general) | 0.5-1.5 | Varies by specific analog | Varies by specific analog | Varies by specific analog | Varies by specific analog | Mealtime glucose control | [46] |
Modeling Approaches for Regimen Visualization
Mechanistic PK/PD Modeling Framework
Mechanistic pharmacokinetic and pharmacodynamic modeling provides a powerful framework for visualizing and predicting insulin action over time. These models typically incorporate sequential first-order processes for subcutaneous insulin absorption, linear elimination kinetics, and various pharmacodynamic components to describe the effects on glucose utilization [6]. The PD effects are often captured using a combination of biophase distribution, indirect response mechanisms, and receptor down-regulation components to account for the complex temporal relationship between insulin concentration and glucose-lowering effects [6].
Advanced modeling approaches can simulate the glucose infusion rate profiles for insulin analogs with different absorption characteristics. For instance, researchers have used identified PK/PD parameters to illustrate GIR profiles for rapid-acting insulin analogs with 30% and 50% faster absorption times than currently available options, providing valuable insights for the development of next-generation insulin formulations [47]. These models serve as the foundation for educational tools that can demonstrate the comparative time-action profiles of different insulin regimens.
Model Development Workflow: This diagram illustrates the sequential process of developing integrated PK/PD models for insulin analogs, from data collection through to simulation of treatment regimens.
Visualization of Time-Action Profiles
The integration of PK/PD parameters into mathematical models enables the visualization of time-action profiles for different insulin analogs and regimens. These visualizations typically display both the pharmacokinetic profile (serum insulin concentration over time) and the corresponding pharmacodynamic response (glucose infusion rate over time) on aligned axes, allowing for direct comparison of onset, peak action, and duration between different insulin formulations [6] [47].
For premixed insulins like lispro 25, these models can illustrate the biphasic action profile resulting from the combination of rapid-acting and intermediate-acting components, showing an initial peak corresponding to the mealtime bolus followed by a sustained plateau from the protamine-formulated portion [3]. Such visualizations are invaluable educational tools for healthcare professionals and patients, facilitating understanding of the temporal characteristics of different insulin therapies and supporting appropriate timing of injections and meals.
Research Reagent Solutions and Essential Materials
The experimental approaches described require specialized reagents, equipment, and analytical tools. The following table details key research solutions essential for conducting rigorous insulin PK/PD studies.
Table 3: Essential Research Reagents and Materials for Insulin PK/PD Studies
| Reagent/Material | Function in Research | Application Examples | References |
|---|---|---|---|
| Euglycemic Clamp System | Maintains constant blood glucose while measuring glucose infusion rate | Gold standard assessment of insulin pharmacodynamics | [3] [47] |
| HPLC-Mass Spectrometry | Quantifies plasma concentrations of insulin analogs | PK analysis of insulin lispro and other analogs | [3] |
| ELISA Kits | Measures C-peptide levels to assess endogenous insulin suppression | Validation of clamp quality and endogenous insulin suppression | [3] |
| Recombinant Insulin Analogs | Reference standards for analytical methods and bioactivity assays | Quality control and comparative studies | [3] [46] |
| MONOLIX/WinNonlin Software | Population PK/PD modeling and bioequivalence assessment | Parameter estimation, model development, and simulation | [6] [3] |
| Validated Immunoassays | Quantifies therapeutic monoclonal antibodies like denosumab | PK analysis of biologic drugs and biosimilars | [48] |
PK/PD Relationship Visualization: This diagram shows the logical relationship between pharmacokinetic processes and pharmacodynamic effects in insulin action, culminating in the measured glucose infusion rate.
The comparative analysis of insulin analog PK/PD properties through sophisticated modeling approaches provides invaluable insights for drug development, clinical practice, and patient education. The structured comparison presented in this guide demonstrates significant differences in absorption kinetics, concentration profiles, and glucose-lowering effects across insulin types, which directly influence their clinical application and dosing regimens. The integration of euglycemic clamp data with mechanistic PK/PD models creates a powerful framework for visualizing insulin action profiles and simulating the effects of different treatment strategies. These models serve as the foundation for developing educational tools that can enhance understanding of insulin therapy among healthcare professionals and patients alike. As research in this field advances, particularly with the development of ultra-rapid-acting analogs and once-weekly insulin formulations, the continued application and refinement of these modeling approaches will be essential for optimizing diabetes management and improving patient outcomes.
Addressing Clinical Variability and Stability Challenges in Insulin Therapy
Hypoglycemia remains a primary limiting factor in achieving optimal glycemic control with insulin therapy and certain non-insulin medications. The risk of hypoglycemia is intrinsically linked to the pharmacokinetic (PK) and pharmacodynamic (PD) profiles of these therapeutic agents. PK properties—absorption, distribution, metabolism, and excretion—determine the timing and concentration of a drug in the bloodstream. PD properties describe the biochemical and physiological effects of the drug, specifically its glucose-lowering activity over time. Discrepancies between a drug's PK and PD profiles can create periods of insulin excess relative to glucose availability, thereby increasing hypoglycemia risk.
Advancements in drug development have focused on creating analogs with PK/PD profiles that more closely mimic physiological insulin secretion or provide glucose-dependent mechanisms of action. This guide objectively compares the hypoglycemia risk profiles of various insulin analogs and non-insulin therapies based on their PK/PD characteristics and supporting clinical data, providing researchers and drug development professionals with a clear framework for evaluating safety considerations in therapeutic design.
PK/PD Profiles of Insulin Analogs and Hypoglycemia Risk
Rapid-Acting Insulin Analogs
Table 1: PK/PD Profiles of Rapid-Acting Insulin Analogs
| Insulin Analog | Onset of Action | Time to Peak Effect | Duration of Action | Hypoglycemia Risk Profile |
|---|---|---|---|---|
| Insulin Lispro [21] | 5-15 minutes | 30-60 minutes | 3-4 hours | Reduced post-absorptive hypoglycemia vs RHI due to shorter duration |
| Insulin Aspart [21] | 10-20 minutes | 40-50 minutes | 3-5 hours | Similar risk reduction profile to insulin lispro |
| Insulin Glulisine [21] | 20 minutes | 1 hour | 4 hours | Shorter duration reduces late postprandial hypoglycemia |
| Faster-acting Aspart [50] | ~5 minutes faster than aspart | Earlier peak than aspart | Similar to aspart | Enhanced postprandial control; potential for better timing alignment |
| Technosphere Insulin (TI) [51] | 7-15 minutes to 10% of max GIR | Rapid absorption | 2-6 hours (dose-dependent) | Ultrarapid absorption requires higher doses for same total effect; unique PK/PD |
Rapid-acting analogs were engineered to address the PK limitations of regular human insulin (RHI), which has a slow onset (30 minutes) and prolonged duration (6-8 hours) that increases hypoglycemia risk between meals and causes "insulin stacking" with multiple daily injections [21]. The faster onset of rapid-acting analogs allows for dosing closer to mealtime, while their shorter duration significantly reduces late postprandial hypoglycemia risk [50].
Notably, the absorption rate profoundly impacts the PD effect. Technosphere Insulin (TI), an inhaled formulation, demonstrates ultrarapid absorption with time to maximum concentration occurring at 13 minutes compared to 121 minutes for subcutaneous RHI [51]. This rapid absorption produces higher peak concentrations and shorter exposure durations, resulting in a smaller total glucose-lowering effect per unit than subcutaneous rapid-acting analogs, making unit-for-unit conversion inappropriate [51].
Long-Acting Insulin Analogs
Table 2: PK/PD Profiles of Long-Acting Insulin Analogs
| Insulin Analog | Onset of Action | Peak Profile | Duration of Action | Hypoglycemia Risk Profile |
|---|---|---|---|---|
| Insulin Glargine U100 [21] [50] | 1-2 hours | Relatively flat | ~24 hours | Lower hypoglycemia risk vs NPH due to peakless profile |
| Insulin Detemir [21] [50] | 1.6-3 hours | Flat | Up to 24 hours (dose-dependent) | Reduced nocturnal hypoglycemia vs NPH; twice-daily dosing often required |
| Insulin Degludec [50] | ~1-2 hours | Stable and flat | >42 hours | Consistently lower hypoglycemia rates, especially nocturnal |
| Insulin Icodec [27] | ~1-2 hours | Stable weekly profile | ~7 days (once-weekly) | Model-predicts no sustained increase in hypoglycemia vs daily basal insulin |
Long-acting analogs provide a more physiological basal insulin replacement than NPH insulin, which has a pronounced peak effect at 3-8 hours and duration of 12-15 hours, creating significant hypoglycemia risk, particularly nocturnal [21]. Insulin glargine and detemir provide relatively peakless profiles for approximately 24 hours, with glargine having a flat time-action profile and detemir showing dose-dependent duration [21] [50].
The American Association of Clinical Endocrinologists and the American College of Endocrinology strongly recommend against NPH insulin in favor of longer-acting insulin analogs due to better reproducibility, consistency between and within patients, and corresponding reduction in hypoglycemia risk [21]. Insulin degludec, with its ultra-long duration exceeding 42 hours and low peak-to-trough fluctuation, demonstrates consistently lower rates of hypoglycemia, especially nocturnal episodes, in clinical trials [50].
Novel weekly insulins like icodec represent the next frontier in basal insulin development. PK/PD modeling of insulin-experienced type 2 diabetes patients switching to icodec predicts that omitting a one-time additional 50% loading dose would not result in sustained effects on hypoglycemia rates or glycemic control over 26 weeks [27].
Non-Insulin Therapies: Glucose-Dependent Mechanisms
GLP-1 Receptor Agonists and Hypoglycemia Risk
Table 3: GLP-1 Receptor Agonists Hypoglycemia Profile
| GLP-1RA | Dosing Frequency | Hypoglycemia Mechanism | Clinical Hypoglycemia Risk |
|---|---|---|---|
| Lixisenatide [52] | Once daily | Glucose-dependent insulin secretion | Highest reporting odds ratio for hypoglycemia (ROR 28.03) among GLP-1RAs |
| Liraglutide [52] [53] | Once daily | Glucose-dependent insulin secretion | Increased risk when combined with sulfonylureas (9.2% vs 2.6% placebo) |
| All GLP-1RAs [53] | Varies by formulation | Glucose-dependent action; minimal risk as monotherapy | Overall lower hypoglycemia risk vs insulin; increased with concomitant insulin/sulfonylurea use |
GLP-1 receptor agonists (GLP-1RAs) lower blood glucose through glucose-dependent insulin secretion, glucagon suppression, delayed gastric emptying, and central appetite regulation [54] [53]. This glucose-dependent mechanism inherently minimizes hypoglycemia risk when used as monotherapy or without concomitant insulin or insulin secretagogues.
However, real-world pharmacovigilance data reveals important differences among GLP-1RAs. An analysis of the FDA Adverse Event Reporting System (FAERS) between 2004-2020 identified 1,164 GLP-1RA-associated hypoglycemia cases, disproportionately affecting middle-aged patients and females [52]. Lixisenatide demonstrated the strongest association with hypoglycemia with a reporting odds ratio of 28.03, while no significant relationship was found for albiglutide [52]. The median time to hypoglycemia onset was 5 days following GLP-1RA initiation, with overall fatality and hospitalization proportions of 3.53% and 56.08%, respectively [52].
Metformin and Minimal Hypoglycemia Risk
Metformin, a first-line biguanide for type 2 diabetes, lowers both basal and postprandial plasma glucose primarily by suppressing hepatic glucose production without stimulating insulin secretion [55]. This mechanism, coupled with its PK properties—not metabolized, excreted unchanged in urine with a half-life of ~5 hours—results in minimal hypoglycemia risk when used as monotherapy [55].
Population PK/PD modeling using a signal transduction model has characterized the antihyperglycemic effect of metformin, with efficacy and potency estimates of 19.8 and 3.68 µg/mL, respectively [56]. Metformin's transport into tissues is mediated by organic cation transporters (OCT1, OCT2, OCT3) and multidrug and toxin extrusion proteins (MATE1, MATE2-K), with polymorphisms in these transporters contributing to the variable glycemic response observed between individuals [55].
Experimental Protocols for PK/PD Assessment
Euglycemic Clamp Studies
The euglycemic clamp technique remains the gold standard for assessing insulin PK/PD relationships. Key methodological considerations include:
Study Population: Participants are typically individuals with type 1 diabetes to eliminate endogenous insulin secretion confounding results. For example, a TI vs. lispro study enrolled type 1 diabetes patients with stable regimens for ≥2 months [51].
Clamp Procedure: The ClampArt device or equivalent systems infuse 20% glucose to maintain blood glucose at a predetermined target level (typically 100 mg/dL). Insulin glulisine may be infused initially to achieve target glucose, with infusion discontinued 20 minutes before study drug administration [51].
Dosing and Measurements: Volunteers receive multiple treatments in crossover designs. In the TI study, participants received three doses each of TI (10, 30, 120 U) and lispro (8, 30, 90 U) while undergoing euglycemic clamps [51]. Serum insulin concentrations are measured using specific radioimmunoassays, with blood samples collected at predetermined intervals.
Endpoint Assessment: Primary PD endpoints include area under the glucose infusion rate (GIR) curve from treatment start to clamp end. Key secondary endpoints include GIRmax, time to GIRmax, time to onset of effect, and end of effect [51].
Pharmacovigilance and Real-World Evidence
Methodologies for assessing hypoglycemia risk in real-world settings:
Data Source Identification: Large databases like the FDA FAERS provide spontaneous adverse event reports. One analysis examined reports from January 2004 to September 2020, resulting in 12,552,899 cases after deduplication [52].
Case Identification: Adverse events are coded using MedDRA preferred terms. Hypoglycemia cases are identified using terms: "Hypoglycemia," "Hypoglycaemia," and "Hypoglycaemic conditions NEC" [52].
Statistical Analysis: Disproportionality analyses using reporting odds ratio and proportional reporting ratio, and Bayesian methods including Bayesian confidence propagation neural network and multi-item gamma Poisson shrinker are applied to detect safety signals [52].
Signaling Pathways and Experimental Workflows
GLP-1 Receptor Agonism Glucose-Lowering Pathway
GLP-1 Agonist Glucose-Dependent Mechanism
Euglycemic Clamp Experimental Workflow
Euglycemic Clamp Methodology
Research Reagent Solutions
Table 4: Essential Research Materials for PK/PD Studies
| Research Tool | Specific Application | Function in Experimental Protocol |
|---|---|---|
| ClampArt Device [51] | Euglycemic clamp studies | Automated glucose monitoring and infusion system for maintaining target blood glucose levels |
| Radioimmunoassays [51] | Insulin concentration measurement | Quantification of serum insulin levels (e.g., Human Insulin-Specific RIA, LisPro Insulin RIA) |
| GLP-1 Receptor Binding Assays | GLP-1RA studies | Determination of agonist affinity and activation of GLP-1 receptors |
| Technosphere Insulin Formulation [51] | Pulmonary insulin delivery | Dry-powder formulation of recombinant human insulin adsorbed onto Technosphere microparticles |
| MedDRA Coding System [52] | Pharmacovigilance studies | Standardized terminology for adverse event classification (hypoglycemia terms) |
| Population PK/PD Modeling Software [27] [56] | Data analysis | NONMEM for population modeling; signal transduction model implementation |
The strategic optimization of PK/PD profiles represents a critical pathway for mitigating hypoglycemia risk in diabetes therapeutics. Rapid-acting insulin analogs with shorter durations reduce late postprandial hypoglycemia, while long-acting analogs with flat, peakless profiles minimize nocturnal hypoglycemia compared to NPH insulin. Beyond insulin, GLP-1 receptor agonists leverage glucose-dependent mechanisms that inherently limit hypoglycemia risk, particularly when used without concomitant insulin secretagogues.
Future directions include the development of weekly insulins like icodec with stable profiles that may further reduce hypoglycemia excursions, and dual/triple receptor agonists that optimize glycemic control through multiple pathways. For researchers and drug development professionals, careful attention to PK/PD relationships through robust methodologies like euglycemic clamp studies and pharmacovigilance analyses remains essential for designing next-generation therapies that maximize efficacy while minimizing the persistent challenge of hypoglycemia.
In pharmacokinetic (PK) and pharmacodynamic (PD) studies of insulin, controlling variability is paramount to achieving predictable glycemic control. Variability in insulin effect hampers the achievement of optimal glycemic control and is associated with diminished health-related quality of life [57]. This guide objectively compares the PK/PD performance of various insulin analogs and formulations while identifying key sources of variability and evidence-based strategies to mitigate them. The content is framed within the broader thesis that understanding and controlling these variables through proper injection technique, consideration of demographic factors, and acknowledgment of comorbidities leads to more reproducible and effective insulin therapy, thereby advancing diabetes treatment outcomes.
PK/PD Profiles of Insulin Analogs and Formulations
Modifications of the insulin molecule have resulted in long-acting (e.g., glargine, detemir) and rapid-acting analogs (e.g., aspart, lispro, glulisine) with improved PK/PD profiles compared to conventional human insulins like NPH (Neutral Protamine Hagedorn) and regular human insulin (RHI) [21]. These profiles determine their clinical use for basal or prandial coverage.
Table 1: Comparison of Insulin PK/PD Profiles
| Insulin Type | Onset of Action | Peak Action | Duration of Action | Key Characteristics |
|---|---|---|---|---|
| Rapid-acting (Lispro) [21] | 5–15 minutes | 30–60 minutes | 3–4 hours | Faster onset and shorter duration than RHI; better postprandial glucose control. |
| Rapid-acting (Aspart) [21] | 10–20 minutes | 40–50 minutes | 3–5 hours | Rapid-acting analog; absorption can be accelerated by jet injection [57]. |
| Short-acting (RHI) [21] | 30 minutes | 60–120 minutes | 6–8 hours | Must be administered 30+ minutes before meals; prolonged action increases hypoglycemia risk. |
| Intermediate-acting (NPH) [21] | 1–2 hours | 3–8 hours | 12–15 hours | Distinct peak, does not match peak-less physiologic basal secretion. |
| Long-acting (Glargine) [21] | 1–2 hours | Flat | ~24 hours | Synthetic analog with a relatively peakless profile for ~24 hours. |
| Long-acting (Detemir) [21] | 1.6 hours | Flat | Up to 24 hours | Dose-dependent duration; lower risk for hypoglycemia than NPH. |
| U-500 Regular [58] | Within 11-16 min | Significantly longer than U-100R | Extended duration | Concentrated formulation; shows lower Cmax and longer tmax/tRmax at high doses (100U). |
| Once-Weekly Icodec [12] | - | - | ~7 days | Novel basal analog; PK/PD modeling supports switching from daily basal without a loading dose. |
The absorption rate is a primary differentiator between insulin types. For instance, mechanistic PK/PD models show that while PK parameters—especially absorption rates—vary significantly between insulin types, a common set of nonlinear PD parameters can account for dose-related differences in glucose utilization [6]. Furthermore, formulation concentration impacts the profile; U-500 regular insulin (500 U/mL) demonstrates a significantly longer duration of action and lower peak concentration compared to an equal unit-dose of U-100 regular insulin, making its time-action profile more suitable for certain highly insulin-resistant patients [58].
Injection Technique and Site Factors
The method of insulin delivery is a major, often overlooked, source of variability. Consistently delivering insulin into the subcutaneous (SC) fat is crucial for predictable absorption and action [59].
- Needle Length and Intramuscular (IM) Injection: Using needles that are too long raises the risk of IM injection. Insulin delivered intramuscularly is absorbed variably and substantially faster, especially if the muscle is exercised, leading to erratic PK and increased risk of hypoglycemia [59]. Evidence-based recommendations state that 4-mm pen needles are appropriate for all patients, regardless of age, sex, or BMI, as they are long enough to penetrate the skin into the SC fat but present a low risk of IM injection when inserted perpendicularly without a skinfold [59].
- Lipohypertrophy (LH): This skin condition, characterized by a raised, rubbery swelling of the SC fat, has a prevalence of ≥50% among injecting patients. Injecting into LH substantially increases PK/PD variability, reduces insulin absorption and action, and raises postprandial glucose. Proper injection site rotation is critical to prevent its development [59].
- Injection Device: Jet injectors, which deliver insulin as a high-velocity spray across the skin, can advance the time to maximal insulin concentration and glucose-lowering effect by ~40% compared to conventional pen injections [57]. While this can accelerate absorption, the associated variability in pharmacologic endpoints remains considerable and is similar to that of conventional administration [57].
Demographic and Clinical Patient Factors
The PK/PD profiles of insulin analogs may be influenced by many patient-specific variables, though these do not have equivalent effects on all insulins [21].
- Body Composition: Subcutaneous adipose tissue thickness is highly variable and depends on BMI, sex, and injection site. For example, post-pubertal females have, on average, 5 mm more SC fat than males at a given BMI and injection site. This variability in SC tissue thickness directly influences the risk of IM injection, particularly when using longer needles [59].
- Renal and Hepatic Function: These conditions can alter the PK/PD of insulins, as the kidneys and liver are primary sites of insulin clearance. Dosing requirements may need adjustment in patients with significant impairment, though the effect varies between different insulin analogs [21].
- Age and Ethnicity: Age and race/ethnicity have been identified as factors that can influence the PK/PD of insulin analogs, necessitating consideration when designing treatment regimens for special patient groups [21].
The Role of Comorbidities and Concomitant Conditions
- Obesity and Insulin Resistance: In conditions of severe insulin resistance requiring high-dose insulin, concentrated formulations like U-500R are used. PK/PD modeling of high-dose U-500R suggests that twice-daily (BID) or thrice-daily (TID) dosing provides a more gradual increase and stable basal insulin effect compared to once-daily (QD) dosing, which shows greater fluctuations [58]. Furthermore, Body Mass Index (BMI) has been identified as a significant covariate contributing to the interindividual variability of the maximum pharmacologic effect (Emax) in PK/PD models [58].
- Pregnancy: Pregnancy and gestational diabetes mellitus can alter insulin pharmacokinetics and dynamics, requiring careful management and monitoring [21].
Experimental Protocols for Assessing Variability
The Euglycemic Clamp Technique
The euglycemic glucose clamp is considered the gold standard for assessing the PK/PD properties of insulin and its analogs [3]. This method directly measures the glucose-lowering effect (pharmacodynamics) of insulin while simultaneously characterizing its pharmacokinetics.
Table 2: Research Reagent Solutions for Euglycemic Clamp Studies
| Research Reagent / Material | Function in Experiment |
|---|---|
| Insulin Analog (e.g., Aspart, Lispro) | The investigational product whose PK/PD profile is being characterized. |
| 20% Glucose Solution | Intravenously infused to maintain target blood glucose levels; the infusion rate (GIR) is the primary PD measure. |
| Glucose Analyzer (e.g., Biosen C-line) | Provides immediate, precise measurement of plasma/blood glucose levels at frequent intervals (e.g., every 5-10 min) to guide glucose infusion [57]. |
| Radioimmunoassay (RIA) / HPLC-MS | Used to measure serum or plasma insulin concentrations from collected blood samples for PK analysis [57] [3]. |
| Heated Box (~55°C) | Used to arterialize venous blood from the sampling arm, ensuring blood samples more closely represent arterial glucose levels [57]. |
| ELISA for C-peptide | Measures C-peptide levels to confirm suppression of endogenous insulin secretion during the clamp, validating the platform's stability [3]. |
Detailed Methodology: In a typical single-dose, crossover clamp study [57] [3]:
- Subject Preparation: Healthy volunteers or patients fast overnight. On the test day, intravenous catheters are placed for blood sampling and glucose/insulin infusion.
- Baseline & Insulin Administration: Baseline blood glucose and insulin levels are measured. A subcutaneous dose of the test insulin (e.g., 0.2-0.3 U/kg) is administered.
- Clamping: Plasma glucose is measured frequently (e.g., every 5-10 minutes). A variable-rate intravenous infusion of 20% glucose is adjusted based on these measurements to maintain blood glucose at a predetermined target level (e.g., 5.0 mmol/L ± 10%).
- Data Collection: The Glucose Infusion Rate (GIR) required to maintain euglycemia is recorded continuously as the primary PD endpoint. Blood is sampled at scheduled intervals for the measurement of serum insulin concentration (PK endpoint) and C-peptide.
PK/PD Modeling and Simulation
Mechanistic PK/PD modeling is used to quantitatively describe the time course of insulin absorption and its effects, and to simulate different dosing scenarios.
- PK Modeling: Insulin absorption from the SC tissue is often described using a one-compartment model with sequential first-order processes and linear elimination. Models may estimate separate absorption rate constants (Ka) for different formulations (e.g., U-500R vs. U-100R) [6] [58].
- PD Modeling: The relationship between insulin concentration and effect often incorporates an "effect compartment" to account for the observed time delay (hysteresis). The PD effect (GIR) is then frequently modeled using a maximum effect (Emax) model, parameterized by Emax and the concentration to achieve 50% of Emax (EC50) [58].
- Application: This approach allows researchers to predict steady-state activity for various regimens (e.g., QD, BID, TID for U-500R) [58] or to model the outcomes of switching therapies, such as transitioning from daily basal insulin to once-weekly icodec [12].
Visualizing Variability Factors and Experimental Flow
The following diagram synthesizes the key sources of insulin PK/PD variability and the primary experimental method used to quantify them, illustrating their interrelationships.
The workflow for conducting a euglycemic clamp study, from setup to data analysis, is outlined in the diagram below.
The pursuit of optimal glycemic control is fundamentally linked to the management of PK/PD variability. Evidence demonstrates that this variability stems from a confluence of factors related to the insulin formulation, the injection technique, and intrinsic patient characteristics. Key strategies for mitigating variability include adopting shorter (4-mm) needles to ensure consistent SC deposition, rigorously avoiding injections into lipohypertrophic sites, and selecting insulin analogs with more favorable and predictable profiles. The euglycemic clamp remains the indispensable tool for objectively characterizing this variability and comparing the performance of insulin products. For researchers and drug development professionals, a rigorous approach that integrates proper injection technique, thoughtful consideration of demographic and clinical variables, and sophisticated PK/PD modeling is essential for developing and deploying insulin therapies that are both effective and reproducible in real-world populations.
The therapeutic management of diabetes mellitus relies heavily on the use of insulin and its engineered analogs. A significant challenge in the development of these biopharmaceuticals, particularly those designed for long-acting or once-weekly administration, is their inherent molecular instability. Recent research has uncovered redox-mediated degradation as a critical mechanism that compromises the integrity of insulin analogs in the bloodstream. This process involves the thiol–disulphide exchange reaction, which leads to the cleavage of insulin's interchain disulfide bonds and its subsequent dissociation into separate, inactive A- and B-chains [60] [61].
For conventional insulin analogs with short half-lives, this degradation pathway is negligible due to their rapid clearance. However, for ultra-long-acting analogs like insulin icodec, which can circulate for up to a week, susceptibility to this redox-driven chain-splitting becomes a major determinant of both in vivo potency and half-life [60] [61]. Consequently, the strategic design of next-generation, ultra-stable insulin analogs now focuses on introducing molecular modifications that confer enhanced resistance to this degradation mechanism, paving the way for more effective and convenient diabetes therapies.
Redox-Mediated Degradation: A Key Mechanism in Insulin Clearance
The Molecular Mechanism of Chain-Splitting
The insulin monomer is a small protein comprising an A-chain and a B-chain, linked by two interchain disulfide bonds (A7-B7 and A20-B19). A third, intrachain disulfide bond exists within the A-chain (A6-A11) [16] [61]. The solvent exposure and structural flexibility around these bonds, particularly the A7-B7 disulfide, make them susceptible to attack by small-molecule thiols present in plasma, such as glutathione and cysteine [60] [61].
This thiol–disulfide exchange reaction can proceed through a series of steps, ultimately resulting in the full separation of the A- and B-chains. Once separated in the circulation, the extremely low concentration of these chains makes their recombination effectively impossible, rendering the insulin molecule permanently inactive [60]. This degradation pathway represents a significant non-receptor-mediated clearance mechanism that gains prominence for insulin analogs with prolonged circulation times.
The following diagram illustrates the logical relationship between insulin's structure, the redox environment, and the resulting degradation pathway.
Comparative Susceptibility of Insulin Analogs
The susceptibility of an insulin analog to redox-mediated degradation is not uniform. It is intrinsically linked to the molecule's thermodynamic folding stability and structural flexibility, which are directly influenced by its specific amino acid sequence and modifications [61]. Analogs with lower stability and greater flexibility allow for increased solvent exposure of their disulfide bonds, accelerating the chain-splitting reaction.
Investigations using in vitro assays under controlled redox potential have demonstrated stark differences between analogs. In one such assay, human insulin was found to be highly susceptible, whereas insulin icodec, which incorporates several stabilizing substitutions, showed significantly greater resistance to degradation [61]. The study further deconstructed the contribution of individual substitutions in insulin icodec, revealing that the A14E (TyrA14→Glu) substitution provided a substantial stabilizing effect, with the B25H (PheB25→His) and B16H (TyrB16→His) substitutions offering additional, smaller contributions to stability [60] [61].
Table 1: Impact of Amino Acid Substitutions on Insulin Stability
| Insulin Analog | Key Substitutions/Modifications | Impact on Redox Stability | Postulated Structural Mechanism |
|---|---|---|---|
| Human Insulin | - | Low (Baseline) | Native structure has flexible regions exposing disulfide bonds to thiol attack [61]. |
| Insulin Icodec | A14E, B16H, B25H, C20 fatty diacid | High | A14E strengthens electrostatic interactions; B25H may form H-bond with AsnA21, reinforcing a salt bridge; combined effect increases folding stability, reducing disulfide accessibility [60] [61]. |
| Insulin Icodec Backbone | A14E, B16H, B25H | High | The combination of these three substitutions significantly stabilizes the molecule against thiol-disulfide exchange [61]. |
| Insulin Detemir | C14 fatty acid chain at B29 | Moderate (Inference) | Fatty acid interaction with the dimer interface stabilizes the monomeric form, an effect correlated with redox stability [61]. |
Experimental Assessment of Insulin Stability
Key Methodologies and Protocols
Research into the redox stability of insulin analogs relies on a combination of rigorous biochemical and biophysical experiments. The following workflows outline the core methodologies used to quantify degradation and correlate it with structural stability.
In Vitro Redox Stability Assay: This assay directly measures an insulin analog's resistance to thiol–disulfide exchange. The protein is incubated in a buffer containing a reducing agent (e.g., glutathione) to create a controlled redox environment. Samples are taken over time and analyzed using reverse-phase high-performance liquid chromatography (RP-HPLC) to separate and quantify the intact insulin from its degradation products—the A-chain and B-chain. This allows researchers to calculate the rate of degradation and directly compare the stability of different analogs [61].
Thermodynamic Folding Stability Analysis: The folding stability of insulin analogs is typically probed by chemical denaturation. The protein is exposed to increasing concentrations of a denaturant, such as guanidine hydrochloride (GuHCl), while its structural integrity is monitored via far-UV circular dichroism (CD) spectroscopy. The CD signal, which reflects the protein's secondary structure, changes as the molecule unfolds. The midpoint of the unfolding transition ((Cm)) is determined from the resulting curve, providing a quantitative measure of the analog's thermodynamic stability. A higher (Cm) value indicates a more stable molecule [61].
Correlating Stability with Pharmacokinetics
The ultimate goal of enhancing in vitro stability is to improve in vivo performance. To confirm this link, pharmacokinetic (PK) and pharmacodynamic (PD) studies are conducted in animal models and humans. The euglycemic glucose clamp technique is the gold standard for assessing the PD profile of insulin [3] [22]. In this method, subjects are infused with insulin, and a variable-rate glucose infusion is administered to maintain blood sugar at a constant, normal level. The Glucose Infusion Rate (GIR) required to maintain euglycemia serves as a real-time measure of insulin action. PK parameters are determined by frequently measuring plasma insulin concentrations over time. Analogs with superior redox stability, such as insulin icodec, demonstrate a prolonged half-life and a stable, flat PD profile, enabling once-weekly dosing [27] [61].
The Scientist's Toolkit: Key Research Reagents and Materials
The study of insulin stability and the development of novel analogs require a specialized set of reagents and analytical tools.
Table 2: Essential Research Reagents and Materials for Insulin Stability Studies
| Reagent / Material | Function in Research | Specific Application Example |
|---|---|---|
| Redox Buffers | To create a controlled in vitro environment that mimics the thiol-disulfide challenge in plasma. | Buffers containing glutathione or cysteine to assess the rate of insulin chain-splitting [61]. |
| HPLC Systems | To separate and quantify proteins based on hydrophobicity. | Reverse-phase HPLC is used to resolve intact insulin from its degraded A- and B-chains in stability assays [3] [61]. |
| Circular Dichroism (CD) Spectrometer | To probe the secondary and tertiary structure of proteins in solution. | Used to monitor the unfolding of insulin analogs during chemical denaturation experiments to determine thermodynamic stability ((C_m)) [61]. |
| Mass Spectrometry | For precise determination of molecular mass and identification of chemical modifications. | Coupled with HPLC (LC-MS) to confirm the identity of insulin, its analogs, and degradation products [3]. |
| Crystallography Systems | To determine the high-resolution three-dimensional atomic structure of proteins. | Used to solve the crystal structure of analogs like insulin icodec, providing insights into the structural basis of their stability [61]. |
| Euglycemic Clamp Setup | The gold standard for in vivo assessment of insulin pharmacodynamics. | Used in clinical and preclinical studies to measure the glucose-lowering effect (GIR profile) of new insulin analogs over time [3] [22]. |
Comparative Analysis of Modern and Emerging Insulin Analogs
The landscape of insulin therapy has evolved significantly from human insulin to rapid-acting, long-acting, and now ultra-long-acting analogs. The following table compares key agents based on their structural features, stability, and resulting pharmacokinetic profiles.
Table 3: Pharmacokinetic and Stability Comparison of Select Insulin Analogs
| Insulin Analog (Category) | Key Structural Modifications | Primary Protraction Mechanism | Redox Stability Profile | Reported Half-life & Dosing Frequency |
|---|---|---|---|---|
| Human Insulin | - | N/A (Reference) | Low | Half-life: 0.08–0.25 hours (IV). Requires multiple daily injections [22] [61]. |
| Insulin Lispro (Rapid-acting) | B28 Lys, B29 Pro (inversion) | Reduced self-association for rapid absorption. | Not a primary concern due to short half-life. | Onset: 10-15 min. Duration: 3-5 hours. Injected at mealtimes [62] [10] [50]. |
| Insulin Glargine (Long-acting) | A21 Gly, B-chain C-terminal extension with 2 Arg | Precipitation at neutral pH at injection site. | Not a primary design focus. | Duration: ~24 hours. Typically injected once daily [62] [22] [10]. |
| Insulin Detemir (Long-acting) | B29 Lys linked to C14 fatty acid, B30 omission | Albumin binding & self-association. | Moderate (inferred from fatty acid-induced monomer stabilization) [61]. | Duration: Dose-dependent, up to ~20 hours. Often requires once or twice-daily dosing [22] [10] [50]. |
| Insulin Icodec (Ultra-long-acting) | A14E, B16H, B25H, B29K-C20 fatty diacid | Strong albumin binding + reduced receptor affinity + enhanced stability. | High (deliberately engineered via substitutions that increase folding stability) [60] [61]. | Half-life: ~196 hours (~1 week). Enables once-weekly dosing [27] [16] [61]. |
| Insulin Efsitora alfa (Ultra-long-acting) | Single-chain insulin (SCI) fusion protein | Fc-fusion protein technology; mechanism may mitigate redox degradation. | Expected to be High (single-chain topology eliminates interchain disulfide bonds susceptible to redox cleavage) [60] [16]. | Half-life: ~1 week. Enables once-weekly dosing [60] [16]. |
Future Directions and Design Strategies for Ultra-Stable Analogs
The discovery of redox-mediated degradation as a significant clearance pathway for long-circulating insulins has opened new avenues for rational drug design. Future efforts will focus on several promising strategies:
- Single-Chain Insulin (SCI) Topology: This innovative approach involves linking the A- and B-chains with a short peptide, effectively eliminating the labile interchain disulfide bonds that are the target of thiol–disulfide exchange. Insulin efsitora alfa is a prime example of this next-generation design, which inherently mitigates the risk of redox-related degradation [60] [16].
- Diselenide Substitutions: A potential biochemical workaround involves replacing the sulfur atoms in critical disulfide bonds with selenium, creating diselenide bridges. These are more stable against thiol-disulfide exchange, potentially offering a direct path to enhanced molecular robustness [60].
- Optimization of Folding Stability: Continued research will focus on identifying novel amino acid substitutions that further increase the thermodynamic folding stability of insulin, reducing structural flexibility and shielding the remaining disulfide bonds from solvent exposure [16] [61].
In conclusion, overcoming redox-mediated degradation is a critical hurdle in the development of ultra-stable insulin analogs. Through a combination of advanced experimental assessment and rational molecular design—including stabilizing amino acid substitutions, albumin binding, and innovative topological changes—researchers are successfully creating a new class of weekly insulins. These advances promise to improve the convenience, efficacy, and safety of diabetes management for millions of patients worldwide.
The pharmacological management of diabetes, particularly with insulin therapy, presents distinct challenges in special populations, including individuals with obesity, renal impairment (RI), or hepatic impairment. These conditions can significantly alter the pharmacokinetic (PK) and pharmacodynamic (PD) profiles of insulin analogs, necessitating tailored therapeutic strategies to optimize efficacy and minimize adverse events such as hypoglycemia [63] [64]. This guide provides a comparative analysis of the performance of various insulin types and non-insulin pharmacotherapies in these special populations, supported by recent experimental and real-world evidence. The content is framed within the broader context of advancing insulin analog PK/PD research, offering methodologies and insights relevant to drug development professionals and clinical researchers.
Comparative Data on Insulin Analogs in Special Populations
Pharmacokinetic and Efficacy Comparison of Insulin Types
Table 1: Pharmacokinetic and Pharmacodynamic Parameters of Various Subcutaneously Dosed Insulin Analogs from Glucose Clamp Studies [6]
| Insulin Type | Key PK Parameters (Absorption Rate) | Key PD Parameters | Modeling Insights |
|---|---|---|---|
| Rapid-acting analogs | Fastest absorption rate | Lower SC(_{50}) (higher potency) | Dose-related differences in glucose utilization best described by a combination of biophase, indirect response, and receptor down-regulation models. |
| Long-acting analogs | Slowest absorption rate | Higher SC(_{50}) (lower potency) | A common set of nonlinear PD parameters can account for glucose utilization across different insulin types. |
| Intermediate-acting | Intermediate absorption rate | Intermediate SC(_{50}) | PK parameters, especially absorption rates, were the primary source of variability between insulin types. |
| Regular human insulin | Reference absorption rate | Reference SC(_{50}) | The maximum glucose stimulation (S(_{max})) was similar across all studied insulin types. |
Insulin Performance in Renal and Hepatic Impairment
Table 2: Impact of Organ Impairment on the Pharmacokinetics of Specific Insulin Analogs
| Insulin Analog | Population | Effect on Total Insulin Exposure (vs. Normal Function) | Recommended Dose Adjustment |
|---|---|---|---|
| Once-Weekly Insulin Icodec [64] | Mild Renal Impairment | ↑ 12% | No specific dose adjustment required; dose according to individual need. |
| Moderate Renal Impairment | ↑ 24% | ||
| Severe Renal Impairment | ↑ 28% | ||
| End-Stage Renal Disease | ↑ 14% | ||
| Mild Hepatic Impairment | ↑ 13% | No specific dose adjustment required. | |
| Moderate Hepatic Impairment | ↑ 15% | ||
| Severe Hepatic Impairment | No significant difference | ||
| Insulin Glargine 300 U/ml (Gla-300) [63] | Renal Impairment (Real-world) | Not quantified (PK) | No adjustment specified; effective and safe in real-world use. |
| Aged ≥70 years (Real-world) | Not quantified (PK) | Effective with low hypoglycemia risk; supports use in older adults. |
Efficacy of Non-Insulin Pharmacotherapy in Obesity
Table 3: FDA-Approved Pharmacologic Treatments for Obesity [65]
| Medication | Mechanism of Action | Formulation and Maximum Dosing | Weight Loss Efficacy (vs. Placebo) |
|---|---|---|---|
| Orlistat | Inhibits pancreatic lipase | 120 mg orally, three times daily with meals containing fat | 2.8–4.8% total body weight loss at 52 weeks. |
| Phentermine | Increased adrenergic signaling in the CNS | Oral, up to 37.5 mg daily for a maximum of 12 weeks | 7.0–8.3% total body weight loss at 12 months. |
| Liraglutide | GLP-1 Receptor Agonist | Subcutaneous injection, 3.0 mg daily | Not quantified in result, but noted as an effective GLP-1 option. |
| Semaglutide | GLP-1 Receptor Agonist | Subcutaneous or oral formulations | Not quantified in result, but noted as an effective GLP-1 option. |
| Tirzepatide | GLP-1 and GIP Receptor Dual Agonist | Subcutaneous injection | Compared favorably to alternative anti-obesity medications. |
Detailed Experimental Protocols and Methodologies
Euglycemic Glucose Clamp Technique for Insulin PK/PD Profiling
The euglycemic glucose clamp is the gold standard method for assessing the PK and PD properties of insulin and its analogs, primarily measuring the glucose infusion rate (GIR) required to maintain stable blood glucose levels [3].
Protocol for a Clamp Study in Healthy Volunteers [3]:
- Subject Preparation: After an overnight fast, healthy volunteers (e.g., male, aged 18-45, BMI 19-24 kg/m², normal glucose tolerance) are admitted to the clinical facility.
- Baseline Establishment: Before insulin administration, baseline blood glucose is determined from samples collected at -30, -20, and -10 minutes.
- Insulin Administration: A single subcutaneous dose of the test or reference insulin preparation is administered (e.g., 0.3 IU·kg⁻¹).
- Frequent Blood Sampling: Blood is drawn frequently for up to 24-35 hours post-dose for:
- PK Analysis: Plasma concentrations of the insulin analog are measured using high-performance liquid chromatography coupled with a mass spectrometer (HPLC-MS/MS) [3].
- PD Analysis (GIR): Blood glucose is measured in real-time (e.g., every 5-30 minutes) using the glucose oxidase method.
- Endogenous Insulin Secretion: C-peptide levels are monitored via ELISA to confirm suppression of endogenous insulin secretion.
- Glucose Infusion: A 20% glucose solution is infused intravenously, and its rate is adjusted in real-time based on the measured blood glucose values to maintain levels within ±10% of the target (baseline blood glucose minus 0.28 mmol·L⁻¹). The GIR is recorded over time.
- Data Analysis: Key PK parameters (AUC₀–t, Cₘₐₓ) and PD parameters (GIRAUC₀–t, GIRₘₐₓ) are calculated. Bioequivalence is concluded if the 90% confidence intervals for the geometric mean ratios of these parameters fall within the 80-125% range [3].
Real-World Observational Study for Insulin Effectiveness
Protocol for a Prospective, Real-World Study (e.g., ATOS Study) [63]:
- Study Design: A prospective, observational, international, multicenter study conducted over 12 months.
- Participants: Insulin-naïve adults (age ≥ 18 years) with type 2 diabetes uncontrolled (HbA1c > 7% and ≤ 11%) on one or more oral antidiabetic drugs.
- Intervention: Initiation of once-daily Gla-300 treatment as per routine physician practice and local titration algorithms.
- Data Collection: Data are collected at baseline, 3, 6, and 12 months.
- Endpoints:
- Primary: Change in HbA1c and proportion of patients achieving individualized HbA1c targets.
- Secondary: Changes in fasting plasma glucose, body weight, and incidence of hypoglycemia events.
Clinical Trials in Renal/Hepatic Impairment Populations
Protocol for a Single-Dose, Open-Label, Parallel-Group Trial [64]:
- Study Population: Participants are allocated to groups based on normal organ function or varying degrees of impairment:
- Renal Impairment: Measured glomerular filtration rate (mGFR) for normal (≥90 mL/min), mild (60-<90 mL/min), moderate (30-<60 mL/min), severe (<30 mL/min), or end-stage renal disease.
- Hepatic Impairment: Child-Pugh Classification for normal, mild (Class A), moderate (Class B), or severe (Class C).
- Dosing: A single subcutaneous dose of the insulin (e.g., 1.5 U/kg of icodec) is administered.
- PK Sampling: Blood is sampled frequently for an extended period (e.g., 35 days for icodec) to fully characterize the PK profile.
- Analysis: Total insulin exposure (AUC) is compared between impairment groups and the normal function group. The clinical relevance of exposure changes is assessed to inform dose adjustment recommendations.
Signaling Pathways and Experimental Workflows
Homeostatic Regulation of Appetite and Drug Targets
The following diagram illustrates the key neurohormonal pathways regulating appetite, which serve as primary targets for modern anti-obesity pharmacotherapy [65].
Experimental Workflow for Insulin PK/PD Clamp Studies
The workflow for conducting a euglycemic clamp study, critical for characterizing insulin analogs, is outlined below [3].
The Scientist's Toolkit: Key Research Reagents and Materials
Table 4: Essential Reagents and Equipment for Insulin PK/PD and Obesity Research
| Item | Specific Example | Function in Research |
|---|---|---|
| Euglycemic Clamp System | Automated clamp device or manual setup with infusion pumps | The core platform for maintaining constant blood glucose while measuring the glucose infusion rate (GIR), the gold standard PD endpoint for insulin action [3]. |
| Analytical Instrument for Insulin Quantification | High-Performance Liquid Chromatograph coupled with Mass Spectrometer (HPLC-MS/MS) | Precisely measures plasma concentrations of insulin analogs for pharmacokinetic analysis (e.g., calculating AUC and Cₘₐₓ) [3]. |
| Glucose Assay Kit | Glucose Oxidase Method | Provides the fundamental, real-time blood glucose measurements required for conducting the euglycemic clamp and adjusting glucose infusion rates [3]. |
| Immunoassay for C-peptide | Enzyme-Linked Immunosorbent Assay (ELISA) | Measures C-peptide levels to confirm the suppression of endogenous insulin secretion during clamp studies, ensuring that the observed effects are from the exogenous insulin analog [3]. |
| Specific Insulin Analogs | Insulin Icodec, Insulin Glargine (Gla-300), Insulin Lispro (Humalog25) | Serve as the reference or test articles in comparative bioequivalence and efficacy studies [63] [3] [64]. |
The management of diabetes, particularly the transition to and optimization of insulin therapy, presents a significant challenge in clinical practice. For many patients with type 2 diabetes, the progressive nature of the disease necessitates insulin therapy, with approximately one in three individuals requiring insulin within seven years of diagnosis [66]. Regimen complexity and injection burden frequently contribute to psychological barriers, poor adherence, and delayed insulin initiation [66]. In response, diabetes therapeutics have evolved substantially toward simplified treatment strategies that maintain efficacy while reducing patient burden.
This review comprehensively compares the latest advances in insulin regimen simplification, focusing on the transition from traditional basal-bolus insulin (BBI) to advanced premixed insulin analogs and novel once-weekly basal insulins. We examine these strategies through the critical lens of pharmacokinetic (PK) and pharmacodynamic (PD) properties, which fundamentally determine the clinical application, dosing schedules, and therapeutic profiles of these formulations. By synthesizing recent clinical evidence and experimental data, we provide researchers and drug development professionals with a rigorous comparison of these therapeutic strategies for diabetes management.
Comparative Analysis of Insulin Regimens
The following table summarizes the key characteristics, advantages, and limitations of the main insulin regimens discussed in this review.
Table 1: Comparison of Insulin Simplification Strategies
| Regimen Type | Key Examples | Dosing Frequency | Glycemic Efficacy (HbA1c Reduction) | Major Advantages | Key Limitations |
|---|---|---|---|---|---|
| Basal-Bolus (BBI) | Insulin glargine + insulin aspart [67] | Multiple daily injections | ~1.00% [67] | Mimics physiological secretion; highly flexible dosing [67] | High injection burden; complex regimen [66] |
| Premixed Insulin | Humalog Mix 25, Novolin 30R [68] | Twice daily | Less satisfactory control vs. BBI [68] | Simplified regimen; fewer injections [68] | Fixed ratio; less flexibility; higher hypoglycemia risk [68] |
| Advanced Premixed Formulations | IDegAsp (insulin degludec/insulin aspart) [68] | Once or twice daily | Superior to traditional premixed [68] | Improved PK/PD profile; lower hypoglycemia risk [68] | Higher cost; still requires daily injection [68] |
| Once-Weekly Basal Insulin | Insulin icodec, Insulin efsitora alfa [66] | Once weekly | -1.26% to -1.19% (non-inferior to daily analogs) [66] | Minimal injection burden; improved adherence [66] | Emerging safety concerns in T1D; long duration if adverse effects occur [66] |
| Fixed-Ratio Combinations | IcoSema (icodec + semaglutide) [66] | Once weekly | Superior to component monotherapies [66] | Dual mechanism; enhanced efficacy [66] | Limited long-term safety data; gastrointestinal side effects [66] |
Pharmacokinetic and Pharmacodynamic Profiles
Understanding the pharmacokinetic (PK) and pharmacodynamic (PD) properties of insulin formulations is crucial for evaluating their clinical utility and positioning them within treatment algorithms. The following table summarizes key PK/PD parameters from recent clinical investigations.
Table 2: Pharmacokinetic and Pharmacodynamic Parameters of Insulin Formulations
| Insulin Formulation | Study Design | PK Parameters | PD Parameters | Reference |
|---|---|---|---|---|
| Premixed insulin lispro 25 (Generic vs. Humalog25) | Randomized, crossover, bioequivalence study in healthy males (n=52) [3] | Cmax: 1.40 ± 0.452 vs. 1.36 ± 0.418 ng·mL-1 AUC0–24h: 497 ± 107 vs. 510 ± 86.2 ng·h·mL-1 [3] | GIRmax: 4.47 ± 2.12 vs. 4.12 ± 1.81 mg·kg-1·min-1 AUCGIR0–24h: 2,994 ± 1,232 vs. 2,994 ± 941 mg·h·kg-1·min-1 [3] | [3] |
| Oral ORMD-0801 (16 mg) vs. SC insulin | Phase I, randomized, crossover clamp study in healthy males (n=20) [4] | AUCIns0-∞: 5.47 ± 3.17 vs. 7.50 ± 2.37 h·ng·mL-1 Relative bioavailability: 0.53 ± 0.25% [4] | GIRmax: 3.87 ± 1.08 vs. 3.51 ± 0.52 mg·kg-1·min-1 AUCGIR0-11h: 26.98 ± 10.69 vs. 23.74 ± 9.04 h·mg·kg-1·min-1 [4] | [4] |
| Once-weekly basal insulin analogs | Multiple Phase 3 trials (QWINT, ONWARDS) [66] | Half-life (icodec): ~196 hours [66] | HbA1c reduction: -1.26% to -1.19% (non-inferior to daily analogs) [66] | [66] |
Critical PK/PD Insights
The data reveal several important trends in insulin development. First, bioequivalence between generic and brand-name premixed insulin lispro formulations has been rigorously demonstrated, with 90% confidence intervals for the geometric mean ratio of primary PK parameters (AUC0-t and Cmax) falling within the 80%-125% range [3]. This confirms the pharmaceutical equivalence of these formulations while offering potential cost reductions.
Second, novel delivery systems such as oral insulin (ORMD-0801) show distinct PK/PD profiles characterized by lower relative bioavailability (0.53%-0.94%) but comparable glucose-lowering effects at higher doses [4]. This suggests alternative pathways or metabolite activities that may differentiate these formulations from subcutaneous administration.
Finally, the development of once-weekly basal insulins represents a fundamental shift in insulin engineering. Molecules like insulin icodec achieve their extended duration through strategic structural modifications that reduce insulin receptor affinity (approximately 100 times weaker than natural insulin for efsitora alfa), resulting in slower clearance and sustained activity [66].
Experimental Methodologies in Insulin Research
Euglycemic Clamp Techniques
The euglycemic glucose clamp remains the gold standard for assessing insulin pharmacodynamics and establishing bioequivalence between formulations [3]. This technique involves maintaining blood glucose at a constant level through variable glucose infusion rates (GIR) while administering the test insulin product.
Table 3: Key Research Reagent Solutions for Euglycemic Clamp Studies
| Reagent/Equipment | Specific Function | Research Application |
|---|---|---|
| Hyperinsulinemic-euglycemic clamp setup [4] | Maintains steady plasma insulin levels while controlling glycemia | Fundamental PD assessment for insulin formulations |
| High-performance liquid chromatography (HPLC) with mass spectrometry [3] | Precisely quantifies plasma insulin concentrations | PK parameter determination (AUC, Cmax, Tmax) |
| ELISA for C-peptide [3] | Measures endogenous insulin secretion | Assesses endogenous insulin suppression during clamp studies |
| Point-of-care (POC) glucometers [67] | Provides immediate glucose measurements | Enables real-time glucose infusion rate adjustments |
| Continuous glucose monitoring (CGM) systems [66] | Tracks interstitial glucose concentrations continuously | Captures glycemic variability and time-in-range metrics |
A typical clamp procedure for premixed insulin evaluation involves administering 0.3 IU·kg-1 of the test preparation subcutaneously to healthy volunteers [3]. Blood samples for PD assessment are collected frequently (every 5 minutes up to 2 hours, every 10 minutes from 2 to 8 hours, then with decreasing frequency up to 24 hours) to immediately determine blood glucose concentration using the glucose oxidase method [3]. The intravenous infusion of 20% glucose solution is adjusted in real-time according to blood glucose levels, and the GIR is calculated to maintain blood glucose within ±10% of the target value [3].
Figure 1: Experimental workflow for insulin pharmacokinetic/pharmacodynamic studies using euglycemic clamp methodology.
Clinical Trial Designs for Regimen Comparison
Randomized controlled trials and real-world evidence studies provide complementary insights into insulin regimen performance. A notable retrospective observational study compared split-mixed insulin regimens (2004-2007) with basal-bolus insulin regimens (2008-2018) in hospitalized patients [67]. This study employed propensity score matching to balance confounding covariates, including sex, age, body mass index, and HbA1c [67]. The findings demonstrated that structured BBI regimens significantly improved both fasting glucose (129.4±3.2 mg/dL vs. 147.4±3.1 mg/dL) and preprandial glucose (152.8±2.8 mg/dL vs. 177.7±2.8 mg/dL) compared to split-mixed regimens by day 6 of hospitalization [67].
For novel once-weekly insulins, phase 3 trials have implemented sophisticated study designs. The QWINT program for efsitora alfa included multiple patient populations: insulin-naïve individuals (QWINT-1, QWINT-2), those requiring basal-bolus therapy (QWINT-4), and a long-term (78-week) assessment in patients previously on basal insulin (QWINT-3) [66]. These trials consistently employed non-inferiority designs with once-daily insulins as comparators and incorporated comprehensive safety assessments, patient-reported outcomes, and continuous glucose monitoring metrics [66].
Emerging Directions and Future Perspectives
Novel Therapeutic Targets and Combinations
Beyond insulin analogs themselves, research into combination therapies represents a promising frontier for regimen simplification. The COMBINE program recently demonstrated that the fixed-ratio combination of icodec and semaglutide (IcoSema) produced superior HbA1c reductions compared to either agent alone, though not superior to a basal-bolus regimen with glargine and aspart insulin [66].
Similarly, research has expanded to include amylin-based therapies, which target a different physiological pathway for weight management and glycemic control. Eloralintide, a once-weekly selective amylin receptor agonist, achieved up to 20.1% weight loss after 48 weeks in a phase 2 trial [69] [70]. This suggests potential for future combination approaches that leverage complementary mechanisms of action.
Figure 2: Decision pathway for simplifying complex insulin regimens using advanced therapeutic options.
Individualized Dosing Strategies
Recent investigations have explored individualized dosing approaches for insulin regimens, particularly in challenging clinical scenarios. A cross-sectional study of prednisolone-associated hyperglycemia demonstrated that individualized BBI dosing based on 24-hour intravenous insulin requirements significantly improved the proportion of glucose measurements within the target range (52.0±4.8% vs. 37.0±4.5%) compared to standard weight-based regimens [71]. This approach highlights the potential for precision medicine in insulin therapy, moving beyond one-size-fits-all dosing algorithms.
Market Trends and Adoption Patterns
The premixed insulin market continues to evolve, with current valuations of approximately $15 billion in 2025 and projected growth to $28 billion by 2033, representing a compound annual growth rate of 7% [72]. This growth is particularly pronounced in the premixed insulin analogues segment, which accounts for approximately 60% of the market, as these formulations offer superior pharmacokinetic properties and improved glucose control compared to traditional premixed human insulin [72]. Geographically, while North America and Europe currently dominate the market, the Asia-Pacific region is expected to show the most significant growth, driven by rising diabetes incidence and improving healthcare access [72].
The landscape of insulin regimen simplification has expanded dramatically with the development of advanced premixed formulations and once-weekly basal insulins. The pharmacokinetic and pharmacodynamic properties of these agents directly influence their clinical application, with each regimen offering distinct advantages and limitations.
Basal-bolus insulin therapy remains the most physiologically precise approach, mimicking normal insulin secretion patterns, but suffers from complexity and high injection burden [67]. Traditional premixed insulins reduce injection frequency but compromise flexibility due to their fixed ratios, often resulting in less satisfactory glycemic control [68]. Advanced premixed analogs like IDegAsp offer improved PK/PD profiles with reduced hypoglycemia risk [68], while once-weekly basal insulins represent a fundamental shift in diabetes management by minimizing injection burden while maintaining glycemic control [66].
For researchers and drug development professionals, these advances highlight several key principles: the importance of PK/PD optimization in regimen design, the value of patient-centered outcomes in clinical trial endpoints, and the potential of novel therapeutic targets to address unmet needs in diabetes management. As the field continues to evolve, the strategic integration of these simplified regimens into treatment algorithms promises to improve both clinical outcomes and quality of life for patients requiring insulin therapy.
Head-to-Head and Model-Based Comparisons: Validating Therapeutic Equivalence and Superiority
The development of generic insulin products represents a critical avenue for increasing treatment accessibility and reducing the financial burden of diabetes management. For researchers and drug development professionals, establishing bioequivalence (BE) between a generic and its reference product is a mandatory and complex regulatory requirement. Unlike simple small-molecule generics, insulins, as biologic products, require a rigorous, evidence-based comparative approach grounded in pharmacokinetic (PK) and pharmacodynamic (PD) profiling. This guide objectively compares the performance of generic and reference insulin products, focusing on the pivotal role of euglycemic clamp studies, the primary PK/PD endpoints used for comparison, and the statistical frameworks essential for demonstrating bioequivalence. This process is situated within the broader context of insulin analog research, which relies on mechanistic PK/PD modeling to understand the underlying properties of these life-sustaining therapies [6].
Analytical Foundations of Insulin Bioequivalence
The approval of generic insulins follows an abbreviated pathway that hinges on demonstrating high similarity to a reference product, avoiding the need for extensive clinical efficacy and safety trials. The cornerstone of this demonstration is the "Totality of Evidence" approach, a comprehensive and stepwise comparison that integrates analytical, non-clinical, and clinical data [73]. The foundational principle is that if a proposed generic insulin product is shown to be highly similar to the reference product on a molecular and functional level, and its PK and PD profiles are equivalent, then its clinical efficacy and safety will likewise be equivalent.
For insulins, the clinical component of this totality of evidence almost invariably involves a comparative euglycemic clamp study in healthy volunteers or patients. This study design is considered the gold standard for assessing the PK and PD properties of insulin, as it directly measures the glucose-lowering effect while maintaining a constant blood glucose level [3]. The resulting PK and PD parameters serve as robust, quantitative surrogates for clinical efficacy, enabling a sensitive and controlled assessment of bioequivalence.
Comparative Study Design and Protocols
The establishment of bioequivalence for generic insulins is predicated on well-controlled, randomized clinical studies. The standard design and methodology ensure that any observed differences in PK/PD profiles can be attributed solely to the product being tested and not to external variables.
Standardized Clinical Trial Design
A typical bioequivalence study for insulin follows a single-dose, randomized, open-label, two-period, crossover design in a homogenous population, such as healthy male volunteers. This design effectively controls for inter-subject variability.
- Population Selection: Studies often recruit healthy volunteers with normal insulin secretion function and glucose tolerance, as their metabolic responses are more predictable. For example, a study on insulin lispro enrolled healthy male volunteers aged 18–45 with a BMI of 19–24 kg/m² and a glycosylated hemoglobin (HbA1c) ≤ 6.0% [3].
- Crossover Design: Each subject randomly receives both the test (T, generic) and reference (R, originator) formulation in two separate periods, with a washout period (e.g., 7–14 days) to eliminate carryover effects [3].
- Dosing: Subjects receive a standardized subcutaneous dose (e.g., 0.3 IU·kg⁻¹) under fasting conditions [3].
The Euglycemic Clamp Methodology
The euglycemic glucose clamp is the definitive technique for quantifying the pharmacodynamic effect of insulin. Its detailed protocol is critical for reproducibility and data quality.
- Procedure: After insulin administration, blood glucose levels are frequently measured (e.g., every 5-10 minutes). A variable-rate intravenous infusion of a glucose solution (e.g., 20%) is adjusted in real-time to maintain blood glucose at a target level, typically within ±10% of a pre-defined baseline value minus 0.28 mmol·L⁻¹ [3].
- Primary Output: The key PD measurement is the Glucose Infusion Rate (GIR), which is the amount of glucose infused over time to maintain euglycemia. The GIR profile over time directly reflects the biological activity of the insulin [3].
- Quality Control: The validity of the clamp is affirmed by stable blood glucose throughout the procedure and significant suppression of endogenous insulin secretion, as measured by C-peptide levels [3].
Table 1: Key Blood Sampling Schedule in a Euglycemic Clamp Study
| Parameter | Pre-dose | Early Phase (0-2h) | Mid Phase (2-8h) | Late Phase (8-24h) |
|---|---|---|---|---|
| Blood Glucose (PD) | -30, -20, -10 min | Every 5 min | Every 10 min | Every 20-30 min |
| Insulin (PK) | -30 min | Frequent sampling (e.g., 10, 20, 30...120 min) | Continued sampling (e.g., 150, 180...480 min) | Sparse sampling (e.g., 600, 720...1440 min) |
| C-peptide | -30 min | 60 min | 120, 240, 360, 480 min | 600, 720...1440 min |
Comparative Data and Endpoint Analysis
The core of a bioequivalence assessment lies in the head-to-head comparison of key PK and PD endpoints derived from the clamp study. The following data, based on a study comparing a generic and reference insulin lispro 25, exemplifies a successful demonstration of bioequivalence.
Table 2: Comparative PK/PD Parameters for Insulin Lispro 25 (Test vs. Reference) [3]
| Parameter | Test (T) Preparation(Mean ± SD) | Reference (R) Preparation(Mean ± SD) | Geometric Mean Ratio (T/R)90% Confidence Interval |
|---|---|---|---|
| Cmax (ng·mL⁻¹) | 1.40 ± 0.452 | 1.36 ± 0.418 | Within 80%–125% |
| AUC0–24h (ng·h·mL⁻¹) | 497 ± 107 | 510 ± 86.2 | Within 80%–125% |
| GIRmax (mg·kg·min⁻¹) | 4.47 ± 2.12 | 4.12 ± 1.81 | Within 80%–125% |
| AUCGIR0–24h (mg·h·kg·min⁻¹) | 2,994 ± 1,232 | 2,994 ± 941 | Within 80%–125% |
Key PK/PD Endpoints for Bioequivalence
- Primary PK Endpoints: These characterize the systemic exposure and absorption speed of the insulin.
- Primary PD Endpoints: These characterize the magnitude and duration of the biological effect.
For a finding of bioequivalence, the 90% confidence intervals for the geometric mean ratios (Test/Reference) of both the primary PK (AUC0-t, Cmax) and PD (AUCGIR0-t, GIRmax) endpoints must fall entirely within the pre-defined acceptance range of 80.00% to 125.00% [3]. The data in Table 2 conclusively demonstrates that the test and reference formulations of insulin lispro 25 met this stringent criteria.
Statistical Considerations and Regulatory Framework
The statistical analysis of BE studies is governed by well-defined regulatory guidance to ensure consistency and scientific rigor.
Statistical Methods for Establishing BE
The standard statistical approach involves an Average Bioequivalence analysis. The PK and PD endpoints (AUC and Cmax) are typically logarithmically transformed to better satisfy the assumptions of normality and homoscedasticity. A linear mixed-effects model is then applied to the transformed data, with the formulation (Test vs. Reference) as a fixed effect and subject and period as random effects [74]. The analysis yields the 90% confidence interval for the ratio of the geometric means of the Test to Reference product, which must be contained within the 80-125% boundary [74].
Evolving Regulatory Perspectives
The regulatory landscape for complex generics and biologics is continuously evolving. Harmonization initiatives like the Global Bioequivalence Harmonisation Initiative (GBHI) are working to align regulatory standards across agencies like the US FDA and European Medicines Agency (EMA) [75]. Key areas of discussion and evolution include:
- Model-Informed Approaches: The use of physiologically-based pharmacokinetic (PBPK) modeling is gaining recognition for supporting biowaivers, for example, for fed BE studies [75].
- Streamlining Clinical Data: There is a global trend toward reducing clinical data requirements when robust analytical and PK data can resolve residual uncertainty. For instance, Health Canada has proposed removing the routine requirement for Phase III efficacy trials for biosimilars, relying more on analytical and PK/PD data [76].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Insulin Bioequivalence Studies
| Item | Function/Application |
|---|---|
| Reference Biologic Drug | The originator insulin product (e.g., Humalog25) used as the comparator to establish bioequivalence [3]. |
| Euglycemic Clamp System | Integrated system for frequent blood glucose monitoring and variable glucose infusion to maintain a constant blood sugar level during PD studies [3]. |
| Validated Bioanalytical Assays | High-performance liquid chromatography-mass spectrometry (HPLC-MS/MS) for precise quantification of plasma insulin concentrations [3]. |
| Glucose Oxidase Reagent | Enzyme-based reagent used in analyzers for the precise and rapid enzymatic measurement of blood glucose levels during clamping [3]. |
| C-peptide ELISA Kit | For quantifying serum C-peptide levels to confirm suppression of endogenous insulin secretion, validating the clamp quality [3]. |
Experimental Workflow and Data Analysis
The following diagram illustrates the integrated workflow of a bioequivalence study for generic insulin, from initial design to final regulatory submission.
Bioequivalence Study Workflow
This guide has detailed the critical components of bioequivalence studies for generic insulins, underscoring the centrality of PK/PD endpoints and rigorous statistical design. The presented data and methodologies confirm that a well-executed euglycemic clamp study, analyzing key parameters like AUC and Cmax for PK and GIRAUC and GIRmax for PD, provides a powerful and definitive framework for demonstrating equivalence to a reference product. For the research community, mastery of these protocols and the evolving regulatory landscape is essential for successfully advancing more affordable insulin alternatives, thereby fulfilling a significant medical and public health need.
The goal of insulin therapy in diabetes management is to mimic endogenous insulin secretion as closely as possible to control both fasting and postprandial plasma glucose [21]. For decades, regular human insulin (RHI) was the standard for prandial glucose control; however, its pharmacokinetic (PK) and pharmacodynamic (PD) properties present significant limitations [21]. The development of rapid-acting insulin analogues—insulin lispro, insulin aspart, and insulin glulisine—through recombinant DNA technology represents a significant advancement by creating insulin molecules with optimized absorption profiles after subcutaneous injection [46] [7]. This guide provides a detailed comparison of the PK/PD profiles of these rapid-acting analogues against RHI, synthesizing key experimental data and methodologies relevant to researchers and drug development professionals.
Pharmacokinetic and Pharmacodynamic Properties: A Structured Comparison
The following tables summarize the core PK and PD parameters of rapid-acting insulin analogues in direct comparison to regular human insulin, compiled from clinical studies and prescribing information [21].
Table 1: Comparison of Key Pharmacokinetic (PK) Parameters
| Insulin Type | Onset of Action | Time to Peak Concentration (Tmax) | Peak Concentration (Cmax) | Duration of Action |
|---|---|---|---|---|
| Insulin Lispro | 5-15 minutes [21] | 30-90 minutes [21] | 116 mU/L [21] | 3-4 hours [21] |
| Insulin Aspart | 10-20 minutes [21] | 40-50 minutes [21] | 82.1 mU/L [21] | 3-5 hours [21] |
| Insulin Glulisine | 20 minutes [21] | 30-90 minutes [21] | 82 mU/L [21] | 4 hours [21] |
| Regular Human Insulin | ~30 minutes [21] | 50-120 minutes [21] | 51 mU/L [21] | 6-8 hours [21] |
Table 2: Comparison of Key Pharmacodynamic (PD) and Clinical Characteristics
| Insulin Type | Molecular Modification | Glucose-Lowering Effect | Hypoglycemia Risk Profile | Injection Timing Advice |
|---|---|---|---|---|
| Insulin Lispro | Proline and lysine reversed at B28 and B29 [16] | Faster onset and shorter duration than RHI [46] | Reduced risk of late postprandial hypoglycemia vs RHI [46] | Injection immediately before meals [46] |
| Insulin Aspart | Proline replaced by aspartic acid at B28 [77] | Faster onset and shorter duration than RHI [46] | Reduced risk of late postprandial hypoglycemia vs RHI [46] | Injection immediately before meals [46] |
| Insulin Glulisine | Lysine at B3 and glutamic acid at B29 [16] | Slightly faster onset in some studies [46] [78] | Reduced risk of late postprandial hypoglycemia vs RHI [46] | Injection immediately before meals [46] |
| Regular Human Insulin | Native human insulin sequence | Slower onset, prolonged tail effect [21] | Higher risk of late postprandial hypoglycemia [21] | Injection 30-45 minutes before meals [21] |
Underlying Mechanisms and Structural Basis
The improved profiles of rapid-acting analogues stem from targeted amino acid substitutions that reduce self-association.
Structural Modifications
In solution, native insulin tends to form hexamers around a zinc ion [7] [16]. Regular human insulin, when injected subcutaneously, dissociates slowly from hexamers into dimers and finally into active monomers, causing a delayed absorption profile [5] [21]. Rapid-acting analogues are engineered to have reduced self-association:
- Insulin lispro is created by reversing the proline at B28 and lysine at B29 on the B-chain [16]. This modification sterically hinders the formation of stable dimers and hexamers.
- Insulin aspart involves substituting the proline at B28 with negatively charged aspartic acid, which introduces electrostatic repulsion that destabilizes hexamer formation [77].
- Insulin glulisine is generated by replacing asparagine at B3 with lysine and lysine at B29 with glutamic acid [16]. These changes also promote a more rapid dissociation into monomers after injection.
These structural alterations facilitate faster absorption from the subcutaneous tissue into the bloodstream, enabling a more rapid onset of action that better mimics physiological mealtime insulin secretion [46] [21].
Key Experimental Models and Protocols
Robust, standardized experimental models are crucial for characterizing the PK/PD profiles of insulins.
The Euglycemic Clamp Technique
The euglycemic glucose clamp is considered the gold standard methodology for assessing the pharmacodynamics of insulin preparations [3] [77]. This procedure directly measures the glucose-lowering effect of insulin by quantifying the glucose infusion rate (GIR) required to maintain a constant target blood glucose level despite exogenous insulin administration.
Detailed Protocol:
- Subject Preparation: Healthy volunteers or patients are fasted overnight to establish a stable baseline [3] [77].
- Baseline Measurements: Blood glucose (BG) and C-peptide (a marker of endogenous insulin secretion) levels are measured multiple times before insulin injection (e.g., at -60, -30, -20, and -10 minutes) [77].
- Insulin Administration: A single subcutaneous dose of the test insulin (e.g., 0.2 U/kg or 0.3 U/kg) is administered [3] [77].
- Clamp Procedure: Following insulin injection, BG is measured frequently (e.g., every 5-10 minutes). A variable intravenous infusion of a 20% glucose solution is adjusted in real-time based on these measurements to maintain BG at a predefined target level, typically 0.28 mmol/L (5 mg/dL) below the individual's fasting baseline [3] [77].
- Data Collection: The Glucose Infusion Rate (GIR) is recorded throughout the study period (e.g., 10-24 hours) and serves as the primary PD endpoint. Key PD parameters derived from the GIR profile include:
- GIR~max~: The maximum glucose infusion rate.
- AUC~GIR,0-t~: The total area under the GIR-time curve, representing the total glucose-lowering effect.
- tGIR~max~: The time to reach GIR~max~.
- Pharmacokinetic Sampling: Blood samples are collected at frequent intervals to measure plasma insulin concentrations over time, allowing calculation of PK parameters like C~max~ (maximum concentration), T~max~ (time to C~max~), and AUC~insulin,0-t~ (total drug exposure) [3] [77].
The quality of a clamp study is validated by low coefficients of variation in blood glucose and significant suppression of endogenous C-peptide, confirming that the observed glucose-lowering effect is due to the administered insulin [3] [77].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Insulin PK/PD Research
| Item | Function in Research | Specific Application Example |
|---|---|---|
| Hyperinsulinemic-Euglycemic Clamp System | Gold standard for assessing insulin sensitivity and pharmacodynamics [3] [77]. | Measures the glucose infusion rate (GIR) required to maintain euglycemia after insulin administration, generating the primary PD profile [3] [77]. |
| High-Performance Liquid Chromatography with Mass Spectrometry (HPLC-MS/MS) | High-sensitivity quantification of specific insulin analog concentrations in plasma [3]. | Used in pharmacokinetic studies to measure plasma concentrations of insulin lispro, aspart, or glulisine over time, free from cross-reactivity with endogenous insulin [3]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Immunoassay-based quantification of proteins and peptides. | Commonly used to measure serum C-peptide levels during clamp studies to confirm suppression of endogenous insulin secretion [3]. |
| Specific Insulin Analog Immunoassays | Antibody-based assays designed for a specific insulin analog. | Critical for accurate PK studies of insulin aspart, avoiding interference from endogenous insulin and other analogs [79]. |
| Glucose Oxidase Method | Enzymatic method for precise and rapid glucose measurement. | Used for real-time analysis of blood glucose levels during euglycemic clamp studies to guide glucose infusion rates [3]. |
The collective data demonstrate that rapid-acting insulin analogues—lispro, aspart, and glulisine—consistently exhibit superior PK/PD profiles compared to regular human insulin. Their key advantages are faster absorption, quicker onset of action, and shorter duration, which translate clinically into improved postprandial glucose control and a reduced risk of late hypoglycemia [46] [21]. While minor differences exist among the analogues (e.g., glulisine may have a marginally faster onset in some studies), their overall clinical efficacy and safety are comparable [46] [78]. The euglycemic clamp technique remains the indispensable methodology for precisely characterizing these profiles. For researchers, the continued evolution of insulin therapy focuses on further improving kinetic profiles, stability, and physiological targeting, as seen in emerging classes like basal insulins and glucose-responsive analogs [16].
The pursuit of optimal basal insulin replacement therapy has been a central focus of diabetes management for decades. The ideal basal insulin aims to provide a consistent, peakless, and predictable supply to mimic physiological fasting insulin secretion, thereby achieving glycemic control without inducing hypoglycemia. Nocturnal hypoglycemia remains a particularly formidable challenge, often going undetected and presenting a significant barrier to achieving tight glycemic targets. This comparison guide objectively analyzes the performance of long-acting insulin analogs (glargine, detemir, degludec) against the traditional neutral protamine Hagedorn (NPH) insulin, with a specific focus on their capacity to reduce nocturnal hypoglycemia, supported by experimental data and grounded in pharmacokinetic and pharmacodynamic principles.
Pharmacokinetic and Pharmacodynamic Foundations
The clinical performance of basal insulins is directly rooted in their pharmacokinetic (PK) and pharmacodynamic (PD) profiles. These properties determine the onset, peak, duration of action, and ultimately, the stability of blood glucose control they can provide.
NPH Insulin: As an intermediate-acting insulin, NPH's protamine-based crystal suspension leads to a distinct peak in its time-action profile approximately 4-6 hours after injection [80]. This peak significantly contributes to the risk of nocturnal hypoglycemia when administered at bedtime. Its duration of action is relatively short (often less than 24 hours) and exhibits considerable day-to-day variability in absorption [81].
Insulin Glargine U100: The first long-acting analog, glargine is designed to precipitate in the subcutaneous tissue, forming a depot from which insulin is slowly released. This results in a more prolonged and flatter profile compared to NPH [80]. Its half-life is approximately 12-13.5 hours [81].
Insulin Detemir: This analog utilizes reversible albumin binding as its protraction mechanism, which buffers against variable absorption and contributes to a more predictable action profile. However, its half-life of 5-7 hours is suboptimal for once-daily dosing in many individuals, often necessitating twice-daily administration [81].
Insulin Degludec: Degludec represents the latest advancement in basal insulin technology. It forms multi-hexamer chains in the subcutaneous tissue that slowly and consistently dissociate into monomers for absorption. This unique mechanism confers an exceptionally long half-life exceeding 24 hours and a remarkably flat and stable PK/PD profile with low day-to-day variability (coefficient of variation of 21% vs. 83% for glargine U100) [81] [82].
The following diagram illustrates the core mechanism behind the stable action profile of modern long-acting analogs, using insulin degludec as a prime example.
Quantitative Efficacy and Safety Comparison
Clinical endpoints from randomized controlled trials and meta-analyses provide the most direct evidence for comparing these insulins. The data consistently demonstrates that while glycemic control (as measured by HbA1c) is generally equivalent across basal insulins, the key differentiator lies in the risk of hypoglycemia, particularly nocturnal events.
Table 1: Comparative Efficacy and Hypoglycemia Risk of Basal Insulins
| Insulin Type | Mechanism of Protraction | Approximate Half-Life | HbA1c Reduction vs. NPH | Nocturnal Hypoglycemia Risk vs. NPH | Key Supporting Evidence |
|---|---|---|---|---|---|
| NPH Insulin | Protamine crystal suspension | ~4.4 hours [81] | (Reference) | (Reference) | - |
| Insulin Glargine U100 | Post-injection precipitation | 12-13.5 hours [81] | Non-inferior [83] | >40% reduction in T2D [83] [80] | HOE 901/3002 Study Group [83] |
| Insulin Detemir | Reversible albumin binding | 5-7 hours [81] | Non-inferior [80] | 26-53% reduction [82] | Meta-analysis of RCTs [80] |
| Insulin Degludec | Multi-hexamer chain formation | >24 hours [82] | Non-inferior [84] [85] | Superior to Glargine/Detemir [84] [85] [82] | SWITCH 1, Meta-analysis 2022 [84] [85] [82] |
A 2022 systematic review and meta-analysis of 20 randomized controlled trials (n=19,048) provides a direct head-to-head comparison between the newer analogs. It found that while insulin degludec provided a similar HbA1c reduction to insulin glargine and detemir, it was associated with a significantly greater reduction in fasting plasma glucose (-0.370 mmol/L). Crucially, the estimated rate ratios of both overall and nocturnal hypoglycemia were significantly lower with degludec compared to glargine or detemir in patients with both type 1 and type 2 diabetes [84] [85].
Key Experimental Protocols and Methodologies
The evidence base for these comparisons relies on rigorous clinical trial designs. Understanding these methodologies is critical for interpreting the data.
Treat-to-Target (TTT) Trial Design
This design is a cornerstone for comparing basal insulins. A seminal TTT trial investigating insulin glargine versus NPH exemplifies this protocol [83].
- Objective: To compare the efficacy and safety of bedtime insulin glargine versus NPH in insulin-naïve patients with type 2 diabetes inadequately controlled on oral antidiabetic drugs (OADs).
- Population: 426 patients randomized to either glargine or NPH.
- Intervention: Both insulins were titrated to a fasting blood glucose (FBG) target of ≤6.7 mmol/L (120 mg/dL), following a strict algorithm. OADs were continued unchanged.
- Primary Endpoints: Change in HbA1c from baseline to 1 year, and the incidence of hypoglycemic events.
- Key Findings: After 1 year, HbA1c reduction was identical (8.3% vs. 8.2%), but the incidence of nocturnal hypoglycemia was less than half with glargine (9.9% vs. 24.0% of patients) [83].
Cross-Over Trials in High-Risk Populations
To test insulins in a more challenging setting, the HypoDeg trial employed a sophisticated cross-over design [82].
- Objective: To investigate if insulin degludec is superior to insulin glargine U100 in reducing nocturnal hypoglycemia in patients with type 1 diabetes and a history of recurrent severe nocturnal hypoglycemia.
- Design: A prospective, randomised, open, blinded endpoint (PROBE), two-year cross-over study.
- Population: Patients with at least one episode of nocturnal severe hypoglycemia (requiring third-party assistance) in the preceding two years.
- Intervention: Patients were randomized to degludec or glargine U100, each for 12 months, with a 3-month dose stabilization period followed by a 9-month endpoint assessment period.
- Endpoint: The primary endpoint was the rate of symptomatic nocturnal hypoglycemic episodes [82]. This design directly tests the hypothesis that degludec's stable profile confers a clinical benefit in the population most vulnerable to hypoglycemia.
Euglycemic Clamp Studies
The euglycemic glucose clamp is the gold standard for assessing the PK/PD properties of insulin [3]. This method was used, for instance, in a bioequivalence study of insulin lispro formulations [3].
- Principle: An intravenous insulin infusion is used to achieve a steady-state insulin level. Subsequently, a variable-rate glucose infusion is administered to maintain blood glucose at a constant target level (e.g., 5.0 mmol/L). The Glucose Infusion Rate (GIR) required to maintain euglycemia is a direct measure of the insulin's pharmacodynamic effect.
- Procedure: After subcutaneous injection of the test insulin, blood glucose is measured frequently (e.g., every 5-30 minutes) for 24 hours. The GIR is adjusted in real-time based on these measurements.
- Output: The procedure generates a GIR-time curve, from which key PD parameters like GIRmax (peak effect) and AUCGIR0–24h (total glucose-lowering effect) are derived [3]. Parallel blood sampling allows for the determination of PK parameters such as serum insulin concentration over time.
The workflow for this rigorous methodology is outlined below.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 2: Essential Materials for Insulin Pharmacokinetic/Pharmacodynamic Research
| Item | Function in Research |
|---|---|
| Long-Acting Insulin Analogs (Glargine U100/U300, Detemir, Degludec) | The primary investigational products for comparing efficacy, safety, and PK/PD profiles against comparators. |
| Comparator Insulins (NPH Insulin, other analogs) | Essential reference products for establishing relative performance in controlled trials. |
| Euglycemic Clamp System | The gold-standard apparatus for quantifying insulin pharmacodynamics by measuring the glucose infusion rate required to maintain stable blood glucose. |
| High-Performance Liquid Chromatography-Mass Spectrometry (HPLC-MS) | A highly sensitive and specific analytical technique for determining plasma concentrations of insulin analogs for pharmacokinetic analysis. |
| Continuous Glucose Monitoring (CGM) Systems | Provides high-resolution, ambulatory glycemic data, including detailed information on nocturnal glucose trends and hypoglycemic events. |
| ELISA Kits | Used for measuring biomarkers like C-peptide to assess endogenous insulin secretion, or for specific insulin assays. |
| Structured Self-Monitored Blood Glucose (SMBG) Diaries | Patient-reported data collection tools for capturing symptomatic hypoglycemia events and generating glucose profiles. |
The evolution from NPH insulin to long-acting analogs represents a significant advancement in diabetes therapeutics, driven by a deeper understanding of pharmacokinetics and pharmacodynamics. The evidence robustly demonstrates that insulin glargine and detemir offer a superior safety profile over NPH insulin, primarily through a significant reduction in the risk of nocturnal hypoglycemia, while maintaining equivalent glycemic control. The newest analog, insulin degludec, builds upon this foundation, with its ultra-long and flat action profile translating into a further statistically significant reduction in nocturnal hypoglycemia events compared even to other long-acting analogs. This progression highlights how innovations in molecular design aimed at optimizing PK/PD properties directly address one of the most pressing limitations of insulin therapy—nocturnal hypoglycemia—thereby enabling safer pursuit of optimal glycemic targets.
The development of once-weekly basal insulin analogues represents a paradigm shift in diabetes management, aiming to reduce treatment burden and improve adherence for patients requiring insulin therapy. Insulin icodec (Novo Nordisk) is a novel basal insulin analogue engineered for once-weekly subcutaneous administration through molecular modifications that enhance its binding to albumin, resulting in a significantly prolonged half-life appropriate for weekly dosing [86]. This innovation addresses a critical challenge in diabetes care, as psychological and practical barriers—including the burden of daily injections—often discourage timely insulin initiation and impair adherence [87] [86]. The pharmacokinetic (PK) and pharmacodynamic (PD) profile of icodec provides the scientific foundation for its weekly dosing schedule and informs its clinical application in both type 1 (T1D) and type 2 diabetes (T2D).
This analysis examines the pharmacological properties of once-weekly insulin icodec within the broader context of insulin analog research, with a specific focus on its head-to-head performance against established daily basal insulins. We present comprehensive PK/PD data, detailed methodological approaches for key experiments, and comparative efficacy and safety profiles to inform researchers, scientists, and drug development professionals about this promising therapeutic advancement.
Pharmacokinetic and Pharmacodynamic Properties
Fundamental PK/PD Characteristics
Insulin icodec's design incorporates strong albumin binding that creates a subcutaneous depot after administration, enabling slow and stable release into circulation. This mechanism results in a prolonged half-life that sustains therapeutic levels throughout the weekly dosing interval [88]. At steady state, icodec demonstrates predictable pharmacokinetics with stable concentration-time profiles.
Clinical trials in individuals with type 2 diabetes have established that icodec reaches steady-state concentrations within 3-4 weeks of initiation [87]. Model-predicted daily proportions of the glucose-lowering effect throughout the 7-day dosing interval at steady state are distributed as follows: day 1 (14.1%), day 2 (16.1%), day 3 (15.8%), day 4 (15.0%), day 5 (14.0%), day 6 (13.0%), and day 7 (12.0%) [87]. This balanced activity profile supports consistent basal glycemic control throughout the week with a single administration.
In type 1 diabetes populations, icodec reaches pharmacokinetic steady state more rapidly, within approximately 2-3 weeks [89]. The model-predicted daily contributions to glucose-lowering effect demonstrate a similar pattern: day 1 (14.3%), day 2 (19.6%), day 3 (18.3%), day 4 (15.7%), day 5 (13.1%), day 6 (10.6%), and day 7 (8.4%) [89]. The slightly more pronounced peak effect on days 2-3 in T1D warrants consideration in clinical management.
Table 1: Steady-State Pharmacodynamic Profile of Once-Weekly Insulin Icodec
| Day of Dosing Interval | Glucose-Lowering Effect in T2D (%) | Glucose-Lowering Effect in T1D (%) |
|---|---|---|
| Day 1 | 14.1 | 14.3 |
| Day 2 | 16.1 | 19.6 |
| Day 3 | 15.8 | 18.3 |
| Day 4 | 15.0 | 15.7 |
| Day 5 | 14.0 | 13.1 |
| Day 6 | 13.0 | 10.6 |
| Day 7 | 12.0 | 8.4 |
Injection Site Pharmacokinetics
A critical consideration for any subcutaneous insulin is the potential for injection site variability to influence pharmacological properties. A randomized, open-label, crossover trial specifically investigated whether the choice of injection region affects icodec exposure and glucose-lowering effect [88].
The study demonstrated that total icodec exposure (area under the curve from zero to infinity, AUC₀–∞) was similar between injections in the thigh, abdomen, and upper arm [88]. The maximum icodec concentration (Cₘₐₓ) after a single dose was higher for abdomen (by 17%) and upper arm (by 24%) compared to thigh injections, though these differences diminished at steady state (11% and 16% higher, respectively) [88]. Most importantly, the glucose-lowering effect profiles were comparable across injection regions, supporting flexible administration based on patient preference [88].
Comparative Clinical Performance
Efficacy Outcomes in Type 2 Diabetes
The ONWARDS clinical trial program has comprehensively evaluated insulin icodec against established daily basal insulins across diverse T2D populations. The collective evidence demonstrates that icodec provides glycemic control that is at least non-inferior to, and in some studies superior to, daily basal insulin analogs.
Table 2: Comparative Efficacy of Once-Weekly Icodec vs. Daily Basal Insulins in Type 2 Diabetes
| Trial | Duration (weeks) | Population | Comparator | HbA1c Reduction (%) | Hypoglycemia Rate (events/person-year) |
|---|---|---|---|---|---|
| ONWARDS 1 | 78 | Insulin-naïve | Glargine U100 | -1.55 (icodec) vs. -1.44 (glargine) [86] | Comparable at 52w, higher with icodec at 89w (ERR 1.63) [86] |
| ONWARDS 2 | 26 | Basal insulin-experienced | Degludec | -0.22% greater with icodec [86] | Similar (ERR 1.93) [86] |
| ONWARDS 3 | 26 | Insulin-naïve | Degludec | -0.2% greater with icodec [86] | Higher with icodec at week 26 (ERR 3.12) [86] |
| ONWARDS 5 | 52 | Insulin-naïve | Degludec/Glargine | -0.38% greater with icodec [86] | Similar (ERR 1.17) [86] |
In the ONWARDS 1 trial, icodec demonstrated superior HbA1c reduction compared to insulin glargine U100 at both 52 weeks (-0.19% difference) and 78 weeks (-0.11% difference) in insulin-naïve patients with T2D [86]. The ONWARDS 5 trial, which implemented a novel simplified dosing algorithm, showed particularly impressive results with icodec achieving a 0.38% greater HbA1c reduction than daily basal insulins at 52 weeks while maintaining similar rates of clinically significant hypoglycemia [86].
Efficacy and Safety in Type 1 Diabetes
The ONWARDS 6 trial specifically evaluated icodec in type 1 diabetes, where both efficacy and safety considerations are particularly important due to the absence of endogenous insulin production. At 26 weeks, icodec demonstrated similar HbA1c reduction to insulin degludec (estimated treatment difference: 0.05%) when both were combined with insulin aspart [86].
However, this comparable efficacy came with an important safety consideration: rates of level 2 or 3 hypoglycemia (plasma glucose <3.0 mmol/L) were significantly higher with icodec compared to degludec (estimated rate ratio 1.9) [89] [86]. This finding suggests that while icodec provides effective basal coverage in T1D, its pharmacokinetic profile may require more meticulous management to mitigate hypoglycemia risk in this population.
Experimental Methodologies for PK/PD Assessment
Glucose Clamp Techniques
The euglycemic glucose clamp remains the gold standard methodology for assessing the pharmacodynamic properties of insulin formulations [3]. This technique involves maintaining blood glucose at a constant target level through variable intravenous glucose infusion, with the glucose infusion rate (GIR) serving as the primary measure of insulin effect.
In icodec trials, clamps were typically conducted at specific timepoints after administration to characterize the time-action profile. For example, in one T2D study, the glucose-lowering effect was assessed at 0–36 h, 40–64 h, and 144–168 h post-dose, thus covering the initial, middle, and final portions of the weekly dosing interval [87]. During these procedures, participants remained in a supine or semi-supine position and received standardized meals before fasting prior to clamp initiation. Plasma glucose was maintained at target levels (typically 7.5 mmol/L [135 mg/dL] for T2D studies) through variable 20% glucose infusion, with the GIR recorded as the primary PD endpoint [87] [88].
Pharmacokinetic Sampling and Analysis
Frequent blood sampling protocols are essential for characterizing icodec's unique pharmacokinetic profile. In clinical trials, blood samples for icodec concentration measurement were typically collected pre-dose and at numerous timepoints extending up to 35 days after administration to adequately capture the complete concentration-time profile [89] [87] [88].
Total serum icodec concentrations (including both free and albumin-bound fractions) were measured using validated specific immunoassays. The analytical methods employed demonstrated appropriate sensitivity (analytical range from 500 to 80,000 pmol/L) and precision (inter-batch coefficient of variation ≤18.2%) to reliably quantify icodec levels throughout the dosing interval [88]. Population pharmacokinetic modeling approaches were then applied to simulate steady-state profiles following multiple once-weekly doses, typically using two-compartment models that account for icodec's unique distribution characteristics [88].
Research Reagent Solutions
The reliable assessment of insulin icodec's PK/PD properties depends on specialized research reagents and methodological approaches.
Table 3: Essential Research Reagents and Methodologies for Icodec PK/PD Studies
| Reagent/Methodology | Specification | Research Application |
|---|---|---|
| Icodec-Specific Immunoassay | Luminescence oxygen channelling immunoassay, range: 500-80,000 pmol/L [88] | Quantification of total serum icodec concentrations (free + albumin-bound) |
| Automated Glucose Clamp System | ClampArt system (Profil, Neuss, Germany) [88] | Precise maintenance of euglycemia during PD assessment |
| Intravenous Glucose Infusion | 20% glucose solution [88] | Variable infusion to maintain target blood glucose levels |
| Insulin Analogue Formulation | Icodec 700 U/mL in PDS290 prefilled pen-injector (Novo Nordisk) [88] | Standardized subcutaneous administration |
| HPLC-MS/MS System | High-performance liquid chromatography with triple quadrupole mass spectrometry [3] | Alternative method for insulin concentration measurement |
| C-peptide ELISA | Enzyme-linked immunosorbent assay [3] | Assessment of endogenous insulin secretion suppression |
Mechanism of Action and Physiological Rationale
Insulin icodec's prolonged action derives from strategic molecular modifications that enhance its binding to albumin in the subcutaneous space and circulation. After administration, icodec slowly diffuses into the bloodstream where it strongly binds albumin, creating a reversible circulating depot [88]. The slow dissociation from albumin and subsequent interaction with insulin receptors underlies its week-long activity.
This mechanism represents an evolution of basal insulin technology that builds upon the principles established by earlier long-acting analogs but extends the duration of action significantly. The stable receptor occupancy resulting from icodec's flat pharmacokinetic profile at steady state enables sustained glycemic control while potentially reducing within-day glucose variability compared to daily basal insulins.
Future Directions and Research Applications
The development of insulin icodec opens several promising research avenues in diabetes pharmacology. First, the combination of icodec with glucagon-like peptide-1 receptor agonists in fixed-ratio formulations (e.g., IcoSema) represents an innovative approach to addressing both fasting and postprandial glucose control with ultra-long-acting properties [86]. The COMBINE trial program has demonstrated that such combinations can produce superior HbA1c reductions compared to either agent alone, though not superior to basal-bolus regimens [86].
Additionally, the simplified titration algorithms developed for icodec, particularly the novel fixed-dose approach used in ONWARDS 5 with only four possible dose levels, represent a significant advancement in making insulin initiation and titration more accessible [86]. This approach has the potential to reduce clinical inertia and improve glycemic outcomes in real-world settings.
Future research should focus on long-term outcomes including cardiovascular safety, effects on microvascular complications, and real-world adherence patterns. Furthermore, exploration of icodec in special populations, including those with hepatic or renal impairment, will be essential to fully characterize its clinical utility across the diabetes spectrum.
Insulin icodec represents a significant innovation in basal insulin therapy, with a favorable PK/PD profile that enables effective once-weekly dosing. The pharmacological data demonstrate consistent glucose-lowering effects throughout the 7-day dosing interval, with comparable efficacy to daily basal insulins in type 2 diabetes and somewhat higher hypoglycemia risk in type 1 diabetes that requires careful management.
For the research community, icodec serves as a compelling example of how molecular engineering can extend insulin action while maintaining predictable pharmacokinetics. Its development has necessitated refined methodological approaches in PK/PD assessment, particularly in the application of glucose clamp techniques over extended durations and population pharmacokinetic modeling to characterize complex absorption and distribution patterns.
As once-weekly insulins progress toward clinical adoption, they offer the potential to transform diabetes management by reducing treatment burden and potentially improving adherence. However, ongoing research is needed to optimize their use in diverse patient populations and to fully understand their long-term benefits and risks in real-world practice.
The therapeutic management of diabetes mellitus relies heavily on the use of exogenous insulin formulations. While the primary goal of insulin therapy is metabolic control, long-term safety considerations extend beyond immediate glucoregulatory effects to include potential mitogenic properties. Mitogenic potency refers to the capacity of a compound to stimulate cell proliferation, a concern particularly relevant to insulin analogs due to their structural similarities to endogenous growth factors [90]. The insulin-like growth factor-1 receptor (IGF-1R) represents a key mediator of these effects, as it shares significant structural homology with the insulin receptor (IR) and regulates growth, differentiation, and survival pathways [91] [92].
The structural engineering of insulin analogs to optimize pharmacokinetic profiles has unintentionally created variants with altered binding affinities to IGF-1R, raising important clinical safety considerations [90] [22]. This comparative analysis examines the relationship between IGF-1R affinity and mitogenic potency across available insulin analogs, providing researchers and drug development professionals with experimental data and methodologies critical for safety assessment in the development of future insulin therapeutics.
IGF-1 Receptor Signaling and Mitogenic Pathways
Structural and Functional Basis of IGF-1R Signaling
The IGF-1 receptor is a transmembrane tyrosine kinase receptor composed of two extracellular α-subunits responsible for ligand binding and two transmembrane β-subunits containing the tyrosine kinase domain [92]. Upon ligand binding, the receptor undergoes autophosphorylation, initiating downstream signaling cascades primarily through the RAS-MAPK and PI3K-AKT pathways [91]. While the metabolic effects of insulin are predominantly mediated through the IR, mitogenic signaling can occur through multiple receptors, with IGF-1R representing the primary pathway for growth and proliferation signals.
The structural homology between IGF-1R and the insulin receptor (approximately 60% similarity) creates potential for cross-reactivity, particularly with modified insulin analogs [92]. This homology is most pronounced in the tyrosine kinase domains, presenting challenges for developing selective inhibitors and engineering insulin variants with reduced IGF-1R affinity [93].
Figure 1: IGF-1 Receptor Signaling Pathways. IGF-1 and certain insulin analogs can activate IGF-1R, triggering downstream signaling through RAS-MAPK and PI3K-AKT pathways that regulate cell proliferation and survival, in contrast to metabolic signaling primarily through the insulin receptor (IR).
Experimental Evidence Linking IGF-1R Signaling to Mitogenicity
The significance of IGF-1R signaling in cell proliferation is well-established through multiple experimental approaches. Genetic studies demonstrate that IGF-1R deletion in mice results in severe growth retardation and lethality during early embryonic development, underscoring its fundamental role in growth [92]. Conversely, IGF-1R overexpression has been documented in numerous malignancies, including breast, prostate, and lung cancers, where it contributes to tumor cell survival and resistance to apoptosis [92] [93].
Molecular studies have identified specific mechanisms through which IGF-1R activation promotes mitogenic effects. Sustained IGF-1R signaling leads to enhanced receptor internalization and prolonged activation of downstream effectors, particularly ERK1/2 in the MAPK pathway, resulting in increased DNA synthesis and cell cycle progression [90]. This signaling paradigm differs from metabolic signaling through the IR, which demonstrates more transient activation and rapid receptor recycling.
Comparative Analysis of Insulin Analogs
Structural Modifications and Receptor Binding Profiles
Insulin analogs are created through deliberate modifications of the human insulin sequence to alter pharmacokinetic properties. Rapid-acting analogs (lispro, aspart, glulisine) typically feature changes near the C-terminus of the B-chain that reduce hexamer formation, while long-acting analogs (glargine, detemir) incorporate modifications that prolong absorption from subcutaneous tissue [22]. These structural changes, while optimizing pharmacokinetics, can inadvertently affect receptor binding specificity.
The binding interface between insulin and IGF-1R involves specific domains critical for determining affinity. Recent research has identified that the IGF-1:p.Ile91 residue (mature peptide residue Ile43) is located at the binding interface of IGF-1–IGF-1R, with substitutions at this position significantly reducing binding stability and affinity [94] [95]. This finding provides a structural basis for understanding how analogous modifications in insulin analogs might influence IGF-1R binding.
Table 1: Structural Modifications and Receptor Binding Profiles of Insulin Analogs
| Insulin Analog | Structural Modifications | IR Binding Affinity (% of human insulin) | IGF-1R Binding Affinity (% of human insulin) | Reference |
|---|---|---|---|---|
| Human insulin | None | 100% | 100% | [22] |
| Insulin lispro | ProB28 → Lys, LysB29 → Pro | ~100% | ~100% | [22] |
| Insulin aspart | ProB28 → Asp | ~100% | ~100% | [22] |
| Insulin glulisine | AsnB3 → Lys, LysB29 → Glu | ~100% | ~100% | [22] |
| Insulin glargine | AsnA21 → Gly, ArgB31-32 | 88% (IR-B) | 480% | [90] |
| Insulin detemir | ThrB30 omitted, C14 FA to LysB29 | ~100% | Not reported | [22] |
| Insulin X10 | HisB10 → Asp | Increased | Significantly increased | [90] |
Quantitative Assessment of Mitogenic Potency
The mitogenic potency of insulin analogs correlates with their IGF-1R binding affinity and residence time. Analogs with increased receptor residence time, such as insulin X10, demonstrate prolonged receptor activation and internalization, leading to enhanced mitogenic signaling [90]. This relationship underscores the importance of dissociation kinetics in determining mitogenic responses alongside absolute binding affinity.
Recent innovations in insulin engineering have focused on creating analogs with reduced mitogenic potential without compromising metabolic activity. The introduction of a rigid dicarba bond between positions A6 and A11 creates a non-reducible C=C linkage that reduces IGF-1R-mediated mitogenic signaling while maintaining metabolic potency [90]. This structural approach demonstrates the potential for designing safer insulin analogs through strategic chemical modifications.
Table 2: Experimentally Determined Mitogenic Potencies and Related Properties
| Insulin Analog | Relative Mitogenic Potency | Cellular Proliferation Assay Results | Receptor Internalization Rate | Reference |
|---|---|---|---|---|
| Human insulin | 1.0 (reference) | Baseline | Baseline | [90] |
| Insulin glargine | Increased vs. human insulin | Enhanced proliferation in MCF-7 cells | Similar to human insulin | [90] |
| Insulin X10 | Significantly increased | Markedly enhanced proliferation | Significantly prolonged | [90] |
| cis-Dicarba insulin | Reduced | Reduced ERK phosphorylation | Reduced | [90] |
| cis-Dicarba glargine | Reduced vs. glargine | Attenuated proliferation response | Reduced | [90] |
Methodologies for Assessing Mitogenic Potential
Receptor Binding Assays
Competitive binding assays represent the fundamental methodology for determining receptor affinity profiles. The standard protocol involves:
Cell Line Preparation: Use engineered cell lines expressing human IR-A, IR-B, or IGF-1R to determine isoform-specific binding [90]. Common systems include fibroblasts overexpressing these receptors.
Radioligand Competition: Incubate cells with a fixed concentration of labeled insulin (e.g., ¹²⁵I-insulin) and increasing concentrations of unlabeled insulin analogs for equilibrium binding (typically 16-20 hours at 4°C) [90].
Data Analysis: Calculate IC₅₀ values from competition curves and determine relative binding affinities compared to human insulin. Results should be validated across multiple independent experiments with appropriate statistical analysis.
The experimental conditions significantly impact binding measurements, with pH, cation concentration, and incubation time requiring careful standardization. Recent advances utilize surface plasmon resonance to determine real-time binding kinetics, providing additional parameters such as association and dissociation rates that may better predict mitogenic potential [90].
Cell Proliferation and Signaling Assays
Functional assessment of mitogenic potency employs multiple complementary approaches:
Cellular Proliferation Assays: MCF-7 breast cancer cells are commonly used due to their sensitivity to IGF-1R-mediated proliferation. Cells are serum-starved and treated with insulin analogs for 48-72 hours, with proliferation measured via ³H-thymidine incorporation or colorimetric assays like MTT [90].
Receptor Phosphorylation and Internalization: Assess time-dependent receptor autophosphorylation via Western blotting with phospho-specific antibodies. Internalization rates are determined using fluorescence-labeled ligands and flow cytometry or confocal microscopy [90].
Downstream Signaling Activation: Monitor phosphorylation of key effectors in the MAPK pathway (ERK1/2) and PI3K pathway (AKT) at multiple time points to distinguish transient versus sustained activation patterns associated with mitogenic responses [90].
Figure 2: Experimental Workflow for Mitogenic Potential Assessment. Comprehensive evaluation requires multiple experimental phases progressing from receptor binding studies through functional assays, culminating in integrated data analysis for safety risk assessment.
Molecular Dynamics Simulations
Advanced computational approaches provide atomic-level insights into receptor-ligand interactions:
System Preparation: Construct full-length or extracellular domain models of IGF-1R based on crystallographic data (e.g., PDB IDs from structural studies) [94] [95].
Simulation Parameters: Perform extended all-atom molecular dynamics simulations (≥100 ns) in explicit solvent with physiological ion concentration using platforms like GROMACS or AMBER [94] [95].
Interaction Analysis: Calculate binding free energies using methods such as MM-PBSA/GBSA, identify critical residue interactions, and assess conformational stability through root-mean-square deviation and fluctuation analyses [94] [95].
These simulations have revealed that longevity-associated IGF-1 variants like IGF-1:p.Ile91Leu form less stable interactions with IGF-1R's critical binding pocket residues, particularly Phe731, resulting in reduced binding affinity [94] [95]. Similar principles apply to understanding the structural basis of insulin analog interactions with IGF-1R.
The Researcher's Toolkit: Essential Reagents and Methodologies
Table 3: Key Research Reagent Solutions for Mitogenicity Assessment
| Research Tool | Specific Example | Experimental Application | Technical Considerations |
|---|---|---|---|
| IGF-1R expressing cell lines | Engineered fibroblasts | Receptor binding and signaling studies | Requires verification of receptor density and functionality |
| Phospho-specific antibodies | Anti-phospho-IGF-1R (Tyr1135/1136) | Detection of receptor activation | Specificity validation essential through knockout controls |
| IR/IGF-1R inhibitors | AG1024, NVP-AEW541 | Specific pathway inhibition | Selectivity profiling required due to kinase domain homology |
| Recombinant insulin analogs | cis-Dicarba insulin analogs | Structure-function studies | Chemical stability and purity verification critical |
| Molecular dynamics software | GROMACS, AMBER | Simulation of receptor-ligand interactions | Computational resource intensive; requires validation |
| Biosensor systems | Surface plasmon resonance | Kinetic binding analysis | Immobilization strategy may affect binding properties |
Implications for Long-Term Safety and Therapeutic Development
The assessment of mitogenic potency extends beyond theoretical concerns to practical clinical implications. Epidemiological studies have identified associations between elevated IGF-1 levels and cancer risk, highlighting the importance of minimizing unnecessary IGF-1R activation [93]. Furthermore, IGF-1R signaling has been implicated in resistance to targeted therapies, including EGFR and HER2 inhibitors, creating additional considerations for patients requiring insulin therapy alongside oncology treatments [93].
The development of insulin analogs with reduced mitogenic potential represents an active area of pharmaceutical research. Approaches include:
- Biased agonists that selectively activate metabolic over mitogenic signaling pathways [90]
- Structural constraints such as dicarba bonds that limit receptor conformational changes associated with proliferative signaling [90]
- Albumin binding modifications that alter distribution and receptor access patterns [22]
Recent discoveries of natural IGF-1 variants associated with exceptional longevity provide additional templates for safer insulin analog design [94] [95]. These variants, including IGF-1:p.Ile91Leu and IGF-1:p.Ala118Thr, demonstrate naturally occurring mechanisms for attenuating IGF-1R signaling while maintaining essential metabolic functions.
The comparative analysis of insulin analog mitogenic potency reveals significant differences attributable to structural modifications and their consequent effects on IGF-1R binding affinity and signaling kinetics. The experimental methodologies reviewed provide a framework for systematic safety assessment during therapeutic development. As insulin therapy continues to evolve, the integration of structural biology, computational modeling, and functional signaling assays will enable the design of increasingly specific insulin analogs that maximize metabolic efficacy while minimizing potential mitogenic risks. The ongoing characterization of IGF-1R signaling pathways and their interplay with other growth factor systems remains essential for advancing the safety profile of insulin therapeutics.
Conclusion
The evolution of insulin analogs represents a convergence of protein engineering and clinical pharmacology, enabling regimens that more closely mimic physiologic secretion. Foundational molecular modifications have successfully produced analogs with optimized PK/PD profiles, which are rigorously characterized using advanced modeling and clamp methodologies. These innovations directly address critical challenges in diabetes management, notably by reducing hypoglycemia risk and intra-patient variability. The ongoing validation and comparison of new entities, including once-weekly basal insulins and ultra-stable single-chain analogs, highlight a trajectory toward unprecedented convenience and physiologic control. Future directions in insulin therapy will likely focus on further personalization through sophisticated PK/PD-informed dosing, the development of glucose-responsive 'smart' insulins, and a deeper understanding of the long-term clinical implications of analog-specific molecular properties, ultimately paving the way for more effective and safer diabetes treatments.
References
- 1. Pharmacokinetic and Pharmacodynamic Properties of ... [https://pubmed.ncbi.nlm.nih.gov/39928225]
- 2. A comparison of ultra-rapid and rapid insulin in automated ... [https://pubmed.ncbi.nlm.nih.gov/39996365/]
- 3. Pharmacokinetics and pharmacodynamics of insulin lispro ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1533548/full]
- 4. A phase I study using hyperinsulinaemic-euglycaemic clamp [https://pubmed.ncbi.nlm.nih.gov/40899618/]
- 5. Pharmacokinetics of the Rapid-Acting Insulin Analog ... [https://www.sciencedirect.com/science/article/abs/pii/S0090955624151227]
- 6. Comparing the Efficacy of Various Insulin Types [https://pubmed.ncbi.nlm.nih.gov/39982761/]
- 7. Insulin- Pharmacology, Therapeutic Regimens and ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK278938/]
- 8. Insulin Analogs: What Are the Clinical Implications of ... [https://www.uspharmacist.com/article/insulin-analogs-what-are-the-clinical-implications-of-structural-differences]
- 9. Emerging Insulin Analogues: A Glimpse into ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567236/]
- 10. Insulin Analogs: Impact on Treatment Success, Satisfaction ... [https://www.clinmedres.org/content/6/2/54]
- 11. Engineering protein-based therapeutics through structural ... [https://www.nature.com/articles/s41467-023-38039-x]
- 12. Pharmacokinetic/Pharmacodynamic Modeling of Efficacy ... [https://www.sciencedirect.com/science/article/pii/S1530891X24008371]
- 13. Self-association properties of monomeric insulin analogs ... [https://pubmed.ncbi.nlm.nih.gov/9755897/]
- 14. Application of SIMSTEX to Oligomerization of Insulin ... [https://www.sciencedirect.com/science/article/pii/S1044030506007136]
- 15. Development of insulin and its pharmacology ... [https://pubmed.ncbi.nlm.nih.gov/40480914/]
- 16. Emerging Insulin Analogues: A Glimpse into How ... [https://www.mdpi.com/1999-4923/17/10/1239]
- 17. Comparison of the effectiveness of fast-acting insulin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574399/]
- 18. Comparing the Efficacy of Various Insulin Types [https://www.semanticscholar.org/paper/Comparing-the-Efficacy-of-Various-Insulin-Types%3A-of-Chang-Jusko/e5e82c6c6f68e40faf9d518ff2d6e0308cefbb6d]
- 19. Structural principles of insulin formulation and analog design [https://pmc.ncbi.nlm.nih.gov/articles/PMC8513154/]
- 20. Insulin Analogs: Impact on Treatment Success, Satisfaction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2572551/]
- 21. Pharmacokinetics and pharmacodynamics of insulin analogs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3258012/]
- 22. A review of modern insulin analogue pharmacokinetic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3380549/]
- 23. Pharmacokinetics and pharmacodynamics of insulin lispro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11893401/]
- 24. Splitting the chains: ultra-basal insulin analog uncovers a ... [https://www.nature.com/articles/s41467-024-54006-6]
- 25. Enhanced disulphide bond stability contributes to the once ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11271312/]
- 26. Design of a novel long-acting insulin analogs by ... [https://www.nature.com/articles/s41598-025-94014-0]
- 27. Pharmacokinetic/Pharmacodynamic Modeling of Efficacy ... [https://pubmed.ncbi.nlm.nih.gov/39631663/]
- 28. Hyperinsulinemic-Euglycemic Clamp Technique [https://www.sciencedirect.com/topics/nursing-and-health-professions/hyperinsulinemic-euglycemic-clamp-technique]
- 29. Hyperinsulinemic euglycemic clamp at Profil [https://www.profil.com/services/hyperinsulinemic-euglycemic-clamp]
- 30. Impact of setting distinct target blood glucose levels on ... [https://pubmed.ncbi.nlm.nih.gov/39959272/]
- 31. A Comparative Clamp Study in Healthy Volunteers [https://pubmed.ncbi.nlm.nih.gov/39778084/]
- 32. How to improve the quality of euglycemic glucose clamp tests ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-025-08749-2]
- 33. Improved detection of decreased glucose handling ... [https://www.nature.com/articles/s43856-025-00819-5]
- 34. Tissue-specific and whole-body insulin sensitivity by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12331569/]
- 35. Pharmacokinetics, Pharmacodynamics, and ... [https://www.mdpi.com/1999-4923/17/4/418]
- 36. Mechanism-Based Pharmacodynamic Modeling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3684160/]
- 37. Application of Pharmacokinetic-Pharmacodynamic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2020.00997/full]
- 38. Development of insulin and its pharmacology ... [https://www.sciencedirect.com/science/article/pii/S000709122500296X]
- 39. Insulin Peak Times Explained [w/ Charts] [https://agamatrix.com/blog/insulin-peak-times/]
- 40. Types of Insulin Chart: Duration, Comparison, and More [https://www.healthline.com/health/type-2-diabetes/insulin-chart]
- 41. New 'smart insulin' shows promise in reducing low blood ... [https://medicine.iu.edu/news/2025/10/type-1-diabetes-fusion-protein]
- 42. [Ultra-fast acting insulin analogs: superiority in the ... [https://pubmed.ncbi.nlm.nih.gov/41235520/]
- 43. Top Type 1 Diabetes Research Breakthroughs to Watch in ... [https://www.type1strong.org/blog-post/top-type-1-diabetes-research-breakthroughs-to-watch-in-2025]
- 44. Physiologically Based Pharmacokinetic Modeling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541349/]
- 45. Prediction of pharmacokinetic/pharmacodynamic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1578117/full]
- 46. The pharmacokinetics and pharmacodynamics of rapid-acting insulin ... [https://pubmed.ncbi.nlm.nih.gov/22321739/]
- 47. Identification of PK - PD Models using Experimental GIR Insulin Data [https://orbit.dtu.dk/en/publications/identification-of-pk-pd-insulin-models-using-experimental-gir-dat]
- 48. Population pharmacokinetics/pharmacodynamics analysis ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1631034/full]
- 49. Pharmacokinetics, Pharmacodynamics, and Urinary ... [https://pubmed.ncbi.nlm.nih.gov/40658345/]
- 50. The effect of insulin analogs in people with type 1 diabetes ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2023.1301931/full]
- 51. Comparison of Pharmacokinetics and Pharmacodynamics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8891188/]
- 52. Hypoglycemia following the use of glucagon-like peptide-1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8506728/]
- 53. Glucagon-Like Peptide-1 Receptor Agonists - StatPearls - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK551568/]
- 54. Glucagon-like peptide-1 receptor: mechanisms and ... [https://www.nature.com/articles/s41392-024-01931-z]
- 55. Metformin pathways: pharmacokinetics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3651676/]
- 56. Population PK/PD analysis of metformin using the signal ... [https://pubmed.ncbi.nlm.nih.gov/22380769/]
- 57. Pharmacokinetic and Pharmacodynamic Variability of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5950987/]
- 58. Application of PK/PD Modeling and Simulation to Dosing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4764242/]
- 59. The Injection Technique Factor: What You Don't Know or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6640874/]
- 60. ultra-basal insulin analog uncovers a redox mechanism of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11555230/]
- 61. Enhanced disulphide bond stability contributes to the once- ... [https://www.nature.com/articles/s41467-024-50477-9]
- 62. Newer Insulin Preparations and Insulin Analogs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11676328/]
- 63. Effectiveness and Safety of Insulin Glargine 300 U/ml ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474787/]
- 64. The Effect of Various Degrees of Renal or Hepatic ... [https://link.springer.com/article/10.1007/s40262-024-01375-2]
- 65. Pharmacotherapy for Obesity: Recent Updates - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12456317/]
- 66. Emerging perspectives on once-weekly insulins in type 1 ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1656884/full]
- 67. Comparison of Prevailing Insulin Regimens at Different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9171166/]
- 68. Premixed insulin: Advantages, disadvantages, and future [https://pmc.ncbi.nlm.nih.gov/articles/PMC11885964/]
- 69. New weight loss drug, taken once weekly, leads to 20% ... [https://www.aol.com/articles/weight-loss-drug-taken-once-153600234.html]
- 70. Amylin could reign supreme in the next wave of obesity drugs [https://www.pharmavoice.com/news/amylin-obesit-weight-loss-drug-pharma-novo-lilly-roche/805713/]
- 71. Performance of an individualized, subcutaneous, basal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598994/]
- 72. Premix Insulin 2025-2033 Trends: Unveiling Growth ... [https://www.archivemarketresearch.com/reports/premix-insulin-144416]
- 73. Regulatory Considerations for Biosimilar Clinical Efficacy ... [https://www.drugpatentwatch.com/blog/regulatory-considerations-for-biosimilar-clinical-efficacy-trials/?srsltid=AfmBOoqj5wq2ApYWAwJAZj_C5LF1Ci5BntWpJoj6GDMcz1myfLcLlxTU]
- 74. FDA Draft Guidance for Industry on Statistical Approaches ... [https://www.gmp-compliance.org/gmp-news/fda-draft-guidance-for-industry-on-statistical-approaches-for-assessing-bioequivalence]
- 75. The Global Bioequivalence Harmonisation Initiative (GBHI) [https://www.sciencedirect.com/science/article/pii/S0928098725001289]
- 76. Regulatory Updates, September 2025 [https://www.caidya.com/resources/regulatory-updates-sept-2025/]
- 77. Similar pharmacokinetics and pharmacodynamics of a new ... [https://www.nature.com/articles/s41598-021-88782-8]
- 78. Comparison of pharmacokinetic properties ... [https://pubmed.ncbi.nlm.nih.gov/21134878/]
- 79. A single-center, randomized, double-blind, two-period, ... [https://www.sciencedirect.com/science/article/abs/pii/S0149291807001464]
- 80. Answering the Challenge With Long-acting Insulin Analogs [https://pmc.ncbi.nlm.nih.gov/articles/PMC1994862/]
- 81. Understanding the Clinical Profile of Insulin Degludec ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7547940/]
- 82. The effect of insulin degludec on risk of symptomatic nocturnal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6652000/]
- 83. Less nocturnal hypoglycemia and better post-dinner ... [https://pubmed.ncbi.nlm.nih.gov/10937510/]
- 84. Efficacy and Tolerability of Insulin Degludec Versus Other ... [https://pubmed.ncbi.nlm.nih.gov/36763996/]
- 85. Efficacy and Tolerability of Insulin Degludec Versus Other ... [https://www.sciencedirect.com/science/article/pii/S0149291822003447]
- 86. Emerging perspectives on once-weekly insulins in type 1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12420296/]
- 87. Pharmacokinetic and pharmacodynamic properties of once ... [https://pubmed.ncbi.nlm.nih.gov/37694740/]
- 88. Pharmacokinetic and Pharmacodynamic Characteristics of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9902323/]
- 89. Pharmacokinetic and pharmacodynamic properties of once ... [https://pubmed.ncbi.nlm.nih.gov/38379002/]
- 90. Minimizing Mitogenic Potency of Insulin Analogues Through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9271792/]
- 91. The IGF1 Signaling Pathway: From Basic Concepts to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10573540/]
- 92. Insulin-like growth factor 1 receptor [https://en.wikipedia.org/wiki/Insulin-like_growth_factor_1_receptor]
- 93. signaling of the insulin-like growth factor 1 receptor ... [https://www.nature.com/articles/ncponc0934]
- 94. Identification of functional rare coding variants in IGF-1 gene ... [https://pubmed.ncbi.nlm.nih.gov/40133344/]
- 95. Identification of functional rare coding variants in IGF-1 ... [https://www.nature.com/articles/s41598-025-94094-y]