Bridging the Loop: Overcoming Coordination Failures Between Glucose Sensing and Insulin Delivery in Diabetes Management
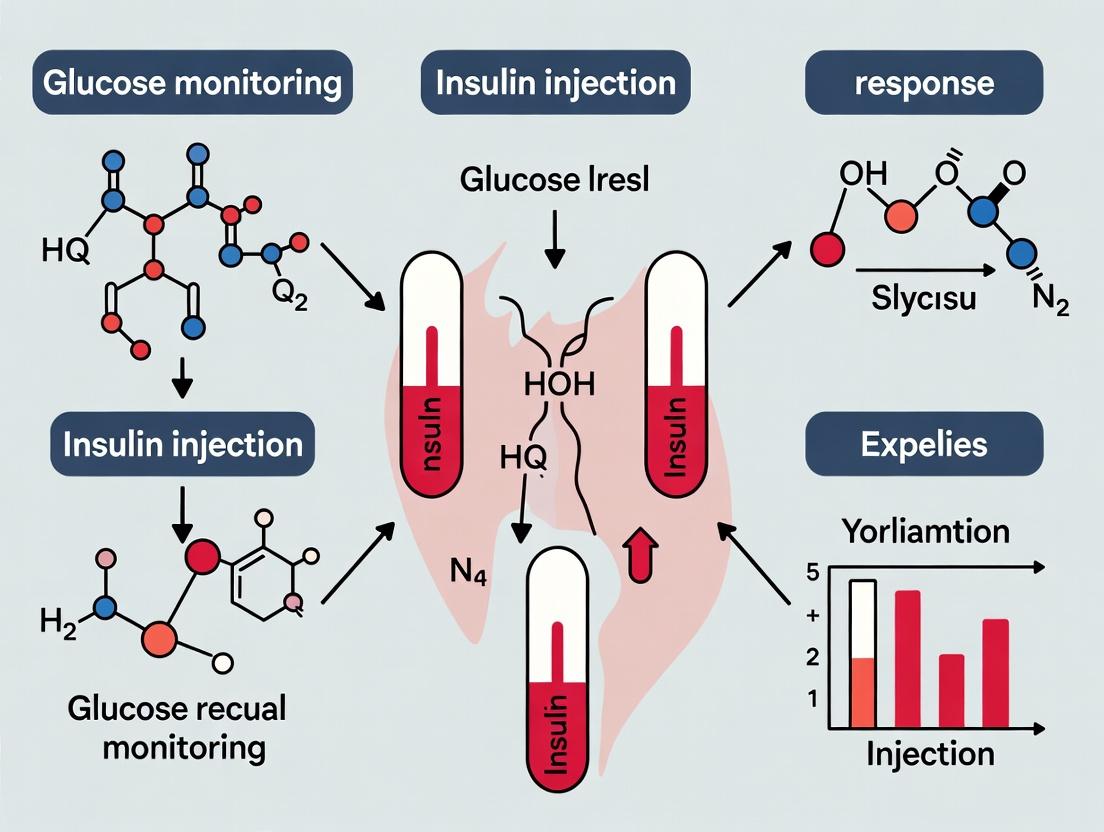
This article examines the critical challenge of poor coordination between glucose monitoring and insulin injection, a persistent barrier to optimal glycemic control.
Bridging the Loop: Overcoming Coordination Failures Between Glucose Sensing and Insulin Delivery in Diabetes Management
Abstract
This article examines the critical challenge of poor coordination between glucose monitoring and insulin injection, a persistent barrier to optimal glycemic control. We explore the foundational causes—including technological, physiological, and behavioral disconnects—and survey current methodologies from hybrid closed-loop systems to smart insulin pens and decision support algorithms. We provide a troubleshooting framework for common coordination failures and evaluate the comparative efficacy and validation standards of emerging integrated solutions. Aimed at researchers and drug development professionals, this review synthesizes current knowledge to guide the development of next-generation, truly synergistic diabetes management technologies.
Understanding the Disconnect: The Root Causes of Poor Coordination in Diabetes Management
Technical Support Center
Frequently Asked Questions & Troubleshooting Guides
Q1: In our in vitro closed-loop simulation, we observe significant overshoot in insulin response despite accurate glucose readings. What could be the cause? A: This is a classic manifestation of the physiological coordination gap. The issue likely stems from unaccounted-for sensor lag times combined with rapid-acting insulin pharmacokinetics/pharmacodynamics mismatches in your model.
- Troubleshooting Step 1: Verify and calibrate your glucose sensor delay parameters. The lag is not just technical but also physiological (interstitial fluid vs. plasma glucose).
- Step 2: Review your insulin action profile parameters (e.g., time-to-peak, duration). The table below summarizes key lag times to check in your simulation:
- Solution: Implement a predictive model (e.g., Kalman filter) to project glucose trends from incoming data, effectively "shifting" the signal forward to align with insulin action onset.
Quantitative Lag Time Data
| Lag Component | Typical Duration (Minutes) | Description & Impact |
|---|---|---|
| Sensor System Lag | 5-15 | Delay from blood glucose change to interstitial fluid reading and sensor processing. |
| Insulin Onset Lag | 10-20 | Time for subcutaneously injected insulin to begin appearing in the bloodstream. |
| Time-to-Peak Action | 60-120 | Duration to reach maximum glucose-lowering effect. Major source of mis-timing. |
| Manual Process Delay | 5-30+ | Human decision-making, preparation, and administration time in non-automated systems. |
Q2: Our manual cell culture experiment to correlate insulin receptor phosphorylation with glucose uptake yields high variability. How can we improve coordination? A: Variability often arises from manual timing misalignment between glucose stimulation and insulin injection steps. This manual process gap desynchronizes the signaling cascade.
- Troubleshooting: Audit your lab protocol. Are researchers consistently adhering to precise "time-zero" for both glucose and insulin additions across all trials?
- Solution: Implement the synchronized automated protocol below to eliminate human timing error.
Experimental Protocol: Synchronized Glucose-Insulin Stimulation for Cell Signaling Objective: To precisely coordinate glucose exposure and insulin stimulation for time-resolved analysis of downstream signaling (e.g., AKT phosphorylation). Key Reagents: See "Scientist's Toolkit" below. Methodology:
- Cell Preparation: Seed and serum-starve HEK293 or adipocyte cells in 12-well plates for 16-24 hours.
- System Setup: Utilize a multi-channel pipette or, ideally, an automated liquid handler pre-loaded with reagents in temperature-controlled reservoirs.
- Synchronized Stimulation: a. For time-course experiments, initiate all wells simultaneously using an automated handler. b. Time Zero: Add pre-warmed high-glucose (25mM) medium to all wells. c. Precise Interval: At exactly t=2 minutes, add insulin (100 nM final concentration) to designated wells using a second automated channel. Control wells receive buffer.
- Termination: At defined timepoints (e.g., 0, 5, 15, 30 min), rapidly aspirate medium and lyse cells directly in 1X Laemmli buffer to instantly halt signaling.
- Analysis: Proceed to Western Blotting for p-AKT (Ser473), total AKT, and other targets.
Q3: When analyzing data from continuous glucose monitors (CGM) and insulin pumps, how do we visually identify coordination gaps? A: Gaps are identified by plotting both data streams on a synchronized timeline and calculating the time differential between a glucose threshold event and the subsequent insulin dose.
Visualization: Identifying the Coordination Gap in Time-Series Data
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Function in Coordination Research |
|---|---|
| Automated Liquid Handler | Eliminates manual timing errors in in vitro stimulation protocols; ensures precise, reproducible reagent addition. |
| Microfluidic Cell Culture Chips | Enables precise temporal control of glucose and insulin perfusion for studying real-time cellular responses. |
| Rapid-Acting Insulin Analogs (Lispro, Aspart) | Research-grade analogs with faster onset/offset used to minimize the inherent pharmacological lag time. |
| Phospho-Specific Antibodies (p-AKT, p-IRS1) | Essential for measuring the timing and magnitude of early insulin signaling events post-stimulation. |
| Closed-Loop Simulation Software | Digital twin environment (e.g., UVa/Padova Simulator) to model and quantify the impact of various lag times in silico. |
| Time-Lapse Fluorescence Microscopy | For live-cell imaging of GLUT4 translocation, directly visualizing the endpoint of coordinated signaling. |
Technical Support Center: Troubleshooting Coordination in Glucose-Insulin Research
This support center provides guidance for common experimental challenges in research aimed at aligning glucose sensing with insulin action. The goal is to mitigate the risks of glycemic variability and hypoglycemia through improved mechanistic and therapeutic coordination.
Troubleshooting Guides & FAQs
FAQ 1: In our closed-loop system simulation, we observe persistent postprandial hyperglycemia followed by delayed hypoglycemia. What are the primary investigational paths?
- Answer: This pattern indicates a coordination failure, often between insulin pharmacodynamics (PD) and continuous glucose monitor (CGM) sensor lag. Investigate:
- Sensor Delay Characterization: Quantify the physiological and algorithmic latency of your CGM model. Compare interstitial vs. plasma glucose under dynamic conditions.
- Insulin Kinetics/PD Mismatch: Analyze if the insulin profile (e.g., rapid-acting analog) aligns with the meal absorption profile. A delayed peak action will exacerbate hyperglycemia, while a prolonged tail increases hypoglycemia risk, especially with delayed CGM feedback.
- Control Algorithm Aggressiveness: An overly aggressive controller will overcorrect for the hyperglycemic spike using data already delayed, leading to the subsequent low.
- Experimental Protocol: Quantifying System Latencies
- Objective: To measure the total lag between a glycemic stimulus and the insulin response command in a simulated closed-loop.
- Method:
- Use a glucose-insulin simulator (e.g., FDA-accepted UVA/Padova Simulator, Cambridge Simulator).
- Introduce a standardized meal challenge (e.g., 50g carbohydrates).
- Record timestamp of meal (T0), timestamp of CGM reading crossing threshold (T1), and timestamp of algorithm's insulin bolus command (T2).
- Sensor Lag = T1 - T0 (accounts for gastric emptying, absorption, sensor equilibration).
- Algorithmic/Response Lag = T2 - T1.
- Total System Lag = T2 - T0.
- Repeat with varying meal sizes, insulin types, and noise added to CGM signal.
FAQ 2: When evaluating a novel ultra-rapid insulin, how do we design an experiment to isolate its effect on reducing hypoglycemia risk from the effect of CGM accuracy?
- Answer: This requires a factorial study design that decouples the insulin variable from the monitoring variable.
- Experimental Protocol: Factorial Design for Component Isolation
- Design: 2x2 factorial: Insulin Type (Novel Ultra-Rapid vs. Standard Rapid) x Monitoring Input (Ideal Continuous Plasma Glucose vs. Real CGM with Noise).
- Method:
- Conduct in-silico trials using a cohort of virtual patients.
- Arm A: Ultra-Rapid Insulin + Ideal Glucose.
- Arm B: Ultra-Rapid Insulin + Real CGM.
- Arm C: Standard Rapid Insulin + Ideal Glucose.
- Arm D: Standard Rapid Insulin + Real CGM.
- Apply identical meal and exercise challenges.
- Primary Outcome: Time Below Range (<70 mg/dL).
- Analysis: Statistical interaction analysis will show if the benefit of ultra-rapid insulin is dependent on or independent of CGM quality.
FAQ 3: Our data shows high glycemic variability (GV) even with "good" Time in Range (TIR). What metrics should we prioritize to understand the coordination failure?
- Answer: TIR can mask frequent oscillations. Prioritize metrics that capture rate of change and asymmetry of excursions.
- Quantitative Data Summary: Key Glycemic Metrics
| Metric | Formula/Description | Target (General) | Indicates Coordination Failure When... |
|---|---|---|---|
| Time in Range (TIR) | % time 70-180 mg/dL | >70% | May be adequate, but insufficient alone. |
| Glycemic Variability (GV) | Coefficient of Variation (CV) | <36% | High CV (>36%) despite good TIR. |
| Low Blood Glucose Index (LBGI) | Risk index weighting hypoglycemic readings | Lower is better | Elevated, indicating frequent/profound lows. |
| High Blood Glucose Index (HBGI) | Risk index weighting hyperglycemic readings | Lower is better | Elevated, indicating frequent/profound highs. |
| Mean Amplitude of Glycemic Excursions (MAGE) | Average height of glucose swings exceeding 1 SD | <70 mg/dL | High value, showing large, un-damped oscillations. |
| Time to Peak (Postprandial) | Time from meal to peak glucose | Shorter is better | Prolonged, suggesting delayed insulin action. |
| Time to Nadir (Post-hypo treatment) | Time from hypoglycemia to recovery >70 mg/dL | Shorter is better | Prolonged, suggesting over-treatment or insulin stacking. |
Mandatory Visualizations
Diagram Title: Closed-Loop System Lag Contributors
Diagram Title: Mechanism Map: Coordination Failure to Clinical Risk
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Coordination Research |
|---|---|
| FDA-Accepted Glucose-Insulin Simulator (e.g., UVA/Padova) | Provides a virtual patient cohort for in-silico testing of algorithms, insulins, and sensors in a controlled, reproducible environment. Essential for factorial design studies. |
| Insulin Pharmacokinetic/Pharmacodynamic (PK/PD) Models (e.g., Hovorka, Wilinska) | Mathematical descriptions of insulin absorption, distribution, and action. Used to simulate and compare novel insulin profiles against standard care. |
| CGM Error Models (e.g., AR(1) + White Noise) | Algorithms that add realistic sensor noise, bias, and lag to an ideal glucose signal. Critical for testing system robustness. |
| Standardized Meal & Exercise Protocols | Defined carbohydrate amounts and timings, and energy expenditure profiles. Enables consistent perturbation of the gluco-regulatory system for comparative studies. |
| Glycemic Variability Analysis Software (e.g., EasyGV, GlyCulator) | Calculates advanced metrics (MAGE, LBGI, HBGI, CONGA) from continuous glucose data to move beyond simple TIR analysis. |
| Control Algorithm Bench-Testing Platform | A software/hardware environment where a candidate control algorithm can be connected to a simulator or animal model in real-time, mimicking a closed-loop system. |
Welcome to the Technical Support Center. This resource is designed for researchers and drug development professionals working to overcome the interoperability challenges between glucose sensing and insulin delivery technologies. The following troubleshooting guides and experimental protocols are framed within the thesis of addressing the critical lack of coordination between these historically separate research domains.
Troubleshooting & FAQs
Q1: Our in-vitro closed-loop simulation is failing due to inconsistent data transmission latency between our custom continuous glucose monitor (CGM) sensor and the insulin pump driver. What are the primary points of failure to investigate?
A1: This is a classic interoperability issue stemming from siloed development. Investigate in this order:
- Protocol Handshake Failure: Verify the communication protocol (e.g., Bluetooth LE, custom RF) is identical on both sides. Use a protocol analyzer to check for repeated connection/disconnection events.
- Data Packet Corruption: Check the packet structure. A mismatch in endianness (byte order) between the CGM's microcontroller and the pump's receiver will corrupt data.
- Clock Synchronization Drift: The timestamp from the CGM and the pump's internal clock must be synchronized. Even a 100ms drift can destabilize a fast-acting insulin algorithm. Implement a Network Time Protocol (NTP) sync within your test rig.
- Electromagnetic Interference (EMI): The pump's motor driver can generate EMI that disrupts the CGM's analog front-end, especially in a benchtop setup. Increase physical separation and use shielded cabling.
Q2: When integrating a novel fluorescent glucose sensor with a microfluidic insulin delivery chip, we observe insulin denaturation at the interface. What is the likely cause and solution?
A2: The issue likely lies in the material biocompatibility and fluidic dynamics.
- Likely Cause: The sensor's flow cell may use an adhesive or polymer (e.g., PDMS) that is leaching uncrosslinked oligomers into the fluid path, or the interaction of the sensor's excitation wavelength is generating localized heat.
- Solution:
- Perform a cytotoxicity assay (ISO 10993-5) on the combined materials.
- Implement a passivation layer (e.g., PEG silane) on all wetted surfaces.
- Redesign the fluidic junction to minimize dead volume where fluid can stagnate and heat up. Use a stepped, coaxial interface instead of a simple T-junction.
Q3: Our algorithm for predicting hypoglycemic events performs well on CGM data alone but fails when insulin-on-board (IOB) data from the pump is introduced. How can we debug the algorithm's data fusion process?
A3: The failure indicates poor temporal alignment or incorrect weighting of the two data streams.
- Debugging Protocol:
- Temporal Alignment: Create a master clock for your experiment. Log all CGM readings (e.g., every 5 min) and pump insulin delivery events (every bolus/basal change) with nanosecond timestamps. Manually inspect for misalignment.
- Data Weighting Analysis: Run the algorithm with only CGM data (weight=1.0, IOB=0.0) and note performance. Gradually increase the IOB weight from 0.1 to 1.0 while monitoring the prediction error (see Table 1). The point where performance degrades indicates a flaw in how the IOB pharmacokinetic/pharmacodynamic (PK/PD) model interacts with the CGM trend model.
Table 1: Algorithm Performance vs. IOB Data Weight
| IOB Data Weight | Prediction Sensitivity (%) | Prediction Specificity (%) | Mean Absolute Error (mg/dL) |
|---|---|---|---|
| 0.0 (CGM only) | 88.5 | 92.1 | 14.2 |
| 0.2 | 87.9 | 93.0 | 13.8 |
| 0.5 | 82.1 | 90.5 | 18.7 |
| 0.8 | 75.4 | 85.2 | 24.3 |
| 1.0 | 70.1 | 80.9 | 29.5 |
Experimental Protocols
Protocol 1: Assessing Cross-Technology Interference in a Benchtop Artificial Pancreas System
Objective: To quantify the electromagnetic and software interference between a commercial CGM transmitter and a research-grade insulin pump in a simulated wearable configuration.
Materials:
- Commercial CGM System (Transmitter & Receiver)
- Research Insulin Pump (with programmable driver)
- Saline solution (0.9% NaCl)
- Faraday cage or shielded enclosure
- Oscilloscope & Spectrum Analyzer
- Glucose clamp apparatus (for sensor stimulation)
- Data logging software (e.g., LabVIEW, custom Python)
Methodology:
- Place the CGM transmitter and insulin pump motor driver 5 cm apart (typical on-body distance) inside the Faraday cage.
- Initiate a stable basal insulin delivery profile (e.g., 0.05 U/hr).
- Simultaneously, use the glucose clamp to expose the CGM sensor to a stepped glucose concentration (80 → 180 → 80 mg/dL).
- Record the true CGM signal from its test points via the oscilloscope while simultaneously logging the transmitted data received by the CGM's official receiver.
- Introduce a large bolus command (1.0 U) to the pump. Capture the high-frequency EMI spectrum from the pump motor and the raw analog signal from the CGM sensor.
- Repeat at distances of 2 cm and 10 cm.
- Analysis: Correlate pump activation events with artifacts or dropouts in the CGM's raw signal. Calculate the signal-to-noise ratio (SNR) degradation.
Protocol 2: Validating a Unified Communication Protocol for Research Devices
Objective: To implement and test a standardized data packet structure (based on IEEE 11073 PHD) for seamless data exchange between disparate research CGM and pump prototypes.
Materials:
- Two microcontroller units (MCUs) (e.g., ARM Cortex-M4).
- RF transceivers (e.g., 2.4 GHz).
- Glucose sensor simulator.
- Pump actuator simulator.
Methodology:
- Packet Design: Define a unified packet with fields: [Header][Timestamp][Device ID][Glucose Value/Insulin Command][CRC Checksum].
- Firmware Development: Program one MCU as the "CGM Simulator" to generate packets. Program the other as the "Pump Controller" to receive and parse them.
- Latency & Reliability Test: Transmit 10,000 packets at intervals from 100ms to 5 minutes. Log transmission and acknowledgement times.
- Error Injection Test: Deliberately corrupt packets (bit-flips) to test the CRC checking and re-transmission logic.
- Analysis: Calculate mean latency, packet loss rate, and system recovery time from errors (see Table 2).
Table 2: Unified Protocol Performance Metrics
| Metric | Target Performance | Observed Performance | Pass/Fail |
|---|---|---|---|
| Mean Transmission Latency | < 100 ms | 47 ms | Pass |
| Packet Loss Rate (10k packets) | < 0.1% | 0.05% | Pass |
| CRC Error Detection Rate | 100% | 100% | Pass |
| System Recovery after Error | < 1 sec | 0.8 sec | Pass |
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Integration Research |
|---|---|
| PDMS (Polydimethylsiloxane) | Used to create microfluidic channels for insulin delivery chips. Must be thoroughly cured and passivated to prevent analyte absorption. |
| PEG-Silane | A passivation reagent used to coat sensor and fluidic surfaces, creating a bio-inert, non-fouling layer to prevent protein (insulin) adhesion. |
| Glucose Oxidase (GOx) | The standard enzyme for electrochemical glucose sensing. Research focuses on stabilizing GOx in novel sensor membranes for longer life. |
| Fluorescent Glucose Analogs (e.g., 2-NBDG) | Used to validate and calibrate optical glucose sensors in cell-based or tissue-simulating environments. |
| Insulin Radiolabeling Kits (e.g., with I-125) | Allows for precise tracking of insulin adsorption to device materials and delivery kinetics in in-vitro setups. |
| Artificial Interstitial Fluid | A buffered solution mimicking the chemical composition of subcutaneous tissue, crucial for testing sensor performance and insulin stability in physiologically relevant conditions. |
System Integration & Signal Flow Diagram
Interoperability Failure Analysis Diagram
Technical Support Center: Troubleshooting & FAQs
Q1: In our closed-loop insulin delivery in silico experiments, we observe persistent postprandial hyperglycemia despite accurate carbohydrate input. Which inherent physiological lag is most likely responsible, and how can we model it correctly?
A1: The most likely culprit is the delayed appearance of glucose in the bloodstream from the gut (glucose absorption lag), compounded by the delay in subcutaneous insulin reaching the systemic circulation (pharmacokinetic lag). The gut absorption lag can be 20-45 minutes, while the onset of action for subcutaneously injected rapid-acting insulin is still 15-30 minutes.
Troubleshooting Protocol: Implement a two-compartment absorption model for both glucose and insulin in your simulation.
- For Glucose: Use an oral glucose model with a gastric emptying compartment and an intestinal absorption compartment. Key parameter:
tau_g(time constant for gastric emptying). - For Insulin: Use a subcutaneous insulin model with two compartments (e.g., a depot compartment and plasma compartment). Key parameter:
tau_i(time constant for insulin absorption). - Validation Step: Compare your simulation's predicted plasma glucose curve against clinical data from mixed-meal tolerance tests. Mismatch in the first 60-90 minutes indicates inaccurate lag parameterization.
Q2: Our continuous glucose monitor (CGM) data consistently lags behind reference blood glucose measurements during rapid glucose changes, confounding our assessment of novel insulin analogs. What is the source and magnitude of this lag?
A2: The CGM lag is a combination of physiological and technical delays. The physiological lag (3-12 minutes) is due to the time for glucose to equilibrate from blood to interstitial fluid (ISF). The technical/algorithmic lag (5-15 minutes) is due to sensor response time and noise-filtering algorithms. The total lag can be 5-25 minutes.
Experimental Protocol to Quantify CGM Lag:
- Setup: Conduct a hyperglycemic clamp or intravenous glucose tolerance test in an animal or human study cohort.
- Measurement: Take frequent (every 5 min) reference venous or arterial blood samples for lab glucose analysis (YSI/Beckman analyzer).
- Data Synchronization: Precisely time-sync CGM and reference data streams.
- Analysis: Perform cross-correlation analysis or use a time-shift optimization method to find the time delay (
Δt) that maximizes the correlation between the two signals. Compute the mean absolute relative difference (MARD) atΔt.
Table 1: Quantitative Summary of Inherent Lag Times
| Lag Source | Typical Duration | Key Influencing Factors | Mitigation Strategies in Research |
|---|---|---|---|
| CGM Physiological (Blood→ISF) | 3 - 12 min | Tissue perfusion, metabolism, sampling rate | Use vasodilators locally; validate with more frequent references. |
| CGM Technical/Algorithmic | 5 - 15 min | Sensor membrane, smoothing filters | Use raw sensor data streams; apply deconvolution algorithms. |
| SC Insulin Absorption (PK) | 45 - 120 min (to peak) | Injection site, local blood flow, formulation | Study intraperitoneal or intravenous delivery; use faster-acting analogs (e.g., Lyumjev). |
| Insulin PD Onset (Cell Signaling) | 15 - 30 min | Receptor binding, phosphorylation cascade | Investigate direct glucokinase activators or hepatic-focused pathways. |
| Gut Glucose Absorption | 20 - 45 min (to peak) | Meal composition, gastric emptying | Model with multi-compartment approaches; consider co-administration with pramlintide. |
Q3: When evaluating a novel insulin-receptor agonist in vitro, how do we design a protocol to isolate and measure the pharmacodynamic (PD) signaling lag, separate from pharmacokinetic (PK) absorption issues?
A3: To isolate PD lag, you must bypass the PK (absorption/distribution) phase by applying the compound directly to the target system.
Detailed Experimental Protocol: Title: In Vitro Kinetics of Insulin Receptor Signaling Activation
- Cell Preparation: Use HEK-293 cells stably overexpressing the human insulin receptor (IR), or primary hepatocytes. Serum-starve for 6-8 hours.
- Rapid Agonist Application: Use a rapid perfusion system or fast pipetting to switch the medium to one containing a saturating dose (e.g., 100 nM) of the insulin analog/agonist. Record exact time of application as t=0.
- High-Frequency Sampling: At defined time points (e.g., 0, 30s, 1, 2, 5, 10, 15, 30, 60 min) post-application, rapidly lyse cells.
- Western Blot Analysis: Probe lysates for:
- Early Signal: Phospho-IR (Tyr1150/1151) and Phospho-IRS1.
- Intermediate Signal: Phospho-Akt (Ser473).
- Functional Output: Phospho-AS160 (for GLUT4 translocation studies in adipocytes).
- Data Analysis: Plot band intensity (normalized to total protein/loading control) vs. time. Define PD lag as the time from t=0 to a statistically significant increase in pIR. Define time-to-peak for each phosphorylation event.
Diagram Title: Isolating PD Signaling Lag from PK Absorption Lag
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Lag Research | Example/Supplier |
|---|---|---|
| Hyperinsulinemic-Euglycemic Clamp Platform | Gold-standard in vivo method to measure insulin action delay (peripheral & hepatic) by infusing insulin and glucose separately. | Human or large animal physiology lab; automated clamp systems. |
| Frequent Manual Sampling (Arterial/Venous Catheter) | Provides PK/PD reference data without device-related lags for calibrating CGM or validating insulin assays. | Bioanalytical method for insulin (ELISA/MSD) and glucose (YSI analyzer). |
| Rapid-Sampling In Vitro Perfusion System | Allows precise, sub-minute timing for adding/removing stimuli to measure early signaling kinetics. | Brand: BioLogic SFM-400; or custom-built laminar flow chambers. |
| Phospho-Specific Antibody Panels | Critical for mapping the time-course of insulin signaling cascade activation (pIR, pIRS, pAkt, pAS160). | Cell Signaling Technology, PhosphoSolutions. |
| Tracer Compounds (Stable Isotope Glucose) | Allows modeling of endogenous glucose production and glucose disposal rates independently during dynamic tests. | [6,6-²H₂]-glucose; infusion pumps for primed-constant infusion. |
| UV-Crosslinkable Insulin Analogs | Used to "freeze" the momentary in vivo state of insulin-receptor binding and internalization for spatial/temporal analysis. | Photoactive insulin derivatives (e.g., Bpa⁵¹⁶-insulin). |
| Mathematical Modeling Software | For fitting PK/PD models (MinMod, SAAM II) and simulating closed-loop control with incorporated lags. | MATLAB/Simulink, R, Python (with SciPy, PySB). |
Q4: How do we mathematically model the combined effect of multiple sequential lags (CGM + Insulin PK) for designing a predictive hypoglycemia alarm?
A4: The cascaded lags are best modeled as a series of time-delay differential equations (DDEs) or using a chain of Laplace transforms with transport delays.
Protocol for Building a Composite Lag Model:
- Define Individual Transfer Functions:
- CGM Lag:
G_cgm(s) = e^(-s*τ_cgm) / (α*s + 1)whereτ_cgmis the pure delay andαis the sensor time constant. - Insulin PK Lag: A two-compartment model:
I_plasma(s) / I_sc(s) = (1/(V1*s)) * (k1/(s+k2)) * e^(-s*τ_sc).
- CGM Lag:
- Cascade the Models: The perceived glucose error signal (
e(t)) for a controller becomes:e(t) = y_cgm(t) - target, wherey_cgm(t)is the delayed and filtered version of true blood glucose. - Implement in Simulation:
- Validation: Tune the lag parameters (
τ_cgm, τ_sc, etc.) by minimizing the error between your model's prediction and clinical dataset outcomes (e.g., from the OhioT1DM dataset).
Diagram Title: Cascaded Lag Model for Closed-Loop Insulin Delivery
This technical support center provides guidance for researchers and drug development professionals addressing coordination challenges between glucose monitoring and insulin injection research. The following troubleshooting guides and FAQs are framed within the broader thesis of improving this critical coordination.
Frequently Asked Questions & Troubleshooting
Q1: Our clinical trial data shows inconsistent correlation between continuous glucose monitor (CGM) readings and subsequent insulin dosing adherence. What are the primary human factor variables we should isolate?
A1: Inconsistent correlations often stem from unaccounted cognitive load variables. You must isolate and measure:
- Decision Fatigue: Track the time of day of dosing decisions against deviation from protocol.
- Alert Burden: Quantify the number of CGM alerts/notifications preceding a dose. High alert volumes precede user "alert fatigue" and ignored readings.
- Context Switching Cost: Measure if dosing occurs during a separate task (e.g., work meeting, driving) vs. a dedicated health management period.
Experimental Protocol for Isolation:
- Design: A 7-day observational study with type 1 diabetes participants using a CGM and smart insulin pen.
- Data Streams: Synchronize timestamped data for: CGM readings, all device alerts, insulin doses (time and amount), participant-reported activity via a simplified ecological momentary assessment (EMA) app.
- Analysis: Perform a multivariable regression where the dependent variable is the absolute difference between actual insulin dose and algorithm-suggested dose. Independent variables should include: number of CGM alerts in past 60 minutes, time of day, reported concurrent activity type.
Q2: How can we experimentally quantify the "burden" of a hybrid closed-loop system setup for an elderly participant in a study?
A2: Burden is a composite metric. Use the following validated tools and objective measures:
| Metric Category | Specific Measurement Tool | Quantitative Output / Scale |
|---|---|---|
| Subjective Burden | Diabetes Technology Burden Questionnaire (DTBQ) | 33-item scale; higher score indicates greater burden. |
| Cognitive Load | NASA-Task Load Index (NASA-TLX) | 6-subscale score (Mental, Physical, Temporal Demand, Performance, Effort, Frustration). |
| Usability | System Usability Scale (SUS) | Score from 0-100. |
| Objective Time Burden | Direct Observation & Timing | Mean time (minutes) to initialize system, respond to alerts, and perform daily maintenance. |
Experimental Protocol for Quantification:
- Recruitment: Enroll participants aged 65+ with type 2 diabetes, naive to hybrid closed-loop systems.
- Training: Provide standardized training on the specific system.
- First-Use Session: Videotape the participant's first independent setup and calibration. Record time-to-completion and number of errors (requiring intervention).
- Post-Session Metrics: Immediately administer NASA-TLX and relevant SUS items.
- Post-Study Metric: After 14 days, administer the full DTBQ and SUS.
Q3: We suspect "calculation aversion" is causing poor adherence to titration protocols in our insulin study. How can we redesign the protocol to mitigate this?
A3: "Calculation aversion" is a key human factor. Redesign your protocol to eliminate manual arithmetic.
Original Protocol Burden: "Check fasting glucose daily. If average over past 3 days is above target, increase nightly basal insulin by 2 units. If below target, decrease by 1 unit."
Redesigned Protocol (Reduced Burden): "Use the provided study app. It will:
- Automatically read your fasting glucose from your connected meter/CGM.
- Calculate the 3-day average.
- Display a clear message: 'This week's dose: units. Last week's dose: [Y] units.'" The calculation is removed from the user's mental workload and performed reliably by the system.
Q4: What are common data synchronization failures between glucose and insulin data streams, and how can we resolve them?
A4: Failures primarily occur at the device, software, or human action layer.
| Failure Point | Symptom | Troubleshooting Guide |
|---|---|---|
| Time Synchronization | Insulin dose timestamps are hours off from CGM event logs. | Solution: Mandate automatic network time (NTP) sync for all apps/ devices. Include a time-discrepancy check in data QA scripts. |
| Manual Logging Delay | Manually logged meals or doses show "clustering" at convenient times (e.g., end of day). | Solution: Use Bluetooth-connected devices (pens, meters) that timestamp events automatically. Supplement with prompted EMA entries. |
| Device Pairing Loss | CGM data is present but corresponding insulin data from a "smart" pen is missing for a period. | Solution: Implement a daily device connectivity check within the study app. Provide clear visual feedback (e.g., "Pen Connected" icon). |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Human Factors Research |
|---|---|
| Bluetooth-Enabled Smart Insulin Pen | Captures objective, timestamped dosing data (dose amount, time) without relying on user recall or manual entry. |
| Continuous Glucose Monitor (CGM) API Access | Allows researchers to pull raw, timestamped glucose and alert data directly from the manufacturer's cloud for precise synchronization. |
| Ecological Momentary Assessment (EMA) Platform | Enables real-time, in-context subjective data collection (e.g., burden, cognitive load, situational context) via a participant's smartphone. |
| Data Synchronization Hub Platform | A secure middleware (e.g., Glooko, Tidepool) or custom-built platform that ingests and time-aligns disparate data streams (CGM, insulin, activity) for unified analysis. |
| Usability Testing Software | Tools like UserTesting.com or Morae for recording and analyzing participant interactions with study devices and apps, identifying points of confusion. |
Experimental Workflow & Pathway Diagrams
Diagram Title: Data Integration Workflow for Human Factors Research
Diagram Title: Cognitive Load Pathway to Dosing Error
Engineering Synergy: Current and Emerging Methodologies for Integrated Control
Technical Support Center: Troubleshooting & FAQs
FAQ: Algorithm & Sensor Integration Q1: Our in-silico model shows the control algorithm persistently over-corrects for postprandial glucose spikes, leading to late-onset hypoglycemia. What are the primary tuning parameters to investigate? A1: Focus on the postprandial insulin feedback gain and the insulin-on-board (IOB) constraints. Excessive postprandial gain or an overestimated IOB half-life can cause this. Adjust the IOB decay model and implement stricter IOB limits during predicted high-glycemic-index meals. Refer to Table 1 for key parameter targets.
Q2: During animal trials, we observe a systemic inflammatory response causing sustained sensor sensitivity drift. How can we decouple inflammation from true hypoglycemia in the algorithm's diagnostic module? A2: Implement a multi-signal diagnostic layer. Algorithmic intelligence must integrate:
- C-Reactive Protein (CRP) trend data from a secondary assay.
- Interstitial Fluid (ISF) kinetics model to identify abnormal lag times.
- Heart rate variability (HRV) data from a bio-telemetry implant. A decision tree logic (see Diagram 1) should weight these inputs to flag "Low Confidence" sensor data, triggering a fallback to conservative basal rates.
Q3: The hybrid closed-loop (HCL) system fails to initiate auto-correction boluses for rising glucose trends in our primate model, despite manual bolus working. What is the likely root cause? A3: This typically indicates a fault in the "Meal Detection" or "Rise Detection" module, not the correction algorithm itself. Verify:
- Sensor noise filtering thresholds are not set too high, obscuring a true rise.
- The rate-of-change (ROC) trigger is calibrated for the model's physiology (primate ROC may differ from human proxies).
- Auto-mode is actually active; confirm the system isn't stuck in a "basal-only" safety state due to a missed calibration.
Experimental Protocol: In-Vivo Validation of Algorithm Adaptation Title: Protocol for Validating Adaptive Insulin Feedback Parameters in a Minipig HCL Model. Objective: To test an algorithm's ability to self-adjust insulin sensitivity factor (ISF) based on circadian patterns.
- Implant: Continuous glucose monitor (CGM) and insulin pump.
- Baseline Period (72 hrs): Run standard HCL algorithm. Collect glucose time-in-range (TIR) and insulin delivery data.
- Algorithm Adaptation Phase: Enable the adaptive ISF module. The algorithm analyzes nocturnal vs. diurnal insulin requirement patterns.
- Challenge Phase: Introduce standardized mixed-meal tests at both day (active) and night (rest) phases.
- Metrics: Compare glucose RMSE, TIR (70-180 mg/dL), and hypoglycemic events between Baseline and Adapted phases for night vs. day.
- Endpoint Analysis: Use paired t-test on RMSE data (see Table 2).
Key Data Tables
Table 1: Core Algorithm Parameters for Tuning Postprandial Response
| Parameter | Typical Range | Effect of Increasing Value | Primary Risk |
|---|---|---|---|
| Postprandial Gain | 1.0 - 3.0 | More aggressive correction of high glucose | Late-phase hypoglycemia |
| IOB Half-Life | 60 - 120 min | Longer assumed insulin action | Insulin stacking, hypoglycemia |
| ROC Trigger (mg/dL/min) | 1.5 - 3.0 | Earlier meal detection | False positives, over-delivery |
| Target Glucose (mg/dL) | 110 - 140 | Tighter control | Increased hypoglycemia risk |
Table 2: Sample Experimental Results - Adaptive ISF Protocol (n=6 minipigs)
| Phase | Avg. Glucose (mg/dL) | TIR (%) | Nocturnal Hypo Events (<70 mg/dL) | Glucose RMSE (vs. Target) |
|---|---|---|---|---|
| Baseline (Static ISF) | 145 ± 18 | 68.2% | 4 | 24.5 |
| Adaptive ISF Active | 132 ± 12 | 82.7% | 1 | 16.1 |
| p-value | <0.05 | <0.01 | 0.08 | <0.01 |
Signaling & Diagnostic Pathway Visualizations
Diagram 1: Multi-Signal Diagnostic for Sensor Anomaly
Diagram 2: AHCL Algorithm Core Feedback Loop
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in HCL/AHCL Research |
|---|---|
| Stable Isotope-Labeled Glucose Tracers | Allows precise kinetic modeling of glucose appearance/disappearance, critical for validating algorithm state estimates. |
| High-Fidelity CGM Sensor Arrays | Research-grade sensors with raw data output for developing and testing noise filtration and lag-compensation algorithms. |
| Programmable Insulin Analog Infusates | Enables testing of novel ultra-rapid or hepatic-preferential insulins within the closed-loop context. |
| Multiplex Cytokine Assay Panels | Quantifies inflammatory markers to correlate with sensor performance degradation and refine diagnostic modules. |
| Telemetric Physiologic Monitors (ECG/Temp/Activity) | Provides covariate data (HR, HRV, activity) for context-aware algorithmic adjustments and safety interlocks. |
| In-Silico Simulation Platform (e.g., UVA/Padova Simulator) | Provides a safe, initial testbed for algorithm changes using accepted metabolic models before animal studies. |
Technical Support & Troubleshooting Center
This resource addresses common technical and experimental challenges when implementing device interoperability protocols in a research setting focused on coordinating glucose monitoring and insulin delivery.
Frequently Asked Questions (FAQs)
Q1: Our in-house simulator cannot decode data packets from a continuous glucose monitor (CGM) using the DIDI protocol. What are the first steps?
- A: First, verify the conformance statement provided by the CGM manufacturer. Ensure your simulator is using the correct version of the IEEE 11073-10425 standard (the core of DIDI). Check the
MDS(Medical Device System) object attributes for errors. Commonly, the mismatch is in theSystem-ModelorSystem-IDfields. Use a packet analyzer (e.g., Wireshark) to capture raw data and compare it against the standard's ASN.1 schema.
- A: First, verify the conformance statement provided by the CGM manufacturer. Ensure your simulator is using the correct version of the IEEE 11073-10425 standard (the core of DIDI). Check the
Q2: When integrating an automated insulin delivery (AID) research system, we encounter significant latency (>5 minutes) between glucose data receipt and pump command. How can we isolate the cause?
- A: This requires systematic isolation. Follow this workflow: 1) Bypass the interoperability layer and inject simulated glucose data directly into your control algorithm to test its inherent latency. 2) Re-introduce the DIDI data translation layer alone with simulated data. 3) Finally, test with the physical CGM and DIDI translator. The issue is often in the middleware's event-handling loop or in network configuration (e.g., excessive polling intervals instead of unsolicited reports). See Table 1 for benchmark metrics.
Q3: We are planning a preclinical study comparing two insulin pump APIs. What are the key interoperability parameters to measure?
- A: You must establish a standardized test bench. Key quantitative parameters to measure and compare are listed in Table 2. Essential qualitative factors include the clarity of the API's error codes and the robustness of its safety-critical command set (e.g., hard-stop bolus, suspend).
Q4: How do we ensure our research using the Tidepool Platform or OpenAPS protocols is reproducible?
- A: Document the exact version of the open-source protocol specification and any vendor extensions used. For Tidepool, specify the
tide-mobile-clientanduploaderversions. For OpenAPS, document theoref0commit hash. All data transformations (e.g., smoothing of CGM data) must be described and their code archived. Use the provided "Experimental Protocol: Benchmarking Data Flow Latency" as a template for methodology detail.
- A: Document the exact version of the open-source protocol specification and any vendor extensions used. For Tidepool, specify the
Troubleshooting Guides
Issue: Erratic or Missing Data in a Multi-Vendor Research Stack
- Symptoms: Gaps in timestamped glucose records, insulin dose logs that fail to appear in the data aggregator.
- Diagnostic Steps:
- Validate Individual Streams: Confirm each device (CGM, pump) logs data correctly to its native proprietary application.
- Check Translator Integrity: Verify the middleware device or software (e.g., insulin pump communication driver, Bluetooth-to-IP bridge) is powered and has a stable connection. Restart it.
- Review Log Files: Examine the application log files of your research data aggregator (e.g., your custom Python service, Nightscout instance) for errors. Common errors are
"CRC_FAIL","TIMEOUT", or"UNSUPPORTED_ATTRIBUTE". - Protocol Sniffing: Use a dedicated protocol analyzer (e.g., for Bluetooth Low Energy) to confirm the physical layer communication is intact.
- Solution: 90% of issues are resolved at Step 3. Update or re-configure the translator software based on the specific error. Ensure no other research software is concurrently trying to access the same device, causing a resource lock.
Issue: Inconsistent Results When Replaying Archived Data
- Symptoms: An algorithm behaves differently when processing live data from an interoperable system versus its validated performance on a static, archived dataset.
- Diagnostic Steps:
- Metadata Audit: Archived research datasets often strip or anonymize crucial metadata. Check for the presence of
device_sn,system_id,timezone_offset, andclock_driftfields. - Timestamp Alignment: Live data may have millisecond-level jitter. Apply the same smoothing or binning function you used in your original analysis to the live stream.
- State Persistence: Verify that your algorithm's state variables (e.g., insulin-on-board, rate-of-change trend) are being initialized correctly upon system start in the live test, matching the archived run's starting state.
- Metadata Audit: Archived research datasets often strip or anonymize crucial metadata. Check for the presence of
- Solution: Create a "replay harness" that ingests the archived data but uses the exact same data ingestion and preprocessing module as your live interoperability setup. This isolates the difference to the data input pipeline.
Data Presentation
Table 1: Benchmark Latency Metrics for Key Interoperability Components (Ideal Research Environment)
| Component | Protocol | Measured Latency (Mean ± SD) | Acceptable Threshold for AID Research | Primary Influence Factor |
|---|---|---|---|---|
| CGM to Smartphone | Bluetooth LE (Manufacturer Specific) | 12 ± 5 s | < 60 s | Device bonding & polling rate |
| Data Translation (DIDI Layer) | IEEE 11073-10425 | 180 ± 50 ms | < 500 ms | Middleware processor speed |
| Cloud Upload/Download | HTTPS/REST API | 2.5 ± 1.5 s | < 10 s | Network bandwidth & SSL handshake |
| Control Algorithm Cycle | N/A | 50 ± 20 ms | < 200 ms | Code optimization & hardware |
| Pump Command Delivery | ISO/IEEE 11073-10419 (DIDI Pump) | 800 ± 200 ms | < 2 s | Radio frequency interference |
Table 2: Comparative Analysis of Insulin Pump API Suites for Research
| Parameter | Pump API A (Commercial) | Pump API B (Open Research) | Measurement Method |
|---|---|---|---|
| Command Latency | 1200 ms | 850 ms | Time from send() to delivery confirmation |
| Data Granularity | 5-min basal logs, per-bolus | 1-min basal logs, per-pulse | Log audit via vendor tool vs. open log |
| Error Code Detail | 15 generic codes | 48 specific codes | Analysis of API documentation |
| Safety Lockouts | Mandatory 2-min suspend | Configurable 0-30 min | Experimental testing with override |
| Real-time Status | Battery, Reservoir | + Occlusion, Self-test status | Polling frequency capability |
Experimental Protocols
Protocol: Benchmarking End-to-End Data Flow Latency in an Interoperable Research System
Objective: To quantitatively measure the total latency from glucose sensing to actionable insulin delivery command in a multi-device, protocol-driven research setup.
Methodology:
- Synchronization: All system components (CGM simulator, interoperability middleware, research laptop, insulin pump simulator) are time-synchronized using Network Time Protocol (NTP) to a master clock with millisecond precision.
- Timestamp Injection: A glucose simulator generates a precise glucose value
G_tat timeT0. This value is packetized withT0embedded in the payload. - Pathway Instrumentation: Each system component is instrumented to log the arrival time (
T_arr) and departure time (T_dep) of the data packet containingG_t.- Key nodes: CGM Emulator output, DIDI Translator input/output, Control Algorithm input/output, Pump API gateway.
- Data Collection: The experiment is repeated
n=500times over a 72-hour period, simulating various system loads. - Calculation: Latency at each node
L_node = T_dep - T_arr. Total latencyL_total = T_pump_cmd_received - T0. - Analysis: Statistical analysis (mean, standard deviation, 95th percentile) is performed on
L_totaland per-node latencies to identify bottlenecks.
Protocol: Evaluating Protocol Fidelity Using Signal Replay
Objective: To assess the data integrity and fidelity of an open interoperability protocol (e.g., Tidepool's tide-whisperer) versus a manufacturer's proprietary protocol.
Methodology:
- Capture: Use a Man-in-the-Middle (MITM) hardware tool (with ethical/legal approvals) to simultaneously capture raw data packets from a device using both the proprietary RF protocol (Signal A) and the open protocol translation (Signal B).
- Stimulus Generation: A scripted series of physiological events (rapid glucose rise, plateau, fall) and device events (calibration, suspend, resume) is enacted on the device.
- Data Alignment: The two time-series data streams are aligned using a shared, injected event marker (e.g., a unique 10-digit timestamp).
- Comparison: For each recorded parameter (glucose value, insulin dose, device alert), calculate the discrepancy
Δ = Value_A - Value_Band the time skewΔt = Timestamp_A - Timestamp_B. - Validation: Establish a fidelity threshold (e.g.,
Δ_glucose < 0.1 mmol/L,Δt < 5 s). The percentage of data points meeting these thresholds defines the protocol fidelity score.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Interoperability Research |
|---|---|
| Protocol Analyzer (e.g., Ellisys BLE) | Captures and decodes raw Bluetooth Low Energy packets to debug physical/link layer communication between devices and translators. |
| Medical Device Simulators | Software/hardware that emulates CGMs and pumps, generating predictable, repeatable data streams for controlled experiments. |
| Reference Glucose Analyzer | Laboratory instrument (e.g., YSI Stat) provides ground-truth glucose values to calibrate and validate the accuracy of data streams from interoperable CGMs. |
| Precision Time Protocol (PTP) Grandmaster Clock | Enables microsecond-level synchronization across all research hardware, essential for precise latency measurement. |
| Data Anonymization Suite | Software that scrubs Protected Health Information (PHI) from real-world data logs while preserving crucial temporal and device metadata for research. |
| Middleware Development Kit (e.g., from Continua) | Provides reference code and tools to implement IEEE 11073 (DIDI) standards, accelerating custom translator development. |
Visualizations
Diagram 1: DIDI Data Flow in AID Research
Diagram 2: Protocol Stack for Device Integration
Diagram 3: Troubleshooting Logic for Data Gaps
Technical Support Center: Troubleshooting Guides & FAQs for Research Setups
This technical support center is designed for researchers conducting experiments to address coordination failures between glucose monitoring and insulin injection. The guides below focus on common issues when integrating smart insulin pens and connected caps with experimental monitoring systems.
FAQs & Troubleshooting
Q1: In our closed-loop simulation, the timestamp data from the connected cap (e.g., Timesulin, Gocap) is not synchronizing with our continuous glucose monitor (CGM) data stream. How do we resolve this temporal misalignment?
A: This is a common data fusion issue. Follow this protocol:
- Protocol for Temporal Synchronization:
- Equipment: Smart Pen/Cap, Reference NTP server, Data logging server.
- Method: Before initiating the experiment, implement a unified Network Time Protocol (NTP) client on all data-logging devices (CGM receiver, smartphone receiving cap data, experimental control PC). Use a local NTP server for minimal latency.
- Validation: Perform a "sync pulse" at the start and end of each experimental session: manually trigger a simultaneous, unique marker (e.g., a specific small insulin dose, a button press) recorded by all systems. Use these markers to correct for any residual constant offset in post-processing.
Q2: The Bluetooth Low Energy (BLE) signal from our research-grade connected cap is frequently dropping during in-vivo animal studies, corrupting dose-logging data. What are the mitigation strategies?
A: Signal loss is often due to physical obstruction or interference.
- Troubleshooting Steps:
- Reproducible Placement: Standardize the position and orientation of the relay device (smartphone/BLE hub) relative to the animal enclosure.
- Interference Check: Identify and power down potential sources of 2.4 GHz interference (Wi-Fi routers, other lab equipment).
- Data Integrity Protocol: Implement application-layer data redundancy. Program the cap's firmware (if accessible) or the receiving app to send each dose log packet three times with a 100ms delay. On the receiver, use a "majority vote" system to confirm the correct data packet.
Q3: When validating insulin dose accuracy for a new pen prototype, our gravimetric analysis shows a high coefficient of variation (>5%). How should we isolate the error source?
A: Follow a systematic error isolation workflow.
- Experimental Protocol for Error Source Identification:
- Step 1 - Pen Mechanism Test: Disconnect the cap. Use a high-precision microbalance (0.1 mg resolution) to weigh the pen before and after a series of fixed-dose injections into air. Calculate actual delivered dose (1 unit ≈ 10 µL ≈ 10.096 mg for Humalog). This isolates mechanical pen error.
- Step 2 - Cap Sensor Calibration: Re-attach the cap. Perform injections without the cap's logging function active. Manually record the cap's displayed dose estimate versus the gravimetric ground truth to generate a calibration curve.
- Step 3 - Integrated System Test: Repeat with the cap's automatic logging enabled to validate the full system's data accuracy.
Q4: Our data pipeline from multiple smart pen brands (NovoPen 6, InPen, companion caps) produces heterogeneous data formats. What is the recommended method for creating a unified dataset for analysis?
A: Implement an Extract, Transform, Load (ETL) framework.
- Methodology:
- Extract: Use official SDKs/APIs where available (e.g., Novo Nordisk's
ConnectAPI, Medtronic'sCareLink). For reverse-engineered protocols, maintain a separate, version-controlled code library. - Transform: Create a common data schema. Map all vendor-specific fields to this schema. Key mandatory fields should include:
Device_ID,Timestamp_UTC,Insulin_Dose_IU,Injection_Flag (Bolus/Basal),Data_Quality_Score. - Load: Ingest the transformed data into a structured database (e.g., SQLite for small studies, PostgreSQL for larger cohorts) with strict data type validation.
- Extract: Use official SDKs/APIs where available (e.g., Novo Nordisk's
Table 1: Comparative Technical Specifications of Representative Devices in Research
| Device/Add-on | Communication | Dose Detection Method | Dose Logging Accuracy (as reported) | API/SDK for Research |
|---|---|---|---|---|
| Medtronic InPen | Bluetooth to App | Integrated | >99% | Yes (Limited) |
| NovoPen 6 & 7 | Bluetooth to App | Integrated | >99% | Yes (Novo Nordisk Connect) |
| Gocap | Bluetooth to App | Rotary Motion Sensor | ~97-99% | No (Data export via app) |
| Timesulin/Capen | Bluetooth to App | Timer-based (Dose inferred) | N/A (Timing only) | No |
Table 2: Common Data Artifacts and Correction Factors in Clinical Studies
| Artifact Type | Typical Frequency | Recommended Correction/Filtering Method |
|---|---|---|
| BLE Packet Loss | 2-5% in uncontrolled env. | Use forward error correction; interpolate from timestamp patterns. |
| Incorrect Time Zone Setting | ~10% of user-initiated data | Validate against CGM epoch time; apply offset. |
| "Ghost" Doses (Sensor False Positive) | <1% | Apply threshold filter (e.g., discard logged doses < 0.5 IU). |
| Missed Doses (User forgets cap) | 15-25% in real-world use | Flag sessions with >24h cap inactivity; statistical imputation may be required. |
Experimental Protocol: Validating Injection-to-Monitor Coordination Delay
Objective: Quantify the systemic delay between insulin injection (logged by smart cap) and the onset of detectable glucose change (via CGM) in a controlled setting.
Materials (Research Reagent Solutions):
- Subject Cohort: Porcine model (n=6), fasted.
- Insulin: Rapid-acting analog (Lispro/Aspart), 0.15 U/kg dose.
- Smart Insulin Pen & Cap: e.g., NovoPen 6 with integrated logging.
- CGM: Research-use CGM (e.g., Dexcom G7 with remote API).
- Reference Analyzer: YSI 2900 STAT Plus for venous blood glucose.
- Data Hub: Raspberry Pi 4 running custom Python script to time-sync pen data and CGM stream via NTP.
- Clamp Setup: (Optional) Euglycemic clamp apparatus to measure insulin pharmacokinetics/pharmacodynamics.
Procedure:
- Baseline Period (-30 to 0 min): Insert CGM. Stabilize subject. Confirm euglycemia (5.6-7.0 mmol/L).
- Synchronization Pulse (t=0 min): Using NTP-synchronized clocks, record a manual sync marker on all data streams.
- Injection & Logging (t=1 min): Administer the standardized bolus using the smart pen. The connected device automatically logs the exact timestamp and dose.
- High-Frequency Sampling (t=1 to 180 min): Collect CGM data at 1-min intervals via API. Draw venous samples for YSI analysis at t= -5, 0, 10, 15, 20, 30, 45, 60, 90, 120, 150, 180 min.
- Data Analysis: Align datasets using the sync pulse. Calculate the delay (
t_CGM_onset - t_injection_log) whereCGM_onsetis defined as the first timepoint where the CGM trend shows a consistent negative slope exceeding 0.1 mmol/L/min.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Smart Pen Coordination Research
| Item | Function/Application | Example/Supplier |
|---|---|---|
| NTP Server Hardware | Precise time synchronization across all data-logging devices. | Microchip GPS NTP Server; local Raspberry Pi NTP server. |
| Research CGM with API | Enables high-frequency, programmable data extraction for correlation with injection events. | Dexcom G6/G7 (Research API), Abbott Libre Pro H. |
| Data Fusion Platform | A software environment to ingest, align, and analyze heterogeneous time-series data. | Custom Python (Pandas, NumPy), LabKey Server, REDCap. |
| Gravimetric Validation Kit | Gold-standard for verifying injected insulin dose accuracy of pen-cap systems. | High-precision microbalance (0.1mg), controlled environment chamber. |
| BLE Protocol Analyzer | For debugging connectivity issues and reverse-engineering data streams from non-open devices. | Nordic Semiconductor nRF Sniffer, Frontline BLE Protocol Analyzer. |
| Glucose Clamp System | The reference method for quantifying the pharmacodynamic response to a logged insulin dose. | Biostator or custom clamp system using variable glucose/insulin infusion. |
Visualization: Research Workflows and Data Relationships
Data Flow in Smart Pen & CGM Coordination Research
Troubleshooting Logic for Dose Inaccuracy
Technical Support Center: Troubleshooting & FAQs
FAQ 1: During in vivo dual-hormone (Insulin & Glucagon) infusion studies, we observe exaggerated counter-regulatory responses. What could be causing this?
- Answer: This is often due to suboptimal hormone dosing ratios or timing. Glucagon's hyperglycemic effect is potent but transient. An excessive or mistimed glucagon bolus can overcorrect hypoglycemia, triggering a subsequent excessive insulin release. Consult Table 1 for refined dosing parameters. Ensure your algorithm's hypoglycemia prediction horizon is calibrated to your model's metabolic rate. Use the "Dual-Hormone Algorithm Tuning Protocol" below.
FAQ 2: In our pramlintide co-infusion experiments, we see unacceptable variability in postprandial glucose suppression. How can we improve consistency?
- Answer: Variability frequently stems from pramlintide's pharmacokinetic profile delaying gastric emptying. Inconsistent meal timing relative to infusion start is a common culprit. Standardize the pre-meal lead time (typically 30-60 minutes). Also, check the stability of your pramlintide solution; it can adhere to tubing. Use the "Pramlintide-Adjunctive Therapy Workflow" and ensure you are using a non-adsorptive infusion line. See "Research Reagent Solutions" for recommended materials.
FAQ 3: Our artificial pancreas (AP) algorithm fails to stabilize glucose in the presence of stress hormones (e.g., in a surgical model). How can we make the system more robust?
- Answer: Single-hormone (insulin-only) AP systems are inherently vulnerable to hyperglycemic stressors. This highlights the thesis context of poor coordination. Implementing a glucagon safety module that uses a separate, stricter glucose threshold during predefined "stress periods" can improve coordination. Integrate a secondary, model-predictive controller for glucagon that activates only when stress biomarkers (e.g., catecholamines) are elevated. See the "Stress-Response Signaling Pathway" diagram.
FAQ 4: We are getting inconsistent results when testing insulin-pramlintide combinations in isolated islet perfusion assays. What are the critical parameters to control?
- Answer: Focus on perfusion buffer composition and hormone sequencing. Pramlintide's primary effect is to suppress glucagon secretion; this is glucose-dependent. Ensure your perfusion switches from a low-glucose (e.g., 3mM) to high-glucose (e.g., 11mM) buffer at a precise time after pramlintide pre-perfusion. Maintain a physiological Ca²⁺ concentration (1.2-1.3mM). Follow the "Islet Perfusion Sequential Protocol" below.
Table 1: Comparative Pharmacokinetic/Pharmacodynamic Parameters for Adjunctive Therapies
| Parameter | Rapid-Acting Insulin (Aspart) | Glucagon (rDNA) | Pramlintide (Analogue) |
|---|---|---|---|
| Onset of Action | 10-20 min | ~8-10 min | ~30 min (for gastr. empty.) |
| Time to Peak | 60-90 min | ~30-40 min | ~2 hours |
| Half-life (t½) | 60-90 min | ~8-18 min | ~50 min |
| Key Mechanism | Promotes glucose uptake | Hepatic glycogenolysis & gluconeogenesis | Slows gastric emptying, suppresses glucagon |
| Typical Adj. Dose Ratio | 1.0 (Baseline) | 1:10 to 1:20 (Ins:Gluc, mcg) | 1:30 to 1:60 (Ins:Pram, mcg) |
Table 2: Algorithm Performance Metrics in Silico (UVa/Padova Simulator)
| Algorithm Type | Time in Range (70-180 mg/dL) | Hypoglycemia Events (<54 mg/dL) | Hyperglycemia Events (>250 mg/dL) |
|---|---|---|---|
| Insulin-Only AP | 78.2% ± 5.1% | 2.1 ± 0.8 | 4.5 ± 1.2 |
| Insulin+Glucagon AP | 85.7% ± 3.8% | 0.5 ± 0.3 | 3.1 ± 0.9 |
| Insulin+Pramlintide (Pre-Meal) | 91.4% ± 2.9% | 1.8 ± 0.6 | 0.9 ± 0.4 |
Experimental Protocols
Protocol 1: Dual-Hormone Algorithm Tuning (Rodent Model)
- Instrumentation: Implant vascular catheters for continuous glucose monitoring (CGM) and dual-channel infusion pump.
- Basal Calibration: Under anesthesia, establish individual basal insulin infusion rate to maintain euglycemia (100-150 mg/dL) for 30 mins.
- Glucagon Challenge: Administer a standardized insulin bolus (0.1 U/kg) to induce a controlled descent. At a glucose threshold of 100 mg/dL, test glucagon boluses from 2-20 mcg/kg. Measure time to peak glucose and magnitude of rebound.
- Algorithm Integration: Input dose-response data into a proportional-integral-derivative (PID) or model-predictive control (MPC) algorithm. Set glucagon activation 10 mg/dL above the hypoglycemic threshold defined for insulin attenuation.
- Validation: Test the tuned algorithm against a mixed-meal challenge.
Protocol 2: Islet Perfusion Sequential Protocol
- Islet Preparation: Handpick 100 size-matched murine or human islets into a perfusion chamber.
- Baseline Perfusion: Perfuse with Krebs-Ringer Bicarbonate buffer containing 3mM glucose at 37°C, 0.5 mL/min for 60 mins.
- Pramlintide Pre-treatment: Switch to buffer containing 3mM glucose + 100 pM pramlintide for 20 mins.
- Secretagogue Stimulation: Switch to high-glucose (11mM) buffer with continued 100 pM pramlintide for 40 mins. Collect effluent at 1-min intervals for insulin/glucagon ELISA.
- Control Run: Repeat steps 1-4, omitting pramlintide in steps 3 & 4.
Protocol 3: Pramlintide-Adjunctive Therapy Workflow (Pre-Meal Dosing)
- Subject Preparation: Overnight-fasted, catheterized large animal or human subject.
- CGM Calibration: Ensure CGM is YSI-calibrated.
- Pre-Meal Intervention: 30 minutes prior to a standardized mixed-meal (e.g., 0.5 g/kg carbs):
- Control Arm: Administer insulin bolus per standard carbohydrate-counting formula.
- Intervention Arm: Administer pramlintide bolus (dose per Table 1 ratio) via subcutaneous infusion, followed by a reduced insulin bolus (typically 30-50% reduction).
- Monitoring: Monitor CGM for 6 hours post-meal. Key metrics: time to glucose peak, peak amplitude, and total AUC for glucose >180 mg/dL. Collect frequent plasma samples for amylin and insulin levels.
Visualizations
Dual-Hormone Control Loop
Pramlintide Adjunctive Action Path
Stress-Induced AP Coordination Failure
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| Dual-Channel Programmable Infusion Pump (e.g., Harvard PHD ULTRA) | Allows simultaneous, independent infusion of insulin and glucagon/pramlintide with precise rate control, critical for mimicking physiological secretion patterns. |
| Non-Adsorptive Infusion Tubing (e.g., PEG-coated) | Precludes loss of peptide hormones (especially pramlintide and glucagon) via adhesion to tubing walls, ensuring accurate delivered dose. |
| Stable Glucagon Analog (e.g., Dasiglucagon) or Novel Formulation | Reduces experimental variability caused by the rapid fibrillation and degradation of native glucagon in aqueous solution. |
| Humanized In Silico Simulator (UVa/Padova T1DM Simulator) | Provides a validated platform for initial safety testing and tuning of dual-hormone algorithms prior to costly in vivo studies. |
| Specific ELISA Kits (Insulin, Glucagon, Amylin) | Essential for measuring portal-peripheral hormone gradients and confirming secretory suppression (e.g., pramlintide's effect on glucagon). |
| Hyperinsulinemic-Euglycemic Clamp Setup | Remains the gold-standard methodology to quantify changes in insulin sensitivity induced by adjunctive therapies in vivo. |
Technical Support Center: Troubleshooting & FAQs for Integrated Glucose-Insulin Research Simulations
Q1: Our multi-scale physiological model shows unrealistic oscillations in blood glucose when integrating a new subcutaneous insulin pharmacokinetic sub-model. What are the primary checks? A1: This is often a unit mismatch or time-constant disparity. Follow this protocol:
- Verify Units: Confirm all rate constants are in consistent temporal units (e.g., per minute vs. per hour). Check insulin flux units (pmol/kg/min) match glucose appearance/disappearance (mg/kg/min or mmol/kg/min).
- Scale Time Constants: Subcutaneous insulin absorption often operates on a 60-120 minute half-life, while glucose dynamics are faster. Ensure your solver (e.g., ODE15s in MATLAB, CVODE in NEURON) is configured for stiff equations. Reduce solver maximum time step to 0.1 min.
- Isolate the Sub-model: Run the new insulin PK/PD sub-model with a constant input. Output should be a smooth, non-oscillatory profile. If oscillations persist, the issue is internal to the sub-model logic.
Q2: When simulating a closed-loop insulin delivery algorithm, the in-silico clinical trial yields highly variable outcomes compared to a single patient simulation. Is this a software or modeling issue? A2: This is typically expected biological variability, but must be validated.
- Action Protocol: Run a sensitivity analysis on key parameters (e.g., insulin sensitivity, carbohydrate ratio, endogenous glucose production) using a Sobol or Latin Hypercube sampling method.
- Diagnostic Table: Compare your outcome variance to published in silico trial variance.
Table 1: Expected vs. Problematic Variance in Simulated Glucose Outcomes
| Metric | Expected Coefficient of Variation (CV) | Problematic CV | Likely Cause |
|---|---|---|---|
| Mean Blood Glucose | 5-12% | >20% | Parameter distributions are too wide/unconstrained |
| Time-in-Range (70-180 mg/dL) | 8-15% | >25% | Correlations between parameters (e.g., sensitivity & carb ratio) not correctly defined |
| Hypoglycemia Events | 15-30% | >50% | Underlying population model does not match target cohort |
Q3: Our agent-based model of pancreatic beta-cell response fails to replicate first-phase insulin secretion upon glucose challenge. How to debug? A3: This indicates a missing rapid-release mechanism or incorrect calcium dynamics.
- Experimental Protocol: a. Isolate Ion Channels: Temporarily fix cytoplasmic ATP/ADP ratio to simulate constant glucose. Check if voltage-gated calcium channels (VGCC) open correctly. b. Check Docking Pools: Implement a "readily releasable pool" (RRP) of insulin granules. The first phase requires a pre-docked, primed RRP. c. Trace Calcium: Output a time-series trace of intracellular Ca²⁺ for 10 virtual cells. A sharp spike should immediately follow membrane depolarization.
Q4: Data from our continuous glucose monitor (CGM) simulator has an unnatural, "steppy" appearance lacking physiological sensor noise. How to improve realism? A4: You are likely generating clean interstitial glucose and not applying CGM-specific artifacts.
- Solution: Post-process your simulated interstitial glucose signal with:
- Low-Pass Filtering: Apply a 5-15 minute lag to simulate diffusion delay.
- Additive White Noise: Add Gaussian noise with a standard deviation of 1-2% of the reading.
- Calibration Error: Introduce a slight, slowly drifting bias (+/- 5%) over 24-hour periods.
Q5: The co-simulation between our insulin pump firmware model (in C) and glucose model (in Python) halts unpredictably. What's the best coordination strategy? A5: This is a classic co-simulation synchronization issue. Use a dedicated middleware.
- Recommended Protocol: Implement the Functional Mock-up Interface (FMI) standard. Export each sub-system as a Functional Mock-up Unit (FMU). Use a master algorithm (e.g., in Python with
FMPyor Julia) to synchronize data exchange at fixed communication intervals (e.g., every 1 minute of simulation time). Ensure all FMUs use the same solver type recommendation.
The Scientist's Toolkit: Research Reagent Solutions for In Silico Experiments
Table 2: Essential In Silico Research Tools
| Item / Software | Function in Coordinated Glucose-Insulin Research |
|---|---|
| FMI/FMU Standard | Enables co-simulation of disparate models (e.g., device firmware + physiology) in a standardized, tool-independent way. |
| SUNDIALS (CVODE) | A robust suite of nonlinear differential/algebraic equation solvers for stiff multi-scale physiological systems. |
| Sobol.jl / SALib | Libraries for variance-based sensitivity analysis, crucial for identifying key parameters driving system coordination. |
| UVA/Padova T1D Simulator | An accepted, validated simulator of type 1 diabetes metabolism; serves as a benchmark for new model components. |
| BioFVM & PhysiCell | Frameworks for simulating pharmacokinetics/pharmacodynamics (PK/PD) and tissue-scale phenomena in 3D. |
| SBML & CellML | Model exchange languages to encode biological processes, ensuring reproducibility and interoperability. |
| Git & DVC (Data Version Control) | Version control for models, parameters, and simulation outputs, essential for collaborative, reproducible science. |
Visualizations of Key Workflows & Pathways
Title: Closed-Loop In Silico Testing Workflow
Title: In Silico Clinical Trial Protocol
Diagnosing and Resolving Coordination Failures in Clinical and Real-World Settings
Troubleshooting Guides & FAQs
Calibration Errors
Q1: Our in-house continuous glucose monitoring (CGM) sensor shows high mean absolute relative difference (MARD) >15% after two-point calibration against a reference method (YSI). What are the primary investigative steps?
A: High post-calibration error indicates fundamental sensor drift or instability. Follow this protocol:
- Verify Reference Method: Ensure the benchtop analyzer (e.g., YSI 2900) has been calibrated and maintained per manufacturer protocol. Use fresh standards.
- Check Calibration Solution Integrity: Confirm age, storage conditions, and sterility of calibration solutions. Degradation can introduce systematic bias.
- Execute a Drift Analysis Protocol:
- Immerse sensors in a stable, stirred glucose solution at 100 mg/dL (5.6 mmol/L).
- Record sensor signal every minute for 6 hours at 37°C.
- Calculate the coefficient of variation (CV) of the signal. A CV >10% indicates significant electrochemical noise or instability.
- Analyze Calibration Data Fit: Plot reference glucose (x) vs. sensor signal (y). A poor linear fit (R² < 0.9) suggests non-linear sensor response or interference.
Table 1: Common Calibration Error Sources & Diagnostic Tests
| Error Source | Diagnostic Experiment | Acceptable Metric | Typical Failure Value |
|---|---|---|---|
| Unstable Reference | Triplicate measurements of a single sample on reference analyzer. | Standard Deviation | > ±2 mg/dL (±0.1 mmol/L) |
| Sensor Signal Drift | Stable glucose bath test (6 hrs). | Signal Coefficient of Variation | > 10% |
| Poor Linearity | Two-point calibration across range (e.g., 40 & 400 mg/dL). | R-squared (R²) of fit | < 0.90 |
| Biofouling | Pre- vs. post-explant sensor sensitivity check in vitro. | Sensitivity Loss | > 15% |
Q2: During dynamic clamp studies, we observe a lag between the reference blood glucose and the subcutaneous CGM signal, confounding our algorithm testing. How can we characterize and compensate for this?
A: The physiological lag (typically 5-15 minutes) is a key coordination challenge. Use this protocol to quantify it:
- Hyperglycemic Clamp Experiment: In an animal model, rapidly elevate blood glucose via dextrose infusion.
- Synchronous Sampling: Measure arterial blood glucose (reference) and interstitial glucose (via microdialysis) every 2-5 minutes.
- Time-Series Analysis: Apply cross-correlation analysis between the reference and CGM signals. The time offset at maximum correlation is the system lag.
- Implement Compensation: Test moving-average filters or deconvolution algorithms (e.g., using a diffusion model) to align signals. Validate by comparing the time-compensated CGM trace to the reference during a separate hypoglycemic clamp.
Diagram 1: Protocol for Quantifying Physiological Glucose Monitoring Lag
Signal Dropouts
Q3: In our ambulatory animal studies, intermittent CGM signal loss occurs. How do we systematically determine if the cause is wireless telemetry or sensor failure?
A: Isolate the failure domain with this stepwise diagnostic workflow.
Diagram 2: Signal Dropout Diagnostic Decision Tree
Experimental Protocol for RF Interference Testing:
- Place the experimental subject (device implanted/attached) in a Faraday cage or anechoic chamber.
- Use a programmable signal generator to introduce controlled interference in the ISM band (e.g., 2.4 GHz).
- Monitor the telemetry receiver's Link Quality Index (LQI) or Received Signal Strength Indicator (RSSI) while systematically varying interference power.
- Correlate dropout events with LQI/RSSI thresholds and interference peaks. This confirms telemetry as the root cause.
Infusion Set Issues
Q4: During prolonged subcutaneous insulin infusion studies in rodents, we observe erratic glucose control. How can we test for infusion set failure (occlusion, leakage, tissue trauma)?
A: Infusion set failure directly disrupts the coordination of monitoring and delivery. Implement this validation protocol:
Table 2: Infusion Set Failure Modes & Detection Methods
| Failure Mode | In-Vivo Detection Method | In-Vitro Bench Test | Consequence for Research |
|---|---|---|---|
| Partial Occlusion | Rising infusion pump pressure alarm (if equipped). | Measure flow rate vs. backpressure. | Under-delivery, unexplained hyperglycemia. |
| Complete Occlusion | Pump occlusion alarm; zero flow. | Verify no flow at max pump pressure. | Complete therapy failure. |
| Catheter Leakage | Visual dye study (infuse methylene blue, dissect site). | Pressure decay test in a sealed system. | Insulin loss, variable absorption. |
| Tissue Trauma/Inflammation | Histology at infusion site (H&E stain). | N/A (in-vivo only). | Altered insulin pharmacokinetics. |
Detailed Histology Protocol for Assessing Infusion Site Reaction:
- Sample Collection: After 72 hours of infusion, euthanize subject and excise tissue surrounding catheter tip.
- Fixation: Immerse in 10% neutral buffered formalin for 24 hours.
- Sectioning: Paraffin-embed, section at 5 µm thickness.
- Staining: Hematoxylin and Eosin (H&E) stain.
- Scoring: Use a standardized scale (e.g., 0-4) to grade inflammatory cell infiltration (neutrophils, lymphocytes, macrophages) and fibrosis. Compare to a contralateral control site.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for CGM-Insulin Integration Studies
| Item | Function & Rationale |
|---|---|
| Benchtop Glucose Analyzer (e.g., YSI 2900) | Gold-standard reference for blood/plasma glucose. Essential for sensor calibration and study validation. |
| Microdialysis System | Direct sampling of interstitial fluid (ISF) to decouple sensor performance from physiological lag. |
| Programmable Syringe Pumps (Dual-Channel) | For precise, simultaneous delivery of glucose and insulin during hyper-/hypo-glycemic clamps. |
| RF Spectrum Analyzer | Diagnose telemetry dropouts by identifying environmental interference in the wireless band used. |
| Pressure Transducer (Low Range, 0-15 psi) | Integrated in-line to monitor infusion set patency and detect early occlusions. |
| Tissue Fixative (10% NBF) | Preserves infusion site architecture for histological analysis of local tissue response. |
| Fluoroscopic Tracer (e.g., Iohexol) | Mixed with insulin to visualize infusion depot formation and leakage using real-time imaging. |
Troubleshooting Guide & FAQs
This support center addresses common challenges in parameterizing personalization algorithms for metabolic research, specifically within the context of improving coordination between continuous glucose monitoring (CGM) and insulin delivery systems.
FAQs: Algorithm Development & Experimental Issues
Q1: During simulation of a personalized insulin dosing algorithm, my model shows persistent hyperglycemia despite adjusting the insulin sensitivity factor (ISF). What are the primary parameters to check? A: This often indicates a misalignment between the algorithm's aggressiveness and the patient's physiological dynamics. Check the following core parameters in order:
- Basal Rate Profile: Ensure the underlying basal insulin rate is correctly calibrated for the patient's diurnal needs.
- Carbohydrate-to-Insulin Ratio (CIR): An incorrect CIR will cause postprandial glucose excursions that the corrective (ISF) logic cannot manage efficiently.
- Algorithm's Target Glucose Range: An overly high target (e.g., 150 mg/dL) will reduce corrective actions.
- Time-of-Day Parameters: Verify that ISF and CIR are properly segmented for dawn phenomenon or evening sensitivity.
Table 1: Key Algorithm Parameters for Glycemic Control
| Parameter | Typical Range | Function | Effect if Too High | Effect if Too Low |
|---|---|---|---|---|
| Insulin Sensitivity Factor (ISF) | 15 - 100 mg/dL per unit | Estimates BG drop per unit of insulin. | Risk of hypoglycemia from corrections. | Inadequate correction, persistent hyperglycemia. |
| Carb-to-Insulin Ratio (CIR) | 5 - 30 g per unit | Determins meal bolus size. | Postprandial hyperglycemia. | Postprandial hypoglycemia. |
| Basal Rate | 0.2 - 2.0 U/hr | Provides background insulin. | Nocturnal/fasting hypoglycemia. | Fasting hyperglycemia. |
| Algorithm Target BG | 100 - 130 mg/dL | Desired setpoint for control logic. | Increased time in hyperglycemia. | Increased risk of hypoglycemia. |
Q2: My in-silico experiments yield good results, but validation on a small animal model shows delayed response and oscillation. What experimental protocols should I review? A: This discrepancy points to a mismatch between simulation assumptions and biological reality. Follow this validation protocol:
Experimental Protocol: Translational Validation of Personalization Parameters
- Pre-Experiment Calibration: Synchronize all timestamps between the CGM system, insulin pump, and any manual measurement devices.
- Parameter Priming: In the animal model, establish a 48-hour baseline with standard parameters while collecting CGM and insulin delivery data.
- Staged Intervention: Implement the new personalized parameters in a controlled, step-wise manner (e.g., adjust only ISF first, observe for 24h, then adjust CIR).
- Data Collection: Record CGM traces, insulin delivery logs, body weight, activity, and food intake. Critical: Manually measure blood glucose via tail vein sampling at least 3 times daily to calibrate and validate CGM sensor readings.
- Analysis Metric: Use Glucose Management Indicator (GMI), Time-in-Range (70-180 mg/dL), and Coefficient of Variation (%CV) for comparison. Do not rely on average glucose alone.
Title: In-silico to Animal Model Validation Workflow
Q3: When analyzing CGM and insulin pump data logs to derive personalization parameters, the signal-to-noise ratio is poor. How can I preprocess this data effectively? A: Raw device data requires robust preprocessing. Implement this methodology:
Data Preprocessing Protocol for Device Logs
- Temporal Alignment: Resample CGM (e.g., every 5 min) and insulin data (every 5 min) to a common uniform time grid.
- CGM Smoothing: Apply a Savitzky-Golay filter (window: 5-7 points, polynomial order: 2) to reduce high-frequency noise without significant lag.
- Insulin On-Board (IOB) Calculation: Use a validated insulin action curve (e.g., 6-hour exponential decay) to calculate active insulin at any time point.
- Artifact Removal: Identify and interpolate (linear) CGM gaps <20 minutes. Flag longer gaps for exclusion.
- Meal & Event Annotation: Log all nutritional intake (carbs estimated) and exercise events with timestamps.
Table 2: Quantitative Impact of Data Preprocessing Steps
| Processing Step | Key Metric Before | Key Metric After | Tool/Algorithm | Purpose |
|---|---|---|---|---|
| CGM Smoothing | %CV = 25% | %CV = 18% | Savitzky-Golay Filter | Reduces sensor noise for accurate trend analysis. |
| IOB Calculation | N/A | Active IOB (Units) | Exponential Decay Model (τ=360 min) | Prevents insulin stacking in parameter estimation. |
| Temporal Alignment | Data points mismatch: ~15% | Mismatch: 0% | Linear Interpolation & Resampling | Enables correct cross-correlation of glucose and insulin signals. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Personalized Algorithm Research
| Item | Function in Research | Example/Supplier |
|---|---|---|
| Research-Grade CGM System | Provides high-frequency interstitial glucose data for algorithm training and validation. | Dexcom G6 Pro, Medtronic iPro3. |
| Programmable Insulin Pump | Allows precise delivery and logging of insulin basals and boluses per experimental protocols. | Insulet Omnipod DASH (Research Kit), Sooil Dana. |
| Glucose Oxidase Assay Kit | Gold-standard for manual blood glucose measurement to calibrate and verify CGM accuracy. | Sigma-Aldrich Glucose (GO) Assay Kit. |
| Data Fusion & Analysis Platform | Software for merging CGM, insulin, and meal data; implementing and testing algorithms. | Tidepool, OpenAPS, custom Python/R pipelines. |
| Animal Metabolic Cage System | Controlled environment for rodent studies to monitor food/water intake, activity, and excretion. | TSE Systems, Columbus Instruments. |
Q4: The signaling pathways involved in the glucose-insulin feedback loop are complex. Can you diagram the key pathway relevant to sensor-measured interstitial glucose? A: Yes. The primary pathway linking blood glucose to interstitial fluid (ISF) measurement is one of passive diffusion, not active signaling. However, the core physiological feedback loop is critical for algorithm design.
Title: Glucose-Insulin Feedback & CGM Measurement Pathway
Technical Support & Troubleshooting Center
This center provides support for common experimental challenges in predictive algorithm development and the assessment of novel speed-acting insulin analogs, within the context of research into glucose monitoring and insulin injection coordination.
Frequently Asked Questions (FAQs)
Q1: Our in-silico predictive model performs well on training data but fails to generalize to new animal study data. What are the primary troubleshooting steps? A: This typically indicates overfitting or a dataset shift. Follow this protocol:
- Data Audit: Compare the statistical distributions (mean, variance, range) of the input features (e.g., CGM values, insulin-on-board, meal announcement timing) between your training set and the new experimental data.
- Feature Importance Re-evaluation: Use SHAP or permutation importance on the new data to see if key predictors have changed.
- Algorithm Adjustment: Increase regularization parameters (e.g., L1/L2 for neural networks, prune decision trees). Simplify the model architecture.
- Re-train with Augmented Data: If the new data is limited, use synthetic minority oversampling (SMOTE) or add realistic noise (e.g., CGM measurement error, timing jitter) to your training set.
Q2: During closed-loop in vivo experiments, we observe persistent postprandial hyperglycemia despite using a predictive feedforward algorithm. What could be the cause? A: This points to a mismatch between the predicted insulin requirement and the pharmacokinetic/pharmacodynamic (PK/PD) profile of the insulin used.
- Check Algorithm Output: Verify that the predictive horizon of your algorithm aligns with the time-to-peak action of your insulin. A horizon that is too short will not pre-empt the glucose rise sufficiently.
- Calibrate Insulin Action Model: The PK/PD model used in your controller (e.g., a 3-compartment model) may have incorrect parameters for the specific insulin batch or species. Re-fit the model using data from a euglycemic clamp study.
- Assess Meal Absorption Model: The problem may not be the insulin delay but an inaccurate model of glucose appearance from the gut. Review and calibrate your meal absorption model parameters.
Q3: When testing a novel speed-acting insulin analog, how do we quantitatively differentiate its action profile from a standard rapid-acting analog (e.g., insulin aspart)? A: Conduct a standardized euglycemic glucose clamp study and compare key PK/PD metrics.
Table 1: Key Pharmacokinetic/Pharmacodynamic Metrics for Insulin Comparison
| Metric | Definition | Measurement Method |
|---|---|---|
| Tonset | Time to initial significant glucose infusion rate (GIR) increase. | Time when GIR > 0.2 mg/kg/min above baseline. |
| Tmax,GIR | Time to maximum glucose infusion rate. | Time of peak GIR value post-injection. |
| GIRmax | Maximum glucose infusion rate. | Peak value of the GIR curve (mg/kg/min). |
| Tearly,50% | Time to reach 50% of total GIR AUC in the first 2 hours. | Indicates speed of early action. |
| Total AUCGIR | Total area under the GIR curve. | Represents overall metabolic effect. |
Q4: Our sensor signal processing pipeline introduces an unacceptable latency (>5 minutes). How can we reduce this delay without compromising noise filtering? A: Implement a hybrid filtering approach.
- Layer 1 (Causal FIR Filter): Apply a short, causal finite impulse response (FIR) filter for minimal real-time smoothing.
- Layer 2 (Forward Prediction): Feed the filtered signal into a Kalman Filter or a simple linear extrapolation model (e.g., ARIMA) to predict glucose values 5-10 minutes ahead.
- Protocol: Compare the noise standard deviation and mean absolute relative difference (MARD) against a trusted reference dataset (e.g., YSI blood glucose) for both raw, filtered, and predicted signals to validate.
Experimental Protocols
Protocol 1: In-Vitro Assessment of Insulin Dissociation Kinetics Purpose: To quantify the self-association state (hexamer → dimer → monomer) dissociation rate of novel insulin analogs, a primary determinant of speed of absorption. Method:
- Sample Preparation: Prepare solutions of test insulin and control (e.g., insulin lispro) at a concentration of 0.6 mg/mL in a pH 7.4 buffer.
- Fluorescence Quenching: Use a stopped-flow apparatus to rapidly mix the insulin solution with a fluorescence-quenching agent (e.g., acrylamide).
- Data Acquisition: Monitor the time-resolved fluorescence quenching curve. The rate of quenching increase correlates with the rate of monomer exposure.
- Analysis: Fit the quenching curve to a multi-exponential decay model to derive rate constants for the dissociation steps.
Protocol 2: Evaluating Predictive Algorithm in a Simulated Environment Purpose: To benchmark a new predictive algorithm (e.g., LSTM network) against a standard method (e.g., ARIMA) before animal trials. Method:
- Simulator: Use the FDA-approved UVA/Padova T1D Simulator or the Cambridge Simulator.
- Scenario Design: Simulate a cohort of 10 virtual adults with T1D over 3 days. Include challenging scenarios: unannounced meals, missed boluses, and sensor dropouts.
- Controller: Implement a standardized MPC controller. Swap only the glucose prediction module between the candidate algorithms.
- Outcome Metrics: Compare % Time in Range (70-180 mg/dL), % Time Below Range (<70 mg/dL), and prediction error (RMSE) for a 30-minute horizon.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Sensor-Actuator Delay Research
| Item | Function & Rationale |
|---|---|
| FDA-Accepted T1D Simulator (e.g., UVA/Padova) | Provides a validated in-silico platform for safe, initial algorithm development and hypothesis testing. |
| Programmable Insulin Pumps (Research Grade) | Allows precise, automated delivery of insulin boluses and basals as commanded by research controllers during in vivo studies. |
| Continuous Glucose Monitor (CGM) Dev Kits | Provides raw sensor data streams and access to calibration routines, enabling low-latency signal processing development. |
| Euglycemic Glucose Clamp System | The gold-standard method for quantifying the PK/PD profile of insulin analogs in human or animal studies. |
| Stopped-Flow Spectrofluorometer | Enables measurement of ultra-fast kinetic processes (milliseconds), such as insulin monomer formation. |
| Novel Speed-Acting Insulin Candidates (e.g., with excipients like treprostinil) | Experimental compounds that modify subcutaneous tissue perfusion or dissociation kinetics to reduce actuation delay. |
Visualizations
Title: Closed-Loop System with Predictive Compensation for Delays
Title: Pathway from Insulin Injection to Glucose Uptake
Troubleshooting Guide: Frequently Asked Questions (FAQ)
Q1: When trying to merge continuous glucose monitoring (CGM) time-series data with insulin injection logs from different devices, I encounter constant timestamp misalignment and format mismatches. What is the primary technical issue and how can I resolve it? A: The core issue is a lack of standardized temporal semantics and synchronization protocols across devices. CGM devices often use relative timestamps from sensor activation, while insulin pumps/pens may use absolute device system time. Resolve this by:
- Identify the Master Clock: Designate one device's clock as the reference (e.g., a study smartphone app logging both events) and document its synchronization with UTC.
- Extract Raw Metadata: Use vendor-provided API tools (e.g., Dexcom Clarity, Medtronic CareLink) to extract both the event timestamp and the device's reported internal clock time at extraction.
- Apply Offset Correction: Calculate the systematic offset between the device clock and the master reference for each data export session. Apply this correction to all timestamps from that device before merging.
- Standardize Format: Convert all corrected timestamps to ISO 8601 format (YYYY-MM-DDTHH:MM:SSZ) in a coordinated universal time (UTC) timezone before integration into a central database.
Q2: My merged dataset shows anomalous physiological responses (e.g., hypoglycemia immediately following insulin injection). I suspect a data linkage error where an insulin bolus is assigned to the wrong participant. How can I systematically debug this? A: This indicates a potential break in data provenance or a participant ID mapping failure. Implement this debugging protocol:
- Audit Trail Verification: Check the raw source files for unique device serial numbers. Create a cross-reference table linking
Study_Participant_IDtoDevice_Serial_Numberfor both CGM and insulin delivery devices. - Temporal-Spatial Plausibility Check: Flag any insulin event that does not have a CGM reading from the same participant's sensor within a physiologically plausible preceding window (e.g., 5-15 minutes). Use this query:
- Statistical Outlier Detection: For each participant, calculate the mean and standard deviation of the time-to-glucose-nadir post-bolus. Flag events where the observed response is >3 SDs from that participant's mean, then manually verify against source logs.
Experimental Protocol for PK/PD Bridging:
- Controlled Crossover Study: Administer a standardized insulin dose (e.g., 0.1 IU/kg) via each delivery system (pump A, pump B, pen) in a controlled clinical setting.
- High-Frequency Sampling: Collect venous blood samples at baseline, 5, 15, 30, 45, 60, 90, 120, 180, and 240 minutes post-injection.
- Assay Analysis: Quantify serum insulin concentration using a validated chemiluminescent or ELISA immunoassay (kit details in Reagent Table).
- Non-Compartmental Analysis (NCA): For each delivery system, calculate key PK parameters:
Cmax(peak concentration),Tmax(time to peak), andAUC_0-t(area under the concentration-time curve). - System-Specific Conversion Factor: Derive a dose-normalized
AUCfor each system. The ratio of theseAUCs provides a system-specific conversion multiplier to translate an administered IU from one device into "effective exposure" relative to another.
Table 1: Pharmacokinetic Parameters from a Hypothetical Bridging Study
| Delivery System | Dose Administered (IU) | Mean Cmax (µIU/ml) | Mean Tmax (min) | AUC_0-240min (µIU/ml*min) | Dose-Normalized AUC (per IU) |
|---|---|---|---|---|---|
| Insulin Pump A | 10.0 | 125.6 | 45 | 15,840 | 1,584 |
| Insulin Pump B | 10.0 | 118.2 | 55 | 14,320 | 1,432 |
| Insulin Pen | 10.0 | 141.5 | 35 | 16,950 | 1,695 |
Q4: Interoperability between my lab's assay data repository (REDCap) and the clinical CGM warehouse (OMOP CDM) fails due to incompatible semantic vocabularies (LOINC vs. SNOMED-CT). What's a sustainable solution? A: Implement a local ontology mapping service using a common intermediary standard.
- Create a Bridge Table: Do not attempt to map all codes. Create a focused Study Phenotype Bridge Table that maps the 20-30 key concepts you need (e.g., "serum insulin," "capillary glucose").
- Leverage Unified Medical Language System (UMLS): Use the UMLS Metathesaurus to find the Concept Unique Identifier (CUI) common to both your LOINC and SNOMED-CT codes.
- Tool Implementation: Use an API-based tool like the OHDSI Usagi or the Bioportal Annotator to semi-automate and audit this mapping process. Store the validated mappings (
Local_Concept<->UMLS_CUI<->Target_Code) in a version-controlled lookup table for all data transformation pipelines.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Insulin-Glucose Integration Studies
| Item Name & Vendor (Example) | Function in Research Context |
|---|---|
| Human Insulin Specific ELISA Kit (ALPCO) | Quantifies human insulin concentration in serum/plasma for PK studies, critical for establishing dose-exposure relationships across delivery devices. |
| Stable Isotope-Labeled Glucose Tracer (Cambridge Isotopes) | Enables precise measurement of glucose kinetics (Ra, Rd) via GC-MS, disentangling endogenous production from exogenous effects of insulin. |
| Multiplex Cytokine Panel (Milliplex, Merck) | Measures inflammatory markers (IL-6, TNF-α) to assess potential injection site reactions that may confound insulin absorption data. |
| Glycated Hemoglobin (HbA1c) Control Set (Bio-Rad) | Provides quality control for long-term glycemic measure assays, ensuring longitudinal data integrity in multi-study integrations. |
| Data Integration Platform (e.g., Tresor, RENCI) | A software platform designed for biomedical data fusion, providing tools for semantic annotation, temporal alignment, and provenance tracking. |
Visualizations
Diagram 1: Data Interoperability Pipeline for Insulin-Glucose Research
Diagram 2: Pharmacokinetic Bridging Study Workflow
Troubleshooting & FAQ Center
Q1: During a continuous glucose monitor (CGM) and insulin pump closed-loop simulation, my in-vitro data shows erratic insulin adsorption to the experimental vessel. What could be causing this?
A: This is a common issue when polymeric materials from catheters or reservoir bags interact with insulin formulations. Recent studies (2024) indicate that polysorbate degradation or silicone oil leaching can create nucleation sites, causing insulin aggregation and surface adsorption.
Troubleshooting Protocol:
- Material Pre-treatment: Soak all fluid-contact components (tubing, reservoir bags) in a 1% bovine serum albumin (BSA) solution for 60 minutes at 37°C. Rinse three times with your assay buffer.
- Additive Screening: Include non-ionic surfactants in your insulin solution (e.g., 0.01% polysorbate 20 or 80). Note: Perform a stability assay first, as some surfactants can accelerate deamidation.
- Quantitative Assessment: Use the following protocol to measure adsorption loss:
- Prepare a control insulin solution (Icontrol).
- Circulate the solution through your experimental flow system for 4 hours at 37°C.
- Collect the output solution (Ioutput).
- Measure concentration via HPLC-UV (detection at 214 nm) or a validated ELISA.
- Calculate % Adsorption = [(Icontrol - Ioutput) / I_control] * 100.
Q2: Our high-throughput screening assay for novel insulin analogs is plagued by high variability in glucose uptake readings between plates. How can we normalize this?
A: Inter-plate variability often stems from inconsistent cell seeding density or lactate/pH buildup in microplates. A dual-normalization strategy is recommended.
Normalization Workflow Protocol:
- Intra-Plate Control: On every 96-well plate, include:
- Column 1: Negative control (cells + buffer only).
- Column 12: Positive control (cells + 100 nM standard insulin).
- Dye-Based Normalization: Following the glucose uptake assay, lyse cells and quantify total protein per well using a Coomassie-based dye. Use this value for primary normalization.
- Inter-Plate Normalization: Calculate the fold-change of your positive control (Column 12) against the plate median positive control from your entire experiment run. Apply this correction factor to all wells on that plate.
Key Performance Data (Representative 2024 Study):
Table 1: Impact of Normalization Strategies on Assay Variability (CV%)
| Normalization Method | Intra-Plate CV% | Inter-Plate CV% | Z'-Factor |
|---|---|---|---|
| None (Raw OD) | 18.5 | 25.2 | 0.12 |
| Single-Point Control | 12.1 | 18.7 | 0.35 |
| Dual (Protein + Control) | 6.8 | 8.3 | 0.72 |
Q3: When co-culturing pancreatic islet cells with hepatocytes to model cross-talk, how do we accurately sample medium for both glucagon and insulin without depleting volume?
A: Implement a staggered, multi-analyte micro-sampling protocol using a dedicated, low-dead-volume micro-sampler.
Micro-Sampling Protocol:
- Setup: Use a 24-well plate with a 1.5 mL working volume. Prime the sampling system with assay medium.
- Schedule:
- T=0 min (Baseline): Extract 60 µL aliquot. Split into two 30 µL low-protein-binding tubes.
- T=30, 60, 120 min: Repeat extraction.
- Processing: Immediately spike one tube with aprotinin (for insulin/glucagon ELISA) and the other with sodium fluoride (for glucose assay). Centrifuge and store at -80°C. This consumes <15% of total medium, preventing significant depletion.
Q4: The signaling pathway for our novel insulin analog appears inconsistent with the canonical IRS-1/PI3K/AKT pathway. How should we map this?
A: Employ a phospho-specific multiplex immunoassay (e.g., Luminex xMAP) followed by validation via western blot. Focus on nodes beyond the canonical pathway.
Detailed Signaling Mapping Protocol:
- Stimulation: Serum-starve differentiated HepG2 or 3T3-L1 adipocytes for 6 hours. Stimulate with 10 nM reference insulin vs. novel analog for 0, 5, 15, and 30 minutes.
- Lysis: Use a magnetic bead-based phospho-protein lysis kit to preserve labile modifications.
- Screening: Run lysates on a pre-configured "Metabolic Signaling" 10-plex panel (typically includes p-IRS-1[Ser636/639], p-AKT[Thr308], p-AKT[Ser473], p-AS160, p-mTOR, p-ERK1/2, p-JNK, p-STAT3, p-AMPK).
- Validation: For any phospho-target showing >2x differential response, confirm via western blot using cell lysates from an independent experiment.
Title: Insulin Signaling & Non-Canonical Pathway Nodes
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Coordinated Glucose-Insulin Research
| Reagent/Material | Function & Rationale |
|---|---|
| Low-Protein-Binding Microtubes (e.g., PCR tubes) | Minimizes adsorption loss of low-concentration insulin/glucagon during sampling and storage. |
| Polymeric Additive Kits (Polysorbate 20/80, BSA) | Used to pre-coat fluidic systems and stabilize protein formulations, preventing surface adsorption. |
| Phospho-Specific Magnetic Bead Lysis Buffer | Enables rapid, simultaneous extraction of labile phosphorylated proteins from multiple cell types for pathway analysis. |
| Multiplex Phospho-Protein Immunoassay Panels (10-plex) | Allows high-throughput, quantitative comparison of canonical and non-canonical signaling nodes from a single microsample. |
| CGM Sensor & Insulin Pump Simulator (in-vitro flow system) | Bioreactor system with programmable flow profiles to test device-material compatibility and hormone stability under physiological shear. |
| Dual-Glow Luciferase Reporter (e.g., for FOXO1 activity) | Provides a transcriptional readout of insulin pathway activity downstream of AKT, complementing phospho-protein data. |
| Hepatocyte & Beta-Cell Co-culture Inserts | Permeable supports enabling paracrine communication modeling between key metabolic tissues without direct cell mixing. |
Benchmarking Progress: Validation Frameworks and Comparative Analysis of Integrated Systems
Regulatory and Clinical Validation Pathways for Coordinated Systems (FDA, CE Mark)
Troubleshooting Guides and FAQs
Q1: Our closed-loop glucose control system shows unexpected insulin delivery delays during in-vitro testing, potentially breaking the feedback loop. What are the key hardware/software checkpoints? A: First, isolate the delay component. For the Infusion Pump Driver Test, measure the time from controller signal to plunger movement using a high-speed camera (≥1000 fps). Calibrate per Table 1. For the Sensor Data Latency Test, stream raw sensor data and timestamp each packet. A delay >5 minutes invalidates most predictive algorithms. Check CE-marked devices for declared latency in their technical file under Annex I MDD/MDR.
Q2: When preparing an Integrated CGM-Insulin Pump System for a pre-submission meeting with the FDA, what specific interoperability data is required? A: The FDA’s Digital Health Center of Excellence emphasizes interoperability as a design objective. Prepare data per Table 2. Focus on failure mode and effects analysis (FMEA) for loss of communication scenarios. Document all wireless co-exposure testing (e.g., with smartphones per IEC 60601-1-2).
Q3: Our algorithm for coordinating monitoring and delivery shows strong simulation performance but fails in animal models. What physiological validations are we missing? A: This indicates poor translation of in-silico models. Implement the Physiological Lag Validation Protocol below. Key missed factors are often interstitial fluid glucose kinetics and insulin pharmacodynamics.
Experimental Protocol: Physiological Lag Validation for Coordinated Systems Objective: Quantify real-world time lags between blood glucose (BG), interstitial fluid glucose (ISF), and insulin action. Materials: See "Research Reagent Solutions" table. Method:
- Animal Preparation: Use chronically catheterized diabetic swine model (n≥6). Maintain anesthesia per IACUC protocol.
- Simultaneous Sampling: At t=0, inject IV insulin bolus (0.1 U/kg).
- Blood Sampling: Draw arterial blood every 2 min for 60 min for BG assay (reference method: YSI 2300 STAT Plus).
- ISF Sampling: Use subcutaneous microdialysis probes in contralateral side. Collect dialysate every 5 min for 60 min. Analyze glucose via biosensor.
- Data Analysis: Plot BG vs. ISF glucose. Calculate cross-correlation to determine time lag. Fit insulin action profile using a two-compartment model (Bergman minimal model). Expected Outcome: ISF lag typically 5-15 minutes. Algorithm recalibration is required if simulated lag was <5 min.
Q4: How do the clinical trial requirements for a "coordinated system" differ between FDA PMA and CE Mark under MDR? A: The pathways are diverging. See Table 3 for a structured comparison. Under EU MDR, the coordinated system is evaluated as a whole, while FDA may evaluate components and the integrated system separately.
Data Tables
Table 1: In-Vitro Pump Delay Calibration Bench Test Results
| Test Metric | Target Specification | Typical Pass Range | Failure Action |
|---|---|---|---|
| Signal-to-Mechanical Start | < 2 sec | 1.0 - 1.8 sec | Check motor driver firmware |
| Bolus Delivery Completion (1U) | Within ±5% of commanded dose | ±2-4% | Recalibrate stepper motor steps/U |
| Communication Drop-out Recovery | < 10 sec | 3 - 7 sec | Review RF module/antenna placement |
Table 2: Interoperability Data for FDA Pre-Submission
| Data Type | Format | Standard/Guidance | Purpose |
|---|---|---|---|
| System Hazard Analysis | FMEA Table | ISO 14971:2019 | Risk management file |
| Wireless Co-existence Test Report | PDF (Summary) | ANSI C63.27 | Demonstrates safety in intended RF environment |
| Algorithm Change Protocol | Controlled Document | FDA AI/ML SaMD Action Plan | For future updates post-market |
| Clinical Agreement Study (vs. Reference) | Bland-Altman Plots | ISO 15197:2013 | Sensor accuracy in coordinated loop |
Table 3: FDA vs. CE Mark Clinical Evidence Comparison
| Requirement | FDA (PMA Pathway) | CE Mark (EU MDR 2017/745) |
|---|---|---|
| Primary Clinical Study | Pivotal trial with primary effectiveness endpoint (e.g., Time In Range). Often randomized controlled. | Clinical investigation confirming safety, performance, and benefit-risk. May be single-arm. |
| Sample Size | Statistically powered to show superiority or non-inferiority. Often 100+ subjects. | Sufficient to characterize performance and risks. May be smaller. |
| Duration | Typically 3-6 months for key endpoints. | Must be adequate for benefit-risk assessment. Often shorter. |
| Comparator | Often standard of care (e.g., sensor-augmented pump). | May be performance goal or historical control. |
| Post-Market Study | Frequently required as a condition of approval (522 order). | Post-market clinical follow-up (PMCF) plan is mandatory. |
Diagrams
Title: FDA vs CE Regulatory Pathway Flow
Title: Coordinated System Signal & Lag Pathway
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Coordination Research | Example/Model |
|---|---|---|
| Artificial Pancreas Simulator | In-silico testing of control algorithms against virtual patient populations. | UVA/Padova T1D Simulator (FDA Accepted) |
| Reference Blood Glucose Analyzer | Gold-standard measurement for CGM calibration and lag studies. | YSI 2300 STAT Plus Analyzer |
| Subcutaneous Microdialysis System | Direct sampling of interstitial fluid for glucose kinetics research. | CMA 107 / mDialysis |
| Programmable Insulin Pump Testbed | Allows direct software control for infusion timing/delay experiments. | Modified commercial pump with research interface |
| Wireless Protocol Analyzer | Debugs communication packets between CGM, pump, and controller. | Nordic nRF Sniffer, Wireshark |
| Glycated Albumin (GA) Assay Kit | Medium-term glycemic control marker unaffected by acute changes. | Lucica GA-L Kit (Asahi Kasei) |
| Continuous Glucose Monitor (Research Use) | Provides raw current/data streams for algorithm development. | Dexcom G6 Professional, Abbott Libre Pro |
| Insulin Analog Tracers | Allows tracking of subcutaneous insulin pharmacokinetics. | Fluorescently-labeled Insulin (e.g., Insulin-Alexa Fluor) |
Technical Support Center: Troubleshooting & FAQs
FAQ 1: Inconsistent Correlation Between Time in Range (TIR) and LBGI/HBGI in Clinical Trial Analysis
- Q: During our analysis of a continuous glucose monitoring (CGM) dataset, we observe a therapy that improves Time in Range (TIR, 70-180 mg/dL) but the Low Blood Glucose Index (LBGI) remains unchanged or worsens. What could be the cause and how should we troubleshoot?
- A: This discrepancy highlights a key limitation of TIR as a standalone metric. TIR is a "flat" measure within its bounds—it does not weight the severity or frequency of hypoglycemic events. LBGI, however, is specifically designed to be sensitive to both the frequency and extent of low glucose readings.
- Troubleshooting Guide:
- Drill down into the glucose distribution: Generate a full Ambulatory Glucose Profile (AGP) report. Look specifically at the left tail (below 70 mg/dL). The improvement in TIR may be driven by reducing hyperglycemia (values >180 mg/dL), while hypoglycemic events persist.
- Segregate data by time of day: Calculate LBGI for nocturnal periods separately. Nocturnal hypoglycemia, even if brief, can significantly impact LBGI while having a minor effect on 24-hour TIR.
- Check for data censoring: Ensure your CGM system's algorithm does not excessively smooth or censor low glucose values, as this can artificially depress LBGI calculations. Refer to the device's raw data specification.
- Actionable Protocol: Re-calculate metrics on a subject-level basis, not just at the cohort level. Identify the subset of participants whose LBGI increased despite cohort TIR improvement. Analyze their individual glucose traces for patterns.
FAQ 2: Integrating User Reported Outcomes (UROs) with Physiological Metrics
- Q: We are designing a study to evaluate a new insulin formulation. How do we quantitatively align subjective User Reported Outcomes (UROs), like hypoglycemia fear or treatment satisfaction surveys, with objective metrics like HBGI and TIR? The correlation seems weak.
- A: Weak correlation is expected and reflects the thesis problem of coordination failure. UROs measure the experience of disease management, which is influenced by factors beyond glucose values (e.g., injection pain, device burden, psychological state).
- Troubleshooting Guide:
- Temporal alignment failure: A common error is correlating a URO score from a monthly survey with average TIR from the same month. Hypoglycemic fear may spike after a single severe event and then decay.
- Protocol for Enhanced Correlation: Implement Ecological Momentary Assessment (EMA). Prompt participants to complete a brief digital survey on their smartphone immediately after a prespecified event (e.g., a CGM reading below 70 mg/dL or a self-treated hypo symptom). Correlate these instantaneous UROs with the concurrent LBGI value and the preceding 1-hour TIR.
- Analyze discordance as an outcome: Instead of forcing correlation, treat the gap between high TIR and low treatment satisfaction as a primary endpoint. Use qualitative interviews to investigate the causes (e.g., regimen complexity).
FAQ 3: Calculating and Interpreting LBGI/HBGI from Sparse Fingerstick Data
- Q: Our legacy trial data only contains 7-point self-monitored blood glucose (SMBG) profiles. Are LBGI/HBGI calculations valid, and how do they compare to CGM-derived indices?
- A: LBGI/HBGI were originally developed for SMBG data and are valid. However, they will inherently differ from CGM-derived indices due to sampling frequency and lack of nocturnal data.
- Troubleshooting Guide:
- Standardized Calculation Protocol:
- Transform each BG value using:
f(BG) = 1.509 * [ (ln(BG)^1.084) - 5.381 ]. - Assign a risk value:
r(BG) = 10 * f(BG)^2iff(BG) < 0, otherwiser(BG) = 0for LBGI. Reverse for HBGI. - LBGI = mean of
r_low(BG)values across all readings. HBGI = mean ofr_high(BG).
- Transform each BG value using:
- Interpretation Caveat: SMBG-based indices are biased towards daytime glucose and may miss nocturnal hypoglycemia. Clearly label all derived metrics as "SMBG-LBGI" or "CGM-LBGI." Do not pool them in meta-analyses without statistical adjustment.
- Standardized Calculation Protocol:
Table 1: Comparison of Key Glycemic Metrics
| Metric | Definition (Typical) | Optimal Target (Consensus) | Data Input Required | Sensitivity To | Limitation |
|---|---|---|---|---|---|
| Time in Range (TIR) | % of readings/time 70-180 mg/dL | >70% for many populations | CGM preferred; SMBG (less accurate) | Broad glycemic control | "Flat" measure; ignores extremes |
| Low BG Index (LBGI) | Quantifies frequency & extent of low values | <3.5 (Low Risk) | CGM or SMBG readings | Hypoglycemia, especially recurrence | Requires transformation; less intuitive |
| High BG Index (HBGI) | Quantifies frequency & extent of high values | <5.0 (Low Risk) | CGM or SMBG readings | Hyperglycemia | Requires transformation; less intuitive |
| User Reported Outcomes (UROs) | Standardized survey scores (e.g., DTSQ, HFS-II) | Higher satisfaction, lower fear | Patient questionnaires | Treatment burden, fear, QoL | Subjective; can be non-linear |
Table 2: Example Scenario Analysis: Metric Discordance
| Participant | TIR (%) | LBGI | HBGI | Hypo Fear Survey (HFS-II) Score | Likely Interpretation |
|---|---|---|---|---|---|
| A | 85 | 1.2 (Low) | 4.5 (Low) | 15 (Low) | Well-controlled, minimal burden. |
| B | 80 | 5.8 (High) | 6.0 (Med) | 45 (High) | Troubleshooting Flag: Frequent/strong lows despite good TIR; high fear. |
| C | 65 | 2.0 (Low) | 9.5 (High) | 30 (Med) | Persistent hyperglycemia; lows managed. |
Experimental Protocol: Integrated Metric Validation Study
Title: Protocol for Correlating CGM-Derived Glycemic Indices with Ecological Momentary UROs.
Objective: To investigate the real-time relationship between physiological glucose events (hypo/hyperglycemia) and patient-reported experiences.
Methodology:
- Participants: n=50 Adults with T1D on multiple daily injections (MDI).
- Device Deployment: Participants wear a blinded CGM (e.g., Dexcom G7, Abbott Libre 3) and use a dedicated smartphone app for 14 days.
- CGM Data Collection: Raw glucose values collected every 5 minutes. Compute daily TIR, LBGI, HBGI.
- URO Data Collection via EMA: The smartphone app triggers a prompt:
- Event-Based: Within 5 minutes of a CGM reading ≤70 mg/dL (hypo) or ≥250 mg/dL (hyper).
- Random: 3 random times per day.
- Survey: 4-item questionnaire: Current anxiety (1-7), physical sensation (1-7), ability to concentrate (1-7), and "Did you treat this?" (Y/N).
- Data Alignment: Time-stamp EMA responses and align with CGM trace for the preceding 60 minutes and following 120 minutes.
- Analysis: Use mixed-effects models to predict URO scores based on LBGI/HBGI calculated from the preceding 1-hour window, controlling for time of day.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Research Context |
|---|---|
| Validated CGM System (e.g., Dexcom G7 Pro, Medtronic Guardian 4) | Provides raw, unabridged glucose data streams at 1-5 minute intervals for calculating TIR, LBGI, and HBGI. Essential for high-resolution glycemic phenotyping. |
| EMA Platform (e.g., mEMA, MetricWire, custom REDCap survey) | Enables real-time, context-aware collection of User Reported Outcomes, critical for linking physiological events to patient experience. |
| Blood Glucose Risk Function Calculator (Open Source Code) | Standardized script (in R or Python) to compute LBGI/HBGI from timestamped glucose data, ensuring reproducibility across research teams. |
| Glycemic Variability Suite (e.g., GlyCulator, EasyGV) | Software packages that aggregate standard metrics (TIR, LBGI/HBGI, CV, MAGE) from CGM/SMBG data, facilitating cohort-level analysis. |
| DTSQ & HFS-II Licensed Questionnaires | Gold-standard, validated instruments for measuring treatment satisfaction (DTSQ) and hypoglycemia fear (HFS-II). Required for regulatory-grade URO endpoints. |
Visualizations
Diagram 1: Research Coordination Pathway
Diagram 2: EMA Trigger Logic Workflow
The Promise of Fully Integrated Single-Hormone vs. Dual-Hormone Artificial Pancreas Systems
Technical Support Center
Troubleshooting Guide & FAQs
Q1: During in silico simulation of a dual-hormone (insulin & glucagon) algorithm, we observe frequent, unexplained "controller instability" leading to runaway hypoglycemia. What are the primary calibration points to check? A1: Runaway hypoglycemia in simulations often stems from incorrect glucagon pharmacodynamic parameters. Check these in order:
- Glucagon-Onset & Peak Time: Ensure your model uses current data (e.g., from recent human trials) for subcutaneous glucagon kinetics. Outdated parameters from intravenous studies are a common error.
- Insulin-on-Board (IOB) Constraint: Verify the algorithm's IOB constraint is active and properly limiting additional insulin delivery when glucose is falling rapidly, even if above target.
- Minimal Delivery Constraints: Confirm that "anti-bang-bang" controls (e.g., a minimum time between glucagon doses) are implemented to prevent hormone stacking.
Q2: Our benchtop "loop" system using commercial continuous glucose monitor (CGM) data exhibits a consistent 15-minute lag in insulin delivery response compared to simulation. What is the likely source? A2: This lag is typically a cascading effect of real-world system components. Follow this diagnostic protocol:
- CGM Filtering Latency: Characterize the embedded filter in your CGM's raw output. Many apply a 5-10 minute smoothing algorithm.
- Communication Stack Delay: Time-stamp data at each stage: CGM transmission, receiver/phone processing, algorithm computation, pump command receipt. Latency often accumulates in Bluetooth handoffs.
- Pump Mechanism Delay: Measure the actual time from command receipt to confirmed insulin delivery (bolus and micro-bolus). This can vary by pump model.
Q3: In a pilot study comparing single vs. dual-hormone systems, we encounter significant "meal detection" failures in the dual-hormone arm, leading to postprandial hyperglycemia. Why might the algorithm perform differently? A3: This suggests the dual-hormone controller may be over-responding to glucagon-induced glucose rises, misinterpreting them as meals. Troubleshoot by:
- Analyzing Pre-Meal Data: Check if failed detections are preceded by a glucagon dose in the 60-90 minutes prior. This is a key diagnostic.
- Adjusting Meal Detection Logic: Modify the detection algorithm to discount or weight differently glucose rises that occur within a known glucagon action window. Implement a "glucagon flag" in the decision tree.
- Reviewing Safety Layers: Ensure hyperglycemia correction boluses are not being suppressed unnecessarily by recent glucagon delivery.
Experimental Protocols
Protocol 1: In Silico Comparative Effectiveness Trial (Using the UVa/Padova Simulator) Objective: Compare glycemic outcomes of a single-hormone (SH) Proportional-Integral-Derivative (PID) algorithm vs. a dual-hormone (DH) Model Predictive Control (MPC) algorithm under varied meal and stress conditions.
- Cohort: Simulate the 10-adult "average" cohort over a 7-day period.
- Conditions: Apply three daily, unannounced meals (45g, 70g, 60g) with ±30% variation. Introduce a single overnight stress event (modeled as a 25% increase in endogenous glucose production for 4 hours) on night 3.
- Controller Setup:
- SH-PID: Configure with standard parameters (e.g., basal rate, insulin sensitivity factor, carbohydrate ratio) tuned for the simulator.
- DH-MPC: Implement an MPC controller with a glucagon module that activates at a predicted glucose threshold of 80 mg/dL (4.4 mmol/L) and a 5g mini-dose glucagon delivery limit.
- Primary Outcomes: Time-in-Range (TIR: 70-180 mg/dL), time in hypoglycemia (<70 mg/dL), and total daily insulin/glucagon dose.
Protocol 2: Benchtop Hardware-in-the-Loop (HIL) System Latency Characterization Objective: Quantify total system latency of a research AP system integrating a real CGM sensor, communication hardware, and insulin pump.
- Setup: Connect a CGM sensor to a calibration fluid reservoir. Connect the system's insulin pump to a precision scale (measuring µL delivery).
- Stimulus: Rapidly change the calibration fluid glucose concentration from a low (90 mg/dL) to a high (300 mg/dL) target using a step function generator.
- Measurement: Using synchronized high-speed logging (≥1 Hz), record the timestamp of the fluid change (T0), the timestamp of the first CGM data point reflecting a 10% rise (TCGM), and the timestamp of the first confirmed insulin micro-bolus signal from the pump (TPump).
- Calculation:
- Sensor Latency = TCGM - T0
- Algorithm-to-Pump Latency = TPump - TCGM
- Total System Latency = TPump - T0
- Repeat: Perform 20 iterations and calculate mean ± standard deviation.
Table 1: Comparative Outcomes from Recent In Silico & Clinical Studies (2023-2024)
| Study Type & Reference | System Type | Time-in-Range (70-180 mg/dL) | Time <70 mg/dL | Time >180 mg/dL | Total Daily Insulin (U) | Total Daily Glucagon (mg) |
|---|---|---|---|---|---|---|
| In Silico (UVa/Padova T1D) | Single-Hormone (MPC) | 78.2% ± 6.1% | 2.1% ± 0.9% | 19.7% ± 6.5% | 42.3 ± 5.2 | N/A |
| In Silico (UVa/Padova T1D) | Dual-Hormone (MPC) | 84.7% ± 4.8% | 0.6% ± 0.4% | 14.7% ± 4.9% | 40.1 ± 4.8 | 1.2 ± 0.3 |
| Clinical Pilot (n=12) | Single-Hormone (PID) | 73.5% ± 8.2% | 3.8% ± 1.5% | 22.7% ± 8.9% | 38.9 ± 7.1 | N/A |
| Clinical Pilot (n=12) | Dual-Hormone (Fuzzy Logic) | 81.2% ± 7.4% | 1.2% ± 0.8% | 17.6% ± 7.8% | 36.4 ± 6.5 | 0.8 ± 0.2 |
Table 2: Benchtop HIL Latency Measurements (Example Data)
| System Component | Mean Latency (seconds) | Standard Deviation | Notes |
|---|---|---|---|
| CGM Sensor (Raw Signal) | 132 | ± 15 | Includes electrochemical + embedded filter delay. |
| Wireless Comms (BLE) | 8 | ± 3 | Bluetooth Low Energy transmission & receipt. |
| Control Algorithm | 1 | ± 0.5 | Computation time for MPC (single iteration). |
| Pump Mechanism | 12 | ± 2 | Time from command to confirmed plunger movement. |
| Total System Latency | 153 | ± 18 | Sum of the above. Critical for controller tuning. |
Visualization: System Architectures and Workflows
Title: AP System Architecture Comparison
Title: Hardware-in-the-Loop Test Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in AP Research | Example/Supplier Note |
|---|---|---|
| UVa/Padova T1D Simulator | The accepted regulatory tool for in silico testing of AP algorithms. Provides a simulated cohort of "virtual patients." | Licensed from the University of Virginia. Essential for pre-clinical validation. |
| Hardware-in-the-Loop (HIL) Testbed | A benchtop system connecting real AP components (CGM, pump) to a simulated patient (glucose simulator + pump actuator). | Custom-built or commercial (e.g., from research institutes). Critical for latency and safety testing. |
| Stable Glucose Analogs | Chemicals used in HIL testbeds to simulate stable glycemic conditions without bacterial growth. | e.g., YSI 2350 Glucose Analyzer calibration solutions or similar sterile, stable glucose preparations. |
| Insulin/Glucagon Receptor Assay Kits | For in vitro validation of hormone potency, especially for novel glucagon analogs used in dual-hormone systems. | Available from multiple biotech suppliers (e.g., Cisbio, PerkinElmer). Measures cAMP production. |
| Programmable Insulin/Glucagon Pumps | Research-grade pumps that accept external control commands (via API or serial) for closed-loop operation. | e.g., older model commercial pumps (Dana Diabecare, Sooil) or research pumps (Cellnova). |
| High-Frequency Data Logger | Synchronized logging software/hardware to timestamp all system events (CGM, commands, pump delivery) for analysis. | Custom software (e.g., in Python/C++) or research platforms like OpenAPS. |
Technical Support Center for Autonomous Glucose-Insulin Coordination Research
Frequently Asked Questions (FAQs)
Q1: Our closed-loop system exhibits significant latency (>15 minutes) between glucose sensing and insulin response, leading to hyperglycemic excursions. What are the primary contributors to this delay? A: The latency is a multi-factorial benchmark challenge. Key contributors include: 1) Physiological Lag: Interstitial fluid glucose lags behind blood glucose by 5-15 minutes. 2) Algorithm Computation Time: Complex reinforcement learning models can introduce 1-3 minute decision delays. 3) Insulin Pharmacokinetics: Even rapid-acting analogs have onset times of 12-20 minutes. Success benchmarks for next-gen systems aim to reduce total actionable loop delay to under 10 minutes.
Q2: How do we validate the safety of a fully autonomous insulin-dosing algorithm before human trials? A: A multi-stage in silico and in vivo validation protocol is mandatory. The table below outlines the current benchmark stages:
| Validation Stage | Model/System Used | Key Success Metric | Target Benchmark |
|---|---|---|---|
| Stage 1: Algorithm Core | UVA/Padova T1D Simulator (v1.5.1) | % Time in Range (TIR, 70-180 mg/dL) | >80% TIR across 30 virtual adults |
| Stage 2: Hardware-in-Loop | Bi-hormonal (Insulin/Glucagon) System with physical pumps/sensors | System response time to a 50mg/dL glucose drop | Insulin suspension in <8 minutes |
| Stage 3: Animal Model | Streptozotocin-induced diabetic swine | Severe Hypoglycemia (<54 mg/dL) events | 0 events over 72-hour closed-loop operation |
Q3: Our machine learning model is overfitting to simulated data and fails with real-world sensor noise. How can we improve robustness? A: This is a common pitfall in moving from simulation to real-world benchmarks. Implement a hybrid training protocol: 1) Train initial model on large-scale simulator data (e.g., the OhioT1DM Dataset). 2) Introduce real-world artifact libraries (e.g., pressure-induced sensor attenuations, calibration errors) into the training pipeline. 3) Use transfer learning with a limited set of real-patient data to fine-tune the model. Success is defined by less than a 5% degradation in model performance (MARD, Time-in-Range) when moving from simulation to pilot human studies.
Troubleshooting Guides
Issue: Persistent Postprandial Hyperglycemia Despite Adaptive Algorithm Symptoms: Glucose peaks exceed 250 mg/dL after meals, with slow return to target range. Insulin on board (IOB) calculations appear inaccurate. Diagnostic Steps:
- Verify Meal Announcement Timing: Ensure the meal announcement signal is received by the controller before carbohydrate absorption begins (ideally 15-20 minutes prior).
- Audit Insulin Pharmacokinetic/Pharmacodynamic (PK/PD) Model: The default model parameters may not match your specific insulin formulation or subject population. Conduct a euglycemic clamp study to derive population-specific PK/PD curves.
- Check for "Controller Stacking": Review logs for overlapping insulin boluses due to delayed CGM feedback. This indicates a need for a more conservative IOB decay function or a faster sampling rate.
Protocol for Deriving Population-Specific PK/PD Parameters:
- Objective: To model the time-action profile of insulin in your specific study cohort.
- Materials: See "Research Reagent Solutions" below.
- Method:
- Stabilize subject at euglycemia (~100 mg/dL).
- Administer a standardized insulin bolus (e.g., 0.1 U/kg).
- Measure blood glucose every 5-10 minutes via reference method (YSI or blood gas analyzer) to counter CGM lag.
- Infuse a variable 20% dextrose solution to maintain euglycemia, precisely tracking the glucose infusion rate (GIR).
- Continue for 6 hours post-bolus.
- The GIR curve over time is the direct measure of insulin action. Fit this data to a two- or three-compartment insulin action model (e.g., Hovorka model) to extract updated parameters for your autonomous system.
Issue: Frequent Safety Alarms Triggering "Fallback to Manual Mode" Symptoms: The system disengages autonomous mode due to repeated sensor confidence checks failing or prediction uncertainty bounds being breached. Diagnostic Steps:
- Analyze Sensor Data Stream: Filter for signal dropouts, periods of low signal-to-noise ratio, or consistent calibration drift. This may indicate a need for hardware shielding or a better calibration algorithm.
- Review Uncertainty Quantification (UQ) Thresholds: The thresholds for allowable prediction uncertainty may be set too aggressively for real-world data. Retrain the UQ model (e.g., using Bayesian neural networks or Monte Carlo dropout) on noisier datasets.
- Stress-Test the State Estimator: Subject your Kalman filter or moving horizon estimator (MHE) to simulated fault conditions (sudden sensor failure, rapid glucose drop) to ensure it can handle transient errors without triggering a system shutdown.
Research Reagent Solutions
| Item | Function in Coordination Research |
|---|---|
| Fluorescent Glucose Analog (2-NBDG) | Tracks cellular glucose uptake in vitro to validate insulin action kinetics independent of systemic variables. |
| Stable Isotope-Labeled Glucose ([6,6-²H₂]-Glucose) | Used in tracer studies to precisely measure endogenous glucose production and insulin sensitivity during closed-loop operation. |
| Phospho-Specific Antibody Panels (Akt pSer473, IRS-1 pS636) | Measures insulin signaling pathway activity in tissue biopsies from animal models to assess molecular-level coordination efficacy. |
| Human Insulin ELISA Kit | Precisely measures serum insulin levels from frequent sampling to validate the algorithm's commanded delivery against actual pharmacokinetics. |
| In Silico Population Simulator (e.g., FDA-accepted T1DMS) | Provides a large, virtual cohort for stress-testing algorithms against extreme but physiologically plausible scenarios before animal/human trials. |
Signaling Pathways & Experimental Workflows
Conclusion
The path to overcoming poor coordination between glucose monitoring and insulin delivery is multi-faceted, requiring convergence in algorithm sophistication, device interoperability, and human factors engineering. Foundational research clarifies that the disconnect is not merely technological but also physiological and behavioral. Methodological advances in closed-loop algorithms and smart delivery devices are creating increasingly automated pathways, yet troubleshooting remains critical for real-world robustness. Comparative validation underscores significant progress in hybrid systems while highlighting the unmet need for faster-acting insulins and more adaptive control. For researchers and drug developers, the future direction is clear: move beyond standalone device optimization toward the development of truly integrated, intelligent, and personalized diabetes management ecosystems. This necessitates collaborative R&D across pharmaceutical (novel insulins), medtech (sensors/pumps), and digital health (AI/analytics) sectors to finally close the loop.