Closed-Loop Control System Design for the Artificial Pancreas: From Foundational Algorithms to Clinical Implementation
This article provides a comprehensive review of the engineering and algorithmic foundations of Artificial Pancreas (AP) systems for automated glucose management in diabetes.
Closed-Loop Control System Design for the Artificial Pancreas: From Foundational Algorithms to Clinical Implementation
Abstract
This article provides a comprehensive review of the engineering and algorithmic foundations of Artificial Pancreas (AP) systems for automated glucose management in diabetes. Tailored for researchers and drug development professionals, it explores the evolution of closed-loop control from seminal concepts to contemporary hybrid and fully automated systems. The scope encompasses core control methodologies like Model Predictive Control (MPC) and PID, the rise of data-driven approaches including deep reinforcement learning, and the integration of feedforward mechanisms for meal and exercise disturbance rejection. It further details performance validation through clinical trials and in-silico simulations, analyzes prevailing challenges in safety and personalization, and discusses future trajectories involving dual-hormone systems, advanced artificial intelligence, and cyber-physical-human frameworks for precision medicine.
The Evolution of Automated Glycemic Control: From Concept to Standard of Care
The development of the Artificial Pancreas (AP) represents a landmark achievement in the treatment of Type 1 Diabetes (T1D), transforming a once-disputed concept into today's standard of care [1]. This revolutionary technology automates blood glucose management through integrated continuous glucose monitoring (CGM) and insulin delivery, significantly reducing the daily burden of diabetes self-care [2] [3]. The journey from theoretical concept to viable commercial systems spans decades of dedicated research, engineering innovation, and collaborative clinical testing, largely accelerated by strategic support from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and the Juvenile Diabetes Research Foundation (JDRF), now known as Breakthrough T1D [1] [4]. This application note traces the critical developmental pathway of closed-loop systems, documenting key historical milestones, experimental paradigms, and technical specifications to inform ongoing research and development in automated insulin delivery.
Historical Timeline and Key Events
The evolution of artificial pancreas technology has progressed through distinct phases of conceptualization, research, development, and commercialization. The following table summarizes the major milestones in this journey:
Table 1: Historical Milestones in Artificial Pancreas Development
| Year | Milestone Event | Significance | Key Participants/Systems |
|---|---|---|---|
| 2005 | First NIH/JDRF Workshop: "Obstacles and Opportunities on the Road to Artificial Pancreas" [1] | Initiated coordinated movement toward solving AID challenges; room divided on viability of subcutaneous CGM/CSII approach [1] | NIH, JDRF, FDA |
| 2006 | JDRF Artificial Pancreas Project Launch [1] | Issued Request for Applications to initiate formal AP research program [1] | JDRF (Breakthrough T1D) |
| 2007 | First Closed-Loop Human Trial in U.S. [1] | APS platform enabled first U.S. closed-loop human subject trial at UCSB [1] | University of California, Santa Barbara |
| 2008 | FDA Acceptance of Computer Simulator [1] | Accepted simulator as substitute for animal trials, accelerating development by years [1] | Universities of Padova and Virginia, FDA |
| 2008-2012 | Outpatient Studies Progress [1] | Systems tested in camp settings (2008) then patients' homes (2010) [1] | Multiple academic centers |
| 2011 | Diabetes Assistant Platform [1] | First portable AP platform using Android smartphone as computational hub [1] | University of Virginia |
| 2016 | First Commercial Hybrid System FDA Approval [5] | MiniMed 670G became first hybrid closed-loop system cleared for clinical use [5] | Medtronic (670G system) |
| 2016-2018 | Research Publication Peak [1] | >150 publications/year on closed-loop systems; AP "coming of age" [1] | Global research community |
| 2019-2024 | Second-Generation Systems & Algorithm Advancements [6] [7] | Introduction of systems with more adaptive algorithms and simpler initialization [6] | Tandem, Insulet, Beta Bionics |
The progression from concept to clinical adoption demonstrates the effective integration of engineering and medicine. Initial systems utilizing laptop computers were cumbersome and unsuitable for routine outpatient use [1], while contemporary systems leverage sophisticated miniaturized technology with embedded control algorithms [7].
Technical Evolution of AP Systems
System Architecture and Components
Modern Artificial Pancreas systems integrate three core components: a continuous glucose monitor (CGM), an insulin pump, and a control algorithm that functions as the system's decision-making center [2]. The CGM measures interstitial glucose levels via a subcutaneous electrode, transmitting data to a receiver or smart device. Modern sensors like Dexcom G7 and Abbott's FreeStyle Libre 3 offer Mean Absolute Relative Difference (MARD) under 9% and require no calibration [2]. Insulin pumps deliver fast-acting insulin analogues subcutaneously, with modern systems allowing programmable basal rates and bolus profiles [2]. The control algorithm represents the most critical innovation, continuously adjusting insulin infusion based on real-time glucose data and predictive modeling [2].
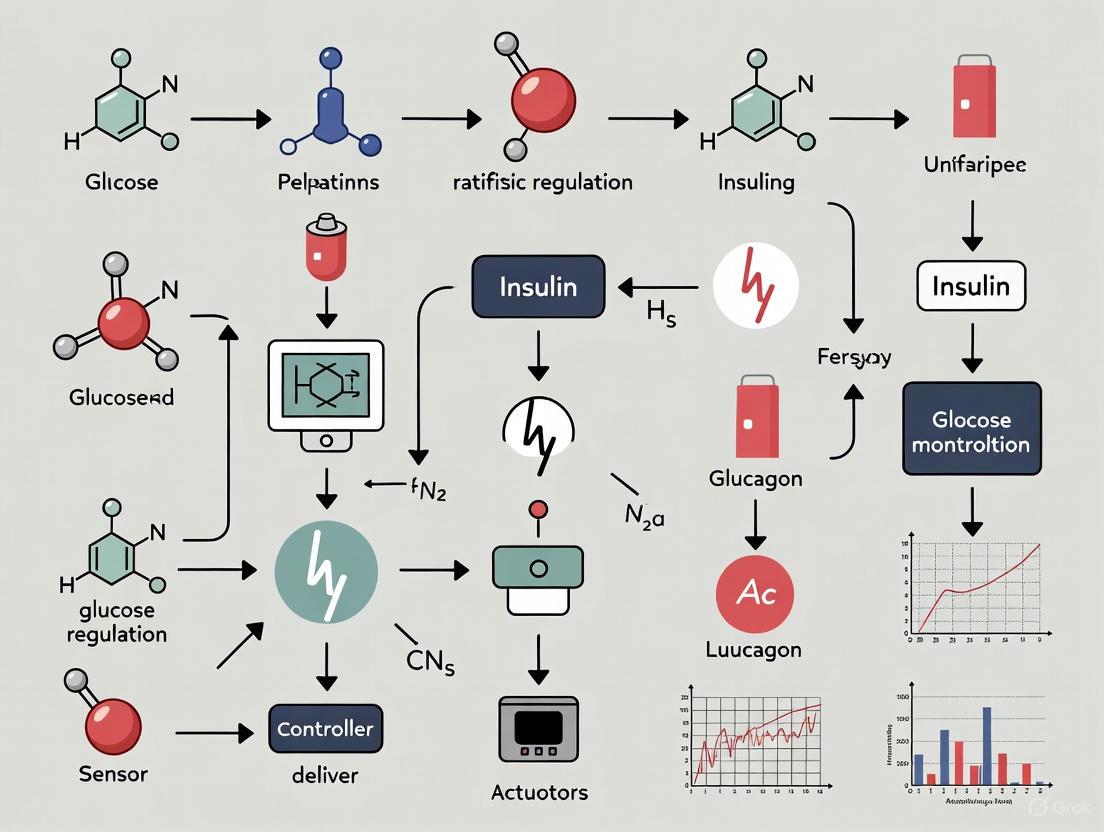
Figure 1: Artificial Pancreas Closed-Loop Control System. The system continuously monitors glucose levels and automatically adjusts insulin delivery in response to real-time data and external disturbances.
Control Algorithm Evolution
Control algorithms have evolved significantly from early prototypes to contemporary sophisticated systems. The two primary algorithm types are Proportional-Integral-Derivative (PID) and Model Predictive Control (MPC) [2]. PID controllers adjust insulin delivery based on current glucose level (proportional), the area under the curve between measured and target glucose (integral), and the rate of change of measured glucose (derivative) [2]. MPC utilizes mathematical models to predict future glucose trajectories and optimize insulin dosing accordingly [2]. More recent approaches incorporate fuzzy logic and deep reinforcement learning to enable more personalized and adaptable insulin dosing [2].
Table 2: Evolution of Control Algorithms in Artificial Pancreas Systems
| Algorithm Type | Core Mechanism | Advantages | Commercial Examples |
|---|---|---|---|
| Proportional-Integral-Derivative (PID) [2] | Adjusts delivery based on current glucose, glucose curve area, and rate of change [2] | Simple, responsive [2] | Medtronic MiniMed systems [1] |
| Model Predictive Control (MPC) [1] [2] | Uses mathematical modeling to predict future glucose trajectories [2] | Forecasting capability [2] | Tandem Control-IQ, CamAPS FX [1] |
| Fuzzy Logic [1] [2] | Codifies clinical decision-making for personalized dosing [2] | Adaptable to individual differences [1] | MiniMed 780G (added to PID) [1] |
| Adaptive Closed-Loop [6] | Initialized with body weight only; learns individual insulin needs over time [6] | Minimal user configuration required [6] | iLet Bionic Pancreas [6] |
Commercial System Landscape
Multiple commercial AP systems are now available, each with distinct control approaches and features:
Table 3: Commercial Artificial Pancreas Systems (2024-2025)
| Commercial System | Algorithm Type | Key Features | Target Population |
|---|---|---|---|
| Medtronic 780G [1] | PID + Fuzzy Logic [1] | Automatic basal rate and correction boluses [1] | Type 1 diabetes |
| Tandem t:slim X2/Mobi with Control-IQ [1] | MPC [1] | Automates basal rate and correction boluses [1] | Type 1 diabetes |
| Insulet OmniPod 5 [1] | MPC [1] | Tubeless patch pump [1] | Type 1 diabetes |
| Beta Bionics iLet [1] [6] | Adaptive Closed-Loop [6] | Weight-based initialization; meal estimation without carb counting [6] | Type 1 diabetes (ages 6+) |
| CamAPS FX [1] | MPC [1] | Mobile app; first approved for pregnant women with T1D [1] | Type 1 diabetes, including pregnancy |
| Inreda AP [1] | Dual-hormone (Insulin + Glucagon) [1] | Bi-hormonal fully automated system [1] | Type 1 diabetes (available overseas) |
Experimental Protocols and Validation
Clinical Validation Framework
The path from research to clinical adoption required rigorous validation frameworks. Early clinical trials focused on overnight control in supervised settings, gradually progressing to longer-term outpatient studies with increasing complexity [1] [8]. The following diagram illustrates a generalized clinical validation pathway for artificial pancreas systems:
Figure 2: Artificial Pancreas Clinical Validation Pathway. Systems progress through increasingly complex environments with corresponding evaluation metrics at each stage.
Standardized Outcome Metrics
Consensus has emerged around standardized metrics for evaluating AP system performance, moving beyond HbA1c alone to comprehensive continuous glucose monitoring (CGM) metrics [3]:
Table 4: Standardized Outcome Metrics for AP System Evaluation
| Metric Category | Specific Measures | Target Values |
|---|---|---|
| Hypoglycemia [3] | Time <70 mg/dL (3.9 mmol/L); Time <54 mg/dL (3.0 mmol/L); Seizure/loss of consciousness | Minimize |
| Time-in-Range [3] | 70-180 mg/dL (3.9-10.0 mmol/L); 70-140 mg/dL (3.9-7.8 mmol/L) | Maximize (>70%) |
| Hyperglycemia [3] | Time >180 mg/dL (10.0 mmol/L); Time >250 mg/dL (13.9 mmol/L); Diabetic ketoacidosis | Minimize |
| Overall Control [3] | Mean glucose; Glycemic variability (coefficient of variation) | Individualized |
| Data Sufficiency [3] | ≥70% of possible CGM readings over 2-week collection | Minimum standard |
The Scientist's Toolkit: Essential Research Reagents
AP research requires specialized tools and platforms for development and testing:
Table 5: Essential Research Tools for Artificial Pancreas Development
| Research Tool | Function | Significance |
|---|---|---|
| University of Virginia/UCSB APS Platform [1] | Universal research platform enabling automated communication between CGMs, pumps, and algorithms [1] | Powered first inpatient clinical trials; enabled standardized testing [1] |
| FDA-Accepted T1D Simulator [1] | Computer simulator of human metabolic system in T1D [1] | Accepted by FDA as substitute for animal trials; accelerated development by years [1] |
| Diabetes Assistant [1] | Mobile-based platform using Android smartphone as computational hub [1] | Enabled portable outpatient studies with remote monitoring [1] |
| mGIPsim Python Simulator [7] | Software simulator for closed-loop control testing with meal and exercise scenarios [7] | Enables algorithm testing without clinical trials [7] |
| Unscented Kalman Filter (UKF) [7] | State estimation technique for real-time glucose prediction [7] | Enhances model predictive control accuracy [7] |
| Recursive Least Squares (RLS) [7] | Parameter estimation algorithm for adaptive control [7] | Enables personalization of system parameters [7] |
| Perphenazine sulfoxide | Perphenazine Sulfoxide | Perphenazine sulfoxide is a key metabolite of the antipsychotic perphenazine. This product is for research use only (RUO). Not for human use. |
| 2-Nitrobenzyl alcohol | 2-Nitrobenzyl alcohol, CAS:612-25-9, MF:C7H7NO3, MW:153.14 g/mol | Chemical Reagent |
The development of artificial pancreas systems from initial concept to standard of care represents a remarkable achievement in biomedical engineering and diabetes care. This journey, facilitated by strategic public and private partnerships, has transformed diabetes management through automated insulin delivery technology. Current systems have established a foundation of safety and efficacy across diverse populations, while next-generation innovations continue to refine personalization, adaptability, and user experience. Future directions include full closed-loop control without meal announcements, integration of additional hormones like glucagon, enhanced machine learning algorithms for personalized adaptation, and expansion to broader populations including those with type 2 diabetes [3] [7]. The historical progression documented in this application note provides both methodological guidance and conceptual framework for researchers continuing to advance the field of automated insulin delivery.
The artificial pancreas (AP), or automated insulin delivery (AID) system, represents a paradigm shift in the management of Type 1 Diabetes (T1D) [1]. This closed-loop system mimics the glucose-regulatory function of a healthy pancreas by integrating three core technological components: a continuous glucose monitor (CGM), an insulin pump, and a control algorithm [9] [10]. This document deconstructs the architecture of these systems, providing application notes and experimental protocols framed within research on AP closed-loop control system design.
Core Component Deconstruction
Continuous Glucose Monitor (CGM)
The CGM serves as the system's sensor, providing real-time estimates of glucose levels in the interstitial fluid [11].
Operating Principle: A disposable sensor is inserted subcutaneously, where it measures glucose concentration in the interstitial fluid via an enzymatic reaction [11] [12]. A transmitter sends this data wirelessly to a receiver, which can be a dedicated device, a smartphone, or the insulin pump itself [11] [10]. It is critical to note an inherent physiological delay of approximately 10 minutes between blood glucose and interstitial fluid glucose readings, which the control algorithm must account for [12].
Key Performance Metrics: Accuracy is primarily quantified by the Mean Absolute Relative Difference (MARD), with a value below 10% considered acceptable for insulin dosing [12]. Recent technological advancements have pushed MARD values below 9% for leading systems [12].
Table 1: Quantitative Performance Metrics of Selected CGMs
| CGM Model | MARD (%) | Warm-up Time | Sensor Life (Days) | Calibration Required? |
|---|---|---|---|---|
| Abbott FreeStyle Libre 3 | 7.9 [12] | 1 hour [12] | 14 [12] | No [12] |
| Dexcom G7 | 8.2 [12] | 0.5 hours [12] | 10 [12] | No [12] |
| Medtronic Guardian 4 | Information Missing | Information Missing | Information Missing | Information Missing |
Research Considerations: Factors such as sensor compression during sleep, prolonged aerobic exercise, and interfering substances (e.g., acetaminophen, ascorbic acid, hydroxyurea) can affect CGM accuracy and are active areas of investigation [11] [12].
Insulin Pump
The insulin pump functions as the system's actuator, delivering rapid-acting insulin analogs subcutaneously [13] [14].
Operating Principle: The pump mimics physiological insulin secretion by providing a continuous low basal rate (background insulin) and on-demand bolus doses (for meals or high glucose corrections) [13]. Pumps are classified as either tubed (tethered) or tubeless (patch pumps) [13]. In a closed-loop system, the pump receives dosing commands from the control algorithm.
Delivery Modes:
- Manual Mode: The user or clinician sets a predetermined basal rate [14].
- Auto Mode (Closed-Loop): The pump automatically modulates the basal insulin delivery based on CGM readings and the control algorithm's instructions [14]. Contemporary commercial systems are primarily hybrid closed-loop systems, which automate basal insulin but require user input for meal boluses [1] [15].
Research Considerations: A significant research challenge involves failures in insulin delivery, which can arise from bent or kinked cannulas, insulin crystallization in the infusion set, inflammation at the infusion site, or tubing issues, all of which can lead to hyperglycemia and diabetic ketoacidosis (DKA) [13]. Safety features like Predictive Low Glucose Suspend (PLGS) are critical, halting insulin delivery up to 30 minutes before predicted hypoglycemia [14].
Control Algorithm
The control algorithm is the central processing unit of the AP, determining the required insulin dose based on CGM data and other inputs [1] [8].
Core Algorithm Types:
- Proportional-Integral-Derivative (PID): Uses a predefined equation to calculate insulin delivery based on the error (difference between current and target glucose) and its integral and derivative [12] [16]. It often incorporates Insulin Feedback (IFB) to account for the suppressive effect of existing plasma insulin [12].
- Model Predictive Control (MPC): A more advanced method that uses a model of the patient's glucose-insulin dynamics to predict future glucose levels and preemptively calculate optimal insulin delivery over a defined "horizon" [1] [12]. This approach is particularly suited for systems with large time delays [12].
- Fuzzy Logic (FL): Mimics human decision-making under uncertainty, allowing the algorithm to respond to non-modeled disturbances such as unannounced meals, illness, or exercise [1] [12]. It is often used in conjunction with other algorithms.
Table 2: Algorithm Types in Commercial AID Systems
| Commercial System | Primary Algorithm | Additional Features |
|---|---|---|
| Medtronic MiniMed 780G | PID [12] | Integrated Fuzzy Logic for correction boluses [1] [12] |
| Tandem t:slim X2 with Control-IQ | MPC [1] [12] | Automates basal and correction boluses [1] |
| Insulet OmniPod 5 | MPC [1] [12] | |
| Beta Bionics iLet | MPC [1] [12] | |
| CamAPS FX | MPC [1] [12] |
Advanced Research Directions: Current research explores the use of multi-hormonal systems (e.g., co-delivery of insulin and glucagon) [12] [14], the integration of machine learning and AI for personalized predictive models [12] [9], and the application of ultra-rapid-acting insulin analogues to improve system responsiveness [12].
Experimental Protocols for System Validation
Robust clinical validation is essential for the translation of AP systems from research to clinical practice. The following protocols outline standardized methodologies.
Protocol 1: Inpatient Meal Challenge Study
Objective: To evaluate the performance and safety of an AID system in a controlled environment, with a specific focus on postprandial glucose control.
Methodology:
- Participant Selection: Recruit adults with T1D. Key exclusion criteria include hypoglycemia unawareness and recent severe hypoglycemic events.
- Study Setup: Conduct the trial in a clinical research unit. Insert the study CGM and connect the investigational insulin pump. For comparison, a control arm may use sensor-augmented pump (SAP) therapy.
- Meal Intervention: After an overnight fast and stabilization period, provide a standardized high-carbohydrate breakfast (e.g., 60-80g). The meal is announced to the system in hybrid closed-loop studies, and a user-initiated bolus is delivered.
- Data Collection: The primary outcome is the mean peak postprandial glucose level in the 3-4 hours following the meal [16]. Secondary outcomes include time-in-range (70-180 mg/dL), time in hypoglycemia (<70 mg/dL), and time in hyperglycemia (>180 mg/dL).
- Analysis: Compare the postprandial glucose trajectories and key metrics between the AID and control groups.
Protocol 2: Outpatient Free-Living Pivotal Trial
Objective: To assess the long-term efficacy, safety, and usability of an AID system in a real-world setting.
Methodology:
- Study Design: A multicenter, randomized, controlled trial.
- Intervention: Participants are randomized to use either the investigational AID system or a control therapy (e.g., SAP) for a period of 3 to 6 months [1].
- Primary Endpoint: The change in HbA1c from baseline to the end of the study.
- Key Secondary Endpoints:
- Time-in-Range (TIR): The percentage of time with CGM values between 70 and 180 mg/dL [1].
- Hypoglycemia Exposure: The area under the curve (AUC) for time spent below 70 mg/dL and below 54 mg/dL.
- Patient-Reported Outcomes (PROs): Measured using validated questionnaires on diabetes distress and quality of life.
- Data Analysis: Perform an intention-to-treat analysis to compare the changes in HbA1c and CGM-derived metrics between groups.
System Architecture and Validation Workflow Visualization
Figure 1: AP System Architecture & Validation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Artificial Pancreas Research
| Research Reagent / Material | Function in AP Research |
|---|---|
| University of Virginia (UVA)/Padova Simulator | A widely accepted computer simulator of the human metabolic system in T1D, accepted by the FDA as a substitute for animal trials in the preliminary testing of AID algorithms [1]. |
| Artificial Pancreas System (APS) | A universal research platform (e.g., from the University of California, Santa Barbara) that enables automated communication between various CGMs, pumps, and control algorithms, powering initial inpatient clinical trials [1]. |
| Continuous Glucose Monitors (e.g., Dexcom G6/G7, Abbott Libre 3) | Provide the continuous stream of glucose data necessary for algorithm operation. Different models offer varying MARD, warm-up times, and form factors for testing [12]. |
| Insulin Pumps (e.g., Tandem t:slim, Insulet OmniPod, Medtronic) | The mechanical actuators for insulin delivery. Research requires pumps with open or documented communication protocols to interface with research algorithms [1] [13]. |
| Rapid-Acting Insulin Analogues (e.g., Lispro, Aspart) | The standard insulin formulation used in pump therapy. Research is ongoing into ultra-rapid-acting analogues (e.g., Fiasp, Lyumjev) to improve system responsiveness [12] [14]. |
| Glucagon (Stable Formulation) | For research into bi-hormonal AP systems. Glucagon can be administered to counteract or prevent hypoglycemia, allowing for more aggressive insulin dosing [12] [16]. |
| Zinc sulfate monohydrate | Zinc Sulfate Monohydrate for Research Applications |
| 3,29-Dibenzoyl Rarounitriol | 3,29-Dibenzoyl Rarounitriol, MF:C44H58O5, MW:666.9 g/mol |
The pursuit of an Artificial Pancreas (AP) represents a paramount endeavor in diabetes management, aiming to restore automated, physiological glucose homeostasis in individuals with insulin deficiency [2] [17]. The core challenge lies in replicating the exquisite biological control of a healthy pancreas, which maintains blood glucose within a narrow range through complex, dynamic interactions between hormones and metabolic processes [18] [19]. This application note delineates the physiological and mathematical foundations of glucose-insulin dynamics, with a specific focus on the compelling rationale for pulsatile hormone delivery as a superior modality for closed-loop control systems. Framed within broader thesis research on AP design, this document provides a detailed analysis for researchers and scientists engaged in developing next-generation automated insulin delivery systems.
Physiological Basis of Glucose Homeostasis
In healthy physiology, glucose homeostasis is maintained by a tightly regulated balance between insulin and glucagon, secreted by pancreatic β-cells and α-cells, respectively [2]. This system operates as a closed-loop feedback mechanism where blood glucose concentration is the primary input and hormone secretion is the output.
- Insulin Physiology: Insulin is an anabolic hormone that promotes cellular glucose uptake, inhibits hepatic glucose production, and facilitates glycogen synthesis [20]. Its secretion occurs in two key patterns: a continuous basal secretion that maintains fasting glucose levels, and a rapid prandial secretion in response to meals [20].
- Glucagon Physiology: Glucagon acts as a counter-regulatory hormone, stimulating hepatic glycogenolysis and gluconeogenesis to prevent hypoglycemia during fasting states [21].
- The Healthy Feedback Loop: Post-meal glucose elevation triggers insulin release, which suppresses glucagon and promotes glucose disposal. As glucose levels normalize, insulin secretion subsides. Conversely, a declining glucose level is countered by glucagon secretion, which stimulates endogenous glucose production [18] [2].
In Type 1 Diabetes (T1D), the autoimmune destruction of β-cells dismantles this feedback loop, necessitating exogenous insulin replacement [2]. Traditional therapy, whether via multiple daily injections or continuous subcutaneous insulin infusion (CSII), struggles to mimic the dynamic, responsive nature of endogenous secretion, leading to significant glycemic variability and an increased risk of both hyper- and hypoglycemia [2] [22].
Mathematical Modeling of Glucose-Insulin Dynamics
Mathematical models are indispensable tools for understanding glucose-insulin physiology and designing effective AP control algorithms. These models range from simple representations to complex, multi-compartmental descriptions of the system.
Table 1: Key Classes of Glucose-Insulin Models
| Model Class | Key Characteristics | Primary Application | Examples/References |
|---|---|---|---|
| Minimal Models | Parsimonious structure; estimates SI (insulin sensitivity) and SG (glucose effectiveness). |
Analysis of Intravenous Glucose Tolerance Test (IVGTT) data. | Bergman's Minimal Model [18] [23] |
| Physiological Compartmental Models | Multi-compartment; represents glucose & insulin kinetics in specific body pools (e.g., plasma, interstitial, liver). | Control-oriented prediction for AP algorithms. | UVA/Padova Simulator [24] [1] |
| Control Algorithm Models | Tailored for real-time insulin dosing decisions; often include safety constraints. | Core of commercial and research AP systems. | Model Predictive Control (MPC), Proportional-Integral-Derivative (PID) [2] [17] [24] |
A control-oriented, physiological long-term model can be described by the following compartmental equations [24]:
Glucose Subsystem:
dG(t)/dt = Ra(t) + EGP(t) - Si * G(t) * I(t) - k * G(t)WhereG(t)is plasma glucose,Ra(t)is glucose rate of appearance from meals,EGP(t)is endogenous glucose production,Siis insulin sensitivity,I(t)is plasma insulin, andkis glucose effectiveness.Insulin Subsystem:
dI(t)/dt = (1/Vi) * [Y(t) - ke * I(t)]dY(t)/dt = u(t) - kb * Y(t)WhereY(t)is subcutaneous insulin,u(t)is the insulin infusion rate,Viis the insulin distribution volume, andke,kbare elimination rate constants.
These equations form the basis for in-silico simulation and testing of AP controllers, such as the accepted UVA/Padova T1D Simulator [24] [1].
Signaling Pathways in Glucose-Stimulated Insulin Secretion
The mechanism by which a healthy pancreatic β-cell senses glucose and secretes insulin in a pulsatile manner involves an integrated oscillator system. The following diagram illustrates the core signaling pathways and their interactions that lead to pulsatile insulin secretion.
Diagram 1: Integrated oscillator model of pulsatile insulin secretion in pancreatic β-cells. The process begins with glucose uptake and metabolism, leading to ATP production. Elevated ATP closes KATP channels, causing membrane depolarization and Ca2+ influx, which triggers insulin exocytosis. Crucially, intrinsic metabolic oscillations (red dashed lines) and Ca2+ feedback on metabolic pathways (blue dashed line) create a coupled oscillator system that generates rhythmic pulses of insulin secretion with a typical period of ~5 minutes [19].
Rationale for Pulsatile Hormone Delivery
A key insight from physiology is that a healthy pancreas secretes insulin and glucagon in a pulsatile manner, with discrete secretory bursts occurring every 5-7 minutes [18] [19]. This stands in stark contrast to the continuous, zero-order hold (ZOH) infusion employed by many conventional insulin pumps. There is a growing body of evidence advocating for the adoption of pulsatile delivery in AP systems.
Physiological and Clinical Advantages
- Enhanced Hepatic Suppression: Pulsatile insulin delivery has been demonstrated to more effectively suppress hepatic glucose production compared to continuous infusion [24]. The liver, being the primary recipient of portal venous insulin, is exquisitely sensitive to the oscillatory signal.
- Improved Insulin Action: Studies suggest that the pulsatile pattern enhances insulin action at the target tissue level, potentially due to the prevention of receptor desensitization that can occur with constant exposure [19].
- Superior Postprandial Control: Simulation and experimental studies indicate that a pulsatile infusion scheme, particularly one that allows for "super-bolus" administration (increasing the meal bolus while temporarily suspending basal insulin), results in better control of postprandial glucose excursions, especially for meals with a high glycemic index [24].
- Mitigation of Delays: The subcutaneous (SC) route for insulin infusion introduces significant pharmacodynamic delays. Pulsatile, discrete micro-boluses align more naturally with the pancreas's native sampling strategy, which itself may have evolved to circumvent transport time effects and ensure stable feedback control [18].
Quantitative Pharmacokinetic/Pharmacodynamic Profiles
Table 2: Pharmacokinetic Profiles of Rapid-Acting Insulin Analogs (Subcutaneous Administration)
| Insulin Type | Onset of Action | Peak Action | Duration of Action | Citation |
|---|---|---|---|---|
| Insulin Lispro | 5-15 minutes | 30-60 minutes | 3-4 hours | [20] |
| Insulin Aspart | 10-20 minutes | 40-50 minutes | 3-5 hours | [20] |
| Insulin Glulisine | 20 minutes | ~1 hour | 4 hours | [20] |
| Regular Human Insulin | ~30 minutes | 60-120 minutes | 6-8 hours | [20] |
The faster pharmacokinetic (PK) profiles of modern analogs are crucial for effective AP operation, but delays remain a challenge. Pulsatile delivery is a strategy to optimize the utilization of these existing insulin formulations.
Experimental Protocols for Pulsatile AP System Evaluation
This section outlines a detailed protocol for evaluating a pulsatile-model predictive control (pZMPC) based AP system using an accepted in-silico environment.
Protocol: In-Silico Evaluation of a Pulsatile Zone MPC
1. Objective: To validate the glycemic performance and stability of a pulsatile Zone MPC (pZMPC) algorithm in controlling blood glucose in a simulated T1D population under conditions of announced and unannounced meals.
2. Materials and Reagents:
- Software: UVA/Padova T1D Metabolic Simulator (T1DMS) Academic Version [24].
- Virtual Cohort: 10 adult in-silico patients from the T1DMS.
- Control Algorithm: Pulsatile Zone MPC (pZMPC) code, implemented in a suitable programming environment (e.g., MATLAB, Python) [24].
- Meal Dataset: Standardized meal plan (e.g., 3 meals per day, with varying carbohydrate content).
3. Methodology:
1. Model Individualization: For each virtual patient, individualize the parameters of the long-term glucose-insulin prediction model within the pZMPC. This typically involves estimating patient-specific insulin sensitivity (Si) and glucose effectiveness (k) parameters [24].
2. Controller Tuning:
- Set the target glucose zone (Y_Tar) to a safe range, e.g., 80 - 140 mg/dL.
- Define the prediction horizon (N) and control horizon (M). Typical values are N = 6-10 steps and M = 2-3 steps (with 5-minute sampling, this equates to 30-50 min prediction).
- Configure input constraints: 0 ≤ u(t) ≤ u_max, where u_max is the maximum allowed insulin pulse.
- Configure state constraints, particularly Insulin-on-Board (IOB) limits to prevent "stacking" [24].
3. State Observer Setup: Implement and tune two augmented observers to handle plant-model mismatch:
- An Output Disturbance Observer (ODO) for general model uncertainty.
- An Input Disturbance Observer (IDO) specifically for unannounced meals [24].
4. Simulation Scenarios:
- Scenario A (Hybrid Closed-Loop): All meals are announced 15 minutes prior. The pZMPC uses this information.
- Scenario B (Unannounced Meals): Meals are not announced to the controller, relying solely on the IDO for compensation.
- Scenario C (Optimal Bolus Calculator): Test an event-triggered pZMPC that computes an optimal bolus upon meal announcement, emulating an optimal Functional Insulin Therapy (FIT) strategy [24].
5. Performance Metrics: Run 24-hour simulations for each scenario and calculate:
- Time-in-Range (TIR): Percentage of time glucose is between 70-180 mg/dL.
- Time in Hypoglycemia: <70 mg/dL.
- Time in Hyperglycemia: >180 mg/dL.
- Mean Glucose.
- Glycemic Risk Indices (e.g, LBGI, HBGI).
4. Data Analysis: Compare the performance metrics across the different scenarios. A robust pZMPC should maintain high TIR (>75%) and minimal hypoglycemia (<2%) across all scenarios, with Scenario B performance demonstrating the resilience of the observer design.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for AP Research
| Item | Function/Application | Example/Notes |
|---|---|---|
| UVA/Padova T1D Simulator | A widely accepted platform for in-silico testing of AP algorithms without the need for animal trials. | FDA-accepted substitute for preclinical testing [24] [1]. |
| Continuous Glucose Monitor (CGM) | Provides real-time, interstitial glucose measurements for feedback control. | Dexcom G7, Abbott FreeStyle Libre 3 (MARD <9%) [2]. |
| Insulin Pumps | Delivers subcutaneous micro-boluses of rapid-acting insulin analogs. | Tandem t:slim X2, Insulet OmniPod 5, Medtronic 780G [2] [1]. |
| Rapid-Acting Insulin Analogs | The therapeutic agent with optimized PK/PD profiles for responsive control. | Insulin Aspart, Lispro, Glulisine [20]. |
| Control Algorithm Platform | A unified software environment to integrate CGM, pump, and control algorithm for clinical testing. | The Artificial Pancreas System (APS) / Diabetes Assistant [1]. |
| Glucagon & GLP-1 Analogs | For bi-hormonal AP systems to mitigate hypoglycemia; GLP-1 can delay gastric emptying and suppress glucagon. | Native Glucagon; GLP-1 derivatives (e.g., NN2211) [21] [23]. |
| 5'-O-DMT-2'-TBDMS-Uridine | 5'-O-DMT-2'-TBDMS-Uridine, CAS:81246-80-2, MF:C36H44N2O8Si, MW:660.8 g/mol | Chemical Reagent |
| 16-Acetoxy-7-O-acetylhorminone | 16-Acetoxy-7-O-acetylhorminone |
The transition from conceptual models to practical AP systems hinges on a deep appreciation of underlying physiology. Modeling glucose-insulin dynamics provides the predictive framework necessary for automation, while embracing the pulsatile nature of endogenous hormone delivery offers a path to more physiological, stable, and effective closed-loop control. The experimental protocols and research tools outlined herein provide a foundation for advancing the development of next-generation AP systems that more closely mimic the elegant biological intelligence of the healthy pancreas. Future work will focus on the integration of ultra-rapid insulin analogs, dual-hormone control, and adaptive learning algorithms to further narrow the performance gap between artificial and biological systems.
The evolution of Artificial Pancreas (AP) systems, also known as closed-loop or automated insulin delivery (AID) systems, represents a paradigm shift in the management of diabetes. The primary control objective for any AP system is to automate the maintenance of glucose homeostasis, mimicking the function of a healthy pancreas. The performance of these systems is quantitatively assessed using a set of standardized, complementary metrics that provide a holistic picture beyond traditional measures like HbA1c. Among these, Time-in-Range (TIR) and the minimization of hypoglycemia have emerged as the most critical endpoints for evaluating the safety and efficacy of closed-loop control algorithms in both research and clinical practice. This document outlines the key metrics, experimental protocols, and methodological tools essential for AP system design research.
The development of AP systems has transitioned from a disputed idea in 2005 to the gold-standard treatment for type 1 diabetes today [1]. Early systems focused on overnight glucose control to mitigate the risks of nocturnal hypoglycemia, but modern hybrid and fully closed-loop systems now aim for 24/7 glycemic control. This evolution has been powered by advances in continuous glucose monitoring (CGM), insulin pump technology, and sophisticated control algorithms such as Model Predictive Control (MPC) and Proportional-Integral-Derivative (PID) control [1]. The validation of these systems relies on a framework of CGM-derived metrics that capture the dynamic, complex nature of glucose physiology, with TIR serving as a primary outcome in pivotal clinical trials [25] [1].
Core Glycemic Metrics and Their Clinical Significance
Definition of Key Metrics
Glycemic metrics derived from CGM data provide a multi-dimensional view of glucose control. The international consensus recommendations have standardized the following core metrics for clinical trials and practice [26] [27]:
- Time-in-Range (TIR): Defined as the percentage of time that glucose levels are within the target range of 70-180 mg/dL (3.9-10.0 mmol/L). For most adults with diabetes, the target is >70% of daily readings (~17 hours per day) [28] [29] [26]. TIR is strongly correlated with a reduced risk of microvascular complications and is considered a primary efficacy endpoint for AP systems.
- Time Below Range (TBR): Categorized into two levels: Level 1 (<70 mg/dL or <3.9 mmol/L) and the more clinically significant Level 2 (<54 mg/dL or <3.0 mmol/L). Targets are <4% and <1% of the day, respectively [26] [27]. Minimizing TBR is the foremost safety objective in AP design, as hypoglycemia carries acute risks, including cognitive impairment and seizures [30].
- Time Above Range (TAR): Also categorized into two levels: Level 1 (>180 mg/dL or >10.0 mmol/L) and Level 2 (>250 mg/dL or >13.9 mmol/L). Targets are <25% and <5% of the day, respectively [26]. Elevated TAR indicates insufficient insulin delivery.
- Glycemic Variability (GV): Measured by the Coefficient of Variation (CV), calculated as (standard deviation / mean glucose) × 100. A CV of ≤36% is the target, indicating stable glucose levels with minimal fluctuations [26] [27]. High GV is an independent risk factor for hypoglycemia.
Table 1: Standardized Targets for Core Glycemic Metrics in Adults with Type 1 or Type 2 Diabetes
| Metric | Definition | Target (for most adults) | Clinical Significance |
|---|---|---|---|
| Time-in-Range (TIR) | % of time in 70–180 mg/dL | ≥ 70% | Primary efficacy endpoint; predicts complication risk [26] |
| Time Below Range (TBR) Level 1 | % of time < 70 mg/dL | < 4% | Non-clinically significant hypoglycemia [26] |
| Time Below Range (TBR) Level 2 | % of time < 54 mg/dL | < 1% | Clinically significant hypoglycemia; key safety metric [26] [30] |
| Time Above Range (TAR) Level 1 | % of time > 180 mg/dL | < 25% | Hyperglycemia burden [26] |
| Time Above Range (TAR) Level 2 | % of time > 250 mg/dL | < 5% | Severe hyperglycemia [26] |
| Coefficient of Variation (CV) | (SD / Mean Glucose) × 100 | ≤ 36% | Measure of glycemic stability; predictor of hypoglycemia risk [26] [27] |
The Relationship Between TIR, Hypoglycemia, and A1C
While HbA1c has been the gold standard for decades, it represents a long-term average and cannot reveal acute glycemic excursions, hypoglycemia, or glucose variability [27]. CGM metrics like TIR provide a more dynamic and detailed picture. Research shows a strong inverse correlation between TIR and HbA1c; a higher TIR is generally associated with a lower HbA1c [28]. However, two patients with the same HbA1c can have vastly different TIR and hypoglycemia profiles, underscoring the necessity of these complementary metrics for a complete assessment [28] [27].
For AP systems, the minimization of hypoglycemia (TBR) is paramount. Hypoglycemia, particularly severe hypoglycemia, is associated with acute risks like seizures and coma, and in young children, it can lead to permanent cognitive impairment and brain-structural abnormalities [30]. Furthermore, hypoglycemia can induce hypoglycemia unawareness, creating a vicious cycle of recurrent events [30]. Therefore, a successful AP system must not only maximize TIR but do so while rigorously minimizing TBR.
Experimental Protocols for Evaluating AP System Performance
Protocol for a Nocturnal Glycemic Control Study
The overnight period is critical for testing AP systems due to the high risk of prolonged, unrecognized hypoglycemia and attenuated counterregulatory hormone responses [25] [30]. The following protocol is adapted from a pivotal study on Predictive Hyperglycemia and Hypoglycemia Minimization (PHHM) [25].
Objective: To determine the safety, feasibility, and efficacy of a PHHM system compared with a predictive low-glucose suspend (PLGS) system in overnight glucose control.
Primary Endpoint: The percentage of time spent in a sensor glucose range of 70–180 mg/dL during the overnight period [25].
Secondary Endpoints:
- Mean overnight and morning blood glucose concentration.
- Percentage of time in hypoglycemia (<70 mg/dL and <54 mg/dL).
- Percentage of time in hyperglycemia (>180 mg/dL).
- Number of hypoglycemic events.
- Safety endpoints: episodes of severe hypoglycemia or diabetic ketoacidosis.
Methodology:
- Study Population: Recruit individuals with type 1 diabetes (e.g., aged 15-45 years) on insulin pump therapy. Exclude those with recent severe hypoglycemia or diabetic ketoacidosis.
- Run-in Phase: Participants use a CGM and insulin pump for 14-21 days to establish baseline metrics and familiarize themselves with the system.
- Randomization & Blinding: Participants are randomly assigned each night to either the experimental (PHHM) or control (PLGS) system. The assignment is blinded to the participant.
- Intervention:
- PHHM Nights: The system suspends basal insulin for predicted hypoglycemia and delivers automated correction boluses for predicted hyperglycemia.
- PLGS Nights: The system only suspends basal insulin for predicted hypoglycemia.
- Data Collection: The system is initiated at bedtime and deactivated upon waking. Overnight CGM data is collected. A capillary blood glucose measurement is taken upon waking.
- Statistical Analysis: Analyze data based on intention-to-treat. Compare primary and secondary endpoints between PHHM and PLGS nights using paired statistical tests (e.g., paired t-test). A sample size of 30 participants provides 90% power to detect a 5% difference in TIR [25].
In Silico Simulation Protocol for Control Algorithm Testing
Before human trials, control algorithms must be rigorously tested in simulation. The FDA-accepted University of Virginia/Padova Type 1 Diabetes Simulator is a critical tool for this purpose [1].
Objective: To validate a new control algorithm for an AP system using a computer-simulated cohort of virtual patients.
Primary Endpoint: Overall TIR (70-180 mg/dL) across the virtual cohort over a 7-day simulation period.
Methodology:
- Simulation Environment: Implement the control algorithm in a software environment that can interface with the T1D simulator (e.g., the Artificial Pancreas System (APS) platform [1]).
- Virtual Cohort: Select a representative cohort of virtual subjects (e.g., adults, adolescents, children) from the simulator's population.
- Simulation Scenarios:
- Nominal Conditions: Simulate standard daily living with standardized meal challenges.
- Perturbation Conditions: Introduce real-world challenges such as missed meal announcements, incorrect carbohydrate counting, and sensor/pump noise or dropouts.
- Data Analysis: Extract CGM traces and calculate all core glycemic metrics (TIR, TBR, TAR, CV, mean glucose) for each virtual subject and for the cohort overall.
- Algorithm Refinement: Use the results to iteratively refine and tune the control algorithm to optimize TIR and minimize TBR before proceeding to clinical trials.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for AP System Research & Development
| Category / Item | Specification / Example | Primary Function in Research |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Enhanced Enlite (Medtronic) [25] / Commercial CGMs | Provides real-time, interstitial glucose measurements for feedback control. Accuracy and reliability are paramount. |
| Insulin Pump | MiniMed Paradigm Veo [25] / T:slim X2 [1] | Subcutaneous delivery of insulin. Must be capable of receiving automated commands from the controller. |
| Control Algorithm | Model Predictive Control (MPC) [1], PID, Fuzzy Logic [1] | The "brain" of the AP. Calculates optimal insulin doses based on CGM data, predictions, and meal information. |
| Research Platform | Artificial Pancreas System (APS) [1], Diabetes Assistant [1] | A unified software/hardware platform (often laptop or smartphone-based) to integrate CGM, pump, and algorithm for research. |
| In Silico Simulator | FDA-Accepted T1D Simulator (UVA/Padova) [1] | Provides a virtual patient cohort for safe, efficient, and reproducible initial testing and tuning of control algorithms. |
| Bi-hormonal System | Glucagon (e.g., INREDA AP [18]) | Utilized in advanced systems to mitigate hypoglycemia risk by administering glucagon as a counter-regulatory agent. |
| Zuclopenthixol Decanoate | Zuclopenthixol Decanoate | Zuclopenthixol decanoate is a long-acting antipsychotic reagent for neuroscience research. This product is for research use only (RUO). Not for human or veterinary use. |
| Cardiogenol C hydrochloride | Cardiogenol C Hydrochloride |
Advanced Concepts: Time-in-Tight-Range and Future Directions
As AP technology advances, enabling tighter glycemic control, the metric of Time-in-Tight-Range (TITR) is gaining attention. TITR is defined as the percentage of time spent in a narrower target range of 3.9-7.8 mmol/L (70-140 mg/dL) [31]. While highly correlated with TIR, TITR is a more sensitive indicator of optimal glucose control, particularly in situations where glucose levels are close to normal or when stricter targets are required, such as in pregnancy [31]. The rise of advanced hybrid closed-loop systems and new hypoglycemic drugs is making the achievement of high TITR a more feasible goal, positioning it as a future key metric for evaluating the performance of next-generation AP systems.
Future research will also focus on fully closed-loop systems that require no meal announcements, the integration of ultra-rapid insulin analogs to improve postprandial control, and the expansion of AP use to broader populations, including pregnant women and people with type 2 diabetes [1]. The standardization of core glycemic metrics, as detailed in this document, provides the essential framework for objectively assessing these innovations and driving the field forward.
The development of Artificial Pancreas (AP) systems represents a paradigm shift in the management of Type 1 Diabetes (T1D), transitioning from reactive insulin administration to automated, closed-loop glucose regulation. This evolution has been critically dependent on the creation and regulatory acceptance of high-fidelity metabolic simulators. These tools have fundamentally altered the development pipeline for diabetes technology, serving as a bridge between conceptual algorithm design and clinical implementation. The University of Virginia/Padova (UVA/Padova) T1D Simulator, accepted by the U.S. Food and Drug Administration (FDA) in 2008 as a substitute for animal trials in the preclinical testing of insulin treatment strategies, marked an unprecedented milestone that accelerated the entire field [32] [33]. This document details the regulatory framework, simulator architecture, and experimental protocols that underpin modern AP development, providing researchers with a roadmap for leveraging these accepted tools to streamline the path to FDA clearance.
The Regulatory Paradigm Shift: From Animal Trials to In Silico Testing
The preclinical assessment of Automated Insulin Delivery (AID) systems historically relied on animal studies, a process that was both time-consuming and limited in its ability to represent human metabolic variability. A pivotal change occurred in 2008 when the FDA accepted the UVA/Padova T1D Simulator as a valid alternative to animal trials for the preclinical testing of insulin treatment strategies and control algorithms [32] [1]. This decision was based on the simulator's sophisticated representation of glucose-insulin dynamics and its incorporation of observed inter-individual variability across a population of virtual subjects.
This regulatory shift enabled rapid, cost-effective, and extensive testing of new treatment approaches. The simulator allows researchers to evaluate algorithm performance and safety across a wide spectrum of metabolic phenotypes and challenging scenarios before ever initiating human trials. This in silico testing framework has become a cornerstone of the AP development process, compressing development timelines and providing a robust platform for iterative algorithm refinement [33]. The acceptance of this simulator, and subsequently others, established a new precedent for the role of computational modeling in the regulatory approval of medical devices.
Table 1: Key Milestones in the Regulatory Acceptance of Metabolic Simulators for AP Development
| Year | Milestone | Impact on AP Development |
|---|---|---|
| 2008 | FDA acceptance of the UVA/Padova T1D Simulator as a substitute for animal trials [33] | Enabled faster, cheaper, and more extensive preclinical algorithm testing. |
| Pre-2008 | Preclinical testing relied on animal studies [33] | Slower development cycles and limited representation of human metabolic variability. |
| 2016 Onwards | FDA clearance of commercial hybrid closed-loop systems (e.g., Medtronic 670G) that leveraged in silico testing [1] | Established a clear pathway from simulator-validated algorithms to commercially approved devices. |
| Recent Years | FDA acceptance of CGM metrics (Time in Range, etc.) as complementary outcome measures to HbA1c [3] | Aligned regulatory endpoints with the rich data outputs generated by simulators. |
Architecture and Validation of Accepted Metabolic Simulators
The UVA/Padova T1D Simulator: A Benchmark Platform
The UVA/Padova T1D Simulator is a large-scale, physiologically-based mathematical model of the human metabolic system. Its development was underpinned by extensive phenotypic data from studies in over 200 adults and children, which utilized the triple tracer technique to derive key metabolic indices and parameters [32] [33]. This methodology provided robust, model-independent estimates of fundamental glucose fluxes, including endogenous glucose production (EGP), whole-body glucose disappearance (Rd), and the systemic appearance rate of meal carbohydrates (MRa).
The simulator's core model is described by a system of differential equations that capture the essential dynamics of glucose regulation. Key features of its architecture include:
- Comprehensive Representation: The model includes sub-models for subcutaneous insulin kinetics, glucose absorption from the gut, insulin action on glucose production and disposal, and glucose-renal excretion [33].
- Virtual Population: The simulator incorporates a population of N=300 in silico "subjects" (100 adults, 100 adolescents, and 100 children) with T1D. These virtual subjects are generated from the joint multivariate probability distribution of model parameters, ensuring they reflect the inter-individual variability observed in the real T1D population [33].
- Integrated Device Models: It includes models of continuous glucose monitors (CGM) and insulin pumps, enabling closed-loop simulation that accounts for the real-world performance characteristics of these devices [33].
Key Model Parameters and Inputs
The simulator requires specific inputs to function and generates outputs that are critical for algorithm assessment.
Table 2: Core Inputs and Outputs of a Metabolic Simulator for AP Testing
| Category | Parameter/Component | Description |
|---|---|---|
| Inputs | Meal Carbohydrate Content | The amount and timing of carbohydrate intake, a major disturbance to the system. |
| Basal Insulin Profile | The underlying (open-loop) basal insulin delivery rate. | |
| Controller Algorithm | The external control algorithm that determines insulin dosing based on CGM readings. | |
| Model Parameters | Insulin Sensitivity (SI) | A key parameter governing the effect of insulin on glucose disposal and production [32]. |
| Glucose Effectiveness (SG) | The ability of glucose itself to promote its own disposal and suppress endogenous production [32]. | |
| Carb Absorption Time Constants | Individual-specific parameters governing the rate of glucose appearance from the gut [33]. | |
| Outputs | Glucose Trajectory | The primary outcome, a time-series of blood glucose concentrations. |
| Insulin Delivery Profile | A time-series of insulin doses commanded by the control algorithm. | |
| CGM Readings | Simulated interstitial glucose readings, including sensor noise. | |
| Performance Metrics | Time in Range (TIR) | Percentage of time glucose is between 70-180 mg/dL [3]. |
| Time in Hypoglycemia | Percentage of time glucose is <70 mg/dL and <54 mg/dL [3]. | |
| Glycemic Variability (CV) | Coefficient of variation, a measure of glucose swings [3]. |
Diagram 1: Closed-loop simulation workflow. The controller algorithm processes CGM values to command insulin doses, which the virtual patient model responds to, creating a feedback loop. Performance is evaluated against standard metrics.
Experimental Protocols for In Silico Evaluation of AID Systems
The following protocols provide a standardized methodology for using accepted simulators in the preclinical evaluation of AP algorithms.
Protocol: Assessing Basal Control and Overnight Performance
1. Objective: To evaluate the ability of the control algorithm to maintain glucose levels in a target range during the fasting state, particularly overnight, and to assess its robustness to variations in basal insulin needs. 2. Virtual Subjects: A cohort of at least 10 adult in silico subjects from the accepted simulator population. 3. Simulation Setup:
- Duration: 24-hour simulation.
- Meals: No meal intake. This isolates the algorithm's basal control performance.
- Initial Conditions: Start each virtual subject at a different initial glucose level (e.g., 90 mg/dL, 120 mg/dL, 150 mg/dL) to test convergence to target.
- Controller: Implement the candidate control algorithm with standard settings. 4. Data Collection & Analysis:
- Record glucose traces and insulin delivery profiles.
- Calculate key performance metrics: Time in Range (70-180 mg/dL), Time Below Range (<70 mg/dL), Mean Glucose, and Glycemic Variability (CV) for the entire 24-hour period and specifically for the overnight period (e.g., 00:00 - 06:00) [3].
- Success Criterion: >95% time in range (70-180 mg/dL) and 0% time <70 mg/dL during the overnight period.
Protocol: Evaluating Meal Challenge Response
1. Objective: To test the algorithm's ability to mitigate postprandial hyperglycemia following a standardized meal without causing late-postprandial hypoglycemia. 2. Virtual Subjects: The same cohort as in Protocol 4.1. 3. Simulation Setup:
- Duration: 6-hour simulation post-meal.
- Meal: A standardized meal (e.g., 50g of carbohydrates) announced to the algorithm at time t=0. For fully closed-loop testing, the meal may be unannounced.
- Initial Conditions: Start each virtual subject at a euglycemic level (~110 mg/dL) to ensure a consistent baseline. 4. Data Collection & Analysis:
- Record glucose traces and insulin delivery profiles.
- Calculate the postprandial glucose peak, time to peak, and time to return to target range.
- Calculate TIR and Time Below Range for the 6-hour period.
- Success Criterion: Peak postprandial glucose <180 mg/dL and >0% time <70 mg/dL during the 6-hour post-meal period.
Protocol: Robustness Testing with Inter-Subject Variability
1. Objective: To validate algorithm performance and safety across the entire spectrum of the virtual population, capturing extreme but plausible metabolic phenotypes. 2. Virtual Subjects: The entire available in silico population (e.g., 100 adults, 100 adolescents, 100 children). 3. Simulation Setup:
- Duration: 3-day simulation with a standardized meal plan (e.g., three 50g carbohydrate meals per day).
- Scenarios: Include variations such as missed meal boluses (for hybrid systems) or unannounced snacks to test robustness. 4. Data Collection & Analysis:
- Aggregate performance metrics (TIR, TBR, Mean Glucose, CV) across the entire population.
- Identify the "worst-case" virtual subjects who experience the most hypoglycemia or hyperglycemia.
- Success Criterion: Population median TIR >70% and percentage of subjects experiencing any severe hypoglycemia (<54 mg/dL) for >1% of the time is <5% [3].
Table 3: Summary of Key Experimental Protocols for In Silico AP Evaluation
| Protocol | Primary Objective | Key Performance Metrics | Success Criteria |
|---|---|---|---|
| Basal Control | Evaluate fasting-state glucose control, especially overnight. | Overnight TIR, Hypoglycemia (%) | >95% TIR, 0% hypoglycemia overnight. |
| Meal Challenge | Assess postprandial glucose control after a standardized meal. | Postprandial peak, Time in Range after meal. | Peak <180 mg/dL, no significant hypoglycemia. |
| Robustness Testing | Validate safety and efficacy across a broad virtual population. | Population median TIR, % of subjects with hypoglycemia. | Median TIR >70%, <5% of subjects with significant hypoglycemia. |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following tools and components are essential for conducting rigorous in silico research and development of AP systems.
Table 4: Essential Research Tools for AP Development
| Tool / Component | Function in Research | Examples / Notes |
|---|---|---|
| Accepted T1D Simulator | The core platform for preclinical in silico trials and algorithm testing. | UVA/Padova T1D Simulator (accepted by FDA) [32] [33]. |
| Control Algorithm Design Software | Environment for developing and prototyping control strategies. | MATLAB/Simulink, Python (with SciPy, TensorFlow for AI approaches [34]). |
| Continuous Glucose Monitor (CGM) Model | Simulates the real-world performance of CGMs, including noise and delays. | Integrated into simulators; key parameter is MARD (Mean Absolute Relative Difference) [33]. |
| Insulin Pump Model | Simulates the delivery mechanism and pharmacokinetics of subcutaneous insulin. | Integrated into simulators; models rapid-acting insulin analogs [33]. |
| Virtual Patient Population | A cohort of in silico subjects with T1D representing inter-individual variability. | Included in the UVA/Padova simulator (n=300 across adults, adolescents, children) [33]. |
| Performance Metric Calculator | Software to compute standardized glycemic metrics from simulation outputs. | Calculates Time in Range, hypoglycemia metrics, GV, etc., as per consensus guidelines [3]. |
| Deep Reinforcement Learning (DRL) Framework | For developing data-driven, adaptive control algorithms. | Used in research for fully closed-loop systems; e.g., Proximal Policy Optimization (PPO) algorithms [34]. |
| 2-Geranyl-4-isobutyrylphloroglucinol | 2-Geranyl-4-isobutyrylphloroglucinol, MF:C20H28O4, MW:332.4 g/mol | Chemical Reagent |
| 5,6-Dimethoxy-2-isopropenylbenzofuran | 5,6-Dimethoxy-2-isopropenylbenzofuran, MF:C13H14O3, MW:218.25 g/mol | Chemical Reagent |
Diagram 2: The role of simulators in the AP development pipeline. In silico testing creates a iterative loop with algorithm design, generating the data needed for regulatory approval to begin clinical trials.
The regulatory and simulator landscape for Artificial Pancreas systems has matured into a sophisticated framework that efficiently translates engineering innovation into clinical reality. The acceptance of metabolic simulators like the UVA/Padova model has not only accelerated development but has also enhanced the safety profile of new AID systems by enabling exhaustive preclinical testing across a diverse virtual population. For researchers, a deep understanding of this landscape—including the architecture of accepted simulators, standardized experimental protocols, and the essential research toolkit—is no longer optional but fundamental to the successful development and regulatory clearance of the next generation of automated insulin delivery technologies.
Algorithmic Core: A Deep Dive into Control Strategies and Emerging AI Paradigms
Proportional-Integral-Derivative (PID) and Model Predictive Control (MPC) represent two fundamental approaches to feedback control with significant implications for safety-critical systems. While PID control has dominated industrial applications for decades due to its simplicity and reliability, MPC has emerged as a sophisticated alternative capable of handling complex constraints and predicting future system behavior. This comparative analysis examines these control paradigms within the context of commercial systems, with particular relevance to closed-loop artificial pancreas (AP) design. Understanding their operational principles, implementation requirements, and performance characteristics provides crucial insights for researchers and drug development professionals working on automated drug delivery systems.
The development of an artificial pancreas represents one of the most challenging control problems in biomedical engineering, requiring precise glucose regulation despite numerous disturbances including meals, physical activity, stress, and physiological variations. This application note analyzes how established control algorithms from industrial applications can inform AP closed-loop control system design, highlighting methodological considerations for preclinical testing and implementation.
Theoretical Foundations and Comparative Analysis
PID Control: Principles and Characteristics
The PID controller is a feedback mechanism that continuously calculates an error value ( e(t) ) as the difference between a desired setpoint and a measured process variable, applying a correction based on proportional, integral, and derivative terms [35] [36]. The mathematical representation of the PID algorithm is:
[ u(t) = Kp e(t) + Ki \int e(t)dt + K_d \frac{de(t)}{dt} ]
where ( u(t) ) is the control signal, ( e(t) ) is the error, and ( Kp ), ( Ki ), and ( K_d ) are the proportional, integral, and derivative gains, respectively [37]. Each component addresses a different aspect of the system response: the proportional term reacts to the present error, the integral term eliminates steady-state offset by accumulating past errors, and the derivative term anticipates future trends based on the rate of error change [36].
PID controllers excel in applications with well-defined dynamics where precise modeling is challenging [35]. Their widespread adoption in industrial settings (over 80% of process control loops) stems from straightforward implementation, reliability, and well-established tuning methodologies [38]. The algorithm's simplicity enables computationally efficient execution on low-power microcontrollers, making it suitable for embedded medical devices with limited processing capabilities [36].
MPC: Principles and Characteristics
Model Predictive Control is an advanced control strategy that employs an explicit dynamic model of the process to predict future system behavior over a finite horizon [39]. At each control interval, MPC solves a constrained optimization problem to determine a sequence of control actions that minimizes a cost function, typically implementing only the first step before repeating the process [39]. This receding horizon approach enables anticipatory control actions based on predictions of future disturbances and system states.
The core components of MPC include [35]:
- Process Model: A mathematical representation (linear or nonlinear) of system dynamics
- Cost Function: An objective function (often quadratic) quantifying control performance
- Optimization Algorithm: Computational method for minimizing the cost function subject to constraints
MPC's distinctive capability to handle multi-variable systems with constraints on both inputs and outputs makes it particularly valuable for complex processes [39] [40]. By anticipating future events and proactively adjusting control actions, MPC can achieve performance superior to reactive approaches like PID, especially for systems with significant time delays or complex dynamics [39].
Comparative Analysis: PID vs. MPC
Table 1: Comparative analysis of PID and MPC control algorithms
| Characteristic | PID Control | Model Predictive Control |
|---|---|---|
| Theoretical Basis | Error-based feedback [35] | Model-based optimization [35] |
| Model Requirement | Not required [40] | Essential (white-box, gray-box, or black-box) [41] |
| Constraint Handling | Limited (requires modifications) [35] | Explicit (directly incorporated in optimization) [39] [40] |
| Predictive Capability | None (reactive only) [39] | Explicit prediction horizon [35] [39] |
| Computational Demand | Low [35] | High (solving optimization at each step) [35] [41] |
| Multi-variable Control | Decoupled loops required [35] | Native multi-variable capability [39] |
| Implementation Complexity | Low [35] | High (requires modeling and optimization) [35] [41] |
| Typical Applications | Temperature, pressure, flow control [35] [38]; HVAC [40] | Chemical processes [35]; building energy management [42] [41]; automotive systems [35] |
Table 2: Performance characteristics in representative applications
| Performance Metric | PID Control | Model Predictive Control |
|---|---|---|
| Setpoint Tracking | Good for simple dynamics [35] | Superior for complex dynamics [35] [40] |
| Disturbance Rejection | Reactive only [39] | Proactive (anticipates disturbances) [35] [40] |
| Time Delay Handling | Performs poorly without modifications [35] | Excellent (explicitly accounts for delays) [35] [40] |
| Energy Efficiency | Moderate [40] | Superior (10-30% improvement in building HVAC) [42] [40] |
| Implementation Scale | Component-level control [35] | System-wide optimization [41] |
The fundamental distinction between these approaches lies in their operational philosophy: PID is reactive, responding to past and present errors, while MPC is proactive, using predictions to optimize future performance [39] [40]. This distinction has significant implications for applications like artificial pancreas systems where meal anticipation and circadian variations create predictable disturbances.
Diagram 1: Architectural comparison of PID and MPC control systems
Applications in Commercial Systems
PID Control Applications
PID controllers maintain a dominant position in industrial automation due to their reliability and simplicity, with an estimated 80% of process control loops utilizing this technology [38]. Their implementation spans numerous sectors:
Temperature Regulation: PID controllers provide precise thermal management in pharmaceutical manufacturing, food processing, and HVAC systems, maintaining setpoints with minimal steady-state error [35] [38]. In commercial buildings, conventional thermostats often employ PID logic to adjust heating and cooling equipment based on temperature deviations [40].
Pressure and Flow Control: In oil and gas refineries, PID controllers stabilize pipeline pressure despite fluctuating inputs, enhancing safety and efficiency [38]. Water treatment facilities utilize PID algorithms to maintain steady flow rates for optimal filtration and chemical dosing, achieving energy reductions up to 10% [38].
Motion Control: Robotics and automation systems deploy PID controllers for precise positioning and velocity control of motors and servos, correcting mechanical drift and timing lag dynamically [43] [36].
The continued prevalence of PID control stems from its straightforward implementation on platforms ranging from simple analog circuits to modern microcontrollers, with extensive documentation and familiarity among engineers [36].
MPC Applications
MPC has gained significant traction in applications where complex dynamics, constraints, or economic objectives make simple feedback control inadequate:
Building Climate Control: MPC implementations in commercial HVAC systems demonstrate 10-30% energy savings compared to conventional control while maintaining or improving thermal comfort [42] [41]. By incorporating weather forecasts, occupancy patterns, and thermal mass dynamics, MPC optimizes building operation across multiple timescales [42] [44].
Chemical Process Industries: Since the 1980s, MPC has been widely deployed in chemical plants and refineries where multi-variable interactions and constraints are significant [39]. These implementations typically use linear empirical models obtained through system identification to handle complex process dynamics [39].
Automotive Systems: Vehicle control applications utilize MPC for tasks such as optimized fuel consumption and trajectory following, leveraging its ability to handle constraints and predict future system states [35] [39].
The growing adoption of MPC in recent years reflects advances in computing hardware, optimization algorithms, and system identification techniques that make implementation more feasible [42] [41].
Experimental Protocols and Methodologies
Protocol 1: PID Controller Implementation and Tuning
Objective: Implement and tune a PID controller for precise regulation of a process variable.
Materials and Equipment:
- Process/simulation testbed (e.g., temperature chamber, glucose-insulin simulator)
- Sensors for process variable measurement (e.g., CGM for glucose monitoring)
- Actuator (e.g., infusion pump for insulin delivery)
- Microcontroller/PLC with PID implementation capability
- Data acquisition system
Procedure:
- System Identification:
- Apply step changes to the process input and record output response
- Determine key process parameters: gain (K), time constant (τ), dead time (θ)
- Calculate initial PID parameters using Ziegler-Nichols or Cohen-Coon methods [43]
Controller Implementation:
- Program PID algorithm on selected hardware platform
- Implement anti-windup protection for integral term
- Configure derivative filtering to reduce measurement noise sensitivity
Closed-Loop Tuning:
- Begin with conservative gains (approximately 50% of calculated values)
- Increase proportional gain until sustained oscillations occur
- Adjust integral time to eliminate steady-state error without excessive overshoot
- Add derivative action to dampen oscillations and improve settling time
- Fine-tune parameters to achieve quarter-wave decay ratio or specified performance metrics
Performance Validation:
- Test controller response to setpoint changes and disturbances
- Quantify performance metrics: rise time, settling time, overshoot, steady-state error
- Verify robustness under varying operating conditions
Troubleshooting:
- Excessive oscillation: Reduce proportional gain or increase derivative time
- Slow response: Increase proportional gain or reduce integral time
- Steady-state error: Reduce integral time
- Actuator saturation: Implement anti-windup strategy
Protocol 2: MPC Implementation for Constrained Systems
Objective: Design, implement, and validate a Model Predictive Controller for a system with constraints and measurable disturbances.
Materials and Equipment:
- Process/simulation testbed with constraint specifications
- Sensors for state estimation and disturbance measurement
- Computing platform capable of solving optimization problems in real-time
- Software tools for system identification and optimization (e.g., MATLAB, Python)
Procedure:
- Model Development:
- Collect input-output data from process under various operating conditions
- Identify model structure (transfer function, state-space, or neural network)
- Estimate model parameters using prediction error or subspace methods
- Validate model accuracy with separate dataset (minimum 70% fit)
Controller Formulation:
- Define prediction horizon (N) and control horizon (N_u)
- Formulate cost function incorporating tracking error and control effort
- Specify constraints on inputs, outputs, and states
- Select optimization algorithm (QP, SQP, or interior-point)
Implementation:
- Code optimization routine with efficient constraint handling
- Implement state estimator (Kalman filter) if not all states are measurable
- Develop disturbance models for measurable disturbances
- Establish real-time execution framework with fixed sampling period
Validation and Tuning:
- Test nominal performance with setpoint changes and disturbance rejection
- Verify constraint handling under extreme conditions
- Evaluate robustness to model mismatch and measurement noise
- Tune weighting matrices to achieve desired performance trade-offs
Performance Metrics:
- Constraint violation frequency and magnitude
- Computational time relative to sampling period
- Integrated absolute error (IAE) and control effort
- Stability under worst-case conditions
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential research tools for control system implementation
| Tool/Category | Representative Examples | Function/Application | Implementation Notes |
|---|---|---|---|
| Microcontrollers | TI MSP430FR2355 [36], STM32G0B1 [36], ATSAMD21G18 [36] | Embedded PID implementation | Low-power operation with analog peripherals |
| Processing Platforms | TMS320F280039C [36] | High-speed MPC implementation | Real-time digital signal processor for optimization |
| System Identification | MATLAB System ID Toolbox, Python SciPy | Process model development | Transfer function/state-space model estimation from data |
| Optimization Solvers | ACADOS [39], GRAMPC [39] | MPC optimization | Fast QP/nonlinear programming for real-time applications |
| Simulation Environments | MATLAB/Simulink, Python | Control algorithm testing | Virtual prototyping before hardware implementation |
| Communication Protocols | Modbus, Ethernet/IP, CAN | System integration | Industrial communication for sensor/actuator networks |
| 1,2,3-Tri-O-methyl-7,8-methyleneflavellagic acid | 1,2,3-Tri-O-methyl-7,8-methyleneflavellagic acid, CAS:69251-99-6, MF:C18H12O9, MW:372.3 g/mol | Chemical Reagent | Bench Chemicals |
| 21,23-Dihydro-23-hydroxy-21-oxozapoterin | 21,23-Dihydro-23-hydroxy-21-oxozapoterin | 21,23-Dihydro-23-hydroxy-21-oxozapoterin is a natural triterpenoid for research. This product is For Research Use Only (RUO). Not for human or veterinary use. | Bench Chemicals |
Relevance to Artificial Pancreas Systems
The comparative analysis of PID and MPC controllers provides valuable insights for artificial pancreas closed-loop control system design. Glucose regulation shares characteristics with many industrial processes: time delays (subcutaneous insulin absorption), measurable disturbances (meal announcements), changing dynamics (insulin sensitivity variations), and safety constraints (hypoglycemia avoidance).
MPC's predictive capabilities and explicit constraint handling make it particularly suitable for AP applications [42] [41]. The ability to incorporate meal announcements as feedforward disturbances and enforce safety constraints on predicted glucose values aligns well with clinical requirements. Recent research demonstrates that MPC can proactively mitigate postprandial hyperglycemia while preventing nocturnal hypoglycemia through optimization of future insulin delivery [42].
PID control offers advantages in implementation simplicity and computational efficiency, making it suitable for initial prototypes or embedded systems with limited processing capabilities [36]. Its clinical performance can be enhanced through gain scheduling to address circadian variations in insulin sensitivity [35].
Hybrid approaches, such as PID controllers with MPC-inspired constraint handling or cascade architectures, may leverage the strengths of both methodologies. The choice between control strategies should consider implementation complexity, computational requirements, and clinical performance specifications.
Diagram 2: Artificial pancreas control system structure
PID and MPC represent complementary approaches to feedback control with distinct advantages for different applications. PID control offers simplicity, reliability, and ease of implementation, while MPC provides sophisticated constraint handling and predictive capabilities. For artificial pancreas systems, both approaches offer viable pathways to automated glucose regulation, with selection dependent on performance requirements, implementation constraints, and clinical considerations.
The ongoing integration of machine learning with MPC [41] and the development of adaptive PID controllers [36] promise enhanced capabilities for handling the complex, time-varying dynamics of physiological systems. These advancements, coupled with continued progress in glucose sensing and insulin delivery technologies, will accelerate the development of more effective and robust artificial pancreas systems.
Hybrid Closed-Loop (HCL) systems represent the established standard of care for the management of type 1 diabetes (T1D), successfully merging automated algorithmic control of basal insulin delivery with mandatory user-initiated boluses for meals [1]. This Application Note details the core architecture, operational protocols, and key performance metrics of HCL systems, providing researchers and development professionals with a foundation for advancing artificial pancreas (AP) technologies. The documented progression from a disputed concept in 2005 to the current gold standard underscores the critical role of interdisciplinary collaboration in achieving clinical translation [1].
System Architecture & Operational Principles
The fundamental objective of an HCL system is to approximate the glucose-regulatory function of a healthy pancreas. This is achieved through the seamless integration of three core components into a single, automated control system [17] [3].
- Continuous Glucose Monitor (CGM): A subcutaneous sensor that measures interstitial glucose levels at regular intervals (typically every 5 minutes), providing the real-time data stream essential for feedback control [17].
- Control Algorithm: The "brain" of the system. Residing on an insulin pump or a paired smartphone, this software uses CGM data, insulin-on-board (IOB) calculations, and user-defined targets to compute necessary insulin delivery adjustments. Predominant algorithm types include Model Predictive Control (MPC) and Proportional-Integral-Derivative (PID) [1] [17].
- Insulin Pump: A device that delivers rapid-acting insulin subcutaneously. It receives commands from the control algorithm to modulate basal rates and administer corrective micro-boluses automatically [17].
The "hybrid" nature of these systems arises from the division of control responsibilities. As visualized in the diagram below, the algorithm fully automates basal insulin delivery and provides corrective boluses, but it requires manual user intervention to announce meals and administer prandial boluses, compensating for the slow pharmacokinetics of subcutaneously administered insulin.
Commercial HCL System Landscape
The translation of academic research into commercially available systems has provided robust evidence for the efficacy of HCL technology. The following table summarizes the key characteristics of leading HCL systems.
Table 1: Key Commercial Hybrid Closed-Loop Systems
| System Name | Control Algorithm Type | Automated Insulin Actions | Required User Input |
|---|---|---|---|
| MiniMed 780G (Medtronic) | PID + Fuzzy Logic [1] | Adjusts basal rate & administers automatic correction boluses [1] | Meal announcement and bolus [17] |
| t:slim X2 with Control-IQ (Tandem Diabetes Care) | Model Predictive Control (MPC) [1] | Automates basal rate and correction boluses [1] | Meal announcement and bolus [17] |
| OmniPod 5 (Insulet Corporation) | Model Predictive Control (MPC) [1] | Adjusts basal insulin delivery automatically [1] | Meal announcement and bolus |
| iLet Bionic Pancreas (Beta Bionics) | Adaptive, MPC-based [45] | Fully automated insulin dosing for basal and meals | Body weight only; meal announcement is optional but recommended [45] |
| CamAPS FX (CamDiab) | Model Predictive Control (MPC) [1] | Adjusts basal insulin and provides corrective boluses | Meal announcement and bolus; approved for use in pregnancy [1] |
Evaluation Protocols & Performance Metrics
The clinical validation of HCL systems has moved beyond relying solely on HbA1c, adopting standardized continuous glucose monitoring (CGM) metrics as primary endpoints in regulatory trials and real-world studies [3]. The table below outlines the consensus-based CGM metrics used to evaluate system performance.
Table 2: Standardized CGM Metrics for HCL System Evaluation [3]
| Metric Category | Definition / Threshold | Clinical or Research Significance |
|---|---|---|
| Time in Range (TIR) | % of time glucose is between 70–180 mg/dL (3.9–10.0 mmol/L) | Primary efficacy endpoint; surrogate for reduced complication risk. |
| Hypoglycemia | % of time < 70 mg/dL (3.9 mmol/L) and < 54 mg/dL (3.0 mmol/L) | Key safety endpoint. |
| Hyperglycemia | % of time > 180 mg/dL (10.0 mmol/L) and > 250 mg/dL (13.9 mmol/L) | Efficacy endpoint for hyperglycemia management. |
| Glycemic Variability | Coefficient of Variation (CV) | Measure of glucose stability; target is CV ≤ 36%. |
| Data Sufficiency | ≥ 70% of possible CGM readings over a 2-week period | Ensures data reliability for analysis. |
Protocol: In-Clinic Meal Challenge Study
Objective: To assess the postprandial glucose control performance of an HCL system following a standardized meal, with and without a user-initiated meal bolus.
Materials:
- HCL System (CGM, Pump, Algorithm)
- Standardized meal (e.g., 50g available carbohydrates)
- Blood glucose meter for calibration/verification
- Data collection software
Methodology:
- Participant Preparation: Participants arrive at the clinic after an overnight fast, with the HCL system active in closed-loop mode for a minimum of 12 hours prior.
- Baseline Period: Stabilize glucose levels within target range (70-180 mg/dL) for 1 hour.
- Intervention Arm (Meal with Bolus): Participant announces meal and administers a pre-meal insulin bolus based on the system's bolus calculator. The meal is consumed within 15 minutes.
- Control Arm (Meal without Bolus): On a separate day, the participant consumes an identical meal without announcing it or administering a bolus.
- Data Collection: CGM data (glucose levels, insulin delivery) is recorded for 6 hours post-meal. Key metrics include:
- Peak Postprandial Glucose
- Time to Peak Glucose
- Glucose Excursion (Area Over Curve)
- Time in Range (70-180 mg/dL) during the 4-hour postprandial period.
- Incidence of hypoglycemia (<70 mg/dL)
Data Analysis: Compare the glucose trajectories and calculated metrics between the two arms using paired t-tests or non-parametric equivalents. The protocol workflow is illustrated below.
The Scientist's Toolkit: Research Reagents & Materials
Research and development in HCL technology rely on a specific set of tools and models, ranging from in silico simulations to clinical-grade hardware.
Table 3: Essential Research Tools for HCL Development
| Tool / Material | Function in HCL Research | Examples / Notes |
|---|---|---|
| FDA-Accepted T1D Simulator | In silico testing and validation of control algorithms without the need for animal or human trials initially [1]. | University of Virginia/Padova Simulator; accepted by the FDA in 2008, significantly accelerating AP development [1]. |
| Universal Research Platform (APS) | Enables automated communication between a variety of CGM devices, insulin pumps, and proprietary control algorithms for inpatient clinical trials [1]. | The APS platform developed at UCSB (c. 2007) powered the first closed-loop human trials in the U.S. [1]. |
| Continuous Glucose Monitor (CGM) | Provides the real-time interstitial glucose data stream that is the primary input for the control algorithm [17]. | Key component; accuracy and reliability are paramount. |
| Subcutaneous Insulin Pump | The actuator device that delivers micro-boluses and basal rate adjustments as commanded by the control algorithm [17]. | Research often uses commercial pumps with investigational use interfaces. |
| Rapid-Acting Insulin Analogue | The therapeutic agent; its pharmacokinetic/pharmacodynamic profile is a key determinant of system performance, especially postprandially [3]. | Research is ongoing into ultra-fast analogues to improve postprandial control [1]. |
| 2-Nitro-5-thiocyanatobenzoic acid | 2-Nitro-5-thiocyanatobenzoic acid, CAS:30211-77-9, MF:C8H4N2O4S, MW:224.20 g/mol | Chemical Reagent |
| 7,4'-Dihydroxy-8-methylflavan | 7,4'-Dihydroxy-8-methylflavan, CAS:82925-55-1, MF:C16H16O3, MW:256.3 g/mol | Chemical Reagent |
Future Research Directions
While HCL systems are the current standard, research continues to address their limitations. The next frontier is the development of fully closed-loop systems that eliminate the need for meal announcements, instead relying on algorithms to detect and respond to glucose rises [45]. Other avenues include:
- Bihormonal Systems: Incorporating glucagon to mitigate hypoglycemia risk and allow for more aggressive insulin dosing [17] [18].
- Adjunct Therapies: Utilizing medications like GLP-1 receptor agonists or SGLT-2 inhibitors in conjunction with HCL systems to improve time in range [45].
- Adaptive and Personalized Algorithms: Developing systems that automatically adapt to an individual's changing insulin sensitivity due to factors like exercise, menstrual cycles, or illness [3].
The development of a fully closed-loop artificial pancreas (AP) represents a paramount objective in diabetes care, aiming to autonomously regulate blood glucose levels (BGL) and alleviate the constant management burden on individuals with Type 1 Diabetes (T1D). While conventional control algorithms like Model Predictive Control (MPC) have been the cornerstone of hybrid closed-loop systems, they often require manual meal announcements and struggle with the profound non-linearity and inter-patient variability of gluco-regulatory dynamics [46]. Deep Reinforcement Learning (DRL), a subset of artificial intelligence, emerges as a transformative paradigm for achieving fully closed-loop, adaptive control by learning optimal insulin dosing policies through direct interaction with the patient's physiological environment [34] [46]. This document outlines application notes and experimental protocols for developing and validating DRL-based controllers, specifically framed within the context of advanced AP closed-loop control system design research.
Core DRL Algorithms for AP Control
DRL frameworks treat the AP system as an interaction between an agent (the controller) and an environment (the patient). The agent observes a state (e.g., current and recent CGM values) and selects an action (insulin dose), receiving a reward based on the effectiveness of that action in regulating BGL [34]. Several DRL algorithms have shown significant promise for this application.
The Proximal Policy Optimization (PPO) algorithm is renowned for its training stability and high performance in complex environments. Its effectiveness can be substantially enhanced for AP control by incorporating implementation "tricks" such as reward scaling, policy gradient clipping, and normalized advantage functions [34]. Research demonstrates that an enhanced PPO controller can achieve a median Time in Range (TIR) of 87.45%, effectively eliminating severe hypoglycemia in simulation studies [34].
The Soft Actor-Critic (SAC) algorithm, an off-policy method, has also demonstrated superior performance in controlling gluco-regulatory dynamics, as noted in comparative studies against other algorithms like Deep Deterministic Policy Gradient (DDPG) [47]. Its ability to handle continuous action spaces efficiently makes it particularly suitable for the nuanced task of insulin dosing.
Table 1: Comparison of Key DRL Algorithms for AP Control
| Algorithm | Type | Key Features | Reported Performance (TIR) | Key Challenges |
|---|---|---|---|---|
| Proximal Policy Optimization (PPO) [34] | On-policy | High stability, suitable for continuous control. | 87.45% (median in simulation) | Requires careful reward shaping and safety mechanisms. |
| Soft Actor-Critic (SAC) [47] | Off-policy | Sample-efficient, handles continuous actions well. | Reported as superior to DDPG in preliminary results. | Complexity of hyperparameter tuning. |
| Deep Q-Network (DQN) [46] | Off-policy | Well-established, good for discrete action spaces. | Less common for fine-grained insulin dosing. | Limited by discretization of insulin actions. |
Experimental Protocol for In-Silico Validation
Simulation Environment Setup
- Platform: Utilize a validated simulation environment such as the Simglucose simulator [34] or the UVA/Padova T1D Simulator.
- Cohort: Employ a virtual subject population representing a wide range of ages, insulin sensitivities, and physiological dynamics to test generalizability and personalization. This cohort must encompass significant inter-patient and intra-patient variability [46].
- Meal Scenarios: Design challenging meal protocols, including single meals, multiple meals, and unannounced meals, to rigorously test the controller's ability to handle real-world perturbations [34].
Agent Training Procedure
- State Space Definition: The state (s_t) should include the current CGM reading, CGM values from the past several time steps (e.g., 4-6 readings), and the history of previously delivered insulin doses [34].
- Action Space Definition: Define a continuous action space representing the insulin infusion rate (in U/h) or a discrete bolus dose. Continuous actions are generally preferred for fine-grained control [34] [47].
- Reward Function Design: The reward function is critical for guiding the agent's learning. A typical function penalizes deviations from the target glucose range (70-180 mg/dL) and heavily penalizes hypoglycemic events [34]. An example function is:
r_t = - ( |BG_t - BG_target| / scaling_factor ) - (heavy_penalty if BG_t < hypoglycemia_threshold) - Training Loop: For each training episode (e.g., a 24-hour simulation): a. The agent observes the initial state st. b. The agent selects an action at (insulin dose) based on its current policy. c. The environment simulates the effect of the action, transitioning to a new state s{t+1} and returning a reward rt. d. The transition (st, at, rt, s{t+1}) is stored in a replay buffer (for off-policy algorithms). e. The agent updates its neural network policy using the collected experiences (e.g., via gradient descent on the PPO or SAC objective functions) [34] [46].
- Safety Module Integration: Implement a dual safety mechanism during training and deployment [34]:
- Proactive Guidance: Integrate safety considerations directly into the reward function (e.g., large negative rewards for hypoglycemia).
- Reactive Correction: Employ an external safety supervisor that can override the agent's action if it is predicted to cause imminent hypoglycemia.
Performance Evaluation Metrics
After training, evaluate the controller's performance on a held-out test set of virtual patients and meal scenarios. Key metrics must include [34]:
- Time in Range (TIR) (70-180 mg/dL): Primary efficacy endpoint.
- Time in Hypoglycemia (<70 mg/dL and <54 mg/dL): Primary safety endpoint.
- Time in Hyperglycemia (>180 mg/dL).
- Glucose Management Indicator (GMI).
Table 2: Key Performance Metrics from a State-of-the-Art DRL Controller (Simulation)
| Metric | Target | Reported Performance (Median) |
|---|---|---|
| Time in Range (TIR) | >70% | 87.45% [34] |
| Time < 70 mg/dL | <4% | Effectively eliminated [34] |
| Time < 54 mg/dL | <1% | 0% (Severe hypoglycemia eliminated) [34] |
| Time > 180 mg/dL | Minimized | Correspondingly reduced [34] |
System Architecture and Workflow
The following diagram illustrates the core closed-loop feedback system of a DRL-based Artificial Pancreas.
The Scientist's Toolkit: Research Reagent Solutions
The transition of DRL-based AP controllers from simulation to clinical application requires a suite of specialized tools and frameworks, guided by emerging regulatory standards.
Table 3: Essential Research Tools and Regulatory Framework
| Item / Concept | Function / Description | Examples / Notes |
|---|---|---|
| Simulation Environment | Provides a safe, in-silico testbed for initial agent training and validation. | Simglucose [34], UVA/Padova T1D Simulator [46]. |
| DRL Algorithm Framework | Software libraries providing implemented and tested DRL algorithms. | OpenAI Spinning Up, Stable-Baselines3, Ray RLLib. |
| Continuous Glucose Monitor (CGM) | The primary sensor providing real-time interstitial glucose measurements to the agent. | Dexcom G6, Medtronic Guardian. |
| Insulin Pump | The actuator that delivers micro-boluses or basal rate adjustments commanded by the agent. | Tandem t:slim X2, Insulet Omnipod. |
| Safety Module | A critical, often rule-based component that acts as a final layer of protection against harmful dosing decisions. | Can suspend insulin delivery if hypoglycemia is predicted [34]. |
| Predetermined Change Control Plan (PCCP) | A regulatory requirement for lifecycle management of AI/ML-enabled devices, outlining how future algorithm updates will be managed and validated [48]. | Mandated by FDA 2025 draft guidance for AI-enabled devices [48]. |
| 14α-Hydroxy Paspalinine | Paspalinine|Ca2+-Activated K+ Channel Inhibitor |
Regulatory Pathway and Lifecycle Management
The U.S. Food and Drug Administration's (FDA) 2025 draft guidance for AI-enabled medical devices establishes a framework emphasizing Total Product Lifecycle (TPLC) management [48]. For a DRL-based AP system, this necessitates:
- Transparency and Labeling: Clearly explaining the AI's function, limitations, and decision-making process to users and clinicians [48].
- Robust Data Governance: Ensuring training and validation data are high-quality, diverse, and representative of the intended population to mitigate algorithmic bias [48].
- Predetermined Change Control Plan (PCCP): A pivotal document that outlines the protocol for future updates to the DRL model (e.g., retraining with new data), including the validation steps required before deployment, thus allowing for safe, continuous improvement without requiring a full new regulatory submission each time [48].
- Post-Market Performance Monitoring: Implementing systems to continuously monitor the controller's real-world performance to detect any performance degradation or unexpected behavior [48].
Application Notes: Advancing Hypoglycemia Prevention in Artificial Pancreas Systems
The integration of glucagon as a counter-regulatory hormone in Dual-Hormone Artificial Pancreas (DHAP) systems represents a paradigm shift in the management of Type 1 Diabetes (T1D). While traditional single-hormone systems using insulin alone have revolutionized care, they remain fundamentally limited in their ability to proactively prevent hypoglycemia, especially during challenging conditions like exercise and overnight fasting [49] [1]. DHAP systems expand the control arsenal by dynamically administering both insulin to lower blood glucose and glucagon to raise it, enabling a more physiological and robust approach to glycemic regulation.
The therapeutic rationale for glucagon supplementation is rooted in the pathophysiology of T1D, where the loss of pancreatic α-cell function and an impaired counter-regulatory response to hypoglycemia are well-documented [50]. By providing an exogenous source of glucagon, DHAP systems can actively defend against hypoglycemia, reducing the patient's reliance on carbohydrate interventions and mitigating the risk of overcorrection and hyperglycemia. This is particularly critical for preventing exercise-induced hypoglycemia, a major barrier to physical activity for individuals with T1D [51]. Meta-analyses of clinical studies confirm that the use of low-dose glucagon significantly reduces both the risk of hypoglycemic events and the time spent below the target glucose range [51].
Modern DHAP implementations are increasingly sophisticated, moving beyond simple reactive control. The development of event-triggered control schemes minimizes unnecessary hormone delivery, enhancing system efficiency and safety [49] [52]. Furthermore, the integration of machine learning (ML) algorithms for the prediction of glycemic trends allows for preemptive intervention, addressing the inherent delays in subcutaneous glucose sensing and insulin absorption [49]. These smart systems classify blood glucose levels and predict future trajectories using models like ARIMA and Gated Recurrent Units (GRU), enabling the controller to administer hormones based on anticipated needs rather than solely on current glucose values [49] [52].
From a commercial and research perspective, the field is rapidly evolving. While several single-hormone automated insulin delivery (AID) systems are commercially available worldwide, bi-hormonal systems are also emerging, such as the Inreda AP in Europe [1]. Concurrently, academic and industry research is focused on overcoming the historical challenges of glucagon stability in liquid formulation, exploring avenues such as ready-to-use soluble formulations and innovative implantable devices that deliver stable powdered glucagon in response to detected hypoglycemia [53].
Quantitative Performance Analysis of DHAP Systems
Table 1: Glycemic Outcomes of Single-Hormone vs. Dual-Hormone Artificial Pancreas Systems
| Metric | Single-Hormone AP | Dual-Hormone AP | Notes & Context |
|---|---|---|---|
| Hypoglycemia Risk (RR) | 1.0 (Reference) | 0.54 (95% CI: 0.35, 0.84) | Meta-analysis for exercise-induced hypoglycemia [51] |
| Time Below Range (TBR <3.9 mmol/L) | Baseline | -3.91 percentage points (95% CI: -6.27, -1.54) | Reduction achieved with low-dose glucagon [51] |
| Post-Hypoglycemia Glucagon Response | Peak: ~30 mg/dL within 15 minutes | Demonstrated with novel implantable device in pre-clinical models [53] | |
| Primary System Benefit | Effective overnight glycemic control [49] | Superior prevention of exercise-induced hypoglycemia [49] [51] |
Table 2: Low-Dose Glucagon Formulations and Dosing for Hypoglycemia Prevention
| Formulation Type | Examples | Typical Low Dose (Prevention) | Emergency High Dose (Treatment) |
|---|---|---|---|
| Reconstituted Powder | GlucaGen Hypo Kit, Glucagon Emergency Kit [51] | 100-300 μg [51] | 1 mg for adults and children ≥6 years (≥25 kg) [54] |
| Ready-to-Use Liquid | Gvoke, Dasiglucagon [51] | 100-300 μg [51] | 1 mg for adults and children ≥12 years [54] |
| Stable Powder (Investigational) | For implantable devices [53] | Pre-clinical validation | -- |
Experimental Protocols
Protocol 1: In Silico Development of an Event-Triggered Smart DHAP
This protocol outlines the methodology for developing and initially validating a Smart DHAP (SDHAP) system, combining machine learning-based prediction with event-triggered control [49] [52].
Aims
To design and simulate a closed-loop control system that reliably maintains euglycemia in T1D by proactively delivering insulin and glucagon based on predicted blood glucose levels and event-triggered rules.
Materials
- Dataset: T1DiabetesGranada dataset (longitudinal CGM data from 736 patients) [49] [52].
- Software: MATLAB/Simulink, Python (with scikit-learn, TensorFlow/PyTorch libraries), SIMetrix for electrical network simulation [49] [18].
- Model: Bergman Minimal Model (BMM) for simulating glucose-insulin dynamics [49].
Methodology
Step 1: Data Preprocessing and Feature Engineering
- Preprocess the raw CGM data, handling missing values and noise.
- Extract temporal, statistical, and spectral features from the glucose time series.
- Calculate diabetes-specific metrics: Time in Range (TIR), Time Below Range (TBR), Time Above Range (TAR), and high/low glucose indexes [49] [52].
- Address class imbalance (e.g., fewer hypoglycemic events) using the Synthetic Minority Over-sampling Technique (SMOTE) [49].
Step 2: Classification of Glycemic Events
- Define classification thresholds (e.g., hypoglycemia: <70 mg/dL, hyperglycemia: >180 mg/dL).
- Train and validate machine learning classifiers, such as Support Vector Machine (SVM) and K-Nearest Neighbor (KNN), to identify hypoglycemia and hyperglycemia events from the extracted features [49].
Step 3: Blood Glucose Prediction
- Develop and train time-series forecasting models.
- Use AutoRegressive Integrated Moving Average (ARIMA) models for linear analysis.
- Use Gated Recurrent Unit (GRU) networks, a type of recurrent neural network, for capturing non-linear temporal dependencies.
- Evaluate prediction accuracy using Root Mean Square Error (RMSE) and Mean Absolute Error (MAE) [49] [52].
Step 4: Event-Triggered Controller Design
- Implement a feedback-feedforward (FB-FF) control structure.
- Feedback Control: Design a Model Predictive Control (MPC) or Proportional-Integral (PI) controller that uses the predicted blood glucose from Step 3 to compute hormone infusion rates.
- Event Trigger: Define trigger conditions (e.g., predicted glucose crossing a threshold, high rate of descent) to activate hormone delivery, minimizing unnecessary continuous infusion [49].
- Feedforward Control: Design a module to reject known disturbances, such as announced meals or exercise, by preemptively adjusting insulin or glucagon delivery [49] [52].
Step 5: In Silico Validation
- Integrate the classification, prediction, and control modules into a closed-loop simulation using the BMM.
- Test the SDHAP performance against various challenge scenarios (e.g., meal ingestion, exercise) and compare its efficacy to a single-hormone controller [49].
Protocol 2: In Vivo Evaluation of Low-Dose Glucagon for Exercise-Induced Hypoglycemia
This protocol details a clinical study design to assess the efficacy of low-dose glucagon in preventing hypoglycemia during and after exercise in individuals with T1D, based on methodologies from a recent meta-analysis [51].
Aims
To determine whether subcutaneous administration of low-dose glucagon reduces the incidence of hypoglycemia and time below range compared to placebo or standard care (carbohydrate consumption or insulin adjustment) in adolescents and adults with T1D undergoing structured exercise.
Materials
- Participants: Adolescents and adults with T1D.
- Glucagon Formulation: Ready-to-use liquid glucagon (e.g., Gvoke) or reconstituted powder (diluted to appropriate concentration).
- Comparators: Placebo (saline), carbohydrate tablets, or insulin pump suspension/basal rate reduction.
- Equipment: Continuous Glucose Monitor (CGM), heart rate monitor, standardized exercise equipment (treadmill or cycle ergometer).
Methodology
Step 1: Participant Preparation and Randomization
- Stabilize participants on their usual insulin therapy (pump or multiple daily injections) prior to the study visit.
- Using a randomized crossover design, assign participants to receive either the low-dose glucagon intervention or the comparator on separate study visits, with a sufficient washout period.
Step 2: Pre-Exercise Protocol
- Participants present in a fasting state or under standardized meal conditions.
- Baseline blood glucose is confirmed to be in a safe range (>100 mg/dL).
- Administer a subcutaneous bolus of low-dose glucagon (e.g., 150 μg) or the comparator 15-30 minutes before the scheduled start of exercise.
Step 3: Exercise Protocol
- Participants perform a standardized moderate-intensity aerobic exercise (e.g., 45 minutes of cycling at 60% VOâ‚‚ max).
- Monitor heart rate, perceived exertion, and CGM readings continuously.
Step 4: Post-Exercise Observation
- Monitor participants for several hours (e.g., 4-6 hours) to capture delayed hypoglycemic events.
- Record all CGM data, any carbohydrate interventions, and adverse events (e.g., nausea).
Step 5: Data Analysis
- Primary Outcomes: Proportion of participants experiencing at least one level 1 hypoglycemic event (SG/PG <3.9 mmol/L) and percent time below range (TBR <3.9 mmol/L) during the observation period.
- Secondary Outcomes: Incidence of level 2 hypoglycemia (<3.0 mmol/L), mean glucose, time in range, and total carbohydrate rescue intake.
- Perform a paired statistical analysis (e.g., repeated measures ANOVA) to compare outcomes between the intervention and control visits [51].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for DHAP System Development
| Item/Category | Function/Application | Specific Examples / Notes |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Provides real-time, interstitial fluid glucose measurements for feedback control. | Freestyle Libre, Dexcom G6; Data used for feature extraction and algorithm training [49] [3]. |
| Insulin & Glucagon Pumps | Subcutaneous or intravenous infusion of hormones. | Dual-chamber pumps for simultaneous infusion; Research platforms like the Diabetes Assistant [1] [18]. |
| Glucagon Formulations | The therapeutic agent for preventing/treating hypoglycemia in experiments. | Reconstituted Powder: GlucaGen Hypo Kit. Ready-to-Use: Gvoke, Dasiglucagon. Investigational Dry Powder: For implantable devices [51] [53]. |
| Metabolic System Simulator | In silico testing and validation of control algorithms without patient risk. | FDA-accepted T1D simulator (University of Padova/Virginia); Enables rapid, safe prototyping [1]. |
| Machine Learning Frameworks | For developing glycemic event classification and prediction models. | Python with scikit-learn (for SVM, KNN), TensorFlow/PyTorch (for GRU networks) [49]. |
| Control Algorithm Platforms | Implementation and deployment of core control logic. | MATLAB/Simulink; Universal research platforms like the Artificial Pancreas System (APS) [49] [1]. |
Biochemical Signaling Pathway of Glucagon
The molecular mechanism by which glucagon prevents hypoglycemia involves the activation of hepatic gluconeogenesis. As illustrated in Figure 2, glucagon binding to its G-protein coupled receptor (GPCR) on hepatocytes stimulates adenylyl cyclase, leading to a rise in intracellular cyclic AMP (cAMP) and subsequent activation of Protein Kinase A (PKA) [50]. PKA then phosphorylates key transcription factors and enzymes, dramatically upregulating the gluconeogenic pathway. Recent research using 13C-labeled substrates reveals that glucagon not only increases the flux through this pathway but also alters substrate preference. While glycerol is a major carbon source under basal conditions, glucagon stimulation causes a disproportionate (6.4-fold) increase in the utilization of glutamine for glucose production, highlighting a complex regulatory mechanism that goes beyond generalized pathway activation [55]. This enhanced gluconeogenic flux ultimately results in the export of glucose into the circulation, effectively raising blood glucose levels.
Application Notes: Core Principles and Performance Data
Modern Artificial Pancreas (AP) systems for Type 1 Diabetes (T1D) management are evolving from simple reactive controllers to intelligent systems that anticipate and automatically respond to glycemic challenges. Event-triggered control, combined with feedforward actions, represents a significant advancement in minimizing user input while maintaining strict glycemic control. These architectures shift from traditional periodic, time-triggered operations to an aperiodic execution of control actions, thereby enhancing computational efficiency and mimicking the body's natural pulsatile endocrine secretion [56] [18]. This approach is particularly vital for managing the slow dynamics of subcutaneous glucose sensing and delayed insulin absorption, which are major challenges in AP systems [49]. By integrating feedforward mechanisms, these systems can proactively reject disturbances caused by meals and exercise, leading to more robust patient-specific drug delivery [49].
The table below summarizes the performance of various advanced control strategies as reported in recent research, providing a comparative overview of their efficacy.
Table 1: Performance Summary of Advanced AP Control Strategies
| Control Strategy | Primary Function | Reported Time-in-Range (TIR) 70-180 mg/dL | Key Performance Metrics | Citation |
|---|---|---|---|---|
| Event-Triggered SDHAP (Smart Dual Hormone AP) | FB-FF control for insulin/glucagon delivery | Not explicitly quantified in results | Effective BG control; rejects meal/exercise disturbance; patient-specific dosing. | [49] |
| Event-Triggered MPC (Unannounced Meals) | Reduced-computation insulin delivery | ~61% (25h of 41h in closed-loop) | Controller active only 18h of 41h; maintains safety with reduced processor runtime. | [56] |
| Event-Triggered MPC (Meal Announcement) | Reduced-computation insulin delivery | Nearly identical to standard MPC | Controller operates only 25.88% of the time compared to standard MPC. | [56] |
| Intermittent Closed-Loop for MDI | Recommends correction boluses & rescue carbs | ~70.5% (vs. ~55.5% in open-loop) | Feasible for Multiple Daily Injection (MDI) therapy; reduces hypoglycemia & hyperglycemia. | [57] |
Key System Components and Their Functions
The implementation of these intelligent control systems relies on a specific toolkit of research reagents and hardware components.
Table 2: Research Reagent Solutions and Essential Materials
| Item Name | Function/Application in AP Research |
|---|---|
| T1DiabetesGranada Dataset | Provides real-world CGM data (recorded every 15 min) for 736 patients over 4 years; used for training ML classification and time-series prediction models [49]. |
| UVA/Padova T1D Metabolic Simulator | FDA-accepted simulation platform for in-silico testing and validation of control algorithms under various conditions (meals, exercise) before clinical trials [1] [56]. |
| Bergman Minimal Model (BMM) | A mathematical framework used to model glucose-insulin dynamics and design Proportional-Integral (PI) and Model Predictive Control (MPC) feedback controllers [49]. |
| Arduino UNO with Stepper Motor & Driver | A low-cost hardware platform for prototyping the mechanical actuation of dual-hormone (insulin/glucagon) delivery systems [49]. |
| Support Vector Machine (SVM) / K-Nearest Neighbor (KNN) | Machine learning algorithms used to classify blood glucose levels into states like hypoglycemia and hyperglycemia based on features extracted from CGM data [49]. |
Experimental Protocols
Protocol 1: In-Silico Validation of Event-Triggered MPC
This protocol outlines the methodology for pre-clinical testing of an event-triggered Model Predictive Control (MPC) algorithm using a widely accepted simulator.
Objective: To validate the safety and efficacy of an event-triggered MPC for embedded AP systems under challenging conditions with announced and unannounced meals [56].
Materials and Setup:
- Software: Full version of the US-FDA accepted UVA/Padova T1D Metabolic Simulator.
- Cohort: A cohort of 47 virtual patients (or as provided by the simulator) [57].
- Controller: Implement the event-triggered MPC algorithm on a wearable embedded platform or a hardware-in-the-loop (HIL) setup [56].
Methodology:
- Algorithm Design:
- Base the MPC on a predictive model of the form
xk+1 = f(xk, uk)andyk = h(xk), wherexis the patient state anduis the insulin infusion rate [56]. - Design the event-triggering mechanism using physiological insights and control-theoretic constructs. The controller should only update when specific events occur, rather than at every fixed time step [56].
- Base the MPC on a predictive model of the form
- Simulation Scenarios:
- Scenario A (Meal Announcement): Conduct a closed-loop simulation where all meals are announced to the system. Record the percentage of time the controller is active and the resulting Time-in-Range (TIR).
- Scenario B (Unannounced Meals): Conduct a more rigorous closed-loop simulation with unannounced meals to test robustness. Similarly, record controller activity and TIR.
- Comparator: Run both scenarios using a standard, time-triggered MPC for performance comparison.
- Data Collection and Analysis:
- Collect continuous glucose data for the entire simulation period.
- Calculate key performance metrics: Percentage of time in range (TIR) 70–180 mg/dL, time in hypoglycemia (<70 mg/dL), time in hyperglycemia (>180 mg/dL), and controller runtime/update frequency.
- Compare the results of the event-triggered MPC against the standard MPC, focusing on the trade-off between glycemic control and computational efficiency.
The following workflow diagram illustrates the experimental procedure for in-silico validation:
Protocol 2: Development and Testing of a Smart Dual-Hormone AP (SDHAP)
This protocol describes the end-to-end process for developing a dual-hormone system that uses event-triggered feedback and feedforward control.
Objective: To design and implement a Smart Dual-Hormone Artificial Pancreas (SDHAP) that classifies glycemic events, predicts future blood glucose (BG), and uses event-triggered control for patient-specific insulin and glucagon delivery [49].
Materials and Setup:
- Dataset: The T1DiabetesGranada dataset [49].
- Software: Machine Learning (e.g., Python with scikit-learn) and control design tools (e.g., MATLAB/Simulink).
- Hardware Prototype: Components for a prototype delivery system: Arduino UNO, NEMA 17 stepper motor with TB6560 driver, and 10ml syringes [49].
Methodology:
- Data Preprocessing and Feature Engineering:
- Preprocess and clean the CGM data from the T1DiabetesGranada dataset.
- Extract relevant time-series, statistical, and clinical features (e.g., TIR, TBR, TAR). Handle data imbalance using techniques like SMOTE (Synthetic Minority Over-sampling Technique) [49].
- Classification and Prediction:
- Classification: Train Machine Learning classifiers (SVM, KNN) using the extracted features to detect hypoglycemia and hyperglycemia events in real-time.
- Prediction: Develop a time-series prediction model (e.g., ARIMA or Gated Recurrent Unit - GRU) to forecast future BG levels. Evaluate accuracy using RMSE and MAE [49].
- Controller Design and Integration:
- Feedback (FB) Control: Design an event-triggered PI or MPC controller based on the Bergman Minimal Model. The controller is activated based on the classified events and predicted BG trends [49].
- Feedforward (FF) Control: Design a feedforward controller to proactively reject measurable disturbances, such as announced meals or exercise [49].
- Integration: Fuse the FB and FF outputs to compute the final hormone (insulin or glucagon) infusion commands.
- Hardware-in-the-Loop (HIL) Testing:
- Deploy the integrated control algorithm to the Arduino-based prototype.
- Connect the hardware to a simulation of the patient (e.g., the UVA/Padova simulator) in a closed loop.
- Test the system's response to various meal and exercise scenarios, verifying the physical actuation of the dual-hormone delivery system.
The high-level architecture and information flow of the SDHAP system is shown below:
Protocol 3: Assessing Behavioral Impact of Hybrid Closed-Loop Systems
Objective: To qualitatively explore how the use of a hybrid closed-loop (HCL) system affects users' food choices, dietary practices, and diabetes self-management behaviors [58].
Materials and Setup:
- Participants: Recruit adults, adolescents, and parents of children with T1D who are transitioning to a hybrid closed-loop system.
- Tools: Semi-structured interview guides tailored for baseline and follow-up interviews.
Methodology:
- Study Design: Conduct a longitudinal qualitative interview study. Perform baseline interviews just before participants commence HCL use and follow-up interviews after 3 months of use [58].
- Data Collection:
- Use in-depth, thematic interviews. At baseline, explore current dietary practices, carbohydrate counting, and mealtime management with an insulin pump.
- At follow-up, explore whether, how, and why food choices and dietary-related diabetes management have changed with the HCL system.
- Data Analysis:
- Transcribe interviews verbatim.
- Analyze data thematically using a method like constant comparison. Have multiple researchers independently code transcripts and then meet to compare interpretations and reach a consensus on key themes [58].
- Key Themes to Investigate:
- Changes in feelings of burden and anxiety related to food.
- Potential for "deskilling" (e.g., less precise carbohydrate counting).
- Shifts towards less healthy eating or increased snacking due to perceived system safety.
- Overall impact on quality of life and daily routines.
- Output: Generate insights to inform the development of tailored nutritional and behavioral support training for future AP users, ensuring that technological advances translate into positive health outcomes without unintended negative behaviors [58].
Addressing Real-World Challenges: Safety, Personalization, and System Integration
A primary challenge in the development of a fully automated artificial pancreas (AP) is the inherent delay associated with subcutaneous (SC) glucose sensing and insulin absorption [1] [3]. These lag times disrupt the closed-loop feedback system, making stable and precise glucose control difficult to achieve, particularly in response to meals [59] [18]. This document outlines key strategies and provides detailed experimental protocols for researchers developing solutions to mitigate these delays, framed within the broader context of AP closed-loop control system design.
Strategic Approaches and Comparative Analysis
Research has converged on several core strategies to overcome delay-related obstacles. The table below summarizes the primary approaches, their underlying mechanisms, and key research findings.
Table 1: Strategic Approaches to Mitigate Sensing and Actuation Delays
| Strategy | Technical Rationale | Key Research Findings | Reported Impact on Delay/Glycemic Control |
|---|---|---|---|
| Alternative Insulin Delivery Routes | Bypasses slow SC insulin absorption kinetics by delivering insulin directly into the peritoneum or bloodstream. | Intraperitoneal (IP) delivery showed significantly higher time in range (4.4–6.6 mmol/L) compared to open-loop SC control (39.1% vs. 27.7%) [59]. Pulse-modulated IV infusion mimics physiological pulsatile secretion [18]. | Reduced actuation delay: IP and IV routes offer faster onset of insulin action compared to SC [59] [18]. |
| Advanced Control Algorithms | Uses predictive models and adaptive learning to anticipate glucose trends and proactively deliver insulin, compensating for system lags. | Model Predictive Control (MPC) and Deep Reinforcement Learning (DRL) algorithms can operate without meal announcements, achieving a median Time-in-Range (TIR) of up to 87.45% in simulations [1] [34]. | Compensates for delay: Algorithms account for sensor lag and insulin pharmacokinetics/pharmacodynamics (PK/PD) to preempt glucose excursions [60] [34]. |
| Bihormonal Systems | Adds micro-doses of glucagon to counter hypoglycemia, allowing for more aggressive insulin dosing to curb postprandial hyperglycemia. | Systems like the INREDA AP utilize both insulin and glucagon. The iLet Bionic Pancreas is also capable of delivering glucagon [1] [18]. | Mitigates risk of delay-induced hypoglycemia: Enables tighter control by providing a rescue hormone, reducing the safety margin required for insulin-only systems [18] [3]. |
| Enhanced Sensor Design | Improves physical sensor properties and signal processing to increase accuracy and reduce measurement lag. | Fourth-generation sensors feature an 80% reduction in implanted volume and electrochemical impedance spectroscopy, achieving a Mean Absolute Relative Difference (MARD) of 8.7–9.6% [61]. | Reduces sensing error and lag: Smaller sensors may cause less tissue disturbance; advanced algorithms minimize signal noise [61]. |
Experimental Protocol: Evaluating Intraperitoneal Insulin Delivery in a Closed-Loop System
The following protocol, adapted from a foundational 2009 study, provides a methodology for comparing IP insulin delivery to standard SC delivery in a closed-loop configuration [59].
Objective
To evaluate the feasibility and efficacy of closed-loop intraperitoneal insulin infusion driven by a subcutaneous glucose sensor and a proportional-integral-derivative (PID) algorithm with a manual premeal bolus (HyPID system), and to compare its performance against open-loop intraperitoneal insulin delivery.
Materials and Reagents
Table 2: Research Reagent Solutions and Essential Materials
| Item | Function/Description |
|---|---|
| Implantable Insulin Pump (e.g., MMT-2007D) | Delivers U-400 regular insulin intraperitoneally. |
| Subcutaneous Glucose Sensors (e.g., CGMS/Guardian RT) | Continuously monitors interstitial glucose levels. |
| HyPID Control Algorithm | Laptop-based algorithm calculating insulin infusion rate from sensor data. |
| U-400 Regular Insulin (e.g., Insuplant) | Stable insulin formulation for implanted pump use. |
| Blood Glucose Meter (e.g., OneTouch Ultra) | For capillary blood glucose (CBG) reference measurements and sensor calibration. |
| Intravenous Catheter | Placed in an antecubital vein for frequent blood sampling for laboratory analysis. |
Procedure
- Subject Selection: Enroll type 1 diabetic patients who have been treated with an implanted intraperitoneal insulin pump for at least 3 months. Key inclusion criteria include plasma anti-insulin antibody level <30% and insulin delivery accuracy within 15% of expected values.
- Study Setup:
- Admit subjects to a clinical research center for an 86-hour period.
- Insert two subcutaneous glucose sensors in the abdominal area as primary and backup.
- Calibrate sensors 2 hours after insertion and then every 4 hours against CBG values.
- Randomized Study Phases: The study comprises a 24-hour control (open-loop) phase and a 48-hour closed-loop phase, the order of which is randomized.
- Control Phase: Patients manage their diabetes via their standard self-monitoring practices (7 CBG tests daily) and program their pumps accordingly.
- Closed-Loop Phase: The pump's basal insulin infusion rate is automatically modulated by the HyPID algorithm. A manual bolus equivalent to 30% of the patient's typical premeal dose is administered 15 minutes before each meal.
- Data Collection: Throughout both phases, collect the following:
- Frequent Blood Sampling: Draw blood every 20 minutes at the start of each meal for 2 hours, every hour during daytime non-postprandial periods, and every 2 hours overnight. Analyze samples for plasma glucose and insulin concentrations.
- Safety Monitoring: Perform CBG tests hourly from 0800 to 2200 and every 2 hours overnight. Conduct additional CBG tests if sensor glucose values fall below 4.4 mmol/L or rise above 13.2 mmol/L, or if hypoglycemic symptoms are reported.
- Data Analysis: The primary endpoint is the percentage of time spent with blood glucose in the 4.4–6.6 mmol/L range. Secondary endpoints include mean blood glucose and time spent in hypoglycemia (<3.3 mmol/L), analyzed separately for early postprandial and non-postprandial periods.
The workflow for this experimental protocol is outlined below.
Advanced Algorithmic Protocol: Deep Reinforcement Learning for Fully Closed-Loop Control
This protocol details the development of a Deep Reinforcement Learning (DRL) controller, a state-of-the-art approach designed to function without meal announcements by learning to manage system delays and metabolic variability [60] [34].
Objective
To develop and validate a safe-enhanced, fully closed-loop AP controller using a DRL algorithm that autonomously regulates blood glucose without external meal or activity announcements.
Materials and Software
Table 3: Reagents and Tools for DRL AP Development
| Item | Function/Description |
|---|---|
| Glucose-Insulin Simulator (e.g., Simglucose) | Provides a simulated, validated environment for training and initial testing of the DRL agent. |
| DRL Framework (e.g., TensorFlow, PyTorch) | Platform for implementing and training the neural network agent. |
| Enhanced Proximal Policy Optimization (PPO) Algorithm | The core DRL algorithm, modified with techniques like gradient clipping and value function clipping for stability [34]. |
| State Representation Vector | Input to the DRL agent, typically containing recent CGM values, delivered insulin, and other relevant historical data. |
| Dual Safety Mechanism | A proactive (safety-guided reward function) and reactive (external safety module) system to minimize hypoglycemia risk [34]. |
Procedure
- Environment Integration: Couple the DRL agent with a T1D simulation environment (e.g., Simglucose). The environment represents the patient's physiology, and the agent interacts with it by observing states, taking actions (insulin doses), and receiving rewards.
- Agent Training:
- State Definition (s): The state should include a time series of recent CGM values, recently delivered insulin doses, and potentially other signals like time of day.
- Action Definition (a): The action is the insulin basal rate or a discrete micro-bolus to be delivered at each time step.
- Reward Function (r): Design a reward function that strongly penalizes hypoglycemia, penalizes hyperglycemia, and rewards time spent in the target range (e.g., 70-180 mg/dL). This is the "proactive" safety component.
- Training Loop: The agent explores the state-action space over millions of simulation time steps. The enhanced PPO algorithm updates the agent's policy (πθ) to maximize cumulative reward.
- Safety Enhancement: Implement a "reactive" safety module that acts as an override. This module monitors the DRL agent's commanded insulin dose and can cap it based on conservative rules (e.g., limiting insulin based on Insulin-on-Board) to prevent excessive infusion.
- In-Silico Validation: Evaluate the trained controller's performance in the simulator using a virtual cohort of patients with varying insulin sensitivities. Key metrics include Time-in-Range (TIR), mean glucose, and percentage of time in hypoglycemia.
The logical structure of the DRL-based closed-loop system is as follows.
The artificial pancreas (AP) represents a transformative advancement in the management of Type 1 Diabetes (T1D), automating blood glucose regulation through a system of continuous glucose monitoring (CGM) and automated insulin delivery [62] [63]. As these systems transition from clinical supervision to real-world, unsupervised use, robust safety mechanisms become paramount [64]. The primary hazards of AP systems are over-dosing and under-dosing of insulin, which can lead to severe hypoglycemia or hyperglycemia respectively [64]. This document details the integration of proactive and reactive safety mechanisms, including a novel safety-enhanced Deep Reinforcement Learning (DRL) controller, within the broader context of closed-loop control system design for AP devices.
Safety in AP systems requires a multi-layered approach that addresses failures at the component level (sensors, pumps, algorithms) and the system level [64]. Proactive safety mechanisms aim to prevent adverse glycemic events before they occur, utilizing predictive algorithms and real-time risk assessment. In contrast, reactive safety mechanisms function as safety nets, intervening when glucose levels breach safe thresholds to correct dangerous trajectories. The dual safety framework of 'proactive guidance + reactive correction' has demonstrated significant promise in reducing the risks of both hyperglycemia and hypoglycemia [65].
A critical foundation for designing safety mechanisms is a clear understanding of the incidence and impact of hypoglycemia. The tables below summarize key epidemiological data on severe hypoglycemia and the performance metrics of advanced AP systems incorporating enhanced safety features.
Table 1: Epidemiology of Severe Hypoglycemia in Insulin-Treated Diabetes
| Patient Population | Incidence of Severe Hypoglycemia | Key Risk Factors |
|---|---|---|
| Type 1 Diabetes (T1D) | 70 to 159 events per 100 person-years [66] | Long duration of diabetes, impaired hypoglycemia awareness, previous severe hypoglycemia, C-peptide negativity [66] |
| Type 2 Diabetes (T2D) - Insulin-Treated | Up to 20 events per 100 person-years (varies by regimen) [66] | Insulin therapy, sulfonylureas, advanced age, renal or hepatic impairment, delayed/missed meals [66] |
Table 2: Performance Comparison of Advanced AP Controllers with Safety Enhancements
| Controller Type | Time in Range (TIR) % | Hypoglycemia Prevention | Key Safety Features |
|---|---|---|---|
| Safety-Enhanced DRL [65] | 87.45% (median) | Eliminated severe hypoglycemia and treatment failures | Dual safety mechanism (proactive + reactive); ten enhanced PPO tricks |
| Event-Triggered Dual-Hormone AP [49] | Effective control under disturbance | Reduced exercise-induced and postprandial hypoglycemia | ML-based glucose prediction; event-triggered PI/MPC control for insulin/glucagon |
| Standard Single-Hormone AP [62] | Improved over open-loop | Reduced but does not eliminate hypoglycemia | Threshold and predictive suspend features for low glucose |
Proactive Safety Mechanisms
Proactive mechanisms anticipate and prevent glycemic excursions, forming the first and most critical line of defense.
Predictive Glucose Monitoring and Alerting
Continuous Glucose Monitors (CGM) provide a stream of glucose values and, crucially, data on the rate of change (ROC) and direction of glucose [63]. Safety algorithms use this trend information to predict future glucose levels and issue alerts for impending hypoglycemia or hyperglycemia, allowing for preemptive action.
Model Predictive Control (MPC) and Safety Assurance
MPC, a dominant algorithm in commercial AP systems, uses a model of the patient's glucose-insulin dynamics to predict future glucose trajectories and compute optimal insulin doses [1]. Proactive safety is embedded by:
- Constraint Enforcement: Defining hard and soft constraints on predicted glucose levels to prevent the algorithm from recommending doses that would drive glucose below a safe threshold [64].
- Insulin-on-Board (IOB) Modeling: Accounting for active insulin already in the patient's system to prevent "stacking" of insulin doses, a common cause of hypoglycemia [1].
Deep Reinforcement Learning with Safety-Guided Learning
The safety-enhanced DRL controller represents a significant advancement in proactive safety [65]. It employs ten enhancements to the Proximal Policy Optimization (PPO) algorithm to improve training efficiency and safety. During the learning process, the DRL agent is guided by a safety critic that penalizes actions leading to dangerous glycemic states, shaping a policy that inherently avoids these regions. This "proactive guidance" ensures the control policy is robust to inter- and intra-patient variability.
Reactive Safety Mechanisms
Reactive mechanisms act as a safety net when proactive measures are insufficient or when rapid, unexpected glucose changes occur.
Threshold-Based Insulin Suspension
This is a foundational reactive safety feature. The system monitors CGM values and automatically suspends insulin delivery:
- Threshold Suspend: Stops insulin when glucose drops to a pre-set level (e.g., 70 mg/dL) [62].
- Predictive Suspend: Uses trend data to stop insulin delivery before glucose reaches the low threshold, offering superior prevention of hypoglycemia [62].
Dual-Hormonal Intervention with Glucagon
For scenarios where insulin suspension alone is inadequate to prevent hypoglycemia (e.g., during intense exercise), a dual-hormone AP can administer glucagon to actively raise blood glucose [62] [49]. The event-triggered SDHAP system uses a feedback controller to calculate and deliver a microdose of glucagon when hypoglycemia is imminent, providing an active counter-measure [49].
DRL Reactive Correction Layer
The safety-enhanced DRL controller incorporates a specific reactive layer that activates when the system's state is projected to enter a dangerous zone [65]. This layer can override the primary policy's actions and execute a pre-defined safety protocol, such as a temporary reduction or suspension of insulin basal rate.
Experimental Protocol: Validating a Safety-Enhanced DRL Controller
This protocol outlines the key steps for in-silico validation of a DRL-based AP controller with dual safety mechanisms, as described in [65].
Objective
To evaluate the safety and efficacy of a safety-enhanced DRL controller for fully closed-loop insulin delivery in T1D, using an approved simulator, and to compare its performance against baseline control strategies.
Materials and Reagents
Table 3: Research Reagent Solutions and Essential Materials
| Item | Function/Description | Example/Note |
|---|---|---|
| Simglucose Simulator | In-silico environment for testing and validating AP algorithms; contains a cohort of virtual T1D patients. | Accepted by regulatory bodies as a substitute for animal trials in early testing [65] [1]. |
| T1DiabetesGranada Dataset | Longitudinal, real-world CGM dataset used for training predictive models and validating system performance. | Contains over 257,000 patient-days of data [49]. |
| Continuous Glucose Monitor (CGM) | Provides real-time interstitial glucose measurements for the control algorithm. | Freestyle Libre, Dexcom G6, etc. [62] [9]. |
| Insulin Infusion Pump | Subcutaneous delivery of micro-boluses of insulin as commanded by the control algorithm. | Can be tethered (with tubing) or patch pump [62] [63]. |
| Deep Learning Framework | Platform for implementing and training the DRL agent (e.g., PyTorch, TensorFlow). | Used to build the enhanced PPO algorithm [65]. |
Methodology
Simulator Setup and Patient Cohort: Initialize the Simglucose simulator. Select a representative cohort of 100 virtual adult T1D patients with varying insulin sensitivities and daily routines.
Controller Implementation:
- Intervention Controller: Implement the safety-enhanced DRL controller. This includes:
- The core PPO algorithm enhanced with ten training tricks for stability and efficiency.
- The proactive guidance module, which shapes the reward function to heavily penalize trajectories toward hypoglycemia (<70 mg/dL) and hyperglycemia (>180 mg/dL).
- The reactive correction layer, which is a rule-based module that triggers a 30-minute insulin suspension if the CGM value is below 70 mg/dL and trending flat or down.
- Control Controllers: Implement baseline controllers for comparison, such as a standard PID controller and a traditional MPC controller without the specific DRL safety layers.
- Intervention Controller: Implement the safety-enhanced DRL controller. This includes:
Experiment Execution:
- Simulate a 7-day period for each virtual patient under each controller.
- Standardize meal challenges (e.g., 45g carbohydrates for breakfast, 60g for lunch, 50g for dinner) with ±10% variation.
- Introduce a moderate-intensity exercise session (45 minutes) on day 3 to test hypoglycemia prevention.
Data Collection and Outcome Measures:
- Record CGM traces for all patients and days.
- Calculate primary outcomes:
- Time in Range (TIR): Percentage of readings between 70-180 mg/dL.
- Time in Hypoglycemia: Percentage of readings <70 mg/dL and <54 mg/dL.
- Time in Hyperglycemia: Percentage of readings >180 mg/dL.
- GV (Glucose Variability): Coefficient of variation (CV).
Anticipated Results
As reported in [65], the safety-enhanced DRL controller is expected to achieve a median TIR of 87.45%, significantly outperforming the baseline controllers. Crucially, it should demonstrate a marked reduction or complete elimination of severe hypoglycemia (<54 mg/dL) due to the effective operation of its dual safety mechanisms.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents and Materials for AP Safety Research
| Category | Essential Item | Research Function |
|---|---|---|
| Software & Data | UVa/Padova T1D Simulator | Gold-standard in-silico testing and feasibility studies for new algorithms [1]. |
| Large-Scale CGM Datasets (e.g., T1DiabetesGranada) | Training and validation of data-driven models (AI/ML); real-world performance benchmarking [49]. | |
| Hardware Components | Research-Grade CGM | Provides high-frequency, reliable glucose measurements for closed-loop control [63] [64]. |
| Programmable Insulin Pump | Allows for precise, automated delivery of micro-boluses as dictated by experimental controllers [63] [64]. | |
| Algorithmic Tools | Model Predictive Control (MPC) | A benchmark control strategy against which new AI methods are compared [1] [49]. |
| Deep Reinforcement Learning (DRL) Frameworks | Platform for developing next-generation, adaptive, and personalized insulin dosing policies [65]. | |
| Event-Triggered Control Schemes | Reduces computational load and prevents simultaneous hormone delivery in DHAP systems [49]. |
The integration of proactive and reactive safety mechanisms is non-negotiable for the successful clinical implementation of artificial pancreas systems. The safety-enhanced DRL controller, with its dual 'proactive guidance + reactive correction' architecture, exemplifies the next generation of intelligent, adaptive, and safe closed-loop control for diabetes management [65]. As research progresses, the combination of advanced machine learning, robust control theory, and redundant safety systems will continue to push the boundaries of performance, minimizing the risk of severe hypoglycemia and hyperglycemia and improving the quality of life for individuals with diabetes.
Application Notes
Quantifying the Variability Challenge in Insulin Sensitivity
Effective closed-loop control for an Artificial Pancreas (AP) must account for significant inter- and intra-patient variability in insulin sensitivity (SI). Intra-patient variability manifests as diurnal patterns, with postprandial SI often lowest at breakfast compared to lunch or dinner, though this pattern is not uniform across all individuals [67]. Inter-patient variability is substantial, as demonstrated by the classification of at least seven distinct empirical SI daily patterns within a cohort of 20 subjects with Type 1 Diabetes (T1D) [67].
Table 1: Quantified Circadian Patterns of Insulin Sensitivity in T1D
| Meal | Average Postprandial SI (Normalized Pattern) | Observed Patterns (Probability) | Key Implication for AP Control |
|---|---|---|---|
| Breakfast (B) | Lower than L and D [67] | h-h-h (20%), h-h-l (15%), h-l-h (10%), h-l-l (15%), l-h-h (15%), l-h-l (15%), l-l-h (10%) [67] | Highest risk of postprandial hyperglycemia; requires aggressive pre-emptive control. |
| Lunch (L) | Higher than B [67] | Pattern-dependent (see previous column) [67] | Risk of over-delivery if breakfast-profile aggression is maintained. |
| Dinner (D) | Higher than B [67] | Pattern-dependent (see previous column) [67] | Requires personalized modulation to prevent nocturnal hypoglycemia. |
The integration of these time-varying SI profiles into the FDA-accepted University of Virginia/Padova T1DM simulator has enabled more robust in-silico testing of AP algorithms under multiple-meal scenarios, closely replicating in-vivo glucose excursions [67].
Adaptive Algorithm Architectures for Personalized Control
Adaptive control algorithms form the "brain" of the AP system, enabling real-time personalization. Two primary algorithmic families are prevalent:
- Model Predictive Control (MPC): This strategy uses a mathematical model of the patient's glucose-insulin dynamics to predict future glucose trajectories and pre-emptively optimize insulin delivery [2]. Its predictive nature is particularly suited to managing the slow dynamics of subcutaneous insulin absorption.
- Proportional-Integral-Derivative (PID) with Adaptation: PID controllers adjust insulin delivery based on the current glucose error (Proportional), the accumulation of past errors (Integral), and the predicted future trend (Derivative) [2]. Hybrid systems often combine MPC for basal regulation with PID for meal response.
Advanced implementations now incorporate machine learning (ML) for heightened personalization. A Smart Dual Hormone AP (SDHAP) can use Support Vector Machines (SVM) and K-Nearest Neighbor (KNN) algorithms to classify glycemic events (hypo-/hyperglycemia) and time-series models like ARIMA and Gated Recurrent Units (GRU) to predict future blood glucose levels [49]. These predictions can trigger a feed-forward controller to administer appropriate doses of insulin or glucagon, thereby rejecting meal and exercise-related disturbances [49].
Furthermore, model (in)validation techniques can be employed to ensure an individualized patient model remains valid throughout treatment. If the model no longer reflects the patient's status, the framework adapts the model to the current physiological condition, minimizing prediction error for dosage guidance [68].
Experimental Protocols
Protocol 1: Characterizing Intra-Patient Insulin Sensitivity Variability
Objective: To quantify diurnal patterns of insulin sensitivity in individuals with T1D for populating adaptive algorithm parameters.
Methodology:
- Subject Population: Recruit T1D subjects (e.g., n=20) with defined inclusion criteria (e.g., HbA1c ≤8.5%, normal gastric emptying) [67].
- Study Design: A 3-day inpatient study using a Latin square design. Subjects receive identical mixed-meal tests at breakfast, lunch, and dinner on separate days [67].
- Data Collection: Perform frequent blood sampling (e.g., at -180, -30, 0, 5, 10, 20, 30, 60, 90, 120, 150, 180, 240, 300, 360 min relative to meal time) to measure plasma glucose and insulin concentrations [67].
- Parameter Estimation: Apply the oral glucose minimal model to the plasma glucose and insulin data to calculate a quantitative SI value for each meal in each subject [67].
- Pattern Analysis: Normalize each subject's SI values to their maximum and classify the daily pattern into one of seven empirical classes (e.g., h-h-h, l-h-h, h-l-l) based on thresholds (e.g., values >60% of max are 'high') [67].
Table 2: Key Reagents and Materials for SI Variability Studies
| Research Reagent / Material | Function in Protocol |
|---|---|
| Triple-Tracer Mixed Meal | Allows for precise tracking of meal-derived glucose kinetics and accurate estimation of endogenous glucose production and SI. |
| Continuous Glucose Monitor (CGM) | Provides high-frequency interstitial glucose measurements between plasma samples; devices like Dexcom G7 offer high accuracy (MARD <9%) [2]. |
| Insulin Pump | Delivers subcutaneous insulin infusions; used to maintain basal rates and administer pre-meal boluses. |
| Oral Glucose Minimal Model | A computational tool used with plasma insulin and glucose data to mathematically derive insulin sensitivity. |
Protocol 2: In-Silico Validation of Adaptive AP Algorithms
Objective: To test and validate the performance of adaptive control algorithms using a simulated cohort of virtual patients before proceeding to clinical trials.
Methodology:
- Simulation Platform: Utilize the FDA-accepted University of Virginia/Padova T1DM Simulator [67].
- Virtual Cohort: Use the 100-adult in-silico population provided within the simulator. Link each virtual subject to a time-varying SI profile based on the probabilities of the seven empirical classes identified in Protocol 1 [67].
- Introduce Variability: Modulate the nominal SI pattern for each virtual subject with a multiplicative random noise (e.g., normal distribution, μ=1, σ=0.2) to simulate intra-subject deviations of up to 40% [67].
- Control Algorithm Testing: Implement the candidate adaptive algorithm (e.g., Event-Triggered MPC, Adaptive PID) to control insulin/glucagon delivery in the virtual cohort.
- Simulation Scenario: Simulate a multiple-meal day (e.g., breakfast at 7 a.m., lunch at 1 p.m., dinner at 7 p.m.) with a defined carbohydrate content. Optionally, introduce disturbances like missed meal boluses or exercise events [67] [49].
- Outcome Metrics: Evaluate algorithm performance based on:
- Percentage of Time in Range (TIR: 70-180 mg/dL)
- Time Below Range (TBR: <70 mg/dL)
- Time Above Range (TAR: >180 mg/dL)
- Mean glucose and glucose variability [49].
Protocol 3: Clinical Validation of a Smart Dual-Hormone AP
Objective: To assess the efficacy of an event-triggered, ML-informed dual-hormone AP system in an outpatient setting.
Methodology:
- System Setup: The SDHAP system integrates a CGM, two infusion pumps (for insulin and glucagon), and a control unit (e.g., a smartphone) running the adaptive algorithm [49].
- Data Preprocessing and Feature Extraction: Use a longitudinal CGM dataset (e.g., T1DiabetesGranada dataset). Extract time-series, statistical, and diabetes-specific features (TIR, TBR, TAR). Address data imbalance using techniques like SMOTE [49].
- Event Triggering: The control algorithm uses ML classifiers (SVM, KNN) to detect hypoglycemia or hyperglycemia events and time-series predictors (ARIMA, GRU) to forecast future glucose levels. A significant prediction or classification triggers the feedback/feed-forward controller [49].
- Hormone Delivery: Upon event triggering:
- For predicted hyperglycemia, the MPC or PI controller calculates an insulin dose.
- For predicted hypoglycemia, the controller calculates a glucagon dose [49].
- Trial Design: A randomized crossover study where participants use the SDHAP system versus a control therapy (e.g., sensor-augmented pump) for several weeks.
- Outcome Analysis: Compare glycemic outcomes (TIR, TBR, TAR) and safety endpoints between the intervention and control periods [49].
Visualization of System Architecture and Workflow
AP Adaptive Control Flow
SI Characterization Protocol
In artificial pancreas (AP) or automated insulin delivery (AID) systems, external disturbances such as meal intake and physical activity represent the most significant challenges to maintaining glucose homeostasis. Current commercial systems largely operate as hybrid closed-loop systems that require manual announcement of meals, creating user burden and potential treatment gaps when meals are unannounced. This article details advanced algorithmic techniques for the automated detection of meals and compensatory strategies for physical activity, which are critical steps toward fully automated insulin delivery. These approaches aim to reduce user burden while improving postprandial glucose control and preventing activity-induced hypoglycemia.
Automated Meal Detection and Size Estimation
Machine Learning Approaches
Recurrent Neural Networks (RNNs) utilizing Long Short-Term Memory (LSTM) with 1D convolution layers have demonstrated high accuracy in detecting meal and physical activity events from free-living data. These models process continuous glucose monitoring (CGM) data, insulin infusion information, and historical meal patterns to identify disturbances without requiring manual input [69] [70]. The best-performing RNN models achieved an overall accuracy of 92.32% in identifying patient states (meal, exercise, both, or neither), with specific detection accuracies of 98.05% for meals, 93.42% for exercise, and 55.56% for concurrent meal-exercise events [70].
Neural network-based meal detection systems have been clinically validated in closed-loop systems. One study utilizing a neural network model for meal detection and size estimation demonstrated a sensitivity of 83.3%, a false discovery rate of 16.6%, and a mean detection time of 25.9 minutes from meal onset [71] [72]. This system contributed to a significant 10.8% reduction in time above range (glucose >180 mg/dL) compared to model predictive control (MPC) alone, without increasing hypoglycemia risk [71].
Table 1: Performance Comparison of Meal Detection Algorithms
| Algorithm Type | Sensitivity | False Discovery Rate | Detection Time | Reference |
|---|---|---|---|---|
| Neural Network Model | 83.3% | 16.6% | 25.9 minutes | [71] [72] |
| LSTM with 1D Convolution | 98.05% | - | - | [70] |
| RNN Models (Range) | 89.9%-95.7% | - | - | [69] |
Meal Detection Experimental Protocol
Objective: To validate the performance of a neural network-based meal detection and size estimation algorithm in a closed-loop artificial pancreas system.
Materials:
- Continuous Glucose Monitoring system (Dexcom G6)
- Insulin pump (t:slim X2 or OmniPod)
- Custom smartphone application or research platform
- Standardized meals (45-66g carbohydrates)
Methodology:
- Participant Preparation: Recruit adults with type 1 diabetes. Participants should have at least 3 months of CGM experience.
- Algorithm Training: Utilize historical data including CGM values, insulin delivery (basal and bolus), and meal carbohydrates to train the neural network model.
- Study Design: Conduct a randomized, single-center crossover trial comparing postprandial glucose control following unannounced meals using:
- Hybrid MPC algorithm (control)
- Robust Artificial Pancreas (RAP) with automated meal detection [71]
- Meal Protocol: Participants consume unannounced meals with carbohydrate content between 45-66g. The meal detection algorithm continuously analyzes CGM data and insulin delivery.
- Detection Parameters: The algorithm generates a meal probability score every 5 minutes. A detection threshold of PTH = 0.86 is used to trigger a meal announcement [71].
- Outcome Measures:
- Primary: Postprandial incremental area under the curve (iAUC) of glucose
- Secondary: Time above range (>180 mg/dL), time in range (70-180 mg/dL), time below range (<70 mg/dL)
- Algorithm performance: Sensitivity, false discovery rate, mean detection time
Analysis: Compare glucose outcomes between MPC and RAP arms using paired t-tests or Wilcoxon signed-rank tests. Statistical significance is defined as p < 0.05.
Figure 1: Meal Detection Algorithm Workflow
Physical Activity Compensation Strategies
Ensemble Model Predictive Control (EnMPC)
The Ensemble Model Predictive Control (EnMPC) framework addresses unannounced exercise by utilizing personalized, physiologically inspired models of glucose homeostasis. This approach identifies patient-specific exercise-induced signatures through regularized deconvolution on historical data (net effect method) [73]. The controller incorporates these signatures to anticipate the impact of future exercise bouts and adjust insulin delivery proactively.
Key Components:
- Multiple Behavioral Scenarios: EnMPC employs a set of regular MPC controllers, each accounting for a specific behavioral scenario (including exercise).
- Probability-Weighted Consensus: The final control action is computed as a consensus among the individual MPC outputs, weighted by the probability of each scenario.
- Net Effect Method: This technique characterizes subject-specific exercise responses by analyzing historical CGM, insulin, meal, and activity data to create personalized disturbance models [73].
Table 2: Physical Activity Compensation Techniques in AP Systems
| Technique | Mechanism | Advantages | Limitations |
|---|---|---|---|
| Ensemble MPC | Multiple model predictive controllers with scenario probability weighting | Anticipates exercise rather than reacting; personalized signatures | Requires extensive historical data [73] |
| Dual-Hormone AP | Delivery of both insulin and glucagon based on glucose predictions | Enhanced hypoglycemia prevention during exercise | Increased system complexity; glucagon stability issues [49] |
| Event-Triggered Control | Controller activation based on glucose level classification | Reduced computational burden; prevents simultaneous hormone infusion | Requires accurate glucose prediction [49] |
Physical Activity Compensation Experimental Protocol
Objective: To validate the efficacy of Ensemble MPC in preventing hypoglycemia during and after unannounced exercise in adults with type 1 diabetes.
Materials:
- CGM system
- Insulin pump
- Activity tracker (optional)
- Glucose analyzer for reference measurements
- Treadmill or stationary bicycle
Methodology:
- Subject Recruitment: Enroll adults with type 1 diabetes using insulin pump therapy.
- Data Collection: Collect at least 30 days of historical data including CGM, insulin delivery, meal records, and physical activity.
- Model Personalization:
- Use the net effect method to derive subject-specific exercise signatures
- Develop personalized models of glucose-insulin dynamics for each participant
- Exercise Protocol:
- Participants perform 30 minutes of mild to moderate intensity exercise (45-60% VOâ‚‚max) in the afternoon (4:00-4:30 PM)
- Exercise is performed in the transition from absorptive to postabsorptive state
- Dinner is scheduled at 7:00 PM to assess late post-exercise hypoglycemia
- Controller Implementation:
- Compare Ensemble MPC against standard MPC
- EnMPC utilizes exercise signatures to anticipate insulin adjustments
- Outcome Measures:
- Primary: Time spent in hypoglycemia (<70 mg/dL) during and after exercise
- Secondary: Mean glucose, glucose variability, time in range (70-180 mg/dL)
Analysis: Compare outcomes between control strategies using paired statistical tests with significance defined as p < 0.05.
Integrated System Architecture
Advanced artificial pancreas systems combine meal detection and physical activity compensation within a unified control framework. The Robust Artificial Pancreas (RAP) system integrates a neural network meal detector with model predictive control, automatically delivering insulin boluses for detected meals while maintaining safety constraints [71]. Similarly, Event-Triggered Smart Dual Hormone Artificial Pancreas (SDHAP) systems incorporate both insulin and glucagon delivery based on classified glycemic events, with feedforward control for disturbance rejection [49].
Figure 2: Integrated AP System Architecture
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for AP Development
| Component | Specification | Research Application |
|---|---|---|
| CGM System | Dexcom G6, Medtronic Guardian, FreeStyle Libre | Continuous glucose monitoring at 1-5 minute intervals; primary input for control algorithms [74] [49] |
| Insulin Pump | Tandem t:slim X2, Insulet OmniPod, Medtronic 670G/780G | Programmable insulin delivery capable of receiving external commands from control algorithms [1] |
| Research Platform | Android APS, OpenAPS, University of Virginia DiAs | Software platform integrating CGM, pump communication, and control algorithms for clinical testing [1] |
| Simulation Environment | FDA-approved UVA/Padova T1D Simulator | Pre-clinical validation of control algorithms; contains virtual patient populations (adults, adolescents, children) [74] [73] |
| Activity Monitor | Wearable devices (ActiGraph, Fitbit), heart rate monitors | Objective measurement of physical activity intensity and duration for model personalization [73] |
| Reference Glucose Analyzer | YSI 2300 STAT Plus | Gold-standard blood glucose measurement for CGM calibration and protocol safety [71] |
Automated meal detection and physical activity compensation represent critical advancements toward fully automated artificial pancreas systems. Machine learning approaches, particularly LSTM-based neural networks, show promising accuracy in detecting meals with minimal delay. For physical activity, Ensemble MPC strategies that anticipate exercise effects through personalized signatures offer improved hypoglycemia protection. Integration of these disturbance management techniques into unified control architectures demonstrates significant improvements in time-in-range metrics while reducing user burden. Future research directions should focus on enhancing detection specificity, reducing false positive rates, and developing adaptive algorithms that continuously refine personalization based on accumulated data.
In the design of cyber-physical-human systems (CPHS), such as the artificial pancreas (AP) for type 1 diabetes management, human-factor engineering is critical for ensuring safety, efficacy, and user adoption. A primary design objective must be the reduction of the significant cognitive burden placed on users by traditional management tasks, which include carbohydrate counting, insulin dose calculations, and constant glucose monitoring [8] [75]. Recent user-centered research reveals that while improving glycemic control is a key outcome, the pervasive desire among both youth and parents is for a system that minimizes the physical and emotional burden of diabetes management [76]. This application note details protocols and design principles for integrating human-factor engineering into the development of closed-loop systems, with a specific focus on quantifying and reducing user burden to enhance long-term engagement and quality of life.
Quantitative Evaluation of User Burden and Interface Aesthetics
A systematic approach to evaluating user interfaces and system interactions is essential for objective improvement. The following methodologies provide a framework for quantifying cognitive load and visual design effectiveness.
Protocol: Thematic Analysis of User Desired Features
Objective: To identify and prioritize the specific features of an AP system that users associate with reduced physical and emotional burden. Methodology:
- Participant Recruitment: Recruit a diverse sample of end-users (e.g., youth with type 1 diabetes, ages 10-25, and parents) aiming for representation across age, gender, and technology experience [76].
- Data Collection: Conduct semi-structured interviews, audio-recorded and transcribed verbatim. Example interview questions should broadly examine preferences for system appearance, functionality for meals and exercise, and beneficial additional features [76].
- Data Analysis: Employ thematic analysis using qualitative data analysis software (e.g., NVivo). Multiple trained coders should independently review transcripts to identify recurring themes. A significant portion (e.g., ~75%) of transcripts should be double-coded to ensure reliability and data saturation, with coders discussing discrepancies until consensus is reached [76].
- Output: A list of prioritized user-desired features, categorized by physical burden reduction (e.g., less user responsibility for glucose management) and emotional burden reduction (e.g., mitigating negative reactions to alerts, increasing feelings of normalcy) [76].
Protocol: Quantitative Aesthetic Evaluation of Human-Machine Interface
Objective: To objectively calculate the aesthetic degree of a human-machine interaction interface layout, a factor critically affecting perceived usability and satisfaction [77]. Methodology:
- Aesthetic Factor Extraction: Using Kansei engineering methods, extract the key aesthetic image factors that affect user perception. Through factor analysis of user surveys, six core factors with their respective weights have been identified [77]:
- Proportion (Weight: 0.244)
- Conciseness (Weight: 0.181)
- Order (Weight: 0.153)
- Rhythm (Weight: 0.133)
- Density (Weight: 0.126)
- Equilibrium (Weight: 0.110)
- Aesthetic Value Calculation: For a given interface layout, calculate the aesthetic value (Q) for each factor using its specific mathematical formula. For example, the aesthetic value for "Proportion" is calculated based on the ratio of element dimensions and their alignment to the golden ratio (1.618) [77].
- Comprehensive Aesthetic Degree: Calculate the overall aesthetic degree (M) of the interface using the weighted sum of the individual factors: M = Σ (Weighti × Qi).
- Scheme Ranking: Use the TOPSIS (Technique for Order Preference by Similarity to Ideal Solution) method to rank different design schemes based on their comprehensive aesthetic degree (M) and proximity to the ideal aesthetic solution [77].
Table 1: Aesthetic Image Factors and Calculation Weights
| Aesthetic Image Factor | Variance Contribution (Weight) | Primary Design Consideration |
|---|---|---|
| Proportion | 0.244 | Alignment of element dimensions to the golden ratio. |
| Conciseness | 0.181 | Minimalism and lack of extraneous elements. |
| Order | 0.153 | Logical grouping and arrangement of elements. |
| Rhythm | 0.133 | Repetition and regular patterns in the layout. |
| Density | 0.126 | The amount of information presented per unit area. |
| Equilibrium | 0.110 | Visual balance and symmetry of the interface. |
Protocol: Modeling Human-Machine Interaction in Multitasking Environments
Objective: To quantitatively model human operator (HO) performance during multiple simultaneous tasks, simulating real-world conditions where a user must interact with a device while managing other activities [78]. Methodology:
- Task Setup: Utilize a standardized task battery like the Multi-Attribute Task Battery (MATB). This software presents subjects with four discrete simultaneous tasks: monitoring lights (L), monitoring dials (D), managing communications channels (C), and managing communications frequencies (F) [78].
- Performance Metric: Model performance using the human-machine interaction (HMI) performance function. The machine presents information at a specific baud rate (BIN, in bits/sec), and the human operator responds with their own baud rate (BO). The key metric is the baud ratio (BÌ„ = BO / BIN), which describes the efficiency of human information processing [78].
- Experimental Design: Conduct a within-subjects factorial design where the total machine-initiated baud rate (B_IN) is varied across several levels (e.g., 0.70, 1.14, 1.27, 1.73, and 2.18 bits/s). The task baud rates are adjusted by proportionally changing interstimulus intervals [78].
- Data Analysis: Calculate the fraction of correct responses for each task component over the test period. The general pattern observed is that the baud ratio (BÌ„) decreases as the machine-initiated baud rate (B_IN) increases, demonstrating a fundamental limit on human multi-task performance [78].
Application to Artificial Pancreas System Design
Integrating the above principles leads to concrete design strategies and validated system architectures for next-generation artificial pancreas systems.
Design Strategies for Burden Reduction
Table 2: Strategies for Reducing Cognitive and Physical Burden in AP Design
| Burden Category | User-Identified Desired Feature | Implementation Example |
|---|---|---|
| Physical Burden | Lessen user responsibility for glucose management for food/exercise. | Fully automated insulin dosing without carbohydrate counting, as seen in the iLet Bionic Pancreas which is initialized only with body weight [75]. |
| Physical Burden | Reduce need to wear or carry multiple devices. | Develop integrated, miniaturized form factors that combine a continuous glucose monitor (CGM) and insulin pump [76] [8]. |
| Emotional Burden | Mitigate negative emotional reactions to alerts. | Implement smart, context-aware alert systems that reduce alarm fatigue and frequency [76]. |
| Emotional Burden | Increase feelings of normalcy. | Design for discreet use and minimize the need for public interactions with the device, enhancing psychosocial well-being [76]. |
Experimental Workflow for Closed-Loop Control Evaluation
The following diagram illustrates the integrated workflow for evaluating a closed-loop artificial pancreas system from a human-factor and physiological control perspective.
Signaling Pathway for Intravenous Pulse-Modulated Closed-Loop Control
A novel approach to stable glucose control involves translating endocrine physiology into an electronic equivalent. The following diagram details the signaling pathway for a pulse-modulated, bi-hormonal (insulin and glucagon) artificial pancreas based on intravenous administration, which offers more rapid response than subcutaneous delivery [18].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for AP Human-Factor Research
| Tool / Reagent | Function in Research |
|---|---|
| Continuous Glucose Monitor (CGM) | Provides real-time interstitial glucose measurements, serving as the primary feedback signal for the closed-loop control algorithm [8] [18]. |
| Insulin Pump | A miniature, wearable device for subcutaneous or intraperitoneal insulin delivery. Acts as the final control element in the automated system [8]. |
| Multi-Attribute Task Battery (MATB) | Standardized software for evaluating human performance and cognitive load during multiple simultaneous tasks, simulating real-world demands on user attention [78]. |
| NVivo Software | A qualitative data analysis platform used for coding and thematic analysis of transcribed user interviews, enabling systematic identification of user needs and burdens [76]. |
| Stable Glucagon Formulation | A bihormonal approach requires a stable, soluble glucagon analog for subcutaneous delivery to mitigate hypoglycemia risk, allowing for more aggressive insulin dosing [8] [18]. |
| Network Simulator (e.g., SIMetrix) | Software used for in-silico testing and validation of control algorithms by simulating the patient's glucose-insulin dynamics (e.g., using resistor-capacitor models of the gastrointestinal tract) before clinical trials [18]. |
| Color Contrast Analyzer | A tool (e.g., integrated in axe DevTools) to verify that text and interface elements meet WCAG AA guidelines (minimum 4.5:1 contrast ratio for small text), ensuring accessibility for users with low vision [79] [80]. |
Benchmarking Performance: From Clinical Trials to Real-World Efficacy
Automated insulin delivery (AID) systems, commonly known as the artificial pancreas, represent the pinnacle of technological advancement in diabetes management. These closed-loop systems have transitioned from a disputed concept in 2005 to the modern standard of care for type 1 diabetes (T1D) today, with expanding applications in type 2 diabetes (T2D) populations [1]. The development and validation of these systems through rigorous pivotal trials have been instrumental in demonstrating their safety and efficacy across diverse patient populations. This review synthesizes pivotal trial outcomes for three major commercial AID systems: Tandem Diabetes Care's Control-IQ, Medtronic's MiniMed 780G, and Insulet's OmniPod 5. We examine the experimental protocols, glycemic outcomes, and safety profiles that underpin regulatory approvals and provide researchers with standardized methodologies for evaluating closed-loop control system performance. The structured analysis of these trials within the context of artificial pancreas design offers critical insights for researchers and drug development professionals working to advance diabetes technology.
Control-IQ System (Tandem Diabetes Care)
Experimental Protocol: The Control-IQ system underwent evaluation through multiple randomized controlled trials (RCTs) that established its efficacy for type 1 diabetes across age groups. The pivotal trials employed a standardized methodology beginning with a run-in phase where participants used sensor-augmented pump therapy without automation. Subsequently, subjects were randomized to either the Control-IQ group or a control group using continuous glucose monitoring (CGM) with non-automated insulin delivery [81]. The primary studies included:
- DCLP3 Trial: 168 adolescents and adults (14-72 years) across seven sites with a 26-week intervention period [81]
- DCLP5 Trial: 101 children (6-<14 years) across four sites with a 16-week intervention period [81]
- PEDAP Trial: 102 children (2-<6 years) across three sites with a 13-week intervention period [81]
A distinctive feature of these trials was the absence of HbA1c restrictions, allowing enrollment of participants with a wide spectrum of baseline glycemic control. The control groups used real-time Dexcom G6 CGM with various insulin delivery methods including multiple daily injections (MDI) or insulin pumps without automation [81].
Type 2 Diabetes Application: More recently, a pivotal trial evaluated Control-IQ+ technology for type 2 diabetes, utilizing a randomized controlled design with 319 participants across 21 clinical centers [82]. This 13-week study compared the AID system against a control group continuing their pre-study insulin delivery method with CGM. The study notably included a racially and socioeconomically diverse population aged 19-87 years, with 75% of participants using fixed-dose insulin regimens prior to enrollment [82].
MiniMed 780G System (Medtronic)
Experimental Protocol: The MiniMed 780G advanced hybrid closed-loop (AHCL) system was evaluated in a multicenter single-arm study involving 157 individuals (39 adolescents aged 14-21 years and 118 adults aged ≥22-75 years) with type 1 diabetes [83]. The study design incorporated:
- Baseline Period: Approximately 14 days using sensor-augmented pump therapy with or without predictive low glucose management [83]
- Intervention Period: Approximately 90 days using AHCL with automated basal and correction bolus features [83]
- Target Rotation: Glucose targets were set at 100 mg/dL or 120 mg/dL for approximately 45 days each in a crossover manner [83]
The system features a default target of 100 mg/dL (with 120 mg/dL option), programmable insulin action time from 2-8 hours, and automatic corrections every five minutes [84]. The U.S. pivotal trial demonstrated high user satisfaction with 96% of participants indicating the system was easy to use [84].
OmniPod 5 System (Insulet)
Experimental Protocol: The OmniPod 5 system, as the first tubeless AID system, underwent evaluation through distinct pivotal trials for type 1 and type 2 diabetes.
Type 1 Diabetes Trial: A single-arm, multicenter, prospective study enrolled 240 participants (111 children aged 6-13.9 years and 124 adults/adolescents aged 14-70 years) with type 1 diabetes [85]. The study design included:
- Standard Therapy Phase: 2 weeks using pre-study diabetes management
- Intervention Phase: 3 months using the OmniPod 5 AID system [85]
All participants had HbA1c levels below 10% at enrollment and had no restrictions regarding eating or exercise during the study period [85].
Type 2 Diabetes Trial (SECURE-T2D): This landmark study represented the largest, longest, and most racially diverse AID study conducted in people with type 2 diabetes [86]. The trial included 305 participants from 21 sites across the U.S., with 24% Black and 22% Hispanic representation [86]. Participants were adults aged 18-75 years with type 2 diabetes requiring insulin, with baseline HbA1c between 7-12% for basal insulin users and ≤12% for those using basal-bolus or pre-mixed insulin [86]. The 13-week study followed an initial 14-day standard therapy period, with OmniPod 5 use thereafter.
Comparative Efficacy Outcomes
Glycemic Control Metrics
Table 1: Glycemic Outcomes from Major AID System Pivotal Trials
| System | Population | Time in Range (TIR) Change | HbA1c Reduction | Time Below Range (<70 mg/dL) |
|---|---|---|---|---|
| Control-IQ | T1D (Pooled analysis) | +11.5% (∼2.8 h/day) [81] | -0.4% to -0.5% [81] | Significant reduction [81] |
| Control-IQ+ | T2D | +16% (3.8 h/day) [82] | -0.9% (from 8.2% to 7.3%) [82] | Low in both groups, no increase [82] |
| MiniMed 780G | T1D (Adolescents & Adults) | +5.7% (from 68.8% to 74.5%) [83] | -0.5% (from 7.5% to 7.0%) [83] | -1.0% (from 3.3% to 2.3%) [83] |
| OmniPod 5 | T1D (Adults/Adolescents) | +9.2% (∼2.2 h/day) [85] | -0.38% (from 7.16% to 6.78%) [85] | -0.9% (from 2.0% to 1.1%) [85] |
| OmniPod 5 | T1D (Children) | +15.5% (∼3.7 h/day) [85] | -0.68% (from 7.67% to 6.99%) [85] | No significant change [85] |
| OmniPod 5 | T2D (SECURE-T2D) | +21% (4.8 h/day) [86] | -0.8% (from 8.2% to 7.4%) [86] | Non-inferior to standard therapy [86] |
Additional Efficacy Endpoints
Control-IQ System: The pooled analysis of three RCTs demonstrated consistent benefits across all age groups from 2-72 years, with statistically similar treatment effects regardless of race-ethnicity, household income, pre-study CGM use, or pre-study insulin delivery method [81]. Participants with the highest baseline HbA1c levels showed the greatest improvements in TIR and HbA1c [81]. The system also significantly reduced mean glucose, hyperglycemia metrics, and HbA1c across all cohorts [81].
MiniMed 780G System: The pivotal trial showed particularly strong overnight glycemic control, with nighttime TIR increasing to 82% [84]. The system achieved a mean sensor glucose of 148 mg/dL overall and 144 mg/dL at the default 100 mg/dL target [84]. Optimization of the active insulin time setting to 2 hours further improved TIR to 79% without increasing hypoglycemia [84].
OmniPod 5 System: In type 1 diabetes, the system demonstrated prominent overnight glycemic control with 78% TIR in both adult/adolescent and pediatric cohorts [85]. For type 2 diabetes, the SECURE-T2D trial showed particularly strong benefits in those with higher baseline HbA1c, with a reduction of 2.1% in participants with baseline HbA1c ≥9.0% [86]. The system also reduced total daily insulin dose from 0.80 U/kg/day to 0.57 U/kg/day, corresponding to an average decrease of 23 U/day [86].
Safety Outcomes and Adverse Events
Table 2: Safety Profiles from Pivotal Trials
| System | Severe Hypoglycemia | Diabetic Ketoacidosis (DKA) | Other Serious Adverse Events |
|---|---|---|---|
| Control-IQ (T1D) | No events reported in pivotal trials [81] | No events reported in pivotal trials [81] | Not specified in available data |
| Control-IQ+ (T2D) | 1 event in treatment group (successfully treated) [82] | No events [82] | No new safety signals unique to T2D [82] |
| MiniMed 780G (T1D) | No events [83] | No events [83] | None reported [83] |
| OmniPod 5 (T1D) | 3 cases across both cohorts [85] | 1 case [85] | Not attributable to automated insulin delivery malfunction [85] |
| OmniPod 5 (T2D) | 1 occurrence (deemed unrelated to device) [86] | No events [86] | 13 additional serious adverse events, none glycemia-related or device-related [86] |
Across all systems, safety was a paramount outcome with no unanticipated safety signals emerging. The MiniMed 780G pivotal trial specifically reported no severe hypoglycemia or diabetic ketoacidosis events during the study phase [83]. Similarly, the Control-IQ trials reported no severe hypoglycemia or DKA events in their T1D trials [81], while the Control-IQ+ T2D trial reported minimal safety events [82]. The OmniPod 5 system had low rates of severe hypoglycemia and DKA that were considered below observed rates in type 1 diabetes generally and not attributable to AID malfunction [85].
System Architectures and Algorithmic Approaches
The major commercial AID systems employ distinct control algorithms that merit examination within artificial pancreas research:
Control-IQ Technology: Utilizes a model predictive control (MPC) algorithm originally developed for chemical process industries [1]. The system automates both basal insulin delivery and correction boluses, with the auto-bolus feature identified as having substantial impact, particularly in participants with poor baseline glycemic control [81].
MiniMed 780G System: Employs proportional integral derivative (PID) algorithms with the addition of a fuzzy logic algorithm responsible for administering correction boluses [1]. The system features automated basal delivery and automated bolus correction every 5 minutes [83]. The ability to set a lower glucose target (100 mg/dL) and programmable insulin action time (2-8 hours) contributes to its efficacy [84].
OmniPod 5 System: As the first tubeless AID system, it uses a MPC-based algorithm [1]. The system integrates with a continuous glucose monitor to automate insulin delivery without multiple daily injections or fingersticks, and can be controlled by a compatible personal smartphone in the U.S. [86].
The Researcher's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Components for AID System Development
| Research Component | Function in AID Development | Exemplars from Pivotal Trials |
|---|---|---|
| Universal Research Platforms | Enable automated communication between various CGM devices, insulin pumps, and control algorithms | APS (University of California, Santa Barbara) [1] |
| Diabetes Simulators | Substitute for animal trials in testing AID algorithms; accelerate development | Padova/Virginia T1D Simulator (FDA-accepted) [1] |
| Control Algorithms | Direct insulin delivery based on CGM readings and other factors | Model Predictive Control (MPC), Proportional Integral Derivative (PID), Fuzzy Logic [1] |
| Standardized Metrics | Enable consistent efficacy evaluation across clinical trials | Time in Range (TIR), HbA1c, Time Below Range (TBR) [83] [86] [81] |
| Patient-Reported Outcome Measures | Assess quality of life and treatment satisfaction | Diabetes distress scales (T2-DDAS), usability questionnaires [83] [86] |
Experimental Workflow for AID System Validation
The pivotal trial outcomes for major commercial AID systems demonstrate consistent and clinically significant improvements in glycemic control across diverse patient populations with both type 1 and type 2 diabetes. These systems have established a new standard for diabetes management, with the artificial pancreas transitioning from research concept to clinical reality within two decades [1]. The structured methodologies and standardized endpoints developed through these trials provide researchers with robust frameworks for evaluating closed-loop control system performance. Future developments in AID technology will likely build upon these foundational trials, potentially incorporating dual-hormone approaches, adaptive algorithms, and increasingly personalized control strategies. The continued refinement of artificial pancreas systems represents one of the most promising frontiers in diabetes technology research, with potential to substantially reduce the burden of diabetes management while improving metabolic outcomes across the spectrum of diabetes populations.
Application Note
In-silico validation, which employs computer modeling and simulation, has become an indispensable tool in the development and regulatory approval of advanced medical devices, including Artificial Pancreas (AP) systems for Type 1 Diabetes management. For researchers and drug development professionals, this methodology provides a powerful, cost-effective, and ethical platform for conducting preliminary algorithm testing and exhaustively identifying edge cases that are rare, dangerous, or impractical to replicate in initial human trials [87]. By creating a virtual replica of the physiological system, in-silico trials enable the rigorous verification of a device's safety and efficacy, de-risking the development process before committing to costly and time-consuming clinical studies [87]. This application note details the implementation of a structured in-silico validation framework, specifically contextualized for closed-loop control system design in artificial pancreas research.
The In-Silico Validation Framework for an Artificial Pancreas
The core of a robust in-silico study is a credible model and a structured validation process. The following workflow, adapted from the ASME V&V 40 standard, provides a systematic approach for AP development [87].
The process begins by defining the Question of Interest, such as "Does my novel PID controller maintain glycemic control without meal announcement for a virtual population?" [88]. This is formalized through the Context of Use (COU), which precisely specifies how the model's predictions will answer the question [87]. A Risk Analysis is then performed, evaluating the consequence of an incorrect model prediction and the model's influence on the final decision [87]. This risk directly informs the Credibility Goals—the required level of evidence from verification and validation (V&V) activities [87]. Verification ensures the model is solved correctly, while Validation ensures it accurately represents the real physiology, such as comparing simulated glucose levels against clinical data [87]. Uncertainty Quantification (e.g., via Monte Carlo simulations) is critical for assessing the impact of parameter variability on the outcomes [89]. Only when the achieved credibility meets the pre-set goals should the model be used for final AP algorithm testing and edge case identification.
Key Advantages in Artificial Pancreas Research
The adoption of in-silico methods offers several distinct advantages for AP research and development:
- Comprehensive Pre-clinical Testing: Simulations allow for the testing of control algorithms under a vast range of conditions, including rare but critical edge cases like sudden glucose surges or sensor failures, which are ethically and practically challenging to create in human trials [87] [90].
- Accelerated Development Cycles: In-silico trials can be run much faster than clinical studies, enabling rapid iterative design and optimization of control algorithms, such as the time-varying PID controller for intraperitoneal insulin delivery described in recent research [88].
- Regulatory De-risking: Regulatory agencies like the FDA and EMA now consider credible in-silico evidence in submissions. Frameworks like ASME V&V 40 provide a pathway for demonstrating model credibility, which supports the qualification of new methods [87] [91].
- Mechanistic Insight: Simulations provide a window into internal physiological states (e.g., insulin concentrations in various compartments) that are difficult or impossible to measure in a clinical setting, thereby offering deeper insights into the algorithm's performance [18].
Protocols
Protocol 1: Implementing a Tidy Simulation for Algorithm Comparison
This protocol provides a standardized, reproducible, and scalable method for comparing the performance of different closed-loop control algorithms using a "tidy simulation" framework [92]. This approach is modular, facilitating iterative exploration and robust statistical analysis.
2.1.1 Objective: To systematically evaluate and compare the performance of multiple control algorithms (e.g., PID vs. Model Predictive Control) across a defined set of virtual patient phenotypes and challenging conditions.
2.1.2 Research Reagent Solutions The following computational tools are essential for implementing this protocol:
Table 1: Essential Research Reagent Solutions for In-Silico AP Testing
Item Function/Description Example/Note T1D Simulator A validated computational model of glucose-insulin dynamics in a virtual population. FDA-accepted T1D simulators (e.g., updated for intraperitoneal delivery [88]). Control Algorithm The logic for automated insulin (and/or glucagon) delivery. Time-varying PID [88], pulse-modulated controllers [18]. Simulation Framework Software environment for designing and running in-silico experiments. R,Python,MATLAB/Simulink; using tidy principles [92].Virtual Patient Cohort A population of in-silico subjects with varying physiological parameters. Represents inter-subject variability (e.g., different insulin sensitivities). Performance Metrics Quantitative measures for evaluating algorithm performance. Time-in-range (TIR), hypoglycemia events, control-variability grid analysis (CVGA). 2.1.3 Workflow The tidy simulation workflow is structured around four sequential, independent components, as illustrated below [92].
Define the Simulation Grid: Create a tidy data frame where each row represents a unique combination of simulation factors (variables) to be tested [92].
- Data Generation Factors: Sample size (number of virtual subjects), treatment effect size, meal composition, virtual patient phenotype.
- Analysis Factors: Type of control algorithm (e.g., PID, MPC), controller parameters (e.g., gain settings), outcome type (e.g., time-in-range).
- Example: A full-factorial grid of 3 algorithms × 100 virtual subjects × 2 meal sizes × 5 controller gain settings would generate 3,000 unique simulation runs.
Implement the Data Generation Function: This function takes parameters from a row of the simulation grid and outputs a simulated dataset. It encapsulates the T1D simulator to generate glucose-time series data for a virtual subject under the specified conditions (e.g., with a specific meal challenge) [92] [88].
Implement the Analysis Function: This function accepts a single generated dataset and the relevant analysis factors from the simulation grid. It runs the specified control algorithm on the dataset and computes the performance metrics (e.g., time-in-range, hypoglycemia events) [92].
Compile the Results Table: The outputs from the analysis function are collected into a final tidy data frame. Each row corresponds to a row in the original simulation grid, with additional columns for the computed performance metrics. This table is the direct input for statistical analysis and visualization [92].
2.1.4 Data Analysis and Interpretation The final Results Table allows for straightforward statistical comparison. Use linear mixed-effects models or ANOVA to analyze the effect of the factors (e.g.,
Algorithm Type,Meal Size) on the performance metrics (e.g.,Time-in-Range). Generate visualizations such as box plots (Algorithm on the x-axis, Time-in-Range on the y-axis, faceted by Meal Size) to interpret the results.
Protocol 2: Systematic Identification of Algorithm Edge Cases
This protocol describes a method for proactively identifying failure modes and edge cases of an AP algorithm using virtual validation techniques [90].
2.2.1 Objective: To stress-test a stable control algorithm under extreme and rare conditions to uncover its performance boundaries and potential failure modes.
2.2.2 Workflow
Define Edge Case Scenarios: Collaborate with clinical experts to define a catalogue of challenging scenarios. These should include:
- Sensor and Actuator Faults: Continuous glucose monitor (CGM) signal drop-out, insulin pump occlusion, corrupted CGM data (e.g., pressure-induced sensor attenuations).
- Unannounced Extreme Events: Very high-glycemic index meals, missed meals leading to fasting, intense physical activity.
- Unrealistic Physiological Parameters: Simulate virtual patients with parameters at the extreme bounds of physiological plausibility (e.g., very low or high insulin sensitivity).
Incorporate Variability: For each scenario, incorporate variability in key parameters (e.g., meal timing and size, initial glucose level) to ensure a wide coverage of the potential event space [90].
Execute Monte Carlo Simulations: Run the simulation framework from Protocol 1, using a simulation grid focused on these edge cases. Employ Monte Carlo techniques to propagate uncertainty in physiological parameters and thereby quantify the probability of adverse outcomes (e.g., severe hypoglycemia) [89].
Analyze Failures and Re-design: For each simulation run that resulted in a performance failure (e.g., glucose < 3.0 mmol/L for > 30 minutes), analyze the root cause. Use this insight to refine the control algorithm, for instance, by adding safety constraints or fault-detection modules.
2.2.3 Data Analysis and Interpretation Present the results in a table summarizing the failure rate for each edge case scenario.
Table 2: Example Summary of Edge Case Testing for a PID Controller
Edge Case Scenario Number of Simulations Simulations Resulting in Hypoglycemia ( < 3.9 mmol/L) Critical Failure Rate (%) CGM signal drop-out (2 hours) 500 45 9.0% Unannounced large meal (100g CHO) 500 12 2.4% Pump occlusion (4 hours) 500 480 96.0% Post-exercise with incorrect basal 500 150 30.0% This quantitative summary allows researchers to prioritize algorithm modifications to address the most critical failures first (e.g., implementing an occlusion detection algorithm).
In-silico validation is a foundational component of modern artificial pancreas research. The structured frameworks and detailed protocols provided here empower researchers and developers to build credibility in their simulations, thoroughly test and compare control algorithms, and proactively identify critical edge cases in a safe, efficient, and cost-effective virtual environment. By adhering to these methodologies, the path to regulatory approval and the delivery of safer, more effective closed-loop systems to patients is significantly accelerated.
The evaluation of Artificial Pancreas (AP) systems has transitioned from relying solely on hemoglobin A1c (HbA1c) to incorporating a suite of standardized, dynamic metrics derived from Continuous Glucose Monitoring (CGM). HbA1c provides a historical average of glucose levels but fails to capture glycemic variability, hypoglycemia, or postprandial hyperglycemia, all critical elements for assessing the safety and efficacy of closed-loop control systems [93] [94] [26]. International consensus reports have now established core CGM metrics, including Time in Range (TIR), Time Below Range (TBR), and Coefficient of Variation (CV), as essential outcomes for clinical trials and advanced AP research [93] [95] [26]. For researchers and scientists developing next-generation AP systems, understanding and applying these metrics is fundamental to optimizing algorithmic performance and demonstrating clinical value.
Core CGM Metrics and Their Clinical Significance
Definition of Standardized Metrics
International consensus has identified a core set of CGM metrics for standardized reporting [93] [95] [26]. These metrics provide a multi-dimensional view of glycemia that is essential for evaluating AP system performance.
- Time in Range (TIR): The percentage of time glucose is between 70–180 mg/dL (3.9–10.0 mmol/L). This is the primary metric for assessing glycemic efficacy [93] [26].
- Time Above Range (TAR): Divided into Level 1 (>180 mg/dL/10.0 mmol/L) and Level 2 (>250 mg/dL/13.9 mmol/L), this metric quantifies hyperglycemia [93].
- Time Below Range (TBR): Categorized as Level 1 (<70 mg/dL/3.9 mmol/L) and the more clinically significant Level 2 (<54 mg/dL/3.0 mmol/L), this is a key safety parameter for AP systems [93] [95].
- Mean Glucose: Provides an overall average glucose level.
- Glucose Management Indicator (GMI): An estimated HbA1c value calculated from the mean CGM glucose, useful for bridging historical and modern data [26].
- Glycemic Variability: Measured by the Coefficient of Variation (CV), calculated as (standard deviation / mean glucose) × 100%. A CV of ≤36% is a recommended target, indicating stable glucose control and lower hypoglycemia risk [93] [26].
Quantitative Targets and Their Implications
Consensus statements provide clear targets for these metrics, which can serve as benchmarks for AP system performance goals [93] [95] [26]. The following table summarizes these targets for the key demographic in AP research.
Table 1: Consensus-Derived Targets for Core CGM Metrics in Adults with Diabetes
| CGM Metric | Target for Adults (>25 years) with Type 1 or Type 2 Diabetes | Clinical and Research Significance |
|---|---|---|
| TIR (70–180 mg/dL) | >70% (>16 hours, 48 minutes) | Correlates with reduced risk of microvascular complications; primary efficacy endpoint [93] [95]. |
| TAR Level 1 (>180 mg/dL) | <25% (<6 hours) | Measures overall hyperglycemia [93]. |
| TAR Level 2 (>250 mg/dL) | <5% (<1 hour, 12 minutes) | Indicates significant hyperglycemia and risk for ketoacidosis [93]. |
| TBR Level 1 (<70 mg/dL) | <4% (<1 hour) | Indicator of mild hypoglycemia [93]. |
| TBR Level 2 (<54 mg/dL) | <1% (<15 minutes) | Critical safety metric; associated with severe physiological risks [93] [95]. |
| Coefficient of Variation (CV) | ≤36% | Predicts hypoglycemia risk; measures glycemic stability achieved by AP control algorithms [93] [26]. |
The relationship between TIR and HbA1c is well-established, with a TIR of 70% corresponding to an HbA1c of approximately 6.7–7.0% [93]. Perhaps most critically for validating these metrics in long-term studies, evidence shows that for every 10% increase in TIR, there is a associated 64% decrease in the risk of retinopathy progression and a 40% reduction in microalbuminuria risk, as derived from Diabetes Control and Complications Trial (DCCT) data [93].
Experimental Protocols for CGM Data Collection and Analysis
Standardized Data Acquisition Protocol
Robust evaluation of an AP system requires meticulous CGM data collection. The following protocol is distilled from international consensus recommendations [93] [95] [26].
- Recommended Wear Duration: A minimum of 14 days of CGM data is required to obtain a representative glycemic profile. While 10 days may suffice for estimating mean glucose and TIR, ≥14 days are needed for reliable assessment of hypoglycemia and glycemic variability [95].
- Data Sufficiency: The CGM device should be active for ≥70% of the time during the chosen wear period. This typically translates to at least 10 full days of data from a 14-day period [93] [26].
- Sensor Calibration: If using a user-calibrated CGM system, calibrations should be performed as per manufacturer instructions, ideally during periods of stable glucose.
- Data Export: Raw CGM data should be exported at the native measurement interval (e.g., every 5 minutes) for analysis. The standard output is the Ambulatory Glucose Profile (AGP) report [95].
Metrics Calculation and Analysis Workflow
Once data is acquired, a standardized analytical approach ensures consistency and comparability across research studies.
Diagram: CGM Data Analysis Workflow for AP Research
This workflow emphasizes not only the calculation of overall metrics but also the importance of stratified analysis. For AP research, comparing performance during nighttime (e.g., 00:00–06:00) vs. daytime and analyzing postprandial periods are critical for evaluating algorithmic efficacy under different physiological challenges [3].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for AP and CGM Studies
| Item | Function/Application in Research |
|---|---|
| iCGM (Integrated CGM) System | A regulatory category for CGM devices with proven accuracy and interoperability for use in automated insulin delivery systems. Essential for ensuring reliable data in AP trials [96]. |
| Ambulatory Glucose Profile (AGP) Report | The standardized visual report for summarizing CGM data. It provides a modal day graph and key metrics, serving as the primary tool for visual interpretation [93] [95]. |
| Reference Glucose Analyzer | A clinical-grade blood glucose analyzer (e.g., YSI, Beckman) used for method comparison studies to validate the accuracy of CGM sensors in a research setting [96]. |
| AP Control Algorithm Simulator | A software simulator of the human metabolic system (e.g., the FDA-accepted UVA/Padova T1D Simulator) used for in-silico testing and refinement of AP algorithms before human trials [1]. |
| Standardized Meal Kits | Meals with known and consistent macronutrient composition used during clinical trials to create a controlled challenge for evaluating postprandial AP performance [3]. |
The adoption of TIR, TBR, and CV as standard performance metrics represents a paradigm shift in AP research, moving beyond the static picture provided by HbA1c. These dynamic measures provide deep insight into the safety, efficacy, and stability of closed-loop control algorithms. By adhering to standardized protocols for data collection and analysis, researchers can ensure their findings are robust, comparable, and clinically relevant, ultimately accelerating the development of advanced AP systems that improve the lives of people with diabetes.
Automated insulin delivery (AID) systems, or artificial pancreases, represent the standard of care for type 1 diabetes (T1D) management. While single-hormone (insulin-only) systems have demonstrated significant benefits, challenges remain in preventing hypoglycemia, particularly during exercise. Dual-hormone (insulin and glucagon) systems have emerged as a promising alternative to mitigate this risk. This application note provides a comparative analysis of the efficacy of single-hormone and dual-hormone closed-loop systems, with a focus on hypoglycemia prevention and meal management. We summarize key clinical findings, present detailed experimental protocols for evaluating system performance, and outline the essential components of a research toolkit for closed-loop system development. The evidence indicates that dual-hormone systems significantly reduce time in hypoglycemia, especially around exercise, though single-hormone systems often provide sufficient overnight control. The choice between systems involves a trade-off between superior hypoglycemia protection and increased device complexity.
Efficacy Data and Comparative Analysis
Quantitative data from clinical studies and meta-analyses provide a clear comparison of the performance of single-hormone and dual-hormone AID systems across different conditions.
Table 1: Overall Glycemic Control with Single-Hormone vs. Dual-Hormone AID Systems
| Metric | Single-Hormone AID | Dual-Hormone AID | P-value | Context & Citation |
|---|---|---|---|---|
| Time in Range (TIR: 70-180 mg/dL) | 74.3% | 72.0% | P = 0.44 | 4-day outpatient study [97] |
| Time in Hypoglycemia (<70 mg/dL) | 2.8% | 1.3% | P < 0.001 | 4-day outpatient study [97] |
| Time in Hypoglycemia (<70 mg/dL) | 11.0% | 0% | P = 0.0001 | During & after exercise (pooled analysis) [98] |
| Time in Hypoglycemia (<54 mg/dL) | N/A | N/A | N/S | Dual-hormone systems can virtually eliminate severe hypoglycemia [34] |
| Improvement in TIR vs. Control | +10.87% | +19.64% | N/A | Meta-analysis result vs. standard therapy [99] |
Table 2: System Performance in Specific Scenarios
| Scenario | Single-Hormone Performance | Dual-Hormone Performance | Conclusion |
|---|---|---|---|
| Exercise | Increased hypoglycemia risk; requires proactive suspension/announcement [98] | Superior hypoglycemia reduction; glucagon counters falling glucose [97] [98] | Dual-hormone provides significant benefit [100] |
| Overnight Control | Sufficient for maintaining euglycemia [100] | Similar efficacy to single-hormone [100] | Both systems perform well overnight |
| Prandial Period | Manages meals effectively as a hybrid system (requires meal announcement) [3] | Manages meals effectively as a hybrid system (requires meal announcement) [3] | Both systems require meal announcements; fully closed-loop is an area of research [34] |
Detailed Experimental Protocols
To ensure reproducible testing of single and dual-hormone AID systems, the following protocols, derived from clinical studies, are provided.
Protocol for Outpatient Efficacy Comparison Over Multiple Days
This protocol is designed to compare the real-world efficacy of single and dual-hormone systems.
- Objective: To determine whether a dual-hormone closed-loop system outperforms a single-hormone system in reducing exercise-related hypoglycemia and improving overall glycemic control during a 4-day outpatient study [97].
- Study Design: Randomized, crossover trial with four arms: dual-hormone, single-hormone, predictive low glucose suspend, and current care.
- Participants:
- Adults (age 21-45) with T1D for ≥1 year.
- Insulin pump users, able to perform 45 minutes of exercise.
- Intervention:
- Systems: Single-hormone and dual-hormone systems use a closed-loop algorithm (e.g., modified fading memory proportional-derivative) on a handheld device. The system communicates with a continuous glucose monitor (CGM) and insulin pump(s). For the dual-hormone system, a glucagon pump is added [97].
- Exercise Sessions: Each 4-day arm includes three 45-minute moderate-intensity aerobic exercise sessions (e.g., treadmill at 60% VOâ‚‚max) [97].
- Exercise Detection: Both systems incorporate a wearable sensor (heart rate monitor and accelerometer) to detect exercise. Upon detection and user confirmation, the algorithm triggers a predefined response: insulin suspension for 30 minutes, followed by a 50% basal rate reduction for 60 minutes. The dual-hormone system additionally increases the glucagon target from 95 mg/dL to 120 mg/dL and doubles the maximum allowed glucagon dose [97].
- Primary Outcomes:
- Percentage of CGM time in hypoglycemia (<70 mg/dL).
- Percentage of CGM time in target range (70–180 mg/dL).
- Assessed across the entire study and from the start of exercise until the next meal [97].
- Statistical Analysis: A sample size of ~20 participants provides >80% power to detect significant differences in time in hypoglycemia, based on prior studies [97].
Protocol for In-Clinic Exercise Challenge
This protocol is designed to directly compare the two systems during a controlled exercise challenge.
- Objective: To assess the efficacy of single-hormone vs. dual-hormone AID systems in preventing hypoglycemia during continuous and interval exercise [98].
- Study Design: Open-label, randomized, crossover study.
- Participants: Adults with T1D on insulin pump therapy.
- Intervention:
- After a standardized lunch, AID control is initiated.
- Exercise is announced to the algorithm 20 minutes prior to commencement.
- Exercise Types:
- Continuous: 60 minutes at 60% V̇O₂peak.
- Interval: 40 minutes of alternating 2-minute periods at 85% and 50% V̇O₂peak, with 10-minute warm-up and cool-down at 45% V̇O₂peak. Sessions are matched for energy expenditure [98].
- Key Measures:
- Plasma glucose <3.3 mmol/L (59 mg/dL) with symptoms or <3.0 mmol/L (54 mg/dL) without symptoms.
- Percentage of CGM time <4.0 mmol/L (72 mg/dL).
- Total glucagon dose administered.
- Analysis: Comparison of hypoglycemia events and time below range between the two systems.
The workflow for a typical AID system evaluation, incorporating the above protocols, is visualized below.
Figure 1: Experimental Workflow for AID System Comparison. This diagram outlines the key stages in a clinical trial comparing single and dual-hormone systems, from participant screening to final analysis.
System Architectures and Control Logic
The fundamental difference between single and dual-hormone systems lies in their control logic and response to declining glucose levels. The following diagram illustrates the core algorithmic pathways.
Figure 2: Control Logic in Single vs. Dual-Hormone AID Systems. The key difference is the reactive pathway: single-hormone systems can only suspend insulin, while dual-hormone systems can actively administer glucagon to raise blood glucose.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for AID System Research
| Component | Example Products/Tools | Function in Research | Key Considerations |
|---|---|---|---|
| Continuous Glucose Monitor (CGM) | Dexcom G-series, Medtronic Guardian | Provides real-time interstitial glucose measurements to the control algorithm. | Accuracy, delay between blood and interstitial glucose, calibration needs [97] [98]. |
| Insulin Pump | Tandem t:slim, Medtronic MiniMed | Delivers subcutaneous rapid-acting insulin as directed by the algorithm. | Precision of micro-boluses, reliability, communication interface [97] [3]. |
| Glucagon & Pump | Reconstituted GlucaGen, MiniMed pump (research use) | Delerves subcutaneous glucagon micro-boluses in dual-hormone systems. | Glucagon stability in solution (requires reconstitution every 24h), pump compatibility [97] [98]. |
| Control Algorithm | MPC, PID, Deep Reinforcement Learning (DRL) | The "brain" of the AP; computes required insulin/glucagon doses based on CGM data and other inputs. | Ability to handle delays, personalization, safety constraints (e.g., to prevent hypoglycemia) [49] [34]. |
| Physical Activity Monitor | ZephyrLife BioPatch (heart rate & accelerometer) | Provides input for exercise detection algorithms to proactively adjust hormone delivery. | Used to estimate metabolic equivalents (METs) for automated exercise detection [97]. |
| Simulation Platform | UVa/Padova T1D Simulator, Simglucose | Validates and tests control algorithms in silico before human trials; accepted by regulatory bodies. | Population variability, meal and exercise scenarios, model fidelity [1] [34]. |
| Data Management | Artificial Pancreas System (APS) | A universal research platform (e.g., from UCSB) that enables communication between various devices and algorithms. | Standardizes device interfacing, data logging, and remote monitoring for clinical trials [1]. |
The evidence demonstrates that both single-hormone and dual-hormone AID systems represent significant advancements in T1D management. The choice between them involves a critical trade-off: dual-hormone systems offer superior protection against hypoglycemia, particularly during challenging perturbations like exercise, at the cost of increased device complexity and the need for a stable glucagon formulation [97] [100] [98]. Single-hormone systems provide robust glycemic control for many scenarios with a simpler architecture.
Future research directions include the development of stable liquid glucagon formulations to simplify dual-hormone systems, the implementation of fully closed-loop algorithms that do not require meal announcements using advanced techniques like deep reinforcement learning [34], and long-term studies to assess the durability of glycemic benefits and cost-effectiveness of dual-hormone therapy.
Automated insulin delivery (AID) systems, also known as artificial pancreas or closed-loop systems, represent a transformative advancement in diabetes management by integrating continuous glucose monitoring (CGM), insulin pumps, and control algorithms to automate insulin delivery [1] [101]. While randomized controlled trials provide evidence of efficacy, real-world evidence (RWE) offers crucial insights into how these systems perform in everyday life across diverse patient populations and clinical settings. This application note synthesizes real-world data from thousands of users to analyze system performance, long-term adherence, and quality-of-life improvements, providing researchers and clinicians with structured protocols for evaluating AID technologies in real-world contexts.
Real-World Performance Data Synthesis
Real-world evidence studies complement findings from controlled trials by demonstrating how AID systems perform under routine clinical conditions. The synthesized data below encompasses findings from multiple real-world studies involving thousands of users with both type 1 and type 2 diabetes [101] [102] [103].
Table 1: Composite Real-World Glycemic Outcomes from AID System Use
| Outcome Metric | Baseline Mean | Post-AID Implementation | Mean Change | Clinical Significance |
|---|---|---|---|---|
| Time in Range (TIR) | 49.5% | 69.8% | +20.3% | Achieved >70% goal |
| HbA1c | 7.9% | 7.1% | -0.8% | Below 7% target |
| Time Above Range (TAR) | 41.2% | 25.5% | -15.7% | Significant reduction |
| Time Below Range (TBR) | 3.8% | 3.5% | -0.3% | Minimal change |
| Coefficient of Variation (CV) | 38.5% | 35.2% | -3.3% | Improved stability |
Comparative Long-Term Performance of Commercial AID Systems
A one-year retrospective study of 174 adults with type 1 diabetes provided direct comparisons between four commercially available AID systems, demonstrating significant variation in their ability to optimize different glycemic parameters [102].
Table 2: One-Year Comparative Performance of AID Systems in Type 1 Diabetes
| AID System | TIR Improvement | HbA1c Reduction | CV Improvement | Achievement of International Targets* |
|---|---|---|---|---|
| MiniMed 780G | +++ | +++ | + | >70% |
| Tandem-Control-IQ | ++ | + | - | >60% |
| Diabeloop (DBLG) | ++ | ++ | ++ | >60% |
| Cam-APS | ++ | ++ | + | >60% |
International targets defined as TIR >70%, TAR <25%, TBR <4% [102]
Experimental Protocols for Real-World Evidence Generation
Protocol 1: Retrospective AID Performance Analysis
Objective: To evaluate the real-world effectiveness of advanced hybrid closed-loop (a-HCL) systems compared to previous diabetes technologies [103].
Methodology:
- Study Design: Retrospective cohort study
- Population: Type 1 diabetes patients transitioning from predictive low glucose suspend (PLGS) or standard hybrid closed-loop (s-HCL) to a-HCL systems
- Data Collection Period: Pre-implementation (3 months) and post-implementation (3-12 months)
- Key Metrics: HbA1c, time in range (TIR), time above range (TAR), time below range (TBR), sensor glucose (SG), coefficient of variation (CV)
- Statistical Analysis: Paired t-tests for continuous variables, multivariate regression to identify predictors of response
Inclusion Criteria:
- Diagnosis of type 1 diabetes
- Previous use of PLGS or s-HCL for ≥3 months
- Complete dataset with ≥70% CGM usage
- Age ≥18 years
Implementation Workflow:
Protocol 2: Longitudinal Adherence and Quality of Life Assessment
Objective: To evaluate long-term adherence patterns and quality of life improvements associated with AID system use over 12 months [102].
Methodology:
- Study Design: Prospective observational cohort with repeated measures
- Population: Type 1 diabetes patients initiating AID therapy
- Timepoints: Baseline, 3 months, 6 months, 12 months
- Primary Endpoints: Device utilization metrics, glycemic outcomes, diabetes distress scale scores
- Secondary Endpoints: Algorithm-specific performance, quality of life measures, adverse events
Data Collection Methods:
- Automated Data Extraction: CGM metrics downloaded from manufacturer cloud platforms (Libreview, Clarity, Carelink)
- Patient-Reported Outcomes: Validated questionnaires on diabetes distress and quality of life
- Clinical Data: HbA1c, hypoglycemia events, hospitalizations
- Adherence Metrics: Percentage of time in automated mode, sensor utilization, user-initiated boluses
Visualization: Real-World Evidence Generation Framework
The following diagram illustrates the integrated framework for generating and analyzing real-world evidence for AID systems, highlighting the relationship between data sources, methodologies, and outcomes.
Research Reagent Solutions: AID System Components
The development and evaluation of artificial pancreas systems rely on specific technological components and assessment tools. The following table details essential research solutions for conducting real-world evidence studies.
Table 3: Essential Research Components for AID System Evaluation
| Component Category | Specific Examples | Research Function | Implementation Considerations |
|---|---|---|---|
| Control Algorithms | Model Predictive Control (MPC), Proportional-Integral-Derivative (PID), Fuzzy Logic [1] | Determines insulin dosing based on CGM values and trends | Algorithm choice affects postprandial control and exercise response |
| Continuous Glucose Monitoring | Dexcom G7, Guardian Sensor 4 [104] [102] | Provides real-time glucose measurements for algorithm decisions | MARD (Mean Absolute Relative Difference) affects system accuracy and safety |
| Insulin Delivery Mechanisms | Tubed pumps (T:slim X2), Patch pumps (OmniPod 5) [1] [104] | Executes algorithm-determined insulin delivery | Formulation speed (rapid-acting vs. ultra-rapid) impacts postprandial control |
| Data Integration Platforms | Libreview, Clarity, Carelink, Yourloops [102] | Aggregates device data for retrospective analysis | Enables large-scale real-world evidence generation across multiple sites |
| Adjunctive Therapies | GLP-1 receptor agonists, SGLT2 inhibitors [101] | Modifies insulin requirements and glycemic variability | Must be accounted for in real-world study analyses |
Real-world evidence from thousands of users demonstrates that AID systems significantly improve glycemic outcomes and maintain long-term adherence across diverse patient populations with both type 1 and type 2 diabetes [101] [102] [103]. The structured protocols and synthesized data presented herein provide researchers with validated methodologies for evaluating system performance in clinical practice. Future directions should focus on expanding accessibility, addressing inter-population variability, and incorporating artificial intelligence to further reduce user burden and optimize glycemic outcomes across the spectrum of insulin-requiring diabetes [105] [106].
Conclusion
The design of closed-loop control systems for the artificial pancreas has matured from a disputed concept to the gold-standard treatment for type 1 diabetes, fundamentally transforming patient care. Key advances in control algorithms—from classical MPC to adaptive and fully autonomous AI-driven systems—have steadily improved glycemic outcomes and reduced user burden. The integration of feedforward control for meals and exercise, alongside the development of dual-hormone systems, addresses persistent challenges in postprandial control and hypoglycemia risk. Looking forward, the field is poised for a new revolution focused on full automation, eliminating the need for user input like meal announcements. Future research must prioritize the development of fault-tolerant and self-adaptive systems, leverage digital twin technology for ultra-personalized therapy, and create scalable solutions accessible to broader populations, including those with type 2 diabetes. The convergence of advanced control theory, artificial intelligence, and cyber-physical-human systems will continue to drive innovation, paving the way for more intelligent, safe, and adaptive artificial pancreas devices.
References
- 1. Artificial Pancreas: The First 20 Years [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213539/]
- 2. The 'Designer' Artificial Pancreas: How Does Current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12296855/]
- 3. Realizing a Closed-Loop (Artificial Pancreas) System for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6821212/]
- 4. Automated Insulin Delivery Systems Archives [https://www.breakthrought1d.org/?jdrf_topic=automated-insulin-delivery-systems]
- 5. The Artificial Pancreas Device System [https://www.fda.gov/medical-devices/consumer-products/artificial-pancreas-device-system]
- 6. FDA Clears New Insulin Pump and Algorithm-Based ... [https://www.fda.gov/news-events/press-announcements/fda-clears-new-insulin-pump-and-algorithm-based-software-support-enhanced-automatic-insulin-delivery]
- 7. Advances in artificial pancreas for treatment of diabetes [https://www.sciencedirect.com/science/article/abs/pii/S1367578825000471]
- 8. Closed-Loop Artificial Pancreas Systems - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3994938/]
- 9. Optimizing the Design of an Artificial Pancreas to Improve ... [https://arxiv.org/html/2402.07949v2]
- 10. Continuous Glucose Monitoring - NIDDK [https://www.niddk.nih.gov/health-information/diabetes/overview/managing-diabetes/continuous-glucose-monitoring]
- 11. Continuous Glucose Monitoring (CGM): What It Is [https://my.clevelandclinic.org/health/articles/continuous-glucose-monitoring-cgm]
- 12. CLOSING THE LOOP: THE LATEST ON ARTIFICIAL ... [https://ondrugdelivery.com/closing-the-loop-the-latest-on-artificial-pancreas-systems/]
- 13. Types of Insulin Pumps - Cleveland Clinic [https://my.clevelandclinic.org/health/articles/insulin-pumps]
- 14. Insulin Pump - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK555961/]
- 15. What are closed loop systems? [https://www.diabetes.org.uk/about-diabetes/looking-after-diabetes/technology/closed-loop-systems]
- 16. Algorithms for a Closed-Loop Artificial Pancreas: The Case ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3876341/]
- 17. Closed-Loop Insulin Delivery Systems: Past, Present, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9207329/]
- 18. A novel pulse-modulated closed-loop artificial pancreas ... [https://www.nature.com/articles/s41598-024-77800-0]
- 19. Closing in on the Mechanisms of Pulsatile Insulin Secretion [https://pmc.ncbi.nlm.nih.gov/articles/PMC5828455/]
- 20. Pharmacokinetics and pharmacodynamics of insulin analogs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3258012/]
- 21. Glucose kinetics: an update and novel insights into its ... [https://pubmed.ncbi.nlm.nih.gov/28463898/]
- 22. Insulin Delivery Route for the Artificial Pancreas [https://pmc.ncbi.nlm.nih.gov/articles/PMC2769765/]
- 23. Pharmacodynamics of NN2211, a novel long acting GLP-1 ... [https://www.sciencedirect.com/science/article/abs/pii/S0928098703000733]
- 24. Artificial pancreas under stable pulsatile MPC [https://www.sciencedirect.com/science/article/abs/pii/S0959152420302456]
- 25. Predictive Hyperglycemia and Hypoglycemia Minimization [https://pmc.ncbi.nlm.nih.gov/articles/PMC5319476/]
- 26. Core Glycemic Metrics Explained. TIR, TBR, TAR, GMI, CV, ... [https://www.adces.org/education/danatech/glucose-monitoring/continuous-glucose-monitors-(cgm)/glycemic-metrics--an-overview]
- 27. Time in Range: How to Measure It, How to Report It, and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7755049/]
- 28. Time in Range (TIR) for Diabetes: What It Is & Target [https://my.clevelandclinic.org/health/articles/time-in-range-diabetes]
- 29. CGM & Time in Range [https://diabetes.org/about-diabetes/devices-technology/cgm-time-in-range]
- 30. The Advanced Diabetes Technologies for Reduction of ... [https://www.mdpi.com/2077-0383/12/3/781]
- 31. Time in tight range: A key metric for optimal glucose control ... [https://pubmed.ncbi.nlm.nih.gov/39529452/]
- 32. Developing the UVA/Padova Type 1 Diabetes Simulator [https://pmc.ncbi.nlm.nih.gov/articles/PMC10658679/]
- 33. Metabolic Models, in Silico Trials, and Algorithms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213549/]
- 34. A safe-enhanced fully closed-loop artificial pancreas controller ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0317662]
- 35. MPC vs PID - A Comprehensive Control Method Comparison - Petrotech | Control Systems Solutions [https://petrotechinc.com/mpc-vs-pid-a-comprehensive-control-method-comparison/]
- 36. PID Control System Explained: Principles, ICs, and ... [https://www.ersaelectronics.com/blog/pid-controller-ic-guide?srsltid=AfmBOopi3PqQVL5AJEKDvyRpYm9AhANLjJQw-N5aVAGya_0pCqHj7W0j]
- 37. A Comprehensive Guide To The Implementation Of A Pid ... [https://www.sinny.com/a-comprehensive-guide-to-the-implementation-of-a-pid-controller.html]
- 38. Industrial PID Controller in the Real World: 5 Uses You'll ... [https://www.linkedin.com/pulse/industrial-pid-controller-real-world-5-uses-youll-actually-gvpgf/]
- 39. Model predictive control - Wikipedia [https://en.wikipedia.org/wiki/Model_predictive_control]
- 40. Carnot Innovations - Model Predictive Control vs. Proportional, Integral, Derivative Control [https://www.carnot-innovations.com/model-predictive-control-vs-proportional-integral-derivative-control]
- 41. Model Predictive Control for Smart Buildings: Applications ... [https://www.mdpi.com/2075-5309/15/18/3298]
- 42. From theory to practice: A critical review of model predictive ... [https://www.sciencedirect.com/science/article/abs/pii/S0306261925008219]
- 43. PID Controller Applications in Industry [https://www.realpars.com/blog/pid-controller-applications]
- 44. Hierarchical, Occupancy-Responsive Model Predictive ... [https://www.energy.gov/eere/buildings/articles/hierarchical-occupancy-responsive-model-predictive-control-mpc-room]
- 45. Fully Closed Loop: Automated Insulin Delivery Takes the ... [https://diatribe.org/diabetes-technology/fully-closed-loop-automated-insulin-delivery-takes-next-step]
- 46. Deep Reinforcement Learning for Automated Insulin ... [https://www.mdpi.com/2673-2688/6/5/87]
- 47. Deep reinforcement learning for closed-loop blood glucose ... [https://www.sciencedirect.com/science/article/pii/S2405896323000630]
- 48. How to Understand the FDA's 2025 Draft Guidance for AI ... [https://www.vergentproducts.com/draft-guidance-for-ai-enabled-medical-devices/]
- 49. Event-triggered smart dual hormone artificial pancreas for ... [https://www.nature.com/articles/s41598-025-18085-9]
- 50. Treatment of severe diabetic hypoglycemia with glucagon [https://pmc.ncbi.nlm.nih.gov/articles/PMC3180523/]
- 51. Low-Dose Glucagon to Prevent and Treat Exercise ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12368384/]
- 52. Event-triggered smart dual hormone artificial pancreas for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12402495/]
- 53. Implantable Device Shows Promise for Preventing ... [https://www.medscape.com/viewarticle/implantable-device-shows-promise-preventing-hypoglycemia-2025a1000l7n]
- 54. Glucagon (injection route) - Side effects & dosage [https://www.mayoclinic.org/drugs-supplements/glucagon-injection-route/description/drg-20064089]
- 55. Glucagon changes substrate preference in gluconeogenesis [https://www.sciencedirect.com/science/article/pii/S0021925822011516]
- 56. Event-Triggered Model Predictive Control For Embedded ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5839516/]
- 57. Intermittent closed-loop blood glucose control for people ... [https://www.sciencedirect.com/science/article/pii/S016926072300233X]
- 58. The impact of using a closedâ€loop system on food choices ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6510609/]
- 59. Closed-Loop Insulin Delivery Using a Subcutaneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2797956/]
- 60. Sensor-based glucose and insulin control by deep ... [https://www.sciencedirect.com/science/article/abs/pii/S0952197625016185]
- 61. Advances in Subcutaneous Glucose Sensing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5568179/]
- 62. Artificial Pancreas - NIDDK [https://www.niddk.nih.gov/health-information/diabetes/overview/managing-diabetes/artificial-pancreas]
- 63. The Artificial Pancreas Device System [https://www.fda.gov/medical-devices/artificial-pancreas-device-system/what-pancreas-what-artificial-pancreas-device-system]
- 64. A Review of Safety and Design Requirements ... [https://pure.amsterdamumc.nl/en/publications/a-review-of-safety-and-design-requirements-of-the-artificial-panc/]
- 65. A safe-enhanced fully closed-loop artificial pancreas ... [https://pubmed.ncbi.nlm.nih.gov/39869550/]
- 66. Treatment and prevention of severe hypoglycaemia in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7079012/]
- 67. Circadian Variability of Insulin : Physiological Input for In... Sensitivity [https://pmc.ncbi.nlm.nih.gov/articles/PMC4290795/]
- 68. Control-Relevant Adaptive Personalized Modeling From ... [https://pubmed.ncbi.nlm.nih.gov/36846361/]
- 69. Detection of Meals and Physical Activity Events From Free- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10658701/]
- 70. Meal and Physical Activity Detection from Free-Living Data ... [https://www.mdpi.com/2673-7426/2/2/19]
- 71. Enabling fully automated insulin delivery through meal ... [https://www.nature.com/articles/s41746-023-00783-1]
- 72. Technology Overview [https://apps.ohsu.edu/research/tech-portal/technology/view/7170676]
- 73. Closed-loop control with unannounced exercise for adults ... [https://www.sciencedirect.com/science/article/abs/pii/S0959152419303610]
- 74. A Closed-Loop Artificial Pancreas Using Model Predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2769914/]
- 75. Beta Bionics aims to reduce 'cognitive burden' associated ... [https://www.drugdeliverybusiness.com/beta-bionics-diabetes-bionic-pancreas-insulin/]
- 76. Youth and Parent Preferences for an Ideal AP System [https://pmc.ncbi.nlm.nih.gov/articles/PMC8530854/]
- 77. Quantitative Evaluation of Visual Aesthetics of Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7085848/]
- 78. A quantitative model of the human–machine interaction ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482506002307]
- 79. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 80. Elements must meet minimum color contrast ratio thresholds [https://dequeuniversity.com/rules/axe/4.8/color-contrast]
- 81. A Meta-Analysis of Randomized Trial Outcomes for the t:slim ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10171957/]
- 82. Tandem Diabetes Care Announces NEJM Publication of ... [https://investor.tandemdiabetes.com/news-releases/news-release-details/tandem-diabetes-care-announces-nejm-publication-positive-pivotal]
- 83. Safety and Glycemic Outcomes During the MiniMed ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/34694909/]
- 84. U.S. pivotal trial of the MiniMed 780G system [https://news.medtronic.com/2020-06-12-Medtronic-Presents-U-S-Pivotal-Trial-Data-for-MiniMed-TM-780G-Advanced-Hybrid-Closed-Loop-System-with-Automated-Correction-Bolus-Feature]
- 85. Study Shows Omnipod® 5 Improved Glycemic Measures ... [https://www.omnipod.com/hcp/blog/clinical-studies/brown-21-summary]
- 86. Insulet's SECURE-T2D Pivotal Trial Results Demonstrate ... [https://investors.insulet.com/news/news-details/2024/Insulets-SECURE-T2D-Pivotal-Trial-Results-Demonstrate-Omnipod-5-Improves-Clinical-Outcomes-and-Quality-of-Life-in-Type-2-Diabetes/default.aspx]
- 87. In silico trials: Verification, validation and uncertainty ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7883933/]
- 88. In silico design and validation of a time-varying PID ... [https://pubmed.ncbi.nlm.nih.gov/37229215/]
- 89. Independent Validation of an In Silico Tool for a Pilot-Scale ... [https://www.mdpi.com/2227-9717/9/4/640]
- 90. Analyzing ADAS Edge Case Failures Using Virtual Validation [https://xitadel.com/webinar/analyzing-adas-edge-case-failures-using-virtual-validation/]
- 91. Our Approach [https://insilicotrials.com/our-approach/]
- 92. Tidy simulation Designing robust, reproducible, and ... [https://arxiv.org/html/2509.11741v1]
- 93. Clinical Application of Time in Range and Other Metrics [https://pmc.ncbi.nlm.nih.gov/articles/PMC8178724/]
- 94. Metrics Beyond Hemoglobin A1C in Diabetes Management [https://pmc.ncbi.nlm.nih.gov/articles/PMC5444503/]
- 95. Beyond A1C—Standardization of Continuous Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8178725/]
- 96. Consensus statement on standardizing CGM evaluation ... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-025-01851-0]
- 97. and Dual-Hormone Closed-Loop Systems That Adapt to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6014543/]
- 98. Efficacy of single-hormone and dual-hormone artificial ... [https://link.springer.com/article/10.1007/s00125-016-4107-0]
- 99. Efficacy and Safety of Automated Insulin Delivery Systems ... [https://www.e-dmj.org/journal/view.php?number=2893]
- 100. Dual-hormone artificial pancreas: benefits and limitations ... [https://pubmed.ncbi.nlm.nih.gov/29337384/]
- 101. Effectiveness and safety of automated insulin delivery in type ... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-025-02014-x]
- 102. One-year evaluation of automated insulin delivery systems ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1596188/full]
- 103. Real-world evidence supporting the use of advanced ... [https://www.sciencedirect.com/science/article/pii/S016882272500049X]
- 104. Diabetes Technology Updates: Revolutionizing Care in 2025 [https://www.byramhealthcare.com/blogs/diabetes-technology-updates-revolutionizing-care-in-2025]
- 105. Research Gaps, Challenges, and Opportunities in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213545/]
- 106. The Future of Automated Insulin Delivery Systems [https://www.sciencedirect.com/science/article/abs/pii/S1530891X25009243]