Glucose Prediction Model Showdown: A Comparative Analysis of Logistic Regression, LSTM, and ARIMA for Clinical and Research Applications
This article provides a comprehensive, evidence-based analysis of the predictive accuracy, clinical applicability, and operational trade-offs of three prominent glucose forecasting models: Logistic Regression, Long Short-Term Memory (LSTM) networks, and...
Glucose Prediction Model Showdown: A Comparative Analysis of Logistic Regression, LSTM, and ARIMA for Clinical and Research Applications
Abstract
This article provides a comprehensive, evidence-based analysis of the predictive accuracy, clinical applicability, and operational trade-offs of three prominent glucose forecasting models: Logistic Regression, Long Short-Term Memory (LSTM) networks, and the Auto-Regressive Integrated Moving Average (ARIMA). Tailored for researchers and drug development professionals, it synthesizes recent findings on model performance across different prediction horizons and patient populations, from septic ICU patients to free-living individuals with diabetes. The review covers foundational principles, methodological deployment, optimization strategies to address common challenges like data scarcity and privacy, and a rigorous comparative validation. The objective is to guide the selection and development of robust, clinically actionable models for improving diabetes management and therapeutic development.
Foundations of Glucose Prediction: Understanding the Core Models and Clinical Imperatives
The Critical Need for Accurate Glucose Forecasting in Diabetes and Critical Care
Accurate forecasting of blood glucose levels is a cornerstone for modern diabetes management and critical care. It enables proactive interventions to prevent dangerous glycemic events, thereby reducing patient morbidity and mortality. Within this field, a key research focus involves the comparative evaluation of predictive models, including Autoregressive Integrated Moving Average (ARIMA), logistic regression, and Long Short-Term Memory (LSTM) networks. Each model offers distinct advantages and limitations, making them suitable for different clinical scenarios and prediction horizons. This guide provides an objective comparison of these models' performance, supported by experimental data and detailed methodologies, to inform researchers and healthcare professionals in selecting the optimal tool for specific applications.
Performance Comparison at a Glance
The performance of ARIMA, logistic regression, and LSTM models varies significantly depending on the prediction horizon and the specific glycemic class of interest (hypoglycemia, euglycemia, or hyperglycemia). The following tables summarize key quantitative findings from comparative studies.
Table 1: Model Performance for 15-Minute Prediction Horizon (Recall Rates %) [1] [2]
| Glycemic Class | Logistic Regression | LSTM | ARIMA |
|---|---|---|---|
| Hypoglycemia (<70 mg/dL) | 98% | Underperformed Logistic Regression | Underperformed |
| Euglycemia (70-180 mg/dL) | 91% | Underperformed Logistic Regression | Underperformed |
| Hyperglycemia (>180 mg/dL) | 96% | Underperformed Logistic Regression | Underperformed |
Table 2: Model Performance for 1-Hour Prediction Horizon (Recall Rates %) [1] [2]
| Glycemic Class | Logistic Regression | LSTM | ARIMA |
|---|---|---|---|
| Hypoglycemia (<70 mg/dL) | Underperformed LSTM | 87% | Underperformed |
| Euglycemia (70-180 mg/dL) | Information Not Provided | Information Not Provided | Underperformed |
| Hyperglycemia (>180 mg/dL) | Underperformed LSTM | 85% | Underperformed |
Table 3: Summary of Model Strengths and Weaknesses
| Model | Best For | Key Limitations |
|---|---|---|
| Logistic Regression | Short-term classification (e.g., 15-minute horizon), especially for hypoglycemia [1] [2]. | Performance degrades at longer prediction horizons [1]. |
| LSTM | Longer-term forecasting (e.g., 1-hour horizon), capturing complex temporal patterns [1] [3]. | Requires large amounts of training data; computationally complex [3]. |
| ARIMA | Small datasets; linear trends; computationally efficient [3]. | Poor performance on non-stationary data; struggles with complex nonlinear patterns and long-term dependencies [1] [3]. |
Detailed Experimental Protocols
To ensure the validity and reproducibility of comparative studies, researchers adhere to rigorous experimental protocols encompassing data collection, preprocessing, and model training.
Data Collection and Preprocessing
- Data Sources: Research typically utilizes two primary data sources: real-patient data from clinical cohort studies and in-silico data generated by simulators like the CGM Simulator (e.g., Simglucose v0.2.1). Real-patient data includes CGM readings, insulin dosing, and carbohydrate intake [1].
- Data Cleaning and Alignment: Raw data is pre-processed to address gaps and bad entries. Time-series data is aligned to a consistent frequency (e.g., 15-minute intervals). Measurements taken in very quick succession (e.g., within 5-minute windows) may be excluded to avoid over-representing a single glycemic episode [1] [4].
- Feature Engineering: For models that rely solely on CGM data, features are engineered from the glucose time series itself. These can include:
Model Training and Evaluation
- Outcome Definition: For classification tasks, glycemic states are defined as:
- Hypoglycemia: Glucose < 70 mg/dL
- Euglycemia: Glucose 70-180 mg/dL
- Hyperglycemia: Glucose > 180 mg/dL [1]
- Prediction Horizon: Models are trained to predict glucose levels at specific future time points, such as 15 minutes or 1 hour ahead [1].
- Performance Metrics: Models are evaluated using standard metrics, including:
- Precision: The proportion of correct positive predictions among all positive predictions.
- Recall (Sensitivity): The proportion of actual positives that were correctly identified. This is critical for detecting dangerous events like hypoglycemia [1].
- Accuracy: The overall proportion of correct predictions.
- F1-Score: The harmonic mean of precision and recall [1].
- Root Mean Squared Error (RMSE): Commonly used for regression tasks to measure the average prediction error [3].
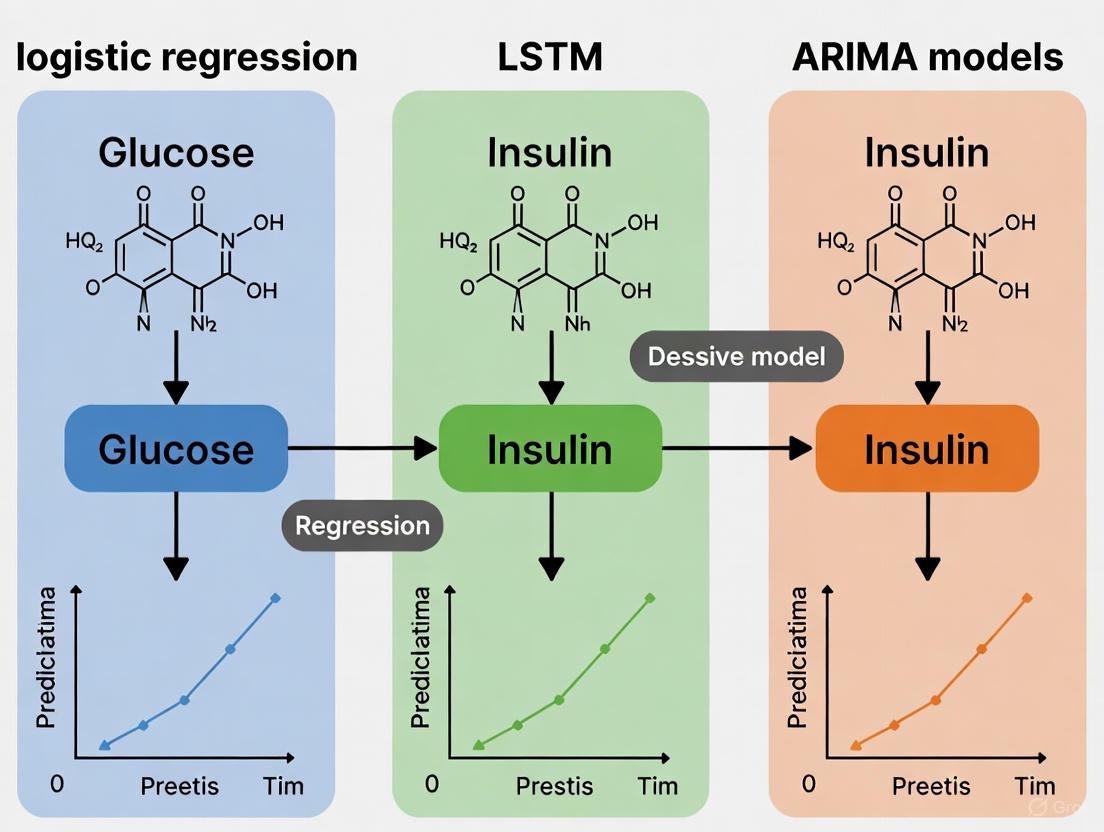
Figure 1: Experimental Workflow for Comparative Model Analysis. This diagram outlines the key stages in a typical study comparing glucose prediction models, from data preparation to final analysis.
Model Selection Logic
Choosing the right model depends on the specific clinical requirement, particularly the needed prediction horizon and the primary glycemic risk.
Figure 2: A Logic Flow for Selecting a Glucose Prediction Model. This chart guides the initial selection of a model based on key project constraints and goals.
The Researcher's Toolkit
Successful development and deployment of glucose forecasting models rely on a suite of essential computational and data resources.
Table 4: Essential Research Reagents and Solutions for Glucose Forecasting Research
| Tool / Resource | Function / Description | Relevance in Research |
|---|---|---|
| Continuous Glucose Monitoring (CGM) Simulator | Software (e.g., Simglucose) that generates synthetic, physiologically plausible CGM data for in-silico testing [1]. | Allows for initial algorithm development and validation in a controlled environment before clinical trials. |
| Federated Learning (FL) Framework | A decentralized machine learning approach where models are trained locally on devices or servers, and only model parameters are shared [5]. | Addresses data privacy concerns by enabling collaborative model training without sharing sensitive patient data. |
| Specialized Loss Functions (e.g., HH Loss) | A cost-sensitive loss function that assigns a higher penalty to prediction errors in the hypoglycemic and hyperglycemic ranges [5]. | Improves model performance on critical glycemic excursions, which are often rare events in imbalanced datasets. |
| Global Burden of Disease (GBD) Data | Comprehensive annual time-series data on diabetes prevalence, deaths, and disability-adjusted life years (DALYs) [3]. | Used for macro-level forecasting of diabetes burden to inform public health policy and resource allocation. |
| Time-Series Analysis Libraries (e.g., pmdarima) | Software libraries that provide implementations for models like ARIMA, often with automated parameter search [6]. | Accelerates model development and benchmarking by providing optimized, ready-to-use statistical models. |
The comparative analysis of ARIMA, logistic regression, and LSTM models reveals a clear trade-off between predictive accuracy, horizon, and computational complexity. No single model is universally superior. Logistic regression excels as a highly accurate and likely efficient tool for short-term classification of glycemic states, particularly for critical hypoglycemia prediction. In contrast, LSTM networks demonstrate stronger capabilities for longer-term forecasting by capturing complex, non-linear temporal dependencies, albeit with greater data and computational demands. ARIMA models, while computationally efficient, are consistently outperformed by machine learning approaches in handling the complexities of glucose dynamics. The choice of model must therefore be driven by the specific clinical application, available data, and required prediction horizon. Future research directions point towards hybrid, ensemble, and personalized models to further enhance accuracy and reliability in both individual patient management and population-level health forecasting.
Effective glucose management is crucial for individuals with diabetes to prevent both acute risks and long-term complications. The development of Continuous Glucose Monitoring (CGM) systems has generated vast amounts of data, creating opportunities for predictive modeling to enhance clinical decision-making. Within this context, probabilistic classification models have emerged as valuable tools for forecasting glycemic events, enabling proactive interventions to prevent dangerous glucose excursions. This guide focuses on logistic regression as a fundamental yet powerful probabilistic classification technique, objectively comparing its performance with other modeling approaches including Long Short-Term Memory (LSTM) networks and Autoregressive Integrated Moving Average (ARIMA) models within the specific domain of glycemic event prediction.
The core strength of logistic regression lies in its ability to estimate the probability of a categorical outcome—in this case, whether a future glucose reading will fall into hypoglycemic, euglycemic, or hyperglycemic ranges. Unlike regression models that predict continuous glucose values, classification models directly address the clinical question of most relevance: "What is the risk of a future hypoglycemic or hyperglycemic event?" This probabilistic framework supports clinical decision-making by quantifying risk in an interpretable manner [1].
Model Comparison: Performance Across Prediction Horizons
Quantitative Performance Metrics
Extensive research has evaluated the performance of various models for predicting glycemic events across different time horizons. The table below summarizes key findings from a comprehensive 2023 study that directly compared logistic regression, LSTM, and ARIMA models for classifying hypoglycemia (<70 mg/dL), euglycemia (70-180 mg/dL), and hyperglycemia (>180 mg/dL) at 15-minute and 1-hour prediction horizons [1].
Table 1: Model Performance Comparison for Glycemic Event Classification
| Model | Prediction Horizon | Hypoglycemia Recall | Euglycemia Recall | Hyperglycemia Recall | Overall Accuracy |
|---|---|---|---|---|---|
| Logistic Regression | 15 minutes | 98% | 91% | 96% | High |
| LSTM | 15 minutes | Lower than LR | Lower than LR | Lower than LR | Moderate |
| ARIMA | 15 minutes | Lowest of all models | Lowest of all models | Lowest of all models | Poor |
| Logistic Regression | 1 hour | Lower than LSTM | Lower than LSTM | Lower than LSTM | Moderate |
| LSTM | 1 hour | 87% | Lower than 15-min | 85% | High |
| ARIMA | 1 hour | Lowest of all models | Lowest of all models | Lowest of all models | Poor |
Clinical Application Analysis
The performance differentials revealed in these comparisons have significant clinical implications. Logistic regression's superior performance at the 15-minute horizon—particularly its 98% recall rate for hypoglycemia—makes it exceptionally valuable for immediate intervention planning. This high sensitivity to impending hypoglycemic events is crucial for preventing acute complications, as missing such events could have serious consequences for patients [1].
In contrast, LSTM's strength at the 1-hour prediction horizon supports longer-term planning, potentially helping patients and clinicians make adjustments to insulin dosing, carbohydrate intake, or physical activity with sufficient lead time. The performance degradation observed in all models as the prediction horizon extends highlights the inherent challenges in glucose forecasting, particularly given the complex physiological processes and external factors affecting glucose dynamics [1] [7].
ARIMA's consistent underperformance across all categories and time horizons suggests it is less suitable for glycemic event classification compared to machine learning approaches. This is likely because ARIMA models are designed for stationary time series and struggle to capture the complex, non-linear relationships that characterize glucose metabolism [1].
Experimental Protocols and Methodologies
Data Collection and Preprocessing Standards
The experimental foundation for comparing glycemic prediction models requires rigorous data collection and preprocessing protocols. Research in this domain typically utilizes two primary data sources: real-world clinical cohort studies and in-silico simulations. In a representative study, real patient data was obtained from 11 participants with type 1 diabetes using CGM devices, with data collected at 15-minute intervals. Simultaneously, simulated data was generated using the Simglucose platform (v0.2.1), creating 10 virtual patients across three age groups (adults, adolescents, children) spanning 10 days with randomized meal and snack patterns [1].
Data preprocessing involves several critical steps to ensure data quality and consistency. Raw CGM data typically requires resampling to a consistent 15-minute frequency, handling of missing values through appropriate imputation methods, and filtering of physiologically implausible values. For hypoglycemia classification studies, data is often structured around hypoglycemic events, defined as episodes with registered glucose levels <3.5 mmol/L (<63 mg/dL). For each event, a time series encompassing the preceding and subsequent 6 hours (12 hours total) from the first recorded hypoglycemic level is extracted for analysis [8].
Table 2: Standard Data Preparation Pipeline
| Processing Step | Description | Purpose |
|---|---|---|
| Data Harmonization | Downsampling all data to 15-minute intervals | Standardize temporal resolution across different sensors |
| Event Definition | Identifying hypoglycemic events (<70 mg/dL) and extracting 12-hour windows around them | Create consistent analysis units |
| Feature Engineering | Calculating rate of change, variability indices, and time-based features | Enhance predictive signal from raw glucose data |
| Data Splitting | Stratified splitting into training (80%), validation (10%), and test sets (10%) | Ensure robust evaluation and prevent data leakage |
Feature Engineering Strategies
Feature engineering is a critical component in developing effective glycemic classification models. When only glucose data is available—whether due to data collection limitations or patient non-compliance—features extracted from the changes in glucose levels themselves become particularly valuable. These engineered features capture the dynamism and trends in glucose fluctuations, enabling more accurate predictions even without additional physiological metrics [1].
Key feature categories include:
- Rate of change metrics: Short-term and long-term glucose velocity calculated over different windows
- Variability indices: Standard deviation, coefficient of variation, and mean amplitude of glycemic excursion
- Time-based features: Rolling averages, seasonal decompositions, and time-of-day indicators
- Threshold-based features: Percentage of time spent in different glycemic ranges prior to prediction point
For studies incorporating additional data modalities, features might include insulin-on-board calculations, carbohydrate intake timing and quantity, and exercise characteristics (type, duration, intensity). However, research has demonstrated that models built with CGM data alone can achieve statistically indistinguishable performance compared to models using multiple data modalities, highlighting the particular value of carefully engineered glucose-derived features [7].
Model Training and Evaluation Framework
The evaluation of glycemic classification models follows rigorous machine learning protocols. Studies typically employ repeated stratified nested cross-validation to ensure reliable performance estimation and mitigate overfitting. This approach is particularly important given the class imbalance often present in glycemic event data, where hypoglycemic events may be significantly less frequent than euglycemic periods [7].
Performance metrics are selected to provide a comprehensive view of model capabilities:
- Recall (Sensitivity): Particularly crucial for hypoglycemia prediction, where missing events has serious consequences
- Precision: Important for minimizing false alarms that could lead to alert fatigue
- Area Under the Receiver Operating Characteristic Curve (AUROC): Provides an aggregate measure of performance across classification thresholds
- Calibration: Assesses how well predicted probabilities match observed frequencies, often measured using Brier scores
For clinical applicability, models must demonstrate not only high discrimination but also excellent calibration. Well-calibrated models ensure that a predicted hypoglycemia probability of 80% corresponds to an actual hypoglycemia occurrence rate of approximately 80%, enabling clinicians and patients to appropriately weigh risks and benefits of interventions [7].
Technical Implementation Guide
Research Reagent Solutions
Implementing effective glycemic classification models requires specific data components and computational resources. The table below details essential "research reagents" for developing logistic regression models for glycemic event prediction.
Table 3: Essential Research Reagents for Glycemic Classification Studies
| Reagent Category | Specific Components | Function in Analysis |
|---|---|---|
| Data Sources | Real-world CGM data (Dexcom G6, Medtronic Guardian), Simulated data (Simglucose, UVA/Padova Simulator) | Provides foundational glucose traces for model development and validation |
| Feature Engineering Tools | Rolling window calculators, Variability indices, Time-based feature extractors | Transforms raw glucose data into predictive features |
| Modeling Frameworks | Scikit-learn (logistic regression), TensorFlow/PyTorch (LSTM), Statsmodels (ARIMA) | Provides algorithmic implementations for model training |
| Evaluation Metrics | Recall, Precision, AUROC, Brier score, Consensus Error Grid analysis | Quantifies model performance and clinical safety |
Comparative Workflow Visualization
The following diagram illustrates the structured workflow for developing and comparing glycemic event classification models, from data preparation through performance evaluation:
Advanced Modeling Considerations
Emerging Approaches in Glucose Forecasting
While this guide focuses on logistic regression, LSTM, and ARIMA models, recent research has explored more advanced architectures. Transformer-based models, including PatchTST and Crossformer, have demonstrated remarkable performance in multi-horizon blood glucose prediction. For 30-minute predictions, Crossformer achieved an RMSE of 15.6 mg/dL on the OhioT1DM dataset, while PatchTST excelled at longer-term predictions (1-4 hours) [9].
Additionally, Large Language Model (LLM) frameworks have shown promise in glucose forecasting. The Gluco-LLM framework, leveraging Time-LLM, reportedly achieves a 21.87% reduction in prediction error compared to state-of-the-art models, with 96.19% of predictions falling within clinically acceptable ranges on the Consensus Error Grid [10].
Another emerging approach focuses specifically on classifying the root causes of hypoglycemic events. Purpose-built convolutional neural networks (HypoCNN) have demonstrated strong performance in identifying underlying reasons for hypoglycemia, such as overestimated bolus (27% of cases), overcorrection of hyperglycemia (29%), and excessive basal insulin pressure (44%), achieving an AUC of 0.917 on ground-truth validation [8].
Practical Implementation Challenges
Translating glycemic classification models from research to clinical practice faces several significant challenges. The "black box" nature of complex models like LSTM and transformer networks can limit clinical trust and adoption, as clinicians and patients may struggle to understand or trust recommendations without transparent reasoning [11].
Data quality and availability present additional hurdles. While studies have shown that models using CGM data alone can achieve excellent performance for exercise-related glycemic events (AUROCs ranging from 0.880 to 0.992), real-world implementation must contend with missing data, sensor errors, and compression artifacts [7].
Furthermore, model performance can vary across different patient subgroups and clinical contexts. Performance degradation may occur when models trained on general populations are applied to specific scenarios like exercise conditions or critical care settings. In septic patients, for instance, unique glucose dynamics due to stress hyperglycemia may require specialized modeling approaches [12].
The comparative analysis presented in this guide demonstrates that model selection for glycemic event classification depends critically on the specific clinical requirements and prediction horizon. Logistic regression emerges as the superior choice for short-term (15-minute) predictions, particularly with its exceptional recall for hypoglycemia events. LSTM networks show strength for longer-term (1-hour) forecasting, while ARIMA models consistently underperform for classification tasks.
For clinical implementation, researchers should consider the trade-off between model complexity and interpretability. While more complex models may offer marginal performance gains in some scenarios, logistic regression provides an compelling combination of high performance, computational efficiency, and interpretability—particularly valuable in clinical settings where understanding model reasoning is as important as prediction accuracy itself.
Future directions in glycemic event classification will likely involve hybrid approaches that combine the strengths of multiple models, ensemble methods that improve robustness, and explainable AI techniques that enhance clinical trust and adoption. As these technologies evolve, probabilistic classification models will play an increasingly important role in creating personalized, adaptive diabetes management systems.
Accurate prediction of blood glucose levels is a cornerstone of modern diabetes management, enabling proactive interventions to prevent dangerous hypoglycemic and hyperglycemic events. Within the field of predictive modeling, three distinct approaches have emerged as prominent solutions: traditional statistical models like the Autoregressive Integrated Moving Average (ARIMA), conventional machine learning algorithms such as Logistic Regression, and advanced deep learning architectures, particularly Long Short-Term Memory (LSTM) networks. Each paradigm offers different capabilities for handling the complex, time-dependent nature of glucose dynamics. LSTMs, a specialized form of recurrent neural network, are uniquely designed to capture long-range temporal dependencies, making them exceptionally suitable for modeling the physiological patterns in glucose data. This guide provides a comparative analysis of these models, focusing on their predictive performance, implementation requirements, and suitability for real-world clinical and research applications.
Performance Comparison at a Glance
The table below summarizes the key performance metrics of LSTM, ARIMA, and Logistic Regression models as reported in recent studies, providing a high-level overview of their capabilities for glucose level prediction.
Table 1: Overall Model Performance for Glucose Prediction
| Model | Best Prediction Horizon | Key Strengths | Reported Performance (Recall/RMSE) | Primary Clinical Utility |
|---|---|---|---|---|
| LSTM | 60 minutes [1] | Captures complex temporal patterns; handles multivariate data [13] | 87% (Hypo/Hyperglycemia, 1-Hour) [1]; RMSE: 20.50 ± 5.66 mg/dL (Aggregated) [13] | Ideal for medium-term forecasting and proactive insulin dosing in artificial pancreas systems. |
| Logistic Regression | 15 minutes [1] | High speed and interpretability; effective for short-term classification [1] | 98% (Hypoglycemia, 15-Min) [1] | Excellent for real-time, short-term alerts for imminent hypoglycemia. |
| ARIMA | Varies | Statistical robustness; efficient for univariate, stationary series [14] [15] | Outperformed by LSTM and Ridge Regression [15] | Serves as a baseline model; most effective when glucose trends are stable and linear. |
A more detailed quantitative comparison across different prediction horizons and metrics reveals the nuanced performance profile of each model.
Table 2: Detailed Quantitative Performance Comparison
| Model | Prediction Horizon | Performance Metric | Result | Dataset / Context |
|---|---|---|---|---|
| LSTM | 60 minutes | Recall (Hypo/Hyperglycemia) | 85%, 87% [1] | Real patient CGM data [1] |
| 60 minutes | RMSE (Aggregated Training) | 20.50 ± 5.66 mg/dL [13] | HUPA UCM Dataset (25 subjects) [13] | |
| 60 minutes | RMSE (Individual Training) | 22.52 ± 6.38 mg/dL [13] | HUPA UCM Dataset (25 subjects) [13] | |
| 30 & 60 minutes | RMSE | 6.45 & 17.24 mg/dL [16] | OhioT1DM Dataset [16] | |
| Logistic Regression | 15 minutes | Recall (Hypoglycemia) | 98% [1] | Real patient CGM data [1] |
| 15 minutes | Recall (Euglycemia/Hyperglycemia) | 91%, 96% [1] | Real patient CGM data [1] | |
| ARIMA | 15 minutes & 1 hour | Recall (Hypo/Hyperglycemia) | Underperformed LSTM & Logistic Regression [1] | Real patient CGM data [1] |
| 30 minutes | RMSE | Outperformed by Ridge Regression [15] | OhioT1DM Dataset [15] |
Experimental Protocols and Model Methodologies
LSTM Model Implementation
Architecture and Training: A common implementation for glucose forecasting uses a sequence-to-sequence architecture. The model takes an input sequence of past data—typically a 180-minute window (36 time steps at 5-minute intervals)—including features like blood glucose levels, carbohydrate intake, bolus insulin, and basal insulin rate. This sequence is processed by an LSTM layer (e.g., with 50 hidden units) followed by fully connected dense layers. The model is trained to output a sequence of future glucose values, such as the next 60 minutes (12 time steps) [13]. The training often employs a walk-forward rolling forecast approach, mirroring real-world deployment where the model updates its predictions as new CGM readings arrive [13]. The Adam optimizer with a learning rate of 0.001 and Mean Squared Error (MSE) as the loss function are standard choices [13].
Personalized vs. Aggregated Training: A critical methodological consideration is the training strategy. Individualized models are trained on a single subject's data, tailoring the parameters to that person's unique physiology. In contrast, aggregated models are trained on a combined dataset from multiple subjects. Research indicates that individualized LSTM models can achieve accuracy comparable to aggregated models (RMSE of 22.52 vs. 20.50 mg/dL) despite using less data, highlighting their data efficiency and potential for privacy-preserving, on-device learning [13].
Competing Model Protocols
Logistic Regression is typically implemented as a classification task, predicting glucose levels categorized into hypoglycemia (<70 mg/dL), euglycemia (70–180 mg/dL), and hyperglycemia (>180 mg/dL). The model is trained on engineered features from CGM data, such as rolling averages and rate-of-change metrics [1].
ARIMA, a univariate statistical model, relies solely on past glucose values. The model order parameters (p, d, q) are determined for each subject via grid search, often guided by the Akaike Information Criterion (AIC), to account for individual time-series characteristics [15]. Its performance is often benchmarked against naive baselines like the persistence model (forecast equals the last observed value) [15].
Workflow and Architectural Diagrams
LSTM for Glucose Prediction Workflow
The following diagram illustrates the end-to-end workflow for developing and deploying an LSTM model for blood glucose prediction, from data collection to clinical application.
LSTM Model Architecture
The core LSTM architecture for processing sequential glucose data is detailed in the diagram below. It shows how the model handles input sequences to generate future predictions.
The Researcher's Toolkit: Essential Materials and Reagents
Table 3: Key Research Reagents and Computational Tools
| Item Name | Function/Application | Example/Specification |
|---|---|---|
| OhioT1DM Dataset | Public benchmark dataset for training and evaluating glucose prediction models. | Contains CGM, insulin, carbohydrate, and activity data from 12 people with T1D [16] [15]. |
| HUPA UCM Dataset | A dataset for researching diabetes management under free-living conditions. | Includes CGM, insulin, carbs, and lifestyle metrics from 25 individuals [13]. |
| CGM Simulator (Simglucose) | In-silico platform for generating synthetic patient data and testing algorithms. | Python implementation of the FDA-approved UVA/Padova T1D Simulator [1]. |
| Deep Learning Framework (Keras) | High-level API for rapid prototyping and training of LSTM models. | Used with Python and TensorFlow backend for model development [13]. |
| Clarke Error Grid Analysis | Clinical validation tool to assess the clinical accuracy of glucose predictions. | Zones A (clinically accurate) and B (benign errors) are target regions [17]. |
The comparative analysis indicates a clear trade-off between model complexity, interpretability, and performance across different prediction horizons. LSTM networks demonstrate superior performance for medium-term forecasts (60 minutes), making them the most suitable backbone for advanced applications like automated insulin delivery. Their ability to learn complex, non-linear temporal patterns from multivariate data is a significant advantage, though it comes at the cost of computational complexity and data requirements [13] [1].
In contrast, Logistic Regression excels as a highly efficient and interpretable model for very short-term (15-minute) classification of glycemic events, particularly for hypoglycemia warning systems [1]. ARIMA provides a statistically sound baseline but is generally outperformed by both machine learning and deep learning alternatives in handling the noisy and complex nature of real-world glucose data [1] [15].
Future research is poised to enhance LSTM frameworks further through hybrid architectures (e.g., Transformer-LSTM) [17], personalized federated learning to improve accuracy while preserving data privacy [5] [18], and advanced loss functions that specifically target the high-risk hypoglycemic and hyperglycemic ranges [5]. This evolution will continue to solidify the role of deep learning in creating safer and more effective personalized diabetes management systems.
The accurate prediction of glucose levels is a critical component of modern diabetes management, enabling proactive interventions to prevent dangerous hypoglycemic and hyperglycemic events. Within this field, a key research thesis has emerged, focusing on the comparative performance of traditional statistical models, like the Auto-Regressive Integrated Moving Average (ARIMA), against machine learning approaches such as logistic regression and Long Short-Term Memory (LSTM) networks. While complex deep learning models often show impressive results, ARIMA remains a fundamentally important tool in the researcher's toolkit. This guide provides an objective comparison of these model types, detailing their performance, underlying methodologies, and appropriate applications to help researchers and drug development professionals select the optimal predictive tool for their specific clinical or investigative context.
Experimental Protocols and Methodologies
To ensure a fair comparison, researchers typically employ standardized experimental protocols. The following workflows and methodologies are common in studies comparing ARIMA, LSTM, and logistic regression for glucose forecasting.
Standardized Experimental Workflow
The experimental process for developing and validating glucose prediction models follows a systematic sequence from data acquisition to final model evaluation. The diagram below outlines this standard workflow.
Core Methodological Components
Data Acquisition and Preprocessing
The OhioT1DM dataset is a publicly available benchmark containing data from individuals with Type 1 Diabetes, often resampled at 5 or 15-minute intervals [10] [15]. Standard preprocessing involves addressing data gaps through linear interpolation for short periods (e.g., ≤30 minutes) and chronological splitting into training, validation, and test sets to prevent data leakage [15] [1]. A rolling-origin evaluation protocol is frequently used to simulate real-world deployment, where models are repeatedly trained on historical data and tested on subsequent unseen points [15].
Feature Engineering Strategies
Feature engineering is crucial, particularly for non-ARIMA models. For logistic regression and LSTM, common engineered features from CGM time series include [1] [19]:
- Lag Features: Glucose values from preceding time points (e.g., t-1, t-2, ..., t-12 for a 60-minute history at 5-minute resolution).
- Rate-of-Change (ROC): The speed of glucose change, often calculated over the past 15-30 minutes.
- Moving Averages & Variability Indices: Short-term averages (e.g., 15-minute) and standard deviations to capture trends and stability.
ARIMA models, in contrast, typically use the raw time series of past glucose values, relying on their inherent autoregressive structure [15].
Model Specification and Training
- ARIMA (Auto-Regressive Integrated Moving Average): For each subject, a univariate ARIMA model is fitted to their CGM series. The order parameters (p, d, q) are selected via grid search, often guided by the Akaike Information Criterion (AIC) [15]. The model's core assumption is that future glucose values are a linear function of past values and past forecast errors.
- Logistic Regression: This model is used for classifying future glucose into ranges (e.g., hypo-/hyperglycemia). It is trained on the engineered features (lags, ROC) with regularization to prevent overfitting [1] [19].
- LSTM (Long Short-Term Memory): A type of recurrent neural network designed to capture long-term temporal dependencies. It processes sequences of past glucose data (and optionally other features) to predict either a future glucose value (regression) or its class (classification) [1] [19].
Comparative Performance Data
The performance of ARIMA, LSTM, and logistic regression models varies significantly depending on the prediction horizon and the specific glycemic range of interest. The following tables synthesize quantitative findings from recent comparative studies.
Table 1: Model Performance for 15-Minute Prediction Horizon (Classification Task)
| Glucose Range | Metric | ARIMA | Logistic Regression | LSTM |
|---|---|---|---|---|
| Hypoglycemia (<70 mg/dL) | Recall | Lower [1] | 98% [19] | 88% [19] |
| Euglycemia (70-180 mg/dL) | Recall | Lower [1] | 91% [1] | Lower than Logistic Regression [1] |
| Hyperglycemia (>180 mg/dL) | Recall | Lower [1] | 96% [1] | Lower than Logistic Regression [1] |
Table 2: Model Performance for 60-Minute Prediction Horizon (Classification Task)
| Glucose Range | Metric | ARIMA | Logistic Regression | LSTM |
|---|---|---|---|---|
| Hypoglycemia (<70 mg/dL) | Recall | 7.3% [19] | 83% [19] | 87% [19] |
| Hyperglycemia (>180 mg/dL) | Recall | ~60% [19] | Lower than LSTM [1] | 85% [19] |
Table 3: Model Performance for Numerical Glucose Forecasting (Regression Task)
| Model | Context / Metric | Performance |
|---|---|---|
| ARIMA | RMSE for Glucose Prediction [20] | 71.7% lower RMSE than LSTM in one study [20] |
| Ridge Regression | RMSE for 30-min forecast vs. ARIMA [15] | Outperformed ARIMA (Significant reduction in RMSE) [15] |
| LSTM | General regression on complex datasets | Can be outperformed by simpler models on linear/short-term tasks [20] [21] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Resources for Glucose Prediction Research
| Resource / Solution | Specification / Function | Example Use Case |
|---|---|---|
| OhioT1DM Dataset | Public benchmark dataset with CGM, insulin, and carbohydrate data from people with T1D. | Model training, benchmarking, and comparative validation [10] [15]. |
| CGM Simulator | Software (e.g., Simglucose) for generating in-silico CGM data for controlled testing. | Initial algorithm testing and validation across virtual patient cohorts [1] [19]. |
| Rolling-Origin Validation Framework | A robust evaluation protocol that simulates real-time forecasting by expanding the training window. | Prevents over-optimistic performance estimates and tests model robustness [15]. |
| Clarke Error Grid Analysis (CEG) | A clinical accuracy assessment tool that categorizes prediction errors based on clinical risk. | Validates the clinical acceptability of model predictions beyond statistical error [15]. |
| Feature Engineering Pipeline | Computational tools for generating lag, rate-of-change, and variability features from raw CGM data. | Essential for preparing inputs for logistic regression and LSTM models [1]. |
Discussion and Comparative Analysis
Model Selection Framework
The experimental data reveals that no single model is universally superior. The optimal choice is a function of the specific prediction horizon and the clinical objective. The following diagram synthesizes the decision-making logic for model selection.
Interpretation of Comparative Results
The performance data underscores a clear trade-off. Logistic Regression excels at short-horizon classification, making it ideal for applications requiring immediate alerts for impending hypoglycemia, where high recall is critical for patient safety [1] [19]. Its strength lies in leveraging simple, engineered features like the recent rate of change.
In contrast, LSTM models demonstrate superior capability for long-horizon predictions (e.g., 60 minutes). Their complex architecture is better suited to modeling the non-linear physiological processes that influence glucose levels over longer periods, making them more reliable for predicting both hyper- and hypoglycemic events further in advance [1] [19].
The performance of ARIMA is more context-dependent. While it can be outperformed by more complex models, particularly on classification tasks [1], it remains a potent tool. It can achieve excellent results in numerical forecasting, sometimes surpassing LSTM, especially when relationships are primarily linear or datasets are limited [20] [21]. Its key advantages are computational efficiency and strong performance for short-term numerical predictions, making it a viable candidate for resource-constrained or embedded systems [15].
The research-driven comparison between ARIMA, logistic regression, and LSTM confirms that the landscape of glucose prediction is not one of outright winners and losers. ARIMA models maintain significant relevance, particularly for short-term numerical forecasting and in settings where computational efficiency and interpretability are valued. Logistic regression is the specialist for imminent classification tasks, while LSTMs are the powerhouse for long-term forecasting. The findings indicate that the future of glucose prediction may not lie in a single model, but in hybrid approaches that leverage the distinct strengths of each to achieve robust, accurate, and clinically actionable forecasting systems.
The accurate prediction of blood glucose levels is paramount for improving the management of diabetes, a chronic disease affecting a significant portion of the global adult population [22]. Predictive models can provide early warnings for hypoglycemic (low blood glucose) or hyperglycemic (high blood glucose) events, enabling timely interventions. However, the reliability of these models is contingent upon the use of robust evaluation metrics that can adequately capture their clinical utility. Evaluation metrics are quantitative measures used to assess the performance and effectiveness of a statistical or machine learning model [23]. The choice of metric is critical, as it determines how model performance is quantified and compared.
This guide focuses on a suite of essential metrics for evaluating regression and classification models, particularly within the context of a broader study comparing the glucose prediction accuracy of three distinct models: Logistic Regression, Long Short-Term Memory (LSTM) networks, and the Autoregressive Integrated Moving Average (ARIMA) model. While regression metrics like RMSE and MAE assess the precision of continuous glucose value predictions, classification metrics such as AUC and clinical accuracy measures (e.g., precision, recall) evaluate the model's ability to correctly categorize glucose states (e.g., hypo-, normo-, or hyperglycemia) [1] [22]. A comprehensive understanding of these metrics allows researchers to select the most appropriate model for a given clinical application, whether the priority is short-term tactical alerts or long-term strategic management.
Defining the Core Evaluation Metrics
Metrics for Continuous Value Prediction (Regression)
When the goal of a model is to forecast a continuous blood glucose value (in mg/dL or mmol/L), regression metrics are used. These metrics quantify the difference between the predicted and the actual measured values.
Root Mean Squared Error (RMSE): RMSE is the square root of the average squared differences between predicted and actual values [24] [25]. It is calculated as: ( \operatorname{RMSE} = \sqrt{\frac{1}{N} \sum{j=1}^{N}\left(y{j}-\hat{y}{j}\right)^{2}} ) where (yj) is the actual value, (\hat{y}_j) is the predicted value, and (N) is the number of observations [26] [24]. As squaring emphasizes larger errors, RMSE is sensitive to outliers and is most appropriate when large errors are particularly undesirable [24] [25]. A perfect model has an RMSE of 0.
Mean Absolute Error (MAE): MAE calculates the average of the absolute differences between predicted and actual values [26] [25]. It is calculated as: ( \operatorname{MAE} = \frac{1}{N} \sum{j=1}^{N}\left|y{j}-\hat{y}_{j}\right| ) MAE provides a linear score, meaning all errors are weighted equally. This makes it more robust to outliers than RMSE and gives a clearer view of the model's typical prediction accuracy [24] [27]. Like RMSE, its value is in the units of the target variable, and an ideal value is 0.
Comparative Properties of RMSE and MAE: The table below summarizes the key characteristics of these two primary regression metrics.
Table 1: Comparison of Regression Metrics RMSE and MAE
| Property | Root Mean Squared Error (RMSE) | Mean Absolute Error (MAE) |
|---|---|---|
| Sensitivity to Outliers | High (penalizes large errors heavily) [24] | Low (treats all errors equally) [24] |
| Interpretation | Error in original data units, but skewed by large errors | Easy to understand; average error in original units [27] |
| Optimal Predictor | Predicts the mean of the target distribution [25] | Predicts the median of the target distribution [25] |
| Best Use Case | When large errors are especially unacceptable | When the cost of an error is proportional to its size |
Metrics for Class-Based Prediction (Classification)
In many clinical scenarios, predicting the exact glucose value is less critical than correctly classifying the patient's state into a relevant category, such as hypoglycemia (<70 mg/dL), euglycemia (70-180 mg/dL), or hyperglycemia (>180 mg/dL) [1]. For these tasks, classification metrics are used, which are derived from a confusion matrix.
Confusion Matrix: A confusion matrix is an N x N table (where N is the number of classes) that summarizes the performance of a classification model by comparing the actual labels to the predicted labels [26] [23]. For binary classification, it contains four key elements:
- True Positives (TP): The model correctly predicts the positive class.
- True Negatives (TN): The model correctly predicts the negative class.
- False Positives (FP): The model incorrectly predicts the positive class (Type I error).
- False Negatives (FN): The model incorrectly predicts the negative class (Type II error) [26] [28].
Precision, Recall, and F1-Score: From the confusion matrix, several crucial metrics can be derived:
- Precision (Positive Predictive Value): Measures the accuracy of positive predictions. ( \text{Precision} = \frac{TP}{TP + FP} ) [26] [27]. High precision is vital when the cost of a false positive is high (e.g., triggering an unnecessary insulin dose).
- Recall (Sensitivity): Measures the model's ability to identify all actual positive cases. ( \text{Recall} = \frac{TP}{TP + FN} ) [26] [27]. High recall is critical when missing a positive event is dangerous (e.g., failing to predict a hypoglycemic episode).
- F1-Score: The harmonic mean of precision and recall, providing a single metric that balances both concerns. ( \text{F1 Score} = 2 \times \frac{\text{Precision} \times \text{Recall}}{\text{Precision} + \text{Recall}} ) [26] [23]. It is especially useful with imbalanced datasets.
Area Under the ROC Curve (AUC-ROC): The Receiver Operating Characteristic (ROC) curve is a graphical plot that illustrates the diagnostic ability of a binary classifier by plotting the True Positive Rate (Recall) against the False Positive Rate (1 - Specificity) at various threshold settings [26] [23]. The Area Under this Curve (AUC) summarizes the model's ability to distinguish between classes. An AUC of 1.0 represents a perfect model, while 0.5 represents a model no better than random guessing [27] [23]. AUC is valuable because it is independent of the classification threshold and the class distribution, making it excellent for model comparison [23].
Figure 1: A decision workflow for selecting the most appropriate evaluation metric based on model output and clinical priority.
Experimental Comparison: Logistic Regression vs. LSTM vs. ARIMA
Recent research has directly compared the performance of Logistic Regression, LSTM, and ARIMA models for predicting glucose levels, using the metrics defined above. The experimental protocols and their results provide critical insights for model selection.
A 2023 study evaluated these three models for predicting hypoglycemia, euglycemia, and hyperglycemia classes 15 minutes and 1 hour ahead [1]. The data was sourced from two primary avenues:
- Clinical Cohort Data: Real patient data was acquired from a study involving participants with type 1 diabetes who used a continuous glucose monitor (CGM). This data included sensor glucose readings, insulin dosing, and carbohydrate intake [1].
- In-Silico Simulation: Data was also generated using the CGM Simulator (Simglucose v0.2.1), a Python implementation of the UVA/Padova T1D Simulator. This simulator created a large cohort of virtual patients across different age groups, simulating glucose dynamics over multiple days with randomized meal and snack schedules [1].
The raw data was pre-processed to a consistent 15-minute frequency. The core of the methodology involved feature engineering, where additional predictive factors were derived from the raw CGM time series. These included rolling averages, rate-of-change metrics, and variability indices, which helped the models capture the dynamism of glucose fluctuations [1]. The models were then trained and evaluated, with their performance compared using precision, recall, and accuracy.
Quantitative Performance Results
The experimental results revealed that no single model was superior across all prediction horizons, highlighting a trade-off between short-term and mid-term accuracy.
Table 2: Model Performance in Glucose Level Classification (Recall Rates) [1]
| Glucose Class | Prediction Horizon | Logistic Regression | LSTM | ARIMA |
|---|---|---|---|---|
| Hyperglycemia | 15 minutes | 96% | (Lower than LR) | (Lowest) |
| (>180 mg/dL) | 1 hour | (Lower than LSTM) | 85% | (Lowest) |
| Euglycemia | 15 minutes | 91% | (Lower than LR) | (Lowest) |
| (70-180 mg/dL) | 1 hour | (Data not specified) | (Data not specified) | (Lowest) |
| Hypoglycemia | 15 minutes | 98% | (Lower than LR) | (Lowest) |
| (<70 mg/dL) | 1 hour | (Lower than LSTM) | 87% | (Lowest) |
For continuous glucose value prediction, another study focusing on non-invasive monitoring found that the ARIMA model could outperform LSTM on their specific dataset, achieving a 71.7% lower RMSE for glucose prediction [20]. This contrasts with the classification-focused study and underscores that the optimal model can depend heavily on the task (classification vs. regression), data characteristics, and prediction horizon.
Analysis and Model Selection Guidelines
The data from these experiments allows for a direct, objective comparison of the three models:
- Logistic Regression demonstrated exceptional performance for short-term (15-minute) classification, achieving the highest recall rates for all glycemia classes [1]. This suggests it is highly effective for immediate, tactical alerts where correctly identifying an impending event is the priority. Its strength lies in its simplicity and efficiency with smaller, engineered features.
- LSTM Networks proved to be the best model for longer-term (1-hour) classification, outperforming logistic regression for hyper- and hypoglycemia prediction [1]. As a type of recurrent neural network, LSTM's ability to capture long-term dependencies and complex temporal patterns in sequential data makes it more suited for forecasting further into the future.
- ARIMA, a classic statistical time-series model, generally underperformed the machine learning models in the classification task [1]. However, its strong performance in the regression-based study [20] indicates it remains a viable and sometimes superior candidate, particularly when the dataset or forecasting task aligns with its underlying assumptions.
Figure 2: A comparative analysis of the strengths and limitations of Logistic Regression, LSTM, and ARIMA models based on experimental results in glucose prediction.
The Scientist's Toolkit: Essential Research Reagents and Materials
To conduct rigorous experiments in glucose prediction modeling, researchers rely on a combination of data, software, and evaluation frameworks. The following table details key components used in the featured studies.
Table 3: Essential Research Reagents and Materials for Glucose Prediction Research
| Item Name | Type | Function / Application in Research |
|---|---|---|
| Continuous Glucose Monitor (CGM) Data | Data Source | Provides real-time, high-frequency time-series data of interstitial glucose levels; the foundational input for training and testing predictive models [1] [22]. |
| In-Silico Simulator (e.g., Simglucose) | Software / Data Source | Generates synthetic data for a large cohort of virtual patients; useful for initial algorithm testing and controlling variables, though may lack real-world complexity [1]. |
| Lifestyle Log (Carb/Insulin) | Data Source | Records carbohydrate intake and insulin dosing; provides crucial contextual features that significantly improve prediction accuracy [1] [22]. |
| Python with Scikit-learn & Keras/TensorFlow | Software | Primary programming environment; provides libraries for data preprocessing (e.g., pandas), implementing models (Logistic Regression, LSTM), and calculating metrics (e.g., scikit-learn.metrics) [24] [28]. |
| Confusion Matrix Analysis | Evaluation Framework | The foundational table for calculating classification metrics like Precision, Recall, and F1-Score, enabling detailed error analysis [1] [23]. |
| ROC Curve Analysis | Evaluation Framework | A graphical and quantitative method (via AUC) to evaluate a classification model's performance across all possible thresholds, independent of class distribution [29] [23]. |
Model Deployment in Practice: Methodological Approaches and Clinical Use Cases
Data Requirements and Preprocessing for Each Model Architecture
In the rapidly evolving field of diabetes management, accurate glucose prediction is paramount for preventing acute complications and long-term health deterioration. The performance of any predictive model is intrinsically tied to the quality and structure of its training data, with different model architectures demanding distinct preprocessing approaches and exhibiting varying capabilities in handling real-world clinical data challenges. This guide provides a systematic comparison of three prominent model architectures—Logistic Regression, Long Short-Term Memory (LSTM) networks, and AutoRegressive Integrated Moving Average (ARIMA)—focusing on their data requirements, preprocessing methodologies, and empirical performance in glucose prediction tasks. Understanding these foundational differences enables researchers and clinicians to select appropriate modeling strategies based on available data resources and clinical objectives, ultimately advancing personalized diabetes care through more reliable forecasting systems.
Model-Specific Data Requirements and Preprocessing Techniques
Logistic Regression
Data Requirements: Logistic Regression operates under strict statistical assumptions that dictate specific data requirements. The model assumes independent observations, meaning there should be no correlation or dependence between input samples in the dataset [30]. It requires a binary dependent variable, typically representing glucose classification outcomes such as hypoglycemic/hyperglycemic events versus normal ranges. The model further assumes a linear relationship between independent variables and the log odds of the dependent variable, necessitating careful feature engineering to satisfy this condition [30]. The dataset should not contain extreme outliers as they can distort coefficient estimation, and sufficient sample size is crucial for producing reliable, stable results.
Preprocessing Workflow: The preprocessing pipeline for Logistic Regression begins with comprehensive data exploration to identify missing values, incorrect data types, and inconsistent categories [31]. For missing values in numeric features, imputation with mean or median values is recommended depending on the distribution, while categorical features should be filled with the most frequent category [31]. Outlier detection and treatment using statistical methods like z-scores or interquartile range is essential to prevent coefficient distortion. Categorical variables require appropriate encoding strategies—label encoding for ordered categories and one-hot encoding for unordered categories [31]. Feature scaling through standardization (zero mean, unit variance) or normalization (0-1 range) is critical for algorithms relying on gradient descent, with the choice depending on the specific implementation. Finally, the dataset must be split into training and testing sets, typically 70-80% for training and 20-30% for testing, with an optional validation set for hyperparameter tuning [31].
Long Short-Term Memory (LSTM) Networks
Data Requirements: LSTM networks excel at processing sequential data with temporal dependencies, making them particularly suitable for continuous glucose monitoring (CGM) data streams. Unlike Logistic Regression, LSTMs can effectively handle multivariate time-series inputs, incorporating additional physiological parameters such as carbohydrate intake, insulin administration (both basal and bolus), physical activity, and heart rate [13]. The model requires substantial temporal continuity with consistent sampling intervals (e.g., 5-minute readings from CGM devices) to effectively capture metabolic patterns [13]. For individualized training approaches, data from individual subjects is sufficient, while aggregated models benefit from combined datasets across multiple patients to capture population-level trends [13].
Preprocessing Workflow: LSTM preprocessing begins with comprehensive data cleaning to address sensor artifacts, missing CGM values, and physiological implausibilities using domain-specific filters [13]. For free-living data, additional preprocessing may include synchronizing timestamps across different data sources (CGM, insulin pumps, activity trackers) and handling irregularly sampled events like meal intake. The critical transformation involves restructuring the temporal data into supervised learning format through sliding window approaches, where past sequences (typically 180 minutes or 36 time steps at 5-minute intervals) are used to predict future glucose values (e.g., 60 minutes ahead) [13]. Feature scaling through normalization (0-1 range) is essential to ensure stable gradient flow during training. For multivariate predictions, all input features (glucose, carbohydrates, insulin) must undergo simultaneous normalization. The dataset should be split chronologically (not randomly) into training, validation, and test sets (e.g., 60:20:20 ratio) to preserve temporal relationships and enable realistic evaluation [32].
ARIMA (AutoRegressive Integrated Moving Average)
Data Requirements: ARIMA models have one fundamental requirement: stationarity [33]. A stationary time series maintains stable statistical properties (mean, variance, autocorrelation) over time, unlike raw glucose data that typically exhibits trends (progressive changes) and seasonality (recurring patterns). The model works exclusively with univariate data, meaning it processes only historical glucose values without incorporating external variables like insulin or carbohydrate intake [33]. While ARIMA can handle missing values through interpolation, substantial data gaps compromise model reliability. The integrated (I) component specifically addresses non-stationarity through differencing operations, transforming the raw series into one with stable statistical properties suitable for autoregressive modeling.
Preprocessing Workflow: The ARIMA preprocessing pipeline focuses intensely on achieving stationarity. The process begins with visual inspection of the glucose series to identify evident trends and seasonal patterns [33]. Statistical tests including the Augmented Dickey-Fuller (ADF) test and Kwiatkowski-Phillips-Schmidt-Shin (KPSS) test provide quantitative assessment of stationarity [33]. For non-stationary series, differencing is applied where each value is replaced by the change between successive periods (Y't = Yt - Yt-1) to remove linear trends [33]. Seasonal differencing (e.g., subtracting the value from 24 hours prior for daily patterns) addresses periodic fluctuations. The appropriate differencing order (d parameter) is determined iteratively until stationarity is achieved. After model fitting, residual analysis confirms whether the transformed series exhibits the white noise properties indicative of successful stationarization. Unlike LSTM, ARIMA typically does not require feature scaling as its estimation procedures are scale-invariant.
Table 1: Comparative Data Requirements for Glucose Prediction Models
| Parameter | Logistic Regression | LSTM | ARIMA |
|---|---|---|---|
| Data Type | Tabular (IID) | Sequential time-series | Univariate time-series |
| Temporal Dependencies | Not supported | Essential requirement | Fundamental aspect |
| Variable Support | Multivariate | Multivariate | Univariate only |
| Stationarity Requirement | Not applicable | Not required | Mandatory |
| Minimum Data Volume | Large sample size | Moderate to large | Smaller series acceptable |
| Handling Missing Data | Imputation required | Imputation or masking | Interpolation or omission |
Experimental Protocols and Performance Comparison
Experimental Designs in Current Literature
Individualized vs. Aggregated LSTM Training: A recent investigation compared two LSTM training strategies using the HUPA UCM dataset containing CGM values, insulin delivery, and carbohydrate intake from 25 T1D subjects [13]. For individualized training, 25 separate LSTM models were trained independently on each subject's data. The aggregated approach trained a single model on combined data from all subjects. The model architecture maintained consistency with a 180-minute input window (36 time steps at 5-minute intervals) predicting 60 minutes ahead, using LSTM layers with 50 hidden units, and mean squared error as the loss function [13].
ARIMA vs. LSTM for Non-invasive Monitoring: Another study developed a non-invasive glucose and cholesterol monitoring system using NIR sensors, comparing ARIMA and LSTM forecasting performance [20]. Data collected from patients over one month was used to train both models, with evaluation based on Root Mean Square Error (RMSE). The research specifically aimed to address the inconvenience of traditional blood tests that often leads to delayed testing and monitoring [20].
Comprehensive Model Benchmarking: A larger-scale comparison evaluated Transformer-VAE, LSTM, GRU, and ARIMA models for diabetes burden forecasting using Global Burden of Disease data from 1990-2021 [14]. Models were trained on 1990-2014 data and evaluated on 2015-2021 data, with performance measured using Mean Absolute Error (MAE) and RMSE. Robustness was assessed through introduced noise and missing data, while computational efficiency was evaluated based on training time, inference speed, and memory usage [14].
Quantitative Performance Comparison
Table 2: Experimental Performance Metrics Across Model Architectures
| Model Architecture | Application Context | Performance Metrics | Comparative Findings |
|---|---|---|---|
| ARIMA | Non-invasive glucose forecasting | RMSE: ~71.7% lower than LSTM for glucose [20] | Surpassed LSTM in non-invasive prediction [20] |
| LSTM (Individualized) | Blood glucose prediction (T1D) | RMSE: 22.52 ± 6.38 mg/dL; Clarke Zone A: 84.07 ± 6.66% [13] | Comparable to aggregated training despite less data [13] |
| LSTM (Aggregated) | Blood glucose prediction (T1D) | RMSE: 20.50 ± 5.66 mg/dL; Clarke Zone A: 85.09 ± 5.34% [13] | Modest performance improvement over individualized [13] |
| ARIMA | Diabetes burden forecasting | Limited long-term trend capability [14] | Resource-efficient but less accurate for complex trends [14] |
| LSTM | Diabetes burden forecasting | Effective for short-term patterns; long-term dependency challenges [14] | Balanced performance but computational demands [14] |
| Transformer-VAE | Diabetes burden forecasting | MAE: 0.425; RMSE: 0.501; Superior noise resilience [14] | Highest accuracy but computational cost and interpretability challenges [14] |
Strengths and Limitations in Clinical Implementation
Logistic Regression offers high interpretability and computational efficiency, making it suitable for classification tasks like hypoglycemia risk stratification. However, its inability to capture temporal patterns and strict assumptions about feature relationships limit its application for continuous glucose forecasting [30].
LSTM Networks excel at capturing complex temporal dependencies in multivariate physiological data, enabling personalized forecasting that adapts to individual metabolic patterns [13]. The architecture's ability to incorporate multiple input signals (glucose, insulin, carbohydrates, activity) aligns well with the multifactorial nature of glucose regulation. Challenges include substantial computational requirements, need for extensive hyperparameter tuning, and limited interpretability ("black-box" characterization) [34] [14].
ARIMA Models provide statistical rigor and interpretability with clearly defined components representing different aspects of the time series structure [33]. Their computational efficiency facilitates deployment in resource-constrained environments. The critical limitation for glucose forecasting is the univariate nature, preventing incorporation of important external factors like insulin dosing, meal intake, or physical activity [14]. The stationarity requirement also poses challenges for glucose data exhibiting diurnal patterns and physiological trends.
Visualization of Preprocessing Workflows
Data Preprocessing Pipeline for Time-Series Models
LSTM and ARIMA Preprocessing Workflow
Model Selection Decision Framework
Model Selection Based on Data Characteristics
Research Reagent Solutions: Essential Materials for Glucose Prediction Research
Table 3: Key Research Datasets and Computational Tools
| Resource | Type | Primary Application | Key Features |
|---|---|---|---|
| HUPA UCM Dataset | Clinical dataset | LSTM glucose prediction [13] | CGM, insulin, carbs, activity from 25 T1D subjects |
| OhioT1DM Dataset | Clinical dataset | LLM-powered glucose prediction [10] | Multi-modal physiological data for personalized forecasting |
| Global Burden of Disease Data | Epidemiological dataset | Diabetes burden forecasting [14] | DALYs, deaths, prevalence (1990-2021) for model benchmarking |
| statsmodels (Python) | Statistical library | ARIMA implementation [33] | Stationarity tests, model fitting, diagnostic plots |
| Keras/TensorFlow | Deep learning framework | LSTM development [13] | Neural network API with LSTM layers, sequence processing |
| scikit-learn | Machine learning library | Logistic Regression preprocessing [31] | Data preprocessing, feature scaling, model evaluation |
| Clarke Error Grid Analysis | Validation methodology | Clinical accuracy assessment [13] | Zone-based classification of prediction clinical accuracy |
The selection of an appropriate model architecture for glucose prediction depends fundamentally on the nature and scope of available data, with each approach offering distinct advantages for specific clinical scenarios. Logistic Regression provides interpretable classification for risk stratification but lacks temporal modeling capabilities. LSTM networks offer powerful multivariate sequence modeling suitable for personalized forecasting incorporating multiple physiological signals, though with substantial computational demands and complexity. ARIMA models deliver statistically rigorous univariate forecasting with computational efficiency but cannot incorporate external factors that significantly influence glucose variability. Contemporary research demonstrates promising directions including hybrid modeling approaches, individualized LSTM training for privacy-preserving applications, and emerging architectures like Transformer-VAE that balance accuracy with robustness to noisy clinical data. As diabetes management increasingly leverages automated insulin delivery systems, the strategic alignment of model architecture with data characteristics and clinical requirements will remain essential for developing reliable, clinically actionable glucose prediction technologies.
The accurate prediction of blood glucose (BG) levels is a cornerstone for advancing type 1 diabetes (T1D) management, particularly in free-living conditions where individuals engage in daily activities like exercise. Reliable forecasting enables proactive interventions to prevent hyperglycemia and hypoglycemia, thereby improving quality of life and reducing long-term complications. Within this field, a critical research focus is the comparative performance of different algorithmic approaches. This guide provides an objective comparison of three prominent models—Long Short-Term Memory (LSTM) networks, Logistic Regression, and the Autoregressive Integrated Moving Average (ARIMA) model—framed within the broader thesis of evaluating their glucose prediction accuracy for T1D. We summarize experimental data, detail methodologies, and provide resources to inform researchers and drug development professionals.
Model Performance Comparison in Free-Living Conditions
The performance of predictive models is typically evaluated using metrics such as Root Mean Squared Error (RMSE) for regression tasks (predicting a specific glucose value) and precision/recall for classification tasks (predicting a glycemic state: hypo-, normo-, or hyperglycemia). The tables below synthesize quantitative findings from recent studies conducted in free-living settings.
Table 1: Comparative Performance of LSTM, Logistic Regression, and ARIMA for Glucose Prediction
| Model | Prediction Horizon | Key Performance Metrics | Context & Dataset |
|---|---|---|---|
| LSTM [1] [35] | 15 minutes | RMSE: ~0.43 mmol/L (~7.74 mg/dL) [36] | Free-living data; CGM data only or with exogenous inputs [37] [36]. |
| 30 minutes | Median RMSE: 6.99 mg/dL [37] | Free-living data with exercise; personalized models [37]. | |
| 60 minutes | RMSE: ~1.73 mmol/L (~31.14 mg/dL) [36]; Recall (Hypo): 87% [1] | Free-living data; outperforms LR for hypoglycemia prediction at this horizon [1]. | |
| Logistic Regression [1] [38] | 15 minutes | Recall (Hypo): 98%; Recall (Normo): 91%; Recall (Hyper): 96% [1] | Free-living data; excels as a classifier for short-term glycemic state prediction [1]. |
| 60 minutes | Performance declines compared to shorter horizons [1] | Free-living data; outperformed by LSTM for longer horizons [1]. | |
| ARIMA [1] [35] | 15 minutes | Lower performance compared to LSTM and Logistic Regression [1] | Free-living data; struggles with non-linear glucose dynamics [1]. |
| 60 minutes | Underperforms LSTM and Logistic Regression [1] | Free-living data; limited capability with complex, multi-factorial data [1]. |
Table 2: Summary of Model Strengths and Data Requirements
| Model | Best Use Case | Strengths | Weaknesses |
|---|---|---|---|
| LSTM | Medium- to long-term BG value prediction (30-90 mins); Classifying hypo-/hyperglycemia at longer horizons [37] [1]. | Captures complex temporal patterns and long-range dependencies; handles multivariate input well [39] [1]. | High computational cost; requires large amounts of data for training; "black box" nature [14]. |
| Logistic Regression | Short-term classification of glycemic states (e.g., 15 mins); Resource-constrained environments [1]. | Computationally efficient, simple to implement, and highly interpretable [1]. | Limited to classification; assumes linear relationships; performance drops with longer prediction horizons [1]. |
| ARIMA | Baseline model for linear time-series analysis; Scenarios with limited computational resources [14] [1]. | Computationally efficient and simple for univariate, linear time-series data [14]. | Poor performance with non-linear, complex datasets; cannot natively incorporate exogenous variables [1]. |
Detailed Experimental Protocols
To ensure the reproducibility of comparative studies, this section outlines standard protocols for data preprocessing and model training as employed in recent research.
Data Preprocessing and Feature Engineering
A consistent preprocessing pipeline is crucial for model performance. Common steps across studies include:
- Data Imputation and Alignment: Missing CGM data points for short gaps (e.g., <60 minutes) are typically estimated using linear interpolation. Longer gaps may lead to the exclusion of the corresponding data segment. Data from different sources (CGM, accelerometer, insulin pump) must be aligned to a common time frequency (e.g., 5-minute intervals) [39] [40] [36].
- Normalization: To improve model convergence and accuracy, each time series (e.g., glucose, insulin) is often normalized with respect to its own minimum and maximum values, transforming the data into a (0,1) range. An inverse transform is applied to the model's output to map predictions back to the original scale [39].
- Stationarity Check (for ARIMA): Before applying ARIMA, time series must be checked for stationarity using statistical tests like the Augmented Dickey-Fuller (ADF) and Kwiatkowski-Phillips-Schmidt-Shin (KPSS) tests. Non-stationary series are made stationary through differencing [40].
- Feature Engineering for Machine Learning: For LSTM and Logistic Regression, the time-series prediction problem is reframed as a supervised learning task. This involves using a sliding window of historical observations (e.g., 180 minutes of past data) as input features to predict future values [40] [13]. When only glucose data is available, features like the rate of change, rolling averages, and variability indices can be engineered to provide more context to the models [1].
Model Training and Evaluation
Robust training and evaluation methodologies are essential for unbiased performance estimates.
- Train-Test Splitting: Conventional random splitting is unsuitable for time-series data due to temporal dependencies. The Forward Chaining (FC) method, a rolling-based technique, is often employed. The model is trained on a chronological subset of data and tested on a subsequent, unseen period. This process is repeated to obtain a robust performance estimate [39].
- Personalized vs. Aggregated Training:
- Aggregated Training: A single model is trained on data combined from multiple individuals. This leverages larger datasets but may lack precision for individual variability [13].
- Personalized Training: A separate model is trained for each individual using only their own data. This can better capture individual patterns and has been shown to achieve accuracy comparable to aggregated models, even with less data [37] [13]. Another effective approach is to start with a population-based model and then fine-tune it on individual patient data [37].
- Evaluation Metrics: Models are evaluated using:
- Regression Metrics: Root Mean Squared Error (RMSE) and Mean Absolute Error (MAE) for predicted glucose values [37] [39].
- Classification Metrics: Precision, Recall (Sensitivity), and Accuracy for predicting hypoglycemia, euglycemia, and hyperglycemia events [1].
- Clinical Safety: The Clarke Error Grid (CEG) or Continuous Glucose-Error Grid Analysis (CG-EGA) is used to assess the clinical accuracy of predictions, categorizing them into zones from A (clinically accurate) to E (erroneous and dangerous) [37] [39].
The following diagram illustrates a typical end-to-end workflow for developing and evaluating glucose prediction models.
The Scientist's Toolkit: Research Reagent Solutions
This section details key datasets, software, and hardware resources essential for conducting research in glucose prediction for T1D.
Table 3: Essential Research Resources for Glucose Prediction Studies
| Resource | Type | Description & Function |
|---|---|---|
| OhioT1DM Dataset [40] [36] | Dataset | A widely used, publicly available clinical dataset containing CGM, insulin, carbohydrate, and physical activity data from 12 individuals with T1D over 8 weeks. Serves as a benchmark for model development and comparison. |
| T1DEXI (Type 1 Diabetes Exercise Initiative) [37] | Dataset | A dataset specifically focused on exercise in free-living conditions. Includes CGM, insulin pump, carbohydrate intake, and detailed exercise information for 79 patients, ideal for studying glycemic impact of physical activity. |
| HUPA UCM Dataset [13] | Dataset | Contains data from 25 T1D individuals in free-living conditions, including CGM, insulin, carbohydrate intake, and lifestyle metrics (steps, heart rate). Useful for developing personalized models. |
| UVA/Padova T1D Simulator [1] | Software/Model | An FDA-accepted simulator of T1D physiology. Used for in-silico testing and validation of glucose prediction and control algorithms before clinical trials. |
| CGM Simulator (e.g., Simglucose) [1] | Software/Model | A Python-based simulator that incorporates CGM sensor error profiles, useful for testing model robustness to noisy data. |
| Dexcom G6 CGM System [35] | Hardware | A real-time CGM system commonly used in research and clinical care. Provides glucose readings every 5 minutes, forming the primary data source for prediction models. |
| ActivPAL Accelerometer [36] | Hardware | A research-grade accelerometer used to objectively measure physical activity, which is a major confounding factor for glucose levels in free-living studies. |
The comparative analysis of LSTM, Logistic Regression, and ARIMA models reveals a clear trade-off between predictive power, computational complexity, and interpretability in the context of T1D glucose forecasting under free-living conditions. No single model is universally superior; the optimal choice is highly dependent on the specific research or clinical objective. Logistic Regression is the optimal tool for highly accurate, short-term classification of glycemic states, particularly for hypoglycemia alerts 15 minutes in advance. LSTM networks demonstrate superior performance for predicting specific glucose values at longer horizons (30-60 minutes) and for classifying events like hypoglycemia one hour ahead, albeit at a higher computational cost and with greater data requirements. Finally, ARIMA serves best as a baseline model due to its limitations in handling the non-linearities and multiple exogenous factors inherent in free-living data. Future work should focus on hybrid models that leverage the strengths of each approach and on improving the interpretability of complex models like LSTM to foster trust and facilitate their integration into clinical decision support systems.
Sepsis, a life-threatening organ dysfunction caused by a dysregulated host response to infection, presents major challenges in critical care, where glucose dysregulation is a common and serious complication [12] [41]. Sepsis-induced glucose fluctuations—encompassing hyperglycemia, hypoglycemia, and increased glycemic variability—are independently associated with poor clinical outcomes and increased mortality [41]. The accurate prediction of these fluctuations is thus paramount for improving patient outcomes in intensive care settings.
The development of predictive models for glucose forecasting in septic patients has evolved significantly, leveraging various mathematical and computational approaches. Traditional time series models like ARIMA (Autoregressive Integrated Moving Average), classical statistical approaches such as logistic regression, and advanced deep learning architectures like LSTM (Long Short-Term Memory) networks each offer distinct advantages and limitations for this clinically critical task [1] [12] [42]. This guide provides an objective comparison of these three modeling approaches, presenting experimental data and methodologies to inform researchers, scientists, and drug development professionals working in the field of critical care analytics.
Model Performance Comparison
Quantitative Performance Metrics Across Prediction Horizons
Experimental data from comparative studies reveal significant differences in model performance across various prediction horizons. The table below summarizes key quantitative metrics for hypoglycemia, euglycemia, and hyperglycemia classification.
Table 1: Model Performance Metrics for Glucose Level Classification
| Prediction Horizon | Model | Glucose Class | Recall (%) | Precision (%) | Accuracy (%) |
|---|---|---|---|---|---|
| 15 minutes | Logistic Regression | Hypoglycemia (<70 mg/dL) | 98 | - | - |
| Euglycemia (70-180 mg/dL) | 91 | - | - | ||
| Hyperglycemia (>180 mg/dL) | 96 | - | - | ||
| 1 hour | LSTM | Hypoglycemia (<70 mg/dL) | 87 | - | - |
| Hyperglycemia (>180 mg/dL) | 85 | - | - | ||
| 15 minutes to 1 hour | ARIMA | All classes | Underperformed other models | - | - |
For the 15-minute forecast horizon, logistic regression demonstrated superior performance with recall rates of 96% for hyperglycemia, 91% for euglycemia, and 98% for hypoglycemia [1]. In contrast, for the 1-hour forecast horizon, the LSTM model outperformed logistic regression for hyper- and hypoglycemia classes, achieving recall values of 85% and 87% respectively [1]. ARIMA consistently underperformed compared to the other models across all glucose classes and time horizons [1].
Beyond classification performance, overall forecasting accuracy measured through error metrics provides additional insights into model capabilities.
Table 2: Forecasting Error Metrics Across Model Architectures
| Model Type | Application Context | RMSE | MAE | MAPE | Primary Strength |
|---|---|---|---|---|---|
| LSTM | Glucose prediction (multivariate) | 10.78 | - | - | Captures complex temporal patterns |
| LSTM | Glucose prediction (univariate) | 11.20 | - | - | Handles sequential data dependencies |
| ARIMA | Glucose prediction (univariate) | 12.43 | - | - | Effective for linear trends |
| PatchTST (Transformer) | Septic glucose forecasting (15 min) | - | - | 3.0% | Short-term forecasting accuracy |
| DLinear | Septic glucose forecasting (60 min) | - | - | 14.41% | Longer-term forecasting |
The multivariate LSTM model achieving an RMSE of 10.78 demonstrates how incorporating additional relevant variables can enhance prediction accuracy compared to univariate LSTM (RMSE: 11.20) and ARIMA (RMSE: 12.43) [43]. Recent research on septic patients has also shown that transformer-based models like PatchTST achieve superior short-term forecasting accuracy (MMPE: 3.0% at 15 minutes), while simpler linear models like DLinear excel at longer horizons (MMPE: 14.41% at 60 minutes) [12].
Experimental Protocols and Methodologies
Data Collection and Preprocessing Standards
Robust data collection and preprocessing form the foundation of reliable glucose forecasting models. Research protocols typically utilize two primary data sources: clinical cohort data from real patients and simulated data from validated physiological simulators [1].
The clinical cohort data for glucose prediction studies often comes from continuous glucose monitoring (CGM) devices, typically recording measurements at 15-minute intervals [1]. For sepsis-specific research, data extraction includes dynamic physiological indicators (heart rate, respiratory rate, blood oxygen saturation, mean arterial pressure, blood glucose) measured at frequencies ranging from 1-10 times per hour depending on the parameter and patient condition [44]. Data preprocessing pipelines generally include:
- Temporal Alignment: Resampling data to consistent frequencies (e.g., 15-minute intervals) and addressing gaps through interpolation [1]
- Outlier Removal: Filtering physiologically implausible values based on clinical knowledge (e.g., glucose: 42-309 mg/dL, SpO2: 21%-100%) [44]
- Feature Engineering: Deriving additional predictive features from raw time series, including rate of change metrics, variability indices, and moving averages [1]
- Normalization: Applying standardization (z-score normalization) or scaling to ensure consistent feature ranges [44]
For sepsis mortality prediction studies, typical exclusion criteria include patients under 18 years old, those with malignant tumors or immunosuppression, and cases where clinical data cannot be extracted [45] [41].
Model Training and Validation Frameworks
Rigorous validation methodologies are essential for evaluating true model performance, especially in clinical applications.
Temporal Validation: Data is split into training and testing sets based on time, rather than random splitting, to prevent data leakage and ensure realistic performance assessment [43]. A common approach uses "rolling forecast origin" validation, where models are repeatedly retrained on expanding windows of historical data [42] [43].
Performance Metrics: Comprehensive evaluation typically includes multiple metrics: RMSE (Root Mean Square Error) for overall prediction error, MAE (Mean Absolute Error) for interpretable error magnitude, MAPE (Mean Absolute Percentage Error) for relative error, and for classification tasks, precision, recall, and F1-score for each glucose class [1] [43].
Hyperparameter Optimization: Each model architecture requires specific hyperparameter tuning. For LSTM, this includes determining the number of neurons (e.g., 8, 64), optimizer selection (Adam, SGDM, RMSprop), and time step configuration [42]. For ARIMA, identifying optimal parameters (p, d, q) through ACF/PACF analysis and AIC minimization is standard [42].
Experimental Workflow for Glucose Forecasting Models
Model Architectures and Technical Implementation
ARIMA (Autoregressive Integrated Moving Average)
ARIMA models represent a classical approach to time series forecasting, combining autoregressive (AR) and moving average (MA) components with a differencing pre-processing step to achieve stationarity [42] [43].
Implementation Protocol:
- Stationarity Assessment: Augmented Dickey-Fuller (ADF) test to determine if the time series is stationary [42]
- Differencing Application: If non-stationary, apply differencing (d) until stationarity is achieved [42]
- Parameter Identification: Use Autocorrelation Function (ACF) and Partial Autocorrelation Function (PACF) plots to identify appropriate AR (p) and MA (q) orders [42]
- Model Selection: Compare candidate models using Akaike Information Criterion (AIC), selecting the model with lowest AIC value [42]
- Residual Analysis: Verify that residuals represent white noise through Box-Ljung test [42]
The model is expressed as ARIMA(p, d, q), where p represents autoregressive terms, d is the degree of differencing, and q represents moving average terms [43]. For seasonal patterns, seasonal ARIMA incorporates additional parameters (P, D, Q) to capture periodic patterns [42].
Logistic Regression
Despite its simplicity, logistic regression remains competitive for glucose classification tasks, particularly for short prediction horizons [1] [45].
Implementation Protocol:
- Feature Selection: Identify significant predictors through univariate analysis (p < 0.05) [45]
- Model Formulation: Apply stepwise regression with backward elimination to achieve the optimal model with minimum AIC [45]
- Variable Shrinkage: Utilize Least Absolute Shrinkage and Selection Operator (LASSO) regression for variable selection to prevent overfitting [45]
- Validation: Employ k-fold cross-validation (typically ten-fold) to ensure robustness [45]
In comparative studies for sepsis mortality prediction, logistic regression models have been constructed using independent risk factors identified through multivariate analysis, such as systolic pressure, lactic acid, NLR, RDW, IL-6, PT, and Tbil [45].
LSTM (Long Short-Term Memory)
LSTM networks are a specialized form of Recurrent Neural Networks (RNNs) designed to capture long-term dependencies in sequential data, making them particularly suitable for glucose time series forecasting [1] [46].
Architecture and Implementation: LSTM nodes incorporate three gates that control information flow:
- Forget Gate: Determines what information to discard from the cell state [46]
- Input Gate: Controls what new information to store in the cell state [46]
- Output Gate: Regulates what information to output based on the cell state [46]
Implementation Protocol:
- Data Normalization: Scale input data to the range [0, 1] due to LSTM sensitivity to input scale [42]
- Time Step Configuration: Set appropriate lookback periods (e.g., previous 7-60 time steps) [42]
- Architecture Design: Determine number of LSTM layers and neurons (e.g., 8-64 neurons) [42]
- Optimizer Selection: Choose appropriate optimization algorithms (Adam, SGD, RMSprop) [42]
- Regularization: Apply techniques like dropout to prevent overfitting [46]
Advanced LSTM architectures have been developed specifically for glucose forecasting, including memory-augmented LSTM (MemLSTM) that incorporates external memory slots for storing and retrieving relevant historical patterns [46].
LSTM Architecture for Glucose Forecasting
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Computational Tools
| Resource Category | Specific Tool/Solution | Function in Research | Application Context |
|---|---|---|---|
| Data Sources | MIMIC-IV Database | Provides deidentified clinical data from ICU patients | Model training and validation [44] |
| CGM Simulator (Simglucose v0.2.1) | Generates synthetic patient data for in silico testing | Algorithm development and testing [1] | |
| Programming Tools | Python with Scikit-learn | Machine learning library for traditional models | Implementing logistic regression, ARIMA [41] |
| TensorFlow/PyTorch | Deep learning frameworks | LSTM model implementation [46] | |
| R Software with "auto.arima()" | Statistical computing | ARIMA model identification [42] | |
| Model Validation | TreeSHAP (SHapley Additive exPlanations) | Model interpretability and feature contribution analysis | Explaining model predictions [44] |
| Ten-fold Cross-Validation | Robust model validation technique | Performance assessment [45] | |
| Clinical Integration | Web-based Prediction Platforms | Real-time risk assessment interfaces | Clinical deployment [44] |
The comparative analysis of ARIMA, logistic regression, and LSTM models for forecasting sepsis-induced glucose fluctuations reveals a nuanced landscape where each approach demonstrates distinct advantages depending on the clinical requirements. Logistic regression excels in short-term classification tasks (15-minute horizon), particularly for hypoglycemia detection where its 98% recall surpasses other approaches. LSTM networks demonstrate superior performance for longer prediction horizons (1-hour), capturing complex temporal patterns that linear models miss. ARIMA, while conceptually straightforward, consistently underperforms compared to both logistic regression and LSTM for glucose fluctuation forecasting.
These performance characteristics suggest a complementary rather than competitive relationship between approaches. Future research directions should explore hybrid models that leverage the respective strengths of each architecture, ensemble methods that combine predictions from multiple models, and enhanced feature engineering that incorporates both physiological variables and clinical context. For researchers and clinicians, the selection of an appropriate modeling approach should be guided by specific clinical needs: logistic regression for short-term alert systems, LSTM for proactive intervention planning, and ARIMA only for baseline comparisons in methodological studies. As glucose forecasting technologies continue to evolve, their integration into clinical decision support systems holds significant promise for improving sepsis management and patient outcomes in critical care settings.
Hypoglycemia remains a significant challenge in managing hospitalized patients with type 2 diabetes mellitus (T2DM), often resulting from complex interactions among clinical factors such as medication usage, renal function, and glycemic variability [47]. Predicting hypoglycemia severity is crucial for implementing preventive strategies and optimizing patient outcomes [47]. Traditional statistical methods like logistic regression have been widely employed for risk prediction due to their interpretability and simplicity [47]. However, these models assume linear relationships and may not effectively capture intricate interactions among clinical variables, limiting their predictive capabilities in clinical practice [47].
With advancements in machine learning techniques, models such as Extreme Gradient Boosting (XGBoost) have demonstrated remarkable performance in predicting complex clinical outcomes due to their ability to capture nonlinear interactions and handle high-dimensional data [47]. This comparison guide objectively evaluates the performance of logistic regression versus XGBoost for predicting hypoglycemia severity in hospitalized patients, providing researchers and clinicians with evidence-based insights for model selection.
Performance Comparison
Quantitative Performance Metrics
Recent clinical studies have directly compared the performance of logistic regression and XGBoost in predicting hypoglycemia events and severity in diabetic patients. The table below summarizes key performance metrics from multiple studies:
Table 1: Performance comparison of XGBoost and Logistic Regression for hypoglycemia prediction
| Study Context | Model | Accuracy | AUC | Kappa | F1-Score | Citation |
|---|---|---|---|---|---|---|
| Hypoglycemia severity in hospitalized T2DM patients (n=1,798) | XGBoost | 92.6% | 0.955 | 0.860 | - | [47] |
| Logistic Regression | 83.8% | 0.788 | 0.685 | - | [47] | |
| Random Forest | 93.3% | 0.960 | 0.873 | - | [47] | |
| Hypo-/hyperglycemia in diabetes hemodialysis patients | XGBoost | - | 0.87 (Hyperglycemia) | - | 0.85 (Hyperglycemia) | [48] |
| Logistic Regression | - | 0.87 (Hyperglycemia) | - | 0.85 (Hyperglycemia) | [48] | |
| Sepsis prediction in severe burn patients (n=103) | XGBoost | - | 0.91 | - | - | [49] |
| Logistic Regression | - | 0.88 | - | - | [49] | |
| Insulin dependency prediction (n=100) | XGBoost | 88% | - | - | 0.88 | [50] |
| Logistic Regression | 76% | - | - | 0.74 | [50] |
Broader Model Context: LSTM and ARIMA
While this guide focuses on logistic regression and XGBoost for classification tasks, research into glucose prediction has also explored time-series approaches, including Long Short-Term Memory (LSTM) networks and Auto-Regressive Integrated Moving Average (ARIMA) models [20] [14]. These models serve different purposes in glucose management:
Table 2: Comparison of modeling approaches for glucose prediction
| Model Type | Primary Use Case | Strengths | Limitations |
|---|---|---|---|
| Logistic Regression | Classification of hypoglycemia risk/events | High interpretability, computational efficiency, well-established statistical properties | Limited capacity for capturing complex non-linear relationships without manual feature engineering [47] |
| XGBoost | Classification of hypoglycemia risk/events | Handles non-linear relationships, robust with missing values, high predictive accuracy | Reduced interpretability, potential overfitting without proper tuning [47] |
| LSTM | Time-series forecasting of continuous glucose values | Captures temporal dependencies in CGM data, effective for pattern recognition | Requires large datasets, computationally intensive, complex implementation [14] |
| ARIMA | Time-series forecasting of continuous glucose values | Effective for stationary time series, statistically rigorous, good for short-term prediction | Assumes linearity, limited by non-stationary data, less effective for long-term trends [20] [14] |
A comparative study on non-invasive glucose and cholesterol monitoring found that ARIMA surpassed LSTM in prediction accuracy, demonstrating about 71.7% lower RMSE for glucose prediction [20]. For diabetes burden forecasting, deep learning models like Transformer-VAE have shown superior accuracy (MAE: 0.425, RMSE: 0.501) compared to traditional statistical methods [14].
Experimental Protocols and Methodologies
Study Design and Patient Population
The referenced study on hypoglycemia severity prediction in hospitalized T2DM patients employed a retrospective design using data from the electronic medical record system of the Affiliated Hospital of Qingdao University [47]. From an initial cohort of 8,947 patients, 1,798 patients were included after applying inclusion and exclusion criteria. Patients were categorized into three groups based on venous plasma glucose levels measured during hospitalization:
- Normal glycemia: >3.9 mmol/L
- Mild hypoglycemia: 3.0 – 3.9 mmol/L
- Moderate-to-severe hypoglycemia: <3.0 mmol/L [47]
Data Collection and Preprocessing
Researchers collected comprehensive clinical and demographic data from electronic medical records, including:
- Demographic characteristics (age, gender)
- Clinical features (body mass index classification, Charlson Comorbidity Index)
- Laboratory findings (HbA1c, mean blood glucose levels, serum creatinine, C-peptide, lipid profile)
- Medication use (insulin, metformin, DPP-4 inhibitors) [47]
Data preprocessing followed rigorous standards, including handling of missing values, normalization of continuous variables, and encoding of categorical variables. For logistic regression, additional preprocessing included feature scaling and creation of interaction terms to capture non-linear relationships [51].
Model Development and Validation
Three predictive models were developed and evaluated: multinomial logistic regression, XGBoost, and Random Forest [47]. The model development process included:
- Hyperparameter tuning: Optimized using cross-validation for XGBoost (nrounds, max_depth, eta) and Random Forest (ntree, mtry)
- Validation method: 5-fold cross-validation without a separate testing set
- Performance metrics: Overall accuracy, Kappa statistic, area under the ROC curve (AUC) [47]
The multiclass ROC curves were constructed using a One-vs-Rest approach to evaluate model discrimination across the three hypoglycemia severity classes [47].
Figure 1: Experimental workflow for hypoglycemia severity prediction models
Model Interpretation and Clinical Insights
Feature Importance Analysis
Both XGBoost and logistic regression provide insights into key predictors for hypoglycemia severity, though through different interpretability frameworks:
Table 3: Key predictors for hypoglycemia identified across modeling approaches
| Model | Key Predictors Identified | Interpretability Method |
|---|---|---|
| XGBoost | Glycemic control metrics, glucose variability, basal metabolic parameters [47] | Built-in feature importance, SHAP analysis [49] |
| Logistic Regression | Age, admission time, burn index, fibrinogen, NLR [49] | Coefficient analysis, odds ratios [49] |
| Random Forest | Glycemic control metrics, glucose variability, medication usage [47] | Feature importance metrics |
In the burn patient study, SHAP (SHapley Additive exPlanations) visualization for XGBoost identified fibrinogen, neutrophil-to-lymphocyte ratio (NLR), burn index, and age as the most important features for predicting sepsis [49]. Similarly, the hypoglycemia severity study found that while both XGBoost and Random Forest identified glycemic control metrics and glucose variability as core predictors, Random Forest additionally emphasized medication usage, whereas XGBoost prioritized basal metabolic parameters [47].
Decision Pathways for Model Selection
The choice between logistic regression and XGBoost depends on the specific clinical context, data characteristics, and implementation requirements. The following diagram illustrates the decision pathway for selecting the appropriate modeling approach:
Figure 2: Decision pathway for model selection between Logistic Regression and XGBoost
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential resources and tools for hypoglycemia prediction research
| Resource/Tool | Specification/Function | Application in Research |
|---|---|---|
| Electronic Health Records | Structured clinical data including demographics, lab results, medications | Primary data source for model training and validation [47] |
| Statistical Software (SPSS, R) | Statistical analysis and traditional modeling | Implementation of logistic regression models, statistical testing [49] |
| Python ML Ecosystem | Scikit-learn, XGBoost, Pandas, NumPy | Implementation and tuning of XGBoost and other ML algorithms [50] |
| SHAP (SHapley Additive exPlanations) | Model interpretability framework | Explaining XGBoost predictions, feature importance analysis [49] |
| Continuous Glucose Monitoring (CGM) | Dexcom G6 system or equivalent | Real-time glucose data for dynamic prediction models [48] |
| Cross-Validation Frameworks | 5-fold or 10-fold cross-validation | Model validation, hyperparameter tuning, performance estimation [47] |
The comparative analysis demonstrates that both logistic regression and XGBoost offer distinct advantages for predicting hypoglycemia severity in hospitalized patients. XGBoost consistently achieves superior predictive performance with higher accuracy, AUC values, and better handling of complex variable interactions [47] [49]. However, logistic regression remains valuable when model interpretability is paramount for clinical decision-making [47].
For researchers and clinicians, the selection between these models should be guided by specific clinical requirements, dataset characteristics, and implementation constraints. Future research directions should focus on developing hybrid approaches that leverage the strengths of both models, enhancing interpretability of XGBoost through techniques like SHAP, and validating these models in diverse clinical settings and patient populations.
Non-invasive monitoring represents a frontier in healthcare technology, aiming to provide continuous, pain-free health assessments. A particularly impactful application is the management of diabetes, where frequent glucose monitoring is essential. Traditional methods relying on finger-prick blood extraction cause discomfort and carry infection risks, making non-invasive alternatives highly desirable [52]. Near-Infrared (NIR) spectroscopy has emerged as a promising sensing technology for this purpose, capable of measuring physiological analytes like glucose through the skin [52] [53]. However, NIR signals for subtle physiological changes like glucose concentration are inherently weak, noisy, and difficult to correlate directly with analyte levels using traditional analysis [52].
This challenge has driven the integration of advanced forecasting models that can interpret complex NIR data and predict future physiological states. This guide objectively compares the performance of three prominent forecasting models—Logistic Regression, Long Short-Term Memory (LSTM) networks, and Autoregressive Integrated Moving Average (ARIMA)—when applied to NIR-based glucose prediction. We provide supporting experimental data and detailed methodologies to help researchers, scientists, and drug development professionals select the optimal sensing and forecasting combination for their specific applications.
NIR Sensing Technology: From Benchtop to Handheld
Technology Fundamentals and Comparison
NIR spectroscopy operates on the principle of light absorption in the 780–2500 nm wavelength range. Molecular bonds such as O-H, C-H, and C-O absorb light at specific wavelengths, creating spectral signatures that convey information about the chemical composition and physical properties of organic materials [52]. The absorption corresponds to overtones and combinations of fundamental molecular vibrations, allowing for quantitative analysis without chemical consumables or sample destruction [54].
Table 1: Comparison of NIR Spectroscopy System Types
| System Type | Typical Wavelength Range | Detector Technology | Key Advantages | Typical Applications | Performance Notes |
|---|---|---|---|---|---|
| Benchtop Spectrometer | 1100–2500 nm | High-performance array | High signal-to-noise ratio, broad range, high resolution | Laboratory analysis, reference measurements | Superior accuracy for most analytes; considered gold standard for validation [55] [56] |
| Portable/Hyperspectral Imaging (SWIR-HSI) | 1000–2500 nm | Mercury Cadmium Telluride (MCT) | Visualizes spatial variability, scans larger areas | Wood properties, industrial process monitoring [55] | Performance comparable to benchtop for some applications; favors wavelengths >1900 nm [55] |
| Portable/Hyperspectral Imaging (NIR-HSI) | 900–1700 nm | Indium Gallium Arsenide (InGaAs) | Faster scanning, visualizes spatial variability | Wood properties, biological materials [55] | Limited wavelength range can provide best models for some properties [55] |
| Handheld Spectral Sensor Module | 850–1700 nm | Fully-integrated multipixel array | Extreme portability, robustness, low cost, suitable for non-specialists | Moisture content quantification, plastic classification, supply chain monitoring [54] | Practical for field use; accuracy generally lower than benchtop but sufficient for many applications [54] [56] |
Performance Considerations for Physiological Monitoring
For glucose prediction in whole blood, research indicates that optimal wavelength regions are 1390–1888 nm and 2044–2393 nm [53]. The accuracy of glucose prediction is influenced by hemoglobin concentration, necessitating that calibration models include samples representing the entire physiological range of hemoglobin levels [53]. Achieving clinically acceptable accuracy remains challenging due to the weak and highly overlapping spectral signals from different blood constituents [52].
Miniaturized NIR sensors represent a significant advancement, moving from traditional bulky, expensive spectrometers to compact, robust devices suitable for portable and continuous monitoring [54]. These integrated modules, such as the SpectraPod based on ChipSense technology, measure a limited number of spectral bands (e.g., 16 pixels) with broad resolution (50–100 nm) rather than full spectra, yet achieve comparable performance to portable spectrometers for applications like moisture quantification and material classification [54].
Forecasting Models for Physiological Prediction
Model Selection and Theoretical Foundations
Time series forecasting is a critical component of non-invasive monitoring systems, enabling the prediction of future physiological states based on historical data [57]. For glucose monitoring, different forecasting models offer distinct advantages and limitations.
ARIMA (Autoregressive Integrated Moving Average) models are classical statistical approaches for time series forecasting. They combine autoregressive (AR) components that use past values, integration (I) to make data stationary, and moving average (MA) components that incorporate past forecast errors [58]. ARIMA models are particularly effective for data with clear trends but minimal seasonality.
Logistic Regression is a statistical model used for classification rather than continuous value prediction. In glucose forecasting, it can categorize future glucose levels into clinically relevant classes such as hypoglycemia, euglycemia, and hyperglycemia [1].
LSTM (Long Short-Term Memory) networks are a type of recurrent neural network designed to model temporal sequences and long-term dependencies. Their gate mechanisms (input, forget, output) allow them to selectively remember and forget information over extended periods, making them powerful for complex physiological forecasting [1].
Comparative Performance in Glucose Forecasting
Recent research provides direct comparisons of these models for glucose prediction. One comprehensive study evaluated ARIMA, Logistic Regression, and LSTM models for predicting hypoglycemia (<70 mg/dL), euglycemia (70-180 mg/dL), and hyperglycemia (>180 mg/dL) at 15-minute and 1-hour horizons [1].
Table 2: Forecasting Model Performance for Glucose Prediction [1]
| Model | Prediction Horizon | Recall (Hyperglycemia) | Recall (Euglycemia) | Recall (Hypoglycemia) | Overall Strengths and Limitations |
|---|---|---|---|---|---|
| Logistic Regression | 15 minutes | 96% | 91% | 98% | Excellent short-term classification; simple, interpretable model |
| LSTM | 15 minutes | Lower than Logistic Regression | Lower than Logistic Regression | Lower than Logistic Regression | Complex; requires more data; not optimal for very short-term |
| ARIMA | 15 minutes | Underperformed others | Underperformed others | Underperformed others | Not suitable for classification tasks; better for continuous value prediction |
| Logistic Regression | 1 hour | Performance decreased | Performance decreased | Performance decreased | Limited capacity for longer-term temporal dependencies |
| LSTM | 1 hour | 85% | Not specified | 87% | Superior for longer-term forecasting; captures complex patterns |
| ARIMA | 1 hour | Underperformed others | Underperformed others | Underperformed others | Consistently the weakest performer for glucose classification |
The results demonstrate that model performance is highly dependent on the prediction horizon. Logistic Regression excelled at short-term prediction (15 minutes), particularly for critical hypoglycemia detection, while LSTM networks showed superior performance for longer-term predictions (1 hour) [1]. ARIMA consistently underperformed for this classification task, as it is fundamentally designed for continuous value forecasting rather than classification [1].
Integrated System Performance: NIR Sensing with Forecasting Models
Experimental Protocols for Integrated Systems
The integration of NIR sensing with forecasting models involves a multi-stage process. For glucose prediction, the experimental workflow typically follows this pathway:
Key methodological considerations for integrated NIR-forecasting systems include:
Data Collection: For glucose prediction, studies use either aqueous glucose solutions with concentrations spanning physiological ranges (40-500 mg/dL) [52] or whole blood samples with varying glucose and hemoglobin concentrations to account for this key interfering variable [53]. Sufficient data volume is critical, with recommendations of at least 2-3 years of data (24-36 data points minimum) for robust forecasting models [58].
Spectral Preprocessing: Raw NIR spectra require preprocessing to reduce noise and enhance relevant features. Common techniques include Standard Normal Variate (SNV), Multiplicative Scatter Correction (MSC), and Savitzky-Golay derivatives [59] [52].
Feature Engineering: When only glucose level data is available, features can be engineered from the changes in glucose levels themselves, including rate of change metrics, variability indices, and time-based features like moving averages [1].
Model Validation: Proper validation involves multiple testing sets rather than a single train-test split, as random splitting can lead to misleading conclusions [52]. Temporal validation should ensure training data precedes test data chronologically to avoid biased evaluations [57].
Integrated System Performance Data
Table 3: Performance of Integrated NIR-Forecasting Systems
| NIR System | Forecasting Model | Analyte/Application | Performance Metrics | Key Findings |
|---|---|---|---|---|
| Laboratory NIR Spectrometer | PLSR, SVMR, RF, ETR, Xgboost, PCA-NN | Aqueous glucose concentration [52] | Best models: SVMR, ETR, PCA-NN achieved high accuracy | Model performance largely affected by pattern of important features learned; different models identified different important wavelengths |
| NIR Spectrometer | PLSR | Glucose in whole blood [53] | Standard error: 25.5 mg/dL, Coefficient of variation: 11.2% | Optimal wavelength regions: 1390-1888 nm and 2044-2393 nm; hemoglobin concentration significantly influences calibration |
| Continuous Glucose Monitor (simulated) | Logistic Regression vs. LSTM vs. ARIMA | Glucose level classification [1] | 15-min recall: Logistic Regression (Hypo: 98%, Hyper: 96%); 1-hr recall: LSTM (Hypo: 87%, Hyper: 85%) | Different models have varying strengths by prediction horizon; ARIMA consistently underperformed for classification |
| Benchtop vs. Handheld NIR | PLSR | Amino acids in frozen mutton [56] | Benchtop: higher accuracy for most amino acids; Handheld: practical for field applications | Benchtop's broader spectral range provided superior accuracy; handheld systems acceptable for real-time field use |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Materials for NIR-Forecasting Integration
| Item | Function/Application | Specification Notes |
|---|---|---|
| NIR Spectrometer | Reference measurements and method validation | Benchtop systems with broad wavelength range (1100-2500 nm) for laboratory development work [55] [56] |
| Handheld NIR Sensor Module | Field deployment and portable monitoring | Integrated multipixel arrays (e.g., 16 pixels, 850-1700 nm) for in-situ measurements [54] |
| Hyperspectral Imaging Systems | Spatial variability assessment and heterogeneous samples | SWIR-HSI (1000-2500 nm) or NIR-HSI (900-1700 nm) cameras for material surface analysis [55] |
| Reference Analytical Instrument | Ground truth validation | HPLC for pharmaceutical validation [60]; amino acid analyzers for nutritional assessment [56] |
| Glucose Reference Materials | Calibration and validation | Aqueous glucose solutions (40-500 mg/dL) [52]; whole blood samples with varying hemoglobin [53] |
| Spectral Preprocessing Software | Data cleaning and enhancement | Capability for SNV, MSC, derivative filters, and feature extraction [59] [52] |
| Time Series Analysis Platform | Forecasting model development | Support for ARIMA, Logistic Regression, LSTM, and performance metrics calculation [1] [58] |
The integration of NIR sensors with forecasting models presents a powerful approach for non-invasive monitoring, with glucose prediction serving as a prominent application. Our comparison reveals several key strategic considerations:
For short-term prediction horizons (15-30 minutes), the combination of handheld NIR sensors with Logistic Regression models provides an optimal balance of performance, interpretability, and computational efficiency, particularly for classification tasks like hypoglycemia detection.
For long-term prediction (60 minutes or more), LSTM networks paired with high-quality NIR spectra (preferably from benchtop or high-performance portable systems) deliver superior performance by capturing complex temporal dependencies, though requiring more substantial computational resources and larger datasets.
ARIMA models show limited utility for classification tasks in physiological monitoring but may remain valuable for continuous value forecasting in applications with clear trends and minimal seasonality.
Benchtop NIR systems maintain advantages in research and development contexts where maximum accuracy is essential, while handheld NIR modules offer compelling capabilities for field deployment and continuous monitoring despite somewhat reduced accuracy.
Future developments should focus on hybrid modeling approaches that combine the strengths of multiple forecasting techniques, enhanced feature selection methods to identify the most clinically relevant spectral variables, and continued miniaturization of NIR technology without compromising analytical performance.
Overcoming Practical Challenges: Optimization and Advanced Strategies
Addressing Data Imbalance and Rare Glycemic Excursions with Custom Loss Functions
Accurate prediction of glycemic excursions, particularly hypoglycemia (<70 mg/dL) and hyperglycemia (>180 mg/dL), represents a significant challenge in diabetes management due to the inherent data imbalance in continuous glucose monitoring (CGM) records. These clinically critical events are relatively rare compared to time spent in the normal range (70-180 mg/dL), creating a classic imbalanced regression problem where standard loss functions like mean squared error (MSE) often prioritize majority patterns at the expense of critical minority events [5]. This analytical limitation has direct clinical consequences, as hypoglycemia can lead to acute symptoms including confusion, seizures, and coma, while persistent hyperglycemia contributes to long-term complications such as heart disease, kidney failure, and blindness [61].
The fundamental statistical challenge stems from the natural distribution of glucose values, where only approximately 2-10% of readings typically fall into the hypoglycemic range and about 30-40% into the hyperglycemic range, creating a significant imbalance that conventional machine learning approaches struggle to model effectively [5]. This article provides a comprehensive comparison of how different modeling frameworks—statistical (ARIMA), traditional machine learning (logistic regression), and deep learning (LSTM)—cope with this imbalance, with particular emphasis on innovative custom loss functions designed to enhance prediction of clinically critical glycemic excursions.
Comparative Model Performance Analysis
Quantitative Performance Metrics Across Model Architectures
Table 1: Comparative Performance of Predictive Models for Glycemic Excursion Classification
| Model | Prediction Horizon | Hypoglycemia Recall | Hyperglycemia Recall | Euglycemia Recall | Key Strengths | Key Limitations |
|---|---|---|---|---|---|---|
| Logistic Regression [1] | 15 minutes | 98% | 96% | 91% | Excellent short-term performance, computationally efficient | Limited temporal dependency modeling |
| LSTM [1] | 60 minutes | 87% | 85% | Not reported | Superior long-term predictions, captures complex temporal patterns | Computationally intensive, requires substantial data |
| ARIMA [1] | 15-60 minutes | Lowest performance across classes | Lowest performance across classes | Lowest performance across classes | Computational efficiency, simplicity | Poor excursion prediction, limited pattern recognition |
| FedGlu with HH Loss [5] | 30-60 minutes | 35% improvement vs. local models | 35% improvement vs. local models | Maintained performance | Data privacy preservation, enhanced excursion detection | Implementation complexity |
Table 2: Glucose Forecasting Accuracy Metrics (Regression Tasks)
| Model | Prediction Horizon | RMSE (mg/dL) | MAE (mg/dL) | Specialized Features | Clinical Validation |
|---|---|---|---|---|---|
| DA-CMTL Framework [62] | 30 minutes | 14.01 | 10.03 | Multi-task learning (glucose forecasting + hypoglycemia classification) | Real-world validation in diabetes-induced rats |
| Transformer-VAE [14] | Long-term trends | 0.501 (normalized) | 0.425 (normalized) | Robustness to noisy/missing data | Population-level burden forecasting |
| Virtual CGM (LSTM) [63] | 15 minutes | 19.49 ± 5.42 | Not reported | Life-log data integration (diet, activity) | Healthy adult population |
| HH Loss Function [5] | 30-60 minutes | 46% improvement over MSE | Not reported | Range-dependent error penalization | 125 patients with type 1 diabetes |
Critical Analysis of Model Architectures for Rare Event Prediction
The comparative data reveals distinct advantages and limitations for each modeling approach in handling glycemic excursions. Logistic regression demonstrates surprisingly strong performance for short prediction horizons (15 minutes), achieving exceptional recall rates of 98% for hypoglycemia and 96% for hyperglycemia [1]. This suggests that for immediate-term predictions, simpler models with appropriate feature engineering can effectively capture the fundamental patterns preceding excursions without the complexity of deep learning architectures.
Long Short-Term Memory (LSTM) networks excel at longer prediction horizons (60 minutes), making them particularly valuable for proactive intervention [1]. Their ability to model complex temporal dependencies allows them to recognize subtle patterns in glucose dynamics that precede critical events. The bidirectional LSTM architecture with encoder-decoder structure has shown particular promise for glucose level inference using life-log data (food intake, physical activity) without relying on previous glucose measurements, achieving an RMSE of 19.49 ± 5.42 mg/dL [63]. This capability is especially valuable during CGM sensor gaps or for virtual CGM applications.
The ARIMA model consistently underperforms for glycemic excursion prediction across all time horizons [1]. Its limitations in capturing the complex, nonlinear nature of glucose dynamics and its inability to effectively incorporate external covariates (meals, insulin, activity) make it poorly suited for the nuanced pattern recognition required for rare event prediction in glucose variability.
Most significantly, the incorporation of custom loss functions specifically designed for glucose prediction has demonstrated substantial improvements over conventional approaches. The Hypo-Hyper (HH) loss function, which applies higher penalties for prediction errors in glycemic excursion ranges compared to the normal range, shows a 46% improvement over standard mean-squared error (MSE) and a 35% improvement in glycemic excursion detection compared to local models [5]. This specialized approach addresses the core imbalance problem by explicitly weighting clinically critical errors more heavily during model training.
Methodological Approaches for Handling Data Imbalance
Custom Loss Functions: The HH Loss Paradigm
The Hypo-Hyper (HH) loss function represents a targeted approach to the data imbalance problem in glucose prediction [5]. Unlike standard loss functions that treat all prediction errors equally, the HH loss implements a range-dependent penalization scheme with substantially higher penalties for errors occurring in hypoglycemic and hyperglycemic ranges compared to the normal euglycemic range. This cost-sensitive approach directly addresses the clinical reality that errors in prediction have varying significance depending on the glycemic context—a 20 mg/dL error in hypoglycemia carries far greater clinical urgency than the same magnitude error in the hyperglycemic or normal ranges.
The mathematical formulation of such specialized loss functions typically incorporates weighting mechanisms that increase the cost associated with errors in critical ranges, forcing the model to prioritize accuracy where it matters most. When implemented within a federated learning framework (FedGlu), this approach has demonstrated significant improvements in glycemic excursion detection while simultaneously addressing data privacy concerns by keeping sensitive patient data localized [5].
Sampling and Architectural Strategies
Beyond custom loss functions, researchers have employed additional strategies to mitigate data imbalance:
Multi-task learning frameworks like the Domain-Agnostic Continual Multi-Task Learning (DA-CMTL) simultaneously perform glucose level forecasting and hypoglycemia event classification within a unified architecture [62]. This approach leverages shared temporal features while specializing in both regression and classification tasks, improving robustness and performance for rare hypoglycemia events. The framework employs Sim2Real transfer, training on diverse simulated datasets before adapting to real-world data, thereby exposing the model to a wider range of glycemic scenarios, including rare events.
Federated learning architectures enable collaborative model training across multiple institutions or patients without sharing sensitive raw data [5]. By aggregating model parameters rather than data, these approaches effectively increase the effective training dataset size, providing more examples of rare glycemic excursions while maintaining privacy compliance. The combination of federated learning with specialized HH loss functions represents a particularly powerful approach for addressing both data scarcity and privacy concerns simultaneously.
Experimental Protocols and Methodologies
Standardized Experimental Framework for Model Comparison
To ensure fair comparison across different model architectures, researchers have established standardized evaluation protocols using publicly available datasets and consistent validation methodologies. The OhioT1DM dataset has emerged as a benchmark for many comparative studies, containing eight weeks of continuous glucose monitoring, insulin dosing, physiological recordings, and self-reported life events for 12 individuals with type 1 diabetes [62] [61].
A typical experimental workflow involves several key stages, as illustrated below:
Diagram 1: Experimental workflow for glucose prediction model development
Feature Engineering and Data Preparation
Effective glucose prediction relies on comprehensive feature engineering that captures both temporal patterns and contextual factors influencing glucose variability. The most successful approaches incorporate multiple data modalities:
Temporal features include rolling averages, rate of change calculations, and seasonal decomposition of glucose trends [1]. These features help capture the dynamic nature of glucose fluctuations and identify patterns preceding excursions.
Contextual features incorporate meal information (carbohydrate quantity, timing), insulin administration (bolus timing, basal rates), physical activity (duration, intensity), and other physiological parameters (heart rate, sleep quality) [63] [1]. The integration of life-log data has proven particularly valuable for virtual CGM systems that operate without continuous glucose measurement input during inference.
Physiological features derived from complementary signals such as ECG (QT interval, heart rate variability), PPG, and electrodermal activity provide additional biomarkers correlated with glycemic states [61]. Multimodal approaches that fuse these diverse data streams have demonstrated improved predictive accuracy for glycemic excursions.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Resources for Glucose Prediction Research
| Resource Category | Specific Examples | Research Application | Key Characteristics |
|---|---|---|---|
| Public Datasets | OhioT1DM [62], PhysioCGM [61], ShanghaiT1DM [62] | Model training & benchmarking | CGM data, insulin records, life-log data, multimodal physiological signals |
| Simulation Tools | UVA/Padova T1D Simulator [1], Simglucose [1] | Data augmentation, algorithm testing | Simulated patients across age groups, meal scenarios, and insulin protocols |
| Deep Learning Frameworks | TensorFlow/Keras [64], PyTorch | Custom model implementation | Support for custom loss functions, LSTM/GRU architectures, federated learning |
| Evaluation Metrics | RMSE, MAE, Recall/Sensitivity, Precision, Parkes Error Grid [65] | Performance validation | Combines statistical accuracy with clinical significance assessment |
| Specialized Loss Functions | HH Loss [5], Weighted Categorical Cross-Entropy [64] | Handling class imbalance | Range-dependent error weighting, class-weighted optimization |
The comparative analysis presented in this guide reveals that model selection for glucose prediction must be guided by specific clinical requirements and implementation constraints. For short-term prediction horizons (15-30 minutes), logistic regression with sophisticated feature engineering provides unexpectedly strong performance with minimal computational overhead [1]. For longer prediction horizons (60 minutes) and more complex pattern recognition, LSTM architectures deliver superior performance despite their computational demands [63] [1].
Most importantly, the implementation of specialized techniques for handling data imbalance—particularly custom loss functions like the HH loss—emerges as a critical factor across all model architectures [5]. These approaches directly address the fundamental challenge of rare glycemic excursions by explicitly weighting clinically significant errors during model optimization.
Future research directions should focus on hybrid approaches that combine the computational efficiency of simpler models with the sophisticated pattern recognition of deep learning, while maintaining the privacy-preserving advantages of federated learning frameworks. The integration of multimodal physiological data with traditional CGM and life-log information presents another promising avenue for improving prediction accuracy, particularly for non-invasive glucose monitoring applications [61]. As these technologies mature, the integration of robust, imbalance-aware prediction models into automated insulin delivery systems will play an increasingly vital role in improving diabetes management outcomes.
Mitigating Overfitting and Improving Generalization with Multi-Task and Federated Learning
Overfitting presents a fundamental challenge in machine learning, where models perform well on training data but fail to generalize to unseen data. This problem is particularly acute in healthcare applications like glucose prediction, where model reliability directly impacts clinical decision-making. Multi-Task Learning (MTL) and Federated Learning (FL) have emerged as powerful paradigms that inherently combat overfitting through different mechanistic approaches.
MTL enhances generalization by learning multiple related tasks simultaneously, forcing models to develop more robust, generalized representations rather than specializing in nuances of a single dataset. Federated Learning addresses overfitting by training models across distributed data sources without data sharing, naturally exposing models to diverse data distributions and reducing dependency on dataset-specific artifacts. When integrated, these approaches offer complementary strengths for building predictive models that maintain accuracy across varying patient populations and clinical settings, making them particularly valuable for glucose prediction systems where data heterogeneity and privacy concerns are significant considerations.
Comparative Analysis of Multi-Task Learning Frameworks
Key MTL Architectures and Their Applications
Multiple MTL frameworks have been developed with distinct approaches to knowledge sharing and overfitting mitigation, each offering different trade-offs between performance, computational efficiency, and implementation complexity.
Table 1: Comparison of Multi-Task Learning Frameworks
| Framework | Core Methodology | Overfitting Mitigation Strategy | Best-Suited Applications | Key Advantages |
|---|---|---|---|---|
| UNITI [66] | Inter-dataset MTL with sequential training | Structural reparameterization, knowledge distillation | Heterogeneous datasets with different label sets | Eliminates need for multi-label datasets; prevents catastrophic forgetting |
| MMOE [67] | Multi-gate mixture-of-experts | Explicit learning of task correlations via gating networks | Tasks with varying correlation levels (e.g., CTR & CVR prediction) | Adapts to task relationships; reduces negative transfer |
| GradNorm [67] | Adaptive loss balancing | Gradient normalization across tasks | Tasks with different loss scales and convergence speeds | Dynamically adjusts task weights; balances learning rates |
| Gradient-Blending [67] | Generalization-aware weighting | Weight tuning based on overfitting rates | Multimodal networks with different overfitting patterns | Penalizes overfitting tasks; maintains generalization |
Quantitative Performance Comparison
Experimental evaluations across diverse domains demonstrate the effectiveness of these MTL frameworks in improving generalization while mitigating overfitting.
Table 2: Experimental Performance of MTL Frameworks
| Framework | Dataset | Evaluation Metrics | Performance Improvement | Generalization Gap Reduction |
|---|---|---|---|---|
| UNITI [66] | Facial age estimation | MAE | 3.4706 (baseline) → 3.0834 (UNITI) | Significant improvement in cross-dataset evaluation |
| UNITI with Knowledge Distillation [66] | Facial age estimation | MAE | 3.4706 (baseline) → 2.9267 (UNITI+KD) | Enhanced robustness to noisy inputs |
| MMOE [67] | Synthetic data (low-correlation tasks) | Accuracy | Consistently superior to OMOE baseline | Maintains performance across varying task correlations |
| GradNorm [67] | Synthetic data (different task scales) | Training efficiency | Faster convergence for small-scale tasks | Balanced learning across tasks with different scales |
Federated Learning Approaches for Enhanced Generalization
FL Frameworks for Heterogeneous Data
Federated Learning introduces additional dimensions to generalization by addressing data distribution challenges across multiple clients or institutions while maintaining data privacy.
Table 3: Comparison of Federated Learning Frameworks
| Framework | Core Methodology | Generalization Strategy | Data Heterogeneity Handling | Theoretical Guarantees |
|---|---|---|---|---|
| FedSWA/FedMoSWA [68] [69] | Stochastic weight averaging with momentum | Finding flat minima | Highly effective for non-IID data | Convergence analysis and generalization bounds provided |
| Sharpness-Aware Minimization (SAM) [70] | Seeking flat minima | Parameter neighborhoods with uniform low loss | Effective in homogeneous and heterogeneous scenarios | Geometrical foundation through loss Hessian eigenspectrum |
| Federated Multi-Task under Mixture of Distributions [71] | Federated EM-like algorithms | Modeling local distributions as mixture of underlying distributions | Encompasses most personalized FL approaches | Novel federated surrogate optimization framework |
| FedDEA [72] | Subspace decoupling | Update-structure-aware aggregation | Specifically designed for highly heterogeneous tasks | Task-level decoupled aggregation within unified global model |
| FedHCA² [73] | Hyper conflict-averse aggregation | Modeling client relationships; cross-attention decoder interactions | Addresses model incongruity in hetero-client FMTL | Theoretical insights into multi-task vs federated optimization |
Performance Evaluation of FL Frameworks
Empirical studies demonstrate how specialized FL algorithms improve generalization under challenging heterogeneous data conditions.
Table 4: Experimental Performance of Federated Learning Frameworks
| Framework | Dataset | Heterogeneity Setting | Performance Improvement | Generalization Advantage |
|---|---|---|---|---|
| FedSWA/FedMoSWA [68] | CIFAR-10/100, Tiny ImageNet | Highly heterogeneous data | Superior to FedSAM and variants | Finds flatter minima; better local-global model alignment |
| Sharpness-Aware Minimization [70] | CIFAR10/100, Landmarks-User-160k, IDDA | Homogeneous and heterogeneous scenarios | Substantial improvement over baseline FL | Converges toward flatter minima with uniform low loss |
| FedHCA² [73] | NYUD-V2, PASCAL-Context | Highly heterogeneous task settings | Superior to representative methods | Mitigates conflicts during encoder updates; handles model incongruity |
Experimental Protocols and Methodologies
UNITI Framework Protocol
The UNITI framework employs a systematic methodology for inter-dataset multi-task learning:
Dataset Preparation: Collect independent datasets with different task annotations rather than a single multi-label dataset.
Sequential Training Strategy: Implement carefully designed sequential training to prevent catastrophic forgetting:
- Train on Dataset A with Task A labels
- Fine-tune on Dataset B with Task B labels while retaining performance on Task A
- Employ knowledge distillation to transfer knowledge from specialized teacher models
Structural Reparameterization: Integrate techniques like RepVGG and RepMixer to optimize model efficiency during inference by merging multiple layers into single-layer representations [66].
Evaluation: Assess performance on each task separately using task-specific metrics (e.g., MAE for age estimation, accuracy for classification) while monitoring for overfitting through validation on unseen data.
FedSWA/FedMoSWA Implementation
For federated learning with highly heterogeneous data:
Client Configuration: Set up multiple clients with non-IID data distributions to simulate real-world data heterogeneity.
Stochastic Weight Averaging:
- Maintain running average of model parameters across training rounds
- Apply momentum to stabilize the averaging process
- Control weight averaging to prioritize flatter minima in the loss landscape
Local Training: Each client performs local optimization using the FedSAM approach, which seeks parameters in neighborhoods with uniformly low loss.
Server Aggregation: Implement novel momentum-based stochastic controlled weight averaging to better align local and global models, effectively dealing with client drift [68] [69].
Convergence Monitoring: Track both optimization metrics and generalization gaps throughout training, using theoretical bounds to identify potential overfitting.
MMOE and GradNorm Experimental Setup
For multi-task learning with task relationship optimization:
Task Correlation Analysis: Pre-evaluate task relationships using correlation metrics or domain knowledge.
MMOE Implementation:
- Design shared expert networks with specialized gating mechanisms
- Implement separate gating networks for each task with linear transformation and softmax layers
- Allow tasks to selectively utilize experts based on their specific needs
GradNorm Optimization:
- Monitor gradient magnitudes for each task throughout training
- Calculate inverse training rates as Li(t) = Li(t)/L_i(0) for each task i at time t
- Implement gradient loss to balance learning across tasks: Lgrad = Σi |GW^(i) - GW(t) × [ri(t)]^α| where GW^(i) is gradient norm for task i, and α is a tuning parameter [67]
- Apply backpropagation on loss weights only to maintain balanced contribution to shared parameter updates
Visualization of Methodologies
UNITI Framework Workflow
Federated Multi-Task Learning Architecture
MMOE and Adaptive Weighting Mechanisms
Research Reagent Solutions
Table 5: Essential Research Tools for MTL and FL Experiments
| Research Tool | Function | Example Implementations |
|---|---|---|
| Structural Reparameterization | Merges multiple training-time layers into inference-efficient blocks | RepVGG [66], RepMixer [66] |
| Knowledge Distillation | Transfers knowledge from teacher to student models | UNITI framework [66] |
| Sharpness-Aware Minimization | Finds parameters in neighborhoods with uniform low loss | FedSAM [70] [68] |
| Stochastic Weight Averaging | Averages multiple points along training trajectory for flat minima | FedSWA, FedMoSWA [68] [69] |
| Multi-Gate Mixture-of-Experts | Learns task relationships through gating mechanisms | MMOE [67] |
| Gradient Normalization | Balances learning across tasks with different scales | GradNorm [67] |
| Federated Aggregation Algorithms | Coordinates multi-client training without data sharing | FedDEA [72], FedHCA² [73] |
The integration of Multi-Task Learning and Federated Learning represents a promising frontier for developing machine learning systems that robustly resist overfitting and generalize effectively across diverse populations and conditions. Through systematic comparisons of architectural frameworks, optimization strategies, and experimental protocols, this guide provides researchers with evidence-based approaches for selecting and implementing these techniques.
For glucose prediction and other healthcare applications where model reliability directly impacts clinical decisions, these approaches offer pathways to more trustworthy AI systems. The continued development of methods that explicitly address data heterogeneity, task relationships, and generalization will be essential for translating machine learning advances into real-world healthcare applications that maintain performance across diverse patient populations and clinical settings.
Handling Data Scarcity and Privacy Concerns with Sim2Real Transfer and Federated Frameworks
The accurate prediction of glucose levels represents a critical challenge in modern healthcare, particularly for managing diabetes and critical conditions like sepsis. Researchers and clinicians face two fundamental constraints: data scarcity, where limited patient-specific data hinders model generalization, and privacy concerns, which restrict data sharing across institutions. Within this context, three modeling approaches—logistic regression, Long Short-Term Memory (LSTM) networks, and the AutoRegressive Integrated Moving Average (ARIMA)—are frequently employed, each with distinct strengths and weaknesses pertaining to these challenges [1] [20].
This guide objectively compares the performance of these models, framing the analysis within a broader thesis on their predictive accuracy for glucose levels. It further explores how advanced computational frameworks, namely Sim2Real Transfer and Federated Learning (FL), can mitigate data scarcity and privacy issues. By synthesizing recent experimental data and detailing relevant methodologies, this article provides researchers, scientists, and drug development professionals with a evidence-based resource for selecting and implementing robust, privacy-preserving predictive models.
Comparative Analysis of Glucose Prediction Models
Experimental data from recent studies allows for a direct comparison of logistic regression, LSTM, and ARIMA models across short- and medium-term forecasting horizons.
Table 1: Comparative Performance of Glucose Prediction Models for Hypo-/Hyperglycemia Classification
| Model | Prediction Horizon | Key Performance Metric | Reported Value | Clinical Context |
|---|---|---|---|---|
| Logistic Regression | 15 minutes | Recall (Hypoglycemia) [1] | 98% | Real & Simulated CGM Data |
| LSTM | 1 hour | Recall (Hypoglycemia) [1] | 87% | Real & Simulated CGM Data |
| LSTM | 1 hour | Recall (Hyperglycemia) [1] | 85% | Real & Simulated CGM Data |
| ARIMA | 15 min & 1 hour | Performance vs. LR & LSTM [1] | Underperformed | Real & Simulated CGM Data |
| ARIMA | N/S | RMSE (Glucose Prediction) [20] | Lower than LSTM | Non-invasive NIR Sensor Data |
| LSTM | N/S | RMSE (Glucose Prediction) [20] | Higher than ARIMA | Non-invasive NIR Sensor Data |
Table 2: Performance of Advanced Architectures on Specific Forecasting Tasks
| Model | Prediction Task | Key Performance Metric | Reported Value | Context |
|---|---|---|---|---|
| PatchTST | 15-minute glucose forecast | Mean Max Percentage Error [12] | 3.0% | Septic ICU Patients |
| DLinear | 60-minute glucose forecast | Mean Max Percentage Error [12] | 14.41% | Septic ICU Patients |
| Transformer-VAE | Diabetes Burden (DALYs) | Mean Absolute Error [14] | 0.425 | Global Health Metrics |
Model-Specific Analysis
Logistic Regression: This model excels in short-term, classification-based predictions. Its superiority at a 15-minute horizon for classifying hypoglycemia demonstrates that simpler, interpretable models can be highly effective for specific, immediate clinical tasks, likely due to lower susceptibility to overfitting on limited data [1].
LSTM Networks: LSTMs show strength in medium-term forecasting, outperforming logistic regression at the 1-hour horizon. This is attributed to their ability to model complex temporal dependencies in sequential data like Continuous Glucose Monitoring (CGM) streams [1]. However, their performance is contingent on sufficient data volume and can be computationally intensive [14].
ARIMA Models: The performance of ARIMA is highly context-dependent. It underperformed compared to both LR and LSTM in classifying glycemic states from CGM data [1]. Conversely, another study found ARIMA superior to LSTM for predicting numerical glucose values from non-invasive sensor data, with a reported 71.7% lower RMSE [20]. This contradiction highlights that dataset characteristics, such as data source (CGM vs. NIR sensors) and preprocessing, significantly influence model efficacy.
Overcoming Data and Privacy Challenges with Advanced Frameworks
Federated Learning (FL) for Privacy Preservation
Federated Learning is a distributed machine learning paradigm that enables model training across multiple decentralized devices or servers holding local data samples without exchanging them [74]. This approach is particularly valuable in healthcare, where patient data is sensitive and subject to strict privacy regulations.
- Basic Workflow: The FL process involves a central server coordinating a series of training rounds. In each round, the server sends the global model to participating clients. Each client trains the model on its local data and sends the model updates back to the server. The server then aggregates these updates to improve the global model [74].
- Personalized Federated Learning: Standard FL assumes data is identically distributed across clients, which is often untrue in healthcare. Personalized FL strategies address this. For instance, the Self-FL method quantifies intra-client and inter-client uncertainty to adaptively adjust local training configurations and aggregation rules, leading to more accurate global and local models in heterogeneous environments [75].
- Experimental Support: Studies in building energy prediction (a domain analogous to healthcare in its data distribution challenges) have shown that personalized FL strategies can achieve a 10% reduction in prediction error compared to localized models and enhance robustness to missing data [76].
Sim2Real Transfer Learning for Data Scarcity
The Sim2Real paradigm involves training a model in a simulated environment and then transferring the learned knowledge to real-world applications. This is a powerful tool for addressing data scarcity, especially when real patient data is limited or costly to acquire.
- In-Silico Data Generation: Platforms like the UVA/Padova T1D Simulator and its Python implementation, Simglucose, can generate synthetic CGM data for virtual patient cohorts, incorporating factors like meal intake and insulin dosing [1]. This synthetic data provides a vast, annotated resource for initial model training.
- Transfer Learning Protocol: The workflow begins with pre-training a model on large-scale synthetic data. This model is then fine-tuned on a smaller, targeted dataset of real patient CGM readings. This process allows the model to learn general physiological patterns from simulation and subsequently adapt to the nuances and noise of real-world data [1].
- Experimental Validation: Research has demonstrated that models pre-trained on simulated data achieve significantly better performance when fine-tuned on real data compared to models trained on real data alone. This approach effectively bootstraps model development where real data is scarce [1].
Detailed Experimental Protocols
Protocol for Federated Learning in Medical Data
A proof-of-concept for a federated learning system suitable for regulatory agencies has been successfully deployed [74]. The methodology can be adapted for glucose prediction models as follows:
- Client and Server Setup: Establish a central coordinator server and multiple client institutions (e.g., hospitals). Each client holds its local dataset of glucose readings and related patient data, which never leaves its firewall.
- Model Distribution: The central server initializes a global glucose prediction model (e.g., an LSTM) and distributes its initial weights to all clients.
- Local Training Rounds: Each client trains the received model on its local data for a predetermined number of epochs. The training uses a consistent protocol (e.g., optimizer, loss function) across clients.
- Secure Aggregation: Clients send their updated model weights back to the server. The server aggregates these weights using an algorithm like Federated Averaging (FedAvg). To enhance security, techniques like Differential Privacy can be applied by adding calibrated noise to the updates, or Secure Multi-Party Computation can be used [74].
- Iteration: Steps 2-4 are repeated for multiple communication rounds until the global model converges to a satisfactory performance level.
Protocol for Sim2Real Transfer Learning
The use of simulated data for model development is a well-established practice [1]. A robust Sim2Real protocol for glucose forecasting involves:
Synthetic Data Pre-training:
- Data Generation: Use a simulator like Simglucose to generate CGM data for a large cohort of virtual patients (e.g., hundreds of patients over several months). The simulation should incorporate realistic meal schedules, insulin dosing, and physiological variability.
- Base Model Training: Train a chosen model architecture (e.g., LSTM, Transformer) on this synthetic dataset to predict future glucose levels. This step allows the model to learn the fundamental dynamics of glucose-insulin regulation.
Real-World Fine-Tuning:
- Data Collection: Gather a smaller, targeted dataset from real patients using CGM devices. This dataset can be limited (e.g., a few weeks of data per patient).
- Transfer Learning: Use the pre-trained model from step 1 as the starting point. Further train (fine-tune) this model on the real patient dataset. A lower learning rate is typically used during this phase to adapt the model gently to the real-world data distribution without catastrophic forgetting.
Validation: Evaluate the fine-tuned model on a held-out test set of real patient data to assess its forecasting accuracy and clinical safety (e.g., using Consensus Error Grid analysis).
The Scientist's Toolkit: Key Research Reagents and Solutions
Table 3: Essential Tools and Frameworks for Glucose Prediction Research
| Item Name | Type | Primary Function | Relevance to Data Scarcity/Privacy |
|---|---|---|---|
| UVA/Padova T1D Simulator | Software Simulator | Generates synthetic, physiologically plausible CGM and insulin data for virtual patient cohorts. | Addresses data scarcity by providing a limitless, low-cost data source for model pre-training (Sim2Real). |
| Simglucose (v0.2.1) | Python Package | A free, open-source Python implementation of the UVA/Padova Simulator for easy integration into ML pipelines. | Facilitates Sim2Real research by making in-silico data generation accessible to a wider research community [1]. |
| Federated Averaging (FedAvg) | Algorithm | The canonical algorithm for aggregating locally trained model updates in Federated Learning. | Core to privacy preservation; enables collaborative learning without raw data sharing [76] [74]. |
| Differential Privacy | Mathematical Framework | A system for publicly sharing information about a dataset by describing patterns of groups within the dataset while withholding information about individuals. | Can be integrated with FL to provide strong, mathematical privacy guarantees against certain attacks [76]. |
| PROBAST Tool | Assessment Tool | A structured tool to assess the risk of bias and applicability of prediction model studies. | Critical for evaluating the methodological quality of existing models and guiding the development of robust new ones [77]. |
| OhioT1DM Dataset | Dataset | A benchmark dataset containing real CGM, insulin, and meal data from individuals with Type 1 Diabetes. | Serves as a key real-world dataset for the fine-tuning and validation phases of Sim2Real protocols. |
Optimizing Computational Efficiency and Resource Usage for Clinical Deployment
The transition of machine learning models from research to clinical practice in glucose prediction hinges on optimizing the trade-off between predictive accuracy and computational resource consumption. For researchers and drug development professionals, selecting an appropriate model is a strategic decision that impacts not only the quality of patient care but also the feasibility and cost of deployment. This guide provides a comparative analysis of three prominent classes of models—Logistic Regression, Long Short-Term Memory (LSTM) networks, and the Auto-Regressive Integrated Moving Average (ARIMA)—framed within the critical context of computational efficiency and resource usage for clinical deployment. The evaluation synthesizes recent findings on their predictive performance, computational demands, and suitability for real-world healthcare settings.
Model Performance and Computational Profile
The following table summarizes the core performance metrics and computational characteristics of the three models based on recent comparative studies.
Table 1: Comparative Analysis of Glucose Prediction Models for Clinical Deployment
| Feature | Logistic Regression | LSTM | ARIMA |
|---|---|---|---|
| Primary Use Case | Classification of glycemic states (e.g., hypo-/hyperglycemia) [78] [5] | Regression for continuous glucose prediction [13] [5] [16] | Regression for continuous glucose and cholesterol prediction [20] [14] |
| Typical Accuracy (Glucose Prediction) | Accuracy: ~89.98% (for T2D prediction) [78] | RMSE: 20.50 ± 5.66 mg/dL (Aggregated) [13] | Superior RMSE vs. LSTM in direct comparison [20] |
| Key Strengths | Computational efficiency, high interpretability, effective for classification tasks [78] | High accuracy for complex sequences, handles multiple input features [13] [16] | High accuracy on temporal patterns, low computational cost [20] [14] |
| Computational & Resource Demands | Low; suitable for on-device deployment [78] | High; requires substantial data and processing power [14] [79] | Low; efficient with limited data and resources [20] [14] |
| Clinical Deployment Advantages | Fast inference, easy to implement and validate [78] | Potential for personalized, adaptive forecasting [13] [5] | Real-time application feasibility, easier maintenance [20] |
Detailed Experimental Protocols and Findings
ARIMA vs. LSTM for Non-Invasive Monitoring
A 2023 study directly compared ARIMA and LSTM for non-invasive glucose and cholesterol forecasting, highlighting a significant trade-off between accuracy and computational complexity [20].
- Methodology: A hardware prototype using Near Infra-Red (NIR) sensors collected patient data over one month. The collected time-series data was used to train both an ARIMA model and an LSTM model. The primary metric for comparison was Root Mean Square Error (RMSE) [20].
- Key Findings: The ARIMA model demonstrated higher prediction accuracy, with an RMSE approximately 71.7% lower for glucose and 50.3% lower for cholesterol compared to the LSTM model. This superior performance, coupled with ARIMA's inherently lower computational cost, positions it as a strong candidate for cost-effective, real-time clinical deployment where hardware resources may be limited [20].
Personalized vs. Aggregated LSTM Training
A 2025 study investigated the data efficiency of LSTM models by comparing individualized and aggregated training strategies for blood glucose prediction in Type 1 Diabetes [13].
- Methodology: Using the HUPA UCM dataset from 25 individuals, researchers developed two types of LSTM models: one set trained on individual-specific data and another trained on aggregated data from all subjects. The models used a sequence-to-sequence architecture, taking a 180-minute window of data (glucose, carbs, insulin) to predict glucose levels 60 minutes ahead. Model performance was evaluated using RMSE and Clarke Error Grid Analysis [13].
- Key Findings: Despite being trained on substantially less data, the personalized models achieved comparable accuracy (RMSE of 22.52 ± 6.38 mg/dL) to the aggregated models (RMSE of 20.50 ± 5.66 mg/dL). This finding is critical for clinical deployment as it suggests that accurate, personalized models can be developed without the massive data and computational overhead required for building large, aggregated models, potentially enabling more efficient on-device learning [13].
Deep Learning vs. Statistical Models for Diabetes Burden Forecasting
A 2025 analysis compared deep learning models (Transformer-VAE, LSTM, GRU) with the statistical ARIMA model for forecasting the global burden of diabetes, providing insights into their computational robustness [14].
- Methodology: The study used annual global health data from 1990-2021. Models were evaluated on predictive accuracy (MAE, RMSE), robustness to noisy and missing data, and computational efficiency (training time, inference speed, memory usage) [14].
- Key Findings: While the Transformer-VAE model achieved the highest predictive accuracy, it came with high computational costs and interpretability challenges. LSTM effectively captured short-term patterns but struggled with long-term dependencies. ARIMA, despite being the most resource-efficient, showed limited capability in modeling complex, long-term trends. The study concluded that hybrid models might offer the best balance, leveraging the efficiency of statistical models for linear components and the power of deep learning for non-linear patterns [14].
Logical Workflow for Model Selection and Deployment
The following diagram illustrates a decision pathway for selecting and implementing a glucose prediction model based on clinical objectives and resource constraints.
Table 2: Key Research Reagents and Computational Resources
| Resource Name | Type | Primary Function in Research |
|---|---|---|
| Continuous Glucose Monitoring (CGM) Data | Dataset | The foundational time-series input for training and validating all glucose prediction models [13] [5] [16]. |
| OhioT1DM / HUPA UCM Dataset | Benchmark Dataset | Publicly available datasets used as standard benchmarks for comparing model performance and generalizability [13] [16]. |
| Hypo-Hyper (HH) Loss Function | Algorithmic Tool | A custom loss function that penalizes prediction errors more heavily in hypoglycemic and hyperglycemic ranges, addressing data imbalance [5] [18]. |
| Federated Learning (FL) Framework | Deployment Architecture | A privacy-preserving training paradigm that allows models to be trained across decentralized devices without sharing raw patient data [5] [18]. |
| Per-Sequence Scaling (PSS) | Preprocessing Technique | A normalization method applied independently to each input sequence, helping models adapt to individual patient variability and non-stationary data [80]. |
The choice between Logistic Regression, LSTM, and ARIMA for clinical glucose prediction is not a quest for a universally superior model, but a strategic alignment of model capabilities with deployment constraints. Logistic Regression remains a highly efficient and interpretable tool for classification-based alerts. LSTM networks, particularly when personalized, offer powerful forecasting capabilities but demand significant computational resources and data. ARIMA models present a compelling balance of solid predictive performance for temporal patterns and low computational cost, making them highly suitable for resource-constrained environments. The emerging paradigms of federated learning and personalized, data-efficient training are poised to mitigate the resource limitations of deep learning, paving the way for more widespread and effective clinical deployment of advanced predictive models.
Recalibration Strategies to Combat Model Performance Drift Over Time
In the dynamic field of AI-driven healthcare forecasting, model performance drift presents a significant challenge to maintaining predictive accuracy over time. This is particularly critical in applications like glucose prediction, where model reliability directly impacts patient health outcomes. As data distributions and relationships evolve in non-stationary clinical environments, even the most accurately developed models experience calibration drift and performance degradation [81] [82]. This comparative analysis examines recalibration strategies for three prominent glucose forecasting approaches—logistic regression, Long Short-Term Memory (LSTM) networks, and AutoRegressive Integrated Moving Average (ARIMA) models—within the broader context of diabetes management research. We evaluate detection methods, recalibration techniques, and performance metrics to provide researchers and drug development professionals with evidence-based guidance for maintaining model efficacy in production environments.
Understanding Model Drift in Clinical Environments
Types and Causes of Drift
Model drift in healthcare settings manifests primarily as data drift and concept drift, both critically impacting forecasting reliability. Data drift occurs when the statistical properties of input features change over time, such as shifts in glucose level distributions due to seasonal variations, changes in patient population, or modifications to monitoring equipment [83] [84]. Concept drift represents a more fundamental challenge where the relationship between input features and target variables evolves, such as when physiological responses to glucose levels change due to factors like medication adjustments or comorbid conditions [81].
Clinical environments are inherently non-stationary, with drift resulting from multiple sources: abrupt changes following new clinical guideline implementation, gradual shifts from evolving patient demographics, and seasonal patterns affecting physiological parameters [81]. The COVID-19 pandemic highlighted how rapidly healthcare environments can change, with significant impacts on model performance due to simultaneous alterations in data collection, patient case mix, and clinical decision-making [81].
Impact on Glucose Forecasting
In glucose prediction, drift manifests as deteriorating calibration where predicted probabilities no longer correspond to actual event rates. For example, a model might consistently overestimate or underestimate hypoglycemia risk, leading to clinically dangerous false assurances or unnecessary alerts [82] [1]. This calibration drift is particularly problematic for logistic regression and LSTM models used in classification tasks, where probability thresholds directly influence clinical decisions.
Drift Detection Methodologies
Effective recalibration begins with robust drift detection. Multiple statistical and algorithmic approaches have been developed for identifying performance degradation in clinical prediction models.
Statistical Process Monitoring
Statistical process control methods, particularly cumulative sum (CUSUM) charts, provide effective frameworks for monitoring calibration drift. The calibration CUSUM approach monitors probability predictions over time, signaling when predictions become significantly miscalibrated [82]. This method operates on probability predictions and event outcomes without requiring access to the underlying model architecture, making it applicable across different model types [82].
The Page-Hinkley test, another popular drift detection method, is particularly effective for detecting abrupt changes in the mean value of model performance metrics [84]. This sequential analysis technique uses the cumulative sum of differences between observed values and their expected mean to identify significant deviations indicative of drift.
Adaptive Windowing Approaches
The Adaptive Windowing (ADWIN) algorithm dynamically adjusts sliding window sizes based on detected rates of change in data streams [84]. This approach maintains a window of recent data points and compares statistical properties between historical and current data, triggering alerts when differences exceed predefined thresholds. Adaptive sliding windows are particularly valuable for clinical applications where drift may be gradual or occur at varying rates [81].
Dynamic Calibration Curves
For ongoing calibration assessment, dynamic calibration curves maintain evolving logistic calibration curves using online stochastic gradient descent with Adam optimization [81]. This approach processes observations in temporal order, incrementally adjusting coefficients toward values that minimize the logistic loss function based on recent data. The method responds to calibration changes by stepping coefficient estimates toward newly optimal values reflecting current relationships between predictions and observed outcomes [81].
Table 1: Comparison of Drift Detection Methods for Glucose Forecasting Models
| Detection Method | Underlying Principle | Streak Detection | Implementation Complexity | Suitable Model Types |
|---|---|---|---|---|
| CUSUM Charts | Cumulative sum of prediction errors | Abrupt and gradual drift | Moderate | All model types |
| Page-Hinkley Test | Sequential analysis of mean values | Abrupt changes | Low | All model types |
| ADWIN Algorithm | Adaptive window comparison | Gradual and abrupt drift | High | Streaming data models |
| Dynamic Calibration Curves | Online gradient descent | Continuous calibration drift | High | Probability-based models |
| Population Stability Index | Distribution comparison | Feature distribution shifts | Low | All model types |
Comparative Model Analysis in Glucose Forecasting
Performance Metrics Across Prediction Horizons
Different glucose forecasting models exhibit distinct strengths and weaknesses across prediction horizons and glucose level classes. Research comparing ARIMA, logistic regression, and LSTM models for hypoglycemia, euglycemia, and hyperglycemia classification demonstrates significant variation in performance [1].
For 15-minute prediction horizons, logistic regression outperforms both ARIMA and LSTM models across all glycemia classes, achieving recall rates of 96% for hyperglycemia, 91% for euglycemia, and 98% for hypoglycemia [1]. This superior performance for short-term predictions highlights logistic regression's effectiveness in capturing immediate patterns in glucose fluctuations.
For extended 1-hour prediction horizons, LSTM models demonstrate superior capability, achieving recall values of 85% for hyperglycemia and 87% for hypoglycemia, outperforming both logistic regression and ARIMA models [1]. This advantage in longer-term forecasting stems from LSTM's ability to capture complex temporal dependencies in glucose time series data.
ARIMA models consistently underperform for both prediction horizons, particularly in detecting extreme glucose levels, highlighting limitations in handling the complex, nonlinear patterns characteristic of physiological glucose dynamics [1].
Table 2: Glucose Prediction Performance Across Models and Time Horizons
| Model Type | 15-min Hypoglycemia Recall | 15-min Hyperglycemia Recall | 1-hr Hypoglycemia Recall | 1-hr Hyperglycemia Recall | Computational Demand |
|---|---|---|---|---|---|
| Logistic Regression | 98% | 96% | <85% | <85% | Low |
| LSTM | <98% | <96% | 87% | 85% | High |
| ARIMA | Lowest performance | Lowest performance | Lowest performance | Lowest performance | Moderate |
Robustness to Data Quality Issues
Real-world clinical data often contains noise, missing values, and measurement artifacts, requiring robust model performance under suboptimal conditions. Studies evaluating diabetes burden forecasting demonstrate that hybrid approaches like Transformer with Variational Autoencoder (VAE) provide superior resilience to noisy and incomplete data (p < 0.01) compared to individual models [14].
LSTM models effectively capture short-term patterns but struggle with long-term dependencies in noisy environments, while GRU models, though computationally efficient, exhibit higher error rates with data quality issues [14]. ARIMA models, despite resource efficiency, show limited capability in modeling long-term trends when data quality is compromised [14].
Recalibration Strategies and Implementation
Model-Specific Recalibration Approaches
Logistic Regression Recalibration
For logistic regression models, regular recalibration using recent patient data is essential. Temperature scaling represents a straightforward post-hoc calibration method that scales model outputs by a single parameter to better align predicted probabilities with actual outcomes [85]. Platt scaling, which fits a logistic regression model to the classifier scores, provides another effective approach for probability calibration [85].
Dynamic logistic regression models can be maintained through online learning approaches that incrementally update model parameters as new data arrives. This continuous adaptation helps maintain calibration without requiring complete model retraining [81].
LSTM Recalibration
Recalibrating LSTM models presents greater computational challenges but can be achieved through several approaches. Fine-tuning on recent data allows the model to adapt to new patterns while retaining previously learned representations [14]. Transfer learning approaches, where models pre-trained on large datasets are adapted to specific patient populations or time periods, have demonstrated effectiveness in maintaining glucose prediction accuracy [1].
For complex LSTM architectures, calibration methods like weight-averaged sharpness-aware minimization (WASAM) have shown positive impacts on model failure prediction performance, enhancing robustness to data drift in quality monitoring applications [85].
ARIMA Model Updating
ARIMA models require regular parameter re-estimation as underlying time series characteristics evolve. Automated model selection procedures that periodically reassess optimal ARIMA parameters (p, d, q) based on recent data help maintain forecasting accuracy [20]. While ARIMA models demonstrate computational efficiency, their limited ability to capture complex physiological patterns restricts their effectiveness in clinical glucose forecasting applications [1].
Structured Recalibration Workflow
A systematic approach to model recalibration ensures consistent performance maintenance across all model types. The following workflow visualizes the comprehensive recalibration process:
Diagram 1: Comprehensive Model Recalibration Workflow. This workflow outlines the systematic process for detecting and addressing model performance drift, from initial monitoring through deployment of recalibrated models.
Decision Framework for Recalibration Response
When drift is detected, researchers must select appropriate responses based on drift characteristics and clinical requirements:
Diagram 2: Recalibration Response Decision Framework. This decision tree guides researchers in selecting appropriate recalibration strategies based on data quality, label availability, and clinical impact of detected drift.
Experimental Protocols and Research Toolkit
Standardized Evaluation Framework
Research comparing glucose forecasting models should implement standardized evaluation protocols to ensure comparable results across studies. The following experimental framework provides a foundation for rigorous model assessment:
Data Partitioning: Segment temporal data into training (60-70%), validation (15-20%), and testing (15-20%) sets while maintaining chronological order to prevent data leakage [1].
Performance Metrics: Employ comprehensive evaluation metrics including precision, recall, F1-score, accuracy, and area under the ROC curve for classification tasks, plus Mean Absolute Error (MAE) and Root Mean Squared Error (RMSE) for continuous predictions [14] [1].
Drift Simulation: Introduce realistic drift scenarios through evaluation periods, with robustness tests incorporating noise and missing data to simulate real-world conditions [14].
Statistical Significance Testing: Implement appropriate statistical analyses such as ANOVA and Tukey's post-hoc tests to validate performance differences between models and recalibration strategies [14].
Research Reagent Solutions
Table 3: Essential Research Toolkit for Glucose Forecasting Experiments
| Research Component | Function | Implementation Examples |
|---|---|---|
| Continuous Glucose Monitoring Data | Primary input for model training and validation | Real patient CGM data, CGM Simulator (Simglucose v0.2.1) [1] |
| Drift Detection Algorithms | Identify performance degradation | CUSUM, Page-Hinkley Test, ADWIN Algorithm [84] [82] |
| Calibration Tools | Maintain probability calibration | Temperature Scaling, Platt Scaling, Dynamic Calibration Curves [81] [85] |
| Performance Monitoring | Track model metrics over time | Evidently AI, Alibi Detect, WhyLabs, Custom Python pipelines [83] |
| Statistical Analysis | Validate significance of results | ANOVA, Tukey's post-hoc tests, correlation analysis [14] |
Recalibration strategies are essential for maintaining glucose prediction model accuracy in dynamic clinical environments. Our comparative analysis demonstrates that optimal recalibration approaches depend on model architecture, with logistic regression benefiting from regular probability calibration for short-term predictions, LSTM models requiring fine-tuning and architectural adjustments for longer horizons, and ARIMA models needing periodic parameter re-estimation despite inherent limitations in capturing complex physiological patterns.
The most effective recalibration strategies implement continuous monitoring using statistical process control methods, trigger appropriate responses based on drift characteristics and clinical impact, and maintain comprehensive documentation of drift events and intervention outcomes. Future research directions should explore hybrid modeling approaches that combine the computational efficiency of simpler models with the adaptive capacity of complex architectures, potentially leveraging ensemble methods that dynamically weight constituent models based on recent performance.
For researchers and drug development professionals, establishing systematic recalibration protocols represents a critical component of model governance, ensuring that glucose forecasting systems maintain reliability throughout their deployment lifecycle. As continuous glucose monitoring technologies evolve and datasets expand, proactive recalibration strategies will become increasingly vital for translating predictive analytics into improved patient outcomes.
Rigorous Model Validation: A Comparative Performance Analysis
The accurate prediction of glucose levels is a cornerstone of modern diabetes management, enabling proactive interventions that can prevent both acute emergencies and long-term complications. Within the field of predictive analytics, three distinct modeling approaches have garnered significant attention: the classical statistical AutoRegressive Integrated Moving Average (ARIMA) model, the interpretable machine learning technique of Logistic Regression, and the deep learning-based Long Short-Term Memory (LSTM) network. Each model brings a unique set of strengths and assumptions to the forecasting task. This review provides a head-to-head comparison of these methodologies, synthesizing quantitative performance data from recent rigorous studies. The analysis is structured to offer researchers, scientists, and drug development professionals a clear, data-driven understanding of their comparative accuracy, supported by detailed experimental protocols and key metrics, to inform both research direction and clinical application development.
The following table synthesizes key quantitative findings from recent comparative studies, highlighting the performance of ARIMA, Logistic Regression, and LSTM models across different prediction tasks.
Table 1: Comparative Model Performance Across Key Studies
| Study Context | Primary Metric | ARIMA Performance | Logistic Regression Performance | LSTM Performance | Reported Statistical Significance |
|---|---|---|---|---|---|
| Non-Invasive Glucose & Cholesterol Forecasting [20] | Root Mean Square Error (RMSE) | Lower RMSE (≈71.7% less for Glucose, 50.3% less for Cholesterol vs. LSTM) | Not Tested | Higher RMSE than ARIMA | Not explicitly reported |
| 15-Minute Glucose Level Classification [1] | Recall (Sensitivity) | Underperformed other models | Hyperglycemia: 96%Euglycemia: 91%Hypoglycemia: 98% | Lower than Logistic Regression | Not explicitly reported |
| 1-Hour Glucose Level Classification [1] | Recall (Sensitivity) | Underperformed other models | Lower than LSTM | Hyperglycemia: 85%Hypoglycemia: 87% | Not explicitly reported |
| Blood Glucose Prediction (Type 1 Diabetes) [13] | Root Mean Square Error (RMSE) | Not Tested | Not Tested | 20.50 ± 5.66 mg/dL (Aggregated Training)22.52 ± 6.38 mg/dL (Individual Training) | Modest differences between training approaches |
| Diabetes Burden Forecasting (DALYs) [14] | Mean Absolute Error (MAE) | Higher error than deep learning models | Not Tested | Effectively captured short-term patterns but struggled with long-term dependencies | Transformer-VAE significantly outperformed others (p < 0.01) |
Detailed Experimental Protocols and Findings
Non-Invasive Monitoring: ARIMA vs. LSTM
A 2023 study directly compared ARIMA and LSTM for forecasting glucose and cholesterol levels using data from a non-invasive hardware prototype employing Near Infra-Red (NIR) sensors [20].
- Objective: To develop a cost-effective, non-invasive, and real-time monitoring system for glucose and cholesterol.
- Data Source: Patient data collected over one month using an NIR sensor-based prototype [20].
- Methodology: The collected longitudinal data was used to train and compare univariate ARIMA and LSTM forecasting models. The models were evaluated based on their Root Mean Square Error (RMSE) [20].
- Key Findings: The study concluded that the ARIMA model surpassed the LSTM model, demonstrating approximately 71.7% lower RMSE for glucose and 50.3% lower RMSE for cholesterol predictions. This indicates that for this specific univariate forecasting task with a non-invasive sensor source, the classical time-series model was significantly more accurate [20].
Short-Term vs. Medium-Term Classification: ARIMA vs. Logistic Regression vs. LSTM
A 2023 investigation provided a critical comparison for classifying glucose levels into hypoglycemia, euglycemia, and hyperglycemia, highlighting how model superiority is dependent on the prediction horizon [1].
- Objective: To evaluate the efficacy of ARIMA, Logistic Regression, and LSTM in predicting glucose level classes 15 minutes and 1 hour ahead [1].
- Data Source: A combination of real patient data from a cohort study and in-silico data generated using the CGM Simulator (Simglucose v0.2.1) [1].
- Methodology: The study employed a multi-model comparison framework. Feature engineering was a core component, deriving inputs such as rolling averages, standard deviations, and rate-of-change metrics from the raw CGM time series data. Model performance was assessed using precision, recall, and accuracy [1].
- Key Findings:
- 15-Minute Horizon: Logistic Regression was the top-performing model, achieving high recall rates for all glycemia classes, most notably 98% for hypoglycemia [1].
- 1-Hour Horizon: The LSTM model demonstrated superior performance for predicting hyperglycemia (85% recall) and hypoglycemia (87% recall), outperforming Logistic Regression for this longer prediction window [1].
- ARIMA Performance: The ARIMA model underperformed compared to the other two models at both forecasting horizons [1].
The workflow for this experimental approach is summarized below.
Data Efficiency in Personalized Glucose Forecasting
While not a direct head-to-head comparison with ARIMA or Logistic Regression, a 2025 study on LSTM models provides critical insight into training strategies that impact predictive performance [13].
- Objective: To compare the data efficiency and accuracy of LSTM models trained on aggregated population data versus individual-specific data [13].
- Data Source: The HUPA UCM diabetes dataset, containing CGM values, insulin delivery, and carbohydrate intake from 25 individuals with Type 1 Diabetes [13].
- Methodology: Two training strategies were implemented: (1) Aggregated, where a single model was trained on data from all subjects, and (2) Individualized, where 25 separate models were trained, each on a single subject's data. The models predicted a 60-minute blood glucose trajectory using a 180-minute history of data (blood glucose, carbohydrate intake, basal and bolus insulin) [13].
- Key Findings: The individualized models, despite being trained on substantially less data, achieved comparable accuracy to the aggregated models. The mean RMSE was 22.52 ± 6.38 mg/dL for individualized models versus 20.50 ± 5.66 mg/dL for aggregated models. This suggests that personalized LSTM models are a data-efficient and accurate approach for clinical deployment [13].
The Scientist's Toolkit: Essential Research Reagents
The following table details key datasets and computational tools referenced in the featured studies that are essential for replicating and advancing research in this field.
Table 2: Key Research Resources for Glucose Prediction Studies
| Resource Name | Type | Primary Function / Utility | Relevant Citation |
|---|---|---|---|
| OhioT1DM Dataset | Clinical Dataset | A public dataset containing CGM, insulin, carbohydrate, and activity data from individuals with type 1 diabetes; used for benchmarking prediction models. | [1] [15] |
| HUPA UCM Dataset | Clinical Dataset | A dataset comprising CGM, insulin delivery, and carbohydrate intake from 25 T1D individuals under free-living conditions. | [13] |
| Simglucose (v0.2.1) | Software Simulator | An open-source Python implementation of the FDA-approved UVA/Padova T1D Simulator; generates in-silico patient data for algorithm testing. | [1] |
| CGM Simulator | Software Simulator | A system designed for in-silico testing of control algorithms, incorporating a cohort of virtual patients and models of CGM sensor errors. | [1] |
| Global Burden of Disease (GBD) Data | Epidemiological Dataset | Provides annual time-series data on diabetes prevalence, DALYs, and deaths; used for macro-level forecasting of disease burden. | [14] |
The head-to-head evidence clearly demonstrates that there is no single "best" model for all glucose prediction contexts. The optimal choice is dictated by a triad of factors: the prediction horizon, the specific clinical task (classification vs. regression), and the available data.
- ARIMA models can be highly effective for univariate, short-term forecasting tasks, as evidenced by their strong performance against LSTM in non-invasive monitoring [20]. Their relative simplicity and low computational cost are advantageous.
- Logistic Regression excels as a lightweight, highly interpretable champion for very short-term classification (e.g., 15-minute horizon), particularly for critical tasks like hypoglycemia prediction where its high recall is vital [1].
- LSTM networks show their strength in capturing complex, longer-term temporal dependencies, making them superior for 1-hour ahead glycemic state classification [1] and personalized forecasting, even with limited individual data [13].
Future research directions likely involve hybrid models that leverage the respective strengths of these approaches, ensemble methods, and a continued focus on robust, clinically-relevant evaluation metrics beyond pure accuracy, such as time in range and clinical outcome improvements.
The accuracy of predictive models in healthcare is not absolute but is intrinsically tied to the forecasting horizon. This comparative guide examines the performance of three modeling approaches—Logistic Regression, Long Short-Term Memory networks (LSTM), and the Auto-Regressive Integrated Moving Average (ARIMA)—in predicting glucose levels at 15-minute and 60-minute horizons. The ability to forecast dysglycemic events (hypoglycemia and hyperglycemia) is crucial for developing automated insulin delivery systems and improving diabetes management. Understanding how model efficacy shifts with prediction horizon empowers researchers and drug development professionals to select the optimal tool for their specific application, whether for real-time alert systems or long-term physiological trend analysis.
Model Performance Comparison
The performance of the three models was evaluated using standard classification metrics, including precision, recall, and accuracy, for predicting glucose level classes: hypoglycemia (<70 mg/dL), euglycemia (70–180 mg/dL), and hyperglycemia (>180 mg/dL) [1].
Table 1: Model Performance Metrics for 15-Minute Prediction Horizon
| Glucose Class | Model | Precision | Recall | Accuracy |
|---|---|---|---|---|
| Hyperglycemia | Logistic Regression | - | 96% | - |
| LSTM | - | - | - | |
| ARIMA | - | - | - | |
| Euglycemia | Logistic Regression | - | 91% | - |
| LSTM | - | - | - | |
| ARIMA | - | - | - | |
| Hypoglycemia | Logistic Regression | - | 98% | - |
| LSTM | - | - | - | |
| ARIMA | - | - | - |
Table 2: Model Performance Metrics for 60-Minute Prediction Horizon
| Glucose Class | Model | Precision | Recall | Accuracy |
|---|---|---|---|---|
| Hyperglycemia | LSTM | - | 85% | - |
| Logistic Regression | - | - | - | |
| ARIMA | - | - | - | |
| Hypoglycemia | LSTM | - | 87% | - |
| Logistic Regression | - | - | - | |
| ARIMA | - | - | - |
Summary of Key Findings: [1]
- At the 15-minute horizon, Logistic Regression demonstrated superior performance for all glycemia classes, achieving high recall rates (96% for hyperglycemia, 91% for euglycemia, and 98% for hypoglycemia).
- At the 60-minute horizon, the LSTM model outperformed others for the critical classes of hyperglycemia (85% recall) and hypoglycemia (87% recall).
- Across both timeframes, the ARIMA model consistently underperformed compared to Logistic Regression and LSTM in predicting hyperglycemia and hypoglycemia.
Detailed Experimental Protocols
Data Sourcing and Preprocessing
The study utilized data from two primary sources to ensure robustness and generalizability [1]:
- Clinical Cohort Data: Real-world data was acquired from a cohort study involving 11 participants with type 1 diabetes (T1D). Participants used a continuous glucose monitor (CGM), and data on insulin dosing and carbohydrate intake were collected.
- In Silico Data: To supplement the real-patient data, the study employed the CGM Simulator (Simglucose v0.2.1), a freely available Python implementation of the UVA/Padova T1D Simulator. This generated data for 30 virtual patients (across adults, adolescents, and children) over 10 days, incorporating meal and snack consumption.
Preprocessing: The raw data from real patients was cleaned to handle gaps and bad entries, then resampled to a consistent 15-minute frequency. The in silico data, generated at 1-minute intervals, was also resampled to 15-minute frequency for uniformity [1].
Feature Engineering
Given the critical role of feature selection in predictive modeling, a set of features was engineered from the original CGM time series. These provided the models with nuanced information on glucose dynamics, which is particularly vital when other physiological data points are unavailable [1]. The engineered features included:
- Rate of Change Metrics: Capturing the velocity and acceleration of glucose fluctuations.
- Variability Indices: Quantifying the stability or volatility of glucose levels over short periods.
- Time-based Features: Including moving averages and seasonal decompositions to identify underlying trends and patterns.
Model Training and Evaluation Framework
The performance of the three models was evaluated using a structured approach [1]:
- Forecasting Task: The models were tasked with predicting glucose level classes (hypoglycemia, euglycemia, hyperglycemia) at two distinct horizons: 15 minutes and 1 hour into the future.
- Performance Metrics: The models were evaluated based on confusion matrices, from which metrics such as precision, recall, and accuracy were computed. These metrics provide a comprehensive view of a model's performance, balancing the cost of false positives and false negatives—a critical consideration in clinical applications.
- Final Evaluation: The forecasting results and performance metrics reported in this guide are based on the real patient data only, ensuring relevance to real-world conditions [1].
Workflow and Conceptual Diagrams
Figure 1: Experimental Workflow for Glucose Prediction Modeling
Figure 2: Model Selection Logic Based on Prediction Horizon
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Glucose Prediction Research
| Item Name | Function / Application in Research |
|---|---|
| Continuous Glucose Monitor (CGM) | Provides the core time-series data on interstitial glucose levels for model training and validation. Real-world clinical data is essential for final evaluation [1]. |
| In Silico Simulator (e.g., Simglucose) | Allows for generating large-scale, synthetic CGM data for preliminary model testing and development, reducing initial reliance on hard-to-acquire clinical data [1]. |
| Near Infra-Red (NIR) Sensors | Enables non-invasive measurement of glucose and cholesterol levels for research focused on developing non-invasive monitoring hardware [20]. |
| Cloud Computing Platform | Provides the computational power necessary for training complex models, especially data-intensive neural networks like LSTM, and for storing large datasets [20]. |
| Logistic Regression Algorithm | Serves as a powerful and interpretable baseline model, particularly for short-term classification tasks. Its strong performance at 15-minute horizons makes it a essential benchmark [1]. |
| LSTM Framework | A critical tool for capturing long-term dependencies in temporal data. Its superior performance at the 60-minute horizon makes it indispensable for longer-term forecasting [1]. |
The experimental data clearly demonstrates a fundamental principle in time series forecasting: the optimal model is contingent on the prediction horizon. Logistic Regression, a relatively simple and interpretable model, dominates for short-term (15-minute) predictions. This suggests that immediate future glucose levels are highly determined by a linear combination of very recent trends and engineered features [1]. In contrast, the LSTM's superior performance at the 60-minute horizon underscores the value of complex, non-linear models capable of learning long-range dependencies in temporal data as predictions extend further into the future [1].
This horizon-dependent performance has direct implications for the design of clinical decision support systems. A hybrid approach, where a Logistic Regression model powers real-time alerts and an LSTM model informs longer-term strategic interventions (e.g., lifestyle adjustments or insulin regimen changes), could be optimal. Furthermore, the consistent underperformance of the ARIMA model in classifying extreme glucose events highlights its limitations in this specific biomedical forecasting context compared to more modern machine learning techniques [1].
In conclusion, researchers and clinicians must align their choice of predictive model with the intended clinical application and its required forecasting horizon. The findings solidify the nuanced understanding that in glucose prediction, there is no universal "best model," but rather a "best model for the timeframe," a principle that likely extends to other complex physiological forecasting tasks.
The selection of optimal predictive models is a fundamental challenge in data-driven scientific research. Within the specific domain of physiological time series forecasting, researchers often weigh the relative merits of traditional statistical methods, such as the Autoregressive Integrated Moving Average (ARIMA), against more complex machine learning approaches, including logistic regression and Long Short-Term Memory (LSTM) networks. Conventional wisdom frequently favors newer, more complex models, assuming they offer superior predictive accuracy. However, a growing body of empirical evidence reveals that this is not universally true. Recent findings from a non-invasive monitoring study on honey bee colonies have reported a surprising edge for ARIMA, demonstrating a lower Root Mean Squared Error (RMSE) compared to other models for specific data types [86].
This discovery is particularly significant when framed within the broader research landscape of glucose prediction, where the performance battle between logistic regression, LSTM, and ARIMA is actively being waged. Numerous studies in this field have shown that model performance is highly context-dependent, varying with the prediction horizon, data characteristics, and the specific physiological metric being forecasted [1] [2] [19]. This guide provides an objective comparison of these models, presenting supporting experimental data to help researchers and drug development professionals make informed methodological choices.
Performance Comparison in Key Studies
The following table synthesizes key findings from recent studies, highlighting the conditions under which each model excels or underperforms.
Table 1: Comparative Model Performance Across Different Forecasting Tasks
| Study Context | Target Variable | Model | Performance Highlights | Key Conditions |
|---|---|---|---|---|
| Non-Invasive Bee Hive Monitoring [86] | Hive Weight & In-Hive Temperature | SARIMA | Lower RMSE vs. non-seasonal ARIMA; Higher forecast accuracy for hive weight than temperature. | Seasonal data; 5-minute interval data; Forecast horizon of several hundred hours. |
| ARIMA | Outperformed by SARIMA, establishing the importance of seasonality. | |||
| Glucose Level Classification [1] [2] | Hypo-/Hyperglycemia (15-min horizon) | Logistic Regression | Recall: Hypo=98%, Hyper=96%; Outperformed ARIMA and LSTM. | 15-minute prediction horizon; Classification task. |
| Hypo-/Hyperglycemia (1-hour horizon) | LSTM | Recall: Hypo=87%, Hyper=85%; Exceeded logistic regression for longer horizon. | 1-hour prediction horizon; Classification task. | |
| Hypo-/Hyperglycemia | ARIMA | Underperformed other models, particularly for 1-hour hypoglycemia prediction. | Both 15-minute and 1-hour horizons. | |
| 30-Minute Glucose Forecasting [15] | Blood Glucose Level | Ridge Regression | Reduced RMSE and MAE vs. ARIMA; >96% predictions in Clarke Error Grid Zone A. | 30-minute forecast horizon; OhioT1DM dataset; Used engineered features (lags, rate-of-change). |
| ARIMA | Was outperformed by the ridge regression model. | Univariate time series approach. | ||
| Diabetes Burden Forecasting [14] | DALYs, Deaths, Prevalence | ARIMA | Resource-efficient but limited capability in modeling long-term trends. | Annual data (1990-2021); Suited for simpler, linear trends. |
The Surprising Edge of ARIMA/SARIMA
Contrary to its performance in glucose studies, ARIMA demonstrated notable strength in a non-invasive monitoring study. Research on managed honey bee colonies found that Seasonal ARIMA (SARIMA) forecasters outperformed their ARIMA counterparts on a curated dataset of hive weight and in-hive temperature, with the hive weight forecasts being consistently more accurate [86]. This highlights that for seasonal, continuous physical sensor data sampled at high frequencies (e.g., every five minutes), a well-specified SARIMA model can be exceptionally robust, achieving a lower RMSE over long forecast horizons of several hundred hours [86].
Detailed Experimental Protocols
Non-Invasive Hive Monitoring Study
The study that revealed ARIMA's surprising edge employed a rigorous, systematic methodology for forecasting hive weight and in-hive temperature [86].
- Data Collection: Ten managed honey bee colonies were monitored using electronic scales and temperature sensors from June to October 2022. Data was recorded every five minutes, resulting in 2160 timestamped observations each for weight and temperature [86].
- Data Curation and Analysis: The collected time series data was rigorously tested for properties like stationarity, trend, and seasonality using the Ljung–Box White Noise test, Augmented Dickey–Fuller test, and Shapiro–Wilk Normality test [86].
- Modeling and Evaluation: Researchers performed a systematic grid search of 1538 ARIMA and SARIMA models (769 for each data type) to identify the best forecaster for each hive and data type. Model performance was evaluated based on forecast accuracy over a long horizon, leading to the conclusion that the best forecasters were often colony-specific and that seasonality matters [86].
Figure 1: Experimental Workflow for Non-Invasive Hive Monitoring Study
Glucose Prediction Studies
Multiple studies have directly compared ARIMA, logistic regression, and LSTM for predicting glucose levels, with performance heavily dependent on the forecast horizon.
- Data Sources: Studies typically use real patient CGM data (e.g., from the OhioT1DM or T1DiabetesGranada datasets) and/or in-silico data generated by simulators like Simglucose (based on the UVA/Padova T1D Simulator) [1] [87] [19].
- Data Preprocessing: Raw CGM data is resampled to a strict frequency (e.g., 5 or 15 minutes). Gaps are handled via interpolation, and data is split chronologically into training and test sets to prevent information leakage [1] [15].
- Feature Engineering (for Logistic Regression/LSTM): A critical step for these models involves creating input features from the raw CGM time series. This includes:
- Model Training and Evaluation:
- ARIMA is typically implemented as a univariate model, with its parameters (p, d, q) selected via grid search guided by the Akaike Information Criterion (AIC) [15].
- Logistic Regression and LSTM models are trained using the engineered features. The LSTM's architecture is designed to capture long-term dependencies in the sequential data [1] [2].
- Models are evaluated using a rolling-origin validation framework to simulate real-world deployment, where the model is repeatedly trained on past data and used to forecast future values [15]. Performance is assessed using metrics like RMSE, MAE, Recall, Precision, and the Clarke Error Grid for clinical relevance [1] [15] [2].
Figure 2: Comparative Workflow for Glucose Prediction Models
Table 2: Essential Materials and Datasets for Time Series Forecasting in Monitoring Studies
| Item Name | Type | Function & Application | Representative Use Case |
|---|---|---|---|
| Electronic Hive Scales & Temperature Sensors [86] | Physical Sensor | Collects continuous, high-frequency weight and temperature data for non-invasive biological monitoring. | Forecasting hive health and phenology in honey bee colonies [86]. |
| Continuous Glucose Monitor (CGM) [1] [87] | Medical Device | Measures interstitial glucose levels at regular intervals (e.g., every 5-15 mins), providing the primary data source for glucose forecasting. | Developing predictive models for hypoglycemia and hyperglycemia in diabetes management [1] [2]. |
| OhioT1DM Dataset [15] [5] | Public Dataset | A benchmark dataset containing CGM, insulin, and carbohydrate data for individuals with type 1 diabetes. Used for training and validating predictive models. | Comparing the performance of ARIMA and ridge regression for 30-minute glucose forecasting [15]. |
| T1DiabetesGranada Dataset [87] | Public Dataset | A detailed, longitudinal dataset with CGM data from 736 patients, useful for fine-grained analysis of glucose trends. | Classifying glycemic events and predicting blood glucose levels [87]. |
| Simglucose (UVA/Padova Simulator) [1] [19] | Software Simulator | An open-source Python implementation of a validated simulator that generates in-silico CGM and patient data for algorithm testing. | Investigating model efficacy and generating synthetic data for initial validation [1] [19]. |
| Clarke Error Grid Analysis (EGA) [15] | Evaluation Tool | A plot that compares predicted vs. reference glucose values to assess clinical accuracy, categorizing predictions into risk zones (A-E). | Clinically validating the accuracy of a 30-minute ahead glucose forecast [15]. |
The body of evidence confirms that there is no single "best" model for every forecasting task in scientific monitoring. ARIMA, and particularly its seasonal variant SARIMA, can deliver superior performance with a lower RMSE in specific contexts, such as forecasting highly seasonal, continuous physical sensor data over long horizons, as demonstrated in the non-invasive hive monitoring study [86].
However, in the context of glucose prediction, the dominance shifts with the prediction horizon. Logistic regression with well-engineered features proves highly effective for very short-term classification (e.g., 15 minutes), while LSTM networks generally excel at longer-term forecasts (e.g., 1 hour) [1] [2] [19]. ARIMA, by comparison, often underperforms in these specific biomedical applications [1] [15] [2].
For researchers, the key takeaway is that model selection must be driven by the specific nature of the data and the research question. A thorough exploratory data analysis to understand trends and seasonality, coupled with a structured comparison of multiple models using robust validation frameworks, is essential for identifying the most accurate and reliable predictive tool.
LSTM's Superiority in Longer-Horizon and Complex Pattern Recognition
Accurate forecasting is a cornerstone of modern data science, particularly in critical fields like diabetes management, where predicting blood glucose levels can directly impact patient health and treatment strategies. Within this context, three distinct modeling paradigms—Long Short-Term Memory (LSTM) networks, logistic regression, and the Autoregressive Integrated Moving Average (ARIMA)—offer contrasting approaches for time-series prediction. Logistic regression provides a simple, interpretable model for classification tasks. ARIMA, a classical statistical method, excels at capturing short-term linear trends and stationarity in time-series data. In contrast, LSTM networks, a type of recurrent neural network (RNN), are specifically engineered to learn long-range, complex temporal dependencies in sequential data. This guide provides an objective, data-driven comparison of these models, with a specific focus on their performance in glucose prediction accuracy across different forecasting horizons, highlighting the scenarios where LSTM's architectural advantages translate into superior predictive performance.
Performance Comparison: Quantitative Results
The following tables synthesize key experimental findings from comparative studies, highlighting model performance across different prediction horizons and contexts.
Table 1: Comparative Performance in Glucose Level Classification (15-Minute vs. 1-Hour Horizon) [1]
| Model / Metric | 15-Minute Horizon (Recall %) | 1-Hour Horizon (Recall %) |
|---|---|---|
| Logistic Regression | Hyper: 96%, Norm: 91%, Hypo: 98% | Not the top performer |
| LSTM | Underperformed Logistic Regression | Hyper: 85%, Hypo: 87% |
| ARIMA | Underperformed other models for all classes | Underperformed other models |
Table 2: Model Performance in Broader Time-Series Tasks
| Model / Metric | Fall Detection (F1-Score %) | Human Activity Recognition (Accuracy %) | Computational Complexity |
|---|---|---|---|
| LSTM | 86.7% (Offline, with CNN) [88] | 99% [89] | (O(L)) Time, (O(L)) Memory [90] |
| Transformer | 82.6% (Offline), Better Real-Time Recall [88] | 96% (YOLO-LSTM fusion) [91] | (O(L^2)) or (O(L \log L)) [90] |
Experimental Protocols and Methodologies
Glucose Prediction Study
A 2023 study directly compared ARIMA, logistic regression, and LSTM for classifying glucose states using data from both real patients and a simulator [1].
- Data Collection: The study utilized two data sources: data from 11 individuals with type 1 diabetes collected as part of a COVID-19 vaccination response study, and in-silico data generated for 10 virtual patients in three age groups using the Simglucose (UVA/Padova T1D Simulator) platform. The dataset included timestamped CGM measurements, insulin dosage, and carbohydrate intake [1].
- Data Preprocessing: Raw data was pre-processed to a consistent 15-minute frequency, addressing gaps and bad entries. For the forecasting task, feature engineering was critical. Even when only glucose data was available, features like the rate of change, variability indices, and moving averages were derived from the raw CGM time series to provide the models with dynamic trend information [1].
- Model Training & Evaluation: The models were tasked with predicting glucose classification into hypoglycemia (<70 mg/dL), euglycemia (70-180 mg/dL), and hyperglycemia (>180 mg/dL) at 15-minute and 1-hour horizons. Performance was evaluated using standard metrics, including precision, recall, and accuracy, derived from confusion matrices [1].
Personalized vs. Aggregated LSTM Training
A 2025 study investigated the data efficiency of LSTM models by comparing personalized and aggregated training strategies [13].
- Data Source: The HUPA UCM diabetes dataset, containing data from 25 individuals with type 1 diabetes under free-living conditions, was used. It includes CGM values, insulin delivery (basal and bolus), and carbohydrate intake recorded at 5-minute intervals [13].
- Model Development: The LSTM architecture was designed for a sequence-to-sequence prediction. The model took a 180-minute window of historical data (36 time steps with 4 features: blood glucose, carbohydrate intake, basal and bolus insulin) as input and predicted blood glucose levels for the next 60 minutes (12 time steps). The architecture consisted of a single LSTM layer with 50 hidden units, followed by two fully connected layers. It was trained using the Adam optimizer and a mean squared error loss function [13].
- Training Strategies: The study compared two approaches:
- Individualized Training: 25 separate LSTM models were trained, each using only one subject's data.
- Aggregated Training: A single LSTM model was trained on a dataset created by combining the training data from all 25 subjects [13].
Analysis of LSTM's Architectural Advantages
LSTM's superior performance in longer-horizon forecasting stems from its core architectural components, which are designed to overcome the fundamental limitations of traditional models.
The diagram above illustrates how LSTM addresses key challenges in time-series forecasting. The gating mechanism and internal cell state work in concert to regulate the flow of information. The forget gate can discard irrelevant historical information, while the input gate decides what new information is important to store. This allows the LSTM to maintain a stable, long-term memory (the cell state) that is resilient to the vanishing gradient problem, enabling it to learn and remember relevant patterns over hundreds of time steps [90]. This stands in stark contrast to ARIMA, which struggles with strong non-linearities and long-term dependencies, and logistic regression, which lacks an inherent mechanism for modeling temporal dynamics beyond engineered features.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Glucose Prediction and Time-Series Analysis
| Tool / Resource | Function & Application | Key Characteristics |
|---|---|---|
| CGM Simulator (Simglucose) | Provides in-silico data for controlled testing and algorithm development; based on the UVA/Padova T1D Simulator [1]. | Includes a cohort of virtual "subjects," simulates CGM sensor errors, and models insulin delivery [1]. |
| OhioT1DM Dataset | A publicly available benchmark dataset for developing and validating data-driven forecasting models [40]. | Contains eight weeks of data per patient, including CGM, insulin, carbohydrates, and activity measures [40]. |
| Functional Data Analysis (FDA) | An advanced statistical method for analyzing CGM data, treating entire glucose trajectories as mathematical functions [92]. | Moves beyond traditional summary metrics to capture nuanced temporal patterns and identify metabolic subphenotypes [92]. |
| SHAP (SHapley Additive exPlanations) | A model-agnostic interpretability tool used to explain the output of "black-box" models like LSTM [93]. | Increases clinical trust by quantifying the contribution of each input feature to a specific prediction [93]. |
The experimental evidence clearly delineates the application domains where LSTM demonstrates superiority. For short-term, classification-oriented predictions like 15-minute glucose level categorization, simpler models like logistic regression can be highly accurate and efficient [1]. However, for longer-horizon forecasts (e.g., 1 hour) and the recognition of complex, non-linear temporal patterns, LSTM's architecture provides a definitive performance advantage. Its ability to learn from long sequences and adaptively manage historical information makes it the model of choice for complex time-series forecasting tasks in glucose prediction and beyond.
For researchers and drug development professionals working on diabetes management systems, selecting the optimal predictive model is crucial. Experimental evidence consistently demonstrates that while complex models like Long Short-Term Memory (LSTM) networks excel at long-term forecasting, Logistic Regression occupies a specific and critical niche: it achieves superior recall for short-term hypoglycemia classification, a scenario where missing a true event (hypoglycemia) carries far greater risk than a false alarm. This guide provides a structured comparison of model performance, experimental protocols, and essential research tools to inform your development process.
Model Performance: A Data-Driven Comparison
The table below synthesizes quantitative findings from recent studies, comparing the performance of Logistic Regression, LSTM, and ARIMA models across different prediction horizons and tasks.
Table 1: Comparative Model Performance for Glucose Prediction and Classification
| Model | Best/Niche Application | Key Performance Metric | Reported Value | Prediction Horizon | Citation |
|---|---|---|---|---|---|
| Logistic Regression | Short-term hypoglycemia classification | Recall (Sensitivity) | 98% | 15 minutes | [1] |
| Logistic Regression | Hyperglycemia prediction in hemodialysis patients | F1 Score | 0.85 | 24 hours | [48] |
| LSTM | Long-term hypoglycemia classification | Recall (Sensitivity) | 87% | 1 hour | [1] |
| LSTM | Multivariate disease incidence forecasting | RMSE | 10.78 | Medium/Long-Term | [94] |
| ARIMA | Univariate time-series forecasting (Non-Invasive Glucose) | RMSE (vs. LSTM) | ~71.7% lower | Short-Term | [20] |
| ARIMA | Glucose level classification (Hyper/Hypo) | Performance | Underperformed LR & LSTM | 15 min & 1 hour | [1] |
| XGBoost | Week-ahead risk of hypo-/hyperglycemia | ROC-AUC | 0.89 - 0.90 | 1 week | [95] |
| Transformer-VAE | Diabetes burden (DALYs) forecasting | MAE | 0.425 | Long-Term | [14] |
Interpreting the Data for Your Research
- Logistic Regression's Niche: The near-perfect 98% recall for 15-minute hypoglycemia prediction is its standout feature [1]. In clinical applications, high recall ensures the vast majority of dangerous hypoglycemic events are detected, making it the prudent choice for short-term, safety-critical alert systems.
- LSTM's Strength: LSTM models show superior performance for longer prediction horizons (e.g., 1 hour and beyond), as they effectively capture complex, non-linear temporal dependencies in glucose data [1] [94].
- ARIMA's Role: While computationally efficient and effective for simple univariate time-series forecasting [20], ARIMA models generally underperform machine learning models in classifying complex physiological events like hypoglycemia [1].
- Advanced Models: For highly specific, long-term forecasting tasks like population-level diabetes burden, advanced architectures like Transformer-VAE deliver the highest accuracy, though at a high computational cost [14].
Experimental Protocols from Key Studies
To validate and build upon these findings, researchers must understand the methodologies behind them.
Protocol 1: Direct 15-Minute Hypoglycemia Classification
This protocol directly demonstrates Logistic Regression's short-term superiority [1].
- Objective: To classify hypoglycemia (<70 mg/dL), euglycemia (70–180 mg/dL), and hyperglycemia (>180 mg/dL) 15 minutes and 1 hour in advance.
- Data Source: Combination of real patient CGM data from a COVID-19 vaccination study and in-silico data generated using the Simglucose (UVA/Padova T1D Simulator) platform [1].
- Feature Engineering: Core features were derived from the CGM time series, including:
- Rate of Change: The speed at which glucose levels are rising or falling.
- Moving Averages: Short-term trends in glucose levels.
- Glycemic Variability Indices: Measures of glucose fluctuations.
- Model Training & Evaluation:
- Models: ARIMA, Logistic Regression, LSTM.
- The dataset was split into training and testing sets.
- Performance was evaluated using precision, recall, and accuracy, with a focus on the recall for the hypoglycemia class.
Protocol 2: Hemodialysis Patient Glycemic Excursion Prediction
This study highlights Logistic Regression's effectiveness in a complex, high-risk patient cohort [48].
- Objective: To predict substantial level 2 hyperglycemia (TAR ≥10%) and level 1 hypoglycemia (TBR ≥1%) over the 24 hours following hemodialysis initiation.
- Data Source: 21 patients with diabetes receiving hemodialysis. Data included CGM metrics, HbA1c levels, and insulin use [48].
- Feature Engineering: Predictions were made per dialysis day. A 24-hour feature segment (CGM data before dialysis) was used to predict outcomes in the subsequent 24-hour prediction segment.
- Model Training & Evaluation:
- Models: Logistic Regression, XGBoost, TabPFN.
- Feature selection was performed using Recursive Feature Elimination with Cross-Validation (RFECV).
- Models were evaluated using F1 score and ROC-AUC.
Decision Framework for Model Selection
The choice between Logistic Regression, LSTM, and ARIMA is not a matter of which is universally "best," but which is most appropriate for the specific research goal. The following diagram maps this decision process.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Computational Tools for Glucose Prediction Research
| Item Name | Type | Function/Application in Research |
|---|---|---|
| Dexcom G6 / G5 CGM System | Data Collection Hardware | Provides real-time interstitial glucose measurements; the primary data source for model training and validation [48] [95]. |
| UVA/Padova T1D Simulator | Software (Simulation) | Validated simulator for generating in-silico type 1 diabetes patient data; useful for initial model testing and augmenting real-world datasets [1]. |
| Stineman Interpolation | Data Preprocessing Algorithm | A method for imputing missing CGM values in larger data gaps (e.g., 30-120 minutes), providing more realistic estimates than linear interpolation [96]. |
| IQR Outlier Detection | Data Preprocessing Algorithm | A robust statistical method for identifying and pruning physiologically implausible outliers in CGM and heart rate data [96]. |
| Recursive Feature Elimination with CV (RFECV) | Computational Method | Feature selection technique to identify the most predictive variables from a pool of CGM-derived metrics and patient characteristics [48]. |
| Scikit-learn / XGBoost / PyTorch | Software Library | Core open-source libraries for implementing Logistic Regression, XGBoost, and LSTM models, respectively [48] [95]. |
| Time Above/Below Range (TAR/TBR) | Analytical Metric | Standardized CGM-derived metrics used as consensus targets for defining and predicting hyperglycemia and hypoglycemia events [48] [95]. |
The accurate forecasting of physiological parameters, such as blood glucose levels, is a critical challenge at the intersection of clinical medicine and data science. Research in this domain has traditionally evaluated statistical models like ARIMA against recurrent neural networks such as LSTMs. However, the emergence of new deep learning architectures, particularly Transformers and simple linear models like DLinear, demands a fresh comparative analysis. This guide provides an objective benchmarking of these emerging architectures, framing the discussion within the broader context of glucose prediction research. It synthesizes current experimental data to offer researchers and drug development professionals a clear understanding of the performance trade-offs, computational requirements, and optimal application scenarios for each model class.
Model Architectures: From Simplicity to Complexity
Transformer-Based Models
Transformer architectures, originally designed for natural language processing, have been adapted for time series forecasting through several innovative variants. These models primarily leverage self-attention mechanisms to capture long-range dependencies in sequential data.
- Informer: Enhances the vanilla Transformer by introducing ProbSparse attention, which reduces time complexity from O(L²) to O(L log L), and a generative decoder that produces long-term forecasts in a single forward pass [97] [98].
- Autoformer: Incorporates an internal decomposition block that progressively separates trend and seasonal components within the series. It replaces standard self-attention with an auto-correlation mechanism that discovers period-based dependencies and aggregates similar sub-series [99] [97].
- FEDformer: Utilizes a frequency-enhanced attention mechanism combined with a mixture of expert decoders to efficiently capture both global and local patterns in time series data [99] [98].
Linear Models
In contrast to the complexity of Transformers, recent research has demonstrated that surprisingly simple linear models can achieve state-of-the-art performance on many time series forecasting tasks.
- DLinear: Decomposes a time series into trend and seasonal components using a moving average. Each component is processed by a separate single linear layer, and their outputs are summed to produce the final prediction [99] [100].
- NLinear: Normalizes the input sequence by subtracting the last value, passes it through a single linear layer, then adds the subtracted value back to the output. This simple adjustment helps address distribution shift between training and testing data [99] [100].
- GLinear: A recently proposed enhancement that integrates a non-linear GeLU-based transformation layer with Reversible Instance Normalization (RevIN) to better capture intricate patterns while maintaining data efficiency [98].
The logical relationship between these model architectures and their core components can be visualized as follows:
Performance Benchmarking
Quantitative Performance Comparison
Experimental results across multiple domains, including healthcare, provide crucial insights into the relative performance of these architectures. The following table summarizes key benchmarking metrics from recent studies:
Table 1: Performance comparison of forecasting models across different domains and datasets
| Model | Domain | Dataset | Metric | Performance | Citation |
|---|---|---|---|---|---|
| Transformer-VAE | Diabetes Burden | GBD (1990-2021) | MAE | 0.425 | [14] |
| Transformer-VAE | Diabetes Burden | GBD (1990-2021) | RMSE | 0.501 | [14] |
| LSTM | Diabetes Burden | GBD (1990-2021) | MAE | Higher than Transformer-VAE | [14] |
| GRU | Diabetes Burden | GBD (1990-2021) | MAE | Higher than Transformer-VAE | [14] |
| ARIMA | Diabetes Burden | GBD (1990-2021) | MAE | Higher than Transformer-VAE | [14] |
| Autoformer (univariate) | Traffic | Traffic Dataset | MASE | 0.910 | [97] |
| DLinear | Traffic | Traffic Dataset | MASE | 0.965 | [97] |
| Autoformer (univariate) | Exchange Rate | Exchange-Rate Dataset | MASE | 1.087 | [97] |
| DLinear | Exchange Rate | Exchange-Rate Dataset | MASE | 1.690 | [97] |
| Autoformer (univariate) | Electricity | Electricity Dataset | MASE | 0.751 | [97] |
| DLinear | Electricity | Electricity Dataset | MASE | 0.831 | [97] |
| iTransformer | Weather | Weather Dataset | MedianAbsE | 1.21 | [101] |
| Informer | Weather | Weather Dataset | Multiple Metrics | Best Performance | [101] |
| GLinear | Multivariate | ETTh1, Electricity, Traffic, Weather | Multiple Metrics | Outperforms DLinear, NLinear, Autoformer | [98] |
Computational Efficiency and Robustness
Beyond pure predictive accuracy, computational requirements and robustness to data imperfections are critical considerations for real-world deployment, particularly in healthcare applications with privacy concerns and potential data sparsity.
Table 2: Computational efficiency and robustness characteristics of different model types
| Model Type | Training Time | Data Requirements | Robustness to Noise | Robustness to Missing Data | Interpretability |
|---|---|---|---|---|---|
| Transformer-VAE | High | Large | Superior (p < 0.01) | Superior (p < 0.01) | Low |
| LSTM | Medium | Medium | Moderate | Moderate | Medium |
| GRU | Medium | Medium | Moderate | Moderate | Medium |
| ARIMA | Low | Small | Low | Low | High |
| DLinear/NLinear | Very Low (seconds) | Small | High | High | High |
| GLinear | Low | Very Small (Data Efficient) | High | High | High |
| FedGlu (Personalized FL) | Medium | Distributed (Privacy-preserving) | High for glycemic excursions | High | Medium |
Experimental Protocols and Methodologies
Standard Benchmarking Procedures
To ensure fair comparisons across studies, researchers have developed standardized evaluation protocols for time series forecasting models:
- Data Partitioning: Most studies follow a chronological split, using earlier periods for training and later periods for testing. For example, studies using Global Burden of Disease (GBD) data from 1990-2021 typically reserve 1990-2014 for training and 2015-2021 for evaluation [14].
- Evaluation Metrics: Common metrics include Mean Absolute Error (MAE), Root Mean Squared Error (RMSE), Mean Absolute Scaled Error (MASE), and for healthcare applications, clinical accuracy metrics like Clark's Error Grid Analysis (EGA) [14] [5].
- Cross-Validation: Time-series cross-validation with expanding or sliding windows is employed to assess model stability across different temporal segments.
- Normalization: Z-score normalization is commonly applied to multivariate series with variables of different scales, particularly in financial and healthcare applications [100] [5].
Specialized Methodologies for Healthcare Applications
Glucose prediction and diabetes burden forecasting present unique challenges that require specialized methodological considerations:
- Imbalanced Data Handling: Glycemic excursion regions (hypoglycemia and hyperglycemia) are inherently rare compared to normal ranges. Advanced techniques like the Hypo-Hyper (HH) loss function, which applies higher penalties for errors in extreme ranges, have shown 46% improvement over standard MSE loss [5].
- Privacy-Preserving Learning: Federated Learning (FL) frameworks like FedGlu enable collaborative model training without sharing sensitive patient data, addressing HIPAA compliance concerns while improving prediction performance for 84% of patients (105 out of 125) in recent studies [5].
- Temporal Dependency Capture: Models are evaluated on their ability to capture both short-term fluctuations (relevant for immediate clinical decisions) and long-term trends (essential for public health planning and resource allocation) [14].
The following workflow diagram illustrates a standardized experimental protocol for benchmarking forecasting models in healthcare applications:
The Researcher's Toolkit
Implementing and benchmarking these forecasting models requires access to specific datasets, software tools, and computational infrastructure:
Table 3: Essential resources for implementing and benchmarking forecasting models
| Resource | Type | Description | Application in Research |
|---|---|---|---|
| GBD Dataset | Data | Global Burden of Disease data from IHME, containing longitudinal health indicators | Forecasting diabetes burden, mortality, and prevalence trends [14] |
| OhioT1DM Dataset | Data | Continuous glucose monitoring data for type 1 diabetes patients | Developing personalized glucose prediction models [5] |
| ETTh Dataset | Data | Electricity Transformer Temperature dataset with multiple variables | Benchmarking long-term time series forecasting models [98] |
| NeuralForecast Library | Software | Python library with unified interface for multiple forecasting models | Comparative studies of transformer and RNN models [101] |
| Transformers | Software | Hugging Face's library with implementations of Autoformer and other transformers | Accessing pre-trained time series models and building custom variants [97] |
| TSFM-Bench | Software | Comprehensive benchmark for Time Series Foundation Models | Standardized evaluation across multiple domains and scenarios [102] |
| NVIDIA A10 GPU | Hardware | Graphics processing unit for accelerated model training | Practical experimentation with complex transformer architectures [100] |
The benchmarking evidence presented in this guide reveals a nuanced landscape for time series forecasting in glucose prediction and related healthcare applications. Transformer-based models demonstrate superior performance in capturing complex long-range dependencies and handling noisy, incomplete data, achieving the highest predictive accuracy for diabetes burden forecasting in recent studies. However, their practical deployment is constrained by high computational costs and interpretability challenges.
Conversely, linear models like DLinear, NLinear, and GLinear offer compelling advantages in computational efficiency, interpretability, and data efficiency, while maintaining competitive—and in some cases superior—predictive performance compared to complex transformers. The recent development of enhanced linear models with non-linear transformations and reversible normalization suggests ongoing innovation in this seemingly simple class of models.
For researchers and drug development professionals working on glucose prediction, the optimal model choice depends critically on the specific application context. When forecasting long-term population-level diabetes trends, Transformer-based architectures may justify their computational overhead through enhanced accuracy. For personal glucose prediction and real-time clinical decision support, simpler linear models or specialized approaches like federated learning with HH loss functions may provide the ideal balance of performance, efficiency, and privacy preservation. As the field evolves, hybrid approaches that combine the strengths of both architectural paradigms likely represent the most promising direction for future research.
Conclusion
The comparative analysis reveals a critical takeaway: no single model universally dominates glucose prediction. Performance is highly contingent on the specific clinical context, prediction horizon, and data characteristics. ARIMA can outperform complex deep learning models like LSTM in specific, short-term forecasting scenarios, offering a compelling balance of accuracy and simplicity. Conversely, LSTM networks excel in capturing long-term, complex temporal dependencies, making them suitable for dynamic, longer-horizon predictions. Logistic regression remains a potent tool for high-stakes, short-term classification of glycemic events like hypoglycemia. Future directions should focus on developing hybrid models that leverage the strengths of each architecture, incorporating federated learning for privacy-preserving collaboration, and advancing personalized, adaptive models that can continuously learn from individual patient data to improve real-world clinical decision-support systems and accelerate the development of closed-loop artificial pancreas systems.
References
- 1. Comparative Analysis of Predictive Interstitial Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10574913/]
- 2. Comparative Analysis of Predictive Interstitial Glucose ... [https://pubmed.ncbi.nlm.nih.gov/37837098/]
- 3. Enhancing AI-driven forecasting of diabetes burden [https://pmc.ncbi.nlm.nih.gov/articles/PMC12335553/]
- 4. Prediction of Next Glucose Measurement in Hospitalized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9929733/]
- 5. A personalized federated learning-based glucose ... [https://www.nature.com/articles/s41598-025-22316-4]
- 6. Prophet ARIMA for Time Series Prediction vs vs LSTM [https://neptune.ai/blog/arima-vs-prophet-vs-lstm]
- 7. Managing Exercise-Related Glycemic Events in Type 1 Diabetes [https://diabetes.jmir.org/2025/1/e68948]
- 8. Classification of Hypoglycemic Events in Type 1 Diabetes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10203083/]
- 9. A Comparative Study of Transformer-Based Models for ... [https://arxiv.org/abs/2505.08821]
- 10. LLM-Powered Personalized Glucose Prediction in Type 1 ... [https://www.sciencedirect.com/science/article/pii/S2950363925000390]
- 11. Study explores AI-enhanced wearable devices for Type 2 ... [https://www.buffalo.edu/news/releases/2025/11/UB-AI-Enhanced-Wearables-Type-2-Diabetes-Study.html]
- 12. Machine learning glucose forecasting models for septic ... [https://www.nature.com/articles/s41598-025-23057-0]
- 13. Data-Efficiency with Comparable Accuracy [https://www.mdpi.com/2673-4540/6/10/115]
- 14. Enhancing AI-driven forecasting of diabetes burden [https://www.nature.com/articles/s41598-025-14599-4]
- 15. IJCMCR-RA-ID-01382 [https://ijclinmedcasereports.com/ijcmcr-ra-id-01382/]
- 16. Optimization of blood glucose prediction with LSTM ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809425003258]
- 17. Exploring the potential of deep learning models integrating ... [https://pubmed.ncbi.nlm.nih.gov/40190336/]
- 18. A personalized federated learning-based glucose prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12583674/]
- 19. Comparison of Three Interstitial Glucose Level Prediction ... [https://www.preprints.org/manuscript/202309.0755]
- 20. Learned prediction of cholesterol and glucose using ... [https://www.sciencedirect.com/science/article/pii/S2666720723001649]
- 21. Hybrid time series and machine learning models for ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-025-23318-7]
- 22. Improved Methods for Mid-Term Blood Glucose Level Prediction Using... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8307794/]
- 23. 12 Important Model Evaluation Metrics for Machine ... [https://www.analyticsvidhya.com/blog/2019/08/11-important-model-evaluation-error-metrics/]
- 24. Understanding Evaluation Metrics for Time Series Forecasting [https://eshban9492.medium.com/understanding-evaluation-metrics-for-time-series-forecasting-5c8a3c877654]
- 25. Forecasting Time Series - Evaluation Metrics [https://auto.gluon.ai/stable/tutorials/timeseries/forecasting-metrics.html]
- 26. Evaluation Metrics in Machine Learning [https://www.geeksforgeeks.org/machine-learning/metrics-for-machine-learning-model/]
- 27. 9 Accuracy Metrics for ML Engineers to Evaluate AI Model | Galileo [https://galileo.ai/blog/accuracy-metrics-ai-evaluation]
- 28. What is Evaluation metrics and When to use Which metrics? [https://medium.com/the-rise-of-unbelievable/what-is-evaluation-metrics-and-when-to-use-which-metrics-23d16446d690]
- 29. Evaluating Prediction Model Performance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10529246/]
- 30. Logistic Regression in Machine Learning [https://www.geeksforgeeks.org/machine-learning/understanding-logistic-regression/]
- 31. Data Preprocessing for ML [https://www.dataentryoutsourced.com/blog/data-preprocessing-for-machine-learning-clean-data-smarter-models/]
- 32. How I Use Pandas to Preprocess Time-Series Data for ... [https://medium.com/@connect.hashblock/how-i-use-pandas-to-preprocess-time-series-data-for-lstm-models-6afb22c5856f]
- 33. Preparing Your Data for the ARIMA Model: The Secret Step ... [https://medium.com/@moubarakmohamed81/preparing-your-data-for-the-arima-model-the-secret-step-to-reliable-forecasts-bbc3ff524734]
- 34. How LSTMs Are Powering Predictive Analytics in Business ... [https://dev.to/vikas76/how-lstms-are-powering-predictive-analytics-in-business-by-2025-2gpb]
- 35. Exploration of Foundational Models for Blood Glucose ... [https://www.mdpi.com/2673-4540/5/6/42]
- 36. Machine learning-based glucose prediction with use of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8224858/]
- 37. A data-driven personalized approach to predict blood ... [https://pubmed.ncbi.nlm.nih.gov/40164029/]
- 38. Type 1 Diabetes Hypoglycemia Prediction Algorithms [https://diabetes.jmir.org/2022/3/e34699/]
- 39. Long-Term Prediction of Blood Glucose Levels in Type 1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10658677/]
- 40. Data-driven blood glucose level prediction in type 1 diabetes [https://www.nature.com/articles/s41598-024-70277-x]
- 41. Identifying early blood glucose trajectories in sepsis linked to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12176745/]
- 42. Comparison of ARIMA and LSTM for prediction of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8759700/]
- 43. Comparison of ARIMA and LSTM in Forecasting the ... [https://www.mdpi.com/1660-4601/18/11/6174]
- 44. Intelligent Prediction Platform for Sepsis Risk Based on Real ... [https://medinform.jmir.org/2025/1/e74940]
- 45. Comparison between traditional logistic regression and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11743956/]
- 46. LSTMs and Neural Attention Models for Blood Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7890945/]
- 47. Machine learning-based prediction of hypoglycemia severity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483848/]
- 48. Development of Machine Learning Models to Predict ... [https://www.medrxiv.org/content/10.1101/2025.10.24.25338707v1.full]
- 49. Comparison between XGboost model and logistic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11067675/]
- 50. Development of a machine learning-based interface for ... [https://www.nature.com/articles/s41598-025-22381-9]
- 51. XGBoost vs Logistic Regression [https://medium.com/@heyamit10/xgboost-vs-logistic-regression-a3dc03b0e6f8]
- 52. Accurate prediction of glucose concentration and ... [https://www.sciencedirect.com/science/article/pii/S1746809420300793]
- 53. Prediction of glucose in whole blood by near-infrared ... [https://pubmed.ncbi.nlm.nih.gov/16965156/]
- 54. Handheld NIR Spectral Sensor Module Based on a Fully- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9501814/]
- 55. Comparative Performance of NIR-Hyperspectral Imaging ... [https://www.mdpi.com/2673-9321/2/3/35]
- 56. Accuracy of near-infrared spectroscopy for prediction ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25009609]
- 57. Time series forecasting: 2025 complete guide [https://www.influxdata.com/time-series-forecasting-methods/]
- 58. Time Series Forecasting: Mastering Predictive Sales ... [https://forecastio.ai/blog/time-series-forecasting]
- 59. Performance evaluation of NIR spectrophotometer ... [https://www.sciencedirect.com/science/article/pii/S0016236123026297]
- 60. A comparative study between Near-Infrared (NIR ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0319523]
- 61. A multimodal physiological dataset for non-invasive blood ... [https://www.nature.com/articles/s41597-025-06090-6]
- 62. Generalized multi task learning framework for glucose ... [https://www.nature.com/articles/s41746-025-01994-4]
- 63. A deep learning framework for virtual continuous glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12065870/]
- 64. Handling Class Imbalance in Multi-class Classification with ... [https://stackoverflow.com/questions/77462336/handling-class-imbalance-in-multi-class-classification-with-custom-loss-function]
- 65. Evaluating Prediction of Continuous Clinical Values [https://pmc.ncbi.nlm.nih.gov/articles/PMC9246512/]
- 66. UNITI: Framework for multi-task learning across datasets to ... [https://www.sciencedirect.com/science/article/pii/S0957417425012758]
- 67. Optimizing Multi-task Learning Models in Practice [https://towardsdatascience.com/optimizing-multi-task-learning-models-in-practice-bde4f18f0bd8/]
- 68. Improving Generalization in Federated Learning with Highly... [https://openreview.net/forum?id=HqmXiuFaOr¬eId=f41Sm8ZCCW]
- 69. FedSWA: Improving Generalization in Federated Learning ... [https://arxiv.org/abs/2507.20016]
- 70. Improving Generalization in Federated Learning by ... [https://arxiv.org/abs/2203.11834]
- 71. Federated Multi-Task Learning under a Mixture of ... [https://proceedings.neurips.cc/paper/2021/hash/82599a4ec94aca066873c99b4c741ed8-Abstract.html]
- 72. Towards Unified Modeling in Federated Multi-Task ... [https://arxiv.org/abs/2505.24185]
- 73. Towards Hetero-Client Federated Multi-Task Learning [https://github.com/innovator-zero/FedHCA2]
- 74. Federated learning: a privacy-preserving approach to data- ... [https://www.frontiersin.org/journals/drug-safety-and-regulation/articles/10.3389/fdsfr.2025.1579922/full]
- 75. Personalized federated learning for a better customer ... [https://www.amazon.science/blog/personalized-federated-learning-for-a-better-customer-experience]
- 76. Personalized federated learning for cross-building energy ... [https://www.sciencedirect.com/science/article/abs/pii/S0306261924003994]
- 77. Performance of diabetes risk prediction models: a systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12586975/]
- 78. An innovative attention-based CNN for accurate type 2 ... [https://pubmed.ncbi.nlm.nih.gov/41026707/]
- 79. Hybrid ARIMA-LSTM for COVID-19 forecasting [https://pmc.ncbi.nlm.nih.gov/articles/PMC12453849/]
- 80. Self-adapting LSTM models for evolving data distributions [https://www.sciencedirect.com/science/article/abs/pii/S0169260725005693]
- 81. Detection of Calibration Drift in Clinical Prediction Models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8627243/]
- 82. Monitoring the calibration of probability forecasts with an ... [https://arxiv.org/html/2510.25573v1]
- 83. Detecting Data Drift: Tools, Techniques, and Best Practices ... [https://medium.com/@Symufolk/detecting-data-drift-tools-techniques-and-best-practices-for-2025-d0d34b863c3e]
- 84. Model Drift: The Ultimate Guide to Maintaining Machine ... [https://buzzclan.com/data-engineering/what-is-model-drift/]
- 85. Handling data drift in deep learning-based quality monitoring [https://link.springer.com/article/10.1007/s10845-025-02569-6]
- 86. Discrete Time Series Forecasting in Non-Invasive ... [https://www.mdpi.com/1424-8220/25/14/4319]
- 87. Event-triggered smart dual hormone artificial pancreas for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12402495/]
- 88. Experimental Study of Long Short-Term Memory and ... [https://www.mdpi.com/1424-8220/24/19/6235]
- 89. A comparative analysis of LSTM models aided with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11785954/]
- 90. Unlocking the Power of LSTM for Long Term Time Series ... [https://arxiv.org/html/2408.10006v1]
- 91. A novel YOLO LSTM approach for enhanced human action ... [https://www.nature.com/articles/s41598-025-01898-z]
- 92. CGM Data Analysis 2.0: Functional Data Pattern Recognition ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12356821/]
- 93. Integration of artificial intelligence and wearable ... [https://www.nature.com/articles/s41746-025-02036-9]
- 94. Comparison of ARIMA and LSTM in Forecasting the Incidence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8201362/]
- 95. Explainable Machine-Learning Models to Predict Weekly ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11571614/]
- 96. Benchmarking ResNet for Short-Term Hypoglycemia ... [https://arxiv.org/html/2511.02849v1]
- 97. Yes, Transformers are Effective for Time Series Forecasting ... [https://huggingface.co/blog/autoformer]
- 98. A Novel Architecture for Enhanced Time Series Prediction [https://arxiv.org/html/2501.01087v1]
- 99. Do Transformers Lose to Linear Models? [https://towardsdatascience.com/transformers-lose-to-linear-models-902164ca5974/]
- 100. A Single Linear Layer Is All You Need [https://simudyne.com/resources/a-single-linear-layer-is-all-you-need-linear-models-outperform-transformers-for-long-term-time-series-forecasting/]
- 101. Deep learning in time series forecasting with transformer ... [https://peerj.com/articles/cs-3001/]
- 102. TSFM-Bench: A Comprehensive and Unified Benchmark of ... [https://arxiv.org/html/2410.11802v6]