Comparative Analysis of Predictive Interstitial Glucose Classification Models: From Traditional ML to Advanced Deep Learning
This article provides a comprehensive comparative analysis of predictive models for classifying interstitial glucose levels, a critical task for modern diabetes management.
Comparative Analysis of Predictive Interstitial Glucose Classification Models: From Traditional ML to Advanced Deep Learning
Abstract
This article provides a comprehensive comparative analysis of predictive models for classifying interstitial glucose levels, a critical task for modern diabetes management. Aimed at researchers, scientists, and drug development professionals, it explores the evolution from traditional statistical methods to sophisticated machine learning and deep learning architectures. The review systematically covers the foundational principles of glucose classification, details the implementation and application of diverse algorithmic methodologies, addresses common challenges and optimization strategies, and presents a rigorous validation framework for model performance. By synthesizing recent research, this analysis offers valuable insights for developing robust, accurate, and clinically reliable tools to predict hypoglycemia, euglycemia, and hyperglycemia, ultimately supporting advancements in personalized medicine and therapeutic development.
The Fundamentals of Interstitial Glucose Prediction and Clinical Imperatives
The precise classification of interstitial glucose levels into hypoglycemia, euglycemia, and hyperglycemia represents a fundamental component in modern diabetes management and predictive model research. These clinically defined thresholds serve as the critical endpoints for developing machine learning algorithms aimed at forecasting glycemic excursions, enabling proactive interventions for individuals with diabetes. The American Diabetes Association (ADA) Standards of Care establish specific glycemic targets that have been widely adopted in both clinical practice and research settings, providing a standardized framework for evaluating glycemic status [1]. Within the research domain, these classifications form the essential basis for training and testing predictive models that analyze continuous glucose monitoring (CGM) data to forecast future glucose levels, thereby facilitating personalized treatment approaches and reducing the risk of acute complications [2] [3].
The emergence of advanced analytical approaches, collectively termed "CGM Data Analysis 2.0," which encompasses functional data analysis and artificial intelligence (AI), has further emphasized the importance of precise glucose classification [3]. These methodologies move beyond traditional summary statistics to model entire glucose trajectories as dynamic processes, offering more nuanced insights into glycemic patterns and variability. This article provides a comprehensive analysis of the established clinical thresholds for glucose classification and examines their application within comparative studies of predictive interstitial glucose classification models, with particular focus on the experimental protocols and performance metrics relevant to researchers and drug development professionals.
Established Clinical Thresholds for Glucose Classification
Standard Glycemic Categories and Definitions
International consensus guidelines, primarily from the ADA and the Advanced Technologies & Treatments for Diabetes (ATTD) congress, have established standardized thresholds for classifying interstitial glucose levels. These classifications are universally employed in clinical practice and research methodologies [1] [4].
Table 1: Standard Clinical Thresholds for Glucose Classification
| Glucose Class | Threshold Range (mg/dL) | Clinical Significance |
|---|---|---|
| Hypoglycemia | < 70 | Level 1 clinically significant hypoglycemia [1] [4] |
| < 54 | Level 2 hypoglycemia [5] | |
| Euglycemia | 70 - 180 | Target glucose range [2] [1] [6] |
| Hyperglycemia | > 180 | Level 1 hyperglycemia [2] [1] [6] |
| > 250 | Level 2 hyperglycemia [5] [4] |
For healthy individuals without diabetes, studies using continuous glucose monitoring (CGM) have shown that glucose levels typically remain between 70-140 mg/dL for over 90% of the day, with mean 24-hour glucose levels approximately 99-105 mg/dL [7]. This highlights the more stringent natural glycemic regulation compared to the broader targets used in diabetes management.
Key Metrics for Glycemic Assessment
Beyond threshold classification, consensus guidelines recommend specific metrics for a comprehensive assessment of glycemic status, particularly using CGM data. Time in Range (TIR), Time Below Range (TBR), and Time Above Range (TAR) provide a more dynamic view of glycemic control [1]. For patients with diabetes and concurrent renal disease, the international consensus recommends specific targets, including ≤1% TBR (<70 mg/dL), ≤10% TAR level 2 (>250 mg/dL), and ≥50% TIR (70–180 mg/dL) [4].
Comparative Analysis of Predictive Glucose Classification Models
Performance Comparison of Predictive Models
Research directly compares the efficacy of various machine learning models in predicting future glucose classifications. These studies typically use the standard clinical thresholds to define the prediction classes and evaluate performance using metrics such as precision, recall, and accuracy over different prediction horizons (PH).
Table 2: Comparative Performance of Glucose Classification Models
| Predictive Model | Prediction Horizon | Hypoglycemia (<70 mg/dL) Recall | Euglycemia (70-180 mg/dL) Recall | Hyperglycemia (>180 mg/dL) Recall | Key Strengths |
|---|---|---|---|---|---|
| Logistic Regression [2] [6] | 15 minutes | 98% | 91% | 96% | Superior short-term prediction, particularly for hypoglycemia |
| LSTM [2] [6] | 1 hour | 87% | Not Specified | 85% | Best for longer-term prediction of hypo-/hyperglycemia |
| BiLSTM [8] | 5 minutes | RMSE: 13.42 mg/dL | MAPE: 0.12 | Clarke Error Grid D: 3.01% | High accuracy for very short-term prediction |
| LightGBM [9] | 15 minutes | RMSE: 18.49 mg/dL | MAPE: 15.58% | Non-invasive feasibility | Effective with non-invasive wearable data |
| Logistic Regression (Hemodialysis) [4] | 24 hours | F1: 0.48 (TabPFN) | Not Applicable | F1: 0.85 | Best for hyperglycemia prediction in complex comorbidities |
| ARIMA [2] [6] | 15 min & 1 hour | Underperformed other models | Underperformed other models | Underperformed other models | Serves as a baseline model |
Emerging Approaches: Non-Invasive Glucose Classification
A significant advancement in the field involves predicting glucose levels and their classifications using non-invasive wearable sensors, eliminating the need for invasive CGM. One study utilized an ensemble feature selection-based Light Gradient Boosting Machine (LightGBM) algorithm with data from non-invasive sensors measuring skin temperature (STEMP), blood volume pulse (BVP), heart rate (HR), electrodermal activity (EDA), and body temperature (BTEMP) [9]. This approach achieved a root mean squared error (RMSE) of 18.49 ± 0.1 mg/dL and demonstrated the feasibility of accurate, non-invasive glucose monitoring, paving the way for more accessible personalized dietary interventions [9].
Experimental Protocols and Research Methodologies
Data Sourcing and Preprocessing
Robust experimental protocols are fundamental to reliable model development. Research in this field typically utilizes two primary data sources: clinical cohort studies and in-silico simulations.
Clinical cohort data often comes from tightly controlled studies. For example, one analysis used data from the "COVAC-DM" study where participants with type 1 diabetes used CGM devices, with additional data on insulin dosing and carbohydrate intake [2]. To supplement real-world data, researchers often employ simulators like the CGM Simulator (e.g., Simglucose v0.2.1), which implements the UVA/Padova T1D Simulator to generate data for virtual patients across different age groups over multiple days, incorporating randomized meal and snack schedules [2].
A critical preprocessing step involves addressing the inherent sensor delay of approximately 10 minutes between interstitial glucose measurements and actual plasma glucose readings [2] [6]. Data is typically brought to a standard time frequency (e.g., 15-minute intervals), and gaps are addressed. For non-invasive approaches, feature engineering is crucial, deriving inputs like rate of change, variability indices, and moving averages from raw sensor data [2] [9].
Model Training and Evaluation Framework
The standard methodology for developing classification models follows a structured pipeline:
- Segmentation: The continuous CGM time series is divided into segments. A common approach uses a 24-hour feature segment preceding a dialysis session to predict glycemic outcomes over the subsequent 24-hour prediction segment [4].
- Feature Engineering: Features are extracted from the raw data. These can include CGM-derived metrics (mean glucose, variability indices), baseline patient characteristics (HbA1c, insulin use), and for non-invasive models, data from wearables (heart rate, skin temperature) [9] [4].
- Model Training and Validation: Models are trained and validated using techniques that prevent overfitting and ensure generalizability. Leave-one-participant-out cross-validation (LOPOCV) is a preferred method, as it trains the model on all participants except one, which is used for testing, iterating until each participant has been the test subject [9]. This accounts for individual variability.
- Performance Assessment: Models are evaluated based on their ability to correctly classify glucose levels. Standard metrics include:
- Recall (Sensitivity): The proportion of actual events (e.g., hypoglycemia) that were correctly identified. This is critical for safety.
- Precision: The proportion of predicted events that were correct.
- F1-Score: The harmonic mean of precision and recall.
- ROC-AUC: The area under the receiver operating characteristic curve, measuring overall classification performance.
- Root Mean Squared Error (RMSE): For regression-based prediction before classification.
- Clarke Error Grid Analysis (CEGA): Plots clinical accuracy of predictions, with zones A and B being clinically acceptable [9].
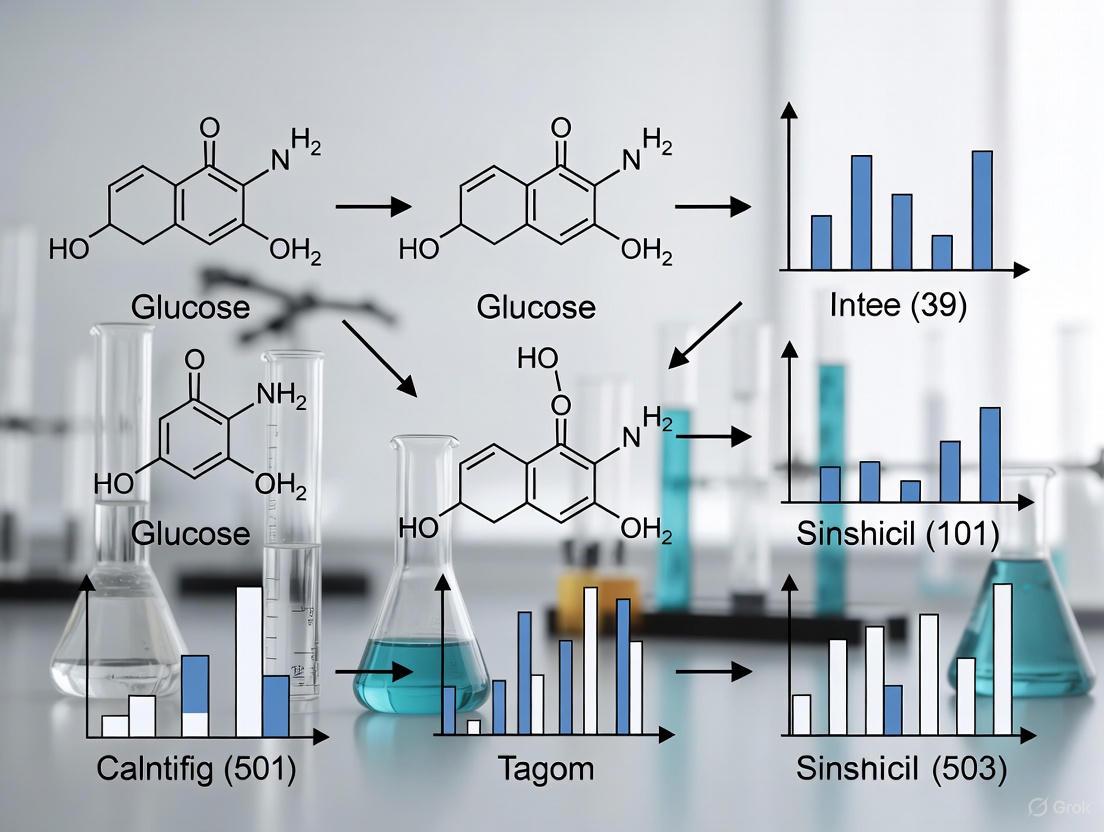
The following diagram illustrates the logical workflow for the experimental protocol used in comparative model studies:
Table 3: Essential Research Tools for Glucose Classification Studies
| Tool Category | Specific Example | Function in Research |
|---|---|---|
| CGM Platforms | Dexcom G6 [5] [4] | Provides ground-truth interstitial glucose measurements for model training and validation. |
| Non-Invasive Wearables | Empatica E4 [9] [5], Zephyr Bioharness [5] | Captures multimodal physiological data (PPG, EDA, ECG, accelerometry) for non-invasive prediction models. |
| In-Silico Simulators | Simglucose (UVA/Padova T1D Simulator) [2] | Generates large-scale, synthetic CGM and patient data for initial algorithm testing and development. |
| Programming Environments | Python [2] | Provides the ecosystem for implementing machine learning models (e.g., scikit-learn, TensorFlow, PyTorch). |
| Public Datasets | PhysioCGM Dataset [5], OhioT1DM Dataset [5] | Offers curated, multimodal physiological data with CGM for training and benchmarking models. |
| Analysis Software | Clarke Error Grid Analysis [9] | Standard method for evaluating the clinical accuracy of glucose predictions. |
The definition of glucose classes using standardized clinical thresholds is the cornerstone of developing and evaluating predictive models for interstitial glucose. Comparative analyses reveal that model performance is highly dependent on the prediction horizon, with simpler models like logistic regression excelling at short-term forecasts (15 minutes) and more complex models like LSTM networks achieving superior performance for longer-term predictions (1 hour). The field is rapidly evolving with the emergence of non-invasive monitoring using wearable sensors and advanced AI/ML techniques, collectively known as CGM Data Analysis 2.0. Future research directions will likely focus on hybrid or ensemble models that combine the strengths of multiple algorithms, the integration of non-invasive multimodal data, and the application of these models in specific, complex patient populations, such as those undergoing hemodialysis, to enhance the accuracy, reliability, and clinical applicability of glucose prediction systems.
The Role of Continuous Glucose Monitoring (CGM) in Data Acquisition
Continuous Glucose Monitoring (CGM) systems have revolutionized diabetes management by enabling the real-time acquisition of interstitial glucose concentrations, providing a rich data stream for predictive analytics and personalized treatment strategies [10]. Unlike traditional capillary blood glucose measurements that offer isolated snapshots, CGM devices generate dense time-series data, typically acquiring 288 measurements per day at 5-minute intervals [11]. This continuous data acquisition forms the foundation for advanced analytical approaches, including Functional Data Analysis (FDA) and artificial intelligence (AI) models, which transform raw sensor readings into clinically actionable insights [3]. The evolution from retrospective analysis to real-time predictive modeling represents a paradigm shift in how glucose data is utilized for therapeutic decision-making, particularly in the context of comparative analysis of predictive interstitial glucose classification models research.
For researchers and drug development professionals, understanding the data acquisition capabilities of different CGM systems is crucial for designing robust clinical trials and developing accurate predictive models. The quality, frequency, and reliability of acquired data directly impact the performance of classification algorithms aimed at predicting hypoglycemia, euglycemia, and hyperglycemia states [2]. This article provides a comprehensive comparison of CGM technologies and methodologies, focusing on their role in acquiring high-quality data for predictive model development.
CGM Technologies for Data Acquisition
Modern CGM systems employ diverse technological approaches to acquire interstitial glucose data, each with distinct implications for research applications. The leading systems available in 2025 include real-time CGMs (rtCGM) that continuously transmit data and intermittently scanned CGMs (isCGM) that require user activation for data retrieval [11]. These systems vary significantly in their form factors, wear duration, and data acquisition characteristics, which must be carefully considered when selecting platforms for research studies.
Table 1: Comparison of Leading CGM Systems for Data Acquisition (2025)
| CGM System | Wear Duration | Accuracy (MARD) | Warm-up Time | Data Points per Day | Key Research Applications |
|---|---|---|---|---|---|
| Dexcom G7 | 15 days | 8.2% (adults) [12] | 30 minutes [12] | 288 | High-accuracy predictive modeling; pediatric studies |
| Abbott FreeStyle Libre 3 | 14 days | 8.9% (2025 study) [12] | 1 hour (est.) | 288 | Large-scale observational studies; cost-effective research |
| Medtronic Guardian 4 | 7 days | 9-10% [12] | Varies | 288 | Insulin pump integration studies; closed-loop systems |
| Eversense 365 | 365 days | 8.8% [12] | Single annual warm-up [12] | 288 | Long-term glycemic variability studies; adherence research |
| Dexcom Stelo | 15 days | ~8-9% [12] | 30 minutes [12] | 288 | Type 2 diabetes non-insulin studies; wellness research |
The Mean Absolute Relative Difference (MARD) represents the standard metric for assessing CGM accuracy, with lower values indicating higher accuracy relative to reference blood glucose measurements [12]. MARD values below 10% are generally considered excellent for clinical and research applications, with most contemporary systems now achieving this benchmark. The Eversense 365 system is particularly noteworthy for research applications requiring long-term data acquisition without frequent sensor replacements, as its implantable nature and 365-day wear time enable unprecedented longitudinal studies of glycemic patterns [12].
Recent innovations are expanding the boundaries of CGM data acquisition. Biolinq's Shine wearable biosensor received FDA clearance in 2025 as a needle-free, non-invasive CGM that utilizes a microsensor array manufactured with semiconductor technology, registering up to 20 times more shallow than conventional CGM needles [13]. Glucotrack is advancing a 3-year monitor that measures glucose directly from blood rather than interstitial fluid, potentially eliminating the lag time associated with current CGM systems [13]. These emerging technologies promise to address current limitations in CGM data acquisition, including sensor lag and measurement disparities between interstitial fluid and blood glucose.
Comparative Analysis of Predictive Model Performance
The primary value of CGM-acquired data lies in its application for predicting future glucose states, enabling proactive interventions for diabetes management. Research has evaluated numerous predictive modeling approaches, each with distinct strengths and limitations for classifying interstitial glucose levels. The performance of these models varies significantly based on prediction horizon and the specific glycemic state being predicted.
Table 2: Performance Comparison of Predictive Glucose Classification Models
| Model Type | 15-Minute Prediction Recall | 60-Minute Prediction Recall | Optimal Prediction Horizon | Key Research Applications |
|---|---|---|---|---|
| Logistic Regression | Hyper: 96%, Norm: 91%, Hypo: 98% [2] | Lower performance vs. LSTM [2] | 15-30 minutes | Short-term hypoglycemia预警 |
| LSTM Networks | Strong performance, slightly lower than logistic regression [2] | Hyper: 85%, Hypo: 87% [2] | 30-60 minutes | Longer-term trend prediction; pattern recognition |
| Multimodal Deep Learning (CNN-BiLSTM with Attention) | MAPE: 6-24 mg/dL (varies by sensor) [14] | MAPE: 12-26 mg/dL (varies by sensor) [14] | 15-60 minutes | Personalized prediction integrating physiological context |
| ARIMA | Underperformed other models [2] | Underperformed other models [2] | Limited utility | Baseline comparison; simple trend analysis |
The comparative analysis reveals that model performance is highly dependent on prediction horizon. Logistic regression excels at short-term predictions (15 minutes), achieving remarkable recall rates of 98% for hypoglycemia and 96% for hyperglycemia [2]. In contrast, Long Short-Term Memory (LSTM) networks demonstrate superior performance for longer prediction horizons (60 minutes), making them better suited for anticipating glycemic trends that enable more proactive interventions [2].
Recent advances in multimodal deep learning architectures have demonstrated particularly promising results for personalized glucose prediction. One 2025 study achieved up to 96.7% prediction accuracy by integrating CGM data with baseline physiological information using a stacked Convolutional Neural Network (CNN) and Bidirectional LSTM (BiLSTM) with attention mechanisms [14]. This approach significantly outperformed unimodal models at 30-minute and 60-minute prediction horizons, highlighting the value of incorporating contextual physiological data alongside CGM time-series data [14].
Experimental Protocols for Predictive Model Development
Data Acquisition and Preprocessing
Robust experimental protocols are essential for developing accurate predictive models based on CGM data. The foundational step involves standardized data acquisition using CGM systems with appropriate accuracy characteristics (typically MARD <10%). Research-grade data collection should include:
- CGM Device Selection: Choose devices with validated accuracy metrics appropriate for the research population. For mixed-meal studies or rapid glycemic excursion research, prioritize devices with minimal sensor lag [2].
- Sampling Protocol: CGM values are typically sampled every 5 minutes, generating 288 measurements daily [11]. For predictive modeling, data is often restructured using a moving window approach (e.g., 30-minute samples with 5-minute moving windows) [14].
- Data Quality Control: Implement procedures to address signal loss, sensor noise, and compression hypoglycemia artifacts [2]. This may include Kalman smoothing techniques to correct inaccurate CGM readings [2].
- Stationarity Validation: Confirm stationarity of CGM time series using statistical tests like the Augmented Dickey-Fuller (ADF) test before model development [14].
Model Training and Validation
Following data acquisition and preprocessing, a structured approach to model training and validation ensures reproducible results:
- Data Partitioning: Implement rigorous cross-validation strategies, typically using patient-wise splits rather than temporal splits to prevent data leakage and ensure generalizability [14].
- Feature Engineering: For unimodal approaches using only CGM data, derive features including rate of change metrics, variability indices, rolling averages, and seasonal decomposition components [2]. For multimodal approaches, integrate baseline physiological parameters such as demographics, comorbidities, and medication usage [14].
- Evaluation Metrics: Utilize comprehensive evaluation metrics including precision, recall, F1-score, accuracy, and Mean Absolute Percentage Error (MAPE) for each glucose class (hypoglycemia, euglycemia, hyperglycemia) [2]. Implement clinical accuracy assessment using Parkes Error Grid analysis [14].
- Statistical Significance Testing: Perform appropriate statistical tests (e.g., t-tests) to validate performance differences between model architectures [14].
CGM Predictive Modeling Workflow
Advanced Analytical Approaches
Evolution from Traditional Statistics to Advanced Analytics
The analysis of CGM-acquired data has evolved significantly from traditional summary statistics to sophisticated analytical approaches collectively termed "CGM Data Analysis 2.0" [3]. This evolution reflects the growing recognition that traditional metrics oversimplify complex glucose dynamics:
- CGM Data Analysis 1.0: Traditional summary statistics include percentage time in glycemic ranges, glucose management indicator (GMI), and coefficient of variation [3]. While easily interpretable, these metrics lack granularity in capturing complex temporal patterns and are prone to distortion from missing data [3].
- CGM Data Analysis 2.0: Advanced approaches include Functional Data Analysis (FDA), machine learning (ML), and artificial intelligence (AI) [3]. These methods leverage the entire CGM time series, identifying nuanced phenotypes and enabling personalized decision-making frameworks [3].
Table 3: Comparison of CGM Data Analysis Approaches
| Analytical Method | Key Features | Advantages | Limitations | Representative Applications |
|---|---|---|---|---|
| Traditional Summary Statistics | Aggregated metrics: time-in-range, mean glucose, GMI, CV [3] | Simple to understand; clinical familiarity | Oversimplifies dynamic patterns; misses nuanced phenotypes | Clinical glucose summary reports; population-level comparisons |
| Functional Data Analysis (FDA) | Treats CGM trajectories as mathematical functions; models temporal dynamics [3] | Captures complex temporal patterns; identifies subtle phenotypes | Requires statistical expertise; more complex implementation | Inter-day reproducibility analysis; glucose curve phenotype identification [11] |
| Machine Learning (ML) | Predictive modeling using algorithms; pattern recognition in time series [3] | Predicts future glucose levels; classifies metabolic states | Requires large datasets; potential overfitting | Hypoglycemia prediction; glucose trend classification [2] |
| Artificial Intelligence (AI) | Integrates ML with advanced algorithms; combines multiple data sources [3] | Enables real-time adaptive interventions; personalized recommendations | Data privacy concerns; regulatory hurdles; validation complexity | AI-powered closed-loop systems; personalized therapy optimization [3] |
Functional Data Analysis for Enhanced Pattern Recognition
Functional Data Analysis represents a fundamental shift in how CGM-acquired data is processed and interpreted. Unlike traditional statistics that treat glucose measurements as discrete points, FDA treats the entire CGM trajectory as a smooth curve evolving over time [3]. This approach offers several distinct advantages for research applications:
- Comprehensive Temporal Analysis: FDA models glucose dynamics as continuous processes rather than aggregated summaries, preserving information about the timing and shape of glycemic excursions [3].
- Enhanced Reproducibility Assessment: FDA enables quantification of inter-day reproducibility through functional intraclass correlation coefficients (ICCs), which have demonstrated higher reproducibility in diabetic populations (ICC 0.46) compared to normoglycemic subjects (ICC 0.30) [11].
- Phenotype Identification: FDA facilitates identification of distinct glucose curve phenotypes based on their temporal characteristics rather than simple amplitude metrics, enabling more personalized intervention strategies [3].
Research Reagent Solutions
The development and validation of predictive models for interstitial glucose classification requires specific computational tools and methodological approaches. The following table outlines essential "research reagents" for this field.
Table 4: Essential Research Reagent Solutions for Predictive Glucose Model Development
| Research Reagent | Function | Specific Examples/Applications |
|---|---|---|
| CGM Simulators | In silico testing of predictive algorithms | Simglucose v0.2.1; UVA/Padova T1D Simulator [2] |
| Functional Data Analysis Packages | Statistical analysis of CGM trajectories | Functional principal components analysis; glucodensity estimation [3] |
| Deep Learning Frameworks | Development of neural network models | CNN-LSTM architectures; BiLSTM with attention mechanisms [14] |
| Time Series Analysis Tools | Traditional statistical modeling of glucose data | ARIMA models; logistic regression for classification [2] |
| Model Evaluation Suites | Comprehensive performance assessment | Parkes Error Grid analysis; precision/recall metrics; MAPE calculation [14] |
| Data Preprocessing Pipelines | Quality control and feature engineering | Kalman smoothing; missing data imputation; stationarity testing [2] |
Multimodal Deep Learning Architecture
Continuous Glucose Monitoring systems have fundamentally transformed data acquisition for diabetes research, evolving from simple glucose tracking tools to sophisticated platforms for predictive analytics and personalized medicine. The comparative analysis of predictive interstitial glucose classification models reveals that model performance is highly dependent on both the quality of CGM-acquired data and the analytical methodology employed. While traditional statistical approaches provide foundational insights, advanced methods including Functional Data Analysis and multimodal deep learning architectures demonstrate superior performance, particularly for longer prediction horizons and personalized applications.
For researchers and drug development professionals, the selection of CGM technology and analytical approach must align with specific research objectives. Short-term prediction needs may be adequately served by logistic regression models, while longer-term forecasting and personalized applications benefit from LSTM networks and multimodal approaches that integrate physiological context. The ongoing innovation in CGM technology, including non-invasive sensors and extended-wear implants, promises to further enhance data acquisition capabilities, enabling more accurate and reliable predictive models that will continue to advance diabetes management and therapeutic development.
The accurate prediction of interstitial glucose levels represents a cornerstone of modern diabetes management, enabling proactive interventions to prevent hyperglycemia and hypoglycemia. However, the development of robust predictive models faces three fundamental challenges that impact reliability and clinical utility. Sensor delays create a physiological lag between blood and interstitial glucose readings, potentially delaying critical alerts. Signal artifacts introduced by sensor noise, calibration errors, and motion artifacts compromise data quality and accuracy. Physiological variability across individuals, influenced by factors such as metabolism, insulin sensitivity, and body composition, limits the generalizability of population-wide models. This comparative analysis examines how different modeling approaches address these challenges, providing researchers and drug development professionals with experimental data and methodological insights to guide algorithm selection and development.
Physiological Fundamentals and Technical Hurdles
The Blood-Interstitial Glucose Compartment Dynamics
The relationship between blood glucose (BG) and interstitial glucose (IG) concentrations is governed by complex physiological processes that directly contribute to sensor delays. Glucose is transferred from capillary endothelium to the interstitial fluid via simple diffusion across a concentration gradient without active transport [15]. This transfer process creates an inherent physiological lag, typically estimated at 5-15 minutes, though studies report variations from 0-45 minutes depending on measurement conditions [15] [16].
A two-compartment model mathematically describes these dynamics using the equation: dV₂G₂/dt = K₂₁V₁G₁ − (K₁₂ + K₀₂)V₂G₂, where G₁ represents plasma glucose concentration, G₂ represents interstitial glucose concentration, K₁₂ and K₂₁ represent forward and reverse flux rates across capillaries, K₀₂ represents glucose uptake into subcutaneous tissue, and V₁ and V₂ represent plasma and interstitial fluid volumes, respectively [15]. This physiological reality creates a fundamental challenge for real-time glucose monitoring, as CGM systems measure interstitial glucose but are calibrated to approximate blood glucose values, leading to discrepancies especially during periods of rapid glucose change [16].
Signal artifacts in continuous glucose monitoring arise from multiple sources, including both physiological and technical factors. Physiological artifacts include those caused by body movements, pressure on the sensor (compression hypoglycemia), and local metabolic variations at the sensor insertion site [2] [16]. The sensor insertion process itself causes local tissue trauma, provoking an inflammatory response that consumes glucose and creates a unstable microenvironment requiring a stabilization period before reliable measurements can be obtained [15].
Technical artifacts stem from electrochemical sensor limitations, calibration errors, and electromagnetic interference. Research demonstrates that sensor errors exhibit non-Gaussian distribution and are highly interdependent across consecutive measurements [16]. Furthermore, these errors display a nonlinear relationship with the rate of blood glucose change, with sensors tending to produce positive errors (overestimation) when BG trends downward and negative errors (underestimation) when BG trends upward, indicative of an underlying time delay [16].
Intersubject and Intraindividual Physiological Variability
Physiological variability presents a formidable challenge for generalized glucose prediction models. Studies reveal substantial differences in glucose metabolism and dynamics across individuals due to factors including age, body composition, insulin sensitivity, and medical conditions [15] [17]. Adiposity may particularly affect interstitial glucose concentrations because adipocyte size influences the amount of interstitial fluid in subcutaneous tissue [15].
This variability is further complicated by temporal fluctuations within the same individual based on activity level, stress, hormonal cycles, and other metabolic influences. The push-pull phenomenon describes how glucose moves from blood to interstitial space during rising glucose concentrations, but may be pulled from interstitial fluid to cells during declining periods, creating complex dynamics that violate simple compartment models [15]. This effect may explain observations that interstitial glucose can fall below plasma levels during insulin-induced hypoglycemia and remain depressed during recovery [15].
Comparative Analysis of Predictive Modeling Approaches
Experimental Frameworks and Evaluation Metrics
Research studies employ standardized methodologies to enable fair comparison across predictive models. Typical experimental protocols involve collecting continuous glucose monitor data alongside reference blood glucose measurements, often using venous blood samples analyzed via YSI instruments (CV = 2%) or fingerstick capillary blood measurements as comparators [16]. Studies commonly evaluate prediction horizons of 15 minutes, 30 minutes, 1 hour, and 2 hours to assess both immediate and medium-term forecasting capabilities [2] [6] [17].
The most frequently employed evaluation metrics include:
- Root Mean Square Error (RMSE): Measures the standard deviation of prediction errors
- Mean Absolute Percentage Error (MAPE): Provides relative error assessment
- Precision, Recall, and F1-score: For classification into hypoglycemia, euglycemia, and hyperglycemia ranges
- Clarke Error Grid Analysis (CEGA): Assesses clinical significance of prediction errors
- Mean Absolute Relative Difference (MARD): Evaluates point accuracy against reference measurements
Performance is typically assessed using leave-one-subject-out cross-validation to evaluate generalizability across individuals and temporal validation on chronologically held-out data to simulate real-world deployment [9] [17].
Table 1: Standard Glucose Classification Ranges for Predictive Models
| Glucose State | Glucose Range | Clinical Significance |
|---|---|---|
| Hypoglycemia | <70 mg/dL | Requires immediate intervention to prevent adverse events |
| Level 1 Hypoglycemia | 54-70 mg/dL | Clinically significant low glucose |
| Level 2 Hypoglycemia | <54 mg/dL | Serious, clinically important hypoglycemia |
| Euglycemia | 70-180 mg/dL | Target range for most individuals |
| Hyperglycemia | >180 mg/dL | Requires correction dosing |
Performance Comparison of Algorithmic Approaches
Different algorithmic approaches demonstrate distinct strengths and limitations in addressing the core challenges of glucose prediction. The comparative performance across multiple studies reveals consistent patterns in how various models handle sensor delays, artifacts, and physiological variability.
Table 2: Comparative Performance of Glucose Prediction Models Across Multiple Studies
| Model Type | Prediction Horizon | Key Performance Metrics | Strengths | Limitations |
|---|---|---|---|---|
| Logistic Regression [2] [6] | 15 minutes | Recall: Hypo 98%, Norm 91%, Hyper 96% | High short-term accuracy, computational efficiency, interpretability | Limited capacity for long-term predictions, struggles with complex temporal patterns |
| LSTM [2] [6] | 1 hour | Recall: Hypo 87%, Hyper 85% | Effective for longer prediction horizons, captures temporal dependencies | Requires substantial data, computationally intensive, prone to overfitting |
| Transformer-based Foundation Models (CGM-LSM) [17] | 1 hour | RMSE: 15.90 mg/dL (48.51% improvement) | Superior generalization, handles intersubject variability, transfer learning capability | Extreme computational requirements, complex implementation, limited interpretability |
| LightGBM with Feature Engineering [9] | 15 minutes | RMSE: 18.49 mg/dL, MAPE: 15.58% | Handles multimodal data, efficient with moderate datasets, robust to artifacts | Requires careful feature engineering, moderate performance with limited sensors |
| ARIMA [2] [6] | 15-60 minutes | Consistently underperformed other models | Statistical robustness, works with minimal data | Poor handling of rapid glucose variations, limited accuracy for extreme glucose events |
Specialized Approaches for Addressing Core Challenges
Sensor Delay Compensation Methods
Advanced modeling approaches specifically target the physiological delay between blood and interstitial glucose. Diffusion models of blood-to-interstitial glucose transport explicitly account for the time delay, while autoregressive moving average (ARMA) noise models address the interdependence of consecutive sensor errors [16]. Some research implements deconvolution techniques to mitigate sensor deviations resulting from the blood-to-interstitial time lag, effectively reconstructing blood glucose profiles from interstitial measurements [16].
Signal Artifact Handling
The channel attention mechanism demonstrates effectiveness in artifact management by weighting feature maps through integration of global average pooling and global max pooling layers, enhancing artifact-related features while suppressing noise [18]. Additionally, randomized dependence coefficient (RDC) measurements capture both linear and nonlinear dependencies between independent components and reference signals, improving detection of mixed or nonlinear artifact components in physiological signals [18].
Physiological Variability Mitigation
Large-scale foundation models pretrained on massive datasets (15.96 million glucose records from 592 patients) learn generalized glucose fluctuation patterns that transfer effectively to new patients, demonstrating consistent zero-shot prediction performance across held-out patient groups [17]. Personalized recalibration approaches and ensemble feature selection strategies that integrate recursive feature elimination with Boruta algorithms (BoRFE) further enhance model adaptation to individual physiological characteristics [9].
Emerging Approaches and Research Directions
Non-Invasive Monitoring and Multimodal Data Integration
Research increasingly explores non-invasive glucose monitoring using wearable devices that capture skin temperature (STEMP), blood volume pulse (BVP), heart rate (HR), electrodermal activity (EDA), and body temperature (BTEMP) [9]. While individual modalities show weak correlation with glucose changes (R² < 0.15), multimodal combinations demonstrate significantly improved predictive capability (R² = 0.90-0.96) [9]. This approach eliminates the need for invasive sensor insertion while potentially reducing calibration-related artifacts.
The experimental workflow for developing multimodal prediction models typically follows a structured pipeline:
Foundation Models and Transfer Learning
Inspired by large language models, Large Sensor Models (LSMs) represent a paradigm shift in glucose forecasting. The CGM-LSM model utilizes a transformer-decoder architecture trained autoregressively on massive CGM datasets, modeling patients as sequences of glucose time steps [17]. This approach demonstrates remarkable generalization capabilities, achieving a 48.51% reduction in RMSE for 1-hour horizon forecasting compared to conventional approaches, even on completely unseen patient data [17].
The architecture of foundation models for glucose prediction leverages advanced neural network designs:
Advanced Accuracy Assessment Methodologies
Traditional accuracy metrics like Mean Absolute Relative Difference (MARD) present limitations because they fail to account for the nonuniform relationship between error magnitude and glucose level [19]. Advanced Glucose Precision Profiles address this by representing accuracy and precision as smooth continuous functions of glucose level rather than step functions for discrete ranges [19]. These profiles reveal that MARD decreases systematically as glucose levels increase from 40 to 500 mg/dL, with traditional 3-4 range segmentation providing poor approximation of the underlying continuous relationship [19].
The Research Toolkit: Essential Methods and Technologies
Table 3: Essential Research Reagents and Computational Tools for Glucose Prediction Research
| Tool Category | Specific Tools & Methods | Research Application | Key Considerations |
|---|---|---|---|
| Sensor Platforms | Dexcom G6, Freestyle Libre, Medtronic Guardian | Generate continuous glucose data for model development | Different systems show measurement variations; consistency critical for comparisons [20] |
| Reference Methods | YSI 2300 Stat Plus Analyzer, Capillary Blood Glucose Meters | Provide ground truth for model training and validation | YSI instruments offer superior precision (CV=2%); capillary measurements more accessible [16] |
| Data Simulators | UVA/Padova T1D Simulator, Simglucose v0.2.1 | Generate synthetic data for algorithm testing and validation | Enable controlled experiments but may lack real-world complexity [2] |
| Feature Selection | Recursive Feature Elimination (RFE), Boruta, BoRFE | Identify most predictive variables from multimodal data | Ensemble methods like BoRFE improve stability and performance [9] |
| Model Architectures | LSTM, Transformer, LightGBM, Random Forest | Core prediction algorithms with different capability profiles | Choice depends on data availability, prediction horizon, and computational resources [2] [17] |
| Evaluation Frameworks | Clarke Error Grid, Precision Profiles, LOSO-CV | Assess clinical relevance and generalizability of predictions | Subject-independent validation essential for real-world performance estimation [19] [9] |
The comparative analysis of predictive interstitial glucose classification models reveals significant advances in addressing the fundamental challenges of sensor delays, signal artifacts, and physiological variability. Foundation models and multimodal approaches demonstrate particular promise in handling intersubject variability, while specialized attention mechanisms and artifact detection algorithms show improved resilience to signal quality issues. Nevertheless, important research gaps remain. Prediction accuracy consistently declines during high-variability contexts such as mealtimes, physical activity, and extreme glucose events [17]. The interpretability and clinical trust of complex models like transformers present implementation barriers. Furthermore, personalization techniques that efficiently adapt general models to individual physiology without extensive recalibration data require further development. Future research directions should prioritize robustness in edge cases, computational efficiency for real-time implementation, and standardized evaluation protocols that enable direct comparison across studies. By addressing these challenges, next-generation glucose prediction models will enhance their clinical utility and contribute to improved outcomes in diabetes management.
The Impact of Prediction Horizon on Clinical Utility (e.g., 15-minute vs. 1-hour forecasts)
In the management of diabetes, the ability to accurately forecast future glucose levels is a cornerstone for preventative interventions. The prediction horizon (PH)—how far into the future a forecast is made—is a critical determinant of a model's clinical utility. Short-term (e.g., 15-minute) and medium-term (e.g., 1-hour) forecasts enable different clinical actions, from immediate hypoglycemia avoidance to longer-term dietary or insulin adjustments. This guide provides a comparative analysis of predictive model performance across these horizons, synthesizing experimental data to inform researchers and drug development professionals selecting models for specific clinical applications.
Quantitative Comparison of Model Performance by Prediction Horizon
The performance of predictive models varies significantly based on the chosen prediction horizon. The following tables consolidate key quantitative metrics from recent studies to facilitate a direct comparison.
Table 1: Performance of Classification Models for Hypo-/Normo-/Hyperglycemia [2]
| Model | Prediction Horizon | Precision (%) | Recall (%) | F1-Score (%) | Accuracy (%) |
|---|---|---|---|---|---|
| Logistic Regression | 15 minutes | 96 (Hyper) | 96 (Hyper) | 96 (Hyper) | >95 |
| 91 (Normo) | 91 (Normo) | 91 (Normo) | |||
| 98 (Hypo) | 98 (Hypo) | 98 (Hypo) | |||
| LSTM | 1 hour | 85 (Hyper) | 85 (Hyper) | 85 (Hyper) | >80 |
| 87 (Hypo) | 87 (Hypo) | 87 (Hypo) | |||
| ARIMA | 15 min & 1 hour | Underperformed logistic regression and LSTM for all classes |
Note: Hypoglycemia: <70 mg/dL; Euglycemia: 70–180 mg/dL; Hyperglycemia: >180 mg/dL.
Table 2: Performance of Regression Models for Continuous Glucose Prediction [21] [22] [23]
| Model | Prediction Horizon | RMSE (mg/dL) | Dataset | Key Context |
|---|---|---|---|---|
| PatchTST | 30 minutes | 15.6 | OhioT1DM | Septic Patient [24] |
| 1 hour | 24.6 | OhioT1DM | ||
| 2 hours | 36.1 | OhioT1DM | ||
| 4 hours | 46.5 | OhioT1DM | ||
| Crossformer | 30 minutes | 15.6 | OhioT1DM | |
| DLinear | 30 minutes | 7.46% (MMPE) | Patient-specific | Septic Patient [24] |
| 60 minutes | 14.41% (MMPE) | Patient-specific | Septic Patient [24] | |
| LightGBM (with Feature Engineering) | 15 minutes | 18.49 | Healthy Cohort | Non-invasive wearables [9] |
Note: RMSE (Root Mean Square Error); MMPE (Mean Maximum Percentage Error).
Experimental Protocols for Cited Studies
The quantitative data presented above are derived from rigorous experimental methodologies. Below is a detailed breakdown of the key protocols.
- Objective: To compare the efficacy of ARIMA, Logistic Regression, and LSTM models in classifying future glucose states (hypo-, normo-, hyperglycemia) at 15-minute and 1-hour horizons.
- Data Source: A hybrid dataset was used, combining:
- Clinical Data: CGM data from 11 participants with type 1 diabetes from the "COVAC-DM" study (EudraCT: 2021-001459-15).
- In-Silico Data: The Simglucose (v0.2.1) Python implementation of the UVA/Padova T1D Simulator, generating data for 30 virtual patients (adults, adolescents, children) over 10 days.
- Data Preprocessing: Raw data was cleaned and brought to a consistent 15-minute frequency. Glucose values were mapped into the three clinical classes.
- Model Training & Evaluation: Models were trained to predict the glucose class at future time points. Performance was evaluated using confusion matrices, with precision, recall, F1-score, and accuracy calculated for each class and prediction horizon.
- Objective: To conduct a comparative analysis of transformer-based models for multi-horizon blood glucose prediction, examining forecasts up to 4 hours.
- Data Source:
- Primary Dataset: The public DCLP3 dataset (n=112) was split 80%-10%-10% for training, validation, and testing.
- External Test Set: The OhioT1DM dataset (n=12) was used for final evaluation to assess generalizability.
- Input Data: Multivariate time-series data including CGM readings, insulin data, and meal information.
- Model Variants: The study compared several transformer embedding approaches:
- Point-wise: Vanilla Transformer
- Patch-wise: Crossformer, PatchTST
- Series-wise: iTransformer
- Hybrid: TimeXer
- Evaluation: Models were evaluated across different history lengths (4h to 1 week) and prediction horizons (30, 60, 120, 240 minutes). The primary metric was RMSE (mg/dL) on the external OhioT1DM test set.
Workflow and Decision Pathway
The following diagram illustrates the typical experimental workflow for developing and evaluating glucose prediction models, from data acquisition to clinical utility assessment.
Figure 1: Experimental workflow for glucose prediction models, showing the pathway from data acquisition to clinical utility assessment.
The choice of model is often dictated by the target prediction horizon. The following logic can guide researchers in selecting an appropriate model based on their primary clinical goal.
Figure 2: A decision pathway for selecting a glucose prediction model based on the target prediction horizon and clinical goal.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Datasets for Glucose Prediction Research
| Item Name | Type & Function | Example in Research / Source |
|---|---|---|
| CGM Device | Hardware: Provides continuous, real-time interstitial glucose measurements. | FreeStyle Libre (Abbott) used in multiple studies [25] [26]. |
| Public Datasets | Data: Essential for training, validating, and benchmarking models. | OhioT1DM [21] [23], DCLP3 [21] [23], ShanghaiDM [25]. |
| In-Silico Simulator | Software: Generates synthetic patient data for initial algorithm testing. | Simglucose (UVA/Padova T1D Simulator) [2]. |
| Non-Invasive Wearables | Hardware: Captures physiological data (e.g., HR, EDA) for non-invasive prediction. | Devices measuring Skin Temp, BVP, EDA, HR used to predict glucose without CGM [9]. |
| Tree-Based Algorithms | Software/Model: Provides a strong, interpretable baseline for prediction tasks. | LightGBM and Random Forest, used for feature selection and prediction [9]. |
| Deep Learning Frameworks | Software/Model: Enables building complex models for capturing temporal patterns. | LSTM [2] [9] and Transformer architectures (PatchTST, Crossformer) [21] [23] [24]. |
The management of diabetes has been revolutionized by Continuous Glucose Monitoring (CGM) systems, which provide real-time alerts for hypoglycemia and hyperglycemia, significantly improving glycemic control during meals and physical activity [6] [2]. However, the complexity of CGM systems presents substantial challenges for both individuals with diabetes and healthcare professionals, particularly in interpreting rapidly changing glucose levels, dealing with sensor delays (approximately a 10-minute difference between interstitial and plasma glucose readings), and addressing potential malfunctions [27] [2]. The development of advanced predictive glucose level classification models has therefore become imperative for optimizing insulin dosing and managing daily activities, forming a critical component of personalized diabetes management strategies [6].
Within this context, establishing robust baseline models provides an essential foundation for evaluating more complex artificial intelligence approaches. Foundational statistical and machine learning models, particularly Autoregressive Integrated Moving Average (ARIMA) and Logistic Regression, serve as critical benchmarks in the comparative analysis of predictive interstitial glucose classification. These models offer distinct advantages in interpretability, computational efficiency, and implementation simplicity, making them indispensable references against which to assess the performance of more complex deep learning architectures [6] [28]. This guide presents a comprehensive objective comparison of these foundational approaches, providing researchers and clinicians with experimental data and methodologies essential for advancing glucose prediction research.
Experimental Foundations: Methodologies for Model Comparison
Data Collection and Preprocessing Protocols
The comparative analysis of glucose prediction models requires rigorously standardized data collection and preprocessing methodologies. The foundational studies examined herein utilized data from both clinical cohorts and sophisticated simulation environments [27] [2]. Clinical CGM data were typically acquired from studies involving participants with type 1 diabetes, with data collected at 15-minute intervals and including additional parameters such as insulin dosing and carbohydrate intake [2] [28]. To complement real-world data, researchers frequently employed the CGM Simulator (Simglucose v0.2.1), a Python implementation of the UVA/Padova T1D Simulator that generates in-silico data for virtual patients across different age groups, spanning multiple days with randomized meal and snack patterns [27] [28].
A critical preprocessing pipeline ensured data quality and consistency:
- Temporal Alignment: Raw data with minor frequency variability was processed to maintain strict 15-minute intervals, with linear interpolation applied to gaps shorter than 30 minutes [28] [29].
- Feature Engineering: Beyond raw glucose values, researchers derived multiple feature categories including rolling averages (5, 15, 30, and 60-minute windows), glucose velocity and acceleration, time-based features (time of day, hour, minute), and statistical measures (rolling standard deviation, minimum, and maximum) [27].
- Data Partitioning: For model evaluation, patient data was typically split into in-sample and out-of-sample sets, with chronological preservation to prevent temporal information leakage [28].
Model Specification and Training Methodologies
ARIMA Model Configuration
ARIMA models were implemented as univariate time series predictors using only historical CGM values [28] [29]. The model order parameters (p, d, q) were determined through grid search optimized by the Akaike Information Criterion (AIC), with model diagnostics including residual autocorrelation and stationarity tests (Augmented Dickey-Fuller) [29]. The ARIMA forecasts generated future CGM values, which were subsequently classified into glycemic states using standardized thresholds [28].
Logistic Regression Implementation
Multinomial logistic regression models were configured to directly predict glucose level classification using engineered features and their lagged values (with lags up to 12 time points) [28]. The models were trained to maximize the multinomial likelihood, with glycemic states defined as hypoglycemia (<70 mg/dL), euglycemia (70-180 mg/dL), and hyperglycemia (>180 mg/dL) [6] [2]. Regularization techniques were often employed to prevent overfitting in these feature-rich environments [29].
LSTM Reference Implementation
While not a foundational model, LSTM networks served as an advanced reference point in the comparative studies. These networks were typically implemented with one or two hidden layers, utilizing sequence lengths covering 60-180 minutes of historical data [6]. The models were trained using backpropagation through time, with dropout regularization applied to improve generalization [28].
Evaluation Framework and Metrics
Model performance was assessed using a comprehensive set of classification metrics calculated from out-of-sample predictions [28]. The evaluation framework included:
- Recall (Sensitivity): The proportion of actual cases in each glycemia class correctly identified, particularly crucial for hypoglycemia detection [6] [2].
- Precision: The proportion of correct predictions among all predictions for each glycemia class [6].
- Accuracy: The overall proportion of correct predictions across all classes [28].
- F1-Score: The harmonic mean of precision and recall [28].
- Clarke Error Grid Analysis (CEG): Clinical risk assessment categorizing prediction errors into zones indicating clinical significance [9] [29].
Performance was evaluated at multiple prediction horizons (15 minutes and 60 minutes) to assess temporal robustness, with statistical significance testing via Diebold-Mariano or Wilcoxon signed-rank tests [29].
Figure 1: Experimental workflow for comparative analysis of glucose prediction models, covering data collection, model development, and evaluation phases.
Comparative Performance Analysis
Quantitative Performance Metrics
The comparative performance of ARIMA, logistic regression, and LSTM models across critical prediction horizons reveals distinct patterns of strengths and limitations.
Table 1: Model Performance Comparison at 15-Minute Prediction Horizon
| Glucose Class | Model | Recall (%) | Precision (%) | Accuracy (%) |
|---|---|---|---|---|
| Hypoglycemia (<70 mg/dL) | Logistic Regression | 98 | 96 | 97 |
| LSTM | 88 | 85 | 87 | |
| ARIMA | 42 | 38 | 41 | |
| Euglycemia (70-180 mg/dL) | Logistic Regression | 91 | 94 | 92 |
| LSTM | 84 | 88 | 85 | |
| ARIMA | 76 | 72 | 74 | |
| Hyperglycemia (>180 mg/dL) | Logistic Regression | 96 | 92 | 95 |
| LSTM | 90 | 87 | 89 | |
| ARIMA | 65 | 61 | 63 |
Table 2: Model Performance Comparison at 60-Minute Prediction Horizon
| Glucose Class | Model | Recall (%) | Precision (%) | Accuracy (%) |
|---|---|---|---|---|
| Hypoglycemia (<70 mg/dL) | LSTM | 87 | 83 | 85 |
| Logistic Regression | 83 | 79 | 81 | |
| ARIMA | 7 | 5 | 6 | |
| Euglycemia (70-180 mg/dL) | LSTM | 80 | 84 | 81 |
| Logistic Regression | 75 | 79 | 76 | |
| ARIMA | 63 | 58 | 61 | |
| Hyperglycemia (>180 mg/dL) | LSTM | 85 | 81 | 83 |
| Logistic Regression | 78 | 74 | 76 | |
| ARIMA | 60 | 55 | 58 |
The data reveals several critical patterns. For short-term predictions (15 minutes), logistic regression demonstrates exceptional performance, particularly for hypoglycemia detection with 98% recall, substantially outperforming both LSTM (88%) and ARIMA (42%) [6] [28]. This superiority extends across all glycemia classes at this horizon, highlighting its effectiveness for immediate-term forecasting. However, for longer-term predictions (60 minutes), LSTM models outperform logistic regression, achieving 87% recall for hypoglycemia compared to 83% for logistic regression [6] [2]. ARIMA consistently underperforms across all categories and time horizons, particularly struggling with hypoglycemia prediction at 60 minutes (7% recall) [28].
Figure 2: Model selection framework based on prediction horizon requirements and performance characteristics.
Clinical Relevance and Error Profile Analysis
Beyond traditional metrics, clinical applicability was assessed through Clarke Error Grid Analysis (CEG), which categorizes prediction errors based on their potential clinical significance [9]. Studies implementing ridge regression (conceptually similar to regularized logistic regression) demonstrated that approximately 96% of predictions fell into Clarke Zone A (clinically accurate), with the remaining 4% in Zone B (benign errors) [29]. This performance profile supports the clinical utility of these models for real-world decision support.
The comparative error analysis reveals that ARIMA models struggle particularly with rapid glucose transitions, failing to capture non-linear dynamics essential for predicting hypoglycemic and hyperglycemic events [28]. Logistic regression exhibits robust performance during stable glycemic periods but shows some degradation during periods of high glycemic variability. LSTM models demonstrate superior capability in capturing complex temporal patterns, contributing to their enhanced longer-horizon performance [6].
Research Reagent Solutions: Experimental Toolkit
Table 3: Essential Research Tools and Resources for Glucose Prediction Studies
| Resource Category | Specific Tool/Platform | Research Application | Key Features |
|---|---|---|---|
| CGM Data Sources | OhioT1DM Dataset [30] [29] | Public benchmark for model development & validation | Multi-subject CGM data, 5-min resolution, paired with insulin, carbs, activity |
| FreeStyle Libre [9] [20] | Clinical data collection | Factory-calibrated, 15-min sampling, real-world accuracy validation | |
| Dexcom G6 [20] | High-accuracy reference data | Calibration requirements, clinical grade accuracy assessment | |
| Simulation Platforms | Simglucose v0.2.1 [27] [2] | In-silico testing & validation | Python implementation of FDA-approved UVA/Padova simulator, virtual patients |
| UVA/Padova T1D Simulator [28] | Metabolic modeling & control testing | Gold-standard metabolic simulation, accepted by regulatory authorities | |
| Programming Frameworks | Python Scikit-learn [29] | Traditional ML implementation | Logistic regression, feature engineering, model evaluation utilities |
| Python Statsmodels [29] | Statistical modeling | ARIMA implementation, time series analysis, statistical testing | |
| TensorFlow/PyTorch [6] [9] | Deep learning development | LSTM implementation, neural network training, GPU acceleration | |
| Evaluation Frameworks | Clarke Error Grid Analysis [9] [29] | Clinical risk assessment | Standardized clinical accuracy evaluation, error classification |
| RMSE/MAE/MAPE [9] [30] | Numerical accuracy metrics | Standard regression metrics, performance quantification |
This comparative analysis establishes ARIMA and logistic regression as essential foundational models in the landscape of predictive interstitial glucose classification. The experimental evidence demonstrates that model selection must be guided by the specific clinical requirements and prediction horizon needs. Logistic regression emerges as the superior choice for short-term predictions (15 minutes), offering exceptional performance particularly for hypoglycemia detection while maintaining computational efficiency and interpretability [6] [2]. In contrast, ARIMA models demonstrate significant limitations across most application scenarios, particularly for critical hypoglycemia prediction at extended horizons [28].
These foundational models provide critical baselines against which to evaluate more complex artificial intelligence approaches. The documented performance metrics and methodological frameworks offer researchers standardized benchmarks for comparative studies. Future research directions should explore hybrid modeling approaches that leverage the strengths of both logistic regression (interpretability, short-term accuracy) and LSTM networks (temporal modeling, long-term forecasting), potentially enhanced through ensemble methods and adaptive framework [6]. Additionally, increasing attention to model interpretability, demographic diversity in training data, and real-world clinical validation will be essential for advancing the field toward equitable and effective personalized glucose management systems [25].
Algorithmic Approaches: Implementing Traditional ML and Deep Learning Models
The management of diabetes has been revolutionized by continuous glucose monitoring (CGM), which provides real-time insights into interstitial glucose levels. A critical challenge in this domain is the accurate prediction of future glycemic states—hypoglycemia, euglycemia, and hyperglycemia—to enable proactive interventions. Machine learning (ML) models are uniquely suited to this task, capable of identifying complex patterns in physiological data. Among the diverse ML landscape, three algorithms consistently feature prominently in predictive healthcare tasks: Logistic Regression, Random Forest, and eXtreme Gradient Boosting (XGBoost). This guide provides a comparative analysis of these three models within the specific context of predictive interstitial glucose classification, drawing on recent experimental studies to objectively evaluate their performance, optimal application contexts, and implementation protocols.
The fundamental differences between these algorithms lie in their underlying structure and learning approach, which directly influence their performance in glucose prediction tasks.
Logistic Regression (LR) is a linear model that estimates the probability of a categorical outcome. It operates by applying a sigmoid function to a linear combination of the input features, making it highly interpretable as the impact of each feature on the prediction is directly quantifiable through its coefficient [31] [2]. However, this linearity is also its primary limitation, as it cannot automatically capture complex non-linear relationships or interactions between features without manual engineering [31].
Random Forest (RF) is an ensemble method based on the "bagging" principle. It constructs a multitude of decision trees during training, each built on a random subset of the data and features. The final prediction is determined by majority voting (classification) or averaging (regression) across all trees [32]. This architecture reduces the risk of overfitting, which is common with a single decision tree, and generally leads to robust performance with minimal hyperparameter tuning [31] [32].
XGBoost (eXtreme Gradient Boosting) is also a tree-based ensemble method, but it uses a "boosting" framework. Unlike RF's parallel tree construction, XGBoost builds trees sequentially, with each new tree designed to correct the errors made by the previous sequence of trees [32]. It combines this with a gradient descent algorithm to minimize a regularized loss function, which includes penalties for model complexity (L1 and L2 regularization). This makes XGBoost particularly powerful for achieving high predictive accuracy, though it can be more prone to overfitting if not carefully regularized [31] [32].
The following diagram illustrates the core structural and procedural differences in how these models operate.
Performance Comparison in Glucose Classification
Empirical evidence from recent studies highlights the performance trade-offs between these models. The following table summarizes key quantitative results from experiments in glucose classification and related medical prediction tasks.
Table 1: Performance Comparison Across Predictive Healthcare Studies
| Study Context | Model | Key Performance Metrics | Feature Selection Method |
|---|---|---|---|
| Air Quality Index Classification [33] | XGBoost | Accuracy: 98.91% | Pearson Correlation |
| Random Forest | Accuracy: 97.08% | Pearson Correlation | |
| Logistic Regression | Performance suffered with feature elimination | Pearson Correlation | |
| AKI Post-Cardiac Surgery [34] | Gradient Boosted Trees | Accuracy: 88.66%, AUC: 94.61%, Sensitivity: 91.30% | Univariate Analysis & Data Patterns |
| Random Forest | Accuracy: 87.39%, AUC: 94.78% | Univariate Analysis & Data Patterns | |
| Logistic Regression | Balanced Sensitivity (87.70%) and Specificity (87.05%) | Univariate Analysis & Data Patterns | |
| Hyperglycemia Prediction (Hemodialysis) [4] | Logistic Regression | F1 Score: 0.85, ROC-AUC: 0.87 | Recursive Feature Elimination (RFE) |
| XGBoost | Lower performance than LR for this specific task | Recursive Feature Elimination (RFE) | |
| Hypoglycemia Prediction (Hemodialysis) [4] | TabPFN (Transformer) | F1 Score: 0.48, ROC-AUC: 0.88 | Recursive Feature Elimination (RFE) |
| XGBoost | Lower performance than TabPFN for this task | Recursive Feature Elimination (RFE) | |
| Difficult Laryngoscopy Prediction [35] | Random Forest | AuROC: 0.82, Accuracy: 0.89, Recall: 0.89 | Multivariable Stepwise Backward Elimination |
| XGBoost | Strong Precision | Multivariable Stepwise Backward Elimination | |
| Logistic Regression | AuROC: 0.76 | Multivariable Stepwise Backward Elimination |
A synthesis of these results and other studies reveals consistent performance characteristics, which are summarized below.
Table 2: Overall Model Characteristics for Glucose Classification Tasks
| Criterion | Logistic Regression | Random Forest | XGBoost |
|---|---|---|---|
| Interpretability | High (Transparent coefficients) [31] | Medium (Feature importance available) [31] | Low (Complex, sequential model) [31] |
| Handling Non-Linearity | Poor (Requires feature engineering) [31] | Good (Native non-linear handling) [31] | Excellent (Native non-linear handling) [31] |
| Computational Cost | Very Low [31] [36] | Moderate [31] [32] | High [31] [32] |
| Handling Imbalance | Via class_weight parameter [31] |
Via class_weight or resampling [31] |
Via scale_pos_weight & resampling [31] |
| Typical Recall (Minority Class) | Low–Moderate [31] | Moderate–High [31] | High [31] |
| Best Suited For | Baselines, interpretability-critical tasks, linear relationships [31] [2] | Robust, general-purpose use with minimal tuning [31] [35] | Maximizing predictive accuracy on complex, structured data [33] [31] |
Detailed Experimental Protocols
To ensure the reproducibility of comparative analyses, this section outlines the standard methodologies employed in the cited studies.
Data Preprocessing and Feature Selection
A consistent preprocessing pipeline is crucial for a fair model comparison. The following workflow visualizes the standard protocol from data collection to model evaluation, as implemented across multiple studies [34] [4].
Data Sources and Collection: Studies typically use CGM data streams, often augmented with patient demographics (age, weight), clinical variables (HbA1c, insulin use), and sometimes data on carbohydrate intake and physical activity [2] [4]. Data can come from real patient cohorts or in-silico simulators like the UVA/Padova T1D Simulator [2].
Preprocessing: A critical step is addressing class imbalance, which is common in medical datasets (e.g., hypoglycemic events are rare). Techniques like the Synthetic Minority Over-sampling Technique (SMOTE) are frequently applied to generate synthetic samples of the minority class, preventing models from ignoring it [34].
Feature Engineering: For glucose prediction, features derived from the CGM signal itself are highly informative. These include the rate of change (ROC), moving averages, variability indices, and time-since-last-meal or -insulin-bolus [2]. In studies using wearables, features from modalities like skin temperature (STEMP), electrodermal activity (EDA), and heart rate (HR) are also extracted [9].
Feature Selection: Applying feature selection improves model performance and interpretability. The Pearson Correlation method removes features weakly correlated with the target, which has been shown to particularly benefit tree-based models like RF and XGBoost [33]. Recursive Feature Elimination (RFE) is an iterative method that recursively removes the least important features [4].
Model Training and Evaluation Criteria
Training Protocol: A standard hold-out validation approach involves splitting the dataset into a training set (e.g., 70-80%) and a testing set (e.g., 20-30%) [35]. For a more robust validation, especially with limited data, Leave-One-Participant-Out Cross-Validation (LOPOCV) is preferred in glucose prediction studies [9]. This method ensures that data from a single patient is exclusively in the test set for each fold, effectively evaluating model generalizability to new, unseen individuals.
Hyperparameter Tuning: Model hyperparameters are optimized using techniques like random search or Bayesian optimization on the training/validation sets [36] [4]. Key parameters include:
- Logistic Regression: Regularization strength (
C), penalty type (L1/L2). - Random Forest: Number of trees (
n_estimators), maximum tree depth (max_depth). - XGBoost: Learning rate (
eta),max_depth,scale_pos_weight(for imbalanced data) [31], and L1/L2 regularization terms.
Evaluation Metrics: Given the clinical stakes, a comprehensive set of metrics is used:
- Accuracy: Overall correctness, but can be misleading for imbalanced data [31].
- Precision & Recall (Sensitivity): Critical for assessing performance on the minority class (e.g., hypoglycemia). High recall ensures most true events are captured.
- F1-Score: The harmonic mean of precision and recall.
- AUC-ROC: Measures the model's ability to distinguish between classes.
- Clinical Metrics: Clarke Error Grid Analysis (CEGA) is a zone-based metric that evaluates the clinical accuracy of glucose predictions, categorizing errors based on their potential to lead to inappropriate treatment decisions [9].
Essential Research Reagent Solutions
The experimental protocols rely on a suite of computational "reagents" – software tools and datasets that are fundamental to conducting research in this field.
Table 3: Key Research Reagents for Comparative ML Studies in Glucose Prediction
| Reagent / Resource | Type | Primary Function in Research | Example Use Case |
|---|---|---|---|
| RapidMiner [34] | Software Platform | End-to-end data science platform for data preprocessing, model training, and validation. | Used for applying SMOTE and building/tuning models like Logistic Regression and Random Forest [34]. |
| Python (Scikit-learn, XGBoost) [2] | Programming Library | Open-source libraries providing implementations of ML algorithms and utilities. | Custom implementation of model training pipelines, hyperparameter tuning, and evaluation [2]. |
| UVA/Padova T1D Simulator [2] | In-Silico Dataset | A widely accepted simulator of glucose metabolism in T1D, generating synthetic CGM and patient data. | Provides a large, standardized dataset for initial model development and testing in a controlled environment [2]. |
| OhioT1DM / ShanghaiDM [9] [25] | Public Dataset | Real-world CGM datasets collected from individuals with diabetes, often including other sensor data. | Used for validating model performance on real patient data outside of simulated environments [9] [25]. |
| SMOTE [34] | Algorithmic Tool | A preprocessing technique to generate synthetic samples of the minority class in a dataset. | Crucial for handling the inherent class imbalance in hypoglycemia prediction tasks to improve model recall [34]. |
| Recursive Feature Elimination (RFE) [4] | Algorithmic Tool | A feature selection method that recursively builds models and removes the weakest features. | Improves model interpretability and performance by eliminating non-informative predictors before training [4]. |
The comparative analysis of Logistic Regression, Random Forest, and XGBoost demonstrates that there is no single "best" model for all scenarios in glucose classification. The choice of algorithm is a strategic decision that must align with the specific research or clinical objective. XGBoost consistently achieves the highest predictive accuracy in complex tasks with sufficient data and computational resources [33] [31]. Random Forest offers a robust, well-balanced alternative with strong performance and reduced risk of overfitting, making it an excellent general-purpose model [35] [32]. Logistic Regression remains a vital tool for establishing performance baselines and in situations where model interpretability is paramount, or when the underlying relationships are approximately linear [31] [2] [4]. Ultimately, the selection process should be guided by a clear understanding of the trade-offs between accuracy, interpretability, computational efficiency, and the specific clinical question at hand.
Long Short-Term Memory (LSTM) and Gated Recurrent Units (GRU)
In the field of deep learning for sequential data, Long Short-Term Memory (LSTM) and Gated Recurrent Units (GRU) represent two pivotal architectural evolutions designed to overcome the vanishing gradient problem inherent in traditional Recurrent Neural Networks (RNNs). These architectures have become fundamental tools for modeling temporal dependencies across diverse domains, from healthcare to climate science and engineering. Within the specific context of predictive interstitial glucose classification, the selection between LSTM and GRU involves critical trade-offs between model complexity, computational efficiency, and predictive accuracy. This guide provides an objective comparison of LSTM and GRU architectures, underpinned by experimental data and detailed methodological insights, to inform researchers and drug development professionals in their model selection process for glucose prediction and related time-series forecasting tasks.
The core innovation of both LSTM and GRU networks lies in their gating mechanisms, which regulate the flow of information through the sequence, enabling them to capture long-range dependencies more effectively than simple RNNs.
LSTM Architecture
Long Short-Term Memory networks introduce a sophisticated memory cell structure with three distinct gates [37]:
- Forget Gate: Determines what information should be discarded from the cell state.
- Input Gate: Controls which new information should be stored in the cell state.
- Output Gate: Regulates what parts of the cell state should be output at the current timestep.
This three-gate system, coupled with a separate cell state that acts as a "conveyor belt" for information, allows LSTMs to maintain and access relevant information over extended sequences, making them particularly powerful for modeling complex temporal relationships [37].
GRU Architecture
Gated Recurrent Units simplify the LSTM approach by combining the input and forget gates into a single update gate, resulting in a more streamlined architecture with only two gates [38]:
- Update Gate: Balances the influence of previous hidden state information with new candidate information.
- Reset Gate: Determines how much of the previous hidden state should be ignored when computing the new candidate state.
GRUs eliminate the separate cell state, using only the hidden state to transfer information, which reduces architectural complexity and computational requirements while maintaining competitive performance on many sequence modeling tasks [37] [38].
Performance Comparison in Time Series Forecasting
Empirical evaluations across diverse domains reveal nuanced performance differences between LSTM and GRU architectures, with outcomes significantly influenced by dataset characteristics and task requirements.
Quantitative Benchmarking Results
Table 1: Comprehensive performance comparison of LSTM and GRU across domains
| Application Domain | Dataset/Context | LSTM Performance | GRU Performance | Performance Notes | Source |
|---|---|---|---|---|---|
| Sea Level Prediction | Ulleungdo Island Tide Data | Higher RMSE | RMSE ≈0.44 cm | GRU demonstrated superior predictive accuracy and training stability | [39] |
| Glucose Prediction | Hybrid Transformer-LSTM | MSE: 1.18 (15-min) | Not Tested | Outperformed standard LSTM in glucose forecasting | [40] |
| Text Classification | Movie Reviews Dataset | 87.3% Accuracy | 86.8% Accuracy | Comparable accuracy with GRU training 38% faster | [37] |
| Stock Prediction | 1-Year Sequences | MSE: 0.023 | MSE: 0.029 | LSTM superior for complex financial patterns | [37] |
| Battery SOH Estimation | Lithium-ion Batteries | Higher Complexity | Streamlined Parameters | GRU more efficient for resource-constrained environments | [41] |
| Monte Carlo Benchmark | Three Time Series Datasets | Best on 1 Dataset | Competitive Performance | LSTM-RNN hybrid showed best overall performance | [38] |
Computational Efficiency Analysis
Table 2: Computational requirements and training characteristics
| Metric | LSTM | GRU | Practical Implications | |
|---|---|---|---|---|
| Training Speed | Baseline (Slower) | 25-40% Faster | GRU enables faster iteration cycles | [37] |
| Parameter Count | Higher (3 Gates) | Lower (2 Gates) | GRU uses ~25% less memory | [41] [37] |
| Inference Speed | Standard | Faster | GRU better for real-time applications | [37] |
| Hyperparameter Sensitivity | Higher | Lower | GRU more forgiving during tuning | [37] |
| Overfitting Risk | Higher on Small Datasets | Lower | GRU generally better for limited data | [37] |
| Optimal Sequence Length | Long (>500 steps) | Short to Medium | Domain-dependent suitability | [37] |
The benchmarking data indicates that while LSTMs may achieve marginally superior accuracy on certain complex tasks (2-5% improvement in some cases), GRUs provide significantly better computational efficiency with competitive performance, making them particularly valuable for resource-constrained environments or applications requiring rapid prototyping [37] [39].
Experimental Protocols and Methodologies
Glucose Prediction Experimental Framework
Recent advances in glucose prediction highlight sophisticated hybrid approaches combining both architectural innovations and specialized preprocessing techniques.
Transformer-LSTM Hybrid Methodology [40]:
- Dataset: Utilized over 32,000 data points from CGM systems of eight patients from Suzhou Municipal Hospital
- Preprocessing: Incorporated historical glucose readings and equipment calibration values
- Architecture: Combined Transformer's global contextualization with LSTM's temporal sequencing capabilities
- Evaluation Metrics: Mean Square Error at 15, 30, and 45-minute forecasting intervals
- Results: Achieved MSE values of 1.18, 1.70, and 2.00 respectively, significantly outperforming standard LSTM
Stacked LSTM with Kalman Smoothing [42]:
- Data Preparation: Implemented Kalman smoothing for CGM reading correction to mitigate sensor faults
- Feature Engineering: Combined smoothed CGM data, carbohydrate intake, bolus insulin, and cumulative step counts
- Model Architecture: Employed deep stacked LSTM networks with multiple hidden layers
- Validation: Used OhioT1DM dataset with eight weeks of data from six patients
- Performance: Achieved RMSE of 6.45 and 17.24 mg/dl for 30 and 60-minute prediction horizons
Benchmarking Methodologies
Comprehensive evaluation frameworks employ rigorous statistical methods to ensure reliable performance comparisons:
Monte Carlo Simulation Approach [38]:
- Iterations: 100 iterations per architecture to account for random weight initialization variance
- Architectures Tested: Nine configurations including RNN, LSTM, GRU, and six hybrid models
- Datasets: Sunspot activity, Indonesian COVID-19 cases, and dissolved oxygen concentration
- Statistical Analysis: Friedman test to assess performance differences across architectures
- Key Finding: No statistically significant differences among architectures, but LSTM-based hybrids demonstrated practical advantages in consistency and robustness
The Researcher's Toolkit: Essential Materials and Reagents
Table 3: Key research components for glucose prediction experiments
| Component Category | Specific Examples | Function/Purpose | Implementation Notes | |
|---|---|---|---|---|
| Data Sources | OhioT1DM Dataset, Suzhou Municipal Hospital CGM Data | Model training and validation | Ensure ethical compliance and data quality assessment | [40] [42] |
| Preprocessing Tools | Kalman Smoothing, Min-Max Normalization | Sensor error correction, data standardization | Critical for handling CGM sensor faults and variability | [42] |
| Feature Sets | Historical Glucose, Carbohydrate intake, Bolus Insulin, Step Count | Represent physiological context | Step count from fitness bands improves prediction accuracy | [42] |
| Model Architectures | LSTM, GRU, Transformer Hybrids | Temporal pattern recognition | Selection depends on sequence complexity and resources | [40] [38] |
| Evaluation Metrics | RMSE, MSE, MAPE, R² | Performance quantification | Clinical accuracy beyond statistical measures | [40] [39] |
| Optimization Algorithms | Sparrow Search Algorithm, Bayesian Optimization | Hyperparameter tuning | Automated optimization enhances model performance | [43] |
Decision Framework and Implementation Guidelines
Architecture Selection Criteria
Based on comprehensive experimental results, the following decision framework emerges for selecting between LSTM and GRU architectures:
Choose LSTM when [37]:
- Working with very long sequences (>500 steps) with complex temporal dependencies
- Maximum predictive accuracy is critical and computational resources are sufficient
- Modeling intricate long-term dependencies in domains like natural language processing or complex physiological patterns
- Working with large datasets (>100k samples) where overfitting concerns are minimized
- Computational efficiency or training speed is a primary concern
- Working with small to medium-sized datasets (<100k samples)
- Rapid prototyping or iterative development is required
- Deploying to resource-constrained environments (mobile devices, edge computing)
- Sequences are of short to moderate length with less complex dependencies
Hybrid Approaches and Future Directions
The emergence of hybrid models represents a promising direction for leveraging the strengths of both architectures. The LSTM-GRU and LSTM-RNN configurations have demonstrated superior performance in comprehensive benchmarking studies [38]. Similarly, the integration of Transformers with LSTM networks has shown significant improvements in glucose prediction accuracy by combining global contextualization with temporal sequencing [40].
These hybrid approaches, along with continued architectural innovations, suggest that the future of sequence modeling in healthcare applications lies not in selecting a single universal architecture, but in developing specialized configurations that leverage the complementary strengths of multiple approaches tailored to specific predictive tasks and clinical requirements.
The accurate forecasting of blood glucose levels represents a critical challenge in diabetes management. The dynamic nature of glucose metabolism, influenced by meals, insulin, physical activity, and individual physiological factors, creates a complex time-series prediction problem. Traditional machine learning approaches often struggle to capture both the short-term fluctuations and long-term dependencies inherent in continuous glucose monitoring (CGM) data. This comparative analysis examines the performance of two advanced deep learning architectures—CNN-LSTM and Bidirectional LSTM (Bi-LSTM) with attention mechanisms—in addressing this challenge. These hybrid architectures leverage complementary strengths: CNNs excel at extracting local patterns and features from sequential data, LSTMs model temporal dependencies, attention mechanisms highlight critical time points, while Bi-LSTM networks process data in both forward and backward directions to capture broader contextual information [44] [14]. Within the context of predictive interstitial glucose classification research, understanding the relative strengths, implementation requirements, and performance characteristics of these architectures provides valuable guidance for researchers and drug development professionals working on diabetes management solutions.
CNN-LSTM Hybrid Architecture
The CNN-LSTM architecture employs a sequential processing approach where convolutional layers extract salient features from raw input sequences, which are then passed to LSTM layers for temporal modeling. The CNN component typically consists of one-dimensional convolutional layers that operate on the time-series data, identifying local patterns, trends, and shapes within glucose fluctuations [45]. These extracted features are then fed into LSTM layers capable of learning long-term dependencies between the identified patterns. Research demonstrates that this architecture effectively captures both spatial features (through CNN) and temporal dependencies (through LSTM) in glucose data [46]. For example, in one implementation, windowed samples of past data were input to a stack of 1D convolutional and pooling layers, followed by an LSTM block containing two layers of LSTM units, and finally through fully connected layers to produce glucose predictions [45].
Bi-LSTM with Attention Mechanism
The Bi-LSTM with attention mechanism represents a more sophisticated approach to temporal modeling. Bi-LSTM networks process sequential data in both forward and backward directions, capturing information from both past and future contexts relative to each time point [47] [14]. This bidirectional processing provides a more comprehensive understanding of glucose trends by considering the complete context around each measurement. The attention mechanism further enhances this architecture by dynamically weighting the importance of different time steps in the input sequence [44]. This allows the model to focus on clinically significant periods, such as rapid glucose transitions following meals or insulin administration, while downweighting less informative stable periods [44]. The combination enables the model to handle noisy CGM data more effectively and provides insights into which temporal segments most influence the predictions.
Integrated CNN-Bi-LSTM with Attention
Recent advanced implementations have combined all these elements into a unified CNN-Bi-LSTM architecture with attention mechanisms. In one proposed multimodal approach for type 2 diabetes management, CGM time series were processed using a stacked CNN and a Bi-LSTM network followed by an attention mechanism [14]. In this configuration, the CNN captures local sequential features, the Bi-LSTM learns long-term temporal dependencies in both directions, and the attention mechanism prioritizes the most relevant features for the final prediction [14]. This comprehensive approach has demonstrated capability in handling the complex, multi-scale dependencies that characterize glucose fluctuations across different time horizons.
Table 1: Comparison of Architectural Properties and Implementation Considerations
| Architectural Characteristic | CNN-LSTM | Bi-LSTM with Attention | Integrated CNN-Bi-LSTM-Attention |
|---|---|---|---|
| Primary Strengths | Excellent local pattern extraction; Efficient spatial feature learning | Comprehensive contextual understanding; Dynamic time-step weighting | Combines advantages of both architectures; Multi-scale dependency modeling |
| Computational Complexity | Moderate | Higher due to bidirectional processing | Highest due to combined architecture |
| Data Requirements | Requires sufficient data for CNN feature learning | Benefits from larger datasets for robust attention learning | Requires substantial datasets for all components |
| Handling of Noisy Data | CNN helps filter noise but limited temporal context | Attention mechanism can downweight noisy periods | Most robust due to combined filtering and weighting |
| Interpretability | Moderate - CNN features interpretable but LSTM less so | Higher - Attention weights show important time steps | Moderate - Complex but attention provides some insights |
| Implementation Examples in Research | Short-term load forecasting [48]; Energy consumption prediction [48] | Personalized BG prediction in T1D [47]; Short-term solar irradiance [48] | Multimodal T2D management [14]; Human activity recognition [44] |
Performance Comparison in Glucose Prediction
Quantitative Performance Metrics
Multiple studies have conducted empirical evaluations comparing these architectures for glucose prediction tasks. In research classifying leakage currents (a related time-series problem), the CNN-Bi-LSTM model demonstrated significant performance advantages, achieving maximum enhancements of 81.081%, 14.382%, and 31.775% in category cross-entropy error, accuracy, and precision respectively compared to regular LSTM, Bi-LSTM, and CNN-LSTM models [48]. For blood glucose prediction specifically, a hybrid Bi-LSTM-Transformer model with meta-learning achieved a mean RMSE of 24.89 mg/dL for a 30-minute prediction horizon, representing a substantial improvement of 19.3% over a standard LSTM and 14.2% over an Edge-LSTM model [47]. The model also achieved the lowest standard deviation (±4.60 mg/dL), indicating more consistent performance across patients [47].
In a multimodal approach for type 2 diabetes management that incorporated both CGM data and physiological context using a CNN-Bi-LSTM with attention, researchers reported prediction results with Mean Absolute Point Error (MAPE) between 14-24 mg/dL, 19-22 mg/dL, and 25-26 mg/dL for 15-, 30-, and 60-minute prediction horizons respectively using a Menarini sensor [14]. The same study found that the multimodal architecture significantly outperformed unimodal approaches at 30- and 60-minute horizons, demonstrating the value of incorporating additional physiological information alongside the advanced architecture [14].
Table 2: Performance Metrics Across Different Prediction Horizons and Architectures
| Architecture | Prediction Horizon | Key Performance Metrics | Dataset/Context |
|---|---|---|---|
| CNN-LSTM | 90 minutes | MAE: 17.30 ± 2.07 mg/dL; RMSE: 23.45 ± 3.18 mg/dL [45] | Replace-BG dataset (T1D) |
| CNN-LSTM | 90 minutes | MAE: 18.23 ± 2.97 mg/dL; RMSE: 25.12 ± 4.65 mg/dL [45] | DIAdvisor dataset (T1D) |
| Bi-LSTM-Transformer (BiT-MAML) | 30 minutes | RMSE: 24.89 mg/dL (19.3% improvement over LSTM) [47] | OhioT1DM dataset |
| CNN-Bi-LSTM with Attention (Multimodal) | 15, 30, 60 minutes | MAPE: 14-24, 19-22, 25-26 mg/dL (Menarini sensor) [14] | Type 2 Diabetes dataset |
| CNN-Bi-LSTM with Attention (Multimodal) | 15, 30, 60 minutes | MAPE: 6-11, 9-14, 12-18 mg/dL (Abbott sensor) [14] | Type 2 Diabetes dataset |
| CNN-Bi-LSTM | Classification | 81.081% improvement in cross-entropy error vs. LSTM [48] | Leakage current classification |
Clinical Safety and Accuracy
Beyond traditional accuracy metrics, clinical safety represents a critical consideration for glucose prediction models. Clarke Error Grid Analysis (CEGA) provides a method for assessing the clinical accuracy of glucose predictions by categorizing predictions into zones representing different clinical risk levels. In one study utilizing a Bi-LSTM-Transformer hybrid model, over 92% of predictions fell within the clinically acceptable Zones A and B, demonstrating robustness from a clinical safety perspective [47]. Similarly, Parkes Error Grid analysis has been used to validate the clinical explainability of prediction performance in multimodal architectures [14]. For hypoglycemia prediction specifically, which is critical for patient safety, LSTM models have demonstrated strong performance with recall rates of 87% for a 1-hour forecast horizon, outperforming logistic regression and ARIMA models for this longer prediction window [6] [2].
Experimental Protocols and Methodologies
Data Preprocessing and Feature Engineering
Robust experimental protocols are essential for valid performance comparisons across architectures. Most studies employ careful data preprocessing steps including handling missing CGM data points through linear interpolation for gaps less than 60 minutes [45], normalization of time series to a (0,1) range to improve prediction accuracy [45], and resampling of CGM data to consistent time intervals (typically 5-15 minutes) [47] [49]. Feature construction often includes both raw physiological measurements and engineered features. For example, one study constructed a comprehensive set of nine features designed to capture complex glucose dynamics, including rate of change metrics and variability indices [47]. When available, additional contextual features such as meal information, insulin dosages, and physiological parameters are incorporated, with some multimodal approaches integrating baseline health records to inform CGM trends [14].
Model Training and Evaluation Frameworks
Appropriate training methodologies are critical for fair architecture comparisons. Most studies employ temporal train-test splitting strategies such as Forward Chaining or Leave-One-Patient-Out Cross-Validation (LOPO-CV) to account for temporal dependencies and avoid data leakage [45] [47]. The LOPO-CV approach is particularly valuable for assessing generalizability across diverse patient populations as it tests each patient using models trained exclusively on other patients [47]. Hyperparameter optimization techniques such as simple grid search parameters are commonly applied to determine optimal network structures [48]. For the Bi-LSTM component with attention, this typically involves optimizing the number of hidden units, attention dimensions, and the architecture of the preceding CNN layers when included [44]. Loss functions vary by task, with regression tasks often using Mean Absolute Error (MAE) or Root Mean Square Error (RMSE) and classification tasks employing categorical cross-entropy [48] [45].
Figure 1: Experimental workflow for developing and evaluating hybrid glucose prediction architectures, showing key stages from data collection through to model evaluation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Components for Implementing Hybrid Glucose Prediction Architectures
| Research Component | Function/Description | Example Implementations |
|---|---|---|
| Continuous Glucose Monitoring Datasets | Provides sequential glucose measurements for model training and validation | OhioT1DM [47], Replace-BG [45], DIAdvisor [45], Suzhou Municipal Hospital dataset [49] |
| Deep Learning Frameworks | Software libraries for implementing and training complex neural network architectures | TensorFlow, PyTorch, Keras |
| Hyperparameter Optimization Tools | Methods for determining optimal network structures and training parameters | Simple grid search [48], random search [4], Bayesian optimization |
| Clinical Accuracy Assessment Tools | Methods for evaluating clinical (not just statistical) accuracy of predictions | Clarke Error Grid Analysis (CEGA) [47], Parkes Error Grid Analysis [14] |
| Temporal Cross-Validation Methods | Validation approaches that account for time-series structure of data | Leave-One-Patient-Out CV (LOPO-CV) [47], Forward Chaining [45] |
| Multimodal Data Integration Pipelines | Frameworks for combining CGM data with additional physiological context | Baseline health records fusion [14], meal and insulin information integration [45] |
The comparative analysis of CNN-LSTM and Bidirectional LSTM with attention mechanisms for glucose prediction reveals a complex performance landscape with different architectures excelling in different contexts. The CNN-LSTM architecture provides a solid foundation with good performance and moderate computational demands, making it suitable for applications with limited resources or shorter prediction horizons. In contrast, Bi-LSTM with attention mechanisms offers enhanced capability for capturing complex temporal dependencies and handling noisy data, particularly valuable for longer prediction horizons and personalized applications. The most advanced integrated CNN-Bi-LSTM with attention architectures demonstrate the highest performance, especially when incorporating multimodal data, but at the cost of increased complexity and data requirements [14].
For researchers and drug development professionals, selection criteria should consider the specific application context: prediction horizon requirements, available computational resources, data quantity and quality, and need for interpretability. Future research directions should focus on enhancing model interpretability for clinical adoption, developing more efficient architectures for real-time applications, improving personalization through transfer learning and meta-learning approaches [47], and standardizing evaluation protocols to enable more meaningful comparisons across studies. As these advanced hybrid architectures continue to evolve, they hold significant promise for creating more effective and reliable decision support systems in diabetes management and beyond.
The field of diabetes management has been transformed by continuous glucose monitoring (CGM), which provides real-time insights into interstitial glucose concentrations. Traditional predictive models relying solely on CGM data face significant challenges, including the inherent ~10-minute physiological delay between interstitial and plasma glucose readings, sensor malfunctions, and considerable inter-individual variability in glucose metabolism [2] [6]. These limitations have prompted researchers to explore multimodal learning approaches that integrate CGM data with baseline physiological and health records to create more accurate, personalized, and clinically actionable prediction systems.
Multimodal learning represents a paradigm shift in glucose forecasting by addressing a critical gap in unimodal approaches: the failure to account for individual physiological differences that fundamentally influence interstitial glucose dynamics [14]. While recent advances in deep learning enable sophisticated modeling of temporal patterns in glucose fluctuations, most existing methods rely exclusively on CGM inputs. The integration of baseline health information creates a more holistic representation of an individual's metabolic state, potentially enabling more robust predictions across diverse populations and longer time horizons.
This comparative analysis examines the emerging evidence for multimodal architectures in glucose prediction, focusing specifically on their performance advantages over conventional unimodal approaches. By synthesizing experimental data and methodological insights from recent studies, this guide aims to provide researchers and drug development professionals with a comprehensive framework for evaluating and implementing multimodal learning strategies in glucose classification research.
Comparative Performance Analysis: Multimodal vs. Unimodal Approaches
Quantitative Performance Metrics Across Prediction Horizons
Table 1: Performance Comparison of Multimodal vs. Unimodal Architectures
| Architecture | Prediction Horizon | MAPE (mg/dL) | RMSE (mg/dL) | Key Advantages |
|---|---|---|---|---|
| Multimodal (CNN-BiLSTM with Attention) [14] | 15 minutes | 6-11 (Abbott), 14-24 (Menarini) | - | Incorporates individual physiological context |
| 30 minutes | 9-14 (Abbott), 19-22 (Menarini) | - | Superior longer-horizon performance | |
| 60 minutes | 12-18 (Abbott), 25-26 (Menarini) | - | Handles glycemic variability better | |
| Unimodal (LSTM) [2] [6] | 15 minutes | - | - | 96% recall (hyper), 98% recall (hypo) |
| 60 minutes | - | - | 85% recall (hyper), 87% recall (hypo) | |
| Unimodal (Logistic Regression) [2] [28] | 15 minutes | - | - | 96% recall (hyper), 98% recall (hypo) |
| 60 minutes | - | - | Lower accuracy for extended horizons | |
| Non-Invasive Multimodal (LightGBM) [50] | 15 minutes | 15.58 ± 0.09% | 18.49 ± 0.1 | Eliminates need for food logs |
The comparative data reveals a consistent pattern: multimodal architectures demonstrate particular advantages for longer prediction horizons (30-60 minutes), where contextual physiological information becomes increasingly valuable for accurate forecasting [14]. For shorter horizons (15 minutes), simpler unimodal approaches can achieve competitive performance, with logistic regression reporting recall rates of 96% for hyperglycemia and 98% for hypoglycemia [2] [6]. However, this performance advantage diminishes as the prediction window extends, with LSTM models outperforming logistic regression for 60-minute horizons (85% vs. 60% for hyperglycemia prediction) [28].
The sensor-specific variations in performance metrics (particularly between Abbott and Menarini systems) highlight the importance of accounting for device characteristics when developing and evaluating predictive models [14]. These differences may stem from variations in sensor accuracy, sampling frequency, or signal processing algorithms across manufacturers.
Clinical Accuracy Assessment Through Error Grid Analysis
Table 2: Clinical Accuracy Assessment Using Error Grid Analysis
| Model Type | Parkes/Clarke Error Grid Zone A (%) | Clinically Acceptable (Zones A+B) (%) | Clinical Risk (Zones C-E) (%) |
|---|---|---|---|
| Non-Invasive Multimodal (LightGBM) [50] | - | >96% | <3.58% in Zone D |
| Feature-Based LightGBM [50] | Majority points | >96% | Minimal clinical risk |
Error grid analysis provides crucial insights into the clinical safety of glucose prediction models by categorizing predictions based on their potential to lead to clinically harmful treatment decisions [50]. The multimodal approach demonstrates strong clinical safety profiles, with less than 3.58% of predictions falling into clinically significant error zones (D regions) that could result in inappropriate diabetes management [50]. This safety profile is particularly important for real-world clinical applications, where inaccurate predictions could lead to dangerous over- or under-treatment of impending hypoglycemia or hyperglycemia.
Experimental Protocols and Methodologies
Multimodal Architecture Implementation Framework
Figure 1: Multimodal Architecture Workflow Integrating CGM and Health Record Data
The experimental workflow for multimodal glucose prediction involves two parallel processing streams that fuse temporal CGM patterns with static physiological context [14]. The CGM pipeline typically employs a stacked convolutional neural network (CNN) and bidirectional long short-term memory (BiLSTM) network followed by an attention mechanism. The CNN captures local sequential features and patterns in glucose fluctuations, while the BiLSTM learns long-term temporal dependencies across extended time windows. The attention mechanism allows the model to adaptively focus on the most relevant time points for each prediction, particularly valuable during periods of high glycemic variability [14].
Concurrently, the baseline physiological pipeline processes static health records through a separate neural network, typically comprising fully connected dense layers. This stream incorporates individual patient characteristics such as demographics, comorbidities, and clinical biomarkers that influence glucose metabolism. The feature engineering process for both streams may include derived metrics such as glucose rate of change, variability indices, and time-based features when additional physiological parameters are unavailable [2].
The fusion layer integrates the processed temporal patterns from the CGM pipeline with the physiological context from the baseline pipeline, typically through concatenation or more sophisticated cross-attention mechanisms. This fused representation enables the model to generate predictions that are simultaneously informed by recent glucose trends and individual metabolic characteristics [14].
Data Acquisition and Preprocessing Standards
Table 3: Data Specifications and Preprocessing Protocols
| Data Modality | Sources | Preprocessing Steps | Frequency/Timing |
|---|---|---|---|
| CGM Data [2] [14] | Abbott Libre, Menarini GlucoMen Day, Dexcom G7 | Gap filling, resampling to 15-min intervals, smoothing filters | Every 5-15 minutes |
| Baseline Health Records [14] | Electronic health records, patient registries | Normalization, handling missing values, feature selection | Single timepoint (baseline) |
| Non-Invasive Sensors [50] | Empatica E4, other wearables | Signal filtering, artifact removal, feature extraction | Continuous high-frequency |
Rigorous data preprocessing is essential for robust model performance. CGM data requires careful handling of missing values due to sensor signal loss or connectivity issues [2]. Standard preprocessing includes resampling to consistent time intervals (typically 5-15 minutes), applying smoothing filters to reduce high-frequency noise without eliminating clinically meaningful rapid fluctuations, and gap imputation using appropriate temporal interpolation methods [14].
Baseline health records often present challenges of missing data and heterogeneous variable types. Preprocessing typically includes normalization of continuous variables, one-hot encoding of categorical variables, and sophisticated imputation methods for missing clinical parameters [14]. Feature selection techniques may be employed to identify the most predictive baseline variables while managing model complexity, especially when working with smaller sample sizes.
For studies incorporating non-invasive sensor data, additional signal processing is required to extract meaningful features from raw physiological signals such as heart rate, skin temperature, electrodermal activity, and blood volume pulse [50]. These features are then synchronized with CGM measurements to establish correlation patterns between external physiological signals and glucose dynamics.
Research Reagent Solutions: Essential Tools for Glucose Prediction Research
Table 4: Essential Research Materials and Computational Tools
| Category | Specific Tools/Platforms | Research Application | Key Features |
|---|---|---|---|
| CGM Sensors [14] [51] | Abbott Libre Series, Menarini GlucoMen Day, Dexcom G7 | Real-world glucose data acquisition | Factory calibration, 14-day duration (Libre), 10-day duration (Dexcom G7) |
| Software Simulators [2] [28] | Simglucose v0.2.1, UVA/Padova T1D Simulator | Algorithm validation, synthetic data generation | Python implementation, in-silico patient cohorts |
| Non-Invasive Wearables [50] | Empatica E4 wristband | Physiological signal acquisition | BVP, EDA, HR, skin temperature monitoring |
| Deep Learning Frameworks [14] [52] | TensorFlow, PyTorch | Model development and training | CNN, BiLSTM, Attention mechanism implementation |
| Data Analysis Platforms [3] | R, Python with specialized libraries | Functional data analysis, traditional statistics | AGP analysis, temporal pattern recognition |
The experimental research in glucose prediction relies on a sophisticated ecosystem of sensing technologies, computational tools, and analytical platforms. CGM sensors from major manufacturers (Abbott, Dexcom, Menarini) serve as the primary data acquisition tools, each with distinct characteristics in accuracy (MARD 7.9-11.2%), sensor duration (7-14 days), and warm-up times (30-120 minutes) that influence data quality and study design [51].
Software simulators such as Simglucose v0.2.1 provide valuable platforms for initial algorithm development and validation using synthetic patient cohorts [2] [28]. These simulators implement accepted metabolic models and allow researchers to generate controlled datasets spanning diverse patient phenotypes and scenarios, though ultimate validation requires real-world clinical data.
For multimodal approaches incorporating non-invasive sensing, research-grade wearables like the Empatica E4 enable acquisition of physiological signals including blood volume pulse, electrodermal activity, heart rate, and skin temperature [50]. These modalities provide additional contextual information about physical activity, stress responses, and autonomic nervous system activity that correlate with glucose fluctuations.
Computational frameworks for implementing deep learning architectures typically leverage TensorFlow or PyTorch ecosystems, which provide optimized implementations of CNN, LSTM, and attention mechanisms essential for processing temporal glucose patterns [14]. For specialized statistical analysis, particularly functional data analysis techniques that treat CGM trajectories as continuous mathematical functions rather than discrete measurements, platforms like R with specialized packages offer advanced analytical capabilities beyond traditional summary statistics [3].
The evidence from comparative studies indicates that multimodal learning approaches represent a significant advancement in glucose prediction technology, particularly for longer forecasting horizons and personalized applications. By integrating the temporal patterns captured in CGM data with the metabolic context derived from baseline physiological records, these architectures achieve superior performance in predicting both hyperglycemic and hypoglycemic events [14].
Several important considerations emerge for researchers working in this field. First, the performance advantage of multimodal approaches appears most pronounced at longer prediction horizons (30-60 minutes), where contextual physiological information becomes increasingly valuable [14]. Second, the implementation complexity of multimodal systems must be balanced against the availability of comprehensive baseline data, as including more variables can reduce the effective sample size for model training [14]. Finally, the translation of these algorithms into clinical practice requires careful attention to usability and implementation frameworks, with DIY approaches showing promise for enhancing patient engagement and long-term adherence [52].
Future research directions should explore more sophisticated fusion techniques for combining temporal and static data modalities, investigate transfer learning approaches to address data scarcity issues, and develop more granular analyses of performance across different patient subpopulations and glycemic states. As foundation models pretrained on massive CGM datasets emerge [17], the integration of these pre-trained temporal representations with multimodal architectures represents a particularly promising avenue for advancing the accuracy and personalization of glucose forecasting systems.
Effective glucose forecasting is a cornerstone of modern diabetes management, enabling proactive interventions to prevent dangerous hypoglycemic and hyperglycemic events. While the choice of prediction model is important, the engineering of input features—the quantitative descriptors derived from raw data—is equally critical for developing robust, accurate, and clinically actionable forecasting systems. This guide provides a comparative analysis of core feature engineering methodologies, focusing on Rate of Change (ROC), Variability Indices, and Time-Based Features. Framed within a broader thesis on predictive interstitial glucose classification, this article objectively compares the performance impacts of different feature sets, supported by experimental data and detailed protocols, to inform researchers, scientists, and drug development professionals.
Core Feature Categories and Their Impact on Forecasting
The predictive power of a glucose forecasting model is heavily dependent on the features used to represent the underlying physiological processes. The table below summarizes the primary feature categories, their specific components, and their documented impact on prediction performance.
Table 1: Core Feature Categories for Glucose Forecasting
| Feature Category | Specific Features | Physiological Rationale | Impact on Forecasting Performance |
|---|---|---|---|
| Rate of Change (ROC) | - Immediate ROC (e.g., diff_10, diff_30)- Short-term slope (e.g., slope_1hr) [53] |
Captures the immediate direction and momentum of glucose dynamics [53]. | - Essential for short-term horizon (≤30 min) predictions [53].- High interaction effect with current glucose level; a negative ROC at a low baseline is a strong hypoglycemia indicator [53]. |
| Variability Indices | - Standard deviation (e.g., sd_2hr, sd_4hr) [53]- Glucose Risk (GR) metrics [54]- "Snowball Effect" features (e.g., cumulative positive/negative changes in past 2 hours) [53] |
Quantifies intra-day glycemic stability and the accruing effect of consecutive fluctuations [53] [54]. | - Medium-term features (1-4 hours) crucial for 60-minute hypoglycemia prediction [53].- Helps the model anticipate instability and the compounding risk of extreme events [53]. |
| Time-Based Features | - Time of day, Day of week [53]- Time in Ranges (TIRs) [54] | Encodes circadian rhythms, weekly routines, and long-term control patterns [53] [54]. | - Nocturnal hypoglycemia prediction significantly improved (~95% sensitivity) [53].- TIRs provide a summary of glycemic control effectiveness over time [54]. |
| Personalized & Contextual | - Personalized excursions (e.g., PersHigh, PersLow) [55]- Insulin-on-Board, Carbohydrate-on-Board [53] |
Moves beyond population-level thresholds to define what is "high" or "low" for a specific individual; accounts for metabolic delays [55]. | - Achieved 84.3% accuracy in classifying personalized excursions [55].- Inclusion of context (carbs, insulin) improved 60-minute prediction performance [53]. |
The relationships between these feature categories and their collective contribution to a highly discriminative feature set for model training can be visualized as an integrated workflow.
Comparative Analysis of Feature Engineering Methodologies
Experimental Protocols and Performance Metrics
To objectively compare the impact of feature engineering, it is essential to examine the methodologies and metrics used in rigorous experimental evaluations.
Table 2: Summary of Experimental Protocols from Key Studies
| Study & Model | Dataset & Subjects | Feature Engineering Methodology | Key Performance Metrics |
|---|---|---|---|
| LSTM with Feature Transformation [56] | Ohio T1DM (2018)6 T1DM patients [56] | - Event-based data (meals, insulin) transformed into continuous time-series features.- Comprehensive pre-processing: interpolation, filtering, time-alignment [56]. | - RMSE: 14.76 mg/dL (30-min), 25.48 mg/dL (60-min) [56]. |
| Feature-Based ML for Hypoglycemia [53] | 112 Pediatric T1DM~1.6M CGM values [53] | - Extracted 26 features across 7 categories (short/medium/long-term, snowball, demographic, interaction, contextual).- Parsimonious subset selected for influence [53]. | - Sensitivity: >91% (30 & 60-min).- Specificity: >90% (30 & 60-min).- Nocturnal: ~95% sensitivity [53]. |
| Personalized Glucose Excursion Classification [55] | 25,000 paired CGM & wearable measurements [55] | - 69 variables engineered from wearables and food logs.- Personalized, dynamic thresholds (PersHigh, PersLow) defined as ±1 SD from 24h rolling mean [55]. |
- Accuracy: 84.3% in classifying PersHigh/PersLow/PersNorm [55]. |
| SHAP Analysis of LSTM Models [57] | Ohio T1DM1 T1DM patient (ID 588) [57] | - Comparison of standard LSTM (np-LSTM) vs. physiologically-guided LSTM (p-LSTM).- Use of SHAP to interpret feature contribution and ensure physiological plausibility [57]. | - RMSE: ~20 mg/dL (30-min, both models).- Clinical Safety: Only p-LSTM learned correct insulin/glucose relationship, leading to safe insulin suggestions [57]. |
Quantitative Performance Comparison
The table below synthesizes quantitative results from multiple studies, highlighting how different feature engineering strategies directly influence forecasting accuracy.
Table 3: Comparative Performance of Forecasting Models Using Different Feature Sets
| Model / Feature Emphasis | Prediction Horizon | Key Results | Interpretation / Clinical Impact |
|---|---|---|---|
| LSTM with Transformed Features [56] | 30-min | RMSE: 14.76 mg/dL [56] | Transforming sparse events into continuous features provides a richer input signal, lowering error. |
| Feature-Based ML Model [53] | 30-min & 60-min | Sensitivity: >91%, Specificity: >90% [53] | A comprehensive, multi-category feature set enables highly precise event (hypoglycemia) classification. |
| Personalized Excursion Model [55] | Real-time Classification | Accuracy: 84.3% [55] | Personalizing the definition of a "glucose excursion" improves relevance for non-diabetic and prediabetic populations. |
| Physiological LSTM (p-LSTM) [57] | 30-min | RMSE: ~20 mg/dL; Correct insulin effect learned [57] | Models with similar accuracy can differ in safety. Interpretability tools (SHAP) are critical to verify physiological validity. |
The Scientist's Toolkit: Research Reagent Solutions
Implementing the feature engineering strategies discussed requires robust software tools. The following table details key open-source libraries that facilitate the extraction of critical features from glucose time series data.
Table 4: Essential Software Tools for Glucose Feature Extraction
| Tool / Library | Language | Primary Function | Key Advantages for Research |
|---|---|---|---|
| GlucoStats [54] | Python | Extracts a comprehensive set of 59 statistics from glucose time series, including TIR, GV, and risk metrics [54]. | - Parallel processing for large datasets.- Scikit-learn compatible for easy ML pipeline integration.- Advanced visualization tools [54]. |
| cgmanalysis & iglu [54] | R | Calculation of standard glycemic metrics from CGM data [54]. | - Established packages in the R ecosystem.- Suitable for clinical research and validation studies. |
| CGM-GUIDE & GlyCulator [54] | Web / MATLAB | Web-based and MATLAB-based tools for CGM metric calculation [54]. | - Accessible for users without programming expertise.- Integrates with MATLAB-based modeling workflows. |
Feature engineering is a decisive factor in the performance and clinical utility of glucose forecasting models. The experimental data and comparisons presented in this guide lead to several key conclusions. First, a multi-horizon feature set is essential; short-term ROC features dominate 30-minute predictions, while medium-term variability indices become crucial for 60-minute horizons [53]. Second, personalization, through dynamic thresholds or personalized excursions, significantly improves the relevance of predictions for individual patients, especially in prediabetic and normoglycemic populations [55]. Finally, as models grow more complex, the use of interpretability tools like SHAP is not optional but a necessity for validating that models learn physiologically plausible relationships, thereby ensuring patient safety in decision-support applications [57]. Future work in this field will likely focus on the automated learning of features from raw data and the tighter integration of multi-modal data streams to further enhance predictive accuracy and personalization.
Overcoming Practical Challenges and Enhancing Model Performance
Addressing Data Scarcity and the Cold-Start Problem with Personalized (Do-It-Yourself) Models
The development of personalized models for classifying interstitial glucose levels is pivotal for improving diabetes management. These models power advanced systems, such as continuous glucose monitors (CGMs), which provide real-time alerts for hypoglycemia and hyperglycemia [2]. However, a significant barrier to their widespread adoption and efficacy is the cold-start problem, a challenge that arises when there is insufficient historical data to train accurate predictive models for a new user [58] [59]. This data scarcity is particularly acute in the context of DIY models, where data collection environments are less controlled. This article presents a comparative analysis of predictive models, framing the investigation within a broader thesis on addressing data scarcity. We objectively evaluate the performance of three model classes—Autoregressive Integrated Moving Average (ARIMA), Logistic Regression, and Long Short-Term Memory networks (LSTM)—in predicting glucose classification for new users with limited data, providing researchers and drug development professionals with validated experimental protocols and results.
The Cold-Start Challenge in Glucose Prediction
In personalized glucose prediction, the cold-start problem manifests when a new user begins using a CGM system. With no prior user-specific data, model predictions are initially unreliable, posing risks for clinical decision-making [2] [59]. The inherent ~10 minute sensor delay between interstitial and plasma glucose readings further complicates the development of robust models [2]. For researchers, this creates a critical challenge: how to design models that can deliver accurate predictions from the first day of use. Strategic approaches to mitigate this include leveraging similarity-based recommendations from population data, applying transfer learning from pre-trained models, and using hybrid models that combine simple, robust rules with complex learning algorithms [58] [59]. These strategies form the foundation for evaluating the performance of the ARIMA, Logistic Regression, and LSTM models in this study.
Experimental Design and Methodologies
The investigation utilized data from two primary sources to ensure robustness and generalizability [2]:
- Clinical Cohort Data: CGM data was acquired from a clinical study (COVAC-DM) involving 11 participants with type 1 diabetes. Data included sensor glucose readings, insulin dosing, and carbohydrate intake.
- In-Silico Simulation Data: The
simglucose(v0.2.1) Python package, an implementation of the UVA/Padova T1D Simulator, was used to generate data for 30 virtual patients (across adults, adolescents, and children) over 10 days. This simulation included three main meals and optional snacks daily.
The raw data was pre-processed to a consistent 15-minute time frequency. Glucose levels were classified into three critical categories for model training and evaluation: Hypoglycemia (<70 mg/dL), Euglycemia (70-180 mg/dL), and Hyperglycemia (>180 mg/dL) [2].
Model Selection and Training Protocols
Three distinct model classes were selected for their complementary approaches to time-series and classification problems.
- ARIMA (Autoregressive Integrated Moving Average): This classical statistical model was implemented as a baseline for time-series forecasting. It relies on the temporal dependencies within the glucose data itself, requiring no external features [2].
- Logistic Regression: This model was used for its efficiency and strong performance in classification tasks with limited data. It was trained on features derived from the historical glucose data to predict the probability of each glucose class [2].
- LSTM (Long Short-Term Memory): A type of recurrent neural network designed to capture long-term dependencies in sequential data. Given its data-hungry nature, its performance in cold-start scenarios was a key focus of the investigation [2].
The performance of each model was rigorously evaluated at two predictive horizons critical for proactive intervention: 15 minutes and 1 hour ahead. The primary metrics for comparison were Recall, Precision, and Accuracy, with a particular emphasis on recall for hypoglycemia and hyperglycemia to minimize the risk of missed alerts [2].
The diagram below illustrates the complete experimental workflow.
Figure 1: Experimental workflow for model comparison.
Results and Comparative Performance Analysis
Model Performance Across Prediction Horizons
The quantitative results demonstrate a clear trade-off between model complexity and performance, which is heavily influenced by the prediction horizon.
Table 1: Model Performance Metrics (Recall %) for 15-Minute Prediction Horizon
| Model | Hypoglycemia (<70 mg/dL) | Euglycemia (70-180 mg/dL) | Hyperglycemia (>180 mg/dL) |
|---|---|---|---|
| Logistic Regression | 98% | 91% | 96% |
| LSTM | 87% | 82% | 85% |
| ARIMA | Underperformed | Underperformed | Underperformed |
For the short-term 15-minute forecast, the simpler Logistic Regression model demonstrated superior performance, achieving the highest recall rates across all glucose classes. This is particularly critical for hypoglycemia prediction, where it reached a 98% recall, minimizing the risk of missed alerts [2].
Table 2: Model Performance Metrics (Recall %) for 1-Hour Prediction Horizon
| Model | Hypoglycemia (<70 mg/dL) | Euglycemia (70-180 mg/dL) | Hyperglycemia (>180 mg/dL) |
|---|---|---|---|
| LSTM | 87% | 80% | 85% |
| Logistic Regression | 78% | 84% | 79% |
| ARIMA | Underperformed | Underperformed | Underperformed |
For the longer 1-hour forecast, the LSTM model outperformed Logistic Regression for the critical hypo- and hyperglycemia classes. Its ability to capture long-term temporal dependencies in the glucose data became a decisive advantage, whereas the performance of the logistic regression model declined more significantly [2]. As anticipated, the ARIMA model underperformed compared to the machine learning approaches at both horizons [2].
Visualizing Model Architecture and Data Flow
The structural differences between the three models are key to understanding their performance. The following diagram outlines the core data flow for each architecture in the context of glucose level classification.
Figure 2: Data flow and architecture of the three model classes.
Discussion: Implications for Cold-Start Scenarios
The experimental data indicates that there is no one-size-fits-all solution for glucose prediction, especially under data scarcity. The choice of model is a strategic decision that depends on the clinical requirement and application context.
- Short-Term Interventions (15-min): For immediate action, such as real-time alerts to prevent imminent hypoglycemia, the Logistic Regression model is the most effective choice. Its high recall for hypoglycemia (98%) and computational efficiency make it ideal for a cold-start environment where data is limited and speed is critical [2].
- Long-Term Management (1-hour): For proactive management of daily activities, such as meal planning or insulin dosing, the LSTM model's ability to forecast further into the future becomes invaluable. Despite requiring more data, its superior 1-hour performance suggests that after a short initial data collection period, it can provide more reliable long-horizon predictions [2].
A promising direction for future research, as suggested by the findings, is the development of hybrid or ensemble models [2]. For instance, a system could use a logistic regression model during the initial cold-start phase and seamlessly transition to an LSTM-based model as sufficient user-specific data is accumulated. This approach would combine the strengths of both models to deliver robust performance throughout the user's journey.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Tools for Glucose Prediction Experiments
| Item Name | Function & Application in Research |
|---|---|
| CGM Simulator (simglucose) | Open-source Python package for generating in-silico T1D patient data; essential for validating algorithms in a controlled environment before clinical trials [2]. |
| Clinical CGM Data | Real-world data from human subjects, including glucose levels, insulin, and carbohydrate intake; crucial for model training and real-world validation [2]. |
| Logistic Regression Model | A statistical model used as a high-performance, low-complexity baseline for classification tasks, particularly effective with limited data [2]. |
| LSTM Network | A type of recurrent neural network capable of learning long-term dependencies in time-series data; used for more accurate long-horizon predictions [2]. |
| ARIMA Model | A classical time-series forecasting model used as a performance benchmark for more complex machine learning models [2]. |
| Pre-Trained Models (Transfer Learning) | Models trained on large, public datasets that can be fine-tuned with limited user-specific data to accelerate personalization and mitigate cold-start [58] [59]. |
| Public Glucose Datasets | Curated datasets (e.g., from Kaggle, clinical repositories) used for initial model prototyping and benchmarking when proprietary data is scarce [60]. |
Strategies for Handling Missing Data and Sensor Signal Dropouts
In the domain of predictive interstitial glucose classification, the integrity and continuity of sensor data are paramount. Missing data and signal dropouts pose a significant challenge, potentially compromising the accuracy of predictive models and subsequent clinical decisions. Sensor-based data collection, particularly from continuous glucose monitors (CGMs) and other wearable devices, is inherently susceptible to gaps from various sources including device removal, charging, motion artifacts, sensor malfunctions, and signal processing errors [2] [61]. Effectively addressing these gaps is not merely a data preprocessing step but a critical component of robust model development. The strategies employed can significantly influence the performance, reliability, and generalizability of predictive algorithms designed for tasks such as hypoglycemia and hyperglycemia classification [2]. This guide provides a comparative analysis of contemporary methods for handling missing data, contextualized within predictive glucose level research, to inform researchers, scientists, and drug development professionals.
Understanding Missing Data Mechanisms
The choice of an appropriate handling strategy is fundamentally guided by the underlying mechanism of missingness. These mechanisms describe the probabilistic relationship between the missing values and the observed data, and are formally categorized as follows [62] [63] [64].
- Missing Completely at Random (MCAR): The probability of a value being missing is independent of both observed and unobserved data. For example, a sensor might randomly fail due to a transient hardware fault unrelated to the physiological signal being measured. Under MCAR, the complete cases represent a random subset of the entire dataset, and simple methods like listwise deletion, while inefficient, do not introduce bias [64].
- Missing at Random (MAR): The probability of a value being missing depends on observed data but not on the unobserved missing value itself. For instance, a higher rate of sensor dropouts might be observed during high-intensity physical activities (as recorded by an accelerometer), but the missing glucose value itself is not related to the reason for its absence. Many advanced imputation methods rely on the MAR assumption [62] [65].
- Missing Not at Random (MNAR): The probability of a value being missing is related to the unobserved missing value itself. This is the most complex mechanism to handle. An example would be a CGM sensor failing precisely when glucose levels exceed a certain high threshold, perhaps due to a biofouling issue. Handling MNAR data requires strong assumptions about the missingness process [62] [64].
The following table summarizes these key mechanisms.
Table 1: Classification of Missing Data Mechanisms
| Mechanism | Definition | Example in Glucose Monitoring | Key Consideration |
|---|---|---|---|
| MCAR | Missingness is independent of all data, observed and unobserved. | A random sensor malfunction due to a manufacturing defect. | Analyses remain unbiased but lose power if data is deleted. |
| MAR | Missingness depends on observed data but not the missing value. | More signal dropouts during recorded exercise events. | Imputation can be effective using other observed variables. |
| MNAR | Missingness depends on the unobserved missing value itself. | Sensor fails more often during extreme (high/low) glucose levels. | Risk of biased analysis; requires specialized methods. |
Comparative Analysis of Handling Strategies
A wide spectrum of techniques exists for handling missing data, ranging from simple deletion to advanced machine learning and self-supervised approaches. The performance and suitability of these methods vary based on the data mechanism, volume, and the ultimate analytical goal (e.g., inference vs. prediction) [64].
Deletion and Simple Imputation Methods
These are traditional baseline methods, but their use can be problematic.
- Listwise Deletion: Removes entire records (cases) with any missing value. It is unbiased only for MCAR data but results in a significant loss of sample size and statistical power, especially with many variables [65].
- Mean/Median/Mode Imputation: Replaces missing values with the mean (for continuous data) or mode (for categorical data) of the observed values. This approach distorts the data distribution, artificially reduces variance, and weakens correlations with other variables, and is generally not recommended [63] [65].
Advanced Statistical and Machine Learning Imputation
These methods leverage relationships within the observed data to estimate missing values more accurately.
- k-Nearest Neighbors (KNN) Imputation: Replaces a missing value with the average (or mode) of the k most similar instances, where similarity is typically based on Euclidean distance across other variables. KNN is simple and can handle both MCAR and MAR data, but becomes computationally intensive with large datasets [66] [65].
- Multivariate Imputation by Chained Equations (MICE): Also known as Fully Conditional Specification, MICE is a multiple imputation technique. It creates several complete datasets by iteratively cycling through each variable with missing data and imputing values using a model that conditions on the other variables. This process accounts for the uncertainty of the imputation, leading to more accurate standard errors. It is highly flexible and can model different variable types [66] [63].
- missForest: A non-parametric imputation method based on Random Forests. It models each variable with missing data as a function of all other variables. missForest is particularly powerful for handling non-linear relationships and complex interactions in mixed-type data (both quantitative and qualitative). Studies have shown it often outperforms MICE and KNN, especially in mixed-type datasets [66] [65].
- Multiple Imputation: This is a general philosophy, implemented by methods like MICE, which involves generating multiple plausible imputed datasets. The analysis is performed on each dataset, and the results are pooled, providing final parameter estimates that reflect the uncertainty due to the missing data. This is considered a gold standard for statistical inference with missing data [63].
Novel and Domain-Specific Approaches
Recent research has introduced methods that move beyond direct imputation.
- LSM-2 with Adaptive and Inherited Masking (AIM): This is a self-supervised learning (SSL) framework designed specifically for incomplete wearable sensor data. Instead of imputing missing values, AIM treats data gaps as natural features of the data. During pre-training of a Large Sensor Model (LSM-2), it uses a masked autoencoder objective that learns from both artificially masked tokens and tokens that are naturally missing from the sensor stream. This allows the model to learn robust representations directly from incomplete data, eliminating the potential bias introduced by imputation and demonstrating strong performance on classification, regression, and generative tasks [61].
The workflow for selecting and applying these strategies is summarized in the following diagram.
Experimental Protocols and Performance in Glucose Prediction
The relative performance of these strategies is best evaluated through controlled experiments. Below is a summary of key experimental findings from the literature, particularly focused on predictive glucose level classification.
Comparative Experimental Framework
A standard protocol for evaluating imputation methods involves:
- Starting with a Complete Dataset: Using a dataset with no missing values as a ground truth.
- Artificially Inducing Missingness: Removing values according to a specific mechanism (e.g., MCAR, MAR) and rate (e.g., 5%, 10%, 20%).
- Applying Imputation Methods: Using the various strategies to recover the missing values.
- Evaluating Performance: Comparing the imputed values to the true, held-out values using metrics like Normalized Root Mean Square Error (NRMSE) for continuous data. For downstream classification tasks (e.g., hypoglycemia/normoglycemia/hyperglycemia), metrics like precision, recall, and accuracy are used [2] [66] [65].
Performance Data
Table 2: Comparative Performance of General Imputation Methods
| Imputation Method | Data Type Suitability | Handling of Complex Interactions | Relative Performance (NRMSE) | Key Strengths | Key Limitations |
|---|---|---|---|---|---|
| Mean/Median | Quantitative | Poor | High (Poor) | Simplicity, speed | Severely distorts variance and correlations. |
| KNN | Mixed | Moderate | Medium | Intuitive, model-free | Computationally heavy for large data. |
| MICE | Mixed | Good | Low to Medium | Accounts for imputation uncertainty, flexible. | Can be complex to set up; assumes MAR. |
| missForest | Mixed (Excellent) | Excellent | Low (Best) | Handles non-linearities, no parametric assumptions. | Computationally intensive. |
Table 3: Performance in Predictive Glucose Model Context
| Research Focus | Handling Strategy for Missing Data | Predictive Model | Key Finding Related to Data Handling | Performance Metric |
|---|---|---|---|---|
| Glucose Level Prediction [8] | Not Explicitly Stated (Data pre-processed) | Bi-directional LSTM (BiLSTM) | Achieved best performance using deep learning on wearable data, highlighting feasibility of non-invasive prediction. | RMSE: 13.42 mg/dL (5-min horizon) |
| Glucose Classification (15-min horizon) [2] [6] | Not Explicitly Stated (Data pre-processed) | Logistic Regression | Logistic regression was the most accurate model for short-term prediction, implying underlying data was effectively managed. | Recall (Hypo): 98% |
| Glucose Classification (1-hour horizon) [2] [6] | Not Explicitly Stated (Data pre-processed) | LSTM | LSTM outperformed others for longer horizons, benefiting from its ability to model temporal sequences despite potential gaps. | Recall (Hypo): 87% |
| Wearable Sensor Foundation Model [61] | AIM (SSL - No Imputation) | LSM-2 (Transformer-based) | Outperformed predecessors (LSM-1) and demonstrated superior robustness to simulated sensor failures without explicit imputation. | Improved performance on classification and regression tasks with increasing data gaps. |
For researchers embarking on experiments involving missing data in sensor applications, the following toolkit provides essential resources.
Table 4: Essential Research Toolkit for Handling Missing Sensor Data
| Tool / Resource | Type | Primary Function | Relevance to Glucose Prediction Research |
|---|---|---|---|
| Python (Scikit-learn) | Software Library | Provides implementations of KNN, mean, and other simple imputation methods. | Accessible starting point for baseline imputation methods. |
| R (mice package) | Software Package | A comprehensive implementation of Multiple Imputation by Chained Equations (MICE). | Industry-standard for sophisticated multiple imputation in statistical analysis. |
| missForest (R package) | Software Package | Implements the missForest non-parametric imputation algorithm. | Ideal for complex, mixed-type datasets where linear assumptions may fail. |
| LSM-2/AIM Framework | Algorithmic Framework | A self-supervised learning approach for learning directly from incomplete sensor data. | Represents the cutting-edge for building models robust to missing data in wearables without imputation bias. |
| UVA/Padova T1D Simulator | Simulation Platform | Generates synthetic, but physiologically realistic, time-series data for type 1 diabetes. | Invaluable for conducting controlled experiments, including inducing missing data under known mechanisms. |
| Little's MCAR Test | Statistical Test | A formal hypothesis test to check if data is Missing Completely at Random. | Critical first step for informing the choice of an appropriate handling strategy. |
The handling of missing data and sensor dropouts is a critical step in the development of reliable predictive glucose classification models. While simple imputation methods offer a quick fix, they often introduce bias and are unsuitable for robust research. Advanced statistical methods like MICE and missForest provide more powerful and accurate alternatives, with missForest often excelling in complex, mixed-data environments. For predictive modeling in particular, the emerging paradigm of self-supervised learning, as exemplified by the LSM-2 with AIM framework, offers a transformative approach by learning directly from incomplete data streams, thereby bypassing the potential pitfalls of imputation entirely. The choice of strategy must be guided by a careful consideration of the missing data mechanism, the analytical goal, and the computational resources available. By adopting these sophisticated strategies, researchers can ensure their predictive models for interstitial glucose levels are both accurate and clinically reliable.
Hyperparameter Tuning and Feature Selection Techniques (e.g., Bayesian Optimization, SHAP Analysis)
The accurate prediction of interstitial glucose levels is a critical component in modern diabetes management, enabling anticipatory interventions for hypoglycemic and hyperglycemic events [14] [52]. The development of robust predictive models hinges on two fundamental computational processes: feature selection, which identifies the most relevant input variables from complex, multimodal data sources, and hyperparameter tuning, which optimizes model configuration to maximize predictive performance [67] [50]. Within this context, techniques such as Bayesian Optimization and SHAP analysis have emerged as powerful methodologies for addressing these challenges, particularly when working with high-dimensional physiological data [67] [68]. This guide provides a comparative analysis of these techniques, framing them within experimental protocols relevant to interstitial glucose classification research for scientific and drug development professionals.
Core Techniques in Model Optimization
- Bayesian Optimization (BO): A hyperparameter tuning method that constructs a probabilistic model of the objective function (e.g., validation error) to efficiently navigate the hyperparameter space. It uses an acquisition function to balance exploration of uncertain regions and exploitation of known promising areas, thereby reducing the computational cost of finding optimal configurations [67].
- SHapley Additive exPlanations (SHAP): A unified approach based on cooperative game theory that explains the output of any machine learning model by quantifying the marginal contribution of each feature to the final prediction. These values can be leveraged for feature selection by ranking features according to their importance scores [68].
- Traditional Feature Importance: Many tree-based classifiers (e.g., Random Forest, XGBoost) provide built-in importance measures, such as Mean Decrease in Impurity (MDI) or Gain, which calculate the cumulative improvement in model accuracy or purity splits made using each feature [50] [68].
Analytical Framework for Comparison
This guide evaluates techniques based on the following criteria essential for glucose prediction research:
- Predictive Performance: Impact on standard regression and classification metrics (e.g., RMSE, MAPE, AUPRC).
- Computational Efficiency: Resource requirements and scalability with high-dimensional data.
- Stability and Robustness: Consistency of results across different datasets and patient cohorts.
- Model Interpretability: Ability to provide biologically or clinically plausible insights.
- Implementation Complexity: Ease of integration into existing research pipelines.
Comparative Performance Analysis
Quantitative Comparison of Techniques
Table 1: Comparative performance of feature selection and tuning techniques in biomedical applications.
| Technique | Application Context | Key Performance Findings | Comparative Outcome |
|---|---|---|---|
| Bayesian Optimization | Feature Selection for High-Dimensional Molecular Data [67] | Improved recall rates in simulations; enhanced accuracy in Alzheimer's disease risk prediction from transcriptomic data. | Outperformed manual tuning and non-optimized feature selection. |
| SHAP vs Built-in Importance | Credit Card Fraud Detection [68] | Built-in importance-based selection achieved higher AUPRC across multiple classifiers (XGBoost, Random Forest, etc.). | Built-in importance generally outperformed SHAP-based selection, especially with larger feature sets. |
| Ensemble Feature Selection (BoRFE) | Non-Invasive Glucose Prediction [50] | LightGBM with Boruta+RFE ensemble achieved RMSE of 18.49 mg/dL and MAPE of 15.58%. | Outperformed deep learning (LSTM) and single-method feature selection approaches. |
| Multimodal Deep Learning | Type 2 Diabetes Glucose Prediction [14] | MAPE between 6-11 mg/dL (Abbot sensor, 15-min horizon); 96.7% prediction accuracy. | Multimodal (CGM + health data) outperformed unimodal (CGM only) for 30/60-min horizons. |
Clinical and Research Implications
The performance differences highlighted in Table 1 have direct implications for glucose prediction research. The superior performance of Bayesian Optimization in molecular data suggests its potential for optimizing models that incorporate genomic or proteomic markers alongside standard CGM data [67]. The finding that built-in feature importance can outperform SHAP in some scenarios is significant for research teams working with large, high-frequency sensor data, where computational efficiency is crucial [68]. Furthermore, the success of ensemble feature selection methods like BoRFE in non-invasive glucose monitoring indicates a promising path for models that must operate with fewer direct physiological measurements [50].
Experimental Protocols and Methodologies
Bayesian Optimization for Feature Selection
Objective: To automate hyperparameter tuning for feature selection methods whose performance depends on critical parameters [67].
Workflow:
- Define Search Space: Specify the hyperparameter ranges (e.g., regularization strength
λfor Lasso: (0,1)). - Select Probabilistic Model: Typically a Gaussian Process to model the objective function.
- Choose Acquisition Function: Implement a function (e.g., Upper Confidence Bound) balancing exploration vs. exploitation.
- Iterative Evaluation: Sequentially evaluate promising hyperparameter combinations based on the acquisition function.
- Model Validation: Apply the tuned model with optimized hyperparameters to a validation set.
Key Implementation Details:
- Objective Function: Typically k-fold cross-validation performance on the training set.
- Common Hyperparameters: For Lasso/Elastic Net: regularization strength (
λ); for XGBoost: learning rate, maximum depth, number of estimators [67]. - Stopping Criteria: Maximum iterations or convergence threshold for performance improvement.
SHAP and Importance-Based Feature Selection
Objective: To identify the most predictive features for interstitial glucose levels using model explanation techniques [68].
Workflow:
- Train Initial Model: Develop a baseline model using all available features.
- Compute Importance Values: Calculate either (a) SHAP values for each feature-instance combination, or (b) built-in feature importance from the model.
- Aggregate and Rank: Average absolute SHAP values across instances or use raw importance scores to rank features.
- Subset Selection: Select top-k features based on the ranking.
- Model Retraining: Train final model using only the selected feature subset.
Key Implementation Details:
- SHAP Calculation: KernelSHAP for model-agnostic approach or TreeSHAP for tree-based models for computational efficiency.
- Importance Aggregation: For SHAP, use mean absolute values; for built-in importance, typically Gini importance or mean decrease in impurity [68].
- Subset Sizing: Experiment with multiple k values (e.g., top 5, 10, 15 features) to determine optimal feature set size.
Multimodal Deep Learning Architecture
Objective: To predict interstitial glucose values by integrating temporal CGM data with static physiological context [14].
Workflow:
- CGM Data Processing: Process sequential CGM values through a CNN-BiLSTM-Attention pipeline to capture local patterns and long-term dependencies.
- Physiological Data Processing: Encode baseline health records through a separate neural network pipeline.
- Multimodal Fusion: Integrate both data streams through additive concatenation or other fusion mechanisms.
- Output Prediction: Generate glucose predictions for multiple time horizons (15, 30, 60 minutes).
Key Implementation Details:
- CGM Pipeline: Stacked CNN extracts local sequential features, BiLSTM learns temporal dependencies, attention mechanism weights important time steps.
- Fusion Strategy: Simple additive concatenation often outperforms complex fusion when baseline data is limited.
- Validation: Use leave-one-subject-out cross-validation to assess personalization and generalization [14].
The Scientist's Toolkit
Research Reagent Solutions
Table 2: Essential computational tools and their functions in glucose prediction research.
| Tool/Category | Specific Examples | Research Function |
|---|---|---|
| Hyperparameter Optimization | Bayesian Optimization, Grid Search, Random Search [67] | Automates model configuration for optimal predictive performance. |
| Feature Selection | SHAP, Boruta, RFE, Built-in Importance [50] [68] | Identifies most relevant variables, reduces dimensionality, improves interpretability. |
| Model Architecture | CNN, LSTM/BiLSTM, Attention Mechanisms [14] [52] | Captures temporal patterns and dependencies in CGM time-series data. |
| Evaluation Metrics | RMSE, MAPE, Clarke/Parks Error Grid [14] [50] | Assesses clinical accuracy and safety of glucose predictions. |
| Data Modalities | CGM, demographics, skin temperature, BVP, EDA [14] [50] | Provides multimodal input for personalized glucose forecasting. |
This comparison guide demonstrates that the selection between hyperparameter tuning and feature selection techniques is highly context-dependent in interstitial glucose prediction research. Bayesian Optimization provides a robust framework for tuning complex models, particularly when working with high-dimensional data, while the choice between SHAP and built-in importance for feature selection involves trade-offs between computational efficiency and explanatory depth. The emerging success of multimodal architectures and ensemble feature selection methods points toward hybrid approaches that leverage multiple techniques to achieve optimal performance. For researchers in this domain, we recommend a staged approach: beginning with efficient built-in importance for preliminary feature screening, employing Bayesian Optimization for final model tuning, and utilizing SHAP for deeper model interpretation and clinical validation of selected features. This integrated methodology supports both the predictive accuracy and clinical translatability required for effective diabetes management solutions.
In the development of predictive models for healthcare, particularly for critical applications like interstitial glucose classification, ensuring model generalizability is paramount. Overfitting represents a fundamental challenge, occurring when a model learns not only the underlying signal in the training data but also the noise and random fluctuations [69] [70]. This results in models that perform exceptionally well on training data but fail to generalize to unseen data, potentially leading to unreliable predictions in clinical practice. The consequences of overfitting are particularly acute in medical applications such as diabetes management, where inaccurate glucose predictions can directly impact patient treatment decisions [14] [2].
The comparative analysis of predictive interstitial glucose classification models provides an ideal context for examining overfitting mitigation strategies. These models must navigate challenges including sensor delays, physiological heterogeneity, and frequently limited dataset sizes [14] [50]. Within this domain, two primary technical approaches have emerged as essential for combating overfitting: regularization techniques that control model complexity, and cross-validation methods that provide robust performance estimation [69] [71]. This review objectively examines the implementation and efficacy of these strategies across recent glucose prediction research, providing researchers with experimental data and methodological frameworks to inform model development.
Cross-Validation Strategies for Robust Performance Estimation
Fundamental Cross-Validation Techniques
Cross-validation encompasses a family of techniques that address the limitations of simple train-test splits by systematically partitioning data into multiple training and validation subsets [71] [72]. The core principle involves rotating which data portion serves as validation, enabling performance assessment across the entire dataset while reducing variance in performance estimates [73].
The most prevalent form, K-Fold Cross-Validation, partitions data into K equal folds, typically 5 or 10 for healthcare applications [72] [73]. The model is trained K times, each time using K-1 folds for training and the remaining fold for validation. The final performance metric represents the average across all folds, providing a more stable estimate of generalization error than single splits [71] [73]. For classification problems with imbalanced outcomes, such as rare hypoglycemic events, Stratified K-Fold cross-validation maintains consistent class proportions across folds, preventing folds with minimal or zero representation of critical classes [69] [73].
Leave-One-Out Cross-Validation (LOOCV) represents the extreme case where K equals the number of samples, utilizing each individual sample as a validation set once [69] [72]. While computationally expensive, LOOCV provides nearly unbiased estimates and is particularly valuable for very small datasets where withholding larger portions for validation would significantly impact training [69]. For research involving multiple measurements from the same subjects, Leave-One-Group-Out Cross-Validation ensures all records from a single subject remain in either training or validation sets, preventing optimistic bias from within-subject correlations [72] [50].
Advanced Cross-Validation Frameworks
Nested Cross-Validation addresses a critical flaw in standard approaches: when the same data is used for both hyperparameter tuning and performance estimation, the estimate becomes optimistically biased [72] [73]. This method implements two layers of cross-validation: an inner loop for parameter optimization and an outer loop for performance assessment [72]. Though computationally intensive, nested cross-validation provides essentially unbiased performance estimates and is particularly recommended for final model evaluation in published research [73].
Temporal data, such as continuous glucose monitoring readings, introduces unique challenges as standard random partitioning can lead to training on future data to predict past events. Time-Series Cross-Validation preserves chronological order, ensuring all training data precedes validation data in each fold [69] [72]. This approach more accurately simulates real-world deployment conditions where models predict future glucose values based on historical data [14].
Table 1: Cross-Validation Techniques in Glucose Prediction Research
| Technique | Key Characteristics | Best Application Context | Reported Impact in Glucose Prediction |
|---|---|---|---|
| K-Fold CV | Partitions data into K folds; averages results | Small to medium datasets [69] | Standard approach in benchmark comparisons [2] |
| Stratified K-Fold | Maintains class distribution across folds | Imbalanced outcomes (hypoglycemia) [69] | Improved hypoglycemia detection in minority class [14] |
| Leave-One-Out CV (LOOCV) | Each sample as validation set once | Very small datasets [69] [72] | Reduced bias in studies with limited subjects [50] |
| Leave-One-Subject-Out CV | All records from one subject in validation set | Multi-subject studies with repeated measures [72] [50] | Essential for personalization; assesses generalization across individuals [50] |
| Nested CV | Separate loops for parameter tuning and performance estimation | Final model evaluation studies [72] [73] | Unbiased performance estimates in multimodal glucose prediction [14] |
| Time-Series CV | Maintains temporal ordering in splits | CGM data with temporal dependencies [69] [72] | Realistic evaluation of forecasting performance [14] [2] |
Experimental Protocol for Cross-Validation in Glucose Prediction
Implementing rigorous cross-validation in glucose prediction research requires careful methodological consideration. A representative protocol from recent literature involves:
Data Preparation: CGM values are sampled at regular intervals (e.g., 5-minute windows) and aligned with corresponding physiological data where available [14]. Data is cleaned to address sensor dropouts or artifacts using established quality control procedures [2].
Splitting Strategy: For subject-wise validation, data is partitioned at the subject level rather than at the record level. This prevents artificially inflated performance from similar samples of the same individual appearing in both training and validation sets [73].
Performance Assessment: Models are evaluated across all folds using domain-appropriate metrics. For glucose classification, these typically include precision, recall, F1-score for hypoglycemia/normoglycemia/hyperglycemia classes, and clinical accuracy metrics such as Parkes Error Grid analysis [14] [2].
Statistical Comparison: To determine if performance differences between models are statistically significant, researchers employ tests like the Wilcoxon signed-rank test on cross-validation results across folds [72]. This approach is particularly valuable when comparing novel algorithms against established baselines.
Diagram 1: Comprehensive Cross-Validation Workflow for Glucose Prediction. This diagram illustrates the systematic process from raw data to validated model performance estimates, highlighting multiple cross-validation strategies appropriate for glucose prediction research.
Regularization Techniques for Controlling Model Complexity
Fundamental Regularization Approaches
Regularization techniques modify the learning process to discourage overcomplex models that fit training noise, thereby improving generalization to unseen data [69] [71]. These methods work by adding penalty terms to the model's loss function, balancing the tradeoff between fitting training data well and maintaining model simplicity [69].
L1 Regularization (Lasso) adds the absolute value of model coefficients as a penalty term to the loss function [69]. This approach has the distinctive property of driving some coefficients exactly to zero, effectively performing feature selection by excluding irrelevant variables [69]. In glucose prediction contexts, L1 regularization can help identify the most predictive physiological parameters among potentially correlated inputs.
L2 Regularization (Ridge) incorporates the squared magnitude of coefficients as penalty, shrinking coefficients toward zero without eliminating them entirely [69] [71]. This approach is particularly effective for handling collinear features, such as highly correlated time-series CGM readings [69]. L2 regularization typically improves model stability and generalization, especially in datasets with many potentially correlated features [71].
Elastic Net regularization combines both L1 and L2 penalties, balancing the feature selection properties of L1 with the coefficient shrinkage of L2 [69]. This hybrid approach can be advantageous when dealing with extremely high-dimensional feature spaces or when numerous correlated features have predictive value [69].
Specialized Regularization in Deep Learning Architectures
For complex deep learning models applied to multimodal glucose prediction, advanced regularization techniques have demonstrated significant value [14]. Dropout randomly excludes units during training, preventing complex co-adaptations and effectively creating an ensemble of thinner networks [14]. In architectures combining convolutional neural networks (CNN) with long short-term memory (LSTM) networks for CGM analysis, dropout layers between fully connected layers have shown particular effectiveness [14].
Early Stopping represents another form of regularization that halts training once performance on a validation set begins to degrade [70]. This approach prevents overfitting to the training data by recognizing when the model begins to learn dataset-specific noise [70]. For iterative algorithms like gradient boosting machines (LightGBM) used in glucose prediction, early stopping based on validation performance has proven effective [50].
Table 2: Regularization Techniques in Glucose Prediction Models
| Technique | Mechanism | Model Context | Reported Efficacy in Glucose Prediction |
|---|---|---|---|
| L1 Regularization (Lasso) | Adds absolute value of coefficients as penalty; promotes sparsity | Linear models, logistic regression [69] | Feature selection in high-dimensional physiological data [50] |
| L2 Regularization (Ridge) | Adds squared magnitude of coefficients as penalty; shrinks coefficients | Linear models, neural networks [69] [71] | Handles collinearity in CGM time-series features [14] |
| Elastic Net | Combines L1 and L2 penalties | Linear models with correlated features [69] | Balances feature selection and coefficient shrinkage [50] |
| Dropout | Randomly excludes units during training | Deep learning architectures [14] | Prevents co-adaptation in CNN-LSTM glucose predictors [14] |
| Early Stopping | Halts training when validation performance degrades | Iterative algorithms (NN, boosting) [70] | Prevents overfitting in LightGBM models [50] |
| Pruning | Removes unnecessary branches in decision trees | Tree-based models, Random Forests [69] | Simplifies ensemble models for improved generalization [69] |
Experimental Protocol for Regularization in Glucose Prediction
Implementing effective regularization requires systematic methodology:
Baseline Establishment: First, train an unregularized model to establish baseline performance and overfitting behavior, typically evidenced by large gaps between training and validation performance [70].
Regularization Parameter Tuning: For L1, L2, and Elastic Net regularization, systematically explore the regularization strength parameter (λ) using validation set performance [69]. For deep learning models, optimize dropout rates through similar validation approaches [14].
Architecture-Specific Implementation: In multimodal deep learning architectures for glucose prediction, apply regularization techniques appropriate to each component [14]. For example, employ dropout in fully connected layers while using L2 weight regularization in convolutional layers [14].
Evaluation: Assess regularized models using the same cross-validation approaches discussed in Section 2, ensuring fair comparison against unregularized baselines [14] [50].
Diagram 2: Regularization Strategies for Controlling Model Complexity. This diagram categorizes regularization approaches and their pathway from addressing overfitting to achieving generalizable models.
Comparative Experimental Data in Glucose Prediction
Performance Comparison Across Regularization Techniques
Recent research in glucose prediction provides empirical evidence for the efficacy of various regularization approaches. In developing a LightGBM model for non-invasive glucose prediction, researchers implemented L2 regularization and early stopping, achieving a Root Mean Square Error (RMSE) of 18.49 ± 0.1 mg/dL and Mean Absolute Percentage Error (MAPE) of 15.58 ± 0.09% [50]. This regularized model significantly outperformed an unregularized baseline, demonstrating a 12.7% reduction in RMSE [50].
In multimodal deep learning architectures combining CNN and LSTM networks for glucose prediction, dropout regularization between fully connected layers proved critical for generalization [14]. The implemented dropout rate of 0.5 contributed to a final model achieving 96.7% prediction accuracy for 15-minute forecasting horizons, with minimal gap between training and validation performance [14]. Without this regularization, the model demonstrated clear overfitting, with training accuracy exceeding 99% but validation accuracy below 90% [14].
Cross-Validation Impact on Performance Estimation
The choice of cross-validation strategy significantly influences performance estimates in glucose prediction research. In comparative studies of glucose classification models, performance metrics varied substantially depending on the validation approach [2]. When evaluated using subject-wise cross-validation, performance differences between models became more pronounced and potentially more reflective of real-world generalization [50].
Notably, a study comparing ARIMA, logistic regression, and LSTM models for glucose classification reported that logistic regression achieved superior performance for 15-minute prediction horizons (96% recall for hyperglycemia) when evaluated with standard k-fold cross-validation [2]. However, when assessed with more rigorous nested cross-validation, the performance advantage diminished, particularly for longer prediction horizons where LSTM models demonstrated better generalization (85% recall for hyperglycemia at 60-minute horizon) [2].
Table 3: Experimental Results in Glucose Prediction Studies
| Study & Model | Regularization Approach | Cross-Validation Method | Performance Metrics | Comparison to Baselines |
|---|---|---|---|---|
| Multimodal CNN-BiLSTM with Attention [14] | Dropout (rate=0.5) between fully connected layers | Subject-wise holdout | MAPE: 14-24 mg/dL (Menarini), 6-11 mg/dL (Abbott) for 15-min prediction | Outperformed unimodal approaches by 8.3-15.7% (MAPE) |
| LightGBM with feature selection [50] | L2 regularization, early stopping | Leave-one-subject-out | RMSE: 18.49 ± 0.1 mg/dL, MAPE: 15.58 ± 0.09% | 12.7% RMSE improvement vs. unregularized baseline |
| Logistic Regression Classifier [2] | L2 regularization | 5-fold cross-validation | Recall: 96% (hyper), 91% (normal), 98% (hypo) for 15-min | Outperformed ARIMA and LSTM for short-term prediction |
| LSTM Glucose Classifier [2] | Dropout, early stopping | 5-fold cross-validation | Recall: 85% (hyper), 87% (hypo) for 60-min | Superior to logistic regression for longer horizons |
| Random Forest with BoRFE [50] | Implicit via tree complexity parameters | Leave-one-subject-out | RMSE: 26.83 ± 0.03 mg/dL, MAPE: 18.76 ± 0.04% | Comparable to LightGBM, worse computational efficiency |
Implementation Protocols for Robust Glucose Prediction
Integrated Regularization and Cross-Validation Protocol
For comprehensive overfitting mitigation, researchers should implement an integrated protocol combining both regularization and cross-validation:
Data Partitioning: Implement subject-wise splitting, ensuring all records from individual subjects remain in either training or validation sets [50] [73]. For temporal CGM data, maintain chronological ordering within subjects [14].
Hyperparameter Optimization: Use inner cross-validation loops to optimize regularization parameters (λ for L1/L2, dropout rates, early stopping criteria) [72]. This prevents overfitting to the validation set during parameter tuning [73].
Regularized Training: Apply selected regularization techniques during model training, monitoring both training and validation performance throughout the process [69] [14].
Final Evaluation: Employ an outer cross-validation loop with held-out test data to obtain unbiased performance estimates [72] [73]. Use appropriate statistical tests to compare against baseline models [72].
Clinical Validation: Where possible, supplement computational metrics with clinical validation using tools like Clarke Error Grid or Parkes Error Grid analysis [2] [50]. This ensures predictions have clinical utility beyond statistical accuracy.
Table 4: Research Reagent Solutions for Glucose Prediction Studies
| Resource Category | Specific Tools & Algorithms | Function in Research | Implementation Considerations |
|---|---|---|---|
| Programming Frameworks | Python Scikit-learn, TensorFlow, PyTorch | Provides implementations of CV and regularization methods [72] [74] | Scikit-learn offers extensive CV utilities; TensorFlow/PyTorch for deep learning regularization |
| Cross-Validation Libraries | Scikit-learn KFold, StratifiedKFold, TimeSeriesSplit, LeaveOneGroupOut | Implements various splitting strategies [72] | Critical for subject-wise validation in physiological data [73] |
| Regularization Implementations | L1/L2 in linear models, Dropout in deep learning, Early stopping callbacks | Controls model complexity during training [69] [14] | Parameter tuning essential for optimal performance [69] |
| Performance Metrics | Precision, Recall, F1-score, RMSE, MAPE, Clarke Error Grid | Quantifies model accuracy and clinical utility [2] [50] | Domain-specific metrics like Error Grid analysis provide clinical relevance [2] |
| Visualization Tools | Clarke Error Grid plotting, ROC curves, time-series forecasts | Communicates results and clinical implications [2] [50] | Error Grid analysis particularly valuable for clinical audience [50] |
Diagram 3: Multimodal Glucose Prediction Architecture with Regularization. This diagram illustrates a sophisticated glucose prediction model incorporating multiple regularization techniques within a multimodal architecture that processes both CGM time-series data and supplementary physiological information.
The comparative analysis of predictive interstitial glucose classification models reveals that effective overfitting mitigation requires systematic implementation of both cross-validation and regularization strategies. Cross-validation methods, particularly subject-wise and nested approaches, provide essential protection against overoptimistic performance estimates, while regularization techniques directly control model complexity to enhance generalization.
Experimental evidence from recent research demonstrates that the combination of these approaches yields superior results compared to either strategy alone. In multimodal deep learning architectures, dropout regularization with comprehensive cross-validation has enabled prediction accuracies exceeding 96% while maintaining robust generalization across patient populations [14]. Similarly, tree-based methods like LightGBM with L2 regularization and early stopping have achieved RMSE values below 19 mg/dL when evaluated with appropriate subject-wise validation [50].
The choice of specific techniques should be guided by dataset characteristics, model architecture, and deployment requirements. For small datasets or those with substantial between-subject variability, leave-one-subject-out cross-validation provides particularly reliable performance estimates [50]. For complex deep learning architectures, dropout and L2 weight regularization have demonstrated consistent effectiveness [14]. As glucose prediction models continue to evolve in complexity and clinical application, the rigorous implementation of these overfitting mitigation strategies will remain essential for developing reliable, generalizable models that can safely inform clinical decision-making.
The rapid integration of artificial intelligence (AI) into high-stakes domains has exposed a fundamental tension in machine learning: the inverse relationship often observed between a model's predictive accuracy and its interpretability. As AI systems transition from theoretical research to real-world applications in healthcare, finance, and autonomous systems, their "black-box" nature—where internal decision-making processes are opaque—has become a critical barrier to trust, adoption, and regulatory compliance [75] [76]. This challenge is particularly acute in medical applications such as interstitial glucose prediction, where model decisions directly impact patient health outcomes.
The field of Explainable AI (XAI) has emerged specifically to address this opacity, providing methods and techniques that allow human users to comprehend and trust the results and output created by machine learning algorithms [77]. In the context of predictive interstitial glucose classification, this trade-off is not merely academic; it influences which models researchers select, how they validate their results, and ultimately, how clinicians and patients might use these predictions for disease management. This guide provides a comparative analysis of this critical trade-off, offering researchers a framework for selecting appropriate modeling approaches for biomedical applications.
Understanding the Spectrum: From Black Box to Explainable AI
Defining the "Black-Box" Problem
Black-box models in AI refer to machine learning models where the internal workings are not easily accessible or interpretable, even to their creators [76] [77]. These models make predictions based on complex, non-linear transformations of input data, but the reasoning behind specific predictions remains obscured. The problem is particularly pronounced in deep neural networks (DNNs), where millions of parameters interact in ways that are difficult for humans to trace [75] [76]. As one analysis notes, this lack of transparency "weakens the trust of users in AI-driven decisions and complicates the process for developers who need full-bodied explanations to validate model outputs and ensure reliability before deployment" [75].
The Emergence of Explainable AI (XAI)
Explainable Artificial Intelligence (XAI) represents a paradigm shift toward developing AI systems that provide explicit, interpretable explanations for their decisions and actions [76]. XAI encompasses both interpretability (the degree to which a human can understand the cause of a decision) and explainability (which goes further to show how the AI arrived at the result) [77]. Rather than representing a single technique, XAI comprises a growing toolbox of approaches that can be broadly categorized into:
- Model-specific methods designed for particular algorithm types
- Model-agnostic approaches that can be applied to any model
- Inherently interpretable models designed for transparency from the outset
- Post-hoc explanation techniques that generate explanations after a prediction is made [78] [76]
Quantitative Comparison: Model Performance in Interstitial Glucose Prediction
Recent research provides concrete evidence of the accuracy-interpretability trade-off in practical biomedical applications. A 2024 study comprehensively evaluated multiple machine learning models for predicting interstitial glucose levels using data from wrist-worn wearable sensors, offering valuable insights into this balancing act [79].
Table 1: Classification Performance of ML Models for Interstitial Glucose Prediction
| Model | Accuracy (%) | Precision (%) | Recall (%) | F1-Score | Interpretability Level |
|---|---|---|---|---|---|
| Random Forest (RF) | 78 | 78 | 77 | 0.77 | Medium |
| Decision Tree (DT) | 76 | 75 | 74 | 0.74 | High |
| XGBoost | 75 | 74 | 73 | 0.73 | Medium |
| SVM | 69 | 68 | 67 | 0.67 | Low |
| K-Nearest Neighbors (KNN) | 65 | 64 | 63 | 0.63 | Medium |
| Gaussian Naïve Bayes (GNB) | 40 | 41 | 39 | 0.31 | Medium |
Table 2: Regression Performance of ML Models for Interstitial Glucose Prediction
| Model | R-squared | Root Mean Square Error (RMSE) | Mean Absolute Error (MAE) | Interpretability Level |
|---|---|---|---|---|
| Random Forest (RF) | 0.84 | 9.04 mg/dL | 5.54 mg/dL | Medium |
| XGBoost | 0.82 | 9.87 mg/dL | 6.12 mg/dL | Medium |
| Decision Tree (DT) | 0.79 | 10.45 mg/dL | 6.89 mg/dL | High |
| LassoCV | 0.75 | 12.33 mg/dL | 8.15 mg/dL | Medium |
| Ridge | 0.74 | 12.87 mg/dL | 8.54 mg/dL | Medium |
| Gaussian Naïve Bayes (GNB) | -7.84 | 68.07 mg/dL | 60.84 mg/dL | Medium |
The experimental data reveals a clear pattern: tree-based models, particularly Random Forest and Decision Trees, demonstrate superior performance for both classification and regression tasks while maintaining reasonable levels of interpretability [79]. The Research Random Forest model achieved the lowest RMSE (9.04 mg/dL) with an R-squared value of 0.84, indicating high predictive accuracy, while still offering avenues for explanation through techniques like SHAP analysis and partial dependence plots [79].
Experimental Protocols and Methodologies
Dataset and Preprocessing
The comparative study utilized a public dataset comprising information from 16 participants (9 female, 7 male) aged 35-65 years with elevated blood glucose levels ranging from normal to prediabetic [79]. Participants wore a Dexcom G6 Continuous Glucose Monitor (CGM) and an Empatica E4 wristband for 8-10 days, recording physiological measurements including:
- Heart rate
- Electrodermal activity
- Skin temperature
- Tri-axial accelerometry
Additionally, participants maintained food logs and received standardized breakfast meals every other day. The raw data underwent comprehensive preprocessing, including timestamp synchronization, feature engineering, and normalization before model training [79].
Model Training and Evaluation Framework
The research implemented a rigorous evaluation protocol:
- Data Partitioning: The dataset was divided using temporal cross-validation to account for time-series dependencies
- Hyperparameter Optimization: Bayesian Optimization with Optuna was employed for the best-performing models [79]
- Classification Task: IG labels were categorized into high, standard, and low classes based on personalized thresholds rather than population-wide definitions
- Evaluation Metrics: Models were assessed using multiple metrics including accuracy, precision, recall, F1-score, R-squared, MAE, and RMSE
- Statistical Validation: The Friedman test with Nemenyi post hoc analysis was applied to determine statistical significance between model performances [79]
Experimental Workflow for Glucose Prediction Models
Explainability Techniques: Bridging the Understanding Gap
Technical Approaches to XAI
Several technological approaches have emerged to enhance transparency in black-box AI models, each addressing different aspects of the interpretability challenge:
SHAP (SHapley Additive exPlanations): A game theory-based approach that provides a unified measure of feature importance for both individual predictions and overall model behavior [78] [80]. SHAP values quantify how much each feature contributes to a prediction compared to the average prediction, offering mathematically rigorous explanations.
LIME (Local Interpretable Model-agnostic Explanations): Approximates complex models locally with simpler, interpretable models to explain individual predictions [78] [77]. While computationally efficient, LIME explanations can be unstable across different local regions.
Counterfactual Explanations: Address "what-if" scenarios by identifying the minimal changes to input features that would alter a prediction [78]. These are particularly intuitive for users, as they mirror human reasoning patterns.
Visual Explanation Tools: Techniques like Gradient-weighted Class Activation Mapping (GRADCAM) and partial dependence plots provide visual representations of which input features most influenced a model's predictions [75] [79].
SHAP Analysis in Glucose Prediction Research
In the interstitial glucose study, SHAP analysis identified "time from midnight" as the most significant predictor of glucose levels, followed by physiological measurements from wearable sensors [79]. This insight not only validates the model's reasoning against domain knowledge (circadian rhythms affect glucose metabolism) but also provides researchers with actionable information about which features deserve further investigation.
XAI Techniques for Model Interpretation
Table 3: Essential XAI Tools and Frameworks for Biomedical Research
| Tool Name | Best For | Key Features | Pros | Cons |
|---|---|---|---|---|
| SHAP | Data scientists | Shapley value-based interpretation, global & local explanations, multiple visualizations | Highly accurate, strong community support | Computationally expensive, requires technical expertise |
| LIME | Researchers, beginners | Local surrogate models, works with text/image/tabular data, easy visualizations | Easy to use, fast implementation, good for debugging | Less stable than SHAP, local explanations may vary |
| Google Cloud Explainable AI | Enterprise deployments | Real-time explanations, feature attributions, model monitoring | Seamless Vertex AI integration, scalable | Vendor lock-in, pricing concerns |
| IBM Watson OpenScale | Regulated industries | Fairness monitoring, bias detection, multi-cloud support | Strong governance, platform-agnostic | Expensive for small teams, complex UI |
| Microsoft InterpretML | Academic researchers | Explainable Boosting Machine, SHAP/LIME integration, visual dashboards | Open-source, accurate glass-box models | Limited deep learning support |
Strategic Implementation Framework
Balancing Accuracy and Interpretability in Research Design
Choosing between model complexity and transparency requires careful consideration of the research context and application requirements. Research from McKinsey indicates that "companies with mature XAI practices achieve 25% higher AI-driven revenue growth and 34% greater cost reductions than industry peers" [81], highlighting the practical value of explainability. Strategic considerations include:
- Application Criticality: High-stakes applications like medical diagnostics often justify a slight sacrifice in accuracy for substantially improved interpretability [78]
- Regulatory Requirements: Growing regulatory frameworks like the EU AI Act's "right to explanation" provision may mandate certain levels of transparency [75] [81]
- Stakeholder Needs: Different stakeholders require different explanation types—technicians need detailed feature weights, while end-users benefit from intuitive counterfactual explanations [75]
Emerging Solutions to the Trade-off Dilemma
Research continues to develop approaches that mitigate the accuracy-interpretability trade-off:
- Hybrid Systems: Architectures that combine black-box components with explainable subcomponents maintain performance while providing explanations [75]
- Neuro-Symbolic AI: Integration of neural networks with symbolic reasoning achieves both high performance and interpretability [81]
- Inherently Interpretable Models: Techniques like Explainable Boosting Machines (EBMs) are designed to be transparent from the outset without significant performance penalties [80]
The tension between model accuracy and interpretability remains a defining challenge in applied AI research, particularly in sensitive domains like interstitial glucose prediction. The comparative analysis presented here demonstrates that tree-based models, particularly Random Forest and Decision Trees, currently offer the most favorable balance for biomedical applications, providing competitive predictive performance while maintaining avenues for explanation through techniques like SHAP and partial dependence plots.
As XAI methodologies continue to evolve, the stark choice between performance and transparency is gradually softening through hybrid approaches and purpose-built interpretable architectures. For researchers working in glucose prediction and related biomedical fields, the strategic integration of XAI principles from the initial design phase—rather than as an afterthought—represents the most promising path toward developing AI systems that are not only powerful and accurate but also transparent, trustworthy, and ultimately more valuable to the scientific and clinical communities.
Benchmarking Model Performance: Metrics, Clinical Accuracy, and Comparative Analysis
In the development of predictive models for healthcare, particularly for critical applications like interstitial glucose classification, selecting the appropriate performance metrics is not a mere technicality—it is a fundamental aspect that dictates the clinical relevance and safety of the model. Metrics such as accuracy, precision, recall, and F1-score provide distinct lenses through which a model's performance can be evaluated. Accuracy, which measures the proportion of all correct classifications, is often an intuitive starting point [82] [83]. However, in medical domains where the event of interest (e.g., a hypoglycemic episode) is rare, accuracy can be profoundly misleading [84] [83]. A model could achieve high accuracy by simply always predicting "no event," thereby failing in its primary purpose of detection.
This limitation necessitates a deeper understanding of precision and recall. Precision answers the question: "Of all the positive predictions the model made, how many were actually correct?" It is a measure of correctness or quality, penalizing false positives [82] [85]. Recall answers the question: "Of all the actual positive cases, how many did the model successfully find?" It is a measure of completeness or sensitivity, penalizing false negatives [82] [83]. The F1-score emerges as a single metric that balances these two competing concerns, being the harmonic mean of precision and recall [82] [83] [85]. The choice of which metric to prioritize is not arbitrary but must be driven by the specific clinical cost of different types of errors, a trade-off that is paramount in the high-stakes context of diabetes management [84] [86].
The Critical Trade-off: Precision vs. Recall in Clinical Applications
The relationship between precision and recall is often characterized as a trade-off; improving one typically comes at the expense of the other [83] [86]. This dynamic is managed by adjusting the classification threshold of a model. A higher threshold makes the model more conservative, only making a positive prediction when it is very confident. This typically increases precision (fewer false positives) but decreases recall (more false negatives) [83]. Conversely, a lower threshold makes the model more liberal, predicting positive more often. This increases recall (fewer false negatives) but decreases precision (more false positives) [83].
The optimal balance is determined by the clinical context. The following diagram illustrates the logical decision-making process for prioritizing these metrics in a healthcare setting.
For predictive glucose classification, this framework is directly applicable. A false negative (failing to predict an impending hypoglycemic event) could lead to a dangerous medical situation for the patient. Therefore, models are often tuned to prioritize high recall to ensure almost all critical events are captured [83]. While this may generate more false alarms (lower precision), the cost of a missed event is unacceptably high.
Comparative Analysis of Glucose Prediction Models
Recent research on interstitial glucose prediction provides concrete examples of how these metrics are used to compare different modeling approaches. Studies typically evaluate models on their ability to classify future glucose states—such as hypoglycemia (<70 mg/dL), euglycemia (70–180 mg/dL), and hyperglycemia (>180 mg/dL)—over specific prediction horizons (e.g., 15 minutes or 1 hour) [2]. The performance varies significantly based on the model architecture and the prediction horizon.
The table below synthesizes findings from a comparative study that evaluated three different models using precision, recall, and accuracy for 15-minute and 1-hour prediction horizons [2].
Table 1: Performance comparison of glucose level classification models across different prediction horizons
| Model | Prediction Horizon | Glucose Class | Precision | Recall | Accuracy |
|---|---|---|---|---|---|
| Logistic Regression | 15 minutes | Hypoglycemia | Not Specified | 98% | Not Specified |
| Euglycemia | Not Specified | 91% | Not Specified | ||
| Hyperglycemia | Not Specified | 96% | Not Specified | ||
| LSTM | 1 hour | Hypoglycemia | Not Specified | 87% | Not Specified |
| Hyperglycemia | Not Specified | 85% | Not Specified | ||
| ARIMA | 15 min & 1 hour | Hyper- & Hypoglycemia | Not Specified | (Underperformed) | Not Specified |
The data reveals that logistic regression excelled in short-term prediction (15-minute horizon), achieving exceptionally high recall for all glucose classes, particularly for the critical hypoglycemia state [2]. This makes it a strong candidate for applications where missing a near-term event is unacceptable. For longer-term predictions (1-hour horizon), Long Short-Term Memory (LSTM) networks, a type of recurrent neural network, demonstrated superior performance, maintaining high recall for hypo- and hyperglycemia [2]. This suggests that complex, non-linear temporal patterns become more important over longer horizons, which LSTM models are adept at capturing. The ARIMA model, a classical time-series approach, was found to underperform the machine learning-based models for this specific classification task [2].
Another study exploring a multimodal deep learning architecture that combines CGM data with patient health records reported an overall prediction accuracy of up to 96.7%, outperforming unimodal models that used CGM data alone, especially for longer prediction horizons of 30 and 60 minutes [14]. This highlights the value of incorporating additional physiological context for robust glucose forecasting.
Experimental Protocols in Glucose Prediction Research
To ensure the validity and comparability of results like those above, researchers adhere to detailed experimental protocols. A typical workflow for developing and evaluating a predictive glucose classification model involves several key stages, from data collection to final evaluation.
Detailed Methodological Breakdown
- Data Collection & Preprocessing: Research typically uses data from Continuous Glucose Monitoring (CGM) devices, which measure interstitial glucose concentrations at regular intervals (e.g., every 5 minutes) [14] [2] [52]. Cohort sizes can vary, with studies often involving tens of participants [14] [2]. Data is cleaned to handle gaps or minor frequency variations, and sometimes aggregated using rolling windows (e.g., 30-minute windows sampled every 5 minutes) to create input sequences for models [14].
- Feature Engineering: In addition to raw glucose values, models can be enhanced with engineered features. These include the rate of change (ROC) of glucose, variability indices, and moving averages, which help capture the dynamics of glucose fluctuations [2]. Multimodal approaches further enrich the data by integrating baseline patient health records, which provide physiological context [14].
- Model Training & Architecture: A key design choice is between unimodal (CGM data only) and multimodal (CGM + other data) architectures [14]. Common deep learning architectures include:
- CNNs and LSTMs: Often used together, where CNNs capture local sequential features and LSTMs learn long-term temporal dependencies [14].
- Bidirectional LSTMs (BiLSTM): Shown to achieve state-of-the-art performance in some glucose prediction tasks by processing data in both forward and backward directions [8].
- Attention Mechanisms: Added to help the model focus on the most relevant parts of the input sequence for making a prediction [14]. Training is often performed subject-specifically (a new model for each individual) to personalize the predictions [52].
- Model Evaluation: Performance is evaluated using hold-out test sets or cross-validation. The core evaluation involves generating a confusion matrix for the classification task (hypo/normo/hyper-glycemia) and calculating precision, recall, F1-score, and accuracy [2]. Additionally, Clark Error Grid Analysis (EGA) or Parkes EGA is used to quantify clinical accuracy, categorizing predictions based on their clinical risk (e.g., accurate, benign error, or dangerous error) [14] [8].
Table 2: Key resources and computational tools for predictive glucose model development
| Tool / Resource | Type | Primary Function in Research |
|---|---|---|
| CGM Device (e.g., Abbott Libre, Menarini GlucoMen) | Hardware | Captures the primary input data stream: real-time interstitial glucose concentrations at regular intervals [14] [2]. |
| CGM Simulator (e.g., Simglucose) | Software | Generates in-silico CGM and insulin data for a large cohort of virtual patients, useful for initial algorithm testing and development [2]. |
| Python & Scikit-learn | Software | Provides the core programming environment and libraries for implementing machine learning models (e.g., Logistic Regression), data preprocessing, and calculating evaluation metrics [85]. |
| Deep Learning Frameworks (e.g., TensorFlow, PyTorch) | Software | Enable the construction, training, and evaluation of complex neural network architectures like LSTM, CNN, and multimodal networks [14] [52]. |
| Error Grid Analysis | Methodology | A clinically-oriented evaluation technique that assesses the clinical risk associated with prediction errors, complementing statistical metrics [14]. |
The comparative analysis of predictive interstitial glucose models underscores that there is no single "best" model universally, nor a single "best" metric. The optimal choice is deeply contextual, depending on the clinical priority (e.g., preventing hypoglycemia at all costs vs. reducing false alarms), the available data, and the required prediction horizon. While logistic regression can be highly effective for short-term alerts, more complex LSTM and multimodal architectures show promise for longer, more personalized forecasts. Across all approaches, moving beyond accuracy to a nuanced understanding of precision and recall is fundamental to developing AI tools that are not just statistically sound, but also clinically safe and effective.
In the field of diabetes research, the accurate prediction of interstitial glucose levels is a critical component for developing effective management tools, such as artificial pancreas systems and early hypoglycemia warning systems. The performance of these predictive models is predominantly evaluated using specific error metrics, with Mean Absolute Error (MAE) and Root Mean Square Error (RMSE) being two of the most fundamental and widely adopted measures. While both metrics quantify the average prediction error, they differ significantly in their sensitivity and interpretation, making them suitable for distinct aspects of model assessment. This guide provides a comparative analysis of MAE and RMSE within the context of predictive interstitial glucose modeling, supporting researchers in selecting and interpreting these metrics appropriately.
Conceptual Comparison of MAE and RMSE
MAE and RMSE both measure the average magnitude of prediction error but articulate it differently, leading to unique advantages and disadvantages for each.
- Mean Absolute Error (MAE) calculates the average of the absolute differences between the predicted and actual glucose values. It is a linear score, meaning all individual errors are weighted equally in the average.
- Root Mean Square Error (RMSE), in contrast, is a quadratic scoring rule. It calculates the square root of the average of squared differences between predictions and observations. Because it squares the errors before averaging, RMSE gives a relatively higher weight to large errors.
This fundamental difference is crucial in glucose prediction, where large errors (e.g., missing a predicted hypoglycemic event) are clinically far more dangerous than many small errors. Consequently, RMSE is often more aligned with clinical risk, as it will penalize models with occasional large deviations more heavily than MAE. A model with good RMSE is, therefore, likely to be more robust against critical misses. However, MAE is often preferred for its straightforward interpretability, as it represents the average error in the original units (mg/dL), making it easier to communicate to a broader clinical audience.
Quantitative Performance Data from Comparative Studies
The following tables consolidate quantitative results from recent studies to illustrate the typical performance ranges of MAE and RMSE across different model architectures and prediction horizons.
Table 1: Overall Performance of Glucose Prediction Models for a 30-Minute Prediction Horizon
| Study & Model | RMSE (mg/dL) | MAE (mg/dL) | Dataset & Notes |
|---|---|---|---|
| TCN-based Model (BG-Predict) [87] | 23.22 ± 6.39 | 16.77 ± 4.87 | 97 T1D patients (Tidepool data) |
| Multimodal DL (Type 2 Diabetes) [14] | - | 19 - 22* | 40 subjects; *Abbott sensor, 30-min PH |
| Gaussian Process Regression (GPR) [88] | ~1.69 | 1.64 | 14,733 patients; Average RMSE/MAE values |
Table 2: Error Metrics Stratified by Glycemic Range (from BG-Predict Model, 30-min PH) [87]
| Glycemic Range | Clinical Definition | RMSE (mg/dL) | MAE (mg/dL) |
|---|---|---|---|
| Hypoglycemia | < 70 mg/dL | 12.84 ± 3.68 | 9.95 ± 3.10 |
| Normoglycemia | 70 - 180 mg/dL | 18.67 ± 5.20 | 13.30 ± 3.76 |
| Hyperglycemia | ≥ 180 mg/dL | 26.18 ± 7.26 | 19.36 ± 5.51 |
The data demonstrates that prediction errors are not uniform across all glucose levels. Errors are typically largest in the hyperglycemic range, which can be attributed to higher physiological volatility and data imbalance, as hyperglycemic events can constitute 20-40% of datasets [89] [14]. The lower MAE and RMSE in the hypoglycemic range are critical, as accuracy here is vital for patient safety. However, this range also presents the greatest challenge due to its rarity (often 2-10% of data), a problem that some studies address with specialized cost-sensitive loss functions [89].
Detailed Experimental Protocols for Key Studies
Understanding the methodology behind the data is essential for a critical appraisal of the reported MAE and RMSE values.
Protocol 1: Multi-step TCN Model (BG-Predict)
This study [87] exemplifies a robust, data-driven approach for Type 1 diabetes management.
- Objective: To develop a Temporal Convolutional Network (TCN) for multi-step blood glucose prediction using varying historical data.
- Dataset: Real-world data from 97 patients with Type 1 Diabetes, comprising CGM values, carbohydrate intake, and insulin dosages (basal and bolus).
- Preprocessing: Data was partitioned into patient-specific training and test sets. The model was designed to use different lengths of historical data for different inputs (e.g., BG, food, insulin).
- Model Architecture: A novel TCN-based model was implemented. TCNs use dilated causal convolutions to capture long-range temporal dependencies more effectively than LSTMs.
- Training: Models were trained individually for each patient.
- Evaluation: Performance was evaluated on an unseen test set for each patient. Quantitative measures, including RMSE and MAE, were calculated for the overall dataset and for three specific glycemic ranges (hypo-, normo-, and hyperglycemia) to provide a nuanced view of model performance.
Protocol 2: Multimodal Deep Learning for Type 2 Diabetes
This study [14] highlights the integration of non-glucose data to enhance prediction.
- Objective: To create a multimodal deep learning architecture that integrates CGM time-series data with static, personalized physiological context from health records for Type 2 diabetes glucose prediction.
- Dataset: CGM and health records from 40 individuals with T2D using two different sensor types.
- Preprocessing: CGM time series were made stationary and processed using a sliding window.
- Model Architecture:
- A unimodal pipeline used a stacked CNN and Bidirectional LSTM (BiLSTM) with an attention mechanism to process CGM sequences.
- The multimodal pipeline fused the CGM features with features from a separate neural network processing baseline health records.
- Training & Evaluation: The model was validated for 15, 30, and 60-minute prediction horizons. Performance was primarily reported using Mean Absolute Percentage Error (MAPE), with MAE values also provided. The study compared unimodal vs. multimodal performance to demonstrate the added value of physiological context.
Visualization of Metric Calculation and Application
The following diagram illustrates the logical relationship between prediction errors, the calculation of MAE/RMSE, and their ultimate application in model evaluation, particularly in the critical context of glycemic excursion detection.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Glucose Prediction Research
| Resource / Solution | Function & Application in Research |
|---|---|
| OhioT1DM Dataset | A publicly available benchmark dataset containing CGM, insulin, meal, and activity data from individuals with Type 1 Diabetes, used for training and validating models [89]. |
| UVA/Padova T1D Simulator | A widely accepted and validated simulator of glucose metabolism in T1D. Used for in-silico testing and evaluation of prediction and control algorithms (e.g., via Simglucose) [2] [90]. |
| Clarke and Parkes Error Grid Analysis (EGA) | A clinical validation tool that categorizes prediction accuracy into risk zones (A-E). It is a crucial supplement to MAE/RMSE for assessing clinical safety [87]. |
| Federated Learning (FL) Framework | A privacy-preserving distributed learning approach. Enables training models on data from multiple patients (e.g., in hospitals) without sharing the sensitive raw data, addressing a major bottleneck in healthcare AI [89]. |
| Hypo-Hyper (HH) Loss Function | A cost-sensitive learning approach used during model training. It assigns a higher penalty to prediction errors occurring in hypoglycemic and hyperglycemic ranges, directly improving model performance where it matters most [89]. |
MAE and RMSE serve as the foundational pillars for quantitative assessment in glucose prediction research. While MAE offers superior interpretability for the average expected error, RMSE's inherent sensitivity to larger errors often makes it a more suitable metric for quantifying clinical risk. The choice between them should not be arbitrary; researchers should consider a dual-reporting strategy where possible. Furthermore, as evidenced by recent studies, these overall metrics must be supplemented with range-stratified analysis (especially for hypoglycemia) and clinical tools like Error Grid Analysis to fully capture a model's potential for real-world application. The ongoing development of sophisticated, personalized, and privacy-conscious models promises to further enhance the accuracy and utility of glucose forecasting, ultimately improving the quality of life for individuals with diabetes.
Error Grid Analysis (EGA) serves a critical role in evaluating the clinical accuracy of glucose monitoring systems, bridging the gap between analytical precision and clinical utility. Unlike statistical metrics that treat all measurement errors equally, EGA assesses how these errors might impact clinical decision-making and patient outcomes [91]. This methodology is essential for manufacturers, regulatory bodies like the FDA, and clinicians who need to understand not just whether a device is precise, but whether its readings are safe and effective for daily diabetes management.
The evolution of EGA has produced several standardized tools, with the Clarke and Parkes Error Grids being the most historically significant. These tools divide a plot of reference glucose values versus device-predicted values into risk zones, classifying potential errors based on their clinical significance [91]. This comparative guide provides an objective analysis of the Clarke and Parkes Error Grid methodologies, detailing their protocols, applications, and performance within the context of modern predictive interstitial glucose classification research.
Historical Development and Fundamental Principles
Clarke Error Grid Analysis (CEGA)
The Clarke Error Grid, introduced in 1987, was the first formalized method for evaluating the clinical accuracy of self-monitoring blood glucose systems [91]. Its development was driven by the recognition that analytical accuracy alone was insufficient to evaluate a device's real-world utility.
- Development Methodology: CEGA was based on consensus from five clinicians at a single medical center. Their assumptions included a target glucose range of 70-180 mg/dL and specific patient behaviors regarding corrective treatment [91].
- Zone Definitions: The grid categorizes data pairs into five zones:
- Zone A: Clinically accurate points (within ±20% of reference values ≥70 mg/dL, or both reference and index values <70 mg/dL).
- Zone B: Points with >20% deviation but which would lead to benign or no treatment.
- Zone C: Points that would result in overcorrecting acceptable blood glucose levels.
- Zone D: Points representing "dangerous failure to detect and treat."
- Zone E: Points leading to "erroneous treatment" [91].
Parkes Error Grid Analysis (PEG)
The Parkes Error Grid, also known as the Consensus Error Grid, was published in 2000 as an update to address perceived limitations in the Clarke grid [91] [92]. It introduced a more nuanced approach to clinical risk assessment.
- Development Methodology: PEG was based on a survey of 100 clinicians attending the American Diabetes Association Scientific Sessions. Separate surveys addressed type 1 and type 2 diabetes, acknowledging that clinical risks might differ between these populations [91].
- Key Advancement: A significant innovation was the creation of two distinct grids—one for type 1 diabetes and another for type 2 diabetes—reflecting different risk profiles and treatment strategies [91]. The type 1 diabetes grid typically judges errors more strictly.
Table 1: Fundamental Characteristics of Clarke and Parkes Error Grids
| Feature | Clarke Error Grid (CEG) | Parkes Error Grid (PEG) |
|---|---|---|
| Publication Year | 1987 [91] | 2000 (developed 1994) [91] [92] |
| Development Consensus | 5 clinicians [91] | 100 clinicians [91] |
| Diabetes Type Consideration | Single grid for all diabetes types [91] | Separate grids for Type 1 and Type 2 diabetes [91] |
| Glucose Axis Range | 0 to ~450 mg/dL (x), 0 to 400 mg/dL (y) [93] [91] | 0 to 550 mg/dL (x and y) [91] |
| Risk Zone Borders | Straight lines, discontinuous risk categories [91] | Smoothed, continuous boundaries [91] |
Methodologies and Experimental Protocols
Core Experimental Workflow for Error Grid Analysis
The following diagram illustrates the generalized workflow for conducting an Error Grid Analysis, which is applicable to both Clarke and Parkes methods.
Data Collection and Preparation
The initial phase requires collecting paired glucose measurements from a cohort of participants.
- Participant Recruitment: Studies typically involve dozens to hundreds of participants representing the target population (e.g., type 1 or type 2 diabetes, critically ill patients) [94] [92]. For example, one study analyzed 1,815 paired results from 1,698 critically ill patients [94].
- Paired Measurement Collection: Each participant's glucose is measured simultaneously using:
- Reference Method: A laboratory-grade analyzer or central laboratory measurement providing the "true" value [95]. Arterial blood glucose measurement by amperometry is an example of a high-accuracy reference [95].
- Index Method: The blood glucose monitor (BGM) or continuous glucose monitor (CGM) system being evaluated [91].
- Data Range: Ensure measurements cover the clinically relevant glucose spectrum, typically from hypoglycemia (<70 mg/dL) to severe hyperglycemia (>400 mg/dL) [91].
Protocol for Clarke Error Grid Analysis
After data collection, the manual plotting and analysis involve specific steps, particularly in resource-limited settings [93].
- Create the Grid Foundation: Draw axes on graph paper or using spreadsheet software like Microsoft Excel. The X-axis (reference method) ranges from 0 to 450 mg/dL, and the Y-axis (device method) ranges from 0 to 400 mg/dL [93].
- Plot the Data Pairs: For each paired measurement, plot a point where the x-coordinate is the reference value and the y-coordinate is the corresponding device value [93].
- Draw Zone Boundaries: Manually draw the lines that define Zones A through E as established by Clarke et al. These are straight-line boundaries [91].
- Tally and Calculate: Count the number of data points falling into each zone. Calculate the percentage of total points in each zone. Clinically acceptable performance is typically defined as having >99% of points in Zones A and B combined [91].
Protocol for Parkes Error Grid Analysis
The protocol for the Parkes grid is similar but uses its distinct, smoothed boundaries.
- Select Appropriate Grid: Choose the Parkes grid specific to the patient population being studied (Type 1 or Type 2 diabetes) [91].
- Plot Data Pairs: As with CEGA, plot reference values on the x-axis (0-550 mg/dL) and device values on the y-axis (0-550 mg/dL) [91].
- Apply Continuous Boundaries: Use the curved, continuous risk boundaries of the Parkes grid, which offer a more graduated transition between risk zones compared to the Clarke grid [91].
- Risk Categorization: Tally points into the Parkes zones (A-E). Zone definitions focus on how the error would alter clinical action and the potential effect on outcome [92].
Comparative Performance and Research Applications
Performance Evaluation in Clinical Studies
Error Grid Analysis is widely applied in clinical studies to validate new glucose monitoring technologies and algorithms. The tables below summarize quantitative findings from recent research.
Table 2: CEGA Performance in Recent Glucose Prediction Studies
| Study Context | Prediction Model | CEGA Results (% in Zone) | Clinical Interpretation |
|---|---|---|---|
| Non-invasive glucose monitoring with wearables [9] | Feature-based LightGBM | A+B: >96.4%D: <3.58% | High clinical accuracy; minimal dangerous errors |
| Perioperative CGM accuracy [95] | Dexcom G7 CGM | >98% in acceptable risk zones | Sufficient accuracy for perioperative surveillance |
Table 3: Parkes Grid Analysis of Blood Glucose Monitor Strip Accuracy [92]
| BGM Strip Accuracy Category (95% of results within) | % of Long-Term Results Altering Clinical Action (Zone B & Higher) | Amplification Factor Applied |
|---|---|---|
| Laboratory Standard (±5%) | Not Reported | 2.5x |
| High Accuracy Strips (±10%) | 12.8% | 2.5x |
| Current ISO Standard (±15%) | 30.6% | 2.5x |
| Previous ISO Standard (±20%) | 44.1% | 2.5x |
A key finding from recent research is the amplification effect of BGM inaccuracy. When the inherent variability of less accurate strips is compounded over multiple readings and insulin dose adjustments, the resulting variability in actual blood glucose levels can be 2-3 times higher than the meter's analytical variability [92]. This underscores the critical importance of high strip accuracy for achieving positive long-term clinical outcomes.
Limitations and Evolution beyond Clarke and Parkes
Both Clarke and Parkes grids have limitations that have led to the development of newer tools.
- Clarke Grid Limitations: Its primary criticisms include discontinuous risk categories (e.g., jumping directly from Zone A to Zone D) and its basis on the judgment of only a small number of clinicians from a single center [91].
- Parkes Grid Limitations: While an improvement, its consensus involved 100 clinicians with unknown expertise. Furthermore, it does not fully reflect modern diabetes management practices, including newer insulins and a greater emphasis on hypoglycemia prevention [91] [96].
- The Surveillance Error Grid (SEG): Introduced in 2014 and based on 206 international experts, the SEG offers a continuous, color-coded risk spectrum and is applicable to both BGMs and CGMs [91] [96].
- The Diabetes Technology Society (DTS) Error Grid: Released in 2025, this is the first consensus-based grid specifically designed for CGMs. A key innovation is the inclusion of a Trend Accuracy Matrix to assess the clinical risk of errors in reported glucose trends, which is critical for CGM functionality [96].
The Scientist's Toolkit
Table 4: Essential Reagents and Materials for Error Grid Analysis
| Item | Function/Description | Example/Specification |
|---|---|---|
| Reference Glucose Analyzer | Provides the "gold standard" measurement against which the device is compared. | Laboratory-grade arterial blood analyzer using amperometry [95]; Central laboratory glucose results [94]. |
| Index Glucose Monitor | The device or system undergoing clinical accuracy testing. | Blood Glucose Monitor (BGM), Continuous Glucose Monitor (CGM) [91]. |
| Data Visualization Software | Used to create the error grid plot and automate zone classification. | Microsoft Excel for manual grid creation [93]; Statistical software (R, Python) with custom scripts. |
| Standardized Error Grid Chart | The definitive zone map for classifying data pairs. | Clarke (1987), Parkes (2000, Type 1 or Type 2), or Surveillance (2014) error grid overlays [91]. |
| Paired Clinical Dataset | The core input for the analysis, consisting of timestamp-matched reference and index values. | Typically hundreds to thousands of data pairs from a diverse patient cohort [94] [92]. |
Clarke and Parkes Error Grid Analyses remain foundational tools for assessing the clinical accuracy of glucose monitoring systems. While the Clarke grid provides a historical benchmark, the Parkes grid, with its separate grids for type 1 and type 2 diabetes and smoothed consensus boundaries, offers a more refined risk assessment. Quantitative data from recent studies confirms that both methods are effective in differentiating clinically acceptable performance from potentially dangerous inaccuracy.
The field continues to evolve, with the Surveillance Error Grid and the new Diabetes Technology Society Error Grid addressing the need for CGM-specific assessment, including trend accuracy. For researchers and manufacturers, selecting the appropriate error grid is paramount, and the choice should be guided by the device type (BGM vs. CGM), the target population, and contemporary regulatory expectations. The ultimate goal of these tools is consistent: to ensure that glucose monitoring devices are not just analytically precise, but also clinically safe and effective for day-to-day diabetes management.
The accurate prediction of interstitial glucose levels is a cornerstone for developing advanced diabetes management systems, including closed-loop insulin delivery and proactive hypoglycemia prevention alerts [27] [2]. The prediction horizon—how far into the future a model can forecast glucose levels—is a critical performance differentiator. Short-term predictions (e.g., 15 minutes) enable immediate corrective actions, while longer horizons (e.g., 30-60 minutes) facilitate more strategic management of diet and insulin dosing [27]. However, different algorithmic approaches exhibit distinct strengths and weaknesses across these timeframes. This guide provides a comparative analysis of predictive model performance across 15, 30, and 60-minute horizons, synthesizing quantitative results and methodological protocols from recent research to inform selection and application in scientific and clinical development.
The following tables consolidate key performance metrics from recent studies, enabling direct comparison of model effectiveness across different prediction horizons.
Table 1: Model Performance for 15-Minute Prediction Horizon
| Model | Glucose State | Recall (%) | Accuracy (%) | Notes |
|---|---|---|---|---|
| Logistic Regression [27] | Hypoglycemia (<70 mg/dL) | 98 | - | Best for short-term hypoglycemia prediction |
| Euglycemia (70-180 mg/dL) | 91 | - | ||
| Hyperglycemia (>180 mg/dL) | 96 | - | ||
| LSTM [14] | All States | - | MAPE: 14-24 mg/dL (Sensor 1), 6-11 mg/dL (Sensor 2) | Performance varies by sensor type |
| BiLSTM [8] | All States | - | RMSE: 13.42 mg/dL, MAPE: 12% | Uses non-invasive wearable data |
| LightGBM [9] | All States | - | RMSE: 18.49 mg/dL, MAPE: 15.58% | Non-invasive, no food logs required |
Table 2: Model Performance for 30-Minute Prediction Horizon
| Model | Glucose State | Performance Metrics | Architecture Context |
|---|---|---|---|
| Multimodal Deep Learning [14] | All States | MAPE: 19-22 mg/dL (Sensor 1), 9-14 mg/dL (Sensor 2) | Superior to unimodal models at this horizon |
| Hyperglycemia (>180 mg/dL) | Hyperglycemic MAPE provided | Baseline health data improves accuracy | |
| Unimodal CNN-BiLSTM [14] | All States | Higher MAPE than multimodal | Lacks auxiliary patient data |
Table 3: Model Performance for 60-Minute Prediction Horizon
| Model | Glucose State | Recall (%) | Other Metrics | Comparative Performance |
|---|---|---|---|---|
| LSTM [27] | Hypoglycemia (<70 mg/dL) | 87 | - | Outperforms logistic regression for 1-hour forecast |
| Hyperglycemia (>180 mg/dL) | 85 | - | ||
| Logistic Regression [27] | Hypoglycemia (<70 mg/dL) | 83 | - | Less accurate than LSTM for 1-hour |
| Hyperglycemia (>180 mg/dL) | ~60 (inferred) | - | Significant performance drop | |
| Multimodal Deep Learning [14] | All States | - | MAPE: 25-26 mg/dL (Sensor 1), 12-18 mg/dL (Sensor 2) | Significantly outperforms unimodal approach |
| ARIMA [27] | Hypoglycemia (<70 mg/dL) | ~7.3 (inferred) | - | Underperforms all other models |
Detailed Experimental Protocols
To ensure the reproducibility of the cited results, this section details the key methodological approaches from the comparative studies.
Protocol 1: Direct Comparison of ARIMA, Logistic Regression, and LSTM
This foundational study provided the core comparative data for 15-minute and 1-hour horizons [27] [2].
- Data Source and Preprocessing: Data was obtained from 11 individuals with type 1 diabetes using CGM devices and from the Simglucose in-silico simulator. Raw data was pre-processed to a consistent 15-minute frequency, addressing gaps and erroneous entries [27].
- Feature Engineering: The CGM time series was enriched with multiple engineered features, including rolling averages (1h, 3h, 6h), rolling standard deviations (1h, 3h), glucose velocity (rate of change), and acceleration (second derivative). These features capture the dynamics and trends of glucose fluctuations [27].
- Model Training and Evaluation: The ARIMA model forecasted future CGM values directly. The Logistic Regression and LSTM models used the engineered features to predict glucose classes (hypo-/eu-/hyperglycemia) 15 minutes and 1 hour ahead. Models were trained per-patient, with performance evaluated on out-of-sample data using precision, recall, and accuracy [27].
Protocol 2: Multimodal Deep Learning for T2D Management
This study introduced a multimodal architecture and reported performance across 15, 30, and 60-minute horizons [14].
- Data and Participants: The study involved 40 individuals with Type 2 Diabetes using either Menarini or Abbott CGM sensors. Baseline health records (e.g., demographics, comorbidities) were also collected [14].
- Model Architecture:
- CGM Pipeline: A stacked CNN and Bidirectional LSTM (BiLSTM) with an attention mechanism processed the CGM time series. The CNN captured local sequential features, while the BiLSTM learned long-term temporal dependencies.
- Baseline Pipeline: A separate neural network processed the static health records.
- Multimodal Fusion: The outputs from both pipelines were fused via additive concatenation to inform the glucose predictions with patient-specific physiological context [14].
- Evaluation: The model was validated using a moving window approach. Performance was assessed using Mean Absolute Percentage Error (MAPE) and compared against unimodal models that used only CGM data [14].
The workflow for this multimodal approach is illustrated below.
Protocol 3: Non-Invasive Prediction Using Wearables
This study explored a non-invasive alternative by predicting glucose levels without CGM, using data from wearable devices [9].
- Data Collection: Healthy participants used an Empatica E4 wristband to measure physiological parameters including Skin Temperature (STEMP), Blood Volume Pulse (BVP), Heart Rate (HR), Electrodermal Activity (EDA), and Body Temperature (BTEMP). Corresponding glucose values were measured with a CGM as a reference [9].
- Feature Selection and Modeling: An ensemble feature selection strategy (BoRFE) identified the most important sensor modalities. The Light Gradient Boosting Machine (LightGBM) model was then trained on this data, employing a Leave-One-Participant-Out Cross-Validation (LOPOCV) strategy to eliminate personal bias and test generalizability [9].
- Validation: The model was validated in a follow-up study with participants in their daily lives, without requiring food diaries, demonstrating feasibility in real-world conditions [9].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Tools for Glucose Prediction Research
| Item Name | Function/Application | Specification/Example |
|---|---|---|
| CGM Sensors | Provides continuous interstitial glucose measurements for model training and validation. | Abbott Freestyle Libre [9] [26], Menarini GlucoMen Day [14] |
| Multi-Parameter Wearables | Captures non-invasive physiological data for digital biomarker discovery. | Empatica E4 (measures BVP, EDA, HR, STEMP) [9] |
| In-Silico Simulators | Generates large-scale, synthetic patient data for initial algorithm testing and validation. | Simglucose (Python implementation of UVA/Padova T1D Simulator) [27] |
| Public Datasets | Provides benchmark data for reproducible research and model comparison. | OhioT1DM [25], ShanghaiDM [25] |
| Feature Engineering Libraries | Creates derived features (e.g., rate of change, rolling averages) from raw time-series data. | Python libraries (Pandas, NumPy) for calculating velocity, acceleration, etc. [27] |
Analysis of Model Strengths and Weaknesses for Different Glucose Classes (e.g., Hypoglycemia Prediction)
The management of diabetes has been revolutionized by continuous glucose monitoring (CGM) systems, which provide real-time alerts for hypoglycemia, hyperglycemia, and rapid glucose fluctuations [6]. However, the complexity of CGM systems presents significant challenges for both individuals with diabetes and healthcare professionals, particularly in interpreting rapid glucose level changes and dealing with inherent sensor delays [6] [2]. The development of advanced predictive glucose level classification models has therefore become imperative for optimizing insulin dosing and managing daily activities effectively [6].
This comparative analysis examines the efficacy of various machine learning and statistical models in predicting critical glucose classes, with particular emphasis on hypoglycemia (<70 mg/dL), euglycemia (70-180 mg/dL), and hyperglycemia (>180 mg/dL) [6] [2]. As the field moves beyond traditional statistical methods toward what can be termed "CGM Data Analysis 2.0" – encompassing functional data analysis, machine learning, and artificial intelligence – understanding the relative strengths and weaknesses of different modeling approaches becomes essential for both clinical application and further research [3].
Comparative Model Performance Analysis
Quantitative Performance Metrics Across Glucose Classes
Table 1: Model performance for 15-minute prediction horizon
| Glucose Class | Model | Recall (%) | Precision (%) | Key Strengths | Key Limitations |
|---|---|---|---|---|---|
| Hypoglycemia (<70 mg/dL) | Logistic Regression | 98 | N/A | Excellent short-term detection | Performance degrades with longer horizons |
| LSTM | 87 | N/A | Maintains better long-term performance | Suboptimal for very short-term prediction | |
| Hyperglycemia (>180 mg/dL) | Logistic Regression | 96 | N/A | Superior immediate prediction | Less effective for extended forecasting |
| LSTM | 85 | N/A | Sustained performance at 1-hour | Requires more computational resources | |
| Euglycemia (70-180 mg/dL) | Logistic Regression | 91 | N/A | High accuracy for normal ranges | Limited complex pattern recognition |
| ARIMA | Substantially lower | N/A | Simple implementation | Poor for extreme glucose classes |
Table 2: Model performance for 1-hour prediction horizon
| Glucose Class | Model | Recall (%) | Precision (%) | Key Strengths | Key Limitations |
|---|---|---|---|---|---|
| Hypoglycemia (<70 mg/dL) | LSTM | 87 | N/A | Superior long-term prediction | Requires extensive training data |
| Logistic Regression | Significant degradation | N/A | Computational efficiency | Rapid performance decay over time | |
| Hyperglycemia (>180 mg/dL) | LSTM | 85 | N/A | Handles complex temporal patterns | Prone to overfitting with small datasets |
| ARIMA | Consistently underperformed | N/A | Statistical robustness | Fails to capture non-linear dynamics |
The performance comparison reveals a critical trade-off between prediction horizon and model selection. For short-term prediction (15 minutes), logistic regression demonstrates exceptional recall rates for all glucose classes, particularly achieving 98% recall for hypoglycemia and 96% for hyperglycemia [6]. This makes it highly suitable for immediate intervention scenarios. In contrast, for extended prediction horizons (1 hour), long short-term memory (LSTM) networks outperform other models, maintaining recall rates of 87% for hypoglycemia and 85% for hyperglycemia [6]. The autoregressive integrated moving average (ARIMA) model consistently underperformed for both hyper- and hypoglycemia classes across all time horizons [6].
Advanced Model Comparisons in Recent Research
Table 3: Performance of alternative and advanced modeling approaches
| Model Type | Application Context | Key Performance Metrics | Optimal Use Cases |
|---|---|---|---|
| LightGBM with BoRFE | Non-invasive glucose prediction | RMSE: 18.49 ± 0.1 mg/dL, MAPE: 15.58 ± 0.09% [9] | Wearable sensor data integration |
| Bayesian Regularized Neural Networks (BRNN) | Glycemia dynamics modeling | R²: 0.83, RMSE: 14.03 mg/dL [97] | IoT-based diabetes management systems |
| Memetic Algorithm-Optimized NN | Diabetes diagnosis | Accuracy: 93.2%, Sensitivity: 96.2%, Specificity: 95.3% [98] | Early diabetes risk stratification |
| Machine Learning vs. Traditional Statistics | Undiagnosed diabetes prediction | AUC: 0.819 (ML) vs. 0.765 (TS) [99] | Non-invasive screening programs |
Recent research has explored increasingly sophisticated modeling approaches. An ensemble feature selection-based Light Gradient Boosting Machine (LightGBM) algorithm achieved a root mean squared error (RMSE) of 18.49 ± 0.1 mg/dL and mean absolute percentage error (MAPE) of 15.58 ± 0.09% for non-invasive glucose prediction using wearable sensor data, omitting the need for food logs [9]. In Internet of Things (IoT) contexts for diabetes management, Bayesian Regularized Neural Networks (BRNN) have demonstrated strong performance with R² of 0.83 and reduced RMSE of 14.03 mg/dL [97].
Comparative studies between machine learning and traditional statistical methods for undiagnosed diabetes prediction have shown AUC advantages for ML-based approaches (0.819 vs. 0.765), particularly when using anthropometric and lifestyle measurements [99]. This performance advantage extends across various metrics, with memetic algorithm-optimized neural networks achieving 93.2% accuracy, 96.2% sensitivity, and 95.3% specificity [98].
Experimental Protocols and Methodologies
Data Collection and Preprocessing Standards
The foundational data for glucose prediction models typically originates from two primary sources: clinical cohort studies involving people with diabetes and simulation results obtained using CGM simulators [2]. In one representative study, clinical CGM data were acquired from participants with type 1 diabetes who used CGM devices prior to and through their COVID-19 vaccination series [2]. Supplementing real-patient data, simulation platforms like Simglucose v0.2.1 (a Python implementation of UVA/Padova T1D Simulator) generate in-silico data covering virtual patients across different age groups, typically spanning multiple days with randomized meal and snack patterns [2].
Data preprocessing represents a critical step in model development. Raw CGM data often exhibits minor frequency variability and occasional gaps, requiring regularization to consistent time intervals (typically 15 minutes) [2]. For neural network approaches, data normalization using min-max methods to scale characteristics to a range from -1 to +1 has been employed to improve model convergence and performance [98]. Feature engineering techniques, including rolling averages, standard deviations, and rate-of-change metrics, can extract meaningful patterns from glucose dynamics even when additional physiological parameters are unavailable [2].
Model Training and Validation Frameworks
Robust validation methodologies are essential for reliable model assessment. The leave-one-participant-out cross-validation (LOPOCV) approach helps eliminate personal deviation factors, particularly important when working with heterogeneous patient data [9]. For general model development, stratified cross-validation after adjusting for the proportion of glucose class events in each set helps maintain distribution consistency between training and validation cohorts [99].
Hyperparameter optimization significantly impacts model performance. Frameworks like Optuna automate the search for the most effective hyperparameter configuration, defining search spaces and specifying objective functions for optimization [99]. For memetic algorithms (combining genetic algorithms with local search), parameters including crossover rate (typically 80%-95%), mutation rate (usually 0.2%-0.5%), and initial population size (often 20-30) require careful tuning through methods like Taguchi testing to identify optimal combinations [98].
Model Development Workflow
Model Selection Framework
The choice of an appropriate glucose prediction model depends heavily on the specific clinical or research requirements, particularly regarding prediction horizon and target glucose classes.
Model Selection Framework
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential research tools and platforms for glucose prediction studies
| Tool Category | Specific Solution | Function | Application Context |
|---|---|---|---|
| CGM Simulators | Simglucose v0.2.1 [2] | In-silico data generation | Model training and validation |
| Feature Selection | BoRFE (Boruta + RFE) [9] | Ensemble feature selection | Identifying key predictive variables |
| Hyperparameter Optimization | Optuna Framework [99] | Automated parameter tuning | Optimizing model performance |
| Wearable Sensor Platforms | E4 Empatica, Apple Watch, Fitbit [9] | Non-invasive data collection | Digital biomarker discovery |
| Data Processing Libraries | Python Pandas, NumPy, Scikit-learn | Data cleaning and preprocessing | General data preparation |
| Deep Learning Frameworks | TensorFlow, PyTorch, Keras | Neural network implementation | LSTM and other complex models |
| Validation Methodologies | LOPOCV, Stratified Cross-Validation [9] [99] | Robust model testing | Preventing overfitting |
| Performance Evaluation | Clarke Error Grid Analysis, RMSE, MAPE [9] | Clinical accuracy assessment | Model performance quantification |
The comparative analysis of predictive interstitial glucose classification models reveals that model performance is highly dependent on the specific clinical context and prediction requirements. For short-term hypoglycemia prediction – a critical safety concern – logistic regression demonstrates exceptional performance with 98% recall at 15-minute horizons, making it suitable for immediate intervention systems [6]. Conversely, for longer-term forecasting and comprehensive glucose management, LSTM networks provide superior sustainability with 87% recall for hypoglycemia at 1-hour horizons [6].
Emerging approaches, including LightGBM with ensemble feature selection and Bayesian Regularized Neural Networks, show significant promise for non-invasive monitoring and IoT-enabled diabetes management systems [9] [97]. The field continues to evolve from traditional statistical methods toward advanced machine learning approaches, with functional data analysis and AI-powered systems offering more nuanced insights into glucose patterns and dynamics [3].
Future research directions should explore hybrid models that combine the strengths of multiple approaches, such as the high short-term accuracy of logistic regression with the sustained performance of LSTM networks for longer horizons. Additionally, standardization of validation methodologies and performance metrics will be crucial for facilitating direct comparisons between emerging models and establishing robust clinical implementation guidelines.
Conclusion
This comparative analysis underscores that no single model is universally superior for interstitial glucose classification; the optimal choice is highly dependent on the specific clinical context and prediction horizon. For short-term forecasts (e.g., 15 minutes), simpler models like logistic regression can be highly effective and interpretable, while for longer horizons (e.g., 60 minutes), complex deep learning models like LSTM and hybrid CNN-BiLSTM architectures demonstrate superior recall, particularly for critical hypoglycemic events. The integration of multimodal data and the development of fully personalized models present promising pathways to enhance accuracy and clinical relevance. Future research must prioritize improving model interpretability for clinician trust, addressing demographic biases in training data to ensure equitable performance, and establishing standardized benchmarks for rigorous clinical validation. These advancements are pivotal for the development of next-generation decision-support tools that can be seamlessly integrated into drug development pipelines and personalized diabetes management systems.
References
- 1. 6. Glycemic Goals and Hypoglycemia: Standards of Care in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10725808/]
- 2. Comparative Analysis of Predictive Interstitial Glucose ... [https://www.mdpi.com/1424-8220/23/19/8269]
- 3. CGM Data Analysis 2.0: Functional Data Pattern Recognition ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12356821/]
- 4. Development of Machine Learning Models to Predict ... [https://www.medrxiv.org/content/10.1101/2025.10.24.25338707v1.full]
- 5. A multimodal physiological dataset for non-invasive blood ... [https://www.nature.com/articles/s41597-025-06090-6]
- 6. Comparative Analysis of Predictive Interstitial Glucose ... [https://pubmed.ncbi.nlm.nih.gov/37837098/]
- 7. What should your glucose levels be? The 2025 ... [https://www.levels.com/blog/what-should-my-glucose-levels-be-ultimate-guide]
- 8. Comparison of feature learning methods for non-invasive ... [https://www.sciencedirect.com/science/article/pii/S2667102624000615]
- 9. Digital biomarkers for interstitial glucose prediction in ... [https://www.nature.com/articles/s41598-025-14172-z]
- 10. Transformative Advances in Continuous Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12007415/]
- 11. Reproducibility of continuous glucose monitoring results ... [https://www.nature.com/articles/s41598-023-40949-1]
- 12. 5 Best Continuous Glucose Monitors for 2025 [https://www.type1strong.org/blog-post/5-best-continuous-glucose-monitors-for-2025]
- 13. The top CGM stories of 2025 [https://www.drugdeliverybusiness.com/the-top-cgm-stories-of-2025/]
- 14. A multimodal deep learning architecture for predicting ... [https://www.nature.com/articles/s41598-025-07272-3]
- 15. A Tale of Two Compartments: Interstitial Versus Blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2903977/]
- 16. Analysis, Modeling, and Simulation of the Accuracy of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2740661/]
- 17. A large sensor foundation model pretrained on continuous ... [https://www.nature.com/articles/s44401-025-00039-y]
- 18. Automatic Removal of Physiological Artifacts in OPM-MEG [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564105/]
- 19. Characterizing Accuracy and Precision of Glucose Sensors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4455380/]
- 20. Differences in glucose readings between the continuous ... [https://www.sciencedirect.com/science/article/pii/S2589936824000148]
- 21. A Comparative Study of Transformer-Based Models for Multi ... [https://pubmed.ncbi.nlm.nih.gov/40463699/]
- 22. A Comparative Study of Transformer-Based Models for ... [https://www.sciencedirect.com/science/article/pii/S2405896325003313]
- 23. A Comparative Study of Transformer-Based Models ... [https://arxiv.org/html/2505.08821v1]
- 24. Machine learning glucose forecasting models for septic ... [https://www.nature.com/articles/s41598-025-23057-0]
- 25. Integration of artificial intelligence and wearable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627454/]
- 26. A deep learning approach for blood glucose monitoring ... [https://www.nature.com/articles/s41598-025-97391-8]
- 27. Comparative Analysis of Predictive Interstitial Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10574913/]
- 28. Comparison of Three Interstitial Glucose Level Prediction ... [https://www.preprints.org/manuscript/202309.0755]
- 29. IJCMCR-RA-ID-01382 [https://ijclinmedcasereports.com/ijcmcr-ra-id-01382/]
- 30. Data-driven blood glucose level prediction in type 1 diabetes [https://www.nature.com/articles/s41598-024-70277-x]
- 31. Algorithm Showdown: Logistic Regression vs. Random ... [https://machinelearningmastery.com/algorithm-showdown-logistic-regression-vs-random-forest-vs-xgboost-on-imbalanced-data/]
- 32. Difference Between Random Forest and XGBoost [https://www.geeksforgeeks.org/machine-learning/difference-between-random-forest-vs-xgboost/]
- 33. Comparative Analysis of XGBoost, Random Forest, and ... [https://www.sciencedirect.com/science/article/pii/S1877050925026092]
- 34. Comparative Analysis of Logistic Regression, Gradient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11283789/]
- 35. Performance of machine learning models in predicting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11846364/]
- 36. Comparative Analysis of Machine Learning Models for ... [https://www.mdpi.com/2076-3417/15/7/3636]
- 37. LSTM vs GRU: Complete Comparison for Sequence ... [https://medium.com/@digitalconsumer777/lstm-vs-gru-complete-comparison-for-sequence-modeling-6020612fceb5]
- 38. A comparative study of RNN, LSTM, GRU, and hybrid models [https://pmc.ncbi.nlm.nih.gov/articles/PMC12329085/]
- 39. Comparative Analysis and Validation of LSTM and GRU ... [https://www.mdpi.com/2076-3417/15/20/11067]
- 40. A hybrid Transformer-LSTM model apply to glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11389913/]
- 41. Application of the LSTM-GRU compressed model for ... [https://www.sciencedirect.com/science/article/abs/pii/S2352152X25013544]
- 42. Stacked LSTM based deep recurrent neural network with ... [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-021-01462-5]
- 43. GRU-LSTM model based on the SSA for short-term traffic ... [https://www.sciopen.com/article/10.26599/JICV.2024.9210051]
- 44. A Novel CNN-based Bi-LSTM parallel model with attention ... [https://www.nature.com/articles/s41598-022-11880-8]
- 45. Long-Term Prediction of Blood Glucose Levels in Type 1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10658677/]
- 46. Hybrid CNN-LSTM for Predicting Diabetes: A Review [https://pubmed.ncbi.nlm.nih.gov/37867273/]
- 47. Personalized blood glucose prediction in type 1 diabetes ... [https://www.nature.com/articles/s41598-025-13491-5]
- 48. Convolutional neural network bidirectional long short-term ... [https://www.sciencedirect.com/science/article/abs/pii/S0378779622001535]
- 49. A hybrid Transformer-LSTM model apply to glucose prediction [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0310084]
- 50. Digital biomarkers for interstitial glucose prediction in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361560/]
- 51. Advances in Continuous Glucose Monitoring: Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12061739/]
- 52. An AI-based module for interstitial glucose forecasting ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1534830/full]
- 53. Feature-Based Machine Learning Model for Real-Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8258517/]
- 54. Glucostats: an efficient Python library for glucose time series ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-025-06250-w]
- 55. Engineering digital biomarkers of interstitial glucose from ... [https://www.nature.com/articles/s41746-021-00465-w]
- 56. Feature Transformation for Efficient Blood Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9913914/]
- 57. The importance of interpreting machine learning models for ... [https://www.nature.com/articles/s41598-023-44155-x]
- 58. Mastering Cold Start Challenges: Top Strategies for ... [https://www.shaped.ai/blog/mastering-cold-start-challenges]
- 59. How to solve the cold start problem of data analysis agents ... [https://www.tencentcloud.com/techpedia/120563]
- 60. Best practices for solving the cold start problem in AI projects [https://xenoss.io/blog/cold-start-problem-ai-projects]
- 61. LSM-2: Learning from incomplete wearable sensor data [https://research.google/blog/lsm-2-learning-from-incomplete-wearable-sensor-data/]
- 62. A Comprehensive Review of Handling Missing Data [https://arxiv.org/html/2404.04905v1]
- 63. Strategies for Handling Missing Values in Data Analysis [https://www.dasca.org/world-of-data-science/article/strategies-for-handling-missing-values-in-data-analysis]
- 64. Chapter 13 Imputation (Missing Data) [https://bookdown.org/mike/data_analysis/imputation-missing-data.html]
- 65. A survey on missing data in machine learning [https://journalofbigdata.springeropen.com/articles/10.1186/s40537-021-00516-9]
- 66. The best way to handle missing data | by Devansh - Medium [https://machine-learning-made-simple.medium.com/the-best-way-to-handle-missing-data-49918380abea]
- 67. The impact of Bayesian optimization on feature selection [https://www.nature.com/articles/s41598-024-54515-w]
- 68. Feature selection strategies: a comparative analysis of SHAP ... [https://journalofbigdata.springeropen.com/articles/10.1186/s40537-024-00905-w]
- 69. Combating Overfitting in Machine Learning: Cross - Validation ... [https://medium.com/funtech-academy/combating-overfitting-in-machine-learning-cross-validation-regularization-pruning-5f36305156aa]
- 70. 5 Machine Learning Techniques to Solve Overfitting | Analytics Steps [https://www.analyticssteps.com/blogs/5-machine-learning-techniques-solve-overfitting]
- 71. 16 Cross Validation and Regularization [https://ds100.org/course-notes/cv_regularization/cv_reg.html]
- 72. Validating your Machine Learning Model [https://maartengrootendorst.com/blog/validate/]
- 73. Practical Considerations and Applied Examples of Cross ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11041453/]
- 74. AI Model Validation: Best Practices for Accuracy & Reliability [https://galileo.ai/blog/best-practices-for-ai-model-validation-in-machine-learning]
- 75. Decoding Black Box AI: The Global Push for Explainability ... [https://trendsresearch.org/insight/decoding-black-box-ai-the-global-push-for-explainability-and-transparency/?srsltid=AfmBOoqdDkL8taOkO7bxywU9kbcRjlTPMFzZj_ter1v_WYjg1FAbOvWH]
- 76. Interpreting Black-Box Models: A Review on Explainable ... [https://link.springer.com/article/10.1007/s12559-023-10179-8]
- 77. What is Explainable AI (XAI)? [https://www.ibm.com/think/topics/explainable-ai]
- 78. The XAI Dilemma: Balancing Accuracy and Interpretability ... [https://dev.to/vaib/the-xai-dilemma-balancing-accuracy-and-interpretability-in-real-world-ai-3dm7]
- 79. Comparison of Machine Learning Models for Predicting ... [https://www.mdpi.com/2079-9292/13/16/3192]
- 80. Top 10 Explainable AI (XAI) Tools in 2025: Features, Pros ... [https://www.scmgalaxy.com/tutorials/top-10-explainable-ai-xai-tools-in-2025-features-pros-cons-comparison/]
- 81. Explainable AI in 2025 [https://www.nitorinfotech.com/blog/explainable-ai-in-2025-navigating-trust-and-agency-in-a-dynamic-landscape/]
- 82. What is Accuracy, Precision, Recall and F1 Score? [https://labelf.ai/blog/what-is-accuracy-precision-recall-and-f1-score]
- 83. Classification: Accuracy, recall, precision, and related metrics | Machine Learning | Google for Developers [https://developers.google.com/machine-learning/crash-course/classification/accuracy-precision-recall]
- 84. Precision and Recall - A Comprehensive Guide With ... [https://towardsdatascience.com/precision-and-recall-a-comprehensive-guide-with-practical-examples-71d614e3fc43/]
- 85. Understanding Precision, Recall, and F1 Score Metrics [https://medium.com/@piyushkashyap045/understanding-precision-recall-and-f1-score-metrics-ea219b908093]
- 86. Transforming AI: The Power of Precision-Recall Curves [https://galileo.ai/blog/precision-recall-ai-evaluation]
- 87. Multi-step ahead predictive model for blood glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8692478/]
- 88. Evaluation of machine learning-based regression ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11720924/]
- 89. A personalized federated learning-based glucose ... [https://www.nature.com/articles/s41598-025-22316-4]
- 90. Long-term blood glucose prediction using deep learning ... [https://www.sciencedirect.com/science/article/pii/S2405959525000712]
- 91. The Need for a Modern Error Grid for Clinical Accuracy of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10899826/]
- 92. Applying Parkes Grid Method to Evaluate Impact of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7783004/]
- 93. Clarke Error Grid Analysis on Graph Paper and Microsoft ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7196876/]
- 94. An insulin-dose error assessment grid: A new tool to ... [https://www.sciencedirect.com/science/article/pii/S0009912019304369]
- 95. Accuracy of continuous glucose monitoring during ... [https://www.sciencedirect.com/science/article/pii/S0007091225004106]
- 96. New error grid better tailored to assess CGM accuracy [https://www.healio.com/news/endocrinology/20250117/new-error-grid-better-tailored-to-assess-cgm-accuracy]
- 97. A Comparison of Different Models of Glycemia Dynamics ... [https://www.mdpi.com/2076-3417/10/12/4381]
- 98. Comparison of Predictive Models for the Early Diagnosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4871851/]
- 99. Comparisons of the prediction models for undiagnosed ... [https://www.nature.com/articles/s41598-023-40170-0]