Dietary Proteins and Amino Acids in Glucose Homeostasis: Molecular Mechanisms, Clinical Applications, and Therapeutic Potential
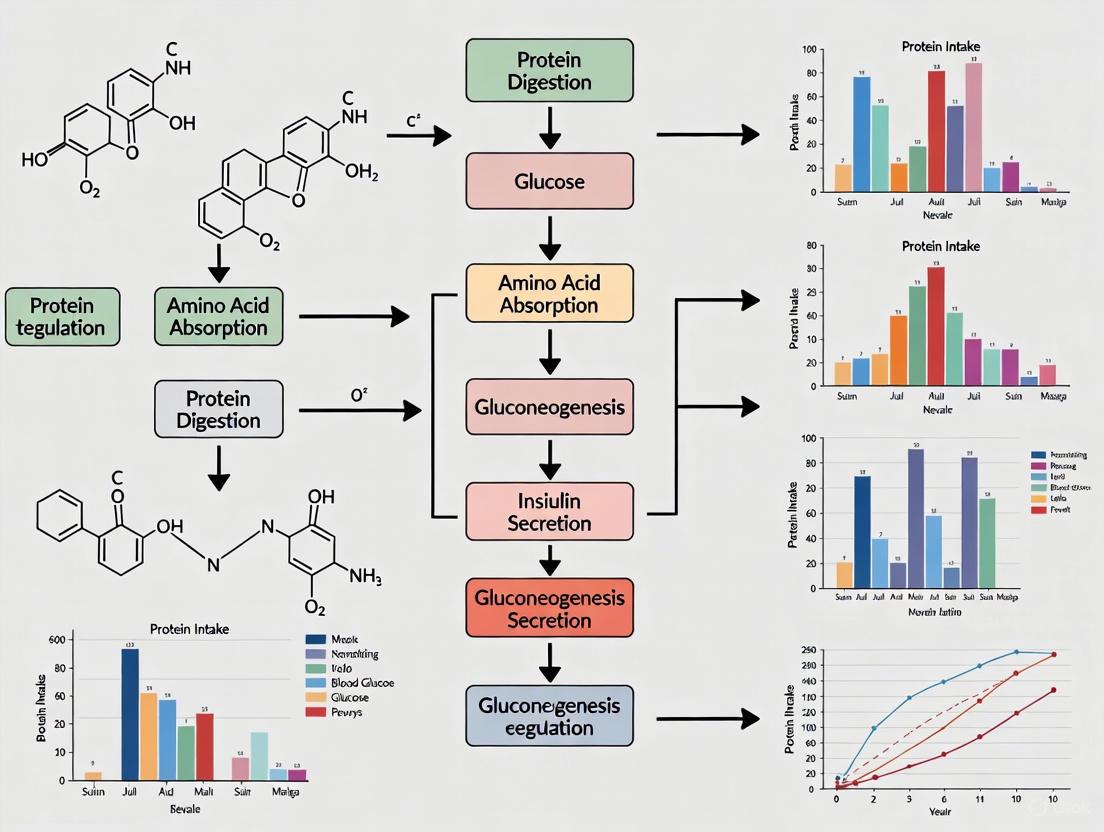
This article synthesizes current evidence on the complex, dual role of dietary proteins and amino acids in regulating glucose metabolism.
Dietary Proteins and Amino Acids in Glucose Homeostasis: Molecular Mechanisms, Clinical Applications, and Therapeutic Potential
Abstract
This article synthesizes current evidence on the complex, dual role of dietary proteins and amino acids in regulating glucose metabolism. It explores foundational mechanisms, including the activation of nutrient-sensing pathways like mTOR and the paradoxical effects of branched-chain amino acids (BCAAs), which can both promote insulin sensitivity and contribute to resistance. For researchers and drug development professionals, the content evaluates methodological approaches such as specialized high-protein diets and amino acid supplementation, detailing their application in weight loss, sarcopenia mitigation, and metabolic health. It addresses key challenges, including the impact of protein source and chronic amino acid elevations, and validates findings through comparative analysis of clinical outcomes across different dietary patterns and populations. The review concludes by highlighting emerging research directions and the potential for targeted nutritional and pharmaceutical interventions.
The Dual Role of Amino Acids: Molecular Mechanisms in Insulin Signaling and Metabolic Regulation
Skeletal Muscle as the Primary Site of Insulin-Stimulated Glucose Disposal
Skeletal muscle is the principal site for postprandial glucose clearance, accounting for approximately 80% of insulin-mediated glucose disposal [1] [2] [3]. This whitepaper details the molecular mechanisms governing glucose uptake in skeletal muscle and examines how dietary proteins and amino acids modulate this process. We explore the signaling pathways involved, the impact of different protein interventions on insulin sensitivity, and the experimental methodologies used to investigate these relationships. The complex, dual role of amino acids—both as potential enhancers and disruptors of insulin signaling—is discussed within the context of developing targeted therapeutic and nutritional strategies for managing insulin resistance and type 2 diabetes (T2D).
Skeletal muscle is the largest organ in the human body and the major determinant of whole-body glucose metabolism. After a meal, the rise in blood glucose triggers insulin secretion, which in turn stimulates skeletal muscle to absorb glucose from the bloodstream. The central role of skeletal muscle in this process is underscored by quantitative assessments showing it is responsible for the majority of insulin-stimulated glucose disposal [1] [3]. This immense capacity makes skeletal muscle insulin sensitivity a critical factor in systemic metabolic health; its dysfunction is a primary feature of insulin resistance and T2D.
Contemporary research into glucose homeostasis increasingly focuses on the interplay between macronutrients, revealing that dietary proteins and amino acids are potent modulators of metabolic pathways beyond their traditional role in muscle protein synthesis. This review will dissect the mechanisms of skeletal muscle glucose disposal and frame these findings within a growing body of research on the impact of dietary proteins and amino acids.
Quantitative Data on Muscle Glucose Disposal
The following table summarizes key quantitative findings related to skeletal muscle's role in glucose disposal and the effects of dietary interventions.
Table 1: Key Quantitative Data on Skeletal Muscle Glucose Disposal and Dietary Protein Effects
| Parameter | Quantitative Finding | Context / Intervention | Source |
|---|---|---|---|
| Glucose Disposal | ~80% of insulin-stimulated glucose disposal | Postprandial state in humans | [1] [3] |
| Weight Loss | -8.05 kg (HPA) / -7.70 kg (HPP) | 6-month low-calorie, high-protein (35%E) diet | [4] |
| HbA1c Reduction | -0.8% | 5-week high-protein (30%E) diet vs. -0.3% with control diet | [5] |
| 24-h Glucose AUC | 40% decrease | 5-week high-protein diet vs. control diet | [5] |
| Optimal Protein Intake | 12.20-16.85 %E | U-shaped association with T2D risk; cut-off at 14.53%E | [6] |
| Leg Glucose Uptake | 45% decline | After 3 days of bed rest in young, healthy adults | [2] [3] |
Molecular Mechanisms of Insulin-Stimulated Glucose Uptake
The translocation of the glucose transporter GLUT4 to the plasma membrane is the fundamental event in insulin-stimulated glucose uptake in skeletal muscle [7]. This process is orchestrated by a highly coordinated insulin signaling cascade and cytoskeletal remodeling.
Canonical Insulin Signaling and GLUT4 Translocation
Insulin binding to its receptor initiates a phosphorylation cascade. A critical downstream effector is the small GTPase Rac1 [7]. Upon insulin stimulation, Rac1 is activated and facilitates the rearrangement of the cortical actin network. This remodeling is essential for the translocation and docking of GLUT4 storage vesicles (GSVs) at the plasma membrane, enabling the uptake of glucose.
The diagram below illustrates the core signaling pathway from the insulin receptor to GLUT4 translocation.
Critical Research Findings on Signaling Components
- Rac1 Activation: Rac1 activation is necessary and sufficient for insulin-stimulated glucose uptake. Expression of a constitutively active Rac1 mutant can induce GLUT4 translocation and glucose uptake even in the absence of insulin [7].
- Akt2 Dependency: The activation of Rac1 in this pathway is dependent on the protein kinase Akt2, highlighting a key link between the canonical insulin signaling pathway and cytoskeletal reorganization [7].
- Molecular Link: The guanine nucleotide exchange factor (GEF) FLJ00068 has been identified as a critical molecular link, transducing signals from Akt2 to activate Rac1 [7].
Impact of Dietary Proteins and Amino Acids on Insulin Sensitivity
The relationship between dietary protein, amino acids, and insulin resistance is complex and exhibits a duality: acute or strategic intake can be beneficial, while chronic imbalances can be detrimental.
Beneficial Effects of High-Protein Diets and Amino Acids
Table 2: Mechanisms and Evidence for Beneficial Effects of Protein/AA
| Mechanism | Experimental Evidence | Outcome |
|---|---|---|
| Muscle Mass Preservation | High-protein (35-45%E) diet during caloric restriction preserves fat-free mass. | Maintains glucose disposal capacity; enhances fat loss [1] [2]. |
| mTOR Activation & MPS | Leucine and Essential AA (EAA) intake acutely activates mTORC1. | Stimulates muscle protein synthesis (MPS), maintaining metabolic tissue [1] [3]. |
| Mitochondrial Biogenesis | Leucine activates SIRT1/AMPK/PGC-1α axis. | Augments mitochondrial function and fatty acid oxidation, improving insulin sensitivity [2] [3]. |
| Direct Glycemic Control | High-protein diet (30%E) vs. control (15%E) in T2D subjects. | 40% lower 24-h glucose AUC; 0.8% greater HbA1c reduction [5]. |
| Source-Independent Benefit | 6-month hypoenergetic diets with protein from 75% animal (HPA) or plant (HPP) sources. | Both HPA and HPP improved body composition and glycemic markers equally [4]. |
Detrimental Effects and the "Amino Acid Paradox"
Paradoxically, chronic elevations of certain amino acids, particularly branched-chain amino acids (BCAAs), are strongly associated with insulin resistance [1] [8] [9].
- Chronic mTOR Activation: Sustained high BCAA levels lead to chronic activation of the mTOR-S6K1 pathway. This results in feedback inhibition of insulin signaling by promoting serine phosphorylation of Insulin Receptor Substrate-1 (IRS-1), which impairs PI3K activation and downstream glucose uptake [1] [9].
- Lipotoxicity: The pathogenic link between BCAAs and insulin resistance often relies on a background of nutrient overload and chronic hyperinsulinemia, which fosters lipotoxicity. This environment exacerbates the defects in insulin signaling [1].
- Context is Key: The detrimental effects are typically linked to chronic postabsorptive elevations, as seen in obesity, in contrast to the beneficial acute postprandial rises that stimulate anabolic processes [2] [3].
The following diagram summarizes the dual role of amino acids in regulating insulin sensitivity.
Key Experimental Models and Protocols
Research in this field relies on a combination of human clinical trials, advanced metabolic phenotyping, and molecular biology techniques.
Human Dietary Intervention Studies
Protocol: Long-Term, High-Protein, Low-Calorie Diet Trial [4]
- Objective: To compare the effects of plant-based versus animal-based high-protein diets on glycaemic outcomes in subjects with overweight/obesity and prediabetes or T2D.
- Design: 6-month randomized controlled trial.
- Participants: 117 adults with BMI >27.5 kg/m² and glucose metabolism disorders.
- Intervention: Two hypoenergetic diets (-30% TCV) with 35% protein. The HPA group derived 75% of protein from animal sources, while the HPP group derived 75% from plant sources.
- Key Methodologies:
- Body Composition: Assessed using Dual-Energy X-ray Absorptiometry (DEXA).
- Glycaemic Measures: Fasting glucose, insulin, HOMA-IR, HbA1c.
- Metabolic Biomarkers: Liver enzymes, lipid profiles, inflammatory biomarkers (e.g., TNF-α, IL-6), and incretins (GLP-1, GIP) measured via immunoassays.
- Outcome: Both diets similarly improved body weight, fat mass, visceral fat, and all key glycaemic parameters, indicating that the protein source was not a primary factor in the context of weight loss.
Acute Metabolic Studies
Protocol: Protein-Only vs. Carbohydrate-Only Ingestion [10]
- Objective: To compare hormonal and metabolic responses to isocaloric drinks of pure whey protein versus pure carbohydrate.
- Design: Randomized, double-blinded, balanced cross-over study.
- Participants: 14 young, healthy, trained individuals.
- Intervention: After an overnight fast, participants consumed a drink containing either 1.2 g·kg⁻¹ whey protein (PRO) or an isocaloric amount of carbohydrate (CHO).
- Key Methodologies:
- Blood Sampling: Frequent sampling over 4 hours to measure plasma glucose, amino acids, insulin, glucagon, GLP-1, and GIP.
- Urine Collection: Collected in 6 consecutive batches over 24 hours to measure nitrogen excretion.
- Outcome: PRO ingestion stimulated a significant insulin response independent of glucose, mediated by a rise in plasma AAs and GLP-1. This highlights the direct insulinotropic effect of protein.
Molecular Profiling in Human Muscle
Protocol: Skeletal Muscle Proteomics and Phosphoproteomics [8]
- Objective: To identify molecular signatures associated with insulin resistance in human skeletal muscle.
- Design: Case-control study with validation cohort.
- Participants: 77 participants (discovery cohort) and 46 (validation cohort) with and without T2D.
- Key Methodologies:
- Muscle Biopsy: Vastus lateralis biopsies taken under fasting conditions and during a hyperinsulinaemic-euglycemic clamp (the gold standard for measuring insulin sensitivity).
- Proteomic Analysis: High-resolution mass spectrometry to quantify ~3,000 proteins and 15,000 phosphorylation sites.
- Outcome: Identified that the fasting muscle proteome was associated with whole-body insulin resistance, independent of diabetic status. Key findings included disruptions in mTOR signaling and oxidative phosphorylation pathways, and identification of novel phospho-sites like AMPKγ3 S65.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Investigating Muscle Glucose Disposal
| Reagent / Material | Critical Function / Application | Example Use Case |
|---|---|---|
| Hyperinsulinaemic-Euglycemic Clamp | Gold-standard in vivo method for quantifying whole-body insulin sensitivity. | Measuring insulin-stimulated glucose disposal rates in human subjects [8]. |
| Dual-Energy X-ray Absorptiometry (DEXA) | Precisely measures body composition (fat mass, lean mass, bone mass). | Assessing changes in fat-free mass during dietary interventions [4]. |
| Mass Spectrometry (Proteomics/Phosphoproteomics) | High-throughput quantification of protein expression and phosphorylation status. | Identifying novel protein signatures and signaling disruptions in insulin-resistant muscle [8]. |
| Whey Protein Isolate | High-quality, rapidly digested protein source rich in essential amino acids and leucine. | Used in acute interventions to study the metabolic effects of protein/AA ingestion [10]. |
| Specific ELISAs / Immunoassays | Quantify plasma/serum levels of hormones (insulin, GLP-1, GIP) and biomarkers. | Measuring insulin and incretin responses to nutrient challenges [4] [10]. |
| ActiGraph Accelerometers | Objective measurement of physical activity levels in free-living individuals. | Monitoring and ensuring consistent activity levels during dietary trials [4]. |
| Validated Food Frequency Questionnaires (FFQ) | Assess habitual dietary intake of macronutrients and micronutrients. | Estimating baseline protein intake and monitoring adherence in cohort studies [6]. |
Skeletal muscle's role as the primary site of insulin-stimulated glucose disposal is unequivocal. Understanding the molecular machinery that governs GLUT4 translocation, and how it is modulated by dietary components like proteins and amino acids, is fundamental to advancing metabolic science. The evidence demonstrates that high-protein diets, irrespective of animal or plant source, can be effective nutritional strategies for improving body composition and glycemic control, particularly in the context of weight loss. However, the paradoxical effects of amino acids underscore the importance of context—the metabolic background of the individual and the pattern of amino acid exposure (acute vs. chronic) are critical determinants of the outcome.
Future research should focus on:
- Personalized Nutrition: Leveraging molecular phenotyping, such as the proteomic signatures identified by Kjaergaard et al. [8], to tailor dietary protein recommendations for different metabolic subtypes.
- Mechanistic Deep Dive: Further elucidating the mechanisms by which specific amino acids and their metabolites influence mitochondrial function, redox status, and insulin signaling.
- Therapeutic Development: Exploring components of the Rac1 signaling pathway [7] or modifiers of mTOR activity as potential targets for novel insulin-sensitizing drugs.
This synthesis of physiology, nutrition, and molecular biology paves the way for more precise and effective interventions against insulin resistance and diabetes.
The mechanistic target of rapamycin complex 1 (mTORC1) serves as a central regulator of cell growth and metabolism, integrating environmental cues to coordinate anabolic and catabolic processes. Among these cues, nutrient availability—particularly the presence of specific amino acids—plays a fundamental role in modulating mTORC1 activity. Leucine, a branched-chain amino acid (BCAA), has emerged as the most potent amino acid regulator of mTORC1 signaling [11] [12]. This review examines the molecular mechanisms through which leucine activates mTORC1, the downstream consequences for muscle protein synthesis, and the implications of this relationship within the broader context of dietary protein and amino acid effects on glucose homeostasis.
The significance of leucine-mediated mTORC1 activation extends beyond basic cellular physiology to applied clinical contexts. Muscle wasting conditions including sarcopenia, cachexia, and disuse atrophy represent substantial clinical challenges, and therapeutic strategies to counteract these processes often leverage leucine's anabolic properties [13]. Simultaneously, the relationship between chronic mTORC1 activation and metabolic diseases such as insulin resistance necessitates a nuanced understanding of context-dependent leucine effects [3] [14]. This article provides a comprehensive technical overview of the mechanisms, experimental methodologies, and research tools relevant to investigating leucine-induced mTORC1 activation and its functional outcomes.
Molecular Mechanisms of Leucine Sensing and mTORC1 Activation
The mTORC1 Complex: Structure and Core Functions
mTORC1 is a multi-protein complex consisting of mTOR as the catalytic subunit, regulatory-associated protein of mTOR (Raptor), mammalian LST8 homolog (mLST8), and additional regulatory components PRAS40 and DEPTOR [11]. Structurally, mTOR contains N-terminal HEAT repeats, FAT and FRB domains, a kinase domain, and a C-terminal FATC domain [11]. The complex functions as a master regulator of cell growth by promoting anabolic processes including protein, lipid, and nucleotide synthesis while suppressing catabolic processes such as autophagy [11]. mTORC1 activation stimulates mRNA translation and ribosome biogenesis through phosphorylation of key downstream effectors, notably the ribosomal protein S6 kinase 1 (S6K1) and the eukaryotic initiation factor 4E binding protein 1 (4E-BP1) [11].
Table 1: Core Components of mTORC1 and Their Functions
| Component | Function | Characteristics |
|---|---|---|
| mTOR | Catalytic kinase subunit | Phosphorylates downstream targets including S6K1 and 4E-BP1 |
| Raptor | Scaffolding protein | Substrate recognition and recruitment; defines mTORC1 identity |
| mLST8 | Stabilizing subunit | Enhances kinase activity; structural stability |
| PRAS40 | Regulatory subunit | Inhibitory component; dissociates upon activation |
| DEPTOR | Regulatory subunit | Inhibitory component; modulates complex activity |
Leucine Sensing and Intracellular Transport
As an essential amino acid, leucine must be obtained through dietary sources and transported into cells via specific amino acid transporters [15]. The L-type amino acid transporter (LAT) family, particularly LAT1 (SLC7A5) and LAT3 (SLC43A1), facilitate leucine uptake across the plasma membrane [15]. These transporters exhibit distinct tissue distribution patterns and functional characteristics, with LAT1 functioning as a heterodimeric exchanger dependent on its heavy chain subunit CD98hc (SLC3A2), while LAT3 operates as a facilitative diffuser with specificity for branched-chain amino acids [15]. Intracellular leucine accumulation initiates a signaling cascade that ultimately activates mTORC1, though the precise sensing mechanisms have only recently been elucidated.
Key Molecular Machinery in Leucine-Dependent Activation
Leucine activates mTORC1 through multiple interconnected mechanisms that converge on the Rag GTPase system. The current model indicates that leucine binding to the Sestrin2 protein releases its inhibitory interaction with GATOR2, thereby permitting activation of the Rag GTPases [16] [14]. The Rag GTPases (RagA/B and RagC/D heterodimers) function as molecular switches that, in their active GTP/GDP-bound state, recruit mTORC1 to the lysosomal surface [11] [16]. This translocation positions mTORC1 in proximity to its essential activator Rheb (Ras homolog enriched in brain), which is itself regulated by growth factor signaling through the TSC complex (TSC1/TSC2/TBC1D7) [11].
Additional regulatory proteins contribute to leucine sensing, including the folliculin-folliculin interacting protein (FLIP) complex that acts as a GAP for RagC/D, and the GATOR1 complex that functions as a GAP for RagA/B [16]. Recent structural studies have revealed that the interaction between the Rag GTPases and the Raptor component of mTORC1 is crucial for lysosomal recruitment [16]. The following diagram illustrates the core leucine sensing pathway and mTORC1 activation mechanism:
Beyond the canonical Rag GTPase pathway, alternative mechanisms contribute to leucine sensing. The class III phosphoinositide 3-kinase Vps34 has been implicated in amino acid-dependent mTORC1 activation, potentially through generation of phosphatidylinositol 3-phosphate [13]. Additionally, the mitogen-activated protein kinase kinase kinase kinase MAP4K3 has been identified as an amino acid sensor that regulates mTORC1 independently of the insulin signaling pathway [13]. These complementary pathways may provide robustness to nutrient sensing under varying cellular conditions and ensure appropriate mTORC1 activation in response to leucine availability.
Downstream Signaling and Physiological Effects
Translation Initiation and Protein Synthesis
Leucine-activated mTORC1 stimulates muscle protein synthesis primarily through phosphorylation of two key downstream effectors: S6K1 and 4E-BP1 [11] [12]. Phosphorylation of S6K1 on Thr389 promotes its activation and subsequent phosphorylation of multiple targets including the ribosomal protein S6, thereby enhancing the translation of mRNAs containing a 5' terminal oligopyrimidine (TOP) motif, which predominantly encode components of the translation machinery [11]. Concurrently, mTORC1-mediated phosphorylation of 4E-BP1 reduces its affinity for the mRNA cap-binding protein eIF4E, releasing eIF4E to form the eIF4F initiation complex with eIF4G and eIF4A [11] [12]. This complex is essential for cap-dependent translation initiation of numerous mRNAs, particularly those with complex secondary structures in their 5' untranslated regions.
The coordinated regulation of S6K1 and 4E-BP1 by mTORC1 enhances the cellular capacity for protein synthesis while simultaneously increasing the efficiency of translation initiation. This dual mechanism allows leucine to potently stimulate muscle protein accretion, as demonstrated in multiple human studies where leucine administration increased muscle protein synthesis rates by approximately 100% [13]. The following diagram illustrates the key downstream signaling events and functional outcomes:
Additional Metabolic Effects
Beyond its canonical role in stimulating protein synthesis, leucine-activated mTORC1 influences multiple aspects of cellular metabolism. Leucine has been demonstrated to promote mitochondrial biogenesis through activation of peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α), enhancing oxidative capacity and fatty acid oxidation [3] [15]. This effect may occur through both mTORC1-dependent and independent pathways, potentially involving AMP-activated protein kinase (AMPK) and sirtuin 1 (SIRT1) [3]. Additionally, leucine contributes to lipid metabolism by inhibiting lipogenesis and promoting fatty acid oxidation, though the precise mechanisms remain incompletely characterized [15].
The metabolic effects of leucine extend to glucose homeostasis, with both beneficial and potentially detrimental consequences depending on context. Acute leucine administration can improve insulin sensitivity and enhance glucose disposal, likely through mTORC1-mediated effects on muscle metabolism [3]. However, chronic elevation of branched-chain amino acids, including leucine, has been associated with insulin resistance in obese individuals, possibly due to persistent mTORC1 activation that disrupts insulin signaling feedback loops [14]. This dual nature underscores the importance of temporal and contextual factors in determining leucine's metabolic impact.
Experimental Methodologies and Key Findings
Quantitative Data from Human and Animal Studies
Research investigating leucine-induced mTORC1 activation has employed various experimental approaches, including cell culture models, animal studies, and human clinical trials. The following table summarizes key quantitative findings from selected studies:
Table 2: Quantitative Effects of Leucine on mTORC1 Signaling and Protein Synthesis
| Study Model | Leucine Intervention | Key Effects | Magnitude of Change | Citation |
|---|---|---|---|---|
| Human skeletal muscle (young adults) | 0.12 g leucine/kg lean mass + EAA + CHO | Phosphorylation of mTOR, S6K1, 4E-BP1; Muscle protein synthesis | ~100% increase in protein synthesis; Large increases in phosphorylation | [13] |
| Elderly humans (65-82 years) | 2.5 g leucine, 3×/day for 6 weeks | Lean body mass, Muscle strength | Significant increases vs. placebo | [15] |
| Rat skeletal muscle | 0.14 g leucine/kg body weight | Muscle protein synthesis | Near maximal increase | [13] |
| L6 myoblasts | 2 mM leucine | Phosphorylation of 4E-BP1, S6K1, S6; Protein synthesis | Increased phosphorylation; Effect abolished by rapamycin | [13] |
| Human skeletal muscle | 10 g essential amino acids (leucine-enriched) | mTOR signaling, Muscle protein synthesis | Activation at 3 hours post-ingestion | [13] |
Detailed Experimental Protocols
Human Skeletal Muscle Biopsy Protocol for mTOR Signaling Analysis
The assessment of mTORC1 activation in human skeletal muscle typically employs the percutaneous needle biopsy technique before and after leucine administration. The following protocol outlines key methodological considerations:
Pre-Intervention Baseline: Following an overnight fast, obtain baseline muscle biopsy from the vastus lateralis under local anesthesia using a Bergström-type needle with suction applied.
Leucine Administration: Administer a leucine-enriched essential amino acid solution typically providing approximately 0.12 g leucine per kg lean body mass, often combined with carbohydrate (30 g) to moderate insulin response [13].
Post-Intervention Sampling: Obtain subsequent muscle biopsies at predetermined timepoints (e.g., 1-3 hours post-administration) from the same leg at proximal sites separated by 2-3 cm.
Sample Processing: Immediately freeze tissue samples in liquid nitrogen and store at -80°C until analysis. For phosphorylation studies, tissue may be homogenized in RIPA buffer containing phosphatase and protease inhibitors.
Western Blot Analysis: Resolve proteins by SDS-PAGE and transfer to PVDF membranes. Probe with phosphospecific antibodies against key mTORC1 signaling components including phospho-S6K1 (Thr389), phospho-4E-BP1 (Thr37/46), and phospho-mTOR (Ser2448), with total protein antibodies serving as loading controls [13].
Protein Synthesis Measurement: Employ stable isotope tracer methods (e.g., L-[ring-²H₅]phenylalanine) with measurement of incorporation into muscle protein via gas chromatography-mass spectrometry to quantify fractional synthetic rates [13].
Cell Culture Model for Leucine Sensing Mechanisms
In vitro approaches utilizing cell lines provide mechanistic insights into leucine sensing pathways:
Cell Culture and Starvation: Culture L6 myoblasts or other relevant cell lines in appropriate media until 70-80% confluence. Subject cells to amino acid starvation for 1-2 hours using EBSS or customized amino acid-free media.
Leucine Stimulation: Stimulate cells with physiological concentrations of leucine (0.1-2 mM) for predetermined durations (15-60 minutes).
Pharmacological Inhibition: Pre-treat cells with mTOR inhibitors (e.g., 20 nM rapamycin for 30 minutes) or other pathway-specific inhibitors to establish mechanism dependence.
Immunofluorescence and Localization Studies: Fix cells and immunostain for mTOR, LAMP2 (lysosomal marker), and Rag GTPases to assess subcellular localization using confocal microscopy.
Co-Immunoprecipitation: Assess protein-protein interactions by immunoprecipitating Raptor or other complex components and probing for associated proteins such as Rag GTPases under varying leucine conditions.
Gene Silencing Approaches: Utilize siRNA or CRISPR/Cas9 to knock down candidate sensors (e.g., Sestrin2, LAT1) and assess impact on leucine-induced mTORC1 activation.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating Leucine-mTORC1 Signaling
| Reagent Category | Specific Examples | Research Application | Mechanistic Insight |
|---|---|---|---|
| mTOR inhibitors | Rapamycin, Torin1 | Establish mTOR dependence; Distinguish mTORC1 vs. mTORC2 functions | Rapamycin-FKBP12 complex binds FRB domain causing steric hindrance [11] |
| Phosphospecific antibodies | p-S6K1 (Thr389), p-4E-BP1 (Thr37/46), p-mTOR (Ser2448) | Assess pathway activation in Western blot, immunohistochemistry | Readouts of mTORC1 kinase activity [13] |
| Amino acid transporters inhibitors | BCH (LAT1 inhibitor), JPH203 (LAT1-specific) | Determine leucine transport requirements | Distinguish system L transport contributions [15] |
| Stable isotopes | L-[ring-²H₅]phenylalanine, L-[1-¹³C]leucine | Quantify protein synthesis rates in vivo | Measure fractional synthetic rate via tracer incorporation [13] |
| Genetic tools | siRNA against Sestrin2, RagA/B, Raptor; CRISPR/Cas9 knockouts | Establish necessity of specific components | Molecular dissection of sensing machinery [16] |
| Metabolic assays | Seahorse extracellular flux analysis, glucose uptake assays | Assess broader metabolic consequences | Evaluate mitochondrial function, energy metabolism [3] |
Contextual Integration: Leucine Signaling and Glucose Homeostasis
The relationship between leucine-induced mTORC1 activation and glucose homeostasis represents a critical interface with significant research and therapeutic implications. Multiple studies have demonstrated that increased dietary protein intake, particularly when rich in leucine, can improve metabolic parameters during weight loss interventions. In one clinical trial comparing high-protein (45% protein) versus high-carbohydrate (20% protein) diets, the high-protein group exhibited greater improvements in insulin-stimulated glucose disposal alongside preservation of fat-free mass [17]. These findings suggest that leucine's anabolic effects on skeletal muscle—the primary site of insulin-stimulated glucose disposal—may indirectly support glucose homeostasis by maintaining metabolic tissue.
The timing and chronicity of leucine exposure appear to critically influence metabolic outcomes. Acute postprandial leucine elevations promote transient mTORC1 activation that supports muscle protein synthesis and remodeling, potentially enhancing insulin sensitivity [3]. In contrast, chronic elevations in branched-chain amino acids, as often observed in obese, insulin-resistant individuals, may promote persistent mTORC1 activation that disrupts insulin signaling through negative feedback mechanisms [14]. This paradoxical relationship underscores the importance of temporal dynamics in leucine signaling, where oscillatory activation patterns likely support metabolic health while sustained activation promotes dysfunction.
Molecular mechanisms linking leucine sensing to glucose homeostasis extend beyond muscle protein synthesis. Leucine has been demonstrated to activate PGC-1α through both mTOR-dependent and independent pathways, enhancing mitochondrial biogenesis and oxidative metabolism in muscle and adipose tissue [3]. Additionally, leucine influences hepatic glucose production and whole-body energy expenditure through mechanisms that remain incompletely characterized but may involve cross-talk with AMPK signaling [3] [14]. The integration of these pathways highlights the systems-level impact of leucine signaling on metabolic regulation.
Leucine activation of mTORC1 represents a fundamental mechanism linking nutrient availability to cellular growth and metabolic regulation. The molecular machinery comprising LAT transporters, Sestrin2, GATOR complexes, Rag GTPases, and Rheb converges to position mTORC1 at the lysosomal surface where it becomes fully activated. This signaling cascade culminates in phosphorylation of downstream effectors that enhance the cellular capacity for protein synthesis through multiple complementary mechanisms. The experimental methodologies summarized herein provide robust approaches for investigating this pathway in various biological contexts.
Future research should address several outstanding questions in the field, including the potential role of leucine metabolites in mTORC1 regulation, the impact of aging and disease states on leucine sensing efficiency, and the development of therapeutic strategies to modulate this pathway for clinical benefit. Additionally, the dual nature of leucine's effects on insulin sensitivity—with acute benefits but potential chronic detrimental effects—warrants further investigation to establish optimal dosing patterns that maximize anabolic responses while supporting metabolic health. As our understanding of leucine sensing mechanisms continues to evolve, so too will opportunities to leverage this pathway for combating muscle wasting disorders while maintaining glucose homeostasis.
{Abstract} Branched-chain amino acids (BCAAs)—leucine, isoleucine, and valine—occupy a complex and paradoxical role in metabolic regulation. While acute exposure facilitates beneficial anabolic signaling and glucose homeostasis, chronic elevation is strongly associated with the pathogenesis of insulin resistance and type 2 diabetes [2] [18] [19]. This whitepaper synthesizes current research to dissect this duality, detailing the molecular mechanisms, presenting key experimental data, and providing a toolkit for researchers navigating this critical field in metabolic disease research.
{1 Introduction: The Duality of BCAAs in Metabolism} The influence of dietary proteins and amino acids on glucose homeostasis is a central theme in metabolic research. Within this context, BCAAs are unique for their tissue-specific metabolism—initial catabolism occurs primarily in skeletal muscle rather than the liver—and their potent signaling capabilities [19]. Elevated circulating BCAA levels are one of the earliest and most consistent biomarkers of obesity and future insulin resistance [20] [21]. Paradoxically, acute supplementation, particularly of leucine, is known to stimulate insulin secretion and support muscle protein synthesis [2] [19]. This document frames the BCAA paradox within the broader investigation of how dietary proteins impact metabolic health, exploring the fine line between essential physiological signaling and chronic metabolic disruption.
{2 Mechanistic Insights: From Signaling to Dysregulation} The paradoxical effects of BCAAs are mediated by distinct molecular pathways, activated in a context-dependent manner.
2.1 Acute Anabolic and Metabolic Signaling Postprandial elevations in BCAAs, especially leucine, act as critical anabolic signals. The primary mediator is the mammalian Target of Rapamycin Complex 1 (mTORC1) [2] [3]. Acute leucine-induced activation of mTORC1 in skeletal muscle promotes protein synthesis and muscle maintenance, which is crucial for systemic glucose disposal [2]. Furthermore, acute BCAA exposure can augment mitochondrial biogenesis via the SIRT1-AMPK-PGC-1α axis, enhancing oxidative metabolism and insulin sensitivity [2] [3].
2.2 Chronic Pathogenic Mechanisms Sustained high levels of BCAAs drive insulin resistance through multiple, non-exclusive mechanisms:
- Chronic mTOR Activation: Persistent mTORC1 signaling leads to the negative feedback inhibition of insulin receptor substrate (IRS) proteins, impairing the proximal insulin signaling cascade [2].
- Induction of Adipose Tissue Inflammation: Recent research highlights that BCAA accumulation in obesity promotes the polarization of adipose tissue macrophages (ATMs) towards a pro-inflammatory M1 phenotype [22] [23]. This occurs via the IFNGR1/JAK1/STAT1 signaling pathway, leading to the secretion of cytokines like TNF-α, IL-1β, and MCP-1, which directly disrupt insulin action [22] [23].
- Hepatic Metabolic Reprogramming: Restricting specific BCAAs, particularly isoleucine, reprograms liver and adipose metabolism, activating the FGF21-UCP1 axis to increase energy expenditure and improve hepatic insulin sensitivity [21].
- Incomplete Catabolism and Metabolite Accumulation: Obesity-related impairment of the branched-chain keto acid dehydrogenase (BCKDH) complex leads to the accumulation of not only BCAAs but also various bioactive catabolic intermediates (e.g., BCKAs, 3-hydroxy-isobutyrate), which can further exacerbate metabolic stress [22] [23] [19].
The following diagram illustrates the core signaling pathways that underlie the BCAA paradox:
{3 Key Experimental Findings and Data Synthesis} Research across animal models and human studies has quantified the distinct metabolic impacts of BCAAs and their restriction. The following tables summarize critical quantitative findings.
Table 1: Metabolic Effects of Acute BCAA Infusion vs. BCAA Restriction in Mouse Models
| Experimental Intervention | Key Metabolic Outcome | Observed Effect | Citation |
|---|---|---|---|
| Single BCAA Infusion (in mice) | Blood Glucose & Plasma Insulin | Acutely elevated | [20] |
| Constant BCAA Infusion (during clamp) | Whole-Body Insulin Sensitivity | Impaired | [20] |
| Single BT2 injection (BCAA-lowering drug in HFD mice) | Glucose Tolerance | Markedly improved | [20] |
| Low-Isoleucine Diet (67% reduction for 3 weeks) | Glucose Tolerance | Significantly improved | [21] |
| Low-Valine Diet (67% reduction for 3 weeks) | Glucose Tolerance | Trend toward improvement (p=0.06) | [21] |
| Low-Leucine Diet (67% reduction for 3 weeks) | Glucose Tolerance | No significant effect | [21] |
Table 2: Human and Mouse Studies on Chronic BCAA Supplementation
| Study Model | Intervention | Key Findings on Metabolism & Inflammation | Citation |
|---|---|---|---|
| Obese, Prediabetic Humans (n=12) | 20g BCAA/day for 4 weeks | No significant impairment of glucose metabolism during OGTT; mixed effects on inflammatory markers. | [24] |
| High-Fat Diet Fed Mice | High BCAA Diet | Induced obesity, insulin resistance, and pro-inflammatory M1 macrophage polarization in adipose tissue. | [22] [23] |
| High-Fat Diet Fed Mice | BCAA Supplementation | Activated IFNGR1/JAK1/STAT1 pathway in adipose tissue macrophages. | [22] [23] |
{4 Detailed Experimental Protocols} To facilitate replication and further investigation, here are detailed methodologies from key studies cited.
4.1 Acute BCAA Infusion and Metabolic Phenotyping in Mice [20]
- Animals: 3-month-old C57Bl/6J mice.
- Catheter Implantation: Jugular vein catheterization under isoflurane anesthesia for precise intravenous infusions and blood sampling.
- Acute Interventions:
- BCAA Group: A single infusion of 2.25 mmole/kg BW BCAAs (in a 2:1:1 ratio of Leu:Ile:Val) prepared in 150 mM saline.
- BT2 Group: A single intraperitoneal injection of BT2 (3,6-dichlorobenzo[b]thiophene-2-carboxylic acid; 4 mg/mL) to acutely lower circulating BCAA levels.
- Metabolic Assessments:
- Frequent Blood Sampling: Via jugular catheter to monitor acute changes in blood glucose and plasma insulin.
- Hyperinsulinemic-Euglycemic Clamp: The gold-standard method for assessing whole-body insulin sensitivity. BCAAs were constantly infused during the clamp to evaluate their direct impact on insulin-stimulated glucose disposal.
- Glucose Tolerance Test (GTT): Performed to assess glycemic control.
4.2 Investigating Adipose Tissue Macrophage Polarization [22] [23]
- Animal Model: C57BL/6J male mice divided into:
- Standard Chow (STC)
- High-Fat Diet (HFD)
- High BCAA Diet (Teklad-based diet with 150% added BCAA)
- Duration: 16 weeks.
- Tissue Collection & Analysis:
- Subcutaneous White Adipose Tissue (sWAT) was collected.
- Histology & Immunostaining: Tissues were sectioned and stained with H&E and antibodies against TNF-α, IL-1β, and MCP-1 to quantify inflammation.
- ELISA: Adipose tissue homogenates were analyzed using commercial kits to quantify TNF-α, IL-1β, and MCP-1 protein levels.
- RNA-Sequencing & Pathway Analysis: ATMs were isolated from STC and High BCAA-fed mice. Transcriptomic analysis identified the INFGR1/JAK1/STAT1 pathway. Targeted gene silencing of IFNGR1 was used for mechanistic validation in vitro.
{5 The Scientist's Toolkit: Key Research Reagents} The following table compiles essential materials and tools for designing experiments in this field.
Table 3: Essential Research Reagents for BCAA and Insulin Resistance Studies
| Reagent / Material | Function / Application | Example & Context |
|---|---|---|
| Defined Amino Acid Diets | To precisely control dietary intake of individual BCAAs and study their specific metabolic effects. | Diets with 67% reduction in all BCAAs, isoleucine, valine, or leucine, as used in [21]. |
| Pharmacological BCAA-Lowering Agent (BT2) | An inhibitor of BCKDH kinase (BDK), which promotes BCAA catabolism. Used to acutely reduce circulating BCAA levels. | 3,6-dichlorobenzo[b]thiophene-2-carboxylic acid; administered via i.p. injection [20]. |
| DREADD Systems (Chemogenetics) | For precise neuronal manipulation to study brain-periphery communication in metabolism. | AAV8-hSyn-DIO-hM3D(Gq)-mCherry injected into the mediobasal hypothalamus to activate AgRP neurons [20]. |
| Jugular Vein Catheters | Enables repeated intravenous infusions, precise compound delivery, and frequent blood sampling in rodent models. | Used for acute BCAA infusion and frequent sampling in mice [20]. |
| ELISA Kits (Cytokines) | To quantify protein levels of pro-inflammatory cytokines in tissues or plasma. | Commercial kits for TNF-α, IL-1β, and MCP-1 (e.g., from R&D Systems) used on adipose tissue homogenates [23]. |
| Antibodies for Immunostaining | For spatial localization and quantification of specific proteins (e.g., inflammatory markers) in tissue sections. | Anti-TNF-α, anti-IL-1β, anti-MCP-1 antibodies (e.g., from Abcam) for immunohistochemistry in adipose tissue [23]. |
{6 Conclusion and Research Directions} The evidence unequivocally demonstrates that BCAAs are not merely passive biomarkers but active players in metabolic health, with their effects critically dependent on temporal exposure and metabolic context. The paradox is resolved by understanding that acute, postprandial signaling is essential for anabolism, while chronic elevation—often driven by an obesogenic environment and impaired catabolism—triggers inflammatory pathways and disrupts insulin action. Future research must focus on:
- Translating the distinct roles of isoleucine, valine, and leucine into targeted dietary or pharmacological interventions.
- Elucidating the precise communication mechanisms between adipose tissue inflammation, the central nervous system, and peripheral insulin sensitivity.
- Validating the IFNGR1/JAK1/STAT1 pathway as a therapeutic target in human metabolic disease.
Understanding the BCAA paradox is fundamental to advancing the broader thesis of how dietary proteins and amino acids orchestrate glucose homeostasis, offering a clear path from basic mechanism to therapeutic application.
Mitochondrial biogenesis is a critical adaptive process that ensures cellular energy homeostasis, with the peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α) serving as its master regulator. This whitepaper examines the intricate regulatory network controlling PGC-1α activity, with particular emphasis on its modulation by SIRT1 deacetylation and the emerging role of amino acid metabolism. Within the context of dietary influences on glucose homeostasis, we explore how nutrient-sensing pathways converge on mitochondrial function. The document provides a technical resource for researchers, featuring synthesized quantitative data, experimental methodologies, and visual signaling pathways, to advance therapeutic strategies targeting mitochondrial dysfunction in metabolic diseases.
PGC-1α is a transcriptional coactivator identified as a central regulator of mitochondrial biogenesis and function [25]. It does not directly bind DNA but serves as a docking platform that interacts with numerous transcription factors to coordinate the expression of nuclear and mitochondrial genes encoding oxidative phosphorylation components [25] [26]. PGC-1α is highly expressed in metabolically active tissues—including liver, kidney, skeletal muscle, brain, and adipose tissue—where it upregulates respiratory gene expression in response to environmental stimuli such as fasting, exercise, and cold exposure [25]. Through its regulation of oxidative phosphorylation, fatty acid metabolism, and reactive oxygen species defense, PGC-1α represents a crucial nodal point integrating environmental signals with mitochondrial lifecycle and energy production.
Molecular Structure and Regulatory Mechanisms of PGC-1α
Structural Domains and Functional Motifs
The human PGC-1α protein consists of 798 amino acids with a molecular weight of 91 kDa and contains several functionally distinct regions [25]:
- Activation Domain: Located at the N-terminal region, contains LXXLL leucine-rich motifs that facilitate interaction with nuclear receptors.
- Inactivation Domain: Adjacent to the activation domain, regulates coactivator activity.
- Serine/Arginine-rich (RS) Domain: Involved in RNA splicing.
- RNA Recognition Motif (RRM): Typical of proteins involved in RNA processing.
The structural organization enables PGC-1α to interact with diverse transcription factors including PPARα, estrogen receptor, NRF-1, and NRF-2, thereby exerting pleiotropic effects on cellular metabolism [25]. The C-terminal functional region participates in mRNA processing, with mutations in RS and RRM motifs impairing PGC-1α's ability to interact with transcription factors and regulate gene transcription [25].
Transcriptional and Post-translational Regulation
PGC-1α is regulated at multiple levels through complex mechanisms:
Transcriptional Control: PGC-1α gene expression is upregulated by transcription factors including CREB, FoxO1, MEF2, and ATF2 in response to various stimuli [25]. Multiple promoter regions and alternative splicing generate several PGC-1α protein variants, with newly discovered isoforms (PGC-1α-b and PGC-1α-c) showing heightened responsiveness to stimulation such as exercise [25].
Post-translational Modifications: PGC-1α undergoes extensive regulation via acetylation, phosphorylation, methylation, and ubiquitination [25]. Key regulatory kinases include AMPK, MAPK, Akt, S6 kinase, and GSK3β, which modulate PGC-1α's transcriptional activity and stability in response to cellular energy status [25].
Table 1: Key Regulators of PGC-1α Activity
| Regulator | Effect on PGC-1α | Activating Stimuli | Functional Outcome |
|---|---|---|---|
| AMPK | Phosphorylation at Thr177 and Ser538 | Increased AMP/ATP ratio, Ca2+ | Enhanced transcriptional activity and stability |
| SIRT1 | Deacetylation | Increased NAD+ levels, fasting | Modulates coactivator function |
| p38 MAPK | Phosphorylation | Stress, exercise | Increased protein stability |
| AKT | Phosphorylation | Insulin signaling | Modulates activity |
| NF-κB | Represses expression and activity | Inflammation | Downregulates antioxidant genes |
The SIRT1-PGC-1α Signaling Axis
Molecular Interrelationships
SIRT1, an NAD+-dependent deacetylase, functions as a critical metabolic sensor that directly deacetylates PGC-1α, modulating its transcriptional activity [27] [28]. This deacetylation enables PGC-1α to promote mitochondrial biogenesis and oxidative metabolism, particularly during nutrient deprivation [27]. The SIRT1-PGC-1α axis represents a fundamental mechanism linking cellular energy status to mitochondrial function, as SIRT1 activation increases with higher NAD+ levels during fasting or caloric restriction [26].
However, research reveals complex and sometimes contradictory aspects of this relationship. Some studies indicate that SIRT1-mediated deacetylation actually decreases PGC-1α coactivator activity and reduces mitochondrial content, suggesting context-dependent effects [28]. The metabolic outcomes of SIRT1 activation appear to depend on tissue type, physiological context, and experimental conditions.
AMPK as a Crucial Intermediate
AMPK serves as an essential intermediary in SIRT1-PGC-1α signaling. SIRT1 deacetylates LKB1, promoting its translocation to the cytoplasm where it activates AMPK [29]. Conversely, AMPK can enhance NAD+ biosynthesis, thereby activating SIRT1 [29]. This reciprocal regulation creates a feed-forward loop that amplifies mitochondrial biogenesis during energy deficit.
Research with SIRT1 activator SRT1720 demonstrates that its metabolic effects require AMPK activation, which occurs through inhibition of cAMP-degrading phosphodiesterases in a SIRT1-independent manner [29]. This finding suggests that SIRT1 activation and AMPK signaling represent parallel pathways that converge on PGC-1α to regulate mitochondrial function.
Figure 1: SIRT1-AMPK-PGC-1α Signaling Network. This diagram illustrates the complex interplay between SIRT1 and AMPK in regulating PGC-1α activity. Solid arrows indicate direct activation; dashed arrows represent indirect effects.
Amino Acids and Mitochondrial Biogenesis: Implications for Glucose Homeostasis
Nutrient Signaling Pathways
Amino acids influence mitochondrial biogenesis through multiple mechanisms that intersect with PGC-1α signaling:
mTOR Activation: Specific blends of essential amino acids, particularly those enriched in branched-chain amino acids (BCAAs), activate mTOR signaling, increasing mitochondrial biogenesis in skeletal muscle and hippocampus [30]. This enhanced mitochondrial function correlates with improved physical and cognitive performance in aging models.
Nitric Oxide Modulation: Certain amino acid mixtures improve mitochondrial biogenesis by increasing endothelial nitric oxide synthase (eNOS) expression [31]. Nitric oxide functions as a key signaling molecule in mitochondrial-nuclear communication, with chronic low-grade NO stimulation promoting mitochondrial biogenesis.
Metabolic Substrate Provision: Amino acid metabolism provides critical intermediates for the TCA cycle, supporting oxidative phosphorylation [30]. Aspartate and arginine synthesis depends directly on respiratory chain activity, creating a direct link between amino acid availability and mitochondrial function.
Integration with Glucose Metabolism
The connection between amino acid metabolism, mitochondrial biogenesis, and glucose homeostasis represents a crucial interface for metabolic health. Enhanced mitochondrial capacity in insulin-sensitive tissues promotes oxidative glucose disposal and improves whole-body glucose tolerance [32]. SIRT1 activation in brown adipose tissue enhances glucose uptake and thermogenesis, contributing to improved systemic glucose homeostasis independent of weight loss [29] [32].
Table 2: Amino Acid-Mediated Effects on Mitochondrial Function
| Mechanism | Key Amino Acids | Signaling Pathways | Metabolic Outcomes |
|---|---|---|---|
| mTOR Activation | Branched-chain amino acids (Leucine, Isoleucine, Valine) | mTORC1 signaling | Increased mitochondrial biogenesis in muscle and brain |
| Nitric Oxide Production | Arginine, Citrulline | eNOS expression | Enhanced mitochondrial biogenesis |
| TCA Cycle Anaplerosis | Glutamine, Aspartate | Metabolic intermediate supply | Supported oxidative phosphorylation |
| GCN2 Sensing | Multiple essential amino acids | eIF2α phosphorylation | Adaptation to amino acid deficiency |
Experimental Approaches and Research Methodologies
Assessing Mitochondrial Biogenesis and Function
Gene and Protein Expression Analysis:
- Real-time PCR: Quantify PGC-1α, TFAM, NRF1, and mitochondrial gene expression [33].
- Western Blotting: Detect PGC-1α protein levels and acetylation status using specific antibodies [27] [28].
- Chromatin Immunoprecipitation (ChIP): Validate direct binding of PGC-1α to promoter regions of mitochondrial dynamics genes (e.g., DRP1) [33].
Functional Mitochondrial Assessment:
- Seahorse XF Analyzer: Measure oxygen consumption rate (OCR) to determine basal respiration, ATP production, maximal respiratory capacity, and spare respiratory capacity [33].
- Flow Cytometry with Mitochondrial Dyes: Use MitoSOX for mitochondrial superoxide, DiOC6(3) for membrane potential, and propidium iodide for cell death assessment [33].
- ATP Production Assays: Quantify mitochondrial ATP generation using luciferase-based methods [27].
Modulating SIRT1-PGC-1α Signaling
Pharmacological Tools:
- SIRT1 Activators: SRT1720 (5-30 mg/kg in vivo, 5 μM in vitro) [29], SCIC2.1 (25 μM in vitro) [27], Resveratrol (variable effects, 1.56±0.28 μM plasma concentration in rats) [28].
- SIRT1 Inhibitors: EX-527 (5 μM in vitro) effectively blocks SIRT1 activity [27].
- AMPK Activators: AICAR and metformin indirectly influence PGC-1α activity.
Genetic Manipulations:
- Overexpression: Lentiviral or adenoviral delivery of SIRT1 or PGC-1α to enhance expression [28].
- Knockdown Approaches: siRNA/shRNA-mediated knockdown to investigate loss-of-function effects [28] [33].
- Transgenic Models: Muscle-specific SIRT1 knockout mice and AMPKα2 knockout models [29].
Figure 2: Experimental Workflow for Investigating SIRT1-PGC-1α Signaling. This diagram outlines a comprehensive approach to studying mitochondrial biogenesis, incorporating molecular and functional assessments.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating SIRT1-PGC-1α Signaling
| Reagent/Cell Line | Application | Key Features | Experimental Use |
|---|---|---|---|
| C2C12 Myotubes | In vitro muscle metabolism model | Differentiate from myoblasts to myotubes | Study exercise-mimetic effects [28] |
| HepG2 Cells | Hepatocellular carcinoma model | High metabolic activity | Investigate liver metabolism and cancer [27] |
| N27 Dopaminergic Cells | Neuronal mitochondrial function | Dopaminergic neuronal origin | Study neurotoxicity and protection [33] |
| SRT1720 | SIRT1 activator | Also inhibits PDEs and activates AMPK | 5-30 mg/kg in vivo, 5 μM in vitro [29] |
| EX-527 | SIRT1 inhibitor | Specific SIRT1 inhibition | 5 μM in vitro [27] |
| SCIC2.1 | SIRT1 activator | Promotes PGC-1α deacetylation | 25 μM in vitro [27] |
| AMPKα2 KO Mice | AMPK deficiency model | AMPKα2 isoform knockout | Determine AMPK-dependent effects [29] |
| Muscle-Specific SIRT1 KO | Tissue-specific SIRT1 deletion | Conditional knockout using Pax7-Cre | Study muscle-specific SIRT1 functions [29] |
Discussion and Research Implications
The regulatory network comprising PGC-1α, SIRT1, and AMPK represents a sophisticated system for maintaining energy homeostasis through mitochondrial biogenesis and functional adaptation. The emerging understanding of amino acid modulation of these pathways provides new insights into nutrient-sensing mechanisms that could be leveraged for therapeutic interventions.
Future research should address several critical questions: How do different amino acid profiles specifically modulate PGC-1α acetylation status? What explains the contradictory findings regarding SIRT1's effects on PGC-1α activity in different tissue contexts? How can tissue-specific modulation of these pathways be achieved for therapeutic benefit in metabolic diseases?
The integration of dietary protein and amino acid metabolism into the SIRT1-PGC-1α signaling framework offers promising avenues for developing nutritional and pharmacological approaches to improve glucose homeostasis through enhanced mitochondrial function. Particular promise lies in designing specific amino acid formulations that optimize mitochondrial biogenesis without overactivating detrimental pathways such as excessive mTOR signaling.
PGC-1α stands as the master regulator of mitochondrial biogenesis, integrating signals from nutrient sensors including SIRT1 and AMPK to coordinate cellular energy production with metabolic demand. The SIRT1-PGC-1α axis represents a crucial target for interventions aimed at improving mitochondrial function and glucose homeostasis. As research continues to elucidate the complex interactions between amino acid metabolism, nutrient signaling, and mitochondrial regulation, new opportunities emerge for addressing metabolic diseases through targeted activation of mitochondrial biogenesis pathways. The experimental methodologies and research tools outlined in this document provide a foundation for advancing our understanding of these critical regulatory mechanisms.
While dietary protein provides carbon skeletons that can be converted into glucose via gluconeogenesis, this process contributes minimally to circulating glucose levels in healthy individuals. This whitepaper examines the hepatic autoregulatory mechanisms that tightly control this process, drawing on stable isotope tracer studies, hormonal regulation research, and molecular pathway analyses. We synthesize findings demonstrating that only 4-10g of glucose enters circulation from 50g protein ingestion over 8 hours, despite theoretical potential for 25g glucose production. The clinical implications for diabetes management and drug development are substantial, as understanding these regulatory mechanisms may reveal novel therapeutic targets for controlling hepatic glucose production in metabolic disease.
The relationship between dietary protein and circulating glucose represents a significant paradox in metabolic physiology. On one hand, the carbon skeletons of most amino acids can be converted into glucose through gluconeogenic pathways [34]. Early 20th century investigations by Janney (1915) demonstrated that deaminated amino acids from dietary proteins could indeed produce glucose [34]. Subsequent research confirmed that 50-80g of glucose could theoretically be derived from 100g of ingested protein [34].
However, contrary to this theoretical potential, empirical observations consistently show minimal impact on blood glucose concentrations following protein ingestion. As early as 1913, Jacobson reported that ingestion of proteins did not raise blood glucose [34]. Later, MacLean (1924) found that feeding 50g of meat protein to subjects with and without mild diabetes produced no change in blood glucose, despite the theoretical production of 25g of glucose [34]. This discrepancy between theoretical potential and observed outcomes forms the core of the protein-glucose paradox that has persisted in metabolic research for over a century.
This whiteppaper examines the molecular mechanisms, regulatory pathways, and experimental evidence underlying hepatic autoregulation that resolves this paradox, with particular emphasis on implications for metabolic disease research and therapeutic development.
Quantitative Evidence: Minimal Glucose Release from Dietary Protein
Multiple controlled metabolic studies employing tracer methodologies have quantified the actual glucose appearance from dietary protein, consistently demonstrating minimal contribution to circulating glucose.
Table 1: Quantitative Studies of Glucose Appearance from Dietary Protein
| Study Population | Protein Source & Amount | Study Duration | Theoretical Glucose Potential | Actual Glucose Appearance | Citation |
|---|---|---|---|---|---|
| Normal young subjects | 50g cottage cheese protein (casein) | 8 hours | ~25g | 9.7g | [34] |
| People with untreated T2D | 50g beef protein | 8 hours | ~25g | 2.0g | [34] |
| Healthy subjects | 23g egg protein | 8 hours | Not specified | 4.0g | [34] |
The striking disparity between theoretical potential and measured glucose appearance is consistent across study populations and protein sources. In the egg protein study, only 4g (8%) of the total 50g glucose entering circulation over 8 hours could be attributed to the ingested protein, despite 79% of the ingested protein being deaminated and thus making carbon skeletons available for gluconeogenesis [34].
The hepatic autoregulatory process responsible for this minimal glucose release operates independently of changes in circulating insulin or glucagon concentrations [34]. This autonomous hepatic regulation represents a crucial homeostatic mechanism that maintains glucose stability despite varying protein intake.
Molecular Mechanisms of Hepatic Autoregulation
The liver employs multiple sophisticated regulatory strategies to prevent excessive glucose release from dietary protein, involving substrate partitioning, allosteric regulation, and transcriptional control.
Substrate Partitioning and Oxidation
The fate of amino acid carbon skeletons after deamination is preferentially directed toward oxidation rather than gluconeogenesis. In the egg protein study, the majority of deaminated amino acid carbon appeared as CO₂, indicating direct oxidation as fuel rather than conversion to glucose [34]. This substrate partitioning ensures that amino acids are primarily utilized for energy production or protein synthesis rather than gluconeogenesis.
The regulatory mechanisms controlling the partitioning of food-derived amino acids between new protein synthesis, deamination, direct oxidation, and conversion to glucose remain incompletely understood but represent a critical area for future research and potential therapeutic intervention [34].
The Glucagon-Ureagenesis Axis
Glucagon plays a dual role in regulating both glucose and amino acid metabolism, creating a feedback loop known as the liver-alpha cell axis [35].
Diagram 1: Glucagon-mediated ureagenesis in amino acid metabolism
This axis functions as a complete feedback loop: amino acids stimulate glucagon secretion, which enhances hepatic amino acid clearance through ureagenesis, thereby reducing circulating amino acids and subsequent glucagon stimulation [35]. Disruption of this axis occurs in hepatic steatosis, where impaired glucagon receptor signaling and reduced expression of amino acid catabolism genes (Cps1, Slc7a2, Slc38a2) diminish ureagenic capacity [35].
Allosteric and Transcriptional Control
Hepatic glucose metabolism is regulated through both allosteric control and transcriptional mechanisms:
- Allosteric regulation: Key glycolytic and gluconeogenic enzymes are regulated by metabolic intermediates including ATP, citrate, fructose-2,6-bisphosphate, and acetyl-CoA [36]
- Transcriptional control: Transcription factors including EPAS1 (HIF2α) regulate the expression of genes involved in both glucose and lipid metabolism pathways [37]
- Hepatic zonation: Heterogeneous distribution of metabolic enzymes across liver lobules creates specialized compartments for glycolytic and gluconeogenic processes
The transcription factor EPAS1 plays a particularly important role as a master regulator that coordinates glucose and lipid metabolic pathways in response to oxygen availability [37].
Key Experimental Approaches and Methodologies
Research elucidating hepatic autoregulation has employed sophisticated experimental designs and tracer methodologies.
Stable Isotope Tracer Protocols
The definitive studies quantifying glucose appearance from protein utilized stable isotope tracers with detailed protocols:
Diagram 2: Multitracer experimental workflow for protein metabolism
This sophisticated approach allows simultaneous tracking of both the amino moiety and carbon skeletons of dietary amino acids, providing comprehensive data on their metabolic fates [34]. The multitracer technology enables precise quantification of glucose production from all sources and attribution of specific portions to dietary protein.
Glucagon Signaling Manipulation Studies
Research on the liver-alpha cell axis has employed multiple interventional approaches:
Table 2: Experimental Approaches to Study Glucagon-Amino Acid Metabolism
| Experimental Approach | Model System | Key Findings | Research Implications |
|---|---|---|---|
| Glucagon receptor antagonist (GRA) | Mice | Reduced amino acid clearance and urea formation | Confirms glucagon dependence of amino acid catabolism |
| Diphtheria toxin α-cell ablation | Transgenic mice | Impaired ureagenesis restored by glucagon administration | Demonstrates necessity of α-cells for amino acid homeostasis |
| Primary hepatocyte studies | Human and mouse hepatocytes | Glucagon increases urea formation within minutes | Reveals direct hepatic action mechanism |
| Transcriptomic analysis | Liver tissue from GRA-treated mice | Downregulation of Cps1, Slc7a2, Slc38a2 | Identifies key regulated genes in amino acid metabolism |
These complementary approaches establish both necessity (through loss-of-function experiments) and sufficiency (through agonist administration) of glucagon signaling for appropriate amino acid clearance and ureagenesis.
Research Reagent Solutions Toolkit
Table 3: Essential Research Reagents for Hepatic Amino Acid Metabolism Studies
| Reagent/Category | Specific Examples | Research Applications | Key Function in Experimental Design |
|---|---|---|---|
| Stable isotope tracers | ¹³C, ¹⁵N-labeled amino acids; ²H-glucose | Glucose flux studies; Amino acid oxidation measures | Metabolic pathway tracing; Flux quantification |
| Hormone modulators | Glucagon receptor antagonists; Recombinant glucagon | Signal transduction studies; Pathway necessity/sufficiency tests | Specific pathway manipulation; Receptor function analysis |
| Animal models | Glucagon receptor KO; α-cell ablation models; "Falconized" EPAS1 mice | In vivo physiology studies; Genetic pathway analysis | Whole organism physiology; Genetic mechanism studies |
| Protein sources | Intrinsically labeled egg protein; Casein; Beef protein | Substrate-specific metabolism studies | Controlled dietary protein delivery |
| Analytical platforms | UPLC-MS/MS; GC-MS; Metabolic cages | Metabolite quantification; Substrate oxidation measures | Precise metabolite measurement; Whole-body energy substrate use |
This toolkit enables comprehensive investigation of hepatic amino acid metabolism from molecular mechanisms to whole-body physiology.
Implications for Metabolic Disease and Therapeutic Development
Understanding hepatic autoregulation of glucose production from protein has significant implications for metabolic disease management and drug development.
Hepatic Steatosis and Metabolic Dysregulation
NAFLD and hepatic steatosis impair glucagon-dependent enhancement of amino acid catabolism [35]. Patients with NAFLD exhibit hyperglucagonemia and increased levels of glucagonotropic amino acids, particularly alanine [35]. The disruption of the liver-alpha cell axis in hepatic steatosis creates a pathological cycle: impaired hepatic amino acid clearance leads to elevated circulating amino acids, which stimulates glucagon secretion, but the liver cannot respond appropriately due to insulin resistance and steatosis [35] [38].
This pathophysiology may contribute to the progression from NAFLD to type 2 diabetes, as chronic hyperaminoacidemia and hyperglucagonemia can promote metabolic dysfunction. Diet-induced reduction in HOMA-IR (a marker of hepatic steatosis) reduces both glucagon and alanine levels, highlighting the potential for therapeutic intervention [35].
Protein-Sparing Therapies and Diabetes Management
The understanding that dietary protein contributes minimally to circulating glucose supports current dietary approaches for diabetes management that emphasize adequate protein intake without significant concern for direct glycemic impact. However, the impaired amino acid clearance in hepatic steatosis suggests that hepatic autoregulatory capacity may be compromised in metabolic disease.
Emerging therapeutic approaches targeting the glucagon signaling pathway, including glucagon receptor antagonists and glucagon-like peptide-1 receptor agonists, may exert part of their beneficial effects through modulation of amino acid metabolism and restoration of hepatic autoregulatory function [35] [38].
Hepatic autoregulation ensures that dietary protein contributes minimally to circulating glucose through integrated mechanisms including substrate partitioning, glucagon-mediated ureagenesis, and allosteric control of metabolic enzymes. The resolution of the protein-glucose paradox represents a significant advancement in our understanding of metabolic integration.
Future research should focus on:
- Elucidating the precise signals and mechanisms that partition amino acid carbon skeletons between oxidation, gluconeogenesis, and other metabolic fates
- Developing targeted therapies that enhance hepatic autoregulatory capacity in metabolic disease
- Investigating the role of hepatic zonation in compartmentalizing amino acid metabolism
- Exploring the potential of dietary protein manipulation to modulate hepatic autoregulation for therapeutic benefit
These research directions promise to yield novel insights into liver physiology and new therapeutic approaches for metabolic diseases characterized by dysregulated hepatic glucose production.
Applied Nutritional Strategies: High-Protein Diets and Amino Acid Supplementation in Metabolic Health
Hypocaloric High-Protein Diets for Weight Loss and Insulin Sensitivity Improvement
Hypocaloric high-protein diets represent a significant evolution in nutritional science, offering a dual-targeted approach for managing obesity and metabolic syndrome. Defined as diets providing >30% of total energy from protein or >1.2 g/kg/day while maintaining a caloric deficit, these diets have demonstrated efficacy not only for weight reduction but also for fundamental improvements in metabolic regulation [39] [40]. The therapeutic potential of hypocaloric high-protein diets extends beyond simple weight management to address core pathophysiological mechanisms in insulin resistance and type 2 diabetes mellitus.
The scientific rationale for high-protein diets is anchored in the unique metabolic properties of dietary proteins and their constituent amino acids. Branched-chain amino acids, particularly leucine, function as critical nutrient signaling molecules that influence glucose homeostasis through both central and peripheral mechanisms [40]. This review synthesizes current evidence from clinical trials, mechanistic studies, and population research to provide a comprehensive technical assessment of hypocaloric high-protein diet implementation, outcomes, and underlying biological pathways for research and drug development applications.
Quantitative Clinical Outcomes of Hypocaloric High-Protein Diets
Body Composition and Metabolic Changes
Table 1: Body Composition Changes Following Hypocaloric High-Protein vs. Conventional Diets
| Parameter | High-Protein Diet | Conventional Diet | P-value | Study Duration | Citation |
|---|---|---|---|---|---|
| Weight Loss (kg) | -8.9 ± 4.6 kg | -10.0 ± 9.4 kg | >0.05 | 3 months | [41] |
| Fat-Free Mass Preservation | -1.5 ± 1.6 kg | -4.4 ± 4.2 kg | <0.01 | 3 months | [41] |
| Fat-Free Mass Index | -0.7 ± 1.1 kg/m² | -2.1 ± 1.9 kg/m² | <0.01 | 3 months | [41] |
| Body Fat Percentage | -5.3 ± 3.3% | -3.2 ± 4.5% | <0.05 | 3 months | [41] |
| Fat Mass Reduction | -7.53 ± 1.44 kg | -6.96 ± 1.36 kg | Not significant | 10 weeks | [17] |
Table 2: Metabolic Parameter Changes in Hypocaloric High-Protein Diet Interventions
| Metabolic Parameter | High-Protein Diet Effect | Comparison Condition | Study Population | Citation |
|---|---|---|---|---|
| Glucose Disposal | Significant increase | Significant decrease | Obese women | [42] |
| Glucose Oxidation | Significant increase | Significant decrease | Obese women | [42] |
| Postprandial Insulin Response | 75 ± 18 pmol/L | 207 ± 21 pmol/L | Adult women with overweight | [17] |
| Fasting Blood Glucose | Stabilized | Reduced | Adult women with overweight | [17] |
| HbA1c Reduction | Significant improvement | Moderate improvement | T2DM patients | [39] |
| 3-Methylhistidine Excretion | Reduced by 48% | Unchanged | Obese women | [42] |
Clinical evidence consistently demonstrates that while weight loss outcomes between hypocaloric high-protein and conventional diets may be similar, high-protein diets confer superior body composition outcomes by preferentially preserving metabolically active fat-free mass [41]. This preservation is critically important for maintaining resting energy expenditure during weight loss and has long-term implications for weight maintenance. The reduction in 3-methylhistidine excretion, a marker of muscle protein breakdown, provides biochemical evidence for the protein-sparing effects of high-protein diets during caloric restriction [42].
Beyond body composition, hypocaloric high-protein diets induce favorable changes in glucose metabolism and insulin sensitivity. Research indicates significant improvements in glucose disposal and oxidation rates under hyperinsulinemic clamp conditions, suggesting enhanced tissue-level insulin sensitivity [42]. The substantial reduction in postprandial insulin response observed in high-protein diets indicates improved pancreatic β-cell function and reduced insulin demand, which may have long-term benefits for preserving pancreatic function in individuals with insulin resistance [17].
Mechanisms of Action: Protein and Amino Acid Signaling in Glucose Homeostasis
Central and Peripheral Signaling Pathways
The metabolic benefits of hypocaloric high-protein diets are mediated through multiple interconnected biological pathways. Understanding these mechanisms provides insights for developing targeted nutritional interventions and pharmacological approaches.
Diagram 1: Integrated signaling pathways of high-protein diets and amino acids in glucose homeostasis
The mechanisms by which hypocaloric high-protein diets improve insulin sensitivity involve complex nutrient-sensing pathways across multiple tissues. As illustrated in Diagram 1, branched-chain amino acids, particularly leucine, serve as critical signaling molecules that access the medio-basal hypothalamus through fenestrated capillaries in the arcuate nucleus [40]. Within hypothalamic neurons, leucine metabolism generates oleoyl-CoA, which activates ATP-sensitive potassium channels, initiating vagal signals to the liver that suppress hepatic glucose production through inhibition of gluconeogenesis and glycogenolysis [40].
Concurrently, high-protein diets influence incretin secretion and pancreatic function. Protein and amino acid ingestion stimulates release of glucagon-like peptide-1 and glucose-dependent insulinotropic polypeptide from intestinal L-cells, enhancing glucose-dependent insulin secretion while suppressing glucagon release [40]. This entero-endocrine axis activation contributes to the improved postprandial glycemic control observed with high-protein diets without excessive insulin secretion.
At the intestinal level, protein hydrolysates and bioactive peptides directly modulate glucose absorption capacity. In vitro and ex vivo studies demonstrate that digested proteins from various sources reduce glucose transport across intestinal epithelium by downregulating GLUT2 transporter expression [43]. This mechanism represents a direct interface between dietary protein and carbohydrate absorption, potentially contributing to the flattened glycemic curves observed with high-protein meals.
The BCAA Paradox in Insulin Resistance
The relationship between branched-chain amino acids and insulin sensitivity presents a complex paradox that requires careful consideration in research and clinical application. While acute administration of BCAAs demonstrates insulin-sensitizing effects through the mechanisms described above, chronically elevated circulating BCAA levels are strongly associated with insulin resistance and increased type 2 diabetes risk in observational studies [44].
This apparent contradiction may be explained by differences in temporal exposure and metabolic context. Chronic elevation of BCAAs, often associated with obesity and metabolic syndrome, may reflect impaired BCAA catabolism rather than solely increased dietary intake [44]. Dysfunctional BCAA catabolism in adipose tissue and skeletal muscle leads to accumulation of metabolic intermediates that activate mTOR-S6K1 signaling, promoting serine phosphorylation of IRS-1 and subsequent insulin receptor substrate degradation [45]. This negative feedback loop represents a fundamental mechanism through which chronic BCAA elevation induces insulin resistance.
The source of dietary protein significantly influences this paradoxical relationship. Plant-based proteins, particularly when consumed with high fiber content, demonstrate attenuated association with diabetes risk compared to animal proteins [46] [6]. This protective effect may be mediated through modified digestion kinetics, differential amino acid composition, or concomitant phytochemical intake that modulates BCAA metabolism.
Experimental Models and Research Methodologies
Key Research Protocols
Table 3: Standardized Experimental Protocols for High-Protein Diet Research
| Methodology | Protocol Specifications | Key Measurements | Applications | Citation |
|---|---|---|---|---|
| Euglycemic Hyperinsulinemic Clamp | 25 mU/kg/h insulin for 150 min + indirect calorimetry | Glucose disposal rate, glucose oxidation, lipid oxidation | Gold standard for insulin sensitivity assessment | [42] |
| INFOGEST Gastrointestinal Digestion | 2g protein in SSF (pH 7, 5 min) → SGF + pepsin (pH 3, 2h) → SIF + pancreatin (pH 7, 2h) | Bioactive peptide generation, amino acid composition | Simulation of protein digestion and metabolite release | [43] |
| Caco-2/TC7 Cell Glucose Uptake | 14C-AMG uptake after 1h pre-incubation with digested proteins (5 mg/ml) | Radioactive glucose analog transport, GLUT2/SGLT1 expression | Intestinal glucose absorption mechanisms | [43] |
| Ex Vivo Jejunal Sac Transport | 1cm rat jejunal sacs with 3H-D-[1-14C] glucose + digested proteins (31.25 mg/ml) | Serosal to mucosal glucose ratio | Validation of intestinal glucose transport findings | [43] |
| Body Composition Analysis | Multifrequency BIA (Inbody 720; 5, 50, 250, and 500 kHz) | Fat-free mass, fat mass, body fat percentage | Body composition changes in clinical trials | [41] |
The euglycemic hyperinsulinemic clamp represents the gold standard methodology for assessing whole-body insulin sensitivity in response to dietary interventions [42]. When combined with indirect calorimetry, this technique provides simultaneous assessment of glucose metabolism at the level of substrate utilization, differentiating between oxidative and non-oxidative glucose disposal. The standardization of this methodology across research centers enables direct comparison of protein-mediated effects on insulin sensitivity.
The INFOGEST static gastrointestinal digestion model provides a harmonized international protocol for simulating human digestion of dietary proteins [43]. This methodology generates protein hydrolysates and bioactive peptides that closely mimic the physiological products of digestion, enabling systematic investigation of structure-function relationships between protein sources and bioactivity. The protocol's standardization across laboratories facilitates reproducibility in protein research.
Cellular and ex vivo intestinal models enable mechanistic investigation of protein-glucose interactions at the absorption interface. The Caco-2/TC7 cell line, which spontaneously differentiates into enterocyte-like cells, provides a robust model for studying glucose transporter regulation and function [43]. When combined with ex vivo jejunal sac preparations, these models offer complementary approaches for validating findings across experimental systems.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Protein and Glucose Metabolism Studies
| Research Reagent | Specifications | Experimental Function | Application Context |
|---|---|---|---|
| Whey Protein Isolate | >90% protein content, rich in BCAAs | High-quality protein source for interventions | Clinical trials, meal replacement studies [41] |
| SGLT1 Inhibitor (Phlorizin) | 0.5 mM in cold PBS | Blocks sodium-glucose cotransporter | Validation of glucose transport mechanisms [43] |
| 14C-α-methyl-D-glucopyranoside | 0.2 μCi/ml in uptake assays | Non-metabolizable glucose analog | Measurement of glucose transporter activity [43] |
| Branched-Chain Amino Acids | L-Leucine, L-Isoleucine, L-Valine (commercial grade) | Signaling pathway activation studies | Mechanism dissection, dose-response studies [40] |
| Simulated Digestive Fluids | SSF, SGF, SIF according to INFOGEST | Standardized protein digestion | Generation of physiological protein hydrolysates [43] |
| Pepsin (Porcine) | 6500 U/mL in SGF, pH 3.0 | Gastric digestion phase enzyme | INFOGEST protocol implementation [43] |
| Pancreatin (Porcine) | 45 U/mL in SIF, pH 7.0 | Intestinal digestion phase enzyme | INFOGEST protocol implementation [43] |
The research reagents detailed in Table 4 represent essential tools for investigating the intersection of protein metabolism and glucose homeostasis. Whey protein isolate has emerged as a particularly valuable intervention protein source due to its high BCAA content, rapid digestion kinetics, and demonstrated efficacy in clinical trials [41]. Its use as a meal replacement component enables standardized protein delivery while controlling for other dietary variables.
Radiolabeled glucose analogs like 14C-α-methyl-D-glucopyranoside provide critical tools for quantifying glucose transporter activity without the confounding influence of subsequent metabolism [43]. When used with specific transporter inhibitors such as phlorizin, these reagents enable precise dissection of transport mechanisms contributing to overall glucose absorption.
The INFOGEST digestive enzyme consortium represents a standardized approach to generating physiologically relevant protein digests for mechanistic studies [43]. The use of enzymes from porcine sources provides the closest approximation to human digestive proteases available for in vitro systems, enhancing the translational potential of findings.
Clinical Translation and Research Gaps
Population Studies and Clinical Applications
Evidence from large-scale population studies reveals a complex relationship between dietary protein and diabetes risk that appears to contradict some intervention findings. Meta-analyses of prospective cohort studies indicate that high intake of total and animal protein is associated with increased type 2 diabetes incidence, while plant protein demonstrates a protective association [46] [6]. This apparent contradiction highlights the importance of considering protein sources, dietary patterns, and population context when interpreting research findings.
The relationship between protein intake and diabetes risk appears to follow a U-shaped association, with both insufficient and excessive intake associated with increased risk. Recent registry-based cohort data identified an optimal protective range of 12.20-16.85% of energy from protein, with a cut-point of approximately 15% energy [6]. This non-linear relationship may explain some of the apparent discrepancies between observational and intervention studies.
The metabolic context significantly modifies the relationship between protein intake and diabetes risk. Individuals with hypertension demonstrate a narrower optimal protein intake range, while those with NAFLD show a linear inverse relationship between protein intake and diabetes risk [6]. These differential associations highlight the need for personalized nutritional approaches based on individual metabolic phenotypes.
Future Research Directions
Despite substantial progress, several critical research gaps remain in understanding hypocaloric high-protein diets and their metabolic effects. The long-term sustainability and safety of high-protein diets require further investigation, particularly regarding renal function, bone health, and cancer risk in susceptible populations. The optimal protein source composition for different metabolic phenotypes remains undetermined, with conflicting evidence regarding animal versus plant protein superiority. The molecular mechanisms underlying the BCAA paradox require elucidation to reconcile the discordant findings between acute intervention studies and chronic observational data.
Additionally, the interaction between dietary protein, gut microbiota, and host metabolism represents an emerging frontier with significant implications for personalized nutrition. The development of biomarkers for predicting individual responses to high-protein interventions would represent a major advance in translational nutrition science. Finally, the integration of high-protein diets with pharmacological approaches for diabetes management requires systematic investigation to establish synergistic therapeutic protocols.
Hypocaloric high-protein diets represent an effective nutritional strategy for simultaneous weight management and improvement of insulin sensitivity. The therapeutic benefits of these diets are mediated through multiple complementary mechanisms, including preservation of metabolically active tissue, modulation of nutrient-sensing pathways, regulation of incretin secretion, and direct effects on intestinal glucose transport. The integration of clinical evidence with mechanistic insights provides a robust scientific foundation for implementing high-protein dietary approaches in research and clinical practice.
Future research directions should focus on personalizing protein recommendations based on metabolic phenotype, elucidating the long-term safety profile of high-protein diets, and exploring synergistic combinations with pharmacological agents. The continued investigation of protein-amino acid-glucose interactions will yield important insights for developing next-generation nutritional and therapeutic approaches for metabolic disease management.
Preservation of Fat-Free Mass and Mitigation of Sarcopenia during Caloric Restriction
Caloric restriction (CR) is a cornerstone intervention for weight loss and metabolic improvement. However, a significant consequence of CR is the loss of fat-free mass (FFM), particularly skeletal muscle, a condition known as sarcopenia. This loss is metabolically detrimental, as skeletal muscle is the largest organ responsible for insulin-stimulated glucose disposal, handling approximately 80% of postprandial glucose [2] [3]. The preservation of FFM during weight loss is therefore critical not only for maintaining physical function but also for systemic metabolic health, including glucose homeostasis. This whitepaper synthesizes current research on strategies to mitigate sarcopenia during CR, with a specific focus on the role of dietary proteins and amino acids, and provides a technical toolkit for researchers in the field.
Physiological Rationale: Muscle as a Metabolic Regulator
Skeletal muscle is not merely a contractile organ; it is a central hub for metabolic regulation. The loss of muscle mass during CR directly impairs glucose disposal capacity, which can paradoxically worsen insulin sensitivity in the long term despite initial improvements from weight loss [2]. Furthermore, during dietary-induced weight loss, 10–35% of the total weight lost can be skeletal muscle, which is particularly problematic for older adults, increasing the risk of frailty, morbidity, and mortality [2] [3].
The mechanisms underlying muscle loss during CR involve a reduction in energy demand and a lack of mechanical stress, leading to perturbations in mitochondrial lipid metabolism and an accumulation of glycogen and lipid intermediates that foster insulin resistance [2]. Counteracting these mechanisms requires targeted nutritional and exercise interventions that promote anabolic signaling and mitochondrial biogenesis.
Strategic Interventions for Mass Preservation
Dietary Protein and Amino Acid Supplementation
Increasing dietary protein intake during CR is a primary strategy for preserving FFM. The metabolic benefits are mediated through essential amino acids (EAAs), particularly leucine, which transiently activates the mammalian target of rapamycin complex 1 (mTORC1), a key regulator of muscle protein synthesis [2] [3].
- Efficacy of High-Protein Diets: Clinical trials demonstrate that hypocaloric high-protein diets (e.g., providing 35% of calories from protein) promote significantly greater retention of fat-free mass and greater reductions in insulin resistance compared to standard-protein diets (e.g., 18% protein) [2] [3]. One study in obese, insulin-resistant women found that a high-protein diet (1.6 g/kg/day) led to a more stable fasting and postprandial blood glucose profile and a reduced postprandial insulin response compared to a high-carbohydrate diet (0.8 g/kg/day) [17].
- Role of Specific Amino Acids: The type of amino acid is crucial. While chronic postabsorptive elevations of branched-chain amino acids (BCAAs) have been associated with insulin resistance, postprandial elevations of EAAs, especially leucine, act as potent anabolic mediators [2]. Leucine and its metabolite, β-hydroxy-β-methylbutyrate (HMB), have been shown to promote mitochondrial function and muscle protein synthesis, even during periods of inactivity like bed rest [2]. Furthermore, higher intake of ketogenic amino acids like leucine and lysine is associated with a reduced risk of diabetic kidney disease, highlighting their protective potential in a comorbid population [47].
- Molecular Mechanisms: EAAs, particularly leucine, activate a signaling network involving mTORC1, Yin-Yang 1 (YY1), and peroxisome proliferator-activated receptor-gamma coactivator-1α (PGC-1α). This pathway works cohesively with nuclear respiratory factors (NRF-1,2) and sirtuins (SIRT1/3) to promote mitochondrial biogenesis. Enhanced mitochondrial function alleviates insulin resistance in skeletal muscle and reduces oxidative stress, thereby improving metabolic health [2] [3].
Table 1: Clinical Outcomes of High-Protein vs. Standard-Protein Hypocaloric Diets
| Parameter | High-Protein Diet (≈35% of kcal) | Standard-Protein Diet (≈18% of kcal) | Clinical Significance |
|---|---|---|---|
| Fat-Free Mass Retention | Significantly greater | Lesser | Preserves metabolic rate and functional capacity [2] |
| Fat Mass Loss | Accelerated | Standard | Improves body composition [2] |
| Insulin Resistance (HOMA-IR) | Two-fold greater reduction | Moderate reduction | Enhances systemic glucose homeostasis [2] [3] |
| Postprandial Insulin Response | Reduced (75 ± 18 pmol/L) | Elevated (207 ± 21 pmol/L) | Indicates improved insulin sensitivity [17] |
Exercise Modalities during Caloric Restriction
While nutrition is critical, exercise is a powerful synergistic intervention. A systematic review and network meta-analysis of 62 randomized controlled trials revealed that the combination of CR and exercise (CR+EX) is superior to CR alone for optimizing body composition [48].
The analysis ranked different exercise modalities based on their Surface Under the Cumulative Ranking (SUCRA) curve. The key findings are:
- Fat Mass Reduction: Low-intensity aerobic exercise (LA) and high-intensity aerobic exercise (HA) were most effective.
- Lean Body Mass Preservation: Resistance exercise was superior. Moderate-intensity mixed exercise (MM, combining aerobic and resistance) and moderate-intensity resistance exercise (MR) were the top-ranked interventions for preserving lean body mass, outperforming CR alone and all aerobic modalities [48].
This underscores that resistance training is non-negotiable for muscle preservation during a calorie deficit. The combination of moderate-intensity resistance or aerobic exercise with CR was concluded to be the optimal strategy for improving overall body composition [48].
Table 2: Efficacy Ranking of Exercise Modalities Combined with Caloric Restriction for Body Composition
| Intervention | Weight Reduction (Rank) | Fat Mass Reduction (Rank) | Lean Body Mass Preservation (Rank) | Recommended Application |
|---|---|---|---|---|
| High-Intensity Aerobic (HA) | 1 | 2 | 9 | Prioritize for maximal weight loss |
| Moderate-Intensity Aerobic (MA) | 2 | 4 | 6 | Balance of weight loss and mass preservation |
| Low-Intensity Aerobic (LA) | 3 | 1 | 7 | Effective for fat loss, less for muscle |
| High-Intensity Resistance (HR) | 9 | 7 | 5 | Good for muscle preservation |
| Moderate-Intensity Resistance (MR) | 8 | 5 | 3 | Optimal for muscle preservation |
| Low-Intensity Resistance (LR) | 7 | 6 | 4 | Good for muscle preservation |
| Moderate-Intensity Mixed (MM) | 4 | 9 | 2 | Optimal overall body composition |
Distinct and Additive Benefits of CR and Pharmacologic Agents
Research comparing CR to the mTORC1 inhibitor rapamycin reveals that their benefits on aging skeletal muscle are largely distinct and can be additive [49]. This suggests that parallel interventions targeting different pathways could be a potent strategy.
While both CR and rapamycin can reverse age-related cardiac hypertrophy and diastolic dysfunction in model organisms, they elicit strikingly different gene expression profiles in skeletal muscle [49] [50]. Crucially, rapamycin provides additional benefits to muscle integrity even in the context of CR, and CR improves muscle quality without necessarily suppressing muscle mTORC1 activity [49]. This indicates that CR confers benefits through both mTORC1-dependent and -independent pathways, opening the possibility for combined therapies with "CR mimetics" like rapamycin to more effectively counteract sarcopenia.
Experimental Models and Methodologies
Pre-Clinical Model: D-Galactose-Induced Aging
The D-galactose injection model is a validated method for inducing premature aging in rodents and is useful for studying sarcopenia [51].
- Protocol: Subcutaneous injections of 150 mg/kg/day of D-galactose are administered for 28 weeks to induce a premature aging phenotype.
- Interventions: At week 13, interventions such as exercise or CR can be introduced. An effective exercise regimen uses a treadmill set at 0° inclination, starting at 8 cm/s and increasing by 2 cm/s daily until reaching 20 cm/s, for 30 minutes per day, 5 days/week. A concurrent CR intervention can involve a 30% reduction in caloric intake [51].
- Endpoint Analyses: Outcomes include total walking distance (locomotor activity), whole-body fatty acid, and carbohydrate oxidation during physical activity (via indirect calorimetry), and molecular analysis of muscle tissue for signaling pathways and oxidative stress markers [51].
Human Clinical Trial: Body Composition and Glucose Metabolism
A typical protocol for assessing the impact of a high-protein diet during CR in humans involves [2] [17]:
- Participants: Overweight or obese, insulin-resistant adults.
- Dietary Intervention: A hypocaloric diet (e.g., 800 kcal/day or 7100 kJ/day) with macronutrient manipulation. The high-protein group receives 1.6 g/kg/day (or ~45% of calories from protein), while the control group receives 0.8 g/kg/day (or ~20% of calories from protein). Diets are matched for fat and total energy.
- Duration: 10 to 12 weeks.
- Key Measurements:
- Body Composition: Assessed via Dual-Energy X-ray Absorptiometry (DXA) to track fat mass and lean soft tissue mass.
- Muscle Mass Quantification: The D3-creatine (D3Cr) dilution method is considered a gold standard for directly measuring whole-body skeletal muscle mass, as it is less confounded by fluid changes than DXA [52].
- Insulin Sensitivity: Measured using the hyperinsulinemic-euglycemic clamp (gold standard) or Homeostatic Model Assessment of Insulin Resistance (HOMA-IR).
- Muscle Function: Handgrip strength and chair stand tests are recommended by the European Working Group on Sarcopenia in Older People (EWGSOP2) [52].
The Scientist's Toolkit: Key Research Reagents and Methods
Table 3: Essential Research Tools for Investigating Muscle Mass Preservation
| Tool / Reagent | Function / Application | Technical Notes |
|---|---|---|
| D3-Creatine (D3Cr) Dilution Method | Direct, quantitative measurement of whole-body skeletal muscle mass. | Superior to DXA for specific SMM measurement; uses mass spectrometry after oral D3-creatine administration [52]. |
| Hyperinsulinemic-Euglycemic Clamp | Gold-standard assessment of insulin sensitivity in vivo. | Quantifies insulin-stimulated glucose disposal rate (M-value) [2]. |
| Deuterated Leucine (2H3-Leucine) | Measures proteome turnover and protein synthesis rates in vivo. | Used with LC-MS/MS to calculate protein half-lives; reveals CR-induced changes in protein dynamics [50]. |
| Rapamycin | mTORC1 inhibitor; used to probe mTOR pathway in muscle preservation. | Considered a potential caloric restriction mimetic; has effects distinct from and additive to CR [49]. |
| Beta-hydroxy-beta-methylbutyrate (HMB) | Leucine metabolite; experimental supplement to reduce muscle catabolism. | Shown to promote mitochondrial function and mitigate muscle loss during disuse [2]. |
| Dual-Energy X-ray Absorptiometry (DXA) | Measures body composition (fat mass, lean soft tissue, bone mineral density). | Common and accessible; note "lean soft tissue" includes water and organ mass, not just muscle [52]. |
Signaling Pathways in Muscle Preservation
The molecular response to dietary protein and energy status involves a complex interplay of signaling pathways that regulate muscle protein synthesis and mitochondrial health. The following diagram illustrates the key pathways activated by essential amino acids (EAAs) and their interaction with energy-sensing mechanisms.
Diagram 1: Anabolic and Metabolic Signaling in Skeletal Muscle. This figure outlines the core pathways through which Essential Amino Acids (EAAs) and energy status (caloric restriction, exercise) influence muscle mass and metabolic health. EAAs, particularly leucine, directly activate mTORC1 to drive protein synthesis. Concurrently, EAAs and low-energy states activate SIRT1/AMPK, which upregulates PGC-1α. PGC-1α is a master regulator of mitochondrial biogenesis, leading to enhanced oxidative metabolism and improved insulin sensitivity.
The preservation of fat-free mass during caloric restriction is an achievable and metabolically critical goal. The evidence strongly supports a multi-pronged strategy:
- Implementing a hypocaloric diet with elevated protein intake (≥1.3 g/kg/day or ~35% of calories) to supply EAAs, specifically leucine, for activating anabolic signaling.
- Incorporating structured exercise, with emphasis on moderate-intensity resistance training, to provide a mechanical stimulus for muscle retention and synergize with nutritional anabolic signals.
- Exploring distinct molecular pathways, such as those targeted by rapamycin, that offer additive benefits to CR alone.
Future research should focus on refining optimal protein and amino acid patterns across diverse populations, validating the long-term functional and metabolic benefits of FFM preservation, and developing combination therapies that leverage both nutritional and pharmacological approaches to combat sarcopenia and its associated metabolic sequelae.
Essential Amino Acid (EAA) Supplementation to Augment Mitochondrial Function and Satiety
Emerging research elucidates the critical role of Essential Amino Acids (EAAs) as potent signaling molecules that extend beyond their function as mere protein substrates. This technical review synthesizes current evidence on the mechanisms by which EAA supplementation enhances mitochondrial biogenesis and function, promotes satiety, and improves metabolic homeostasis. The dual impact of EAAs on energy expenditure and energy intake positions them as a compelling nutritional intervention within metabolic disease research and therapeutic development. Framed within the broader context of dietary protein's influence on glucose homeostasis, this review details the specific signaling pathways—including mTOR, SIRT1/PGC-1α, and incretin responses—orchestrated by EAAs, providing methodologies and key reagents for preclinical and clinical investigation.
Within the framework of dietary protein and amino acid research, their impact on glucose homeostasis has garnered significant scientific interest. Essential Amino Acids (EAAs), which cannot be synthesized de novo and must be obtained from the diet, serve as critical regulators of metabolic pathways. Recent advances have shifted the perspective of EAAs from passive building blocks to active modulators of mitochondrial dynamics and appetite regulation. This review dissects the specific mechanisms by which EAA supplementation augments mitochondrial function—enhancing cellular energy production and reducing oxidative stress—and concurrently promotes satiety—modulating hormonal signals to reduce energy intake. Understanding these coordinated effects is paramount for developing targeted nutritional and pharmacological strategies against obesity, type 2 diabetes, and related metabolic disorders.
Quantitative Data Synthesis: EAA Effects on Metabolic Parameters
The following tables consolidate key quantitative findings from recent studies on EAA supplementation, providing a reference for expected effect magnitudes in metabolic research.
Table 1: Preclinical Studies - EAA Supplementation in Rodent Models
| Metabolic Parameter | Experimental Group (HFD-EAA) | Control Group (HFD) | p-value / Significance | Study Duration | Citation |
|---|---|---|---|---|---|
| Body Weight Gain | Prevented & Reversed obesity | Significant weight gain | p < 0.0001 | 33 weeks | [53] |
| Glucose Tolerance (AUC) | Significant improvement | Impaired glucose tolerance | p < 0.05 | 33 weeks | [53] |
| Intestinal Barrier Integrity (TEER) | Upregulated & Maintained | Disrupted | p < 0.05 | 33 weeks | [53] |
| Plasma Calprotectin | Reduced | Elevated | p < 0.05 | 33 weeks | [53] |
| Citrulline (Enterocyte Mass) | Normalized | Decreased | p < 0.05 | 33 weeks | [53] |
Table 2: Clinical and Human Study Outcomes - EAA/BCAA Supplementation
| Outcome Measure | Supplementation Protocol | Study Population | Key Findings | Citation |
|---|---|---|---|---|
| Muscle Protein Synthesis (MPS) | Leucine-enriched EAA (10g EAA, 3.5g Leucine) post-exercise | Older Men | Prolonged MPS rate for up to 4 hours post-exercise | [54] |
| Insulin Sensitivity (HOMA Index) | 24g HMB/Glutamine/Arginine mix twice daily for 8 weeks | Post-bariatric surgery patients | Significant worsening in supplemented group (p=0.04) | [55] |
| Inflammatory Marker (CRP) | 24g HMB/Glutamine/Arginine mix twice daily for 8 weeks | Post-bariatric surgery patients | Significantly higher in supplemented vs. control at 8 weeks (p=0.018) | [55] |
| Fasting Glucose | 24g HMB/Glutamine/Arginine mix twice daily for 8 weeks | Post-bariatric surgery patients | Decreased vs. baseline (p<0.0001), no inter-group difference | [55] |
| Amino Acid Plasma Profiles | Observational | Obese Children & Adolescents | ↑ Leucine, Isoleucine, Valine, Phe, Tyr; ↓ Glycine, Serine | [14] |
Core Mechanistic Pathways
EAA-Driven Enhancement of Mitochondrial Biogenesis and Function
EAAs, particularly leucine, act as potent epigenetic and metabolic signals to enhance mitochondrial capacity, a process crucial for metabolic health.
Diagram 1: EAA & Mitochondrial Biogenesis Pathway (76 characters)
Detailed Workflow and Rationale: The pathway initiates with EAA supplementation, providing leucine and arginine. Leucine directly and indirectly activates the SIRT1/PGC-1α axis [56], a master regulator of mitochondrial biogenesis. Concurrently, EAA availability stimulates endothelial Nitric Oxide Synthase (eNOS) activation, increasing nitric oxide production and improving oxygen and nutrient delivery to tissues [56]. The resulting mitochondrial biogenesis increases energy production capacity but is inherently coupled with a rise in Reactive Oxygen Species (ROS). Rather than being purely detrimental, this EAA-induced ROS serves as a crucial signaling molecule that upregulates intrinsic antioxidant defense systems like glutathione (GSH) and superoxide dismutase (SOD) and promotes mitophagy, the selective autophagy of damaged mitochondria [56]. The net outcome is a refinement of the mitochondrial network, leading to improved cellular bioenergetics. This enhanced energy status is critical for maintaining metabolically demanding processes such as gut barrier integrity; indeed, EAA supplementation has been shown to upregulate PGC-1α and mitochondrial ETC genes in intestinal epithelial cells, preserving tight junction proteins and attenuating obesity-induced gut inflammation [53].
EAA Modulation of Satiety and Food Intake
EAAs influence central and peripheral satiety signals through multiple biochemical pathways, creating a synergistic effect on reducing energy intake.
Diagram 2: EAA & Satiety Signaling Pathway (74 characters)
Detailed Workflow and Rationale: The satiety effects of EAAs are mediated by their role as precursors for gut hormones and neurotransmitters. Phenylalanine has been shown to stimulate the release of satiety hormones like cholecystokinin (CCK) [14]. Furthermore, EAA supplementation can influence the secretion of glucagon-like peptide-1 (GLP-1), a potent incretin hormone that slows gastric emptying and promotes feelings of fullness [55] [57]. Concurrently, EAAs provide critical precursors for brain neurotransmitters. Tryptophan is the sole precursor for serotonin, a neurotransmitter that suppresses appetite and promotes satiety by acting in the hypothalamus [14]. Tyrosine and phenylalanine are precursors for catecholamines like dopamine and norepinephrine, which are involved in reward-driven feeding behavior and energy balance, often leading to appetite suppression and increased energy expenditure [14]. The convergence of these hormonal and neural signals results in a net effect of reduced food intake and promoted satiety.
Experimental Protocols for Key Investigations
Protocol: Evaluating EAA Effects on Mitochondrial Function in an Obese Mouse Model
This protocol is adapted from a study demonstrating EAA protection of intestinal barrier integrity via mitochondrial protection [53].
- Objective: To determine whether EAA substitution in a high-fat diet (HFD) prevents mitochondrial dysfunction and gut barrier disruption in diet-induced obese mice.
- Study Design:
- Animals: Male C57BL/6N mice (n=10-12/group, 8 weeks old).
- Groups: (1) Control diet; (2) High-Fat Diet (HFD); (3) Isocaloric, isonitrogenous HFD with EAA substitution (HFD-EAA).
- Duration: 33 weeks.
- Key Methodologies:
- Glucose Tolerance Test (GTT): Perform after 20 and 30 weeks. Fast mice for 6h, administer glucose i.p. (2g/kg body weight). Measure blood glucose from tail vein at 0, 15, 30, 60, 90, and 120 minutes.
- Intestinal Barrier Function: At endpoint, isolate ileum and colon. Using Ussing chambers, measure Transepithelial Electrical Resistance (TEER) ex vivo. Administer FITC-dextran (4 kDa) to mice and measure serum flux to assess in vivo permeability.
- Mitochondrial Biogenesis Assay: Isolate intestinal epithelial cells (IECs). Analyze gene expression of PGC-1α and electron transport chain complexes (e.g., ATP5A, NDUFB8, SDHB, CYC1) via qRT-PCR and Western Blot.
- Tissue Analysis: Collect plasma for citrulline (marker of enterocyte mass) and calprotectin (inflammation marker) via ELISA. Analyze mesenteric fat pad weight.
Protocol: Assessing the Impact of an EAA Formula on Human Satiety and Metabolism
This protocol incorporates elements from clinical studies on amino acid supplementation [55] [54].
- Objective: To investigate the acute effects of a specific EAA formula on satiety hormone release, energy expenditure, and mitochondrial function in overweight human subjects.
- Study Design:
- Participants: Overweight/obese adults (BMI 28-35 kg/m²), randomized, double-blind, placebo-controlled, crossover design.
- Intervention: After an overnight fast, participants consume either:
- EAA Drink: 15g EAA formula (enriched with leucine and Krebs cycle intermediates).
- Isovolumetric Placebo Drink: Matched for color and taste.
- Washout Period: 7 days.
- Key Methodologies:
- Blood Sampling: Collect at 0 (fasting), 30, 60, 90, and 120 min post-supplement. Analyze plasma for:
- Satiety Hormones: GLP-1, PYY, CCK via ELISA/Luminex.
- Amino Acids: LC-MS/MS profiling of BCAA and aromatic AA levels.
- Insulin/Glucose: For HOMA-IR calculation.
- Indirect Calorimetry: Perform at 0 and 120 min to calculate Respiratory Quotient (RQ) and Resting Energy Expenditure (REE).
- Satiety Visual Analog Scales (VAS): Administer at each blood draw time point to subjectively rate hunger, fullness, and prospective food consumption.
- Peripheral Blood Mononuclear Cell (PBMC) Assay: Isolate PBMCs at 0 and 120 min. Measure mitochondrial respiration using a Seahorse XF Analyzer.
- Blood Sampling: Collect at 0 (fasting), 30, 60, 90, and 120 min post-supplement. Analyze plasma for:
The Scientist's Toolkit: Key Research Reagents and Models
Table 3: Essential Research Reagents and Models for EAA Metabolic Studies
| Reagent / Model | Specific Example / Product Code | Research Function & Rationale | Key Citation |
|---|---|---|---|
| In Vivo Model | C57BL/6N Male Mice | Standardized model for diet-induced obesity & metabolic phenotyping. | [53] |
| In Vitro Barrier Model | Differentiated Caco-2 Cells | Human colorectal adenocarcinoma cell line; forms polarized monolayers for transepithelial resistance (TEER) & permeability studies. | [53] |
| EAA Formulation (Research Grade) | E7 Formula (enriched with Krebs cycle intermediates) | Standardized research-grade EAA blend for consistent in vitro & in vivo testing of mitochondrial & barrier effects. | [53] |
| Mitochondrial Respiration Assay | Seahorse XF Cell Mito Stress Test (Agilent) | Real-time, live-cell analysis of OCR to assess mitochondrial function in cells (e.g., myocytes, hepatocytes, PBMCs). | [56] |
| Metabolic Hormone Profiling | MILLIPLEX MAP Human Metabolic Hormone Magnetic Bead Panel (Merck) | Multiplexed quantification of key hormones (GLP-1, GIP, Leptin, Ghrelin, Insulin) from single plasma/serum samples. | [55] |
| Amino Acid Quantification | LC-HRMS (Liquid Chromatography-High Resolution Mass Spectrometry) | Gold-standard for precise, simultaneous quantification of full plasma/serum amino acid profiles. | [58] [14] |
| Insulin Sensitivity Calculation | HOMA2 Calculator (University of Oxford) | Validated software using fasting glucose & insulin to estimate beta-cell function & insulin resistance from clinical samples. | [55] |
Discussion and Research Implications
The evidence delineated in this review solidifies the role of EAA supplementation as a multifaceted intervention with significant potential to modulate core aspects of metabolic health. The biphasic and context-dependent nature of EAA signaling is a critical consideration for researchers. Acute, postprandial elevations of EAAs, particularly leucine, are anabolic and beneficial, promoting mitochondrial function and muscle protein synthesis [1] [54]. However, chronic hyperaminoacidemia, as often observed in obese, insulin-resistant states, is associated with mTOR overactivation, impaired insulin signaling, and elevated inflammatory markers (e.g., CRP, IL-6) [1] [55] [14]. This paradox underscores the importance of dosage, timing, and the metabolic baseline of the target population in study design.
Future research must prioritize several key areas:
- Elucidating Tissue-Specific Effects: The differential impact of EAAs on organs like the liver, skeletal muscle, intestine, and pancreas requires deeper mechanistic exploration using tissue-specific knockout models.
- Optimal Formulation and Dosing: Determining the ideal EAA composition (e.g., leucine content, inclusion of conditionally essential AAs like arginine and glutamine) and dosing regimen (bolus vs. pulsed) for targeted outcomes is essential.
- Translational Clinical Trials: Well-controlled, long-term human studies are needed to confirm the efficacy of EAA supplementation in improving mitochondrial function and satiety in clinical populations, moving beyond proof-of-concept rodent models.
EAA supplementation represents a powerful, non-pharmacological strategy to simultaneously target mitochondrial dysfunction and dysregulated satiety—two hallmarks of metabolic disease. The efficacy of EAAs is mediated through well-defined pathways, including SIRT1/PGC-1α-driven mitochondrial biogenesis and hormone/neurotransmitter-mediated satiety signaling. Integrating this approach into the broader context of dietary protein research on glucose homeostasis opens promising avenues for therapeutic development. For the research community, success will hinge on the meticulous application of the detailed experimental protocols and specialized reagents outlined herein, coupled with a nuanced understanding of the delicate balance required in EAA signaling to achieve therapeutic benefit.
Dietary Interventions for Inactivity-Induced Insulin Resistance (e.g., Bed Rest Models)
Physical inactivity, modeled experimentally through bed rest studies, serves as a powerful paradigm for investigating the rapid metabolic deterioration that occurs during sedentary behavior and metabolic disease progression. Research has consistently demonstrated that strict bed rest induces systemic insulin resistance—a key pathological feature of type 2 diabetes—within remarkably short timeframes [59] [60] [61]. This model provides a controlled environment for elucidating fundamental biological mechanisms and testing targeted dietary countermeasures.
The physiological overlap between inactivity-induced metabolic alterations and naturally occurring insulin resistance makes this approach particularly valuable for therapeutic development. Studies have confirmed that bed rest-induced insulin resistance occurs primarily in muscle tissue, mirroring defects observed in type 2 diabetes [61]. This whitepaper synthesizes current evidence regarding dietary interventions, with particular emphasis on the role of dietary proteins and amino acids in counteracting metabolic impairments resulting from physical inactivity, framed within the broader context of glucose homeostasis research.
Metabolic Consequences of Inactivity
Temporal Progression of Insulin Resistance
Bed rest studies have meticulously documented the rapid timeline of metabolic deterioration following reduced physical activity:
Table 1: Temporal Progression of Insulin Resistance During Bed Rest
| Duration | Key Metabolic Alterations | Underlying Mechanisms | Study Population |
|---|---|---|---|
| 6 days | • Decreased whole-body insulin sensitivity• Reduced GLUT4 localization at muscle cell membrane• Intramuscular glycogen accumulation | • Nutrient overload mismatch• Altered GLUT4 trafficking | Healthy adults (n=24) [62] |
| 9 days | • Significant decrease in whole-body insulin sensitivity• Augmented hepatic insulin resistance in FDR subjects• Impaired nonoxidative glucose metabolism | • Peripheral and hepatic defects• Genetic predisposition effects | FDR (n=13) & Control (n=20) [59] |
| 14 days | • Increased glucose and insulin AUC during OGTT• Reduced Matsuda index• Elevated α-klotho concentrations | • Systemic insulin resistance• Altered endocrine function | Older adults (55-65 years, n=22) [60] |
| 55-60 days | • Intramuscular lipid droplet accumulation• Mitochondrial structural and functional impairments• Ceramide and sphingomyelin deposition | • Lipotoxicity• Metabolic inflexibility | Healthy adults (n=24) [62] |
Molecular Mechanisms of Disuse-Induced Metabolic Impairment
The pathophysiology of inactivity-induced insulin resistance involves coordinated disruptions across multiple tissue systems:
Figure 1: Molecular pathways of inactivity-induced insulin resistance. Bed rest triggers skeletal muscle and hepatic adaptations that converge into systemic insulin resistance through multiple mechanisms. Key nodes represent physiological processes, with red indicating primary defects, yellow the initiating stimulus, and gray specific molecular mechanisms.
Skeletal Muscle Adaptations
The rapid reduction in insulin sensitivity following bed rest is characterized by diminished GLUT4 transporter localization at the muscle cell membrane, occurring within just 6 days of inactivity [62]. This redistribution limits glucose entry into myocytes despite maintained or even increased total GLUT4 protein expression. Concurrently, intramuscular glycogen stores become saturated, creating a nutrient overload state that further dampens insulin signaling sensitivity. With prolonged inactivity (55-60 days), lipotoxic species including ceramides and sphingomyelins accumulate within muscle tissue, promoting inflammatory pathways and mitochondrial dysfunction [62].
Hepatic Metabolic Alterations
First-degree relatives of individuals with type 2 diabetes exhibit heightened susceptibility to hepatic insulin resistance following bed rest, suggesting genetic predisposition influences hepatic vulnerability to physical inactivity [59]. This manifests as inappropriate endogenous glucose production despite hyperinsulinemia, a defect not consistently observed in healthy control subjects under short-term bed rest conditions.
Dietary Interventions: Mechanistic Insights and Evidence
Protein and Amino Acids: Dual Roles in Glucose Metabolism
Dietary proteins demonstrate complex, multifaceted relationships with glucose homeostasis, presenting both therapeutic potential and metabolic risks:
Table 2: Amino Acids and Proteins in Glucose Homeostasis: Mechanisms and Effects
| Compound | Experimental Model | Key Effects on Glucose Metabolism | Proposed Mechanisms | Research Context |
|---|---|---|---|---|
| Mixed Dietary Proteins (casein, fish gelatin) | Wistar rats (in vivo) | Improved glucose tolerance | Reduced intestinal GLUT2 mRNA expression; modulated glucose absorption [43] | Acute feeding studies |
| Branched-Chain Amino Acids (Leucine, Isoleucine, Valine) | Human observational & cell studies | Elevated levels correlate with insulin resistance; potential therapeutic benefits at optimal doses | Modulation of insulin signaling pathways; reduction of inflammatory responses [63] | Dose-dependent dual effects |
| Egg Protein (23g dose) | Human clinical trial | Minimal contribution to circulating glucose (4g over 8h) despite high deamination rate | Hepatic autoregulation of gluconeogenesis independent of insulin/glucagon [34] | Stable isotope tracer study |
| Casein (50g dose) | Human clinical trial | Modest glucose appearance (9.7g over 8h) without altering plasma glucose | Controlled hepatic glucose release; efficient amino acid oxidation [34] | Glucose isotope-dilution technique |
| Various Dietary Proteins (hemoglobin, ovalbumin, pea, gluten) | In vitro Caco-2/TC7 cells | Reduced intestinal glucose uptake | Inhibition of glucose transporters (SGLT1/GLUT2) [43] | Simulated gastrointestinal digestion |
The Protein Paradox: Gluconeogenic Substrates Versus Glucose Regulators
Despite being potent gluconeogenic precursors, most dietary proteins minimally impact circulating glucose levels when consumed orally. Studies utilizing isotope tracers demonstrate that only approximately 8-20% of ingested protein carbon appears as circulating glucose within 8 hours post-consumption [34]. This discrepancy between theoretical gluconeogenic potential and actual glucose appearance highlights sophisticated hepatic autoregulatory mechanisms that operate independently of pancreatic hormones.
The timing and composition of protein intake appear critical to its glucoregulatory effects. Acute protein ingestion prior to carbohydrate exposure may modulate intestinal glucose absorption through inhibition of SGLT1 and GLUT2 transporters, potentially explaining the improved glycemic control observed with mixed-meal consumption [43].
Branched-Chain Amino Acids: A Complex Relationship with Insulin Sensitivity
Branched-chain amino acids (BCAAs) demonstrate a paradoxical relationship with metabolic health. While observational studies consistently associate elevated circulating BCAA levels with insulin resistance, controlled interventional studies suggest potential therapeutic benefits when administered in specific contexts and doses [63]. This apparent contradiction may reflect dose-response relationships and the influence of overall metabolic state on BCAA metabolism.
Comparative Effectiveness of Dietary Patterns
Beyond isolated nutrients, entire dietary patterns have been evaluated for their efficacy in improving metabolic parameters in insulin-resistant states:
Table 3: Dietary Pattern Efficacy on Glycemic Control in Insulin Resistance
| Dietary Pattern | HbA1c Reduction vs. Control | Weight Loss vs. Control | Other Metabolic Benefits | Evidence Base |
|---|---|---|---|---|
| Mediterranean | -0.47% (P < 0.00001) | -1.84 kg (P < 0.00001) | Increased HDL-C | RCTs in T2DM [64] |
| High-Protein | -0.28% (P < 0.00001) | Not significant | Improved satiety, lean mass preservation | RCTs in T2DM [64] |
| Low-Glycemic Index | -0.14% (P = 0.008) | Variable | Reduced postprandial glucose excursions | RCTs in T2DM [64] |
| Low-Carbohydrate | -0.12% (P = 0.04) | -0.69 kg (P = 0.21) | Increased HDL-C, reduced triglycerides | RCTs in T2DM [64] |
The Mediterranean diet emerges as particularly effective, possibly due to synergistic effects between its component foods—including healthy fats, fiber, and plant proteins—that collectively address multiple pathological pathways in insulin resistance [64].
Experimental Approaches and Research Methodologies
Bed Rest Protocol Standardization
Well-controlled bed rest studies implement standardized methodologies to ensure metabolic changes reflect inactivity rather than confounding variables:
Figure 2: Experimental workflow for bed rest studies. Standardized methodologies include strict activity control, dietary standardization, and comprehensive metabolic phenotyping across study phases to isolate the effects of physical inactivity.
Key Methodological Considerations
- Participant Selection: Studies often compare healthy controls against at-risk populations (e.g., first-degree relatives of type 2 diabetics) to examine genetic susceptibility [59]
- Dietary Standardization: Isocaloric diets provided throughout study periods prevent weight changes from confounding results [59] [62]
- Activity Strictness: Half-recumbent position maintenance with minimal (15 min/day) toilet privileges ensures consistent disuse [59]
- Countermeasure Testing: Exercise protocols (aerobic, HIIT, resistive) demonstrate partial protection against metabolic impairment [60]
Advanced Metabolic Phenotyping Techniques
Hyperinsulinemic-Euglycemic Clamp
The gold standard method for assessing whole-body insulin sensitivity involves maintaining a target blood glucose concentration (typically 5 mmol/L) via variable glucose infusion during fixed-rate insulin infusion (e.g., 80 mU/m² per min) [59]. Insulin sensitivity is quantified as the glucose infusion rate required to maintain euglycemia.
Stable Isotope Tracers
Primed constant infusions of non-radioactive isotopic tracers (e.g., [6,6-²H₂]glucose, [1,1,2,3,3-²H₂]glycerol) enable precise quantification of glucose and glycerol kinetics under basal and insulin-stimulated conditions [59].
Combined Methodologies
Advanced studies integrate multiple approaches:
- Clamp + Indirect Calorimetry: Assesses substrate oxidation rates under insulin-stimulated conditions [59]
- IVGTT/OGTT + Mathematical Modeling: Provides beta-cell function indices (BIGTT-AIR) and tissue-specific insulin sensitivity (Matsuda index) [60]
- Muscle Biopsy + Multi-omics: Reveals molecular adaptations in signaling pathways, transporter localization, and metabolite accumulation [62]
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Inactivity-Induced Insulin Resistance Studies
| Reagent/Category | Specific Examples | Research Application | Function/Mechanism |
|---|---|---|---|
| Stable Isotope Tracers | [6,6-²H₂]glucose; [1,1,2,3,3-²H₂]glycerol | Glucose and glycerol kinetics | Metabolic flux quantification via GC-MS [59] |
| Clamp Reagents | Human insulin; D20W (20% dextrose solution); OneTouch glucose meters | Hyperinsulinemic-euglycemic clamp | Direct insulin sensitivity measurement [59] |
| Immunoassays | AutoDELFIA time-resolved fluoroimmunoassay (insulin, C-peptide); ELISA (FGF-23, α-klotho) | Hormone and biomarker quantification | Metabolic and endocrine profiling [59] [60] |
| Cell Culture Models | Caco-2/TC7; HT29-MTX | Intestinal glucose transport studies | SGLT1/GLUT2 transporter activity assessment [43] |
| Protein Digestion Systems | INFOGEST static gastrointestinal digestion protocol (pepsin, pancreatin) | Simulated protein digestion | Bioactive peptide generation for mechanistic studies [43] |
| Molecular Biology Kits | RT-PCR (SGLT1/GLUT2 expression); BCA protein assay; Western blot (GLUT4) | Tissue and cellular analysis | Transporter quantification and localization [62] [43] |
The bed rest model provides a validated, controlled system for investigating dietary countermeasures to inactivity-induced insulin resistance. Evidence suggests that dietary protein manipulation represents a promising therapeutic strategy, with potential mechanisms including modulation of intestinal glucose absorption, hepatic autoregulation of gluconeogenesis, and preservation of muscle metabolic health.
Future research should prioritize several key areas:
- Dose-response characterization of protein and specific amino acids across different metabolic phenotypes
- Temporal optimization of protein intake relative to carbohydrate consumption
- Synergistic effects of combined dietary approaches (e.g., Mediterranean diet with targeted protein supplementation)
- Molecular mechanistic studies focusing on tissue-specific protein sensing and signaling pathways
The evolving understanding of how dietary components regulate glucose homeostasis under conditions of metabolic stress continues to inform both clinical management strategies and fundamental biological knowledge of nutrient-sensing pathways.
Protein-Induced Secretion of Insulin, GLP-1, and Glucagon
The regulation of glucose homeostasis is a complex process involving multiple organs and hormone systems. Among dietary macronutrients, protein and its constituent amino acids play a critically important, yet dualistic role in metabolic regulation. This technical review examines the mechanisms by which dietary proteins influence the secretion of three key glucoregulatory hormones—insulin, glucagon-like peptide-1 (GLP-1), and glucagon—and integrates these findings into the broader context of glucose homeostasis research. Understanding these hormonal responses is essential for developing targeted nutritional and pharmacological interventions for metabolic disorders such as type 2 diabetes mellitus (T2DM).
Hormonal Regulation of Glucose Homeostasis
Key Glucoregulatory Hormones
Table 1: Key Glucoregulatory Hormones Influenced by Dietary Protein
| Hormone | Secretion Site | Primary Stimuli | Glucose Homeostasis Actions |
|---|---|---|---|
| Insulin | Pancreatic β-cells | Glucose, Amino acids, Incretins | Promotes glucose uptake in muscle and adipose tissue; stimulates glycogenesis; suppresses gluconeogenesis [65] |
| GLP-1 | Intestinal L-cells | Nutrients (AA, FA, carbs), Neural signals | Potentiates glucose-dependent insulin secretion; suppresses glucagon secretion; slows gastric emptying; promotes satiety [66] [67] |
| Glucagon | Pancreatic α-cells | Amino acids, Hypoglycemia, Sympathetic input | Stimulates gluconeogenesis and glycogenolysis; increases hepatic glucose output [65] |
| GIP | Intestinal K-cells | Nutrients (carbs, fats) | Enhances glucose-dependent insulin secretion; promotes lipid metabolism [65] |
The Incretin Effect and Protein
The "incretin effect" describes the phenomenon whereby oral nutrient administration stimulates a significantly greater insulin response compared to intravenous administration of the same nutrients, even at identical plasma glucose concentrations. This effect is primarily mediated by the gut-derived hormones GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) [65]. While carbohydrates are the classical stimulants of incretin secretion, emerging evidence demonstrates that dietary protein and amino acids also potently stimulate GLP-1 release, contributing to the insulinotropic response to protein ingestion [65] [67].
Mechanisms of Protein-Induced Hormone Secretion
Direct Effects on Pancreatic Islets
Amino acids directly modulate pancreatic endocrine function through multiple established mechanisms:
The "Triggering Pathway": Cationic amino acids (e.g., arginine, lysine) enhance β-cell depolarization, while neutral amino acids (e.g., alanine, proline) co-transport with sodium ions, contributing to membrane depolarization [65]. This leads to voltage-dependent calcium channel activation, calcium influx, and ultimately insulin exocytosis [65].
Metabolic Signaling: Amino acids enter metabolic pathways to generate ATP, which closes ATP-sensitive potassium channels, further promoting membrane depolarization and insulin secretion [65].
mTORC1 Activation: The mammalian target of rapamycin complex 1 (mTORC1), a protein kinase signaling complex, plays a key role in amino acid-mediated insulin secretion through regulation of protein synthesis, particularly insulin synthesis in β-cells [65] [2].
The following diagram illustrates the direct effects of amino acids on pancreatic β-cell insulin secretion:
Enteroendocrine L-Cell Secretion of GLP-1
Intestinal L-cells sense dietary protein and amino acids through multiple mechanisms:
Nutrient-Sensing Receptors: L-cells express various G protein-coupled receptors (GPCRs) with affinity for amino acids, including GPR40 (for fatty acids and amino acids) and GPR119 (for fatty acid amides and monoacylglycerols) [66]. Receptor activation stimulates intracellular cAMP production and Ca2+ mobilization, triggering GLP-1 secretion [66].
Electrogenic Transport: Similar to pancreatic β-cells, L-cells are electrically excitable. Electrogenic uptake of amino acids can generate action potentials that trigger depolarization-induced Ca2+ influx through voltage-dependent Ca2+ channels, leading to GLP-1 exocytosis [66].
Calcium-Protein Synergy: Emerging evidence suggests that co-ingestion of protein and calcium potently stimulates GLP-1 release, potentially through activation of the calcium-sensing receptor (CaSR) [67].
The following diagram illustrates GLP-1 secretion from intestinal L-cells:
Protein-Induced Glucagon Secretion
While insulin and GLP-1 lower blood glucose levels, dietary protein simultaneously stimulates glucagon secretion through:
Direct α-Cell Stimulation: Amino acids, particularly alanine and arginine, directly stimulate pancreatic α-cells to secrete glucagon [65]. This creates a counter-regulatory mechanism that helps prevent hypoglycemia during protein-rich meals, especially when carbohydrate content is low.
Hepatic Glucose Production: Glucagon promotes hepatic gluconeogenesis, providing a pathway for the carbon skeletons of glucogenic amino acids to be converted to glucose [65].
Quantitative Hormonal Responses to Dietary Protein
Hormone Secretion Kinetics
Table 2: Hormonal Responses to Protein and Amino Acid Administration
| Hormone | Basal Concentration | Postprandial Peak | Time to Peak | Stimulatory Amino Acids |
|---|---|---|---|---|
| Insulin | 5-15 μU/mL (fasting) | 2-5x increase | 30-45 minutes | Arginine, Leucine, Lysine, Alanine [65] |
| GLP-1 | 5-15 pmol/L (fasting) | 2-4x increase | 45-60 minutes | Mixed amino acids; Phenylalanine, Glutamine [67] |
| Glucagon | 50-100 pg/mL (fasting) | 1.5-3x increase | 30-60 minutes | Alanine, Arginine, Asparagine [65] |
Factors Modifying Hormonal Responses
Several factors influence the magnitude of hormone secretion in response to dietary protein:
Protein Source: Animal proteins (whey, casein, egg, fish, beef, chicken) and plant-based proteins (soy, pea, brown rice, chickpea) may differentially affect hormone secretion due to varying amino acid compositions and digestion kinetics [65].
Dose-Response Relationship: Hormonal responses generally exhibit dose-dependency within physiological ranges, though saturation kinetics may occur at very high protein doses [44].
Co-ingested Nutrients: The presence of carbohydrates, fats, and fiber modifies the hormonal response to dietary protein [68] [44].
Individual Metabolic Status: Insulin resistance, beta cell dysfunction, and other metabolic parameters significantly influence hormonal responses to protein ingestion [68].
Experimental Methodologies for Hormone Secretion Studies
In Vivo Human Studies
Table 3: Key Experimental Approaches for Studying Protein-Induced Hormone Secretion
| Methodology | Key Features | Measured Parameters | Considerations |
|---|---|---|---|
| Mixed Meal Tolerance Test | Contains protein, carbs, fat; reflects physiological conditions | Glucose, insulin, GLP-1, glucagon over 2-5 hours | Standardized meals improve reproducibility [69] |
| Oral Amino Acid/Protein Challenge | Isolated protein/AA without other macronutrients | Hormone secretion kinetics; dose-response relationships | Non-physiological but mechanism-focused [65] |
| Euglycemic Clamp with AA Infusion | Maintains fixed glucose during hormone measurement | Insulin sensitivity; insulin secretion capacity | Technically demanding; gold standard [2] |
| Continuous Glucose Monitoring | Ambulatory glucose monitoring in free-living conditions | Glycemic variability; postprandial glucose excursions | Real-world data; limited hormone measurement [68] |
In Vitro and Animal Models
Isolated Pancreatic Islets: Used to study direct effects of amino acids on insulin and glucagon secretion without neural or incretin influences [66].
Enteroendocrine Cell Lines: Model systems (e.g., STC-1, GLUTag, NCI-H716) for studying GLP-1 secretion mechanisms and screening secretagogues [67].
Perfused Gut Models: Isolated intestinal segments to study regional differences in GLP-1 secretion and nutrient sensing [66].
Research Reagent Solutions
Table 4: Essential Research Reagents for Studying Protein-Induced Hormone Secretion
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| GLP-1 Receptor Agonists | Exenatide, Liraglutide, Semaglutide | Pharmacological activation of GLP-1 signaling; diabetes/obesity research [66] [70] |
| DPP-IV Inhibitors | Sitagliptin, Vildagliptin, Saxagliptin | Inhibition of GLP-1 degradation; enhances endogenous GLP-1 activity [66] |
| Amino Acid Receptor Modulators | GPR40 agonists, GPR119 agonists, CaSR modulators | Investigation of nutrient-sensing mechanisms in enteroendocrine cells [66] [67] |
| Hormone Assays | ELISA, RIA, Multiplex Immunoassays | Quantification of insulin, GLP-1 (total and active), glucagon in plasma/serum [69] |
| Cell Line Models | STC-1, GLUTag, NCI-H716, INS-1, MIN6 | In vitro screening of secretagogues; mechanism studies [67] |
Research Implications and Therapeutic Applications
Dietary Protein in Diabetes Management
The hormonal responses to dietary protein have important implications for nutritional management of metabolic diseases:
High-Protein Diets (HPDs): Defined as diets supplying ≥35% of daily total energy intake as protein, HPDs can promote weight loss, enhance satiety, and improve glycemic control in some individuals [65] [44].
Mitigation of Glucose Spikes: Consuming protein or fiber before carbohydrates can lower postprandial glucose spikes in metabolically healthy individuals, though this effect may be blunted in those with insulin resistance [68].
Source Considerations: Plant-based proteins may offer advantages over animal proteins for diabetes risk reduction, though confounding factors (e.g., associated fiber intake) complicate interpretation [44].
Drug Development Targeting Protein-Induced Hormone Secretion
Understanding the mechanisms of protein-induced hormone secretion has enabled several drug development strategies:
GLP-1 Receptor Agonists: Stable, long-acting GLP-1 analogs (exenatide, liraglutide, semaglutide) that resist DPP-IV degradation have revolutionized T2DM and obesity treatment [66] [70].
GPR Agonists: Investigational agents targeting GPR119 and GPR40 receptors on L-cells to stimulate endogenous GLP-1 release represent a promising therapeutic approach [66].
Dual and Triple Agonists: Novel agents simultaneously targeting receptors for GLP-1, GIP, and glucagon show enhanced efficacy for weight loss and glycemic control compared to selective GLP-1 receptor agonists [70].
Dietary protein and amino acids orchestrate a complex hormonal response involving insulin, GLP-1, and glucagon that collectively influences glucose homeostasis. The direct effects on pancreatic islets combined with incretin-mediated mechanisms position protein as a potent modulator of metabolic regulation. Understanding these pathways provides crucial insights for developing targeted nutritional strategies and pharmacological interventions for diabetes, obesity, and related metabolic disorders. Future research should focus on personalized approaches that account for individual metabolic phenotypes, protein sources, and timing of ingestion to optimize metabolic outcomes.
Navigating Complexities: Protein Source, Dosage, and Context-Dependent Effects
This technical review examines the mechanistic and clinical evidence for the differential effects of animal and plant-based proteins on glycemic control and cardiometabolic outcomes. Findings from recent randomized controlled trials, meta-analyses, and cohort studies indicate that while both protein sources can improve metabolic parameters, plant proteins may offer superior benefits for certain cardiovascular risk factors when they replace red and processed meats. The effects are mediated through distinct amino acid profiles, digestion kinetics, gastrointestinal hormone responses, and accompanying food matrix components. This analysis synthesizes current evidence for researchers investigating dietary protein's role in glucose homeostasis and cardiometabolic disease prevention.
Dietary protein is essential for metabolic health, but emerging evidence suggests that its source—animal versus plant—significantly modifies its effects on glycemic control and cardiometabolic outcomes. The distinct physiological responses to these protein classes stem from fundamental differences in their amino acid composition, digestibility, and the non-protein components present in their food matrices. Understanding these differences is critical for developing targeted nutritional interventions for metabolic syndrome, type 2 diabetes (T2D), and cardiovascular disease (CVD) prevention.
Animal-based proteins (AP) typically contain all essential amino acids in sufficient proportions and have high digestibility (90-95%), while plant-based proteins (PP) often have lower digestibility (75-80%) and may be limited in certain essential amino acids like lysine, leucine, and methionine [71]. Beyond protein quality, the accompanying nutrients in whole food sources—such as saturated fats in animal products and fiber, polyphenols, and unsaturated fats in plants—create a complex nutritional signature that influences metabolic outcomes [72].
Mechanistic Insights: Pathways Mediating Protein Effects on Metabolism
Gastrointestinal Signaling Pathways
Dietary proteins influence glucose homeostasis through coordinated effects on gastrointestinal function. As illustrated below, protein digestion products stimulate hormone release and modulate gastric emptying, creating a cascade of signals that regulate appetite, insulin secretion, and glycemia.
This gastrointestinal signaling pathway illustrates how protein digestion products stimulate enteroendocrine cells to release hormones including cholecystokinin (CCK), glucagon-like peptide-1 (GLP-1), glucose-dependent insulinotropic polypeptide (GIP), and peptide YY (PYY) [73]. These hormones collectively slow gastric emptying, stimulate insulin secretion, and transmit satiety signals to the brain via vagal afferents and bloodstream signaling.
Animal and plant proteins differ in their capacity to stimulate these pathways due to variations in:
- Digestion kinetics: Whey protein is rapidly digested, leading to swift amino acid absorption and potent GLP-1 response, while casein forms gastric gels that prolong digestion [73].
- Amino acid specificity: Branched-chain amino acids (BCAAs), particularly leucine, are potent stimulators of insulin secretion and are more abundant in animal proteins [71].
- Hormone induction: Animal proteins generally elicit stronger insulinotropic effects than plant proteins, which may influence postprandial glucose disposal [71].
Postprandial Metabolism and Substrate Oxidation
The metabolic fate of dietary protein differs between sources. Animal proteins typically induce greater postprandial energy expenditure and diet-induced thermogenesis (DIT) compared to plant proteins [71]. This enhanced thermic effect may be attributed to the higher ATP cost of peptide bond utilization, increased gluconeogenesis, urea production, and protein synthesis stimulation by animal proteins rich in essential amino acids.
The following diagram illustrates the comparative postprandial metabolic responses to animal versus plant protein ingestion:
These divergent metabolic responses contribute to the differential long-term effects of animal and plant proteins on body weight, body composition, and glycemic control—factors critically important in metabolic disease prevention and management.
Clinical Evidence: Comparative Outcomes from Human Studies
Effects on Glycemic Control and Insulin Sensitivity
Clinical trials demonstrate that both animal and plant proteins can improve glycemic parameters, but through potentially different mechanisms. Animal proteins, particularly whey, have strong insulinotropic effects that can enhance postprandial glucose disposal, while plant proteins may improve insulin sensitivity through different pathways.
Table 1: Acute Effects of Different Protein Sources on Postprandial Glycemia and Energy Intake
| Protein Source | Dose (g) | Study Population | Effects on Glycemia | Effects on Energy Intake | Reference |
|---|---|---|---|---|---|
| Whey | 45 | T2D patients | Significant reduction in postprandial glucose | Not assessed | [73] |
| Casein | 45 | T2D patients | Moderate reduction in postprandial glucose | Not assessed | [73] |
| Pea Protein | 30 | Healthy adults | Moderate reduction in postprandial glucose | Significant reduction in subsequent energy intake | [73] |
| Soy Protein | 45 | T2D patients | Mild reduction in postprandial glucose | Moderate reduction in subsequent energy intake | [73] |
| Milk Blend (80% casein, 20% whey) | 30 | Healthy adults | Mild reduction in postprandial glucose | Moderate reduction in subsequent energy intake | [73] |
Long-term studies suggest that the source of dietary protein may have implications for diabetes risk. Epidemiological evidence indicates that long-term consumption of animal-based protein is associated with increased risk of T2D, while plant-based protein shows protective or neutral effects [73]. This may relate to the accompanying nutrients in animal protein foods (e.g., saturated fats) versus plant protein foods (e.g., fiber, antioxidants).
Impact on Cardiometabolic Risk Factors and Cardiovascular Disease
The ratio of plant to animal protein in the diet appears to significantly influence cardiovascular risk profiles. A landmark study using data from nearly 203,000 participants in the Nurses' Health Studies and Health Professionals Follow-up Study found that a higher ratio of plant to animal protein was associated with substantially lower cardiovascular disease (CVD) and coronary heart disease (CHD) risk [74].
Table 2: Cardiovascular Risk Reduction by Plant:Animal Protein Ratio
| Plant:Animal Protein Ratio | Comparison | CVD Risk Reduction | CHD Risk Reduction | Reference |
|---|---|---|---|---|
| ~1:1.3 (Highest) | vs. ~1:4.2 (Lowest) | 19% lower risk | 27% lower risk | [74] |
| ≥1:2 (with high total protein) | vs. low protein intake (16% of energy) | 28% lower risk | 36% lower risk | [74] |
The cardioprotective effects of plant proteins are likely mediated through multiple pathways, including improvements in blood lipid profiles, blood pressure, inflammatory biomarkers, and body weight management. Importantly, these benefits appear most pronounced when plant proteins replace red and processed meats rather than fish or dairy proteins [74].
Recent clinical trials have specifically examined how partial replacement of animal protein with plant protein affects metabolic syndrome components. A 2025 parallel randomized clinical trial with 73 participants with metabolic syndrome compared diets containing 70% plant-based protein/30% animal-based protein versus 30% plant-based protein/70% animal-based protein for 10 weeks [75]. Both groups showed significant improvements in weight, BMI, blood pressure, atherogenic index of plasma, and adropin levels. However, waist circumference and triglycerides decreased significantly only in the plant protein group, while HDL-cholesterol increased significantly only in the animal protein group [75]. Notably, between-group differences were not statistically significant, suggesting that both dietary patterns can be beneficial within a calorie-restricted diet.
Effects on Body Weight and Body Composition
Both animal and plant proteins contribute to satiety and weight management, but may operate through partially different mechanisms. Animal proteins generally exhibit stronger effects on satiety hormones and thermogenesis, while plant proteins benefit from the satiating effects of accompanying fiber and the lower energy density of plant-based foods.
Table 3: Effects of Protein Sources on Energy Expenditure and Substrate Oxidation
| Protein Comparison | Study Population | Effects on Energy Expenditure | Effects on Substrate Oxidation | Reference |
|---|---|---|---|---|
| Pork vs. Soy | Overweight-to-obese adults | Pork > Soy (1.9% higher) | Pork and soy not significantly different | [71] |
| Whey vs. Soy vs. Casein | Lean, healthy subjects | Whey > Soy and Casein | Fat oxidation: Whey > Soy | [71] |
| Whey vs. Pea Protein | Young and old men | Not significantly different | Fat oxidation: Not significantly different | [71] |
| Meat vs. Dairy vs. Soy | Healthy participants | Meat > Soy (1.1%, not significant) | Protein oxidation: Meat < Soy | [71] |
Long-term observational evidence suggests that dietary patterns emphasizing plant proteins are associated with lower body weight and reduced risk of obesity. A 2025 cross-sectional study of a nationally representative Brazilian population found that high intake of a whole plant-based dietary pattern was associated with significantly lower prevalence of obesity (OR 0.64) compared to low intake [76]. The food matrix and accompanying nutrients appear critically important, as processed plant-based foods showed weaker beneficial associations.
Experimental Methodologies for Protein Research
Clinical Trial Designs for Protein Interventions
Well-controlled clinical trials investigating protein sources require careful methodological consideration. The following diagram illustrates a representative study design from a recent randomized controlled trial comparing animal and plant protein effects in metabolic syndrome:
Key methodological considerations for protein intervention trials include:
- Dietary control: The 2025 trial used personalized dietary recommendations rather than provided foods, requiring careful monitoring of adherence [75].
- Intervention duration: Most trials range 8-12 weeks, sufficient to detect changes in metabolic parameters while maintaining adherence [75].
- Outcome measures: Comprehensive assessment should include anthropometrics, clinical biomarkers, and emerging biomarkers like adropin and atherogenic index of plasma (AIP) [75].
- Statistical approaches: Both intention-to-treat and per-protocol analyses are recommended to account for potential adherence issues [75].
Laboratory Assessments and Biomarkers
Advanced metabolic research incorporates multiple biomarker assessments to elucidate mechanisms:
- Glycemic control: Fasting glucose, insulin, HbA1c, oral glucose tolerance tests, continuous glucose monitoring [77].
- Lipid metabolism: Standard lipid panel plus atherogenic index of plasma (AIP) - a logarithmically transformed ratio of TG to HDL-c [75].
- Novel biomarkers: Adropin (energy homeostasis peptide), gastrointestinal hormones (CCK, GLP-1, GIP, PYY), inflammatory markers [75] [73].
- Body composition: DEXA, MRI, or CT for fat distribution, plus standard anthropometrics [75].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Protein Metabolism Studies
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Purified Proteins | Whey isolate, casein, soy protein isolate, pea protein concentrate | Controlled intervention studies; mechanistic research | Varying amino acid profiles; solubility characteristics; purity levels |
| Amino Acid Mixtures | Branched-chain amino acids (leucine, isoleucine, valine); essential amino acid blends | Mechanism elucidation; receptor studies | Species-specific requirements; ratio optimization |
| Biomarker Assays | ELISA kits for adropin, GLP-1, GIP, PYY, CCK; metabolic hormone panels | Outcome assessment; mechanism exploration | Sample stability; cross-reactivity; dynamic range |
| Stable Isotopes | ¹³C-labeled amino acids; ¹⁵N-labeled proteins | Metabolic trafficking studies; protein synthesis measures | Isotope enrichment analysis; mass spectrometry requirements |
| Cell Culture Systems | Enteroendocrine cell lines (STC-1, GLUTag); intestinal organoids | In vitro screening; pathway analysis | Physiological relevance; culture conditions |
The evidence synthesized in this review demonstrates that both animal and plant proteins can contribute beneficially to metabolic health, but through partially distinct mechanisms. Animal proteins generally exert stronger acute effects on satiety hormones, insulin secretion, and thermogenesis, while plant proteins offer advantages for long-term cardiovascular risk reduction, particularly when they replace red and processed meats.
Critical research gaps remain in understanding:
- The optimal plant:animal protein ratio for specific populations and health outcomes
- The role of specific protein types within the broad categories of "animal" and "plant" proteins
- The interaction between protein sources and the gut microbiome in modulating metabolic effects
- Long-term effects of protein substitutions on body composition, metabolic health, and diabetes risk
Future research should prioritize randomized controlled trials that control for the food matrix effect, mechanistic studies elucidating pathways affected by different protein sources, and personalized nutrition approaches considering genetic and metabolic heterogeneity in response to dietary proteins.
The Impact of Underlying Metabolic Health and Energy Status on Amino Acid Response
The physiological response to dietary amino acids is not uniform but is profoundly shaped by an individual's underlying metabolic health and energy status. This whitepaper synthesizes current evidence demonstrating how conditions such as obesity, insulin resistance, and physical inactivity modulate amino acid metabolism and signaling, ultimately influencing systemic glucose homeostasis. Central to this discussion is the dichotomous role of amino acids—particularly branched-chain amino acids (BCAAs)—which can acutely promote anabolic processes yet contribute to insulin resistance when chronically elevated in pathological states. This document provides a comprehensive technical guide, detailing key molecular pathways, experimental methodologies for assessing amino acid response, and essential research tools for investigators in the field of metabolic disease and drug development.
Amino acids function not only as building blocks for protein synthesis but also as critical signaling molecules that regulate metabolic pathways central to glucose homeostasis [78]. The impact of dietary protein and amino acid intake on insulin sensitivity, however, is complex and context-dependent. Research indicates that the same amino acids can produce beneficial or detrimental effects based on the metabolic health of the individual and the timing of exposure—a distinction primarily framed as acute postprandial versus chronic postabsorptive elevations [2]. In healthy, insulin-sensitive states, amino acids facilitate glucose disposal and promote muscle protein synthesis. In contrast, in metabolically compromised states such as obesity and type 2 diabetes (T2D), chronic elevations of specific amino acids, particularly BCAAs, are strongly associated with the pathogenesis of insulin resistance [1] [79]. This whitepaper explores the mechanisms underlying these divergent responses, emphasizing how metabolic phenotypes dictate amino acid metabolism and subsequent effects on glucose regulation.
Molecular Mechanisms: Key Signaling Pathways
The metabolic response to amino acids is governed by several highly conserved nutrient-sensing pathways. Understanding these mechanisms is crucial for developing targeted interventions.
The mTORC1 Signaling Axis
The mechanistic target of rapamycin complex 1 (mTORC1) serves as a primary sensor of amino acid availability, particularly leucine [78] [2]. Activation of mTORC1 promotes protein synthesis, cell growth, and anabolic processes. However, chronic activation of mTORC1, as seen with persistently high BCAA levels, can lead to inhibitory serine phosphorylation of insulin receptor substrate 1 (IRS-1), impairing insulin signaling and contributing to peripheral insulin resistance [1] [2]. This pathway represents a critical molecular bridge between amino acid availability and insulin action.
The SIRT1/PGC-1α Pathway and Mitochondrial Function
Sirtuin 1 (SIRT1) and peroxisome proliferator-activated receptor-gamma coactivator-1α (PGC-1α) are key regulators of mitochondrial biogenesis and function. Leucine and other essential amino acids can activate this pathway, enhancing oxidative metabolism and mitigating lipid-induced insulin resistance [2]. Conversely, downregulation of PGC-1α is linked to intramyocellular lipid accumulation, increased ceramide production, and impaired insulin signaling [2]. The integrity of this pathway is therefore essential for maintaining metabolic flexibility and insulin sensitivity in response to amino acid intake.
BCAA Metabolism and Insulin Resistance
BCAAs (leucine, isoleucine, valine) demonstrate a clear dual role in metabolic health. In obesity, their plasma levels are consistently elevated due to reduced oxidative capacity in liver and muscle tissues [79]. This impairment leads to accumulation of BCAA-derived metabolites that chronically activate mTORC1 and inhibit insulin signaling [1] [79]. Furthermore, BCAA catabolism is intimately linked to glucose metabolism; the enzyme branched-chain α-keto acid dehydrogenase (BCKDH) is regulated by phosphorylation, and its activity is diminished in insulin-resistant states, creating a vicious cycle of BCAA accumulation and worsening metabolic health [78].
The following diagram illustrates the core signaling pathways that connect amino acid availability to metabolic outcomes, highlighting the divergent effects based on metabolic context.
Diagram 1: Core signaling pathways linking amino acid availability to metabolic outcomes. The underlying metabolic health and energy status determine whether amino acid flux promotes healthy anabolism or contributes to insulin resistance.
Metabolic Phenotypes and Amino Acid Dysregulation
Metabolic health status dramatically alters amino acid metabolism and response. Research comparing metabolically healthy non-obese (MHN), metabolically healthy obese (MHO), and metabolically unhealthy obese (MUO) individuals reveals distinct amino acid network signatures.
Network analysis of plasma metabolomes shows that tryptophan maintains high centrality in MHN and MHO phenotypes, whereas phenylalanine becomes the central amino acid in MUO phenotypes [58]. This shift in network centrality suggests a fundamental rewiring of amino acid metabolism in progressive metabolic disease. Furthermore, pathway analyses reveal that phenylalanine-centered metabolic communities in obese groups are enriched with fatty acid oxidation pathways, indicating integrated dysregulation of amino acid and lipid metabolism [58].
Elevated circulating levels of BCAAs and aromatic amino acids (AAAs) like phenylalanine and tyrosine are strongly associated with insulin resistance and predict future risk of T2D [79]. Following metabolic and bariatric surgery (MBS), these amino acid levels decrease significantly, which correlates with improved insulin sensitivity independent of weight loss, highlighting their pathogenic role [79].
Table 1: Amino Acid Metabolites as Biomarkers of Metabolic Health and Surgical Outcomes
| Metabolite | Metabolic Role | Association with Metabolic Health | Clinical/Prognostic Insight |
|---|---|---|---|
| Isoleucine (BCAA) | Energy metabolism, insulin signaling | Elevated in obesity & insulin resistance [79] | Higher pre-op levels predict greater post-MBS weight loss [79] |
| Phenylalanine | Oxidative stress, neurotransmitter synthesis | Central node in MUO networks [58] | Marker of metabolic stress; predicts T2D improvement post-MBS [79] |
| L-DOPA | Dopamine precursor, β-cell signaling | - | Higher pre-op levels predict T2D remission post-MBS (AUC: 0.92) [79] |
| 3-HAA | Tryptophan metabolite, antioxidant, β-cell protector | - | Strongest predictor of insulin resistance improvement post-MBS [79] |
| IPA | Gut microbiota-derived indole metabolite | Decreased in metabolic dysfunction | ↑ Post-MBS correlates with improved insulin sensitivity [79] |
Experimental Methodologies for Assessing Amino Acid Response
Rigorous assessment of amino acid metabolism and its impact on glucose homeostasis requires specialized experimental protocols. Below are detailed methodologies for key approaches cited in the literature.
Dual Tracer Methodology for Whole-Body Leucine Kinetics
This method allows for the simultaneous measurement of whole-body protein synthesis, breakdown, and oxidation following amino acid ingestion [80].
Protocol:
- Tracer Administration: Primed, continuous intravenous infusions of two stable isotope tracers of leucine (e.g., [1-¹³C]leucine and [⁵,⁵,⁵-²H₃]leucine) are initiated after a baseline fasting period.
- Test Protein Ingestion: Participants ingest a single meal containing intrinsically labeled protein (e.g., ¹³C-leucine-labeled casein or whey protein).
- Blood Sampling: Frequent arterialized venous blood samples are collected over a prolonged period (e.g., 7-8 hours) postprandially.
- Sample Analysis: Plasma is analyzed via gas chromatography-mass spectrometry (GC-MS) to determine enrichments of leucine, α-ketoisocaproate (KIC, a transamination product), and expired ¹³CO₂.
- Kinetic Calculations: Using stochastic or compartmental models, whole-body leucine kinetics are calculated:
- Leucine Ra (Rate of Appearance): Reflects whole-body protein breakdown.
- Non-Oxidative Leucine Disposal: An indicator of whole-body protein synthesis.
- Leucine Oxidation: Determined from ¹³CO₂ excretion in breath.
Application: This protocol demonstrated that "slow" digesting casein promoted a more positive net leucine balance than "fast" digesting whey protein, despite identical leucine intake [80].
Hyperinsulinemic-Euglycemic Clamp with Leg Balance Technique
This gold-standard method assesses peripheral insulin sensitivity and tissue-specific glucose disposal, and can be combined with amino acid tracer infusion.
Protocol:
- Catheterization: Insert catheters into an artery (e.g., radial), a peripheral vein for infusions, and a deep vein (e.g., femoral) for deep venous blood sampling.
- Baseline Period: Measure basal arterial and deep venous substrate (glucose, amino acids) concentrations and blood flow via Doppler ultrasound.
- Clamp Initiation: A primed, continuous intravenous infusion of insulin is started at a fixed rate (e.g., 40 mU/m²/min) to achieve hyperinsulinemia. Simultaneously, a variable rate of 20% glucose is infused to maintain euglycemia (~5 mmol/L).
- Tracer Co-Infusion: Amino acid tracers (e.g., [¹³C]leucine) can be co-infused to measure protein metabolism under insulin-stimulated conditions.
- Steady-State Measurement: Once steady-state is achieved (typically after 2 hours), repeated paired arterial and deep venous blood samples are taken alongside blood flow measurements.
- Calculations:
- Whole-Body M-value: Glucose infusion rate (GIR) during steady-state, normalized to body weight, reflects whole-body insulin sensitivity.
- Leg Glucose Uptake: (Arterial [glucose] - Venous [glucose]) × Blood Flow.
Application: This method has quantified the rapid decline in insulin-stimulated leg glucose uptake (45%) and muscle protein synthesis following short-term bed rest [2].
Metabolomic Profiling for Phenotypic Stratification
High-throughput metabolomics enables the systematic identification of amino acid signatures associated with metabolic phenotypes and intervention outcomes.
Protocol:
- Sample Collection & Preparation: Collect plasma/serum samples from fasted subjects. Deproteinize using cold methanol or acetonitrile. Derivatize if necessary for analysis.
- Liquid Chromatography-High Resolution Mass Spectrometry (LC-HRMS):
- Separation: Use reverse-phase (e.g., C18) or HILIC columns to separate metabolites.
- Detection: Analyze samples with a high-resolution mass spectrometer (e.g., Q-TOF, Orbitrap) in both positive and negative electrospray ionization modes.
- Data Processing: Use software (e.g., XCMS, Progenesis QI) for peak picking, alignment, and normalization. Identify metabolites by matching accurate mass and fragmentation spectra to databases (e.g., HMDB, METLIN).
- Statistical & Network Analysis:
- Multivariate Analysis: Employ Partial Least Squares-Discriminant Analysis (PLS-DA) to identify metabolites (e.g., BCAAs, AAAs) that best discriminate between groups (MHN, MHO, MUO) [58].
- Network Analysis: Construct metabolic networks and calculate Eigenvector Centrality Scores to identify key hub metabolites (e.g., the shift from Tryptophan to Phenylalanine centrality in MUO) [58].
- Predictive Modeling: Use Receiver Operating Characteristic (ROC) analysis to evaluate the predictive power of specific metabolites (e.g., L-DOPA, 3-HAA) for clinical outcomes like T2D remission post-MBS [79].
The following diagram outlines a typical workflow for a metabolomic study designed to investigate amino acid responses.
Diagram 2: Experimental workflow for metabolomic profiling in amino acid research. LC-HRMS = Liquid Chromatography-High Resolution Mass Spectrometry; PLS-DA = Partial Least Squares-Discriminant Analysis; ROC = Receiver Operating Characteristic.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Investigating Amino Acid Metabolism
| Reagent / Material | Function / Application | Example Use in Research |
|---|---|---|
| Stable Isotope Tracers (e.g., [¹³C]Leucine, [²H₃]Leucine) | Quantitative metabolic flux analysis; measurement of protein synthesis, breakdown, and oxidation. | Dual tracer methodology for whole-body leucine kinetics [80]. |
| Intrinsically Labeled Dietary Proteins (e.g., ¹³C-Casein, ¹³C-Whey) | Track metabolic fate of ingested protein without altering physicochemical properties. | Comparing postprandial metabolism of "slow" vs. "fast" proteins [80]. |
| Hyperinsulinemic-Euglycemic Clamp Setup (Insulin, 20% Dextrose, infusion pumps) | Gold-standard assessment of insulin sensitivity in vivo. | Measuring bed rest-induced insulin resistance and the impact of amino acid supplementation [2]. |
| LC-HRMS Platform with UPLC/HILIC and Q-TOF/Orbitrap | High-coverage, high-sensitivity identification and quantification of plasma amino acids and metabolites. | Metabolomic phenotyping and discovery of predictive biomarkers for surgical outcomes [79] [58]. |
| Specific Pathway Modulators (e.g., Rapamycin, AICAR, SR-18292) | Pharmacological inhibition/activation of key nodes (mTORC1, AMPK, PGC-1α) to establish mechanistic causality. | Elucidating the role of mTORC1 in BCAA-induced insulin resistance [1] [2]. |
| ELISA/Kits for Hormones & Cytokines (Insulin, Leptin, Adiponectin, Inflammatory markers) | Assess endocrine and inflammatory context of amino acid intervention. | Correlating amino acid levels with insulin resistance and metabolic inflammation [79]. |
The response to dietary amino acids is highly personalized, contingent upon an individual's metabolic phenotype, energy status, and the health of key metabolic tissues. The evidence underscores that chronic elevations of BCAAs and a shift in amino acid network centrality toward phenylalanine are hallmarks of unhealthy obesity and insulin resistance. Future research must prioritize longitudinal studies that track individual responses to controlled amino acid challenges across the spectrum of metabolic health. Integrating metabolomic data with other omics technologies (proteomics, genomics) and advanced network analysis will be crucial for developing personalized nutritional strategies and pharmacologic interventions that target amino acid metabolism to restore glucose homeostasis. The tools and methodologies detailed herein provide a foundation for such innovative research, paving the way for more effective, precision-based approaches to combat metabolic disease.
Addressing the Risks of Chronic Postabsorptive BCAA Elevation and Nutrient Overload
Branched-chain amino acids (BCAAs)—leucine, isoleucine, and valine—are essential nutrients with dual roles in metabolism, serving as both substrates for protein synthesis and critical signaling molecules. While their anabolic properties are well-recognized, chronic elevation of postabsorptive BCAA levels is increasingly identified as a significant risk factor for metabolic disease pathogenesis. This whitepaper synthesizes current evidence elucidating the mechanisms by which chronic BCAA excess, particularly under conditions of nutrient overload, contributes to insulin resistance, cardiovascular impairment, and overall metabolic dysregulation. We further explore therapeutic strategies targeting BCAA catabolism and provide standardized experimental methodologies for investigating BCAA-mediated metabolic consequences, offering a resource for researchers and drug development professionals working at the intersection of nutrition and metabolic disease.
Branched-chain amino acids (BCAAs) constitute approximately 20% of dietary protein intake and are unique among essential amino acids for their extensive metabolism in skeletal muscle rather than the liver [81]. In the postprandial state, BCAAs, particularly leucine, act as potent nutrient signals that activate the mechanistic target of rapamycin (mTOR) pathway, promoting muscle protein synthesis and supporting metabolic health [2]. However, chronic elevation of postabsorptive BCAA levels—a hallmark of obesity and insulin resistance—shifts this signaling from adaptive to maladaptive, contributing to the pathogenesis of type 2 diabetes (T2D) and cardiovascular disease [82] [81].
Epidemiological and clinical studies consistently demonstrate that fasting plasma BCAA levels are elevated by 20-50% in individuals with obesity and insulin resistance compared to healthy controls [81] [83]. These elevated levels not only correlate with insulin resistance but also predict future diabetes development, suggesting a potential causative role [81]. The mechanisms underlying this association involve complex interactions between dietary intake, tissue-specific catabolic efficiency, and cellular signaling pathways that become dysregulated under conditions of chronic nutrient excess.
Mechanisms Linking Chronic BCAA Elevation to Metabolic Dysregulation
Dysregulation of Insulin Signaling and Glucose Homeostasis
Chronic BCAA elevation impairs insulin sensitivity through multiple interconnected mechanisms. Unlike acute postprandial elevations that transiently activate mTOR to support protein synthesis, persistent fasting hyperaminoacidemia leads to chronic mTOR activation, resulting in phosphorylation of insulin receptor substrate-1 (IRS-1) at inhibitory serine residues rather than activating tyrosine residues [2]. This aberrant phosphorylation impairs downstream insulin signaling, reducing glucose transporter type 4 (GLUT4) translocation and diminishing peripheral glucose uptake.
Table 1: Mechanisms of BCAA-Induced Insulin Resistance
| Mechanism | Molecular Pathway | Metabolic Consequence |
|---|---|---|
| Chronic mTOR Activation | IRS-1 serine phosphorylation | Impaired insulin signal transduction |
| Mitochondrial Dysfunction | Reduced PGC-1α expression, Accumulation of lipid intermediates | Decreased oxidative capacity, Lipotoxicity |
| Cellular Stress | Increased oxidative stress, Ceramide accumulation | Insulin signaling inhibition |
| Hepatic Metabolism | Altered gluconeogenic regulation | Hyperglycemia |
Furthermore, BCAA catabolism is intrinsically linked to mitochondrial function. Dysfunctional BCAA metabolism reduces peroxisome proliferator-activated receptor-gamma coactivator-1α (PGC-1α) expression, a master regulator of mitochondrial biogenesis [2]. This suppression contributes to the accumulation of lipid intermediates such as ceramides and diacylglycerols in skeletal muscle and liver, which further inhibit insulin signaling through activation of protein kinase C isoforms and pro-inflammatory pathways [2] [81].
BCAA-Mediated Cardiovascular Risk Pathways
Emerging evidence indicates that chronic BCAA elevation adversely affects cardiovascular health. Amino acids derived from animal protein, particularly leucine, trigger signaling activity in macrophage cells that normally clear debris from blood vessels [84]. When consumed in excess, this leucine-mediated signaling becomes overactive, leading to accumulation of spent cells in the vascular system that promote plaque buildup and atherosclerosis [84]. This mechanism explains the association between high-protein diets enriched in BCAAs and increased risk of heart attack and stroke, with research indicating that consuming more than 22% of daily calories from protein carries significant cardiovascular downside risk [84].
Amino Acid Imbalance and Appetite Dysregulation
Beyond their direct signaling effects, chronically elevated BCAAs create an amino acid imbalance that disrupts central regulation of appetite. Research demonstrates that diets with disproportionately high BCAA content relative to other essential amino acids, particularly tryptophan and threonine, trigger compensatory hyperphagia as organisms attempt to reach their target intake of these limiting amino acids [85]. This BCAA-induced hyperphagia drives increased energy intake and weight gain, exacerbating nutrient overload. The mechanism involves competition for transport across the blood-brain barrier, where elevated BCAAs reduce tryptophan availability and subsequent serotonin synthesis, a key neurotransmitter regulating satiety [85].
Methodological Approaches for Investigating BCAA Metabolism
Acute BCAA Challenge Protocol
Purpose: To assess the direct effects of BCAA elevation on glucose homeostasis and insulin sensitivity independent of long-term adaptive changes.
Experimental Model: 3-month-old male and female C57BL/6J mice (Stock No. 000664, Jackson Laboratory), group-housed with ad libitum access to regular chow diet (Lab diet, 5001) and water [82].
Intervention:
- Prepare 150 mM BCAA solution in saline (~450 mOsm/l) using a standardized 2:1:1 ratio (leucine:isoleucine:valine) reflecting typical dietary proportions [82].
- Administer single infusion via jugular vein catheter (2.25 mmole/kg BW) based on mean single meal size of a 30g mouse (~0.216 g) [82].
- For intraperitoneal injection, use 10 µl/g BW of 225 mM BCAA solution [82].
Assessment Timeline:
- Baseline (-30 min): Collect fasting blood samples via catheter.
- Acute Response (0-120 min): Frequent blood sampling at 0, 15, 30, 60, 90, 120 min post-infusion for glucose and insulin measurements.
- Glucose Tolerance Test (120-180 min): Administer glucose load (1-2 g/kg) with sampling every 15-30 min.
- Hyperinsulinemic-Euglycemic Clamp (Separate cohort): Maintain constant BCAA infusion during clamp to assess whole-body insulin sensitivity [82].
Chronic BCAA Dietary Manipulation Model
Purpose: To investigate long-term metabolic adaptations to BCAA manipulation and identify amino acid imbalance effects.
Experimental Design:
- Utilize isocaloric diets (e.g., 18% total protein, 64% carbohydrate, 18% fat) with varying BCAA content against fixed macronutrient background [85].
- Implement four dietary conditions: BCAA200 (200% standard), BCAA100 (control, 100% standard), BCAA50 (50% standard), BCAA20 (20% standard) [85].
- Maintain 312 male and female C57BL/6J mice on assigned diets for lifespan analysis or euthanize at 15 months for tissue analysis [85].
Outcome Measures:
- Energy Homeostasis: Daily food intake, body weight, body composition (EchoMRI).
- Glucose Metabolism: Glucose tolerance tests, insulin tolerance tests, hyperinsulinemic-euglycemic clamps.
- Molecular Analyses: Hepatic mTOR signaling (phospho-mTOR, phospho-S6K, phospho-AKT), plasma metabolomics (LC-QQQ-MS).
- Lifespan & Healthspan: Survival analysis, age-related pathology assessment.
Pharmacological BCAA Reduction Approach
Purpose: To determine whether reducing elevated BCAA levels improves metabolic parameters.
Intervention:
- Utilize BCKD kinase inhibitor BT2 (3,6-dichlorobenzo[b]thiophene-2-carboxylic acid) to enhance BCAA catabolism [82] [86].
- Prepare BT2 formulation: dissolve in DMSO, then add to mixture of Cremophor EL and 0.1 M sodium bicarbonate (pH 9.0) for final concentration of 4 mg/mL in 5% DMSO, 10% Cremophor EL, and 85% of 0.1 M sodium bicarbonate [82].
- Administer single injection (15-120 mg/kg) or once-daily dosing for chronic studies [86].
Assessment: Monitor plasma and cardiac BCAA/BCKA levels via mass spectrometry, glucose tolerance, insulin sensitivity, and in hyperinsulinemic-euglycemic clamps [86].
Table 2: Quantitative Effects of BCAA Manipulation on Metabolic Parameters
| Parameter | Acute BCAA Infusion [82] | Chronic High BCAA Diet [85] | BT2 Treatment [86] |
|---|---|---|---|
| Plasma BCAA | Increase ~40-60% | Plateau at ~40 μg/ml despite 2x intake | Reduction up to 40% |
| Blood Glucose | Acutely elevated | Normal fasting, elevated during GTT | Improved glucose tolerance |
| Insulin Sensitivity | Impaired during clamp | Progressive deterioration | Improved insulin sensitivity |
| Food Intake | Not assessed | ~20% increase (BCAA200) | Not reported |
| Body Weight/Adiposity | Not assessed | Significantly increased | Not reported |
| Lifespan | Not assessed | ~10% reduction (BCAA200) | Not reported |
Molecular Pathways in BCAA Metabolism and Signaling
BCAA metabolism involves a tightly regulated enzymatic cascade that becomes dysregulated under conditions of nutrient overload. The first step is reversible transamination by branched-chain amino acid aminotransferase (BCAT) to form branched-chain α-keto acids (BCKAs), followed by irreversible oxidative decarboxylation by the branched-chain α-keto acid dehydrogenase (BCKD) complex, the rate-limiting enzyme in BCAA catabolism [81]. BCKD activity is regulated by phosphorylation-dephosphorylation mechanisms, with BCKD kinase (BCKDK) inhibiting and protein phosphatase 2Cm (PP2Cm) activating the complex [86].
The diagram above illustrates the core BCAA catabolic pathway and its relationship to insulin resistance development. Under conditions of nutrient overload or genetic predisposition, impaired BCKD activity leads to BCAA accumulation, resulting in chronic mTOR activation and subsequent inhibition of insulin signaling through IRS-1 serine phosphorylation. Pharmacological inhibition of BCKDK with compounds like BT2 enhances BCAA catabolism and represents a promising therapeutic approach for conditions characterized by BCAA elevation.
Research Reagent Solutions for BCAA Investigations
Table 3: Essential Research Tools for BCAA Metabolism Studies
| Reagent/Model | Specifications | Research Application |
|---|---|---|
| BT2 (BCKDK Inhibitor) | 3,6-dichlorobenzo[b]thiophene-2-carboxylic acid; Formulation: 4 mg/mL in 5% DMSO, 10% Cremophor EL, 85% 0.1 M sodium bicarbonate (pH 9.0) [82] [86] | Enhances BCAA catabolism; Dosing: 15-120 mg/kg single or repeated administration |
| Defined BCAA Diets | Isocaloric diets with fixed macronutrient background (e.g., 18% protein, 64% carbohydrate, 18% fat) with varying BCAA:non-BCAA ratios [85] | Investigates amino acid imbalance effects; Enables pair-feeding studies to isolate hyperphagia effects |
| AAV8-hSyn-DIO-hM3Dq-mCherry | pAAV-hSyn-DIO-hM3D(Gq)-mCherry (#44361-AAV8, Addgene) [82] | Chemogenetic activation of specific neuronal populations (e.g., AgRP neurons) to study neural circuits in BCAA metabolism |
| Stable Isotope Tracers | [1-¹³C] or [1-¹⁴C]-leucine for flux studies [81] | Quantifies protein turnover, BCAA flux and oxidation rates in different metabolic states |
| Targeted Metabolomics | LC-QQQ-MS for BCAA, BCKA, tryptophan metabolites [85] | Comprehensive profiling of amino acids and related metabolites in plasma and tissues |
Chronic elevation of postabsorptive BCAAs represents a significant metabolic risk factor under conditions of nutrient overload, contributing to insulin resistance, cardiovascular disease, and appetite dysregulation through multiple interconnected mechanisms. The evidence reviewed herein supports a model wherein persistent fasting hyperaminoacidemia leads to chronic mTOR activation, impaired mitochondrial function, and amino acid imbalance that collectively disrupt metabolic homeostasis.
Therapeutic strategies targeting BCAA metabolism show considerable promise, with pharmacological enhancement of BCAA catabolism via BCKDK inhibition demonstrating efficacy in preclinical models for improving glucose homeostasis and insulin sensitivity [86] [81]. Additionally, dietary approaches that maintain appropriate ratios of BCAAs to other essential amino acids, particularly tryptophan and threonine, may prevent the hyperphagia and weight gain associated with amino acid-imbalanced diets [85].
Future research should focus on elucidating tissue-specific contributions to BCAA metabolism, particularly the role of adipose tissue, and developing targeted interventions that enhance BCAA catabolism without compromising the anabolic functions of postprandial BCAA signaling. The experimental methodologies outlined in this whitepaper provide a standardized framework for advancing our understanding of how dietary proteins and amino acids influence glucose homeostasis, ultimately contributing to improved therapeutic strategies for metabolic disease.
Gut Microbiome-Dependent and Independent Pathways in Diet-Induced Metabolic Inflammation
Diet-induced metabolic inflammation is a critical pathological process linking modern dietary patterns to the disruption of glucose homeostasis and the development of chronic metabolic diseases. This complex process unfolds through two interconnected yet distinct pathways: one mediated by the gut microbiome and another operating independently of microbial influence. Within the context of dietary proteins and amino acids research, understanding these pathways is paramount for developing targeted nutritional and therapeutic strategies. The gut microbiota modulates host metabolism through the production of bioactive metabolites from dietary components, while simultaneously, dietary elements can directly activate host inflammatory signaling regardless of microbial presence. This whitepaper provides an in-depth technical analysis of the mechanisms underlying both pathways, with particular emphasis on their implications for glucose regulation and protein metabolism research. We synthesize current experimental evidence, delineate methodological approaches for pathway dissection, and visualize key signaling networks to provide researchers and drug development professionals with a comprehensive resource for navigating this complex physiological landscape.
Gut Microbiome-Dependent Pathways
The gut microbiota serves as a crucial intermediary in diet-induced metabolic inflammation, translating dietary signals, particularly from fibers and proteins, into biochemical messages that regulate host inflammation and glucose metabolism. These microbiome-dependent effects are primarily mediated through microbial structural components and metabolites derived from dietary fermentation.
Key Microbial Metabolites and Mechanisms
Table 1: Key Microbial Metabolites in Diet-Induced Metabolic Inflammation
| Metabolite | Dietary Precursor | Producing Bacteria | Receptors/Pathways | Net Effect on Inflammation |
|---|---|---|---|---|
| Short-chain fatty acids (SCFAs) | Dietary fiber | Bifidobacterium, Lactobacillus, Faecalibacterium prausnitzii | GPR41/43, HDAC inhibition | Anti-inflammatory [87] [88] |
| Trimethylamine N-oxide (TMAO) | Choline, L-carnitine | Enterobacteriaceae | MAPK, NF-κB | Pro-inflammatory [89] [90] |
| Lipopolysaccharide (LPS) | Gram-negative bacterial membranes | Enterobacteriaceae | TLR4, NF-κB | Pro-inflammatory [89] [91] |
| Secondary bile acids | Primary bile acids | Bacteroides, Clostridium | FXR, TGR5 | Mixed (context-dependent) [89] [90] |
| Branched-chain fatty acids | Branched-chain amino acids | Various | PPARγ, mTOR | Pro-inflammatory [92] [91] |
| Tryptophan derivatives | Tryptophan | Lactobacillus | Aryl hydrocarbon receptor | Anti-inflammatory [89] [90] |
Mechanistic Insights
Short-chain fatty acids (SCFAs), including acetate, propionate, and butyrate, are produced through microbial fermentation of dietary fibers and resistant starches. These metabolites signal through G-protein coupled receptors (GPR41 and GPR43) on intestinal epithelial and immune cells, leading to enhanced gut barrier function and reduced inflammation through inhibition of NF-κB signaling [88] [93]. Butyrate additionally inhibits histone deacetylases (HDACs), promoting anti-inflammatory gene expression programs and supporting glucose homeostasis through enhanced insulin sensitivity [87] [94]. Inconsistent microbial responses in human trials highlight significant interindividual variation, with gut barrier integrity and inflammatory markers proving more reliable indicators of benefit than microbial composition changes alone [87].
Lipopolysaccharide (LPS) from Gram-negative bacteria promotes metabolic inflammation through TLR4 activation, particularly in the context of high-fat diets. This triggering of innate immune pathways induces insulin resistance in peripheral tissues and activates adipose tissue inflammation, establishing a chronic low-grade inflammatory state that disrupts glucose homeostasis [89] [95]. Elevated circulating LPS levels correlate with increased abundance of Proteobacteria and Enterobacteriaceae species observed in obesity and type 2 diabetes [92] [91].
Branched-chain amino acids (BCAAs) and their microbial metabolites activate mTORC1-PPARγ signaling, driving adipogenesis and adipose tissue inflammation. Recent human metabolomic studies reveal elevated circulating BCAAs in obese individuals, with specific microbial taxa enriched in BCAA metabolic pathways [92] [91]. This microbial BCAA metabolism represents a crucial interface between dietary protein intake and host metabolic inflammation, with significant implications for glucose regulation.
Gut Microbiome-Independent Pathways
Dietary components can directly instigate metabolic inflammation through host-specific pathways without microbial intermediation. These microbe-independent mechanisms are particularly relevant for understanding the direct inflammatory effects of specific dietary lipids, proteins, and advanced glycation end-products.
Direct Dietary Signaling Mechanisms
Table 2: Microbiome-Independent Pro-Inflammatory Dietary Components
| Dietary Component | Target Receptors/Pathways | Cellular Effects | Impact on Glucose Homeostasis |
|---|---|---|---|
| Saturated fatty acids | TLR2/TLR4, NLRP3 inflammasome | Macrophage infiltration, IL-1β secretion | Insulin resistance [95] |
| Trans-fatty acids | ASK1-p38 MAPK pathway | Mitochondrial dysfunction, ER stress | Impaired insulin signaling [95] |
| Advanced glycation end-products (AGEs) | RAGE | NF-κB activation, oxidative stress | Vascular dysfunction, insulin resistance [89] |
| High glucose concentrations | PKC, AGE/RAGE, hexosamine pathways | Mitochondrial oxidative stress | Glucotoxicity, β-cell dysfunction [89] |
| Oxidized LDL | CD36, TLR4 | Foam cell formation, inflammation | Atherosclerosis, endothelial dysfunction [95] |
Molecular Mechanisms
Saturated fatty acids directly activate TLR2 and TLR4 signaling on macrophages and adipocytes, initiating NF-κB-mediated transcription of pro-inflammatory cytokines including TNF-α, IL-1β, and IL-6 [95]. This cascade recruits immune cells to adipose tissue, establishing a chronic inflammatory state that disrupts insulin signaling through serine phosphorylation of insulin receptor substrate (IRS) proteins. The resulting insulin resistance represents a key defect in glucose homeostasis [89] [95].
Metabolically stressed tissues release damage-associated molecular patterns (DAMPs) such as mitochondrial DNA and ATP, which activate the NLRP3 inflammasome independently of microbial signals [95]. In pancreatic β-cells, glucolipotoxicity induces similar sterile inflammatory responses that contribute to β-cell dysfunction and apoptosis, further compromising glucose regulation [89].
Dietary advanced glycation end-products (AGEs) engage the receptor for AGEs (RAGE), activating multiple signaling pathways including JAK/STAT, PI3K/Akt, and MAPK/NF-κB in various cell types [89]. This signaling promotes oxidative stress, proinflammatory gene expression, and profibrotic remodeling, ultimately contributing to myocardial stiffening and diastolic dysfunction in diabetic cardiomyopathy [89].
Experimental Approaches for Pathway Dissection
Disentangling microbiome-dependent and independent effects requires carefully controlled experimental designs and specific methodological approaches.
Model Systems and Methodologies
Table 3: Experimental Approaches for Pathway Differentiation
| Methodology | Key Applications | Advantages | Limitations |
|---|---|---|---|
| Germ-free (GF) mice | Direct comparison with conventionalized counterparts | Complete absence of microbiota; allows FMT studies | Altered immune development; physiological differences [88] [95] |
| Antibiotic depletion | Acute microbiota elimination in established models | Temporal control over microbial ablation | Off-target effects; incomplete depletion [88] [91] |
| Fecal microbiota transplantation (FMT) | Establish causal role of microbiota | Transfers microbial community phenotypes | Strain-specific effects; variable engraftment [87] [91] |
| Gnotobiotic models | Reductionist approach with defined microbial consortia | Precise control over microbial composition | Limited complexity; may not reflect natural state [88] [96] |
| Specific pathogen-free (SPF) models | Standardized baseline microbiota | Consistent experimental baseline | Facility-specific microbial differences [95] |
Protocol for Microbiome-Dependent Pathway Analysis
Fecal Microbiota Transplantation in Metabolic Inflammation Research:
Donor Selection: Recruit human donors with defined phenotypes (e.g., lean vs. obese, diabetic vs. normoglycemic) or use diet-induced animal models. Characterize donor microbiota through 16S rRNA sequencing and metabolomic profiling [92] [91].
Fecal Slurry Preparation: Homogenize fresh or frozen fecal material in sterile anaerobic PBS (100 mg/mL). Centrifuge at low speed (500 × g, 2 min) to remove large particulate matter [91].
Recipient Preparation: Utilize germ-free or antibiotic-treated (e.g., ampicillin 1 mg/mL, vancomycin 0.5 mg/mL in drinking water for 2-4 weeks) murine models. For metabolic studies, C57BL/6J males at 8-10 weeks are commonly used [95] [91].
Transplantation Protocol: Administer 200 μL of fecal slurry via oral gavage daily for 3 consecutive days. Maintain control groups receiving vehicle or autoclaved slurry [91].
Phenotypic Assessment: Monitor body weight, food intake, and body composition for 4-8 weeks post-FMT. Perform glucose tolerance tests (IPGTT) and insulin tolerance tests (ITT) at defined endpoints. Collect tissues for molecular analysis including:
Protocol for Microbiome-Independent Pathway Analysis
Germ-Free Mouse Studies for Direct Dietary Effects:
Germ-Free Mouse Maintenance: Maintain GF mice in flexible film isolators with autoclaved food, water, and bedding. Regularly monitor sterility through bacterial culture and PCR of fecal samples [95].
Dietary Interventions: Utilize defined diets with controlled macronutrient composition:
- High-fat diet (60% kcal from fat, primarily lard)
- High-sucrose/fructose diet (50-60% kcal from simple sugars)
- Western-style diet (high fat and high sugar combined)
- Control matched diets with identical micronutrient profiles [95]
Metabolic Phenotyping: In vivo assessments include:
- Weekly body weight and body composition (EchoMRI)
- Energy expenditure and respiratory quotient (indirect calorimetry)
- Glucose and insulin tolerance tests
- Tissue collection for histological and molecular analyses [95]
Immune Phenotyping: Flow cytometric analysis of immune cells in adipose tissue, liver, and intestine. Measure cytokine profiles in serum and tissues. Histological assessment of crown-like structures in adipose tissue [95].
Signaling Pathways and Molecular Mechanisms
The following diagrams visualize key signaling pathways in diet-induced metabolic inflammation, highlighting both microbiome-dependent and independent mechanisms.
Microbiome-Dependent Inflammatory Signaling
Diagram 1: Microbial metabolite signaling in metabolic inflammation. SCFAs from fiber fermentation exert anti-inflammatory effects via GPR41/43 and HDAC inhibition, while LPS from dysbiotic microbiota triggers TLR4-NF-κB-mediated inflammation and insulin resistance.
Microbiome-Independent Dietary Signaling
Diagram 2: Microbiome-independent dietary signaling. Saturated fats, DAMPs, and AGEs activate innate immune receptors and inflammasomes, promoting inflammation and insulin resistance through direct host pathways.
Research Reagent Solutions
Table 4: Essential Research Reagents for Metabolic Inflammation Studies
| Reagent/Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Gnotobiotic Models | Germ-free C57BL/6J mice | Pathway dissection | Enable microbiota-controlled studies [88] [95] |
| Antibiotic Cocktails | Ampicillin, vancomycin, neomycin | Microbiota depletion | Eliminate specific microbial groups [88] [91] |
| TLR Signaling Inhibitors | TAK-242 (TLR4), CU-CPT22 (TLR2) | Mechanistic studies | Block specific pattern recognition receptors [95] |
| Metabolite Analogs | Sodium butyrate, propionate | SCFA signaling studies | Activate GPR41/43, inhibit HDACs [87] [93] |
| Cytokine Assays | Luminex, ELISA for TNF-α, IL-6, IL-1β | Inflammation quantification | Measure inflammatory endpoints [92] [95] |
| 16S rRNA Sequencing | V3-V4 region primers, Illumina MiSeq | Microbial composition | Characterize community structure [92] [96] |
| Metabolomics Platforms | LC-MS/MS, GC-MS | Metabolite profiling | Quantify SCFAs, BCAAs, TMAO [92] [90] |
| Flow Cytometry Panels | CD45, CD11b, F4/80, CD3 | Immune phenotyping | Characterize tissue immune cells [95] |
The intricate interplay between gut microbiome-dependent and independent pathways in diet-induced metabolic inflammation represents a fundamental biological framework with profound implications for understanding glucose homeostasis disruption. Microbial metabolites including SCFAs, LPS, and BCAAs modulate host inflammation and insulin sensitivity through specific receptor-mediated pathways, while dietary components simultaneously activate parallel inflammatory cascades directly through host signaling systems. This dual-pathway model underscores the complexity of nutritional physiology and highlights the necessity of integrated experimental approaches that account for both microbial and host contributions. For research focused on dietary proteins and amino acids, these pathways offer complementary mechanistic insights: microbiome-dependent processing of protein-derived substrates generates bioactive metabolites, while direct amino acid sensing and signaling occurs through host nutrient-sensing pathways. Future research integrating multi-omics technologies, precisely engineered microbial consortia, and tissue-specific pathway manipulation will further elucidate these complex interactions, ultimately advancing targeted nutritional and therapeutic strategies for metabolic diseases. The experimental frameworks and methodological considerations outlined in this technical guide provide researchers with essential tools for navigating this rapidly evolving field and developing interventions that simultaneously target both microbial and host pathways for optimal metabolic health.
Optimizing Protein Quality, Timing, and Bioavailability for Therapeutic Efficacy
Therapeutic proteins and dietary amino acids play a critical role in modulating metabolic health, particularly glucose homeostasis. Glucose homeostasis—the maintenance of blood glucose within a tight physiological range (4-6 mmol/L)—is primarily regulated by pancreatic insulin and glucagon secretion [65]. Disruption of this system, characterized by insulin resistance and β-cell dysfunction, underlies type 2 diabetes mellitus (T2DM), a global health epidemic affecting hundreds of millions worldwide [65]. Dietary proteins modulate glucose homeostasis through multiple insulinotropic mechanisms, including direct stimulation of insulin secretion from pancreatic β-cells, potentiation of incretin hormones (GLP-1 and GIP), and enhancement of satiety signals [65]. Beyond their nutritional value, therapeutic proteins have emerged as a major class of pharmaceuticals, with nearly 380 marketed products and a global market projected to reach $655.7 billion by 2029 [97] [98]. However, their efficacy is constrained by inherent limitations in stability, bioavailability, and optimal timing. This review synthesizes current evidence on strategic optimization of protein quality, timing, and bioavailability to maximize therapeutic efficacy, with particular emphasis on applications in glucose homeostasis research.
Protein Quality: Source, Composition, and Functional Efficacy
Structural Determinants of Protein Quality
Protein quality is fundamentally determined by amino acid composition, digestibility, and structural properties. Both animal and plant proteins comprise 20 amino acids, nine of which are essential and must be obtained through diet [99]. The conformational structure of proteins significantly influences their digestibility, with tightly folded globular proteins and those containing hydrophobic cores being more resistant to enzymatic hydrolysis [99]. Table 1 compares key characteristics of major dietary protein sources and their implications for glucose metabolism.
Table 1: Protein Sources and Metabolic Impacts
| Protein Source | Amino Acid Profile | Digestibility Considerations | Documented Effects on Glucose Homeostasis |
|---|---|---|---|
| Whey | Complete, high BCAA | Rapid digestion | Potent insulinotropic effects; enhances postprandial insulin response [65] |
| Casein | Complete | Slow digestion due to coagulation | Sustained amino acid release; moderate insulin secretion [43] |
| Plant Proteins (Pea, Soy) | Often incomplete (limiting methionine, lysine) | Variable; anti-nutrients (phytates, tannins) may limit bioavailability [99] | Fish gelatin and pea proteins demonstrated reduced intestinal glucose absorption in vitro and ex vivo [43] |
| Animal Proteins (Egg, Meat) | Complete | Generally high bioavailability | Higher intake associated with insulin resistance via BCAA mechanisms in some studies [100] [65] |
Impact of Protein Source on Glucose Regulation
The protein source significantly influences glucose regulatory mechanisms through multiple pathways. Animal studies demonstrate that various digested proteins, particularly casein and fish gelatin, acutely improve glucose tolerance without significantly affecting insulin secretion, suggesting a mechanism involving reduced intestinal glucose absorption [43]. Specifically, digested proteins from diverse sources decreased GLUT2 mRNA expression in enterocytes, indicating a potential pathway for modulating postprandial glucose excursions [43]. Conversely, proteins high in branched-chain amino acids (BCAAs), particularly animal proteins, may paradoxically contribute to insulin resistance through overstimulation of mTOR signaling pathways when consumed chronically in excess [65]. This dual role highlights the context-dependent nature of protein quality evaluation.
Temporal Patterning of Protein Intake
Chrono-Nutrition and Metabolic Outcomes
The timing of protein intake across the day (temporal protein patterning) represents an emerging dimension of nutritional optimization. A 2025 analysis of NHANES 2017-2020 data identified three distinct temporal protein patterns in American adults [100]. Class 1 featured higher protein consumption at 18:00h; Class 2 exhibited similar patterns but approximately 1 hour later with higher overall intake; while Class 3 showed variable timing with lower total protein intake [100]. Notably, men in Class 1 demonstrated lower probabilities for poor glycemic control (5.9%), though this association was attenuated after adjusting for BMI [100]. Overall, the study concluded that temporal protein patterns alone showed no significant associations with diabetes prevalence or glycemic measures after comprehensive adjustment for confounders [100].
Evening Protein Distribution and Clinical Implications
Randomized controlled trials investigating temporal distribution have yielded mixed results. One trial among adults with T2DM found that standard evening meals (15-20% protein evenly distributed across three daily meals) produced greater improvements in HbA1c and BMI after ten weeks compared to high-protein evening meals (40-45% of total energy from protein consumed at dinner and evening snack) [100]. This suggests that evenly distributed moderate protein intake may be superior to concentrated evening loading for glycemic management. The diagram below illustrates the metabolic fate of dietary proteins based on timing and composition.
Enhancing Protein Bioavailability and Stability
Therapeutic Protein Delivery Challenges
Therapeutic proteins face significant bioavailability challenges, including rapid enzymatic degradation, poor membrane permeability, renal clearance based on hydrodynamic size (<6 nm), metabolic clearance primarily in the liver, and immunogenicity leading to anti-drug antibody production [101] [102]. These limitations necessitate sophisticated delivery strategies to optimize therapeutic efficacy, particularly for chronic conditions like diabetes requiring sustained glycemic control.
Strategic Solutions for Enhanced Delivery
Table 2 summarizes FDA-approved and emerging strategies to enhance protein delivery, along with their mechanisms of action and research applications.
Table 2: Protein Delivery Enhancement Strategies
| Strategy | Mechanism of Action | Research/Clinical Applications | Considerations |
|---|---|---|---|
| PEGylation | Increases hydrodynamic size; provides stealth effect against opsonization and enzymatic degradation [102] | PEGylated uricase (pegloticase) for gout; extends half-life from 8h (native) to 300h (PEGylated) [102] | Potential anti-PEG immunogenicity; 38 FDA-approved PEGylated drugs as of 2024 [102] |
| Amino Acid Substitution | D-amino acids and β-amino acids resist enzymatic degradation due to altered peptide bond configuration [102] | Research stage for therapeutic peptides; enhanced metabolic stability | Requires extensive efficacy and safety validation |
| Polypeptide Conjugation | Biocompatible polypeptides (e.g., elastin-like polypeptides) improve stability and extend half-life [98] | Experimental platforms for controlled release and targeted delivery | Modular design allows incorporation of multiple functional domains [98] |
| Fc Fusion | Leverages IgG Fc domain to engage neonatal Fc receptor (FcRn) recycling pathway [102] | Recombinant factor VIII Fc fusion (rFVIIIFc) for hemophilia A; extends half-life to 19h vs 13h for native [98] | Large molecular weight may affect tissue penetration |
| Nanocarrier Systems | Protection from degradation; enhanced cellular uptake via encapsulation | Research stage for oral protein delivery; improved bioavailability | Complex manufacturing; potential toxicity concerns |
The following diagram illustrates the primary clearance mechanisms for therapeutic proteins and corresponding strategies to overcome them.
Experimental Methodologies for Protein Research
In Vitro Digestion and Absorption Models
The INFOGEST static gastrointestinal digestion protocol provides a standardized methodology for simulating human protein digestion [43]. Key steps include:
- Oral Phase: Incubate protein sample (2g adjusted to protein content) with simulated salivary fluid (SSF) at pH 7.0 for 5 minutes
- Gastric Phase: Add simulated gastric fluid (SGF) containing pepsin (6,500 U/mL), adjust to pH 3.0, incubate 2 hours
- Intestinal Phase: Add simulated intestinal fluid (SIF) containing pancreatin (45 U/mL), adjust to pH 7.0, incubate 2 hours
- Termination: Heat at 95°C for 10 minutes to denature enzymes, centrifuge at 13,400g for 10 minutes, collect supernatants for analysis [43]
For glucose uptake assessment, Caco-2/TC7 intestinal cell models are employed with the following protocol:
- Culture cells on transwell membranes for 3 weeks to achieve differentiation
- Pre-incubate with digested proteins (5 mg/mL) for 1 hour
- Measure uptake using 14C-α-methyl-D-glucopyranoside as tracer
- Terminate with cold PBS containing phlorizin, quantify radioactivity via scintillation counting [43]
In Vivo Glucose Tolerance Assessment
Animal models provide critical translational insights:
- Utilize fasted Wistar rats (16-hour fast)
- Administer protein digest via oral gavage
- Measure blood glucose at regular intervals post-administration
- Compare area under the curve (AUC) for glucose tolerance between treatments [43]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Protein and Glucose Homeostasis Studies
| Reagent/Cell Line | Research Application | Key Function/Characteristic |
|---|---|---|
| Caco-2/TC7 Cells | Intestinal glucose uptake studies | Differentiated enterocyte model for transport studies [43] |
| HT29-MTX Cells | Mucosal permeability and absorption | Mucus-secreting intestinal cell line [43] |
| INFOGEST Digestive Enzymes | Simulated gastrointestinal digestion | Standardized pepsin and pancreatin for reproducible digestion [43] |
| 14C-α-methyl-D-glucopyranoside | Glucose transporter activity assessment | Non-metabolizable glucose analog for uptake quantification [43] |
| Recombinant Therapeutic Proteins | Bioavailability and efficacy testing | Fc fusion proteins, PEGylated variants with extended half-lives [102] [98] |
Future Directions and Clinical Translation
The future of protein optimization research points toward several promising frontiers. Artificial intelligence and machine learning are accelerating protein design, enabling precise optimization of stability and reduced immunogenicity [97]. Personalized protein therapeutics, informed by individual genomics and proteomics, represent the next paradigm in precision medicine [97]. Oral protein drug formulations, while currently limited by enzymatic degradation and poor epithelial transport, are the subject of intensive research utilizing enzyme inhibitors, penetration enhancers, and advanced nanoparticulate systems [101]. The integration of synthetic biology may enable creation of entirely novel protein modalities with enhanced therapeutic profiles for glucose management [97]. Furthermore, research must address the nuanced balance between protein benefits and potential risks, as chronic excessive intake—particularly of animal proteins high in BCAAs—may induce insulin resistance through mTOR overstimulation [65]. Future studies should prioritize longitudinal designs with standardized protein timing assessments and consideration of protein sources to elucidate optimal strategies for leveraging dietary and therapeutic proteins in glucose homeostasis.
Evidence Synthesis: Validating Outcomes Across Diets, Populations, and Biomarkers
The management of prediabetes and type 2 diabetes mellitus (T2DM) requires innovative dietary strategies that address fundamental metabolic disturbances. High-protein diets (HPDs), particularly when combined with caloric restriction, have emerged as significant modulators of glucose homeostasis through multiple physiological pathways. Research demonstrates that dietary protein influences glucose metabolism not only indirectly through weight loss and body composition changes, but also directly via endocrine signaling, neuronal pathways, and nutrient-sensing mechanisms [103]. This review synthesizes current clinical evidence on the efficacy of low-calorie, high-protein (LC-HP) diets, examining the mechanistic role of amino acids in pancreatic function, hepatic glucose production, intestinal glucose absorption, and central nervous system regulation. Understanding these pathways provides a scientific foundation for utilizing LC-HP diets as therapeutic interventions in metabolic disease.
Mechanisms of Action: Amino Acids and Protein in Glucose Regulation
Direct and Indirect Pathways of Protein-Induced Glucose Homeostasis
Dietary proteins influence glucose regulation through multiple coordinated pathways. The diagram below illustrates the primary mechanisms through which dietary amino acids and high-protein diets modulate insulin secretion and glucose homeostasis.
Figure 1. Multiple pathways through which dietary amino acids and high-protein diets influence insulin secretion and glucose homeostasis. Direct effects include pancreatic β-cell stimulation, while indirect effects involve incretin release, neuronal signaling, intestinal glucose transport modulation, and central nervous system-mediated hepatic glucose regulation [103] [43].
Key Cellular Mechanisms
Pancreatic β-Cell Stimulation: Amino acids directly stimulate insulin secretion through activation of nutrient receptors and transporters expressed by pancreatic β-cells. Branched-chain amino acids (BCAAs), particularly leucine, serve as both metabolic fuels and signaling molecules that enhance insulin release [103] [40].
Incretin-Mediated Effects: Protein ingestion stimulates the release of gut-derived incretin hormones, including glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP). These hormones amplify glucose-stimulated insulin secretion while inhibiting glucagon release and slowing gastric emptying [103] [104].
Intestinal Glucose Transport Modulation: Digested protein-derived peptides reduce intestinal glucose absorption by decreasing expression of glucose transporter type 2 (GLUT2) at the basolateral membrane of enterocytes. This mechanism represents a non-pancreatic pathway for improving glucose tolerance [43].
Hypothalamic Nutrient Sensing: Leucine crosses the blood-brain barrier in the arcuate nucleus of the mediobasal hypothalamus, where it is metabolized to produce signaling molecules that activate hypothalamic ATP-sensitive potassium (KATP) channels. This generates a neuronal signal transmitted via the vagus nerve that reduces hepatic glucose production [40].
Clinical Evidence: Efficacy of LC-HP Diets in Metabolic Disorders
Table 1. Clinical outcomes of low-calorie, high-protein diets in prediabetes and T2DM
| Study & Design | Participant Characteristics | Intervention Details | Weight Loss Outcomes | Glycemic Parameters | Other Cardiometabolic Effects |
|---|---|---|---|---|---|
| RCT: Low-calorie HP diets (2025) [105] | n=117 with prediabetes or T2DM, BMI >27.5 kg/m² | 6-month LC-HP (35% protein), 75% plant (HPP) or animal (HPA) protein | -8.05±5.12 kg (HPA)-7.70±5.47 kg (HPP) | Improved fasting glucose, insulin, HOMA-IR, HbA1c (both groups) | Improved lipid profiles, liver enzymes, adipokines, inflammatory biomarkers |
| RCT: HP vs NP with T2DM (2023) [106] | n=106 with T2DM, 52-week intervention | HP (40% protein) with red meat vs NP (21% protein) without red meat | -10.2±1.6 kg (HP)-12.7±4.8 kg (NP) | HbA1c, glucose, insulin, and insulin resistance improved with no between-group differences | Reduced fat mass, increased fat-free mass percent, improved BP and triglycerides |
| OPEN-LABEL: DSNF-Pro in prediabetes (2025) [104] | n=15 with prediabetes, crossover design | Diabetes-specific nutritional formula-pro (DSNF-Pro) vs standard formula | Not measured | 73.4% reduction in postprandial glucose iAUC (p=0.0001)36.4% reduction in c-peptide iAUC | No significant difference in postprandial insulin iAUC |
| SYSTEMATIC REVIEW: HPD in T2DM (2024) [40] | 8 clinical studies in T2DM | HPD (>30% or >1.0 g/kg/day) | Consistent weight loss across studies | Reduced hyperglycemia, especially with Paleolithic diets | Higher-quality protein sources particularly effective |
Protein Source Comparative Effectiveness
Table 2. Comparative effects of animal vs plant-based high-protein diets
| Parameter | Animal Protein Diets | Plant Protein Diets | Statistical Significance |
|---|---|---|---|
| Weight Loss | -8.05±5.12 kg [105] | -7.70±5.47 kg [105] | p>0.05 (NS) |
| Fat Mass Reduction | Significant decrease [105] [106] | Significant decrease [105] | p>0.05 (NS) |
| Visceral Fat Reduction | Significant decrease [105] | Significant decrease [105] | p>0.05 (NS) |
| Fasting Glucose | Improved [105] | Improved [105] | p>0.05 (NS) |
| HbA1c | Improved [105] [106] | Improved [105] | p>0.05 (NS) |
| HOMA-IR | Improved [105] | Improved [105] | p>0.05 (NS) |
| Lipid Profiles | Improved [105] [106] | Improved [105] | p>0.05 (NS) |
| Inflammatory Biomarkers | Improved [105] | Improved [105] | p>0.05 (NS) |
Long-Term Efficacy and Prediabetes Remission
The PREVIEW trial, a 3-year multinational study, provides critical insights into long-term dietary effects on prediabetes remission. Following initial weight loss, participants assigned to a moderate-protein (15% of energy), moderate-glycemic index diet showed significantly higher remission rates compared to those on a high-protein (25% of energy), low-glycemic index diet at both 1 year (26.3% vs 20.7%; RR 1.26) and 3 years (20.6% vs 15.5%; RR 1.26) [107]. This suggests that long-term prediabetes remission may be better achieved with moderate rather than high protein intake, independent of weight maintenance.
Experimental Models and Methodologies
Research Models for Investigating Protein-Glucose Interactions
The experimental workflow for studying the effects of dietary protein on glucose regulation involves multiple model systems, from in vitro approaches to human clinical trials, as illustrated below.
Figure 2. Experimental models and workflow for investigating the effects of dietary protein on glucose regulation. Research typically progresses from in vitro protein digestion and cell culture models to ex vivo intestinal preparations, animal studies, and finally human clinical trials [43] [104].
Key Methodological Protocols
In Vitro Gastrointestinal Digestion (INFOGEST Protocol)
The standardized INFOGEST static simulation of gastrointestinal digestion enables reproducible generation of protein hydrolysates for mechanistic studies [43]:
- Salivary Phase: Protein samples (2g adjusted to protein content) solubilized in water and mixed with simulated salivary fluid (SSF) at pH 7.0 for 5 minutes
- Gastric Phase: Addition of simulated gastric fluid (SGF) containing pepsin (6,500 U/mL), pH adjustment to 3.0, incubation for 2 hours
- Intestinal Phase: Addition of simulated intestinal fluid (SIF) containing pancreatin (45 U/mL), pH adjustment to 7.0, incubation for 2 hours
- Termination: Heat inactivation at 95°C for 10 minutes, centrifugation at 13,400 g for 10 minutes, collection of supernatants for analysis
Clinical Trial Design Considerations
Recent high-quality trials share several methodological features [105] [104] [106]:
- Participant Characterization: Clear definition of prediabetes (fasting glucose 5.6-6.9 mmol/L and/or 2h glucose 7.8-11.0 mmol/L) and T2DM diagnostic criteria
- Dietary Control: Provision of specific food products or detailed meal plans to ensure adherence to protein targets
- Outcome Measures: Comprehensive assessment including body composition (DXA), glycemic parameters (HbA1c, fasting glucose, OGTT), and cardiometabolic biomarkers
- Duration: Minimum 6-month interventions to assess medium-term efficacy with some trials extending to 52 weeks or longer
Table 3. Key research reagents and materials for investigating protein-glucose interactions
| Research Tool | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Cell Lines | Caco-2/TC7, HT29-MTX | Intestinal glucose transport studies | Model human intestinal epithelium, glucose absorption mechanisms |
| Protein Sources | Casein, whey, pea, soy, hemoglobin, ovalbumin, fish gelatin, gluten | Protein-specific effect studies | Source variation examines amino acid composition and peptide bioactivity |
| Digestion Enzymes | Pepsin (P6887), pancreatin (P1750) | In vitro digestion simulations | Gastrointestinal proteolysis to generate bioactive peptides |
| Isotopic Tracers | 14C-α-methyl-D-glucopyranoside, 3H-D-glucose | Glucose transport quantification | Enable precise measurement of glucose flux and absorption |
| Animal Models | Wistar rats, diet-induced obese mice | In vivo glucose tolerance testing | Preclinical assessment of glucose homeostasis mechanisms |
| Clinical Formulations | Diabetes-specific nutritional formulas (DSNF-Pro) | Human intervention studies | Standardized protein delivery for clinical trials |
| Analytical Assays | Glucose oxidase assay, radioimmunoassay for insulin/c-peptide, ELISA for incretins | Biomarker quantification | Precise measurement of metabolic parameters |
Clinical evidence robustly supports the efficacy of low-calorie, high-protein diets for improving glucose metabolism in prediabetes and T2DM. The mechanisms extend beyond simple weight loss to include direct modulation of insulin secretion, incretin responses, intestinal glucose absorption, and central regulation of hepatic glucose production. Importantly, recent studies indicate that both animal and plant-based protein sources produce comparable metabolic benefits, offering flexibility in dietary approaches. However, long-term prediabetes remission may be better achieved with moderate protein intake rather than very high protein consumption. Future research should focus on personalized protein recommendations based on individual metabolic phenotypes, optimal protein timing and distribution, and the synergistic effects of combined dietary and pharmacological approaches for diabetes management.
Comparative Efficacy of Mediterranean, DASH, and Ketogenic Dietary Patterns
Dietary intervention represents a cornerstone of management for metabolic diseases, including type 2 diabetes (T2D) and cardiovascular conditions. The Mediterranean (MD), Dietary Approaches to Stop Hypertension (DASH), and Ketogenic (KD) diets are three prominent dietary patterns with distinct macronutrient profiles and proposed mechanisms of action. Within the broader context of research on the impact of dietary proteins and amino acids on glucose homeostasis, this whitepaper provides a technical comparison of these diets. We evaluate their efficacy based on recent clinical evidence, delineate underlying molecular mechanisms, and detail standardized experimental protocols to guide preclinical and clinical research in metabolic drug development.
Dietary Pattern Definitions and Macronutrient Composition
The three dietary patterns are defined by their unique nutritional philosophies and macronutrient distributions, which underlie their physiological effects.
- Mediterranean Diet (MD): The MD is characterized by high consumption of fruits, vegetables, whole grains, legumes, nuts, and olive oil; moderate intake of fish and poultry; and low intake of red meat, processed foods, and sweets [108] [109]. It is rich in fiber, polyphenols, and unsaturated fatty acids. Its anti-inflammatory and antioxidant properties are considered central to its health benefits [109].
- DASH Diet: The DASH diet emphasizes fruits, vegetables, whole grains, and low-fat dairy products. It favors lean protein sources, such as beans and lean meats, and limits saturated fats, sugar-sweetened foods, and beverages [110] [111]. A modified version for diabetes (DASH4D) adjusts carbohydrate intake to approximately 45% of total calories, increases unsaturated fats, and reduces potassium to protect kidney health in vulnerable populations [110] [112].
- Ketogenic Diet (KD): The KD is a very high-fat, very low-carbohydrate diet. A classic KD derives 60-80% of daily energy from fat, 10-30% from protein, and restricts carbohydrates to 5-10% (typically <50 g/day) [113]. This composition aims to induce a state of nutritional ketosis, where the liver produces ketone bodies to serve as an alternative fuel source for the brain and other tissues [113].
Table 1: Standard Macronutrient Composition of Dietary Patterns
| Dietary Pattern | Carbohydrates (%) | Fat (%) | Protein (%) | Key Nutritional Features |
|---|---|---|---|---|
| Mediterranean | 40-50 [114] | 35 [114] | ~15-20 | High fiber, polyphenols, MUFA/PUFA (olive oil, nuts) |
| DASH (Standard) | ~55 [110] | ~27 (low sat.) | ~18 | High fiber, potassium, calcium, magnesium; low sodium |
| DASH4D (Modified) | ~45 [110] [112] | Higher unsat. fats [112] | ~Similar to standard | Lower carb, controlled potassium, higher unsaturated fat |
| Ketogenic (KD) | 5-10 (<50 g/day) [113] | 60-80 [113] | 10-30 [113] | Very low carb, high fat, induces ketosis |
Quantitative Efficacy Comparison in Metabolic Health
Recent clinical trials and observational studies provide robust data on the effects of these diets on key metabolic parameters, including glycemia, body composition, and cardiovascular risk factors.
- Glycemic Control: The DASH4D diet demonstrated a significant reduction in mean glucose by 11 mg/dL and increased time in the optimal glucose range (70-180 mg/dL) by 75 minutes per day compared to a standard American diet [110] [112]. The Mediterranean diet is consistently associated with improved insulin sensitivity and reduced risk of diabetes and prediabetes [115] [108]. A 2025 study found that both a high-protein KD and a hypocaloric MD led to significant reductions in insulin concentrations, though the MD is often noted for its long-term sustainability [114] [108]. Mouse models reveal a paradox with KD: while it can rapidly normalize blood glucose, it may impair insulin secretion from pancreatic beta-cells and lead to dysregulated glucose tolerance upon carbohydrate challenge [116].
- Body Composition: Both the KD and MD are effective for weight loss. A 3-month intervention in overweight/obese individuals with high-normal blood pressure resulted in substantial weight loss (KD: 98.6 to 87.3 kg; MD: 93.8 to 86.1 kg) and reductions in waist circumference, with no significant difference between the diets [114]. The KD's weight loss is attributed to factors including reduced hunger and satiety hormonal changes [113].
- Cardiovascular and Hepatic Markers: Both the KD and MD significantly improved 24-hour systolic and diastolic blood pressure and lipid profiles in a 3-month study [114]. The DASH diet's primary benefit is its potent antihypertensive effect [111]. However, long-term mouse studies on KD raise concerns about potential adverse effects, including fatty liver disease and hyperlipidemia, particularly in males [116].
Table 2: Summary of Key Clinical Outcomes from Recent Studies
| Outcome Measure | Mediterranean Diet | DASH / DASH4D Diet | Ketogenic Diet |
|---|---|---|---|
| HbA1c / Mean Glucose | Improves glycemic control, reduces T2D risk [115] [108] | ↓ Mean glucose by 11 mg/dL; ↑ Time in Range by 75 min/day [112] | Rapidly normalizes blood glucose; may impair insulin secretion long-term [116] [117] |
| Body Weight / BMI | Significant reduction (e.g., -7.7 kg in 3 mo) [114] | Promotes weight loss, reduces BMI [111] | Significant reduction (e.g., -11.3 kg in 3 mo); prevents weight gain [114] [116] |
| Blood Pressure | ↓ Mean 24h SBP & DBP [114] | Significant reduction in SBP & DBP; primary purpose [111] | ↓ Mean 24h SBP & DBP [114] |
| Lipid Profile | ↓ TG, LDL; ↑ HDL [114] [109] | Improves lipid metabolism [111] | ↓ TG, LDL; ↑ HDL in short term; long-term hyperlipidemia risk [114] [116] |
| Fatty Liver Disease | Protective effect [109] | Not a primary outcome, but improvements seen [111] | Associated with increased risk in male mice [116] |
| Noted Risks | None significant reported | Requires potassium modification in CKD [112] | Fatty liver, dysregulated glucose response, nutrient deficiency [116] |
Mechanisms of Action: Focus on Glucose Homeostasis and Protein Signaling
The differential effects of these diets on metabolic health can be traced to distinct molecular pathways, with dietary protein and amino acid composition playing a key modulating role.
- Mediterranean Diet: The MD enhances insulin sensitivity primarily through its anti-inflammatory and antioxidant properties. Bioactive compounds like polyphenols reduce oxidative stress and inhibit pro-inflammatory signaling pathways, thereby improving insulin signal transduction [108]. The diet's high fiber content slows glucose absorption and moderates postprandial glycemia. Furthermore, the specific lipid profile (rich in MUFAs and omega-3 PUFAs) and the quality of plant-based proteins contribute to favorable changes in cell membrane fluidity and inflammatory mediator production.
- DASH Diet: The DASH diet improves glycemic control by leveraging high dietary fiber to slow glucose absorption and improve insulin sensitivity [111]. Its high potassium and magnesium content may also contribute to better glucose metabolism and vascular function. The DASH4D modification optimizes this further by reducing the carbohydrate load, thereby decreasing the direct substrate for postprandial glucose spikes [110] [112].
- Ketogenic Diet: The KD's primary mechanism is substrate-driven. Severe carbohydrate restriction drastically reduces glucose availability, forcing a metabolic shift to fatty acid oxidation and ketone body production. This state of ketosis is associated with reduced basal insulin levels and increased fat oxidation [113]. However, research in mice suggests that chronic exposure to high lipid levels can induce cellular stress in pancreatic beta-cells, impairing their ability to secrete insulin in response to a glucose load, which explains the observed glucose intolerance [116]. The type and amount of dietary protein in a KD may influence gluconeogenic flux, adding another layer of metabolic regulation.
The following diagram illustrates the core pathways through which these diets influence glucose homeostasis, highlighting the role of dietary protein and amino acids.
Diagram 1: Molecular Pathways in Glucose Homeostasis. This diagram illustrates the primary mechanisms—including the role of protein and amino acids—by which the Mediterranean, DASH, and Ketogenic diets influence glucose metabolism. The KD shows a potential risk pathway for impaired insulin secretion.
Detailed Experimental Protocols
To ensure reproducibility and facilitate future research, we outline key methodologies from recent high-impact studies.
- Objective: To evaluate the efficacy of a modified DASH diet (DASH4D) on glycemic control in adults with T2D.
- Study Design: Randomized, crossover, controlled feeding trial.
- Participants: 89 adults with T2D (mean age 67, 67% female, 88% African American).
- Interventions: Participants were provided with all meals in a random order for four 5-week periods:
- Low-sodium DASH4D diet
- High-sodium DASH4D diet
- Low-sodium standard American diet (control)
- High-sodium standard American diet (control) Diets were isocaloric to maintain stable body weight.
- Data Collection:
- Glycemic Measurement: Continuous Glucose Monitors (CGM) worn during weeks 3 and 4 of each period, measuring glucose every 15 minutes. Key metrics: mean glucose, time-in-range (70-180 mg/dL), glycemic variability.
- Blood Pressure: Standardized office and ambulatory monitoring.
- Biochemical Analysis: Fasting blood draws for HbA1c, lipids, and other biomarkers.
- Objective: To compare the effects of a hypocaloric, high-protein KD versus a hypocaloric, low-sodium, high-potassium MD on cardiovascular and metabolic parameters.
- Study Design: Prospective, observational, bicentric, open-label pilot study.
- Participants: 26 non-diabetic adult outpatients with overweight/obesity (BMI >27 kg/m²) and high-normal BP or grade I hypertension.
- Interventions:
- KD Group (n=15): ~1300 kcal/day; 10-15% carbohydrate (<50 g/day), 55-60% fat, 25-30% protein (≥1.2 g/kg ideal body weight).
- MD Group (n=11): ~1300 kcal/day; 40-50% carbohydrate, 35% fat, ~15% protein.
- Assessments (at baseline and 3 months):
- Anthropometrics & Body Composition: Body weight, waist circumference, Bioelectrical Impedance Analysis (BIA) for fat mass (FM) and fat-free mass (FFM).
- Blood Pressure: 24-hour Ambulatory Blood Pressure Monitoring (ABPM).
- Blood Analysis: Lipid profile, insulin concentration.
- Objective: To investigate the long-term metabolic effects of a ketogenic diet in a mouse model.
- Study Design: Long-term dietary intervention.
- Animals: Adult male and female mice.
- Interventions: Mice were assigned to one of four ad libitum diets for over nine months:
- High-fat Western diet (control)
- Low-fat, high-carbohydrate diet (control)
- Classic ketogenic diet (~90% fat)
- Protein-matched low-fat diet
- Data Collection:
- Metabolic Phenotyping: Body weight, food intake, body composition (fat/lean mass).
- Glucose Metabolism: Blood glucose and insulin levels, glucose and insulin tolerance tests. Advanced microscopy and gene expression analysis in pancreatic islets.
- Liver Health: Histological and biochemical assessment of liver fat (triglyceride content), markers of liver function.
- Key Finding: KD protected against weight gain but induced fatty liver disease in males and impaired insulin secretion, leading to glucose intolerance.
The workflow for a comprehensive metabolic study integrating these elements is outlined below.
Diagram 2: Clinical Trial Workflow for Dietary Interventions. A standardized protocol for comparing the efficacy of MD, DASH, and KD, highlighting key phenotyping steps at baseline and study end.
The Scientist's Toolkit: Key Research Reagents and Materials
This section details essential tools and methodologies for conducting rigorous research on dietary interventions.
Table 3: Essential Research Reagents and Materials
| Tool / Reagent | Function / Application | Example Use in Context |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Measures interstitial glucose levels every 5-15 minutes, providing dense data on glycemic variability and time-in-range. | Primary endpoint in DASH4D trial to detect differences in 24/7 glucose control [110] [112]. |
| Ambulatory Blood Pressure Monitor (ABPM) | Automatically records BP at regular intervals over 24 hours, providing a comprehensive BP profile. | Used in KD vs. MD study to assess true efficacy on blood pressure outside the clinic [114]. |
| Bioelectrical Impedance Analysis (BIA) | Estimates body composition (fat mass, fat-free mass) by measuring the resistance of body tissues to a small electrical current. | Critical for differentiating fat loss from lean mass loss during weight loss interventions [114]. |
| Standardized Meal Kits | Pre-prepared, isocaloric meals designed to match specific macronutrient profiles of MD, DASH, or KD. | Ensures strict dietary adherence and eliminates self-reporting bias in controlled feeding trials [112]. |
| Ketone Meters | Measures blood concentration of beta-hydroxybutyrate (BHB) to confirm a state of ketosis. | Essential for verifying adherence to the ketogenic diet in KD intervention arms [113]. |
| ELISA/Multiplex Assay Kits | Quantifies specific biomarkers in serum/plasma (e.g., insulin, adipokines, inflammatory cytokines like IL-6, CRP). | Used to mechanistically link dietary changes to improvements in insulin resistance and inflammation [115]. |
| Dual-Energy X-ray Absorptiometry (DEXA) | Gold-standard method for precisely measuring body composition, including regional fat distribution. | Provides high-precision data on visceral and subcutaneous fat mass changes [115]. |
The Mediterranean, DASH, and Ketogenic diets offer distinct pathways to improving metabolic health, with efficacy demonstrated across multiple clinical and preclinical studies. The MD and DASH diets provide sustainable, evidence-based patterns with broad benefits for glucose control and cardiovascular health, largely mediated through anti-inflammatory and fiber-rich food components. The KD is a potent intervention for rapid weight loss and short-term glycemic improvement but may carry long-term risks for pancreatic function and hepatic health, necessitating careful monitoring. Future research should focus on the precise role of dietary protein sources and amino acid composition within these patterns to further optimize personalized nutrition strategies for diabetes management and cardiovascular risk reduction.
The precise assessment of insulin sensitivity is a cornerstone of metabolic research, particularly in the context of type 2 diabetes (T2DM) and obesity. Insulin resistance, a state of impaired biological response to normal circulating levels of insulin, represents an early pathophysiology in the progression of diabetes and is associated with both microvascular and macrovascular complications [118]. This technical guide provides an in-depth analysis of three critical methodological approaches used in metabolic research: the Homeostatic Model Assessment of Insulin Resistance (HOMA-IR), the hyperinsulinemic-euglycemic clamp (HEC), and body composition analysis. Within the framework of a broader thesis on the impact of dietary proteins and amino acids on glucose homeostasis, understanding these assessment tools is paramount for designing robust experiments, interpreting findings related to nutritional interventions, and advancing therapeutic development. The complex interplay between specific amino acids, protein intake, and tissue-specific insulin sensitivity necessitates precise measurement tools capable of detecting subtle metabolic shifts in response to dietary manipulation.
Core Biomarkers and Methodologies
HOMA-IR: The Surrogate Index
Principle and Calculation: The Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) is a mathematical model derived from fasting glucose and insulin concentrations that provides a surrogate estimate of insulin resistance. It is based on the principle of a feedback loop between the liver and beta-cells, estimating insulin resistance from fasting steady-state conditions. The formula is:
HOMA-IR = [Fasting Insulin (μU/mL) × Fasting Glucose (mmol/L)] / 22.5
Clinical and Research Utility: HOMA-IR serves as a valuable tool for large-scale epidemiological studies and clinical settings where more complex procedures are impractical. A 2023 study demonstrated that high HOMA-IR values were an independent predictor for new-onset T2DM (odds ratio 1.86 [1.17–2.96]) and chronic kidney disease (CKD) (OR 1.49 [1.12–1.98]) in non-diabetic individuals, even after adjusting for HbA1c and other risk factors [118]. The study divided participants into tertiles, with the high HOMA-IR group (tertile >1.84) showing significantly higher incidence of both conditions over a median follow-up of 9.9 years [118]. In postmenopausal women, a HOMA-IR value ≥2.8 (75th percentile) identified individuals with a high risk of abnormal glucose metabolism, with 90% showing glucose abnormalities and 45% having silent diabetes [119].
Table 1: HOMA-IR Tertiles and Associated Health Risks in a Non-Diabetic Cohort (n=4,314) [118]
| HOMA-IR Tertile | Range | New-Onset T2DM Incidence | CKD Incidence | Key Associated Comorbidities |
|---|---|---|---|---|
| Low | <1.37 | Lower | Lower | Lower prevalence of hypertension |
| Moderate | 1.37-1.84 | Intermediate | Intermediate | Intermediate risk profile |
| High | >1.84 | 5.8% (Higher) | 12.2% (Higher) | Higher prevalence of hypertension, dyslipidemia |
Advantages and Limitations: The primary advantages of HOMA-IR include its simplicity, low cost, and minimal patient burden, requiring only a single fasting blood sample. However, it has limitations: it primarily reflects hepatic insulin resistance and is less sensitive to peripheral insulin sensitivity. Its accuracy can be affected by variables such as beta-cell function and the assay methods used for insulin measurement.
Hyperinsulinemic-Euglycemic Clamp: The Gold Standard
Experimental Principle: The hyperinsulinemic-euglycemic clamp (HEC) is considered the gold standard for direct measurement of whole-body insulin sensitivity. The procedure involves the continuous intravenous infusion of insulin at a constant rate to achieve and maintain hyperinsulinemia, while a variable glucose infusion is simultaneously administered to maintain euglycemia (typically 5.5 mmol/L ± 0.5 mmol/L) [120]. The glucose infusion rate (GIR) required to maintain euglycemia during steady-state hyperinsulinemia provides a direct measure of insulin sensitivity, known as the M-value (whole-body glucose disposal rate).
Detailed Protocol [120] [121]:
- Pre-test Conditions: Participants arrive fasted (>10 hours). No exercise, alcohol, or caffeine is permitted prior to the test to minimize confounding variables.
- Vascular Access: Two intravenous catheters are placed—one for infusions (insulin and glucose) and another in a warmed hand or arm for frequent arterialized venous blood sampling.
- Insulin Infusion: A primed-continuous intravenous infusion of insulin (e.g., 56 mU/m²/min) is initiated to rapidly achieve and sustain a steady-state hyperinsulinemic plateau.
- Glucose Monitoring and Infusion: Plasma glucose is measured at 5-minute intervals. A variable 20% glucose infusion is adjusted based on these frequent measurements to "clamp" the plasma glucose at the target euglycemic level.
- Steady-State Measurement: The clamp period typically lasts 2-4 hours. The M-value is calculated from the mean glucose infusion rate during the final 30-60 minutes of the clamp when steady-state has been achieved, often normalized to body weight or lean mass.
Advanced Applications: Tissue-Specific Assessment The combination of HEC with dynamic whole-body Positron Emission Tomography and Magnetic Resonance Imaging (PET/MRI) using the glucose tracer [¹⁸F]FDG allows for the quantification of tissue-specific metabolic rates of glucose uptake (MRGlu) under insulin-stimulated conditions [120]. This method has demonstrated excellent repeatability for skeletal muscle (ICC 0.94) and good repeatability for adipose tissue depots, enabling researchers to dissect organ-specific contributions to whole-body insulin resistance [120]. This is particularly relevant for dietary protein research, as different interventions may preferentially affect hepatic versus muscle insulin sensitivity.
Table 2: Repeatability of Whole-Body and Tissue-Specific Glucose Uptake Measurements via PET/MRI-HEC [120]
| Measured Parameter | Tissue/System | Intraclass Correlation Coefficient (ICC) | Clinical/Research Insight |
|---|---|---|---|
| M-value | Whole-body | 0.95 (Excellent) | Gold-standard measure of whole-body insulin sensitivity. |
| MRGlu (Metabolic Rate of Glucose Uptake) | Skeletal Muscle | 0.94 (Excellent) | Major site of insulin-stimulated glucose disposal. |
| MRGlu | Subcutaneous Adipose Tissue (SAT) | Good to Fair | Important for understanding lipid storage capacity. |
| MRGlu | Visceral Adipose Tissue (VAT) | Good to Fair | Strongly associated with cardiometabolic risk. |
| MRGlu | Myocardium | Good to Fair | Assesses cardiac metabolism. |
Body Composition Analysis
Relevance to Insulin Resistance: Body composition, particularly the distribution of body fat, is a critical determinant of insulin sensitivity. The body mass index (BMI) is a poor indicator of cardiometabolic health at the individual level, as it does not discriminate between fat and muscle mass or account for fat distribution [122]. Visceral adipose tissue (VAT), abdominal subcutaneous adipose tissue (aSAT), and ectopic fat deposition in organs like the liver and skeletal muscle are strongly associated with whole-body and tissue-specific insulin resistance [122] [123].
Assessment Technologies:
- Bioelectrical Impedance Analysis (BIA): A rapid, non-invasive, and low-cost method that estimates body composition, including percent body fat (PBF) and visceral fat rating (VFR), by measuring the body's resistance to a low-level electrical current [123]. A study of 557 women with overweight and obesity found that VFR could serve as a valuable additional biomarker for assessing insulin resistance, though its predictive power (AUC) was slightly lower than that of BMI and waist circumference [123].
- Whole-Body Magnetic Resonance Imaging (MRI): This state-of-the-art methodology provides highly accurate and detailed quantification of body composition, including VAT and aSAT volumes, liver fat percentage, and thigh muscle fat infiltration [122]. Research has shown that VAT is inversely associated with whole-body, liver, and muscle insulin sensitivity, while liver fat content is specifically associated with worse liver insulin sensitivity [122].
Integration with Dietary Protein and Amino Acid Research
The assessment methodologies detailed above are indispensable for investigating the nuanced effects of dietary proteins and amino acids on glucose homeostasis.
Elucidating Mechanisms of Action: High-protein diets during weight loss are known to preserve skeletal muscle mass, which is responsible for ~80% of insulin-stimulated glucose disposal [3]. The HEC, particularly when combined with PET/MRI, can quantify the extent to which protein-induced muscle mass preservation translates to improved peripheral glucose uptake. Furthermore, amino acids like leucine transiently activate the mTORC1/PGC-1α signaling pathway, which promotes mitochondrial biogenesis and may improve insulin sensitivity [3]. HOMA-IR can track longitudinal changes in insulin sensitivity in response to these interventions in larger cohorts.
Differentiating Tissue-Specific Effects: Dietary interventions can have disparate effects on different tissues. For example, a 12-week isocaloric dietary intervention comparing a low-fat, high-protein, high-fiber (LFHP) diet and a high mono-unsaturated fatty acid (HMUFA) diet found that both reduced VAT, aSAT, and liver fat. However, only improvements from the LFHP diet were associated with improved whole-body and liver insulin sensitivity [122]. Such findings highlight the necessity of tools that can discriminate between changes in fat distribution and changes in metabolic tissue function.
Resolving the Amino Acid Paradox: The relationship between amino acids and insulin resistance is complex. While acute postprandial elevations of essential amino acids (EAAs) promote muscle protein synthesis and can improve metabolic health, chronic fasting elevations of branched-chain amino acids (BCAAs) are strongly associated with insulin resistance [3]. This paradox may be explained by chronic nutrient overload fostering lipotoxicity. The HEC is critical for unraveling this dichotomy, as it can precisely measure how chronic versus acute amino acid exposure modulates insulin action in vivo.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Reagents
| Item | Function/Application | Example Usage & Rationale |
|---|---|---|
| Human Insulin Solution | To create a steady-state hyperinsulinemic condition during HEC. | Actrapid (Novo Nordisk) used at 56 mU/m²/min [120]. |
| D-[1⁴C] or D-[³H] Glucose | Tracer for measuring endogenous glucose production and kinetics during more advanced clamp protocols. | Allows for the calculation of Ra (rate of appearance) and Rd (rate of disappearance) of glucose. |
| [¹⁸F]FDG ([¹⁸F]Fluorodeoxyglucose) | Radioactive glucose analog for PET imaging to quantify tissue-specific metabolic activity under insulin stimulation. | Injected as an intravenous bolus (e.g., 4 MBq/kg) during HEC-PET/MRI to calculate tissue MRGlu [120]. |
| Tanita Body Composition Analyzer | Bioelectrical impedance device for measuring body fat %, visceral fat rating, and lean mass. | Model DC-430MA used in clinical studies to correlate VFR with HOMA-IR [123]. |
| Albumin Solution | Added to insulin infusates to prevent insulin adsorption to tubing and containers. | Personalized insulin solutions are prepared containing albumin to ensure accurate dosing [120]. |
| Gas Exchange Chamber & Microscope | For intravital video microscopy (IVVM) to study real-time microvascular hemodynamics in animal models. | Used in rodent studies to measure capillary RBC velocity and O2 saturation in response to insulin [124]. |
Signaling Pathways and Experimental Workflows
Amino Acid Sensing and Insulin Signaling Pathway
Hyperinsulinemic-Euglycemic Clamp Workflow
The strategic application of HOMA-IR, hyperinsulinemic-euglycemic clamps, and body composition analysis provides a powerful, multi-faceted toolkit for advancing research into the impact of dietary proteins and amino acids on glucose homeostasis. HOMA-IR offers a practical tool for population screening and longitudinal monitoring, the HEC remains the indispensable gold standard for precise quantification of whole-body and tissue-specific insulin action, and body composition analysis delivers critical context on how body fat distribution and ectopic fat deposition influence metabolic health. Integrating these methodologies allows researchers to dissect the complex mechanisms by which specific amino acids and dietary patterns modulate insulin sensitivity, paving the way for more personalized and effective nutritional strategies for the prevention and management of type 2 diabetes and related metabolic disorders.
Epidemiological Insights vs. Controlled Intervention Trial Findings
The investigation into the impact of dietary proteins and amino acids on glucose homeostasis is a cornerstone of nutritional metabolism research. This field relies on two fundamental, yet distinct, methodological approaches: epidemiological insights, which identify associations in broad populations, and controlled intervention trials, which establish causality under tightly regulated conditions. While epidemiological studies have highlighted correlations between branched-chain amino acid (BCAA) levels and metabolic disease risk, controlled interventions have revealed a more nuanced picture, demonstrating that the metabolic effects of protein intake are critically dependent on context, such as energy balance and the specific pattern of amino acid elevation. This whitepaper synthesizes evidence from both approaches to provide researchers and drug development professionals with a comprehensive technical guide, detailing key findings, experimental protocols, and the underlying molecular mechanisms.
Comparative Analysis of Research Findings
The table below synthesizes the primary findings from epidemiological studies and controlled intervention trials regarding dietary protein and amino acids.
Table 1: Contrasting Evidence from Epidemiological and Interventional Research
| Aspect of Investigation | Epidemiological Insights | Controlled Intervention Trial Findings |
|---|---|---|
| BCAA Levels & Insulin Resistance | Chronic postabsorptive elevations of BCAAs are consistently associated with an increased prevalence of insulin resistance and type 2 diabetes [2] [3]. | The causal link is context-dependent; acute, postprandial EAA elevations do not induce insulin resistance and can be beneficial [2]. |
| High-Protein Diets & Body Composition | Observational data often link certain dietary patterns with body weight and metabolic health outcomes. | During hypocaloric diets, high protein intake (up to 35% of calories) preserves fat-free mass and augments fat loss compared to standard protein diets [2]. |
| Primary Proposed Mechanism | Chronic hyperinsulinemia and nutrient overload leading to lipotoxicity, driven by persistent mTOR activation [2] [3]. | Leucine-induced, transient activation of mTOR and PGC-1α, promoting muscle protein synthesis and mitochondrial biogenesis [2]. |
| Overall Interpretation | Suggests BCAAs are predictive biomarkers for the development of insulin resistance. | Indicates that the anabolic, postprandial signal from EAAs/BCAAs is metabolically beneficial, particularly when it stimulates muscle tissue. |
Detailed Experimental Protocols from Key Studies
To enable replication and critical evaluation, this section outlines the methodologies of pivotal controlled intervention trials.
Table 2: Detailed Protocol of a 10-Week Weight Loss Intervention [17]
| Protocol Component | Detailed Specification |
|---|---|
| Objective | To test if increased dietary protein with reduced carbohydrates stabilizes blood glucose and insulin during weight loss. |
| Participants | 24 adult women (>15% above ideal body weight). |
| Study Groups | - Protein Group (n=12): 1.6 g protein/(kg · d); CHO <40% of energy.- CHO Group (n=12): 0.8 g protein/(kg · d); CHO >55% of energy. |
| Diet Design | - Energy: Equal for both groups at 7100 kJ/d.- Fat: Equal for both groups at 50 g/d. |
| Test Meal | Administered after a 12-hour fast at the 10-week endpoint.- Protein Group Test Meal: 1.67 MJ, containing 39g CHO, 33g protein, 13g fat.- CHO Group Test Meal: 1.67 MJ, containing 57g CHO, 12g protein, 14g fat. |
| Primary Outcomes | - Fasting and postprandial plasma glucose and insulin.- Plasma amino acids.- Body weight. |
| Key Results | - Similar weight loss (Protein: 7.53 kg; CHO: 6.96 kg).- Protein Group had more stable fasting/postprandial glucose and a significantly lower postprandial insulin response. |
Another seminal trial compared high-protein (HP: 45% protein, 35% carbohydrate) and high-carbohydrate (HC: 20% protein, 60% carbohydrate) hypocaloric diets (800 kcal) in obese subjects [2]. The primary outcome was insulin-stimulated glucose disposal, measured via the euglycemic-hyperinsulinemic clamp method. The HP diet resulted in greater retention of fat-free mass and improved insulin sensitivity compared to the HC diet, underscoring the role of protein in preserving metabolic tissue during energy restriction [2].
Visualizing Key Signaling Pathways
The molecular mechanisms underlying the effects of amino acids on insulin sensitivity involve complex, interconnected pathways. The following diagrams, defined using the DOT language and adhering to the specified color palette and contrast rules, illustrate these pathways.
The Dual Role of mTOR in Insulin Sensitivity
Leucine-Induced Mitochondrial Biogenesis Pathway
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Methodologies for Investigating Amino Acids and Glucose Homeostasis
| Reagent / Methodology | Function & Application in Research |
|---|---|
| Euglycemic-Hyperinsulinemic Clamp | The gold-standard method for directly measuring whole-body insulin sensitivity. It involves the continuous infusion of insulin and a variable glucose infusion to maintain euglycemia, quantifying glucose disposal rate (M-value) [2]. |
| Mass Spectrometry | Essential for the precise quantification of specific amino acid concentrations (e.g., BCAAs, EAAs) in plasma and tissue samples from clinical and preclinical studies [2] [3]. |
| 3-Methylhistidine Excretion | A biochemical marker used to assess the rate of muscle protein breakdown, often measured in urine [2]. |
| β-hydroxy-β-methylbutyrate (HMB) | A metabolite of leucine used in supplementation studies to investigate its effects on mitigating muscle atrophy and promoting mitochondrial function (e.g., OXPHOS complex content) during inactivity [2]. |
| PGC-1α Knockout Models | Genetic models (e.g., in mice) used to establish the causal role of PGC-1α in mitochondrial metabolism and its link to insulin resistance and hepatic steatosis [2]. |
| Specific mTOR Pathway Modulators | Pharmacological agents (e.g., rapamycin) used to inhibit mTOR signaling, allowing researchers to dissect its specific role in mediating the effects of amino acids on protein synthesis and insulin action. |
The integration of epidemiological and controlled interventional research is vital for a complete understanding of how dietary proteins and amino acids regulate glucose homeostasis. While population studies successfully identified BCAAs as strong biomarkers for diabetes risk, controlled trials were necessary to reveal the critical distinction between the detrimental effects of chronic fasting elevations and the beneficial anabolic effects of acute postprandial elevations. The key mechanistic insight is the context-dependent role of the mTOR pathway, which, when chronically activated, can impair insulin signaling, but when transiently activated by postprandial EAAs, promotes muscle protein synthesis and mitochondrial biogenesis, thereby enhancing metabolic health. For future drug development and personalized nutrition, strategies must leverage the anabolic potential of proteins and specific amino acids while avoiding states of chronic nutrient excess that drive lipotoxicity and insulin resistance.
Long-Term Outcomes and Safety Considerations of High-Protein Dietary Regimens
High-protein diets (HPDs), often defined as providing over 20% of total daily energy from protein or more than 1.2-1.6 g/kg/day, have garnered significant scientific and public interest for weight management and metabolic health [125]. Within research on dietary proteins and amino acids' impact on glucose homeostasis, HPDs present a complex interplay of benefits and risks. Evidence suggests that protein intake modulates energy metabolism through satiety enhancement and increased thermic effect of feeding, while specific amino acids directly influence insulin secretion, insulin signaling pathways, and metabolic fate [126] [127]. This technical review examines the long-term outcomes and safety considerations of HPDs, synthesizing recent clinical evidence, elucidating underlying molecular mechanisms, and providing methodological guidance for researchers investigating protein-mediated metabolic effects. The analysis is particularly framed within the context of optimizing dietary strategies for glucose regulation while understanding potential long-term physiological consequences.
Molecular Mechanisms: Protein-Mediated Metabolic Signaling Pathways
Dietary proteins exert their metabolic effects through multiple signaling pathways that regulate glucose homeostasis, cellular growth, and metabolic stress responses. Understanding these mechanisms is crucial for contextualizing both benefits and risks of long-term high-protein intake.
Amino Acid Sensing and mTORC1 Signaling
The mechanistic target of rapamycin complex 1 (mTORC1) serves as a central nutrient sensor that integrates amino acid availability with cellular growth and metabolism. As illustrated in Figure 1, specific amino acids activate mTORC1 through distinct sensor proteins:
- Leucine-mediated activation: Under sufficient leucine conditions, leucine binds to Sestrin-2, causing its dissociation from GATOR2. This releases inhibition on Rag GTPases, allowing mTORC1 translocation to lysosomal membranes and subsequent activation [128].
- Arginine-mediated activation: Arginine binding to CASTOR1 prevents its interaction with GATOR2, similarly resulting in mTORC1 activation [128].
- Methionine/S-adenosylmethionine (SAM) axis: Methionine is converted to SAM, which activates mTORC1 by disrupting the SAMTOR-GATOR1 complex. High SAM concentrations also methylate protein phosphatase 2A (PP2A), enhancing Npr2 dephosphorylation and promoting autophagy inhibition [128].
Figure 1: Amino acid-sensing pathways regulating mTORC1 activity
Chronic mTORC1 activation from sustained high protein intake may contribute to insulin resistance through negative feedback on insulin receptor substrate (IRS) proteins, presenting a potential limitation for long-term HPD use in glucose homeostasis management [128].
FGF21 Signaling in Protein Restriction
Conversely, reduced protein intake activates an adaptive metabolic response through fibroblast growth factor 21 (FGF21), as shown in Figure 2. Protein restriction activates general control nonderepressible 2 (GCN2), which phosphorylates eukaryotic initiation factor 2α (eIF2α), leading to activating transcription factor 4 (ATF4) induction and subsequent hepatic FGF21 production [128]. Elevated FGF21 enhances insulin sensitivity, glucose uptake, and fatty acid oxidation, explaining some metabolic benefits of moderate protein diets. This pathway represents a counter-regulatory mechanism to HPD-mediated signaling.
Figure 2: FGF21 pathway activation under low protein conditions
Long-Term Health Outcomes: Evidence Synthesis
Long-term studies reveal complex, condition-dependent outcomes for HPDs, with significant implications for glucose homeostasis research and clinical practice.
Table 1: Long-Term Health Outcomes of High-Protein Diets
| Health Domain | Reported Outcomes | Protein Intake Range | Population Characteristics | Key References |
|---|---|---|---|---|
| Type 2 Diabetes Risk | U-shaped association (protective range: 12.20-16.85%E); Plant protein inversely associated with risk | 14.53%E optimal cut-point | General population; narrower protective range (12.20-15.35%E) in hypertension | [6] |
| Cardiovascular Outcomes | No significant association with cardiovascular mortality, stroke, or non-fatal MI | >18%E from protein | Adults without established CVD | [125] |
| Body Composition | Short-term weight loss via satiety ↑, thermogenesis ↑; long-term sustainability uncertain | 25-35%E | Mixed populations | [126] [127] |
| Bone Health | Potential long-term bone loss via urinary calcium excretion ↑ | >2-3x RDA | General population | [126] |
| Critical Care Outcomes | In-hospital mortality ↓, muscle mass preservation ↑ | 1.67 g/kg/day vs. 0.93 g/kg/day | Critically ill patients | [129] |
Glycemic Control and Type 2 Diabetes Risk
The relationship between long-term protein intake and type 2 diabetes (T2D) risk demonstrates a non-linear pattern. A comprehensive registry-based cohort study and meta-analysis revealed a U-shaped association, with both insufficient and excessive protein intake increasing T2D incidence [6]. The optimal protective range was identified at 12.20-16.85% of total energy intake (%E), with a cut-point at 14.53%E. This relationship varied significantly by metabolic status:
- Hypertension: Narrower protective range (12.20-15.35%E)
- NAFLD: Linear inverse association (HR per 1%E: 0.952)
- Hyperlipidemia/Central obesity: No significant association
Notably, plant protein sources demonstrated an inverse association with T2D risk, suggesting protein quality modifies long-term outcomes [6]. Proposed mechanisms include differential effects of amino acid composition on insulin secretion, insulin resistance, and metabolic signaling pathways.
Cardiovascular Outcomes
Current evidence does not support significant adverse cardiovascular effects of HPDs in generally healthy populations. A 2023 meta-analysis of 14 prospective cohort studies found no statistically significant differences in cardiovascular mortality, stroke, or composite cardiovascular endpoints between high-protein and normal-protein diets [125]. However, study authors noted important limitations, including variable definitions of "high protein" intake and potential confounding by overall dietary patterns.
Experimental research has identified potential mechanisms for cardiovascular risk with specific amino acids. Excessive leucine intake triggers macrophage mTORC1 signaling, promoting atherosclerosis through increased foam cell formation and vascular inflammation [84]. This suggests that the specific amino acid composition, rather than total protein quantity, may drive cardiovascular outcomes in the long term.
Special Populations: Renal Function and Critical Illness
The long-term safety of HPDs varies substantially across patient populations, with pre-existing conditions modifying risk-benefit ratios:
- Chronic Kidney Disease: HPDs may worsen renal function through increased glomerular filtration pressure and accelerated decline in glomerular filtration rate [126] [130]. Patients with diabetes appear particularly susceptible to this effect.
- Critical Illness: Contrary to conventional caution, a 2025 RCT in critically ill patients demonstrated significantly reduced in-hospital mortality (28.6% vs. 57.1%) and better muscle mass preservation with higher protein intake (1.67 g/kg/day vs. 0.93 g/kg/day) [129]. This suggests catabolic states may warrant different protein recommendations.
Methodological Approaches for Glucose Homeostasis Research
Investigating HPDs in the context of glucose regulation requires precise methodological approaches to generate comparable, clinically relevant data.
Metabolic Phenotyping Protocols
Comprehensive metabolic phenotyping should incorporate the following methodologies:
- Continuous Glucose Monitoring (CGM): Assess 24-hour glucose variability, postprandial responses, and time-in-range metrics during dietary interventions [68].
- Oral Glucose Tolerance Tests (OGTT): Measure glucose tolerance and insulin secretion capacity at baseline and post-intervention.
- Hyperinsulinemic-Euglycemic Clamps: Quantify insulin sensitivity directly (gold standard).
- Metabolomic Profiling: Analyze amino acids, lipids, organic acids, and other metabolites to identify potential mechanisms [68].
- Body Composition Analysis: Use DEXA, MRI, or bioimpedance to differentiate lean mass from fat mass changes.
Dietary Challenge Tests for Macronutrient Response
Standardized challenge tests can elucidate individual variability in response to different protein sources and quantities:
- Procedure: Participants consume test meals (e.g., 30g protein from various sources) after an overnight fast, with blood sampling at baseline, 30, 60, 120, and 180 minutes postprandial.
- Analytes: Glucose, insulin, amino acids, glucagon, GLP-1.
- Test Meals: Should include diverse protein sources (whey, casein, soy, pea, beef) to assess source-dependent effects.
Research using similar approaches has demonstrated substantial interindividual variability in postprandial glucose responses to different carbohydrates, suggesting parallel variability may exist for protein responses [68].
Assessment of Protein Intake and Compliance
Accurate protein intake assessment is methodologically challenging but essential for valid intervention studies:
- Dietary Records: Multiple-day weighed food records provide the most precise intake data but impose significant participant burden.
- Biomarkers: 24-hour urinary nitrogen excretion remains the gold standard validation method for protein intake assessment.
- Stable Isotopes: Carbon-13 and nitrogen-15 isotopic markers can objectively track specific protein sources.
The Scientist's Toolkit: Essential Research Reagents and Methods
Table 2: Key Research Reagents and Methodologies for Protein-Glucose Homeostasis Studies
| Reagent/Method | Application | Technical Considerations |
|---|---|---|
| Continuous Glucose Monitors | Ambulatory glucose monitoring during free-living conditions | Measures interstitial fluid glucose; requires calibration; provides high-frequency data [68] |
| Amino Acid Analytical Kits | Quantifying plasma/serum amino acid concentrations | HPLC-MS/MS preferred for sensitivity; fasting and postprandial measurements needed [128] |
| Validated FFQs | Assessing habitual protein intake in observational studies | Must be validated for specific population; semi-quantitative; recall bias potential [6] |
| Stable Isotope Tracers | Measuring protein metabolism, gluconeogenesis | ²H- or ¹³C-labeled amino acids; requires specialized mass spectrometry [128] |
| mTOR Pathway Antibodies | Western blot analysis of signaling activation | Key targets: p-mTOR, p-S6K1, p-4E-BP1; requires careful sample preparation [128] |
| Body Composition Analyzers | Quantifying lean mass changes | DEXA gold standard; MRI for organ-specific analysis; BIA for field studies [129] |
Long-term outcomes of high-protein dietary regimens present a complex risk-benefit profile that varies by individual metabolic characteristics, protein sources, and specific health outcomes. The U-shaped relationship with T2D risk, coupled with source-dependent effects, underscores the need for personalized nutritional approaches rather than universal recommendations. Future research should prioritize:
- Precision Nutrition Approaches: Identifying genetic, metabolic, and microbiome biomarkers that predict individual responses to HPDs.
- Source-Specific Effects: Controlled trials comparing long-term outcomes of animal versus plant-based HPDs on glucose homeostasis.
- Molecular Mechanism Elucidation: Further exploration of how specific amino acids regulate insulin signaling, mitochondrial function, and metabolic health.
- Lifecycle Considerations: Age-specific protein requirements and long-term outcomes across the lifespan.
The integration of these research directions will advance our understanding of how dietary proteins influence glucose homeostasis and contribute to evidence-based dietary recommendations for metabolic health maintenance and disease prevention.
Conclusion
The interplay between dietary proteins, amino acids, and glucose homeostasis is complex and highly context-dependent. Key takeaways indicate that high-protein diets and specific amino acids, particularly when used in a hypocaloric setting, are potent tools for improving insulin sensitivity, primarily through skeletal muscle preservation and enhanced mitochondrial function. However, the source of protein appears less critical than the overall dietary pattern and energy balance. The paradoxical role of BCAAs underscores that nutrient signaling is not binary; chronic elevation, often linked to obesity and metabolic dysregulation, can promote insulin resistance, whereas acute postprandial exposure supports anabolism. Future research must prioritize long-term studies, personalized nutrition approaches accounting for genetic and microbiome profiles, and the development of targeted therapies that harness the beneficial signaling of amino acids while mitigating their potential lipotoxic and inflammatory side effects. For drug development, modulating amino acid-sensing pathways like mTOR presents a promising, yet challenging, frontier for treating metabolic diseases.
References
- 1. Dietary proteins, amino acids and insulin resistance [https://pubmed.ncbi.nlm.nih.gov/41190149/]
- 2. Dietary proteins, amino acids and insulin resistance: a mini ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1671286/full]
- 3. Dietary proteins, amino acids and insulin resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12580144/]
- 4. Low‐calorie, high‐protein diets, regardless ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11618321/]
- 5. An increase in dietary protein improves the blood glucose ... [https://www.sciencedirect.com/science/article/pii/S0002916522033822]
- 6. Dietary protein and risk of type 2 diabetes: findings from a ... [https://www.nature.com/articles/s41387-025-00380-z]
- 7. Regulation of energy homeostasis by the small guanosine ... [https://www.sciencedirect.com/science/article/abs/pii/S0898656825003948]
- 8. Molecular signatures of skeletal muscle insulin resistance [https://www.nature.com/articles/s41392-025-02412-7]
- 9. Amino acids are necessary for the insulin-induced ... [https://www.sciencedirect.com/science/article/abs/pii/S0261561408000344#!]
- 10. Effect of high intakes of protein-only and carbohydrate ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1618142/full]
- 11. Amino acid-dependent control of mTORC1 signaling: a variety of regulatory modes | Journal of Biomedical Science | Full Text [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-020-00679-2]
- 12. Signaling pathways involved in translational control of ... [https://pubmed.ncbi.nlm.nih.gov/11238774/]
- 13. Leucine-Enriched Nutrients and the Regulation of mTOR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5096790/]
- 14. Current Data on the Role of Amino Acids in ... [https://www.mdpi.com/1422-0067/26/15/7129]
- 15. Research progress in the role and mechanism of Leucine ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2023.1252089/full]
- 16. How the amino acid leucine activates the key cell-growth regulator mTOR [https://www.nature.com/articles/d41586-021-01943-7]
- 17. Increased Dietary Protein Modifies Glucose and Insulin ... [https://www.sciencedirect.com/science/article/pii/S0022316622156154]
- 18. The contradictory role of branched - chain in lifespan and... amino acids [https://pmc.ncbi.nlm.nih.gov/articles/PMC10318341/]
- 19. Branched-chain amino acids in health and disease [https://nutritionandmetabolism.biomedcentral.com/articles/10.1186/s12986-018-0271-1]
- 20. drive glucose dysregulation and BCAAs ... acutely insulin resistance [https://www.nature.com/articles/s41387-024-00298-y?error=cookies_not_supported]
- 21. The adverse metabolic effects of branched-chain amino acids ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8102360/]
- 22. Branched-chain amino acids supplementation induces ... [https://pubmed.ncbi.nlm.nih.gov/39267003/]
- 23. Branched-chain amino acids supplementation induces insulin ... [https://molmed.biomedcentral.com/articles/10.1186/s10020-024-00894-9]
- 24. Effects of branched-chain amino acids on glucose ... [https://www.sciencedirect.com/science/article/pii/S000291652203218X]
- 25. PGC-1α Is a Master Regulator of Mitochondrial Lifecycle and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10215733/]
- 26. Caloric Restriction and the Nutrient-Sensing PGC-1α in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3399559/]
- 27. SIRT1 activation promotes energy homeostasis and ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-023-04440-9]
- 28. Effects of Resveratrol and SIRT1 on PGC-1α Activity and ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.1001603]
- 29. Specific Sirt1 Activator-mediated Improvement in Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5405165/]
- 30. Role of amino acid metabolism in mitochondrial homeostasis [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2023.1127618/full]
- 31. Amino acids and mitochondrial biogenesis [https://pubmed.ncbi.nlm.nih.gov/18514622/]
- 32. SIRT1 enhances glucose tolerance by potentiating brown ... [https://www.sciencedirect.com/science/article/pii/S2212877814002099]
- 33. PGC-1α controls mitochondrial biogenesis and dynamics ... [https://www.aging-us.com/article/100790/text]
- 34. Dietary Protein and the Blood Glucose Concentration - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3636610/]
- 35. Glucagon acutely regulates hepatic amino acid catabolism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7560169/]
- 36. Regulation of glucose metabolism from a liver-centric ... [https://www.nature.com/articles/emm2015122]
- 37. Homeostasis of glucose and lipid metabolism during ... [https://www.nature.com/articles/s41467-025-64110-w]
- 38. Regulation of hepatic glucose metabolism in health and disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC5777172/]
- 39. Efficacy of a High-Protein Diet to Lower Glycemic Levels in ... [https://pubmed.ncbi.nlm.nih.gov/39456742/]
- 40. Efficacy of a High-Protein Diet to Lower Glycemic Levels in ... [https://www.mdpi.com/1422-0067/25/20/10959]
- 41. Evaluation of Effects of a High-Protein Hypocaloric Diet on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11960474/]
- 42. Hypocaloric high-protein diet improves glucose oxidation ... [https://pubmed.ncbi.nlm.nih.gov/7990700/]
- 43. An Exploratory Study of the Role of Dietary Proteins in ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2021.769773/full]
- 44. Dietary protein, amino acids and type 2 diabetes mellitus [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2024.1445981/full]
- 45. Role of dietary proteins and amino acids in the ... [https://pubmed.ncbi.nlm.nih.gov/17666010/]
- 46. Dietary Protein Consumption and the Risk of Type 2 Diabetes [https://pmc.ncbi.nlm.nih.gov/articles/PMC6893550/]
- 47. Associations of Dietary Protein Intake and Amino Acid ... [https://www.mdpi.com/2072-6643/17/13/2168]
- 48. Comparing exercise modalities during caloric restriction [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1579024/full]
- 49. Distinct and additive effects of calorie restriction ... [https://www.nature.com/articles/s41467-022-29714-6]
- 50. Altered proteome turnover and remodeling by short-term ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4040127/]
- 51. Exercise and Caloric Restriction Exert Different Benefits on ... [https://www.mdpi.com/2072-6643/15/23/5004]
- 52. Sarcopenic obesity and weight loss-induced muscle mass loss [https://pmc.ncbi.nlm.nih.gov/articles/PMC12147736/]
- 53. Essential amino acids preserve intestinal barrier integrity ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1694723/full]
- 54. Effects of Amino Acid Supplementation on Muscle protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530991/]
- 55. The Effects of an Amino Acid Supplement on Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3230243/]
- 56. Use of Amino Acids as Supplements for Matching Nutrition ... [https://www.mdpi.com/2072-6643/17/16/2667]
- 57. Review Amino acid transporters as modulators of glucose ... [https://www.sciencedirect.com/science/article/abs/pii/S1043276021002678]
- 58. Amino Acid Associations in Healthy and Unhealthy Obesity [https://www.sciencedirect.com/science/article/pii/S0022316625003098]
- 59. Impact of 9 Days of Bed Rest on Hepatic and Peripheral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2780872/]
- 60. Exercise attenuates bed rest-induced increases in insulin ... [https://www.nature.com/articles/s41598-025-12770-5]
- 61. Bed-rest-induced insulin resistance occurs primarily in ... [https://www.sciencedirect.com/science/article/pii/0026049588900182]
- 62. The impact of bed rest on human skeletal muscle metabolism [https://pmc.ncbi.nlm.nih.gov/articles/PMC10829795/]
- 63. The Essentiality of Amino Acids in Healthiness and Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12124235/]
- 64. Systematic review and meta-analysis of different dietary ... [https://www.sciencedirect.com/science/article/pii/S0002916523054400]
- 65. How dietary amino acids and high protein diets influence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9875820/]
- 66. Regulation of Glucose Homeostasis by GLP-1 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4159612/]
- 67. Protein- and Calcium-Mediated GLP-1 Secretion [https://pmc.ncbi.nlm.nih.gov/articles/PMC8634310/]
- 68. Blood sugar response to various carbohydrates can point to ... [https://med.stanford.edu/news/all-news/2025/06/carb-sugar-spikes.html]
- 69. Dietary impact on fasting and stimulated GLP-1 secretion in ... [https://www.sciencedirect.com/science/article/pii/S0002916524000054]
- 70. Glucagon-like peptide-1 receptor: mechanisms and ... [https://www.nature.com/articles/s41392-024-01931-z]
- 71. Animal and plant‐based proteins have different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10420774/]
- 72. Plant Protein and Animal Proteins: Do They Differentially ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4642426/]
- 73. Impacts of dietary animal and plant protein on weight and ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1412182/full]
- 74. Higher ratio of plant protein to animal protein may improve ... [https://hsph.harvard.edu/news/higher-ratio-of-plant-protein-to-animal-protein-may-improve-heart-health/]
- 75. Does partial replacement of animal protein with plant ... [https://www.nature.com/articles/s41387-025-00401-x]
- 76. Plant and Animal-Based Dietary Patterns ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12608340/]
- 77. Physiology, Glucose Metabolism - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK560599/]
- 78. Amino acid metabolism in health and disease [https://www.nature.com/articles/s41392-023-01569-3]
- 79. Amino Acid Metabolite Profiling for Predicting and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12411142/]
- 80. Slow and fast dietary proteins differently modulate ... [https://pubmed.ncbi.nlm.nih.gov/9405716/]
- 81. Role of branched-chain amino acid metabolism in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9356071/]
- 82. BCAAs acutely drive glucose dysregulation and insulin ... [https://www.nature.com/articles/s41387-024-00298-y]
- 83. BCAA metabolism in cancer progression and therapy ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1595176/full]
- 84. Too Much of a Good Thing: Overconsuming Protein Can Be ... [https://medicine.missouri.edu/news/too-much-good-thing-overconsuming-protein-can-be-bad-your-health]
- 85. Branched chain amino acids impact health and lifespan ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6814438/]
- 86. Evaluation of therapeutic strategies targeting BCAA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9744226/]
- 87. Dietary fibre and the gut microbiome: implications for ... [https://pubmed.ncbi.nlm.nih.gov/40889147/]
- 88. Mechanisms and implications of the gut microbial ... [https://www.nature.com/articles/s44324-025-00066-1]
- 89. Gut Microbiota‐Derived Metabolites Orchestrate Metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406765/]
- 90. Mechanisms and key mediators of gut microbiota and type ... [https://www.sciencedirect.com/science/article/pii/S2590097825000254]
- 91. Recent advances in gut microbiota-mediated regulation of ... [https://www.oaepublish.com/articles/mrr.2025.25]
- 92. Integrated gut microbiota and metabolomic profiling reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12591972/]
- 93. Mechanistic insights into β-glucans and gut microbiota ... [https://link.springer.com/article/10.1007/s44187-025-00503-6]
- 94. Gut Microbiota: An Ally in the Mechanisms and ... [https://www.mdpi.com/2624-5647/7/4/68]
- 95. Microbe-dependent and independent effects of diet on ... [https://www.sciencedirect.com/science/article/abs/pii/S030881462502103X]
- 96. The relationship between gut microbiome and human ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1516010/full]
- 97. The Future of Protein Drugs in 2025: Breakthroughs, ... [https://blog.bccresearch.com/the-future-of-protein-drugs-in-2025-breakthroughs-challenges-and-whats-next]
- 98. Polypeptide-protein conjugation: A new paradigm for ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925005735]
- 99. Adhering to recommended dietary protein intake for optimizing ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d4ra08221d]
- 100. Associations of temporal protein patterns with diabetes and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506268/]
- 101. Progress in peptide and protein therapeutics: Challenges ... [https://www.sciencedirect.com/science/article/pii/S221138352500704X]
- 102. Strategies to Enhance Protein Delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11924232/]
- 103. How dietary amino acids and high protein diets influence ... [https://pubmed.ncbi.nlm.nih.gov/36695783/]
- 104. Can high-protein diabetes-specific oral nutritional ... [https://www.nature.com/articles/s41387-025-00399-2]
- 105. Low-calorie, high-protein diets, regardless of ... [https://pubmed.ncbi.nlm.nih.gov/39420528/]
- 106. High and normal protein diets improve body composition and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10421635/]
- 107. Long-term effects of dietary protein and carbohydrate ... [https://link.springer.com/article/10.1007/s00125-025-06560-x]
- 108. Mediterranean Diet Meal Plan for Diabetes [https://diet.mayoclinic.org/us/blog/2025/mediterranean-diet-diabetes-blood-sugar-control-backed-by-science/]
- 109. Effects of the Mediterranean Diet on the Components ... [https://www.mdpi.com/2072-6643/17/2/358]
- 110. DASH-style diet helps control blood glucose [https://www.nih.gov/news-events/nih-research-matters/dash-style-diet-helps-control-blood-glucose]
- 111. The DASH diet in diabetes related complications or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12602225/]
- 112. DASH Diet Modified for Diabetes Lowers Blood Sugar Levels ... [https://publichealth.jhu.edu/2025/dash-diet-modified-for-diabetes-lowers-blood-sugar-levels-in-clinical-trial-of-adults-with-type-2-diabetes]
- 113. Ketogenic Diets for Body Weight Loss: A Comparison with ... [https://www.mdpi.com/2072-6643/17/6/965]
- 114. Low-Calorie, High-Protein Ketogenic Diet ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114320/]
- 115. Beneficial Effect of the Mediterranean Diet on the Reduction of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12195878/]
- 116. New Study in Mice Reveals Long-Term Metabolic Risks ... [https://healthcare.utah.edu/newsroom/news/2025/10/new-study-mice-reveals-long-term-metabolic-risks-of-ketogenic-diet]
- 117. A ketogenic diet enhances aerobic exercise adaptation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11838742/]
- 118. Assessment HOMA as a predictor for new onset diabetes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10652621/]
- 119. Clinical and biochemical indicators of homeostasis model ... [https://www.sciencedirect.com/science/article/pii/S172649011100219X]
- 120. Tissue-specific and whole-body insulin sensitivity by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12331569/]
- 121. Protocol for the hyperinsulinemic euglycemic clamp to ... [https://www.sciencedirect.com/science/article/pii/S2666166724003083]
- 122. Body composition and body fat distribution in tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11003022/]
- 123. A Retrospective Analysis | Gołacki | Clinical Diabetology [https://journals.viamedica.pl/clinical_diabetology/article/view/102456]
- 124. Skeletal muscle microvascular hemodynamic responses ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2025.1568145/full]
- 125. The Impact of High Protein Diets on Cardiovascular ... [https://www.mdpi.com/2072-6643/15/6/1372]
- 126. - High weight-loss protein : are they safe and do they work? diets [https://pubmed.ncbi.nlm.nih.gov/12144197/]
- 127. The role of high-protein diets in the management ... [https://pubmed.ncbi.nlm.nih.gov/40889146/]
- 128. The impact of dietary protein intake on longevity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6562018/]
- 129. The efficacy of high-protein nutritional support on mortality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506466/]
- 130. - High : Are they safe? - Mayo Clinic protein diets [https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/expert-answers/high-protein-diets/faq-20058207]