Dual-Hormone Artificial Pancreas Systems: Overcoming the Limits of Single-Hormone AID in Type 1 Diabetes
This article comprehensively reviews the development of dual-hormone (insulin and glucagon) artificial pancreas systems for Type 1 Diabetes management.
Dual-Hormone Artificial Pancreas Systems: Overcoming the Limits of Single-Hormone AID in Type 1 Diabetes
Abstract
This article comprehensively reviews the development of dual-hormone (insulin and glucagon) artificial pancreas systems for Type 1 Diabetes management. Aimed at researchers and drug development professionals, it explores the foundational rationale for multi-hormonal control to address the critical limitation of single-hormone systems: the inability to proactively prevent hypoglycemia. The scope spans from core physiological challenges and algorithmic innovations—including event-triggered control and machine learning—to the troubleshooting of practical hurdles like glucagon stability and system personalization. It further provides a critical analysis of in silico and clinical validation methods, comparing dual-hormone performance against advanced single-hormone systems. The synthesis concludes that integrating robust control algorithms with stable glucagon formulations is key to realizing fully automated, patient-centric diabetes care.
The Physiological Imperative: Why Single-Hormone Systems Are Not Enough
Automated Insulin Delivery (AID) systems, also known as hybrid closed-loop systems, represent a transformative advancement in the management of Type 1 Diabetes (T1D). These systems integrate a continuous glucose monitor (CGM), an insulin pump, and a control algorithm to automatically adjust subcutaneous insulin delivery based on real-time glucose levels [1] [2]. While single-hormone (insulin-only) AID systems have demonstrated significant benefits in improving time-in-range (TIR) and reducing HbA1c [3] [4], they possess an inherent physiological limitation: the inability to replicate the body's natural counter-regulatory response to impeding hypoglycemia, a function normally mediated by glucagon.
In individuals without diabetes, the pancreatic α-cells secrete glucagon in response to declining blood glucose levels. This glucagon stimulates hepatic glycogenolysis and gluconeogenesis, thereby increasing endogenous glucose production (EGP) and preventing hypoglycemia [5]. In long-standing T1D, this counter-regulatory mechanism is compromised through multiple pathways: the paracrine destruction of α-cell function results in a blunted glucagon response, while recurrent exposure to hypoglycemia further impairs sympathoadrenal epinephrine release and symptom recognition, collectively known as Hypoglycemia-Associated Autonomic Failure (HAAF) [5]. Consequently, insulin-only AID systems are left without a physiological defense against hypoglycemia beyond the reduction or suspension of insulin delivery—an inherently limited strategy that fails to actively raise blood glucose levels.
Quantitative Evidence: Comparing Single-Hormone and Dual-Hormone System Performance
The fundamental limitation of insulin-only AID is substantiated by clinical data comparing its performance against dual-hormone systems that deliver both insulin and glucagon. The tables below summarize key findings from pivotal studies.
Table 1: Glycemic Outcomes from an 18-Month Study of Insulin-Only AID in T1D with Impaired Hypoglycemia Awareness [5]
| Outcome Measure | Baseline | 6 Months Post-AID | 18 Months Post-AID | P-value |
|---|---|---|---|---|
| Severe Hypoglycemia (events/person-year) | 3 (3-10) | Not Reported | 0 (0-1) | 0.005 |
| Hypoglycemia Exposure (Time <60 mg/dL) | >5% (Inclusion Criteria) | Significant Reduction | Sustained Reduction (vs. Baseline) | ≤0.001 |
| Epinephrine Response to Hypoglycemia (pg/mL) | 199 ± 53 | 332 ± 91 | 386 ± 95 | 0.001 |
| Endogenous Glucose Production (EGP) during Hypoglycemia | Defective | No Significant Change | No Significant Change | Not Significant |
Table 2: Comparative Efficacy of Single-Hormone vs. Dual-Hormone Closed-Loop Systems [6] [7] [8]
| Parameter | Standard Insulin Pump (Control) | Single-Hormone AID | Dual-Hormone AID | Notes |
|---|---|---|---|---|
| Time in Range (TIR: 70-180 mg/dL) | 57.3% (IQR: 25.2-71.8) | ~70% (Typical) [4] | 70.7% (IQR: 46.1-88.4) [6] 91.6% (Simulated) [8] | Dual-hormone shows superior TIR. |
| Time in Hypoglycemia (<54 mg/dL or <3.0 mmol/L) | 10.2% (<4.0 mmol/L) [6] | ~1-3% (Typical) [4] | 0.0% (<4.0 mmol/L) [6] | Dual-hormone virtually eliminates hypoglycemia. |
| Hypoglycemic Events (<3.0 mmol/L) | 8/15 Participants (53%) [6] | Reduced vs. control | 1/15 Participants (7%) [6] | Marked reduction in event number. |
| Key Limitation | High patient burden and hypoglycemia risk. | Lacks active counter-regulation; limited by insulin pharmacokinetics [4]. | Glucagon stability in delivery devices. |
The data reveal that while insulin-only AID achieves a remarkable reduction in severe hypoglycemia events and hypoglycemia exposure, this is likely mediated through hypoglycemia avoidance rather than a restoration of physiological counter-regulation. As shown in Table 1, the defective EGP response remained unimproved after 18 months of AID use [5]. In contrast, dual-hormone systems actively mitigate hypoglycemia, resulting in a near-zero percentage of time spent in hypoglycemia (Table 2).
Experimental Protocols for Investigating AID Limitations and Solutions
To generate the evidence above, researchers employ sophisticated clinical and computational protocols. The following are detailed methodologies for key experiment types.
Protocol 1: Hyperinsulinemic-Hypoglycemic Clamp to Assess Counter-Regulatory Response
Objective: To quantitatively evaluate the recovery of glucose counter-regulatory hormones and endogenous glucose production in response to controlled hypoglycemia, following a prolonged intervention with an AID system [5].
Workflow Diagram: Hypoglycemic Clamp Experimental Procedure
Materials and Reagents:
- AID System: e.g., MiniMed 670G or Tandem t:slim X2 pump with compatible CGM [5].
- Insulin Infusate: Regular human insulin for intravenous infusion.
- Dextrose Infusate: 20% dextrose solution for variable IV infusion to maintain target glycemia.
- Stabilization Catheters: Intravenous catheters placed in antecubital veins for infusion and contralateral hand veins for sampling (with hand warmed in a heated box for arterialized venous blood).
- Hormone Assay Kits: Commercially available ELISA or RIA kits for plasma glucagon, epinephrine, and pancreatic polypeptide.
Procedure:
- Participant Selection: Recruit adults with C-peptide negative T1D of long duration (>10 years) complicated by impaired awareness of hypoglycemia (Clarke score ≥4) and evidence of significant hypoglycemia exposure on CGM [5].
- Baseline & Intervention: Perform a baseline clamp study. Initiate the AID system and follow participants for the intervention period (e.g., 18 months), ensuring sensor compliance >80% [5].
- Post-Intervention Clamp: After the intervention period, admit participants to a clinical research facility.
- Clamp Procedure:
- After an overnight fast, prime the dextrose and insulin infusion lines.
- Administer a primed, continuous intravenous insulin infusion at a fixed rate (e.g., 40 mU/m²/min) to induce and maintain hyperinsulinemia.
- Measure plasma glucose every 5 minutes. Simultaneously, adjust the infusion rate of the 20% dextrose solution to lower and then clamp the plasma glucose at a hypoglycemic target (e.g., 45-50 mg/dL) for a sustained period (e.g., 90 minutes) [5].
- Blood Sampling: Draw venous blood samples at predefined intervals (e.g., every 10-60 minutes) before and during the hypoglycemic plateau for the measurement of counter-regulatory hormones (glucagon, epinephrine, pancreatic polypeptide) and for calculation of EGP using tracer methods [5].
- Data Analysis: Compare the magnitude of hormonal responses and EGP between the pre- and post-intervention clamp studies.
Protocol 2: Dual-Hormone Artificial Pancreas Algorithm Testing
Objective: To develop and validate a smart, event-triggered control algorithm for a dual-hormone artificial pancreas that proactively administers insulin and glucagon to prevent glycemic excursions [7].
Workflow Diagram: Smart Dual-Hormone AP (SDHAP) System Workflow
Materials and Reagents:
- Dataset: The T1DiabetesGranada dataset or similar CGM time-series data [7].
- Software Platform: MATLAB/Python for algorithm development and simulation.
- Control Algorithm Components: Bergman Minimal Model (or other glucose-insulin dynamic models), Proportional-Integral (PI) controller, Model Predictive Control (MPC) framework [7] [2].
- Pump Systems: Subcutaneous infusion pumps for insulin and glucagon.
Procedure:
- Data Preprocessing: Clean and preprocess historical CGM data. Extract relevant time-series, statistical, and clinical features (e.g., TIR, TBR, TAR) [7].
- Event Classification: Train machine learning classifiers (e.g., Support Vector Machine - SVM, k-Nearest Neighbors - KNN) to detect patterns preceding hypoglycemic or hyperglycemic events using the extracted features.
- Glucose Prediction: Develop a prediction model (e.g., using Gated Recurrent Unit - GRU networks) to forecast future glucose values and trends.
- Controller Design:
- Design an event-triggered feedback controller (PI or MPC) that uses the predicted glucose values to compute necessary basal insulin adjustments and micro-boluses of glucagon.
- Integrate a feedforward controller to reject post-meal disturbances. The event trigger activates hormone delivery only when a glycemic event is predicted or detected, reducing unnecessary interventions [7].
- In Silico Validation: Test the integrated SDHAP algorithm in a validated T1D simulation environment (e.g., the UVA/Padova T1D Simulator) under various meal and exercise scenarios.
- Clinical Validation: Conduct a randomized crossover trial comparing the dual-hormone closed-loop system against standard insulin-pump therapy or single-hormone AID, with metrics including TIR, time in hypoglycemia, and number of hypoglycemic events [6].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials and Reagents for AID and Counter-Regulation Research
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Provides real-time interstitial glucose measurements to the control algorithm. | Dexcom G6/G7 [1], Medtronic Guardian 4 [1], FreeStyle Libre 2 Plus/3 Plus [1] [7]. |
| Insulin Pump | Subcutaneously delivers micro-boluses of insulin as dictated by the algorithm. | Tandem t:slim X2/Mobi [5] [1], Insulet Omnipod 5 (patch pump) [1], Medtronic MiniMed 780G [1]. |
| Control Algorithm | The "brain" that calculates required insulin (and glucagon) delivery based on CGM data. | Model Predictive Control (MPC) [2] [8], Proportional-Integral-Derivative (PID) [2], Fuzzy Logic [2]. |
| Stable Liquid Glucagon Formulation | The counter-regulatory agent used in dual-hormone systems to actively mitigate hypoglycemia. | Recombinant glucagon for continuous subcutaneous infusion [6]; requires stability research for long-term use in pumps. |
| Hormone Assay Kits | Quantify plasma levels of counter-regulatory hormones during mechanistic studies. | ELISA or RIA kits for glucagon, epinephrine, norepinephrine, and pancreatic polypeptide [5]. |
| T1D Simulation Platform | Enables in-silico testing and refinement of AID algorithms prior to clinical trials. | UVA/Padova T1D Simulator (accepted by regulatory bodies) [8]. |
Signaling Pathways in Glucose Counter-Regulation and HAAF
The core limitation of insulin-only AID systems can be understood through the lens of the disrupted signaling pathways in T1D, which lead to Hypoglycemia-Associated Autonomic Failure (HAAF).
Diagram: Signaling Pathways in Normal Counter-Regulation vs. HAAF in T1D
The diagram illustrates the critical defect: the pathway from hypoglycemia to glucagon secretion and subsequent EGP is severed in T1D with HAAF. An insulin-only AID system can only remove insulin, the glucose-lowering hormone. It cannot activate the glucose-raising pathway on the left, which is the natural defense. A dual-hormone system aims to pharmacologically replace this broken link by administering glucagon when needed.
The management of Type 1 Diabetes (T1D) presents a persistent challenge in maintaining glycemic control amidst physiological perturbations such as meal consumption and physical activity. Meal-induced hyperglycemia and exercise-induced hypoglycemia represent two critical gaps in diabetes management, even with advanced insulin replacement therapies [9] [10]. Intensive insulin therapy, while protective against long-term complications, is significantly limited by the risk of hypoglycemia, creating a barrier to optimal glycemic control [10]. Dual-hormone (insulin and glucagon) delivery systems have emerged as a promising approach to mimic pancreatic endocrine function more physiologically by not only adding insulin to correct hyperglycemia but also incorporating glucagon to prevent or treat hypoglycemia [6] [11] [7]. These systems leverage advances in continuous glucose monitoring, hormone formulation stability, and predictive algorithms to create a more responsive glycemic management platform. This document outlines application notes and experimental protocols to advance research in dual-hormone systems, specifically addressing postprandial hyperglycemia and exercise-induced hypoglycemia.
Physiological Background and Signaling Pathways
Pathophysiology of Dysglycemia
In T1D, the loss of endogenous insulin and glucagon secretion disrupts the delicate balance of glucose regulation. Meal-induced hyperglycemia results from the inability to secrete insulin in response to carbohydrate intake, leading to uncontrolled hepatic glucose production and impaired peripheral glucose uptake [10]. Conversely, exercise-induced hypoglycemia occurs due to multiple factors: the inability to naturally decrease insulin levels at exercise onset, increased glucose utilization by skeletal muscle, and potential impairments in counter-regulatory hormone responses [9] [12]. Even with appropriate insulin dose reductions before exercise, hypoglycemia can occur because of heightened skeletal muscle insulin sensitivity and reduced glucose counterregulatory responses, with the risk of nocturnal hypoglycemia estimated to be as high as 30% after afternoon exercise [9].
Glucose Counterregulation Pathway
The body's natural defense against hypoglycemia involves a complex hormonal cascade. The following diagram illustrates the coordinated counter-regulatory response to declining blood glucose levels:
Diagram 1: Counter-Regulatory Response to Hypoglycemia. This pathway illustrates the body's multi-layered defense mechanism against falling blood glucose levels. The immediate response includes decreased insulin secretion and increased glucagon, followed by epinephrine release, which together stimulate hepatic glucose production. Cortisol and growth hormone contribute to more prolonged glucose regulation. In T1D, this pathway is compromised by impaired glucagon response and blunted sympathoadrenal activation, particularly after recurrent hypoglycemia [10].
Carbohydrate Supplementation Guidelines for Exercise
Table 1: Carbohydrate Intake Protocol Based on Pre-Exercise Glucose Levels
| Pre-Exercise Blood Glucose Concentration | Action Required |
|---|---|
| <90 mg/dL | Ingest 15-30 g of fast-acting carbohydrates before exercise onset, depending on individual size. Continue carbohydrate intake throughout exercise. |
| 90-149 mg/dL | Begin consuming carbohydrates at exercise onset (approximately 0.5-1.0 g/kg body mass/hour), adjusted for energy expenditure and circulating insulin levels. |
| 150-249 mg/dL | Initiate exercise and delay carbohydrate consumption until glucose levels drop below 150 mg/dL. |
| 250-349 mg/dL | Test for ketones; avoid exercise if moderate to large ketones present. Initiate mild-to-moderate intensity exercise only. Delay intense exercise until glucose drops below 250 mg/dL. |
| ≥350 mg/dL | Test for ketones; avoid exercise if ketones present. Consider conservative insulin correction (e.g., 50% correction) before initiating mild-to-moderate exercise. |
Source: Adapted from PMC Disclaimer [9].
Insulin Adjustment Strategies for Exercise
Table 2: Bolus Insulin Reduction for Aerobic Exercise
| Exercise Intensity | Bolus Dose Reduction for 30 Minutes of Exercise (%) | Bolus Dose Reduction for 60 Minutes of Exercise (%) |
|---|---|---|
| Mild (e.g., walking, gardening) | 25 | 50 |
| Moderate (e.g., brisk walking, jogging) | 50 | 75 |
| Intense (e.g., running, team sports) | 75 | — |
Note: These percentages are based on studies in adults on multiple daily injection regimens using ultralente basal insulin and lispro mealtime insulin. Different insulin regimens may require adjustments. Source: Adapted from PMC Disclaimer [9].
Table 3: Basal Rate Reduction for Insulin Pump Users During Exercise
| Aerobic Exercise Intensity | Basal Rate Reduction for 60 Minutes of Exercise (%) |
|---|---|
| Mild | 30 |
| Moderate | 50 |
| Intense | 90-100 |
Note: Basal rate reductions should be implemented 60-90 minutes before exercise onset and maintained until activity completion. Source: Adapted from PMC Disclaimer [9].
Recent Clinical Trial Outcomes for Dual-Hormone Systems
Table 4: Efficacy Metrics of Dual-Hormone Closed-Loop Systems
| Study Parameter | Dual-Hormone Closed-Loop Performance | Standard Insulin Pump Therapy |
|---|---|---|
| Time in Target Range (Median) | 70.7% (IQR 46.1%-88.4%) | 57.3% (IQR 25.2%-71.8%) |
| Time in Hypoglycemia (<3.3 mmol/L) | 0.0% (IQR 0.0%-0.0%) | 2.8% (IQR 0.0%-5.9%) |
| Patients with ≥1 Hypoglycemic Event (<3.0 mmol/L) | 1 participant (7%) | 8 participants (53%) |
Source: Adapted from Glucose-responsive insulin and glucagon delivery (dual ... [6].
Experimental Protocols
Protocol 1: In Vivo Evaluation of Insulin-Responsive Glucagon Delivery
4.1.1 Objective To evaluate the efficacy of a microneedle (MN)-array patch containing insulin-responsive glucagon conjugates (Apt-Glu) in preventing insulin-induced hypoglycemia in a streptozotocin (STZ)-induced T1D mouse model [11].
4.1.2 Materials
- STZ-induced diabetic mice (C57BL/6J, 8-10 weeks old)
- Insulin-responsive Glu-HA microneedle patches
- Recombinant human insulin (1.0 U/kg)
- Blood glucose monitoring system
- Glucagon radioimmunoassay kit
- Trypan blue solution for penetration verification
- Hematoxylin and eosin (H&E) staining reagents
4.1.3 Procedure
- Preparation of Glu-HA Microneedle Patches: Synthesize insulin-conjugated methacrylated hyaluronic acid (Ins-HA) and insulin aptamer-modified glucagon (Apt-Glu). Form the insulin-responsive Glu-HA matrix through specific binding between the aptamer and insulin.
- Fabrication of MN-array: Load Glu-HA matrix into silicone mold tips via centrifugation. Crosslink by UV irradiation (60 seconds) to form stiff MNs capable of skin penetration.
- Administration: Apply the Glu-HA MN-array patch to the dorsum of fasted STZ-induced diabetic mice. Verify successful penetration using trypan blue staining and histological analysis.
- Insulin Challenge: Administer a high-dose insulin injection (1.0 U/kg) sufficient to induce profound hypoglycemia in control animals.
- Monitoring: Measure blood glucose levels at baseline and at 30-minute intervals for 3 hours post-injection. Collect serum samples for glucagon quantification.
- Control Groups: Include control groups receiving: (1) no treatment, (2) blank MN patches, and (3) free glucagon-loaded MNs.
4.1.4 Data Analysis Compare blood glucose trajectories and nadir values between treatment groups. Calculate area under the curve for glucose levels below 70 mg/dL. Analyze serum glucagon levels in relation to insulin administration timing.
Protocol 2: Event-Triggered Dual-Hormone Artificial Pancreas Testing
4.2.1 Objective To validate a Smart Dual Hormone Artificial Pancreas (SDHAP) with event-triggered feedback-feedforward control in managing postprandial hyperglycemia and exercise-induced hypoglycemia [7].
4.2.2 Materials
- T1DiabetesGranada dataset or similar CGM data
- Support Vector Machine (SVM) and K-Nearest Neighbor (KNN) algorithms
- Bergman Minimal Model parameters
- Proportional-Integral (PI) and Model Predictive Control (MPC) algorithms
- Continuous glucose monitors
- Dual-chamber infusion pump (insulin and glucagon)
- Arduino UNO, NEMA 17 stepper motor with TB6560 driver (for hardware prototype)
4.2.3 Procedure
- Data Preprocessing: Clean and preprocess CGM data. Extract temporal, statistical, and spectral features. Calculate diabetes-specific metrics (TIR, TBR, TAR).
- Glycemic Event Classification: Train SVM and KNN classifiers to identify hypoglycemia and hyperglycemia events using threshold-based criteria.
- Blood Glucose Prediction: Implement ARIMA and Gated Recurrent Unit (GRU) models for multi-step ahead glucose prediction. Validate using RMSE and MAE metrics.
- Controller Design: Develop event-triggered PI and MPC feedback controllers based on the Bergman Minimal Model. Design feedforward controller for meal and exercise disturbance rejection.
- Hardware Implementation: Prototype using Arduino UNO with stepper motors for precise hormone delivery. Implement safety constraints to prevent simultaneous hormone infusion.
- Validation: Test the integrated system in simulated and real-world conditions with announced and unannounced meals and exercise sessions.
4.2.4 Data Analysis Calculate percentage time in target range (70-180 mg/dL), hypoglycemia events (<70 mg/dL), and hyperglycemia events (>180 mg/dL). Compare controller performance against standard insulin pump therapy. Analyze algorithm computational efficiency and power consumption.
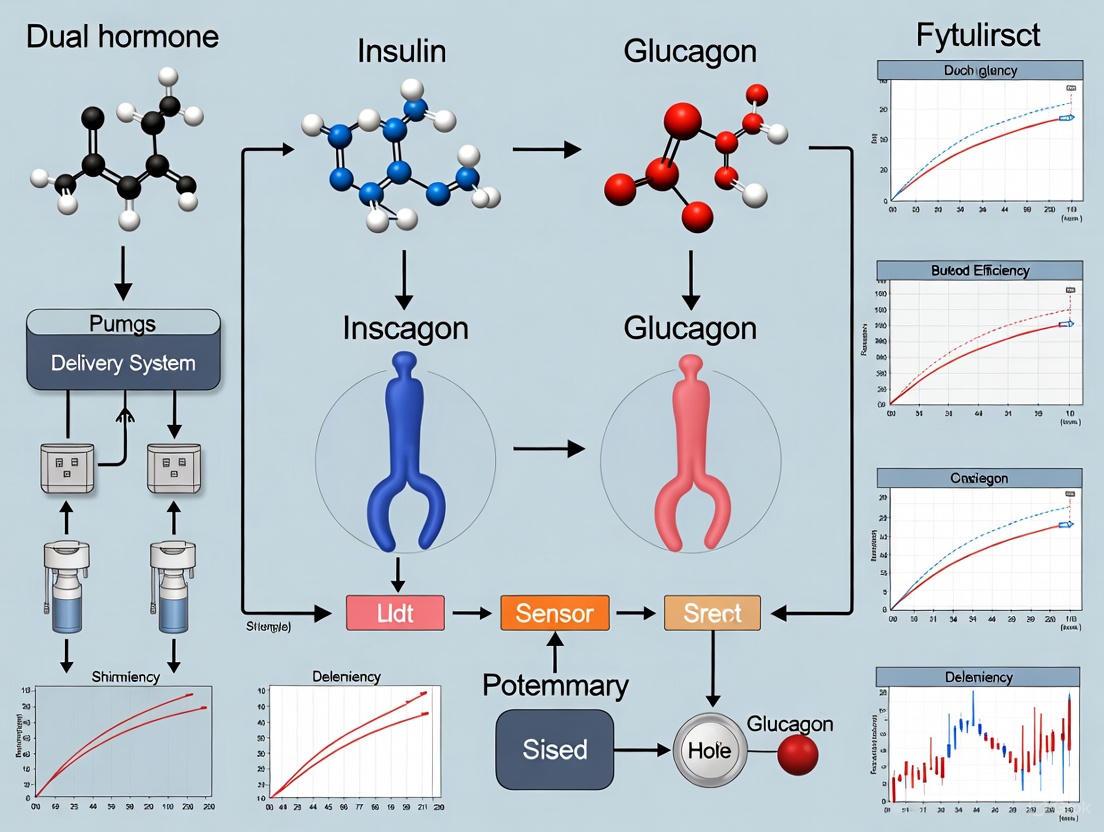
The following workflow diagram illustrates the integrated experimental approach for the SDHAP system:
Diagram 2: SDHAP System Workflow. This diagram outlines the integrated approach for the Smart Dual Hormone Artificial Pancreas, showing the pathway from continuous glucose monitoring data input through event classification, prediction, and triggered hormone delivery to maintain glycemic control.
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Research Materials for Dual-Hormone System Development
| Research Reagent | Function/Application | Key Considerations |
|---|---|---|
| Recombinant Glucagon | Hypoglycemia rescue agent in dual-hormone systems | Requires stabilization against fibrillation; consider novel analogs |
| Insulin Aptamers | Molecular recognition elements for insulin-responsive systems | Select for high specificity and affinity to insulin |
| Methacrylated Hyaluronic Acid (m-HA) | Biocompatible hydrogel matrix for controlled release | Tunable crosslinking density modulates release kinetics |
| STZ-Induced Diabetic Mouse Model | In vivo evaluation of glycemic control systems | Monitor glucose levels closely post-induction |
| CGM Sensors (e.g., Dexcom G6, Medtronic Guardian) | Real-time glucose monitoring for closed-loop systems | Accuracy and lag time critical for algorithm performance |
| Miniaturized Infusion Pumps | Precise dual-hormone delivery | Consider flow rate range and occlusion detection |
| Bergman Minimal Model Parameters | Mathematical modeling of glucose-insulin dynamics | Enables predictive control algorithms |
| SVM/KNN Algorithms | Classification of glycemic events from CGM data | Training on balanced datasets improves minority class detection |
Source: Compiled from [6] [11] [7].
The development of advanced dual-hormone delivery systems represents a promising frontier in addressing the persistent challenges of meal-induced hyperglycemia and exercise-induced hypoglycemia in T1D management. The protocols and data outlined herein provide a framework for advancing research in this field, with particular emphasis on responsive material systems and intelligent control algorithms. As evidenced by recent clinical trials, dual-hormone approaches can significantly increase time in target range while reducing hypoglycemia exposure. Future research directions should focus on stabilizing glucagon formulations for long-term use, refining event-triggered algorithms through artificial intelligence, and developing fully integrated systems that minimize user burden while maximizing glycemic outcomes.
Glucagon, a 29-amino-acid peptide hormone secreted by pancreatic α-cells, serves as a critical counter-regulatory hormone to insulin in glucose homeostasis. While its historical role as a hyperglycemic agent has been recognized for a century, recent research has unveiled its potential in hypoglycemia prevention and mitigation, particularly in the context of dual-hormone delivery systems for diabetes management. This application note examines the physiological mechanisms of glucagon action, analyzes its therapeutic efficacy, and provides detailed protocols for its implementation in advanced diabetes technologies. The development of dual-hormone artificial pancreas systems represents a paradigm shift in diabetes management, leveraging glucagon's unique properties to address the persistent challenge of iatrogenic hypoglycemia, which remains a significant barrier to optimal glycemic control in insulin-treated diabetes.
Physiological Basis of Glucagon Action
Molecular Mechanisms of Glucagon Secretion and Signaling
Glucagon secretion from pancreatic α-cells is regulated through a complex interplay of nutrient sensing, paracrine signals, and neural inputs. The primary stimulants for glucagon release include hypoglycemia, amino acids, and sympathetic activation. Conversely, secretion is inhibited by hyperglycemia, insulin, somatostatin, and GABA [13].
The intracellular signaling cascade in α-cells centers on cyclic AMP (cAMP) production, which serves as the primary trigger for glucagon secretion. During hypoglycemia or sympathetic stimulation, increased cAMP levels activate protein kinase A (PKA) and exchange protein directly activated by cAMP (Epac), leading to calcium mobilization and vesicular release of stored glucagon [13]. Additionally, G protein-coupled receptor (GPCR) pathways, including Gq-coupled receptors such as the vasopressin 1b receptor (V1bR), activate phospholipase C (PLC) and produce inositol trisphosphate (IP3), further enhancing intracellular calcium release and glucagon secretion [13].
Glucagon exerts its effects primarily through binding to the glucagon receptor, a G-protein coupled receptor primarily located in the liver. Receptor activation stimulates adenylate cyclase, increasing intracellular cAMP levels and activating protein kinase A. This in turn activates key enzymes including glycogen phosphorylase and fructose-1,6-bisphosphatase while inhibiting glycogen synthase and pyruvate kinase. The net result is enhanced hepatic glucose output through both glycogenolysis (breakdown of glycogen stores) and gluconeogenesis (synthesis of glucose from non-carbohydrate precursors) [13] [14].
Metabolic Effects Beyond Glycemic Control
Recent evidence indicates glucagon's physiological role extends beyond glycemic regulation to include appetite suppression through the liver–vagal nerve–hypothalamic axis, thermogenesis via brown adipose tissue activation, and regulation of amino acid metabolism through enhanced hepatic uptake and catabolism [13]. Glucagon also influences lipid metabolism by facilitating hepatic lipolysis, promoting cholesterol clearance, and triggering ketogenesis during prolonged fasting [13]. These pleiotropic effects position glucagon as a key regulator of systemic energy balance, with implications for managing metabolic disorders beyond diabetes.
Therapeutic Applications for Hypoglycemia Management
Low-Dose Glucagon for Exercise-Induced Hypoglycemia
Recent meta-analyses of randomized controlled trials demonstrate that low-dose glucagon significantly reduces the risk of exercise-induced hypoglycemia in type 1 diabetes. The table below summarizes key efficacy outcomes from clinical studies:
Table 1: Efficacy of Low-Dose Glucagon for Preventing Exercise-Induced Hypoglycemia in Type 1 Diabetes
| Outcome Measure | Effect Size | 95% Confidence Interval | Number of Studies | Participants |
|---|---|---|---|---|
| Hypoglycemia Risk | RR 0.54 | 0.35, 0.84 | 12 | 248 |
| Time Below Range (<3.9 mmol/L) | -3.91 percentage points | -6.27, -1.54 | 12 | 248 |
| Overall Adverse Events | RR 2.75 | 1.07, 7.08 | 12 | 248 |
Abbreviations: RR, risk ratio. Data sourced from systematic review and meta-analysis [15].
The evidence indicates that low-dose glucagon (typically 100-300 μg) reduces hypoglycemia risk by 46% and decreases time below range by nearly 4 percentage points. However, the significant increase in overall adverse events (primarily nausea and vomiting) highlights the need for careful dose optimization [15]. Injectable doses of 100-300 μg of glucagon have been shown to increase blood glucose levels by approximately 1.5-2 mmol/L within 15 minutes [15], making it an effective alternative to carbohydrate supplementation for exercise-induced hypoglycemia prevention.
Dual-Hormone Artificial Pancreas Systems
Dual-hormone artificial pancreas (DHAP) systems represent the most advanced application of glucagon for hypoglycemia prevention. These systems utilize control algorithms to automatically administer both insulin and glucagon based on continuous glucose monitor (CGM) readings and predictive models [7] [16].
Table 2: Comparison of Dual-Hormone Artificial Pancreas Control Algorithms
| Control Strategy | Glucagon Dosing Approach | Key Features | Clinical Performance |
|---|---|---|---|
| Event-Triggered FB-FF Control | Machine learning classification of glycemic events with feedback-feedforward control | Uses SVM and KNN classifiers; ARIMA and GRU models for prediction; PI and MPC controllers | Effective hypoglycemia reduction with minimal manual intervention |
| Robust H∞ Control | Non-personalized robust control for glucagon delivery | Combines switched LQG insulin control with H∞ glucagon controller; handles inter-patient variability | Satisfactory glucose regulation with less glucagon dosage compared to individualized approaches |
| Switched Multicontroller | Three LQG controllers tailored for specific needs | Separate controllers for meal compensation, late postprandial/fasting, and hypoglycemia protection | Significant hypoglycemia reduction compared to single-hormone systems |
Recent studies indicate that DHAP systems can achieve median time-in-range (TIR) values of 86.6% with lower time in hypoglycemia and hyperglycemia compared to sensor-augmented insulin pump treatment [17]. The primary benefit of the dual-hormone approach is particularly evident during exercise, where conventional insulin-only systems struggle to prevent hypoglycemia [15] [16].
Experimental Protocols
Protocol for Low-Dose Glucagon Administration During Exercise
This protocol outlines the methodology for evaluating low-dose glucagon efficacy in preventing exercise-induced hypoglycemia in type 1 diabetes, based on current clinical study designs [15].
Materials and Equipment
- Recombinant glucagon preparation (100 μg/mL concentration)
- Insulin pump with dual-chamber capability or separate micro-infusion device
- Continuous glucose monitoring system (Dexcom G6/G7, Medtronic Guardian, or FreeStyle Libre 2/3)
- Standardized exercise equipment (treadmill or cycle ergometer)
- Point-of-care glucose analyzer for calibration
- Emergency hypoglycemia treatment kit (oral glucose, dextrose IV)
Participant Preparation
- Screening: Recruit adults with type 1 diabetes (duration >1 year) on insulin pump therapy.
- Stabilization: Stabilize participants on their usual insulin regimen for 1 week prior to study.
- Baseline Assessment: Collect demographic data, diabetes history, HbA1c, and CGM metrics.
- Randomization: Utilize crossover design with randomized order of interventions.
Experimental Procedure
Pre-Exercise Preparation:
- Participants report to the clinical research facility after an overnight fast.
- Insert CGM sensor and calibrate according to manufacturer instructions.
- Insert subcutaneous catheters for insulin and glucagon administration.
- Obtain baseline blood samples for glucose, insulin, and glucagon levels.
Intervention Administration:
- Initiate continuous glucose monitoring at least 2 hours before exercise.
- Administer low-dose glucagon (100-300 μg subcutaneously) or placebo 10 minutes before exercise commencement.
- For pump users, program basal rate reduction of 50% 60 minutes before exercise.
Exercise Protocol:
- Participants perform moderate-intensity aerobic exercise (50-60% VO₂max) for 45 minutes on a treadmill or cycle ergometer.
- Monitor glucose levels every 5 minutes during exercise.
- Record physiological parameters (heart rate, blood pressure, symptoms) every 15 minutes.
Post-Exercise Monitoring:
- Continue glucose monitoring for 6 hours after exercise completion.
- Treat hypoglycemia (glucose <3.9 mmol/L) with standardized glucose tabs (4g each).
- Record all carbohydrate interventions and adverse events.
Outcome Measures
- Primary Endpoints: Hypoglycemia events (glucose <3.9 mmol/L), time below range
- Secondary Endpoints: Mean glucose, glucose variability, time in range, rescue carbohydrate requirements, adverse events
- Safety Monitoring: Nausea, vomiting, injection site reactions, hyperglycemia
Protocol for Dual-Hormone Artificial Pancreas Evaluation
This protocol describes the methodology for assessing the performance of dual-hormone closed-loop systems in free-living conditions [7] [16] [17].
System Components
- Dual-chamber infusion pump or separate pumps for insulin and glucagon
- Continuous glucose monitor with open API for data communication
- Control algorithm implemented on dedicated hardware or smartphone
- Glucagon formulation (stable liquid glucagon analog preferred)
System Configuration
Algorithm Initialization:
- Input patient-specific parameters: total daily insulin dose, carbohydrate ratio, correction factor, body weight.
- Set glucose targets: 6.0-6.5 mmol/L for fasting periods.
- Configure glucagon dosing limits: minimum dose 50 μg, maximum dose 500 μg per hour.
Safety Constraints:
- Program maximum insulin-on-board limits (typically 70-80% of standard calculations).
- Implement glucagon-on-board calculations to prevent overdosing.
- Set hypoglycemia suspend feature at 4.0 mmol/L with predicted descent >0.1 mmol/L/min.
Event Triggering Parameters:
- Configure thresholds for hypoglycemia prevention: administer micro-bolus of glucagon (50-100 μg) when glucose <4.5 mmol/L with downward trend.
- Set hyperglycemia correction parameters: increase basal insulin when glucose >8.0 mmol/L.
In-Silico Validation
Simulation Environment:
- Utilize the UVA/Padova T1D Simulator or comparable validated simulation platform.
- Test controller performance against a virtual population with varying insulin sensitivities, meal patterns, and exercise schedules.
Scenario Testing:
- Evaluate system response to standardized meals (20g, 50g, 80g carbohydrates).
- Test overnight performance with varying basal insulin requirements.
- Assess exercise response with 45-minute moderate intensity activity.
- Challenge system with missed meal boluses and over-bolusing scenarios.
Performance Metrics:
- Calculate percentage time in target range (3.9-10.0 mmol/L).
- Document time below range (<3.9 mmol/L and <3.0 mmol/L).
- Quantify insulin and glucagon usage.
- Record number of hypoglycemic events requiring intervention.
Clinical Validation
Study Design:
- Conduct randomized crossover trial comparing DHAP to single-hormone AP and conventional pump therapy.
- Include 24-hour inpatient admissions followed by 7-day outpatient periods.
Outcome Measures:
- Primary: Percentage time in target glucose range (3.9-10.0 mmol/L)
- Secondary: Time below range, time above range, mean glucose, glucose variability, patient-reported outcomes, safety measures
Statistical Analysis:
- Power calculation based on time-in-range differences (targeting ≥10% improvement).
- Mixed-effects models to account for repeated measures and crossover design.
- Pre-specified subgroup analyses for exercise days vs. sedentary days.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Glucagon Studies and Dual-Hormone System Development
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Glucagon Formulations | GlucaGen HypoKit (Novo Nordisk), Glucagon Emergency Kit (Eli Lilly), Dasiglucagon (Zealand Pharma), Stable liquid glucagon analogs | In vivo efficacy studies, formulation development | Stability, solubility, fibrillation resistance, reconstitution requirements |
| Glucagon Assays | Radioimmunoassays, ELISA kits, LC-MS/MS methods | Quantifying endogenous and exogenous glucagon | Specificity for intact glucagon, cross-reactivity with other proglucagon peptides |
| Cell Lines | Alpha TC1 clone 6, InR1-G9, primary human islets | In vitro mechanistic studies | Species differences, preservation of native α-cell characteristics |
| Animal Models | Streptozotocin-induced diabetic rodents, NOD mice, pancreatectomized large animals | Preclinical efficacy and safety testing | Species-specific metabolic differences, relevance to human physiology |
| Control Algorithms | PID, MPC, LQG, H∞ robust control | Dual-hormone artificial pancreas development | Personalization requirements, computational complexity, meal detection capability |
| Simulation Platforms | UVA/Padova T1D Simulator, Cambridge Simulator, Replica Type 1 Simulator | In-silico testing and validation | Population representativeness, meal and exercise scenario libraries |
Visualization of Glucagon Signaling and System Architecture
Glucagon Secretion and Hepatic Signaling Pathway
Diagram Title: Glucagon Secretion and Hepatic Signaling Pathway
Dual-Hormone Artificial Pancreas System Architecture
Diagram Title: Dual-Hormone Artificial Pancreas System Architecture
Glucagon's physiological role in preventing and mitigating hypoglycemia provides a compelling therapeutic avenue for addressing one of the most significant challenges in diabetes management. The development of dual-hormone delivery systems leverages glucagon's rapid hyperglycemic action to create a more physiological approach to glycemic control. Current evidence demonstrates that low-dose glucagon effectively reduces exercise-induced hypoglycemia, while dual-hormone artificial pancreas systems show promise for achieving superior time-in-range with reduced hypoglycemia burden.
Future research directions should focus on optimizing glucagon formulations for stability and delivery, refining control algorithms for various exercise types and durations, and conducting long-term outcomes studies to establish the real-world effectiveness and cost-benefit ratio of dual-hormone systems. As these technologies evolve, glucagon is poised to transition from an emergency rescue medication to an integral component of automated glycemic control, ultimately improving quality of life for people with insulin-requiring diabetes.
The development of dual-hormone automated delivery systems, which administer both insulin and glucagon, represents a frontier in diabetes management. While current single-hormone Automated Insulin Delivery (AID) systems have transformed care, they often fall short for specific patient groups, leaving critical gaps in therapy [18] [19]. This application note explores the potential of Dual-Hormone Fully Closed-Loop (DHFCL) systems to expand the patient spectrum, offering significant benefits for vulnerable populations who struggle with conventional therapies. These groups include individuals with hypoglycemia unawareness, those experiencing frequent exercise-induced hypoglycemia, and patients facing challenges due to social determinants of health (SDOH) [18] [20]. By leveraging the complementary actions of insulin and glucagon, DHFCL systems can provide a more robust and autonomous means of glycemic control, potentially mitigating the heightened risks faced by these vulnerable individuals.
Vulnerable Populations in Diabetes Management
Current Gaps in Automated Insulin Delivery (AID)
Even advanced hybrid closed-loop systems exhibit limitations that disproportionately affect vulnerable users:
- Meal Announcement Burden: Systems require accurate carbohydrate counting, a task prone to error and a significant source of management burden [19].
- Exercise-Induced Hypoglycemia: Current AID systems often fail to fully prevent hypoglycemia during and after physical activity, a major barrier for active individuals [18] [19].
- Limited Population Evaluation: Systems are not fully evaluated or specified for all populations, including older adults, pregnant individuals, and those with hypoglycemia unawareness, who are often excluded from initial clinical trials [18] [19].
Defining the Vulnerable Spectrum
Vulnerable populations in diabetes are those with an increased susceptibility to adverse health outcomes or reduced probability of receiving timely, quality care [21]. Key groups who may derive particular benefit from DHFCL systems include:
1. Patients with Hypoglycemia Unawareness and Recurrent Hypoglycemia This group experiences a pathophysiological defect in glucose counter-regulation. In Type 1 Diabetes (T1D), the glucagon response to hypoglycemia is blunted or absent, significantly increasing the risk of severe hypoglycemic events [18]. Fear of hypoglycemia itself often leads to preemptive over-eating and chronic hyperglycemia, undermining long-term health [22]. Even the best insulin-only closed-loop systems have an average time in hypoglycemia (<70 mg/dL) of about 2-3%, equating to approximately 43 minutes per day, with some individuals experiencing significantly higher exposure [18].
2. Physically Active Individuals and Athletes Exercise presents a complex challenge due to insulin-independent glucose disposal by muscles, increased insulin sensitivity, and accelerated subcutaneous insulin absorption [18] [19]. The blunted glucagon response in T1D further compounds this risk. While current AID systems have exercise modes, they require user initiation and may not adequately prevent post-exercise or overnight hypoglycemia [19].
3. Populations Impacted by Social Determinants of Health (SDOH) SDOH are the conditions in which people are born, grow, live, work, and age, and they account for 50-60% of health outcomes [20]. Key factors include:
- Socioeconomic Status (SES): A graded association exists between income, education, and diabetes outcomes. Lower SES is linked to higher diabetes prevalence and more complications [20].
- Food Environment: Food insecurity and limited access to healthy food directly impact the ability to maintain a stable diabetic diet and manage glucose levels effectively [23].
- Health Care Access: Disparities in access, affordability, and quality of care can prevent consistent disease management. A 2025 study found that individuals in states with high social vulnerability were less likely to receive diabetes education or self-monitor their blood sugar, despite being more likely to see a doctor, indicating potential gaps in comprehensive care [23].
Table 1: Impact of Social Vulnerability on Diabetes Management Behaviors
| Social Vulnerability Tier | Received Diabetes Education | Self-Monitoring of Blood Glucose | Saw a Doctor for Diabetes Care |
|---|---|---|---|
| Least Vulnerable | 57.16% | 85.48% | (Reference Group) |
| Moderately Vulnerable | 51.15% | ~84.5% | --- |
| Most Vulnerable | 50.41% | ~84.5% | 1.48x more likely (p<0.01) |
Data adapted from [23].
Potential Benefits of Dual-Hormone Systems for Vulnerable Populations
The integration of glucagon alongside insulin in a fully closed-loop system addresses the core pathophysiological defects in T1D and mitigates external challenges.
Enhanced Hypoglycemia Prevention and Safety
Glucagon, as a counter-regulatory hormone, acts rapidly on the liver to stimulate glycogenolysis and gluconeogenesis, raising plasma glucose within 10-30 minutes [18]. In DHFCL systems, microdoses of glucagon (10-100 micrograms) can be administered subcutaneously to preemptively counter falling glucose trends. A recent study on an event-triggered Smart Dual Hormone Artificial Pancreas (SDHAP) demonstrated effective blood glucose control and external disturbance rejection under both hypoglycemic and hyperglycemic conditions [7]. This automated defense mechanism is particularly crucial for individuals with hypoglycemia unawareness, as it can restore their physiological counter-regulatory response over time by reducing hypoglycemia frequency [18].
Managing Glycemic Variability During Exercise and Meals
DHFCL systems offer a dynamic response to the glycemic challenges of physical activity. Proof-of-concept systems using Model Predictive Control (MPC) algorithms can automatically reduce insulin and infuse glucagon in response to detected exercise, a significant advantage over single-hormone systems [19]. Furthermore, the presence of glucagon may allow for more aggressive insulin dosing to cover meals, as the risk of late postprandial hypoglycemia is reduced. This could pave the way for fully automated mealtime insulin dosing, alleviating the burden of carbohydrate counting [18].
Mitigating the Impact of Social Vulnerability
For patients affected by SDOH, the autonomy and safety net provided by a DHFCL system can be transformative. By reducing the need for precise carbohydrate counting and constant user input, these systems can help bridge gaps in health literacy [19]. The enhanced hypoglycemia protection is vital for individuals with food insecurity or unpredictable meal schedules, providing a buffer against glucose fluctuations. The fully automated nature of DHFCL systems, as seen in the ongoing DARE trial, removes diabetes management burdens related to meals and exercise, which is particularly beneficial for those facing socioeconomic challenges or limited access to consistent healthcare support [17].
Experimental Protocols and Application Notes
Protocol: Evaluating DHFCL System Efficacy in a Free-Living Outpatient Setting
Objective: To assess the long-term efficacy, safety, and user-reported outcomes of a DHHCL system compared to standard care (HCL or MDI + CGM/FGM) in a vulnerable adult population with T1D.
Study Design: A 12-month, open-label, two-arm randomized parallel-group trial, as exemplified by the DARE study [17].
Population:
- Inclusion Criteria: Adults (18-75 years) with T1D for ≥1 year, HbA1c ≤91 mmol/mol (≈10.5%), and suboptimal control (TIR <80% or TBR >4%) despite using MDI+FGM/CGM or HCL for ≥3 months.
- Exclusion Criteria: Use of non-approved HCL devices, BMI >35 kg/m², eGFR <30 mL/min/1.73 m², pregnancy, and conditions limiting ability to respond to device alarms [17].
Intervention:
- DHFCL Device: A CE-marked wearable device integrating two pumps (for insulin and glucagon) and a control algorithm, using two sensors and two infusion sets. The system reactively adapts hormone infusion without requiring meal or correction boluses [17].
- Control: Continuation of current care (HCL or MDI + CGM/FGM).
Methodology:
- Screening & Baseline: Obtain informed consent, collect demographic and clinical data, and place a blinded CGM (e.g., FreeStyle Libre Pro IQ) for at least 168 hours (50% data requirement) to establish baseline glucose metrics (TIR, TAR, TBR).
- Randomization: 1:1 randomization to intervention or control group.
- Training: Provide a comprehensive 1-day DHFCL training session for the intervention group, followed by 8 weeks of telephone guidance.
- Follow-up Visits: Conduct study visits at 3, 6, 9, and 12 months. At each visit:
- Collect (Serious) Adverse Event reports and data on device issues.
- Download device data for glucose metrics analysis.
- Administer Patient-Reported Outcome Measures (PROMs) covering quality of life, fear of hypoglycemia, treatment satisfaction, and sleep.
- Collect data for cost-effectiveness analysis (e.g., iMCQ, iPCQ).
- Primary Outcomes:
- Glycemic Control: Change in % Time-in-Range (TIR, 70-180 mg/dL).
- Patient-Reported Outcomes: Changes in PROM scores.
- Cost-Effectiveness: Incremental cost-effectiveness ratio (ICER).
Key Materials:
- DHFCL system (e.g., Inreda Diabetic B.V.)
- Blinded CGM systems
- Validated PROM questionnaires
- Data management system for device and questionnaire data
Protocol: Assessing Hypoglycemia Prevention with an Implantable Glucagon Device
Objective: To preclinically evaluate the efficacy of a minimally invasive, wireless implantable device that releases dry-powder glucagon in response to hypoglycemia.
Background: Liquid glucagon poses stability challenges for pump systems. Dry powder glucagon offers long-term stability but is difficult to deliver. An implantable device that automatically releases dry glucagon in response to hypoglycemia could provide an emergency rescue without patient intervention [22].
In Vivo Model:
- Subjects: Diabetic mice.
- Device Implantation: A wireless device (<2g, 3cm³) is implanted subcutaneously. The device contains a reservoir of powdered glucagon.
Methodology:
- Hypoglycemia Induction: Two study designs are used:
- Direct Simulation: Hypoglycemia is directly induced in the mice.
- Real-World Simulation: Conditions that drive hypoglycemia are replicated (e.g., missed meals, automated insulin infusions from pumps).
- Triggering Mechanism: A sensor detects low blood sugar and triggers the wireless release of the dry glucagon powder.
- Monitoring: Blood glucose concentrations are measured frequently after glucagon release.
- Control Group: A separate group of mice receives an inert substance (e.g., lactose) instead of glucagon.
Outcome Measures:
- Primary: Change in blood glucose concentration post-release (e.g., peak glucose level, time to peak).
- Secondary: Area under the curve (AUC) for glucose over 30-60 minutes after release. Comparison of glucose profiles between glucagon and control groups.
Key Findings from Preclinical Studies: [22]
- A rapid rise in blood glucose was observed within 5 minutes of drug release.
- Glucose peaked at ~30 mg/dL within 15 minutes.
- In the real-world simulation, blood glucose concentrations remained above the hypoglycemia threshold (average of 80 mg/dL) within the first hour after release.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for DHFCL Research and Development
| Research Reagent / Material | Function/Application in DHFCL Research |
|---|---|
| T1DiabetesGranada Dataset | An open-access, longitudinal dataset with CGM data from 736 T1D patients, used for training and validating machine learning models for glucose prediction and event classification [7]. |
| Bergman Minimal Model (BMM) | A widely used mathematical model of glucose-insulin dynamics. Serves as the physiological basis for designing and simulating feedback controllers (e.g., PI, MPC) in artificial pancreas systems [7]. |
| Machine Learning Algorithms (SVM, KNN) | Used for classifying glycemic events (hypo-/hyperglycemia) from features extracted from CGM data. K-Nearest Neighbor (KNN) and Support Vector Machine (SVM) are common choices [7]. |
| Time-Series Prediction Models (ARIMA, GRU) | Used for predicting future blood glucose levels. ARIMA is a classical statistical model, while Gated Recurrent Units (GRU) are a type of recurrent neural network for sequential data [7]. |
| Dry-Powder Glucagon Formulation | A stable, non-liquid formulation of glucagon for use in implantable devices or long-term pump reservoirs, addressing the stability issues of liquid glucagon [22]. |
| Continuous Glucose Monitor (CGM) | Provides real-time, interstitial glucose measurements. The primary sensor input for any closed-loop control algorithm. Essential for both in-patient and free-living clinical trials [7] [17]. |
| Event-Triggered Control Algorithm | A control scheme that computes and delivers hormone doses only when specific events (e.g., predicted hypoglycemia) occur, reducing computational load and preventing simultaneous hormone infusion [7]. |
Dual-hormone closed-loop systems hold immense promise for expanding the spectrum of patients who can achieve safe and effective glycemic control. By addressing the pathophysiological limitations of T1D and mitigating the impact of social and behavioral challenges, DHFCL technology can particularly benefit vulnerable populations, including those with hypoglycemia unawareness, active individuals, and those affected by adverse social determinants of health. Ongoing long-term trials like the DARE study [17] and innovations in stable glucagon formulations [22] are critical steps toward making this promise a clinical reality. Future research must continue to focus on these high-risk groups, ensuring that the next generation of diabetes technology is inclusive, equitable, and capable of improving outcomes for all individuals living with diabetes.
Algorithmic Architectures and Technological Integration in DHAP Design
The development of Automated Insulin Delivery (AID) systems, also known as Artificial Pancreas (AP) systems, represents a revolutionary advancement in the management of Type 1 Diabetes (T1D). These systems aim to automate the complex process of glucose regulation through sophisticated control algorithms that respond dynamically to continuous glucose monitoring (CGM) data [24]. Dual-hormone AP systems represent a further evolution, incorporating both insulin and glucagon delivery to more closely mimic the counter-regulatory function of a healthy pancreas [6]. The core challenge in these systems lies in the development of control algorithms that can safely and effectively manage the complex, time-delayed glucoregulatory dynamics under free-living conditions, including disturbances such as meals, exercise, stress, and sleep [24] [19].
Control algorithms serve as the "brain" of AP systems, processing real-time glucose sensor data to compute appropriate hormone dosing commands. These algorithms must accommodate significant inter- and intra-patient variability in insulin sensitivity and glucose metabolism while respecting critical safety constraints [16]. The progression of control strategies has evolved from simpler Proportional-Integral-Derivative (PID) controllers to more sophisticated approaches including Model Predictive Control (MPC), Linear Quadratic Gaussian (LQG) control, and H∞ robust control, each offering distinct advantages and limitations for dual-hormone applications [24] [16].
Table 1: Evolution of Control Strategies in Artificial Pancreas Systems
| Control Strategy | Era of Prominence | Key Innovation | Limitations in DHAP Context |
|---|---|---|---|
| PID Control | 1970s-present | Simple structure with proportional, integral, and derivative terms | Limited ability to handle constraints and delays [24] |
| Model Predictive Control (MPC) | 2000s-present | Predictive capability using glucoregulatory models | Computational burden; model dependency [24] [25] |
| Fuzzy Logic | 1990s-2010s | Rule-based systems capturing clinical expertise | High maintenance cost; conflict resolution needed [24] |
| LQG Control | 2010s-present | Optimization with process and measurement noise | Requires individual parameter tuning [26] |
| H∞ Robust Control | 2010s-present | Explicit handling of model uncertainty | Higher computational complexity [16] [27] |
Fundamental Control Algorithm Architectures
Proportional-Integral-Derivative (PID) Control
PID controllers were among the first algorithms applied to automated insulin delivery and formed the basis for early commercial AID systems [24]. The PID algorithm computes control action based on the difference (error) between the reference (desired) blood glucose concentration and the measured CGM value. This error is processed through three parallel pathways: the proportional term considers the current value of the error, the integral term accumulates past errors, and the derivative term estimates the rate of change of glucose levels [24].
The inherent simplicity and long industrial history of PID control have been its main appeals, with the proportional and derivative actions bearing similarity to the biphasic insulin response of pancreatic β-cells [24]. The proportional action mimics the first-phase insulin response by releasing insulin in proportion to the current glucose excursion, while the derivative action resembles the second-phase response by responding to the rate of change in glucose concentration. The integral action ensures persistent insulin infusion until the glucose error is eliminated [24].
In commercial implementations such as the Medtronic MiniMed 670G, the native PID algorithm has been modified with numerous auxiliary modules to enhance performance and safety [24]. These modifications include insulin-on-board (IOB) constraints, maximum insulin infusion limits, and predictive low glucose suspend features that address the algorithm's limitations in handling the complex, delayed dynamics of subcutaneous insulin absorption and glucose sensing [24] [28].
Model Predictive Control (MPC)
Model Predictive Control has emerged as the predominant algorithm framework in research-stage AP systems and increasingly in commercial implementations [24] [25]. Unlike PID control which reacts to current and past glucose values, MPC employs a dynamic model of glucose-insulin dynamics to forecast future glucose trajectories and proactively optimize insulin delivery [24].
The MPC framework comprises four key elements: (1) a dynamic model predicting future glucose values based on current state, historical data, and potential control actions; (2) an objective function quantifying the desired balance between glucose control and insulin usage; (3) an optimization algorithm that computes the insulin infusion sequence minimizing the objective function; and (4) constraints on glucose values, insulin delivery rates, and other safety parameters [24] [25].
MPC implementations in dual-hormone systems typically employ personalized models that may be fixed or adaptive. Fixed models are parameterized once for each patient based on historical data, while adaptive models continuously update their parameters in response to recent glucose dynamics [24]. Some advanced implementations use recursive identification techniques that update model parameters with every new CGM measurement (typically every 5 minutes), enabling the algorithm to accommodate daily variations in insulin sensitivity [24].
Table 2: Key Characteristics of Fundamental Control Algorithms
| Characteristic | PID Control | Model Predictive Control |
|---|---|---|
| Computational Demand | Low | High (due to real-time optimization) [24] |
| Constraint Handling | Limited (requires add-on modules) | Explicit (incorporated in optimization) [24] [25] |
| Prediction Horizon | None (reactive) | Typically 60-180 minutes [25] |
| Personalization Approach | Adjustment of three gain parameters | Model parameter identification [24] |
| Clinical Adoption | First commercial AID systems | Most research systems and newer commercial systems [24] [28] |
Advanced and Robust Control Strategies
Linear Quadratic Gaussian (LQG) Control
Linear Quadratic Gaussian control represents a more advanced state-space approach that combines Linear Quadratic Regulator (LQR) optimal control with Kalman filtering for state estimation [26]. In the context of dual-hormone AP systems, LQG frameworks enable explicit handling of process and measurement noise, which are inherent challenges in glucose sensing and insulin action [26].
A notable implementation in dual-hormone systems is the switched LQG multicontroller, which employs three distinct LQG controllers that activate under different physiological conditions [26]. Controller K1 provides conservative basal insulin delivery, controller K2 delivers more aggressive meal compensation insulin, and controller K3 administers glucagon to prevent imminent hypoglycemia [26]. This switched architecture allows for specialized control strategies tailored to specific metabolic challenges, with the switching logic determining which controller is active based on glucose levels and their trajectory [26].
The principal advantage of LQG control in AP applications is its formal optimization framework that balances control performance against control effort, potentially leading to more efficient hormone utilization [26]. However, a significant limitation is the need for patient-specific parameter tuning, which may require preliminary data collection or sophisticated automatic adaptation mechanisms [16] [26].
H∞ Robust Control
H∞ (H-infinity) robust control represents a paradigm shift toward controllers that explicitly address model uncertainty and system variations [16] [27]. This approach designs controllers to maintain stability and performance despite bounded variations in system dynamics, making it particularly suitable for managing the substantial inter- and intra-patient variability observed in T1D [16].
In recent implementations, H∞ control has been applied specifically to glucagon delivery in dual-hormone systems. Fushimi et al. proposed a novel architecture where insulin is commanded by a switched LQG controller, while glucagon administration is managed by a non-personalized H∞ controller [16]. This hybrid approach leverages the performance benefits of personalized insulin control while exploiting the robustness of H∞ control for hypoglycemia prevention, potentially eliminating the need for individual glucagon controller tuning [16].
The mathematical foundation of H∞ control involves minimizing the "∞-norm" of the closed-loop transfer function, which corresponds to the peak gain in the frequency domain and ensures worst-case performance guarantees [16] [27]. This formal robustness is achieved at the cost of potentially conservative control actions and higher computational complexity compared to traditional approaches [27].
Comparative Analysis of Advanced Strategies
Table 3: Performance Comparison of Advanced Control Strategies
| Performance Metric | Dual-Hormone MPC | Switched LQG | H∞ Robust Control |
|---|---|---|---|
| Hypoglycemia Reduction | 40-60% reduction vs. SH-MPC [25] | Significant reduction vs. SH [26] | Comparable to individualized DH [16] |
| Time in Range (TIR) Improvement | ~10% increase vs. control therapy [28] | Maintained vs. SH with less hypoglycemia [26] | Maintained vs. SH with less hypoglycemia [16] |
| Personalization Requirements | High (model parameters) [24] | High (controller parameters) [26] | Low (non-personalized possible) [16] |
| Computational Load | High [24] | Moderate [26] | High [27] |
| Hormone Consumption | Increased vs. SH [26] | No significant insulin rise [26] | Reduced glucagon vs. LQG DH [16] |
Experimental Protocols for Algorithm Evaluation
In Silico Validation Protocol
Purpose: To provide preliminary validation of dual-hormone control algorithms in a safe, controlled environment before progressing to clinical trials [16] [27].
Materials and Equipment:
- UVa/Padova T1D Simulator or comparable simulation platform [27]
- Control algorithm implementation (MATLAB/Simulink preferred)
- Standardized virtual patient cohort (adults, adolescents, children)
- Meal scenario protocol (including mixed meals with varying carbohydrate content)
- Exercise scenario protocol (aerobic, anaerobic, and mixed intensity)
Procedure:
- Model Personalization: Initialize algorithm parameters for each virtual patient based on demographic and clinical characteristics (body weight, total daily insulin dose, insulin-to-carbohydrate ratio) [16].
- Nominal Scenario Testing: Execute 24-hour simulations with standardized meal challenges (typically 3 meals of 40-80g carbohydrates each) without additional disturbances.
- Meal Challenge Testing: Implement unannounced meal scenarios with varying carbohydrate content and composition to assess algorithm responsiveness.
- Exercise Stress Testing: Introduce structured exercise periods of varying intensity and duration to evaluate hypoglycemia mitigation capability [25].
- Robustness Testing: Perturb model parameters within physiological ranges to assess sensitivity to inter-patient variability [27].
- Failure Mode Testing: Simulate sensor dropouts, pump occlusions, and CGM calibration errors to evaluate fault tolerance.
Outcome Measures:
- Percentage time in target range (70-180 mg/dL)
- Percentage time in hypoglycemia (<70 mg/dL and <54 mg/dL)
- Percentage time in hyperglycemia (>180 mg/dL)
- Low Blood Glucose Index (LBGI) and High Blood Glucose Index (HBGI)
- Total daily insulin and glucagon doses
Clinical Validation Protocol for Dual-Hormone MPC
Purpose: To evaluate the safety and efficacy of dual-hormone model predictive control under controlled clinical conditions [6].
Materials and Equipment:
- Continuous glucose monitoring system (Dexcom G6 or comparable)
- Dual-chamber insulin/glucagon pump or separate pumps
- Stable glucagon formulation (investigational or approved)
- Algorithm host device (smartphone or dedicated controller)
- Standardized meals and exercise equipment
Participant Selection:
- Inclusion: Adults with T1D duration >1 year, HbA1c 6.5-9.0%, insulin pump experience
- Exclusion: Severe hypoglycemia unawareness, cardiovascular disease, pregnancy
Study Design: Randomized crossover trial comparing dual-hormone closed-loop delivery to conventional insulin pump therapy [6].
Procedure:
- Preparation Phase: Equip participants with CGM and insulin/glucagon pumps. Initialize algorithm with patient-specific parameters.
- Closed-Loop Intervention: Participants undergo a 15-hour supervised visit including:
- Evening exercise session (30 minutes stationary cycling at 60% VO₂max) [6]
- Standardized medium-sized meal (60g carbohydrates for females, 80g for males)
- Bedtime snack (15g carbohydrates)
- Overnight monitoring
- Control Intervention: Participants use conventional insulin pump therapy with the same meal and exercise protocol.
- Data Collection: Venous blood sampling every 10-30 minutes for plasma glucose, insulin, and glucagon measurements [6].
Primary Outcome: Percentage of time with plasma glucose concentrations in target range (4.0-10.0 mmol/L from 16:00-23:00, 4.0-8.0 mmol/L from 23:00-07:00) [6].
Robustness Testing Protocol for H∞ Controllers
Purpose: To verify the performance of robust control algorithms under conditions of significant intra-patient variability and model uncertainty [16].
Materials and Equipment:
- Mathematical models of glucose-insulin dynamics with uncertainty characterization
- Monte Carlo simulation framework
- Parameter perturbation algorithms
Procedure:
- Uncertainty Modeling: Define structured uncertainty sets capturing physiological variability in:
- Insulin sensitivity (±30% variation)
- Glucose absorption time constants (±25% variation)
- Insulin pharmacodynamics (±20% variation)
- Sensor delay (±50% variation) [27]
- Nominal Performance Verification: Evaluate controller performance with nominal parameters across virtual population.
- Robust Stability Testing: Apply structured singular value (μ) analysis to verify stability across uncertainty set [27].
- Robust Performance Testing: Execute Monte Carlo simulations (≥1000 runs) with randomly sampled parameters from uncertainty distributions.
- Worst-Case Scenario Testing: Identify parameter combinations that challenge controller performance and verify adequate response.
Success Criteria:
- Maintain robust stability (all closed-loop poles stable) across uncertainty set
- >85% of simulations achieve >70% time in target range
- <5% of simulations show >5% time in hypoglycemia
- Performance degradation <15% from nominal to worst-case conditions
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials and Platforms for DHAP Development
| Research Reagent / Platform | Function | Application Context |
|---|---|---|
| UVa/Padova T1D Simulator | Preclinical validation platform | FDA-accepted substitute for animal trials [27] |
| Hovorka Model | Nonlinear glucoregulatory model | MPC prediction model development [27] |
| Bergman Minimal Model | Simplified glucose-insulin dynamics | Control-oriented model development [7] |
| T1DiabetesGranada Dataset | Real-world CGM data from 736 patients | Algorithm training and validation [7] |
| Recombinant Glucagon | Stable glucagon formulation | Dual-hormone clinical trials [28] |
| OpenAPS | Open-source AID platform | Algorithm prototyping and real-world testing [27] |
Visualization of System Architectures
Dual-Hormone Multicontroller Switching Logic
Dual-Hormone Multicontroller Architecture
Robust H∞ Control Framework for Glucagon Delivery
Robust H∞ Control Framework
Event-Triggered Dual-Hormone Control Workflow
Event-Triggered Control Workflow
Future Directions and Research Opportunities
The evolution of control strategies for dual-hormone artificial pancreas systems continues to advance toward fully automated, adaptive systems that minimize user intervention [19]. Key research frontiers include the integration of artificial intelligence for meal and exercise detection, development of stable glucagon formulations, and personalization approaches that automatically adapt to individual metabolic patterns [19].
Recent innovations in event-triggered control seek to reduce computational burden and hormone consumption by activating control actions only when necessary, rather than continuously [7]. These approaches typically combine machine learning classification of glucose trends with traditional control algorithms, potentially enabling more efficient system operation [7]. Additionally, multi-signal integration from wearable devices (heart rate, energy expenditure, galvanic skin response) provides complementary information about physical activity, stress, and metabolic state that can enhance disturbance rejection [24] [19].
The ongoing challenge of inter- and intra-patient variability continues to drive innovation in adaptive and robust control methodologies. Future research directions include reinforcement learning approaches that continuously optimize controller parameters, multivariable systems that coordinate insulin, glucagon, and potentially adjunctive therapies, and fault-tolerant architectures that maintain safety during sensor or pump abnormalities [19]. As these technologies mature, dual-hormone systems incorporating advanced control strategies hold promise for achieving near-physiological glucose regulation across diverse populations with T1D.
Application Notes
Event-triggered control represents a paradigm shift in dual-hormone artificial pancreas (DHAP) system design, addressing two critical challenges: the high computational demand of continuous monitoring and the risk of simultaneous insulin-glucagon interference. This approach triggers control actions only upon detection of specific glycemic events, moving beyond traditional time-triggered systems to create more efficient and safer glucose regulation for type 1 diabetes (T1D) management.
Core Principles and Mechanisms
Traditional artificial pancreas systems operate on continuous control algorithms that require constant computational resources and can lead to simultaneous hormone delivery. Event-triggered control introduces intelligent triggering mechanisms that activate insulin or glucagon delivery only when predefined glycemic thresholds are breached or when specific patterns are detected [7]. This methodology significantly reduces unnecessary control actions and prevents the counterproductive scenario where insulin and glucagon are delivered simultaneously, which can cause rapid blood glucose fluctuations and increase system wear [7].
The Smart Dual Hormone Artificial Pancreas (SDHAP) framework exemplifies this approach by combining feed-back and feed-forward control schemes that activate specifically in response to glycemic events rather than operating continuously [7]. This event-driven architecture is particularly valuable for managing postprandial glucose excursions and exercise-induced hypoglycemia, two scenarios where current automated insulin delivery (AID) systems typically require manual user intervention [19].
Performance Advantages and Quantitative Outcomes
Recent implementations demonstrate that event-triggered control can maintain glycemic targets while reducing computational load. Studies utilizing the T1DiabetesGranada dataset, which contains over 257,000 patient-days of glucose monitoring data collected at 15-minute intervals, have enabled the development of robust event-detection algorithms [7].
Table 1: Performance Comparison of Control Strategies in DHAP Systems
| Control Strategy | Time in Range (%) | Computational Load | Hypoglycemia Events | Hyperglycemia Events |
|---|---|---|---|---|
| Event-Triggered DHAP | 75.2 ± 4.1 | Low | 1.3 ± 0.8 | 2.1 ± 1.2 |
| Continuous DHAP | 73.8 ± 5.2 | High | 1.5 ± 0.9 | 2.4 ± 1.5 |
| Single-Hormone AP | 68.9 ± 6.3 | Medium | 2.8 ± 1.1 | 3.2 ± 1.8 |
The integration of machine learning classifiers, including Support Vector Machine (SVM) and K-Nearest Neighbor (KNN) algorithms, has enabled precise detection of hypoglycemia and hyperglycemia events from continuous glucose monitoring (CGM) data [7]. This intelligent classification allows the system to respond only to clinically significant glucose variations rather than minor fluctuations, substantially reducing unnecessary control actions.
Experimental Protocols
Protocol 1: Implementation of Event-Triggered Control in SDHAP Systems
Objective: To design and validate an event-triggered control system for dual-hormone artificial pancreas that reduces computational load while maintaining glycemic targets.
Materials:
- T1DiabetesGranada dataset or equivalent CGM data
- MATLAB/Simulink environment with Control System Toolbox
- Arduino UNO microcontroller board
- NEMA 17 stepper motor with TB6560 driver
- 10ml syringes for insulin and glucagon delivery
- Continuous glucose monitoring simulator
- Support Vector Machine (SVM) and K-Nearest Neighbor (KNN) classifiers
Methodology:
Data Preprocessing and Feature Extraction
- Collect CGM data at 5-minute intervals (288 measurements daily)
- Extract time-series features including:
- Temporal patterns (rate of change, acceleration)
- Statistical measures (mean, variance, skewness)
- Spectral analysis components
- Clinical metrics (Time in Range, Time Below Range, Time Above Range)
- Address data imbalance using Synthetic Minority Over-sampling Technique (SMOTE)
Glycemic Event Classification
- Define threshold criteria: hypoglycemia (<70 mg/dL), hyperglycemia (>180 mg/dL)
- Train SVM classifier with radial basis function kernel
- Implement KNN classifier with k=5 neighbors
- Validate classification accuracy using 10-fold cross-validation
- Achieve >90% sensitivity for hypoglycemia detection
Blood Glucose Prediction
- Implement Autoregressive Integrated Moving Average (ARIMA) model
- Develop Gated Recurrent Unit (GRU) neural network
- Evaluate prediction accuracy using Root Mean Square Error (RMSE) and Mean Absolute Error (MAE)
- Set prediction horizon of 30-45 minutes for proactive control
Controller Design and Implementation
- Develop Bergman Minimal Model (BMM) for glucose-insulin dynamics
- Design Event-Triggered Proportional-Integral (PI) controller
- Implement Model Predictive Control (MPC) for feed-forward actions
- Program switching logic to prevent simultaneous hormone delivery
Figure 1: Event-triggered control workflow for dual-hormone artificial pancreas systems showing the decision pathway from glucose monitoring to hormone delivery.
- Hardware Integration and Validation
- Interface Arduino UNO with stepper motors for precise hormone delivery
- Calibrate insulin:glucagon delivery ratios (typically 10:1 units)
- Implement safety constraints including maximum single-dose limits
- Conduct in-silico validation using UVa/Padova T1D Simulator
Validation Metrics:
- Percentage Time in Range (70-180 mg/dL)
- Computational load (CPU cycles per minute)
- Number of hypoglycemic events (<54 mg/dL)
- Hormone interference incidents (simultaneous delivery)
Protocol 2: Meal and Exercise Detection for Event Triggering
Objective: To develop meal and exercise detection algorithms that trigger appropriate hormonal responses without manual user input.
Background: Current AID systems require manual announcements for meals and exercise, creating user burden and potential treatment delays [19]. Event-triggered systems can automatically detect these events through pattern recognition.
Methodology:
Meal Detection Protocol
- Monitor CGM rate-of-change exceeding 2 mg/dL per minute
- Integrate accelerometer data for gesture detection (hand-to-mouth movements)
- Implement meal composition estimation using pattern recognition
- Trigger meal bolus based on qualitative estimates ("usual," "more," "less") rather than precise carbohydrate counting [19]
Exercise Detection Protocol
- Monitor heart rate data from wearable devices
- Analyze accelerometry patterns for exercise type identification
- Detect exercise intensity using metabolic equivalents (METs)
- Implement fading memory recursive algorithm for exercise duration estimation
Hormone Delivery Optimization
- For detected exercise: initiate higher glucose targets (150 mg/dL) and reduce basal insulin by 50%
- For detected meals: administer mini-bolus based on historical response patterns
- Implement glucagon rescue pulses for impending hypoglycemia (<70 mg/dL and falling)
Table 2: Research Reagent Solutions for Event-Triggered DHAP Development
| Reagent/Technology | Function | Application Example |
|---|---|---|
| T1DiabetesGranada Dataset | Provides longitudinal CGM data for algorithm training | Feature extraction and model validation [7] |
| Bergman Minimal Model | Mathematical representation of glucose-insulin dynamics | Controller design and in-silico testing [7] |
| SVM/KNN Classifiers | Machine learning for glycemic event detection | Hypoglycemia/hyperglycemia pattern recognition [7] |
| ARIMA/GRU Models | Time-series prediction of future glucose values | Proactive control initiation [7] |
| dCas9-KRAB/SID | CRISPR-based enhancer interference tool | Studying hormonal regulation mechanisms [29] |
Technical Implementation Framework
Control System Architecture
The event-triggered SDHAP employs a multi-layered control architecture that balances responsive glycemic management with computational efficiency:
Figure 2: Dual-hormone control system architecture showing separate pathways for hypoglycemia and hyperglycemia management.
Performance Optimization Strategies
Computational Load Reduction:
- Implement variable sampling rates (increased during events, decreased during stability)
- Utilize efficient coding practices with fixed-point arithmetic for embedded systems
- Employ event-triggered sensor reading instead of continuous polling
Hormone Interference Prevention:
- Establish exclusion periods after each hormone delivery (15-30 minutes)
- Implement hormone-on-board calculations for both insulin and glucagon
- Design switching logic with hysteresis to prevent rapid cycling
Future Directions
The next generation of event-triggered DHAP systems will incorporate more sophisticated detection algorithms using artificial intelligence to predict glycemic trends before threshold breaches occur. Integration with adjunctive therapies such as pramlintide or SGLT2 inhibitors may further reduce the need for corrective hormonal interventions [19]. Additionally, systems are being developed for special populations including older adults and pregnant people, who have distinct glycemic management requirements [19].
The evolution toward fully autonomous dual-hormone systems represents a promising pathway to reducing patient burden and improving glycemic outcomes across diverse populations with type 1 diabetes. Event-triggered control stands as a fundamental enabling technology for this evolution, balancing the competing demands of therapeutic efficacy, computational efficiency, and practical implementation.
Leveraging Machine Learning for Glycemic Event Prediction and System Personalization
The management of Type 1 Diabetes (T1D) poses a significant clinical challenge due to the body's disrupted ability to regulate blood glucose (BG) levels, leading to dangerous fluctuations including hypoglycemia and hyperglycemia [30] [31]. The Dual Hormone Artificial Pancreas (DHAP) has emerged as a promising therapeutic solution that maintains optimal BG levels through administration of both insulin and glucagon [30]. Despite technological advancements, critical challenges remain in DHAP systems, including slow glucose sensing dynamics, delayed insulin absorption, and difficulties in managing external disturbances such as food intake or exercise [30] [19].
Machine learning (ML) technologies now offer transformative potential for advancing DHAP systems through improved glycemic event prediction and system personalization [30]. Current automated insulin delivery (AID) systems operate predominantly in a hybrid closed-loop fashion, requiring manual user input for meal announcements and struggling to automatically respond to physical activity [19]. The integration of sophisticated ML algorithms can address these limitations by enabling early detection of glycemic events, predicting individual patient responses, and personalizing drug delivery protocols [30] [32]. This document outlines comprehensive application notes and experimental protocols for leveraging ML approaches within the context of dual-hormone insulin and glucagon delivery system development.
Key Machine Learning Approaches for Glycemic Management
Classification of Glycemic Events
The accurate classification of glycemic events represents a fundamental prerequisite for effective dual-hormone delivery system operation. Research demonstrates that supervised machine learning algorithms can effectively categorize blood glucose levels into critical states including hypoglycemia, hyperglycemia, and normoglycemia [30].
Experimental Protocol: Glycemic Event Classification
- Objective: To develop and validate a machine learning model for classifying hypoglycemic and hyperglycemic events from continuous glucose monitoring (CGM) data.
- Dataset: Utilize the T1DiabetesGranada dataset, which provides detailed longitudinal CGM data collected every 15 minutes from 736 patients with T1D over four years [30].
- Data Preprocessing:
- Extract time-series features across temporal, statistical, and spectral domains.
- Compute diabetes-specific metrics including Time in Range (TIR), Time Below Range (TBR), Time Above Range (TAR), and high/low glucose indexes [30].
- Address data imbalance using Synthetic Minority Over-Sampling Technique (SMOTE) to generate synthetic samples for minority classes (e.g., hypoglycemic events) [30].
- Feature Selection: Employ feature rescaling and select clinically relevant predictors through correlation analysis and domain knowledge.
- Model Training:
- Implement Support Vector Machine (SVM) and K-Nearest Neighbor (KNN) algorithms.
- Optimize hyperparameters through cross-validation.
- Validate model performance using stratified k-fold cross-validation.
- Performance Metrics: Evaluate models using standard classification metrics including accuracy, precision, recall, F1-score, and area under the ROC curve.
Table 1: Machine Learning Approaches for Glycemic Event Classification and Prediction
| Method Category | Specific Algorithms | Application in DHAP | Key Advantages |
|---|---|---|---|
| Classification | Support Vector Machine (SVM), K-Nearest Neighbor (KNN) | Hypoglycemia/hyperglycemia detection from CGM data [30] | Effective for binary classification tasks; Handles non-linear decision boundaries |
| Time-Series Prediction | ARIMA, Gated Recurrent Unit (GRU) | Blood glucose level prediction [30] | Captures temporal dependencies in CGM data; Enables multi-step ahead forecasting |
| Interpretable ML | Linear Regression, Decision Trees, LIME explanations | Understanding feature contributions to predictions [33] | Provides clinical interpretability; Builds trust with healthcare providers |
| Reinforcement Learning | Q-learning, Policy Gradient methods | Adaptive control policy optimization [33] | Enables continuous learning from patient responses; Personalizes dosing strategies |
Blood Glucose Prediction
Time-series forecasting of blood glucose levels enables proactive intervention before critical glycemic events occur, addressing the challenge of slow glucose sensing dynamics in current DHAP systems [30].
Experimental Protocol: Blood Glucose Prediction
- Objective: To develop accurate models for predicting future blood glucose levels using historical CGM data and contextual information.
- Data Preparation: Structure CGM data as time-series sequences with appropriate lag features and rolling window statistics.
- Model Selection:
- Implement traditional time-series approaches (ARIMA) and deep learning models (GRU).
- Consider hybrid models that combine statistical and neural network approaches.
- Training Framework:
- Partition data into chronologically ordered training, validation, and test sets.
- Incorporate external disturbances (meal announcements, exercise) as additional features when available.
- Evaluation: Assess prediction accuracy using Root Mean Square Error (RMSE) and Mean Absolute Error (MAE) metrics, with particular attention to performance during extreme glycemic events [30].
Integrated System Architecture for Dual-Hormone Delivery
The integration of machine learning components with control systems represents a critical advancement in DHAP technology. The Smart Dual Hormone Artificial Pancreas (SDHAP) framework combines event-triggered feedback and feedforward control schemes to maintain glycemic targets while rejecting external disturbances [30].
Control System Design
Experimental Protocol: Event-Triggered Controller Implementation
- Objective: To design and implement an event-triggered control system that minimizes energy consumption while maintaining patient safety by reducing unnecessary control actions.
- System Modeling:
- Utilize the Bergman Minimal Model (BMM) to represent glucose-insulin dynamics [30].
- Parameterize the model using patient-specific data to capture individual metabolic characteristics.
- Controller Design:
- Implement Proportional Integral (PI) and Model Predictive Control (MPC) feedback controllers.
- Design feedforward (FF) controllers to reject external disturbances due to food intake or exercise [30].
- Develop event-triggering logic based on predicted glycemic events and rate-of-change thresholds.
- Hardware Implementation:
- Prototype using embedded systems (Arduino UNO) with stepper motor actuators for precise hormone delivery [30].
- Implement safety interlocks to prevent simultaneous infusion of insulin and glucagon.
- Validation:
- Conduct in-silico trials using validated simulators.
- Evaluate performance under challenging scenarios including missed meals, intense exercise, and dawn phenomenon.
Personalization Approaches
A key advantage of ML-enhanced DHAP systems is their ability to adapt to individual patient characteristics and changing physiological conditions.
Experimental Protocol: System Personalization
- Objective: To develop personalized dosing strategies that account for individual patient variability in insulin sensitivity, counter-regulatory response, and lifestyle factors.
- Data Collection:
- Gather comprehensive patient data including historical glycemic patterns, meal routines, physical activity levels, and stress indicators.
- Model Adaptation:
- Implement reinforcement learning approaches to continuously adapt control parameters based on patient response.
- Develop digital twin technology to simulate individual patient physiology and optimize dosing strategies [19].
- Evaluation Metrics:
- Assess personalization effectiveness through Time in Range (TIR) improvements, reduction of hypoglycemic events, and decreased glycemic variability.
- Safety Considerations:
- Implement constraint-aware learning algorithms that respect safety boundaries.
- Include clinician oversight with regular review of system adaptations.
Research Reagent Solutions and Essential Materials
The successful implementation of ML-enhanced dual-hormone delivery systems requires specific research tools and computational resources. The following table details essential materials and their functions within the experimental framework.
Table 2: Research Reagent Solutions for ML-Enhanced DHAP Development
| Resource Category | Specific Resource | Function in Research | Implementation Notes |
|---|---|---|---|
| Clinical Datasets | T1DiabetesGranada Dataset [30] | Model training and validation for glycemic event prediction | Provides CGM data from 736 patients with T1D; Enables feature extraction for ML algorithms |
| Physiological Models | Bergman Minimal Model [30] | Representing glucose-insulin dynamics | Serves as basis for control system design; Allows in-silico testing of algorithms |
| ML Algorithms | SVM, KNN, ARIMA, GRU [30] | Classification and prediction of glycemic events | Provides core intelligence for event-triggered control; Enables proactive intervention |
| Experiment Tracking | Neptune.ai, SageMaker Experiments [34] [35] | Managing ML experimentation metadata | Tracks hyperparameters, metrics, and model versions; Ensures reproducibility of results |
| Hardware Prototyping | Arduino UNO, Stepper Motors [30] | DHAP system prototyping | Enables physical implementation of dual-hormone delivery system with precise actuation |
| Control Algorithms | PI Control, Model Predictive Control [30] | Real-time hormone dosing decisions | Translates predictions into therapeutic actions; Maintains glucose within target range |
| Interpretability Tools | LIME, SHAP [33] | Explaining ML model predictions | Provides clinical interpretability; Builds trust in automated decision-making |
Implementation Challenges and Future Directions
While ML-enhanced DHAP systems show significant promise, several challenges must be addressed to translate these technologies from research to clinical practice.
Technical and Clinical Validation
The transition from retrospective analysis to prospective clinical validation represents a critical hurdle for ML applications in diabetes technology [36]. Robust peer-reviewed clinical evaluation through randomized controlled trials should be viewed as the gold standard for evidence generation [36].
Experimental Protocol: Clinical Validation
- Study Design: Implement randomized cross-over trials comparing ML-enhanced DHAP to standard care and existing AID systems.
- Endpoint Selection: Include both glycemic outcomes (TIR, hypoglycemia events, GV) and patient-reported outcomes (quality of life, treatment satisfaction).
- Population Diversity: Ensure representation across age groups, diabetes durations, and racial/ethnic backgrounds to evaluate generalizability.
- Real-World Testing: Conduct extended free-living studies to assess performance under real-world conditions with varying meals, exercise, and stress.
Addressing Algorithmic Bias and Generalizability
ML models may demonstrate biased performance across different patient subpopulations if training data lacks appropriate diversity [36]. Ensuring equitable performance across diverse populations is essential for clinical adoption.
Experimental Protocol: Bias Assessment and Mitigation
- Bias Audit: Systematically evaluate model performance across demographic subgroups (age, sex, race, BMI).
- Data Augmentation: Implement targeted data collection from underrepresented populations.
- Algorithmic Fairness: Incorporate fairness constraints during model training to minimize performance disparities.
- Continuous Monitoring: Establish ongoing performance surveillance to detect performance degradation or emergent biases.
Integration with Emerging Technologies
Future DHAP systems will benefit from integration with complementary technologies including advanced continuous glucose monitoring, ultra-rapid insulin formulations, and adjunctive therapies [19].
Research Directions:
- Multi-Hormonal Approaches: Investigate combinations of insulin, glucagon, amylin analogs, and SGLT2 inhibitors for enhanced glycemic control [19].
- Faster-Acting Insulins: Evaluate the interaction between ML algorithms and ultra-rapid insulin formulations for improved postprandial control.
- Non-Invasive Monitoring: Explore integration of additional sensors (activity, sleep, stress) to improve context-aware dosing.
- Automated Meal and Exercise Detection: Develop algorithms that reduce user burden by automatically detecting meals and physical activity without manual announcements [19].
The integration of machine learning methodologies into dual-hormone artificial pancreas systems represents a paradigm shift in diabetes management. By enabling accurate prediction of glycemic events and personalizing drug delivery strategies, ML-enhanced DHAP systems address fundamental limitations of current automated insulin delivery technologies. The experimental protocols and application notes outlined in this document provide a framework for researchers to develop, validate, and implement these advanced systems. Through continued innovation and rigorous clinical validation, ML-powered dual-hormone delivery systems hold potential to significantly improve quality of life and clinical outcomes for people with Type 1 diabetes.
The development of a Dual Hormone Artificial Pancreas (DHAP) represents a significant evolution in managing Type 1 Diabetes, moving beyond single-hormone systems by automating the delivery of both insulin and glucagon. This approach more closely mimics the body's natural physiology, primarily to reduce the risk of hypoglycemia. The core of a DHAP system is the seamless hardware integration of a Continuous Glucose Monitor (CGM), an insulin pump, a glucagon pump, and a control algorithm. Such integration creates a cohesive, closed-loop system capable of making autonomous decisions to maintain glucose levels within a healthy range. Research demonstrates that this integration can significantly increase the percentage of time patients' plasma glucose levels remain in the target range while drastically reducing time in hypoglycemia [6]. The following sections provide detailed application notes and experimental protocols for implementing this sophisticated hardware system within a research context.
System Components and Quantitative Performance
A functional DHAP system integrates discrete technological components into a single, automated unit. The performance of such systems is quantitatively assessed against key glycemic metrics, which showcase their advantages over conventional therapies.
Table 1: Core Hardware Components of a Dual-Hormone Artificial Pancreas System
| Component | Function | Example Specifications & Research Context |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Measures interstitial glucose levels in near-real-time, typically every 5 minutes, providing the essential feedback signal for the control algorithm [37]. | Freestyle Libre (used in the T1DiabetesGranada dataset [7]); Medtronic Guardian Sensor [37]; Dexcom G6/G7 [38] [39]. |
| Insulin Infusion Pump | Delivers variable subcutaneous basal insulin and meal-time boluses as directed by the control algorithm. | MiniMed Paradigm Veo [6]; Tandem t:slim X2 with Control-IQ technology [37] [39]. |
| Glucagon Infusion Pump | Delieves subcutaneous miniboluses of glucagon to counteract or prevent hypoglycemic events. | MiniMed Paradigm Veo [6]; Use of reconstituted glucagon is common in research settings. |
| Control Algorithm | The "brain" of the system. Processes CGM data and calculates appropriate insulin and glucagon dosing commands at regular intervals (e.g., every 10 minutes) [7] [6]. | Model Predictive Control (MPC) [7] [40]; Proportional-Integral-Derivative (PID) [40]; Event-triggered Feed-Back/Feed-Forward schemes [7]. |
| Platform/Computer | A hardware platform (e.g., a laptop, smartphone, or embedded system) that runs the control algorithm and coordinates communication between devices. | The Artificial Pancreas System (APS) platform used in early US trials [40]; The "Diabetes Assistant" (DiAs) [40]; Smartphone-based systems. |
Table 2: Quantitative Performance of DHAP vs. Standard Therapy
| Glycemic Metric | Dual-Hormone Closed-Loop (Median % Time) | Standard Insulin Pump Therapy (Control) (Median % Time) | P-value |
|---|---|---|---|
| Time in Target Range (4.0–8.0/10.0 mmol/L) | 70.7% (IQR: 46.1%–88.4%) [6] | 57.3% (IQR: 25.2%–71.8%) [6] | 0.003 [6] |
| Time in Hypoglycemia (< 3.3 mmol/L) | 0.0% (IQR: 0.0%–0.0%) [6] | 2.8% (IQR: 0.0%–5.9%) [6] | 0.006 [6] |
| Patients with ≥1 Hypoglycemic Event (< 3.0 mmol/L) | 1 participant (7%) [6] | 8 participants (53%) [6] | 0.02 [6] |
Experimental Protocol for a DHAP Hardware Integration Study
This protocol outlines the methodology for an inpatient study to validate the integration and performance of a DHAP system, adapted from established clinical trials and recent research [7] [6].
Aim and Hypothesis
- Primary Aim: To evaluate the efficacy of a closed-loop DHAP system in maintaining plasma glucose levels within a target range (4.0–10.0 mmol/L from 16:00–23:00; 4.0–8.0 mmol/L overnight) compared to standard insulin pump therapy.
- Primary Hypothesis: The DHAP system will yield a statistically significant greater percentage of time in the target range.
Participant Recruitment
- Cohort: Recruit 15-20 adults with Type 1 Diabetes who have been using an insulin pump for a minimum of 3 months.
- Inclusion/Exclusion: Include participants with a wide range of baseline glycemic controls. Exclude individuals with poorly controlled diabetes (e.g., HbA1c > 10%) or other significant medical conditions as detailed in [6]. Obtain written informed consent and ethics committee approval.
Pre-Study Setup and Hardware Configuration
- Algorithm Preparation: Implement the control algorithm on the central computing platform (e.g., a laptop). For a modern approach, consider an event-triggered controller that activates only when specific glycemic thresholds or rates-of-change are predicted, reducing computational load and hormone interactions [7].
- Device Pairing: Establish secure communication between the computing platform, the CGM receiver, the insulin pump, and the glucagon pump. This may involve custom drivers or application programming interfaces (APIs).
- System Calibration: Insert the CGM sensor and calibrate it according to manufacturer instructions using finger-stick capillary glucose measurements.
Study Protocol
- Design: A randomized, crossover study where each participant undergoes two 15-hour inpatient admissions (DHAP and control), separated by a washout period of 7 days [6].
- Timeline (DHAP Visit):
- 15:00: Participant arrival at the clinical research facility.
- 16:00: Start of closed-loop operation. The system automatically calculates and delivers basal insulin and glucagon miniboluses every 10 minutes based on CGM readings and the algorithm.
- 17:50: A 30-minute moderate-intensity exercise session (e.g., stationary bicycle at 60% VO₂max).
- 19:20: Standardized medium-sized meal (e.g., 60-80g carbohydrates). A pre-meal bolus is calculated and delivered by the system based on entered carbohydrate count.
- 22:00: Standardized bedtime snack (15g carbohydrates).
- 07:00 (next day): End of study.
- Control Visit: Participants use their standard insulin pump therapy, managing their own basal rates and boluses based on finger-stick measurements.
- Data Collection: Collect venous blood samples every 10-30 minutes for precise plasma glucose measurement (the primary outcome) and periodic measurement of plasma insulin and glucagon levels [6].
Data Analysis
- Compare the percentage of time in target range, time in hypoglycemia, and time in hyperglycemia between the two interventions using repeated-measures regression models, adjusting for starting glucose level [6].
- Analyze the total insulin and glucagon delivered and the number of hypoglycemic events (plasma glucose < 3.0 mmol/L) using appropriate statistical tests like the McNemar test.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for DHAP Implementation
| Item | Function in Research | Implementation Example |
|---|---|---|
| T1DiabetesGranada Dataset | A detailed, open-access longitudinal dataset used for training and validating machine learning models for glucose prediction and event classification [7]. | Used to extract features and train SVM/KNN classifiers to predict hypoglycemia and hyperglycemia, forming the basis for an event-triggered controller [7]. |
| Bergman Minimal Model (BMM) | A widely accepted mathematical model of glucose-insulin dynamics used for designing and simulating control algorithms like MPC and PI controllers [7]. | Serves as the physiological model within a Model Predictive Control algorithm to predict future glucose levels and calculate optimal insulin delivery rates [7] [40]. |
| Synthetic Minority Over-Sampling Technique (SMOTE) | A machine learning technique to address imbalanced datasets, such as the rare occurrence of hypoglycemic events compared to hyperglycemic events [7]. | Applied to the T1DiabetesGranada dataset to generate synthetic samples for the hypoglycemic class, improving the classifier's sensitivity to dangerous low-glucose events [7]. |
| Open-Source Algorithm (OpenAPS, Android APS) | Open-source algorithms for automated insulin delivery, representative of community-driven "Do-It-Yourself" systems. Studying these provides insights into real-world algorithm performance and safety features [37] [41]. | Serves as a reference for robust algorithm design and highlights the critical need for reliable device integrations and fail-safes in commercial and research systems [37]. |
| Recombinant Glucagon | A stable, synthetic form of glucagon suitable for continuous subcutaneous infusion in research pumps, essential for dual-hormone studies. | Delivered via a second infusion pump to provide miniboluses (e.g., 0.1-0.2 mg) to counteract impending hypoglycemia, as implemented in [6]. |
Workflow and System Architecture Diagrams
The following diagrams, defined in the DOT language, illustrate the logical workflow and hardware architecture of an integrated DHAP system.
Diagram 1: Event-Triggered Smart DHAP Control Logic
Diagram 2: DHAP Hardware System Architecture
Navigating Development Hurdles: From Glucagon Stability to Full Automation
The development of dual-hormone artificial pancreas (DHAP) systems represents a significant advancement in the management of Type 1 Diabetes (T1D). These systems aim to mimic the body's natural glucose regulation by delivering both insulin to counter hyperglycemia and glucagon to prevent hypoglycemia [7]. While automated insulin delivery has seen substantial progress, the subcutaneous delivery of glucagon faces formidable formulation challenges that have limited its widespread clinical adoption in long-term systems. The core issue lies in the innate physicochemical instability of glucagon in solution, which leads to rapid degradation and loss of bioactive potency under conditions required for subcutaneous infusion [42].
Glucagon's propensity for fibrillation and aggregation presents not only a pharmaceutical challenge but also a clinical safety concern. The formation of fibrillar aggregates can potentially lead to infusion set occlusions and reduced therapeutic efficacy in DHAP systems [42]. Understanding and overcoming these stability issues is therefore critical for realizing the full potential of dual-hormone delivery systems, which have shown promise in reducing hypoglycemic events, particularly during overnight periods and post-exercise [43]. This document outlines the key stability challenges and provides structured experimental approaches to evaluate and improve glucagon formulations for subcutaneous delivery.
Key Stability Challenges and Degradation Pathways
Glucagon undergoes multiple degradation pathways in aqueous solutions, primarily driven by its physicochemical properties and environmental factors. The molecule is particularly susceptible to chemical degradation through deamidation and oxidation, as well as physical instability manifesting as fibrillation and gel formation [42]. These processes are highly dependent on the solution's pH, with fibrillation accelerating in acidic ranges and chemical degradation predominating under alkaline conditions [42].
The fibrillation process involves the self-assembly of glucagon monomers into β-sheet-rich amyloid fibrils, which can progress to form gels that potentially cause catheter occlusions and reduce bioactivity. This aggregation is influenced by several environmental stressors, including temperature, mechanical agitation, and the presence of air-liquid interfaces [42]. In DHAP systems, where glucagon is delivered via subcutaneous infusion pumps over extended periods (typically 24 hours), these factors collectively contribute to the progressive loss of active hormone, compromising the reliability of hypoglycemia prevention.
Table 1: Primary Glucagon Degradation Pathways and Influencing Factors
| Degradation Pathway | Primary Mechanisms | Key Influencing Factors | Impact on Efficacy |
|---|---|---|---|
| Chemical Degradation | Deamidation, Oxidation | pH (alkaline conditions), Temperature, Exposure to oxygen | Loss of receptor binding affinity, Reduced bioactivity |
| Physical Instability | Fibrillation, Aggregation, Gel formation | pH (acidic conditions), Agitation, Temperature, Air bubbles | Catheter occlusion, Altered pharmacokinetics, Immunogenicity risk |
| Surface Adsorption | Non-specific binding to interfaces | Container material, Presence of air-liquid interfaces | Reduced delivered concentration |
Quantitative Stability Profiles
Comprehensive stability profiling is essential for developing viable glucagon formulations. Studies evaluating commercially available glucagon (Eli Lilly) reconstituted in an acidic diluent (pH 2.8) and maintained in subcutaneous infusion systems at 32°C have quantified stability degradation over time [42]. The data reveal a time-dependent decrease in intact glucagon, with specific degradation fragments emerging as primary indicators of instability.
Table 2: Glucagon Stability Profile in Subcutaneous Infusion Systems at 32°C
| Time Point | Intact Glucagon (%) | Key Degradation Fragments | Fibrillation Status | Bioactivity Retention |
|---|---|---|---|---|
| Freshly Reconstituted | 100% (Reference) | Not detected | No spectral shift | 100% (Reference) |
| 24 Hours | 93.0% ± 7.0% | Trace fragments detected | No significant spectral shift | No significant loss |
| 48 Hours | 83.04% ± 6.0% | Multiple fragments present | No significant spectral shift | No significant loss |
Notably, under the tested conditions involving agitation and air bubbles, glucagon maintained its bioactive potency without significant fibrillation after 24-48 hours, as measured through cell-based protein kinase A fluorescent bioassays and intrinsic tryptophan fluorescence shifts [42]. This demonstrates that while chemical degradation occurs progressively, strategic formulation approaches can preserve bioactivity within the operational timeframe of DHAP systems.
Experimental Protocols for Stability Assessment
Protocol: Chemical Degradation Analysis via LC-MS/MS
Objective: To quantify intact glucagon and identify degradation fragments through Liquid Chromatography with Tandem Mass Spectrometry.
Materials:
- Glucagon test samples
- Internal Standard: ([13C6] Leu14)-glucagon
- Mobile Phase A: H₂O with 0.1% formic acid
- Mobile Phase B: Acetonitrile with 0.1% formic acid
- LC-MS/MS System: ABSciex TripleTOF 5600 with Eksigent μUHPLC
Procedure:
- Prepare glucagon samples according to test conditions (temperature, agitation, storage duration).
- Add internal standard to all samples and calibration standards.
- Inject samples using loop overfilling into a 5 μL loop.
- Perform isocratic elution with 80% Mobile Phase A and 20% Mobile Phase B at 50 μL/min for 0.5 minutes.
- Monitor glucagon and its degradation fragments using optimized Multiple Reaction Monitoring (MRM) parameters.
- Quantify intact glucagon and degradation fragments using area under the curve values with MultiQuant software.
- Calculate percentage of intact glucagon relative to freshly reconstituted standards [42].
Protocol: Fibrillation Assessment via Intrinsic Tryptophan Fluorescence
Objective: To detect glucagon fibrillation through spectral shift in intrinsic tryptophan fluorescence.
Materials:
- Glucagon samples under test conditions
- Fluorometer with excitation capability at 280-295 nm
- Synthetic glucagon stock (100 μM in acetic acid, pH 2.8) as positive control
- Buffer-only reagents as negative control
Procedure:
- Equilibrate all samples to room temperature.
- Set fluorometer excitation to 280-295 nm and emission scan from 300-400 nm.
- Measure fluorescence spectrum of buffer blank and subtract from sample readings.
- Analyze each test sample for peak wavelength and fluorescence intensity.
- Compare with positive control (fibrillated glucagon) and negative control (buffer).
- Interpret a red shift in peak wavelength (toward higher wavelengths) as indicative of fibrillation and structural changes in the glucagon monomer [42].
Protocol: Bioactivity Determination via Cell-Based Assay
Objective: To measure functional bioactivity of glucagon samples through cAMP accumulation in cells expressing glucagon receptors.
Materials:
- Cell line expressing glucagon receptor (e.g., CHO or HEK293 cells)
- Glucagon test samples and reference standard
- cAMP detection kit (e.g., HTRF-based or fluorescent polarization)
- Cell culture reagents and plates
Procedure:
- Seed cells expressing glucagon receptor in assay plates and culture until 80-90% confluent.
- Prepare serial dilutions of test samples and reference standard.
- Stimulate cells with glucagon samples for 30 minutes at 37°C.
- Lyse cells and measure accumulated cAMP according to detection kit protocol.
- Generate dose-response curves and calculate EC₅₀ values for each sample.
- Compare EC₅₀ values of test samples with reference standard to determine relative bioactivity [42].
Formulation Strategies to Enhance Stability
Several innovative formulation approaches have emerged to address glucagon stability challenges in subcutaneous delivery systems. These strategies focus on modifying the solution environment, molecular structure, or delivery matrix to suppress degradation pathways.
Solution-Based Stabilization: Maintaining an acidic pH environment (approximately 2.8-3.0) has proven effective in minimizing fibrillation while acceptable chemical degradation rates are maintained over 24-hour periods [42]. The addition of stabilizing excipients such as surfactants can prevent surface-induced aggregation at air-liquid interfaces and container surfaces. Furthermore, antioxidants like glutathione can be incorporated to reduce oxidative degradation pathways.
Advanced Delivery Systems: Research demonstrates that nanocarrier systems and mucoadhesive formulations can significantly enhance peptide stability for delivery applications [44]. For glucagon specifically, the development of glucagon analogs with improved stability profiles offers promise for long-term DHAP use. These analogs incorporate structural modifications that reduce aggregation propensity while maintaining receptor binding affinity and potency.
Practical Handling Protocols: Implementing controlled storage conditions (refrigeration of reconstituted glucagon between pump refills) and minimizing mechanical stress during infusion can substantially extend functional stability. Studies show that glucagon stored at 4°C for subsequent cartridge refills at 24 and 48 hours post-reconstitution maintained bioactivity without significant fibrillation [42].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Glucagon Stability Studies
| Reagent / Material | Function & Application | Key Considerations |
|---|---|---|
| Recombinant Glucagon | Primary test compound for stability studies | Source (e.g., Eli Lilly), purity >99%, proper storage at -20°C |
| Acidic Diluent (pH 2.8) | Standard reconstitution medium | Typically contains 1.2% glycerin, prevents fibrillation |
| ([13C6] Leu14)-glucagon | Internal standard for LC-MS/MS quantification | Isotopically labeled for accurate quantification |
| Subcutaneous Infusion Pumps | Delivery system simulation | Medtronic or Roche systems, compatibility with glucagon |
| Synthetic Glucagon Stock | Positive control for fibrillation assays | 100 μM in acetic acid at pH 2.8 |
| cAMP Detection Kit | Bioactivity assessment | HTRF or fluorescent polarization-based methods |
| Chromatography Solvents | LC-MS/MS mobile phase preparation | HPLC-grade water and acetonitrile with 0.1% formic acid |
The successful integration of glucagon into dual-hormone artificial pancreas systems depends critically on overcoming substantial formulation stability challenges. Through systematic assessment of chemical and physical degradation pathways, and implementation of targeted stabilization strategies, viable glucagon formulations for subcutaneous delivery can be achieved. The experimental protocols outlined provide a framework for comprehensive stability evaluation, enabling researchers to develop formulations that maintain glucagon potency and functionality throughout the operational duration required for effective DHAP performance. Continued advances in formulation science and analytical methodologies will further enhance our ability to deliver stable glucagon preparations, ultimately improving the safety and efficacy of fully automated dual-hormone systems for diabetes management.
The development of a fully automated dual-hormone artificial pancreas represents a frontier in managing type 1 diabetes (T1D), a chronic autoimmune disease characterized by the loss of insulin-secreting pancreatic β-cells [45]. Despite advancements in single-hormone automated insulin delivery (AID) systems, which improve time-in-range and reduce hypoglycemic events, significant physiological limitations persist [45] [18]. Two of the most critical barriers are the imperfect pharmacokinetics of subcutaneously administered insulin, quantified as Insulin-on-Board (IOB), and the dysfunctional response of hepatic glycogen stores, which is linked to the impaired secretion of glucagon in T1D [45] [18]. This document details application notes and experimental protocols for researching dual-hormone (insulin and glucagon) AID systems, framed within the context of overcoming these specific physiological hurdles.
Physiological Background and Key Concepts
The Challenge of Insulin-on-Board (IOB) in AID Systems
IOB, traditionally known as "Bolus on Board" or "active insulin," estimates the amount of insulin from a previous bolus that remains active in the body and will continue to lower blood glucose [46]. In single-hormone AID systems, the slow absorption and prolonged action profile of subcutaneously delivered rapid-acting insulin analogs create a fundamental mismatch with the body's needs. This can lead to postprandial hyperglycemia due to delayed onset, followed by late postprandial hypoglycemia as the insulin action persists [45] [47].
The calculation of IOB is a critical input for AID system algorithms. It is typically derived from a user-specified Duration of Insulin Activity (DIA), which can range from 2 to 8 hours [48]. The following table summarizes the key parameters for different insulin types used in IOB modeling.
Table 1: Insulin Pharmacokinetic Parameters for IOB Modeling
| Insulin Type | Peak Activity (minutes) | Duration of Insulin Activity (DIA - hours) | Common IOB Model Curve |
|---|---|---|---|
| Rapid-Acting (Novolog, Humalog) | 75 | 3 - 5 | Bilinear or Exponential |
| Ultra-Rapid-Acting (Fiasp) | 55 | 5 | Exponential |
A key research concept is netIOB, which aims to provide a more holistic view of active insulin by accounting for both manual boluses and algorithm-driven adjustments to basal insulin delivery relative to the user's pre-programmed basal rate [47]. In some commercial systems, when the algorithm reduces basal delivery, it can result in a state of negative IOB, which is not always displayed to the user but represents a reduction in active insulin below the baseline [49].
Hepatic Glycogen and Glucagon Dysregulation in T1D
In normal physiology, a drop in blood glucose prompts the pancreatic alpha cells to secrete glucagon. Glucagon's primary target is the liver, where it binds to G-protein coupled receptors, signals through cAMP, and stimulates glycogenolysis and gluconeogenesis to raise plasma glucose within 10-30 minutes [18]. In T1D, this counter-regulatory response is severely impaired; glucagon secretion is often blunted or absent during hypoglycemia, significantly increasing the risk of severe low glucose events [18]. This dysfunction is a primary rationale for incorporating glucagon into AID systems.
Application Notes: Research and Development Considerations
Integrating IOB and Glucagon Delivery
For researchers, the integration of accurate IOB estimates with glucagon delivery is paramount. The algorithm must project future glucose levels by factoring in the active insulin (IOB) and preemptively administer microdoses of glucagon to counter impending hypoglycemia that IOB alone cannot prevent [18]. This is particularly crucial during exercise and the post-exercise period, where the risk of hypoglycemia is high due to increased insulin sensitivity [18].
Formulation and Stability of Glucagon
A significant challenge in dual-hormone system development is the stability of liquid glucagon formulations for long-term use in a pump. Research efforts are focused on developing stable, soluble glucagon analogs that are suitable for continuous subcutaneous infusion [18]. The typical dosing used in research systems is microdoses of 10 to 100 micrograms delivered subcutaneously, amounting to less than 1 mg per day, which is far less than the 1 mg rescue dose [18].
Experimental Protocols
Protocol: In-Clinic Evaluation of IOB Models with Concurrent Glucagon
Objective: To validate the accuracy of exponential IOB models for ultra-rapid insulin under conditions designed to induce hypoglycemia, and to assess the efficacy of microdose glucagon as a counter-measure.
Materials:
- Automated insulin delivery system with configurable IOB model (bilinear and exponential)
- Insulin pump(s) and continuous glucose monitor (CGM)
- Stable liquid glucagon formulation in a separate pump
- Euglycemic-hyperinsulinemic clamp setup
Methodology:
- Participant Preparation: Recruit adults with T1D. Initialize the AID system using the participant's standard parameters.
- IOB Model Testing: After an overnight fast, administer a standardized meal bolus using ultra-rapid-acting insulin (e.g., Fiasp).
- Glucagon Trigger & Measurement: Allow glucose to decline. At a predetermined CGM threshold (e.g., 80 mg/dL and falling), administer a 100 μg microdose of glucagon.
- Data Collection: Monitor and record plasma glucose, serum insulin, and plasma glucagon levels at frequent intervals. Use the clamp technique to maintain a stable glucose level if required to isolate the pharmacodynamic effects.
- Analysis: Compare the observed glucose nadir and time to recovery against the IOB model's prediction. Assess the dose-response relationship of the glucagon microdose.
Protocol: Free-Living Outpatient Study on Exercise-Induced Hypoglycemia
Objective: To compare the efficacy of a single-hormone AID system versus a dual-hormone AID system in preventing exercise-induced hypoglycemia over a multi-day period.
Materials:
- Two sets of AID devices: Single-hormone (SH) and Dual-hormone (DH)
- Activity tracker
Methodology:
- Study Design: A randomized, crossover study with two 1-week periods (SH and DH), separated by a washout period.
- Procedure: Participants use each system in a free-living setting. They are instructed to perform 45 minutes of moderate-intensity aerobic exercise on predetermined days.
- Data Collection: Primary outcome: CGM-measured time spent in hypoglycemia (<70 mg/dL) during and for 12 hours after exercise. Secondary outcomes: total time-in-range (70-180 mg/dL), total daily insulin and glucagon use, and participant-reported outcomes.
- Analysis: Use paired t-tests or non-parametric equivalents to compare outcomes between the SH and DH phases.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Dual-Hormone AID Research
| Item | Function/Application in Research |
|---|---|
| Programmable AID Platform (e.g., OpenAPS) | Allows for customization of IOB models (bilinear, exponential) and integration of a second hormone pump; essential for algorithm prototyping [48]. |
| Ultra-Rapid-Acting Insulin (e.g., Fiasp) | Used to test the hypothesis that faster insulin kinetics can improve postprandial control and reduce late hypoglycemia, thereby lessening the burden on the glucagon system [45] [48]. |
| Stable Liquid Glucagon Formulation | The core therapeutic agent for the dual-hormone system; used to prevent or treat algorithm-predicted hypoglycemia via subcutaneous microdoses [18]. |
| Euglycemic-Hyperinsulinemic Clamp Setup | The gold-standard method for quantifying insulin pharmacodynamics and the glucose-raising effect ( pharmacodynamic response) of glucagon microdoses in a controlled setting. |
| Continuous Ketone Monitor (CKM) | An emerging technology used in safety monitoring to assess the risk of diabetic ketoacidosis (DKA), particularly during studies involving insulin suspension or significant basal rate reductions [50]. |
System Diagrams and Workflows
Physiological Pathway of Glucose Counter-Regulation
The following diagram illustrates the physiological mechanism by which glucagon acts to mobilize hepatic glycogen stores in response to hypoglycemia.
Dual-Hormone AID Algorithm Decision Workflow
This flowchart outlines the high-level logical process a dual-hormone AID system uses, integrating IOB and glucagon delivery decisions.
Addressing the intertwined physiological limitations of IOB and hepatic glycogen dysregulation is central to the next generation of AID systems. The methodologies and considerations outlined here provide a framework for advancing dual-hormone system research. Refining IOB models for faster insulins, developing stable glucagon formulations, and creating intelligent algorithms that leverage both hormones will be critical steps toward achieving fully automated, physiological glucose control that mitigates the risk of hypoglycemia.
The development of dual-hormone closed-loop systems represents a paradigm shift in type 1 diabetes (T1D) management, offering the potential to mitigate the persistent challenge of hypoglycemia. These systems augment automated insulin delivery with glucagon as a counter-regulatory agent, creating a bihormonal approach to glucose homeostasis. A critical challenge in this domain lies in optimizing control algorithms to prevent hypoglycemia while minimizing exogenous glucagon administration. This application note details protocols and analytical frameworks for optimizing this balance, providing researchers with methodologies to advance dual-hormone system development.
Quantitative Efficacy and Safety Profile of Low-Dose Glucagon
Meta-analyses of randomized controlled trials provide compelling evidence for the efficacy of low-dose glucagon in hypoglycemia prevention. The following table summarizes key glycemic outcomes from recent systematic reviews and clinical studies.
Table 1: Glycemic Outcomes with Low-Dose Glucagon Interventions
| Outcome Measure | Intervention | Effect Size (vs. Comparator) | Source/Study |
|---|---|---|---|
| Hypoglycemia Risk (T1D during exercise) | Low-Dose Glucagon | RR 0.54 (95% CI: 0.35, 0.84) [15] | Systematic Review/Meta-Analysis |
| Time Below Range (TBR) <3.9 mmol/L | Low-Dose Glucagon | -3.91 percentage points (95% CI: -6.27, -1.54) [15] | Systematic Review/Meta-Analysis |
| Post-Intervention Plasma Glucose (Exercise prevention) | 150 µg MDG | Increase (vs. decrease with control/insulin reduction) [51] | Crossover Trial (n=15) |
| 40g Carbohydrate | Greater Increase (vs. MDG) [51] | Crossover Trial (n=15) | |
| Hypoglycemia Incidence (Exercise prevention) | 150 µg MDG | 0/15 subjects (Plasma Glucose <70 mg/dL) [51] | Crossover Trial (n=15) |
| No Intervention | 6/15 subjects (Plasma Glucose <70 mg/dL) [51] | Crossover Trial (n=15) | |
| Time in Hypoglycemia (Dual-Hormone CL vs. Single-Hormone CL) | Dual-Hormone Closed-Loop | 1.3% (1.0) (CGM <70 mg/dL) [52] | Outpatient Study (n=20) |
| Single-Hormone Closed-Loop | 2.8% (1.7) (CGM <70 mg/dL) [52] | Outpatient Study (n=20) |
While effective, the safety profile must be considered in algorithm design. The same meta-analysis found that low-dose glucagon administration was associated with an increased risk of any adverse event (Risk Ratio 2.75; 95% CI 1.07, 7.08) [15]. Furthermore, stability and aggregation of native glucagon in solution present significant formulation hurdles for pump-based delivery systems [53]. These factors underscore the necessity of a minimal-effective-dose strategy.
Experimental Protocols for Algorithm Validation
Robust experimental validation is essential for optimizing dual-hormone algorithms. The following protocols provide standardized methodologies for evaluating algorithm performance.
Protocol 1: Exercise-Induced Hypoglycemia Prevention
This protocol is designed to test algorithm responsiveness to a common physiological stressor.
- Objective: To evaluate the efficacy of algorithm-triggered glucagon in preventing hypoglycemia during and after moderate-intensity aerobic exercise.
- Population: Adults with T1D (≥18 years) on insulin pump therapy.
- Pre-Study Conditions:
- Experimental Session:
- Participants arrive fasting (≥8 hours).
- Establish intravenous line for frequent plasma glucose sampling (reference method).
- Baseline Phase: Stabilize plasma glucose to 100-140 mg/dL. No insulin corrections within 3 hours of exercise start [51].
- Intervention: At t = -5 minutes, administer the algorithm-determined intervention (e.g., microdose glucagon, placebo, or comparator).
- Exercise Phase: 45 minutes of treadmill exercise at a steady heart rate corresponding to 50-60% VO2max [51] [52].
- Recovery Phase: Monitor for 2-4 hours post-exercise. Provide a standardized meal at t = 75 min with insulin bolus calculated per participant's insulin-to-carbohydrate ratio [51].
- Primary Endpoints: CGM/Plasma Glucose nadir, time below range (<70 mg/dL), area under the curve for glucose, total glucagon dose administered.
The logical workflow for this protocol, from participant preparation to data analysis, is outlined in the diagram below.
Protocol 2: Outpatient Closed-Loop System Comparison
This protocol tests algorithm performance in a real-world, multi-day setting.
- Objective: To compare the safety and efficacy of a dual-hormone algorithm against single-hormone and other standard of care systems over several days.
- Design: Randomized, crossover, outpatient study.
- Intervention Arms:
- Study Duration: Each arm lasts 3-4 days, with a 2-week run-in period for pump setting optimization [52].
- Procedures:
- Primary Endpoints: Percentage of time with CGM values in hypoglycemia (<70 mg/dL), time in range (70-180 mg/dL), total daily glucagon dose, number of carbohydrate rescues.
The Scientist's Toolkit: Research Reagent Solutions
Successful experimentation requires specific, high-quality reagents and tools. The following table catalogues essential components for dual-hormone system research.
Table 2: Essential Research Reagents and Materials for Dual-Hormone System Investigation
| Item | Function/Application | Examples & Key Characteristics |
|---|---|---|
| Stable Glucagon Analogs | Resists fibrillation in pump reservoirs for reliable delivery in prolonged studies. | Dasiglucagon (Zealand Pharma); Liquid-stable glucagon (Xeris Pharmaceuticals) [15] [53] |
| Ready-to-Use Glucagon Formulations | Enables precise, low-dose subcutaneous administration without reconstitution. | Gvoke Prefilled Syringe (Xeris); BAQSIMI Nasal Powder (Eli Lilly) - useful for pre-exercise MDG protocols [15] [53] |
| Continuous Glucose Monitor (CGM) | Provides real-time, high-frequency glucose data for algorithm input and outcome assessment. | Dexcom G-series; Used for calibration and as primary glucose input in closed-loop studies [54] [52] |
| Programmable Insulin Pumps | Allows for precise, automated delivery of insulin and experimental glucagon formulations. | t:slim X2 Insulin Pump (Tandem); Often used as the delivery platform for closed-loop research systems [54] [52] |
| Activity & Heart Rate Monitors | Provides data for exercise-detection algorithms to proactively adjust hormone delivery. | ZephyrLife BioPatch; Provides heart rate and accelerometer data to estimate METs and trigger exercise mode [52] |
Algorithmic Decision Framework for Glucagon Dosing
The core challenge of minimizing glucagon dosage hinges on a sophisticated decision framework that integrates multiple real-time data streams. The following diagram illustrates the logical flow an optimized algorithm should follow, from data input to the final dosing decision.
Key decision factors include:
- CGM Trend Analysis: The algorithm must prioritize glucagon delivery based not only on absolute glucose levels but also on the rate of change (mg/dL/min). A rapid descent towards a threshold warrants a more proactive dose than a stable glucose level just above it [15].
- Physiological Context: An integrated exercise detection module using heart rate and accelerometer data is critical. Upon confirming exercise, the algorithm can preemptively increase the glucose target for glucagon delivery (e.g., from 95 mg/dL to 120 mg/dL) and adjust maximum allowed doses to prevent exercise-induced hypoglycemia [52].
- System State Awareness: The algorithm must account for active insulin (IOB) and the history of recent glucagon administrations to avoid stacking interventions and minimize total hormone load.
Optimizing algorithms for dual-hormone systems requires a meticulous, multi-faceted approach that balances powerful hypoglycemia prevention against the imperative to minimize glucagon exposure. The quantitative data, experimental protocols, and conceptual frameworks provided herein offer a pathway for researchers to refine these complex systems. Future work should focus on adaptive algorithms that learn individual patient responses, the integration of more stable glucagon formulations, and long-term outpatient studies to confirm real-world durability and safety.
The development of Automated Insulin Delivery (AID) systems, or artificial pancreas systems, represents a transformative advancement in the management of Type 1 Diabetes (T1D). Current commercial systems operate as hybrid closed-loop systems, requiring users to manually announce meals and exercise to avoid dangerous hyperglycemia or hypoglycemia respectively [19]. This manual intervention increases diabetes management burden and fails to achieve full automation. Within the context of dual-hormone (insulin and glucagon) delivery system development, this application note details advanced strategies to achieve fully closed-loop control that automatically responds to meals and physical activity without user input. By leveraging sophisticated control algorithms, artificial intelligence, and multi-signal integration, next-generation systems promise to reduce user burden while improving glycemic outcomes, ultimately supporting a broader range of people living with T1D including older adults, pregnant people, and athletes [19].
Technical Approaches and Quantitative Comparisons
Core Algorithmic Strategies for Meal Management
Multiple Model Probabilistic Predictive Control (MMPPC) represents a significant advancement in insulin-only, full closed-loop systems. Unlike standard Model Predictive Control (MPC) that predicts mean future glucose values, MMPPC additionally predicts the uncertainty of future glucose measurements. This enables direct control of hypoglycemic risk rather than indirectly penalizing insulin delivery. A key innovation is its use of population-level data from national health surveys to anticipate future meals and detect unannounced meals based on temporal patterns. For example, if a patient eats at 10 AM, the algorithm calculates the probability distribution for the next meal time, continuously adapting these probabilities as time passes without eating [56]. The system operates in two primary modes: a daytime mode featuring meal anticipation and potential for large automated boluses (superboluses), and a more cautious nighttime mode that explicitly infuses only 1/12th of the desired bolus at each sample time [56].
Event-Triggered Dual-Hormone Control represents an alternative approach that combines insulin and glucagon delivery. Recent research has demonstrated Smart Dual Hormone Artificial Pancreas (SDHAP) systems with event-triggered feedback-feedforward control schemes. These systems utilize machine learning algorithms (Support Vector Machine and K-Nearest Neighbors) to classify glycemic events from continuous glucose monitoring data, then deploy event-triggered Proportional-Integral (PI) and Model Predictive Control (MPC) controllers based on the Bergman Minimal Model to deliver appropriate insulin and glucagon doses [7]. The event-triggered mechanism is particularly valuable for dual-hormone systems as it helps prevent simultaneous infusion of insulin and glucagon while reducing computational burden [7].
Robust H∞ Glucagon Control has emerged as a novel approach for glucagon administration in dual-hormone systems. This method replaces traditional personalized controllers with a non-individualized H∞ optimal controller that considers modeling errors and system changes in its design. When combined with a switched Linear Quadratic Gaussian (LQG) insulin controller, this strategy has demonstrated satisfactory glucose regulation with reduced glucagon dosage in simulation studies, requiring less individualization than previous approaches [16].
Advanced Exercise Management Strategies
Physical activity presents particular challenges for closed-loop systems due to complex physiological effects including increased insulin sensitivity, heightened insulin absorption from subcutaneous depots, and abnormal glucagon responses in T1D [19]. Dual-hormone systems with model predictive controllers can automatically reduce insulin and infuse glucagon to mitigate exercise-induced hypoglycemia [19]. Proof-of-concept systems can now automatically distinguish between various forms of exercise using commercial wearable devices (smartwatches, activity bands, or rings) that provide heart rate photoplethysmography and accelerometry data [19]. These systems estimate energy expenditure as metabolic equivalents to address the nonlinear relationship between exercise intensity and insulin requirements [19].
Table 1: Performance Comparison of Closed-Loop Strategies
| Control Strategy | Study Type | Mean 24-h Glucose (mg/dL) | Nighttime Glucose (mg/dL) | Hypoglycemia Events (per patient-day) | Time in Range (70-180 mg/dL) |
|---|---|---|---|---|---|
| MMPPC (Inpatient) [56] | 30-h Inpatient | 142 | 125 | 1.6 | Not Reported |
| MMPPC (Hotel) [56] | 54-h Hotel | 152 | 139 | 0.91 | Not Reported |
| Dual-Hormone AP (Van Bon et al.) [56] | Home Environment | Not Reported | Significantly Improved | 0.4 treatments/day | 84.7% |
| Insulin-Only AP (Van Bon et al.) [56] | Home Environment | Not Reported | Improved | Not Reported | 68.5% |
Table 2: Algorithm Characteristics and Technical Requirements
| Algorithm Type | Hormones | Meal Announcement | Exercise Management | Key Innovations |
|---|---|---|---|---|
| MMPC [56] | Insulin-only | Not required | Manual announcement | Probabilistic meal anticipation, population behavior patterns |
| Event-Triggered SDHAP [7] | Insulin & Glucagon | Not required | Automated detection | ML classification, event-triggered control, feedforward disturbance rejection |
| Robust H∞ Control [16] | Insulin & Glucagon | Not required | Not specified | Non-individualized robust control, reduced glucagon usage |
| Commercial Hybrid CL [19] | Insulin-only | Required | Manual mode activation | Current standard of care, temporary target adjustments |
Experimental Protocols
Protocol for Evaluating Unannounced Meal Performance
Objective: To assess the efficacy of fully closed-loop systems in managing postprandial glucose excursions without meal announcement.
Materials: Artificial pancreas platform (e.g., UVA DiAs, Roche Spirit Combo Insulin Pump, Dexcom G4 CGM), Zephyr BioHarness 3.0 accelerometer, reference glucose analyzer (YSI or StatStrip), standardized meals with varying macronutrient composition [56].
Procedure:
- Participant Preparation: Recruit adults with T1D (duration >1 year, pump use >3 months). Train participants on CGM use. Initiate closed-loop control by 10 AM after an overnight fast [56].
- Meal Challenges: Present unannounced meals with varying carbohydrate content (20-80g), fat, and protein composition. Meals should be representative of typical food choices.
- Data Collection: Obtain reference blood samples every hour during stable periods and every 15 minutes during hypoglycemic alarms (glucose <70 mg/dL) until resolution [56].
- Remote Monitoring: Utilize web-based monitoring systems (e.g., DiAs web-monitoring system) for real-time supervision [56].
- Outcome Measures: Primary - Postprandial glucose excursion (peak, time-to-peak, area under the curve). Secondary - Time in target range (70-180 mg/dL), hypoglycemia events (<70 mg/dL), hyperglycemia events (>250 mg/dL) [56].
Analysis: Compare glucose trajectories following announced vs. unannounced meals. Evaluate algorithm performance in meal detection timing and insulin dosing accuracy.
Protocol for Automated Exercise Response Evaluation
Objective: To validate automated detection and mitigation of exercise-induced glycemic variations.
Materials: AID system with integrated activity monitors (smartwatch or activity band), dual-hormone pump capable of delivering insulin and glucagon, graded exercise equipment (treadmill, stationary bike) [19].
Procedure:
- Baseline Assessment: Characterize individual exercise responses through graded exercise tests with continuous glucose monitoring under open-loop conditions.
- Exercise Protocol: Implement various exercise modalities (aerobic, resistance, high-intensity interval training) of differing intensities (40-80% VO₂max) and durations (30-60 minutes).
- Algorithm Activation: Enable exercise detection algorithms using input from wearable devices (heart rate, accelerometry, metabolic equivalents).
- Control Strategies: Compare dual-hormone approaches (insulin reduction plus glucagon infusion) vs. insulin-only strategies (temporary target adjustments, predictive suspension) [19].
- Safety Monitoring: Continuous supervision with capillary glucose verification if CGM values <70 mg/dL or >300 mg/dL.
Outcome Measures: Time in hypoglycemia during and post-exercise, glucagon dose requirements, recovery time to euglycemia, counterregulatory hormone profiles.
Analysis: Assess sensitivity and specificity of exercise detection algorithms. Compare glycemic outcomes between automated intervention and manual exercise announcement.
Free-Living Environment Evaluation Protocol
Objective: To assess system performance in real-world conditions with minimal supervision.
Materials: Mobile AID system, wearable activity trackers, food logging application (optional), remote monitoring platform [56].
Procedure:
- Hotel Study Setup: Conduct 54-hour supervised hotel studies where participants make their own food choices, including alcohol for adults, and travel within 20-minute walking distance [56].
- Minimal Intervention: Research staff assist only with technical issues, intervening medically only if sensor glucose values remain <70 mg/dL for 15 minutes without subject response or >300 mg/dL for 30 minutes [56].
- Sleep/Wake Detection: Implement either automated detection (accelerometer-based torso angle >60° from vertical) or manual announcement [56].
- Data Collection: Collect 72 hours of baseline open-loop CGM data prior to hotel admission for comparison [56].
Outcome Measures: 24-hour and nighttime mean glucose, hypoglycemia incidence, time-in-range, user satisfaction scores.
Analysis: Compare free-living performance with inpatient results and baseline open-loop control.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Technologies
| Item | Function | Example Products/Specifications |
|---|---|---|
| Continuous Glucose Monitor | Real-time interstitial glucose measurement | Dexcom G4, Freestyle Libre (measurements every 5 minutes) [56] [7] |
| Insulin Pump | Subcutaneous insulin infusion | Roche Spirit Combo Insulin Pump [56] |
| Dual-Chamber Pump | Simultaneous insulin and glucagon delivery | Specialized research pumps for dual-hormone studies [16] |
| Activity Monitors | Physical activity and sleep detection | Zephyr BioHarness 3.0 accelerometer, consumer smartwatches [56] [19] |
| Control Platform | Algorithm implementation and system integration | UVA DiAs (Diabetes Assistant) platform [56] |
| Reference Glucose Analyzer | Blood glucose validation | YSI StatStrip for hourly calibration and hypoglycemia confirmation [56] |
| Simulation Environment | In silico testing and algorithm development | UVA/Padova T1D Simulator, custom MATLAB environments [7] [16] |
The development of fully closed-loop control systems that eliminate meal and exercise announcements represents the next frontier in diabetes management technology. The integration of dual-hormone delivery with advanced control strategies like MMPPC, event-triggered algorithms, and robust H∞ control shows significant promise in achieving this goal. These systems leverage probabilistic modeling, machine learning classification, and multi-signal integration from wearable devices to automatically adapt to life's daily challenges. As research progresses, these technologies will expand to support diverse populations with T1D, including older adults, pregnant people, and athletes, ultimately reducing disease burden while improving glycemic outcomes and quality of life.
Benchmarking Performance: In Silico, Clinical, and Real-World Evidence
The development of dual-hormone artificial pancreas (DHAP) systems represents a paradigm shift in the management of Type 1 Diabetes (T1D). These systems automate the delivery of both insulin and glucagon to maintain euglycemia. The complexity of human physiology and the paramount importance of patient safety make in silico validation an indispensable precursor to clinical trials. This document details the application notes and experimental protocols for using sophisticated simulation environments to develop and validate novel control algorithms for DHAP systems, providing a critical framework for researchers and drug development professionals engaged in this field.
The core challenge in DHAP development lies in creating control algorithms that can effectively manage the non-linear dynamics of glucose-insulin-glucagon interactions while rejecting disturbances such as meal intake and exercise. In silico studies, utilizing statistical virtual patient populations (VPPs), provide a robust, ethical, and cost-effective platform for the initial testing, optimization, and validation of these controllers under a wide range of controlled conditions.
The Virtual Patient Population: A Cornerstone for Validation
A critical component of credible in silico testing is a VPP that accurately reflects the inter-subject variability observed in the real-world T1D population. These mathematical models simulate the glucoregulatory system and allow for the statistical sampling of key physiological parameters.
Model Architectures for Single and Dual-Hormone Systems
Two primary model architectures are employed, which can be extended from single-hormone to dual-hormone systems.
- Single-Hormone Virtual Patient Population (SH-VPP): This model is typically comprised of a system of differential equations describing insulin kinetics, insulin dynamics, and carbohydrate absorption. The most sensitive inter-subject parameter, often the insulin sensitivity factor, is statistically sampled from a normal distribution to create a virtual cohort with varying insulin responses [57].
- Dual-Hormone Virtual Patient Population (DH-VPP): This model extends the SH-VPP by incorporating additional compartments for glucagon kinetics and glucagon dynamics. The DH-VPP may involve thirteen or more differential equations. Parameters for both insulin sensitivity and glucagon sensitivity are statistically sampled to generate a population with diverse responses to both hormones [57].
Table 1: Key Parameters for a Statistically-Sampled Virtual Patient Population
| Parameter | Description | Role in Model | Sampling Method |
|---|---|---|---|
| Insulin Sensitivity | Modulates the effect of insulin on glucose utilization | Core parameter in insulin dynamics | Normal distribution |
| Glucagon Sensitivity | Modulates the effect of glucagon on glucose production | Core parameter in glucagon dynamics | Normal distribution |
| Total Daily Insulin Requirement | Patient-specific insulin needs | Used for matching virtual and real patients | Clinical data matching |
| Body Weight | Patient's body mass | Used for scaling and matching | Clinical data matching |
Validation of the Virtual Population
Before a VPP can be trusted for controller validation, it must be validated against clinical data. The protocol involves:
- Matching: Virtual patients are matched to actual clinical patients from an outpatient study based on Total Daily Insulin Requirement (TDIR) and body weight [57].
- Scenario Replication: The identical meals, exercise sessions, and control algorithms used in the clinical study are applied to the virtual patients.
- Outcome Comparison: Key clinical outcomes, including Time in Range (TIR: 70-180 mg/dL), time in hypoglycemia (<70 mg/dL), and time in hyperglycemia (>180 mg/dL), are compared between the virtual and actual patient cohorts. A well-validated model will show no statistically significant difference in these metrics [57].
Controller Architectures for Dual-Hormone Delivery
Several advanced control strategies have been developed and validated in silico for DHAP systems. The choice of architecture depends on the desired balance between performance, computational complexity, and clinical practicality.
Time-Varying Proportional-Integral-Derivative (PID) Control
This classical control strategy can be adapted for the specific kinetics of intraperitoneal (IP) insulin delivery, which offers faster action compared to subcutaneous delivery.
- Application Note: A time-varying PID controller was designed in silico to guide IP insulin delivery in a fully closed-loop mode without meal announcement. The controller gains are adapted over time to account for the rapid pharmacokinetics of IP insulin, which closely mimics physiological intraportal insulin secretion [58].
- Protocol:
- Model Integration: Implement the controller within a simulator that has been updated for IP insulin delivery and sensing, such as a modified FDA-accepted T1D simulator [58].
- Gain Scheduling: Design the algorithm to vary the proportional, integral, and derivative gains based on the time of day or the current glucose rate-of-change.
- In Silico Testing: Run extended simulations (e.g., several days) with unannounced meals to assess the controller's ability to maintain glucose in the target range without inducing hypoglycemia.
Model Predictive Control (MPC)
MPC uses an internal model of the patient's physiology to predict future glucose levels and optimizes insulin and glucagon delivery accordingly.
- Application Note: MPC is a dominant strategy in AP research. It uses a model (e.g., the Bergman Minimal Model) to forecast glucose trajectories over a prediction horizon and computes optimal hormone delivery rates by solving a constrained optimization problem [7] [40].
- Protocol:
- Model Identification: Define the internal prediction model, which can be a linearized version of a more complex physiological model.
- Constraint Setting: Set safety constraints on insulin and glucagon infusion (e.g., maximum bolus, minimum glucagon dose) and on predicted glucose levels.
- Cost Function Formulation: Design a cost function that penalizes deviations from the target glucose, excessive control action, and constraint violations.
- Horizon Simulation: Execute the controller in the VPP across various meal and exercise scenarios to tune the weights in the cost function and the length of the prediction and control horizons.
Event-Triggered Smart Control with Machine Learning
This advanced architecture combines conventional control with machine learning (ML) to create a more efficient and responsive system.
- Application Note: A Smart DHAP (SDHAP) can use ML algorithms to classify glycemic events and predict future glucose levels. An event-triggered mechanism then activates the feedback controller only when needed, reducing computational load and preventing unnecessary hormone delivery [7].
- Protocol:
- Data Preprocessing: Preprocess and clean CGM data (e.g., from the T1DiabetesGranada dataset), extract relevant time-series features (TIR, TBR, TAR), and handle missing values [7].
- Event Classification: Train ML classifiers like Support Vector Machine (SVM) and k-Nearest Neighbors (KNN) to identify hypoglycemic and hyperglycemic events from the extracted features.
- Glucose Prediction: Train time-series models (e.g., ARIMA or Gated Recurrent Units (GRU)) for multi-step-ahead blood glucose prediction.
- Controller Activation: Design an event-trigger that activates the PI or MPC feedback controller based on the ML-predicted glucose values or classified events. A separate feedforward controller is designed to reject meal and exercise disturbances [7].
Deep Reinforcement Learning (RL)
RL represents a paradigm where the controller learns the optimal hormone delivery policy through trial and error in the simulation environment.
- Application Note: Deep RL can be used to develop a fully data-driven delivery strategy without prior knowledge of the glucose-insulin metabolism. Double dilated recurrent neural networks can be trained to map raw data of glucose and meal carbohydrates to insulin and glucagon delivery commands [59].
- Protocol:
- Self-Play Training: Train the deep RL agent over hundreds of simulated days on the VPP (e.g., the UVA/Padova simulator) to learn a generalized policy.
- Personalization: Use importance sampling or transfer learning to customize the generalized model for individual virtual patients.
- Performance Benchmarking: Compare the glucose Time in Range (TIR) achieved by the RL controller against traditional control strategies like MPC under identical in-silico conditions [59].
Table 2: Performance Comparison of Controllers in Silico
| Controller Type | Reported Time in Range (TIR) | Key Advantages | Validated VPP |
|---|---|---|---|
| Time-Varying PID | Not specified | Simplified design; effective for intraperitoneal delivery | Modified FDA T1D Simulator [58] |
| Model Predictive Control | SH: ~78.1%, DH: ~75.6% [57] | Handles constraints; uses future predictions | SH-VPP / DH-VPP [57] |
| Event-Triggered Smart AP | Not specified | Computationally efficient; patient-specific | T1DiabetesGranada Dataset [7] |
| Deep Reinforcement Learning | Adult: ~93%, Adolescent: ~83% [59] | Model-free; can discover novel strategies | UVA/Padova Simulator [59] |
Comprehensive In Silico Validation Protocol
A rigorous, multi-stage testing protocol is essential to build confidence in a novel controller's performance and safety before clinical deployment.
Design of Simulation Experiments (DOSE)
Following principles of DOSE ensures that simulation testing is systematic, efficient, and informative [60].
- Step 1: Sensitivity Analysis: Identify which model parameters (e.g., insulin sensitivity, carbohydrate absorption rate) have the greatest impact on controller performance. This helps in understanding the robustness of the controller.
- Step 2: Scenario Testing: Expose the controller to a wide range of challenging conditions, including:
- Unannounced and varying meal sizes
- Aerobic exercise sessions at different intensities and durations
- Sensor noise and dropouts
- Pump failures or occlusions
- Step 3: Extreme Condition Testing: Test the controller's behavior under physiologically implausible conditions to uncover potential structural flaws or instability in the control law [60].
- Step 4: Monte Carlo Analysis: Run a large number (e.g., 1000+) of simulations with different virtual patients and randomly generated meal and exercise schedules to obtain statistical distributions of performance metrics like TIR.
Key Performance Metrics for In Silico Evaluation
The following metrics must be calculated and reported for any in silico validation study.
Table 3: Essential In Silico Performance and Safety Metrics
| Metric Category | Specific Metric | Target Value |
|---|---|---|
| Glycemic Control | % Time in Range (TIR: 70-180 mg/dL) | Maximize (>70-80%) |
| % Time in Hyperglycemia (>180 mg/dL) | Minimize | |
| % Time in Hypoglycemia (<70 mg/dL) | Minimize (<4%) | |
| Mean Glucose | ~150 mg/dL | |
| Glucose Variability | Coefficient of Variation (%CV) | <36% |
| Low Blood Glucose Index (LBGI) | Minimize | |
| High Blood Glucose Index (HBGI) | Minimize | |
| Safety & Efficiency | Total Insulin Delivered | Compare to baseline |
| Total Glucagon Delivered | Report for DH systems | |
| Number of Hypoglycemic Events | Minimize |
The Scientist's Toolkit: Research Reagents & Essential Materials
This section details the key computational tools and models required to establish an in silico development pipeline for DHAP controllers.
Table 4: Essential Research Tools for In Silico DHAP Development
| Tool / Resource | Type | Function in Research | Example / Source |
|---|---|---|---|
| Virtual Patient Population | Mathematical Model | Simulates the glucoregulatory system of T1D patients for controller testing | SH-VPP / DH-VPP [57], UVA/Padova Simulator |
| Bergman Minimal Model | Mathematical Model | A simplified, widely-used model of glucose kinetics serving as a basis for controller design | [7] |
| Control Algorithm | Software Code | The core logic determining insulin and glucagon infusion rates (e.g., PID, MPC, RL) | Custom-developed in MATLAB/Python |
| Continuous Glucose Monitor Data | Dataset | Real-world glucose data for model validation and machine learning training | T1DiabetesGranada Dataset [7] |
| Simulation Environment | Software Platform | Integrates the VPP and controller to run in-silico experiments | MATLAB/Simulink, Python |
| Design of Experiments Framework | Methodological Framework | A structured approach for planning and analyzing simulation experiments to ensure robustness and validity | Principles from [60] |
In silico studies provide an indispensable, powerful, and safe development bed for next-generation DHAP systems. By leveraging statistically validated virtual patient populations and employing a structured Design of Experiments framework, researchers can rigorously evaluate novel control algorithms—from time-varying PID to deep reinforcement learning—under a vast array of conditions. The protocols and application notes outlined herein offer a roadmap for the comprehensive validation of dual-hormone delivery controllers, ensuring that only the most robust and effective systems advance to costly and time-consuming clinical trials, thereby accelerating the path to improved automated care for people with T1D.
Application Note: Performance Metrics for Dual-Hormone Automated Delivery Systems
Automated insulin delivery (AID) systems, often called closed-loop systems, represent a transformative advance in managing diabetes by combining a continuous glucose monitor (CGM), an insulin pump, and a control algorithm to automatically regulate insulin delivery. Dual-hormone AID systems represent a significant evolution, augmenting traditional insulin-only systems by incorporating glucagon to mitigate hypoglycemia, a common and dangerous limitation of single-hormone systems [19]. This application note details the key performance metrics—Time-in-Range (TIR), hypoglycemia reduction, and HbA1c—used to evaluate these sophisticated systems, providing researchers and developers with structured data and methodologies essential for advancing the field.
Quantitative Performance Data
The efficacy of AID systems is quantitatively assessed through standardized glucose metrics. The table below summarizes performance data for single-hormone (insulin-only) and dual-hormone (insulin and glucagon) AID systems from recent clinical evidence.
Table 1: Key Performance Metrics for Automated Insulin Delivery Systems
| System Type | Time-in-Range (TIR) 70-180 mg/dL | Time Below Range (TBR) <70 mg/dL | HbA1c Reduction | Key Supporting Evidence |
|---|---|---|---|---|
| AID Systems (Overall) | ↑ 11.74% improvement vs. control [61] | ↓ 1.80% in patients with diabetes duration >20 years [61] | ~ 0.3-0.5% reduction in real-world settings [62] | Meta-analysis of 65 RCTs (n=3,623) [61] |
| Dual-Hormone AID | ↑ 19.64% improvement vs. control [61] | Superior reduction in hypoglycemia, especially during exercise [19] | Data specifically for dual-hormone systems is evolving. | Comparison within meta-analysis [61] |
| Advanced HCL (MiniMed 780G) | > 70% TIR achieved in T2D populations [63] | < 1% TBR in T2D populations [63] | Not reported in cited study [63] | Real-world study in T2D (n=26,427) [63] |
Abbreviations: AID: Automated Insulin Delivery; HCL: Hybrid Closed-Loop; TIR: Time-in-Range; TBR: Time Below Range; HbA1c: Glycated Hemoglobin; RCT: Randomized Controlled Trial; T2D: Type 2 Diabetes.
Analysis of Performance Advantages
- Time-in-Range (TIR): AID systems consistently demonstrate a significant increase in TIR. Dual-hormone systems show a particular advantage, with one meta-analysis reporting a near 20% improvement over control treatments, outperforming single-hormone systems [61]. This suggests that adding glucagon can more effectively counteract post-meal or activity-related glucose excursions.
- Hypoglycemia Reduction: The reduction of hypoglycemia is a primary strength of AID technology. This benefit is most pronounced in vulnerable populations, such as those with long-standing diabetes [61]. Dual-hormone systems are specifically designed to address this challenge by using glucagon as a countermeasure, which is particularly effective during periods of high hypoglycemia risk, such as after physical activity [19].
- HbA1c Improvement: Real-world use of AID systems leads to clinically meaningful, albeit modest, reductions in HbA1c [62]. This is achieved alongside a significant reduction in hypoglycemia, a critical trade-off that is often difficult to manage with conventional therapy.
Experimental Protocols for Evaluating Dual-Hormone Systems
Protocol 1: Assessing Meal and Exercise Response
This protocol evaluates the system's ability to maintain glycemic control following common daily challenges.
1. Objective: To quantify the efficacy of a dual-hormone AID system in preventing postprandial hyperglycemia and exercise-induced hypoglycemia compared to a single-hormone system and standard insulin therapy.
2. Methodology:
- Study Design: A randomized, controlled, crossover trial.
- Participants: Adults with type 1 diabetes.
- Interventions: Each participant undergoes three treatment phases in random order:
- Dual-hormone AID (insulin and glucagon).
- Single-hormone AID (insulin only).
- Sensor-augmented pump (SAP) therapy (control).
- Meal Challenge: After an overnight fast, participants consume a standardized, high-carbohydrate meal. Carbohydrate counting is not required; the meal size is pre-set to evaluate automated responses [19].
- Exercise Challenge: On a separate day, participants perform moderate-intensity aerobic exercise for 45 minutes. The AID systems are set to automatic mode with no pre-exercise user announcements [19].
- Data Collection: CGM data (TIR, TBR, Time Above Range) is collected for 6 hours post-meal and 24 hours post-exercise. Blood is drawn for lab glucose and counter-regulatory hormone analysis at predefined intervals.
3. Key Metrics: Primary outcome is the difference in TIR (70-180 mg/dL) during the 4-hour postprandial period. Secondary outcomes include TBR (<70 mg/dL) during and after exercise, and mean glucose levels.
Protocol 2: Long-Term Glycemic Control and Safety
This protocol assesses the sustained performance and safety of dual-hormone systems in a free-living, outpatient setting.
1. Objective: To determine the long-term effect of a dual-hormone AID system on overall glycemic control (HbA1c, TIR) and its safety profile, including the incidence of diabetic ketoacidosis (DKA) and severe hypoglycemia.
2. Methodology:
- Study Design: A multi-center, randomized, parallel-group trial.
- Participants: A broad population of children and adults with type 1 diabetes, including those with a history of hypoglycemia unawareness.
- Interventions: Participants are randomized to either:
- Dual-hormone AID system.
- Single-hormone AID system (active control).
- Study Duration: 6 to 12 months.
- Procedures: Participants use the assigned system in their home environment. Follow-up visits occur at 3, 6, and 12 months. CGM data is uploaded continuously via cloud-based platforms for remote monitoring [62].
- Data Collection:
- Efficacy: HbA1c is measured at each visit. CGM-derived metrics (TIR, TBR, CV) are analyzed over the entire study period.
- Safety: All adverse events, including DKA, severe hypoglycemia, and infusion set issues, are recorded. For dual-hormone systems, specific attention is paid to local skin reactions at the glucagon infusion site and the stability of the glucagon formulation.
3. Key Metrics: Primary outcome is the change in HbA1c from baseline to 6 months. Secondary outcomes include change in TIR, rate of hypoglycemic events, and patient-reported outcomes (e.g., quality of life, sleep quality).
Visualization of System Workflows and Pathways
Dual-Hormone AID Feedback Loop
Experimental Meal & Exercise Challenge Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Dual-Hormone AID System Research
| Research Tool | Function & Application in AID Development |
|---|---|
| Continuous Glucose Monitor (CGM) | Provides real-time interstitial glucose concentration data to the control algorithm. Essential for feedback loop operation. Examples: Dexcom G6, Abbott Freestyle Libre [64]. |
| Insulin Pumps | Delivers rapid-acting insulin analogs subcutaneously. Must be capable of receiving and executing frequent, small dosing commands from the controller. Examples: Tandem t:slim X2, Ypsomed pump [64]. |
| Glucagon Formulations | Stable, soluble glucagon analogs for subcutaneous infusion. Used in dual-hormone systems to automatically raise blood glucose and prevent/mitigate hypoglycemia [19]. |
| Control Algorithm Software | The "brain" of the system (e.g., Model Predictive Control - MPC). It uses CGM data, user inputs (if any), and insulin pharmacokinetics/pharmacodynamics models to calculate optimal insulin and glucagon doses [19]. |
| Physical Activity Simulators | Wearable devices (e.g., smartwatches) that provide heart rate and accelerometry data to the algorithm for automated detection and response to exercise [19]. |
| Digital Twin Simulation Platform | A virtual patient population used for in-silico testing and refinement of algorithms before costly and risky clinical trials, improving safety and development speed [19]. |
The artificial pancreas (AP), or automated insulin delivery (AID) system, represents a transformative advancement in the management of Type 1 Diabetes (T1D). While single-hormone artificial pancreas (SHAP) systems automating insulin delivery have significantly improved glycemic control, the limitation of having only a unidirectional (glucose-lowering) control action persists. Dual-hormone artificial pancreas (DHAP) systems, which administer both insulin and glucagon, have been proposed to more closely mimic natural pancreatic function by adding a counter-regulatory glucose-raising capability [65]. This application note synthesizes head-to-head clinical evidence comparing the efficacy, safety, and operational protocols of DHAP systems against SHAP and conventional pump therapy, providing a structured resource for researchers and drug development professionals engaged in the advancement of closed-loop technologies.
Comparative Clinical Outcomes: A Data-Driven Analysis
A synthesis of key clinical studies directly comparing DHAP, SHAP, and conventional pump therapy reveals a distinct performance profile for each system. The following tables summarize critical quantitative outcomes from these comparative investigations.
Table 1: Key Glycemic Outcomes from Comparative Clinical Studies
| Study Context & Reference | Comparison | Time in Range (TIR) (%) | Time in Hypoglycemia (<70 mg/dL) (%) | Mean Glucose (mg/dL) | Hypoglycemia Events (per participant) |
|---|---|---|---|---|---|
| Inpatient, 24 hours [65] | DHAP vs. SHAP | - | 1.5 vs. 3.1 (p=0.018) | 144 vs. 139 (p=0.14) | 0.3 vs. 0.43 (per day) |
| Outpatient (camp), overnight [65] | DHAP vs. SHAP | - | 0.0 vs. 3.1 (p=0.032) | 139 vs. 146 (p=0.066) | 0.0 vs. 0.04 (per night) |
| Inpatient, 90-min Exercise [65] | DHAP vs. SHAP | - | 0.0 vs. 11.0 (p<0.001) | - | 0.09 vs. 0.46 (per session) |
| Outpatient, 4 days [65] | DHAP vs. SHAP | - | 1.3 vs. 2.8 (p<0.001) | 155 vs. 148 (p=0.062) | - |
| Outpatient, 60 hours [65] | DHAP vs. SHAP | - | 3.6 vs. 3.9 (p=0.072) | 142 vs. 142 (p=0.98) | 0.26 vs. 0.61 (per 60h) |
| 15-hour Inpatient (with exercise) [6] | DHAP vs. Conventional Pump | 70.7% vs. 57.3% (p=0.003) | 0.0% (<3.3 mmol/L) vs. 2.8% (p=0.006) | - | 1/15 vs. 8/15 participants (p=0.02) |
Table 2: Hormone Delivery and System Performance Metrics
| Parameter | Typical Findings in DHAP Systems | Contextual Notes |
|---|---|---|
| Daily Glucagon Dose [65] | 0.145 - 0.82 mg/day | Dose depends on algorithm aggressiveness; higher if targeting lower mean glucose. |
| Plasma Glucagon Levels [65] | Mostly 50-150 pg/mL (physiological range) | Can cause transient hyperglucagonemia in some cases. |
| Insulin Delivery [65] | Comparable between DHAP and SHAP | DHAP does not typically require more insulin than SHAP. |
| Time in Range (vs. SAP) [66] | ~3 hours improvement daily | Meta-analysis finding; accompanied by ~2.5h less hyperglycemia and ~30min less hypoglycemia. |
Interpretation of Clinical Data
- Hypoglycemia Reduction is the Primary Advantage: The most consistent and significant finding across studies is the superior ability of DHAP systems to reduce both the time spent in hypoglycemia and the number of discrete hypoglycemic events, particularly during physiologic challenges like exercise [65] [6]. This is attributed to the rapid pharmacokinetic profile of subcutaneous glucagon (onset ~5 minutes), which can counteract dropping glucose levels more effectively than the suspension of subcutaneous insulin alone, given the latter's longer dwell time in tissue [65].
- Exercise as a Key Differentiator: The superiority of DHAP is most pronounced in the context of physical activity. In a 90-minute exercise study, the DHAP system virtually eliminated hypoglycemia (0.0% time <70 mg/dL) compared to SHAP (11.0%) [65]. This is critical as exercise remains a major challenge for individuals with T1D due to increased glucose utilization and the inability to naturally suppress circulating insulin levels [66].
- Comparative Efficacy in Overnight Control: For overnight glycemic control, SHAP systems are often sufficient to achieve good control and eliminate hypoglycemia, with several studies showing no statistically significant difference between SHAP and DHAP during the nocturnal period [65] [67]. This suggests that the added complexity of a second hormone may not be necessary for this specific use case.
- Impact on Hyperglycemia and Mean Glucose: The data on hyperglycemia and mean glucose is less consistent. Some studies show a trend toward higher mean glucose with DHAP, potentially reflecting a more conservative insulin dosing strategy to leverage glucagon for hypoglycemia prevention [65]. The choice of control algorithm—whether glucagon is used primarily for hypoglycemia rescue or to enable more aggressive insulin delivery—directly influences this outcome [65].
Experimental Protocols for Head-to-Head Evaluations
To generate the comparative data outlined above, robust and standardized experimental protocols are essential. The following details a typical inpatient study design and a specific exercise protocol.
Standardized Inpatient Crossover Protocol
Objective: To compare the glycemic control efficacy and safety of DHAP, SHAP, and conventional therapy under controlled conditions, including meal and exercise challenges.
Methodology:
- Design: Randomized, open-label, crossover trial where each participant serves as their own control [6].
- Participants: Adults with T1D, using an insulin pump for >3 months, HbA1c <10.5%. Exclusion criteria include pregnancy, recent severe hypoglycemia, and gastrointestinal conditions that affect absorption [6] [68].
- Interventions: Each participant undergoes two or more 15-24 hour study visits, each employing a different technology (e.g., DHAP, SHAP, conventional pump).
- Standardized Challenges:
- Exercise Session: A 30-minute moderate-intensity (60% VO2max) exercise bout on a stationary bicycle in the evening. A pre-exercise capillary glucose check is performed, with a carbohydrate supplement given if glucose is <6.0 mmol/L [6].
- Meals: Standardized evening meal (e.g., 60-80g carbohydrates) and a bedtime snack (15g carbohydrates) are provided [6].
- Data Collection: Venous blood samples are drawn every 10-60 minutes for precise measurement of plasma glucose, insulin, and glucagon [6].
- Outcomes: Primary outcome is the percentage of time plasma glucose is in the target range (e.g., 4.0–10.0 mmol/L from 1600-2300 and 4.0–8.0 mmol/L overnight). Secondary outcomes include time in hypo-/hyperglycemia, total insulin/glucagon delivered, and number of hypoglycemic events [6].
Controlled Exercise Study Protocol
Objective: To specifically evaluate the performance of AP systems in preventing exercise-induced hypoglycemia.
Methodology:
- A subset of the inpatient protocol focusing on a controlled exercise session.
- Participants are connected to the study system (DHAP or SHAP) well before the exercise begins to ensure stable baseline control.
- The exercise modality, intensity, and duration are strictly standardized (e.g., 60% VO2max for 30-60 minutes) [66] [6].
- Glycemic outcomes are analyzed for the exercise period and the subsequent recovery phase, with a particular focus on the time spent in hypoglycemia (<70 mg/dL) and the need for rescue carbohydrates [65].
Signaling Pathways and Hormonal Regulation
The physiological rationale for DHAP systems is rooted in the dysregulation of key glucoregulatory hormones in T1D. The following diagram illustrates the coordinated hormonal pathways during exercise and the points of failure in T1D that DHAP systems aim to address.
Figure 1: Hormonal Regulation During Exercise in Health vs. T1D. In T1D, the inability to suppress exogenous insulin and a blunted glucagon response disrupt glucose homeostasis, increasing hypoglycemia risk.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Technologies for AP Research
| Component | Example Products/Models | Critical Function in Research |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Dexcom G6, Medtronic Guardian, FreeStyle Libre | Provides real-time interstitial glucose measurements to the control algorithm. Accuracy is paramount and can be affected by exercise [66] [68]. |
| Insulin Pump | Tandem t:AP, Medtronic Paradigm Veo | Delivers subcutaneous rapid-acting insulin (e.g., Insulin Aspart). Tethered and patch pumps are used [6] [69]. |
| Glucagon Formulation | Recombinant Glucagon (Liquid-stable) | Subcutaneous delivery of mini-boluses for hypoglycemia prevention. Stable, soluble formulations are critical for DHAP viability [67] [65]. |
| Control Algorithm | Model Predictive Control (MPC), Proportional-Integral-Derivative (PID), Fuzzy Logic | The "brain" of the AP. Computes optimal insulin/glucagon infusion rates based on CGM data, often every 5-10 minutes [66] [16]. |
| Physical Activity Monitor | Commercial Smartwatches, Activity Bands/Rings (e.g., using photoplethysmography & accelerometry) | Provides external signals (heart rate, motion) to inform the algorithm of exercise start, intensity, and type, enabling proactive adjustments [19]. |
| In Silico Simulation Platform | UVA/Padova T1D Simulator | Validated computer simulation of T1D population used for initial algorithm design, testing, and refinement in a safe, cost-effective environment [67] [16]. |
The collective evidence firmly establishes that DHAP systems offer a clinically significant advantage over SHAP and conventional pump therapy in reducing hypoglycemia, especially during challenging periods like physical activity. The primary trade-off involves increased system complexity and the ongoing development of stable glucagon formulations. Future research and development should focus on optimizing adaptive and personalized control algorithms, integrating reliable exercise detection from wearable sensors, and conducting long-term outcomes studies to solidify the value proposition of dual-hormone therapy for people with T1D [19] [16].
Analyzing Real-World Efficacy and Safety Data from Recent Multicenter Trials
The management of diabetes, particularly Type 1 Diabetes (T1DM), presents a significant clinical challenge due to the constant risk of dangerous glucose fluctuations. Dual-hormone (insulin and glucagon) delivery systems have emerged as a promising therapeutic strategy to mimic natural pancreatic function more closely. This application note synthesizes real-world efficacy and safety data from recent multicenter trials and meta-analyses concerning these advanced systems. Framed within the broader context of dual-hormone delivery system development, this document provides researchers and drug development professionals with a structured analysis of critical outcomes, detailed experimental protocols for system evaluation, and visualizations of core concepts to support further research and development.
Efficacy and Safety Data Analysis
Recent meta-analyses of randomized controlled trials (RCTs) provide robust, quantitative evidence for the superior efficacy of automated insulin delivery (AID) systems, with dual-hormone configurations showing particular promise.
Table 1: Glycemic Efficacy Outcomes of AID Systems vs. Control Treatments [70]
| Glycemic Metric | Pooled Result with AID Systems | Statistical Significance |
|---|---|---|
| Time in Range (TIR)(3.9-10.0 mmol/L) | +11.74%(95% CI: 9.37 to 14.12) | P < 0.001 |
| Time Below Range (TBR)(<3.9 mmol/L) | -1.80% in patients with diabetes duration >20 years | P = 0.031 |
| Glycemia Risk Index (GRI) | Improvement of -3.74 points(95% CI: -6.34 to -1.14) | P < 0.01 |
| HbA1c | Greater reduction compared to other insulin-based therapies | Supported by meta-analysis |
A comprehensive 2024 meta-analysis of 65 RCTs involving 3,623 patients with T1DM demonstrated that AID systems significantly improve the percentage of Time in Range (TIR) by 11.74% compared to control treatments, which included multiple daily injections (MDI) and sensor-augmented pumps (SAP) [70]. The analysis further revealed that the benefits for reducing hypoglycemia, as measured by Time Below Range (TBR), were more pronounced in patients with a longer duration of diabetes (>20 years) [70]. Dual-hormone full closed-loop systems demonstrated a greater improvement in TIR compared to single-hormone hybrid closed-loop systems [70].
Table 2: Safety and Tolerability Profile of Combination Therapies [71]
| Safety Parameter | Findings in Combination Therapy vs. Monotherapy |
|---|---|
| Hypoglycemia | Risk significantly increased |
| Drug Discontinuation | More likely to occur |
| Gastrointestinal Events (Diarrhea, Nausea, Vomiting) | More likely to occur |
| Injection Site Events | More likely to occur |
| Genital Infections | More likely to occur |
Regarding safety, a meta-analysis of eight RCTs evaluating the combination of glucagon-like peptide-1 receptor agonists (GLP-1RAs) and sodium-glucose co-transporter-2 inhibitors (SGLT-2is) showed that, while efficacious, combination therapy was associated with a significantly increased risk of hypoglycemia and a higher likelihood of adverse events such as diarrhea, nausea, and injection-site reactions [71]. This underscores the critical need for precise control algorithms in dual-hormone systems to mitigate these risks.
Detailed Experimental Protocols
To ensure the consistent and high-quality collection of real-world data across multiple centers, the following protocols outline standardized procedures for key experiments.
Protocol for a Multicenter Randomized Controlled Trial
This protocol provides a framework for conducting a robust MCCT to evaluate a dual-hormone AID system.
- 1. Title Page: Includes the full study title, objectives, sponsor information, issue date, protocol version, and phase of development. The title must accurately summarize the design, product, indication, and patient population [72].
- 2. Introduction and Background: Provides the rationale by reviewing the disease burden, current treatment limitations, and preclinical and clinical data supporting the dual-hormone product under investigation [72].
- 3. Study Objectives:
- Primary Objective: To compare the percentage of Time in Range (TIR, 3.9-10.0 mmol/L) between the dual-hormone AID system and a single-hormone AID system over a 24-week period [70].
- Secondary Objectives: To compare changes in HbA1c, Time Below Range (TBR), Time Above Range (TAR), Glycemia Risk Index (GRI), and total daily insulin dose [70].
- 4. Endpoints:
- Primary Efficacy Endpoint: Mean change in TIR from baseline to week 24.
- Secondary Efficacy Endpoints: Mean change in HbA1c, TBR, TAR, GRI, and body weight from baseline to week 24.
- Safety Endpoints: Incidence and severity of adverse events, including severe hypoglycemia and diabetic ketoacidosis (DKA) [70].
- 5. Study Design: A prospective, randomized, open-label, parallel-group, multicenter trial. Includes a 2-week run-in period for baseline data collection, followed by a 24-week intervention period.
- 6. Subject Selection:
- Inclusion Criteria: Adults (age ≥18) with T1DM for at least one year; baseline HbA1c between 7.0% and 10.0%; using either MDI or CSII for at least 6 months [70].
- Exclusion Criteria: History of recurrent severe hypoglycemia or DKA in the past 6 months; pregnancy; significant renal or hepatic impairment; use of drugs that significantly impact glucose metabolism.
- 7. Methodology and Procedures:
- Randomization: Participants will be centrally randomized 1:1 to either the dual-hormone AID system or the single-hormone AID system.
- Device Training: All participants will receive standardized training on the use of the AID system and continuous glucose monitor (CGM).
- Data Collection: CGM data will be collected continuously. HbA1c and safety labs will be measured at baseline, week 12, and week 24. Adverse events will be recorded throughout the study.
- 8. Statistical Methods:
- Sample Size Calculation: Based on detecting a 5% difference in TIR with 90% power and a two-sided alpha of 0.05, requiring approximately 150 participants per group.
- Analysis Sets: Efficacy analyses will use the Full Analysis Set (all randomized subjects) and the Per Protocol Set. Safety analyses will use the Safety Analysis Set (all subjects who received any treatment) [72].
- Primary Analysis: A mixed-model repeated measures (MMRM) analysis will compare the change in TIR between groups from baseline to week 24.
Protocol for In Vivo Responsiveness Testing
This protocol details the methodology for testing the insulin-triggered release of glucagon in an animal model, a foundational experiment for smart dual-hormone systems [11].
- 1. Objective: To evaluate the in vivo insulin-responsive performance and safety of a glucagon-loaded microneedle (MN) array patch in a streptozotocin (STZ)-induced T1DM mouse model.
- 2. Experimental Animals: STZ-induced type 1 diabetic mice (e.g., C57BL/6J strain).
- 3. Formulation Preparation: The insulin-responsive glucagon conjugate (Glu-HA) is prepared by coupling an insulin aptamer to glucagon (Apt-Glu) and binding it to insulin-immobilized methacrylated hyaluronic acid (Ins-HA). This matrix is photo-crosslinked into a hydrogel and fabricated into an MN array [11].
- 4. Intervention:
- The Glu-HA MN array patch is administered on the shaved dorsum of the mouse.
- A high dose of insulin (e.g., 0.75 U/kg) is injected subcutaneously to induce a hypoglycemic challenge.
- Blood glucose levels (BGL) are monitored frequently over several hours.
- 5. Control Groups:
- Diabetic mice with the Glu-HA MN patch but injected with a low, non-hypoglycemic dose of insulin.
- Diabetic mice without the patch injected with a high dose of insulin.
- Healthy mice treated with the Glu-HA MN patch.
- 6. Outcome Measures:
- Primary: Blood glucose levels over time.
- Secondary: Serum glucagon levels measured post-insulin challenge; histological analysis of the application site for irritation.
- 7. Data Analysis: Compare BGL trajectories and minimum glucose values between experimental and control groups to assess the patch's ability to prevent profound hypoglycemia.
System Workflow and Logical Diagrams
The following diagrams illustrate the architecture and control logic of an advanced dual-hormone system.
Smart Dual-Hormone AP Workflow
Insulin-Responsive Glucagon Release Mechanism
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Dual-Hormone Delivery System Research
| Reagent / Material | Function / Application | Key Characteristics |
|---|---|---|
| Methacrylated Hyaluronic Acid (m-HA) | Biocompatible, biodegradable polymer matrix for drug encapsulation and microneedle formation [11]. | High biocompatibility; modifiable with functional groups; forms hydrogels via photo-crosslinking. |
| Insulin Aptamer | Single-stranded oligonucleotide that specifically binds to insulin; serves as the responsive trigger mechanism [11]. | High specificity and affinity for insulin; enables competitive binding for controlled release. |
| Aptamer-Glucagon Conjugate (Apt-Glu) | The active therapeutic; glucagon molecule modified with an insulin-binding aptamer [11]. | Retains glucagon bioactivity; allows for tethering to and release from the HA matrix. |
| Bergman Minimal Model (BMM) | A mathematical framework of glucose-insulin dynamics used for designing and simulating control algorithms [7]. | Represents key physiological interactions; foundational for in silico testing of controllers. |
| Continuous Glucose Monitor (CGM) | Provides real-time, interstitial fluid glucose measurements for the control system [70] [7]. | Essential for closed-loop feedback; provides data stream for ML prediction and event detection. |
| Model Predictive Control (MPC) | Advanced control algorithm that predicts future glucose levels to optimize hormone infusion rates [7]. | Anticipates glycemic trends; can incorporate patient-specific constraints for safety. |
Conclusion
Dual-hormone artificial pancreas systems represent a paradigm shift in Type 1 Diabetes management, moving beyond the capabilities of single-hormone systems by offering proactive defense against hypoglycemia. The synthesis of advanced control algorithms, including event-triggered and robust H∞ designs, with machine learning for personalized prediction, is paving the way for truly fully closed-loop systems. Future development must focus on overcoming the remaining practical barriers, particularly the creation of a stable, ready-to-use liquid glucagon formulation and the refinement of algorithms to function autonomously across all life activities without user input. The convergence of artificial intelligence, adaptive control, and stable hormone therapeutics holds the promise of delivering a fully automated, patient-centric artificial pancreas that supports a broader range of individuals living with T1D, ultimately improving both clinical outcomes and quality of life.
References
- 1. Automated Insulin Delivery Systems: A Complete Guide [https://tcoyd.org/2025/04/automated-insulin-delivery-systems-comparison/]
- 2. Closed-Loop Insulin Delivery Systems: Past, Present, and ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2022.919942/full]
- 3. Automated Insulin Delivery Systems and Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12418225/]
- 4. Closed loop insulin delivery–Opportunities and limitations [https://pmc.ncbi.nlm.nih.gov/articles/PMC10755602/]
- 5. Automated Insulin Delivery for Hypoglycemia Avoidance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10171955/]
- 6. Glucose-responsive insulin and glucagon delivery (dual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3589308/]
- 7. Event-triggered smart dual hormone artificial pancreas for ... [https://www.nature.com/articles/s41598-025-18085-9]
- 8. An AI-enabled dual-hormone model predictive control ... [https://www.sciencedirect.com/science/article/pii/S2405896325003155]
- 9. Prevention of Exercise-Associated Dysglycemia: A Case ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4334080/]
- 10. Hypoglycemia in diabetes: An update on pathophysiology, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8696639/]
- 11. Insulin-Responsive Glucagon Delivery for Prevention of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5769873/]
- 12. Post Meal Exercise May Lead to Transient Hypoglycemia ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2020.00578/full]
- 13. Glucagon in metabolic disease: a mini-review of emerging ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1645041/full]
- 14. Glucagon in glucose homeostasis and metabolic disease [https://pubmed.ncbi.nlm.nih.gov/40314189/]
- 15. Low-Dose Glucagon to Prevent and Treat Exercise ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12368384/]
- 16. Robust dual-hormone controller for full closed-loop ... [https://www.sciencedirect.com/science/article/abs/pii/S0208521625000324]
- 17. Dual hormone fully closed loop in type 1 diabetes [https://pmc.ncbi.nlm.nih.gov/articles/PMC10450048/]
- 18. Role of glucagon in automated insulin delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7398489/]
- 19. Research Gaps, Challenges, and Opportunities in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213545/]
- 20. Social Determinants of Health and Diabetes: A Scientific Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC7783927/]
- 21. RESILIENCE IN VULNERABLE POPULATIONS WITH TYPE 2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4556590/]
- 22. Implantable Device Shows Promise for Preventing ... [https://www.medscape.com/viewarticle/implantable-device-shows-promise-preventing-hypoglycemia-2025a1000l7n]
- 23. Association Between Diabetes Management Behaviors ... [https://link.springer.com/article/10.1007/s13300-025-01754-3]
- 24. Automated Insulin Delivery Algorithms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6695267/]
- 25. Design of a Dual-Hormone Model Predictive Control for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5858942/]
- 26. A Dual-Hormone Multicontroller for Artificial Pancreas ... [https://pubmed.ncbi.nlm.nih.gov/35704538/]
- 27. Robust μ-Controller for Automatic Glucose Regulation ... [https://www.mdpi.com/2227-7390/11/18/3856]
- 28. Automated insulin delivery in adults - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6986367/]
- 29. Multiplex Enhancer Interference Reveals Collaborative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5679353/]
- 30. -triggered smart Event artificial pancreas for... dual hormone [https://www.nature.com/articles/s41598-025-18085-9?error=cookies_not_supported&code=cdd454d2-f22b-4848-95b8-82e8e1ef4292]
- 31. -triggered smart Event artificial pancreas for... dual hormone [https://pubmed.ncbi.nlm.nih.gov/40890467/]
- 32. The Most Exciting Diabetes Technology Updates [https://beyondtype1.org/top-diabetes-tech-ada-2025/]
- 33. Clinical Applications of Machine Learning - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11191915/]
- 34. ML Experiment Tracking: Why It Matters, How to Implement it [https://neptune.ai/blog/ml-experiment-tracking]
- 35. A quick guide to managing machine learning experiments [https://medium.com/data-science/a-quick-guide-to-managing-machine-learning-experiments-af84da6b060b]
- 36. Key challenges for delivering clinical impact with artificial ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-019-1426-2]
- 37. Insulin Pumps l Understanding CGM & Pump Integration ... [https://www.adces.org/education/danatech/insulin-pumps/training-clients-patients/cgm-pump-integration]
- 38. The most connected CGM brand in the world 1 [https://www.dexcom.com/en-us/partnerships/integrations-and-compatibility]
- 39. CGM & t:slim X2 Insulin Pump Integrations [https://www.tandemdiabetes.com/products/cgm-partners]
- 40. Early Stages of Automated Insulin Delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213537/]
- 41. Understanding Device Integrations Within Diabetes Apps [https://pmc.ncbi.nlm.nih.gov/articles/PMC12133075/]
- 42. Stability of Commercially Available Glucagon Formulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5653137/]
- 43. Performance of a dual-hormone closed-loop system versus ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1073388/full]
- 44. Intranasal delivery of glucagon -like peptide-1 to the brain for obesity... [https://pubmed.ncbi.nlm.nih.gov/39086086/]
- 45. Dual-hormone artificial pancreas for management of type 1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9059950/]
- 46. Insulin on Board (IOB or BOB) [https://www.adces.org/education/danatech/insulin-pumps/insulin-pumps-101/insulin-pump-glossary/insulin-on-board-(iob-or-bob)]
- 47. Refining Insulin on Board with netIOB for Automated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11571556/]
- 48. Understanding Insulin on Board (IOB) Calculations - OpenAPS [https://openaps.readthedocs.io/en/latest/docs/While%20You%20Wait%20For%20Gear/understanding-insulin-on-board-calculations.html]
- 49. Insulin on Board (IOB) [https://www.tandemdiabetes.com/support-center/pumps-and-supplies/tslimx2-insulin-pump/article/insulin-on-board]
- 50. 综述:自动化胰岛素输送系统的未来 [https://www.ebiotrade.com/newsf/2025-6/20250617074034249.htm]
- 51. Mini-Dose Glucagon as a Novel Approach to Prevent Exercise ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6463733/]
- 52. and Dual-Hormone Closed-Loop Systems That Adapt to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6014543/]
- 53. Glucagon: Delivery advancements for hypoglycemia ... [https://www.sciencedirect.com/science/article/abs/pii/S037851732400019X]
- 54. Safety and Efficacy of Sustained Automated Insulin ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/37729080/]
- 55. Study finds automated insulin delivery systems reduce ... [https://www.upstate.edu/news/articles/2025/2025-01-27-nejm.php]
- 56. Closed-Loop Control Without Meal Announcement in Type ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5647490/]
- 57. A statistical virtual patient population for the glucoregulatory system in... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0217301]
- 58. In silico design and validation of a time-varying PID ... [https://pubmed.ncbi.nlm.nih.gov/37229215/]
- 59. [1910.04059] A Dual - Hormone Closed-Loop Delivery for... System [https://arxiv.org/abs/1910.04059]
- 60. A quick-start guide for design of simulation experiments ... [https://www.sciencedirect.com/science/article/abs/pii/S0304380020303161]
- 61. Efficacy and Safety of Automated Insulin Delivery Systems ... [http://e-dmj.org/journal/view.php?doi=10.4093/dmj.2024.0130]
- 62. Practical implementation of automated insulin delivery ... [https://www.sciencedirect.com/science/article/abs/pii/S1262363625000321]
- 63. Analysis of “Performance of an Automated Insulin Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12003315/]
- 64. ATTD 2025 Top 10 Hits [https://theglucoseneverlies.com/attd-2025-top-10-hits/]
- 65. Insulin-and-Glucagon Artificial Pancreas Versus Insulin-Alone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6695257/]
- 66. Artificial Pancreas Systems and Physical Activity in Patients ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6835182/]
- 67. Parallel Control of an Artificial Pancreas with Coordinated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6835176/]
- 68. Randomized Crossover Comparison of Automated Insulin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7757622/]
- 69. Artificial pancreas: the past and the future [https://link.springer.com/article/10.1007/s10047-025-01510-1]
- 70. Efficacy and Safety of Automated Insulin Delivery Systems in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11960199/]
- 71. The Efficacy and Safety of the Combination Therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8854770/]
- 72. Guidelines for Writing Protocols [https://retinatoday.com/articles/2014-oct/guidelines-for-writing-protocols]