From Glucose to ATP: Molecular Mechanisms, Metabolic Regulation, and Therapeutic Targeting
This article provides a comprehensive analysis of the molecular machinery and regulatory networks governing cellular glucose uptake and utilization for ATP production.
From Glucose to ATP: Molecular Mechanisms, Metabolic Regulation, and Therapeutic Targeting
Abstract
This article provides a comprehensive analysis of the molecular machinery and regulatory networks governing cellular glucose uptake and utilization for ATP production. Tailored for researchers and drug development professionals, it synthesizes foundational biochemistry with cutting-edge discoveries in signaling pathways and metabolic reprogramming. We explore advanced methodologies for investigating metabolic flux, examine dysregulation in disease contexts such as diabetes and cancer, and evaluate computational and experimental approaches for pathway optimization and therapeutic intervention. The scope spans from fundamental transport mechanisms to the application of machine learning and real-time metabolomics, offering an integrated perspective essential for innovating metabolic therapies.
The Core Machinery: Unraveling Glucose Transport and Metabolic Pathways
Glucose serves as the primary source of energy for metabolic processes in mammalian cells, fueling ATP production through glycolysis and oxidative phosphorylation [1]. As a polar, hydrophilic molecule, glucose cannot freely diffuse across the lipophilic plasma membrane and requires specific carrier proteins for cellular uptake [2]. The study of glucose transporters is fundamental to understanding the mechanistic basis of glucose uptake and utilization for ATP production, with profound implications for metabolic diseases, cancer biology, and therapeutic development. Two principal families of transport proteins facilitate this process: the facilitative glucose transporters (GLUTs or SLC2A family) that enable passive glucose movement down concentration gradients, and the sodium-glucose cotransporters (SGLTs or SLC5A family) that mediate active transport against concentration gradients by coupling glucose uptake to sodium import [3] [1]. These transporters exhibit distinct tissue distributions, kinetic properties, and regulatory mechanisms that collectively maintain whole-body glucose homeostasis and ensure adequate substrate provision for cellular energy production.
The Facilitative Glucose Transporter (GLUT/SLC2A) Family
Structural Organization and Classification
The GLUT proteins are integral membrane proteins belonging to the major facilitator superfamily (MFS), characterized by 12 membrane-spanning α-helical domains with both amino and carboxyl termini exposed on the cytoplasmic side of the plasma membrane [4] [2]. These transporters operate via an alternate conformation model, exposing a single substrate binding site toward either the extracellular or intracellular environment [4]. Binding of glucose to one site triggers a conformational change that releases glucose to the opposite side of the membrane, with putative substrate binding regions located in transmembrane segments 9, 10, and 11 [4].
The human genome encodes 14 GLUT proteins categorized into three classes based on sequence similarity [4] [2]. Class I includes the most extensively characterized transporters GLUT1-4 and GLUT14, sharing 48-63% sequence identity and containing characteristic motifs including a QLS motif in transmembrane helix 7 associated with glucose selectivity [2]. Class II comprises GLUT5, GLUT7, GLUT9, and GLUT11, which lack the QLS motif and display divergent substrate specificities [2]. Class III includes GLUT6, GLUT8, GLUT10, GLUT12, and GLUT13 (HMIT), distinguished by conserved motifs in transmembrane domains and loops despite lower overall sequence identity (19-41%) [2].
Table 1: Classification and Properties of Major Facilitative Glucose Transporters (GLUTs)
| Transporter | Class | Gene | Tissue Distribution | Key Physiological Functions | Substrate Specificity |
|---|---|---|---|---|---|
| GLUT1 | I | SLC2A1 | Ubiquitous; high in erythrocytes, blood-brain barrier | Basal glucose uptake, blood-brain barrier transport [4] | Glucose, galactose, glucosamine [2] |
| GLUT2 | I | SLC2A2 | Liver, pancreatic β-cells, renal tubules, small intestine | Bidirectional transport, glucose sensing [5] [4] | Glucose, galactose, fructose [4] |
| GLUT3 | I | SLC2A3 | Neurons, placenta | High-affinity neuronal glucose transport [4] | Glucose [2] |
| GLUT4 | I | SLC2A4 | Skeletal muscle, adipose tissue, heart | Insulin-regulated glucose storage [6] [4] | Glucose [2] |
| GLUT5 | II | SLC2A5 | Small intestine, testes, kidney, adipose tissue | Fructose transport [5] [2] | Fructose [2] |
| GLUT8 | III | SLC2A8 | Testes, brain, liver, adipose tissue | Insulin-regulated in some tissues [5] | Glucose [2] |
| GLUT12 | III | SLC2A12 | Heart, prostate, placenta, mammary gland | Insulin-responsive transport [5] | Glucose [2] |
Tissue-Specific Functions and Regulatory Mechanisms
GLUT1 in Barrier Tissues and Erythrocytes
GLUT1 demonstrates widespread expression in fetal tissues and maintains high expression in adult erythrocytes and endothelial cells of barrier tissues such as the blood-brain barrier [4]. It provides the basal glucose uptake necessary to sustain cellular respiration across all cell types [1] [4]. GLUT1 expression is sensitive to glucose availability, with increased membrane localization under reduced glucose conditions [4]. Notably, GLUT1 overexpression represents a common feature in many tumors, supporting the heightened glycolytic flux characteristic of cancer cells [7] [4].
GLUT2 in Metabolic Sensing and Interorgan Coordination
GLUT2 functions as a high-capacity, low-affinity bidirectional transporter expressed in hepatocytes, pancreatic beta cells, renal tubular cells, and the basolateral membrane of intestinal epithelial cells [5] [4]. In hepatocytes, GLUT2 enables both glucose uptake for glycolysis and glycogen synthesis, as well as glucose release during gluconeogenesis [4]. pancreatic beta cells, GLUT2-mediated glucose transport facilitates glucose sensing and insulin secretion regulation, establishing a critical link between blood glucose levels and hormonal response [4].
GLUT3 in Neuronal Glucose Utilization
As the primary glucose transporter in neurons, GLUT3 exhibits high affinity for glucose, enabling efficient substrate capture even at low extracellular concentrations [4] [8]. This kinetic property is particularly crucial in brain tissue where glucose availability may fluctuate, ensuring a constant supply of glucose for neuronal energy metabolism and neurotransmitter synthesis [8].
GLUT4 in Insulin-Regulated Glucose Homeostasis
GLUT4 serves as the principal insulin-responsive glucose transporter, mediating the bulk of insulin-stimulated glucose uptake into skeletal muscle and adipose tissue [5] [6]. Under basal conditions, approximately 90% of GLUT4 resides within intracellular vesicles, rapidly translocating to the plasma membrane upon insulin stimulation or muscle contraction [6]. This translocation process increases the maximal velocity of glucose transport without altering substrate affinity [6]. Insulin signaling triggers GLUT4 externalization through two parallel pathways: one involving phosphatidylinositol 3-kinase (PI3K) activation and another requiring the proto-oncoprotein c-Cbl and its associated protein CAP, which activates the GTPase TC10 in lipid rafts [6]. Exercise-stimulated GLUT4 translocation occurs independently of PI3K via AMP-activated protein kinase (AMPK) activation, providing an alternative mechanism for enhancing glucose uptake during increased metabolic demand [6].
The critical importance of GLUT4 in metabolic health is underscored by its dysregulation in insulin resistance and type 2 diabetes mellitus (T2DM), where impaired GLUT4 translocation contributes to defective glucose disposal and hyperglycemia [6]. Research demonstrates that increasing intracellular GLUT4 concentrations can reverse insulin resistance in animal models, highlighting its potential as a therapeutic target [6].
Diagram Title: GLUT4 Translocation Signaling Pathways
The Sodium-Glucose Cotransporter (SGLT/SLC5A) Family
Structural Basis of Secondary Active Transport
SGLTs constitute a distinct family of membrane transporters that utilize the electrochemical sodium gradient established by Na+/K+ ATPase to drive active glucose transport against concentration gradients [3]. These symporters belong to the sodium/solute symporter family (SSSF) within the SLC5A gene family and function through an alternating-access mechanism, cycling through multiple conformational states to transport substrates across the membrane [3]. Structural studies reveal that SGLT proteins contain 14 transmembrane helices (TM0-TM13) with a LeuT structural fold [9]. High-resolution cryo-EM structures have illuminated the molecular details of substrate recognition and transport, showing that SGLT2 transitions through outward-open, occluded, and inward-open conformations during its transport cycle [9].
The sodium-glucose cotransport process begins with the binding of sodium ions to the outward-facing transporter, increasing its affinity for glucose binding [8]. Subsequent conformational changes occlude the substrate binding site before transitioning to an inward-open conformation that releases first sodium then glucose into the cytoplasm [9] [8]. The transporter then returns to the outward-facing conformation to complete the cycle [9]. This mechanism allows SGLTs to accumulate glucose intracellularly even when extracellular concentrations are low, a critical function in the intestinal lumen and renal tubules [3].
Table 2: Characteristics of Sodium-Glucose Cotransporters (SGLTs)
| Transporter | Gene | Sodium:Glucose Stoichiometry | Tissue Distribution | Primary Physiological Functions | Substrate Specificity |
|---|---|---|---|---|---|
| SGLT1 | SLC5A1 | 2:1 | Small intestine (brush border), kidney (S3 segment) | Intestinal glucose absorption, renal glucose reabsorption [3] | Glucose, galactose [3] |
| SGLT2 | SLC5A2 | 1:1 | Kidney (S1/S2 segments of proximal tubule) | Bulk renal glucose reabsorption (80-90%) [3] [9] | Glucose [3] |
| SGLT3 | SLC5A4 | N/A (glucose sensor) | Small intestine, skeletal muscle, cholinergic neurons | Glucose sensing without transport [3] | Glucose [3] |
| SGLT4 | SLC5A9 | Sodium-dependent | Small intestine, kidney, liver, brain | Mannose, fructose, glucose transport [3] | Mannose, fructose, glucose [3] |
| SGLT5 | SLC5A10 | Sodium-dependent | Kidney | Glucose, galactose, fructose transport [3] | Glucose, galactose, fructose [3] |
| SGLT6 | SLC5A11 | Sodium-dependent | Brain, kidney | Glucose, myo-inositol transport [3] | Glucose, myo-inositol [3] |
Complementary Roles in Glucose Homeostasis
SGLT1 in Intestinal Glucose Absorption
SGLT1 serves as the primary mediator of dietary glucose absorption in the small intestine, located at the brush border membrane of enterocytes [10]. As a high-affinity, low-capacity transporter with 2:1 sodium:glucose stoichiometry, SGLT1 efficiently captures luminal glucose even at low concentrations [3] [10]. Recent research has revealed that in obesity, the adipose tissue-derived secretome enhances SGLT1 affinity for glucose through altered phosphorylation, potentially contributing to hyperglycemia and type 2 diabetes pathogenesis [10].
SGLT2 in Renal Glucose Reclamation
SGLT2 represents the dominant glucose transporter in the renal proximal tubule, responsible for reabsorbing 80-90% of filtered glucose [3] [9]. Its low-affinity, high-capacity transport characteristics complement SGLT1's high-affinity, low-capacity function in the later nephron segments [3]. The central role of SGLT2 in renal glucose handling has made it an attractive therapeutic target for diabetes management, with SGLT2 inhibitors promoting glycosuria and reducing hyperglycemia [3] [9].
Experimental Approaches in Glucose Transporter Research
Methodologies for Investigating Transporter Function
Glucose Uptake Assays in Cell Culture Systems
The assessment of glucose transporter activity typically employs radiolabeled or fluorescent glucose analogs in controlled cell culture systems. For SGLT function studies, the fluorescent substrate 1-NBD-glucose provides a sensitive measure of transport activity, with inhibition experiments using specific competitors like 4-deoxy-4-fluoro-D-glucopyranoside (4FDG) to characterize transporter kinetics [9]. These assays are conducted under sodium-containing buffers to maintain the sodium gradient essential for SGLT function, with potassium substitution serving as a negative control [9].
Detailed Protocol: SGLT Inhibition Assay
- Culture epithelial cells (e.g., IEC-18) to 80-90% confluence in appropriate medium
- Pre-incubate cells with experimental treatments (e.g., adipose-derived secretome) for specified durations [10]
- Replace medium with transport buffer containing 1-NBD-glucose (10-100 μM) with or without inhibitor (4FDG) [9]
- Incubate for precise time intervals (typically 2-10 minutes) at 37°C
- Terminate uptake by rapid washing with ice-cold phosphate-buffered saline
- Lyse cells and quantify fluorescence using appropriate excitation/emission wavelengths (Ex: 465 nm, Em: 540 nm)
- Calculate kinetic parameters (Km, Vmax) from substrate saturation curves
Brush Border Membrane Vesicle (BBMV) Preparation
For transport studies in polarized epithelial cells, BBMV isolation provides a purified membrane system for characterizing transporter kinetics without confounding effects of intracellular metabolism.
Detailed Protocol: BBMV Preparation from Intestinal Tissue
- Isolate intestinal segments and flush with ice-cold saline
- Scrape mucosal layer and homogenize in hypotonic buffer (50 mM mannitol, 2 mM HEPES/Tris, pH 7.4)
- Add MgCl2 to 10 mM final concentration and incubate on ice for 20 minutes to aggregate intracellular membranes
- Centrifuge at 3,000 × g for 15 minutes to remove aggregated material
- Collect supernatant and centrifuge at 30,000 × g for 30 minutes to pellet BBMV
- Resuspend vesicles in appropriate buffer and assess purity by marker enzyme (alkaline phosphatase) enrichment [10]
Cryo-Electron Microscopy for Structural Analysis
High-resolution structural studies of glucose transporters utilize cryo-EM to capture conformational states during the transport cycle.
Detailed Protocol: SGLT2 Structural Analysis
- Express hSGLT2-MAP17 complex in mammalian cell system (e.g., HEK293 cells)
- Purify complex using affinity and size-exclusion chromatography
- Incubate with Fab90 antibody fragment to improve particle orientation [9]
- Prepare cryo-EM grids by applying sample and vitrifying in liquid ethane
- Collect images using modern cryo-EM equipped with direct electron detector
- Process images to generate 3D reconstructions at 2.5-3.5 Å resolution
- Build atomic models and analyze substrate binding sites and conformational states [9]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Glucose Transporter Research
| Reagent/Cell Line | Category | Research Application | Key Features |
|---|---|---|---|
| 1-NBD-Glucose | Fluorescent substrate | SGLT transport assays | Non-metabolizable glucose analog for real-time uptake measurement [9] |
| 4FDG | Transport competitor | SGLT inhibition studies | Glucose analog that competes with substrate binding [9] |
| Cytochalasin B | GLUT inhibitor | GLUT binding studies | High-affinity inhibitor that binds to intracellular site [2] |
| IEC-18 cells | Cell line | Intestinal transport studies | Rat intestinal epithelial cell line for SGLT1 regulation [10] |
| Fab90 antibody | Structural biology tool | Cryo-EM studies | Monoclonal antibody fragment improving SGLT2 particle orientation [9] |
| HEK293 cells | Expression system | Transporter overexpression | Mammalian cell line for recombinant GLUT/SGLT expression [9] |
| Obese Zucker Rat | Animal model | Obesity/metabolism studies | Genetic obesity model for adipose-tissue regulation of transporters [10] |
Diagram Title: Glucose Transporter Research Workflow
Pathophysiological Implications and Therapeutic Targeting
Dysregulation of glucose transporters features prominently in metabolic disorders, neurodegenerative diseases, and cancer [5] [7] [2]. In type 2 diabetes, impaired GLUT4 translocation in skeletal muscle and adipose tissue contributes to insulin resistance and hyperglycemia [6]. Simultaneously, increased SGLT1-mediated intestinal glucose absorption may exacerbate postprandial hyperglycemia [10]. Therapeutically, SGLT2 inhibitors have emerged as effective antidiabetic agents that promote urinary glucose excretion, while selective SGLT1 inhibition represents an emerging approach targeting intestinal glucose absorption [3]. In cancer biology, upregulated GLUT1 expression supports the Warburg effect and increased glycolytic flux in tumor cells, positioning GLUT inhibitors as potential anticancer agents [7]. Neurologically, disrupted glucose transporter expression at the blood-brain barrier (GLUT1) and in neurons (GLUT3) may contribute to neurodegenerative processes in Alzheimer's and Parkinson's diseases through impaired energy metabolism [2]. These pathophysiological connections highlight the fundamental importance of glucose transport systems in health and disease, reinforcing their value as therapeutic targets across multiple disease states.
The entry of glucose into the cell is a critical first step in energy production, serving as a fundamental process in cellular metabolism. Glucose uptake is mediated by specialized membrane transport proteins that overcome the impermeability of the phospholipid bilayer to hydrophilic molecules [11]. Two primary mechanisms facilitate this process: facilitated diffusion and secondary active transport. These systems enable the controlled passage of glucose from the extracellular environment into the cytoplasm, where it can undergo glycolysis and subsequent oxidative phosphorylation to produce adenosine triphosphate (ATP) [12]. The specific mechanism employed varies by cell type, physiological context, and energy requirements, creating a complex regulatory landscape essential for maintaining metabolic homeostasis. Understanding these distinct transport pathways is crucial for research focused on neuronal bioenergetics, metabolic disorders, and drug development targeting nutrient uptake pathways.
Facilitated Diffusion: Passive Transit via Carrier Proteins
Mechanism and Molecular Players
Facilitated diffusion is a passive transport process where carrier proteins mediate the selective passage of molecules down their concentration gradient without direct energy expenditure [11]. The transported molecules do not dissolve in the phospholipid bilayer; instead, their passage is enabled by proteins that allow them to cross the membrane without interacting with its hydrophobic interior [11]. For glucose, this process is accomplished by the GLUT (GLucose Transporters) family of proteins, which are integral membrane proteins containing 12 membrane-spanning helices with both amino and carboxyl termini exposed on the cytoplasmic side of the plasma membrane [4].
These transporters operate according to an alternating conformation model, where the transporter exposes a single substrate-binding site toward either the outside or the inside of the cell [4]. The binding of glucose to one site provokes a conformational change associated with transport, releasing glucose to the other side of the membrane [4]. The inner and outer glucose-binding sites are thought to be located in transmembrane segments 9, 10, and 11 [4].
Table 1: Key Facilitative Glucose Transporters (GLUTs) in Mammalian Cells
| Transporter | Primary Tissue Distribution | Kinetic Properties (Km) | Functional Role |
|---|---|---|---|
| GLUT1 | Erythrocytes, blood-brain barrier, fetal tissues | ~1 mM [12] | Basal glucose uptake; responsible for low-level glucose required to sustain respiration in all cells [4] |
| GLUT2 | Liver, pancreatic beta cells, renal tubular cells | 15-20 mM [12] | Bidirectional transport; high-capacity, low-affinity transporter; functions in glucose sensing [4] |
| GLUT3 | Neurons, placenta | ~1 mM [12] | High-affinity neuronal glucose transporter; ensures glucose supply even during low glucose availability [4] |
| GLUT4 | Adipose tissue, skeletal and cardiac muscle | ~5 mM [12] | Insulin-responsive transporter; responsible for regulated glucose storage [4] |
Kinetic Properties and Regulation
The transport kinetics of facilitated diffusion follows a saturable pattern characteristic of carrier-mediated processes. The glucose transporter alternates between two conformational states [11]. In the first conformation, a glucose-binding site faces the outside of the cell, where glucose binding induces a conformational change in the transporter so the glucose-binding site faces the interior, allowing release into the cytosol [11]. The affinity of different GLUT isoforms for glucose varies significantly, with Km values (the concentration at which transport is half-maximal) ranging from approximately 1 mM for high-affinity transporters like GLUT1 and GLUT3 to 15-20 mM for low-affinity transporters like GLUT2 [12].
Regulation of these transporters occurs through multiple mechanisms. While most GLUT transporters are constitutively active at the plasma membrane, GLUT4 represents a specialized case of regulated trafficking. Under basal conditions, GLUT4 resides primarily in cytoplasmic vesicles. Upon insulin binding to its receptor, a signaling cascade triggers the translocation of GLUT4-containing vesicles to the cell surface, dramatically increasing glucose uptake into muscle and adipose tissue [12]. This process represents a critical point of dysregulation in metabolic diseases like diabetes.
Secondary Active Transport: Coupled Energy Utilization
Sodium-Glucose Cotransport Mechanism
In contrast to facilitated diffusion, secondary active transport couples the movement of glucose against its concentration gradient to the facilitated diffusion of a second solute (usually an ion) down its electrochemical potential [13]. This mechanism is particularly important in epithelial absorption contexts, such as the intestinal lumen and renal tubules, where glucose must be extracted from low-concentration environments into the bloodstream [12].
The sodium-glucose cotransporters (SGLTs) exemplify this mechanism through a symport process, where both sodium and glucose are transported in the same direction across the membrane [12]. The established sodium gradient provides the driving force for this process. The Na+/K+ ATPase pump actively extrudes three sodium ions from the cell while importing two potassium ions, consuming ATP in the process and creating both a low intracellular sodium concentration and an electrochemical gradient favoring sodium entry [12] [14]. This gradient represents stored energy that SGLT proteins harness to co-transport glucose against its concentration gradient.
Table 2: Sodium-Glucose Cotransporters (SGLTs) in Mammalian Systems
| Transporter | Tissue Distribution | Sodium:Glucose Stoichiometry | Functional Role |
|---|---|---|---|
| SGLT1 | Small intestine (brush border), kidney (distal tubule) | 2:1 [12] | High-affinity, low-capacity glucose absorption; responsible for dietary glucose uptake |
| SGLT2 | Kidney (proximal tubule) | 1:1 [12] | Low-affinity, high-capacity glucose reabsorption; responsible for ~90% of renal glucose reabsorption |
Renal Glucose Reabsorption: A Case Study
The kidney provides a compelling physiological example of secondary active transport coordination. In the nephron, SGLT2 transporters located in the early proximal tubule reabsorb the majority of filtered glucose from the tubular lumen [12]. These transporters have a low affinity but high capacity for glucose, handling the bulk of glucose reabsorption when glucose concentrations are high. Further along the tubule, SGLT1 transporters with high affinity but low capacity recapture remaining glucose, ensuring minimal glucose loss in urine under normal physiological conditions [12]. The glucose transported into the epithelial cells then exits into the bloodstream via facilitated diffusion through GLUT2 transporters located on the basolateral membrane [12].
Experimental Methodologies for Studying Glucose Transport
Transport Kinetics and Inhibition Assays
Characterizing glucose transporter function requires specialized methodologies to quantify uptake rates and kinetic parameters. The patch clamp technique, developed by Erwin Neher and Bert Sakmann in 1976, enables the study of ion channel activity by using a micropipette with a tip diameter of about 1 μm to isolate a small patch of membrane, allowing the flow of ions through a single channel to be analyzed [11]. While particularly useful for studying ion channels, this technique can be adapted to study electrogenic transporters like SGLT that generate current during transport cycles.
For kinetic analysis, researchers often employ radiolabeled glucose analogs (e.g., 2-deoxy-D-[³H]glucose) to measure uptake rates over time under varying substrate concentrations. By measuring initial uptake rates at different glucose concentrations, researchers can determine Km and Vmax values using Michaelis-Menten kinetics. Specific inhibitors can further distinguish between transport mechanisms: phlorizin competitively inhibits SGLT transporters, while cytochalasin B blocks facilitative GLUT transporters.
Metabolic Flux Analysis
Understanding how transport mechanisms influence cellular energy production requires assessment of metabolic flux. Cellular respirometry assays, particularly using platforms like the Seahorse XF Analyzer, enable real-time measurement of oxygen consumption rate (OCR) and extracellular acidification rate (ECAR) as proxies for mitochondrial oxidative phosphorylation and glycolysis, respectively [15]. This approach allows researchers to correlate transport activity with downstream metabolic pathways.
In practice, cells are subjected to sequential injections of metabolic inhibitors: oligomycin (ATP synthase inhibitor), FCCP (mitochondrial uncoupler), and rotenone/antimycin A (electron transport chain inhibitors) [16]. The resulting OCR profile reveals key parameters of mitochondrial function, including basal respiration, ATP-linked respiration, proton leak, and spare respiratory capacity. Simultaneous ECAR measurements provide insight into glycolytic flux, creating a comprehensive picture of cellular bioenergetics.
Table 3: Key Research Reagents for Glucose Transport and Metabolism Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Transport Inhibitors | Phlorizin, Cytochalasin B | Distinguish between SGLT and GLUT-mediated transport mechanisms [12] |
| Metabolic Inhibitors | Oligomycin, FCCP, Rotenone, Antimycin A, 2-Deoxyglucose | Probe mitochondrial function and glycolytic capacity in respirometry assays [15] [16] |
| Labeled Tracers | 2-Deoxy-D-[³H]glucose, [¹⁴C]glucose | Quantify glucose uptake rates and metabolic fate |
| Imaging Tools | Mitochondrial dyes (e.g., TMRM, MitoTracker), GLUT-GFP constructs | Visualize subcellular localization of organelles and transporters |
Physiological Context and Research Implications
Neuronal Energetics and Glucose Transport
The brain's heavy reliance on glucose as a primary fuel source makes neuronal glucose transport a critical research area. Interestingly, neurons express primarily GLUT3, a high-affinity transporter (Km ~1 mM) that ensures sufficient glucose supply even during periods of low glucose availability [12] [4]. This is particularly important given that brain glucose concentrations typically range between 1-3 mM, significantly lower than standard cell culture media containing 25 mM glucose [15].
Recent research has revealed that this discrepancy in glucose concentration significantly impacts neuronal metabolism. Neurons cultured in standard hyperglycemic media (25 mM glucose) show heavy dependence on glycolysis for ATP production, contrary to the predominant reliance on oxidative phosphorylation observed in vivo [15]. In contrast, neurons cultured in more physiological glucose conditions (5 mM) demonstrate a more balanced dependence on glycolysis and mitochondrial oxidative phosphorylation, greater reserve mitochondrial respiration capacity, and increased mitochondrial population [15]. These findings highlight how transport mechanisms interface with downstream metabolic pathways and suggest that historical in vitro studies may have misrepresented neuronal energy metabolism.
Disease Connections and Therapeutic Targeting
Dysregulation of glucose transport mechanisms contributes to various pathological conditions. In diabetes, impaired GLUT4 translocation in response to insulin represents a fundamental defect in skeletal muscle and adipose tissue glucose uptake [12] [4]. Meanwhile, in cancer, many tumors exhibit upregulated GLUT1 expression, enabling enhanced glucose uptake to support aerobic glycolysis (the Warburg effect) and biomass production for rapid proliferation [4].
Therapeutic interventions have been developed to target specific transport mechanisms. SGLT2 inhibitors (e.g., canagliflozin, dapagliflozin) represent a recent class of diabetes drugs that block renal glucose reabsorption, promoting glucosuria and reducing blood glucose levels [12]. Research is also exploring modulators of GLUT expression and trafficking as potential therapeutic approaches for metabolic disorders and cancer.
Comparative Analysis and Research Integration
Side-by-Side Mechanistic Comparison
The fundamental differences between facilitated diffusion and secondary active transport for glucose entry can be summarized across multiple parameters:
- Energy Requirement: Facilitated diffusion operates passively without direct energy input, while secondary active transport indirectly consumes ATP via the maintenance of ion gradients [11] [12]
- Directionality: Facilitated diffusion is bidirectional, with net flow determined by concentration gradients; secondary active transport is typically unidirectional under physiological conditions [11] [13]
- Consequence of Transport: Facilitated diffusion equilibrates glucose concentrations across membranes; secondary active transport creates and maintains concentration gradients [11] [12]
- Tissue Distribution: Facilitated diffusion via GLUT transporters occurs in nearly all cell types; secondary active transport via SGLT is specialized for epithelial absorption [12] [4]
- Kinetic Properties: GLUT transporters exhibit Km values ranging from 1-20 mM depending on isoform; SGLT transporters generally have lower Km values, suited for extracting glucose from low-concentration environments [12]
Integrated View of Glucose Utilization for ATP Production
The interplay between glucose transport mechanisms and ATP production forms a coordinated system for cellular energy management. Glucose entry represents the first committed step in a metabolic cascade that culminates in ATP generation through glycolysis in the cytoplasm and oxidative phosphorylation in the mitochondria. The specific transport mechanism employed influences the rate and regulation of this process.
In cells utilizing facilitated diffusion, glucose uptake is primarily governed by extracellular glucose concentrations and the kinetic properties of the expressed GLUT isoforms. For instance, neurons with high GLUT3 expression can maintain consistent glucose uptake even during brief fluctuations in glucose availability, supporting their continuous high energy demands [4]. Conversely, in cells employing secondary active transport, glucose uptake is coupled to ion gradients that are actively maintained, allowing accumulation against concentration gradients but at the cost of indirect energy expenditure.
Diagram 1: Glucose Transport Mechanisms Comparison
The cellular entry of glucose via facilitated diffusion and secondary active transport represents a finely tuned system that matches uptake mechanisms to tissue-specific requirements. Facilitated diffusion through GLUT proteins provides efficient, regulated transport down concentration gradients, while secondary active transport via SGLT cotransporters enables active accumulation against concentration gradients at the expense of pre-established ion gradients. Understanding these mechanisms and their interface with downstream metabolic pathways for ATP production is essential for research on neuronal bioenergetics, metabolic diseases, and therapeutic development. The experimental methodologies outlined provide researchers with tools to dissect these processes in health and disease, offering insights for future investigations into cellular energy metabolism.
Diagram 2: Experimental Analysis of Glucose Metabolism
Glycolysis, also known as the Embden-Meyerhof-Parnas (EMP) pathway, is a universal metabolic pathway that serves as the foundational mechanism for glucose catabolism in virtually all organisms, from microbes to mammals [17] [18]. This evolutionarily ancient biochemical sequence occurs in the cytosol of cells and functions as the initial stage of cellular energy production, converting a single six-carbon glucose molecule into two three-carbon pyruvate molecules while generating a net yield of adenosine triphosphate (ATP) and reduced nicotinamide adenine dinucleotide (NADH) [18] [19]. For research scientists and drug development professionals, understanding the intricate regulation of this pathway is paramount, particularly given its central role in pathological conditions such as cancer (the Warburg effect) and metabolic disorders like type 2 diabetes [20] [21] [22].
The glycolytic sequence represents a critical interface between glucose uptake mechanisms and ATP production systems within the cell. Recent research has revealed that glycolytic enzymes can form self-organizing wave structures on the cell membrane and cortex, suggesting a previously unrecognized level of spatial organization that may locally enhance ATP production to fuel energy-intensive processes such as cell migration and macropinocytosis [22]. This compartmentalization challenges the traditional view of glycolysis as a purely cytosolic process and opens new avenues for therapeutic intervention in diseases characterized by aberrant metabolic states. Furthermore, exercise-stimulated glucose uptake demonstrates how glycolytic flux can be dramatically increased through mechanisms distinct from insulin signaling, preserving metabolic flexibility even in insulin-resistant states [21]. This review provides a comprehensive technical analysis of the glycolytic sequence, with particular emphasis on its regulatory mechanisms, experimental methodologies for flux quantification, and implications for drug discovery targeting metabolic diseases.
The Glycolytic Pathway: A Two-Phase Process
Glycolysis proceeds through ten enzyme-catalyzed reactions that can be conceptually divided into two distinct phases: the energy investment phase and the energy payoff phase [17] [18]. This division reflects the metabolic strategy of initial ATP expenditure to activate glucose, followed by energy recovery and net gain through substrate-level phosphorylation.
Phase 1: Energy Investment
The first phase of glycolysis prepares the glucose molecule for cleavage by phosphorylating and rearranging it into two interconvertible three-carbon sugars. This preparatory phase consumes two ATP molecules per glucose molecule [18] [23].
Step 1: Phosphorylation to Glucose-6-Phosphate - The enzyme hexokinase (in most tissues) or glucokinase (in liver and pancreatic β-cells) catalyzes the transfer of a phosphate group from ATP to glucose, forming glucose-6-phosphate (G6P) [18]. This reaction is physiologically irreversible and serves to trap glucose within the cell by adding a charged phosphate group that cannot easily cross the plasma membrane [20] [18].
Step 2: Isomerization to Fructose-6-Phosphate - Phosphoglucose isomerase converts the aldose sugar (G6P) to the ketose sugar fructose-6-phosphate (F6P) through an isomerization reaction [18]. This step prepares the molecule for the subsequent phosphorylation at carbon 1.
Step 3: Second Phosphorylation to Fructose-1,6-Bisphosphate - Phosphofructokinase-1 (PFK-1), a key regulatory enzyme, catalyzes the transfer of a second phosphate group from ATP to F6P, yielding fructose-1,6-bisphosphate (F1,6BP) [18]. This committed step of glycolysis is highly exergonic and represents the primary rate-limiting control point of the pathway.
Step 4: Aldol Cleavage - The enzyme fructose bisphosphate aldolase cleaves the six-carbon F1,6BP into two different three-carbon sugars: glyceraldehyde-3-phosphate (G3P) and dihydroxyacetone phosphate (DHAP) [18].
Step 5: Triose Phosphate Interconversion - Triosephosphate isomerase rapidly catalyzes the reversible isomerization of DHAP to G3P, ensuring both three-carbon products can proceed through the remainder of the pathway [18]. At this point, the first phase concludes with one glucose molecule yielding two molecules of G3P.
Phase 2: Energy Payoff
The second phase of glycolysis extracts energy through oxidation and substrate-level phosphorylation, generating ATP and NADH from the G3P molecules produced in the first phase [18] [19].
Step 6: Oxidation to 1,3-Bisphosphoglycerate - Glyceraldehyde-3-phosphate dehydrogenase catalyzes the first redox reaction of glycolysis, oxidizing G3P while simultaneously incorporating inorganic phosphate (Pi) to produce 1,3-bisphosphoglycerate (1,3-BPG) [18]. During this reaction, NAD+ is reduced to NADH, capturing high-energy electrons from the oxidized aldehyde group.
Step 7: First ATP Generation - Phosphoglycerate kinase facilitates the transfer of a high-energy phosphate group from 1,3-BPG to ADP, forming 3-phosphoglycerate (3-PG) and ATP [18]. This constitutes the first substrate-level phosphorylation event in glycolysis.
Step 8: Phosphate Group Migration - Phosphoglycerate mutase relocates the phosphate group from carbon 3 to carbon 2 of the glycerate backbone, converting 3-PG to 2-phosphoglycerate (2-PG) [18].
Step 9: Dehydration to Phosphoenolpyruvate - The enzyme enolase catalyzes the dehydration of 2-PG to form phosphoenolpyruvate (PEP), creating a high-energy enol phosphate bond [18].
Step 10: Second ATP Generation - Pyruvate kinase, another key regulatory enzyme, catalyzes the irreversible transfer of the phosphate group from PEP to ADP, generating pyruvate and ATP [18]. This final step completes the glycolytic sequence.
Table 1: Quantitative Input and Output of the Glycolytic Sequence
| Parameter | Input/Output | Quantity per Glucose Molecule |
|---|---|---|
| Input | Glucose | 1 |
| ATP | 2 | |
| NAD+ | 2 | |
| Inorganic Phosphate (Pi) | 2 | |
| ADP | 4 | |
| Output | Pyruvate | 2 |
| Net ATP | 2 | |
| NADH | 2 | |
| H₂O | 2 |
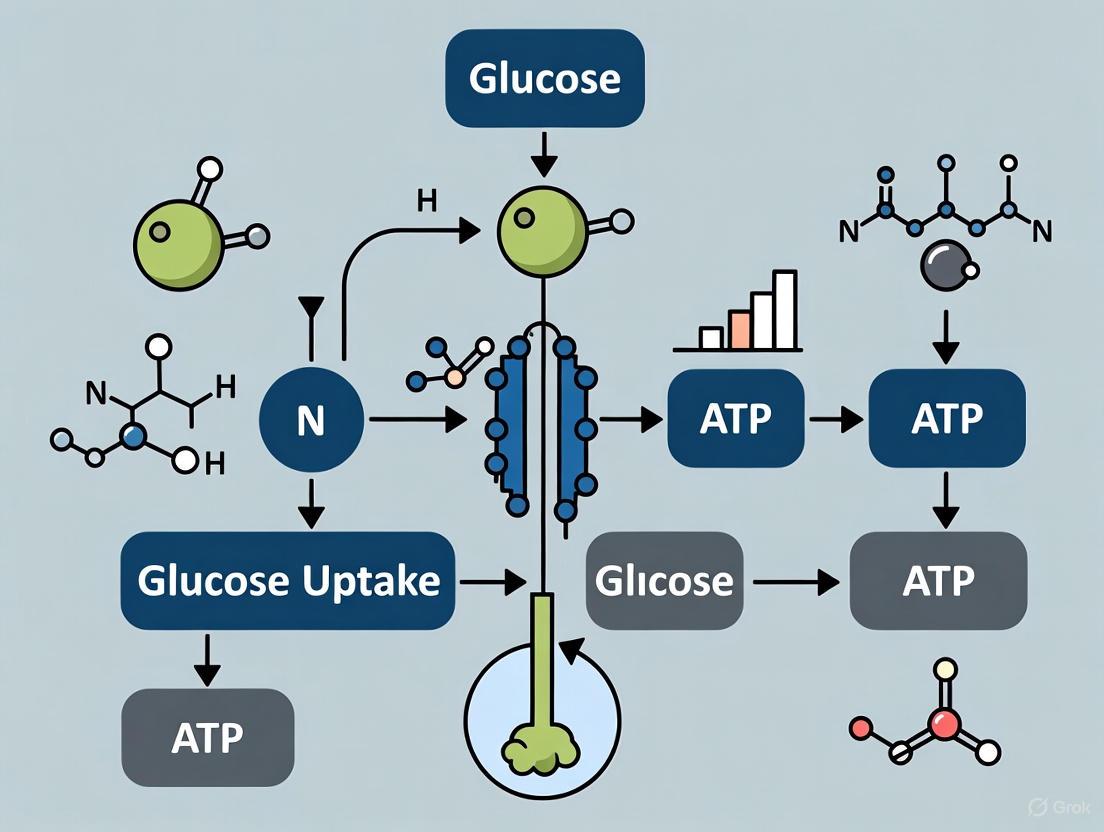
The following diagram illustrates the complete glycolytic pathway with its two distinct phases, key enzymes, and intermediate metabolites:
Diagram 1: The complete glycolytic pathway from glucose to pyruvate, showing energy investment and payoff phases, key enzymes, and cofactor utilization.
Metabolic Fate of Pyruvate and Regulation
Post-Glycolytic Pathways
Pyruvate, the end product of glycolysis, occupies a critical metabolic branch point whose fate depends on cellular conditions and organism type [17] [19]. Under aerobic conditions in most tissues, pyruvate is transported into the mitochondria where it undergoes oxidative decarboxylation to acetyl-CoA via the pyruvate dehydrogenase complex [20]. This acetyl-CoA then enters the citric acid cycle (Krebs cycle), generating additional NADH and FADH₂ molecules that drive oxidative phosphorylation to produce the majority of ATP (up to approximately 30 additional ATP molecules per glucose) [24] [19]. Conversely, under anaerobic conditions or in tissues with limited mitochondrial capacity, pyruvate is reduced to lactate through lactic acid fermentation, regenerating NAD+ from NADH to allow glycolysis to continue in the absence of oxygen [18] [19]. This anaerobic pathway yields only the net 2 ATP molecules from glycolysis itself but is crucial for maintaining energy production during oxygen debt or in cells like erythrocytes that lack mitochondria entirely [18].
Allosteric and Hormonal Regulation
Glycolytic flux is tightly regulated through multiple mechanisms to match cellular energy demands with nutrient availability [18]. The three key irreversible steps catalyzed by hexokinase/glucokinase, phosphofructokinase-1 (PFK-1), and pyruvate kinase serve as primary regulatory nodes through allosteric effectors and hormonal signaling [18].
Phosphofructokinase-1 (PFK-1) represents the most important control point, inhibited by high levels of ATP and citrate (indicating ample energy and biosynthetic precursors), and activated by AMP and fructose-2,6-bisphosphate (signaling energy depletion) [18]. Fructose-2,6-bisphosphate, produced by phosphofructokinase-2 (PFK-2), serves as a potent allosteric activator whose concentration is regulated by insulin and glucagon, thus linking glycolytic flux to hormonal status [18].
Pyruvate kinase, the final key regulatory enzyme, is allosterically inhibited by ATP and activated by fructose-1,6-bisphosphate, implementing a feed-forward activation mechanism that ensures coordinated flux through the latter stages of glycolysis [18]. The liver isoform is also regulated through phosphorylation by glucagon-activated protein kinase A, which decreases enzyme activity during fasting states [18].
Hexokinase is inhibited by its product glucose-6-phosphate, providing feedback regulation when glycolytic intermediates accumulate [18]. The liver-specific glucokinase isoform has a higher Km for glucose and is not subject to product inhibition, allowing the liver to respond to postprandial glucose elevations [18].
The following diagram illustrates the complex regulatory network controlling glycolytic flux:
Diagram 2: Regulatory network of glycolysis showing allosteric inhibition/activation and hormonal control mechanisms.
Table 2: Key Regulatory Enzymes in Glycolysis and Their Modulators
| Enzyme | Activators | Inhibitors | Physiological Significance |
|---|---|---|---|
| Hexokinase | - | Glucose-6-phosphate | Prevents accumulation of glycolytic intermediates when downstream metabolism is limited [18] |
| Glucokinase | Insulin (induction) | - | Liver enzyme with high Km allows response to postprandial glucose elevation [18] |
| Phosphofructokinase-1 (PFK-1) | AMP, Fructose-2,6-bisphosphate, ADP | ATP, Citrate, H+ | Primary rate-controlling step; inhibited when energy and biosynthetic precursors are abundant [18] |
| Pyruvate Kinase | Fructose-1,6-bisphosphate | ATP, Alanine, Glucagon (via PKA phosphorylation) | Coordinates final step with upstream flux; reduced activity during fasting [18] |
Research Methodologies and Experimental Approaches
Stable Isotope Tracing for Metabolic Flux Analysis
Advanced techniques for quantifying glycolytic flux have become essential tools in metabolic research, particularly for investigating pathological states such as cancer metabolism [25]. Stable isotope tracing represents a powerful methodology that enables researchers to track the fate of individual atoms through the glycolytic pathway and connected metabolic networks. In this approach, cells or organisms are fed substrates labeled with stable isotopes (e.g., ¹³C-glucose), and the incorporation of these labels into downstream metabolites is quantified using mass spectrometry or nuclear magnetic resonance (NMR) spectroscopy [25]. This technique allows researchers to determine relative flux through various metabolic pathways, identify alternative routing of carbons, and detect compartmentalized metabolite pools. For Crabtree-positive yeasts and cancer cells, protocols have been developed that combine ¹³C-glucose labeling with computational modeling to quantitatively assess glycolytic flux and its contribution to central carbon metabolism [25]. The resulting flux maps provide unprecedented insight into how metabolic networks are rewired in disease states and in response to therapeutic interventions.
Assessing Glycolytic Function in Physiological Contexts
In mammalian systems, particularly in research on exercise metabolism and insulin resistance, several standardized protocols have been developed to assess glycolytic capacity and regulation [21]. The oral glucose tolerance test (OGTT) measures the body's ability to clear glucose from the bloodstream following an oral glucose load, providing insight into whole-body glucose metabolism and insulin sensitivity [20]. For more reductionist approaches in cell culture systems, glycolytic rate can be determined by measuring extracellular acidification rate (ECAR) using specialized analytical instrumentation, as lactic acid production from glycolysis lowers the pH of the media [21]. Additional biochemical assays include measuring lactate accumulation, glucose consumption, and enzyme activities in cell or tissue extracts. For exercise studies, measurements of arterial-venous glucose differences across working muscles, combined with stable isotope tracers, have revealed that skeletal muscle glucose uptake can increase by up to 50-fold during physical activity through mechanisms that remain functional even in insulin-resistant states [21].
The following diagram illustrates a generalized workflow for experimental assessment of glycolytic function:
Diagram 3: Generalized experimental workflow for assessing glycolytic function using metabolic measurements and stable isotope tracing.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Key Research Reagent Solutions for Glycolysis Research
| Research Tool | Function/Application | Specific Examples/Context |
|---|---|---|
| Stable Isotope Tracers | Tracking metabolic flux through glycolysis and interconnected pathways | ¹³C-glucose for mass spectrometry-based flux analysis [25] |
| GLUT Transporters | Studying glucose uptake mechanisms; tissue-specific expression patterns | GLUT4 (adipocytes, muscle), GLUT1 (RBCs, blood-brain barrier) [18] |
| Enzyme Inhibitors | Probing specific steps in glycolytic pathway; potential therapeutic agents | 2-deoxyglucose (hexokinase inhibitor), Oxamate (LDH inhibitor) |
| Glycolytic Enzymes (Tagged) | Visualizing subcellular localization and dynamics | GFP-tagged aldolase, PFK for live-cell imaging of wave dynamics [22] |
| Metabolic Phenotyping Assays | Measuring glycolytic output and capacity | Extracellular acidification rate (ECAR), lactate production assays [21] |
| Allosteric Modulators | Studying regulatory mechanisms of key control points | Fructose-2,6-bisphosphate (PFK-1 activator) [18] |
Implications for Disease and Therapeutic Development
The glycolytic sequence represents more than just a core metabolic pathway—it is a dynamic, highly regulated system whose dysfunction underpins numerous pathological conditions. In cancer biology, the Warburg effect (aerobic glycolysis) describes the propensity of cancer cells to favor glycolysis over oxidative phosphorylation even in oxygen-rich environments [22]. Recent research has revealed that this metabolic reprogramming may be facilitated by the self-organizing wave behavior of glycolytic enzymes at the cell cortex, which creates localized compartments of enhanced glycolytic activity that fuel invasive behaviors [22]. Specifically, studies across human mammary epithelial and other cancer cell lines with increasing metastatic potential demonstrate that wave activity and glycolytic ATP levels increase in parallel, suggesting a mechanistic link between spatial organization of glycolysis and cancer progression [22].
In metabolic diseases, particularly type 2 diabetes, impaired glucose metabolism results from defects in both insulin signaling and cellular glucose utilization [20] [21]. Notably, exercise-stimulated glucose uptake occurs through mechanisms distinct from insulin signaling and remains functional in insulin-resistant muscle, highlighting glycolysis as a therapeutic target for bypassing insulin resistance [21]. Research has shown that exercise recruits multiple redundant signaling pathways—sensing either alterations in the intracellular metabolic milieu (mediated by AMPK) or mechanical stress (partly mediated by RAC1)—to increase glucose transport and glycolytic flux [21]. This redundancy ensures maintenance of muscle energy supply during physical activity and provides multiple potential intervention points for restoring metabolic health.
The comprehensive understanding of glycolytic regulation and the development of sophisticated research methodologies for assessing metabolic flux have positioned this ancient pathway as a promising target for therapeutic intervention across a spectrum of diseases. From small molecule inhibitors targeting specific glycolytic enzymes in cancer to exercise mimetics that activate glucose uptake in metabolic disease, the continued elucidation of glycolytic mechanisms promises to yield novel approaches for manipulating cellular metabolism in human disease.
The complete oxidation of glucose is the cornerstone of aerobic energy metabolism, with the majority of its potential energy harvested not in glycolysis but within the mitochondrion. While glycolysis breaks down glucose into pyruvate in the cytosol for a net gain of two ATP molecules, the subsequent orchestrated processes of the Tricarboxylic Acid (TCA) cycle and oxidative phosphorylation are required to unleash the full energy yield, producing more than 30 additional ATP molecules per glucose [26] [20]. This mitochondrial phase of glucose catabolism is not merely an energy-generating pathway; it is a critical hub of cellular signaling and metabolism, and its dysregulation is implicated in a spectrum of diseases, from diabetes to neurodegenerative disorders. Understanding the precise mechanisms of the TCA cycle and oxidative phosphorylation is therefore paramount for research aimed at modulating cellular energy status for therapeutic benefit.
The Tricarboxylic Acid (TCA) Cycle: A Central Metabolic Hub
The TCA cycle, also known as the Krebs or citric acid cycle, serves as the final common pathway for the oxidation of fuel molecules—carbohydrates, fatty acids, and amino acids. In eukaryotic cells, it is localized to the mitochondrial matrix.
Sequential Enzymatic Steps and Key Outputs
The cycle begins when acetyl-CoA, derived from pyruvate (the end-product of glycolysis) or fatty acid beta-oxidation, condenses with oxaloacetate. This reaction, catalyzed by citrate synthase, forms citrate and initiates a sequence of eight enzymatic steps that regenerate oxaloacetate [27] [28]. The cycle results in the complete oxidation of the acetyl group to two molecules of CO₂ and the generation of high-energy electron carriers.
Table 1: Enzymatic Steps and Outputs of the TCA Cycle
| Step | Reaction | Enzyme | Key Products (per acetyl-CoA) |
|---|---|---|---|
| 1 | Acetyl-CoA + Oxaloacetate → Citrate | Citrate synthase | - |
| 2 | Citrate Isocitrate | Aconitase | - |
| 3 | Isocitrate → α-Ketoglutarate | Isocitrate dehydrogenase | 1 NADH, 1 CO₂ |
| 4 | α-Ketoglutarate → Succinyl-CoA | α-Ketoglutarate dehydrogenase | 1 NADH, 1 CO₂ |
| 5 | Succinyl-CoA → Succinate | Succinyl-CoA synthetase | 1 GTP (or ATP) |
| 6 | Succinate → Fumarate | Succinate dehydrogenase | 1 FADH₂ |
| 7 | Fumarate → Malate | Fumarase | - |
| 8 | Malate → Oxaloacetate | Malate dehydrogenase | 1 NADH |
For each molecule of glucose, which yields two acetyl-CoA molecules, the net output of the TCA cycle is doubled: six NADH, two FADH₂, two GTP (or ATP), and four CO₂ [27] [28]. The GTP produced by succinyl-CoA synthetase can be readily converted to ATP by nucleoside-diphosphate kinase [28].
Anaplerotic and Cataplerotic Functions
Beyond energy production, the TCA cycle provides critical precursors for biosynthetic pathways, a function termed "cataplerosis." Key intermediates are siphoned off for processes like gluconeogenesis (oxaloacetate), fatty acid synthesis (citrate), and heme synthesis (succinate) [27]. To maintain cycle function, these depleted intermediates must be replenished via "anaplerotic" reactions, such as the carboxylation of pyruvate to form oxaloacetate [29].
Regulatory Mechanisms
The TCA cycle is exquisitely regulated by substrate availability, product inhibition, and allosteric effectors to match cellular energy demands. Key control points include:
- Citrate synthase, inhibited by ATP and citrate.
- Isocitrate dehydrogenase, the rate-limiting enzyme, which is allosterically stimulated by ADP and inhibited by NADH and ATP.
- α-Ketoglutarate dehydrogenase, inhibited by its products, NADH and succinyl-CoA, and by high ATP levels [27] [28].
This regulatory network ensures the cycle slows when cellular energy charge is high (high ATP/ADP and NADH/NAD⁺ ratios) and accelerates when energy demand increases.
Oxidative Phosphorylation: Chemiosmotic Coupling and ATP Synthesis
The primary role of the TCA cycle is to generate reducing equivalents in the form of NADH and FADH₂. These electron carriers donate electrons to the electron transport chain (ETC), fueling the process of oxidative phosphorylation, which generates the vast majority of cellular ATP [26].
The Electron Transport Chain
The ETC consists of four protein complexes (I-IV) embedded in the inner mitochondrial membrane, along with two mobile electron carriers, coenzyme Q (ubiquinone) and cytochrome c [26] [30].
- Complex I (NADH-CoQ oxidoreductase): Accepts electrons from NADH and transfers them to coenzyme Q, coupling this transfer to the pumping of four protons from the matrix to the intermembrane space [30].
- Complex II (Succinate-CoQ oxidoreductase): Catalyzes the oxidation of succinate to fumarate in the TCA cycle, transferring electrons via FADH₂ to coenzyme Q. This step is not coupled to proton pumping [26].
- Complex III (CoQ-cytochrome c oxidoreductase): Transfers electrons from reduced coenzyme Q to cytochrome c, pumping four protons in the process [26].
- Complex IV (Cytochrome c oxidase): Transfers electrons from cytochrome c to molecular oxygen (O₂), the final electron acceptor, forming water. This complex pumps two protons across the membrane [26].
Table 2: Proton and ATP Yield from Electron Carriers
| Electron Carrier | Entry Point | Protons Pumped | ~ATP Yield (Theoretical Max) |
|---|---|---|---|
| NADH | Complex I | 10 H⁺ (4 from I, 4 from III, 2 from IV) | 2.5 ATP |
| FADH₂ | Complex II | 6 H⁺ (0 from II, 4 from III, 2 from IV) | 1.5 ATP |
Chemiosmotic Coupling and ATP Synthase
The energy released from electron flow through the ETC is used to pump protons (H⁺) from the mitochondrial matrix to the intermembrane space. This establishes an electrochemical gradient, or proton-motive force, with both a chemical (pH) gradient and an electrical (membrane potential) component [26] [30].
ATP synthase (Complex V) harnesses this stored energy. As protons flow back into the matrix through a channel in the F₀ subunit of ATP synthase, the energy drives the rotation of part of the complex. This mechanical energy is coupled to the synthesis of ATP from ADP and inorganic phosphate (Pᵢ) in the catalytic F₁ subunit [26]. The flow of approximately four protons is required for the synthesis of one ATP molecule [26].
Integrating the outputs of glycolysis, the pyruvate dehydrogenase complex, the TCA cycle, and oxidative phosphorylation provides the total ATP yield from one molecule of glucose.
Table 3: Theoretical Maximum ATP Yield from Complete Glucose Oxidation
| Metabolic Process | ATP Yield (Net) | Notes |
|---|---|---|
| Glycolysis | 2 ATP | Substrate-level phosphorylation |
| Pyruvate Dehydrogenase | 0 ATP | Produces 2 NADH (cytosolic) |
| TCA Cycle (2 turns) | 2 GTP | Substrate-level phosphorylation; GTP = ATP |
| 6 NADH | From 2 acetyl-CoA | |
| 2 FADH₂ | From 2 acetyl-CoA | |
| Oxidative Phosphorylation | ||
| 2 NADH (Glycolysis) | 5 ATP | ~2.5 ATP/NADH via malate-aspartate shuttle |
| 2 NADH (PDH) | 5 ATP | ~2.5 ATP/NADH |
| 6 NADH (TCA) | 15 ATP | ~2.5 ATP/NADH |
| 2 FADH₂ (TCA) | 3 ATP | ~1.5 ATP/FADH₂ |
| Total | 32 ATP | Theoretical maximum |
This theoretical yield of 32 ATP per glucose is a maximum; in practice, the yield is lower due to proton leakage and the cost of transporting metabolites across membranes [26] [30].
Research Methodologies and Experimental Protocols
Studying mitochondrial function requires a multidisciplinary approach to dissect the integrated processes of the TCA cycle and oxidative phosphorylation.
Isolating Functional Mitochondria
Protocol: Mitochondrial Isolation from Rodent Skeletal Muscle
- Tissue Homogenization: Euthanize the animal and rapidly excise skeletal muscle (e.g., gastrocnemius). Mince the tissue in ice-cold isolation buffer (containing 100 mM sucrose, 50 mM KCl, 5 mM EDTA, 50 mM Tris-HCl, pH 7.4) to preserve organelle integrity.
- Differential Centrifugation:
- Centrifuge the homogenate at 800 × g for 10 minutes at 4°C to pellet nuclei and cellular debris.
- Transfer the supernatant to a new tube and centrifuge at 10,000 × g for 15 minutes at 4°C. The resulting pellet contains the intact mitochondrial fraction.
- Washing: Gently resuspend the mitochondrial pellet in fresh isolation buffer and repeat the high-speed centrifugation step to wash the mitochondria.
- Protein Quantification: Resuspend the final mitochondrial pellet in a small volume of buffer and determine protein concentration using a Bradford or BCA assay for normalization in subsequent functional assays.
Measuring Oxygen Consumption
The rate of oxygen consumption is a direct indicator of ETC activity and overall mitochondrial function. This is typically measured using a Clark-type oxygen electrode in a sealed, stirred chamber maintained at 37°C.
- Basal Respiration: Add isolated mitochondria to the chamber containing respiration buffer. Record the oxygen consumption rate (State 2 respiration).
- ADP-Stimulated Respiration: Add a known amount of ADP. In the presence of excess substrates (e.g., pyruvate and malate), mitochondria rapidly consume oxygen to phosphorylate ADP to ATP (State 3 respiration). This measures the maximum phosphorylating capacity.
- Uncoupled Respiration: After ADP is depleted, the respiration rate slows (State 4). Addition of an uncoupler like FCCP dissipates the proton gradient, forcing the ETC to operate at maximum velocity independent of ATP synthase, revealing the electron transport system's intrinsic capacity.
Assessing Membrane Potential and ROS Production
- Membrane Potential (ΔΨm): Fluorescent dyes like Tetramethylrhodamine, Methyl Ester (TMRM) are accumulated by energized mitochondria in a membrane potential-dependent manner. A decrease in fluorescence indicates depolarization of ΔΨm, a key parameter of mitochondrial health [31].
- Reactive Oxygen Species (ROS) Production: The ETC is a major source of ROS. Dihydroethidium (DHE) or MitoSOX Red (targeted to mitochondria) can be used to detect superoxide production. Fluorescence intensity is proportional to ROS levels.
The Researcher's Toolkit: Essential Reagents and Assays
Table 4: Key Research Reagents for Mitochondrial Function Analysis
| Reagent / Assay | Function / Target | Research Application |
|---|---|---|
| Rotenone | Inhibits Complex I | Used to probe the contribution of NADH-linked substrates to respiration. |
| Antimycin A | Inhibits Complex III | Halts electron flow, allowing measurement of upstream ETC function and non-mitochondrial oxygen consumption. |
| Oligomycin | Inhibits ATP Synthase | Induces State 4 respiration; used to measure proton leakage and calculate coupling efficiency. |
| FCCP | Uncoupler | Dissipates the proton gradient, unmasking maximum ETC capacity. |
| TMRM / JC-1 | ΔΨm-sensitive dyes | Quantitative and qualitative assessment of mitochondrial membrane potential by fluorescence. |
| Seahorse XF Analyzer | Live-cell metabolic profiling | Platform for simultaneously measuring oxygen consumption rate (OCR) and extracellular acidification rate (ECAR) in live cells. |
| Antibodies (Total/OxPhos) | OXPHOS complexes | Western blotting to determine the protein expression levels of individual ETC complexes. |
Integrated View: From Glucose Uptake to ATP Production
Glucose metabolism is a continuous pathway from the cell surface to the mitochondrial matrix. Insulin or exercise-stimulated signaling pathways, such as those involving AMPK and CaMK, promote the translocation of the GLUT4 glucose transporter to the plasma membrane, allowing glucose entry [21] [32]. After glycolysis, the resulting pyruvate is actively transported into the mitochondrion. There, it is decarboxylated to acetyl-CoA, which enters the TCA cycle. The cycle's reduction of NAD⁺ to NADH and FAD to FADH₂ provides the high-energy electrons that drive the ETC. The chemiosmotic coupling of electron transport to ATP synthesis ultimately transforms the chemical energy of glucose into the universal energy currency, ATP. This integrated system allows the cell to adapt to energetic demands, and its dysregulation is a hallmark of metabolic disease, making its components prime targets for therapeutic intervention.
The precise regulation of glucose uptake and utilization is fundamental to cellular energy homeostasis and is governed by a complex interplay of hormonal signals and allosteric mechanisms. This whitepaper delineates the sophisticated regulatory networks involving insulin, glucagon, and key metabolites such as citrate and fatty acids in controlling glucose metabolism for ATP production. We synthesize recent advances demonstrating how hormonal signaling pathways—insulin via its receptor and AKT cascade, glucagon through cAMP-mediated processes—orchestrate glucose transporter trafficking and enzymatic activity. Furthermore, we explore emerging paradigms of allosteric control, including metabolite transporter interactions (NaCT/GLUT) and fatty-acid-mediated modulation of insulin receptor phosphorylation via CD36-Fyn kinetics. Designed for researchers and drug development professionals, this review integrates structural, functional, and pharmacological insights with experimental protocols and reagent solutions to support ongoing mechanistic investigations and therapeutic innovation in metabolic diseases.
Glucose serves as the primary metabolic fuel for mammals, and its regulated uptake and conversion to ATP are critical for cellular function [20]. The hormonal systems of insulin and glucagon provide a classic endocrine framework for maintaining blood glucose homeostasis, while allosteric regulation by metabolites allows for rapid, localized fine-tuning of metabolic fluxes [33] [34]. Insulin, secreted by pancreatic β-cells in response to elevated blood glucose, promotes glucose uptake into muscle and adipose tissue via the GLUT4 transporter and stimulates glycogenesis, thereby lowering blood glucose [34]. Conversely, glucagon, released from pancreatic α-cells during hypoglycemia, elevates blood glucose by triggering hepatic glycogenolysis and gluconeogenesis [35].
Beyond this canonical hormonal balance, recent research reveals intricate crosstalk at the molecular level. Allosteric regulation, where molecules bind to regulatory sites on proteins to modulate their activity, is a key mechanism. Metabolites including citrate and fatty acids can directly influence transporter function and insulin signaling efficacy [36] [37]. For instance, the liver citrate transporter NaCT interacts with glucose transporters to synchronize nutrient uptake, while the fatty acid transporter CD36 forms complexes with the insulin receptor to enhance its tyrosine phosphorylation [36] [37]. Disruptions in these pathways are hallmarks of metabolic diseases such as Type 2 Diabetes Mellitus (T2DM), characterized by insulin resistance and dysregulated glucagon secretion [20] [35]. This whitepaper delves into the molecular mechanics of these regulatory systems, providing a technical foundation for research aimed at diagnosing and treating metabolic disorders.
Hormonal Regulation of Glucose Metabolism
Insulin Signaling and Glucose Utilization
The insulin signaling cascade begins with insulin binding to its transmembrane receptor (IR), a receptor tyrosine kinase, leading to its autophosphorylation and activation [38]. The activated IR then phosphorylates direct substrates, primarily Insulin Receptor Substrate (IRS) proteins, which recruit and activate phosphoinositide 3-kinase (PI3K) [38]. PI3K catalyzes the production of phosphatidylinositol-3,4,5-triphosphate (PIP3) from phosphatidylinositol-4,5-bisphosphate (PIP2), a critical step that recruits downstream effectors like phosphoinositide-dependent kinase 1 (PDK1) and Protein Kinase B (AKT) to the plasma membrane [38]. AKT activation is a central node in metabolic signaling, promoting the translocation of the glucose transporter GLUT4 from intracellular vesicles to the cell surface via phosphorylation and inactivation of proteins such as RAB GAP AS160 (TBC1D4) [38]. This results in a tenfold increase in glucose uptake into muscle and adipose cells [38]. AKT also stimulates glycogen synthesis and inhibits gluconeogenesis, thereby coordinating a reduction in blood glucose levels [38]. Defects in this pathway, such as impaired IR tyrosine phosphorylation or reduced AKT activity, are pivotal in the development of insulin resistance [37] [38].
Table 1: Key Effectors in the Insulin Signaling Pathway
| Protein/Component | Function in Signaling | Downstream Metabolic Effect |
|---|---|---|
| Insulin Receptor (IR) | Receptor tyrosine kinase; autophosphorylates upon insulin binding | Initiates the metabolic signaling cascade |
| IRS1/2 | Docking proteins for IR; phosphorylated by IR | Recruits and activates PI3K |
| PI3K | Kinase that converts PIP2 to PIP3 | Generates lipid second messenger for AKT recruitment |
| AKT (PKB) | Serine/threonine kinase; key signaling node | Promotes GLUT4 translocation, glycogen synthesis, inhibits gluconeogenesis |
| AS160 (TBC1D4) | RAB GAP; inactivated by AKT phosphorylation | Releases inhibition on GLUT4 vesicle trafficking |
| GLUT4 | Insulin-responsive glucose transporter | Facilitates glucose uptake into muscle and adipose tissue |
Glucagon Signaling and Hepatic Glucose Output
Glucagon acts primarily on the liver to elevate blood glucose levels during fasting or stress. It binds to glucagon receptors, which are G-protein coupled receptors (GPCRs) primarily linked to Gs proteins [35]. This binding activates adenylate cyclase (AC), increasing intracellular cyclic adenosine monophosphate (cAMP) levels. cAMP then activates Protein Kinase A (PKA), which in turn phosphorylates and activates key enzymes like phosphorylase kinase. This cascade culminates in the stimulation of glycogenolysis (breakdown of glycogen to glucose) and gluconeogenesis (synthesis of glucose from non-carbohydrate precursors like amino acids) [35] [34]. Glucagon also regulates amino acid metabolism and lipid oxidation, highlighting its role as a broader regulator of energy balance [35]. In diabetes, dysregulated glucagon secretion—hyperglucagonemia—and hepatic "glucagon resistance" contribute significantly to fasting and postprandial hyperglycemia, making the glucagon pathway a target for therapeutic intervention [35].
Diagram 1: Glucagon signaling pathway in hepatocytes, showing key steps from receptor binding to glucose output.
Allosteric Regulation by Metabolites
Metabolite Transporter Interactions: NaCT and GLUT
Emerging evidence positions metabolite transporters not merely as passive conduits but as active regulators of cellular metabolism through allosteric interactions. A seminal discovery is the functional coordination between the sodium-coupled citrate transporter (NaCT, SLC13A5) and glucose transporters (GLUTs) in hepatocytes [36]. This interaction forms a "first-line" metabolic pathway that synchronizes the uptake of citrate and glucose in response to nutrient availability. During glucose starvation, citrate uptake increases, potentially to substitute for glucose in energy production. Upon glucose re-saturation, this increased uptake is halted. Inhibition of NaCT disrupts this synchronization and paradoxically elevates glucose uptake, suggesting that NaCT exerts an allosteric-like, reciprocal regulation on GLUT function [36]. This transceptor interaction is mediated by a specific region, the H4c helix on transmembrane domain 4 of NaCT, and controls cellular bioenergetics by coordinating the influx of two key carbon sources [36].
CD36-Fyn Kinase Modulation of the Insulin Receptor
The fatty acid transporter CD36 provides another layer of allosteric regulation by directly influencing the insulin receptor (IR). CD36 forms a complex with IR and the Src-family kinase Fyn, which promotes Fyn-mediated tyrosine phosphorylation of IR, thereby enhancing its activity and the subsequent recruitment of downstream effectors like PI3K [37]. This mechanism is crucial for optimal insulin responsiveness in skeletal muscle. Notably, this enhancement is sensitive to the type of dietary fatty acids: saturated fatty acids rapidly disrupt the CD36-Fyn interaction, suppressing IR phosphorylation, while unsaturated fatty acids are neutral or stimulatory [37]. This represents a nutrient-sensing, allosteric mechanism where metabolites (fatty acids) directly modulate a key hormonal signaling pathway. Genetically determined low levels of CD36 in muscle are linked to impaired glucose disposal and a higher incidence of type 2 diabetes, underscoring its pathophysiological relevance [37].
Table 2: Allosteric Regulators of Glucose Metabolic Pathways
| Allosteric Regulator | Molecular Target | Effect on Target/Pathway | Physiological Outcome |
|---|---|---|---|
| Saturated Fatty Acids | CD36-Fyn-IR complex | Dissociates complex, suppresses IR phosphorylation [37] | Contributes to insulin resistance |
| Citrate | Phosphofructokinase-1 (PFK-1) | Allosteric inhibitor [36] | Slows glycolysis when TCA cycle is full |
| Extracellular Citrate (via NaCT) | GLUT transporters | Reciprocally regulates transport function [36] | Synchronizes glucose/citrate uptake for energy management |
| Glucose (D-Glucose) | GLUT1 transporter | Accelerates exchange flux (allosteric accelerator) [39] | Increases transport efficiency |
Experimental Methodologies for Investigating Regulation
Investigating Insulin Receptor Phosphorylation and Interaction
Protocol: Co-immunoprecipitation and Proximity Ligation Assay (PLA) for CD36-IR Complex This protocol is used to demonstrate the physical and functional interaction between CD36 and the Insulin Receptor [37].
- Cell Culture and Treatment: Use primary-derived human skeletal muscle myotubes (HSMMs) or CHO cells stably expressing human IR and CD36. Serum-starve cells for 16 hours before treatment. Pre-treat cells with saturated (e.g., palmitate) or unsaturated (e.g., oleate) fatty acids complexed with BSA (2:1 ratio) for 15 minutes, followed by insulin stimulation (e.g., 100 nM) for a defined period (e.g., 10-30 minutes) [37].
- Cell Lysis: Lyse cells in ice-cold lysis buffer (e.g., 20 mM Tris-HCL pH 7.5, 150 mM NaCl, 1% Triton X-100, 60 mM octyl β-d-glucopyranoside, plus protease and phosphatase inhibitors) for 30-60 minutes. Clear lysates by centrifugation at 10,000g for 10 minutes [37].
- Co-immunoprecipitation (Co-IP): Determine protein concentration of the supernatant. Incubate lysates with an antibody against CD36 or IR overnight at 4°C. Add Protein A/G beads for 2-4 hours to capture the immune complexes. Wash beads extensively with lysis buffer to remove non-specifically bound proteins [37].
- Immunoblotting: Elute proteins from beads, separate by SDS-PAGE, and transfer to a membrane. Probe the membrane with antibodies against phospho-tyrosine, IRβ, and CD36 to assess interaction and phosphorylation status [37].
- Proximity Ligation Assay (In Situ): For visual confirmation of protein complexes in cells or tissue sections. Culture cells on coverslips, treat, and then fix with ice-cold methanol. Block and incubate with primary antibodies against CD36 and IRβ overnight. Follow the Duolink PLA kit instructions: add PLUS and MINUS PLA probes, ligate, and amplify with a fluorescent DNA circle. Mount and image using a fluorescence microscope. Red fluorescent spots indicate close proximity (<40 nm) of CD36 and IR [37].
Synchronized Metabolite Transport Assay
Protocol: Measuring Synchronized Citrate and Glucose Uptake in Hepatocytes This protocol assesses the coordinated transport of citrate and glucose via NaCT and GLUT [36].
- Primary Hepatocyte Isolation and Culture: Isolate primary mouse hepatocytes or use human hepatocyte lines (e.g., THLE2, HepG2). Culture cells in appropriate media [36].
- Glucose Starvation and Re-saturation: Subject cells to glucose-free medium for varying periods (4, 6, 8, 10 hours) to simulate starvation. For re-saturation, add glucose back to the medium for set times (30, 120, 240 minutes) after an 8-hour fast [36].
- Radiolabeled Uptake Measurement:
- Citrate Uptake: Incubate cells with ³H-citrate for a set time (e.g., 15 minutes). Terminate the reaction by washing with ice-cold PBS. Solubilize cells and measure radioactivity by liquid scintillation counting [36].
- Glucose Uptake: Similarly, measure the uptake of ³H-2-deoxyglucose (³H-2-DG), a non-metabolizable glucose analog. Incubate cells with ³H-2-DG, wash extensively with cold PBS containing excess unlabeled 2-DG, and count radioactivity [36].
- Pharmacological Inhibition: To probe NaCT's role, repeat uptake measurements in the presence of a specific NaCT inhibitor (e.g., BI01383298) across a range of concentrations. This will demonstrate the dependency of synchronized transport on NaCT function [36].
- Data Analysis: Normalize uptake counts to total cellular protein. Plot uptake rates against starvation/re-saturation time or inhibitor concentration to visualize synchronization and its disruption.
Diagram 2: Experimental workflow for studying hormonal and allosteric regulation of glucose metabolism.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Research on Metabolic Regulation
| Reagent / Tool | Function / Specificity | Example Application |
|---|---|---|
| CD36 siRNA | Silences CD36 gene expression | Investigating CD36's role in insulin receptor signaling and glucose uptake [37] |
| NaCT Inhibitor (BI01383298) | Potent and specific inhibitor of the SLC13A5 citrate transporter | Probing the role of citrate transport in synchronized glucose/citrate uptake and cellular bioenergetics [36] |
| ³H-2-Deoxyglucose (2-DG) | Non-metabolizable glucose analog for tracing uptake | Measuring rates of glucose transporter activity [37] [36] |
| ³H-Citrate | Radiolabeled citrate for transport studies | Quantifying citrate uptake via NaCT and other transporters [36] |
| Phospho-specific Antibodies | Detect phosphorylated proteins (e.g., p-Tyrosine, p-AKT) | Assessing activation status of insulin signaling pathways [37] |
| Proximity Ligation Assay (PLA) Kit | Visualizes protein-protein interactions in situ | Validating close proximity between CD36 and IR, or other interacting proteins [37] |
| Palmitate-BSA / Oleate-BSA complexes | Deliver saturated or unsaturated fatty acids to cells | Studying the allosteric effects of different fatty acids on insulin signaling [37] |
| Seahorse XF Analyzer | Measures cellular metabolic fluxes in real-time (glycolysis, mitochondrial respiration) | Functional assessment of metabolic pathway utilization after hormonal or genetic perturbation [37] |
Advanced Tools for Profiling Metabolic Flux and Energetics
Hyperpolarized 13C-NMR and Real-Time Tracking of Glycolytic Kinetics
The study of glycolysis, the fundamental pathway converting glucose to pyruvate for ATP production, has been revolutionized by the advent of hyperpolarized 13C-Nuclear Magnetic Resonance (NMR) spectroscopy. This transformative technology enables real-time, non-invasive observation of metabolic kinetics with unprecedented temporal resolution, revealing dynamic cellular processes previously inaccessible to researchers. Traditional metabolic assays provide static snapshots of metabolite concentrations, but fail to capture the rapid flux through glycolytic pathways that is crucial for understanding energy metabolism in diverse contexts from cancer to immune cell activation [40] [41].
At its core, this technique addresses a critical gap in metabolic research: the ability to directly observe substrate influx and conversion through central carbon metabolism on a timescale of seconds. By temporarily enhancing NMR sensitivity by more than four orders of magnitude, hyperpolarized 13C-NMR allows researchers to track the fate of 13C-labeled substrates as they traverse the glycolytic pathway in living systems, providing unique insights into the kinetic barriers and regulatory checkpoints that govern glucose utilization for ATP production [40]. This technical guide explores the methodology, applications, and implementation of hyperpolarized 13C-NMR for investigating the mechanistic details of glucose uptake and utilization.
Technical Foundations of Hyperpolarized 13C-NMR
Fundamental Principles and Mechanism
Dissolution Dynamic Nuclear Polarization (dDNP) forms the physical basis for the signal enhancement in hyperpolarized 13C-NMR. The process involves transferring the high polarization of unpaired electrons in stable radicals to 13C nuclei through microwave irradiation at cryogenic temperatures (~1 K) in a strong magnetic field [40] [41]. This temporary redistribution of nuclear spin states drastically enhances the detectable NMR signal, allowing observation of metabolic reactions in real-time.
The hyperpolarized state is transient, decaying with the spin-lattice relaxation time (T1), which typically ranges from 10-50 seconds for non-protonated carbons in metabolic substrates [40]. This limited temporal window necessitates rapid injection and measurement protocols but is sufficient to monitor the uptake and conversion of rapidly transported and metabolized substrates in their natural intracellular environment [40] [42]. The technique is particularly valuable for identifying kinetic bottlenecks in metabolic networks, as it directly reveals intermediates that accumulate at thermodynamically favored but kinetically slow metabolic steps [40].
Key Metabolic Probes and Detection
The most common substrates for hyperpolarized 13C-NMR studies of glycolysis include:
[1-13C]pyruvate: Serves as a probe for the final step of glycolysis, readily converting to lactate, alanine, or bicarbonate, providing information on lactate dehydrogenase (LDH) activity, alanine transaminase activity, and pyruvate dehydrogenase (PDH) flux, respectively [41] [43] [44].
[U-13C,2H]glucose: Enables tracking of flux through the entire glycolytic pathway, from initial uptake to downstream metabolite formation, revealing bottlenecks at specific enzymatic steps such as phosphofructokinase and pyruvate kinase [40] [41].
The detection of 13C-labeled metabolites occurs with a temporal resolution of approximately 3 seconds, allowing precise kinetic measurements of metabolic fluxes in living cells and tissues [43]. The high sensitivity enables studies with cell numbers as low as 10 million, making it applicable to various biological systems from microbial cultures to primary human cells [41].
Experimental Methodologies and Protocols
Cell Preparation and Bioreactor Integration
Successful hyperpolarized NMR experiments require careful cell preparation and maintenance within an NMR-compatible bioreactor system that ensures cell viability during measurements. The following protocol outlines key steps for cell preparation:
Cell Culture and Harvesting: Culture sufficient cells (typically ~4 × 10⁷ cells for each measurement) under standard conditions. For immune cells such as CAR T cells, isolate from donor samples and activate using CD3/CD28 Dynabeads and IL-2 following established expansion protocols [41]. Harvest cells at appropriate densities during key metabolic transition points (e.g., days 1, 7, 14, and 21 for CAR T cells to capture different activation states) [41].
Cell Encapsulation in Alginate Gels: Resuspend cell pellets in 2% (w/v) biological research-grade sodium alginate solution. Form cell-loaded gels through calcium cross-linking by adding the cell-alginate mixture to 50 mM CaCl₂ solution and centrifuging gently at 200 × g for 5 minutes [42]. This encapsulation maintains cell viability and position during NMR measurements.
Bioreactor Assembly: Construct an NMR-compatible bioreactor using a screw-cap NMR tube (10 mm diameter) with modified caps for tubing insertion. Use chemically resistant PEEK tubing (inner diameter 1.0 mm) for medium delivery and integrate a 3D-printed cylindrical holder with a borosilicate glass capillary to secure the cell-containing matrix within the measurement volume [42]. Maintain continuous medium circulation at approximately 0.2 mL/min using a peristaltic pump with medium pre-warmed to 37°C [42].
Sample Polarization and Data Acquisition
The polarization and dissolution process requires specialized equipment and precise timing:
Polarizer Preparation: Dope 18 μL of [1-13C]pyruvic acid with 25 mM OX063 trityl radical as a polarization source. Insert the sample vial into the bore unit of a DNP polarizer (typically operating at 6.7 T, 1.25 K, 1.2 mbar) and apply microwave irradiation at approximately 188 GHz (22 mW) for 60-80 minutes [42]. Monitor polarization buildup using the solid-state NMR spectrometer built into the DNP system.
Rapid Dissolution and Injection: Rapidly dissolve the polarized sample in 3.2 mL of preheated dissolution buffer (40 mM Tris, 50 mM NaOH, 100 mM NaCl) to achieve a physiological temperature and pH [42]. Immediately inject the hyperpolarized solution into the cell-containing bioreactor already positioned in the NMR spectrometer magnet.
NMR Data Collection: Acquire 13C NMR spectra using low-angle RF pulses (typically 8-15°) with rapid repetition times (TR = 2-3 s) to maximize signal detection while preserving the hyperpolarized magnetization [41]. Continue acquisition for approximately 2-3 minutes to track the conversion of the hyperpolarized substrate into metabolic products.
Data Analysis and Kinetic Modeling
Quantify metabolic fluxes by fitting the time-dependent changes in substrate and product signals to appropriate kinetic models. For simple two-site exchange reactions (e.g., pyruvate lactate), use a linear differential equation model that accounts for metabolic conversion, signal relaxation (T1), and RF pulsing effects [41]. Calculate apparent rate constants (e.g., kPyr→Lac) to quantify metabolic activity. For more complex pathways involving multiple steps (e.g., glucose → lactate), employ multi-compartment models that account for sequential conversion through pathway intermediates [40] [41].
Research Applications and Key Findings
Quantitative Insights into Glycolytic Regulation
Application of hyperpolarized 13C-NMR across diverse biological systems has yielded fundamental insights into glycolytic regulation:
Table 1: Key Metabolic Flux Measurements Using Hyperpolarized 13C-NMR
| Cell Type/System | Substrate | Key Metabolic Findings | Quantitative Flux Data | Reference |
|---|---|---|---|---|
| Lactococcus lactis (Gram-positive bacterium) | [U-13C,2H]glucose | Identified accumulation of F6P, F1,6BP, DHAP, 3PG at kinetic barriers; overflow to acetoin | Rate of upper glycolysis: L. lactis < E. coli < S. cerevisiae < human cancer cells | [40] |
| CAR T cells (human, day 7 post-activation) | [U-13C,2H]glucose | 30-fold increase in glycolytic flux during activation phase | Apparent rate constant: 9.4 × 10⁻⁵ s⁻¹ | [41] |
| CAR T cells (human, day 7 post-activation) | [1-13C]pyruvate | Elevated lactate production during glycolytic phase | Apparent rate constant: 10.7 × 10⁻⁵ s⁻¹ | [41] |
| Rat skeletal muscle (with DCA treatment) | [1-13C]lactate | Shift toward oxidative metabolism | rLac→HCO₃⁻ increased from 0.002 to 0.039 | [43] |
Mapping Metabolic Reprogramming in Disease and Cellular Activation
Hyperpolarized 13C-NMR has proven particularly valuable for detecting metabolic reprogramming in pathological states and during cellular activation:
Immune Cell Activation: Studies with expanded CAR T cells revealed a dramatic metabolic transition from oxidative phosphorylation to aerobic glycolysis by day 7 of expansion, followed by a return to oxidative phosphorylation by day 21. This metabolic plasticity was quantified using hyperpolarized [U-13C,2H]glucose, which showed a more than 30-fold difference in glycolytic flux between minimum (day 1) and maximum (day 7) activity [41].
Inflammatory States: Research on pro-inflammatory M1 polarized macrophages demonstrated significantly elevated conversion of hyperpolarized [1-13C]pyruvate to lactate compared to resting macrophages or anti-inflammatory M2 states. This glycolytic phenotype serves as a metabolic biomarker of inflammation and can be modulated by anti-inflammatory treatments [44].
Muscle Bioenergetics: Investigations using hyperpolarized [1-13C]lactate in rat muscle provided direct evidence for the intracellular lactate shuttle hypothesis, showing rapid lactate oxidation particularly when stimulated with dichloroacetate (DCA) to enhance pyruvate dehydrogenase activity. These findings challenge the traditional view of lactate as merely a waste product [43].
Essential Research Tools and Reagents
Table 2: Research Reagent Solutions for Hyperpolarized 13C-NMR Studies
| Reagent/Material | Specification | Function in Experimental Workflow |
|---|---|---|
| 13C-labeled Substrates | [1-13C]pyruvate, [U-13C,2H]glucose, [1-13C]lactate | Metabolic probes with specific isotopic labeling for tracking pathway flux |
| Polarizing Agent | OX063 trityl radical | Stable radical for electron polarization transfer to 13C nuclei |
| Cell Encapsulation Matrix | 2% (w/v) sodium alginate solution | 3D scaffold for maintaining cell viability and position during NMR |
| Cross-linking Solution | 50 mM CaCl₂ | Ionic cross-linker for alginate gel formation |
| Dissolution Buffer | 40 mM Tris, 50 mM NaOH, 100 mM NaCl | Adjusts polarized sample to physiological pH and ionic strength |
| NMR-compatible Bioreactor | PEEK tubing, modified NMR tube, 3D-printed holders | Maintains controlled environment for cells during measurement |
| Culture Medium with D₂O | RPMI-1640 with 5% (v/v) D₂O | Maintains cell viability while providing NMR lock signal |
Visualizing Metabolic Pathways and Experimental Workflows
Glycolytic Pathway with Hyperpolarized NMR Detection
Glycolytic Pathway with NMR Detection Points
This diagram illustrates key glycolytic intermediates and endpoints detectable via hyperpolarized 13C-NMR, highlighting metabolites that accumulate at kinetic barriers (F6P, F16BP) and alternative endpoints like acetoin that reflect specific metabolic states [40].
dDNP-NMR Experimental Workflow
dDNP-NMR Experimental Workflow
This workflow outlines the sequential steps in hyperpolarized NMR experiments, from sample preparation and polarization to data acquisition and analysis, highlighting the critical time-sensitive steps of dissolution and injection [41] [42].
Technical Considerations and Implementation Challenges
Successful implementation of hyperpolarized 13C-NMR for glycolytic kinetics studies requires careful attention to several technical considerations:
Temporal Constraints: The transient nature of the hyperpolarized state (T1 ~ 10-50 s) demands optimized rapid mixing and injection systems to minimize delays between dissolution and measurement [40] [42]. Custom bioreactor designs with integrated injection pathways can reduce this latency significantly.
Cell Viability Maintenance: Ensuring physiological conditions during NMR measurements is crucial. Continuous perfusion systems with pre-warmed medium (37°C) and proper cell encapsulation matrices are essential for maintaining metabolic activity throughout the experiment [42].
Spectral Assignment and Quantification: Accurate metabolite identification requires reference to pH-dependent chemical shift tables, as intracellular pH variations can affect peak positions [40]. Employing lineshape fitting algorithms that account for 13C-13C coupling in uniformly labeled substrates improves quantification accuracy [41].
Data Interpretation Challenges: The observed flux represents an apparent rate constant influenced by multiple factors including substrate transport, enzyme activity, and cofactor availability. Complementary measurements using isotopically labeled substrates at natural abundance can help validate findings and provide additional context for interpretation [40] [41].
Hyperpolarized 13C-NMR spectroscopy represents a paradigm shift in metabolic research, providing unprecedented access to the dynamic kinetics of glycolytic pathways in functioning biological systems. By enabling real-time observation of substrate utilization with second-scale resolution, this technology has revealed critical insights into metabolic regulation, including kinetic barriers in glycolysis, metabolic reprogramming in disease states, and the remarkable plasticity of cellular energy metabolism. As the methodology becomes more accessible through standardized protocols and commercial instrumentation, its application continues to expand across diverse research domains from fundamental biochemistry to drug development and diagnostic imaging. The continued refinement of polarization techniques, novel metabolic probes, and analytical methods promises to further enhance the spatial and temporal resolution of this powerful technology, opening new frontiers in our understanding of cellular bioenergetics.
Metabolomics and Nutrient Consumption Profiling in Cell Cultures
Metabolomics and nutrient consumption profiling provide a powerful, integrated approach for investigating the real-time metabolic status of cell cultures. This guide details the application of these techniques to study core metabolic processes, with a specific focus on the mechanisms of glucose uptake and utilization for ATP production. Metabolomics is the comprehensive analysis of small-molecule metabolites, which represent the ultimate functional readout of cellular processes [45]. When combined with precise measurements of nutrient consumption from the culture medium, this approach offers an unparalleled view of cellular metabolic fluxes. For research on energy metabolism, this integrated strategy can delineate the contributions of glycolysis and mitochondrial respiration to ATP generation, a distinction crucial for understanding cellular bioenergetics in various physiological and pathological states.
Recent research challenges the long-held assumption that glycolysis is preferentially used for its superior ATP production rate per unit of protein. In fact, quantitative flux analysis in diverse systems, including yeasts and mammalian cells, has demonstrated that mitochondrial respiration is more proteome-efficient than aerobic glycolysis, generating more ATP per mass of enzyme protein invested [46]. This paradigm shift underscores the necessity of precise experimental methodology to accurately map a cell's metabolic routing of nutrients like glucose.
Experimental Workflow for Integrated Metabolomics and Nutrient Profiling
The complete experimental pipeline, from cell culture to biological interpretation, involves a series of methodical steps designed to ensure the accurate capture of metabolic information.
Comprehensive Experimental Workflow
The following diagram outlines the integrated workflow for metabolomics and nutrient consumption analysis:
Cell Culture and Sample Preparation
Cell Culture Protocol:
- Culture Conditions: Maintain cells in appropriate medium (e.g., DMEM, Ham's F10) supplemented with necessary sera (e.g., Fetal Bovine Serum) and growth factors [47]. For nutrient consumption studies, ensure consistent seeding density and culture volume across replicates.
- Treatment and Harvest: Apply experimental treatments for a defined duration. For metabolomics, rapidly quench metabolic activity using cold methanol (-20°C) or liquid nitrogen to instantly arrest enzyme activity and preserve metabolic fingerprints [47].
- Metabolite Extraction: Suspend cell pellets in cold lysis buffer (e.g., 50 mM ammonium bicarbonate) and sonicate. Quantify protein concentration using a BCA assay. Extract metabolites from a standardized protein amount (e.g., 100 µg) using cold methanol (4 volumes, -20°C for 2 hours). After centrifugation, transfer the supernatant and dry completely using a speed-vac centrifugal vacuum concentrator. Reconstitute the dried metabolite content in a suitable solvent (e.g., 100 µL of 0.1% formic acid in water) for LC-MS/MS analysis [47].
Nutrient Consumption Profiling:
- Medium Analysis: Collect culture medium at experimental start and end points. Analyze using the same LC-MS/MS platform or dedicated assays for key nutrients like glucose, glutamine, and amino acids.
- Consumption Calculation: Quantify nutrient depletion by comparing analyte concentrations in spent versus fresh medium, normalized to cell number or total protein.
Analytical Techniques: LC-MS/MS Profiling
Liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS) is the cornerstone technique for comprehensive metabolomic profiling due to its high sensitivity and capacity to detect a broad range of metabolites.
LC-MS/MS Analysis Protocol [47]:
- Instrumentation: Use a high-resolution mass spectrometer (e.g., Q-Exactive Orbitrap) coupled with a UHPLC system (e.g., Vanquish).
- Chromatography: Inject sample (e.g., 5 µL) onto a reverse-phase column (e.g., Eclipse Plus C18 RRHD, 50 × 2.1 mm; 1.8 µm) at 40°C. Employ a gradient elution with mobile phase A (0.1% formic acid in water) and B (0.1% formic acid in 80% acetonitrile) at a flow rate of 0.2 mL/min. A typical gradient runs: 2.5% B for 2 min, 2–12% B over 2–11 min, 12–28% B over 11–15 min; 28–60% B over 15–22 min; 96% B over 22–26 min; returning to 2.5% B for re-equilibration.
- Mass Spectrometry: Operate in both positive and negative ionization modes with switching. Parameters include: Full-MS scans from 100-1000 m/z (positive) or 50-500 m/z (negative) at 70,000 resolution; data-dependent MS2 (dd-MS2) scans at 17,500 resolution with normalized collision energy (NCE) of 30. Use sheath gas flow rate of 19 (positive) and 5 (negative); spray voltage of 3.80 kV (positive) and -3.40 kV (negative); capillary temperature of 320°C.
Data Analysis and Computational Methods
Data Preprocessing and Metabolite Identification
Raw LC-MS/MS data requires extensive preprocessing before biological interpretation.
Preprocessing Workflow [45] [48]:
- Feature Extraction: Use software (e.g., Compound Discoverer, XCMS, MZmine) for peak detection, noise reduction, retention time correction, and chromatographic alignment. Group related ions (adducts, multiply charged species) to represent a single metabolite.
- Quality Control: Employ pooled quality control (QC) samples. Remove metabolites with coefficient of variation (CV) >30% in QCs to ensure data quality [47].
- Metabolite Identification: Compare acquired mass spectra (m/z) and retention times against authentic standards in in-house libraries or public databases (mzCloud, METLIN, ChemSpider). Follow the Metabolomics Standards Initiative (MSI) levels for identification confidence, aiming for Level 1 (identified compounds) or Level 2 (putatively annotated compounds) whenever possible [45] [47].
Statistical Analysis and Integration
A combination of univariate and multivariate statistical methods is essential to extract meaningful biological insights from complex metabolomic datasets.
Key Statistical Approaches [49] [48]:
- Univariate Analysis: Apply Student's t-test (for two-group comparisons) or ANOVA (for multiple groups) to identify individual metabolites with significant abundance changes. Use false discovery rate (FDR) correction for multiple testing. Visualize results with volcano plots (significance vs. fold-change) and box plots.
- Multivariate Analysis:
- Unsupervised: Principal Component Analysis (PCA) to visualize inherent data structure, detect outliers, and observe sample clustering without prior knowledge of group membership.
- Supervised: Partial Least Squares-Discriminant Analysis (PLS-DA) or Orthogonal PLS-DA (OPLS-DA) to maximize separation between pre-defined sample groups and identify metabolites most responsible for the discrimination.
- Pathway and Integration Analysis: Perform pathway enrichment analysis (e.g., via MetaboAnalyst) to identify metabolic pathways significantly enriched with altered metabolites. Integrate nutrient consumption rates with intracellular metabolite levels to infer metabolic flux changes.
The Scientist's Toolkit: Essential Reagents and Materials
Table 1: Key Research Reagent Solutions for Metabolomics and Nutrient Profiling
| Item | Function/Application | Examples/Details |
|---|---|---|
| Cell Culture Media | Supports cell growth and provides nutrients for consumption studies | DMEM, Ham's F10; often supplemented with Fetal Bovine Serum (FBS) and growth factors (e.g., FGF2) [47]. |
| Metabolite Extraction Solvents | Quenches metabolism and extracts intracellular metabolites | Cold methanol, lysis buffers (e.g., 50 mM ammonium bicarbonate). Cold methanol at -20°C is standard for instant quenching [47]. |
| Chromatography Columns | Separates metabolite mixtures prior to mass spectrometry | Reverse-phase columns (e.g., Eclipse Plus C18 RRHD) for LC-MS/MS [47]. |
| Mass Spectrometry Standards | Enables metabolite identification and quantification | Isotope-labeled internal standards. Use of databases (mzCloud, METLIN, ChemSpider) for spectral matching [47] [48]. |
| Data Analysis Software | Processes raw data, performs statistics, and visualizes results | Compound Discoverer, XCMS, MetaboAnalyst for statistical analysis and pathway mapping [47] [49]. |
Investigating Glucose Metabolism: Key Metabolites and Pathways
For studies focused on glucose uptake and utilization for ATP production, targeted analysis of specific metabolites and pathways provides direct insight into metabolic routing and efficiency.
Glucose Utilization Pathways
The following diagram illustrates the primary metabolic pathways involved in glucose utilization, highlighting key metabolites measured in metabolomic studies:
Key Metabolites for Tracking Glucose Fate and ATP Production
Table 2: Key Metabolites for Assessing Glucose Utilization and Energy Production
| Metabolite Class | Specific Metabolites | Biological Significance in Energy Metabolism |
|---|---|---|
| Central Carbon Metabolites | Glucose, Hexose, Pyruvate, Lactate | Lactate secretion indicates glycolytic flux; intracellular pyruvate levels can reflect substrate availability for mitochondria [50] [51]. |
| TCA Cycle Intermediates | Citrate, Succinate, Fumarate, Malate, α-Ketoglutarate | Markers of mitochondrial metabolic activity and aerobic energy generation. Truncated TCA cycle is a feature of some highly glycolytic cells [46]. |
| Amino Acids & Derivatives | Alanine, Branched-Chain Amino Acids (Isoleucine, Leucine, Valine), Glutamine | BCAAs can be linked to oxidative stress and insulin resistance; glutamine is a key anaplerotic substrate for the TCA cycle [50] [46]. |
| Energy Carriers & Cofactors | ATP, ADP, AMP, NAD+, NADH | Direct readouts of cellular energy charge and redox state. Crucial for understanding the bioenergetic status. |
| Other Pathway Metabolites | Acylcarnitines, Hexosamine pathway metabolites | Acylcarnitines indicate fatty acid oxidation; HBP flux is a specialized glucose use pathway for glycosylation [50] [51]. |
Interpretation in the Context of Glucose Uptake and ATP Research
Interpreting metabolomic and nutrient consumption data requires integration with the current understanding of metabolic efficiency. A critical finding from recent research is that mitochondrial respiration is more proteome-efficient than aerobic glycolysis, generating more ATP per mass of enzyme protein invested across diverse systems including yeasts, T cells, and cancer cells [46]. This challenges the historical assumption that aerobic glycolysis (the Warburg effect) is employed for its superior speed of ATP production.
Metabolomic data can reveal this metabolic strategy. A profile showing significant glucose consumption and lactate secretion, despite available oxygen, indicates aerobic glycolysis. However, simultaneous measurement of TCA cycle intermediates and oxygen consumption rates may reveal that a substantial portion of ATP is still generated via efficient oxidative phosphorylation [46]. Furthermore, the discovery of spatiotemporally resolved waves of glucose utilization during mammalian gastrulation, where glucose is differentially routed through the Hexosamine Biosynthetic Pathway (HBP) or glycolysis to instruct distinct cell-fate decisions, underscores that nutrient utilization can directly control complex biological processes beyond energy production [51].
Pathway enrichment analysis of metabolomic data often highlights disruptions in pathways like arginine biosynthesis, arginine-proline metabolism, and branched-chain amino acid metabolism in conditions like metabolic syndrome [50]. These pathways interact with core energy metabolism, providing a more holistic view of the metabolic state. By employing machine learning models, such as stochastic gradient descent or decision tree classifiers, on metabolomic datasets, researchers can develop robust predictive models for metabolic phenotypes or conditions, enhancing the translational potential of the findings [50] [52].
Genome-Scale Metabolic Models (GEMs) for Predicting Flux Distributions
Genome-scale metabolic models (GEMs) are computational representations of the complete metabolic network of an organism, enabling mathematical simulation of metabolism for archaea, bacteria, and eukaryotic organisms [53]. These models quantitatively define the relationship between genotype and phenotype by contextualizing different types of Big Data, including genomics, metabolomics, and transcriptomics [53]. GEMs contain all known metabolic reactions, their associated genes, gene-protein-reaction (GPR) rules, and metabolites, providing a structured framework for predicting metabolic fluxes under various conditions [53]. Since the first GEM for Haemophilus influenzae was reconstructed in 1999, the development of GEMs has expanded dramatically, with models now available for 5,897 bacteria, 127 archaea, and 215 eukaryotes as of February 2019 [54].
The primary application of GEMs in flux distribution analysis lies in their ability to predict how metabolic resources are allocated throughout the network to achieve specific cellular objectives, most commonly biomass production for growth. This capability makes GEMs particularly valuable for investigating fundamental biological processes such as glucose uptake and utilization for ATP production. By simulating the metabolic fate of glucose from transport through membrane proteins to its conversion into energy molecules, researchers can identify key regulatory nodes, potential drug targets, and metabolic engineering strategies for improved bio-production [54].
Core Principles of Constraint-Based Modeling and Flux Prediction
Mathematical Foundation of GEMs
GEMs transform cellular growth and metabolism processes into a mathematical model based on a stoichiometric matrix (S) of m metabolites and n reactions, which is solved at steady-state assuming mass balance [55]. The fundamental equation governing this system is:
[ S \cdot v = 0 ]
where v represents the flux vector of reaction rates in the network. This equation is subject to additional constraints that define the operating bounds of each reaction:
[ \alphai \leq vi \leq \beta_i ]
where αi and βi represent lower and upper bounds for flux i, respectively [55]. The steady-state assumption implies that metabolite concentrations remain constant over time, meaning the production and consumption of each metabolite are balanced.
Flux Balance Analysis
Flux Balance Analysis (FBA) is the most widely used optimization technique for predicting metabolic flux distributions in GEMs [54]. FBA uses linear programming to identify a flux distribution that maximizes or minimizes a particular cellular objective function, most commonly biomass production as a proxy for cellular growth [55]. The generic FBA formulation is:
[ \begin{align} \text{Maximize } & Z = c^T v \ \text{subject to } & S \cdot v = 0 \ & \alpha_i \leq v_i \leq \beta_i \end{align} ]
where Z represents the objective function, and c is a vector of weights indicating how much each reaction contributes to the objective [54]. For simulations of glucose uptake and utilization, the glucose transport reaction would typically be constrained to observed uptake rates, while ATP maintenance reactions would be included to represent cellular energy requirements.
Table 1: Common Optimization Methods for Flux Prediction in GEMs
| Method | Mathematical Approach | Primary Application | Key Features |
|---|---|---|---|
| FBA [54] | Linear programming | Steady-state flux prediction | Assumes optimal growth; fast computation |
| dFBA [53] | Dynamic simulation using FBA | Time-dependent processes | Incorporates changing extracellular conditions |
| 13C MFA [53] | Isotope labeling patterns | Experimental flux validation | Uses tracer data; high precision for central metabolism |
| TMFA [55] | Mixed-integer linear programming | Thermodynamically feasible fluxes | Incorporates energy constraints |
Advanced Constraint-Based Approaches
While FBA provides a foundational approach, several extensions have been developed to improve the biological realism of flux predictions. Dynamic FBA (dFBA) extends the basic framework to simulate time-dependent processes by incorporating changing extracellular conditions [53]. 13C Metabolic Flux Analysis (13C MFA) utilizes isotope labeling patterns from experiments with 13C-labeled glucose to validate and refine intracellular flux predictions [53]. Thermodynamics-based Flux Analysis (TMFA) incorporates thermodynamic constraints to eliminate flux distributions that would be energetically infeasible, using estimates of Gibbs free energy to determine reaction directionality [55].
Methodological Framework for GEM Reconstruction and Simulation
GEM Reconstruction Pipeline
The reconstruction of high-quality GEMs follows a systematic workflow that transforms genomic information into a mathematical model capable of predicting flux distributions. The reconstruction process begins with genome annotation to identify metabolic genes, followed by compilation of corresponding reactions and metabolites into a draft network [53]. This draft model is subsequently refined through extensive manual curation to fill knowledge gaps, verify mass and charge balances, and incorporate organism-specific physiological information.
Table 2: Key Tools for GEM Reconstruction and Analysis
| Tool Name | Primary Function | Input Requirements | Output |
|---|---|---|---|
| ModelSEED [55] | Automated model reconstruction | Genome annotation | Draft GEM |
| CarveMe [55] | Template-based model building | Genome sequence | Species-specific GEM |
| GECKO [56] | Enzyme-constrained modeling | GEM + proteomic data | ecGEM with enzyme limits |
| MEMOTE [55] | Model quality assessment | GEM in SBML format | Quality report |
| COBRA Toolbox [56] | Simulation and analysis | GEM + constraints | Flux predictions |
The reconstruction process establishes GPR associations that define the molecular mechanism connecting genes to metabolic fluxes through enzyme activities. These Boolean rules specify how genes encode subunits of enzyme complexes (AND logic) or isozymes (OR logic) that catalyze specific metabolic transformations [53]. For glucose uptake modeling, this includes explicit representation of glucose transporter genes (e.g., GLUT proteins in humans or PTS system components in bacteria) and their associated reactions.
Integration of Enzymatic Constraints
The GECKO (Enhancement of GEMs with Enzymatic Constraints using Kinetic and Omics data) toolbox represents a significant advancement in flux prediction accuracy by incorporating enzyme capacity constraints [56]. This approach extends traditional GEMs by adding pseudo-reactions that represent enzyme usage, with constraints derived from measured enzyme kinetic parameters (kcat values) and proteomic abundances. The enzyme capacity constraint for a reaction i is formulated as:
[ vi \leq [Ei] \cdot k_{cat,i} ]
where [Ei] represents the enzyme concentration and kcat,i is the turnover number [56]. The total enzyme usage is limited by the measured or estimated total protein mass available for metabolic functions. This approach significantly improves predictions of glucose uptake rates and overflow metabolism by accounting for the proteomic cost of maintaining metabolic pathways.
Diagram 1: GEM Reconstruction Workflow
Multi-Scale Modeling Approaches for Enhanced Flux Predictions
Integration of Multi-Omics Data
Contemporary GEMs have evolved beyond static metabolic networks to dynamic, multi-scale models that integrate diverse omics datasets to improve flux prediction accuracy. Transcriptomic, proteomic, and metabolomic data can be incorporated as additional constraints to generate context-specific models that reflect particular physiological states or environmental conditions [53]. The Integrative Metabolic Analysis Tool (iMAT) algorithm, for instance, uses transcriptomic data to define highly and lowly expressed reactions, then finds a flux distribution that maximizes the consistency between flux activity and expression levels [55].
For glucose uptake studies, proteomic data on glucose transporter abundance can directly constrain uptake reaction bounds, while transcriptomic data on glycolytic enzyme expression can inform flux capacity through central carbon metabolism. Metabolomic measurements of intracellular metabolite pools can further refine flux estimations by providing additional mass balance constraints [53]. This multi-omics integration is particularly valuable for investigating tissue-specific glucose utilization patterns in multi-cellular organisms or condition-specific metabolism in microbial production hosts.
ME-Models and Thermodynamic Constraints
Metabolism and Expression models (ME-models) represent a significant expansion of traditional GEMs by explicitly incorporating macromolecular biosynthesis processes, including transcription and translation [53]. These models simulate the metabolic trade-offs between biomass production and the protein synthesis capacity required to implement metabolic pathways. The rETFL (recombinant Expression and Thermodynamic Flux) framework extends this approach to predict metabolic burden in recombinant organisms, enabling quantitative analysis of how heterologous protein expression impacts glucose uptake and energy metabolism [57].
Thermodynamic constraints further refine flux predictions by eliminating thermodynamically infeasible cycles and constraining reaction directionality based on estimated Gibbs free energy values [55]. Methods like Network Embedded Thermodynamic (NET) analysis and Thermodynamics-based Metabolic Flux Analysis (TMFA) integrate quantitative metabolomic data with thermodynamic principles to identify putative regulatory sites and improve the biological validity of predicted flux distributions [55].
Diagram 2: Multi-Omics Data Integration
Application to Glucose Uptake and Utilization Analysis
Modeling Glucose Transport Mechanisms
In the context of glucose uptake and ATP production research, GEMs provide a systems-level framework for investigating the complex interplay between glucose transport, glycolytic flux, and energy generation. Glucose uptake in mammalian systems occurs primarily through facilitated diffusion via GLUT transporters or secondary active transport through SGLT transporters [12]. These transport mechanisms can be explicitly represented in GEMs through corresponding transport reactions with appropriate kinetic parameters.
Table 3: Key Glucose Transporters and Their Properties for Modeling
| Transporter | Transport Mechanism | Km for Glucose | Tissue Expression | Modeling Considerations |
|---|---|---|---|---|
| GLUT1 [12] [58] | Facilitated diffusion | 3 mM | Ubiquitous, especially RBCs and blood-brain barrier | Basal glucose uptake; constitutive expression |
| GLUT2 [12] [58] | Facilitated diffusion | 14-17 mM | Pancreatic beta-cells, liver, kidney | High capacity; glucose sensing; wide dynamic range |
| GLUT3 [12] [58] | Facilitated diffusion | 1.4 mM | Neurons, testis | High affinity; ensures glucose supply to critical tissues |
| GLUT4 [12] [58] | Facilitated diffusion | 5 mM | Muscle, adipose tissue, heart | Insulin-responsive; intracellular compartmentalization |
| SGLT1/2 [12] | Secondary active transport | Varies by type | Kidney, intestine | Energy-dependent; against concentration gradient |
When modeling glucose uptake in specific tissues or cell types, the appropriate transporter complement must be represented with constraints reflecting their kinetic properties and regulatory mechanisms. For instance, insulin-responsive GLUT4 translocation in muscle and adipose tissue can be modeled through dynamic constraint adjustments that reflect increased glucose uptake capacity in the presence of insulin signaling [12].
Predicting Flux Distributions in Central Carbon Metabolism
Following glucose uptake, GEMs simulate the distribution of carbon flux through glycolysis, pentose phosphate pathway, and tricarboxylic acid (TCA) cycle to meet cellular energy and biosynthetic demands. The flux distribution is optimized to achieve cellular objectives, typically maximizing ATP production or biomass generation, while respecting network stoichiometry and capacity constraints [54].
Experimental validation of these predictions often involves 13C metabolic flux analysis, where cells are fed 13C-labeled glucose and the labeling patterns in intracellular metabolites are measured to infer actual flux distributions [53]. Comparisons between predicted and measured fluxes have demonstrated GEMs' ability to accurately capture the redistributions of glucose-derived carbon under different physiological conditions, such as hypoxia, nutrient limitations, or genetic perturbations [54].
For ATP production studies, GEMs quantitatively account for the ATP yields from glucose metabolism, including substrate-level phosphorylation in glycolysis and oxidative phosphorylation linked to the electron transport chain. This enables prediction of how changes in glucose uptake impact cellular energy charge and how metabolic adaptations occur in energy-deficient states [54].
Experimental Protocols for GEM-Guided Research
Protocol for Validating Glucose Uptake Predictions
Purpose: To experimentally validate GEM-predicted flux distributions for glucose uptake and utilization.
Materials:
- Cell culture system (microbial or mammalian)
- 13C-labeled glucose (e.g., [1-13C]glucose, [U-13C]glucose)
- LC-MS or GC-MS system for isotopomer analysis
- Extracellular metabolite analysis platform
- Supplies for gene knockout or knockdown (CRISPR, RNAi, etc.)
Procedure:
- Constrain the appropriate GEM with measured glucose uptake rates and simulate flux distributions under experimental conditions.
- Cultivate cells in minimal medium containing 13C-labeled glucose as the sole carbon source.
- Measure extracellular metabolite fluxes (glucose uptake, secretion products) throughout cultivation.
- Harvest cells during exponential growth phase and extract intracellular metabolites.
- Analyze mass isotopomer distributions of key metabolites using LC-MS/GC-MS.
- Calculate experimental flux distributions using 13C-MFA software (e.g., INCA, OpenFLUX).
- Compare experimental fluxes with GEM predictions and refine model parameters if discrepancies exist.
- Validate key predictions through genetic perturbations (e.g., knockout of predicted essential genes).
Expected Outcomes: The protocol should yield quantitative flux maps that can be used to validate and refine GEM predictions, particularly for glucose entry points and partitioning between glycolysis, pentose phosphate pathway, and TCA cycle.
Protocol for Integrating Proteomic Constraints
Purpose: To build an enzyme-constrained GEM (ecGEM) for improved prediction of glucose uptake and utilization fluxes.
Materials:
- Reference GEM for target organism
- Proteomics data (mass spectrometry-based quantification)
- Kinetic parameters from BRENDA database or literature
- GECKO toolbox installation
- MATLAB or Python environment
Procedure:
- Download and install the GECKO toolbox following instructions at https://github.com/SysBioChalmers/GECKO.
- Prepare proteomics data with enzyme abundances in mg/gDCW (gram dry cell weight).
- Retrieve kcat values for enzymes in the model from BRENDA database using GECKO's automated query functions.
- Apply the GECKO pipeline to enhance the base GEM with enzyme usage reactions and constraints.
- Calibrate the protein pool constraint using measured growth rates and glucose uptake rates.
- Simulate glucose-limited growth conditions and compare flux predictions with experimental data.
- Adjust kcat values for key glucose metabolism enzymes based on literature evidence if predictions deviate from measurements.
- Use the calibrated ecGEM to predict flux changes in response to genetic modifications or environmental perturbations.
Expected Outcomes: Generation of an enzyme-constrained model that more accurately predicts metabolic fluxes, particularly under conditions where enzyme capacity limits glucose utilization rates.
Research Reagent Solutions
Table 4: Essential Research Reagents for GEM-Related Glucose Uptake Studies
| Reagent/Category | Specific Examples | Function in GEM Research | Application Notes |
|---|---|---|---|
| Isotope-Labeled Substrates | [U-13C]glucose, [1-13C]glucose | Experimental flux validation via 13C-MFA | Enables precise tracking of carbon fate; required for flux validation |
| Gene Editing Tools | CRISPR-Cas9 systems, RNAi constructs | Model validation through genetic perturbations | Tests predictions of gene essentiality; creates knockout mutants |
| Proteomics Platforms | Mass spectrometry with label-free or TMT quantification | Enzyme abundance measurement for ecGEMs | Provides quantitative constraints for enzyme concentrations |
| Metabolomics Platforms | LC-MS, GC-MS systems | Extracellular and intracellular metabolite measurement | Provides data for constraint definition and model validation |
| Kinetic Databases | BRENDA, SABIO-RK | Source of enzyme kinetic parameters | Provides kcat values for enzyme constraint implementation |
| GEM Reconstruction Tools | ModelSEED, CarveMe, RAVEN | Automated model generation | Accelerates initial model building from genomic data |
| Simulation Software | COBRA Toolbox, GECKO, COBRApy | Flux prediction and analysis | Enables constraint-based simulations and advanced analysis |
Genome-scale metabolic modeling represents a powerful computational framework for predicting flux distributions in biological systems, with particular relevance for understanding glucose uptake and utilization mechanisms. By integrating biochemical knowledge with mathematical optimization, GEMs enable quantitative prediction of how carbon from glucose is distributed through metabolic networks to support energy production and biomass synthesis. The continued development of multi-scale models that incorporate enzymatic constraints, regulatory information, and multi-omics data will further enhance the predictive accuracy and application scope of these models in both basic research and drug development contexts. As the field advances, GEMs are poised to play an increasingly important role in elucidating the metabolic basis of diseases characterized by dysregulated glucose metabolism and in guiding metabolic engineering strategies for bio-production.
Machine Learning in Pathway Construction, Optimization, and Enzyme Engineering
This technical guide explores the transformative impact of machine learning (ML) on metabolic engineering, focusing on the construction and optimization of biochemical pathways and the engineering of enzymes, with specific relevance to glucose uptake and utilization for ATP production. The "Warburg effect"—a hallmark of cancer cell metabolism where cells favor glycolysis over oxidative phosphorylation for ATP production even under aerobic conditions—highlights the critical importance of understanding glucose metabolic pathways in both health and disease [59]. This whitepaper provides researchers and drug development professionals with in-depth methodologies, practical protocols, and resources for implementing ML-driven approaches in metabolic research, offering powerful new tools to decipher the complex regulatory mechanisms governing cellular energy production.
Machine learning has emerged as a pivotal technology in metabolic engineering, enabling researchers to navigate the immense complexity of biological systems with unprecedented efficiency. Where traditional methods struggle with the nonlinear interactions, vast parameter spaces, and intricate regulatory networks that characterize metabolic pathways—particularly the central pathways of glucose metabolism that govern ATP production—ML algorithms can identify patterns, predict behaviors, and optimize biological systems at multiple scales.
The integration of ML is revolutionizing three fundamental areas of metabolic engineering: (1) the de novo construction of novel biosynthetic pathways, (2) the optimization of existing pathways for enhanced flux and yield, and (3) the engineering of enzymes with tailored properties. Within glucose metabolism research, these capabilities are particularly valuable for understanding and manipulating the fundamental processes that convert glucose to ATP, with applications ranging from bio-based chemical production to therapeutic interventions in metabolic diseases and cancer [59].
This guide examines state-of-the-art ML applications through both conceptual frameworks and practical implementations, with special attention to methodologies relevant to investigating the mechanisms of glucose uptake and utilization.
ML-Driven Pathway Construction and Prediction
The prediction and construction of novel metabolic pathways represents a foundational application of machine learning in metabolic engineering. Traditional approaches to pathway discovery relied heavily on literature curation and expert knowledge, limiting scalability and completeness.
Expanded Pathway Prediction Frameworks
Recent advancements have substantially broadened the scope of pathway prediction beyond the metabolic pathways traditionally focused on in databases like KEGG. A groundbreaking approach has developed a binary classifier model trained on the entire KEGG pathway hierarchy—not just metabolism—encompassing over 3 million entries and allowing predictions across all pathway types, including those related to genetic information processing, environmental information processing, and cellular processes [60].
This expanded framework demonstrated a mean performance score of 0.847, significantly outperforming models trained exclusively on metabolic pathways (score: 0.800), illustrating how incorporating diverse biological pathways enhances prediction accuracy through transfer learning [60]. For researchers studying glucose metabolism, this approach enables more comprehensive mapping of connections between glycolytic pathways and related cellular processes.
Data Processing and Model Architecture
The predictive power of pathway identification models depends critically on rigorous data processing and appropriate model selection:
- Dataset Construction: Curated from KEGG using automated tools, with careful removal of duplicate entries to prevent evaluation bias [60]
- Feature Engineering: Incorporates both compound characteristics and pathway attributes to facilitate association analysis [60]
- Model Selection: Binary classification using multi-layer perceptrons, with performance evaluated through accuracy, precision, recall, and F1 scores [60]
- Hierarchical Considerations: Accounts for the KEGG hierarchy of pathway categories (L1: main categories, L2: subcategories, L3: specific pathways) [60]
Table 1: Performance Metrics for Pathway Prediction Models
| Model Scope | Mean Performance | Standard Deviation | Key Advantages |
|---|---|---|---|
| All KEGG Pathways | 0.847 | 0.0098 | Broad applicability, transfer learning benefits |
| Metabolic Pathways Only | 0.800 | 0.021 | Specialized for metabolism |
Application to Glucose Metabolism Research
For researchers focusing on glucose uptake and utilization, these pathway prediction tools enable:
- Identification of Novel Connections: Discovering previously unrecognized links between glycolytic enzymes and other cellular processes
- Cross-Species Pathway Analysis: Comparing glucose metabolic pathways across organisms to identify conserved and specialized elements
- Drug Target Identification: Predicting alternative pathways that might be activated in response to therapeutic interventions targeting glucose metabolism
Pathway Optimization through Kinetic Modeling
Once pathways are identified, optimizing their flux and regulation represents a critical challenge, particularly for central metabolic pathways like glycolysis that directly influence ATP production kinetics.
The RENAISSANCE Framework
The RENAISSANCE (REconstruction of dyNAmIc models through Stratified Sampling using Artificial Neural networks and Concepts of Evolution strategies) framework addresses the fundamental challenge of kinetic parameter estimation in metabolic models [61]. This generative machine learning approach efficiently parameterizes large-scale kinetic models that accurately characterize intracellular metabolic states by integrating diverse omics data, extracellular medium composition, physicochemical constraints, and domain expertise.
The framework employs feed-forward neural networks as generators of kinetic parameters, optimized through natural evolution strategies (NES) to produce models with dynamic properties matching experimental observations [61]. This approach substantially reduces parameter uncertainty and improves accuracy while dramatically decreasing computation time compared to traditional kinetic modeling methods.
Implementation Protocol
Step 1: Data Integration and Steady-State Calculation
- Input structural properties of the metabolic network (stoichiometry, regulatory structure, rate laws)
- Integrate available omics data (metabolomics, fluxomics, proteomics, transcriptomics)
- Compute steady-state profiles of metabolite concentrations and fluxes using thermodynamics-based flux balance analysis [61]
Step 2: Generator Network Initialization
- Initialize population of generator neural networks with random weights
- Network architecture typically consists of three layers, sized according to model complexity [61]
Step 3: Iterative Optimization via Natural Evolution Strategies
- Step II: Each generator produces batches of kinetic parameters from multivariate Gaussian noise input
- Step III: Evaluate dynamics of parameterized models by computing Jacobian eigenvalues and dominant time constants
- Step IV: Assign rewards based on biological relevance (e.g., matching experimentally observed doubling times)
- Update generator weights weighted by normalized rewards, with mutation via noise injection [61]
Step 4: Model Validation and Selection
- Validate robustnes through perturbation tests (±50% metabolite concentration changes)
- Verify return to steady state within biologically relevant timescales [61]
Application to Escherichia coli Kinetic Modeling
In a validation study, RENAISSANCE generated kinetic models for anthranilate-producing E. coli comprising:
- 113 nonlinear ordinary differential equations
- 502 kinetic parameters (including 384 Michaelis constants)
- 123 reactions covering core metabolic pathways [61]
The generated models successfully captured experimentally observed doubling times (134 minutes) with 92-100% incidence of valid models after 50 generations, demonstrating robust dynamic behavior where 75.4% of perturbed models returned to steady state within 24 minutes [61].
Table 2: RENAISSANCE Performance Metrics for E. coli Modeling
| Metric | Performance | Biological Significance |
|---|---|---|
| Incidence of Valid Models | 92-100% | Models match observed cellular doubling times |
| Perturbation Recovery (24 min) | 75.4% | Robustness to metabolic fluctuations |
| Key Metabolite Recovery | 99.9% (NADH, ATP), 100% (NADPH) | Energy cofactor stability |
ML-Guided Enzyme Engineering
Enzyme engineering represents a critical application of machine learning, enabling the optimization of biocatalysts for specific metabolic functions, including those in glucose utilization pathways.
Integrated ML-Guided Platforms
Recent advances have established automated platforms that combine ML with high-throughput experimental methods. One such platform integrates cell-free DNA assembly, cell-free gene expression, and functional assays to rapidly map fitness landscapes across protein sequence space [62].
The platform employs a Design-Build-Test-Learn (DBTL) workflow that:
- Maps sequence-function relationships for enzyme variants
- Uses these data to train supervised ridge regression ML models augmented with evolutionary zero-shot fitness predictors
- Extrapolates to higher-order mutants with increased activity [62]
This approach was successfully applied to engineer amide synthetases, evaluating 1217 enzyme variants across 10,953 unique reactions, resulting in ML-predicted variants with 1.6- to 42-fold improved activity relative to parent enzymes [62].
Experimental Protocol for ML-Guided Enzyme Engineering
Phase 1: Substrate Promiscuity Evaluation
- Test wild-type enzyme against diverse substrate arrays (primary, secondary, alkyl, aromatic, complex pharmacophores)
- Identify native limitations and preferences under industrially relevant conditions (~1μM enzyme, 25mM substrate) [62]
- Document stereoselectivity, chemo-selectivity, and regioselectivity patterns
Phase 2: Cell-Free Protein Engineering
- Implement cell-free DNA assembly and gene expression to build site-saturated libraries
- Five-step workflow: (i) mutagenic PCR, (ii) DpnI digestion, (iii) Gibson assembly, (iv) LET amplification, (v) CFE protein synthesis [62]
- Validate system with control proteins (e.g., monomeric ultra-stable GFP)
Phase 3: Machine Learning Model Training
- Collect sequence-function data from variant screening
- Train augmented ridge regression models with evolutionary zero-shot fitness predictors
- Predict higher-order mutants with improved activity [62]
Phase 4: Model Validation and Iteration
- Test ML-predicted variants experimentally
- Iterate DBTL cycle with expanded training data
- Assess performance improvements relative to design objectives
Automated In Vivo Engineering Approaches
Complementing cell-free methods, automated in vivo enzyme engineering platforms combine:
- ML-guided prediction of beneficial modifications
- Growth-coupled selection systems that link enzyme activity to microbial fitness
- In vivo hypermutators to increase mutation rates in target genes
- High-throughput continuous cultivation platforms [63]
These integrated systems enable continuous directed evolution campaigns where ML both predicts initial modifications and analyzes enrichment patterns in evolved populations [63].
Table 3: ML-Guided Enzyme Engineering Platforms and Applications
| Platform | Key Methodology | Reported Improvement | Applications in Glucose Metabolism |
|---|---|---|---|
| ML-Cell-Free Platform [62] | Ridge regression with zero-shot predictors, CFE | 1.6- to 42-fold activity increase | Engineering glycolytic enzymes for altered flux control |
| Automated In Vivo Platform [63] | Growth-coupled selection, hypermutators | Varies by target | Optimization of glucose uptake systems |
| Directed Evolution 2.0 [64] | Semi-rational design with CRISPR/Cas | Enhanced stability, specificity | Thermostable enzymes for industrial bioprocessing |
Applications in Glucose Metabolism and ATP Production Research
The integration of ML approaches provides powerful tools for investigating the mechanisms of glucose uptake and utilization for ATP production, with particular relevance to both biotechnology and human disease.
Analyzing Glycolytic Dysregulation in Disease
Machine learning analysis of glucose metabolism pathways has identified novel therapeutic targets in clear cell renal cell carcinoma (ccRCC), a cancer type characterized by pronounced glycolytic dysregulation [59]. Through integration of three machine learning algorithms (LASSO, Random Forest, and Boruta), researchers analyzed 89 glucose metabolism genes from the REACTOME database, identifying ADPGK as a key regulator promoting invasion and metastasis in ccRCC [59].
The analytical workflow included:
- Gene Selection: 89 glucose metabolism genes from REACTOME database
- Multi-Algorithm Feature Selection: LASSO, RF, and Boruta for robust identification
- Immune Infiltration Analysis: Connection between metabolic reprogramming and tumor microenvironment
- Experimental Validation: In vitro confirmation of ADPGK role in invasion and metastasis [59]
This approach demonstrates how ML can identify critical regulatory nodes in glucose metabolism that represent potential therapeutic targets.
Metabolomic Profiling and Aging Clocks
ML analysis of plasma metabolite data has established powerful "aging clocks" that predict biological age and health outcomes based on metabolomic profiles [65]. In a study of 225,212 UK Biobank participants, researchers applied 17 machine learning algorithms to NMR spectroscopy data encompassing 168 metabolites representing lipid profiles, amino acids, and glycolysis products [65].
Key findings relevant to glucose metabolism research:
- The Cubist rule-based regression model outperformed other algorithms (MAE = 5.31 years)
- Positive "MileAge delta" values (accelerated aging) correlated with frailty, shorter telomeres, and increased mortality risk
- A 1-year increase in MileAge delta corresponded to 4% rise in all-cause mortality risk [65]
These metabolomic aging clocks demonstrate the profound connections between metabolic pathways—including glucose utilization—and systemic aging processes.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Essential Research Reagents for ML-Guided Metabolic Engineering
| Reagent/Resource | Function | Example Application | Key Features |
|---|---|---|---|
| KEGG Database [60] | Pathway information repository | Training data for pathway prediction models | Hierarchical pathway organization, extensive curation |
| REACTOME Database [59] | Curated pathway database | Source of glucose metabolism genes for analysis | Detailed reaction mechanisms, expert curation |
| Cell-Free Expression System [62] | Rapid protein synthesis without living cells | High-throughput enzyme variant testing | Bypasses transformation, enables direct functional testing |
| TCGA Database [59] | Cancer genomics resource | Analyzing metabolic dysregulation in disease | Multi-omics data from clinical samples |
| UK Biobank Metabolomics [65] | Large-scale metabolomic dataset | Training aging clocks and health predictors | NMR spectroscopy, 168 metabolites, 225k+ participants |
| OrthoRep System [64] | In vivo mutagenesis platform | Continuous evolution of target genes | Orthogonal DNA polymerase with high mutation rate |
| CRISPR-EvolvR [64] | CRISPR-mediated directed evolution | Precise in vivo mutations | CRISPR-guided polymerase for targeted diversity |
Machine learning is fundamentally transforming pathway construction, optimization, and enzyme engineering, providing researchers with powerful new methodologies to investigate and manipulate glucose uptake and utilization for ATP production. The integration of ML approaches across multiple scales—from atomic-level enzyme engineering to system-level pathway optimization—enables a more comprehensive understanding of metabolic regulation.
Future developments will likely focus on:
- Increased automation through self-driving laboratories that integrate ML with robotic experimentation
- Enhanced multi-omics data integration for more accurate metabolic state characterization
- Improved generative models for de novo enzyme design beyond natural scaffolds
- Application of large language models for biological knowledge extraction and hypothesis generation
For researchers focused on the mechanisms of glucose uptake and utilization, these ML technologies offer unprecedented capabilities to decipher the complex regulatory networks governing cellular energy production and their dysregulation in disease. By adopting these methodologies, the scientific community can accelerate both fundamental understanding and therapeutic innovation in metabolic research.
Integrating Multi-Omics Data to Decipher Metabolic Network States
The comprehensive understanding of cellular behavior in systems biology relies on dismantling the complex interplay between different regulatory layers that govern metabolism. Metabolic states are governed by a sophisticated hierarchy of controls, ranging from gene expression that sets the theoretical maximum capacity for biochemical reactions to metabolic regulation that fine-tunes actual flux through substrate availability and allosteric interactions [66]. Multi-omics technologies—including transcriptomics, proteomics, and metabolomics—provide detailed snapshots of these molecular processes, yet when analyzed in isolation, they offer limited predictive power for understanding the integrated metabolic phenotype [66]. The central challenge lies in effectively integrating these heterogeneous data types to disassemble the interdependence between different regulatory layers controlling metabolism.
The study of glucose uptake and utilization for ATP production presents a paradigm for understanding these regulatory complexities. Glucose metabolism involves not just the core enzymatic pathways but also the crucial initial step of cellular uptake, mediated by specialized glucose transporters such as GLUT2 in specific tissues [67]. The integration of multi-omics data within structured computational frameworks enables researchers to move beyond correlative observations toward mechanistic models that can predict metabolic flux states under varying physiological and pathological conditions, including metabolic diseases like diabetes and cancer [67] [66].
Computational Frameworks for Multi-Omics Data Integration
Hybrid Modeling Approaches
Hybrid modeling approaches that combine mechanistic knowledge with data-driven machine learning represent the cutting edge in metabolic network reconstruction. The Metabolic-Informed Neural Network (MINN) framework exemplifies this approach by embedding Genome-Scale Metabolic Models (GEMs) within neural network architectures [68]. This hybrid design leverages the structured biochemical knowledge encoded in GEMs while utilizing the pattern recognition capabilities of neural networks to detect complex relationships within multi-omics data. MINN has demonstrated superior performance compared to traditional methods like parsimonious Flux Balance Analysis (pFBA) and Random Forests (RF) in predicting metabolic fluxes in E. coli under different growth conditions and genetic perturbations [68].
The INTEGRATE pipeline provides another sophisticated framework specifically designed to characterize multi-level metabolic regulation by combining transcriptomics and metabolomics data using constraint-based stoichiometric metabolic models as a scaffold [66]. This approach discriminates between reactions controlled primarily at the metabolic level versus those regulated at the gene expression level by intersecting predictions from both data types. The methodology identifies three distinct regulatory modes: transcriptional control (flux variations determined mainly by enzyme abundance), metabolic control (flux variations determined mainly by substrate availability), and combined control (concerted variations in both substrate and enzyme levels) [66].
Addressing Methodological Biases
A critical consideration in pathway analysis of multi-omics data involves understanding the inherent biases of different analytical methods. Recent research utilizing in silico metabolic modeling to simulate metabolic profiles for entire pathway knockouts has revealed that even when a pathway is completely blocked, it may not appear significantly enriched in certain pathway analysis methods [69]. This can result from the chosen analytical method, initial pathway set definition, or the network's inherent structure, potentially leading to false assumptions about the true cause of perturbed metabolic states [69]. These findings highlight the importance of method selection and interpretation caution when applying enrichment-based approaches to metabolomics data.
Methodological Guide for Multi-Omics Integration
Experimental Design and Data Generation
Successful multi-omics integration begins with careful experimental design that ensures biological replicates, matched samples across omics layers, and appropriate temporal resolution for capturing dynamic processes. For studying glucose uptake and ATP production, experimental setups should capture the cascade from transporter expression (transcriptomics/proteomics) through metabolic intermediate abundance (metabolomics) to ultimate flux phenotypes.
Table 1: Core Multi-Omics Data Types for Metabolic Network Analysis
| Data Type | Biological Layer Captured | Key Technologies | Relevance to Glucose Metabolism |
|---|---|---|---|
| Transcriptomics | Gene expression potential | RNA-Seq, Microarrays | Expression of glucose transporters (GLUTs, SGLTs) and metabolic enzymes |
| Proteomics | Enzyme abundance and post-translational modifications | LC-MS/MS, Antibody arrays | Actual levels of hexokinase, GAPDH, pyruvate kinase, ATP synthase subunits |
| Metabolomics | Substrate and metabolite abundances | LC-MS, GC-MS, NMR | Concentrations of glucose, glycolytic intermediates, TCA cycle metabolites, ATP/ADP/AMP |
| Fluxomics | Metabolic reaction rates | 13C tracer analysis, FBA | Direct measurement of glycolytic flux, TCA cycle activity, ATP production rates |
Data Integration Workflow
The INTEGRATE pipeline provides a robust methodological framework for combining transcriptomics and metabolomics data to characterize metabolic regulation [66]:
Differential Reaction Expression Analysis: Compute differential expression of metabolic reactions from transcriptomics data using Gene-Protein-Reaction (GPR) associations encoded in genome-scale metabolic models.
Constraint-Based Flux Prediction: Use constraint-based modeling approaches (e.g., eFlux, TRFBA, GX-FBA) to predict how global differences in gene expression translate to differences in metabolic fluxes. This involves setting flux boundaries as a function of gene expression and scaling fluxes relative to maximum capacity identified through Flux Variability Analysis.
Metabolomic Integration: Incorporate intracellular metabolomics data using mass action law principles to predict how differences in substrate availability translate to flux differences.
Regulatory Level Discrimination: Identify whether each reaction is under transcriptional, metabolic, or combined control by intersecting the predictions from transcriptomics and metabolomics analyses.
Validation and Refinement: Compare predictions with experimental flux measurements where available, and incorporate additional constraints from exo-metabolomics data to improve model accuracy.
Pathway Modeling and Visualization Standards
Effective visualization of integrated metabolic pathways requires adherence to community standards to ensure both human comprehension and computational usability. The following guidelines should be implemented:
Standardized Naming Conventions: Use resolvable identifiers from authoritative databases (UniProt for proteins, ChEBI for metabolites, Ensembl or NCBI for genes) rather than common names or synonyms to ensure computational interoperability [70].
Appropriate Scope and Detail: Determine the appropriate level of detail based on the biological question. For glucose utilization focused on ATP production, detailed representation of glycolytic and oxidative phosphorylation pathways is essential, while peripheral pathways can be condensed [70].
Visual Clarity: Implement high color contrast (minimum 3:1 for adjacent elements), direct labeling of pathway components, and avoidance of color as the sole means of conveying information to ensure accessibility [71].
Diagram 1: Glucose Uptake and ATP Production Pathway
Glucose Transport and Utilization in Context
Glucose Transporter Physiology
The initiation of glucose metabolism depends on cellular uptake mediated by two principal classes of glucose transporters. Sodium-glucose linked transporters (SGLTs) utilize the sodium concentration gradient generated by Na+/K+ ATPase to actively transport glucose against its concentration gradient, with SGLT1 primarily responsible for intestinal glucose absorption and renal reabsorption [72]. Facilitated diffusion glucose transporters (GLUTs) mediate bidirectional glucose transport down concentration gradients, with tissue-specific isoforms fulfilling distinct physiological roles [72].
GLUT2, expressed in pancreatic beta cells, liver, and kidney, plays a crucial role in systemic glucose homeostasis. In pancreatic beta cells, GLUT2 works in concert with glucokinase to facilitate glucose sensing, though research indicates glucokinase rather than the transporter itself serves as the primary sensor [72]. GLUT4 represents another critical transporter as an insulin-responsive isoform present in heart, skeletal muscle, and adipose tissue. Insulin stimulation triggers translocation of GLUT4 from intracellular vesicles to the plasma membrane, resulting in a 10- to 20-fold increase in glucose uptake capacity [72].
ATP Production Pathways
Glucose-derived ATP production occurs through three interconnected biochemical processes: glycolysis, the tricarboxylic acid (TCA) cycle, and oxidative phosphorylation [73]. Glycolysis partially converts glucose to pyruvate in the cytoplasm, generating a net yield of 2 ATP molecules per glucose molecule along with 2 NADH. This process involves key regulatory enzymes including hexokinase, which traps glucose within cells by phosphorylation, and pyruvate kinase, which undergoes allosteric regulation to control glycolytic rate [73].
Under aerobic conditions, pyruvate enters mitochondria and is converted to acetyl-CoA, which fuels the TCA cycle. This mitochondrial cycle completely oxidizes acetyl carbons, generating reduced cofactors (NADH and FADH2) that donate electrons to the electron transport chain. The resulting proton gradient drives ATP synthase to produce the majority of cellular ATP through oxidative phosphorylation [73]. In anaerobic conditions or in specific cell types like erythrocytes and many cancer cells, pyruvate is reduced to lactate, regenerating NAD+ for continued glycolytic flux but with substantially lower ATP yield per glucose molecule [73].
Table 2: ATP Production from Glucose Metabolism Pathways
| Metabolic Pathway | Location | Net ATP per Glucose | Regulatory Enzymes | Conditions |
|---|---|---|---|---|
| Glycolysis | Cytoplasm | 2 ATP + 2 NADH | Hexokinase, PFK-1, Pyruvate Kinase | Universal first step |
| Pyruvate Dehydrogenase | Mitochondria | 0 ATP (2 NADH) | PDH complex | Aerobic only |
| TCA Cycle | Mitochondria | 2 ATP + 6 NADH + 2 FADH2 | Citrate synthase, Isocitrate DH, α-KG DH | Aerobic only |
| Oxidative Phosphorylation | Mitochondria | ~25-30 ATP (from NADH/FADH2) | ATP synthase | Aerobic only |
| Lactic Fermentation | Cytoplasm | 2 ATP | Lactate dehydrogenase | Anaerobic/Warburg effect |
Essential Research Reagents and Tools
Table 3: Research Reagent Solutions for Multi-Omics Metabolic Studies
| Reagent/Tool Category | Specific Examples | Function in Research | Application Context |
|---|---|---|---|
| Genome-Scale Metabolic Models | Recon3D, AGORA, EcoCyc | Structured biochemical knowledge bases | Constraint-based flux prediction [68] [66] |
| Pathway Analysis Databases | Reactome, WikiPathways, KEGG, BioCyc | Curated pathway information | Pathway enrichment analysis, model construction [70] |
| Multi-Omics Integration Tools | INTEGRATE pipeline, MINN, NEXT-FBA | Computational data integration | Hybrid modeling, regulatory level discrimination [68] [66] [74] |
| Glucose Transport Assays | Radiolabeled 2-DG, GLUT-specific inhibitors | Quantify glucose uptake capacity | Functional validation of transporter activity |
| Metabolic Tracers | 13C-glucose, 15N-glutamine, 2H2O | Track metabolic flux patterns | Experimental flux determination [69] |
| ATP Measurement Assays | Luciferase-based kits, HPLC | Quantify ATP production and energy charge | Validation of metabolic state predictions |
Applications in Disease Research and Therapeutic Development
The integration of multi-omics data to decipher metabolic network states finds particularly valuable application in understanding and treating human diseases with metabolic components. In cancer research, analyses of breast cancer cell lines have revealed how metabolic rewiring contributes to proliferation and survival, informing targeted therapeutic strategies [66]. The INTEGRATE pipeline successfully discriminates reactions controlled at the metabolic versus transcriptional level, enabling identification of key regulatory nodes that could serve as therapeutic targets [66].
In metabolic disorders such as diabetes, understanding the regulation of glucose transporters provides insights into disease mechanisms and treatment opportunities. Genetic variations in SGLT1 cause glucose-galactose malabsorption, while SGLT2 defects lead to renal glucosuria [72]. The natural loss or downregulation of GLUT2 causes abnormal blood glucose concentrations, including fasting hypoglycemia and glucose intolerance [67]. These findings have spurred development of SGLT2 inhibitors as clinically effective diabetes medications that promote urinary glucose excretion.
The hybrid modeling approaches like MINN and NEXT-FBA offer promising platforms for drug development by enabling more accurate predictions of metabolic responses to perturbations, potentially reducing the need for extensive experimental screening [68] [74]. These models can simulate the metabolic effects of transporter inhibition or enzyme modulation, helping prioritize the most promising therapeutic targets before costly experimental validation.
Diagram 2: Multi-Omics Data Integration Workflow
Future Directions and Implementation Recommendations
The field of multi-omics integration for metabolic network analysis continues to evolve rapidly. Future advancements will likely focus on dynamic modeling approaches that capture temporal relationships between omics layers, moving beyond the static snapshots currently enabled by most frameworks. Additionally, incorporation of spatial omics technologies will provide critical insights into subcellular compartmentalization of metabolic processes, particularly important for understanding glucose metabolism where mitochondrial and cytoplasmic pools of metabolites serve distinct functions.
For researchers implementing these approaches, we recommend:
Structured Model Reuse: Begin with existing, curated genome-scale metabolic models and pathway databases rather than building entirely new frameworks, following the principle of "reuse and extend" to maximize reproducibility and interoperability [70].
Multi-method Validation: Employ multiple complementary integration methods (e.g., both MINN and INTEGRATE) to mitigate methodological biases and strengthen conclusions, particularly given the demonstrated limitations of individual pathway analysis methods [69].
Iterative Experimental-Computational Cycles: Design research programs that alternate between computational predictions and experimental validations, using targeted flux measurements and transporter activity assays to refine models.
Standardized Visualization and Reporting: Adhere to community standards for pathway modeling and visualization to ensure both human comprehension and computational reusability, implementing sufficient color contrast and explicit labeling [70] [71].
As these methodologies mature, integrated multi-omics approaches will increasingly enable predictive modeling of metabolic responses to genetic, environmental, and therapeutic perturbations, advancing both basic understanding of glucose metabolism and development of targeted interventions for metabolic diseases.
Dysregulation and Intervention in Disease and Therapy
{start of main content}
Insulin Resistance and Glucose Uptake Defects in Type 2 Diabetes Pathophysiology
Type 2 diabetes (T2D) is characterized by a fundamental defect in insulin-mediated glucose disposal, primarily due to insulin resistance in skeletal muscle, liver, and adipose tissue. This pathological state disrupts the finely tuned process of glucose uptake and its subsequent utilization for ATP production, leading to systemic hyperglycemia. The molecular etiology involves defects in the proximal insulin signaling cascade, endoplasmic reticulum (ER) stress, mitochondrial dysfunction, and inflammatory pathways. These disruptions collectively impair the translocation of the glucose transporter GLUT4 to the cell membrane and alter metabolic fluxes, reducing substrate availability for oxidative phosphorylation. This whitepaper provides an in-depth analysis of the molecular mechanisms underlying insulin resistance and glucose uptake defects, framed within the context of bioenergetic research. It further summarizes key quantitative findings, details essential experimental methodologies, and visualizes critical signaling pathways and their dysregulation, offering a comprehensive resource for researchers and drug development professionals.
Insulin resistance is identified as an impaired biologic response to insulin stimulation in target tissues, primarily skeletal muscle, liver, and adipose tissue [75]. This resistance impairs glucose disposal, leading to a compensatory increase in beta-cell insulin production and hyperinsulinemia [75]. The metabolic consequences include hyperglycemia, dyslipidemia, and a heightened risk for cardiovascular disease [75] [76]. From a bioenergetic perspective, insulin resistance represents a critical failure in the organism's ability to efficiently direct nutrient substrates toward ATP production. In skeletal muscle—the tissue responsible for up to 80% of postprandial glucose disposal [77]—insulin resistance manifests as a blunted ability to translocate GLUT4 to the plasma membrane, severely limiting glucose entry into myocytes [78]. This defect in the initial step of fuel acquisition creates a cellular energy deficit and, paradoxically, a systemic surplus of energy-rich substrates, which in turn drives pathogenic processes such as ectopic lipid accumulation and glucotoxicity. Understanding the molecular pathways that link defective insulin signaling to impaired mitochondrial ATP production is therefore central to developing therapies that restore metabolic flexibility and energy homeostasis.
Molecular Mechanisms of Insulin Signaling and Defects
The Canonical Insulin Signaling Pathway and GLUT4 Translocation
Insulin exerts its effects by binding to the insulin receptor (INSR), a receptor tyrosine kinase on the plasma membrane of target cells [79]. This binding induces a conformational change, resulting in trans-autophosphorylation of the INSR β-subunit and the recruitment and tyrosine phosphorylation of insulin receptor substrate (IRS) proteins [78] [77]. Phosphorylated IRS then activates phosphoinositide 3-kinase (PI3K), which catalyzes the production of phosphatidylinositol (3,4,5)-trisphosphate (PIP3) [77]. PIP3 serves as a docking site for proteins such as 3-phosphoinositide-dependent protein kinase 1 (PDK1), which, along with mTORC2, phosphorylates and activates AKT [77]. AKT activation is a central node in insulin signaling; its downstream effects include the phosphorylation and inhibition of GSK3 to promote glycogen synthesis [77]. Critically, AKT phosphorylates AS160 (TBC1D4), inactivating its Rab-GTPase activity [78]. This leads to the translocation of intracellular GLUT4 storage vesicles (GSVs) to the plasma membrane, facilitating glucose uptake [78] [77].
The following diagram illustrates this core signaling pathway and its primary disruptions in the insulin-resistant state.
Primary Molecular Defects in Insulin Resistance
In insulin resistance, the canonical signaling pathway is disrupted at multiple points, leading to a failure in GLUT4 translocation and glucose uptake. Key mechanisms include:
- Inflammatory Signaling: Obesity and overnutrition create a state of chronic, low-grade inflammation. This activates stress kinases such as JNK and IKKβ, which phosphorylate IRS proteins on serine residues, disrupting their interaction with the insulin receptor and marking them for degradation [78] [76].
- Lipotoxicity: Ectopic accumulation of lipid metabolites, particularly diacylglycerol (DAG) and ceramides, is a hallmark of insulin-resistant skeletal muscle [77]. DAG activates Protein Kinase C theta (PKCθ), which serine-phosphorylates and inhibits IRS1 [77]. Ceramides activate PKCζ and protein phosphatase 2A (PP2A), leading to the dephosphorylation and inhibition of AKT, thereby blocking GLUT4 translocation [77].
- Endoplasmic Reticulum (ER) Stress: Chronic nutrient excess disrupts ER homeostasis, leading to the activation of the unfolded protein response (UPR) [80]. Sustained ER stress activates JNK, contributing to inhibitory serine phosphorylation of IRS, and can also trigger the degradation of key proteins, including insulin receptors and glucose transporters like GLUT2 and GLUT4, via autophagy [81].
Quantitative Data on Metabolic and Molecular Defects
Table 1: Quantitative Metabolic Defects in Human Insulin Resistance and T2D
| Parameter / Measurement | Normal / Control Value | Insulin-Resistant / T2D Value | Experimental Context & Notes | Source |
|---|---|---|---|---|
| Whole-Body Glucose Disposal | ~8-12 mg/kg/min | Reduced by ~40-50% | Hyperinsulinemic-euglycemic clamp (gold standard). | [79] |
| Muscle Mitochondrial ATP Production | Baseline level | ↓ 25-30% after 8-9h insulin deprivation | Type 1 diabetic subjects; measured in muscle. | [82] |
| Fasting Insulin Level | <10 μU/mL | Often >15-20 μU/mL | Indicator of compensatory hyperinsulinemia. | [75] [76] |
| Proinsulin Synthesis Rate | Basal level | ↑ Up to 25-fold upon glucose stimulation | Imposes a heavy biosynthetic burden on pancreatic β-cells. | [80] |
| HOMA-IR Index | ~1.0 | >2.5 (commonly used cutoff) | Homeostatic Model Assessment of Insulin Resistance. | [75] |
| Insulin Receptor Kinase Activity | Normal activity | Decreased in obese/diabetic muscle | Measured in skeletal muscle biopsies. | [78] |
Table 2: Key Molecular Changes in Target Tissues
| Target Tissue | Molecular Defect / Alteration | Observed Change in Insulin Resistance | Functional Consequence | Source |
|---|---|---|---|---|
| Skeletal Muscle | IRS-1 Tyrosine Phosphorylation | Decreased | Impaired proximal insulin signaling. | [78] |
| Skeletal Muscle | Intramyocellular DAG / Ceramide | Increased | Activation of PKCθ/PKCζ and inhibition of IRS/AKT. | [77] |
| Skeletal Muscle | Insulin-stimulated GLUT4 Translocation | Markedly Impaired | Primary defect reducing glucose uptake. | [78] |
| Liver | GLUT2 & GLUT4 Protein Levels | Decreased (Hyperglycemia model) | ER stress-mediated autophagic degradation. | [81] |
| Liver | Hepatic Glucose Output (HGP) | Failed suppression by insulin | Contributes to fasting hyperglycemia. | [78] [79] |
| Adipose Tissue | Suppression of Lipolysis by Insulin | Impaired | Increased circulating Free Fatty Acids (FFAs). | [75] [79] |
| Pancreatic β-cell | IRE1α-XBP1 & PERK-eIF2α Signaling | Dysregulated (Glucolipotoxicity) | Contributes to β-cell dysfunction and apoptosis. | [80] |
Detailed Experimental Protocols for Key Investigations
Hyperinsulinemic-Euglycemic Clamp (Gold Standard In Vivo Assessment)
Objective: To quantitatively assess whole-body insulin sensitivity in vivo [75] [79].
Procedure:
- Subject Preparation: After an overnight fast, intravenous catheters are placed in an antecubital vein for infusion and in a contralateral hand vein for blood sampling (with the hand kept in a heated box ~55°C for arterialized venous blood).
- Primed-Continuous Insulin Infusion: A primed, continuous intravenous infusion of insulin (e.g., 40 mU/m²/min) is initiated to rapidly raise and maintain plasma insulin at a super-physiological, fixed level (e.g., ~100 μU/mL).
- Variable Glucose Infusion: A variable 20% glucose infusion is simultaneously started and adjusted based on frequent (typically every 5 min) plasma glucose measurements to "clamp" the blood glucose concentration at a predetermined basal level (e.g., 90-100 mg/dL).
- Steady-State Measurement: The clamp is maintained for at least 120 minutes. Once a steady state is achieved (where blood glucose is stable and exogenous glucose infusion rate (GIR) matches glucose disposal), the GIR is recorded.
- Data Analysis: The GIR required to maintain euglycemia is a direct measure of whole-body insulin sensitivity. A lower GIR indicates greater insulin resistance.
Assessing GLUT4 Translocation in Skeletal Muscle (In Vitro)
Objective: To measure the translocation of GLUT4 from intracellular vesicles to the plasma membrane in response to insulin [78].
Procedure:
- Cell Culture or Muscle Explants: Use differentiated human or rodent myotubes (e.g., L6 or C2C12 cell lines) or isolated muscle strips.
- Experimental Incubation: Incubate cells/tissues in low-serum media for several hours. Stimulate with a physiological dose of insulin (e.g., 100 nM) for a defined period (e.g., 15-30 min). Include control groups without insulin.
- Cell Fractionation: Rapidly lyse cells using a homogenization buffer. Separate the plasma membrane (PM) fraction from the low-density microsome (LDM) fraction (containing intracellular GLUT4 vesicles) using differential centrifugation (e.g., ~19,000 g pellet for PM; ~180,000 g pellet for LDM).
- Immunoblotting: Resolve proteins from PM and LDM fractions by SDS-PAGE. Perform Western blotting using antibodies specific for GLUT4.
- Data Analysis: Quantify band intensity. Insulin sensitivity is indicated by an increase in the PM GLUT4 to LDM GLUT4 ratio. Validate fraction purity by blotting for marker proteins (e.g., Na+/K+ ATPase for PM).
Evaluating ER Stress and UPR Signaling in Liver
Objective: To investigate the activation of the Unfolded Protein Response (UPR) and its impact on glucose transporter expression in hepatocytes under hyperglycemic conditions [81].
Procedure:
- Cell Culture and Treatment: Culture human hepatoma cells (HepG2) and treat with high glucose medium (e.g., 30 mM D-glucose) for various durations (e.g., 6h, 24h, 72h). A control group should be maintained in normal glucose (e.g., 5.5 mM). Optionally, treat with a chemical chaperone (e.g., 4-PBA) or an ER stress inducer (e.g., Tunicamycin) as controls.
- Protein Extraction and Western Blot: Lyse cells and quantify total protein. Resolve proteins by SDS-PAGE and transfer to a membrane.
- Probing for UPR and GLUT Proteins: Probe the membrane with specific antibodies:
- UPR Activation: Phospho-PERK (Thr980), Total PERK, Phospho-eIF2α (Ser51), ATF4, CHOP, XBP1s.
- Autophagy Markers: LC3B-I/II, p62/SQSTM1.
- Glucose Transporters: GLUT2, GLUT4.
- Loading Control: β-actin.
- Immunofluorescence Microscopy: Plate cells on coverslips. After treatment, fix, permeabilize, and stain for GLUT2/GLUT4 and an ER marker (e.g., PDI). Use fluorescent secondary antibodies and confocal microscopy to visualize transporter localization and abundance.
- Data Analysis: A hallmark of ER stress-mediated degradation is a time-dependent decrease in GLUT2/GLUT4 protein levels, concurrent with increased UPR marker expression and LC3-II accumulation, which can be reversed by ER stress inhibitors.
Visualization of Experimental Workflow
The following diagram outlines a generalized, integrated workflow for investigating insulin resistance mechanisms, from in vivo phenotyping to in vitro molecular dissection.
The Scientist's Toolkit: Key Research Reagents
| Category | Reagent / Resource | Function / Application | Key Notes / Example Targets |
|---|---|---|---|
| Cell & Tissue Models | C2C12 / L6 GLUT4-myc myoblasts | In vitro model for studying insulin-stimulated GLUT4 translocation. | Engineered with an exofacial myc-epitope tag for quantitative surface staining. |
| Primary human skeletal myocytes | Physiologically relevant model for human metabolic studies. | Retain donor phenotype; crucial for translational research. | |
| HepG2 / Primary Hepatocytes | Model for studying hepatic insulin resistance, gluconeogenesis, and lipid metabolism. | Used in hyperglycemia/ER stress studies [81]. | |
| Critical Antibodies | Phospho-Specific Antibodies | Detect activated signaling proteins. | p-AKT (Ser473), p-IRS-1 (Tyr612/Ser636), p-eIF2α (Ser51) [81]. |
| Total Protein Antibodies | Measure total protein abundance. | Insulin Rβ, IRS-1, AKT, GLUT4, GLUT2, β-Actin [81]. | |
| UPR & Autophagy Antibodies | Probe ER stress and degradation pathways. | PERK, CHOP, ATF4, LC3B, p62/SQSTM1 [80] [81]. | |
| Chemical Modulators | Insulin (Human Recombinant) | Primary hormone for stimulation assays. | Used in clamps and cell culture. |
| PI3K Inhibitors (e.g., LY294002) | Tool to establish necessity of PI3K/AKT pathway. | Confirms pathway specificity in glucose uptake. | |
| ER Stress Inducers/Inhibitors | Manipulate ER homeostasis. | Tunicamycin (inducer), 4-PBA/TUDCA (chaperones, inhibitors). | |
| Lipid Metabolites (e.g., Palmitate) | Induce lipotoxicity and insulin resistance in vitro. | Complexed with BSA for cell culture treatment. | |
| Assay Kits | Glucose Uptake Assay Kits | Quantify cellular glucose uptake. | Use 2-NBDG or fluorescent/colorimetric glucose analogs. |
| ELISA for Hormones/Cytokines | Measure plasma/tissue levels of key factors. | Insulin, Adiponectin, TNF-α, IL-6. | |
| Mitochondrial Stress Test Kits | Assess OXPHOS and mitochondrial function (Seahorse). | Measures OCR (Oxygen Consumption Rate). |
{end of main content}
Metabolic reprogramming is a established hallmark of cancer, enabling rapidly proliferating cells to meet their heightened demands for energy, biosynthetic precursors, and redox homeostasis [83] [84]. A pivotal manifestation of this reprogramming is the Warburg effect, or aerobic glycolysis, wherein cancer cells preferentially metabolize glucose to lactate even in the presence of sufficient oxygen to support mitochondrial oxidative phosphorylation (OXPHOS) [85] [83]. This metabolic shift, first observed by Otto Warburg, is surprisingly ubiquitous across cancer types and provides a selective advantage by facilitating rapid ATP generation, supplying carbon skeletons for nucleotides, lipids, and amino acids, and maintaining cellular redox balance [85]. The transition is driven by oncogenic signals, such as MYC, RAS, and HIF-1α, which orchestrate the overexpression of key glycolytic enzymes and glucose transporters (GLUTs) [86] [83]. This guide details the molecular mechanisms underlying the Warburg effect, explores its functional consequences for the tumor microenvironment (TME) and immune evasion, and outlines associated therapeutic vulnerabilities and state-of-the-art research methodologies for investigators in the field.
The rewiring of glucose metabolism is initiated by a surge in glucose uptake, primarily mediated by the upregulation of facilitative glucose transporters, with GLUT1 being frequently overexpressed in a wide array of malignancies, including colorectal carcinoma (CRC) and others [86]. Intracellular glucose is rapidly phosphorylated by hexokinase 2 (HK2), a transcriptional target of oncogenes like MYC and HIF-1α, trapping glucose within the cell and committing it to glycolytic processing [83]. The metabolic flux is further channeled by the activity of key enzymes such as pyruvate kinase M2 (PKM2) and lactate dehydrogenase A (LDHA), which favor the production of lactate from pyruvate, cementing the glycolytic phenotype [85] [83]. The resulting lactate is exported from the cancer cells, acidifying the TME. This acidosis promotes tumor invasion, metastasis, and immune suppression by inhibiting cytotoxic T cells and polarizing macrophages towards a pro-tumoral M2 phenotype [85] [83]. Beyond glycolysis, glucose metabolism interfaces with other critical pathways. The pentose phosphate pathway (PPP) is often enhanced, generating NADPH to combat oxidative stress and providing ribose-5-phosphate for nucleotide synthesis, thereby supporting rapid proliferation and survival [83].
Therapeutic Targeting of Glycolytic Dependencies
The profound reliance of many cancers on aerobic glycolysis presents a strategic vulnerability for targeted therapy. Key nodes of the glycolytic pathway, including specific isoforms of transporters and enzymes, are being prioritized for interventional strategies.
Table 1: Key Therapeutic Targets in Cancer Glycolysis
| Therapeutic Target | Function in Glycolysis | Therapeutic Agent / Approach | Mechanism of Action | Noteworthy Context |
|---|---|---|---|---|
| GLUT1 [86] | Facilitates glucose entry into cells | Small molecule inhibitors (from synthetic lethality screens) | Block glucose uptake, starving cancer cells of their primary fuel | Tumor-specific GLUTs are promising for targeted therapy. |
| Hexokinase 2 (HK2) [83] | Catalyzes the first committed step of glycolysis | 2-deoxy-D-glucose (2-DG) | Competitive inhibitor that mimics glucose, reducing G6P production | A transcriptional target of HIF-1α; drives oncogenic functions. |
| Lactate Dehydrogenase A (LDHA) [85] [83] | Converts pyruvate to lactate, a key step in the Warburg effect | Pharmacological or epigenetic inhibition | Disrupts lactate production, dampening the Warburg effect | A transcriptional target of MYC; its product, lactate, acidifies the TME. |
| PKM2 [85] [83] | Converts PEP to pyruvate; can interact with HIF-1α | Targeted inhibition | Alters glycolytic flux and disrupts pro-tumorigenic signaling | Its expression is often upregulated in early-stage premalignant lesions. |
| ALDOB [85] | A key enzyme in fructose metabolism that bypasses glycolytic rate-limiting steps | ALDOB inhibition | Disrupts fructose-driven amplification of glycolytic flux and NADPH production | Targets the synergistic effect of fructose metabolism in promoting CRC aggressiveness. |
| G6PD [83] | Rate-limiting enzyme of the PPP | 6-aminonicotinamide | Reduces NADPH levels, sensitizing cells to oxidative stress and radiotherapy | Critical for redox homeostasis; regulated by NRF2. |
A significant challenge in targeting glycolysis is the metabolic plasticity of cancer cells. For instance, inhibition of glycolytic enzymes can be circumvented by a compensatory upregulation of mitochondrial OXPHOS or other complementary pathways like the TCA cycle and glutamine metabolism [85]. This underscores the necessity for multi-targeted or combinatorial approaches, such as dual inhibition of HK2 and G6PD, which has shown synergistic effects in preclinical models [83]. Furthermore, the "reverse Warburg effect" describes a metabolic symbiosis where cancer-associated fibroblasts (CAFs) undergo glycolysis and export lactate, which is then utilized by adjacent cancer cells for OXPHOS, presenting another layer of complexity for therapeutic design [85]. Finally, a critical consideration is the potential for on-target toxicities, as several key nodes of the Embden–Meyerhof–Parnas (EMP) pathway are also essential for normal tissues with high glycolytic demand, such as the brain and retina [85].
Experimental Analysis of Metabolic Flux
Understanding and quantifying metabolic activity in real-time is crucial for basic research and for assessing therapeutic efficacy. Advanced technologies now enable sensitive, dynamic tracking of metabolic fluxes.
Table 2: Experimental Methods for Analyzing Glycolytic Flux
| Methodology | Key Reagents / Tools | Primary Readout | Key Advantage | Example Application |
|---|---|---|---|---|
| Hyperpolarized Micromagnetic Resonance Spectrometer (HMRS) [84] | Hyperpolarized [1-13C]pyruvate | Real-time conversion of pyruvate to lactate, quantified as a metabolic flux metric (ξ) | 1000x more sensitive than conventional DNP-NMR; requires only ~10^4 cells; non-destructive to cells | Profiling metabolic flux in leukemia stem cells (LSCs) and renal cell carcinoma. |
| Multimodal Optical Imaging (SIMPLE Platform) [87] | Label-free autofluorescence (NAD(P)H, FAD) and multiharmonic generation (SHG, THG) | Fluorescence lifetime imaging (FLIM) and phasor analysis to decompose free/bound NAD(P)H; collagen structure | Label-free, rapid histopathological assessment of fresh tissue; reveals metabolic state and tissue architecture | Identifying metastatic margins and analyzing cancer invasion in pancreatic cancer models. |
| Metabolomic & Imaging Diagnostics [85] | 18F-fluorodeoxyglucose (FDG) for PET/CT; Mass spectrometry | FDG uptake (correlates with glucose uptake and hexokinase activity); circulating metabolite profiles | Non-invasive clinical tool for tumor detection, staging, and monitoring; reveals distinct metabolic signatures | Early detection and disease stratification in colorectal cancer (CRC). |
The HMRS platform exemplifies a major technological leap. It utilizes a microcoil to achieve a 1000-fold increase in sensitivity over conventional nuclear magnetic resonance (NMR), allowing for the quantification of the pyruvate-to-lactate conversion rate—a direct measure of glycolytic flux—in mass-limited samples like primary cancer cells and stem cells within minutes, all while preserving cell viability for downstream analyses [84]. Separately, the SIMPLE platform integrates confocal, nonlinear, and fluorescence lifetime microscopy to provide a label-free, metabolic analysis of fresh tissue. By measuring the autofluorescence of NAD(P)H and FAD and applying phasor-based FLIM, it can discriminate the metabolic signatures of cancer cells and map the metastatic colonization within tissues, offering profound insights into the tumor microenvironment [87].
Diagram 1: Key nodes and pathways in cancer glycolysis
The Scientist's Toolkit: Key Research Reagents
This table catalogues essential reagents and tools for investigating the Warburg effect and glycolytic dependencies in cancer models.
Table 3: Research Reagent Solutions for Glycolysis Studies
| Reagent / Tool | Function / Application | Key Feature / Consideration |
|---|---|---|
| Hyperpolarized [1-13C]pyruvate [84] | NMR-based tracer for real-time monitoring of pyruvate-to-lactate conversion in live cells. | Enables quantification of glycolytic flux (kPL); requires specialized HMRS or DNP-NMR equipment. |
| 2-Deoxy-D-Glucose (2-DG) [83] | Competitive HK2 inhibitor; mimics glucose to disrupt glycolytic flux. | A canonical tool for probing glycolytic dependence; used in preclinical models to assess tumor growth. |
| 6-Aminonicotinamide [83] | Inhibitor of G6PD, the rate-limiting enzyme of the PPP. | Useful for studying redox balance and nucleotide synthesis; can be combined with glycolytic inhibitors. |
| 13C-enriched metabolites (e.g., [U-13C]glucose) [84] | Tracers for detailed mapping of carbon fate in metabolic pathways via mass spectrometry or NMR. | Provides comprehensive view of pathway utilization (glycolysis, TCA, PPP); requires analytical infrastructure. |
| Label-free Autofluorescence Imaging (NAD(P)H, FAD) [87] | Assessing cellular metabolic status via fluorescence lifetime imaging microscopy (FLIM). | Non-invasive; reveals ratio of free/bound NAD(P)H, indicative of glycolytic vs. oxidative metabolism. |
| siRNA/shRNA against HK2, LDHA, PKM2 [83] | Genetic knockdown to validate the functional role of specific glycolytic enzymes. | Confirms target specificity and explores compensatory metabolic mechanisms. |
Diagram 2: HMRS workflow for metabolic flux analysis
Cellular energy production is a fundamental process governed by thermodynamics and kinetic efficiency. The journey of glucose from extracellular space to intracellular ATP involves traversing several potential bioenergetic bottlenecks, points where the flow of energy is constrained by thermodynamic inefficiencies or kinetic limitations. Within the context of glucose uptake and utilization for ATP production, these bottlenecks often manifest at the stages of membrane transport, phosphorylation, and mitochondrial oxidative phosphorylation. Overcoming these constraints is essential for optimizing the driving forces that make these processes efficient. This whitepaper delves into the thermodynamic constraints inherent in cellular energy production, with a specific focus on the mechanism of glucose uptake and utilization, and provides a detailed analysis of strategies to optimize the driving forces that overcome these bioenergetic bottlenecks. The principles of driving force optimization are not merely academic; they have direct implications for therapeutic drug development in areas ranging from metabolic disorders like diabetes and heart failure to cancer and neurodegenerative diseases [88] [89] [90].
Core Thermodynamic Principles and Bioenergetic Bottlenecks
Fundamental Thermodynamic Constraints
At its core, cellular bioenergetics is governed by the laws of thermodynamics. The adenylate energy charge (AEC), a quantitative measure of the energy status of a cell, and the ATP/ADP ratio are key indicators of a cell's thermodynamic state [91]. AEC is calculated as ([ATP] + 0.5[ADP]) / ([ATP] + [ADP] + [AMP]). When ATP consumption outpaces production, cells experience bioenergetic stress, characterized by a decreased ATP/ADP ratio and AEC [91]. This state impairs growth and can amplify metabolic processes like glycolysis and oxidative phosphorylation in an attempt to restore energy homeostasis. Furthermore, the sodium ion gradient (ΔNa+) across the plasma membrane, maintained by the Na+/K+ ATPase, is a crucial driving force for secondary active transport systems. This electrochemical gradient is a form of stored energy that powers the uphill transport of nutrients like glucose, directly linking ion homeostasis to metabolic fueling [92] [93].
Identified Bioenergetic Bottlenecks
The pathway from glucose to ATP is punctuated by several key bottlenecks, as illustrated in the diagram below, which depicts the interconnected stages and their primary constraints.
Diagram 1: Key bioenergetic bottlenecks in the glucose-to-ATP pathway.
Research indicates that bioenergetic stress, defined by a low ATP/ADP ratio and AEC, is a significant metabolic bottleneck that can paradoxically potentiate antimicrobial resistance and persistence in bacteria, highlighting its broad impact on cellular physiology [91]. In mammalian cells, the efficiency of glucose transporter systems and the subsequent metabolic flux through glycolysis and OXPHOS are critical determinants of the overall bioenergetic output [88] [90].
Glucose Uptake Systems: Kinetic and Thermodynamic Properties
Facilitative Glucose Transporters (GLUTs)
The GLUT family of facilitative transporters allows glucose to move down its concentration gradient. A prime example is GLUT2, a low-affinity, high-capacity transporter expressed in the hypothalamus, pancreas, liver, and kidneys [88]. Its kinetic properties enable rapid equilibration of glucose across cell membranes, making it a critical glucose sensor in hypothalamic neurons that regulate food intake and energy homeostasis [88]. Structurally, GLUT2 comprises 12 transmembrane domains and functions as a reversible carrier. Dysfunction in GLUT2 is linked to metabolic diseases; for instance, reduced GLUT2 levels in pancreatic β-cells are observed in diabetes, correlating with a loss of glucose-stimulated insulin secretion [88].
Sodium-Driven Glucose Transporters (SGLTs)
In contrast to GLUTs, Sodium-glucose cotransporters (SGLTs) utilize the energy stored in the sodium electrochemical gradient to actively transport glucose against its concentration gradient. They are secondary active transporters belonging to the SLC5A family [92]. SGLT1 is a high-affinity, low-capacity transporter primarily responsible for intestinal glucose and galactose absorption and reclaims the remaining ~10% of glucose in the S3 segment of the renal proximal tubule [92]. SGLT2, a low-affinity, high-capacity transporter located in the S1/S2 segments of the renal tubule, is responsible for reabsorbing approximately 80-90% of filtered glucose, preventing its loss in urine [92]. The transport model for SGLTs, such as the cloned Na+/glucose cotransporter, is described by a 6-state ordered kinetic model with a Na+:glucose stoichiometry of 2:1 for SGLT1 [93]. In this model, carrier translocation and Na+ binding/dissociation are voltage-dependent, and the main effect of the membrane potential is on carrier translocation [93].
Table 1: Comparative Analysis of Key Glucose Transporters
| Transporter | Type | Stoichiometry (Na+:Glucose) | Affinity | Capacity | Primary Tissue Expression | Key Function |
|---|---|---|---|---|---|---|
| GLUT2 [88] | Facilitative | N/A | Low (Km ~17 mM) | High | Pancreatic β-cells, Liver, Hypothalamus, Kidneys | Basolateral glucose efflux, systemic glucose sensing |
| GLUT3 [88] | Facilitative | N/A | High | High | Neurons | Primary neuronal glucose uptake |
| GLUT1 [88] | Facilitative | N/A | High | High | Brain endothelial, Erythrocytes, Astrocytic endfeet | Basal glucose uptake, blood-brain barrier |
| SGLT1 [92] | Secondary Active | 2:1 | High | Low | Small Intestine, Renal S3 Tubule Segment | Intestinal absorption, final renal reabsorption (~10%) |
| SGLT2 [92] | Secondary Active | 1:1 | Low | High | Renal S1/S2 Tubule Segments | Primary renal reabsorption (~90%) |
Driving Force Optimization: Strategies and Experimental Assessment
Optimizing Electrochemical Gradients
The driving force for SGLT-mediated glucose transport is the transmembrane sodium gradient. Maintaining this gradient is thermodynamically expensive, consuming a significant portion of cellular ATP via the Na+/K+ ATPase. Optimization can be achieved by ensuring robust mitochondrial ATP production to fuel this pump. Furthermore, the membrane potential itself facilitates transport; a negative membrane potential inside the cell accelerates SGLT1-mediated sugar transport by favoring the translocation of the charged carrier [93]. Kinetic modeling indicates that at 0 mV and saturating substrate concentrations, the rate-limiting step for the SGLT1 transporter is the translocation of the empty carrier. As the membrane potential becomes more negative, this step accelerates, and internal Na+ dissociation becomes increasingly rate-limiting [93].
Targeting Transporters and Metabolic Pathways
Pharmacological inhibition of SGLT2 has emerged as a powerful clinical strategy to optimize whole-body bioenergetics. By blocking renal glucose reabsorption, SGLT2 inhibitors like empagliflozin and dapagliflozin promote urinary glucose excretion, thereby reducing hyperglycemia in diabetes [92]. Beyond glycemic control, these inhibitors have demonstrated unexpected benefits in heart failure. It is proposed that SGLT2 inhibitors improve cardiomyocyte energetics by restoring the mitochondrial respiratory chain and reducing aberrant Ca/calmodulin-dependent kinase II activity, although the precise mechanisms are still under investigation [89]. This represents a form of driving force optimization at the organ level, improving the heart's metabolic efficiency. In cancer, the bioenergetic bottleneck often shifts. While many tumors exhibit high glycolysis (the Warburg effect), some resistant tumors activate mitochondrial OXPHOS [90]. Targeting this pathway with OXPHOS inhibitors is being explored as an alternative therapy for resistant cancers, effectively creating a lethal bioenergetic bottleneck for the malignancy [90].
Experimental Protocols for Studying Bioenergetic Flux
Metabolomic Profiling for Energy Status
Objective: To quantitatively measure intracellular energy status and identify bioenergetic stress. Methodology (LC-MS/MS Metabolomics):
- Cell Quenching: Rapidly cool cells in a cold methanol bath (-40°C) to instantly halt metabolic activity.
- Metabolite Extraction: Use a pre-chilled mixture of methanol:acetonitrile:water (40:40:20, v/v) for extraction. Lyse cells via freeze-thaw cycles or sonication on ice.
- Sample Analysis: Centrifuge to pellet debris and analyze the supernatant via Liquid Chromatography with tandem mass spectrometry (LC-MS/MS).
- Data Quantification: Quantify key metabolites: ATP, ADP, AMP, NAD+, NADH, and TCA cycle intermediates. Calculate the Adenylate Energy Charge (AEC) =
([ATP] + 0.5[ADP]) / ([ATP] + [ADP] + [AMP])and ATP/ADP ratio [91]. Application: This protocol was used to demonstrate that ciprofloxacin treatment in E. coli significantly decreases intracellular ATP, NADH, AEC, and ATP/ADP, confirming antibiotic-induced bioenergetic stress [91].
Functional Transport Assays
Objective: To characterize the kinetic parameters (Km, Vmax) and voltage dependence of glucose transporters. Methodology (Heterologous Expression in Oocytes):
- mRNA Microinjection: Synthesize and purify mRNA coding for the target transporter (e.g., hSGLT1). Microinject this mRNA into Xenopus laevis oocytes.
- Incubation: Allow 3-5 days for protein expression.
- Electrophysiology: Use a two-electrode voltage clamp to measure transporter-associated currents. Hold the oocyte membrane potential at a set voltage (e.g., -50 mV) and superfuse with solutions containing Na+ and/or glucose analogs like α-Methyl-D-glucopyranoside (αMDG).
- Data Analysis: The induced currents are proportional to transport activity. By varying substrate concentrations and membrane potential, kinetic parameters and voltage dependence can be derived and fitted to a 6-state ordered kinetic model [93].
Structural Biology for Inhibitor Design
Objective: To obtain high-resolution structures of transporters to guide rational drug design. Methodology (Cryo-Electron Microscopy):
- Protein Purification: Express and purify the target transporter (e.g., hSGLT1) in a membrane mimetic environment.
- Grid Preparation: Embed the protein in vitreous ice on a cryo-EM grid.
- Data Collection: Image the samples in an electron microscope under cryo-conditions, collecting thousands of micrographs.
- Image Processing: Use computational single-particle analysis to reconstruct a high-resolution 3D density map.
- Model Building: Build an atomic model of the transporter, often with an inhibitor bound (e.g., LX2761 in SGLT1), to reveal the binding mode and molecular basis for selectivity [92]. This structural information is crucial for designing selective SGLT1 inhibitors, an ongoing challenge in the field.
The following diagram outlines a consolidated workflow integrating these key experimental approaches to systematically identify and characterize bioenergetic bottlenecks.
Diagram 2: Integrated experimental workflow for bioenergetic bottleneck analysis.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagent Solutions for Bioenergetic and Transport Studies
| Reagent / Material | Function / Application | Experimental Context |
|---|---|---|
| LX2761 [92] | Selective SGLT1 inhibitor; used to probe SGLT1 function and for co-crystallization in structural studies. | Cryo-EM structure determination of human SGLT1. |
| Empagliflozin [92] [89] | Selective SGLT2 inhibitor; used to study renal glucose handling and cardiac energetics. | Investigating cardiometabolic improvements in heart failure models. |
| α-Methyl-D-glucopyranoside (αMDG) [93] | Non-metabolizable glucose analog; used to study transport kinetics without interference from metabolism. | Voltage-clamp studies of SGLT kinetics in oocytes. |
| Triphenylphosphonium (TPP) [94] | A lipophilic cation used to conjugate and target compounds to mitochondria, leveraging the mitochondrial membrane potential. | Delivering therapeutic or probe molecules to mitochondria in cancer cells. |
| Ciprofloxacin [91] | A fluoroquinolone antibiotic that induces bioenergetic stress, decreasing ATP/ADP and AEC. | Modeling bioenergetic stress and its link to antimicrobial resistance evolution. |
| Soluble F1 ATP synthase (pF1 plasmid) [91] | Genetic construct for constitutive ATP hydrolysis; used to induce bioenergetic stress by lowering ATP/ADP. | Synthetic biology approach to study the effects of bioenergetic stress in E. coli. |
| NADH Oxidase (pNOX plasmid) [91] | Genetic construct for constitutive NADH oxidation; used to induce redox and bioenergetic stress. | Synthetic biology approach to study the effects of altered NADH/NAD+ ratio. |
Overcoming bioenergetic bottlenecks requires a deep and integrated understanding of thermodynamic constraints across the entire system of glucose uptake and utilization. The optimization of driving forces—from the sodium electrochemical gradient powering SGLT transporters to the mitochondrial proton gradient driving ATP synthesis—is paramount. Modern research, powered by advanced techniques in metabolomics, structural biology (cryo-EM), and computational modeling, is rapidly elucidating the molecular details of these processes. This knowledge is directly translating into novel therapeutic strategies, evidenced by the success of SGLT2 inhibitors in diabetes and heart failure, and the ongoing development of OXPHOS inhibitors and mitochondrial-targeted agents like TPP conjugates for cancer. The continued focus on understanding and manipulating these fundamental bioenergetic principles will undoubtedly yield new avenues for intervention in a wide spectrum of human diseases.
The canonical insulin signaling pathway, centered on phosphatidylinositol-3 kinase (PI3K) and Akt, has long been recognized as the primary mechanism regulating glucose uptake. However, emerging research has identified several novel signaling molecules that play critical roles in glucose homeostasis, both independently of and in concert with traditional insulin signaling. This whitepaper provides an in-depth technical analysis of three key emerging regulators: the Rho GTPase Rac1, the Tether containing a UBX domain for GLUT4 (TUG), and the adipokine Isthmin-1 (Ism1). We examine their mechanisms of action, quantitative contributions to glucose uptake, dysregulation in metabolic disease states, and potential as therapeutic targets for conditions such as type 2 diabetes and insulin resistance. The synthesis of these findings redefines our understanding of glucose uptake mechanisms and reveals new opportunities for therapeutic intervention in metabolic disorders.
Skeletal muscle accounts for approximately 75% of postprandial glucose disposal in humans, making normal insulin action in this tissue crucial for maintaining systemic glucose homeostasis [95]. While the PI3K-Akt pathway remains a cornerstone of insulin-stimulated glucose transport, evidence now indicates that Akt alone does not fully account for all insulin-mediated glucose uptake [96]. This recognition has spurred investigation into complementary and alternative pathways that regulate the translocation of glucose transporter type 4 (GLUT4) vesicles to the plasma membrane.
The actin cytoskeleton plays a previously underappreciated role in GLUT4 trafficking, with dynamic rearrangement necessary for efficient transporter translocation [95]. Furthermore, insulin-independent pathways offer additional therapeutic opportunities, particularly valuable in insulin-resistant states. This whitepaper examines three recently characterized key players—Rac1, TUG, and Isthmin-1—that represent significant advances in our understanding of glucose uptake regulation. For researchers investigating glucose metabolism and ATP production, these pathways offer new mechanistic insights and potential intervention points for improving metabolic health.
Rac1: A Master Regulator of GLUT4 Trafficking
Mechanism of Action and Signaling Pathway
Rac1, a member of the Rho family of GTPases, regulates insulin-stimulated GLUT4 translocation by initiating cortical actin remodeling, creating the structural framework necessary for GLUT4 vesicle movement to the plasma membrane [97]. Upon insulin stimulation, Rac1 is activated through a PI3K-dependent mechanism, though it functions independently of Akt [97]. Active Rac1 (Rac1-GTP) then signals through its downstream effector, p21-activated kinase (PAK), which phosphorylates substrates on threonine 423 (PAKThr423) to facilitate cytoskeletal reorganization [95].
Table 1: Key Experimental Findings on Rac1 in Glucose Metabolism
| Experimental Model | Key Finding | Effect on Glucose Uptake | Citation |
|---|---|---|---|
| Muscle-specific Rac1 KO mice | Decreased insulin-stimulated glucose transport in soleus and EDL muscles | ~55% reduction in soleus, 20-58% in EDL | [95] |
| High-fat diet mice | Impaired Rac1 activation and decreased PAKThr423 phosphorylation | Contributes to insulin resistance | [95] |
| Human skeletal muscle (obese/T2D) | Reduced insulin-stimulated PAK activation | Correlates with insulin resistance | [95] [98] |
| Pharmacological Rac1 inhibition | Blunted insulin-stimulated glucose uptake | Similar to genetic knockout | [95] |
| Contraction stimulation | Rac1 activation during exercise | Regulates exercise-mediated glucose uptake | [99] |
This pathway is crucial for both insulin-stimulated and contraction-stimulated glucose uptake, representing a convergence point for multiple physiological stimuli [99]. Rac1 activation leads to the formation of actin remodeling structures that guide GLUT4-containing vesicles to specific membrane compartments, including transverse tubules in mature skeletal muscle [95].
Dysregulation in Metabolic Disease
Rac1 signaling is significantly compromised in insulin-resistant states. In high-fat-fed mice, both Rac1 protein expression and insulin-stimulated PAK phosphorylation are markedly decreased [95]. Human studies confirm these findings, demonstrating impaired insulin-stimulated PAK activation in both acute (lipid infusion-induced) and chronic (obesity and type 2 diabetes) insulin-resistant states [95] [98].
A key mechanism underlying Rac1 dysfunction in metabolic disease appears to be the upregulation of guanine dissociation inhibitor alpha (GDIɑ), a natural inhibitor of Rac1 activation [96]. This dysregulation represents a specific defect in the insulin signaling cascade that occurs independently of Akt signaling, which often remains intact in insulin-resistant muscle despite reduced glucose uptake [97].
Experimental Approaches and Protocols
Genetic Manipulation Models
- Inducible Muscle-Specific Rac1 Knockout: Cross Rac1-floxed mice with transgenic mice expressing Cre recombinase under control of the human skeletal actin promoter and tetracycline-responsive element. Induce knockout with doxycycline (1 g/L in drinking water for 21 days) [95].
- Phenotypic Assessment: Conduct glucose tolerance tests (intraperitoneal injection of 2 g/kg glucose after 6-hour fast) and insulin tolerance tests (0.5 units insulin/kg after 2-hour fast) with blood collection at 0, 20, 40, 60, 90, and 120 minutes for glucose and insulin measurements [95].
Ex Vivo Muscle Incubation
- Muscle Preparation: Dissect soleus and extensor digitorum longus (EDL) muscles from fasted mice (4 hours) and suspend at resting tension (4-5 mN) in incubation chambers with Krebs-Ringer-Henseleit buffer containing 2 mmol/L pyruvate and 8 mmol/L mannitol at 30°C [95].
- Rac1 Inhibition: Preincubate muscles for 40 minutes with Rac1 Inhibitor II (10 μmol/L) or vehicle control (DMSO) [95].
- Glucose Uptake Measurement: Stimulate with insulin (60 nmol/L) for 30 minutes, then measure 2-deoxyglucose uptake using [3H]2DG and [14C]mannitol tracers during the final 10 minutes of stimulation [95].
TUG: Regulator of GLUT4 Vesicle Sequestration and Release
Mechanism of Action
Tether containing a UBX domain for GLUT4 (TUG) functions as a intracellular tether that sequesters GLUT4-containing vesicles in a stable storage compartment near the Golgi apparatus and endoplasmic reticulum [96]. In the basal state, TUG maintains a reservoir of GLUT4 vesicles within the cell interior. Upon insulin stimulation, proteolytic cleavage of TUG releases these vesicles, allowing their trafficking to the plasma membrane [96].
The insulin-dependent cleavage of TUG not only mobilizes GLUT4 vesicles but also generates a C-terminal TUG fragment that translocates to the nucleus, where it drives the expression of genes involved in oxidative metabolism and thermogenesis [96]. This dual function links acute glucose uptake to longer-term metabolic adaptations.
Dysregulation in Metabolic Disease
In insulin-resistant states, the TUG-regulated GLUT4 storage system becomes compromised. The insulin-responsive vesicle pool is depleted, and TUG cleavage is impaired [96]. Consequently, the cell loses the ability to rapidly mobilize GLUT4 to the cell surface in response to elevated blood glucose levels, contributing to the hyperglycemia characteristic of type 2 diabetes.
Isthmin-1: An Insulin-Mimetic Adipokine with Unique Properties
Discovery and Signaling Mechanism
Isthmin-1 (Ism1) is a recently identified adipokine secreted by thermogenic adipose tissue that promotes glucose uptake through a novel mechanism. Although Ism1 activates the PI3K-AKT signaling pathway similarly to insulin, it notably does not signal through the insulin receptor [96] [100]. This unique receptor engagement allows Ism1 to achieve selective insulin-mimetic effects while avoiding certain undesirable insulin actions.
Table 2: Comparative Analysis of Isthmin-1 vs. Insulin Signaling
| Characteristic | Isthmin-1 | Insulin |
|---|---|---|
| Secretory Source | Thermogenic adipose tissue | Pancreatic β-cells |
| Primary Receptor | Unknown (not insulin receptor) | Insulin receptor |
| Signaling Pathway | PI3K-AKT | PI3K-AKT |
| GLUT4 Translocation | Promotes | Promotes |
| Hepatic Lipid Synthesis | Suppresses | Promotes |
| Adipose Glucose Uptake | Increases | Increases |
| Therapeutic Potential | Dual benefit for diabetes and fatty liver | Limited by lipogenic effects |
Ism1 is expressed almost exclusively in mature adipocytes, with higher expression in brown adipose tissue (BAT) compared to white adipose tissue (WAT), and is further induced by cold exposure [100]. The protein undergoes N-linked glycosylation and may form dimers or oligomers under native conditions [100].
Metabolic Effects and Therapeutic Potential
Ism1 exhibits a unique dissociation of metabolic effects, increasing peripheral glucose uptake while simultaneously suppressing hepatic lipid synthesis [100]. This dual action addresses two key pathological features of metabolic syndrome—hyperglycemia and hepatic steatosis—making it particularly attractive as a therapeutic candidate.
Genetic ablation of Ism1 in mice results in impaired glucose tolerance, reduced adipose glucose uptake, and decreased insulin sensitivity, confirming its endogenous role in glucose regulation [100]. Conversely, therapeutic administration of recombinant Ism1 improves diabetic parameters in diet-induced obese mice and ameliorates hepatic steatosis in a fatty liver mouse model [100].
Clinical Correlations and Experimental Methodology
Circulating Ism1 Measurement
- Sample Preparation: Collect blood in EDTA tubes, centrifuge at 400× g for 10 minutes at room temperature to separate plasma. Recentrifuge at 800× g for 10 minutes, aliquot supernatant, and store at -80°C [101].
- ELISA Protocol: Thaw plasma samples at room temperature, centrifuge at 10,000× g for 5 minutes to remove particulates. Use commercial Ism1 ELISA kits following manufacturer protocols [101].
Clinical Associations
Human studies reveal complex relationships between circulating Ism1 and metabolic health:
- Kuwaiti Adult Study (n=450): Lower Ism1 levels associated with obesity, insulin resistance, metabolic-associated fatty liver disease (MAFLD), and type 2 diabetes [101].
- Macrovascular Complications: Ism1 levels are elevated in type 2 diabetes patients with macrovascular complications compared to those without, and positively correlate with HbA1c, HOMA-IR, and triglyceride levels [102].
These apparently contradictory findings—both protective associations and compensatory elevations in disease states—suggest a complex physiological role for Ism1 that merits further investigation.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating Novel Glucose Uptake Pathways
| Reagent / Model | Specific Example | Research Application | Key Findings Enabled |
|---|---|---|---|
| Rac1 Inhibitors | NSC23766 [103] | Inhibits Rac1-GEF interaction | Blocks serum/PDGF-induced Rac1 activation and lamellipodia formation |
| Rac1 Inhibitor II [95] | Pharmacological Rac1 inhibition | Reduces insulin-stimulated glucose uptake in mouse muscle ex vivo | |
| Genetic Models | Inducible muscle-specific Rac1 KO mice [95] | Tissue-specific Rac1 ablation | Established Rac1 requirement for insulin- and contraction-stimulated glucose uptake |
| Ism1 knockout mice [100] | Whole-body Ism1 ablation | Demonstrated Ism1's endogenous role in glucose tolerance | |
| Recombinant Proteins | Recombinant Ism1 (C-terminal myc-his tag) [100] | Therapeutic administration | Improved diabetes and hepatic steatosis in mouse models |
| Antibodies | Anti-phospho-PAKThr423 [95] | Detection of Rac1 pathway activity | Revealed impaired Rac1 signaling in insulin-resistant human muscle |
Integrated View of Glucose Uptake Regulation
The emerging understanding of glucose uptake regulation reveals a multi-layered control system with both convergent and parallel pathways. While Rac1 and TUG operate within the broader insulin signaling framework, Isthmin-1 represents a distinct insulin-mimetic pathway with unique metabolic properties.
These pathways exhibit significant crosstalk and compensation. For instance, when Rac1 is knocked out in muscle tissue, increased Akt phosphorylation and glucose uptake occur in adipose tissue, suggesting inter-tissue compensation [97]. Similarly, Ism1 appears to be upregulated in obesity as a counter-regulatory mechanism to combat insulin resistance [96].
From a therapeutic perspective, these novel pathways offer several advantages over traditional insulin-centric approaches:
- Rac1 activation could bypass insulin signaling defects in muscle [95] [98]
- TUG cleavage enhancement might restore GLUT4 vesicle pools in insulin resistance [96]
- Isthmin-1 therapy could improve glycemia without promoting hepatic lipogenesis [100]
The identification of Rac1, TUG, and Isthmin-1 as regulators of glucose uptake significantly expands our understanding of metabolic regulation beyond the canonical insulin signaling pathway. These discoveries reveal new layers of complexity in the control of glucose homeostasis and offer promising avenues for therapeutic intervention in metabolic diseases.
Future research should focus on:
- Elucidating the precise receptor mechanism for Isthmin-1
- Developing specific activators of Rac1 signaling
- Understanding the protease system responsible for TUG cleavage
- Exploring potential crosstalk between these novel pathways
- Investigating tissue-specific contributions to whole-body glucose homeostasis
For researchers studying glucose utilization for ATP production, these pathways represent important modulators of substrate availability that must be considered in comprehensive models of cellular energy metabolism. The continued dissection of these mechanisms will not only advance fundamental knowledge but may also yield novel therapeutic strategies for the simultaneous treatment of multiple metabolic disorders, including type 2 diabetes and fatty liver disease.
Therapeutic Targeting of Metabolic Enzymes and Transporters in Drug Development
Cellular metabolism, particularly the processes of glucose uptake and utilization for adenosine triphosphate (ATP) production, represents a fundamental axis in maintaining physiological homeostasis. The reprogramming of these metabolic pathways is a hallmark of numerous diseases, including cancer, type 2 diabetes (T2D), and neurodegenerative disorders, making their constituent enzymes and transporters attractive targets for therapeutic intervention [104] [105]. This guide examines the strategic targeting of key components in glucose metabolism, focusing on the mechanistic insights and experimental approaches that inform modern drug development. The core of this approach lies in understanding the "metabolic currency" of the cell: ATP. This molecule provides readily releasable energy in the bond between its second and third phosphate groups, hydrolyzing to ADP or AMP and releasing approximately 30.5 kJ/mol (7.3 kcal/mol) of energy to drive essential cellular processes [106] [107]. The high demand for ATP—cells hydrolyze 100 to 150 moles of ATP per day—necessitates efficient continuous production, primarily through the oxidative metabolism of glucose [106]. It is this critical dependency on ATP-producing pathways that offers a vulnerable node for therapeutic manipulation in disease states.
Core Targets in Glucose Metabolism
Glucose Transporters (GLUTs)
The first regulatory checkpoint for glucose utilization is its transport across the plasma membrane, mediated by a family of facilitative glucose transporters (GLUTs). GLUT1 is ubiquitously expressed and is critical for basal glucose uptake. Its overexpression is a common feature in many cancers, supporting the enhanced glycolytic activity and rapid proliferation of tumor cells, a phenomenon known as the Warburg effect [105] [104]. In contrast, GLUT4 is expressed primarily in skeletal muscle and adipose tissue and is responsible for insulin-stimulated glucose uptake. Its dysregulation is a central feature of insulin resistance in T2D and obesity [6]. A novel layer of regulation for GLUT1 has recently been described, wherein upon growth factor stimulation, GLUT1 co-endocytoses with receptors (like PDGFR) into vesicles that localize near mitochondria, delivering glucose directly to the glycolytic machinery [108]. This discovery redefines the paradigm of glycolytic regulation by cellular membrane dynamics.
Mitochondrial Transporters and Metabolic Reprogramming
Following cytosolic glycolysis, the mitochondrial pyruvate carrier (MPC) shuttles pyruvate into the mitochondrial matrix for oxidative phosphorylation. Dysregulation of MPC and other mitochondrial transporters (MTs), such as the citrate carrier (SLC25A1) and dicarboxylate carrier (SLC25A10), disrupts energy metabolism and contributes to the pathogenesis of cancer, neurodegenerative diseases, and T2D [104] [109]. In cancer, metabolic reprogramming (MR) supports tumor growth through aerobic glycolysis, glutaminolysis, and altered lipid metabolism [104]. Targeting these MTs offers significant therapeutic potential, with inhibitors of glutamine transporters and the voltage-dependent anion channel (VDAC1) currently under exploration to disrupt tumor metabolism [104].
Key Metabolic Enzymes
The glycolytic pathway is controlled by several rate-limiting enzymes. Hexokinase (HK) catalyzes the first committed step, phosphorylating glucose to glucose-6-phosphate. Phosphofructokinase-1 (PFK1) is the primary control point of glycolysis and is allosterically inhibited by high ATP concentrations, providing a negative feedback loop when cellular energy is sufficient [106] [107]. Pyruvate kinase (PK) catalyzes the final step, generating ATP and pyruvate. These enzymes often localize in proximity to mitochondria or on specialized signaling vesicles to optimize metabolic flux [108] [104].
Table 1: Key Therapeutic Targets in Glucose Metabolism for ATP Production
| Target | Class | Primary Function | Therapeutic Rationale | Associated Diseases |
|---|---|---|---|---|
| GLUT1 (SLC2A1) | Transporter | Basal glucose uptake | Overexpressed in tumors; supports Warburg effect [105] | Various Cancers |
| GLUT4 (SLC2A4) | Transporter | Insulin-stimulated glucose uptake | Downregulated in insulin resistance; improves glycemic control if activity is increased [6] | Type 2 Diabetes, Obesity |
| SGLT2 (SLC5A2) | Transporter | Renal glucose reabsorption | Inhibition promotes urinary glucose excretion, reducing blood glucose [110] | Type 2 Diabetes |
| Mitochondrial Pyruvate Carrier (MPC) | Transporter | Pyruvate import into mitochondria | Dysfunction drives insulin resistance and metabolic dysregulation [104] | Type 2 Diabetes, Cancer |
| Hexokinase (HK) | Enzyme | First glycolysis step | Often overexpressed in cancer; inhibition blocks glycolytic flux [108] | Various Cancers |
| Phosphofructokinase (PFK1) | Enzyme | Rate-limiting glycolysis step | Key regulatory node; inhibited by ATP [106] | Cancer, Metabolic Syndromes |
Quantitative Data on Inhibitors and Modulators
The development of inhibitors against metabolic targets has yielded a diverse array of compounds, both natural and synthetic, with defined mechanisms and anti-disease efficacy.
Table 2: Inhibitors of Glucose Metabolism Targets
| Compound | Target | Molecular Structure | Mechanism of Action / Effect | Experimental Context |
|---|---|---|---|---|
| WZB117 | GLUT1 | Synthetic Inhibitor | Blocks glucose transport; activates AMPK; inhibits mTOR; impairs DNA repair; enhances radiotherapy sensitivity [105] | Breast cancer cells (MCF7, MDA-MB-231) [105] |
| 2-Deoxy-D-Glucose (2-DG) | GLUT1, Hexokinase | Glucose analog | Competitive inhibitor; phosphorylated by HK but not metabolized further, accumulating and inhibiting glycolysis [105] | Breast, Pancreatic, Liver cancer models [105] |
| Apigenin | GLUT1 (indirect) | Natural Flavonoid | Reduces GLUT1 expression via PI3K/Akt pathway; increases cisplatin and radiotherapy sensitivity [105] | Laryngeal cancer models (Hep-2 cells) [105] |
| Curcumin | GLUT1 (indirect) | Natural Product | Induces autophagy and apoptosis; enhances radiotherapy sensitivity, especially with GLUT1 AS-ODN [105] | Laryngeal cancer models [105] |
| Canagliflozin | SGLT2 | C-glucoside | Binds outward-facing conformation of SGLT2, inhibiting renal glucose reabsorption [110] | Approved drug for Type 2 Diabetes [110] |
| Phlorizin | SGLT2/SGLT1 | O-glucoside | Binds inward-open conformation of SGLT2; natural product progenitor of gliflozins [110] | Experimental model for diabetes research [110] |
Experimental Protocols for Key Assays
Protocol: Nanoparticle-Based Isolation of Endocytic Vesicles for GLUT1 Trafficking Studies
This protocol isolates endocytic vesicles containing GLUT1 and growth factor receptors to study a novel glucose uptake mechanism [108].
Principle: Streptavidin-coated magnetic iron oxide nanoparticles (10 nm diameter) conjugated to biotinylated PDGF-BB ligand bind to PDGFR on the cell surface. Upon ligand stimulation, the receptor-ligand-nanoparticle complex is endocytosed. Vesicles containing these complexes are magnetically isolated.
Procedure:
- Cell Culture and Starvation: Culture Swiss 3T3 fibroblasts (or other relevant cell line) to 70-80% confluence. Serum-starve cells for 12-24 hours to arrest growth and suppress basal signaling.
- Nanoparticle Conjugation: Conjugate biotinylated PDGF-BB to streptavidin-coated magnetic iron oxide nanoparticles in a sterile, serum-free buffer for 30 minutes on ice.
- Stimulation and Endocytosis: Add the PDGF-BB-conjugated nanoparticles to starved cells. Incubate at 37°C for 5-10 minutes to allow receptor binding and endocytosis. Include controls: cells with nanoparticles + free PDGF-BB (competition control), and cells with nanoparticles at 4°C (endocytosis inhibition control).
- Surface Stripping: Place cells on ice and immediately wash with a cold, low-pH buffer (e.g., glycine-HCl, pH 2.5-3.0) to remove nanoparticles bound to the cell surface without internalizing.
- Cell Lysis and Fractionation: Wash cells with cold PBS and lyse using a gentle, non-ionic detergent lysis buffer. Centrifuge the lysate at low speed (e.g., 1,000 × g) to remove nuclei and generate a post-nuclear supernatant.
- Magnetic Affinity Purification: Pass the post-nuclear supernatant through a magnetic separation column placed in a strong magnetic field. The nanoparticle-containing endocytic vesicles will be retained in the column.
- Vesicle Elution and Analysis: Elute the bound vesicles by removing the column from the magnetic field and applying elution buffer. Analyze the eluate by:
- Immunoblotting: Probe for GLUT1, PDGFR, endosomal markers (EEA1, clathrin), and glycolytic enzymes (HK2, GPI, etc.).
- Mass Spectrometry (LC-MS/MS): For an unbiased proteomic analysis of the vesicle contents.
Protocol: Kinetic Binding Assay for Drug-Target Residence Time
Measuring the kinetics of drug-target binding (kon and koff) provides critical information beyond equilibrium affinity (Kd), which is essential for predicting in vivo efficacy, especially for drugs targeting the central nervous system where exposure may be low [111].
Principle: A surface plasmon resonance (SPR) or similar biosensor-based assay can be used. The target protein (e.g., a purified enzyme or transporter) is immobilized on a sensor chip. A solution of the drug candidate is flowed over the chip, and the binding (association) is measured in real-time. The drug solution is then replaced with buffer, and the dissociation of the drug from the target is measured.
Procedure:
- Target Immobilization: Purify the recombinant target protein (e.g., SGLT2, a kinase). Use standard amine-coupling or other chemistry to immobilize the protein on a biosensor chip surface at a density that minimizes mass transport effects.
- Association Phase (kon): Prepare a dilution series of the drug candidate in a suitable running buffer. Flow each concentration over the immobilized target surface for a fixed period (e.g., 2-5 minutes) at a constant flow rate. The biosensor records the association curve (Response Units vs. Time).
- Dissociation Phase (koff): Switch the flow to drug-free buffer and monitor the decrease in signal as the drug dissociates from the target for a sufficient time (e.g., 10-60 minutes).
- Data Analysis:
- Fit the association and dissociation phases globally to a 1:1 binding model (or other appropriate model) using the biosensor's software.
- The software will calculate the association rate constant (kon, units: M⁻¹s⁻¹) and the dissociation rate constant (koff, units: s⁻¹).
- Calculate the equilibrium dissociation constant: Kd = koff / kon.
- Calculate the target residence time: τ = 1 / koff.
Significance: A long residence time (slow koff) can sustain target engagement even after systemic drug concentration has declined, which is a valuable property for drugs with poor penetration or short plasma half-lives [111].
Pathway and Workflow Visualizations
Insulin and Growth Factor Signaling in Glucose Uptake
This diagram illustrates the classical (GLUT4) and newly discovered (GLUT1) pathways regulating glucose uptake.
Workflow for Isolating GLUT1 Endocytic Vesicles
This diagram outlines the experimental workflow for studying the novel GLUT1 endocytosis mechanism.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating Glucose Transport and Metabolism
| Reagent / Tool | Category | Function in Research | Example Application |
|---|---|---|---|
| Biotinylated Ligands & Magnetic Nanoparticles | Protein & Cell Assay | To isolate specific ligand-induced endocytic vesicles for proteomic analysis [108]. | Studying GLUT1/PDGFR co-endocytosis [108]. |
| SGLT2-MAP17 Co-expression System | Protein Production | Essential for producing stable, functional human SGLT2 protein for structural and biochemical studies [110]. | Determining cryo-EM structures of SGLT2 with inhibitors [110]. |
| 2-Deoxy-D-Glucose (2-DG) | Metabolic Inhibitor | Competitive inhibitor of hexokinase and GLUT1; used to block glycolytic flux [105]. | Studying dependence on glycolysis in cancer cells [105]. |
| WZB117 | Synthetic Inhibitor | Specific small-molecule inhibitor of GLUT1-mediated glucose transport [105]. | Evaluating anti-cancer effects of GLUT1 blockade in vitro and in vivo. |
| Surface Plasmon Resonance (SPR) | Instrumentation / Assay | Measures binding kinetics (kon, koff) and affinity (Kd) between a drug and its purified target [111]. | Determining drug-target residence time for lead optimization [111]. |
| Cryo-Electron Microscopy (Cryo-EM) | Structural Biology | Determines high-resolution 3D structures of proteins and protein-drug complexes in near-native states [110]. | Elucidating inhibition mechanisms of SGLT2 by gliflozins [110]. |
Conclusion
The intricate process of glucose uptake and ATP production is governed by a highly regulated network of transporters, enzymes, and signaling molecules, extending far beyond a simple linear pathway. Foundational knowledge, combined with advanced methodologies like real-time NMR and machine learning, is revolutionizing our capacity to map and manipulate cellular metabolism. Understanding dysregulation in diseases such as diabetes and cancer provides critical insights for troubleshooting and reveals novel therapeutic targets. Future directions must focus on integrating these multi-faceted approaches to design precise metabolic interventions, optimize cell-based therapies, and develop next-generation drugs that target the core energetic infrastructure of the cell, ultimately translating mechanistic understanding into clinical breakthroughs.
References
- 1. Glucose Transporter Proteins | News-Medical [https://www.news-medical.net/life-sciences/Glucose-Transporter-Proteins.aspx]
- 2. Human Glucose Transporters in Health and Selected ... [https://www.mdpi.com/1422-0067/26/15/7392]
- 3. advancing toward selective SGLT1 inhibition - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605011/]
- 4. Glucose transporter - Wikipedia [https://en.wikipedia.org/wiki/Glucose_transporter]
- 5. Glucose transporters in adipose tissue , liver, and skeletal muscle in... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7462924/]
- 6. Physiology, Glucose Transporter Type 4 - StatPearls - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK537322/]
- 7. Recent Progress in the Development of Glucose ... [https://pubmed.ncbi.nlm.nih.gov/39746141/]
- 8. Glucose Transport - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/glucose-transport]
- 9. Mechanism of substrate recognition and release of human ... [https://www.nature.com/articles/s41467-025-62421-6]
- 10. The Adipose Tissue-Derived Secretome (ADS) in Obesity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384572/]
- 11. Transport of Small Molecules - The Cell - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK9847/]
- 12. Glucose uptake [https://en.wikipedia.org/wiki/Glucose_uptake]
- 13. [Secondary active transport] [https://pubmed.ncbi.nlm.nih.gov/3017449/]
- 14. Active transport [https://en.wikipedia.org/wiki/Active_transport]
- 15. Low‐Glucose Culture Conditions Bias Neuronal Energetics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12178110/]
- 16. An impaired glycolysis induces ATP deficiency and ... [https://www.nature.com/articles/s41598-025-22327-1]
- 17. Catabolism of Glucose (1)- Stages 1-3 of Cellular Respiration [https://bio.libretexts.org/Courses/Prince_Georges_Community_College/PGCC_Microbiology/07%3A_Microbial_Metabolism/7.02%3A_Catabolism_of_Glucose_(1)-_Stages_1-3_of_Cellular_Respiration]
- 18. Biochemistry, Glycolysis - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK482303/]
- 19. Glucose Catabolism: Energy Releasing Pathways [https://www.employees.csbsju.edu/ssaupe/biol121/respiration.htm]
- 20. Physiology, Glucose Metabolism - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK560599/]
- 21. Exercise-stimulated glucose uptake — regulation and ... [https://www.nature.com/articles/nrendo.2016.162]
- 22. Self-organizing glycolytic waves tune cellular metabolic ... [https://www.nature.com/articles/s41467-025-60596-6]
- 23. 8.2: Overview of Glycolysis [https://chem.libretexts.org/Bookshelves/General_Chemistry/Book%3A_Structure_and_Reactivity_in_Organic_Biological_and_Inorganic_Chemistry_(Schaller)/III%3A_Reactivity_in_Organic_Biological_and_Inorganic_Chemistry_1/08%3A_Mechanisms_of_Glycolysis/8.02%3A_Overview_of_Glycolysis]
- 24. Carbohydrate catabolism [https://en.wikipedia.org/wiki/Carbohydrate_catabolism]
- 25. Protocol to quantitatively assess glycolysis and related ... [https://www.sciencedirect.com/science/article/pii/S2666166725001923]
- 26. The Mechanism of Oxidative Phosphorylation - The Cell - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK9885/]
- 27. The TCA Cycle - Steps - Krebs Cycle [https://teachmephysiology.com/biochemistry/atp-production/tca-cycle-2/]
- 28. Citric acid cycle [https://en.wikipedia.org/wiki/Citric_acid_cycle]
- 29. ATP is not consumed solely by hydrolytic reactions [https://pmc.ncbi.nlm.nih.gov/articles/PMC12548155/]
- 30. Oxidative phosphorylation [https://en.wikipedia.org/wiki/Oxidative_phosphorylation]
- 31. Review article Mitochondrial electron transport chain [https://www.sciencedirect.com/science/article/pii/S221323172030879X]
- 32. Biochemical and Molecular Mechanisms of Glucose Uptake ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7021273/]
- 33. 8.11: Hormonal Regulation of Metabolism [https://chem.libretexts.org/Courses/Brevard_College/CHE_301_Biochemistry/08%3A_Metabolism_of_carbohydrates/8.11%3A_Hormonal_Regulation_of_Metabolism]
- 34. Hormonal Regulation of Metabolism | Biology for Majors II [https://courses.lumenlearning.com/wm-biology2/chapter/hormonal-regulation-of-metabolism/]
- 35. Glucagon in metabolic disease: a mini-review of emerging ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1645041/full]
- 36. Regulatory interaction between metabolite transporters ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289959/]
- 37. Regulation of Insulin Receptor Pathway and Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6014550/]
- 38. Insulin signaling and its application [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1226655/full]
- 39. Insight into the Mechanism of d-Glucose Accelerated ... [https://pubmed.ncbi.nlm.nih.gov/39874207]
- 40. Hyperpolarized 13C NMR Reveals Pathway Regulation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11397382/]
- 41. Mapping real-time metabolic kinetics of expanded CAR T ... [https://www.nature.com/articles/s41598-025-24712-2]
- 42. Real-Time Metabolic Detection in Living Cells Using ... [https://www.jove.com/t/68539/real-time-metabolic-detection-living-cells-using-hyperpolarized-13c]
- 43. Hyperpolarized 13C NMR observation of lactate kinetics in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4644943/]
- 44. Molecular detection of inflammation in cell models using ... [https://www.thno.org/v08p3400.htm]
- 45. Guide to Metabolomics Analysis: A Bioinformatics Workflow [https://pmc.ncbi.nlm.nih.gov/articles/PMC9032224/]
- 46. Mitochondrial ATP generation is more proteome efficient than ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11925356/]
- 47. Metabolomic insights of cultured meat compared to ... [https://www.nature.com/articles/s41598-025-00719-7]
- 48. Metabolomics Data Analysis | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/industrial/mass-spectrometry/mass-spectrometry-learning-center/mass-spectrometry-applications-area/metabolomics-mass-spectrometry/metabolomics-data-analysis.html]
- 49. Visualizing Metabolomics Data: Graphical Insights [https://metabolomics.creative-proteomics.com/resource/visualizing-metabolomics-data-graphical-insights.htm]
- 50. Metabolomics and nutrient intake reveal metabolite–nutrient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366009/]
- 51. Selective utilization of glucose metabolism guides ... [https://www.nature.com/articles/s41586-024-08044-1]
- 52. Combining Metabolomics and Interpretable Machine Learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8630631/]
- 53. Genome-Scale Metabolic Modeling Enables In-Depth ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8778254/]
- 54. Current status and applications of genome-scale metabolic ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-019-1730-3]
- 55. Construction of Multiscale Genome-Scale Metabolic Models [https://pmc.ncbi.nlm.nih.gov/articles/PMC9139095/]
- 56. Reconstruction of a catalogue of genome-scale metabolic ... [https://www.nature.com/articles/s41467-022-31421-1]
- 57. Genome-scale models of metabolism and expression ... [https://www.sciencedirect.com/science/article/pii/S1096717624000788]
- 58. Glucose Transport - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/glucose-transport]
- 59. Machine learning-based analysis identifies glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479329/]
- 60. Advancements in Predicting Biomolecule Pathways - Simple Science [https://scisimple.com/en/articles/2025-07-10-advancements-in-predicting-biomolecule-pathways--a98mz68]
- 61. Generative machine learning produces kinetic models that ... [https://www.nature.com/articles/s41929-024-01220-6]
- 62. Accelerated enzyme engineering by machine-learning guided cell-free expression | Nature Communications [https://www.nature.com/articles/s41467-024-55399-0]
- 63. Automated in vivo enzyme engineering accelerates ... [https://www.nature.com/articles/s41467-024-46574-4]
- 64. Enzyme Engineering: Performance Optimization, Novel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11639928/]
- 65. reveals how metabolite profiles predict aging and... Machine learning [https://www.news-medical.net/news/20250101/Machine-learning-reveals-how-metabolite-profiles-predict-aging-and-health.aspx]
- 66. INTEGRATE: Model-based multi-omics data ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8853556/]
- 67. Physiological functions of glucose transporter-2: From cell ... [https://www.sciencedirect.com/science/article/pii/S2405844024014907]
- 68. MINN: A metabolic-informed neural network for integrating ... [https://www.sciencedirect.com/science/article/pii/S2001037025003265]
- 69. Simulated metabolic profiles reveal biases in pathway ... [https://pubmed.ncbi.nlm.nih.gov/40926162/]
- 70. Ten simple rules for creating reusable pathway models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8375987/]
- 71. Data Visualizations, Charts, and Graphs - Digital Accessibility [https://accessibility.huit.harvard.edu/data-viz-charts-graphs]
- 72. Glucose transporters: physiological and pathological roles [https://pmc.ncbi.nlm.nih.gov/articles/PMC5425736/]
- 73. ATP synthesis and storage - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3360099/]
- 74. NEXT-FBA: A hybrid stoichiometric/data-driven approach to ... [https://www.sciencedirect.com/science/article/pii/S1096717625000461]
- 75. Insulin Resistance - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK507839/]
- 76. Insulin Resistance: Background, Pathophysiology, Etiology [https://emedicine.medscape.com/article/122501-overview]
- 77. Mitochondrial (Dys)function and Insulin Resistance [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2019.00532/full]
- 78. Trends in insulin resistance: insights into mechanisms and ... [https://www.nature.com/articles/s41392-022-01073-0]
- 79. Mechanisms of Insulin Action and Insulin Resistance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6170977/]
- 80. Endoplasmic Reticulum Stress and Type 2 Diabetes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3684428/]
- 81. Endoplasmic reticulum stress induces degradation of ... [https://www.sciencedirect.com/science/article/abs/pii/S0014299922002734]
- 82. Effect of insulin deprivation on muscle mitochondrial ATP ... [https://pubmed.ncbi.nlm.nih.gov/17660267/]
- 83. Glucose metabolism and its direct action in cancer and ... [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-025-01167-1]
- 84. Real-time quantitative analysis of metabolic flux in live cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5473678/]
- 85. colorectal Metabolic : a review of aerobic... reprogramming in cancer [https://www.nature.com/articles/s41420-025-02623-5?error=cookies_not_supported&code=d7f96e83-8151-4830-a9a3-c1177f7b7c90]
- 86. Glucose transporters in cancer metabolism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6392426/]
- 87. Label-free whole-colony imaging and metabolic analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6993220/]
- 88. sciencedirect.com/topics/neuroscience/ glucose - transporter - 2 [https://www.sciencedirect.com/topics/neuroscience/glucose-transporter-2]
- 89. Proving SGLT Inhibitor-Mediated Improvement in Cardiomyocyte... [https://pubmed.ncbi.nlm.nih.gov/38847114/]
- 90. clinical insights into OXPHOS inhibition for cancer therapy [https://www.sciencedirect.com/org/science/article/pii/S2755158X2500003X]
- 91. Bioenergetic stress potentiates antimicrobial resistance ... [https://www.nature.com/articles/s41467-025-60302-6]
- 92. Frontiers | Molecular mechanisms and computational insights into... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1668400/full]
- 93. Electrogenic properties of the cloned Na+/ glucose cotransporter: II .... [https://link.springer.com/article/10.1007/BF00235798]
- 94. Triphenylphosphonium-based mitochondrial targeting in ... [https://pubs.rsc.org/en/content/articlehtml/2025/cc/d5cc05709d?page=search]
- 95. Rac1 Signaling Is Required for Insulin-Stimulated Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3661612/]
- 96. New signaling molecules redefine understanding of ... [https://www.adameetingnews.org/new-signaling-molecules-redefine-understanding-of-glucose-uptake/]
- 97. Rac1 supports muscle glucose uptake independently of Akt [https://pmc.ncbi.nlm.nih.gov/articles/PMC6187031/]
- 98. Rac1 signaling is required for insulin-stimulated glucose ... [https://pubmed.ncbi.nlm.nih.gov/23423567/]
- 99. Rac1 is a novel regulator of contraction-stimulated glucose ... [https://pubmed.ncbi.nlm.nih.gov/23274900/]
- 100. Isthmin-1 is an adipokine that promotes glucose uptake and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8429235/]
- 101. Circulating Isthmin-1 Levels and Their Relationship with ... [https://www.mdpi.com/2227-9059/13/1/101]
- 102. Serum Isthmin-1 levels are positively correlated with ... [https://pubmed.ncbi.nlm.nih.gov/40642506/]
- 103. Rational design and characterization of a Rac GTPase- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC419655/]
- 104. Targeting mitochondrial transporters and metabolic ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06976-4]
- 105. Targeting Glucose Transporter 1 (GLUT1) in Cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12481445/]
- 106. Physiology, Adenosine Triphosphate - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK553175/]
- 107. Adenosine triphosphate [https://en.wikipedia.org/wiki/Adenosine_triphosphate]
- 108. Endocytic vesicles act as vehicles for glucose uptake in response to growth factor stimulation | Nature Communications [https://www.nature.com/articles/s41467-024-46971-9]
- 109. Targeting mitochondrial transporters and metabolic ... [https://pubmed.ncbi.nlm.nih.gov/41102706/]
- 110. Transport and inhibition mechanism of the human SGLT2– ... [https://www.nature.com/articles/s41594-023-01134-0]
- 111. Drug–Target Kinetics in Drug Discovery - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC5767540/]