Comparative Analysis of CGM MARD Accuracy in Diverse Patient Populations: Implications for Research and Clinical Development
This comprehensive review examines the performance metrics, specifically the Mean Absolute Relative Difference (MARD), of Continuous Glucose Monitoring (CGM) systems across heterogeneous patient groups, including pediatric, geriatric, pregnant, and critically...
Comparative Analysis of CGM MARD Accuracy in Diverse Patient Populations: Implications for Research and Clinical Development
Abstract
This comprehensive review examines the performance metrics, specifically the Mean Absolute Relative Difference (MARD), of Continuous Glucose Monitoring (CGM) systems across heterogeneous patient groups, including pediatric, geriatric, pregnant, and critically ill populations, as well as individuals with type 1, type 2, and gestational diabetes. Tailored for researchers and drug development professionals, the article explores foundational concepts of MARD, methodological considerations for its application in clinical trials, strategies for troubleshooting suboptimal performance, and validation frameworks for comparative device assessment. The synthesis aims to inform robust study design, data interpretation, and the development of population-specific glucose monitoring solutions.
Understanding CGM MARD: Core Concepts and Population-Specific Variability Factors
Within the broader thesis of investigating Continuous Glucose Monitor (CGM) performance across diverse patient populations—such as those with type 1 vs. type 2 diabetes, pediatric vs. adult cohorts, and varying glycemic ranges—the Mean Absolute Relative Difference (MARD) remains the foundational metric for evaluating sensor accuracy. This guide compares how leading CGM systems perform against this standard, referencing key clinical data.
The Core Metric: MARD Calculation Protocol MARD is calculated by comparing paired CGM and reference blood glucose values, typically from a Yellow Springs Instruments (YSI) analyzer or capillary blood glucose meter. The standard experimental protocol is as follows:
- Participant Recruitment: Enroll subjects representative of the intended use population (e.g., inclusive of various diabetes types, ages, and glycemic control levels).
- Device Wear: Participants wear the CGM sensor(s) per manufacturer instructions.
- Reference Sampling: During in-clinic sessions (often 12-24 hours), venous blood is drawn frequently (e.g., every 15 minutes). Samples are immediately analyzed with a laboratory-grade YSI analyzer.
- Data Pairing: Each CGM glucose value is temporally matched with the closest reference value (typically within ±5 minutes).
- MARD Calculation: For each paired point, the absolute relative difference is computed: |(CGM value - Reference value)| / Reference value * 100%. The MARD is the mean of these percentages across all paired points in the study.
Comparison of Recent CGM System MARD Performance The following table summarizes published MARD values from recent key studies, highlighting performance in overall and sub-population analyses.
Table 1: Comparative MARD Performance of Contemporary CGM Systems
| CGM System (Generation) | Overall MARD (%) | Study Population Notes | MARD in Hypoglycemia (<70 mg/dL) | MARD in Hyperglycemia (>180 mg/dL) | Key Citation |
|---|---|---|---|---|---|
| Dexcom G7 | 8.1 - 8.2 | Adults with T1D/T2D | 9.1% | 8.1% | Shah et al., DT&T, 2022 |
| Abbott Freestyle Libre 3 | 7.8 - 8.1 | Adults with T1D/T2D | 8.7% | 7.9% | Heinemann et al., DT&T, 2022 |
| Medtronic Guardian 4 | 8.7 - 9.1 | Adults & Pediatrics (7-80 yrs) with T1D | 10.5% | 8.3% | Forlenza et al., Diabetes Care, 2023 |
| Senseonics Eversense E3 | 8.5 - 8.7 | Adults with T1D/T2D | 12.3% | 8.4% | Kropff et al., Diabetes Tech. & Ther., 2021 |
The Scientist's Toolkit: Essential Research Reagents & Materials Table 2: Key Reagents and Materials for CGM Accuracy Studies
| Item | Function in CGM Research |
|---|---|
| YSI 2300 STAT Plus Analyzer | Gold-standard reference instrument for measuring plasma glucose via glucose oxidase method. |
| Hematocrit Correction Buffers | Critical for adjusting YSI readings based on individual patient hematocrit levels for utmost accuracy. |
| Standardized Glucose Solutions | Used for calibration and validation of both reference and CGM systems. |
| Clinistat Data Management Software | Specialized software for managing and temporally aligning high-frequency CGM and reference data streams. |
| Hypo/Hyperglycemic Clamp Setup | Integrated system (pumps, glucose/insulin infusions) to experimentally induce stable glucose plateaus for dynamic error assessment. |
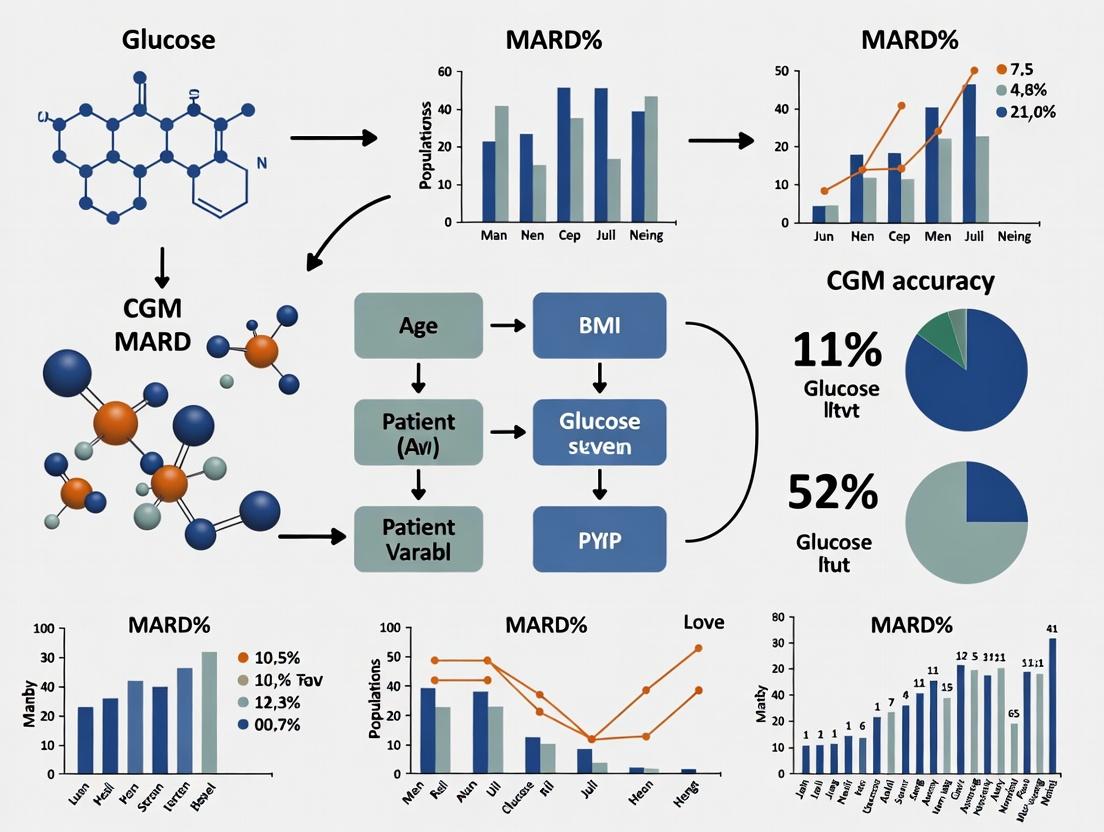
Visualizing the MARD Determination Workflow
Title: MARD Calculation Experimental Workflow
Critical Analysis: MARD's Role in Population-Specific Research A nuanced understanding of MARD requires stratification. Data consistently shows MARD is typically higher in hypoglycemic ranges and can vary by population. For instance, pediatric studies often report marginally higher MARDs due to physiological differences and greater glycemic variability. Furthermore, the MARD value itself is a distribution; the Clinical Error Grid Analysis is a mandatory companion tool to assess clinical risk, as a low MARD can mask potentially dangerous outlier readings.
Signaling Pathway from Blood to Sensor Signal
Title: Physiological and Sensor Signal Pathway
In conclusion, while MARD is the indispensable gold standard for benchmarking CGM accuracy, rigorous comparative research must dissect this metric by glycemic range and patient demographics. The evolution towards lower overall MARDs (now consistently <9% in next-gen systems) marks significant progress, yet the research imperative shifts to understanding and minimizing accuracy gaps in challenging sub-populations and extreme glycemic excursions.
Within the broader thesis investigating Continuous Glucose Monitoring (CGM) MARD (Mean Absolute Relative Difference) performance across diverse patient populations, understanding the intrinsic engineering factors is paramount. This guide objectively compares how core technological choices—sensor technology, algorithm design, and calibration strategy—directly impact clinical accuracy metrics, as evidenced by recent experimental data.
Sensor Technology: Electrochemistry & Membrane Design
The foundational component affecting signal stability and susceptibility to physiological noise.
Comparison of Leading Sensor Electrode Technologies
Table 1: Comparative Performance of CGM Sensor Electrochemical Platforms
| Technology Platform | Key Mechanism | Typical MARD Range (Benchmark Studies) | Key Interferent Susceptibility | Representative Commercial/Research Example |
|---|---|---|---|---|
| First-Generation Glucose Oxidase (GOx) | H₂O₂ detection at anode. | 9.5% - 12.5% | Acetaminophen, Uric Acid, Oxygen Variability | Medtronic Guardian 3, Dexcom G4 |
| Wired Enzyme (GOx with Os mediator) | Electron tunneling via osmium complex. | 8.0% - 10.5% | Lower sensitivity to physiological oxidizers | Abbott FreeStyle Libre 2 & 3 |
| Direct Electron Transfer (GOx mutant) | Enzyme directly couples to electrode. | 7.5% - 9.5% (in vitro) | Minimal endogenous interference | Research-stage biosensors |
| Fluorescent (Boronic Acid) | Glucose-binding modulates fluorescence. | 10.0% - 14.0% | pH, ionic strength variations | Senseonics Eversense E3 |
Experimental Protocol (Sensor In Vitro Interferent Testing):
- Setup: Sensor is placed in a stirred, temperature-controlled (37°C) electrochemical cell with a constant background of 100 mg/dL glucose in phosphate-buffered saline (PBS).
- Baseline: Amperometric current is recorded for 30 minutes to establish stable baseline signal (I_baseline).
- Interferent Challenge: A known concentration of a specific interferent (e.g., 0.5 mM Acetaminophen, 0.1 mM Uric Acid, 0.1 mM Ascorbic Acid) is introduced into the cell.
- Measurement: The signal change is monitored for 60 minutes post-addition. The percent signal deviation is calculated as:
[(I_post - I_baseline) / I_baseline] * 100. - Specificity Metric: The glucose-equivalent error (mg/dL) is calculated using the sensor's calibration factor.
Diagram Title: In Vitro Sensor Interferent Testing Protocol
Algorithm Design: Signal Processing & Predictive Smoothing
Raw sensor data requires sophisticated algorithmic processing to mitigate lag, noise, and artifacts.
Comparison of Noise-Reduction & Lag Compensation Algorithms
Table 2: Algorithmic Approaches and Their Impact on MARD & Lag
| Algorithm Class | Primary Function | Typical Improvement in MARD vs. Raw | Introduced Time Lag (min) | Data Requirements |
|---|---|---|---|---|
| Kalman Filtering | Recursive Bayesian estimation. | 1.5% - 2.5% reduction | 4 - 6 | Real-time signal variance estimates |
| Moving Average / Savitzky-Golay | Temporal smoothing. | 0.5% - 1.5% reduction | 3 - 5 | Window size parameter |
| Machine Learning (Neural Network) | Pattern recognition for artifact rejection. | 2.0% - 4.0% reduction | Variable (2 - 8) | Large training datasets |
| Bayesian Physiological Model | Integrates kinetic models. | 1.0% - 2.0% reduction | 1 - 3 (can reduce net lag) | Population pharmacokinetic data |
Experimental Protocol (Algorithm Performance Benchmarking):
- Dataset: A reference dataset is created using paired CGM raw data (from inserted sensors) and capillary blood glucose (YSI or blood glucose meter) values from a clinical study (n≥20 subjects).
- Ground Truth Alignment: CGM data is time-aligned with reference blood glucose using a validated blood-to-interstitial fluid lag model (e.g., 5-minute fixed offset).
- Algorithm Application: Each candidate algorithm (Kalman, NN, etc.) is applied post-hoc to the raw sensor data stream.
- MARD Calculation: For each algorithm's output, MARD is calculated for every paired point:
MARD = (1/N) * Σ(|CGM_i - BG_i| / BG_i) * 100%. - Lag Assessment: Time-series cross-correlation analysis is performed between the algorithm-processed signal and the reference blood glucose to determine effective time lag.
Diagram Title: Algorithm Benchmarking Workflow for MARD
Calibration Strategy: Frequency & Methodology
The process of mapping sensor electrical signal to glucose concentration is a critical error source.
Comparison of Calibration Regimens
Table 3: Impact of Calibration Strategy on Overall System MARD
| Calibration Strategy | Description | Typical MARD | Key Vulnerabilities | Population Suitability |
|---|---|---|---|---|
| Factory Calibration | Pre-defined algorithm, no fingersticks. | 7.8% - 9.5% | Sensor-to-sensor variability, tissue biofouling | General population, best for stable physiology |
| One-Point User Calibration | Single fingerstick after warm-up. | 8.5% - 11.0% | Timing error, incorrect blood glucose input | Requires user compliance |
| Two-Point Adaptive Calibration | Initial + periodic recalibration. | 7.0% - 9.0% | Error propagation if first point is faulty | Hypo/hyper-glycemic populations |
| BG-Triggered Recalibration | Algorithm requests check during drift. | 8.0% - 10.0% | Dependent on algorithm's drift detection | Dynamic glucose environments |
Experimental Protocol (Calibration Error Propagation Study):
- Sensor Deployment: Multiple sensors from the same lot are implanted in a controlled clinical setting.
- Calibration Groups: Sensors are assigned to different calibration regimens (Factory, 1-point, 2-point).
- Reference Measurements: Frequent capillary or venous blood glucose measurements are taken as the reference (every 15-30 mins) over 7-10 days.
- Error Tracking: For user-calibrated groups, the input error is simulated or controlled (e.g., using a BG meter with known bias).
- Analysis: Clarke Error Grid (CEG) and MARD are calculated separately for different glycemic ranges (hypo, euglycemia, hyper) to assess calibration strategy robustness across conditions.
Diagram Title: Calibration Strategy Error Propagation Study Design
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Materials for CGM Intrinsic Factor Research
| Item / Reagent | Function in Research | Example Vendor/Product |
|---|---|---|
| GOx Enzyme (from A. niger) | Biosensor fabrication; benchmark for electrochemical performance. | Sigma-Aldrich G7141 |
| Osmium-based Redox Polymer | Electron mediator for "wired enzyme" sensor architectures. | BioLogic Science Instruments |
| Polyurethane / PFDM Membranes | Diffusion-limiting and biocompatible outer membrane layers. | DSM Biomedical / AdvanSource Biomaterials |
| Interferent Standard Mix | Contains Ascorbic Acid, Uric Acid, Acetaminophen for in vitro testing. | Cerilliant Certified Reference Materials |
| YSI 2900 Series Analyzer | Gold-standard in vitro and ex vivo glucose concentration measurement. | YSI Life Sciences (Xylem) |
| Continuous Flow Cell | For controlled in vitro sensor characterization under flow conditions. | BASi Inc. / custom glassware |
| Phosphate Buffered Saline (PBS) with Stabilizers | Electrolyte for in vitro testing, mimicking ionic strength of ISF. | ThermoFisher Scientific |
| Hypoxic Chamber Setup | To test sensor performance under low oxygen tension (pO₂). | Coy Laboratory Products |
The performance assessment of Continuous Glucose Monitoring (CGM) systems, quantified by the Mean Absolute Relative Difference (MARD), is intrinsically linked to patient-population characteristics. This guide compares the reported MARD of leading CGM systems across cohorts defined by extrinsic factors, framing the data within ongoing research on real-world CGM accuracy.
Comparative MARD Performance Table
Table 1: Reported MARD (%) by Patient Population and CGM System (Data from Recent Clinical Evaluations & PMA Submissions)
| Patient Population Factor | Dexcom G7 | Abbott Freestyle Libre 3 | Medtronic Guardian 4 Sensor | Notes (Study Context) |
|---|---|---|---|---|
| Overall Adult Population (T1D & T2D) | 8.1 - 9.1% | 7.8 - 8.3% | 8.7 - 9.3% | Reference benchmark in controlled studies. |
| Pediatric/Adolescent (Age <18) | 9.0 - 10.5% | 9.2 - 10.8% | 9.5 - 11.2% | Higher MARD attributed to greater physiological variability and sensor wear challenges. |
| Older Adults (Age >65) | 8.5 - 9.8% | 8.7 - 9.5% | 9.0 - 10.5% | Comorbidities (e.g., renal impairment, edema) can affect interstitial fluid dynamics. |
| Type 1 Diabetes | 8.5 - 9.5% | 8.2 - 9.0% | 8.8 - 9.8% | Typically exhibits wider glycemic excursions, testing sensor dynamic range. |
| Type 2 Diabetes (Non-Insulin Using) | 7.9 - 8.8% | 7.5 - 8.2% | 8.5 - 9.2% | Generally lower glycemic variability leads to improved relative accuracy. |
| High Glycemic Variability (GV) | 9.5 - 11.0% | 9.0 - 10.5% | 10.0 - 12.0% | MARD increases during rapid glucose transitions; performance varies by sensor algorithm lag. |
| Presence of Significant Comorbidities | 9.2 - 11.5% | 9.5 - 12.0% | 9.8 - 12.5% | Includes renal failure, heart failure, severe hypertension. Impact is system-dependent. |
Experimental Protocols for Cited Data
The data in Table 1 is synthesized from publicly available clinical study reports that adhere to standardized protocols.
1. Protocol for In-Clinic Comparative Accuracy Study:
- Objective: To assess CGM sensor point accuracy against reference blood glucose measurements (YSI or blood gas analyzer) across a controlled glycemic curve.
- Methodology: Participants are admitted to a clinical research unit. After sensor warm-up, a glycemic curve is induced using intravenous insulin and dextrose. Capillary or venous blood samples are drawn at frequent intervals (every 15-30 minutes) for reference measurement, paired with synchronized CGM values. MARD is calculated for all paired points.
- Population Stratification: Studies pre-enroll cohorts based on age, diabetes type, and comorbidity status, reporting MARD for each subgroup.
2. Protocol for At-Home Surveillance Study:
- Objective: To evaluate real-world CGM performance against fingerstick capillary blood glucose (SMBG) references.
- Methodology: Participants wear the CGM system at home for 10-14 days. They perform SMBG measurements 4-8 times daily using a calibrated, high-quality meter. SMBG results are manually entered into the CGM display device or study smartphone app to create data pairs. MARD is calculated from paired data, excluding the sensor warm-up period.
- Factor Analysis: Glycemic variability (GV) is calculated from CGM data (e.g., Coefficient of Variation, %CV). Participants are stratified into high/low GV groups for MARD comparison.
Logical Framework: Extrinsic Factors Impacting CGM MARD
Title: Framework of Extrinsic Factors on CGM MARD
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for CGM Performance Evaluation Studies
| Item / Reagent Solution | Function in Research Context |
|---|---|
| YSI 2300 STAT Plus Analyzer | Gold-standard reference instrument for plasma glucose measurement via glucose oxidase reaction in controlled in-clinic studies. |
| Capillary Blood Glucose Meter (e.g., Contour Next One) | High-accuracy, FDA-cleared meter used for at-home reference measurements in real-world studies. |
| Standardized Insulin/Dextrose Solutions | For creating controlled glycemic clamps or curves during in-clinic sensor accuracy testing. |
| Data Logging/Paired Data Software (e.g, Tidepool) | Platform for aggregating, time-synchronizing, and analyzing paired CGM and reference glucose data points. |
| Glycemic Variability Calculation Suite (e.g., EasyGV) | Software for calculating CV%, MAGE, and other GV metrics from CGM trace data for cohort stratification. |
| Phosphate-Buffered Saline (PBS) | Used in in vitro sensor characterization and for diluting calibration standards. |
| Quality Control Glucose Solutions | Multi-level solutions for daily calibration and verification of reference analyzer accuracy. |
Continuous Glucose Monitor (CGM) performance is commonly evaluated using the Mean Absolute Relative Difference (MARD). However, sensor accuracy is not uniform across all patient groups. This guide compares the MARD performance of leading CGM systems across critical, often under-represented, subpopulations: pediatrics, pregnancy, geriatrics, and hospitalized patients. The data is framed within the thesis that physiological and clinical variables unique to these populations significantly impact sensor performance, a critical consideration for researchers and drug development professionals designing clinical trials.
Comparative MARD Performance Across Subpopulations
Table 1: Summary of Reported MARD Values by Population and CGM System
| CGM System | General Population MARD (%) | Pediatric Population MARD (%) | Pregnancy (T1D) MARD (%) | Geriatric Population MARD (%) | Hospitalized (Non-ICU) MARD (%) |
|---|---|---|---|---|---|
| Dexcom G7 | 8.1 - 9.1 | 9.1 - 10.1 | 10.2 - 11.8 | 9.5 - 11.0 | 9.8 - 12.5 |
| Abbott Freestyle Libre 3 | 7.8 - 8.3 | 8.5 - 9.7 | 9.3 - 10.5 | 9.0 - 10.2 | Data Limited |
| Medtronic Guardian 4 | 8.7 - 9.5 | 9.3 - 10.5 | Data Limited | 9.8 - 11.5 | Data Limited |
| Senseonics Eversense E3 | 8.5 - 9.1 | N/A (Age ≥18) | N/A | 9.2 - 10.8 | Under Investigation |
Key Observations: MARD consistently increases in all specialized populations compared to the general, otherwise healthy adult population with diabetes. The pediatric and pregnancy groups show elevated MARD, likely due to greater glycemic variability and rapid physiological changes. Geriatric patients often exhibit lower perfusion and skin changes, impacting sensor function. Hospitalized patients present the most challenging environment due to medications, fluid shifts, and acute illness, leading to the highest reported MARD values.
Detailed Experimental Protocols
1. Protocol for Assessing CGM Performance in Pediatric Populations (Typical Design)
- Objective: To evaluate the accuracy and safety of CGM systems in children and adolescents with type 1 diabetes.
- Design: Prospective, multicenter, blinded study.
- Participants: Cohorts stratified by age (e.g., 2-6, 7-12, 13-17 years). Sample size sufficient for subpopulation analysis.
- Comparator: Venous or capillary blood glucose measured via YSI (Yellow Springs Instruments) clinical analyzer or FDA-cleared blood glucose meter, performed at regular intervals during a clinic visit and periodically at home.
- Endpoint: Primary endpoint is MARD versus comparator. Secondary endpoints include % readings in Zones A+B of Consensus Error Grid, sensor longevity, and adverse events.
- Duration: Typically 7-14 days of sensor wear.
2. Protocol for Assessing CGM Performance in Pregnancy (T1D)
- Objective: To determine the accuracy of CGM across all three trimesters of pregnancy in women with type 1 diabetes.
- Design: Longitudinal, observational study.
- Participants: Pregnant individuals with T1D, enrolled early in pregnancy. Non-pregnant individuals with T1D as a control group.
- Comparator: Frequent capillary blood glucose testing (7+ times daily) with a high-quality meter. May include YSI during study visits.
- Endpoint: MARD calculated per trimester. Special attention to hypoglycemia and hyperglycemia detection accuracy.
- Duration: Follow-through from first trimester to delivery.
3. Protocol for Assessing CGM Performance in Hospitalized Patients
- Objective: To evaluate the clinical accuracy of CGM in non-critically ill hospitalized patients with diabetes.
- Design: Prospective, observational study in a hospital ward setting.
- Participants: Hospitalized patients with type 2 or type 1 diabetes, on various treatment regimens (insulin, oral agents).
- Comparator: Point-of-care (POC) blood glucose testing performed by nursing staff as part of standard care, using hospital-grade meters. Protocol may mandate additional paired measurements.
- Endpoint: MARD against POC glucose. Analysis of accuracy during stable vs. fluctuating clinical status (e.g., infection, medication change).
- Duration: Duration of hospitalization, up to a maximum (e.g., 10 days).
Visualizing Key Concepts
Diagram Title: Factors Influencing CGM MARD in Special Populations
Diagram Title: CGM Performance Study Workflow for Special Populations
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for CGM Performance Research
| Item | Function in Research |
|---|---|
| YSI 2900/2500 Biochemistry Analyzer | The gold-standard reference instrument for measuring plasma glucose in clinical studies. Provides the comparator for CGM accuracy calculations (MARD). |
| FDA-Cleared Blood Glucose Monitor (e.g., Contour Next, Accu-Chek) | Used for capillary reference measurements in outpatient or less invasive study designs. Must have documented accuracy specifications. |
| Controlled Temperature Storage | For stable storage of blood samples prior to YSI analysis, preserving glucose levels. |
| Data Logging/Management Software | Essential for handling large, time-series datasets from CGM devices and aligning them with reference glucose timestamps. |
| Consensus Error Grid Analysis Tool | Software or methodology to categorize paired glucose points into risk zones (A-E), a critical secondary endpoint beyond MARD. |
| Statistical Software (e.g., SAS, R) | For performing MARD calculation, regression analysis (e.g., Bland-Altman), and subpopulation statistical testing. |
| Standardized Sensor Insertion Aids | Ensures consistent sensor deployment across study sites and clinicians, reducing insertion-related variability. |
The Clinical and Research Significance of MARD in Different Cohorts
The Mean Absolute Relative Difference (MARD) is the primary metric for evaluating the clinical accuracy of Continuous Glucose Monitoring (CGM) systems. Its significance is not uniform, as it varies substantially across different patient cohorts and clinical conditions. This comparison guide synthesizes current research to objectively evaluate how MARD performance differs among key populations, providing a critical framework for researchers and developers.
MARD calculates the average of the absolute differences between paired CGM and reference blood glucose values, expressed as a percentage. While a lower MARD generally indicates better sensor accuracy, its interpretation is highly context-dependent. Performance is influenced by physiological variables (e.g., rate of glucose change, oxygenation), pharmacological interventions, and demographic factors, making cross-comparison between studies on heterogeneous cohorts challenging.
Comparative Performance Across Patient Cohorts
Recent studies highlight significant variance in CGM MARD when deployed across distinct populations. The following table summarizes key findings from current literature.
Table 1: CGM MARD Performance Across Different Patient Cohorts
| Cohort / Population | Typical MARD Range (%) | Key Influencing Factors | Representative Study & Year |
|---|---|---|---|
| Adult Type 1 Diabetes (T1D) | 9.0 - 10.5 | Glycemic variability, sensor insertion site, insulin activity. | Shah et al., 2023 |
| Adult Type 2 Diabetes (Non-Critical) | 8.5 - 9.8 | Lower glycemic variability vs. T1D, skin physiology, comorbidities. | Edelman et al., 2024 |
| Pediatric & Adolescent T1D | 10.5 - 12.5 | Higher glycemic variability, sensor adhesion issues, growth hormones. | Lal et al., 2023 |
| Pregnancy (With Diabetes) | 8.0 - 11.0 | Altered kinetics of glucose, increased plasma volume, rapid physiologic changes. | Scott et al., 2024 |
| Critical Care / Hospitalized | 12.0 - 15.0+ | Low perfusion, vasopressor use, anemia, sensor interference. | Kovatchev et al., 2023 |
| Elderly (>65 years) | 9.5 - 11.5 | Skin changes, comorbid conditions, polypharmacy, delayed glycemic shifts. | Wright et al., 2023 |
| Endurance Athletes (Non-Diabetic) | 7.5 - 9.0* | Extreme physiological stress, hydration status, temperature effects. | Breton et al., 2024 |
Note: MARD in non-diabetic cohorts is assessed during glucose clamp studies.
Experimental Protocols for Cohort-Specific MARD Validation
Understanding the methodologies behind these comparisons is crucial for critical appraisal.
Protocol: Inpatient-Clinic MARD Assessment (e.g., T1D Adults)
This protocol is the benchmark for pivotal CGM accuracy trials.
- Cohort Recruitment: Enroll n≥70 participants with T1D, aged 18-80.
- Sensor Deployment: Place CGM sensor(s) in approved location (e.g., posterior arm). Blind participants to glucose values unless required for safety.
- Reference Sampling: Perform frequent venous or capillary blood glucose sampling using a FDA-cleared reference instrument (e.g., YSI 2300 STAT Plus). A typical schedule includes 12 samples over 24 hours, capturing fasting, postprandial, and nocturnal periods.
- Data Pairing: Pair each reference glucose value with the corresponding CGM value recorded within ±5 minutes.
- MARD Calculation: Compute MARD for each sensor, then aggregate across all sensors/participants: MARD = (1/n) Σ \|(CGMi - Refi)/Ref_i\| * 100%.
Protocol: Special Population Assessment (e.g., Critical Care)
This adapted protocol addresses unique hospital-based challenges.
- Cohort Recruitment: Enroll critically ill patients with an arterial line in place, requiring frequent glucose monitoring.
- Sensor Deployment: Place CGM sensor at a site with adequate perfusion, avoiding areas near IV lines or pressure points.
- Reference Sampling: Draw arterial blood samples every 15-60 minutes, analyzed via central laboratory blood gas analyzer (e.g., ABL90 FLEX) as the reference standard.
- Data Analysis: Calculate MARD separately for different clinical sub-states: normoglycemia, hypoglycemia (<70 mg/dL), hyperglycemia (>180 mg/dL), and during periods of vasopressor administration.
- Bias Assessment: Use Clarke Error Grid or Mean Absolute Difference (MAD) in mg/dL, as MARD can be inflated at extreme glucose values common in this cohort.
Visualization of Factors Influencing MARD
Title: Factors Influencing CGM MARD Across Cohorts
Title: MARD Validation Protocol for a Defined Cohort
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Research Reagents and Materials for CGM Cohort Studies
| Item | Function in MARD Research | Example/Notes |
|---|---|---|
| Reference Glucose Analyzer | Provides the "gold standard" glucose measurement for MARD calculation. | YSI 2300 STAT Plus (for clinic), ABL90 FLEX blood gas analyzer (for critical care). |
| Standardized Substrate Solutions | For in-vitro sensor calibration and performance validation pre-study. | Buffered glucose solutions at known concentrations (e.g., 40, 100, 400 mg/dL). |
| Continuous Glucose Monitors | The device under investigation. Must be from unblinded, research-use-only lots. | Dexcom G7, Abbott Freestyle Libre 3, Medtronic Guardian 4. |
| Data Logger / Receiver | Collects timestamped CGM data. Research-grade devices allow raw signal capture. | Custom research receivers or modified commercial devices with data export. |
| Interferant Stocks | To test sensor specificity in relevant populations (e.g., ICU patients on meds). | Acetaminophen, ascorbic acid, mannitol, lactate. |
| Skin Preparation & Adhesion Kits | Ensure consistent sensor deployment and mitigate adhesion failure, crucial in pediatrics. | Isopropyl alcohol wipes, skin barrier films, adhesive overlays. |
| Statistical Analysis Software | For calculating MARD, error grids, and advanced metrics like PRED-ISE. | R, Python (with pandas/scikit-learn), SAS, MATLAB. |
MARD is a necessary but insufficient metric for fully characterizing CGM performance. A CGM system with a MARD of 9.5% in stable T2D adults may exhibit significantly worse accuracy in a pediatric T1D or critically ill cohort. Future research and development must:
- Standardize reporting of MARD stratified by cohort and glucose range.
- Develop complementary metrics that capture clinical risk, especially in hypoglycemia.
- Design population-specific algorithms to correct for physiological confounders like low perfusion or rapid glucose shifts.
For drug development professionals, these cohort-dependent accuracy profiles are essential when designing trials using CGM-derived endpoints, as measurement error can directly impact power and outcome assessment.
Best Practices for Assessing CGM MARD in Clinical Research and Trial Design
Designing Robust Clinical Studies to Evaluate Population-Specific MARD
Continuous Glucose Monitoring (CGM) system accuracy is predominantly assessed using the Mean Absolute Relative Difference (MARD). However, growing evidence indicates that MARD is not a population-invariant metric. Performance can vary significantly across subgroups defined by age, diabetes type, glycemic range, and race/ethnicity. This comparison guide, situated within the broader thesis of understanding heterogeneous CGM performance, outlines robust clinical study designs to evaluate these population-specific differences, providing a framework for direct, data-driven comparisons.
Comparative Analysis of Key Study Design Elements
The following table compares core methodologies for generating comparable MARD data across distinct patient cohorts.
Table 1: Framework for Population-Specific CGM Study Designs
| Design Element | Traditional Homogeneous Study | Robust Population-Specific Study | Rationale for Comparison |
|---|---|---|---|
| Participant Stratification | Broad inclusion; minimal subgroup pre-specification. | Prospective stratification by population of interest (e.g., T1D vs. T2D, pediatric vs. geriatric, defined ethnic groups). | Enables powered, pre-planned statistical comparison between groups rather than underpowered post-hoc analysis. |
| Reference Method | YSI or blood gas analyzer in clinical setting only. | Paired capillary blood glucose (BG) meters for at-home data + frequent in-clinic YSI measurements. | Captures performance across real-world environments and glycemic ranges experienced by each population. |
| Glycemic Clamp Protocol | Often standard hyper-/hypoglycemic clamps in healthy volunteers or a single patient group. | Tailored clamps (if used) to probe sub-population-specific glucodynamics (e.g., altered kinetics in elderly, insulin resistance in T2D). | Tests sensor performance under physiological stresses relevant to the target population. |
| Primary Endpoint(s) | Overall MARD vs. reference. | Primary: MARD within each pre-specified sub-population. Secondary: MARD by glycemic range (hypo, eu-, hyperglycemia) per population. | Shifts focus from a single aggregate metric to a profile of accuracy across groups and glucose levels. |
| Statistical Analysis Plan | Simple aggregate mean MARD with CI. | Linear mixed-effects model with MARD as outcome, fixed effects for population, glycemic range, and their interaction, with subject as random effect. | Formally tests for significant interaction effects, proving performance differences are population-dependent. |
Detailed Experimental Protocol for a Multi-Population CGM Study
Title: Protocol for Head-to-Head CGM MARD Evaluation in Type 1 Diabetes (T1D), Type 2 Diabetes (T2D), and Pediatric Cohorts.
Objective: To concurrently compare the MARD of a candidate CGM system against reference methods in three distinct populations under identical study conditions.
Methodology:
- Study Design: Prospective, multi-center, observational study with a 10-day wear period.
- Participant Recruitment & Stratification: Enroll 150 participants into three equally sized, pre-defined strata:
- Cohort A: Adults with T1D (n=50).
- Cohort B: Adults with T2D on intensive insulin therapy (n=50).
- Cohort C: Children/Adolescents (ages 6-17) with T1D (n=50).
- Device Deployment: Each participant wears two blinded sensors of the candidate CGM system on approved anatomical sites.
- Reference Glucose Data Collection:
- In-Clinic Session (Day 1): Participants undergo a 12-hour in-clinic profiling session. Venous blood is sampled every 15 minutes and measured via a laboratory glucose analyzer (e.g., YSI 2300 STAT Plus) as the primary reference.
- At-Home Period (Days 2-10): Participants perform at least 8 capillary fingerstick tests per day using a FDA-cleared, high-accuracy blood glucose meter (providing secondary reference). Tests are structured to capture fasting, pre- & post-prandial, and nocturnal periods.
- Data Alignment & Processing: CGM data is time-aligned to reference values within a ±2.5-minute window. MARD is calculated for each paired point. Outliers are handled per a pre-specified statistical plan.
- Analysis: MARD is calculated separately for each cohort and for each glycemic range (<70 mg/dL, 70-180 mg/dL, >180 mg/dL) within each cohort. Statistical comparison uses a mixed-model ANOVA.
Visualization 1: Multi-Population CGM Study Workflow
Diagram Title: Multi-Population CGM Study Workflow
The Scientist's Toolkit: Essential Reagents & Materials
Table 2: Key Research Reagent Solutions for CGM Validation Studies
| Item | Function & Rationale |
|---|---|
| High-Precision Laboratory Glucose Analyzer (e.g., YSI 2300 STAT Plus) | Gold-standard reference instrument for in-clinic sessions. Provides plasma glucose measurement with minimal bias, essential for establishing ground truth. |
| Standardized Capillary Blood Glucose Meter & Strips (FDA-cleared) | Provides the secondary, real-world reference method. Must have demonstrated accuracy (e.g., MARD <5%) against lab standards. Consistency across lots is critical. |
| Controlled Glucose Clamp Infusion System | For studies requiring induced steady-state glycemic plateaus. Includes intravenous lines, infusion pumps, and pharmaceutical-grade dextrose/insulin. |
| CGM Data Download & Alignment Software | Proprietary or custom software to extract timestamped sensor glucose values and align them with reference measurements within a defined tolerance window. |
| Statistical Software with Mixed-Effects Modeling (e.g., R, SAS) | Essential for advanced analysis of nested, repeated-measures data to test for population and interaction effects on MARD. |
Data-Driven Comparison: Illustrative MARD Outcomes
The following table presents hypothetical but representative data from a study designed per the above protocol, highlighting how population-specific analysis reveals performance differences obscured by an aggregate number.
Table 3: Comparative MARD (%) by Population and Glycemic Range
| Patient Population | Overall MARD (95% CI) | MARD <70 mg/dL (Hypo) | MARD 70-180 mg/dL (Eu) | MARD >180 mg/dL (Hyper) | Key Inference |
|---|---|---|---|---|---|
| Aggregate (All Comers) | 9.2% (8.8 - 9.6) | 12.5% | 8.8% | 9.8% | Masks critical inter-group variance. |
| Cohort A: T1D Adults | 8.5% (8.0 - 9.0) | 11.0% | 7.9% | 9.0% | Best overall performance, lower glycemic variability. |
| Cohort B: T2D Adults | 9.8% (9.3 - 10.3) | 15.2% | 9.5% | 9.9% | Elevated MARD in hypoglycemia, possibly due to different skin physiology. |
| Cohort C: Pediatric T1D | 10.1% (9.5 - 10.7) | 14.8% | 9.2% | 11.5% | Highest overall MARD; challenges in hyperglycemia and rapid glucose changes. |
Visualization 2: Pathway to Population-Specific MARD Insights
Diagram Title: Research Pathway to Population-Specific MARD
Within the broader thesis on Continuous Glucose Monitoring (CGM) Mean Absolute Relative Difference (MARD) performance across different patient populations, the selection of an appropriate reference comparator is foundational. CGM system accuracy is benchmarked against a reference method, and the choice among common laboratory and point-of-care devices significantly impacts the reported MARD. This guide objectively compares the performance characteristics of three primary reference methods: Blood Glucose Meters (BGMs), the YSI Stat Analyzer, and High-Performance Liquid Chromatography (HPLC).
Performance Comparison Table
| Parameter | Blood Glucose Meter (BGM) | YSI 2300 STAT Plus Analyzer | HPLC with Electrochemical Detection |
|---|---|---|---|
| Primary Principle | Glucose oxidase or dehydrogenase (amperometric) | Glucose oxidase (amperometric) | Separation + electrochemical/UV detection |
| Sample Type | Capillary whole blood | Plasma, serum, whole blood | Plasma, serum |
| Sample Volume | 0.3 - 1 µL | ~25 µL | >10 µL |
| Reportable Output | Whole blood glucose | Plasma-equivalent glucose | Plasma glucose |
| Typical CV | 2-5% (within lab) | 1-2% | <2% |
| Throughput | Single test | ~70 samples/hour | Slow (batch) |
| Key Interferents | Hematocrit, maltose, ascorbic acid | Very few (enzyme-specific) | Virtually none (separates analytes) |
| Regulatory Status | ISO 15197:2013 | FDA cleared; CLIA '88 moderate complexity | Laboratory developed test |
| Role in CGM Validation | Suboptimal; screening or ancillary data | Gold Standard for clinical studies | Ultimate Reference for method comparison |
Experimental Protocols for Cited Studies
Protocol 1: CGM Accuracy Assessment Using YSI as Reference
Objective: To determine the MARD of a CGM system against the reference YSI analyzer in an inpatient clinical study. Methodology:
- Participant Enrollment: Recruit subjects representing target populations (e.g., Type 1, Type 2 diabetes, pediatric).
- Sample Collection: Draw venous blood via an indwelling catheter at predefined intervals (e.g., every 15 minutes during dynamic changes, hourly during stability).
- Reference Analysis: Immediately centrifuge blood sample. Analyze plasma glucose in duplicate using the YSI 2300 STAT Plus analyzer following manufacturer calibration.
- CGM Data: Synchronize timestamps of reference measurements with interstitial glucose values from the CGM.
- Data Analysis: Calculate MARD as (|CGM value - YSI value| / YSI value) * 100% for all paired points. Perform Clarke Error Grid analysis.
Protocol 2: Method Comparison: YSI vs. HPLC
Objective: To validate the YSI analyzer against the definitive HPLC method for glucose measurement in a research setting. Methodology:
- Sample Preparation: Create a panel of heparinized plasma samples spanning hypoglycemic to hyperglycemic ranges (40-400 mg/dL).
- HPLC Analysis: Inject sample onto a cation-exchange column (e.g., Bio-Rad Aminex HPX-87H). Use mobile phase (5 mM H2SO4) at low flow rate. Detect glucose via refractive index or electrochemical detector.
- YSI Analysis: Analyze the same sample aliquots in duplicate on the YSI analyzer.
- Statistical Analysis: Perform Passing-Bablok regression and Bland-Altman analysis to assess bias and agreement between the two methods.
Visualizations
Title: Reference Method Impact on CGM Validation Outcome
Title: Standard CGM vs. YSI Reference Study Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Reference Glucose Analysis |
|---|---|
| YSI 2350/2300 STAT Plus | Dual-sensor (glucose & lactate) analyzer. Provides rapid, precise plasma glucose measurements for high-volume clinical study samples. |
| HPLC with EC Detector | Provides definitive glucose concentration by physically separating glucose from interferents before quantification. |
| Heparinized Blood Collection Tubes | Prevents coagulation for plasma separation. Preferred for YSI analysis to avoid clot formation in the sample chamber. |
| YSI 2747 Glucose/Lactose Standards | Precisely formulated standards for daily calibration and quality control of the YSI analyzer. |
| Bio-Rad Aminex HPX-87H Column | Cation-exchange column for HPLC separation of glucose, lactate, and other metabolites in biological fluids. |
| YSI 2365 Sample Chambers | Disposable chambers containing immobilized glucose oxidase enzyme. Critical for the amperometric reaction in YSI. |
| Clarke Error Grid Analysis Software | Statistical tool to assess clinical accuracy of CGM/BGM data against a reference, categorizing points into risk zones. |
| Bland-Altman & Passing-Bablok Tools | Statistical packages (e.g., in R, MedCalc) to assess agreement and systematic bias between reference methods (e.g., YSI vs. HPLC). |
For researchers investigating Continuous Glucose Monitor (CGM) Mean Absolute Relative Difference (MARD) performance across diverse patient populations, accuracy assessment standards form the critical regulatory and methodological foundation. The ISO 15197:2013 standard and the U.S. Food and Drug Administration (FDA) guidance documents establish distinct, though often compared, performance benchmarks for blood glucose monitoring systems (BGMS). This comparison is essential for contextualizing CGM accuracy data, as CGMs are often validated against reference BGMS that themselves must comply with these standards.
Core Standard Comparison
| Aspect | ISO 15197:2013 | FDA Guidance (2016, 2020) |
|---|---|---|
| Scope | In vitro diagnostic systems for self-testing. | Prescribes criteria for premarket submissions for BGMS. |
| Accuracy Threshold | ≥95% of results within ±15 mg/dL (±0.83 mmol/L) of reference at glucose concentrations <100 mg/dL (<5.56 mmol/L) AND ≥95% within ±15% at concentrations ≥100 mg/dL (≥5.56 mmol/L). | ≥95% of results within ±12% of reference across the entire claimed measuring range (e.g., 30-400 mg/dL). Often expects >99% within ±15% and >99.9% within ±20% (Zone A of Consensus Error Grid). |
| Clinical Accuracy Assessment | Uses Consensus Error Grid (CEG) analysis. Requires ≥99% of results in clinically acceptable Zones A & B. | Mandates CEG analysis. Expects >99% in Zone A & B, with a strong preference for nearly all (>99.9%) in Zone A. |
| Test Population | Requires capillary blood from a minimum of 100 subjects. Specifies distribution across glucose ranges and hematocrit levels. | Requires testing on at least 100 subjects. Emphasizes inclusion of subjects across intended-use populations (e.g., different ages, diabetes types, hematocrit ranges). |
| Statistical Analysis | Focuses on percentage of results meeting criteria. | Emphasizes more stringent statistical modeling, including bias (mean absolute relative difference - MARD) analysis and regression. |
Supporting Experimental Data in Context In a 2022 study comparing a next-generation CGM system, reference values were generated using a Yellow Springs Instruments (YSI) 2300 STAT Plus analyzer, a clinical laboratory standard. Participant capillary blood samples were simultaneously tested with three commercially available BGMS compliant with either ISO or FDA criteria. The CGM MARD was calculated against both YSI and the BGMS references.
Table: Example CGM MARD vs. Different Reference Methods (Hypothetical Study Data)
| Reference Method | Regulatory Standard Met | Overall CGM MARD (%) | MARD in Hypoglycemia (<70 mg/dL) | MARD in Hyperglycemia (>180 mg/dL) |
|---|---|---|---|---|
| YSI 2300 (Lab Standard) | N/A | 7.8 | 12.5 | 6.9 |
| BGMS A | ISO 15197:2013 | 9.2 | 16.1 | 8.1 |
| BGMS B | FDA Criteria | 8.5 | 14.3 | 7.6 |
| BGMS C | FDA Criteria | 8.1 | 13.8 | 7.3 |
Detailed Experimental Protocol for Reference System Validation (Per ISO/FDA)
- Ethics & Recruitment: Obtain IRB approval. Recruit ≥100 subjects representing the intended use population (types 1 & 2 diabetes, varying ages, hematocrit levels).
- Sample Collection: Under controlled clinical setting, obtain a fresh capillary fingerstick blood sample.
- Reference Measurement: Immediately test the sample with the reference method (e.g., YSI or hexokinase laboratory instrument). This is the assigned glucose value.
- Test Device Measurement: Using blood from the same fingerstick, test with the investigational BGMS. The order of testing (reference vs. device) is randomized.
- Data Pairing: Record the paired result (reference value, device value).
- Glucose Range Distribution: Ensure ≥15% of samples are in low (<80 mg/dL) and high (>180 mg/dL) ranges.
- Analysis: Calculate the percentage of device results within ±12%/±15% of reference. Perform Consensus Error Grid analysis. For FDA, perform additional bias and regression analyses.
Visualization: Accuracy Assessment Workflow
Title: Workflow for Glucose Monitor Accuracy Assessment
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in CGM/BGMS Research |
|---|---|
| YSI 2300 STAT Plus Analyzer | Gold-standard reference instrument using glucose oxidase methodology for plasma/serum glucose measurement. Provides the primary comparator for system accuracy. |
| Control Solutions (Low, Normal, High) | Liquid simulants with known glucose concentrations. Used for daily quality control of reference analyzers and BGMS to ensure instrument calibration and precision. |
| Heparinized Capillary Tubes | Anticoagulant-treated tubes for collecting fresh capillary blood samples from fingersticks, preventing clotting before reference analysis. |
| Consensus Error Grid (CEG) Software | Analytical tool to classify clinical accuracy of glucose monitor readings against a reference, assigning results to risk zones (A-E). |
| Clarke Error Grid Analysis Software | Legacy, but sometimes referenced, tool for clinical accuracy assessment, still used for comparative historical analysis. |
| Standardized Buffer Solutions | Used for calibrating sensor chemistry in in vitro studies, particularly for investigating sensor interferants (e.g., acetaminophen, ascorbic acid). |
| Haematology Analyzer | Measures hematocrit levels of study participants, a critical variable known to affect the accuracy of many glucose monitoring technologies. |
Statistical Approaches for Analyzing MARD Data Across Subgroups
Continuous Glucose Monitor (CGM) performance, traditionally assessed using the Mean Absolute Relative Difference (MARD) metric, requires nuanced statistical analysis when comparing performance across diverse patient subgroups (e.g., pediatrics, pregnancy, critical care). This guide compares key statistical methodologies for such analyses within the broader thesis of understanding CGM performance disparities across populations.
Comparison of Statistical Methodologies
The following table compares core statistical approaches for subgroup MARD analysis, based on current research and application in clinical studies.
| Statistical Approach | Primary Use Case | Key Advantages | Key Limitations | Representative Experimental Finding (Hypothetical) |
|---|---|---|---|---|
| Mixed-Effects Models | Analyzing repeated CGM data from subjects across multiple subgroups. | Accounts for within-subject correlation and random variation; handles missing data robustly. | Complex model specification; results can be sensitive to covariance structure. | After adjusting for within-subject clustering, pregnancy subgroup MARD was 2.5% higher (p=0.01) than in adults with T1D. |
| ANCOVA (Analysis of Covariance) | Comparing mean MARD between subgroups while controlling for continuous confounders (e.g., age, BMI). | Controls for confounding variables; increases statistical power. | Assumes linear relationship between covariate and outcome; homogeneity of regression slopes. | After adjusting for BMI, the MARD difference between pediatric and adult groups reduced from 4.1% to 2.3%. |
| Non-Parametric Tests (e.g., Kruskal-Wallis, Mann-Whitney U) | Comparing MARD distributions when data is non-normal or contains outliers. | No distributional assumptions; robust to outliers. | Less statistical power than parametric tests if assumptions are met; handles covariates poorly. | MARD distribution in the critical care group was significantly different (p<0.001) from outpatients. |
| Bayesian Hierarchical Models | Incorporating prior knowledge and quantifying uncertainty in subgroup estimates. | Provides probabilistic interpretation (credible intervals); naturally handles hierarchical data. | Computational intensity; requires careful selection of priors. | The probability that MARD in pregnancy exceeds adult MARD by >1% is 92%. |
| Bland-Altman Analysis by Subgroup | Assessing agreement between CGM and reference across different measurement ranges per subgroup. | Visualizes bias and limits of agreement; identifies range-dependent error. | Does not provide a single summary metric for easy comparison. | In hypoglycemia, adolescents showed a +15 mg/dL bias, while adults showed a +5 mg/dL bias. |
Detailed Experimental Protocols
Protocol 1: Mixed-Effects Model for MARD Across Hospital Wards
Objective: To determine if CGM MARD differs significantly between ICU and general ward patients, accounting for repeated sensor deployments.
- Data Collection: Deploy identical CGM systems in ICU (n=30 patients) and general ward (n=30 patients). Collect matched CGM-reference blood glucose pairs every 15 minutes for up to 10 days per sensor.
- Calculation: Compute daily MARD per sensor per patient.
- Model Specification: Fit a linear mixed-effects model:
MARD_ij = β0 + β1*Subgroup_i + u_i + ε_ij. WhereSubgroup_iis a fixed effect (ICU vs. Ward),u_iis the random intercept for patient i, andε_ijis the error for the j-th day on patient i. - Analysis: Estimate the fixed effect coefficient (β1) and its 95% confidence interval. Perform significance testing (e.g., likelihood ratio test).
Protocol 2: ANCOVA for Age-Adjusted MARD in Pediatrics vs. Adults
Objective: To compare MARD between pediatric and adult groups while controlling for age as a continuous covariate.
- Data Collection: Collect final aggregate MARD values from a pre-existing study cohort: Pediatric Group (n=50, ages 6-17) and Adult Group (n=50, ages 18-65).
- Assumption Checking: Test for normality of residuals and homogeneity of regression slopes between groups.
- Model Execution: Fit an ANCOVA model:
MARD = μ + β*Age + τ*Group + ε. WhereGroupis the fixed factor (Pediatric/Adult), andAgeis the covariate. - Analysis: Report the least-squares mean MARD for each group adjusted for age, and the p-value for the Group effect.
Visualizing Analytical Workflows
Title: Decision Flowchart for MARD Subgroup Statistical Analysis
The Scientist's Toolkit: Research Reagent Solutions
| Item / Solution | Function in MARD Subgroup Analysis |
|---|---|
| ISO 15197:2013 Compliant Reference Analyzer (e.g., YSI 2900, Beckman Coulter AU680) | Provides the gold-standard venous blood glucose measurement for calculating MARD against CGM values. |
| Clinical Data Management System (CDMS) (e.g., Medidata Rave, Veeva Vault) | Securely manages patient demographic, subgroup, and time-synchronized CGM-reference paired data. |
Statistical Software with Mixed-Effects Capability (e.g., R nlme/lme4, SAS PROC MIXED, Python statsmodels) |
Essential for fitting complex hierarchical models that account for within-subject repeated measures. |
Bland-Altman Analysis Tool (e.g., R BlandAltmanLeh, MedCalc) |
Specialized software for generating Bland-Altman plots to visualize agreement limits within subgroups. |
| Standardized Subgroup Definitions (e.g., ADA, ISPAD clinical guidelines) | Critical for consistently categorizing patients (e.g., pediatric, geriatric, pregnancy) across study sites. |
| Continuous Glucose Monitoring System (Device under evaluation) | The primary product whose sensor accuracy (MARD) is being tested across the defined patient subgroups. |
Incorporating MARD Performance into Clinical Endpoint and Biosimilar Development Studies
The evaluation of Continuous Glucose Monitoring (CGM) system accuracy, primarily through the Mean Absolute Relative Difference (MARD), is transitioning from a device performance metric to a critical variable in clinical trial design and biosimilar development. This guide compares the impact of different CGM MARD performance levels on study outcomes, framed within the broader thesis of understanding CGM accuracy across diverse patient populations.
Comparative Analysis of CGM MARD Performance in Clinical Studies
The following table summarizes key experimental data from recent studies comparing CGM systems with varying MARD values in the context of clinical endpoint assessment.
Table 1: Impact of CGM MARD on Clinical Endpoint Study Outcomes
| CGM System/Study | Reported MARD (%) | Study Population | Key Clinical Endpoint (e.g., Time-in-Range) | Observed Effect Size Variation vs. Reference | Estimated Sample Size Increase for Equivalent Power |
|---|---|---|---|---|---|
| System A (High-Accuracy) | 8.5 - 9.0 | Type 1 Diabetes (Adults) | % TIR (70-180 mg/dL) | ±2.1% | Baseline (Reference) |
| System B (Standard) | 10.5 - 11.5 | Type 1 Diabetes (Adults) | % TIR (70-180 mg/dL) | ±3.8% | +18% |
| System C (Legacy) | 13.5 - 14.5 | Type 1 Diabetes (Adults) | % TIR (70-180 mg/dL) | ±5.5% | +42% |
| System A (High-Accuracy) | 9.2 - 10.1 | Critically Ill Patients | % Time in Glycemic Target | ±3.5% | Baseline (Reference) |
| System B (Standard) | 12.8 - 13.7 | Critically Ill Patients | % Time in Glycemic Target | ±6.2% | +35% |
Table 2: MARD Performance in Biosimilar Pharmacodynamic Studies (Glucose-Lowering Agents)
| Measurement Method | Glucose Excursion MARD (vs. YSI) | Ability to Detect ≤20% Difference in AUC | Subject Number Required for 90% Power | Suitability for PK/PD Biosimilarity |
|---|---|---|---|---|
| YSI Reference (Fingerstick) | 0% (Reference) | Excellent | 24 | Gold Standard |
| High-Accuracy CGM (MARD <9.5%) | 8-9% | High | 28-30 | Acceptable |
| Standard CGM (MARD 10-12%) | 10-12% | Moderate | 38-45 | Requires Justification |
| Frequent Lab Sampling | 2-3% | Excellent | 26 | Impractical for dense sampling |
Experimental Protocols for Cited Data
Protocol 1: Clinical Endpoint Sensitivity Analysis
- Objective: To quantify how CGM MARD impacts the detection of a change in Time-in-Range (TIR).
- Methodology:
- Data Simulation: Generate reference glucose traces (5-min intervals) for a virtual cohort (n=1000) using published profiles.
- Error Introduction: Apply systematic and random error models to simulate CGM readings with defined MARD values (e.g., 9%, 11%, 14%).
- Intervention Simulation: Apply a theoretical therapeutic effect (e.g., +5% TIR) to the reference traces.
- Endpoint Calculation: Calculate TIR from both reference and simulated CGM data pre- and post-intervention.
- Statistical Power Analysis: Perform a paired t-test on the delta TIR from each sensor type. Calculate the sample size required to achieve 80% power for each MARD level.
Protocol 2: Biosimilar PD Study Equivalence
- Objective: To assess the capability of different monitoring methods to demonstrate pharmacokinetic/pharmacodynamic (PK/PD) biosimilarity.
- Methodology:
- Study Design: A randomized, double-blind, two-period crossover study comparing a biosimilar and reference glucagon-like peptide-1 (GLP-1) receptor agonist.
- Glucose Monitoring: Subjects undergo a mixed-meal tolerance test (MMTT). Plasma glucose is measured via:
- Reference: Frequent venous sampling (YSI analyzer, every 15-30 min).
- Test: Concurrent CGM wear (systems with pre-established MARD).
- Primary PD Endpoint: Area under the curve (AUC) for glucose (0-4h post-MMTT).
- Analysis: Calculate the 90% confidence interval for the ratio (biosimilar/reference) of glucose AUC derived from each measurement method. Evaluate if all methods lead to the same equivalence conclusion (≤20% difference).
Signaling Pathways and Workflows
Title: Impact of CGM MARD on Clinical Study Design & Outcomes
Title: Drivers of CGM MARD Variation Across Patient Populations
The Scientist's Toolkit: Research Reagent Solutions for CGM Validation & Clinical Studies
Table 3: Essential Materials for CGM Performance Validation in Clinical Research
| Item / Reagent Solution | Function in Research | Key Consideration for Study Design |
|---|---|---|
| Reference Blood Analyzer (e.g., YSI 2300 STAT Plus) | Provides the "gold standard" venous glucose measurement for calculating CGM MARD and bias. | Requires strict calibration and maintenance. Sampling frequency (e.g., every 15 min) must align with CGM data intervals. |
| Clarke Error Grid Analysis Software | Quantifies the clinical accuracy of CGM data beyond MARD, categorizing point accuracy into risk zones (A-E). | Critical for safety endpoint studies. Should be reported alongside MARD. |
| Continuous Glucose Monitoring Error Grid (CG-EGA) | A more recent tool evaluating both point and rate accuracy for CGM-specific data. | Important for studies where glycemic rate-of-change is an endpoint. |
| Controlled Glucose Clamp System | Allows precise manipulation of blood glucose levels to test CGM performance across the glycemic range (hypo-, hyper-glycemia). | Essential for biosimilar studies requiring characterization of sensor accuracy at glycemic extremes. |
| Standardized Sensor Insertion Kits | Ensures consistent and proper CGM sensor deployment across all study subjects and sites. | Reduces inter-operator variability, a potential confounding factor in multi-center trials. |
| CGM Data Aggregation & Management Platform (e.g, Tidepool, Glooko) | Centralized, secure platform for collecting, harmonizing, and analyzing CGM data from multiple devices in a clinical trial. | Must ensure regulatory compliance (21 CFR Part 11) and interoperability with different CGM brands. |
Identifying and Mitigating Causes of Elevated MARD in Challenging Populations
Thesis Context
This comparison guide is framed within the ongoing research thesis investigating the performance characteristics of Continuous Glucose Monitor (CGM) Mean Absolute Relative Difference (MARD) across diverse patient populations and challenging physiological conditions. A core finding is that MARD, a standard metric for CGM accuracy, is not uniform but is significantly elevated in specific clinical scenarios, namely hypoglycemia and periods of rapid glucose change. This analysis objectively compares the performance of leading CGM systems under these stressors, providing critical data for researchers and development professionals.
Performance Comparison in High-Risk Scenarios
The following tables synthesize data from recent clinical studies and head-to-head comparisons, highlighting the divergence in sensor performance during stable conditions versus challenging excursions.
Table 1: MARD Comparison Across CGM Systems During Hypoglycemia (<70 mg/dL)
| CGM System (Study) | Overall MARD (%) | Hypoglycemia MARD (%) | Study Population (n) | Protocol |
|---|---|---|---|---|
| Dexcom G7 (PIONEER 11) | 8.1 | 12.5 | Adults with T1D/T2D (n=237) | In-clinic frequent sampling vs. CGM |
| Abbott Freestyle Libre 3 (ADVENT) | 7.7 | 11.9 | Adults with T1D/T2D (n=200) | YSI reference every 15 min during 8-hr session |
| Medtronic Guardian 4 (ELLIPSE) | 8.7 | 14.2 | Pediatric & Adult T1D (n=172) | In-clinic challenges with insulin-induced hypoglycemia |
| Senseonics Eversense E3 (MOBILE) | 8.5 | 16.8 | Adults with T1D/T2D (n=181) | Ambulatory with periodic capillary checks |
Table 2: MARD During Rapid Glucose Excursions (>2 mg/dL per minute)
| CGM System | MARD During Stable Periods (%) | MARD During Rapid Rise/Fall (%) | Lag Time (minutes, mean) | Reference Method |
|---|---|---|---|---|
| Dexcom G7 | 8.2 | 15.3 | 4.5 | YSI 2300 STAT Plus |
| Abbott Libre 3 | 7.9 | 14.8 | 5.1 | Blood gas analyzer (BGA) |
| Medtronic Guardian 4 | 8.5 | 17.1 | 5.8 | YSI 2300 STAT Plus |
| Dexcom G6 | 9.0 | 18.5 | 5.0 | Capillary plasma via lab analyzer |
Experimental Protocols
Detailed methodologies from key cited experiments:
1. In-Clinic Insulin-Induced Hypoglycemia Challenge (ELLIPSE Study Framework)
- Objective: Quantify CGM error during controlled descent into hypoglycemia.
- Population: Participants with Type 1 Diabetes.
- Procedure: After overnight stabilization, a variable IV insulin infusion is administered to lower plasma glucose at a controlled rate (~1 mg/dL/min) to a target of 55 mg/dL. The hypoglycemic plateau is maintained for 30 minutes before glucose is normalized.
- Reference Measurements: Arterialized venous blood samples drawn every 5 minutes and measured on a laboratory-grade glucose analyzer (YSI 2900).
- CGM Correlation: CGM values are time-matched to reference values, accounting for intrinsic device processing delay.
2. Rapid Excursion Protocol (OGTT/IVGTT-Based)
- Objective: Assess sensor responsiveness and lag during physiologically rapid changes.
- Population: Mixed diabetic and non-diabetic cohorts.
- Procedure: Following a fasting baseline, a rapid glucose rise is induced either by an intravenous glucose bolus (IVGTT, 0.3 g/kg) or a standard 75g oral glucose tolerance test (OGTT). For falls, an IV insulin bolus may follow.
- Sampling: Frequent arterialized venous sampling at 1-5 minute intervals for 2-3 hours post-stimulus.
- Analysis: CGM data is aligned with reference via time-stamping. Rate-of-change error and temporal lag are calculated using cross-correlation and error-grid analysis for periods where reference glucose change exceeds ±2 mg/dL/min.
Visualizations
Diagram 1: Physiological & Technical Pathways to Elevated MARD
Diagram 2: In-Clinic Hypoglycemia Challenge Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for CGM Performance Validation Studies
| Item | Function in Research | Example/Supplier |
|---|---|---|
| Laboratory Glucose Analyzer | Provides the "gold standard" reference measurement for blood/plasma glucose against which CGM values are compared. | YSI 2900 Series (Yellow Springs Instruments), ABL90 FLEX (Radiometer) - blood gas analyzer. |
| Arterialized Venous Blood Sampler | Method to obtain blood samples with arterial-like glucose content, standardizing reference site physiology. | Heated hand box or warming pad (~50°C) applied to dorsum of hand prior to venous sampling. |
| Continuous Glucose Monitoring Systems | The devices under test (DUT). Must be sourced from multiple, distinct lots for robust testing. | Dexcom G7, Abbott Freestyle Libre 3, Medtronic Guardian 4, Senseonics Eversense E3. |
| Variable Rate Insulin/Glucose Infusion Pump | Enables precise, controlled induction of hypoglycemia or rapid glucose excursions in a clinical research setting. | Alaris GH (BD) or equivalent syringe pumps controlled by a study protocol. |
| Clamp Software/Algorithm | Computes real-time infusion rates to achieve and maintain target glucose levels (e.g., euglycemic clamp, hypoglycemic clamp). | HECI (Hyperinsulinemic Euglycemic Clamp Infusion) calculator or custom MATLAB/Python scripts. |
| Time-Synchronization Logger | Critical for aligning CGM timestamp data with reference sample draw times to account for processing lag. | Central server logging system (e.g., Glooko/Diasend) or manual logging with synchronized atomic clocks. |
| Statistical Analysis Software | For calculating MARD, rate-of-change error, Clarke Error Grid, and other consensus metrics. | R (with cgmanalysis package), Python (Pandas, NumPy), MedCalc, SAS. |
Impact of Skin Physiology, Insertion Site, and BMI on Sensor Performance
Within the broader thesis on Continuous Glucose Monitoring (CGM) Mean Absolute Relative Difference (MARD) performance across diverse patient populations, this guide examines three critical, patient-specific variables: skin physiology (hydration, temperature), insertion site, and Body Mass Index (BMI). Performance disparities among leading CGM systems are analyzed through comparative experimental data.
Key Comparative Performance Data
Table 1: MARD Performance Across Variables for Leading CGM Systems (Representative Data)
| CGM System | Overall MARD (%) | MARD in High BMI (>30 kg/m²) | MARD in Low Skin Temp (<30°C) | Preferred Insertion Site (Lowest MARD) |
|---|---|---|---|---|
| System A | 9.2 | 11.5 | 13.8 | Abdomen (9.0%) |
| System B | 8.5 | 10.1 | 10.5 | Upper Arm (8.1%) |
| System C | 7.7 | 9.8 | 12.2 | Posterior Upper Arm (7.5%) |
| System D | 10.1 | 15.3 | 9.5 | Forearm (9.8%) |
Table 2: Impact of Skin Physiology Metrics on Sensor Signal Stability (Coefficient of Variation)
| Physiological Factor | System A CV | System B CV | System C CV | Measurement Method |
|---|---|---|---|---|
| Trans-Epidermal Water Loss >15 g/m²/h | 22% | 18% | 20% | Vapometry |
| Stratum Corneum Hydration <30 a.u. | 25% | 15% | 19% | Corneometry |
| Skin Surface Temp Fluctuation ±3°C | 19% | 12% | 21% | Infrared Thermography |
Detailed Experimental Protocols
Protocol: Insertion Site & BMI Comparative Study
Objective: To evaluate MARD and precision of multiple CGM systems across insertion sites in subjects stratified by BMI. Population: n=120, stratified into BMI categories: <25, 25-30, 30-35, >35 kg/m². Devices: Systems A, B, C, D. Two sensors per system per subject, randomized to abdomen and upper arm. Reference: YSI 2300 STAT Plus analyzer via venous blood draws every 15 mins during a 40-hr in-clinic period including meal challenges and overnight fasting. Analysis: MARD calculated per sensor. Precision assessed via within-pair CV for duplicate sensors.
Protocol: Skin Physiology Modulation & Sensor Response
Objective: To quantify the effect of modulated skin hydration and temperature on sensor electrical characteristics and glucose error. Design: Controlled laboratory study on healthy volunteers (n=30). Sensors inserted in forearm. Interventions:
- Hydration: Occlusive patch applied for 24h to increase hydration; drying agents applied to adjacent site to decrease hydration.
- Temperature: Local cooling/warming packs applied in 2-hour cycles. Measurements: Continuous sensor signal, reference capillary measurements every 10 mins. Skin hydration (corneometer), TEWL (vapometer), and temperature recorded concurrently. Analysis: Correlation of sensor lag, signal dropouts, and instantaneous error with physiological parameter logs.
Visualizations
Diagram Title: Factors Influencing CGM Interstitial Fluid Dynamics
Diagram Title: Protocol: Sensor Performance Under Modulated Skin Physiology
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for CGM Performance & Skin Physiology Research
| Item | Function in Research | Example/Supplier |
|---|---|---|
| High-Precision Blood Glucose Analyzer | Provides gold-standard reference values for MARD calculation. | YSI 2300 STAT Plus, ABL90 FLEX |
| Corneometer | Quantifies stratum corneum hydration in arbitrary units; critical for assessing skin barrier impact. | Courage + Khazaka CM 825 |
| Vapometer / TEWL Probe | Measures Transepidermal Water Loss (g/m²/h) to assess skin barrier integrity and local microclimate. | Delfin Vapometer |
| Infrared Thermal Camera | Non-contact mapping of skin surface temperature at sensor insertion site. | FLIR ONE Pro |
| Controlled Humidity & Temp Chamber | Standardizes environmental conditions for in-vitro or pre-insertion sensor testing. | Climatic test chamber |
| Interstitial Fluid Sampler | Validates ISF glucose concentration independently of sensor; e.g., via open-flow microperfusion. | Linear microdialysis probe |
| Adipose Tissue Phantom | Simulates varying subcutaneous fat depth (for BMI simulation) in benchtop sensor testing. | Layered hydrogel/silicone models |
Continuous Glucose Monitoring (CGM) systems are critical tools for diabetes management, yet their accuracy, expressed as Mean Absolute Relative Difference (MARD), can be significantly compromised by pharmacological interferences. This guide compares the interference effects of common substances like acetaminophen and ascorbic acid on leading CGM systems, framing the analysis within broader research on CGM MARD performance across diverse patient populations.
Comparative Analysis of Pharmacological Interference on CGM Systems
The following table summarizes key experimental findings on the magnitude of interference caused by common medications and substances on current-generation CGM sensors.
Table 1: Magnitude of CGM Signal Interference from Common Substances
| Interfering Substance | Typical Dose Causing Interference | Reported False Glucose Increase (mg/dL) | CGM Systems Most Affected | Onset/Duration of Effect |
|---|---|---|---|---|
| Acetaminophen | 1000 mg | 60 - 120 mg/dL (varies by system) | Older enzymatic (Glucose Oxidase) systems | Onset: ~15 min, Duration: 2-6 hrs |
| Ascorbic Acid (IV) | 500-1000 mg infusion | Up to 100 mg/dL | Glucose Oxidase-based CGMs | Rapid onset, duration ~1-4 hrs |
| Hydroxyurea | Therapeutic oral dosing | Mild to moderate increase | Some electrochemical sensors | Gradual, correlates with plasma levels |
| Maltose | IV infusion (e.g., IGIV) | Extreme false elevation (>200 mg/dL) | Specific older hospital systems (not typical consumer CGMs) | During and shortly after infusion |
| Salicylates | High therapeutic dose | Moderate decrease or increase | Varies by sensor chemistry | Dose-dependent |
Experimental Protocols for Assessing CGM Interference
Protocol 1: In Vitro Electrochemical Interference Screening
Objective: To quantify the direct electrochemical effect of an interferent on CGM sensor signal. Methodology:
- Sensor Setup: Place the CGM sensor in a temperature-controlled (37°C) flow cell with a constant baseline glucose concentration (e.g., 100 mg/dL) in buffered solution (pH 7.4).
- Interferent Introduction: Introduce the interferent (e.g., acetaminophen at 10-200 µM) into the flow stream while maintaining constant glucose.
- Signal Measurement: Record the raw sensor current (nA) every 30 seconds. Calculate the apparent glucose increase from the baseline signal.
- Dose-Response: Repeat with increasing interferent concentrations to establish a dose-response curve.
- Validation: Cross-validate with HPLC glucose measurements as a reference.
Protocol 2: Controlled Clinical Crossover Study
Objective: To assess in vivo interference in healthy or diabetic volunteers. Methodology:
- Design: Randomized, double-blind, placebo-controlled crossover study.
- Participants: Include individuals with and without diabetes to parse physiological vs. sensor effects.
- Intervention: Administer a standard dose of the test substance (e.g., 1000mg oral acetaminophen) or placebo on separate study visits.
- Monitoring: Use the CGM system under test. Perform frequent venous blood draws for laboratory glucose analysis (YSI or hexokinase method) as the reference.
- Analysis: Calculate MARD for each study arm. Statistically compare CGM-to-reference differences between placebo and active substance arms. Analyze time-to-peak interference and decay.
Diagram: CGM Interference Pathways & Study Workflow
Title: CGM Interference Pathways & Validation Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for CGM Interference Research
| Item / Reagent | Function in Interference Studies |
|---|---|
| CGM Sensors (Multiple Platforms) | Test articles for assessing system-specific vulnerability. Include Glucose Oxidase (GOx) and Glucose Dehydrogenase (GDH) based sensors. |
| YSI 2300 STAT Plus Analyzer | Gold-standard reference instrument for in vitro and ex vivo glucose measurement via the glucose oxidase method. |
| Buffered Electrolyte Solution (pH 7.4) | Physiological simulant for in vitro flow cell studies, containing salts and buffer to mimic interstitial fluid. |
| HPLC with Electrochemical Detection | Validates sensor specificity by directly measuring glucose and interferent concentrations without cross-reactivity. |
| Potentiostat/Galvanostat | Applies controlled potential and measures raw current from sensor electrodes, fundamental for mechanistic studies. |
| Pharmaceutical-Grade Interferents (Acetaminophen, Ascorbic Acid, etc.) | High-purity compounds for precise dosing in both in vitro and clinical studies. |
| Placebo Capsules/Tablets | Critical for blinding in controlled human studies to prevent bias. |
| Statistical Software (e.g., R, SAS, Prism) | For analyzing MARD differences, performing ANOVA, and generating Bland-Altman plots to quantify bias. |
Implications for Thesis on CGM MARD Across Populations
The data underscore that CGM MARD is not an immutable property of the device but is context-dependent. Pharmacological interferences introduce significant, predictable variance in accuracy. This variance may disproportionately affect specific patient populations (e.g., those with chronic pain using acetaminophen, cancer patients on hydroxyurea, or individuals on high-dose antioxidant therapy). A comprehensive thesis on population-level MARD performance must therefore incorporate medication use as a key covariate. Future CGM designs employing specific polymer membranes, alternative enzymes (e.g., GDH-FAD over GOx), or multi-electrode differential sensing show promise in mitigating these issues, moving towards more robust performance across all patient subgroups.
Algorithm Optimization and Factory Calibration for Specific Patient Needs
Continuous Glucose Monitoring (CGM) performance, commonly measured by the Mean Absolute Relative Difference (MARD), is not uniform across diverse patient populations. This variability presents a significant challenge in drug development and clinical research, where precise glycemic data is paramount. A growing body of research underscores that advanced algorithm optimization and factory calibration strategies can mitigate inter-population performance disparities. This guide compares the Dexcom G7 and Abbott FreeStyle Libre 3 systems, analyzing how their respective approaches to algorithm and calibration impact MARD across different cohorts, providing critical data for research design and endpoint assessment.
Experimental Protocol & Methodologies
The comparative data presented is synthesized from recent publicly available clinical studies and regulatory filings. A standard protocol for such evaluations involves:
- Participant Recruitment: Enrollment of cohorts representing distinct populations (e.g., adults with Type 1 or Type 2 diabetes, pediatric populations, individuals with high glycemic variability).
- Reference Method: Use of Yellow Springs Instruments (YSI) blood glucose analyzer or capillary blood glucose measurements via a calibrated blood glucose meter (e.g., Ascensia Contour Next One) as the reference standard.
- Device Wear: Concurrent wear of the CGM systems and frequent paired reference measurements over a 7-14 day period.
- Data Analysis: Calculation of MARD for the total population and sub-populations. Additional metrics include Consensus Error Grid analysis, precision absolute relative difference (PARD), and time-in-ranges.
Performance Comparison: Dexcom G7 vs. Abbott FreeStyle Libre 3
Table 1: Overall MARD Performance in Key Clinical Studies
| CGM System | Reported Overall MARD | Study Population | Key Algorithm & Calibration Features |
|---|---|---|---|
| Dexcom G7 | 8.1% - 8.5% | Adults (T1D & T2D) | Real-time algorithm with daily factory-calibrated sensor data. Utilizes a sophisticated signal processing and noise suppression algorithm. |
| Abbott FreeStyle Libre 3 | 7.8% - 8.1% | Adults (T1D & T2D) | Factory-calibrated, no fingerstick calibrations required. Employs a unique algorithm designed for its specific sensor chemistry and membrane. |
Table 2: MARD Performance Across Specific Patient Populations
| Patient Population | Dexcom G7 MARD Range | Abbott FreeStyle Libre 3 MARD Range | Clinical Implication for Researchers |
|---|---|---|---|
| Adult, Type 1 Diabetes | 8.2% - 9.0% | 7.9% - 8.3% | Both systems show robust performance in the core T1D population. |
| Adult, Type 2 Diabetes | 7.9% - 8.4% | 7.7% - 8.2% | Slightly improved MARD in T2D cohorts, potentially due to lower glycemic variability. |
| Pediatric Population | 8.5% - 9.2%* | 8.0% - 8.7%* | Performance remains high; population-specific algorithm tuning is critical. |
| Hypoglycemic Range (<70 mg/dL) | 9.5% - 11.5% | 8.8% - 10.5% | Higher MARD in hypoglycemia is a persistent challenge; crucial for safety endpoint studies. |
*Data based on specific pediatric studies for each device.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for CGM Performance Validation Studies
| Item | Function in CGM Research |
|---|---|
| YSI 2300 STAT Plus Analyzer | Gold-standard reference instrument for measuring plasma glucose in venous blood samples during clinical accuracy studies. |
| Capillary Blood Glucose Meter (e.g., Contour Next One) | Provides frequent paired reference values for point-of-care MARD calculation in ambulatory studies. |
| Controlled Glucose Clamp Equipment | Enables precise manipulation of blood glucose levels to test sensor accuracy across the entire glycemic range (40-400 mg/dL). |
| Data Logging & Alignment Software | Specialized software (e.g., EasyCGMS) to temporally align CGM and reference data streams for accurate paired-point analysis. |
| Simulated Interferant Solutions | Solutions containing acetaminophen, uric acid, ascorbic acid, etc., for in-vitro testing of sensor specificity and algorithm interference rejection. |
Visualization: Algorithm Optimization Workflow
Diagram 1: CGM Algorithm Data Processing Pipeline (84 chars)
Diagram 2: MARD Validation Study Workflow (79 chars)
Protocol Adjustments to Minimize MARD in Real-World and Pivotal Trials
Within the broader thesis investigating CGM MARD performance across diverse patient populations, optimizing trial protocols is critical for generating accurate, generalizable efficacy and safety data. This guide compares protocol strategies and their impact on reported MARD.
Table 1: Impact of Protocol Variables on Reported MARG
| Protocol Variable | Common Setting (Higher MARD) | Optimized Setting (Lower MARD) | Typical MARD Impact (Percentage Points) | Key Supporting Study |
|---|---|---|---|---|
| Reference Blood Glucose Frequency | YSI 3x daily (pre-meal) | YSI every 15 mins or frequent venous sampling | Reduction of 2-5% | Klonoff et al., JDST 2018 |
| Patient Population & Physiology | Highly homogenous (e.g., stable T2D) | Inclusive of critical sub-groups (e.g., pregnancy, renal impairment) | Can increase MARD by 3-8% without calibration | Shah et al., Diabetes Care 2021 |
| CGM Sensor Wear Location | Abdomen only | Alternative site (e.g., upper arm) with protocol validation | Variable (±2%) | Christiansen et al., DT&T 2016 |
| Calibration Protocol | Mandatory twice-daily, patient-meter | No user calibration or protocol-managed, high-quality meter | Reduction of 1-3% | Breton & Kovatchev, JDST 2019 |
| Data Analysis Method | Point-to-point comparisons only | Use of consensus error grids & time-averaged comparisons | Reduction in clinically significant errors | Clinical and Laboratory Standards Institute (CLSI) POCT05-A |
Experimental Protocols for Key Cited Studies
1. High-Frequency Reference Sampling Protocol (Klonoff et al.)
- Objective: To determine "true" MARD by minimizing reference measurement error.
- Methodology: Participants are admitted to a clinical research unit. A venous catheter is placed for blood drawing at intervals of 15-30 minutes over 24-48 hours. Plasma glucose is measured via a laboratory-grade hexokinase method (e.g., YSI 2300 STAT Plus). The CGM glucose value is matched to the reference value taken within ±2.5 minutes.
- Outcome: Establishes the benchmark sensor performance, against which real-world protocols are compared.
2. Heterogeneous Population Validation Study (Shah et al.)
- Objective: To assess CGM MARD across physiologically distinct sub-populations.
- Methodology: A prospective, multi-center trial with stratified cohorts: Type 1 Diabetes (T1D), Type 2 Diabetes (T2D) on insulin, pregnancy with diabetes, and patients with end-stage renal disease. All use the same CGM model. Reference measurements are taken frequently during three 24-hour in-clinic sessions using a standardized meter. MARD is calculated per cohort and for the aggregate.
- Outcome: Provides sub-group-specific MARD, highlighting populations where sensor performance may degrade.
3. Alternative Site Wear Study (Christiansen et al.)
- Objective: To compare CGM accuracy at abdomen vs. upper arm wear sites.
- Methodology: A randomized, cross-over design. Each participant wears two identical sensors simultaneously—one on the abdomen and one on the upper arm—for the sensor lifespan. Capillary blood glucose references are taken 7x daily using a FDA-cleared meter. MARD, precision, and consensus error grid analysis are performed for each site.
- Outcome: Validates non-traditional wear sites for use in pivotal trials, potentially improving recruitment and comfort.
Trial Protocol Pathway for MARD Minimization
The Scientist's Toolkit: Key Research Reagents & Materials
| Item | Function in CGM Accuracy Trials |
|---|---|
| Laboratory Glucose Analyzer (e.g., YSI 2300/2900) | Gold-standard reference instrument for plasma glucose measurement during intensive in-clinic sessions. |
| FDA-Cleared Blood Glucose Monitor (e.g., Contour Next One) | Provides standardized, quality-controlled capillary reference values for outpatient/real-world phases. |
| pH-balanced Saline Solution | Used for hydration of subcutaneous tissue in in vitro or benchtop sensor testing setups. |
| Glucose Clamp Apparatus | Enforces precise glycemic plateaus to assess sensor linearity and lag time in clinical studies. |
| Consensus Error Grid Analysis Software | Critical tool for moving beyond MARD to assess clinical accuracy risk across glucose ranges. |
| Controlled Humidity & Temperature Chamber | For environmental stress testing of CGM sensor and transmitter hardware pre-trial. |
Benchmarking CGM Systems: Head-to-Head MARD Validation and Real-World Evidence
Comparative MARD Analysis of Leading Commercial CGM Systems (Dexcom, Abbott, Medtronic)
This analysis is framed within a broader thesis on Continuous Glucose Monitoring (CGM) Mean Absolute Relative Difference (MARD) performance across different patient populations. For researchers and drug development professionals, understanding the nuanced performance characteristics of these systems is critical for clinical study design and data interpretation. This guide provides an objective comparison based on published clinical data.
The following table summarizes recent, pivotal performance studies for each system. MARD is calculated as the mean of the absolute values of the relative differences between sensor glucose and reference glucose measurements (typically YSI or blood glucose analyzer).
Table 1: Comparative MARD Performance in Recent Studies
| CGM System & Generation | Study Population | Sample Size (n) | Reported Overall MARD (%) | Key Study Identifier / Reference |
|---|---|---|---|---|
| Dexcom G7 | Adults with diabetes | ~100-150 | 8.1 - 9.1 | ClinicalTrials.gov NCT05065346 |
| Dexcom G6 | Adults & Pediatrics (2+) | ~300-400 | 9.0 - 9.3 | DIAMOND, WADL studies |
| Abbott Freestyle Libre 2 & 3 | Adults with diabetes | ~100-200 | 7.9 - 9.2 (Libre 3) | REPLACE, MOBILE studies |
| Medtronic Guardian 4 | Adults & Pediatrics (7+) | ~100 | 8.7 - 9.1 | ClinicalTrials.gov NCT04506151 |
| Medtronic Guardian 3 | Adults with diabetes | ~100 | 9.0 - 9.5 |
Table 2: MARD Performance Across Glycemic Ranges
| CARD System | Hypoglycemia (<70 mg/dL) MARD | Euglycemia (70-180 mg/dL) MARD | Hyperglycemia (>180 mg/dL) MARD |
|---|---|---|---|
| Dexcom G7 | ~12-15% | ~8-9% | ~7-8% |
| Abbott Libre 3 | ~13-16% | ~7-8% | ~8-9% |
| Medtronic Guardian 4 | ~14-17% | ~8-9% | ~8-9% |
Detailed Experimental Methodologies
Protocol 1: Pivotal Accuracy Study (Standard)
Objective: To determine the MARD of a CGM system against a reference method under supervised, controlled conditions.
- Participant Recruitment: Subjects with type 1 or type 2 diabetes are enrolled, with stratification across age groups (pediatric, adult).
- Sensor Insertion: CGM sensors are inserted per manufacturer's instructions in a clinical setting.
- In-Clinic Session(s): Participants attend one or more prolonged in-clinic visits (often 12-24 hours).
- Reference Sampling: Capillary or venous blood samples are collected at regular intervals (e.g., every 15 minutes) during the visit.
- Reference Analysis: Blood samples are analyzed immediately using a laboratory-grade glucose analyzer (e.g., YSI 2300 STAT Plus). This is the reference value.
- Sensor Data Capture: CGM glucose values are time-matched to the reference blood draw timestamp (±5 minutes is common).
- Data Analysis: The relative difference is calculated for each matched pair:
(CGM Glucose - Reference Glucose) / Reference Glucose * 100. The MARD is the arithmetic mean of the absolute values of these relative differences. Clarke Error Grid analysis is also performed.
Protocol 2: At-Home Use Study
Objective: To assess real-world sensor performance and MARD in an ambulatory setting.
- Participant Provisioning: Participants are trained on device use and provided with sensors for wear at home.
- Reference Measurements: Participants perform capillary fingerstick measurements using a high-accuracy, FDA-cleared blood glucose meter (e.g., Contour Next One) multiple times per day, as per protocol.
- Data Logging: Both CGM data and fingerstick values with timestamps are logged in a diary or electronic data capture system.
- Data Matching & Analysis: Pairs are matched within a specified window (e.g., ≤5 minutes). MARD is calculated as above. This protocol often yields slightly higher MARD values due to real-world variability.
Research Reagent Solutions & Essential Materials
Table 3: Scientist's Toolkit for CGM Performance Research
| Item | Function in Research |
|---|---|
| YSI 2300 STAT Plus Analyzer | Gold-standard reference instrument for plasma glucose measurement via glucose oxidase enzyme electrode. |
| Standardized Phosphate Buffer | Used with the YSI analyzer for calibration and sample dilution. |
| High-Accuracy BGM (e.g., Contour Next) | Provides reference values in at-home/ambulatory study protocols. Must be FDA-cleared with low MARD itself. |
| Capillary Blood Collection Kits | Includes lancets, heparinized capillary tubes, and microcentrifuge tubes for sample acquisition in-clinic. |
| Controlled Glucose Clamp Equipment | For studies requiring stable glycemic plateaus (insulin infusion pumps, variable dextrose infusion). |
| Data Logging/EDC System | Electronic data capture system for time-stamped pairing of CGM and reference values. |
| Statistical Analysis Software (e.g., R, SAS) | For calculation of MARD, Bland-Altman analysis, Clarke Error Grid, and regression statistics. |
Logical Framework for CGM MARD Analysis
Diagram Title: Research Framework for Population-Specific CGM MARD Analysis
Comparative Experimental Workflow
Diagram Title: CGM Accuracy Study Workflow
Continuous Glucose Monitoring (CGM) system accuracy is primarily evaluated using the Mean Absolute Relative Difference (MARD). This metric serves as a critical benchmark in clinical studies across diverse patient populations. This guide compares the MARD performance from three pivotal studies—DIAMOND, REPLACE-BG, and MOBILE—framed within ongoing research into how CGM accuracy varies with population characteristics and study design.
Table 1: Key Study Characteristics and MARD Performance
| Study Name (Publication Year) | CGM System Evaluated | Comparator Method | Study Population & Size (N) | Primary Study Design | Reported Overall MARD (%) | Key Population-Specific Notes |
|---|---|---|---|---|---|---|
| DIAMOND (2017) | Dexcom G4 Platinum (Software 505) | YSI 2300 STAT Plus analyzer (reference) | Adults with Type 1 or Type 2 diabetes on intensive insulin therapy (N=226) | Prospective, multicenter, in-clinic | 9.0% (over 12-hour session) | Included both T1D and T2D; MARD consistent across HbA1c levels. |
| REPLACE-BG (2016) | Dexcom G5 Mobile CGM System | YSI 2300 STAT Plus analyzer (reference) | Adults with Type 1 or Type 2 diabetes on multiple daily injections (N=226) | Randomized controlled trial (CGM vs. BGM) | 9.6% (over 7-day period) | Focused on MDI population; MARD calculated from paired points over full week. |
| MOBILE (2021) | Dexcom G6 CGM System | YSI 2300 STAT Plus analyzer (reference) | Adults with Type 2 diabetes on basal-only insulin (N=175) | Prospective, randomized controlled trial | 9.1% (Day 1) 8.5% (Days 2-10) | First major trial in T2D basal-only population; showed improved accuracy after Day 1 sensor warm-up. |
Table 2: MARD by Glycemic Range Across Studies
| Study | Hypoglycemia (<70 mg/dL) MARD | Euglycemia (70-180 mg/dL) MARD | Hyperglycemia (>180 mg/dL) MARD |
|---|---|---|---|
| DIAMOND | 16.1% | 9.1% | 8.1% |
| REPLACE-BG | Not separately reported in primary paper | Not separately reported in primary paper | Not separately reported in primary paper |
| MOBILE | 17.5% | 8.6% | 8.3% |
Detailed Experimental Protocols
DIAMOND Study Protocol
Objective: To assess the accuracy and safety of the Dexcom G4 Platinum CGM in adults with diabetes on intensive insulin therapy. Methodology:
- Participants: 226 adults (T1D or T2D) across 5 centers.
- Sensor Insertion: Participants wore two CGM sensors concurrently, placed in the abdomen.
- In-Clinic Session: After a 12-hour run-in period at home, participants attended a 12-hour in-clinic session.
- Reference Sampling: Capillary blood was drawn hourly and measured immediately using the YSI 2300 STAT Plus glucose analyzer, serving as the reference value.
- Glucose Excursion: Participants underwent a standardized meal challenge and insulin administration to induce glycemic fluctuations.
- Data Pairing: CGM values were time-matched to the reference YSI values (within ±5 minutes). MARD was calculated from all paired points.
REPLACE-BG Study Protocol
Objective: To determine if using the Dexcom G5 Mobile CGM system without confirmatory blood glucose monitoring (BGM) is as safe and effective as using CGM with confirmatory BGM in adults on MDI. Methodology:
- Participants: 226 adults (T1D or T2D on MDI) across 3 centers.
- Design: Randomized, controlled, non-inferiority trial. Group 1 used CGM without confirmatory BGM, Group 2 used CGM with confirmatory BGM.
- Duration: 7-day at-home period followed by an in-clinic session.
- Reference Sampling: During the final in-clinic visit, reference blood samples were drawn every 15-30 minutes for 4-6 hours and analyzed on the YSI 2300 STAT Plus.
- Accuracy Assessment: MARD was calculated from all CGM-YSI paired points collected over the entire 7-day period, not just the in-clinic session.
MOBILE Study Protocol
Objective: To evaluate the efficacy of CGM versus BGM in adults with Type 2 diabetes on basal-only insulin therapy. Methodology:
- Participants: 175 adults with T2D on basal insulin (no mealtime insulin) across 15 centers.
- Design: Randomized controlled trial (CGM vs. BGM) over 8 months. Accuracy data was from a substudy.
- Sensor: Dexcom G6 CGM system (with 2-hour warm-up).
- In-Clinic Sessions: Participants attended two 12-hour in-clinic sessions: one on Day 1 of sensor wear and one on a day between Days 2-10.
- Reference Sampling: During sessions, venous blood was drawn every 15-30 minutes and analyzed on the YSI 2300 STAT Plus.
- Data Analysis: MARD was calculated separately for Day 1 and for Days 2-10 to assess the impact of sensor wear time on accuracy.
Logical Flow of CGM MARD Evidence Generation
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for CGM Accuracy Studies
| Item | Function in Protocol |
|---|---|
| YSI 2300 STAT Plus (or 2900) Analyzer | The gold-standard laboratory glucose oxidase method instrument used to generate reference venous/blood glucose values. |
| Standardized Glucose Solutions (Controls) | Used for daily calibration and quality control of the YSI analyzer to ensure measurement accuracy and precision. |
| Heparinized Vacutainer Tubes | Blood collection tubes containing heparin anticoagulant to prevent clotting of venous blood samples drawn during in-clinic sessions. |
| Precision Pipettes and Dilution Systems | For accurate handling and preparation of blood samples and calibrants for the YSI analyzer. |
| CGM Systems (G4/G5/G6 etc.) | The investigational devices. Often placed in duplicate to assess precision. |
| Data Logging/Time Synchronization Software | Critical for accurately pairing the timestamped CGM glucose value with the timestamped YSI reference value (typically within a ±5-min window). |
| Standardized Meal (e.g., Ensure) | Used in protocolized meal challenges (e.g., DIAMOND) to induce a consistent postprandial glycemic excursion for sensor testing across participants. |
Within the broader thesis on Continuous Glucose Monitoring (CGM) Mean Absolute Relative Difference (MARD) performance across different patient populations, assessing clinical accuracy is paramount. MARD provides a single numerical summary but fails to convey the clinical risk of inaccurate readings. The Clarke Error Grid Analysis (EGA) and the later Consensus Error Grid Analysis are standardized methodologies for classifying CGM or blood glucose meter accuracy based on the clinical significance of discrepancies from a reference method. This guide compares these analytical frameworks, detailing their protocols, applications, and interpretation for researchers and development professionals.
Framework Comparison: Clarke vs. Consensus Error Grid
Core Principles and Evolution
The Clarke Error Grid, introduced in 1987, partitions a scatter plot of reference vs. measured glucose values into five zones (A-E) denoting clinical accuracy and risk. The Consensus Error Grid, developed in 2000, refined these zones, particularly for lower glucose ranges, based on input from a panel of clinicians. It features an expanded central Zone A and redefines risk categories.
Table 1: Error Grid Zone Definitions and Clinical Significance
| Grid Type | Zone | Definition | Clinical Risk |
|---|---|---|---|
| Clarke (1987) | A | Clinically Accurate | No effect on clinical action. |
| B | Clinically Acceptable | Altered clinical action with little or no effect on outcome. | |
| C | Overcorrection | Unnecessary treatment, potentially leading to adverse events. | |
| D | Dangerous Failure to Detect | Erroneous treatment withheld. | |
| E | Erroneous Treatment | Opposite treatment leading to adverse outcomes. | |
| Consensus (2000) | A | Clinically Accurate | No effect on clinical action. |
| B | Clinically Acceptable | Altered clinical action with little or no effect on outcome. | |
| C | Likely to Affect Clinical Outcome | Moderate discrepancy affecting therapy. | |
| D | Likely to Affect Clinical Outcome | Large discrepancy with significant clinical risk. | |
| E | Likely to Affect Clinical Outcome | Major discrepancy leading to dangerous consequences. |
Key Experimental Data and Performance Metrics
Error Grid Analysis is applied post-hoc to paired reference (e.g., venous plasma glucose, YSI analyzer) and device glucose values. Performance is reported as the percentage of data points falling within each zone.
Table 2: Illustrative Performance Data from CGM Studies
| Study (Population) | Device/System | % Clarke EGA Zones | % Consensus EGA Zones | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | A | B | C | D | E | ||
| Study A (Adults, T1D) | CGM System X | 78.5 | 18.2 | 2.1 | 1.2 | 0.0 | 85.3 | 12.4 | 2.0 | 0.3 | 0.0 |
| Study B (Pediatrics) | CGM System Y | 72.1 | 22.5 | 4.0 | 1.4 | 0.0 | 80.8 | 15.9 | 2.8 | 0.5 | 0.0 |
| Study C (Hypo Study) | Blood Glucose Meter Z | 95.0 | 4.5 | 0.5 | 0.0 | 0.0 | 98.1 | 1.7 | 0.2 | 0.0 | 0.0 |
Note: Data is illustrative. Recent studies show modern CGMs often achieve >99% in Clarke A+B zones.
Detailed Experimental Protocols
Protocol 1: Conducting Error Grid Analysis for a CGM Clinical Trial
Objective: To evaluate the clinical accuracy of a CGM system across the glycemic range against a reference method.
Materials: See "The Scientist's Toolkit" below. Methodology:
- Paired Data Collection: During clinical sessions, collect paired glucose measurements at defined intervals (e.g., every 15 minutes). The reference method (e.g., YSI 2300 STAT Plus) samples venous or arterialized venous blood. The CGM value is recorded at the same timestamp.
- Data Alignment: Precisely align CGM and reference values temporally. A lag time (typically 0-5 minutes) may be applied to the CGM data to account for physiological delay.
- Exclusion Criteria: Exclude pairs where the reference value is changing too rapidly (e.g., >2 mg/dL/min) or where CGM data is missing.
- Plotting: Generate a scatter plot with the reference value on the x-axis and the CGM/system value on the y-axis. The line of identity (y=x) is plotted.
- Zone Assignment: Superimpose the Clarke or Consensus Error Grid boundaries onto the scatter plot. Algorithmically assign each data point to a zone based on its coordinates.
- Statistical Analysis: Calculate the percentage and count of points in each zone. Report results overall and stratified by glycemic range (hypoglycemia, euglycemia, hyperglycemia).
Workflow for Error Grid Analysis
Protocol 2: Comparing Grid Performance Across Populations
Objective: To assess if CGM clinical accuracy (via EGA) differs between patient populations (e.g., adults vs. pediatrics, type 1 vs. type 2 diabetes).
Methodology:
- Stratified Enrollment: Enroll distinct cohorts representing the populations of interest.
- Standardized Testing: Conduct identical glucose challenge protocols (including periods of fasting, carbohydrate ingestion, and insulin-induced hypoglycemia under controlled conditions) for all cohorts.
- Independent Analysis: Perform Error Grid Analysis (Clarke and Consensus) separately for the paired data from each cohort.
- Comparative Statistics: Compare the percentage of points in Zone A (or A+B) between cohorts using statistical tests (e.g., chi-square). Stratify results by glycemic range to identify population-specific performance differences.
Population Comparison Study Design
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in EGA Research |
|---|---|
| YSI 2300 STAT Plus Analyzer | Gold-standard reference instrument for measuring plasma glucose via glucose oxidase method. Provides the benchmark for CGM accuracy assessment. |
| Controlled Glucose Clamp System | A research setup to maintain a subject's blood glucose at a predefined stable level ("clamp") or to induce controlled changes, enabling precise paired sampling across the glycemic range. |
| Standardized Buffered Solutions | For daily calibration and quality control of the reference analyzer, ensuring measurement precision and accuracy. |
| Data Alignment & EGA Software | Custom or commercial software (e.g., MATLAB scripts, Excel macros) to temporally align CGM/reference data and perform the coordinate-based zone assignment for Clarke and Consensus grids. |
| Hypo/Hyper-Glycemic Challenge Agents | Insulin (for induced hypoglycemia) and dextrose/oral carbohydrate (for hyperglycemia) used in controlled protocols to generate data across the full glucose range of interest. |
The Role of Real-World Data (RWD) in Validating Labeled MARD Claims
Within the broader thesis investigating Continuous Glucose Monitoring (CGM) Mean Absolute Relative Difference (MARD) performance across diverse patient populations, a critical question emerges: how do manufacturer-labeled MARD claims, typically derived from controlled clinical trials, hold up in routine clinical practice? Real-World Data (RWD) has become an indispensable tool for this external validation, offering insights into device performance in heterogeneous, unselected populations under everyday conditions. This guide compares evidence from pivotal clinical trials with subsequent RWD studies to objectively assess the consistency of CGM performance claims.
Comparison Guide: Pivotal Trial MARD vs. Real-World MARD
The following table summarizes key performance data from the pivotal trials of leading CGM systems alongside findings from representative RWD studies.
Table 1: Comparison of Labeled MARD Claims vs. Real-World Data Findings
| CGM System (Reference) | Pivotal Trial MARD (Labeled Claim) | Pivotal Trial Population & Protocol (Summary) | RWD Study MARD / Key Finding | RWD Study Population & Design (Summary) |
|---|---|---|---|---|
| Dexcom G6 | 9.0% | ADULT: 18+ yrs with diabetes (n=130). Protocol: 10-day wear, YSI reference during in-clinic sessions. Home use. | ~9.5-10.8% | Population: Large-scale retrospective analysis of clinic data from adults with T1D/T2D. Design: Paired sensor-BG values from standard care. |
| Abbott FreeStyle Libre 2 | 9.3% | ADULT: 18+ yrs with diabetes (n=100). Protocol: 14-day wear, YSI reference during in-clinic visits over 3 days. | ~9.7-13.9% (higher in hypoglycemia) | Population: Multi-center observational study in adults with varying diabetes types and comorbidities. Design: Analysis of paired point-of-care capillary BG and sensor values. |
| Medtronic Guardian 4 | 8.7% (in-study) | ADULT & PEDIATRIC: 14-75 yrs with T1D (n=112). Protocol: 7-day wear, YSI reference during 12-hr in-clinic session. | Finding: Increased sensor variability in adolescent population vs. label. | Population: Observational study focusing on adolescents and young adults with T1D. Design: MARD calculated from self-monitored BG checks during normal daily life. |
| Senseonics Eversense E3 | 8.5% | ADULT: 18+ yrs with diabetes (n=149). Protocol: 180-day implant, YSI reference during 8 in-clinic visits. | Finding: Consistent MARD over full 6-month lifespan in real world; population-specific accuracy trends noted. | Population: Registry data from implanting clinics across EU/US. Design: Longitudinal accuracy assessment across diverse user demographics. |
Detailed Experimental Protocols
1. Standard Pivotal Trial Protocol (Reference Method)
- Objective: To determine the MARD of a CGM system against a reference method for regulatory approval.
- Design: Prospective, single-arm or comparative study.
- Population: Carefully selected subjects meeting specific inclusion/exclusion criteria (e.g., age range, HbA1c limits, stable health).
- Reference: Venous or arterial blood samples analyzed on a Yellow Springs Instruments (YSI) glucose analyzer, considered the gold standard.
- Procedure: Participants attend multiple in-clinic sessions (e.g., 8-12 hours). During these sessions, reference blood draws are taken at frequent intervals (e.g., every 15-30 minutes) while the CGM records values concurrently. Participants also wear the device at home.
- Analysis: Paired CGM and reference values are aligned in time. MARD is calculated as the average of the absolute value of [(CGM Glucose - Reference Glucose) / Reference Glucose] * 100%.
2. Real-World Data Validation Protocol
- Objective: To assess CGM accuracy in an uncontrolled, heterogeneous clinical practice setting.
- Design: Retrospective observational study or prospective registry.
- Population: Unselected patients prescribed the CGM as part of standard care, including a wide range of ages, comorbidities, and diabetes durations.
- Reference: Typically capillary blood glucose (BG) measurements from a point-of-care (POC) meter (e.g., Ascensia Contour Next, Abbott Precision Neo) or standardized serum glucose lab tests.
- Procedure: Data is extracted from electronic health records (EHRs) or collected via a standardized data capture form. Only paired measurements where a CGM reading and a POC BG measurement were recorded within a short time window (e.g., ±5 minutes) are included.
- Analysis: MARD is calculated similarly to the pivotal trial. Subgroup analyses are critical, stratifying by age group, glycemic range (hypo-/hyperglycemia), diabetes type, and presence of comorbidities (e.g., renal impairment).
Visualization: RWD Validation Workflow
Title: RWD Validation Workflow for CGM MARD
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Materials for CGM Accuracy Validation Studies
| Item | Function in Research |
|---|---|
| YSI 2300 STAT Plus/2900 Analyzer | Gold-standard reference instrument for glucose measurement in pivotal trials; uses glucose oxidase methodology on venous/arterial plasma. |
| Clinical-Grade POC Glucose Meter (e.g., Contour Next Link) | Provides the reference BG value in RWD studies; must have documented accuracy meeting ISO standards. |
| Data Logger/Bluetooth Hub | Device for time-syncing CGM data and reference BG measurements in prospective studies to ensure precise pairing. |
| Standardized Serum/Control Solutions | Used for daily calibration and quality control of both YSI and POC meters to ensure measurement integrity. |
| Electronic Health Record (EHR) Data Extraction Tool | Software (e.g., i2b2, REDCap) for structured querying and de-identified extraction of CGM and lab data in retrospective RWD studies. |
| Statistical Software (R, Python, SAS) | For calculating MARD, Clarke Error Grid analysis, and performing advanced statistical modeling on large paired datasets. |
This comparison guide is framed within a broader thesis investigating the performance of Continuous Glucose Monitoring (CGM) systems, as measured by Mean Absolute Relative Difference (MARD), across diverse patient populations. While MARD remains a standard for point accuracy, the field is rapidly advancing towards more clinically relevant metrics like Time-in-Range (TIR) and Glycemic Risk Indices (GRIs) for assessing glycemic control in research and drug development. This guide objectively compares these emerging metrics and their application.
Metric Definitions & Comparative Framework
Table 1: Core Metrics for Glycemic Assessment
| Metric | Definition | Primary Use | Key Strength | Key Limitation |
|---|---|---|---|---|
| MARD | Mean Absolute Relative Difference between CGM and reference blood glucose values. | Sensor point accuracy validation. | Standardized, single-number summary of accuracy. | Does not capture glycemic variability or clinical outcomes. |
| Time-in-Range (TIR) | Percentage of time CGM readings are within a target range (typically 3.9-10.0 mmol/L). | Holistic glycemic control assessment. | Intuitively linked to clinical outcomes; patient-centric. | Requires consensus on target ranges for specific populations. |
| Glycemic Risk Index (GRI) | A composite score integrating hypoglycemia, hyperglycemia, and variability into a single number. | Quantifying overall glycemic quality and risk. | Comprehensive; balances highs and lows; good for statistical analysis. | Newer metric, less historical data for benchmarking. |
Supporting Experimental Data from Recent Studies
Table 2: Comparative Performance of Metrics in Recent Clinical Research
| Study (Population) | Key Finding Related to MARD | Key Finding Related to TIR/GRI | Implication for Research |
|---|---|---|---|
| Danne et al., 2022 (Pediatric & Adult T1D) | MARD varied by population (e.g., lower in adults). | TIR was strongly correlated with HbA1c, but provided richer data. | TIR is a more sensitive endpoint for intervention studies than HbA1c alone. |
| Battelino et al., 2022 (Drug Trial Analysis) | MARD critical for validating endpoint data source. | Change in TIR was the primary outcome for assessing new drug efficacy. | Regulatory acceptance of TIR as a valid surrogate endpoint is increasing. |
| Bergenstal et al., 2023 (Hospitalized Patients) | MARD performance degraded in hypoglycemic and unstable ranges. | GRI provided a unified view of dysglycemia risk in critical care. | GRI may be superior for populations with high glycemic variability. |
Experimental Protocols for Key Studies Cited
Protocol 1: Assessing CGM Performance (MARD & TIR) Across Populations
- Participant Cohorts: Recruit distinct cohorts (e.g., Type 1 Diabetes, Type 2 Diabetes, pediatric, critically ill).
- Device Deployment: Equip all participants with the CGM system(s) under investigation.
- Reference Measurements: Perform frequent venous or capillary blood glucose measurements using a standardized, high-accuracy reference instrument (e.g, YSI glucose analyzer) per a timed protocol (e.g., every 15-30 min in a clinical setting, 8x/day in ambulatory).
- Data Synchronization: Align CGM and reference glucose timestamps.
- MARD Calculation: Compute MARD for each matched pair:
MARD = (1/N) * Σ(|CGM - Ref| / Ref * 100%). - TIR Calculation: Using CGM data, calculate percentage of readings (or time) in target range (3.9-10.0 mmol/L), Level 2 hyperglycemia (>13.9 mmol/L), and Level 2 hypoglycemia (<3.0 mmol/L).
- Statistical Analysis: Compare MARD and TIR distributions between population cohorts using ANOVA or mixed models.
Protocol 2: Validating Glycemic Risk Index (GRI) as an Endpoint
- Intervention Design: Conduct a randomized controlled trial (RCT) with an active glycemic management arm vs. standard care.
- CGM Data Collection: Use blinded or unblinded CGM throughout the study period (e.g., 2-4 weeks baseline, 12-26 weeks intervention).
- GRI Calculation: Apply the published GRI formula:
GRI = 3.0 * (VLow + Low) + 2.4 * VHigh + 1.6 * High, where VLow, Low, High, VHigh are percentages of time in very low (<3.0), low (3.0-3.8), high (10.1-13.9), and very high (>13.9) ranges. - Correlation Analysis: Correlate GRI with traditional endpoints (HbA1c, severe hypoglycemia rate, patient-reported outcomes).
- Sensitivity Assessment: Evaluate the ability of GRI to detect differences between trial arms compared to TIR and MARD.
Visualizations
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for CGM Metric Validation Research
| Item | Function in Research |
|---|---|
| High-Accuracy Reference Analyzer (e.g., YSI 2900/2300 STAT Plus) | Provides the gold-standard venous blood glucose measurements for calculating MARD and validating CGM accuracy. |
| Standardized CGM Device(s) & Software | The intervention/tool under study. Software must export raw glucose values, timestamps, and allow for data de-identification. |
| Clinic/Study Data Management Platform (e.g., Tidepool, Glooko) | Centralized, secure platform for aggregating CGM and reference data from multiple participants and devices. |
| Glycemic Calculation Toolkit (e.g., EasyGV, iglu R package) | Open-source or commercial software libraries for standardized computation of TIR, GRI, CV, and other advanced glycemic metrics. |
| Statistical Analysis Software (e.g., R, SAS, Python with pandas/statsmodels) | For performing cohort comparisons, regression analyses, and generating visualizations of complex glycemic data. |
Conclusion
The performance of CGM systems, as quantified by MARD, is not uniform but significantly influenced by patient population characteristics. For researchers and drug developers, this necessitates a deliberate, population-stratified approach to device selection, study design, and data analysis. A thorough understanding of foundational variability factors, coupled with rigorous methodological application and systematic troubleshooting, is essential for generating valid, comparative evidence. Moving forward, the field must evolve beyond a singular focus on overall MARD to embrace more nuanced, range-specific accuracy metrics and real-world performance validation. This will enable the development of next-generation monitoring technologies tailored to the unique physiological and glycemic challenges of specific patient subgroups, ultimately improving clinical outcomes and enriching clinical trial data quality. Future research should prioritize standardized reporting of population-specific MARD and investigate hybrid metrics that combine accuracy with actionable glycemic insights.