High-Protein Diets for Glucose Control: Mechanisms, Efficacy, and Clinical Applications in Diabetes Management
This article systematically examines the efficacy of high-protein diets (HPDs) for glycemic control, addressing the needs of researchers and drug development professionals.
High-Protein Diets for Glucose Control: Mechanisms, Efficacy, and Clinical Applications in Diabetes Management
Abstract
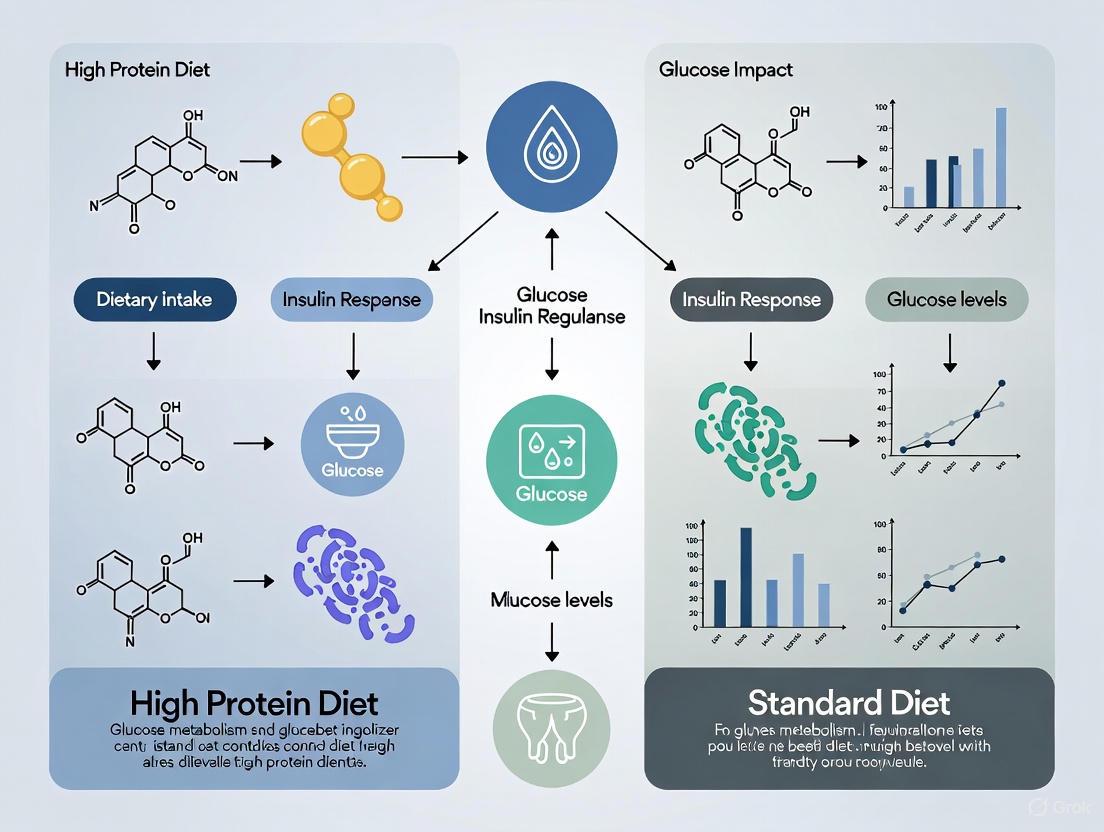
This article systematically examines the efficacy of high-protein diets (HPDs) for glycemic control, addressing the needs of researchers and drug development professionals. We explore the foundational physiological mechanisms by which dietary proteins and amino acids modulate insulin secretion and glucose homeostasis. The analysis covers methodological approaches for implementing HPDs in clinical settings and specialized nutritional formulations, including their effects on postprandial glucose, insulin resistance, and body composition. We troubleshoot implementation challenges, including variability in protein sources, long-term sustainability, and safety considerations. Finally, we provide comparative validation against other dietary interventions, such as low-carbohydrate diets, and discuss implications for future therapeutic development and personalized nutrition strategies for diabetes management.
Molecular Mechanisms: How Dietary Proteins Regulate Glucose Homeostasis and Insulin Signaling
Insulinotropic Effects of Amino Acids: Direct Pancreatic β-Cell Stimulation Pathways
The management of blood glucose is a central tenet of metabolic health, with pancreatic β-cell insulin secretion playing the pivotal role. While glucose is the primary stimulus for insulin release, the contribution of amino acids to this process is significant and complex. Understanding the direct pathways through which amino acids stimulate pancreatic β-cells is not only a matter of fundamental physiology but also critically informs the ongoing debate regarding the efficacy of high-protein diets (HPD) versus standard diets for glucose control. This review objectively compares the direct insulinotropic mechanisms of amino acids, framing them within the broader context of dietary protein research. We synthesize experimental data from key studies, detail the methodologies used to acquire them, and visualize the core signaling pathways, providing a resource for therapeutic development.
Mechanisms of Amino Acid-Stimulated Insulin Secretion (AASIS)
Amino acids stimulate insulin secretion through distinct and complementary mechanisms, primarily functioning as metabolic fuels to generate ATP or as signaling molecules that amplify secretion. The following pathway diagram synthesizes these core mechanisms, showing how different amino acids are sensed to ultimately trigger insulin exocytosis.
Diagram 1: Integrated pathways of amino acid-stimulated insulin secretion. The map shows three primary modes of action: the triggering pathway (blue) where amino acid oxidation elevates the ATP/ADP ratio; the signaling amplification pathway (green) where amino acids potentiate secretion; and the mTORC1 feedback pathway (red) that intrinsically limits excessive insulin release via actin remodeling.
The core mechanisms illustrated above are further elucidated by specific disease models, particularly congenital hyperinsulinism (HI), which provide powerful insights into the regulation of AASIS. The following table systematically compares the mechanisms and key experimental findings across three such models.
Table 1: Mechanisms of Amino Acid-Stimulated Insulin Secretion in Congenital Hyperinsulinism (HI) Models
| HI Model | Genetic Defect | Primary Mechanism of AASIS | Key Experimental Findings |
|---|---|---|---|
| GDH-HI [1] | Gain-of-function mutation in Glutamate Dehydrogenase (GDH) | Increased amino acid oxidation → ↑ ATP production → KATP channel closure and cell depolarization [1]. | Transgenic (H454Y) islets showed hypersensitivity to glutamine and leucine; increased GDH flux and ammonia production; EGCG inhibited GDH and blocked hypoglycemia [1]. |
| KATP-HI [1] | Loss-of-function in ATP-dependent K+ channel (KATP) | Constitutive membrane depolarization; amino acids provide amplifying signals independent of KATP closure [1]. | Insulin secretion is decoupled from metabolic regulation; amino acids directly augment calcium-triggered exocytosis [1]. |
| SCHAD-HI [1] | Short-chain 3-hydroxyacyl-CoA dehydrogenase deficiency | Loss of GDH inhibition → Increased GDH flux and amino acid oxidation, mimicking GDH-HI [1]. | SCHAD protein binds to and inhibits GDH; knockout mice showed increased GDH activity and leucine-stimulated insulin secretion [1]. |
Furthermore, the nutrient sensor mTORC1 has been identified as a critical intrinsic feedback regulator. Activated by glucose via the insulin secretion machinery, mTORC1 constrains insulin exocytosis, particularly the second phase, by promoting RhoA-dependent F-actin polymerization, which limits vesicle movement [2]. This mechanism prevents excessive insulin release and maintains metabolic balance.
Quantitative Data from Human and Animal Studies
The physiological mechanisms of AASIS translate into significant functional outcomes, which have been quantified in various experimental systems. The following table consolidates key quantitative findings from pivotal studies on amino acid and high-protein diet effects.
Table 2: Quantitative Summary of Amino Acid and High-Protein Diet Effects on Insulin Secretion and Metabolic Parameters
| Study System / Intervention | Key Metabolic Outcome | Quantified Change | Citation |
|---|---|---|---|
| GDH-TG Mouse Islets (AASIS) | Insulin secretion response to glutamine | Responsive to glutamine alone (control islets unresponsive) [1]. | [1] |
| GDH-TG Mouse Islets (AASIS) | GDH flux with [2-¹⁵N]glutamine | ~3-fold stimulation of flux vs. control [1]. | [1] |
| Obese Humans (T2D)52-week HP Diet | Weight Loss | -10.2 ± 1.6 kg (HP) vs -12.7 ± 4.8 kg (NP); p=0.336 [3]. | [3] |
| Obese Humans (T2D)52-week HP Diet | HbA1c, insulin, triglycerides | Significant improvement with weight loss, no difference between HP and NP diets [3]. | [3] |
| Obese Prediabetic Humans6-month HP Diet | Remission of prediabetes | 100% remission in HP group (0% in HC group) [4]. | [4] |
| Obese Prediabetic Humans6-month HP Diet | GLP-1 and GIP response | Greater increase in GLP-1 and GIP with HP vs HC diet [4]. | [4] |
| Obese Women (No Diabetes)6-month HP Diet | Insulin sensitivity and β-cell function | Insulin sensitivity: +4 vs +0.9 (HC); β-cell function: +7.4 vs +2.1 (HC) [5]. | [5] |
| Humans with T2D5-week HP Diet | 24-hour integrated glucose area | 40% decrease with HP diet vs control diet [6]. | [6] |
| Humans with T2D5-week HP Diet | Glycated hemoglobin (HbA1c) | Decreased 0.8% (HP) vs 0.3% (control); p < 0.05 [6]. | [6] |
Detailed Experimental Protocols for Key AASIS Models
To enable replication and critical evaluation, this section outlines the core methodologies used in the studies cited to investigate AASIS.
- Objective: To measure real-time, dynamic insulin secretion from isolated pancreatic islets in response to specific amino acid challenges.
- Procedure:
- Islet Isolation: Pancreatic islets are isolated from model animals (e.g., wild-type or transgenic mice) via collagenase digestion and density gradient centrifugation.
- Perifusion System: A batch of size-matched islets is loaded into a chamber maintained at 37°C.
- Buffer Perifusion: A basal buffer (e.g., containing 2.8 mM glucose) is continuously perfused through the chamber to establish a stable baseline.
- Stimulus Application: The perfusate is switched to a test buffer containing a specific amino acid (e.g., 10 mM glutamine, a leucine mixture) or a combination of nutrients.
- Sample Collection: Effluent from the chamber is collected at frequent intervals (e.g., every 2-5 minutes) into tubes.
- Insulin Assay: The insulin concentration in each collected fraction is quantified by radioimmunoassay (RIA) or enzyme-linked immunosorbent assay (ELISA).
- Key Measurements: The insulin secretion rate over time, allowing for the distinction between first-phase and second-phase secretion in response to the stimulus.
- Objective: To quantitatively measure the flux of amino acids through specific metabolic pathways, such as the GDH reaction, in isolated islets.
- Procedure:
- Islet Incubation: Isolated islets are incubated in media containing a stable isotope-labeled substrate (e.g., [2-¹⁵N]glutamine).
- Metabolite Extraction: At designated time points, islets are rapidly harvested and metabolites are extracted.
- Metabolomic Analysis: The extracts are analyzed using techniques like gas chromatography/mass spectrometry (GC-MS).
- Flux Calculation: The transfer of the ¹⁵N label from [2-¹⁵N]glutamine to [2-¹⁵N]glutamate and subsequently to [¹⁵N]ammonia is tracked. The specific flux via the GDH reaction is calculated based on the enrichment of the products.
- Key Measurements: Metabolic flux rates (e.g., GDH flux), production of specific metabolites (e.g., ammonia, α-ketoglutarate), and the ATP/ADP ratio.
- Objective: To compare the long-term effects of a high-protein (HP) diet versus a high-carbohydrate (HC) or normal-protein (NP) diet on weight loss, body composition, and glucose control in human subjects.
- Protocol:
- Participant Recruitment: Enrollment of adults with obesity, often with prediabetes or type 2 diabetes, who are weight-stable.
- Randomization: Participants are randomly assigned to either the HP or control diet group.
- Dietary Intervention: The intervention period typically lasts from 6 months to 1 year.
- HP Diet: ~25-30% protein, ~30% fat, ~40% carbohydrate.
- Control Diet: ~15-21% protein, ~30% fat, ~53-55% carbohydrate.
- Both diets are energy-restricted (e.g., -500 kcal/day).
- Outcome Measurements:
- Anthropometrics: Body weight, BMI, body composition (via DXA scan).
- Glycemic Control: Fasting glucose and insulin, HbA1c, Oral Glucose Tolerance Test (OGTT).
- Hormonal Response: Plasma levels of insulin, C-peptide, GLP-1, GIP, ghrelin.
- Cardiometabolic Markers: Lipid profile, blood pressure, oxidative stress markers.
- Key Measurements: Changes from baseline to endpoint within and between diet groups for all outcome variables.
The Scientist's Toolkit: Essential Research Reagents
Research into AASIS relies on a specific set of reagents, inhibitors, and model systems. The following table details key tools used in the featured experiments.
Table 3: Essential Research Reagents for Investigating Amino Acid-Stimulated Insulin Secretion
| Reagent / Model | Function/Description | Experimental Application |
|---|---|---|
| Epigallocatechin Gallate (EGCG) | Natural polyphenol that inhibits GDH by binding to its ADP-activation site [1]. | Used to probe GDH function; shown to block glutamine-stimulated insulin secretion in GDH-HI islets and prevent amino acid-induced hypoglycemia in vivo [1]. |
| GDH-HI Transgenic Mouse | Animal model expressing a gain-of-function mutation (e.g., H454Y) in the GDH enzyme under an insulin promoter [1]. | Used to study the mechanisms of protein-sensitive hypoglycemia and test potential therapeutics like EGCG [1]. |
| Diazoxide | KATP channel agonist that keeps the channel open, preventing membrane depolarization. | Used to dissect KATP-dependent and -independent pathways of insulin secretion [1]. |
| Stable Isotope-Labeled Amino Acids (e.g., [2-¹⁵N]Glutamine) | Amino acids with heavy isotopes (e.g., ¹⁵N) incorporated, allowing tracking of metabolic fate. | Essential for using GC-MS to quantify metabolic flux through specific pathways like the GDH reaction [1]. |
| Rapamycin | Specific allosteric inhibitor of the mTORC1 complex. | Used to investigate the role of mTORC1 in the feedback regulation of insulin secretion [2]. |
| Perifusion System | An ex vivo setup that allows continuous, real-time monitoring of hormone secretion from cultured tissues. | Superior to static incubation for characterizing the dynamic kinetics (phasic release) of insulin secretion from isolated islets [1]. |
The direct stimulation of pancreatic β-cells by amino acids is a multifaceted process involving distinct triggering and amplifying pathways, elegantly revealed by disease models like GDH-HI and SCHAD-HI. The intrinsic feedback mechanism mediated by mTORC1 further adds a layer of sophistication, ensuring that insulin release is precisely calibrated [2] [1]. When these molecular insights are viewed in the context of clinical dietary studies, a nuanced picture emerges. While the weight loss achieved through caloric restriction remains the dominant factor for improving glucose control [3], high-protein diets exert significant direct effects on β-cell function and incretin response [5] [4]. The choice between dietary regimens should, therefore, be informed by a deep understanding of these underlying insulinotropic pathways, which continue to offer valuable targets for future diabetes therapeutics and personalized nutrition strategies.
{Abstract} The mediobasal hypothalamus (MBH) serves as a critical nutrient-sensing center for systemic metabolic regulation. Emerging research demonstrates that the metabolism of the branched-chain amino acid leucine within the MBH is a previously unrecognized mechanism that couples central nutrient sensing with the control of hepatic glucose production (HGP). This neural circuit is essential for maintaining glucose homeostasis and its dysregulation may contribute to hyperglycemia. This guide compares the efficacy of this specific signaling pathway against other dietary and central regulatory mechanisms, providing a focused analysis for the development of therapeutic strategies targeting brain-liver communication.
{1 Introduction} The central nervous system, particularly the hypothalamus, plays a pivotal role in regulating peripheral glucose metabolism. While the arcuate nucleus (ARC) of the MBH is known to integrate hormonal signals like insulin and leptin to influence energy and glucose homeostasis, its role as a sensor for specific nutrients, such as amino acids, has been elucidated more recently. The discovery that hypothalamic leucine metabolism can directly regulate HGP provides a novel axis for understanding how high-protein diets might influence glucose control. This guide details the experimental evidence for this pathway, juxtaposes it with other regulatory mechanisms, and provides the methodological toolkit required for its investigation.
{2 The Hypothalamic Leucine-Sensing Pathway: Mechanism and Key Experiments}
{2.1 Core Signaling Pathway} Central leucine sensing is a multi-step process initiated in the MBH. Leucine is first transaminated to α-ketoisocaproic acid (KIC) by the enzyme branched-chain amino acid aminotransferase (BCAT). KIC is then metabolized via branched-chain ketoacid dehydrogenase (BCKDH). This biochemical network is notably insensitive to rapamycin, indicating independence from the mammalian target of rapamycin (mTOR) pathway, and is also independent of acetyl- and malonyl-CoA. The signaling cascade ultimately requires functional ATP-sensitive K+ (KATP) channels to transmit the signal that suppresses HGP [7] [8].
The diagram below illustrates this specific signaling pathway from hypothalamic leucine sensing to the suppression of liver glucose production.
{2.2 Key Experimental Evidence} The foundational evidence for this pathway comes from a series of sophisticated clamp studies in rodent models. The key findings from these experiments are summarized in the table below.
| Experimental Intervention | Key Outcome on Blood Glucose / HGP | Interpretation & Mechanistic Insight |
|---|---|---|
| Central (MBH) Leucine Infusion [7] | Lowered blood glucose; Suppressed HGP [7] | The MBH is a direct site of leucine sensing for glucose regulation. |
| Central KIC Infusion [7] | Lowered blood glucose [7] | Leucine must be metabolized to KIC to exert its effect. |
| BCAT Inhibitor (Aminooxyacetic acid) [7] | Blocked leucine-induced suppression of HGP [7] | Confirms the necessity of the first metabolic step (leucine to KIC). |
| BCKDH Kinase (BCKDK) Overexpression [7] | Attenuated leucine-induced suppression of HGP; Caused hyperglycemia after a meal [7] | Inhibiting KIC metabolism disrupts the pathway and impairs glucose homeostasis. |
| KATP Channel Blockade | Blocked leucine-induced suppression of HGP [7] | KATP channel activity is a mandatory final step in the signal transduction. |
| MCD Overexpression (blocks malonyl-CoA accumulation) | Did not block leucine-induced suppression of HGP [7] | The pathway is independent of malonyl-CoA sensing. |
| Rapamycin Co-infusion (blocks mTOR) | Did not block leucine-induced suppression of HGP [7] | The pathway is independent of the mTOR signaling cascade. |
{2.3 Detailed Experimental Protocol} To investigate this pathway, researchers employ a combination of stereotaxic surgery, central infusions, and pancreatic-euglycemic clamp techniques.
- Animal Models and Surgery: Studies are performed in male Sprague-Dawley rats (10-12 weeks old) or mice (e.g., SUR1-null models). Animals undergo stereotaxic surgery for the implantation of a chronic cannula directed into the third cerebral ventricle (ICV) or bilaterally into the MBH. Correct placement is verified post-mortem [7].
- Central Infusions: After recovery, fasted animals receive continuous ICV or MBH infusions of test compounds. These include:
- Leucine: The primary amino acid of interest.
- KIC: The first metabolite of leucine.
- Inhibitors: Such as aminooxyacetic acid (BCAT inhibitor), α-chloroisocaproate (BCKDH inhibitor), or KATP channel blockers like glibenclamide.
- Control: Artificial cerebrospinal fluid (aCSF) is used as a vehicle control [7].
- Pancreatic-Euglycemic Clamp: During the central infusion, a basal pancreatic clamp is initiated. This technique involves the infusion of somatostatin to suppress endogenous insulin and glucagon secretion, while insulin is replaced at a basal rate to maintain fasting levels. This creates a steady hormonal background, allowing researchers to isolate the effect of the central intervention on HGP without the confounding effects of variable peripheral hormone levels. Glucose production is traced with [3-³H]glucose [7].
- Molecular Interventions: To establish causality, genetic tools are used. Adeno-associated virus (AAV) vectors are injected into the MBH to overexpress genes of interest (e.g., BCKDK to inhibit BCKDH) or control proteins (e.g., GFP) [7].
The workflow of a typical experiment integrating these components is visualized below.
{3 Comparative Efficacy: Central Leucine vs. Other Regulatory Systems}
{3.1 Comparison with Other Central Nutrient-Sensing Pathways} The hypothalamic leucine-sensing pathway operates distinctly from other well-characterized central nutrient-sensing mechanisms. The following table provides a detailed comparison.
| Regulatory Pathway / Signal | Key Molecular Components | Primary Metabolic Outcome | Distinction from Leucine Pathway |
|---|---|---|---|
| Hypothalamic Leucine | BCAT, BCKDH, KATP channels | Suppresses HGP [7] [8] | Unique reliance on BCAA catabolism; mTOR-independent; malonyl-CoA-independent. |
| Central Insulin [9] | Insulin receptor, IRS/PI3K, KATP channels | Suppresses HGP (reduces gluconeogenesis & glycogenolysis) [9] | Signals energy sufficiency; acts primarily via inhibition of AgRP neurons; impaired in insulin resistance. |
| Central Leptin [9] | Leptin receptor, JAK/STAT, Melanocortin system | Modulates HGP (decreases glycogenolysis, increases gluconeogenesis) [9] | Signals adiposity; complex effects on hepatic glucose fluxes; involves POMC neurons. |
| Central Fatty Acids | Malonyl-CoA, CPT-1, KATP channels | Suppresses HGP [9] | Relies on de novo lipid synthesis and malonyl-CoA accumulation, a step bypassed by leucine signaling [7]. |
{3.2 Comparison with Peripheral Diets and Interventions} Placing the central leucine mechanism in the context of whole-diet interventions reveals a complex picture of how protein intake might influence glucose control.
| Dietary / Intervention Strategy | Reported Impact on Glucose Control | Potential Link to Central Leucine Signaling |
|---|---|---|
| High-Protein (HP) Diet [10] [11] | Improves HbA1c, fasting glucose, and insulin resistance; effects often tied to weight loss [10] [11]. | Increased dietary protein elevates plasma BCAAs, potentially enhancing central leucine sensing and contributing to HGP suppression. |
| Normal-Protein (NP) Diet [10] | Also improves glucose control when it results in equivalent weight loss [10]. | Suggests that achieved weight loss is a dominant factor, and the specific leucine mechanism may be one of several beneficial mediators. |
| Low-Carbohydrate Diets (e.g., LoBAG) [11] [12] | Significant reduction in HbA1c and 24-h glucose profiles [11] [12]. | These diets are often high in protein, suggesting a potential synergistic effect between low glucose availability and enhanced central leucine signaling. |
| Intermittent Leucine-Deprivation [13] | Shown to intervene in type 2 diabetes in db/db mice [13]. | Provides a contrasting approach, suggesting that modulating rather than increasing leucine levels can be therapeutic, highlighting the pathway's complexity. |
{4 The Scientist's Toolkit: Essential Research Reagents} To experimentally probe the hypothalamic leucine-sensing pathway, the following reagents and tools are essential.
| Research Reagent / Tool | Function / Purpose in Research |
|---|---|
| Stereotaxic Apparatus | Precise surgical implantation of guide cannulae into the MBH or third ventricle for central infusions. |
| Chronic Indwelling Cannulae (ICV/MBH) | Allows for repeated or continuous delivery of compounds directly to the brain region of interest. |
| Aminooxyacetic Acid (AOAA) | A pharmacological inhibitor of BCAT; used to block the first step of leucine metabolism and validate its necessity [7]. |
| α-Chloroisocaproate (α-CIC) | A pharmacological inhibitor of BCKDH; used to block the metabolism of KIC [7]. |
| KATP Channel Modulators (e.g., Glibenclamide, Diazoxide) | To open or block KATP channels and test their requirement in the signaling cascade [7]. |
| Pancreatic-Euglycemic Clamp Setup | The gold-standard method for in vivo assessment of HGP and peripheral tissue insulin sensitivity under controlled conditions. |
| AAV Vectors (e.g., AAV-BCKDK, AAV-MCD) | For targeted genetic manipulation (overexpression or knockdown) of specific pathway components within the MBH [7]. |
| [3-³H]Glucose Tracer | Enables the precise measurement of the rate of HGP during clamp studies via isotope dilution. |
{5 Discussion and Research Implications} The elucidation of the hypothalamic leucine-sensing pathway represents a significant advance in understanding brain-liver communication. Its independence from the mTOR and malonyl-CoA pathways suggests a previously unknown biochemical network within the MBH that is dedicated to amino acid sensing. From a therapeutic perspective, this pathway offers a promising target for drug development aimed at restoring central nutrient sensing in conditions like type 2 diabetes. However, the human translatability requires careful consideration, as chronic elevation of plasma BCAAs is also epidemiologically associated with insulin resistance. This paradox may be explained by potential "leucine resistance" in the hypothalamus under obese conditions or by opposing, potentially detrimental, effects of chronic high leucine on the liver, such as promoting triglyceride accumulation via a myostatin-AMPK pathway [14]. Therefore, therapeutic strategies would need to precisely target the central pathway without causing systemic or hepatic side effects. Future research should focus on identifying the exact molecular sensors downstream of KIC metabolism and the detailed neurocircuitry that relays the signal from the MBH to the liver.
Incretin hormones, primarily glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP), play a pivotal role in metabolic homeostasis by amplifying glucose-stimulated insulin secretion following nutrient ingestion [15]. This physiological phenomenon, known as the incretin effect, accounts for 50-70% of postprandial insulin responses in healthy individuals [15]. While carbohydrates represent the classical stimulus for incretin release, emerging evidence demonstrates that protein digestion serves as a potent secretagogue for both GLP-1 and GIP, though with distinct activation patterns [16] [17]. Understanding these protein-mediated pathways provides crucial insights for developing nutritional strategies and pharmacological interventions for metabolic disorders, particularly in the context of comparing high-protein diets against standard diets for glucose control. This review systematically compares the mechanisms and efficacy of protein-induced GLP-1 and GIP secretion, integrating recent experimental findings to elucidate their differential activation patterns and therapeutic implications.
Physiological Fundamentals of Incretin Hormones
GLP-1 and GIP: Origin and Core Functions
GLP-1 and GIP are peptide hormones secreted by enteroendocrine cells in response to nutrient ingestion. GIP is primarily produced by K cells located in the upper portion of the gastrointestinal tract (duodenum and jejunum), while GLP-1 is secreted by L cells concentrated in the distal gut (ileum and colon) [15]. Both hormones function as incretins, potentiating glucose-dependent insulin secretion from pancreatic β-cells, but exhibit complementary physiological roles: GLP-1 suppresses glucagon secretion and delays gastric emptying, whereas GIP exerts glucagonotropic effects during hypoglycemia [15]. Beyond their insulinotropic effects, both hormones influence central appetite regulation, with GLP-1 demonstrating particularly potent satiety-promoting properties [15] [18].
Receptor Signaling and Metabolic Integration
GLP-1 and GIP initiate signaling cascades by binding to specific class B G protein-coupled receptors (GPCRs) – GLP-1R and GIPR, respectively [15] [19]. These receptors exhibit distinct tissue distribution patterns: GIPR is expressed in pancreatic islets, brain, and adipocytes, while GLP-1R is found in pancreas, brain, and gastrointestinal tract [15]. Despite shared signaling pathways such as adenylate cyclase/cAMP activation, they engage distinct downstream effectors; in murine pancreatic β-cells, GLP-1 activates both Gαs and Gαq proteins, whereas GIP selectively activates Gαs [15]. This differential signaling contributes to their unique metabolic profiles and therapeutic applications.
Comparative Analysis: Protein-Induced GLP-1 vs. GIP Secretion
Quantitative Secretion Patterns
Recent human investigations directly comparing incretin responses to isolated protein versus carbohydrate ingestion reveal distinct secretion dynamics. A 2025 cross-over study examining isocaloric whey protein-only (1.2 g·kg⁻¹) and carbohydrate-only drinks demonstrated that protein stimulates significantly greater GLP-1 release, while carbohydrates elicit a more pronounced GIP response [16]. The temporal secretion patterns also differ, with protein-induced GLP-1 remaining elevated for extended periods (>240 minutes) compared to the more transient GIP response to carbohydrates [16].
Table 1: Comparative Hormonal Responses to Protein vs. Carbohydrate Ingestion
| Parameter | Whey Protein (1.2 g·kg⁻¹) | Carbohydrate | Statistical Significance |
|---|---|---|---|
| GLP-1 response | Significantly increased | Moderate increase | p < 0.001 (PRO > CHO) |
| GIP response | Moderate increase | Significantly increased | p < 0.001 (CHO > PRO) |
| Insulin response | Moderate increase | Significantly increased | p < 0.001 (CHO > PRO) |
| Response duration | GLP-1 remains elevated >240min | Transient response | Not specified |
Table 2: Nutrient Composition and Experimental Conditions
| Factor | Whey Protein Condition | Carbohydrate Condition |
|---|---|---|
| Energy content | Isoenergetic | Isoenergetic |
| Macronutrient | 1.2 g·kg⁻¹ whey protein | Matched carbohydrate quantity |
| Study population | 14 healthy, moderate-to-well-trained participants | Same participants |
| Design | Randomized, balanced cross-over | Randomized, balanced cross-over |
Synergistic Effects of Protein with Other Nutrients
The combination of protein with specific micronutrients potently enhances GLP-1 secretion. Emerging evidence indicates that co-ingestion of protein and calcium generates synergistic effects on GLP-1 release, potentially mediated by calcium-sensing receptors on intestinal L-cells [17]. This synergy produces some of the highest reported physiological concentrations of GLP-1 following nutrient ingestion, suggesting strategic nutrient combinations could optimize endogenous incretin secretion for metabolic benefits [17].
Experimental Models and Methodologies
Human Intervention Protocols
The standard methodology for investigating protein-induced incretin secretion involves randomized, balanced cross-over designs with isocaloric nutrient challenges [16]. Participants typically report after an overnight fast, with intravenous catheters inserted for serial blood collection. Test beverages include protein-only (e.g., whey isolate) and carbohydrate-only formulations, administered in randomized order on separate days. Blood samples are collected at fasting baseline and at regular intervals post-ingestion (e.g., every 30-60 minutes for 4+ hours) for hormone and metabolite analyses [16]. This protocol enables direct within-subject comparison of hormonal responses while controlling for potential confounding factors.
Analytical Techniques and Assessments
Plasma GLP-1 and GIP concentrations are quantified via specific immunoassays that distinguish active forms (GLP-1₇–₃₆ amide and GIP₁–₄₂) from inactive metabolites [16] [17]. Simultaneous measurement of glucose, amino acids, insulin, and glucagon provides comprehensive metabolic profiling. For protein metabolism studies, urinary nitrogen excretion serves as an indicator of protein degradation and amino acid oxidation, with collections typically performed in consecutive batches over 24 hours to assess temporal patterns [16].
Diagram 1: Protein-mediated Incretin Secretion Pathway. This diagram illustrates the sequential process from protein ingestion to amino acid absorption, stimulation of intestinal endocrine cells, hormone secretion, receptor binding, and ultimately potentiation of glucose-dependent insulin secretion.
Research Reagents and Methodological Toolkit
Table 3: Essential Research Reagents for Investigating Protein-Incretin Axis
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Protein Sources | Whey isolate, casein, plant proteins | Standardized protein challenges for incretin response studies |
| Hormone Assays | GLP-1₇–₃₆ amide ELISA, GIP₁–₄₂ RIA | Quantification of active incretin forms in plasma samples |
| Metabolic Analyzers | Glucose analyzers, amino acid profilers | Concurrent metabolic parameter assessment |
| Receptor Agonists/Antagonists | Exendin-4 (GLP-1R agonist), GIPR antibodies | Mechanistic studies of receptor-specific contributions |
| Cell Models | STC-1, GLUTag, primary intestinal cultures | In vitro screening of secretagogue potential |
Therapeutic Implications and Research Translation
Nutritional Strategies for Incretin Modulation
Strategic dietary approaches can optimize endogenous incretin secretion for metabolic benefits. Evidence-based nutritional interventions include: (1) prioritizing dietary protein from diverse sources (lean meats, fish, eggs, legumes), (2) combining protein with fiber-rich foods to enhance GLP-1 secretion, (3) incorporating healthy fats (olive oil, avocados, nuts) that augment GLP-1 release, and (4) practicing meal sequencing (consuming protein and vegetables before carbohydrates) to potentiate postprandial incretin responses [20]. These approaches provide widely accessible, cost-effective alternatives to pharmacological interventions for enhancing hormone release [17].
Pharmacological Applications and Drug Development
Understanding protein-mediated incretin secretion informs the development of next-generation therapeutics. The differential secretion patterns of GLP-1 and GIP following protein ingestion have inspired novel dual receptor agonists (e.g., tirzepatide) that simultaneously engage both GLP-1R and GIPR, demonstrating superior efficacy for weight loss and glycemic control compared to selective GLP-1 receptor agonists [18] [21]. Interestingly, both GIPR activation and blockade can enhance the weight-reducing effects of GLP-1R agonism, suggesting complex receptor-specific mechanisms that can be therapeutically exploited [21].
Diagram 2: Research Translation from Basic Science to Therapeutics. This diagram outlines the pathway from fundamental discoveries about protein-induced incretin secretion to the development of pharmacological interventions that harness these mechanisms for metabolic disease treatment.
Protein digestion activates distinct incretin-mediated pathways, with preferential stimulation of GLP-1 over GIP secretion. This differential activation pattern, coupled with the synergistic effects of protein combined with specific micronutrients like calcium, provides a scientific foundation for nutritional strategies targeting endogenous incretin enhancement. The mechanistic insights from protein-incretin research continue to drive innovation in therapeutic development, particularly in the design of multi-receptor agonists that mimic the coordinated hormone secretion observed with nutrient ingestion. Future research should focus on optimizing protein sources, quantities, and timing to maximize metabolic benefits, while exploring individual variability in response to protein-mediated incretin secretion for personalized nutrition approaches to glucose control.
Intestinal glucose absorption is a critical process for maintaining systemic energy balance, primarily mediated by the specialized transporters Sodium-Glucose Cotransporter 1 (SGLT1) and Glucose Transporter 2 (GLUT2). Understanding the modulation of these transporters is essential for developing new strategies to manage hyperglycemia, a hallmark of metabolic diseases. This guide provides a comparative analysis of how different interventions—specifically high-protein diets and pharmaceutical agents—affect these transporters and overall glycemic control. Framed within broader research on the efficacy of high-protein versus standard diets, this review synthesizes current experimental data to inform researchers, scientists, and drug development professionals about the mechanisms and potential applications of these modulatory approaches.
Transporter Mechanisms and Modulation Pathways
Glucose absorption in the small intestine involves coordinated actions of specific transporters. At low luminal glucose concentrations (typically <30 mM), SGLT1 on the apical membrane of enterocytes mediates active glucose uptake via a sodium-coupled mechanism [22]. Once inside the cell, glucose exits through the basolateral membrane into circulation via GLUT2, which facilitates passive diffusion [22]. At high luminal glucose concentrations, additional mechanisms may contribute, including paracellular transport and potential apical insertion of GLUT2 [22] [23].
Recent research has identified multiple pathways for modulating these transporters, ranging from dietary interventions to hormonal and pharmaceutical regulation. The following diagram illustrates the key mechanisms by which high-protein diets and the hormone estrogen regulate this system, based on recent findings.
Diagram 1: Signaling Pathways in Glucose Absorption Modulation. This figure illustrates the distinct mechanisms by which high-protein diets (yellow nodes) and estrogen (red nodes) modulate systemic glucose control, ultimately converging on improved postprandial glucose outcomes (blue nodes). The high-protein diet pathway involves hypothalamic signaling and GLP-1 secretion, while the estrogen pathway directly regulates transporter expression via ERα and PKC signaling.
Comparative Efficacy of Dietary Interventions
High-Protein vs. Standard Nutritional Formulas
Clinical studies directly compare the effects of diabetes-specific high-protein nutritional formulas (DSNF-Pro) against standard nutritional formulas (STNF). The quantitative outcomes from a recent cross-over clinical trial are summarized below.
Table 1: Effects of High-Protein vs. Standard Nutritional Formulas on Glycemic Response in Prediabetes [24] [25]
| Parameter | DSNF-Pro | STNF | Relative Change | P-value |
|---|---|---|---|---|
| Postprandial Glucose iAUC | Significantly Lower | Reference | -73.4% | 0.0001 |
| Postprandial C-peptide iAUC | Significantly Lower | Reference | -36.4% | 0.0001 |
| Postprandial Insulin iAUC | No Significant Difference | No Significant Difference | Not Significant | N/S |
| Carbohydrate Content (g/serving) | 12.0 | 21.0 | -42.9% | - |
| Protein Content (g/serving) | 12.0 | 4.9 | +144.9% | - |
This table demonstrates that DSNF-Pro, characterized by higher protein and lower carbohydrate content, significantly improves postprandial glycemic response without increasing insulin secretion, suggesting enhanced insulin sensitivity [24] [25].
Broader Dietary Pattern Comparisons
Beyond specific formulas, various dietary patterns also significantly impact glycemic control and transporter activity. Research across different patient populations, including those with gestational diabetes mellitus (GDM) and type 2 diabetes mellitus (T2DM), provides valuable comparative insights.
Table 2: Efficacy of Broader Dietary Interventions on Glycemic Control [26] [27] [28]
| Dietary Intervention | Population | Key Glycemic Outcomes | Effect Size / Statistical Significance | Proposed Impact on SGLT1/GLUT2 |
|---|---|---|---|---|
| High-Protein Diet (HPD) | T2DM | ↓ Mean 24-h integrated glucose area; ↓ HbA1c | 40% reduction in glucose AUC; HbA1c ↓ 0.8% [6] | Not directly measured, but systemic improvement suggests indirect modulation. |
| DASH Diet | GDM | ↓ Fasting Blood Glucose (FBG); ↓ 2h Postprandial Glucose (2h-PBG); ↓ HOMA-IR | SMD = -2.35 for FBG; SMD = -1.41 for 2h-PBG [26] | Not directly measured. |
| Low-Carbohydrate Diet (LCD) | T2DM | ↓ HbA1c (short-term); improved insulin sensitivity (short-term) | Significant reduction in 16/21 studies [28] | Likely reduces functional load on SGLT1/GLUT2 by limiting substrate availability. |
| Low-Glycemic Index (GI) Diet | GDM | ↓ Risk of macrosomia; improved postprandial glucose regulation | OR = 0.12 for macrosomia [26] | May influence expression/activity via reduced glucose flux and hormonal responses. |
The DASH diet shows the most potent effects on fasting and postprandial glucose in GDM, while HPDs and LCDs demonstrate significant benefits in T2DM management [26] [27] [28].
Experimental Models and Protocols
Key Methodologies for Studying Transporter Function
Understanding the modulation of SGLT1 and GLUT2 relies on robust experimental models, ranging from cellular systems to whole-organ perfusion.
Table 3: Key Experimental Protocols in Intestinal Glucose Absorption Research
| Experimental Model | Protocol Overview | Key Measurements | Context of Use |
|---|---|---|---|
| Cell Culture (Caco-2/TC7) | Differentiated human intestinal epithelial cell monolayers grown in transwell plates. Treated with compounds (e.g., dexamethasone, estrogen) for specified durations. [29] [30] | Glucose uptake assays (e.g., using 2-deoxy-D-glucose); Western blot for transporter protein expression; qPCR for mRNA levels. [30] | Mechanistic studies of hormonal and drug effects on transporter expression and function. |
| Vascularly Perfused Rat Intestine | Isolation and perfusion of the entire rat small intestine with a physiological buffer. Luminal and vascular infusions of glucose and specific inhibitors. [23] | Absorption quantified via radioactive tracers (14C-D-glucose). Paracellular transport assessed with 14C-D-mannitol. [23] | Quantifying contributions of transcellular (SGLT1/GLUT2) vs. paracellular glucose absorption pathways. |
| Using Chamber Experiments | Ex vivo segments of mouse duodenum mounted in chambers separating mucosal and serosal sides. [29] | Electrogenic glucose transport measured as short-circuit current (Isc). | Functional ex vivo assessment of glucose absorption capacity in tissue from different treatment groups. |
| Human Cross-Over Clinical Trials | Participants (e.g., with prediabetes) consume test products (DSNF-Pro vs. STNF) on different visits with washout periods. [24] [25] | Postprandial plasma glucose, serum insulin, and C-peptide measured over 3 hours. Incremental Area Under the Curve (iAUC) calculated. [24] [25] | Direct evaluation of the glycemic impact of dietary interventions in a human physiological context. |
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs critical reagents used in the featured experiments to study SGLT1 and GLUT2 function.
Table 4: Key Research Reagent Solutions for Glucose Transporter Studies
| Reagent / Tool | Function / Application | Example Use in Context |
|---|---|---|
| Phlorizin | Potent and specific competitive inhibitor of SGLT1. | Used in perfused intestine models to block apical SGLT1 activity, allowing quantification of its contribution to total glucose absorption. [23] |
| Phloretin | Inhibitor of facilitative glucose transporters, including GLUT2. | Applied in vascularly perfused rat intestine to block basolateral GLUT2, demonstrating its critical role in glucose efflux. [23] |
| 2-Deoxy-D-Glucose | Non-metabolizable glucose analog. | Used in Caco-2/TC7 cell uptake assays to measure glucose transporter activity specifically, without interference from metabolism. [30] |
| 14C-D-Glucose | Radioactive tracer for glucose. | Enables sensitive and accurate quantification of glucose absorption kinetics in complex ex vivo models like the perfused intestine. [23] |
| Dexamethasone | Synthetic glucocorticoid. | In Caco-2/TC7 cells, it dose-dependently upregulates SGLT1 expression and increases glucose transport, modeling drug-induced hyperglycemia. [30] |
| siRNA (ERα/ERβ) | Silences specific gene expression. | Used in SCBN cell lines to demonstrate that estrogen's upregulation of SGLT1/GLUT2 is mediated specifically by ERα, not ERβ. [29] |
Discussion and Research Implications
The comparative data indicates that high-protein diets and diabetes-specific nutritional formulas achieve significant improvements in glycemic control primarily through systemic effects, such as enhanced insulin sensitivity, increased GLP-1 secretion, and reduced hepatic glucose output, rather than direct inhibition of intestinal glucose transporters [24] [27] [25]. This is a distinct mechanism compared to the direct SGLT1/GLUT2 modulation observed with pharmaceutical agents like dexamethasone or hormonal influences like estrogen [29] [30].
The finding that estrogen enhances SGLT1 and GLUT2 expression via an ERα-PKC pathway provides a plausible physiological explanation for observed fluctuations in glucose tolerance during the menstrual cycle and highlights a significant sex-based variable in glucose metabolism research [29]. Conversely, the pro-hyperglycemic effect of dexamethasone, a widely used anti-inflammatory drug, which potently induces SGLT1 expression, reveals a key mechanism for a common clinical side effect [30].
From a drug development perspective, the direct inhibition of SGLT1 remains a valuable therapeutic target for hyperglycemia, as evidenced by the development of SGLT inhibitors [22]. However, the dietary strategies reviewed here, particularly high-protein and low-carbohydrate diets, offer a complementary approach by reducing the functional load on these transporters and improving whole-body glucose regulation through multiple pathways. Future research should focus on elucidating the precise molecular interactions between dietary components, gut hormones, and transporter regulation, and explore personalized nutrition strategies based on genetic background, sex, and gut microbiome composition.
Branched-chain amino acids (BCAAs)—leucine, isoleucine, and valine—are essential nutrients that exert a complex and dual influence on glucose metabolism. While they are well-known for their role in stimulating protein synthesis, their impact on insulin sensitivity presents a paradox that is of critical importance to researchers and drug development professionals. On one hand, acute postprandial elevations of BCAAs, particularly leucine, can signal nutrient abundance and trigger pathways that improve glycemic control [27] [31]. On the other hand, chronically elevated fasting levels of BCAAs are strongly and consistently associated with obesity, insulin resistance, and the pathogenesis of type 2 diabetes (T2D) [32] [33] [34]. This review synthesizes current experimental data to objectively compare these opposing roles, framing the evidence within the broader thesis on the efficacy of high-protein diets for glucose control.
The Beneficial Face: Mechanisms of BCAA-Induced Insulin Sensitivity
Acute and postprandial exposure to BCAAs, especially within the context of a high-protein diet, can enhance glucose regulation through several well-documented mechanisms. The evidence for these benefits is summarized in the table below.
Table 1: Evidence for the Insulin-Sensitizing Effects of BCAAs and High-Protein Diets
| Mechanism/Effect | Supporting Experimental Data | Model System | Key Findings |
|---|---|---|---|
| Hypothalamic Signaling | [27] | Rodent Studies | Leucine sensing in the medio-basal hypothalamus activates a vagal signal to the liver, reducing hepatic glucose production. |
| Postprandial Glucose Control | [24] [35] | Human Clinical Trial (Prediabetes) | A high-protein, diabetes-specific formula reduced postprandial glucose iAUC by 73.4% (p=0.0001) without increasing insulin secretion. |
| Overall Glycemic Control (HbA1c) | [6] | Human Clinical Trial (T2DM) | A 5-week high-protein diet (30% protein) resulted in a 40% decrease in 24-hour glucose area response and a significant reduction in HbA1c. |
| Mitochondrial Biogenesis | [31] [36] | Pre-clinical & Clinical Evidence | Leucine activates the SIRT1-AMPK-PGC-1α axis, augmenting mitochondrial biogenesis and fatty acid oxidation in muscle and adipose tissue. |
| Muscle Mass Preservation | [37] [31] | Human Clinical Trials | Increased dietary protein during weight loss preserves skeletal muscle mass, the primary site for insulin-stimulated glucose disposal. |
Experimental Insight: Clinical Trials on Diabetes-Specific Nutritional Formulas
A recent open-label, cross-over clinical trial provides a clear example of a beneficial application. The study compared a high-protein, diabetes-specific nutritional formula (DSNF-Pro) against a standard nutritional formula (STNF) in subjects with prediabetes [24] [35].
- Methodology: Fifteen subjects consumed either DSNF-Pro (12g protein, 12g carbohydrate) or an isocaloric STNF (4.9g protein, 21g carbohydrate) after an overnight fast.
- Data Collection: Postprandial plasma glucose, serum insulin, and serum c-peptide were measured over 180 minutes to calculate incremental area under the curve (iAUC).
- Outcome: DSNF-Pro significantly reduced glucose iAUC by 73.4% and c-peptide iAUC by 36.4%, indicating markedly improved glucose handling without requiring increased insulin output [24] [35]. This demonstrates that the macronutrient composition, specifically high protein and low carbohydrate, is critical for glycemic outcomes.
The Adverse Face: BCAA-Induced Insulin Resistance
Paradoxically, despite the benefits of acute intake, chronic elevations in fasting BCAA levels are one of the earliest and strongest predictive biomarkers for the development of insulin resistance and T2D [32] [33] [34]. The mechanisms underlying this detrimental role are outlined below.
Table 2: Mechanisms Linking Elevated BCAAs to Insulin Resistance
| Proposed Mechanism | Experimental Support | Model System | Key Findings |
|---|---|---|---|
| Chronic mTOR Activation | [31] [33] | Cell & Rodent Studies | Chronic, as opposed to acute, activation of mTORC1-S6K1 signaling leads to serine phosphorylation of IRS-1, impairing insulin signaling. |
| Disrupted Tissue Catabolism | [33] [34] | Human & Rodent Studies | Obesity-related downregulation of BCKDH complex in adipose tissue and liver shunts BCAA oxidation to skeletal muscle, disrupting metabolic homeostasis. |
| Toxic Metabolite Accumulation | [33] [34] | Rodent Studies | Incomplete BCAA oxidation in muscle leads to accumulation of metabolites like 3-hydroxyisobutyrate (3-HIB), which promotes fatty acid uptake and lipid-induced insulin resistance. |
| Acute Impairment of Insulin Sensitivity | [32] | Rodent Study | A single acute infusion of BCAAs was sufficient to elevate blood glucose and impair whole-body insulin sensitivity during hyperinsulinemic-euglycemic clamps. |
| AgRP Neuron Mediation | [32] | Rodent Study | Chemogenetic over-activation of AgRP neurons (as in obesity) impaired glucose tolerance, an effect normalized by acute BCAA reduction, linking neural pathways to BCAA-driven dysregulation. |
Experimental Insight: Acute BCAA Infusion and AgRP Neuron Studies
A pivotal 2024 study demonstrated that BCAAs per se can directly and acutely drive glucose dysregulation [32].
- Methodology: Catheter-guided frequent sampling was used in mice to assess the acute metabolic effects of a single BCAA infusion. Separately, hyperinsulinemic-euglycemic clamps (the gold standard for assessing insulin sensitivity) were performed with constant BCAA infusion. The BCAA-lowering compound BT2 was used to test the converse.
- Data Collection: Frequent measurements of blood glucose and plasma insulin were taken. During clamps, the glucose infusion rate required to maintain euglycemia was measured.
- Outcome: Acute BCAA infusion elevated blood glucose and insulin and directly impaired whole-body insulin sensitivity. Conversely, a single BT2 injection improved glucose tolerance in obese mice. Furthermore, impaired glucose tolerance induced by stimulating AgRP neurons was fully normalized by lowering BCAAs, establishing a causal pathway [32].
Signaling Pathways: The Dual Molecular Mechanisms of BCAAs
The following diagrams illustrate the key signaling pathways that explain the dual roles of BCAAs, integrating the mechanisms discussed above.
Pathway 1: Insulin-Sensitizing signaling
Diagram 1: BCAA insulin-sensitizing pathways.
Pathway 2: Insulin-Resistance signaling
Diagram 2: BCAA insulin-resistance pathways.
The Scientist's Toolkit: Key Research Reagents and Models
Table 3: Essential Reagents and Models for BCAA-Insulin Resistance Research
| Tool/Reagent | Function/Application | Example Use in Research |
|---|---|---|
| Hyperinsulinemic-Euglycemic Clamp | Gold-standard in vivo method for quantifying whole-body insulin sensitivity. | Used to demonstrate that acute BCAA infusion impairs insulin sensitivity in mice [32]. |
| BCAA-Lowering Compound (BT2) | Pharmacological inhibitor of BCKDK, increasing BCAA oxidation and lowering circulating BCAA levels. | Acute injection prevented fasting BCAA rise and improved glucose tolerance in high-fat-fed mice [32]. |
| DREADD (Designer Receptors) | Chemogenetic tool for selective activation or inhibition of specific neuronal populations. | Used to activate AgRP neurons in the hypothalamus, linking their activity to BCAA-mediated glucose dysregulation [32]. |
| Stable Isotope Tracers | Allow for tracing the metabolic fate of BCAAs and measuring tissue-specific oxidation rates. | Used in human studies to identify brown adipose tissue as a significant site of BCAA clearance [33]. |
| Mass Spectrometry (CG-MS/MS, HPLC-MS/MS) | Analytical platform for precise quantification of BCAAs and their downstream metabolites (e.g., 3-HIB, acylcarnitines). | Used to profile plasma metabolites and correlate BCAA levels with insulin resistance in human cohorts [34]. |
| AgRP-IRES-Cre Mouse Model | Genetic model enabling targeted manipulation of AgRP neurons, which are implicated in feeding behavior and glucose metabolism. | Critical for establishing the role of AgRP neurons in BCAA-driven glucose intolerance [32]. |
The relationship between BCAAs and insulin sensitivity is fundamentally dichotomous, hinging on context—acute versus chronic exposure, postprandial versus fasting states, and the metabolic health of the individual. High-protein diets can be effective for glucose control, as shown by the success of specialized nutritional formulas, largely through the acute signaling properties of leucine and the preservation of metabolically active muscle mass [24] [27] [6]. However, in states of energy overload and obesity, a cascade of events—including dysfunctional BCAA catabolism in adipose tissue, shunting to muscle, and accumulation of toxic metabolites—flips this relationship, establishing BCAAs as drivers of insulin resistance [32] [33] [34]. For drug development, this implies that therapeutic strategies should not seek to broadly inhibit BCAA action but rather to correct the underlying dysregulation of their metabolism, such as by enhancing BCAA oxidation in key tissues or targeting specific downstream effectors like 3-HIB. Future research should focus on the precise molecular switches that transition BCAA effects from beneficial to detrimental.
Clinical Translation: Implementing High-Protein Interventions in Diabetes Management
Medical Nutrition Therapy (MNT) represents a cornerstone in the prevention and management of diabetes, with particular emphasis on postprandial glucose regulation for overall glycemic control [38]. As prediabetes and diabetes continue to reach epidemic proportions globally, the development of targeted nutritional strategies has become increasingly crucial [38] [28]. Diabetes-Specific Nutritional Formulas (DSNF) have emerged as scientifically-designed interventions that modify macronutrient composition to optimize glycemic response. These formulas are characterized by their distinctive macronutrient profiles, which typically include reduced carbohydrate content, increased protein, elevated monounsaturated fatty acids (MUFAs), and added dietary fiber [38] [39]. This review examines the composition and efficacy evidence for DSNFs, positioning them within the broader context of high-protein dietary strategies for glucose control, and provides researchers with methodological insights for evaluating their therapeutic potential.
Composition Analysis: DSNF Versus Standard Nutritional Formulas
Macronutrient Architecture
DSNFs are engineered with specific macronutrient modifications that differentiate them from standard nutritional formulas. The compositional adjustments are strategically designed to attenuate postprandial glycemic excursions while providing adequate nutritional support.
Table 1: Comparative Macronutrient Composition of DSNF Versus Standard Formulas
| Formula Type | Energy (kcal) | Protein (g) | Carbohydrates (g) | Fat (g) | MUFA Content | Dietary Fiber | Special Carbohydrates |
|---|---|---|---|---|---|---|---|
| DSNF-Pro [38] | 140 | 12 | 12 | 6 | 60% of total fat | Included | Xylitol, Palatinose |
| Standard Formula [38] | 140 | 4.9 | 21 | 4.2 | Not specified | Not specified | Standard carbohydrates |
| DSNF (Nucare) [40] | 200 | 10.4 | 22.4 | 10.4 | 30.3% of total energy | Included | Allulose (D-psicose) |
| Standard ONS [40] | 200 | 7 | 30 | 6 | Not specified | Not specified | Standard carbohydrates |
Functional Components and Glycemic Modulation Mechanisms
The efficacy of DSNFs extends beyond basic macronutrient distribution to include specific functional components that actively modulate glucose metabolism:
- Carbohydrate Quality Modification: DSNFs incorporate low glycemic index (GI) carbohydrates such as palatinose, xylitol, and allulose (D-psicose), which slow digestion and absorption rates, thereby producing more gradual postprandial glucose elevations [38] [40].
- Protein Enrichment: High-protein DSNF variants provide approximately 12g of protein per serving, representing a significant increase compared to standard formulas (4.9g), which may enhance satiety and stimulate insulin secretion without disproportionate glucose elevation [38].
- Lipid Profile Optimization: The strategic inclusion of monounsaturated fatty acids (MUFAs), comprising up to 60% of total fat content in some formulations, contributes to improved insulin sensitivity and favorable lipid profiles [38] [39].
- Fiber Supplementation: Dietary fiber content in DSNFs delays gastric emptying and intestinal carbohydrate absorption, further blunting postprandial glycemic spikes [40].
Efficacy Evidence: Quantitative Clinical Outcomes
Effects on Glycemic Parameters
Randomized controlled trials and clinical studies have consistently demonstrated the superior glycemic efficacy of DSNFs compared to standard nutritional formulas across multiple parameters.
Table 2: Efficacy Outcomes of DSNF Versus Standard Formulas in Clinical Studies
| Study Design | Population | Intervention | Primary Outcomes | Statistical Significance |
|---|---|---|---|---|
| Open-label, cross-over clinical trial [38] [25] | 15 prediabetic adults | DSNF-Pro vs. STNF | ↓ 73.4% in glucose iAUC | p = 0.0001 |
| ↓ 36.4% in c-peptide iAUC | p = 0.0001 | |||
| No significant difference in insulin iAUC | Not significant | |||
| Open-label, crossover clinical trial [40] | 15 prediabetic adults | DSNF vs. standard ONS | ↓ Significant reduction in glucose iAUC | P < 0.0001 |
| ↓ Significant reduction in insulin iAUC | P = 0.0181 | |||
| ↓ Significant reduction in c-peptide iAUC | P < 0.0001 | |||
| Longitudinal pilot study [39] | 11 overweight/obese diabetic patients | DSNF for 4 weeks | ↑ Time in Range (TIR) from 64% to 75% | p = 0.01 |
| ↓ Time Above Range (TAR) from 34% to 23% | p = 0.02 |
Comparative Efficacy Against Other Dietary Interventions
The efficacy of DSNFs must be contextualized within the broader landscape of dietary interventions for glucose management:
- Low-Carbohydrate Diets (LCDs): A recent umbrella meta-analysis of 21 randomized controlled trials demonstrated that LCDs (≤130g carbohydrate/day) significantly reduce HbA1c in 16 of 21 studies, with substantial short-term improvements in glycemic control [28]. However, benefits attenuated over longer durations, highlighting sustainability challenges.
- High-Protein Diets: Systematic reviews indicate that high-protein diets (25-35% of energy intake) improve postprandial glycemia through increased insulin secretion, with protein source appearing more relevant in acute studies than longer interventions [41] [27].
- DASH and Low-GI Diets: A network meta-analysis of gestational diabetes management identified the DASH diet as most effective for reducing fasting blood glucose, while both DASH and Low-GI diets reduced adverse pregnancy outcomes [42].
Experimental Methodology for DSNF Evaluation
Standardized Clinical Trial Protocols
Robust evaluation of DSNF efficacy requires carefully controlled experimental designs with standardized protocols:
Laboratory Assessment Methodologies
Consistent laboratory techniques are essential for reliable comparison of DSNF efficacy across studies:
- Plasma Glucose Measurement: Enzymatic colorimetric glucose oxidase assays (e.g., ADAMS glucose GA-1171) provide precise quantification of glucose concentrations in EDTA-treated blood samples [38] [40].
- Insulin and C-Peptide Quantification: Radioimmunoassay methods (e.g., RK-400CT, C-peptide IRMA KIT) enable sensitive detection of insulin secretion and beta-cell function from serum separator tubes [38] [40].
- Data Analysis Parameters: Key efficacy endpoints include incremental Area Under the Curve (iAUC), maximum concentration (Cmax), and incremental maximal concentration (iCmax) for glucose, insulin, and c-peptide, typically analyzed using non-parametric tests like Wilcoxon's signed-rank test for paired comparisons [38] [40].
Mechanistic Insights: Metabolic Pathways of DSNF Action
The glycemic benefits of DSNFs are mediated through multiple physiological mechanisms that extend beyond simple carbohydrate reduction:
Neurological and Endocrine Pathways
Emerging research elucidates sophisticated mechanisms through which high-protein DSNFs influence glycemic control:
- Hypothalamic Nutrient Sensing: Branched-chain amino acids (BCAAs), particularly leucine, directly access the medio-basal hypothalamus through the permeable microvasculature in the arcuate nucleus, where metabolic conversion to oleoyl-CoA activates hypothalamic ATP-sensitive potassium (KATP) channels [27]. This generates a neuronal signal transmitted via the vagus nerve to the liver, reducing hepatic glucose production through inhibition of gluconeogenesis and glycogenolysis [27].
- Incretin-Mediated Effects: BCAAs stimulate secretion of gut hormones including glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic peptide (GIP), which enhance the functional balance of pancreatic α and β cells, decreasing glucagon production while increasing insulin release [27].
- Insulin-Sparing Action: Clinical evidence indicates that DSNF-Pro significantly reduces postprandial glucose without increasing insulin secretion, as demonstrated by reduced c-peptide iAUC without significant changes in insulin iAUC, suggesting improved insulin sensitivity and reduced beta-cell demand [38].
Research Reagent Solutions: Essential Materials for DSNF Investigation
Table 3: Essential Research Reagents and Materials for DSNF Investigations
| Category | Specific Reagents/Assays | Research Application | Key Features |
|---|---|---|---|
| Blood Collection | EDTA-treated tubes, Serum Separator Tubes (SST) | Sample collection and preservation | Prevents coagulation, maintains sample integrity |
| Glucose Assessment | Enzymatic colorimetric glucose oxidase assay (ADAMS glucose GA-1171) | Plasma glucose quantification | Specific glucose oxidation reaction |
| Insulin Measurement | Radioimmunoassay (RK-400CT) | Serum insulin detection | High sensitivity for low concentration peptides |
| C-Peptide Analysis | C-peptide IRMA KIT (Beckman Coulter) | Beta-cell function assessment | Distinguishes endogenous from exogenous insulin |
| Body Composition | Bioelectrical impedance analysis (Inbody 970) | Anthropometric evaluation | Quantifies muscle mass, fat mass, body fat percentage |
| Continuous Monitoring | FreeStyle Libre CGM System (Abbott) | Real-time glycemic assessment | Measures interstitial glucose, calculates TIR, TAR, TBR |
| Dietary Assessment | CAN-Pro 6.0 Software | Nutritional intake analysis | Standardized nutrient composition database |
| Physical Activity | International Physical Activity Questionnaire (IPAQ) | MET-min/week calculation | Quantifies energy expenditure across intensity levels |
Diabetes-Specific Nutritional Formulas represent a scientifically-validated approach to glycemic management through targeted macronutrient modification. Evidence from controlled clinical trials demonstrates that DSNFs significantly improve postprandial glycemic parameters compared to standard nutritional formulas, with high-protein variants exhibiting particular efficacy in reducing glucose excursions without proportionally increasing insulin secretion [38] [25] [40]. The mechanisms underlying these benefits involve complex interactions between nutrient composition, neurological signaling pathways, and endocrine responses [27].
Future research should address several critical knowledge gaps: (1) long-term efficacy and sustainability of DSNF interventions beyond acute postprandial studies; (2) comparative effectiveness of different protein sources (animal versus plant-based) within DSNF formulations; (3) personalized nutrition approaches to match specific DSNF compositions to individual metabolic phenotypes; and (4) potential synergistic effects between DSNFs and pharmacological antidiabetic agents. The ongoing development and refinement of DSNFs holds significant promise for enhancing medical nutrition therapy as both a preventive and management strategy across the diabetes spectrum.
The management of blood glucose levels is a critical focus in metabolic health research, particularly for conditions like prediabetes and type 2 diabetes mellitus (T2DM). Within this context, high-protein diets (HPDs), typically defined as providing >30% of total energy from protein or >1.0-1.2 g/kg/day, have emerged as a significant dietary strategy against standard diets [27]. These diets are thought to improve glycemic control through multiple mechanisms, including enhanced insulin sensitivity, increased satiety leading to weight loss, and direct signaling effects of amino acids on metabolic pathways [27]. However, simply increasing total daily protein intake does not tell the complete story. Emerging evidence suggests that the temporal distribution of protein intake across meals—the specific dosage per meal and the timing of consumption—plays a crucial role in optimizing metabolic outcomes and anabolic potential [43] [44]. This guide provides a comparative analysis of experimental data and methodologies to inform research on protein distribution strategies, with a specific focus on implications for glucose control.
Comparative Analysis: High-Protein vs. Standard Nutritional Formulas
Clinical trials directly comparing diabetes-specific nutritional formulas (DSNF) with standard formulas provide compelling evidence for the role of macronutrient composition in postprandial metabolism.
Table 1: Postprandial Metabolic Responses to Nutritional Formulas
| Metabolic Parameter | DSNF-Pro (High-Protein) | Standard Formula (STNF) | Relative Change (%) | P-value |
|---|---|---|---|---|
| Postprandial Glucose iAUC | Significantly Reduced | Baseline | -73.4% | 0.0001 |
| Postprandial C-peptide iAUC | Significantly Reduced | Baseline | -36.4% | 0.0001 |
| Postprandial Insulin iAUC | No Significant Difference | No Significant Difference | N.S. | N.S. |
| Carbohydrate Content (g/serving) | 12.0 | 21.0 | -42.9% | - |
| Protein Content (g/serving) | 12.0 | 4.9 | +144.9% | - |
| Dietary Fiber Content (g/serving) | 5.0 | 0.84 | +495.2% | - |
Source: Adapted from Kim et al. (2025). An open-label, cross-over clinical trial in subjects with prediabetes (n=15) [24].
A recent open-label, cross-over clinical trial demonstrated the efficacy of a high-protein, diabetes-specific nutritional formula (DSNF-Pro) compared to a standard nutritional formula (STNF) in individuals with prediabetes. The DSNF-Pro provided 12g of protein and 12g of carbohydrates per 140 kcal serving, whereas the STNF provided 4.9g of protein and 21g of carbohydrates for the same caloric content [24]. As summarized in Table 1, the DSNF-Pro group exhibited a dramatic 73.4% reduction in postprandial glucose incremental Area Under the Curve (iAUC) and a 36.4% reduction in C-peptide iAUC, indicating a significantly improved glycemic response without a corresponding increase in insulin secretion [24]. This suggests that the high-protein, low-carbohydrate formulation improves glucose metabolism through enhanced insulin sensitivity rather than by increasing β-cell demand.
Experimental Protocol: Nutritional Formula Cross-Over Trial
Objective: To evaluate the effects of a high-protein, diabetes-specific nutritional formula (DSNF-Pro) versus a standard nutritional formula (STNF) on postprandial glycemic control, insulin, and C-peptide levels in subjects with prediabetes [24].
Methodology:
- Design: Open-label, randomized, cross-over clinical trial.
- Subjects: Fifteen adults with prediabetes (defined by HbA1c 5.6-6.4% or fasting blood glucose 100-125 mg/dL).
- Intervention: After a 10-12 hour overnight fast, subjects consumed either DSNF-Pro or STNF on separate visits, with a washout period of 1-14 days between visits.
- Blood Sampling: Venous blood samples were collected via catheter at fasting (0 min) and at 30, 60, 90, 120, and 180 minutes post-consumption.
- Sample Analysis:
- Plasma Glucose: Measured using an enzymatic colorimetric glucose oxidase assay.
- Serum Insulin and C-peptide: Measured using radioimmunoassay (RIA) kits.
- Data Analysis: The incremental Area Under the Curve (iAUC) for glucose, insulin, and C-peptide was calculated. Statistical comparisons were performed using Wilcoxon’s signed-rank test [24].
Protein Dosage Per Meal and Metabolic Utilization
A foundational question in protein distribution research involves determining the optimal dosage per meal to maximize metabolic utilization, particularly for musculoskeletal accretion, which is critical for overall metabolic health.
Single-Meal Protein Dosing and Muscle Protein Synthesis
Groundbreaking research has challenged the long-held belief that muscle protein synthesis (MPS) is maximized at a dose of approximately 20-25 grams of protein per meal. A rigorous study investigated the metabolic fate of ingested protein over a 12-hour period following a full-body resistance training session.
The study by Trommelen et al. (as reviewed by Trexler) involved administering 0g, 25g, or 100g of milk protein to trained males after exercise. The results revealed a clear dose-dependent relationship. While the 25g dose elevated protein synthesis, the 100g dose resulted in a significantly greater cumulative anabolic response. Crucially, the advantage of the large dose was its ability to extend the duration of the anabolic window; protein synthesis rates remained elevated for up to 12 hours, compared to a return to baseline by approximately 6 hours with the 25g dose [45]. This demonstrates that the body can effectively utilize large boluses of protein, primarily by sustaining a higher rate of protein synthesis over many hours, with only a negligible amount being oxidized ("wasted") [45].
Table 2: Protein Distribution Patterns in Resistance Training
| Parameter | Three High-Protein Meals (PRO3x) | Five High-Protein Meals (PRO5x) | Between-Group Difference |
|---|---|---|---|
| Daily Protein Intake | Similar (Optimal per meal) | Similar (Optimal per meal) | Not Significant |
| Lean Mass Gain (kg) | 1.15 ± 1.54 | 0.63 ± 1.32 | N.S. |
| Vastus Lateralis CSA Gain (cm²) | 3.41 ± 3.79 | 2.53 ± 3.31 | N.S. |
| Knee Extension 1RM Gain (kg) | 19.08 ± 7.56 | 16.01 ± 5.17 | N.S. |
Source: Adapted from Randomized Controlled Trial (2025) in young, resistance-trained men (n=18 completers) over 8 weeks [43].
When protein intake is sufficient and energetically balanced, the frequency of distribution may be of secondary importance for body composition. An 8-week randomized trial with resistance-trained men compared consuming high-protein meals (>0.24 g/kg/meal) three times per day (PRO3x) versus five times per day (PRO5x). As shown in Table 2, both groups achieved significant and comparable gains in lean mass, muscle cross-sectional area (CSA), and strength, with no statistically significant differences between the protocols [43]. This indicates that for muscle anabolism, achieving an optimal per-meal dose (in this case, >0.24 g/kg/meal) is a key factor, and this can be effectively accomplished with either three or five meals per day.
Synergy with Time-Restricted Eating and Other Dietary Regimens
Integrating high-protein diets with other dietary strategies, such as time-restricted eating (TRE), creates a synergistic approach that can simultaneously improve body composition and metabolic health.
High-Protein Time-Restricted Eating
Research has demonstrated that combining TRE with high-protein intake can yield superior outcomes. A randomized controlled trial in women with overweight compared four groups: TRE with high protein (THP), TRE with regular protein, high protein only (HP), and regular protein only, with all groups undergoing resistance training and a calorie deficit.
Table 3: High-Protein TRE vs. Other Diets in Overweight Women
| Outcome Measure | TRE + High Protein (THP) | High Protein Only (HP) | TRE + Regular Protein | Regular Protein Only |
|---|---|---|---|---|
| Visceral Adipose Tissue (VAT) Reduction | Δ = -146.98 ± 12.66 (Greatest decrease) | Significant Reduction | Significant Reduction | Significant Reduction |
| Fat-Free Mass (FFM) Change | Δ = +1.06 ± 1.75 (Preserved) | Δ = +2.37 ± 0.64 (Increased) | Not Specified | Not Specified |
| Leptin Reduction | Significant (vs. Regular Protein Only) | Not Specified | Significant (vs. Regular Protein Only) | Baseline |
Source: Adapted from International Journal of Sport Nutrition and Exercise Metabolism (2025). 8-week RCT in young women with overweight (n=32) [46].
The results, summarized in Table 3, show that while all groups lost adipose tissue, the THP group exhibited the greatest reduction in visceral adipose tissue (VAT). Notably, the high-protein groups (THP and HP) were the only ones to show a significant increase in fat-free mass, demonstrating the power of elevated protein intake to preserve or even build muscle during a calorie-restricted diet—a critical factor for maintaining metabolic rate [46].
Comparison with Other Dietary Interventions for Glycemic Control
Other dietary interventions also show efficacy for glycemic control. A meta-analysis of eight randomized controlled trials concluded that fasting interventions (including intermittent fasting and TRE) significantly improved fasting blood glucose, HbA1c, and HOMA-IR (a measure of insulin resistance) [47]. Another umbrella meta-analysis found that low-carbohydrate diets (LCDs) provide substantial short-term improvements in HbA1c for patients with T2DM, though long-term sustainability varies [28]. A head-to-head comparison of intermittent energy restriction (IER), TRE, and continuous energy restriction (CER) in patients with obesity and T2DM found that all three improved HbA1c and body weight, but the IER group showed greater advantages in reducing fasting glucose and improving insulin sensitivity [48].
The following diagram synthesizes the mechanistic pathways through which high-protein diets, particularly those rich in leucine, are believed to exert their glucoregulatory effects, integrating findings from pre-clinical and clinical studies [27].
The Scientist's Toolkit: Key Research Reagents and Methodologies
To conduct rigorous research in protein metabolism and glycemic control, specific tools and methodologies are essential. The following table details key components used in the featured experiments.
Table 4: Research Reagent Solutions for Metabolic Studies
| Reagent / Material | Function / Application | Example Use in Cited Research |
|---|---|---|
| Intrinsically Labeled Milk Protein | Metabolic tracer to directly follow the fate, oxidation, and incorporation of ingested amino acids into body proteins. | Trommelen et al. used L-[1-13C]-phenylalanine and L-[ring-2H5]-phenylalanine labels to quantify protein metabolism over 12 hours [45]. |
| Stable Isotope Infusions (L-[ring-13C6]-phenylalanine) | Intravenous infusion of labeled amino acids to measure whole-body and muscle-specific protein synthesis and breakdown rates. | Used in conjunction with ingested labeled protein to create a comprehensive model of protein flux [45]. |
| Radioimmunoassay (RIA) Kits | High-sensitivity measurement of hormone concentrations in serum/plasma (e.g., insulin, C-peptide). | Used to measure serum insulin and C-peptide levels in the DSNF-Pro vs. STNF trial [24]. |
| Enzymatic Colorimetric Assays (Glucose Oxidase) | Standardized method for precise quantification of plasma glucose concentrations. | Used for all plasma glucose measurements in the nutritional formula clinical trial [24]. |
| Dual-Energy X-ray Absorptiometry (DXA) | Gold standard for in vivo body composition analysis (fat mass, lean soft tissue mass, bone mineral density). | Used to assess lean mass changes in the protein distribution and TRE studies [43] [46]. |
| Muscle Biopsy & Analysis | Collection of muscle tissue for direct measurement of fractional synthesis rate (FSR), signaling pathways, and gene expression. | Vastus lateralis biopsies were used to measure muscle protein synthesis and molecular responses [45]. |
The evidence demonstrates that high-protein diets offer a significant advantage over standard diets for glycemic control, primarily by improving postprandial glucose responses and enhancing insulin sensitivity without necessarily increasing insulin secretion [24] [27]. The optimization of this strategy, however, depends on protein distribution. Key considerations for researchers and clinicians include:
- Per-Meal Dosage: The concept of a rigid upper limit for protein utilization per meal is outdated. Doses as high as 100g can be effectively utilized over a prolonged period, sustaining an elevated anabolic state, particularly when combined with exercise [45].
- Distribution Frequency: When per-meal protein intake meets a theorized optimal threshold (e.g., >0.24 g/kg/meal), distributing intake across three or more meals per day is effective for anabolism, with no clear superiority of more frequent feeding in balanced conditions [43] [44].
- Synergistic Protocols: Combining high-protein intake with time-restricted eating or energy restriction creates a powerful intervention for reducing adipose tissue while critically preserving fat-free mass, leading to superior overall body composition and metabolic health outcomes [46] [48].
Future research should focus on refining optimal protein dosages for diverse populations (e.g., elderly, clinically compromised) and further elucidating the molecular mechanisms, such as hypothalamic signaling, by which amino acids regulate systemic glucose metabolism.
High-protein diets (HPDs) have become a prominent dietary strategy for managing obesity and type 2 diabetes (T2D). For researchers and drug development professionals, understanding the precise effects of HPDs on body composition and glycemic control is crucial for developing targeted nutritional interventions and adjuvants to pharmacotherapy. This guide objectively compares the efficacy of HPDs against standard-protein diets (SPDs) by synthesizing data from recent clinical trials, animal studies, and mechanistic investigations. The evidence is framed within the broader thesis that HPDs offer specific metabolic advantages beyond mere weight loss, particularly for glucose homeostasis, though key variables such as protein source and genetic background can modulate these effects.
Comparative Analysis of High-Protein vs. Standard-Protein Diets
Clinical trials consistently demonstrate that energy-restricted HPDs are effective for weight loss and improving metabolic parameters. However, their superiority over SPDs can depend on the specific patient population and outcome measures. The table below synthesizes key findings from controlled interventions.
Table 1: Clinical Outcomes of High-Protein vs. Standard-Protein Diets in Weight Loss Interventions
| Study Population | Intervention Duration | Diet Composition | Weight Loss (High-Protein vs. Standard-Protein) | Impact on Glycemic Parameters | Effect on Body Composition |
|---|---|---|---|---|---|
| Overweight/obese adults with T2D [3] | 52 weeks | HP: 40% Protein, 32% CHONP: 21% Protein, 53% CHO | HP: -10.2 kgNP: -12.7 kg (p=0.336) | No significant difference in HbA1c, glucose, or insulin improvement between groups. | Both groups reduced fat mass and increased fat-free mass percentage similarly. |
| Overweight/obese patients with Heart Failure and T2D [49] | 12 weeks | HP: 30% Protein, 40% CHOSP: 15% Protein, 55% CHO | HP: -3.6 kgSP: -2.9 kg | HP superior: HbA1c reduced by 0.7% vs. 0.1% (p=0.002). | Both diets reduced visceral fat; greater improvement in BP and lipid profile with HP. |
| Individuals with Overweight/Obesity [50] | 4 weeks | HPLC: ~100 g protein/day, 800 kcal | Significant decreases in weight, BMI, WC, and WHR (all p<0.05). | Not the primary focus; diet modified the obesogenic effect of FTO gene variation. | Significant reduction in waist circumference (WC) and waist-to-hip ratio (WHR). |
| Untreated T2D (Weight-Stable) [6] | 5 weeks (metabolic effects) | HP: 30% Protein, 40% CHOSP: 15% Protein, 55% CHO | Weight-stable study design. | HP superior: 40% decrease in 24-h glucose AUC; HbA1c decreased 0.8% vs. 0.3%. | Not assessed (weight-stable). |
Key Comparative Insights
- Weight Loss Efficacy: The data does not consistently show that HPDs yield significantly greater weight loss than SPDs under conditions of equal calorie restriction [3]. The primary driver of weight loss appears to be energy restriction itself.
- Glycemic Control Superiority: HPDs can demonstrate a significant advantage in improving glycemic parameters, such as HbA1c and 24-hour glucose area-under-the-curve, even in the absence of greater weight loss [6] [49]. This suggests a direct, weight-independent metabolic benefit of increased protein intake on glucose metabolism.
- Cardiometabolic Benefits: HPDs may offer broader cardiometabolic improvements compared to SPDs, including greater reductions in blood pressure, triglycerides, and total cholesterol, as observed in high-risk populations [49].
The Influence of Protein Source
A critical question is whether the source of dietary protein—animal versus plant—alters the effectiveness of a high-protein diet. Evidence from human and animal studies provides a nuanced perspective.
Table 2: Animal vs. Plant Protein Sources in High-Protein Diets
| Study Model | Intervention Diets | Key Findings on Body Composition | Key Findings on Metabolic Parameters |
|---|---|---|---|
| Human RCT (Prediabetes/T2D) [51] | HPA: 75% Animal ProteinHPP: 75% Plant Protein(Both: 35% Protein) | Similar improvements in weight loss (HPA: -8.05 kg, HPP: -7.70 kg) and reduction in visceral fat mass. | Nearly identical improvements in fasting glucose, insulin, HOMA-IR, HbA1c, lipid profile, and inflammatory biomarkers. |
| Rodent Model (fa/fa Zucker rats) [52] | HPDs (35% protein) from Casein, Egg White, Soy+Pea, or a mixture. | HPDs with egg white or plant mixes led to smaller adipocytes despite more visceral fat (plant group). | Diets with egg white, soy+pea, or a mixture reduced fasting insulin and prevented pancreatic islet enlargement vs. casein. |
Interpretation of Protein Source Data
- Human Clinical Reality: In the context of calorie-restricted diets for weight loss, the source of protein (animal or plant) does not appear to significantly impact the diet's effectiveness for improving body composition or glycemic control [51]. This suggests that for these primary outcomes, achieving the target protein intake is more important than its source.
- Mechanistic Animal Evidence: Animal models, however, indicate that protein source can indeed influence underlying metabolic pathways, such as adipocyte morphology and insulinemia [52]. This highlights that while clinical endpoints may be similar, the pathophysiological mechanisms may differ.
- Considerations Beyond Efficacy: While efficacy may be equivalent, plant-based HPDs may offer advantages for long-term health and sustainability, aligning with recent Dietary Guidelines Advisory Committee recommendations to prioritize plant-based proteins for chronic disease prevention [53]. Plant proteins also introduce considerations of amino acid completeness and the presence of anti-nutrients, which can affect digestibility and nutrient bioavailability [54] [55].
Detailed Experimental Protocols
To enable replication and critical appraisal, below are the methodologies from two key cited studies.
Protocol 1: Human RCT on Protein Source (2025)
This randomized controlled trial investigated the effect of protein source in a high-protein, low-calorie diet [51].
- Participants: 117 adults aged >18 years with BMI >27.5 kg/m² and prediabetes or T2D.
- Intervention: Participants were randomized to one of two isocaloric, hypocaloric diets (35% of calories from protein, 30% from fat, 35% from carbohydrates) for 6 months.
- HPA Diet: 75% of total protein from animal sources (e.g., meat, dairy).
- HPP Diet: 75% of total protein from plant sources (e.g., legumes, nuts, soy).
- Outcome Measures:
- Primary: Changes in body weight, body composition (including visceral fat via DXA), and glycemic control (fasting glucose, insulin, HOMA-IR, HbA1c).
- Secondary: Lipid profile, liver enzymes, adipokines, inflammatory biomarkers, and fasting incretins (GLP-1).
- Statistical Analysis: Linear mixed models were used to assess changes over time between the two diet groups.
Protocol 2: Rodent Model on Protein Source (2025)
This preclinical study examined the mechanistic role of protein sources in obesity and insulin resistance [52].
- Animals: Obese male fa/fa Zucker rats.
- Intervention: Rats were fed high-protein diets (35% of energy) for 8 weeks. Protein sources included:
- Casein
- Egg white protein
- Soy and pea protein mix
- A mixture of egg white, soy, and pea proteins
- A control group received a normal protein diet (15% energy) with casein.
- Outcome Measures:
- Metabolic Phenotyping: Oral glucose tolerance test, weight gain, fat depot mass.
- Serum Biochemistry: Insulin, non-esterified fatty acids (NEFAs).
- Tissue Analysis: Adipocyte and pancreatic islet size histomorphometry.
- Molecular Signaling: Markers of adipose tissue lipolysis (ATGL, HSL), insulin signaling (Akt, AS160), and immune cell infiltration (CD3, F4/80).
Signaling Pathways and Conceptual Workflows
The following diagrams illustrate the proposed mechanistic pathways through which high-protein diets and specific protein sources influence metabolic outcomes.
Protein-Mediated Metabolic Improvement Pathway
Diagram: Multifactorial pathways linking high-protein intake to metabolic improvements, involving both weight-loss dependent and direct mechanisms.
Protein Source Impact on Adipose Tissue
Diagram: Proposed mechanism whereby protein sources like egg white and plant mixes favorably influence adipose tissue morphology and pancreatic function, independent of total fat mass, as seen in rodent models [52].
The Scientist's Toolkit: Research Reagent Solutions
This table outlines key reagents and tools essential for conducting research in this field, as derived from the analyzed studies.
Table 3: Essential Research Reagents and Materials for High-Protein Diet Studies
| Item Name | Function/Application | Example Use in Context |
|---|---|---|
| Dual-Energy X-ray Absorptiometry (DXA) | Precisely measures body composition, including fat mass, lean mass, and visceral adipose tissue. | Primary outcome tool for quantifying changes in body composition in human RCTs [51] [3]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Quantifies specific proteins or biomarkers in serum/plasma (e.g., insulin, adipokines, incretins, inflammatory cytokines). | Used to measure GLP-1, IL-6, and CML (advanced glycation end-product) in human and rodent studies [51] [50]. |
| Oral Glucose Tolerance Test (OGTT) | Assesses glucose clearance and insulin response to a standardized glucose load, measuring insulin sensitivity. | Standard metabolic phenotyping tool used in both clinical and rodent studies [52]. |
| High-Resolution Histomorphometry | Quantifies cellular-level changes in tissue architecture (e.g., adipocyte size, pancreatic islet area). | Key technique in rodent studies for showing differences in adipocyte and islet size between protein sources [52]. |
| Genotyping Assays (e.g., TaqMan) | Determines genetic variants of participants (e.g., FTO rs9939609) to investigate diet-gene interactions. | Used to stratify human participants by FTO genotype to analyze differential diet response [50]. |
| Standardized Food Frequency Questionnaire (FFQ) | Estimates habitual dietary intake of participants in observational studies or to verify compliance in trials. | Critical for assigning exposure groups in large cohort studies emulating dietary trials [56]. |
The collective evidence strongly supports the inclusion of high-protein diets as an effective strategy within weight loss interventions for improving body composition and glycemic parameters. For researchers, the key takeaways are that the achieved weight loss is a primary mediator of metabolic benefits, but high protein intake itself can confer additional, direct advantages for glucose control. While the protein source may not drastically alter overall weight loss efficacy in short-to-medium-term human trials, mechanistic studies reveal that sources like egg white and plant-protein blends can positively influence adipose tissue function and insulin dynamics. Future research and drug development should consider these nuanced interactions between diet composition, genetic background, and fundamental metabolic pathways.
Within the broader thesis on the efficacy of high-protein diets (HPDs) versus standard diets for glucose control research, a critical and often debated factor is the source of the dietary protein. While HPDs, often defined as providing >30% of energy or >1.0 g/kg/day from protein, are recognized for their potential to improve glycemic control, emerging evidence suggests that their metabolic impacts are significantly modulated by whether the protein is derived from animal or plant-based sources [27]. Furthermore, the specific context of red meat consumption presents a particular controversy, with studies linking it to increased health risks while also exploring its role in balanced dietary patterns. This guide objectively compares the experimental data on animal-based, plant-based, and mixed protein sources, with a focused examination of red meat, to inform research and development strategies in metabolic health.
Epidemiological and Clinical Evidence
Large-scale observational studies and randomized controlled trials (RCTs) provide crucial data on the long-term health outcomes associated with different dietary protein patterns.
Table 1: Association of Dietary Patterns with Type 2 Diabetes Risk from Meta-Analyses
| Dietary Pattern | Study Type | Relative Risk (RR) / Findings | Key Observations |
|---|---|---|---|
| Vegan Diet [57] | Systematic Review & Meta-Analysis | RR = 0.65 (95% CI 0.42, 1.00) | Strongest inverse association with T2D risk, though statistically imprecise. |
| Lacto-Ovo Vegetarian Diet [57] | Systematic Review & Meta-Analysis | RR = 0.68 (95% CI 0.57, 0.82) | Significant inverse association with T2D risk. |
| Healthy Plant-Based Diet (hPDI) [57] | Systematic Review & Dose-Response Meta-Analysis | RR = 0.76 (95% CI 0.69, 0.82) | Inverse, almost linear association with reduced T2D risk. |
| Unhealthy Plant-Based Diet (uPDI) [57] | Systematic Review & Dose-Response Meta-Analysis | RR = 1.13 (95% CI 0.98, 1.30) | Directly correlated with increased T2D risk. |
| High Red Meat Consumption [58] | Prospective Cohort Study | 62% higher risk (highest vs. lowest consumption) | Every additional daily serving of processed and unprocessed red meat was associated with 46% and 24% greater risk, respectively. |
| Replacing Red Meat [58] | Prospective Cohort Study | 30% lower risk (with nuts/legumes); 22% lower risk (with dairy) | Substituting one daily serving of red meat was associated with reduced T2D risk. |
| Moderate Lean Red Meat in Mixed Diet [59] | Randomized Control Trial | No adverse effects on LDL cholesterol; improved blood pressure and lipids | Up to nine 3-ounce servings of lean red meat per week within a healthy dietary pattern promoted cardiovascular health. |
Preclinical Interventional Studies
Controlled animal studies allow for precise investigation into the physiological mechanisms driven by specific protein sources.
Table 2: Metabolic Outcomes of Specific Protein Sources in a Rodent Model of Obesity
| Dietary Intervention | Model & Duration | Key Metabolic Outcomes | Interpretation |
|---|---|---|---|
| High-Casein Diet (HPcasein) [60] [61] | Obese male fa/fa Zucker rats, 8 weeks | Baseline for comparison in adipocyte size, insulin levels, and pancreatic islet size. | Animal-based milk protein served as a control. |
| High-Egg White Diet (HPegg white) [60] [61] | Obese male fa/fa Zucker rats, 8 weeks | Smaller adipocytes; Reduced fasting insulin; No pancreatic islet enlargement. | High-quality animal protein improved adipose tissue function and insulinemia. |
| High-Plant Protein Diet (HPplant: Soy+Pea) [60] [61] | Obese male fa/fa Zucker rats, 8 weeks | Smaller adipocytes; But also: Greater weight gain, elevated serum NEFA, more visceral fat; Reduced fasting insulin. | Beneficial effects on adipocytes and insulin were accompanied by less favorable fat distribution and energy metabolism. |
| Mixed Protein Diet (HPmix: Egg White+Soy+Pea) [60] [61] | Obese male fa/fa Zucker rats, 8 weeks | Smaller adipocytes; Reduced fasting insulin; No pancreatic islet enlargement. | A blend of animal and plant sources conferred benefits similar to high-quality animal protein alone. |
Detailed Experimental Protocols
To ensure reproducibility and provide insight into the generation of the data presented, this section outlines the key methodologies from the cited research.
This protocol is critical for investigating the mechanistic role of different protein sources on metabolic pathways.
- Animal Model and Group Allocation: Six-week-old male fa/fa Zucker rats (a genetic model of obesity, insulin resistance, and leptin receptor deficiency) are housed under controlled conditions (12h light/dark cycle, 25°C). After acclimation, rats are randomly assigned to experimental groups (n=8/group).
- Dietary Interventions: Groups are fed one of the following isoenergetic diets for 8 weeks:
- Normal Protein Diet (NPcasein): 15% of energy from casein.
- High-Protein Diets (35% of energy): Protein sources include casein (HPcasein), egg white protein (HPegg white), a 1:1 blend of soy and pea protein (HPplant), or a 2:1:1 blend of egg white, soy, and pea protein (HPmix). Carbohydrate is replaced isoenergetically with protein.
- In Vivo and Terminal Assessments:
- Weekly Monitoring: Body weight and food intake.
- Body Composition: Measured via EchoMRI.
- Oral Glucose Tolerance Test (OGTT): Conducted after a 5-hour fast at week 8; serum glucose and insulin are measured at baseline and post-glucose challenge.
- Tissue Collection: After euthanasia, visceral fat depots (epididymal, peri-renal, mesenteric) and pancreas are dissected, weighed, and processed.
- Histological Analysis: Epididymal adipose tissue is embedded for adipocyte size measurement. Pancreatic sections are stained (H&E) for islet size analysis.
- Serum Biochemistry: Analysis of non-esterified fatty acids (NEFA), leptin, and adiponectin via commercial immunoassays.
- Western Blotting: Assessment of adipose tissue markers for lipolysis (ATGL, HSL) and insulin signaling (Akt, AS160).
This protocol exemplifies a practical approach to studying protein ratios in a free-living population.
- Study Design: A randomized controlled trial where approximately 30 participants follow different dietary patterns over a 5-week period.
- Dietary Interventions: Participants consume healthy meals with varying types and amounts of protein.
- Protein Variables: Unprocessed lean red meat (steak, ground beef) and plant-based proteins (nuts, seeds, tofu).
- Servings per Week: The study arms include consumption of 1, 5, or 9 servings of lean red meat per week, with a corresponding inverse variation in plant-based protein servings (8, 5, or 2 servings per week). Some meals feature 50/50 ratios.
- Outcome Measures:
- Clinical Metrics: Body weight, height, and blood pressure.
- Blood Sampling: Fasting blood draws for analysis of lipid profiles (LDL cholesterol) and glucose.
Mechanisms of Action: Signaling Pathways
A primary mechanism by which high-protein diets, particularly those rich in the branched-chain amino acid (BCAA) leucine, improve glycemic control involves nutrient signaling in the brain that regulates hepatic glucose production [27].
Diagram Title: Hypothalamic Pathway of Leucine-Induced Glycemic Control
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and reagents used in the featured rodent experiment [60] [61], providing a resource for researchers aiming to replicate or build upon this work.
Table 3: Key Research Reagents for Protein Source Metabolic Studies
| Reagent / Material | Function / Application in Study | Example from Protocol |
|---|---|---|
| fa/fa Zucker Rats | A genetic model of obesity, insulin resistance, and leptin receptor deficiency, ideal for studying T2DM mechanisms. | Obtained from Charles River Laboratories. |
| Defined Protein Diets | Precisely formulated diets where the sole variable is the protein source, enabling controlled comparison. | Casein, Egg White, Soy Protein, Pea Protein (Dyets). |
| EchoMRI-700TM | Non-invasive quantitative magnetic resonance instrument for measuring whole-body fat and lean mass in live animals. | Body composition analysis. |
| OGTT Assay Kits | For measuring key metabolic biomarkers in serum during an oral glucose tolerance test. | Colorimetric assay for glucose (Megazyme); U-PLEX immunoassay for insulin (MesoScale Discovery). |
| Enzyme Colorimetric Kits | For quantifying metabolites and hormones indicative of metabolic state. | LabAssay NEFA kit (Wako) for non-esterified fatty acids. |
| U-PLEX Immunoassay Kits | Multiplexed immunoassays for sensitive and simultaneous quantification of multiple adipokines/hormones. | Measurement of leptin and adiponectin (MesoScale Discovery). |
| Histology Stains (H&E) | For morphological analysis of tissues like pancreas and adipose tissue. | Staining of pancreatic sections for islet size measurement (ScyTek). |
The evidence indicates that the efficacy of high-protein diets for glucose control is not solely a function of quantity but is profoundly influenced by protein source. Plant-based and vegetarian dietary patterns demonstrate a strong association with reduced risk of type 2 diabetes, though the quality of plant foods is paramount, as unhealthy plant-based diets can increase risk. Preclinical models suggest that both high-quality animal proteins (e.g., egg white) and blended animal-plant sources can improve adipose tissue health and insulin metrics, while some plant-only diets may present a mixed metabolic profile. The controversy around red meat is contextual; while high consumption is epidemiologically linked to diabetes, moderate intake of lean red meat within a overall healthy, plant-forward dietary pattern does not appear to adversely affect cardiovascular risk factors and may be part of an effective dietary strategy. For researchers, the key lies in designing interventions that consider not just protein quantity, but its source, quality, and the overall dietary matrix to optimize metabolic outcomes.
In the evolving landscape of metabolic disease management, the integration of High Protein Diets (HPDs) with pharmacological interventions represents a promising combinatorial approach for Type 2 Diabetes (T2D) treatment. This guide objectively compares the efficacy of HPDs against standard dietary regimens when implemented alongside established T2D management protocols. The term "HPD" in this context specifically refers to dietary interventions with elevated protein content, distinct from other medical acronyms such as HPD-101, an investigational antibody-drug conjugate for multiple myeloma [62] [63]. For researchers and drug development professionals, understanding the interplay between nutritional biochemistry and pharmacodynamics is crucial for designing holistic treatment strategies. The existing evidence suggests that dietary composition may significantly influence pharmacological efficacy, particularly for glucose-lowering medications, though the precise mechanisms require further elucidation.
Current research indicates that HPDs typically provide 40% of total caloric intake from protein sources, while normal protein diets (NPDs) contain approximately 21% protein, compared to the average American diet which provides only 14-16% protein [64]. This macronutrient manipulation forms the basis for investigating how dietary patterns can enhance conventional T2D management beyond mere caloric restriction. The rationale for combining HPDs with pharmacological treatments stems from protein's potential effects on insulin sensitivity, satiety regulation, and metabolic rate—all factors that may synergize with antidiabetic medications to improve glycemic outcomes and body composition parameters.
Experimental Comparisons: Study Design and Methodologies
Key Clinical Trial Parameters
Table 1: Comparative Overview of HPD versus NPD Clinical Trial Design
| Parameter | High Protein Diet (HPD) Group | Normal Protein Diet (NPD) Group |
|---|---|---|
| Study Duration | 52 weeks | 52 weeks |
| Participant Profile | 106 adults with T2D (80 female), BMI ≥27 kg/m², diagnosis within past 6 years | Same as HPD group |
| Dietary Composition | 40% protein, 32% carbohydrate, 28% fat | 21% protein, 53% carbohydrate, 26% fat |
| Protein Sources | ≥4 weekly servings of lean beef (only red meat source) | Exclusion of all red meat |
| Caloric Status | Energy-restricted | Energy-restricted |
| Exercise Regimen | Up to 70 minutes/day, 6 days/week | Same as HPD group |
| Weight Management Program | State of Slim (SOS) program | Modified SOS program with adjusted protein portions |
Detailed Experimental Protocol
The methodological framework for comparing HPDs with NPDs employed a rigorous randomized controlled trial (RCT) design conducted across multiple research sites [3] [64]. Participants were recruited from metropolitan areas in Denver, Colorado, and Birmingham, Alabama, with the study conducted in three sequential cohorts to ensure methodological consistency. The inclusion criteria specifically targeted adults with confirmed T2D diagnosis (within 6 years) and elevated BMI (≥27 kg/m²), while exclusion criteria eliminated individuals with HbA1c ≥12%, current eating disorders, drug/alcohol dependence, untreated hypothyroidism, insulin use, or vegetarian/vegan dietary practices.
The intervention utilized the State of Slim (SOS) weight management program, which incorporates three distinct phases with specific food lists and portion control guidance rather than calorie counting [3]. This program emphasizes five core dietary rules: (1) consuming five to six meals daily, (2) eating breakfast within one hour of waking, (3) measuring portions rather than counting calories, (4) combining one carbohydrate and one protein source at each meal, and (5) including two daily servings of healthy fats. The HPD group received specific instructions to include at least four weekly servings of lean beef as their exclusive red meat source, while the NPD group completely abstained from red meat consumption. Both groups maintained equivalent exercise regimens, gradually increasing to 70 minutes of daily activity, six days per week.
Data collection included comprehensive biometric measurements at baseline and intervention conclusion: body weight, body composition (via validated methods), hemoglobin A1c (HbA1c), fasting glucose, insulin levels, insulin resistance (HOMA-IR), blood pressure, and lipid profiles [3]. Medication changes were monitored through monthly self-reporting and communication with primary care providers. Due to COVID-19 restrictions, the originally planned in-person group classes were transitioned to an online Zoom platform, maintaining intervention fidelity while adapting to logistical constraints.
Comparative Outcomes: Efficacy Data Analysis
Primary and Secondary Endpoint Results
Table 2: Efficacy Outcomes of HPD versus NPD Interventions
| Outcome Measure | High Protein Diet (HPD) Group | Normal Protein Diet (NPD) Group | P-value |
|---|---|---|---|
| Weight Loss (kg) | -10.2 ± 1.6 kg | -12.7 ± 4.8 kg | 0.336 |
| Fat Mass Reduction | Significant decrease | Significant decrease | NSD |
| Fat Free Mass Percentage | Significant increase | Significant increase | NSD |
| HbA1c Improvement | Significant improvement | Significant improvement | NSD |
| Fasting Glucose | Significant improvement | Significant improvement | NSD |
| Insulin Sensitivity | Significant improvement | Significant improvement | NSD |
| Blood Pressure | Significant improvement | Significant improvement | NSD |
| Triglycerides | Significant improvement | Significant improvement | NSD |
NSD: No Significant Difference between groups
The comparative analysis revealed no statistically significant differences between HPD and NPD interventions across all primary and secondary endpoints [3] [64]. Both dietary approaches resulted in clinically meaningful weight loss (HPD: -10.2±1.6 kg; NPD: -12.7±4.8 kg; p=0.336) with no significant between-group difference. Similarly, improvements in body composition were comparable, with both groups demonstrating reduced fat mass and increased fat-free mass percentage. Glycemic control parameters, including HbA1c, fasting glucose, insulin levels, and insulin resistance (as measured by HOMA-IR), showed significant improvement from baseline in both groups without interventional superiority.
Cardiometabolic risk factors followed this same pattern, with both dietary strategies producing significant improvements in blood pressure and triglyceride levels without significant between-group differences [3]. The consistency of these findings across multiple metabolic parameters suggests that the achieved weight loss itself, rather than the specific macronutrient composition, drives therapeutic benefits for T2D management. This conclusion aligns with previous research such as the Diabetes Remission Clinical Trial (DiRECT), which demonstrated that weight loss of 10-15 kg can reverse T2D in recently diagnosed patients [3].
Experimental Workflow and Decision Pathway
The following diagram illustrates the experimental workflow and key decision points in comparing HPD versus NPD interventions:
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Reagents and Methodological Solutions for Metabolic Studies
| Research Tool Category | Specific Examples/Applications | Function in HPD-T2D Research |
|---|---|---|
| Body Composition Analysis | DEXA, BIA, Anthropometric measurements | Quantifies fat mass, fat-free mass changes in response to dietary interventions |
| Glycemic Control Assays | HbA1c testing, Oral Glucose Tolerance Test (OGTT), Fasting Glucose & Insulin | Measures primary T2D outcomes and insulin sensitivity improvements |
| Cardiometabolic Risk Panels | Lipid profiles (Triglycerides, HDL, LDL), Blood pressure monitoring | Assesses comprehensive cardiovascular risk modification |
| Dietary Compliance Tools | Food logs, 24-hour dietary recalls, Biomarker validation (e.g., urinary nitrogen) | Monitors adherence to prescribed macronutrient distribution |
| Physical Activity Monitoring | Accelerometers, Exercise logs, Heart rate monitors | Standardizes and quantifies exercise components across intervention groups |
| Statistical Analysis Packages | R, SPSS, SAS with mixed-effects models, intention-to-treat analysis | Handles longitudinal data, missing data, and comparative efficacy testing |
Mechanistic Insights: Metabolic Pathways in Protein-Mediated Glucose Regulation
The following diagram illustrates the potential mechanistic pathways through which high-protein diets may influence glucose regulation and how these intersect with pharmacological actions:
Research Implications and Future Directions
The comparable outcomes between HPD and NPD interventions carry significant implications for clinical practice and research methodology. For drug development professionals, these findings suggest that weight loss remains the principal determinant of T2D improvement, with dietary macronutrient composition playing a secondary role [64]. This understanding should inform the design of future combination therapies integrating pharmacological agents with dietary interventions.
Future research should explore whether specific patient subgroups (e.g., those with particular genetic polymorphisms, gut microbiota compositions, or metabolic phenotypes) demonstrate differential responses to HPDs versus NPDs when combined with specific antidiabetic medications. Additionally, longer-term studies are needed to assess the sustainability of both dietary approaches and their continued interaction with pharmacological management over extended periods. The integration of HPDs with newer drug classes such as GLP-1 receptor agonists and SGLT2 inhibitors represents a particularly promising research direction, as these medications have pronounced effects on both glycemic control and body weight.
For researchers designing similar trials, meticulous attention to dietary adherence monitoring remains crucial, as self-reported dietary intake often introduces measurement error [3]. The successful implementation of the State of Slim program, which emphasized portion control rather than calorie counting, provides a valuable methodological framework for future nutritional intervention studies. Furthermore, the multimodal assessment approach—incorporating body composition, glycemic parameters, and cardiometabolic risk factors—offers a comprehensive template for evaluating the efficacy of combined dietary and pharmacological interventions.
Challenges and Refinements: Addressing Variability, Safety, and Long-Term Efficacy
Within the context of evaluating the efficacy of high-protein diets versus standard diets for glucose control, a critical and often overlooked aspect is the significant individual variability in patient responses. While population-level data from meta-analyses can guide general recommendations, the clinical application of dietary interventions is complicated by the fact that individuals with similar baseline characteristics can exhibit dramatically different metabolic outcomes. This variability stems from a complex interplay of genetic predispositions, underlying metabolic conditions, and molecular adaptations that modulate how dietary signals are processed at the cellular and systemic levels. Understanding these factors is paramount for researchers and drug development professionals seeking to develop personalized nutrition strategies and targeted therapeutics that move beyond one-size-fits-all approaches.
The investigation into individual response variability requires a multidisciplinary approach, drawing from evidence across randomized controlled trials, mechanistic animal studies, large-scale cohort analyses, and advanced neuroimaging. This guide systematically compares key findings across these methodological domains, providing structured data, experimental protocols, and molecular pathway visualizations to equip researchers with the analytical frameworks necessary to dissect the sources of heterogeneity in dietary responses and advance the field toward more precise, effective interventions for type 2 diabetes management.
Quantitative Evidence: Comparative Data on Dietary Interventions
Table 1: Efficacy of Different Macronutrient Compositions on Glycemic and Metabolic Parameters in T2DM
| Dietary Intervention | Duration | HbA1c Change (%) | FPG Change (mmol/L) | Weight Change (kg) | LDL Change (mmol/L) | Key Findings |
|---|---|---|---|---|---|---|
| Very Low-CHO, High-Pro, Calorie-Restricted [65] | 6 months | -1.79 to -1.0 | -2.88 to -2.20 | -10.96 to -5.83 | -0.59 to -0.49 | Largest initial improvements in all parameters |
| Very Low-CHO, High-Pro, Calorie-Restricted [65] | 12 months | -1.30 to -1.25 | -1.27 to -1.21 | NS | NS | Glycemic benefits sustained at 1 year |
| Low-CHO, High-Pro, Non-Calorie-Restricted [65] | 12 months | NS | NS | -14.52 to -10.05 | NS | Most effective for long-term weight loss |
| Low-Carbohydrate Diet (LCD) [28] | 3-6 months | Significant reduction in 16/21 studies | Inconclusive overall | Variable | Not reported | Substantial short-term glycemic improvement |
| High-Protein Diet (HPD) [66] | 2-12 months | NS | NS | Variable | Significant reduction | No significant glycemic effect, but improved HOMA-IR and lipids |
| Moderate CHO, Standard Pro, Calorie-Restricted [65] | 12 months | NS | NS | NS | -0.87 | Best for long-term LDL improvement |
CHO: Carbohydrate; Pro: Protein; FPG: Fasting Plasma Glucose; NS: Not Significant
Table 2: Genetic and Metabolic Factors Contributing to Response Variability
| Factor Category | Specific Factor | Impact on Dietary Response | Evidence Source |
|---|---|---|---|
| Genetic Variants | TCF7L2 | Strongest risk gene for T2DM; affects β-cell function | [67] |
| HLA Class I/II Genes | Primary genetic risk factors for T1DM | [67] | |
| FTO | Influences obesity risk and potentially dietary weight response | [67] | |
| MTNR1B, CDKAL1, IRS1 | Associated with gestational diabetes risk | [67] | |
| Metabolic Conditions | Hypertension | Creates U-shaped protein response (optimal 12.20-15.35%E) | [68] |
| NAFLD | Linear improvement in diabetes risk with increased protein | [68] | |
| Hyperlipidemia/Central Obesity | No significant association with protein intake effect | [68] | |
| Protein Source | Animal vs. Plant | Differential effects on adipocyte size, insulinemia, pancreatic islet size | [60] |
| Egg White & Plant Mix | Reduced fasting insulin without pancreatic islet enlargement | [60] | |
| Casein | Less favorable metabolic outcomes in rodent models | [60] | |
| Neurometabolic Factors | Brain Insulin Sensitivity | Prolonged disruption after short-term overeating, affects reward signaling | [69] |
| Liver Fat Content | Rapidly increases with high-calorie diet, correlates with brain insulin response | [69] |
Experimental Protocols: Methodologies for Investigating Variability
Rodent Model of Protein Source Effects
Objective: To evaluate how different dietary protein sources in high-protein diets (HPDs) affect obesity-related metabolic markers in a genetic model of obesity [60].
Methodology Details:
- Animals: Six-week-old male fa/fa Zucker (obese) rats (n=48) with genetic leptin receptor deficiency causing obesity and insulin resistance
- Study Design: 8-week intervention with 6 experimental groups:
- Baseline group (sacrificed at start)
- NPcasein: Normal protein diet (15% energy from casein)
- HPcasein: High-protein diet (35% energy from casein)
- HPegg white: HPD with egg white protein
- HPplant: HPD with soy+pea protein (1:1 ratio)
- HPmix: HPD with egg white+soy+pea protein (2:1:1 ratio)
- Diet Composition: Protein replaced carbohydrate in HPDs while fat content remained constant across all diets
- Outcome Assessments: Oral glucose tolerance tests, EchoMRI body composition, tissue collection (visceral adipose depots, pancreas), serum biochemistry, adipocyte and pancreatic islet size quantification, adipose tissue protein analysis (lipolysis, insulin signaling, immune cell markers)
Key Findings: The source of dietary protein significantly influenced metabolic outcomes independent of weight gain. HPDs containing egg white, plant proteins, or their mixture resulted in smaller adipocytes and reduced fasting insulin without compensatory pancreatic islet enlargement compared to casein-based diets, highlighting the importance of protein quality in metabolic responses [60].
Human Cohort Analysis of Protein-Diabetes Relationship
Objective: To investigate the associations between various protein intake exposures and risk of incident type 2 diabetes in adults with or without metabolic diseases [68].
Methodology Details:
- Study Population: 29,517 residents from Shanghai Suburban Adult Cohort and Biobank without diabetes at baseline
- Follow-up: Median 5.69 years with incident T2D identified through electronic health systems
- Dietary Assessment: Validated food frequency questionnaire (FFQ) with household condiment inventory
- Statistical Analysis: Cox proportional hazard models adjusted for age, sex, family history, total energy intake, HbA1c, triglycerides, waist circumference, and hypertension
- Protein Exposure Categorization: Total protein, plant protein, animal protein, and processed food protein expressed as percentage of total energy intake (%E)
- Additional Analyses: Restricted cubic splines for non-linear relationships, propensity-score matching, subgroup analysis by metabolic diseases, and dose-response meta-analysis
Key Findings: A U-shaped association between total protein intake and T2D risk was identified, with an optimal protective range of 12.20-16.85%E and a cut-off point at 14.53%E. This relationship was modified by underlying metabolic conditions, with a narrower protective range (12.20-15.35%E) in hypertensive individuals and a linear association in those with NAFLD [68].
Molecular Mechanisms: Pathways and Systems Underlying Variability
Brain Insulin Signaling and Dietary Regulation
The brain plays a crucial role in metabolic regulation, and its responsiveness to dietary signals exhibits significant individual variability. Research demonstrates that short-term overeating with high-calorie diets can trigger prolonged disruptions in brain insulin action, even before significant weight gain occurs [69].
Figure 1: Neural Response Pathway to High-Calorie Diet
Genetic Networks in Diabetes Pathophysiology
Advancements in network pharmacology and genetic mapping have identified key gene networks that contribute to diabetes susceptibility and potentially modulate responses to dietary interventions.
Figure 2: Genetic Network in Diabetes and Complications
Adipose Tissue Remodeling and Protein Source Effects
The source of dietary protein significantly influences adipose tissue remodeling and systemic metabolism through multiple interconnected pathways.
Figure 3: Adipose Tissue Remodeling by Protein Source
Research Toolkit: Essential Reagents and Methodologies
Table 3: Essential Research Reagents and Methodological Solutions
| Category | Specific Tool/Reagent | Research Application | Key Function |
|---|---|---|---|
| Animal Models | fa/fa Zucker rats | Obesity and insulin resistance studies | Genetic leptin receptor deficiency models human metabolic disease |
| Diet Formulations | Casein-based diets | Control protein source comparison | Standardized animal protein source |
| Egg white protein diets | High-quality animal protein intervention | Low-fat, high-biological value protein | |
| Soy+pea protein mixtures | Plant protein interventions | Complementary amino acid profile | |
| Assessment Tools | EchoMRI-700TM | Body composition analysis | Non-invasive fat/lean mass quantification |
| Oral glucose tolerance test (OGTT) | Glucose homeostasis assessment | Measures insulin sensitivity and β-cell function | |
| Intranasal insulin (INI) with fMRI | Brain insulin action assessment | Non-invasive central insulin delivery with neural activity monitoring | |
| Biomarker Assays | HbA1c measurement | Long-term glycemic control | Reflects 3-month average blood glucose |
| HOMA-IR calculation | Insulin resistance index | Estimates insulin resistance from fasting measures | |
| Adipokine panels (adiponectin, leptin) | Adipose tissue function assessment | Measures adipose-derived signaling molecules | |
| CD3+/F4/80+ staining | Immune cell infiltration in adipose tissue | Quantifies T-cell and macrophage presence | |
| Molecular Biology | AMSTAR2 tool | Methodological quality assessment | Evaluates systematic review quality |
| Network meta-analysis | Comparative intervention effectiveness | Ranks multiple interventions simultaneously | |
| RNA sequencing | Transcriptomic profiling | Identifies gene expression changes |
The evidence compiled in this guide demonstrates that individual response variability to dietary interventions, particularly high-protein diets for glucose control, is not random noise but rather a scientifically tractable phenomenon with identifiable genetic, metabolic, and neurological determinants. The efficacy of any dietary approach is moderated by a complex interplay of factors including genetic background (TCF7L2, HLA genes), preexisting metabolic conditions (hypertension, NAFLD), protein source and quality (plant vs. animal, specific amino acid profiles), and neurometabolic adaptations (brain insulin sensitivity, reward pathway function).
For researchers and drug development professionals, these findings highlight the necessity of moving beyond population-level recommendations toward stratified and personalized approaches. Future research should prioritize the identification of biomarkers that predict dietary responsiveness, the development of algorithms that integrate genetic and metabolic data for personalized nutrition planning, and the design of targeted therapeutics that address the specific molecular pathways underlying poor dietary responsiveness. By accounting for the documented sources of variability, the field can advance toward more effective, personalized metabolic disease management strategies that optimize outcomes for individual patients.
For researchers and drug development professionals, understanding the long-term efficacy of nutritional interventions is paramount. While high-protein diets demonstrate significant short-term benefits for weight loss and glycemic control, their ultimate clinical value hinges on long-term sustainability. This review synthesizes current evidence on the adherence patterns and weight regain dynamics associated with high-protein diets compared to standard dietary approaches, providing a critical evidence base for designing sustainable metabolic interventions.
Comparative Efficacy of Dietary Approaches
Short-term vs. Long-term Glycemic and Weight Outcomes
Table 1: Comparative Effects of Macronutrient Compositions on Type 2 Diabetes Outcomes
| Dietary Intervention | HbA1c Reduction at 6 Months | HbA1c Reduction at 12 Months | Weight Loss at 6 Months | Weight Loss at 12 Months |
|---|---|---|---|---|
| Very low-carbohydrate, high-protein, calorie-restricted | -1.79% to -1.0% | -1.30% to -1.25% | -10.96 kg to -5.83 kg | Not sustained |
| Low-carbohydrate, high-protein, calorie-restricted | - | - | - | -10.05 kg to -14.52 kg |
| Moderate carbohydrate, standard protein, calorie-restricted | - | - | - | - |
| High-protein, low-glycemic index | - | - | - | - |
Data synthesized from network meta-analysis of 80 RCTs with 9,232 patients [65]
The comparative effectiveness of macronutrient compositions reveals a significant time-dependent efficacy pattern. Very low-carbohydrate, high-protein diets demonstrate potent initial effects but show diminished returns over longer durations. Specifically, while these diets achieved the greatest reduction in HbA1c (range of mean difference: -1.79% to -1.0%) and weight (-10.96 kg to -5.83 kg) at the 6-month follow-up, the weight loss effect was not sustained at 12 months, though HbA1c reduction remained significant (-1.30% to -1.25%) [65].
For sustained weight loss maintenance at 12 months, a low-carbohydrate, high-protein diet (without severe carbohydrate restriction) probably represents the most effective approach (range of mean difference: -10.05 kg to -14.52 kg) [65]. This suggests that milder carbohydrate restriction may offer better long-term adherence for weight management while maintaining the benefits of higher protein intake.
Long-term Prediabetes Remission Outcomes
Table 2: PREVIEW Trial: 3-Year Prediabetes Remission and Weight Maintenance
| Outcome Measure | High-Protein, Low-GI Diet (25% protein, GI<50) | Moderate-Protein, Moderate-GI Diet (15% protein, GI>56) | Risk Ratio (95% CI) |
|---|---|---|---|
| Prediabetes Remission at 1 Year | 20.7% | 26.3% | RR 1.26 (1.04, 1.53) |
| Prediabetes Remission at 3 Years | 15.5% | 20.6% | RR 1.26 (1.06, 1.50) |
| ≥8% Weight Loss Maintenance at 1 Year | 57.3% | 54.0% | Not significant |
| ≥8% Weight Loss Maintenance at 3 Years | 30.4% | 31.4% | Not significant |
Data from PREVIEW randomized multinational trial (n=1,856) [70]
The PREVIEW trial, a 3-year multinational study, provides critical insights into long-term sustainability. Contrary to expectations, the moderate-protein, moderate-GI diet achieved significantly higher prediabetes remission rates at both 1 year (26.3% vs. 20.7%) and 3 years (20.6% vs. 15.5%) compared to the high-protein, low-GI diet [70].
Notably, these differences in remission rates were independent of weight changes, as both groups maintained similar weight loss maintenance at 1 year (54.0% vs. 57.3%) and 3 years (31.4% vs. 30.4%) [70]. This suggests that the benefits of the moderate-protein diet for glucose regulation extend beyond mere weight management and may relate to better long-term adherence and metabolic adaptation.
Mechanisms Underlying Sustainability Challenges
Metabolic and Behavioral Adaptation Pathways
The sustainability challenges of restrictive dietary patterns like high-protein diets involve complex physiological and behavioral adaptations. The following diagram illustrates the primary pathways contributing to weight regain and adherence issues:
This diagram illustrates the primary pathways through which metabolic and behavioral factors contribute to the sustainability challenges of high-protein diets. The mechanisms include:
Metabolic Adaptations: Resting metabolic rate (RMR) reduction and adaptive thermogenesis can decrease daily energy expenditure by up to 142 kcal/day during weight loss, creating a physiological environment predisposing to weight regain [71].
Hormonal Changes: Alterations in leptin, ghrelin, and other appetite-regulating hormones increase hunger and cravings, directly challenging long-term adherence [71].
Behavioral Factors: Dietary monotony, social restrictions, and practical challenges of maintaining high-protein intake patterns contribute to declining adherence over time [71] [70].
Protein Distribution and Body Composition
The timing and distribution of protein intake has been hypothesized to influence fat-free mass preservation during weight loss, potentially affecting long-term metabolic rate and weight maintenance sustainability. However, recent evidence challenges this assumption:
Experimental Protocol: A randomized parallel feeding study investigated whether daily dietary protein distribution pattern during energy restriction influences changes in body composition in women of reproductive age [72].
Methodology:
- Participants: 43 healthy women (age 20-44 y, BMI 28-45 kg/m²)
- Intervention: 8-week controlled 20% energy restriction (all foods provided) followed by 8-week self-choice phase
- Groups: Even protein distribution across meals (n=21) vs. skewed distribution with most protein consumed at evening meal (n=22)
- Measurements: Body composition via DEXA at baseline, week 8, and week 16
Findings: No significant main effects of group or group-by-time interactions were observed for fat-free mass preservation. All measures exhibited main effect of time only, with overall decreases in body weight (-5.6 ± 0.4 kg), fat-free mass (-1.0 ± 0.2 kg), and fat mass (-4.6 ± 0.4 kg) [72]. This suggests that daily dietary protein distribution at a fixed protein level does not significantly influence body composition changes during weight loss.
Research Reagent Solutions Toolkit
Table 3: Essential Research Materials and Methodologies for Dietary Sustainability Studies
| Reagent/Methodology | Function/Application | Key Characteristics |
|---|---|---|
| Dual-Energy X-ray Absorptiometry (DEXA) | Body composition assessment | Quantifies fat mass, lean mass, and bone density changes during interventions [72] |
| Continuous Glucose Monitoring (CGM) | Glycemic variability assessment | Provides continuous glucose data without fingersticks; essential for diabetes remission studies [27] |
| Indirect Calorimetry | Metabolic rate measurement | Precisely measures resting metabolic rate and substrate utilization [71] |
| Life Cycle Assessment (LCA) | Environmental impact quantification | Standardized method (ISO) for modeling environmental impact of dietary patterns [73] |
| Validated Food Frequency Questionnaires (FFQ) | Dietary adherence measurement | Assesses compliance to specific macronutrient distributions in long-term trials [65] [70] |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Hormone and biomarker quantification | Measures appetite regulators (leptin, ghrelin), insulin, and other metabolic markers [74] |
The long-term sustainability of high-protein diets reveals a complex interplay between potent short-term physiological effects and challenging long-term behavioral adherence. While high-protein, low-carbohydrate approaches demonstrate significant initial efficacy for weight loss and glycemic control, milder dietary modifications may offer superior long-term sustainability for prediabetes remission and weight maintenance.
The evidence suggests that for drug development professionals targeting metabolic diseases, consideration of adherence patterns and weight regain dynamics should inform both pharmacological and behavioral intervention design. The optimal approach may involve combining the initial metabolic advantages of higher-protein diets with more moderate, sustainable dietary patterns for long-term disease management, potentially enhanced by pharmacological agents that target the physiological drivers of weight regain.
The management of diabetes through dietary intervention, particularly with high-protein diets (HPDs), presents a complex risk-benefit profile. While substantial evidence demonstrates the efficacy of HPDs for glycemic control, their application in diabetic populations necessitates a rigorous assessment of nephrotoxicity risks. Diabetic kidney disease (DKD) is a major microvascular complication, affecting 30–40% of patients with diabetes and serving as the leading cause of end-stage renal disease (ESRD) worldwide [75]. The pathophysiological interplay between diabetes-induced renal damage and dietary protein intake creates a critical therapeutic challenge. This review systematically evaluates the renal safety profile of high-protein nutritional strategies against standard diets within a context of glucose control research, providing researchers and drug development professionals with a comparative analysis of experimental data, mechanistic insights, and clinical recommendations.
Pathophysiology of Diabetic Kidney Disease
The development and progression of DKD are driven by multiple interconnected pathological pathways. Understanding these mechanisms is fundamental to assessing how dietary protein influences renal safety in diabetic populations.
Hemodynamic and Metabolic Pathways
Persistent hyperglycemia initiates a cascade of hemodynamic and metabolic alterations within the kidney. Chronically elevated blood glucose increases glomerular pressure and causes afferent arteriolar dilation, leading to glomerular hyperfiltration and an elevated glomerular filtration rate (GFR) [75]. This hemodynamic stress activates several vasoactive systems, including the renin-angiotensin-aldosterone system (RAAS), and triggers metabolic pathways involving protein kinase C (PKC), polyol flux, and advanced glycation end-product (AGE) formation [75]. Angiotensin II, a key effector of RAAS, promotes efferent arteriolar vasoconstriction, further exacerbating intraglomerular pressure and hyperfiltration, ultimately resulting in glomerular and tubular injury [75].
Oxidative Stress and Inflammation
Oxidative stress is a critical mediator in DKD pathogenesis [75]. Chronic hyperglycemia disrupts the pro-oxidant/antioxidant balance, leading to overproduction of reactive oxygen species (ROS) via upregulated NADPH oxidases (NOX4 and NOX5) and impaired antioxidant defense mechanisms [75]. This oxidative environment stimulates the production of pro-inflammatory cytokines and activation of transcription factors like NF-κB, driving renal inflammation through recruitment of monocytes and macrophages and expression of cytokines (e.g., IL-1, IL-6, TNF-α) and chemokines (e.g., MCP-1) [75]. These processes collectively promote the structural hallmarks of DKD, including mesangial expansion, glomerulosclerosis, basement membrane thickening, and tubulointerstitial fibrosis [75].
The following diagram illustrates the core pathways involved in the pathophysiology of Diabetic Kidney Disease.
Comparative Analysis of Dietary Interventions
High-Protein Diets and Specialized Formulas
Recent clinical investigations have evaluated the efficacy and renal safety of high-protein, diabetes-specific nutritional formulas (DSNF-Pro). A 2025 open-label, crossover trial in subjects with prediabetes demonstrated that DSNF-Pro (providing 12g protein per serving) significantly improved glycemic control by reducing postprandial glucose incremental area under the curve (iAUC) by 73.4% compared to a standard nutritional formula (STNF, providing 4.9g protein) [24]. This improvement occurred without increasing insulin secretion, suggesting enhanced insulin sensitivity [24]. The DSNF-Pro was characterized by higher protein and fat content, with monounsaturated fatty acids (MUFA) comprising 60% of total fat, and contained low-glycemic index carbohydrates and dietary fiber [24].
A separate 2024 systematic review of HPDs (>30% total energy or >1.0 g/kg/day) in Type 2 Diabetes Mellitus (T2DM) concluded that such diets effectively reduce hyperglycemia, potentially through branched-chain amino acid (leucine)-mediated signaling in the medio-basal hypothalamus, which increases hepatic insulin sensitivity [27]. The review noted that Paleolithic diets, featuring higher-quality protein sources and exclusion of grains, dairy, and refined foods, appeared particularly beneficial [27].
Alternative Dietary Patterns
Research on other dietary patterns reveals additional options for glycemic and renal management. The Dietary Approaches to Stop Hypertension (DASH) diet, when modified for diabetes (DASH4D) with lower carbohydrate content and adjusted potassium, demonstrated significant benefits in a controlled feeding trial [76]. Participants with T2DM following DASH4D experienced an average blood glucose reduction of 11 mg/dL and spent an additional 75 minutes daily within optimal glucose range, without increased hypoglycemia risk [76].
Low-carbohydrate diets (LCDs), typically defined as <130g carbohydrate daily (<26% total energy), have also shown efficacy. A 2025 umbrella meta-analysis confirmed that LCDs significantly reduce HbA1c in the short term and improve insulin sensitivity, though long-term sustainability remains challenging [28]. For Type 1 diabetes, a systematic review found that carbohydrate-restricted diets (≤45% energy) increased time-in-range and reduced insulin needs, but did not significantly affect HbA1c [77].
Renal Outcomes with Protein Restriction
For patients with established CKD, evidence supports dietary protein restriction. A 10-year retrospective cohort study published in 2025 found that T2DM patients with CKD (stages 1-4) following a restricted protein diet (≤1.0 g/kg/day) experienced improved prognosis and delayed progression to composite endpoints (dialysis, ESRD, transplant, creatinine doubling, cardiovascular events) [78]. In advanced CKD (stages 3-4), more intensive restriction (<0.8 g/kg/day) provided significant benefit [78]. These findings align with a systematic review of international guidelines, which recommends protein intake of 0.8 g/kg/day for diabetic patients with non-dialysis-dependent CKD, though some guideline discrepancies exist [79].
Table 1: Comparative Effects of Dietary Interventions on Glycemic and Renal Parameters
| Dietary Intervention | Patient Population | Glycemic Effects | Renal Effects | Key Clinical Evidence |
|---|---|---|---|---|
| High-Protein Diabetes-Specific Formula (DSNF-Pro) | Prediabetes | ↓ Postprandial glucose iAUC by 73.4% [24] | No significant difference in insulin iAUC; no renal safety data reported [24] | Open-label, crossover trial (N=15) [24] |
| High-Protein Diet (>1.0 g/kg/day or >30% energy) | T2DM | ↓ HbA1c, ↓ FPG via leucine-mediated CNS signaling [27] | Potential exacerbation of hyperfiltration; long-term renal safety concerns [27] [78] | Systematic review of clinical studies [27] |
| Restricted Protein Diet (≤1.0 g/kg/day) | T2DM with CKD | Not primary outcome | ↓ Composite endpoint risk (dialysis, ESRD, creatinine doubling) [78] | 10-year retrospective cohort (N=820) [78] |
| Intensive Protein Restriction (<0.8 g/kg/day) | T2DM with CKD Stages 3-4 | Not primary outcome | Significantly improved composite endpoints [78] | 10-year retrospective cohort [78] |
| Modified DASH Diet (DASH4D) | T2DM | ↓ Average glucose by 11 mg/dL, ↑ 75 min/day in range [76] | Lowered potassium for CKD safety; no adverse renal effects reported [76] | Randomized crossover trial (N=89) [76] |
| Low-Carbohydrate Diet (<130g/day) | T2DM | ↓ HbA1c short-term, ↑ insulin sensitivity [28] | Individual variability; not specifically reported [28] | Umbrella meta-analysis (21 studies) [28] |
Experimental Models and Methodologies
Clinical Trial Designs and Protocols
The evidence base for renal safety assessment derives from diverse methodological approaches. Recent clinical trials have employed sophisticated designs to isolate dietary effects:
Crossover Clinical Trials: The DASH4D study utilized a randomized crossover design where participants served as their own controls, consuming both experimental and standard diets during different periods [76]. This approach enhances statistical power by reducing inter-individual variability and allows for detection of meaningful treatment effects even with moderate sample sizes.
Open-Label Cross-Over Designs: The DSNF-Pro trial employed an open-label, cross-over methodology where all subjects received both the intervention (DSNF-Pro) and control (standard nutritional formula) in sequence, with a washout period of 1-14 days between interventions [24]. This design efficiently compares interventions within the same population.
Long-Term Retrospective Cohort Studies: The 10-year retrospective analysis of protein restriction in T2DM with CKD employed propensity score matching to create balanced comparison groups from real-world clinical data, enhancing the validity of observational findings [78].
Renal Function Assessment Methods
Comprehensive renal safety profiling in these studies incorporates multiple assessment modalities:
Glomerular Filtration Rate (GFR) Monitoring: Estimated GFR (eGFR) calculated from serum creatinine serves as the primary metric for renal function staging and progression tracking [78] [80].
Urinary Biomarkers: Albuminuria assessment via urine albumin-to-creatinine ratio (UACR) provides a sensitive indicator of glomerular damage [78].
Serum-Based Protein Intake Estimation: The DPIsUCR method estimates dietary protein intake based on serum urea creatinine ratio, validated against the gold-standard Maroni method (Pearson's r = 0.786) [78]. This approach leverages the principle that over 90% of protein-derived nitrogen is metabolized to urea and excreted renally.
Composite Endpoints: Studies frequently employ composite endpoints incorporating both hard outcomes (dialysis initiation, renal transplant, death) and surrogate markers (serum creatinine doubling, progression to ESRD) to comprehensively capture disease progression [78].
Table 2: Key Methodologies for Renal Safety Assessment in Dietary Interventions
| Assessment Method | Measured Parameters | Utility in Renal Safety profiling | Example Application |
|---|---|---|---|
| Estimated GFR (eGFR) | Serum creatinine-based calculation | Primary renal function assessment; CKD staging | Risk stratification in T2DM/CKD cohorts [78] [80] |
| Urinary Albumin-to-Creatinine Ratio (UACR) | Urinary albumin and creatinine | Early marker of glomerular damage | Inclusion criterion for CKD diagnosis [78] |
| Serum Urea Creatinine Ratio (sUCR) | Blood urea nitrogen and creatinine | Estimation of dietary protein intake (DPIsUCR) | Protein intake assessment in retrospective cohorts [78] |
| Continuous Glucose Monitoring (CGM) | Mean glucose, time-in-range, glycemic variability | Assessment of glycemic control without frequent phlebotomy | DASH4D trial [76] |
| Composite Renal Endpoints | Dialysis initiation, ESRD, transplant, creatinine doubling | Comprehensive capture of disease progression | Primary outcome in long-term cohort studies [78] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Diabetic Nephropathy Research
| Research Tool | Specific Application | Experimental Function | Representative Use |
|---|---|---|---|
| Enzymatic Colorimetric Glucose Oxidase Assay | Plasma glucose quantification | Measures glucose concentrations in blood samples | Arkray GA-1171 kit [24] |
| Radioimmunoassay (RIA) | Insulin and C-peptide measurement | Quantifies hormone levels using radioactive labeling | Izotop RK-400CT insulin RIA; Beckman Coulter C-peptide IRMA kit [24] |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Cytokine/protein biomarker detection | Quantifies specific proteins in serum, plasma, or urine | Inflammatory cytokine assessment (IL-1, IL-6, TNF-α, MCP-1) [75] |
| Continuous Glucose Monitoring (CGM) Systems | Ambulatory glucose profiling | Tracks interstitial glucose levels in free-living conditions | Abbott Diabetes Care CGM in DASH4D trial [76] |
| Urinary Albumin/Creatinine Assays | Albuminuria assessment | Measures kidney damage through urinary protein leakage | CKD diagnosis and monitoring [78] |
| Serum Urea Nitrogen (BUN) Test | Renal function assessment | Evaluates urea nitrogen as marker of renal filtration | DPIsUCR calculation for protein intake estimation [78] |
The renal safety profile of dietary interventions in diabetic populations necessitates careful consideration of disease stage and individual risk factors. High-protein diets and specialized nutritional formulas demonstrate significant efficacy for glycemic control in prediabetes and early-stage T2DM, potentially through multiple mechanisms including hypothalamic signaling and incretin effects [24] [27]. However, in established diabetic kidney disease, protein restriction to ≤1.0 g/kg/day (with more intensive restriction to <0.8 g/kg/day in advanced CKD) provides clear renoprotective benefits, delaying progression to composite endpoints including dialysis and ESRD [78]. Alternative approaches like the modified DASH4D diet offer promising strategies for concurrent glycemic and blood pressure control without exacerbating renal risk [76]. Future research should prioritize long-term, prospective trials with standardized renal safety endpoints to optimize personalized nutritional strategies across the spectrum of diabetic renal disease.
The role of dietary protein in metabolic health extends beyond mere quantity, with increasing scientific evidence pointing to the critical importance of protein source. Within the broader thesis on the efficacy of high-protein diets versus standard diets for glucose control research, understanding how different protein types—animal versus plant—differentially influence metabolic parameters is fundamental for developing targeted nutritional strategies. This review synthesizes current evidence from interventional and observational studies to compare how various protein sources modulate outcomes including glucose metabolism, body composition, lipid profiles, and vascular function. The findings provide crucial insights for researchers, scientists, and drug development professionals seeking to develop evidence-based dietary recommendations and nutritional therapeutics for metabolic disease management.
Table 1: Acute Postprandial Effects of Animal vs. Plant Protein Sources
| Metabolic Parameter | Animal Protein Effects | Plant Protein Effects | Study Details |
|---|---|---|---|
| Energy Expenditure | Higher diet-induced thermogenesis (DIT) [81] | Lower DIT compared to animal protein [81] | Acute RCT in overweight/obese men [81] |
| Appetite Response | Potentially greater satiating effects [81] | Potentially less satiating effects [81] | Acute RCT in overweight/obese men [81] |
| Postprandial Lipemia | Lower triglyceride levels [81] | Higher triglyceride levels compared to animal protein [81] | Acute RCT in overweight/obese men [81] |
| Arterial Stiffness | Under investigation (PWV, PWA) [81] | Under investigation (PWV, PWA) [81] | Acute RCT measuring vascular function [81] |
Table 2: Long-Term Metabolic Effects of Different Protein Sources in Weight Loss Interventions
| Metabolic Parameter | High-Protein Diet (Incl. Red Meat) | Normal-Protein Diet (No Red Meat) | Study Details |
|---|---|---|---|
| Weight Loss | -10.2 ± 1.6 kg [3] | -12.7 ± 4.8 kg (p=0.336) [3] | 52-week RCT in T2D patients [3] |
| HbA1c Improvement | Significant improvement [3] | Significant improvement, no between-group difference [3] | 52-week RCT in T2D patients [3] |
| Body Composition | Reduced fat mass, increased fat-free mass % [3] | Reduced fat mass, increased fat-free mass % [3] | 52-week RCT in T2D patients [3] |
| Fasting Glucose | Improved [3] | Improved, no between-group difference [3] | 52-week RCT in T2D patients [3] |
| Insulin Resistance | Improved (HOMA-IR) [3] | Improved, no between-group difference [3] | 52-week RCT in T2D patients [3] |
Table 3: Longitudinal Associations Between Protein Sources and Metabolic Syndrome Risk
| Protein Source | Hazard Ratio/Risk Association | Confidence Intervals | Population |
|---|---|---|---|
| Total Protein | OR 0.83 (per additional weekly serving) [82] | 95% CI 0.81-0.85 [82] | Iranian adults (11.25-year follow-up) [82] |
| Animal Protein | OR 0.80 (per additional weekly serving) [82] | 95% CI 0.77-0.83 [82] | Iranian adults (11.25-year follow-up) [82] |
| Plant Protein | OR 0.70 (per additional weekly serving) [82] | 95% CI 0.64-0.76 [82] | Iranian adults (11.25-year follow-up) [82] |
| Red Meat | OR 0.74 (per additional weekly serving) [82] | 95% CI 0.70-0.78 [82] | Iranian adults (11.25-year follow-up) [82] |
| Processed Meat | OR 0.96 (per additional weekly serving) [82] | 95% CI 0.87-1.01 [82] | Iranian adults (11.25-year follow-up) [82] |
Key Biological Mechanisms and Pathways
Amino Acid Sensing and Metabolic Regulation
The mechanistic target of rapamycin complex 1 (mTORC1) serves as a crucial nutrient sensor that is differentially activated by various amino acids present in dietary proteins. Branched-chain amino acids (BCAAs), particularly leucine, which is more abundant in animal proteins, bind to Sestrin-2 and promote mTORC1 activation by disrupting the Sestrin-2-GATOR2 interaction [83]. Similarly, arginine activates mTORC1 by preventing the interaction between CASTOR1 and GATOR2 [83]. Activated mTORC1 promotes protein synthesis and inhibits autophagy, while restriction of protein and specific amino acids suppresses mTORC1 activity, potentially benefiting metabolic health and longevity [83].
Figure 1: mTORC1 Activation by Amino Acids from Dietary Protein
Methionine Metabolism and Hepatic Signaling
Methionine, predominantly found in animal proteins, significantly influences metabolic regulation through its conversion to S-adenosylmethionine (SAM). Elevated methionine intake increases SAM levels, which inhibits autophagy through methylation of protein phosphatase 2A (PP2A) and activates mTORC1 via SAMTOR, creating a synergistic effect that may accelerate metabolic aging [83]. Conversely, methionine restriction activates fibroblast growth factor 21 (FGF21), an endocrine hormone that improves glucose control, lipid homeostasis, and energy expenditure [83]. The differential methionine content between animal and plant proteins may partially explain their varying metabolic effects.
Figure 2: Methionine Metabolism Pathways in Metabolic Regulation
Detailed Experimental Protocols
Acute Postprandial Metabolic Response Assessment
Objective: To evaluate the acute effects of dietary protein sources (animal-based vs. plant-based) on appetite response, energy metabolism, and arterial stiffness in overweight and obese men [81].
Study Design:
- Type: Acute randomized crossover clinical trial
- Participants: 46 healthy overweight and obese men (aged 18-60 years, BMI 25-35 kg/m²)
- Interventions: Two isocaloric high-protein breakfast meals with different protein sources:
- Animal-based protein (AP)
- Plant-based protein (PP)
- Washout Period: 1 week between interventions [81]
Methodological Details:
- Pre-test Conditions: Participants abstained from food, drinks (except water), alcohol, and caffeine for 12 hours prior to testing. No severe physical activity within 48 hours before test days.
- Test Day Protocol: Participants arrived at the research center at 7 a.m. via taxi to minimize physical activity. Anthropometric measurements were taken, and an intravenous catheter was inserted into an antecubital vein.
- Baseline Measurements: Fasting assessments of indirect calorimetry, pulse wave velocity (PWV) and pulse wave analysis (PWA) for arterial stiffness, subjective appetite, and venous blood collection.
- Meal Consumption: Participants consumed test meals within 15 minutes under researcher supervision.
- Postprandial Monitoring: Continuous monitoring for 6 hours postprandially, with repeated measurements of all parameters [81].
Primary Outcomes: Appetite response, energy metabolism parameters (resting metabolic rate, diet-induced thermogenesis, substrate oxidation), and arterial stiffness indices (PWV, PWA). Secondary Outcomes: Changes in lipemia, glycemia, and insulinemia [81].
Long-Term Weight Loss and Metabolic Improvement Trial
Objective: To compare a high-protein diet including red meat versus a normal-protein diet without red meat for weight loss, body composition changes, and glucose control in individuals with type 2 diabetes [3].
Study Design:
- Type: 52-week randomized controlled trial
- Participants: 106 adults (80 female) with type 2 diabetes (diagnosis within past 6 years), BMI ≥27 kg/m², weight stable (±3 kg in past 3 months)
- Interventions:
- High-protein (HP) diet: 40% protein, 32% carbohydrate, 28% fat, with ≥4 weekly servings of lean beef
- Normal-protein (NP) diet: 21% protein, 53% carbohydrate, 26% fat, excluding red meat
- Weight Management Program: Both groups followed the State of Slim (SOS) program with phased dietary approaches and progressive exercise up to 70 minutes daily, 6 days/week [3].
Methodological Details:
- Dietary Compliance: Participants received customized food lists with defined portion sizes. The SOS program emphasized five rules: eating 5-6 times daily, breakfast within 1 hour of waking, portion measurement instead of calorie counting, specific protein-carbohydrate combinations at each meal, and twice-daily healthy fat consumption.
- Data Collection: Body weight, body composition (DXA), hemoglobin A1c, fasting glucose, insulin, lipid profile, and blood pressure measured at baseline and 52 weeks.
- Statistical Analysis: Between-group differences analyzed using appropriate statistical methods with significance set at p<0.05 [3].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials for Protein-Metabolism Studies
| Reagent/Equipment | Specific Application | Research Function |
|---|---|---|
| Indirect Calorimetry | Energy expenditure measurement [81] | Quantifies resting metabolic rate, diet-induced thermogenesis, and respiratory quotient |
| Pulse Wave Velocity (PWV) | Arterial stiffness assessment [81] | Gold standard method for measuring vascular function and cardiovascular risk |
| Dual-Energy X-ray Absorptiometry (DXA) | Body composition analysis [84] | Precisely measures visceral adipose tissue, lean mass, and fat mass distribution |
| Casein and Whey Protein Mix | Protein supplementation [84] | Standardized animal protein source for interventional studies |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Metabolic hormone quantification [84] | Measures insulin, leptin, adiponectin, and inflammatory markers |
| Mixed-Meal Tolerance Test | Postprandial metabolism assessment [81] | Evaluates metabolic responses to controlled nutrient challenges |
| Validated Food Frequency Questionnaire (FFQ) | Dietary intake assessment [82] | Captures habitual protein consumption patterns from different sources |
| Mixed-Effects Regression Models | Statistical analysis of longitudinal data [82] | Accounts for within-subject correlations in crossover and repeated-measures designs |
The efficacy of high-protein diets for glucose control presents a complex paradox. Short-term studies consistently demonstrate significant benefits for weight loss and glycemic improvement, whereas emerging evidence suggests that chronic, high-level intake may activate counter-regulatory mechanisms that promote insulin resistance. This analysis examines the experimental data supporting both facets of this phenomenon, providing researchers and drug development professionals with a comparative evaluation of outcomes, methodologies, and underlying molecular pathways.
The broader thesis on dietary efficacy must reconcile findings from network meta-analyses, which show that very low-carbohydrate, high-protein, calorie-restricted diets have the greatest effect on reducing HbA1c at 6 months [85], with molecular studies indicating that chronic elevations of certain amino acids can blunt insulin signaling [36]. The context of energy intake appears critical, as these detrimental effects are often observed in the setting of hypercaloric regimens or nutrient overload.
Table 1: Efficacy Outcomes of High-Protein Diets in Clinical Trials
| Study Focus | Intervention Details | Key Efficacy Findings | Potential Adverse Metabolic Findings |
|---|---|---|---|
| Macronutrient Composition & T2D Management [85] | Very Low-Carbohydrate, High-Protein, Calorie-Restricted Diet | HbA1c reduction: -1.0% to -1.79% (6 months); Weight loss: -5.83 kg to -10.96 kg (6 months) [85] | LDL cholesterol reduction was less effective vs. other diets at 12-month follow-up [85] |
| Protein Source in Hypocaloric Diets [86] | Low-Calorie, High-Protein (35% TCV), Animal vs. Plant Source (6 months) | Weight loss: -8.05 kg (Animal) & -7.70 kg (Plant); Improved body composition, glucose metabolism, and lipid profiles [86] | No significant difference in cardiometabolic improvements between animal and plant protein sources [86] |
| Protein Quantity in Hypocaloric Diets [64] | High-Protein (40%) vs. Normal-Protein (21%) Diet (52 weeks) | Both diets effectively improved glucose control and body composition; Weight loss itself was the primary factor [64] | Avoiding red meat provided no additional benefit for weight loss or blood sugar control [64] |
| Eucaloric Protein Restriction [87] | Low-Protein Diet (meeting minimum requirements) for 5 weeks | --- | Increased energy intake required to maintain weight (19-21%); Fasting plasma FGF21 increased by 208-361% [87] |
Table 2: Molecular and Hormonal Responses in Preclinical and Human Studies
| Experimental Context | Observed Metabolic Adaptations | Implicated Mediators & Mechanisms |
|---|---|---|
| Postprandial EAA Elevation [36] | Promotes muscle protein synthesis; Maintains skeletal muscle mass (major site of glucose disposal) [36] | Leucine-induced, transient activation of mTORC1; Anabolic signaling [36] |
| Chronic Postabsorptive BCAA Elevation [36] | Associated with pathogenesis of insulin resistance [36] | Chronic mTOR activation; Impaired insulin action; Reliant on concurrent hyperinsulinemia and nutrient overload fostering lipotoxicity [36] |
| Dietary Protein Restriction [87] | Increased energy expenditure; Enhanced insulin sensitivity in mice; Elevated FGF21 in humans [87] | FGF21-mediated mitochondrial adaptations in white adipose tissue; Altered electron transport chain components [87] |
Detailed Experimental Protocols
To enable replication and critical evaluation, the methodologies from several key studies are outlined below.
Network Meta-Analysis on Macronutrient Composition [85]: This analysis included 80 randomized controlled trials (RCTs) with 9,232 T2D patients. Diets were classified by carbohydrate intake (Very Low: ≤10% or 50g/d; Low: 11-26%; Moderate: 26-45%; High: >45%) and protein intake (Standard: <15%; Moderate: 15-25%; High: >25%). A Bayesian framework with random-effects models was used to calculate mean differences (MD) and 95% credible intervals (CrI) for outcomes like HbA1c, body weight, and LDL cholesterol at 6 and 12 months. The certainty of evidence was rated using the GRADE approach [85].
Randomized Controlled Trial on Protein Sources [86]: This 6-month dietary intervention involved 117 participants with overweight/obesity and prediabetes or T2D. Participants were randomized to one of two hypocaloric, high-protein (35% of calories) diets where 75% of the protein was from either animal (HPA) or plant (HPP) sources. The remaining macronutrients were fixed (30% fat, 35% carbohydrates). Body composition was assessed via DEXA, and glucose metabolism was evaluated using HOMA-IR and HbA1c. Dietary adherence was monitored via 3-day weighed food records [86].
Eucaloric Dietary Intervention on Protein Restriction [87]: In this study, healthy, lean men consumed a eucaloric, low-protein diet for 5 weeks, followed by a 5-week return to their habitual higher-protein diet. The low-protein diet was designed to meet minimum requirements, with the protein deficit replaced by either carbohydrates (LPHC) or fat (LPHF). Energy intake was precisely adjusted to maintain body weight. Fasting plasma FGF21 was measured, and proteomic analysis of white adipose tissue was performed. Mechanistic follow-up used wild-type and FGF21-knockout mice [87].
Hyperinsulinemic-Hypoglycemic Clamp Study [88]: This study enrolled 25 men newly diagnosed with T2D. After achieving glycemic control via insulin pump therapy, participants underwent a hyperinsulinemic-hypoglycemic clamp. Insulin was infused at a fixed rate, and blood glucose was lowered to <2.8 mmol/L for 30 minutes. Blood samples were drawn at euglycemia and hypoglycemia to measure counter-regulatory hormones (ACTH, GCG, GH, Cor). This protocol assessed the integrity of the counter-regulatory response [88].
Signaling Pathways and Molecular Mechanisms
The paradoxical effects of dietary protein on insulin sensitivity are governed by several key signaling pathways, integrating energy status, hormonal signals, and substrate metabolism.
Diagram: Amino Acid Sensing and Metabolic Fate in Insulin Sensitivity
Title: Amino Acid Fate Dictates Metabolic Outcomes
The diagram illustrates the critical role of metabolic context. Acute postprandial elevations of essential amino acids (EAAs), particularly leucine, promote anabolic signaling and metabolic health. In contrast, chronic postabsorptive elevations, often linked to nutrient overload, can lead to insulin resistance. Separately, protein restriction triggers a distinct endocrine pathway mediated by FGF21 to enhance energy expenditure [36] [87].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Assays for Investigating Diet-Induced Metabolic Pathways
| Reagent / Assay | Primary Function / Application | Experimental Context |
|---|---|---|
| Hyperinsulinemic-Euglycemic Clamp | Gold-standard method for quantifying whole-body insulin sensitivity [36] [88] | Assessing peripheral glucose disposal in response to dietary interventions [36] |
| Hyperinsulinemic-Hypoglycemic Clamp | Provokes controlled hypoglycemia to assess counter-regulatory hormone response (GCG, ACTH, Cor, GH) [88] | Evaluating HPA axis and hormonal counter-regulation in obesity/T2D [88] |
| Plasma FGF21 Measurement (e.g., Chemiluminescent Immunoassay) | Quantifies circulating levels of FGF21, a key hepatokine induced by protein restriction and low-carbohydrate diets [87] | Mechanistic studies on energy expenditure and mitochondrial adaptation [87] |
| Dual-Energy X-ray Absorptiometry (DEXA) | Precisely measures body composition (fat mass, lean mass, visceral fat) [86] | Evaluating changes in body composition during weight loss diets [86] |
| Indirect Calorimetry | Measures respiratory exchange ratio (RER) and whole-body metabolic rate [87] | Determining substrate utilization (carbs vs. fats) and energy expenditure [87] |
| Western Blot / Proteomic Analysis (e.g., of white adipose tissue) | Detects protein expression and phosphorylation of key signaling molecules (mTOR, PGC-1α, SIRT1) [36] [87] | Elucidating molecular mechanisms in tissue-specific metabolic adaptations [87] |
The relationship between high-protein diets and glucose control is not monolithic but is fundamentally shaped by dosage, temporal pattern, overall energy balance, and the individual's metabolic health. The compelling short-term efficacy of high-protein, hypocaloric diets for T2D management is well-supported [85] [86] [64]. However, a complete efficacy thesis must incorporate the potential for counter-regulatory effects, where chronic high intake, particularly in an environment of energy surplus, may engage pathways like sustained mTOR activation and lipotoxicity that can paradoxically induce insulin resistance [36]. The FGF21 response to low protein intake further highlights the body's complex hormonal regulation of energy balance in response to dietary macronutrients [87]. For drug development, these findings underscore the importance of targeting specific nodes within these nutrient-sensing pathways, such as FGF21 mimetics or modulators of mTOR activity, to mimic the benefits of dietary interventions while avoiding their potential paradoxical drawbacks.
Evidence Synthesis: Comparative Efficacy Against Alternative Dietary Approaches
The management of metabolic diseases, particularly type 2 diabetes (T2D) and obesity, represents a significant global health challenge. Dietary intervention remains a cornerstone of first-line treatment strategies, with high-protein diets (HPDs) generating substantial scientific interest for their potential metabolic advantages over standard-protein diets (SPDs). This guide provides an objective, data-driven comparison of HPD versus SPD performance in randomized controlled trials (RCTs), focusing on efficacy for glucose control, weight management, and body composition. The analysis is contextualized within broader research on dietary efficacy for metabolic health, providing researchers and drug development professionals with synthesized experimental data and methodological insights.
Clinical Outcomes: Quantitative Data Synthesis
Weight Loss and Body Composition
Evidence from multiple meta-analyses of RCTs demonstrates that HPDs provide superior outcomes for weight loss and body composition compared to SPDs under isoenergetic conditions.
Table 1: Effects of HPDs vs. SPDs on Body Weight and Composition (Meta-Analysis Data)
| Outcome Measure | HPD Effect (Mean) | SPD Effect (Mean) | Mean Difference (95% CI) | Source/Study |
|---|---|---|---|---|
| Body Weight (kg) | - | - | -0.79 kg (-1.50 to -0.08) | Wycherley et al. [89] |
| Fat Mass (kg) | - | - | -0.87 kg (-1.26 to -0.48) | Wycherley et al. [89] |
| Fat-Free Mass (kg) | - | - | +0.43 kg (0.09 to 0.78) | Wycherley et al. [89] |
| Resting Energy Expenditure | - | - | +595.5 kJ/day (67.0 to 1124.1) | Wycherley et al. [89] |
| Body Mass Index (kg/m²) | - | - | -0.37 kg/m² (-0.56 to -0.19) | Santesso et al. [89] |
A key physiological advantage of HPDs is the preservation of fat-free mass (FFM) during weight loss. This is critically important because FFM is a primary determinant of resting metabolic rate. The maintenance of FFM helps prevent the decline in resting energy expenditure (REE) that typically accompanies weight loss, thereby supporting long-term weight maintenance [89]. Furthermore, HPDs significantly enhance diet-induced thermogenesis (DIT), as protein has a markedly higher thermic effect compared to carbohydrates and fats, contributing to a greater overall energy expenditure [89].
Glycemic Control and Cardiovascular Risk Factors
HPDs exert significant effects on glycemic markers and cardiovascular risk profiles, though outcomes can vary based on patient population and diet composition.
Table 2: Effects of HPDs on Glycemic and Cardiovascular Risk Factors
| Parameter | Findings with HPD | Study Context |
|---|---|---|
| Fasting Glucose | No significant change vs. SPD [89] | Energy-restricted diets |
| Fasting Insulin | Significant decrease vs. SPD (-0.03 μIU/mL [-0.05 to -0.01]) [89] | Non-energy-restricted diets |
| Insulin Sensitivity | Significant improvement (4 vs. 0.9, p<0.0001) [5] | 6-month RCT in obese women |
| β-Cell Function | Significant improvement (7.4 vs. 2.1, p<0.0001) [5] | 6-month RCT in obese women |
| Triglycerides | Significant reduction vs. SPD (-20.3 mg/dL [-29.2 to -10.6]) [89] | Energy-restricted diets |
| Blood Pressure | Significant reduction in SBP & DBP vs. SPD [89] | Non-energy-restricted diets |
A 6-month RCT comparing hypocaloric HPD (30% protein) and high-carbohydrate diet (HC, 15% protein) in obese premenopausal women demonstrated that the HPD led to dramatically greater improvements in insulin sensitivity and β-cell function [5]. The same study also showed that the HPD was more effective at reducing proinflammatory cytokines and markers of oxidative stress, suggesting broader systemic benefits beyond pure glycemic control [5].
Experimental Protocols and Methodologies
Common RCT Designs for Diet Comparison
Robust head-to-head trials share key methodological features to ensure valid and comparable results.
Table 3: Key Methodological Elements in HPD vs. SPD Trials
| Element | Typical Implementation | Purpose |
|---|---|---|
| Study Population | Adults with obesity, prediabetes, or T2D; often premenopausal women without diabetes for metabolic studies [5]. | Controls for confounding metabolic variables. |
| Diet Composition | HPD: 25-35% of total energy, 1.07-1.60 g/kg/BW [89]. SPD: 15-21% of total energy, 0.55-0.88 g/kg/BW [89]. | Ensures clinically relevant protein difference. |
| Energy Intake | Isoenergetic design or matched energy deficit (~500 kcal/day restriction) [5]. | Isolates effect of macronutrient composition. |
| Diet Delivery | Pre-packaged meals or detailed meal plans with provided foods [5]. | Enhances dietary adherence and control. |
| Intervention Duration | Short-term (≤3 months) to long-term (6-12 months) [89] [5]. | Assesses sustainability and long-term efficacy. |
| Control for Weight Loss | Statistical adjustment for weight loss in analyses of metabolic parameters. | Differentiates weight-dependent and independent effects. |
Detailed Protocol: 6-Month RCT in Obese Women
A seminal study provides a robust template for direct HPD vs. SPD comparison [5]:
- Participants: 32 obese premenopausal women without diabetes, randomized to HP (30% protein, 40% carbohydrate) or HC (15% protein, 55% carbohydrate) groups.
- Energy Restriction: Both diets were hypocaloric, providing 500 kcal/day less than individual calculated maintenance needs.
- Diet Control: All food was provided in prepackaged form to ensure strict adherence to macronutrient targets.
- Outcome Measures: Assessed at baseline and 6 months included oral glucose tolerance tests, mixed-meal tolerance tests, DXA scans for body composition, REE measurement, and comprehensive blood sampling for biomarkers.
- Statistical Analysis: Utilized Wilcoxon rank sum tests for between-group comparisons of change from baseline.
Figure 1: Experimental workflow for a 6-month RCT comparing HPDs and SPDs [5].
Mechanistic Insights: How HPDs Influence Glucose Metabolism
The metabolic benefits of HPDs extend beyond simple weight loss and involve multiple direct physiological mechanisms.
Appetite Regulation and Energy Balance
HPDs modulate the secretion of key gut-derived hormones involved in appetite regulation:
- Increased anorexigenic hormones: Glucagon-like peptide-1 (GLP-1), cholecystokinin (CCK), and peptide tyrosine-tyrosine (PYY) reduce appetite [89].
- Decreased orexigenic hormone: Ghrelin, which stimulates appetite [89].
- This hormonal shift results in enhanced satiety signaling, reduced food intake, and facilitation of weight loss [89].
Direct Effects on Glucose Homeostasis
Emerging evidence indicates that branched-chain amino acids (BCAAs), particularly leucine, play a direct role in glucose regulation through central nervous system signaling.
Figure 2: Central nervous system pathway for leucine-mediated glucose regulation [27].
Additionally, protein ingestion stimulates insulin secretion, which can improve postprandial glycemia, particularly when combined with carbohydrates [41]. This insulinotropic effect, along with the potential for HPDs to enhance insulin sensitivity, contributes to improved overall glycemic control [5] [27].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials for HPD Clinical Trials
| Tool/Reagent | Function/Application | Example Use Cases |
|---|---|---|
| Validated Food Frequency Questionnaire (FFQ) | Assesses habitual dietary intake at baseline and during follow-up. | Shanghai Suburban Adult Cohort dietary assessment [68]. |
| Pre-packaged Meal Systems | Ensures strict adherence to defined macronutrient and energy targets. | 6-month RCT providing all study meals [5]. |
| Dual-Energy X-ray Absorptiometry (DXA) | Precisely measures body composition (fat mass, fat-free mass). | Body composition analysis in weight loss trials [5]. |
| Oral Glucose Tolerance Test (OGTT) | Assesses β-cell function and insulin sensitivity in response to glucose load. | Standardized metabolic phenotyping [5]. |
| Continuous Glucose Monitoring (CGM) | Provides continuous, real-time interstitial glucose measurements. | Evaluating 24-hour glycemic excursions in free-living subjects. |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Quantifies specific hormones and biomarkers (insulin, GLP-1, PYY, etc.). | Gut hormone measurement in satiety studies [89]. |
| Indirect Calorimetry | Measures resting energy expenditure (REE) and substrate utilization. | Assessing diet-induced thermogenesis [89]. |
Head-to-head randomized trial evidence demonstrates that HPDs consistently outperform SPDs for weight loss, fat mass reduction, and preservation of metabolically active fat-free mass. The benefits for glycemic control are significant, particularly in improving insulin sensitivity and β-cell function, though effects on fasting glucose can be variable. The mechanisms underlying these advantages involve complex interactions among hormonal satiety signals, enhanced energy expenditure, and direct nutrient signaling pathways that improve hepatic glucose regulation. For researchers designing clinical trials in metabolic disease, HPD protocols featuring controlled feeding, adequate intervention duration (>6 months), and comprehensive metabolic phenotyping offer the most robust approach for evaluating dietary efficacy.
The management of type 2 diabetes mellitus (T2DM) and prediabetes necessitates effective dietary strategies to improve glycemic control and insulin sensitivity. Among various nutritional approaches, high-protein diets have garnered significant scientific interest for their potential benefits on metabolic parameters. This review synthesizes meta-analytic evidence comparing the effects of high-protein diets against standard diets and other interventions on key glycemic markers: hemoglobin A1c (HbA1c), fasting blood glucose (FBG), and Homeostatic Model Assessment of Insulin Resistance (HOMA-IR). Framed within a broader thesis on the efficacy of high-protein diets for glucose control, this analysis provides researchers, scientists, and drug development professionals with a comprehensive comparison of experimental data and methodologies.
Quantitative Data Synthesis: Comparative Effects on Glycemic Markers
The following tables synthesize quantitative findings from multiple clinical trials and meta-analyses, comparing the effects of high-protein diets, standard diets, and psyllium supplementation on primary glycemic endpoints.
Table 1: Effects of High-Protein vs. Standard-Protein Diets on Glycemic and Cardiometabolic Parameters
| Parameter | High-Protein Diet (Mean Change) | Standard-Protein Diet (Mean Change) | P-value | Study Duration | Population | Citation |
|---|---|---|---|---|---|---|
| HbA1c (%) | -0.7% | -0.1% | 0.002 | 3 months | Obese/Overweight, HF, DM | [49] |
| HbA1c (%) | -0.8% | -0.3% | <0.05 | 5 weeks | T2DM | [6] |
| Weight (kg) | -8.4 kg | -5.0 kg | <0.05 | 9 months | Obese | [90] |
| HOMA-IR | -0.8 units | -0.3 units | <0.05 | 9 months | Obese | [90] |
| Fasting Triglycerides (mg/dL) | -25.7 | -5.7 | 0.032 | 3 months | Obese/Overweight, HF, DM | [49] |
| Systolic BP (mmHg) | -5.1 | -3.1 | <0.05 | 9 months | Obese | [90] |
Table 2: Effects of Psyllium Supplementation on Glycemic Parameters: Meta-Analysis Results
| Parameter | Weighted Mean Difference (WMD) vs. Placebo | 95% Confidence Interval | P-value | Number of RCTs (Participants) | Citation |
|---|---|---|---|---|---|
| Fasting Blood Sugar (mg/dL) | -6.89 | -10.62, -3.16 | <0.001 | 19 (962) | [91] [92] |
| HbA1c (%) | -0.75 | -1.21, -0.29 | <0.001 | 19 (962) | [91] [92] |
| HOMA-IR | -1.17 | -2.11, -0.23 | <0.05 | 19 (962) | [91] [92] |
| Insulin | -2.08 | -4.21, 0.035 | >0.05 (NS) | 19 (962) | [91] [92] |
Abbreviations: HF: Heart Failure; DM: Diabetes Mellitus; T2DM: Type 2 Diabetes Mellitus; NS: Not Significant; BP: Blood Pressure.
Detailed Experimental Protocols and Methodologies
Protocol for Long-Term High-Protein Diet Trials
The evidence for high-protein diets is derived from rigorous, randomized controlled trials (RCTs). Key methodological elements include:
- Diet Composition and Design: High-protein diets typically provided 25-35% of total energy intake from protein, 30% from fat, and 40% or less from carbohydrates [49] [6]. Standard-protein control diets contained 15-20% protein, 55% carbohydrates, and 30% fat. Diets were primarily hypocaloric, designed with a daily energy deficit of 500-800 kcal to promote weight loss of 0.5-1.0 kg per week [49] [90].
- Participant Profile: Studies focused on specific populations, including overweight and obese adults, often with co-morbid conditions such as heart failure and type 2 diabetes [49], or premenopausal women without diabetes [5]. Sample sizes ranged from 12 to over 300 participants [49] [5] [90].
- Intervention Duration and Monitoring: Trial durations varied from 5 weeks to 9 months [49] [90] [6]. Participants received regular consultations with licensed dietitians for nutritional counseling, adherence monitoring, and dietary adjustments. Body weight, waist circumference, and blood pressure were tracked at follow-up visits [49].
- Outcome Measurements: Blood samples were collected after a 12-hour overnight fast at baseline and the end of the study. Key biomarkers analyzed included HbA1c, fasting glucose, insulin, lipid profile (total cholesterol, LDL, HDL, triglycerides), and inflammatory markers. HOMA-IR was calculated to assess insulin resistance [49] [5] [90].
Protocol for Acute Postprandial Response Studies
Acute studies investigate the immediate effects of high-protein nutritional supplements on glycemic response.
- Study Design: Typically utilize an open-label, cross-over design. Participants consume a high-protein diabetes-specific nutritional formula (DSNF-Pro) on one visit and a standard nutritional formula (STNF) on another, with a washout period in between [38].
- Product Composition: The DSNF-Pro is characterized by high protein (e.g., 12g per 140 kcal serving), low carbohydrate (e.g., 12g), and contains monounsaturated fats and dietary fiber. The STNF is isocaloric but has lower protein (e.g., 4.9g) and higher carbohydrates (e.g., 21g) [38].
- Measurement of Glycemic Response: After a 10-12 hour fast, participants consume the investigational product. Venous blood samples are taken at fasting and at regular intervals post-consumption (e.g., 30, 60, 90, 120, and 180 minutes). The incremental area under the curve (iAUC) for plasma glucose, serum insulin, and serum c-peptide is calculated to quantify the postprandial response [38].
Protocol for Psyllium Supplementation Meta-Analysis
The evidence for psyllium is consolidated from a systematic review and meta-analysis.
- Search Strategy and Eligibility: Comprehensive searches of databases (PubMed, Scopus, Web of Science) were conducted for RCTs up to July 2022. The PICOS criteria were applied, including RCTs in adults (≥18 years) that compared psyllium with a control/placebo and reported changes in FBS, HbA1c, HOMA-IR, or insulin [92].
- Data Extraction and Analysis: Two independent researchers extracted data, including study design, participant characteristics, psyllium dosage, intervention duration, and outcome means and standard deviations. A random-effects model was used to pool data and calculate weighted mean differences (WMD) with 95% confidence intervals (CI). Subgroup analyses were performed based on dosage and intervention duration [91] [92].
Proposed Signaling Pathways and Mechanisms of Action
The following diagrams illustrate the proposed physiological pathways through which high-protein diets and psyllium supplementation exert their effects on glycemic control.
High-Protein Diet Action Pathway
Title: Proposed mechanisms of action for high-protein diets.
Psyllium Action Pathway
Title: Proposed mechanisms of action for psyllium fiber.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Materials for Dietary Intervention Metabolic Research
| Item | Function & Application in Research | Example Context in Cited Studies |
|---|---|---|
| Dual-Energy X-ray Absorptiometry (DXA/Deltatrac) | Precisely measures body composition (fat mass, lean body mass) and resting energy expenditure to determine individualized caloric requirements. | Used to assess energy requirements and body composition changes [49] [5]. |
| Enzymatic Colorimetric Assays (e.g., Glucose Oxidase) | Quantifies plasma glucose concentrations from blood samples. A fundamental assay for determining fasting and postprandial glucose levels. | Used to measure plasma glucose in postprandial response studies [38]. |
| Radioimmunoassay (RIA) Kits | Measures concentrations of hormones and peptides such as insulin and C-peptide with high sensitivity. Critical for assessing pancreatic β-cell function. | Used to measure serum insulin and c-peptide levels [38]. |
| Standardized Nutritional Software (e.g., NDSR, CAN-Pro) | Analyzes and ensures nutrient adequacy of experimental diets. Used to design meal plans and verify macronutrient and micronutrient content. | CAN-Pro program used for daily nutritional intake analysis [38]. |
| HbA1c Testing Systems | Measures glycated hemoglobin (HbA1c), providing an index of average blood glucose over the preceding 2-3 months. A primary endpoint in long-term glycemic control studies. | A key outcome measured in all long-term dietary intervention trials [49] [90] [91]. |
| Prepackaged Meal Kits | Ensures strict adherence to the prescribed macronutrient composition of experimental diets, reducing variability and confounding from self-reported intake. | Diets were provided in prepackaged food to control nutrient composition [5]. |
The synthesized evidence strongly indicates that high-protein, hypocaloric diets are more effective than standard-protein, hypocaloric diets in improving key markers of glycemic control, including HbA1c, HOMA-IR, and fasting glucose, particularly in overweight and obese individuals with or without type 2 diabetes [49] [90] [6]. The benefits extend to superior weight loss and enhancements in cardiovascular risk factors such as triglycerides and blood pressure.
Notably, the mechanism appears multifaceted. While acute protein ingestion enhances insulin secretion and improves postprandial glycemia [38] [6], the long-term benefits are likely mediated by significant weight loss, preservation of lean mass, and sustained reductions in insulin resistance [90]. As a comparator, psyllium fiber presents an alternative non-pharmacological approach that effectively lowers HbA1c, FBG, and HOMA-IR, likely through distinct mechanisms involving delayed carbohydrate absorption [91] [92] [93].
For the research and drug development community, these findings highlight high-protein diets as a potent dietary strategy for managing glucose dysregulation. Future long-term trials are needed to fully establish the durability of these benefits and to explore the molecular pathways, including the role of specific amino acids and gut hormones, to identify potential targets for future therapeutic agents.
Within the broader investigation into the efficacy of high-protein diets versus standard dietary approaches for glucose control, a critical comparison must be made with another prominent dietary strategy: low-carbohydrate diets (LCDs). Both dietary paradigms represent a significant departure from traditional high-carbohydrate, low-fat recommendations and have shown promise for managing metabolic diseases. However, their underlying physiological mechanisms, specific efficacy profiles, and applicability to different patient populations exhibit distinct differences. This guide objectively compares the performance of high-protein and low-carbohydrate diets by synthesizing data from controlled trials and mechanistic studies, providing researchers and drug development professionals with a structured analysis of their differential metabolic effects.
Comparative Efficacy Data from Clinical Trials
Direct comparisons of dietary interventions require examination of key metabolic parameters. The following tables summarize quantitative data from randomized controlled trials and systematic reviews, highlighting differential outcomes for glucose control, body composition, and lipid profiles.
Table 1: Glycemic Control and Body Composition Outcomes
| Parameter | High-Protein Diet (HP) | Low-Carbohydrate Diet (LCD) | Study Duration | P-Value |
|---|---|---|---|---|
| HbA1c Reduction (%) | -- | -0.23% to -0.5% [94] | 6 months | <0.05 |
| Fasting Glucose Reduction | -- | -10.3 mg/dL [94] | 6 months | -- |
| HOMA-IR Improvement | -1.78 [95] | -- | 21 days (HP) [95] | 9 × 10-3 (HP) [95] |
| Weight Loss (kg) | -- | -5.9 kg [94] | 6 months | -- |
| Glycemic Variability (mg/dL) | -3.13 [95] | -- | 21 days (HP) [95] | 4 × 10-4 (HP) [95] |
| Insulin Reduction (µIU/mL) | -6.98 [95] | -- | 21 days (HP) [95] | 0.01 (HP) [95] |
Table 2: Lipid Profile and Inflammatory Biomarkers
| Parameter | High-Protein Diet (HP) | Low-Carbohydrate Diet (LCD) | Study Duration | P-Value |
|---|---|---|---|---|
| Triglycerides | -- | Consistent reduction [94] | 6 months | -- |
| HDL-C | -- | Increase [94] | 6 months | -- |
| C-Reactive Protein (CRP) | -2.1 mg/L [5] | -- | 6 months (HP) [5] | 0.0003 (HP) [5] |
| Interleukin-6 (IL-6) | -1.3 pg/mL [5] | Inverse association with high-quality LCD [96] [97] | 6 months (HP) [5] | <0.0001 (HP) [5] |
| Tumor Necrosis Factor-α (TNF-α) | -1.8 pg/mL [5] | -- | 6 months (HP) [5] | <0.0001 (HP) [5] |
| Adiponectin | +1284 ng/mL [5] | -- | 6 months (HP) [5] | 0.0011 (HP) [5] |
Experimental Protocols and Methodologies
Inpatient Crossover Feeding Trial (High-Protein vs. Mediterranean Diet)
Objective: To compare the acute metabolic effects of an isocaloric high-protein (HP) diet versus a Mediterranean (M) diet in a tightly controlled setting [95].
Population: 20 insulin-resistant, obese premenopausal women (BMI 35–64 kg/m², HOMA-IR ≥3) excluding those with type 2 diabetes [95].
Design:
- Model: Randomized, open-label, crossover controlled feeding trial.
- Intervention Sequences: Hypocaloric M diet followed by hypocaloric HP diet (M–HP) or vice versa (HP–M). Each diet period lasted 10 days with no washout [95].
- Diet Composition:
- HP Diet: 40% carbohydrate, 30% fat, 30% protein.
- M Diet: 55% carbohydrate (whole wheat), 25% fat (PUFA from olive oil, nuts), 20% protein (fish, legumes) [95].
- Caloric Provision: Individualized to 500 kcal less than the calculated total energy expenditure (TEE = REE × 1.2) [95].
Key Outcome Measures:
- Primary: Changes in insulin, HOMA-IR, and glycemic variability (mean standard deviation of continuous glucose monitor readings) [95].
- Secondary: Body composition (bioimpedance), lipid profiles, gut microbiome analysis (16S rRNA sequencing) [95].
Workflow Diagram: This diagram illustrates the controlled crossover design of the study.
Long-Term Observational Cohort (Low-Carbohydrate Diet Patterns)
Objective: To prospectively examine associations between LCD patterns varying in carbohydrate quality and changes in biomarkers of inflammation and oxidative stress [96] [97].
Population: 2,225 participants from the Framingham Offspring Study (mean baseline age: 60.1 years), followed for a median of 6.7 years [96].
Design:
- Model: Prospective longitudinal cohort study.
- Exposure Assessment: Dietary intake was assessed at baseline (examination cycle 7, 1998-2001) using a semi-quantitative food frequency questionnaire (FFQ) [96].
- LCD Scoring: Two distinct LCD scores (LCDS) were created:
- HQ-LCDS: Represents lower intake of low-quality carbohydrates (refined grains, added sugars) with higher total fat and protein.
- LQ-LCDS: Represents lower intake of high-quality carbohydrates (whole grains, fruits, vegetables) with higher total fat and protein [96].
- Outcome Measurement: An inflammation and oxidative stress (IOS) score was calculated by summing standardized values of 9 circulating and urinary biomarkers, measured at baseline and follow-up (examination cycle 8, 2005-2008) [96].
Key Outcome Measures:
- Change in the composite IOS score.
- Changes in individual biomarkers (e.g., intercellular adhesion molecule-1, lipoprotein phospholipase A2) [96] [97].
Underlying Physiological Mechanisms
The efficacy patterns of high-protein and low-carbohydrate diets are rooted in distinct, though sometimes overlapping, physiological pathways.
Metabolic Pathways of Low-Carbohydrate and Ketogenic Diets
LCDs, particularly very-low-carbohydrate ketogenic diets (typically <50g carbs/day), induce a fundamental shift in fuel metabolism from glucose to fat-derived ketone bodies [98] [99].
Mechanism Diagram: This diagram outlines the primary metabolic shift induced by severe carbohydrate restriction.
This metabolic state, nutritional ketosis, is characterized by moderate levels of ketone bodies (acetoacetate, beta-hydroxybutyrate, and acetone) in the blood without altering blood pH [98]. Ketone bodies are a more efficient fuel than glucose, producing more ATP per unit and reducing free radical damage [98]. The concomitant low insulin levels reduce fat storage and promote lipolysis [99].
Mechanisms of High-Protein Diets
High-protein diets exert their effects through different primary mechanisms:
- Enhanced Insulin Sensitivity and β-Cell Function: HP diets significantly improve HOMA-IR and β-cell function, as evidenced by a 6-month trial where the HP group showed vastly superior improvements compared to a high-carbohydrate group [5].
- Increased Thermic Effect and Energy Expenditure: Protein has a higher thermic effect of feeding compared to carbohydrates and fats, leading to a greater increase in resting energy expenditure (REE). One study recorded a 259 kcal increase in REE on an HP diet versus only 26 kcal on an HC diet [5].
- Reduction of Oxidative Stress and Inflammation: HP intake is associated with significant reductions in markers of oxidative stress (dichlorofluorescein), lipid peroxidation (malondialdehyde), and proinflammatory cytokines (TNF-α, IL-6) [5]. This suggests a direct role in modulating underlying metabolic inflammation.
- Modulation of the Gut Microbiome: Specific microbial genera (e.g., Coprococcus, Lachnoclostridium) have been identified as predictive of the differential response in glycemic variability between HP and Mediterranean diets, indicating a potential gut-mediated mechanism [95].
The Critical Role of Carbohydrate Quality in LCDs
The metabolic effects of an LCD are not solely determined by carbohydrate quantity. Evidence indicates that the quality of the remaining carbohydrates is a critical effect modifier. A prospective cohort study found that a high-quality LCD (HQ-LCDS), which replaces low-quality carbohydrates (refined grains, added sugars) with fat and protein, was inversely associated with inflammation and oxidative stress over nearly 7 years of follow-up [96] [97]. Conversely, a low-quality LCD (LQ-LCDS), which reduces intake of high-quality carbohydrates (whole grains, fruits), showed no such benefit [96] [97]. This highlights that the health impacts of an LCD are contingent on the specific food sources of macronutrients.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Assays for Metabolic Diet Research
| Reagent/Assay | Function in Research | Exemplary Application |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Measures interstitial glucose levels to assess glycemic variability, mean glucose, and time-in-range. | Calculating mean standard deviation of glucose as a measure of glycemic variability [95]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Quantifies specific proteins (hormones, cytokines, adipokines) in serum/plasma. | Measuring insulin, TNF-α, IL-6, adiponectin levels [95] [5]. |
| Homeostasis Model Assessment (HOMA) | Calculates indices of insulin resistance (HOMA-IR) and β-cell function (HOMA-%B) from fasting glucose and insulin. | Primary outcome to compare insulin sensitivity between diets [95] [5]. |
| 16S rRNA Gene Sequencing | Profiling the composition of the gut microbiome from fecal samples. | Identifying microbial genera associated with differential diet response [95]. |
| Food Frequency Questionnaire (FFQ) | Assesses long-term habitual dietary intake for epidemiological studies. | Creating low-carbohydrate diet scores (LCDS) based on carbohydrate quality [96]. |
| Indirect Calorimetry | Measures resting energy expenditure (REE) and respiratory quotient by analyzing oxygen consumption and CO2 production. | Determining individual caloric needs and assessing diet-induced thermogenesis [95] [5]. |
| Dichlorofluorescein Assay | A fluorescent probe used to measure overall oxidative stress in biological samples. | Demonstrating significant reduction in oxidative stress on an HP diet [5]. |
| Dual-Energy X-ray Absorptiometry (DXA) | Precisely measures body composition (fat mass, lean mass, bone density). | Tracking changes in body composition independent of weight [5]. |
The escalating global prevalence of type 2 diabetes mellitus (T2DM) necessitates the development of effective therapeutic strategies capable of inducing sustained remission rather than mere glycemic management. Dietary interventions have re-emerged as powerful tools in this endeavor, with very-low-calorie diets (VLCDs) and ketogenic diets (KDs) demonstrating significant potential to reverse disease progression [100]. While the efficacy of high-protein diets (HPDs) for glucose control is a critical area of investigation, this review objectively examines the current evidence for VLCDs and KDs, focusing on their remission potential, underlying mechanisms, and practical application in clinical research. The growing understanding of T2DM as a reversible metabolic state, particularly through dietary means that promote substantial weight loss and improve insulin sensitivity, underscores the importance of this analysis for researchers and drug development professionals seeking non-pharmacological avenues for disease modification [100] [101].
Comparative Efficacy for T2DM Remission
Remission Rates and Glycemic Control
Table 1: Remission Rates and Glycemic Outcomes from Clinical Studies
| Study & Design | Intervention Diet | Follow-up Duration | T2DM Remission Rate | HbA1c Reduction | Weight Loss |
|---|---|---|---|---|---|
| Systematic Review (n=6 studies) [100] | LCD/KD | 1-8 years | Up to 62% (1 yr); 13% (5 yr) | Significant reduction | Significant |
| Homemade VLCD Pilot (n=22) [102] | VLCD (800 kcal) | 48 weeks | 67% (prediabetes or no diabetes) | Significant (p<0.001) | 15 kg mean loss |
| Real-world ICR (n=1,069) [101] | Intermittent Calorie Restriction | 3-6 months | 20% vs. 2% (control) | Data not specified | Data not specified |
| Healthy KD RCT (n=80) [103] | HKD vs. ERD | 6 months | Data not specified | -0.3±0.3% (HKD) vs. -0.1±0.2% (ERD) | -7.8±5.2 kg (HKD) vs. -4.2±5.6 kg (ERD) |
The data from multiple studies consistently demonstrate that carbohydrate-restricted diets and very-low-calorie approaches can induce significant T2DM remission. A systematic review of studies with follow-up periods ranging from one to eight years found that low-carbohydrate and ketogenic diets led to significant reductions in HbA1c and body weight, with remission rates highest at one year (up to 62%) though declining to 13% by year five, indicating challenges with long-term sustainability [100]. Notably, a real-world study of an intermittent calorie-restricted diet demonstrated substantially higher remission rates (20%) compared to conventional dietary approaches (2%), highlighting the potential for these interventions even outside highly controlled trial settings [101].
Metabolic and Cardiovascular Improvements
Table 2: Cardiometabolic Outcomes from Dietary Interventions
| Parameter | VLCD/Ketogenic Diet Impact | Study Evidence |
|---|---|---|
| Systolic BP | Significant reduction (-7.7 to -12.9%) | [100] [103] [104] |
| Diastolic BP | Significant reduction (-10.8%) | [104] |
| Lipid Profile | Improved triglycerides, no LDL-C elevation | [103] |
| Liver Function | Reduced aspartate transaminase | [103] |
| Inflammation | Reduced high-sensitivity CRP | [104] |
| Medication Use | Reduced dependency on glucose-lowering and antihypertensive drugs | [100] [101] |
Beyond glycemic control, these dietary interventions demonstrate broad cardiometabolic benefits. A study specifically examining the very low-calorie ketogenic diet in women with obesity and hypertension found significant reductions in both systolic (-12.89%) and diastolic blood pressure (-10.77%) after 45 days [104]. The development of a Healthy Ketogenic Diet paradigm addresses historical concerns about potential LDL-cholesterol elevation, with studies showing no increase in LDL-cholesterol while achieving superior weight loss and metabolic improvements compared to energy-restricted diets [103].
Experimental Protocols and Methodologies
Ketogenic Diet Interventions
The ketogenic diet protocol typically restricts carbohydrate intake to ≤50 grams per day while emphasizing adequate protein and high fat intake [105] [106]. In research settings, several variants have been developed:
Healthy Ketogenic Diet (HKD): Designed to optimize metabolic benefits while mitigating potential LDL-cholesterol elevation through emphasis on monounsaturated fats, omega-3 fatty acids, adequate fiber (20-30 g/day), and energy restriction [103]. The HKD protocol includes eight key components: (1) energy restriction with at least 500 kcal deficit daily, (2) 50 g net carbohydrate daily limit, (3) low saturated and trans fat, (4) total fat within 50% of energy intake emphasizing healthy fats, (5) adequate protein (1.0-1.2 g/kg body weight), (6) adequate fiber, (7) adequate fluid (≥2 L/day), and (8) micronutrient supplementation [103].
Very Low-Calorie Ketogenic Diet (VLCKD): Characterized by more severe calorie restriction (700-800 kcal/day) with carbohydrate restriction of 30-50 g/day (≈13% of total energy intake), fats at 30-40 g/day (≈44%), and protein at 1.2-1.4 g/kg body weight (≈43%) [105]. This protocol is typically implemented in phases, beginning with an active ketosis phase, followed by refeeding and maintenance phases [105] [104].
Very Low-Calorie and Intermittent Calorie-Restricted Diets
VLCD protocols generally provide 800 kcal per day or less while maintaining nutrient adequacy [102]. One pilot study utilized a homemade VLCD consisting of three meal replacements daily with the addition of vegetables and multivitamin/omega-3 supplements for 12 weeks, followed by gradual food reintroduction over subsequent weeks [102]. This approach demonstrated that commercially available ingredients can effectively replace proprietary formula diets, potentially improving accessibility and cost-effectiveness.
The intermittent calorie-restricted diet protocol from a large real-world study involved six cycles of 15-day intervals, each consisting of 5 days of hypocaloric meals (917 kcal/day) followed by 10 days of an unrestricted diet guided by standard dietary guidelines for diabetes [101]. This cyclic approach may enhance long-term adherence while still providing significant metabolic benefits.
Adherence Support and Monitoring
Successful implementation of these dietary interventions in research settings typically involves comprehensive adherence support strategies:
- Digital Monitoring: Use of mobile applications (e.g., Nutritionist Buddy app) for tracking dietary intake, weight, and physical activity [103].
- Regular Coaching: Dietitian support through in-person consultations, group workshops, and digital messaging platforms [103] [107].
- Biomarker Monitoring: Regular assessment of ketone bodies (capillary R-beta-hydroxybutyrate), glycemic parameters, and metabolic markers to verify adherence and physiological response [107].
- Partial Food Provision: Some studies provide ketogenic-appropriate food items or meals to facilitate adherence and ensure dietary quality [107].
Signaling Pathways and Mechanistic Insights
Figure 1: Metabolic Pathways in VLCD and Ketogenic Diet-Induced T2DM Remission
The physiological mechanisms through which VLCDs and ketogenic diets induce T2DM remission involve multiple interconnected pathways. Carbohydrate restriction directly reduces glucose load and postprandial insulin secretion, creating an energy deficit that promotes free fatty acid mobilization from adipose tissue [106]. In the liver, these fatty acids undergo beta-oxidation and are converted to ketone bodies (β-hydroxybutyrate, acetoacetate, acetone) through ketogenesis, establishing a state of nutritional ketosis that provides alternative energy substrates for peripheral tissues [105] [106].
This metabolic shift has several downstream effects: (1) Improved insulin sensitivity through reduced ectopic fat deposition in liver and muscle tissue; (2) Reduced inflammation mediated by lower production of pro-inflammatory cytokines and adipokines; (3) Beta-cell rest through decreased demand for insulin secretion; and (4) Significant weight loss, particularly visceral adipose tissue, further ameliorating insulin resistance [100] [104] [106]. The correlation between reductions in high-sensitivity C-reactive protein and blood pressure observed in VLCKD studies suggests that anti-inflammatory effects may represent a particularly important mechanism for the cardiovascular benefits of these diets [104].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents and Tools for Dietary Intervention Research
| Category | Specific Tools/Assays | Research Application |
|---|---|---|
| Ketosis Verification | Capillary R-beta-hydroxybutyrate meters, Urinary ketone strips | Quantification of nutritional ketosis achievement and adherence [107] |
| Glycemic Assessment | HbA1c assays, Continuous glucose monitors, Oral glucose tolerance tests | Evaluation of glycemic control and diabetes remission status [100] [108] |
| Body Composition | Bioelectrical impedance analysis, DEXA, Waist circumference measurement | Assessment of fat mass, fat-free mass, and visceral adipose tissue changes [109] [102] [104] |
| Cardiometabolic Panels | Lipid profiles, High-sensitivity CRP, Liver enzymes, Renal function tests | Comprehensive safety and efficacy monitoring [103] [104] |
| Dietary Adherence | Food frequency questionnaires, 3-day food records, Mobile tracking apps (nBuddy) | Assessment of intervention fidelity and nutrient intake [103] |
| Psychological Measures | PHQ-9, HRSD, Quality of Life (EQ-5D), Self-regulation of Eating Behaviour | Evaluation of psychological effects and eating behavior changes [102] [107] |
The accumulating evidence from randomized controlled trials, systematic reviews, and real-world studies substantiates the significant remission potential of very-low-calorie and ketogenic diets for type 2 diabetes. These dietary interventions facilitate substantial weight loss, improved insulin sensitivity, and reductions in antihypertensive and glucose-lowering medications, with remission rates substantially higher than conventional dietary approaches [100] [101]. The development of Healthy Ketogenic Diet protocols that emphasize food quality addresses historical concerns about potential adverse lipid effects, enhancing the safety profile of these interventions [103].
For the research community, critical considerations include the development of standardized protocols that can be implemented across diverse populations, strategies to enhance long-term adherence, and identification of predictive biomarkers to guide personalized dietary recommendations. Future investigations comparing the efficacy of HPDs versus VLCDs/KDs should incorporate rigorous assessment of body composition, inflammatory markers, and metabolic parameters beyond weight and HbA1c alone. As the scientific understanding of T2DM remission mechanisms deepens, dietary interventions may offer viable alternatives or adjuncts to pharmacological approaches, potentially revolutionizing therapeutic paradigms for this prevalent metabolic disorder.
This review provides a comparative analysis of the effects of various dietary patterns, with a focused examination of high-protein diets (HPDs) versus standard diets, on key cardiometabolic parameters. Synthesizing evidence from recent randomized controlled trials, meta-analyses, and cohort studies, we evaluate the efficacy of these diets in modulating lipid profiles, blood pressure, glycemic control, and overall cardiovascular risk markers. The findings indicate that while HPDs offer significant advantages for weight loss and glycemic management, their effects on lipid profiles and long-term cardiovascular health are nuanced and dependent on protein source and patient demographics. This guide aims to equip researchers and drug development professionals with a structured overview of experimental data and methodologies to inform future clinical interventions and investigative protocols.
The escalating global prevalence of cardiometabolic diseases necessitates evidence-based dietary strategies for prevention and management. Among various nutritional interventions, high-protein diets (typically defined as providing >25-30% of total daily calories from protein or >1.0-1.2 g/kg/day) have garnered significant scientific and public interest for their potential role in weight management and metabolic control [49] [27]. Framed within the broader thesis of evaluating the efficacy of high-protein diets versus standard diets for glucose control research, this guide objectively compares their performance against other dietary patterns. The assessment is anchored on experimental data pertaining to their effects on lipid profiles, blood pressure, and cardiovascular risk markers, providing researchers with a consolidated resource of comparative outcomes and methodological approaches.
Methodological Approaches in Dietary Intervention Studies
Understanding the experimental protocols from key studies is crucial for interpreting data and designing future research.
Protocol for High-Protein Diet Interventions
A representative 3-month randomized controlled trial (RCT) in overweight/obese patients with diabetes and heart failure provides a robust methodological template [49]. The high-protein intervention arm followed a calorie-restricted diet consisting of 30% protein (approximately 110 g/day), 40% carbohydrates, and 30% fat. The comparator was a standard-protein diet (15% protein, ~55 g/day, 55% carbohydrates, 30% fat). Energy requirements were personalized using resting energy expenditure measurements from indirect calorimetry, with prescribed daily calorie deficits of 500-800 kcal. Dietary adherence was monitored through 45-60 minute counseling sessions with licensed dietitians at weeks 2, 4, 8, and 12, which included reviews of body weight and dietary intake records.
Network Meta-Analysis Methodology
A 2025 network meta-analysis (NMA) compared eight dietary patterns by employing Bayesian statistical models with Markov Chain Monte Carlo (MCMC) sampling [110]. The analysis included 21 RCTs with 1,663 participants and evaluated interventions such as low-fat, Mediterranean, ketogenic, low-carbohydrate, high-protein, vegetarian, intermittent fasting, and DASH diets. Dietary efficacy was ranked for each cardiometabolic outcome using Surface Under the Cumulative Ranking Curve (SUCRA) scores, providing a probabilistic hierarchy of interventions. The random-effects model analyzed mean differences (MD) in body composition, lipid profiles, glycemic markers, and blood pressure, offering a comprehensive cross-modal evaluation.
Comparative Efficacy of Dietary Patterns
Effects on Body Composition and Weight Loss
Table 1: Efficacy of Various Diets for Weight and Body Composition Management
| Dietary Pattern | Weight Reduction (MD, kg) | SUCRA Score | Waist Circumference Reduction (MD, cm) | SUCRA Score |
|---|---|---|---|---|
| Ketogenic | -10.5 (-18.0 to -3.05) | 99 | -11.0 (-17.5 to -4.54) | 100 |
| High-Protein | -4.49 (-9.55 to 0.35) | 71 | - | - |
| Low-Carbohydrate | - | - | -5.13 (-8.83 to -1.44) | 77 |
| Intermittent Fasting | - | - | - | - |
| DASH | - | - | - | - |
| Mediterranean | - | - | - | - |
MD = Mean Difference; SUCRA = Surface Under the Cumulative Ranking Curve (higher scores indicate greater efficacy) [110]
Ketogenic and high-protein diets demonstrate superior efficacy for weight reduction according to network meta-analysis [110]. In direct comparisons, a 3-month RCT found that both high-protein and standard-protein diets resulted in significant weight loss (3.6 kg vs. 2.9 kg, respectively), with no statistically significant difference between the two approaches [49].
Impact on Lipid Profiles
Table 2: Effects of Dietary Patterns on Lipid Parameters
| Dietary Pattern | LDL-C | HDL-C | Triglycerides | Total Cholesterol |
|---|---|---|---|---|
| Low-Carbohydrate | - | ↑ 4.26 mg/dL (2.46-6.49) [110] | - | - |
| Low-Fat | - | ↑ 2.35 mg/dL (0.21-4.40) [110] | - | - |
| High-Protein | - | - | ↓ 25.7 mg/dL (P=0.032) [49] | ↓ 16.8 mg/dL (P=0.031) [49] |
| Mediterranean | ↓ -27.5 mg/dL (P<0.001) [111] | - | ↓ -21.4 mg/dL (P<0.001) [111] | ↓ -35.4 mg/dL (P<0.001) [111] |
The effects on lipid profiles are diet-specific. Carbohydrate-restricted diets (low-carbohydrate and low-fat) optimally increase HDL-C levels [110]. In overweight and obese patients with diabetes and heart failure, a high-protein diet resulted in significantly greater reductions in triglycerides and total cholesterol compared to a standard-protein diet over 3 months [49]. Conversely, a study in obese women found that both high-protein and balanced diets increased LDL-C and HDL-C levels, with no significant differences between the two approaches [112]. The Mediterranean diet demonstrates comprehensive benefits across multiple lipid parameters [111].
Blood Pressure Modulation
Table 3: Blood Pressure Effects of Different Dietary Patterns
| Dietary Pattern | Systolic BP Reduction (MD, mmHg) | SUCRA Score | Diastolic BP Reduction (MD, mmHg) | Key Findings |
|---|---|---|---|---|
| DASH | -7.81 (-14.2 to -0.46) [110] | 89 | - | Most effective for systolic BP reduction |
| Intermittent Fasting | -5.98 (-10.4 to -0.35) [110] | 76 | - | Significant BP-lowering effects |
| High-Protein | - | - | - | Greater reduction than standard-protein (P<0.001) [49] |
| Mediterranean | -12.7 (ABPM day) (P<0.001) [111] | - | -8.4 (ABPM day) (P<0.001) [111] | Intensive lifestyle intervention context |
The DASH diet demonstrates the most pronounced effects on systolic blood pressure reduction according to network meta-analysis [110]. However, in a 3-month RCT, a high-protein diet resulted in significantly greater improvements in both systolic and diastolic blood pressure compared to a standard-protein diet in overweight/obese patients with comorbidities [49]. Intensive implementation of the Mediterranean diet also produces substantial blood pressure benefits [111].
Epidemiological evidence suggests that the relationship between protein intake and blood pressure may depend on the protein source. Vegetable protein intake shows a significant inverse relationship with blood pressure, while animal protein does not demonstrate this consistent benefit after adjusting for confounders [113].
Glycemic Control Parameters
For the central thesis comparing high-protein versus standard diets for glucose control, the evidence is particularly relevant. A systematic review of clinical studies concluded that high-protein diets (>30% or >1.0 g/kg/day) are an effective alternative for reducing hyperglycemia in patients with T2DM, with so-called Paleolithic diets (higher-quality protein from animal and vegetal sources) showing particular promise [27].
In a 52-week RCT comparing high-protein (40% protein) and normal-protein diets (21% protein) in adults with Type 2 diabetes, both diets were equally effective in improving glucose control, with the primary benefit attributed to weight loss itself rather than the specific protein composition [64]. However, another 3-month RCT reported that a high-protein diet resulted in a significantly greater reduction in HbA1c compared to a standard-protein diet (0.7% vs. 0.1%, P=0.002) [49].
For low-carbohydrate diets, an umbrella meta-analysis found significant short-term improvements in HbA1c levels in 16 out of 21 analyzed studies, though long-term sustainability remains uncertain [28].
Mechanistic Insights: Pathways of Protein-Mediated Metabolic Effects
High-protein diets, particularly those rich in branched-chain amino acids (BCAAs) like leucine, influence glucose metabolism through specific signaling pathways.
Diagram 1: Metabolic Pathways of High-Protein Diet Effects on Glucose Regulation. This illustrates the dual mechanisms through which high-protein diets, particularly their branched-chain amino acid (BCAA) components, influence glucose homeostasis. The primary pathway involves leucine sensing in the hypothalamus leading to reduced hepatic glucose production, while the secondary pathway involves incretin-mediated effects on insulin secretion and satiety [27].
The mechanism involves leucine crossing the blood-brain barrier at the arcuate nucleus of the medio-basal hypothalamus, where its metabolism leads to the production of oleoyl-CoA. This activates hypothalamic KATP channels, generating a signal transmitted via the vagus nerve to the liver, ultimately reducing hepatic glucose production through inhibition of gluconeogenesis and glycogenolysis [27].
Additionally, BCAAs stimulate the release of gut hormones GLP-1 and GIP, which enhance insulin secretion from pancreatic β-cells and promote satiety, contributing to improved glycemic control and weight management [27].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials and Analytical Tools for Dietary Intervention Studies
| Reagent/Instrument | Application in Research | Experimental Context |
|---|---|---|
| Indirect Calorimetry (Deltatrac) | Measurement of resting energy expenditure for personalized calorie prescriptions | Used to determine energy requirements in high-protein diet RCTs [49] |
| 24-hour Urinary Urea Measurement | Objective biomarker for total protein intake assessment | Employed in epidemiological studies to validate dietary recalls [113] |
| High-sensitivity CRP (hs-CRP) Latex-ALTA Kit | Quantification of inflammatory markers | Used to assess low-grade inflammation in diet studies [112] |
| Automated Lipid Profile Analyzer | Simultaneous measurement of TC, TG, HDL-C, LDL-C | Standard biochemical analysis in cardiometabolic diet studies [112] [111] |
| Ambulatory Blood Pressure Monitoring (ABPM) | 24-hour blood pressure profiling outside clinical settings | Gold standard for BP assessment in hypertension diet studies [111] |
| Dual-energy X-ray Absorptiometry (DEXA) | Precise measurement of body composition changes | Used to assess fat mass and lean mass changes in diet interventions [49] |
| Nutrition Data System (e.g., version 2.91) | Standardized nutrient calculation from dietary recalls | Ensures consistent nutrient analysis across research sites [113] |
Discussion and Research Implications
The comparative analysis reveals that high-protein diets offer distinct advantages for weight loss, glycemic control, and certain lipid parameters compared to standard diets, supporting their potential role in managing cardiometabolic risk. However, the effects are context-dependent, influenced by factors such as protein source (animal vs. vegetable), individual age, and pre-existing health conditions.
Notably, recent evidence suggests a nuanced cardiovascular risk profile for high-protein diets. A large prospective cohort study from the UK Biobank found that high protein intake (≥1.8 g·kg⁻¹·day⁻¹) was associated with increased risk of major adverse cardiovascular events (MACE), particularly in participants aged over 55 years (HR=1.36) [114]. This highlights the importance of considering demographic factors in dietary recommendations.
For researchers and drug development professionals, these findings suggest several strategic implications. First, the glucoregulatory mechanisms of BCAAs, particularly leucine-mediated hypothalamic signaling, represent promising targets for novel therapeutic agents. Second, the differential effects of various dietary patterns on specific cardiometabolic parameters support a personalized medicine approach to nutritional interventions. Finally, the potential age-dependent risks associated with high protein intake warrant careful consideration in long-term intervention studies and drug safety assessments.
Future research should prioritize long-term randomized controlled trials comparing isocaloric diets matched for protein sources, investigations into the molecular mechanisms underlying the age-dependent effects of high protein intake, and studies exploring synergistic effects of combining dietary approaches (e.g., Mediterranean-inspired high-protein diets) for optimal cardiometabolic outcomes.
Conclusion
High-protein diets demonstrate significant potential for improving glycemic control through multiple physiological mechanisms, including direct insulinotropic effects, hypothalamic signaling, and incretin pathway modulation. Clinical evidence supports their efficacy, particularly in short-term interventions and when implemented through diabetes-specific nutritional formulations. However, response variability, long-term sustainability concerns, and unresolved questions about optimal protein sources necessitate a personalized medicine approach. Future research should focus on identifying biomarkers for predicting individual responses, developing targeted protein-based therapeutics that mimic beneficial effects without requiring high dietary intake, and conducting long-term safety studies. For drug development, understanding protein-derived peptides and their receptors may reveal novel targets for next-generation diabetes medications that harness these natural metabolic pathways without the practical challenges of dietary adherence.
References
- 1. Mechanisms of amino acid-stimulated insulin secretion in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3527006/]
- 2. Beta cells intrinsically sense and limit their secretory ... [https://www.sciencedirect.com/science/article/pii/S2211124725004188]
- 3. High and normal protein diets improve body composition ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10421635/]
- 4. High protein diet leads to prediabetes remission and ... [https://www.sciencedirect.com/science/article/abs/pii/S0939475320305044]
- 5. Effects of High-Protein Versus High-Carbohydrate Diets on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3687312/]
- 6. An increase in dietary protein improves the blood glucose ... [https://www.sciencedirect.com/science/article/pii/S0002916522033822]
- 7. Hypothalamic Leucine Metabolism Regulates Liver Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3237640/]
- 8. Hypothalamic leucine metabolism regulates liver glucose ... [https://pubmed.ncbi.nlm.nih.gov/22187376/]
- 9. Frontiers | CNS Control of Glucose Metabolism: Response ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2013.00020/full]
- 10. 高蛋白和正常蛋白饮食可改善2 型糖尿病成人的身体成分 ... [https://suppr.wilddata.cn/browses/detail/pubmed/37475689]
- 11. 高蛋白低碳飲食:有效改善2型糖尿病血糖控制 [https://www.ok1.com.tw/%E9%AB%98%E8%9B%8B%E7%99%BD-%E4%BD%8E%E7%A2%B3%E9%A3%B2%E9%A3%9F-%E6%94%B9%E5%96%84-2%E5%9E%8B%E7%B3%96%E5%B0%BF%E7%97%85-%E8%A1%80%E7%B3%96%E6%8E%A7%E5%88%B6]
- 12. 四種不同飲食法對糖尿病管理的效果 - 蔡明劼醫師 [https://tsai63.com/blog/f60a7731-b297-4405-9e67-a5bef1117404]
- 13. 陈雁 [http://www.sinh.cas.cn/rcdw/qtyjzz/202312/t20231211_6908469.html]
- 14. Leucine alters hepatic glucose/lipid homeostasis via the ... [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/1868-7083-6-27]
- 15. Mechanisms of action and therapeutic applications of GLP-1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11304055/]
- 16. Effect of high intakes of protein-only and carbohydrate ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1618142/full]
- 17. Protein- and Calcium-Mediated GLP-1 Secretion [https://pmc.ncbi.nlm.nih.gov/articles/PMC8634310/]
- 18. The agony and the efficacy: central mechanisms of GLP-1 ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1530985/full]
- 19. Glucagon-like peptide-1 receptor: mechanisms and ... [https://www.nature.com/articles/s41392-024-01931-z]
- 20. How to activate GLP-1 naturally - Ohio State Health & Discovery [https://health.osu.edu/wellness/exercise-and-nutrition/activiating-glp-1-naturally]
- 21. GIP Receptor: Activation and Blockade Support Weight Loss [https://www.dzd-ev.de/en/press/press-releases/press-releases-2025/gip-receptor-activation-and-blockade]
- 22. Mechanisms of Glucose Absorption in the Small Intestine ... [https://www.mdpi.com/2072-6643/13/7/2474]
- 23. Glucose absorption by isolated, vascularly perfused rat intestine [https://pmc.ncbi.nlm.nih.gov/articles/PMC11971594/]
- 24. Can high-protein diabetes-specific oral nutritional ... - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623745/]
- 25. Can high-protein diabetes-specific oral nutritional ... [https://pubmed.ncbi.nlm.nih.gov/41249140/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=pubmed-2&utm_content=1fgJURi2yzL9sGmXbwcyPtaNovqHTlNxYiKFYYJpQR9J93lY5m&fc=20230328041640&ff=20251118061432&v=2.18.0.post22+67771e2]
- 26. Comparative efficacy of dietary interventions for glycemic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12127149/]
- 27. Efficacy of a High-Protein Diet to Lower Glycemic Levels in ... [https://www.mdpi.com/1422-0067/25/20/10959]
- 28. The efficacy of low-carbohydrate diets on glycemic control in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12362953/]
- 29. Glucose absorption in the duodenum is modulated by an ... [https://pubmed.ncbi.nlm.nih.gov/40716951/]
- 30. Dexamethasone enhances intestinal glucose absorption ... [https://www.nature.com/articles/s41598-025-22312-8]
- 31. Dietary proteins, amino acids and insulin resistance: a mini ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1671286/full]
- 32. BCAAs acutely drive glucose dysregulation and insulin ... [https://www.nature.com/articles/s41387-024-00298-y]
- 33. The role of branched-chain amino acids and their downstream ... [https://www.frontierspartnerships.org/journals/journal-of-pharmacy-pharmaceutical-sciences/articles/10.3389/jpps.2024.13040/full]
- 34. Branched-chain amino acid metabolism, insulin sensitivity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7801320/]
- 35. Can high-protein diabetes-specific oral nutritional ... [https://pubmed.ncbi.nlm.nih.gov/41249140/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1-MHQbRSTjFbtlTjjVNcCLd_MJgXZfuQ2pPbAN6NaUGgWTvYKi&fc=None&ff=20251124161638&v=2.18.0.post22+67771e2]
- 36. Dietary proteins, amino acids and insulin resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12580144/]
- 37. Dietary proteins, amino acids and insulin resistance [https://pubmed.ncbi.nlm.nih.gov/41190149/]
- 38. Can high-protein diabetes-specific oral nutritional ... [https://www.nature.com/articles/s41387-025-00399-2]
- 39. Impact of diabetes-specific nutrition formulas on time in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12508538/]
- 40. Diabetes-specific oral nutritional supplement for ... [https://www.e-nrp.org/DOIx.php?id=10.4162/nrp.2025.19.e50]
- 41. The role of high-protein diets in the management ... [https://pubmed.ncbi.nlm.nih.gov/40889146/]
- 42. Comparative efficacy of dietary interventions for glycemic ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1512493/full]
- 43. Effects of daily protein intake frequency during 8 weeks ... [https://pubmed.ncbi.nlm.nih.gov/40673785/]
- 44. Dietary Protein Distribution Positively Influences 24-h ... [https://www.sciencedirect.com/science/article/pii/S0022316622009087]
- 45. How Much Protein Can You Really “Use” From a Single ... [https://massresearchreview.com/2025/06/27/how-much-protein-can-you-really-use-from-a-single-meal/]
- 46. High-Protein Time-Restricted Eating Alongside Resistance ... [https://pubmed.ncbi.nlm.nih.gov/40796095/]
- 47. The effect of intermittent fasting on insulin resistance, lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12363089/]
- 48. Intermittent energy restriction may improve outcomes in ... [https://www.endocrine.org/news-and-advocacy/news-room/endo-annual-meeting/endo-2025-press-releases/zhang-press-release]
- 49. High‐protein vs. standard‐protein diets in overweight and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8006643/]
- 50. Impact of high-protein, low-calorie diet on anthropometric ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1619543/full]
- 51. Low-calorie, high-protein diets, regardless of ... [https://pubmed.ncbi.nlm.nih.gov/39420528/]
- 52. Protein Source Determines the Effectiveness of High ... [https://pubmed.ncbi.nlm.nih.gov/41156477/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=0AhWt5D3W3g62p87Qtuk_bQQhhrxeJ8D7RfAjnUePhC&fc=None&ff=20251030204719&v=2.18.0.post22+67771e2]
- 53. Prioritizing Plant-Based Protein in the Scientific Report of ... [https://www.pcrm.org/news/news-releases/prioritizing-plant-based-protein-scientific-report-2025-2030-dietary-guidelines]
- 54. Adhering to recommended dietary protein intake for optimizing ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d4ra08221d]
- 55. Understanding Dietary Protein Quality: Digestible ... [https://www.sciencedirect.com/science/article/pii/S0022316625004286]
- 56. Association of a high-protein and low-glycemic-index diet ... [https://www.nature.com/articles/s41430-025-01666-2]
- 57. Plant-based diets and risk of type 2 diabetes [https://pubmed.ncbi.nlm.nih.gov/40789787/]
- 58. Red meat consumption associated with increased type 2 ... [https://hsph.harvard.edu/news/red-meat-consumption-associated-with-increased-type-2-diabetes-risk/]
- 59. College of Health and Human Sciences [https://www.purdue.edu/hhs/news/2025/07/purdue-nutrition-science-research-examines-metabolic-health-effects-of-red-meat-during-grilling-season/]
- 60. Protein Source Determines the Effectiveness of High ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567468/]
- 61. Protein Source Determines the Effectiveness of High ... [https://www.mdpi.com/2072-6643/17/20/3225]
- 62. Heidelberg Pharma Announces New Clinical Data on Lead ... [https://heidelberg-pharma.com/en/press-investors/announcements/press-releases-and-ad-hoc-announcements/pr-heidelberg-pharma-announces-new-clinical-data-on-lead-atac-candidate-hdp-101-to-be-presented-at-international-myeloma-society-annual-meeting-2025]
- 63. HDP-101 Receives FDA Fast Track Designation in Multiple ... [https://www.cancernetwork.com/view/hdp-101-receives-fda-fast-track-designation-in-multiple-myeloma]
- 64. Both high-protein and normal-protein diets are effective for ... [https://www.uab.edu/news/research-innovation/both-high-protein-and-normal-protein-diets-are-effective-for-t2d-management]
- 65. Comparative effects of different macronutrient compositions for ... [https://jhpn.biomedcentral.com/articles/10.1186/s41043-025-00818-1]
- 66. Effects of high-protein diet on glycemic control, insulin ... [https://www.sciencedirect.com/science/article/abs/pii/S0261561419330201]
- 67. Genetics of diabetes and its complications: a comprehensive ... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-025-01748-y]
- 68. Dietary protein and risk of type 2 diabetes - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12134278/]
- 69. A short-term, high-caloric diet has prolonged effects on ... [https://www.nature.com/articles/s42255-025-01226-9]
- 70. Long-term effects of dietary protein and carbohydrate ... [https://link.springer.com/article/10.1007/s00125-025-06560-x]
- 71. Protein, fiber, and exercise: a narrative review of their roles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255039/]
- 72. Daily Dietary Protein Distribution Does Not Influence ... [https://www.sciencedirect.com/science/article/pii/S0022316624000956]
- 73. Reporting of environmental outcomes in randomised clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12458732/]
- 74. Randomized phase I trial outcomes show safe and ... [https://www.nature.com/articles/s41467-025-62925-1]
- 75. Diabetes and Renal Complications: An Overview on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11118045/]
- 76. DASH Diet Modified for Diabetes Lowers Blood Sugar Levels ... [https://publichealth.jhu.edu/2025/dash-diet-modified-for-diabetes-lowers-blood-sugar-levels-in-clinical-trial-of-adults-with-type-2-diabetes]
- 77. Effects of different dietary patterns on glucose management ... [https://www.sciencedirect.com/science/article/pii/S2589537025001543]
- 78. Type 2 diabetes mellitus with chronic kidney disease benefits ... [https://bmcnutr.biomedcentral.com/articles/10.1186/s40795-025-01119-w]
- 79. Current Guidelines on Dietary Protein Intake for Patients ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538418/]
- 80. Kidney failure risk higher for adults with diabetes, low eGFR [https://www.healio.com/news/nephrology/20250922/realworld-study-reveals-risks-for-kidney-failure-death-for-adults-with-diabetes]
- 81. Postprandial effects of dietary protein source on metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10278248/]
- 82. The long-term association of different dietary protein ... [https://www.nature.com/articles/s41598-021-98688-0]
- 83. The impact of dietary protein intake on longevity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6562018/]
- 84. Effect of Protein Intake on Visceral Abdominal Fat and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8140050/]
- 85. Comparative effects of different macronutrient compositions for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11977911/]
- 86. Low‐calorie, high‐protein diets, regardless ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11618321/]
- 87. Dietary protein restriction elevates FGF21 levels and ... [https://www.nature.com/articles/s42255-025-01236-7]
- 88. Differences in the insulin counterregulatory hormones ... [https://www.nature.com/articles/s41598-025-89543-7]
- 89. Clinical Evidence and Mechanisms of High-Protein Diet ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7539343/]
- 90. Effects of a high-protein/low carbohydrate versus ... [https://pubmed.ncbi.nlm.nih.gov/26166555/]
- 91. The effect of psyllium on fasting blood sugar, HbA1c, ... [https://pubmed.ncbi.nlm.nih.gov/38844885/]
- 92. The effect of psyllium on fasting blood sugar, HbA1c, HOMA IR ... [https://bmcendocrdisord.biomedcentral.com/articles/10.1186/s12902-024-01608-2]
- 93. Effects of dietary fiber on glycemic control and insulin ... [https://www.sciencedirect.com/science/article/pii/S1756464621001493]
- 94. Efficacy of Low-Carbohydrate Diets Versus Low-Fat Diets ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11797075/]
- 95. A High Protein Diet Is More Effective in Improving Insulin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8707429/]
- 96. Low-Carbohydrate Diet Patterns That Favor High-Quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12221638/]
- 97. Low-Carbohydrate Diet Patterns That Favor High-Quality ... [https://www.sciencedirect.com/science/article/pii/S2475299125029403]
- 98. Ketogenic Diet - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK499830/]
- 99. Ketogenic diet for human diseases: the underlying ... [https://www.nature.com/articles/s41392-021-00831-w]
- 100. Long-Term Efficacy and Safety of a Low-Carbohydrate Diet in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476234/]
- 101. Real-world effect of intermittent calorie-restricted diet on ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1648314/full]
- 102. Efficacy of a Homemade Very Low Calorie Diet to Achieve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12461181/]
- 103. Development and Pragmatic Randomized Controlled Trial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11677078/]
- 104. Very low-calorie ketogenic diet (VLCKD): an antihypertensive ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-023-03956-4]
- 105. Very Low-Calorie Ketogenic Diet (VLCKD) as Pre- ... [https://www.mdpi.com/2072-6643/15/8/1907]
- 106. Ketogenic Diets for Body Weight Loss: A Comparison with ... [https://www.mdpi.com/2072-6643/17/6/965]
- 107. A pilot study examining a ketogenic diet as an adjunct ... [https://www.nature.com/articles/s41398-025-03544-8]
- 108. Efficacy of Low-Carbohydrate vs. Conventional Diets in ... [https://nhsjs.com/2025/efficacy-of-low-carbohydrate-vs-conventional-diets-in-type-2-diabetes-remission-the-role-of-carbohydrate-intake-threshold-a-systematic-review/]
- 109. Low-Calorie, High-Protein Ketogenic Diet ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114320/]
- 110. Comparative effect of dietary patterns on selected ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12328653/]
- 111. Impact of Dietary Patterns on the Lipidemic Profile and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389368/]
- 112. Effects of High Protein and Balanced Diets on Lipid Profiles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5036282/]
- 113. Association Between Protein Intake and Blood Pressure [https://pmc.ncbi.nlm.nih.gov/articles/PMC6593153/]
- 114. Associations between High Protein Intake and ... [https://www.sciencedirect.com/science/article/pii/S1279770725002520]