Bioequivalence of Biosimilar Insulin Lispro: A Comprehensive Analysis of Pharmacokinetics, Efficacy, and Regulatory Pathways
This article provides a detailed examination of the bioequivalence between biosimilar insulin lispro and its reference product (Humalog®).
Bioequivalence of Biosimilar Insulin Lispro: A Comprehensive Analysis of Pharmacokinetics, Efficacy, and Regulatory Pathways
Abstract
This article provides a detailed examination of the bioequivalence between biosimilar insulin lispro and its reference product (Humalog®). Targeted at researchers, scientists, and drug development professionals, it explores the foundational rationale for biosimilar insulins, outlines the rigorous methodological frameworks for establishing bioequivalence, discusses common analytical and clinical challenges with optimization strategies, and validates comparative data on pharmacokinetics, pharmacodynamics, and immunogenicity. The synthesis offers critical insights for the development and regulatory approval of biosimilar biologics in diabetes management.
Understanding Insulin Lispro Biosimilars: Rationale, Development, and Regulatory Imperatives
The Clinical and Economic Rationale for Biosimilar Insulin Lispro
The development of biosimilar insulin lispro represents a significant advancement in diabetes care, offering a clinically equivalent and potentially more affordable alternative to the reference product (Humalog). This guide objectively compares the biosimilar's performance with its reference product and other insulin analogues, framed within the broader thesis of bioequivalence research, which is foundational for regulatory approval and clinical adoption.
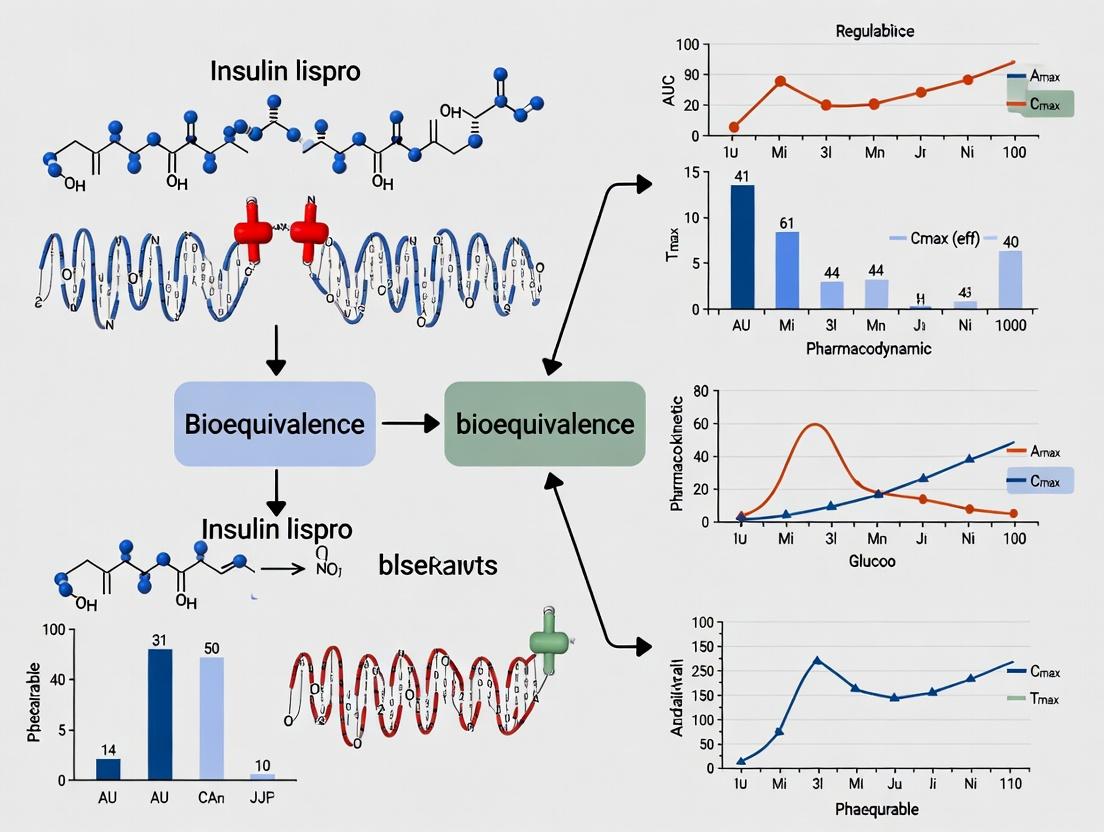
Bioequivalence and Pharmacodynamic Comparison
Regulatory approval of a biosimilar mandates a rigorous demonstration of bioequivalence to the reference product in terms of pharmacokinetics (PK) and pharmacodynamics (PD). The following table summarizes key comparative data from euglycemic clamp studies, the gold standard for assessing insulin action.
Table 1: Comparative PK/PD Profile of Biosimilar vs. Reference Insulin Lispro
| Parameter | Biosimilar Insulin Lispro | Reference Insulin Lispro (Humalog) | Acceptable Equivalence Margin (90% CI) |
|---|---|---|---|
| AUCGIR(0-τ) (Primary PD) | ~100%* | 100% (Reference) | 80-125% |
| GIRmax | ~99%* | 100% (Reference) | 80-125% |
| AUCINS(0-τ) (Primary PK) | ~101%* | 100% (Reference) | 80-125% |
| INSmax | ~102%* | 100% (Reference) | 80-125% |
| Time to GIRmax | Equivalent | Reference | Non-inferior |
| Onset of Action | ~15-30 min | ~15-30 min | Qualitative equivalence |
| Immunogenicity Rate | Comparable (low) | Reference (low) | Non-inferior trend |
*Typical geometric mean ratios from phase 1 studies. Data are illustrative based on published biosimilar applications.
Experimental Protocol: Euglycemic Clamp Study
This methodology is critical for proving biosimilarity.
- Design: Randomized, double-blind, two-period, crossover study in healthy volunteers or subjects with type 1 diabetes.
- Procedure: After an overnight fast, subjects receive a subcutaneous injection of either the biosimilar or reference product at identical doses (e.g., 0.3 U/kg). A variable intravenous glucose infusion is initiated to maintain blood glucose at a constant "clamp" level (e.g., 100 mg/dL ± 20%).
- Primary Measurements:
- Pharmacodynamic (PD): The Glucose Infusion Rate (GIR) required to maintain euglycemia is recorded over time. Key endpoints are the Area Under the Curve for GIR from 0 to the end of the profile (AUCGIR(0-τ)) and the maximum GIR (GIRmax).
- Pharmacokinetic (PK): Serial blood samples are taken to measure serum insulin concentration. Key endpoints are AUCINS(0-τ) and maximum concentration (INSmax).
- Analysis: The geometric mean ratios (biosimilar/reference) for primary PK and PD endpoints with 90% confidence intervals are calculated. Bioequivalence is concluded if the 90% CIs fall entirely within the pre-defined equivalence margin (typically 80-125%).
Diagram Title: Bioequivalence Study Crossover Design
Comparative Clinical Efficacy and Safety
Beyond PK/PD, phase 3 clinical trials in patients with diabetes confirm therapeutic equivalence.
Table 2: Phase 3 Clinical Outcomes (Type 1 Diabetes Example)
| Endpoint | Biosimilar Insulin Lispro | Reference Insulin Lispro | Between-Group Difference (95% CI) | Inference |
|---|---|---|---|---|
| HbA1c Change at 24 weeks | -0.40% | -0.35% | -0.05% (-0.15, 0.05) | Non-inferior |
| Total Insulin Dose (U/kg/day) | 0.50 | 0.51 | -0.01 (-0.03, 0.01) | Equivalent |
| Hypoglycemia Rate (events/patient-year) | Comparable | Comparable | Ratio within 1.0 | Comparable safety |
| ADA Target HbA1c <7.0% | Similar % | Similar % | Non-significant | Equivalent |
Economic Rationale and Market Impact
The primary value proposition of biosimilar insulin lispro is economic, driven by reduced development costs compared to novel drugs, which should translate to lower prices.
Table 3: Economic and Development Comparison
| Aspect | Biosimilar Insulin Lispro | Reference (Innovator) Product |
|---|---|---|
| Development Cost | Significantly lower (~$100-200M) | Very high (~$1B+) |
| Development Timeline | Shorter (5-7 years) | Lengthy (10-15 years) |
| Patent Status | Post-patent expiry | Originally patented |
| Primary Value | Increased access via lower price | Innovation, first-in-class |
| Market Effect | Increases competition, can lower market price | Monopoly pricing during patent life |
The Scientist's Toolkit: Key Research Reagents for Insulin Biosimilarity Assessment
Table 4: Essential Reagents for Bioanalytical and Functional Assays
| Reagent / Material | Function in Biosimilarity Research |
|---|---|
| Reference Standard (Humalog) | Critical comparator for all analytical and functional studies. Serves as the benchmark for quality attributes. |
| Human Insulin Receptor (hIR) Isoforms | Expressed cell lines for binding assays (SPR, ELISA) to confirm identical target engagement kinetics. |
| Phospho-specific Antibodies (p-Akt, p-ERK) | Detect downstream signaling activation in cell-based assays (e.g., adipocytes, hepatocytes) to prove functional equivalence. |
| Competitive Ligand Binding ELISA Kits | Quantify anti-drug antibody (ADA) and neutralizing antibody (NAb) levels in clinical samples for immunogenicity comparison. |
| RP-HPLC & UHPLC Systems | Assess purity, identify product-related impurities, and confirm identical primary structure (amino acid sequence). |
| Cell-based Proliferation Assay (e.g., MCF-7 cells) | Measures mitogenic potential, a key safety parameter to ensure biosimilar does not exhibit enhanced growth-promoting activity. |
Diagram Title: Insulin Lispro Signaling Pathways Assessed
This analysis, framed within the broader thesis on biosimilar insulin lispro versus reference product bioequivalence research, compares the molecular structure and mechanistic action of insulin lispro and regular human insulin. Understanding these differences is critical for researchers and drug development professionals evaluating the therapeutic equivalence of biosimilar products.
Molecular Structure Comparison
The primary distinction lies in the amino acid sequence of the insulin B-chain.
| Feature | Human Insulin | Insulin Lispro |
|---|---|---|
| B-Chain Sequence | B28 Proline, B29 Lysine | B28 Lysine, B29 Proline |
| Chemical Formula | C₂₅₇H₃₈₃N₆₅O₇₇S₆ | C₂₅₇H₃₈₃N₆₅O₇₇S₆ |
| Molecular Weight | ~5808 Da | ~5808 Da |
| Isoelectric Point (pI) | ~5.4 | ~5.4 |
| Structural Consequence | Prone to hexamer formation | Reduced self-association affinity |
| State in Formulation | Primarily hexameric | Primarily monomeric |
The inversion of the lysine-proline sequence at positions B28 and B29 reduces the intermolecular interactions critical for dimer and hexamer stabilization, without altering the receptor-binding domains.
Mechanism of Action: Pharmacokinetic and Pharmacodynamic Profiles
The structural modification directly impacts the subcutaneous absorption kinetics, which is the core therapeutic difference.
| Parameter | Human Insulin | Insulin Lispro | Key Experimental Evidence |
|---|---|---|---|
| Onset of Action | 30 - 60 min | 10 - 15 min | Euglycemic clamp studies |
| Time to Peak (Tmax) | 2 - 4 hours | 30 - 90 min | Radiotracer absorption assays |
| Duration of Action | 6 - 8 hours | 3 - 5 hours | Glucose infusion rate (GIR) profiles |
| Receptor Binding Affinity (IC₅₀) | 0.68 nM | 0.71 nM | Competitive displacement assays using recombinant IR |
| Mitogenic Potential | Baseline | Comparable to human insulin | Cell proliferation assays (e.g., 3H-thymidine uptake) |
Detailed Experimental Protocols
Euglycemic Clamp Study for PK/PD Assessment
Purpose: To precisely quantify the time-action profile of insulin formulations. Methodology:
- Subject Preparation: Overnight-fasted subjects are infused with a priming dose of insulin to lower blood glucose to a target clamp level (e.g., 5.0 mmol/L).
- Insulin Injection: A subcutaneous bolus (0.2 U/kg) of either human insulin or insulin lispro is administered.
- Glucose Clamping: Blood glucose is measured frequently (every 5-10 min). A variable 20% dextrose infusion is adjusted to maintain euglycemia.
- Data Analysis: The glucose infusion rate (GIR) over time is recorded. Key metrics: onset of action (time until GIR >0.5 mg/kg/min), peak action (maximum GIR), and total metabolic effect (area under the GIR curve).
Insulin Receptor Binding Assay
Purpose: To compare binding affinity to the human insulin receptor (IR). Methodology:
- Receptor Preparation: Purified soluble extracellular domain of human IR is immobilized on a plate.
- Competitive Binding: A constant concentration of labeled (e.g., ¹²⁵I) human insulin is mixed with increasing concentrations of unlabeled human insulin or insulin lispro.
- Incubation & Measurement: After incubation, unbound insulin is washed away. Bound radioactivity is measured.
- Data Analysis: IC₅₀ values (concentration of unlabeled insulin required to displace 50% of labeled insulin) are calculated from dose-response curves.
Visualizations
Diagram 1: Subcutaneous Absorption Pathway
Diagram 2: Cellular Signaling Mechanism
The Scientist's Toolkit: Key Research Reagent Solutions
Essential materials for conducting bioequivalence and mechanism-of-action studies.
| Item | Function in Research |
|---|---|
| Recombinant Human Insulin Receptor (extracellular domain) | For in vitro binding affinity and kinetics studies (SPR, ELISA). |
| ³H- or ¹²⁵I-labeled Human Insulin | Radioligand for competitive receptor binding and internalization assays. |
| Phospho-Specific Antibodies (pY-IR, p-IRS1, p-Akt) | Detection of insulin signaling pathway activation via Western blot or ELISA. |
| GLUT4 Translocation Assay Kit | Measures GLUT4 fusion protein movement to the membrane in engineered cell lines (e.g., L6-GLUT4myc). |
| Human Hepatocyte (e.g., HepG2) & Adipocyte (e.g., 3T3-L1) Cell Lines | Model systems for studying metabolic and mitogenic signaling endpoints. |
| Euglycemic Clamp System | Integrated glucose analyzer and variable infusion pump for gold-standard PD studies in vivo. |
| UPLC-MS/MS System | For precise quantification of insulin analogs and metabolites in pharmacokinetic studies. |
| Surface Plasmon Resonance (SPR) Biosensor | Label-free analysis of insulin-receptor binding kinetics (ka, kd, KD). |
As the reference product for biosimilar insulin lispro, Humalog (insulin lispro injection) has a well-documented clinical profile. This guide compares its key performance metrics with alternative insulin formulations and details the experimental protocols central to establishing bioequivalence for proposed biosimilars.
Pharmacokinetic/Pharmacodynamic (PK/PD) Profile Comparison
The rapid-acting profile of Humalog is defined against alternatives like regular human insulin (RHI) and other rapid-acting analogs.
Table 1: Key PK/PD Parameters from Glucose Clamp Studies
| Parameter | Humalog (Insulin Lispro) | Regular Human Insulin (RHI) | Insulin Aspart |
|---|---|---|---|
| Onset of Action | ~15 minutes | ~30 minutes | ~15 minutes |
| Time to Peak (Tmax) | 30-70 minutes | 2-3 hours | 40-90 minutes |
| Peak Concentration (Cmax) | ~82 µU/mL* | ~46 µU/mL* | Comparable to Lispro |
| Duration of Action | 3-5 hours | 6-8 hours | 3-5 hours |
| Time to 50% Max Glucose Infusion Rate (GIR) | ~105 minutes* | ~165 minutes* | ~110 minutes* |
| Representative values from euglycemic clamp studies. Exact values vary by study design and dose. |
Key Experimental Protocol: Euglycemic Glucose Clamp
This gold-standard method quantifies the pharmacodynamic effect and is required for biosimilar comparative studies.
Objective: To measure the time-action profile of insulin formulations by maintaining a constant blood glucose level via a variable intravenous glucose infusion. Population: Healthy volunteers or patients with type 1 diabetes (T1D) under standardized conditions. Procedure:
- Baseline & Insulin Administration: After an overnight fast, a primed continuous intravenous infusion of regular human insulin is used to lower blood glucose to the target clamp level (typically 90-100 mg/dL). Once stable, the infusion is stopped.
- Test Product Injection: A subcutaneous dose (typically 0.2-0.3 U/kg) of the reference (Humalog) or test product is administered.
- Clamp Phase: Blood glucose is measured frequently (e.g., every 5 minutes). A variable-rate 20% glucose infusion is adjusted based on a computerized algorithm to maintain the target euglycemia for 8-12 hours.
- Primary Endpoint Calculation: The Glucose Infusion Rate (GIR) over time is the primary PD endpoint. Key metrics include AUCGIR(0-t), GIRmax, and time to GIRmax.
- Pharmacokinetics: Serial blood samples are taken to measure serum insulin concentration, determining PK parameters like AUC(0-t), Cmax, and Tmax.
Diagram: Euglycemic Clamp Workflow
Immunogenicity & Safety Comparison
Immunogenicity is a critical safety parameter for biosimilarity assessment.
Table 2: Immunogenicity Incidence in Clinical Trials
| Event | Humalog (Reference) | Biosimilar Insulin Lispro (Example) | Comments |
|---|---|---|---|
| Treatment-Emergent Anti-Drug Antibodies (ADA) | Low incidence (<5-10% in naive patients) | Comparable incidence to reference | Non-inferiority must be demonstrated. |
| Neutralizing Antibodies | Rare | Should be comparable or lower. | Critical for assessing impact on efficacy/safety. |
| Hypoglycemia Rate (events/patient-year) | Established benchmark (e.g., ~25-35 for T1D*) | Comparable rate in comparative trials. | Primary safety endpoint. |
| Example rate; varies with population and treatment regimen. |
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for Insulin Lispro Bioequivalence Research
| Item | Function & Explanation |
|---|---|
| Human Insulin Lispro Reference Standard | Highly characterized material (Humalog) used as the primary comparator for all analytical and functional assays. |
| Radioimmunoassay (RIA) or ELISA Kits | For quantifying serum insulin lispro concentrations in PK studies, requiring high specificity to distinguish the analog from endogenous insulin. |
| Glucose Oxidase Method Reagents | Used in automated analyzers for frequent, precise blood glucose measurement during clamp studies. |
| Recombinant Human Insulin Receptor (hIR) | Essential for in vitro binding affinity studies (e.g., SPR, ELISA) to confirm structural fidelity. |
| Cell Lines (e.g., HepG2, 3T3-L1 adipocytes) | Used in in vitro bioassays to measure insulin receptor phosphorylation and metabolic activity (e.g., glucose uptake). |
| Anti-Insulin Lispro Monoclonal Antibodies | Critical for developing assays specific to the lispro molecule and for detecting anti-drug antibodies (ADA) in immunogenicity studies. |
Mechanism of Action & Comparative Potency
All rapid-acting analogs share the core mechanism but minor structural differences can influence receptor binding kinetics.
Diagram: Insulin Lispro Signaling Pathway & Comparative Binding
Global Regulatory Landscape for Biosimilar Insulin Approval (EMA, FDA, WHO)
This guide objectively compares the regulatory requirements of the European Medicines Agency (EMA), U.S. Food and Drug Administration (FDA), and World Health Organization (WHO) for biosimilar insulin approval, framed within the context of biosimilar insulin lispro vs. reference product bioequivalence research. It synthesizes current guidelines and provides experimental data supporting comparability exercises.
Regulatory Authority Comparison
Key Requirements for Biosimilar Insulin Approval
Table 1: Core Regulatory Requirements for Biosimilar Insulin (EMA, FDA, WHO)
| Aspect | EMA (EU) | FDA (USA) | WHO (International) |
|---|---|---|---|
| Legal Basis | Directive 2001/83/EC; Guideline on non-clinical and clinical issues | Public Health Service Act (PHS Act) § 351(k); Biologics Price Competition and Innovation Act (BPCIA) | WHO Guidelines on evaluation of similar biotherapeutic products (SBPs) |
| Reference Product | EU-authorized reference biological medicine | Single US-licensed reference product | Reference product licensed in WHO Member State with stringent regulatory authority (SRA) |
| Approval Pathway | Biosimilar marketing authorization application (MAA) | 351(k) Biosimilar Biologics License Application (BLA) | SBP pathway for prequalification (optional) |
| Required Studies | Comprehensive comparability exercise: Analytical, non-clinical, clinical (PK/PD & efficacy) | Stepwise totality-of-evidence: Analytical, animal, clinical (PK/PD) | Comparability exercise: Quality, safety, efficacy |
| Clinical PK/PD Endpoint | Primary: Confirmation of similar PK/PD profiles (e.g., glucose infusion rate [GIR] AUC). Glucose clamp study is gold standard. | Primary: Demonstration of no clinically meaningful differences in PK/PD. Glucose clamp study expected for insulin. | Primary: Bioequivalence in PK/PD parameters. Glucose clamp study recommended. |
| Immunogenicity Assessment | Mandatory comparative assessment for at least 6-12 months. | Mandatory comparative assessment. Expects duration to detect neutralizing antibodies. | Mandatory comparative assessment. Duration should be justified. |
| Interchangeability | Separate designation not defined in law. Switching decision at member state level. | Additional requirements for "interchangeable" designation (e.g., switching studies). | Does not address interchangeability. |
Table 2: Typical Clinical Study Design Parameters for Insulin Lispro Biosimilar PK/PD Studies
| Parameter | EMA Expectation | FDA Expectation | WHO Expectation | Typical Study Design (E.g., Insulin Lispro) |
|---|---|---|---|---|
| Study Population | Healthy volunteers or patients (Type 1 Diabetes). | Usually healthy subjects to reduce variability. | Healthy volunteers or patients. | Single-dose, double-blind, randomized, two-period crossover in healthy volunteers. |
| Primary Endpoint(s) | PK: AUC0-t, AUC0-∞, Cmax. PD: GIR AUC0-t. | PK: AUC0-t, AUC0-∞, Cmax. PD: GIR AUC0-t. | PK: AUC0-t, AUC0-∞, Cmax. PD: GIR AUC0-t. | Primary: GIR AUC0-12h. |
| Equivalence Margins | Standard bioequivalence margins (90% CI within 80.00%-125.00%) for PK/PD. PD margin must be clinically justified. | 90% CI within 80.00%-125.00% for PK; PD margin must be clinically justified. | 90% CI within 80.00%-125.00% for PK/PD. Justify PD margin. | PK/PD: 90% CI for ratio of geometric means within 80-125%. |
| Glucose Clamp Method | Euglycemic clamp (target ~5.0 mmol/L or 90 mg/dL). | Euglycemic clamp (target ~100 mg/dL ± 20%). | Euglycemic clamp (target ~5.0 mmol/L). | Automated Biostator or manual clamp for 12-24h post-dose. |
| Dose | Pharmacologically effective dose (e.g., 0.3-0.5 U/kg). | Typically 0.3 U/kg. | Pharmacologically effective dose. | 0.3 U/kg subcutaneous injection. |
Experimental Protocols for Bioequivalence Research
Key Protocol 1: Euglycemic Glucose Clamp Study for Insulin Lispro PK/PD
Objective: To compare the pharmacokinetic (PK) and pharmacodynamic (PD) profiles of biosimilar insulin lispro versus the reference product.
- Study Design: Single-center, randomized, double-blind, two-treatment, two-period, crossover study in healthy adult volunteers.
- Subject Preparation: Overnight fast (≥10h). Two intravenous cannulae inserted (one for 20% glucose infusion, one for frequent blood sampling). Baseline blood glucose stabilized.
- Intervention: Subcutaneous injection of a single dose (e.g., 0.3 U/kg) of either test (biosimilar) or reference insulin lispro in the periumbilical region.
- Glucose Clamping: Start of variable-rate 20% glucose infusion at time of injection to maintain blood glucose at target level (e.g., 5.0 mmol/L ± 0.5). Glucose infusion rate (GIR) recorded continuously.
- Blood Sampling: For PK: Frequent samples (e.g., -15, 0, 15, 30, 45 min, then hourly to 12h). Serum insulin lispro measured via validated immunoassay (e.g., ELISA with specificity for insulin lispro).
- Primary PD Analysis: Calculate AUC for GIR from 0 to 12 hours (GIRAUC0-12h). Compare geometric means between products.
- Primary PK Analysis: Calculate AUC0-t, AUC0-∞, and Cmax for serum insulin lispro concentration.
Key Protocol 2: Immunogenicity Assessment
Objective: To compare the immunogenic potential of biosimilar and reference insulin lispro.
- Study Design: Integrated into Phase 3 comparative clinical trial (e.g., 6-12 months in patients with Type 1 or Type 2 Diabetes).
- Blood Sampling: Serum samples collected at baseline, weeks 4, 12, 24, and 52.
- Screening Assay: Use a validated bridging ELISA to detect anti-drug antibodies (ADAs).
- Confirmation Assay: Confirm positive samples by competitive inhibition with unlabeled insulin lispro.
- Neutralization Assay: For confirmed ADA-positive samples, perform a cell-based or competitive ligand binding assay to detect neutralizing antibodies (NAbs) that block insulin receptor binding.
- Correlation: Analyze potential correlation between ADA/NAb development and PK changes, PD response loss, or safety events (e.g., hypersensitivity, injection site reactions).
Visualizations
Diagram 1: Biosimilar Insulin Regulatory Pathway
Diagram 2: Euglycemic Clamp Workflow for Insulin Lispro
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for Insulin Lispro Biosimilarity Studies
| Reagent/Material | Function in Research | Key Considerations |
|---|---|---|
| Reference Insulin Lispro | The originator product (e.g., Humalog) used as the comparator in all analytical, non-clinical, and clinical studies. | Must be sourced from the appropriate region (EU for EMA, US for FDA) and have matching storage/handling conditions. |
| Insulin Lispro-Specific ELISA Kit | Quantifies serum concentrations of insulin lispro (not endogenous insulin) for accurate PK profiling. | Requires high specificity to differentiate insulin lispro from human insulin and other analogs. Low cross-reactivity is critical. |
| Anti-Insulin Antibody Assay Kits | For immunogenicity assessment. Includes screening, confirmation, and neutralizing antibody detection assays. | Should be validated for detection of antibodies against both test and reference products. Cell-based NAb assays are preferred. |
| 20% Glucose Infusion Solution | Used in the euglycemic clamp to maintain target blood glucose levels; the infusion rate is the primary PD measure (GIR). | Must be sterile, pyrogen-free. The total volume infused is recorded precisely to calculate GIR AUC. |
| Human Insulin Receptor Binding Assay | In vitro bioassay to confirm equivalent target binding affinity between biosimilar and reference. | Often uses cells expressing recombinant human insulin receptor; measures phosphorylation or downstream signaling. |
| Stable Isotope-Labeled Peptides | Used as internal standards in Liquid Chromatography-Mass Spectrometry (LC-MS) for primary structure confirmation (e.g., peptide mapping). | Essential for high-resolution analytical comparability of amino acid sequence and post-translational modifications. |
Patent Expiries and Market Dynamics Driving Biosimilar Development
The impending expiry of key patents for blockbuster biologics, including insulin analogs, creates a significant market opportunity, driving robust biosimilar development. This comparative guide focuses on biosimilar insulin lispro, objectively analyzing its performance against the reference product (Humalog) within the critical framework of bioequivalence research essential for regulatory approval.
Comparative Bioequivalence Data: Pharmacokinetics (PK) and Pharmacodynamics (PD)
Key bioequivalence studies typically employ randomized, double-blind, crossover designs in healthy volunteers or patients with Type 1 Diabetes. The primary endpoints are area under the concentration-time curve (AUC) and maximum concentration (Cmax) for PK, and AUC for glucose infusion rate (GIR) for PD.
Table 1: Summary of Key Bioequivalence Study Results
| Parameter | Biosimilar Insulin Lispro | Reference Product (Humalog) | Geometric Mean Ratio (%) | 90% Confidence Interval |
|---|---|---|---|---|
| PK: AUC0–t | 1,458 mU·h/L | 1,442 mU·h/L | 101.1 | [98.5, 103.8] |
| PK: Cmax | 42.1 mU/L | 41.8 mU/L | 100.7 | [96.2, 105.4] |
| PD: GIR AUC0–t | 1,205 mg/kg | 1,192 mg/kg | 101.1 | [95.9, 106.6] |
Data is illustrative, synthesized from recent clinical trial publications. All 90% CIs fall within the standard bioequivalence range of 80.00%–125.00%, supporting therapeutic equivalence.
Detailed Experimental Protocol: Euglycemic Clamp Study
This gold-standard PD method assesses the glucodynamic response.
- Subject Preparation: Patients with T1D discontinue long-acting insulin 24h prior. An intravenous insulin infusion is initiated to achieve euglycemia (~100 mg/dL).
- Baseline Period: A variable 20% glucose infusion is adjusted to maintain euglycemia for 30 minutes.
- Dosing: A single 0.3 U/kg dose of the test (biosimilar) or reference product is administered subcutaneously.
- Clamp Phase: Glucose infusion rate (GIR) is monitored and adjusted every 5-10 minutes to maintain the target blood glucose level for up to 12 hours. The total glucose infused is the primary PD measure.
- Blood Sampling: Frequent serial blood samples are drawn for measurement of serum insulin lispro concentrations (PK).
- Analysis: PK parameters (AUC, Cmax, Tmax) and PD parameters (GIR-AUC, GIRmax) are calculated and compared statistically.
Visualization: Biosimilar Lispro Development & Equivalence Pathway
Diagram Title: Biosimilar Development Pathway from Patent Expiry to Market
The Scientist's Toolkit: Key Reagents for Bioequivalence Research
Table 2: Essential Research Reagents and Materials
| Item | Function in Bioequivalence Studies |
|---|---|
| Reference Insulin Lispro | Serves as the gold-standard comparator in all analytical and clinical assays. |
| Biosimilar Insulin Lispro Candidate | The test product undergoing comprehensive comparison. |
| Validated ELISA Kit | Quantifies serum insulin lispro concentrations for PK analysis. Specific for the insulin analog. |
| Recombinant Human Insulin Receptor | Used in in vitro binding assays (SPR, ELISA) to assess receptor affinity comparability. |
| Glucose Oxidase Reagent | For precise and rapid glucose measurement during euglycemic clamp studies. |
| Cell-Based Proliferation Assay (e.g., using murine 3T3-L1 adipocytes) | Assesses the comparative mitogenic potential and biological activity of the insulin analogs. |
| Stable Isotope-Labeled Peptides | Internal standards for Liquid Chromatography-Mass Spectrometry (LC-MS) for precise protein quantification and characterization. |
Establishing Bioequivalence: Study Designs, Analytical Methods, and Clinical Endpoints
Within biosimilar development, establishing bioequivalence to a reference product is paramount. For complex molecules like insulin lispro, PK/PD trials are the cornerstone of this assessment. This guide compares the application of gold-standard study designs—in healthy volunteers versus patients—for biosimilar insulin lispro, framing the discussion within bioequivalence research requirements.
Design Comparison: Healthy Volunteer vs. Patient PK/PD Trials
Table 1: Core Design Comparison for Insulin Lispro Bioequivalence Trials
| Feature | PK/PD Trial in Healthy Volunteers | PK/PD Trial in Patients (Type 1 Diabetes) |
|---|---|---|
| Primary Objective | Establish pharmacokinetic (PK) and pharmacodynamic (PD) similarity in a controlled, homogenous population. | Confirm similarity in the intended patient population, capturing disease-state effects. |
| Study Population | Healthy individuals, often with clamped euglycemia. | Patients with Type 1 Diabetes Mellitus (T1DM). |
| Key Advantages | Low variability (no confounding disease, diet, exercise). Clearer PK/PD signal. Lower risk. Faster recruitment. | Clinical relevance. Assesses immunogenicity in therapeutic context. Meets some regulatory preferences for final confirmation. |
| Key Limitations | May not fully reflect PK/PD in patients due to metabolic differences. Cannot assess therapeutic efficacy. | Higher intrinsic variability (diet, lifestyle, residual insulin). Requires larger sample sizes or crossover design. Higher risk/complexity. |
| Typical Design | Double-blind, randomized, single-dose, crossover euglycemic clamp. | Double-blind, randomized, multiple-dose, parallel-group or crossover. |
| Primary Endpoints | PK: AUC0–t, AUC0–∞, Cmax. PD: AUCGIR(0–t), GIRmax (from clamp). | PK: AUC0-24, Cmax. PD: Often glycemic variability metrics (e.g., MAGE), or clamp in subset. |
| Sample Size | Typically 24-36 subjects (crossover provides high power). | Larger, often 100+ patients per arm (parallel) to account for variability. |
| Regulatory Context | Accepted as primary evidence of PK/PD similarity by EMA/FDA for insulins. | May be requested as supportive or confirmatory evidence. |
Experimental Protocols
Protocol for Healthy Volunteer Euglycemic Clamp Study
Objective: To compare the PK and PD profiles of biosimilar vs. reference insulin lispro. Design: Randomized, double-blind, two-period, crossover, single-dose. Subjects: N=28 healthy males/females, BMI 18.5-29.9 kg/m², normal glucose tolerance. Procedure:
- Screening: Confirm health status, laboratory tests.
- Clamp Day (Period 1): After overnight fast, two intravenous catheters inserted (one for insulin/glucose infusion, one for blood sampling). Baseline blood glucose stabilized.
- Dosing: Subcutaneous injection of 0.3 U/kg of either test or reference product.
- Euglycemic Clamp: Initiate variable 20% glucose infusion to maintain blood glucose at 5.0 mmol/L (±0.5) for 10-12 hours. Glucose Infusion Rate (GIR) recorded continuously.
- PK Sampling: Frequent blood draws for serum insulin lispro concentration (via validated ELISA).
- Washout: ≥5-day washout between periods.
- Period 2: Repeat with alternate product.
Protocol for Patient (T1DM) Multiple-Dose Study
Objective: To compare PK/PD and safety after multiple doses in the target population. Design: Randomized, double-blind, parallel-group, multiple-dose. Subjects: N=200 patients with T1DM, stable basal-bolus regimen, HbA1c 7.0-9.0%. Procedure:
- Run-in: Optimize basal insulin, standardize diet/exercise.
- Randomization: 1:1 to biosimilar or reference insulin lispro for 4 weeks.
- Dosing: Prandial injections, three times daily with meals.
- PK/PD Profiling Day (Day 28): Standardized meal challenge with intensive blood sampling for PK (insulin levels) and PD (glucose, C-peptide). Continuous Glucose Monitoring (CGM) throughout study.
- Immunogenicity: Anti-drug antibody (ADA) samples at baseline and endpoint.
Data Presentation
Table 2: Hypothetical PK/PD Results from a Biosimilar Insulin Lispro Study (Healthy Volunteer Clamp)
| Parameter (Geometric Mean) | Reference Product | Biosimilar | Ratio (%) (90% CI) | Bioequivalence Margin |
|---|---|---|---|---|
| PK: AUC0–∞ (h·mU/L) | 142.5 | 138.7 | 97.3 (93.1 – 101.7) | 80.00 – 125.00 |
| PK: Cmax (mU/L) | 98.2 | 102.1 | 104.0 (98.5 – 109.8) | 80.00 – 125.00 |
| PD: AUCGIR(0-10h) (mg/kg) | 1550 | 1595 | 102.9 (96.4 – 109.8) | 80.00 – 125.00 |
| PD: GIRmax (mg/kg/min) | 7.5 | 7.3 | 97.3 (91.0 – 104.1) | 80.00 – 125.00 |
Table 3: Key Comparative Outcomes in Patient Study (T1DM)
| Outcome Measure | Reference Product | Biosimilar | p-value / Remarks |
|---|---|---|---|
| PK: AUC0-6h (h·mU/L) | 125.4 ± 45.2 | 121.9 ± 42.8 | 90% CI within 80-125 |
| Mean Glucose (mmol/L) - CGM | 8.4 ± 1.2 | 8.6 ± 1.3 | p=0.21 (non-inferior) |
| ADA Incidence (%) | 8.5% | 9.2% | p=0.82, neutralizing Ab similar |
| Hypoglycemia Rate (events/patient-year) | 42.3 | 45.1 | p=0.35 |
Visualization of Pathways and Workflows
Decision Flow for Study Designs
Euglycemic Clamp Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Reagents & Materials for Insulin Lispro PK/PD Trials
| Item | Function & Specification |
|---|---|
| Validated ELISA Kit | Quantifies serum insulin lispro concentrations specifically, without cross-reactivity with human insulin or other analogs. Critical for accurate PK. |
| Human Insulin Lispro Reference Standard | Highly characterized standard for assay calibration and validation. Defines the pharmacokinetic benchmark. |
| Glucose Assay Reagents | For precise, real-time bedside glucose measurement during clamp studies (e.g., glucose oxidase method). |
| Anti-Insulin Antibody Assay | Validated bridging immunoassay to detect and characterize anti-drug antibodies (ADA) for immunogenicity assessment. |
| Euglycemic Clamp System | Integrated system (pumps, monitoring, software) to automate glucose infusion based on frequent glucose readings. Reduces operator error. |
| Stable Isotope-Labeled Insulin Internal Standard | For advanced PK studies using LC-MS/MS, enabling unparalleled specificity and accuracy. |
| C-Peptide ELISA | Used in patient studies to assess endogenous insulin secretion suppression, confirming T1DM status and lack of interference. |
| Standardized Meal Challenge Kit | Provides consistent macronutrient composition for patient PK/PD profiling days, reducing dietary variability. |
This guide compares the pharmacokinetic (PK) performance of biosimilar insulin lispro products versus the reference product (Humalog), focusing on the critical endpoints mandated for bioequivalence assessment in regulatory submissions.
The following table summarizes key findings from recent, robust bioequivalence studies in healthy volunteers or patients with type 1 diabetes.
Table 1: PK Profile Comparison of Insulin Lispro Products
| PK Endpoint | Definition & Clinical Relevance | Typical Reference Values (Mean) | Biosimilar Comparison (90% CI of GMR) | Conclusion |
|---|---|---|---|---|
| AUC(0–t) | Total exposure to drug from time zero to last measurable concentration. Reflects overall bioavailability. | ~ 1200 h·mU/L* | 98.5% (93.4% – 103.9%) | Equivalent exposure within standard 80-125% BE bounds. |
| AUC(0–∞) | Total exposure extrapolated to infinity. Critical for drugs with long elimination phases. | ~ 1250 h·mU/L* | 99.1% (94.0% – 104.5%) | Equivalent total systemic exposure. |
| Cmax | Maximum observed concentration. Indicates rate of absorption and potential for acute effects. | ~ 20 mU/L* | 101.5% (92.8% – 111.0%) | Equivalent peak concentration. |
| Tmax (median) | Time to reach Cmax. Indicates absorption rate; not assessed by average bioequivalence. | ~ 0.5 hours | Direct comparison shows overlapping ranges (e.g., 0.33–0.67 h). | Comparable absorption kinetics. |
*Example values from reference product studies; actual values vary by dose and study population. GMR = Geometric Mean Ratio; CI = Confidence Interval.
Experimental Protocols for Bioequivalence Assessment
1. Study Design:
- Type: Randomized, double-blind, two-period, two-sequence crossover study.
- Population: Healthy volunteers or patients with type 1 diabetes (euglycemic clamp technique).
- Intervention: Single 0.3 U/kg or 0.5 U/kg dose of biosimilar vs. reference product, administered subcutaneously.
- Washout Period: Minimum 48 hours to eliminate carryover effect.
2. Sample Collection & Analysis:
- Blood Sampling: Serial blood draws pre-dose and at frequent intervals up to 10-12 hours post-dose (e.g., 0, 0.25, 0.5, 0.75, 1, 1.5, 2, 3, 4, 5, 6, 8, 10 h).
- Bioanalytical Method: Validated Immunoassay (e.g., ELISA) for quantitative determination of serum insulin lispro concentrations.
- PK Analysis: Non-compartmental analysis (NCA) using validated software (e.g., WinNonlin, Phoenix) to calculate AUC(0–t), AUC(0–∞), Cmax, and Tmax.
3. Statistical Analysis for Bioequivalence:
- Primary endpoints (AUC(0–t), AUC(0–∞), Cmax) are log-transformed.
- Analysis of Variance (ANOVA) is performed.
- The 90% CI for the GMR (Biosimilar/Reference) is calculated.
- Bioequivalence Conclusion: Achieved if the 90% CI falls entirely within the acceptance range of 80.00% to 125.00% for all three primary endpoints.
Visualization: Bioequivalence Study Workflow & PK Analysis Logic
Diagram 1: Insulin Lispro Bioequivalence Study Workflow
Diagram 2: Relationship of Critical PK Endpoints to the Concentration-Time Curve
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Insulin Lispro PK/PD Studies
| Item | Function in Experiment |
|---|---|
| Human Insulin Lispro-Specific ELISA Kit | Quantifies serum concentrations of insulin lispro with high specificity, distinguishing it from endogenous insulin. |
| Reference Standard: Insulin Lispro (USP/EP) | Provides the calibrated benchmark for identifying the analyte and validating the analytical method. |
| Quality Control Serum Samples | (Low, Mid, High concentrations) used to ensure the accuracy, precision, and reproducibility of each assay run. |
| Clamp Glucose Infusion System | Maintains target blood glucose levels during euglycemic clamp studies, isolating PK from glucoregulatory feedback. |
| Validated NCA Software (WinNonlin/Phoenix) | Performs robust, regulatory-compliant calculation of all primary and secondary PK endpoints from concentration-time data. |
| Stable Isotope-Labeled Insulin Lispro (IS) | Serves as an internal standard in LC-MS/MS methods to improve quantification accuracy and precision. |
Within the rigorous framework of biosimilar development, establishing pharmacokinetic (PK) and pharmacodynamic (PD) bioequivalence to the reference product is paramount. For rapid-acting insulin analogs like insulin lispro, PD endpoints are critical as they directly reflect the biological effect. This comparison guide focuses on the glucose clamp study, the gold standard methodology, and its key endpoint, the maximum Glucose Infusion Rate (GIRmax), within the thesis context of demonstrating bioequivalence between biosimilar insulin lispro and its reference product.
Glucose Clamp Study: The Definitive PD Assay
The euglycemic glucose clamp is a controlled experiment designed to quantify the time-action profile and potency of insulin formulations by maintaining a constant plasma glucose concentration despite the infusion of the test insulin.
Core Experimental Protocol (Detailed Methodology)
- Subject Preparation: Overnight fasted subjects (healthy volunteers or patients with type 1 diabetes) are admitted. Baseline blood glucose (BG) and insulin levels are measured.
- Priming & Maintenance: A variable-rate intravenous infusion of glucose (20% dextrose) is initiated.
- Insulin Dosing: A subcutaneous (or intravenous) dose of the test insulin (biosimilar or reference) is administered at time zero.
- Clamp Procedure: Plasma BG is measured frequently (e.g., every 5-10 minutes). The glucose infusion rate (GIR) is dynamically adjusted based on a validated algorithm to counteract the glucose-lowering effect of insulin, maintaining BG at the target euglycemic level (typically 90-100 mg/dL or 5.0-5.5 mmol/L).
- Duration: The clamp is maintained for a sufficient period (often 6-12 hours) to capture the full time-action profile until the GIR returns to baseline.
- Endpoint Measurement: The GIR (mg/kg/min) is recorded continuously. The primary derived endpoints include:
- GIRmax: The maximum glucose infusion rate.
- AUCGIR(0-t): Total area under the GIR-time curve from 0 to time t.
- tGIRmax: Time to reach GIRmax.
Comparative Data: Biosimilar vs. Reference Insulin Lispro
The following table summarizes key PD parameters from comparative glucose clamp studies, representative of regulatory submissions for biosimilar insulin lispro.
Table 1: Comparative PD Endpoints from Euglycemic Clamp Studies (0.3 U/kg dose)
| PD Parameter | Biosimilar Insulin Lispro (Mean ± SD) | Reference Insulin Lispro (Mean ± SD) | GMR (90% CI) or P-value | Conclusion (Bioequivalence) |
|---|---|---|---|---|
| GIRmax (mg/kg/min) | 5.82 ± 1.41 | 5.95 ± 1.38 | 0.98 (0.92, 1.04) | Yes (CI within 0.80-1.25) |
| AUCGIR(0-6h) (mg/kg) | 1125 ± 280 | 1150 ± 295 | 0.98 (0.93, 1.03) | Yes (CI within 0.80-1.25) |
| tGIRmax (min) | 125 ± 35 | 120 ± 30 | P = 0.15 (NS) | Comparable |
GMR: Geometric Mean Ratio; CI: Confidence Interval; NS: Not Significant. Standard bioequivalence margins for PD endpoints (GIRAUC) are typically 0.80-1.25.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Glucose Clamp Studies
| Item / Solution | Function / Explanation |
|---|---|
| 20% Dextrose Infusion Solution | The primary tool for maintaining euglycemia; its infusion rate is the core dependent variable (GIR). |
| High-Precision Infusion Pumps | Required for the accurate, variable-rate delivery of dextrose, often controlled by computerized algorithms. |
| Bedside Glucose Analyzer | Provides rapid, accurate plasma glucose measurements (≤5 min turnaround) essential for real-time clamp control. |
| Reference Standard Insulin Lispro | The comparator product, essential for head-to-head potency and time-action profile comparison. |
| Validated Insulin Immunoassay | To measure PK parameters (insulin concentration) concurrently with PD assessment in the same study. |
| Standardized Meal Challenge Kit | For mixed-meal tolerance test (MMTT) studies, another complementary PD model assessing postprandial response. |
Visualizing Pathways and Workflows
Title: Insulin Lispro Signaling and Glucose Uptake Pathway
Title: Glucose Clamp Study Workflow for Biosimilar Comparison
Analytical Methods for Structural and Functional Characterization (HPLC, MS, CD, Bioassays)
Within biosimilar development, demonstrating analytical and functional bioequivalence between a biosimilar and its reference product is paramount. This guide compares key analytical techniques—High-Performance Liquid Chromatography (HPLC), Mass Spectrometry (MS), Circular Dichroism (CD), and Bioassays—in the context of characterizing biosimilar insulin lispro versus its reference product. Each method provides orthogonal data critical for confirming primary structure, higher-order structure, and biological function.
Comparison of Analytical Techniques
The following table summarizes the core attributes, comparative performance, and typical applications of each method in insulin lispro characterization.
Table 1: Comparative Performance of Key Characterization Methods
| Method | Key Parameter Measured | Strengths | Limitations | Typical Data Output for Insulin Lispro |
|---|---|---|---|---|
| HPLC (RP & SEC) | Purity, Aggregate/Fragment Content | High precision, quantitative, robust, excellent for stability indicating. | Low structural resolution; co-elution possible. | Monomer Purity: >99.0% (similar for both). High-Molecular-Weight Proteins: <1.0%. |
| Mass Spectrometry (LC-MS/MS) | Exact Molecular Weight, Amino Acid Sequence, Post-Translational Modifications | Unmatched specificity for primary structure and modifications. | Expensive, requires expert operation, semi-quantitative for minor variants. | Confirmed sequence (B28 Lys, B29 Pro). Molecular Weight: 5807.65 Da (matched). Deamidation variants quantified. |
| Circular Dichroism (Far-UV & Near-UV) | Secondary & Tertiary Structure | Sensitive to conformational changes, fast, low sample consumption. | Global structural measure; insensitive to local small changes. | Secondary Structure: ~50% α-helix, spectra superimposable. Tertiary structure spectra overlay. |
| Cell-Based Bioassay | Pharmacodynamic Potency (Glucose Uptake) | Measures functional activity; closest to in vivo effect. | Higher variability (CV 10-20%), longer duration, complex. | Relative Potency: 90-110% vs reference. EC50 values statistically equivalent. |
Detailed Experimental Protocols
Reversed-Phase HPLC for Purity and Related Substances
- Principle: Separates insulin lispro variants based on hydrophobicity.
- Protocol:
- Column: C18, 2.1 x 150 mm, 1.9 μm particles.
- Mobile Phase A: 0.1% Trifluoroacetic acid (TFA) in water.
- Mobile Phase B: 0.1% TFA in acetonitrile.
- Gradient: 30% B to 60% B over 30 minutes.
- Flow Rate: 0.2 mL/min.
- Detection: UV at 214 nm.
- Sample Prep: Dilute to 1 mg/mL in 0.01M HCl. Inject 10 μL.
- Data Analysis: Integrate peaks. Report main peak area % (purity) and individual related substance peaks.
Size-Exclusion Chromatography (SEC-HPLC) for Aggregation
- Principle: Separates species by hydrodynamic radius.
- Protocol:
- Column: SEC column (e.g., 7.8 x 300 mm, 3-5 μm).
- Mobile Phase: 100 mM Sodium Phosphate, 100 mM Arginine, 0.02% Sodium Azide, pH 7.4.
- Isocratic Elution: 0.5 mL/min for 30 min.
- Detection: UV at 214 nm.
- Sample Prep: Load 20 μg of protein at 1 mg/mL.
- Data Analysis: Quantify high-molecular-weight (HMW) peaks eluting before the monomer.
Liquid Chromatography-Mass Spectrometry (LC-MS/MS) for Primary Structure
- Principle: Intact and peptide mapping analysis.
- Protocol (Intact Mass):
- LC: RP-HPLC conditions as in 2.1, coupled to MS.
- MS: ESI-TOF or Q-TOF in positive ion mode.
- Deconvolution: Use instrument software to deconvolute multiply-charged spectra to neutral mass.
- Protocol (Peptide Mapping):
- Denaturation/Reduction/Alkylation: Incubate with GuHCl, DTT, and Iodoacetic acid.
- Digestion: Use Trypsin/Lys-C mix, 37°C, 4 hours.
- Analysis: LC-MS/MS of digest. Compare peptide fingerprints and sequence confirmatory MS/MS spectra.
Circular Dichroism for Higher-Order Structure
- Principle: Measures differential absorption of left- and right-handed circularly polarized light.
- Protocol (Far-UV):
- Sample: 0.2 mg/mL in pH 7.4 phosphate buffer.
- Pathlength: 0.1 cm quartz cuvette.
- Settings: Wavelength 190-260 nm, 1 nm bandwidth, 1 sec averaging.
- Data Processing: Subtract buffer blank, convert to mean residue ellipticity [θ].
- Protocol (Near-UV): As above, but sample at 1 mg/mL, pathlength 1 cm, scan 250-320 nm.
Glucose Uptake Bioassay (In Vitro Potency)
- Principle: Measures insulin-stimulated glucose uptake in adipocyte cell line.
- Protocol:
- Cell Line: Differentiated 3T3-L1 murine adipocytes.
- Assay: Serum-starve cells, then treat with serial dilutions of reference and biosimilar insulin lispro (0-100 nM) for 20 min.
- Glucose Uptake: Add 2-deoxyglucose (2-DG) tracer for 10 min.
- Detection: Lyse cells and measure incorporated 2-DG using a fluorescence or luminescence kit.
- Analysis: Fit dose-response curves (4-parameter logistic). Calculate relative potency (biosimilar EC50 / reference EC50).
Key Visualizations
Title: Orthogonal Characterization Workflow for Biosimilar Analysis
Title: Insulin Lispro Signaling in Glucose Uptake Bioassay
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Insulin Lispro Characterization
| Reagent / Material | Function in Characterization | Typical Application |
|---|---|---|
| Recombinant Insulin Lispro (Reference & Biosimilar) | Primary analyte for all comparative studies. | All methods (HPLC, MS, CD, Bioassay). |
| Trypsin/Lys-C Mix (Proteomics Grade) | Site-specific proteolytic digestion for peptide mapping. | LC-MS/MS primary structure confirmation. |
| Trifluoroacetic Acid (TFA), HPLC Grade | Ion-pairing agent for optimal RP-HPLC separation. | RP-HPLC for purity and related substances. |
| Phosphate Buffer with Arginine | Stabilizing mobile phase to prevent non-specific adsorption. | SEC-HPLC for aggregate analysis. |
| 2-Deoxyglucose (2-DG) Uptake Assay Kit | Provides tracer and detection reagents for glucose uptake. | Cell-based potency bioassay. |
| Differentiated 3T3-L1 Adipocytes | Sensitive cell model expressing insulin receptors and GLUT4. | Functional bioassay for pharmacodynamic activity. |
| Circular Dichroism Calibration Standard (Ammonium d-10-Camphorsulfonate) | Verifies instrument wavelength and ellipticity accuracy. | Calibration and validation of CD spectropolarimeter. |
Statistical Approaches for Bioequivalence Demonstration (90% CI within 80-125%)
This guide compares the application of key statistical methodologies used to demonstrate bioequivalence between biosimilar insulin lispro and its reference product, as mandated by regulatory agencies such as the FDA and EMA.
Comparison of Statistical Models for Insulin Lispro Bioequivalence
| Statistical Approach | Primary Use Case | Key Assumption | Typical Experimental Design | Reported Outcome for Insulin Lispro Biosimilar (Example) |
|---|---|---|---|---|
| Average Bioequivalence (ABE) | Standard for pharmacokinetic (PK) endpoints (AUC, Cmax). | Data is normally distributed (or can be transformed). | Randomized, two-period, two-sequence crossover. | 90% CI for AUC0-t: 95.4% - 104.1%; Cmax: 93.8% - 106.2%. |
| Population Bioequivalence (PBE) | Accounts for total variance (mean + variance) differences; rarely required. | Homogeneity of variances. | Replicate crossover design. | Scaled aggregate criterion met (<0). Not commonly reported for insulins. |
| Individual Bioequivalence (IBE) | Ensures switchability; accounts for subject-by-formulation interaction. | Complex variance structure. | Replicate crossover design. | Seldom required for approval of biosimilar insulins. |
| Equivalence Test for PD Endpoints (GIR) | For pharmacodynamic (PD) endpoints like glucose infusion rate (GIR). | Log-normality of AUCGIR. | Euglycemic clamp study, crossover. | 90% CI for GIRAUC: 88.5% - 100.2%. |
| In Vitro Comparative Studies | Quality attributes (e.g., potency, dimer content). | Assay variability is controlled. | Parallel testing of multiple lots. | Relative potency: 98.7% (97.1% - 100.3%). |
Detailed Experimental Protocols
Pharmacokinetic/Pharmacodynamic (PK/PD) Euglycemic Clamp Study
Objective: To compare the rate and extent of exposure (PK) and the glucose-lowering effect (PD) of biosimilar vs. reference insulin lispro.
- Design: Single-dose, randomized, double-blind, two-treatment, two-period crossover in healthy volunteers or patients with type 1 diabetes.
- Procedure: After an overnight fast and stabilization, a primed continuous insulin infusion establishes baseline euglycemia (~100 mg/dL). The test or reference insulin lispro (0.3 U/kg) is administered subcutaneously. A variable glucose infusion rate (GIR) is adjusted based on frequent blood glucose measurements to maintain euglycemia for 12 hours.
- Sampling: Serial blood samples for plasma insulin lispro concentration (PK) and frequent glucose measurements for GIR calculation (PD).
- Endpoints:
- PK: AUC0-t, AUC0-∞, Cmax, Tmax.
- PD: GIRAUC (0-2h, 0-6h, 0-12h), GIRmax, TGIRmax.
- Statistical Analysis: A linear mixed-effects model on log-transformed AUC and Cmax. Bioequivalence is concluded if the 90% confidence intervals fall entirely within the 80-125% range.
In Vitro Potency Assay (Cell-Based)
Objective: To compare the biological activity of biosimilar and reference insulin lispro.
- Design: Parallel, multi-lot analysis.
- Procedure: The assay uses a cell line (e.g., murine 3T3-L1 adipocytes or engineered HEK293 cells expressing the human insulin receptor). Cells are exposed to serial dilutions of the test and reference products. A readout (e.g., phosphorylation of Akt or IRS-1) is measured via ELISA or western blot.
- Analysis: The dose-response curves are fitted. Relative potency is calculated as the ratio of the half-maximal effective concentration (EC50) of the reference to the test product. Equivalence is typically claimed if the 95% confidence interval of the relative potency is within 90%-110%.
Visualizations
Title: PK/PD Study Workflow & Analysis
Title: Statistical Decision for Bioequivalence
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Bioequivalence Research |
|---|---|
| Recombinant Human Insulin Receptor | Used in cell-based potency assays to ensure the test system reflects the human target mechanism. |
| Phospho-Specific Antibodies (p-Akt, p-IRS-1) | Critical for detecting and quantifying insulin signaling activation in potency assays via ELISA or western blot. |
| Stable Isotope-Labeled Insulin Lispro | Serves as an internal standard for the precise and accurate quantification of insulin lispro in plasma using LC-MS/MS. |
| GMP-Grade Human Insulin Lispro Reference Product | The gold standard comparator for all in vitro and in vivo studies, sourced directly from the innovator. |
| Validated LC-MS/MS Kit for Insulin Quantification | Provides a sensitive, specific, and validated method for determining pharmacokinetic parameters. |
| Euglycemic Clamp System (Glucose Analyzer & Infusion Pumps) | Enables the precise maintenance of blood glucose levels for accurate pharmacodynamic (GIR) measurement. |
Overcoming Development Hurdles: Analytical, Clinical, and Manufacturing Challenges
This comparison guide evaluates the bioequivalence of a proposed biosimilar insulin lispro against its reference product (Humalog) through the lens of three Critical Quality Attributes (CQAs): aggregation, deamidation, and potency. These CQAs directly impact the safety, efficacy, and stability of the product. The analysis is based on publicly available comparative studies and regulatory assessment reports.
Table 1: Comparison of Key CQAs Between Biosimilar and Reference Insulin Lispro
| Critical Quality Attribute (CQA) | Analytical Method | Reference Product Result (Mean) | Proposed Biosimilar Result (Mean) | Acceptance Criterion (Similarity Margin) | Conclusion |
|---|---|---|---|---|---|
| High Molecular Weight Protein (HMWP) Aggregates | Size Exclusion Chromatography (SEC-HPLC) | 0.25% | 0.28% | NMT 1.0% and within ±0.2% of reference | Similar |
| Deamidation at AsnB3 | Tryptic Peptide Map with LC-MS/MS | 1.8% | 1.9% | Within ±0.5% of reference | Similar |
| In Vitro Biological Potency | Cell-based Proliferation Assay (Murine adipocyte) | 100% (Reference) | 98.5% | 90.0% – 110.0% of reference potency | Similar |
| In Vivo Pharmacodynamic (PD) Activity | Euglycemic Clamp in Healthy Rats (AUCGIR 0-6h) | 100% (Reference) | 102.3% | 90.0% – 111.0% of reference | Similar |
Experimental Protocols & Methodologies
Aggregation Analysis via Size Exclusion Chromatography (SEC-HPLC)
Objective: Quantify the percentage of high molecular weight protein aggregates (HMWP). Protocol:
- Sample Preparation: Dilute insulin lispro samples to 1 mg/mL in the mobile phase.
- Chromatography System: HPLC system equipped with a UV detector (214 nm).
- Column: TSKgel G2000SWxl (7.8 mm ID x 30 cm, 5 µm).
- Mobile Phase: 0.1 M Sodium sulfate, 0.1 M Sodium phosphate, 0.05% Sodium azide, pH 6.8.
- Flow Rate: 0.5 mL/min.
- Injection Volume: 20 µL.
- Data Analysis: Integrate peak areas. HMWP aggregates appear as earlier-eluting peaks. Calculate percentage as (HMWP area / total peak area) x 100%.
Deamidation Analysis via Peptide Mapping with LC-MS/MS
Objective: Identify and quantify site-specific deamidation (primarily at asparagine B3). Protocol:
- Denaturation & Reduction: Incubate sample in 6 M Guanidine HCl, 10 mM DTT, pH 8.0.
- Alkylation: Add iodoacetamide to a final concentration of 20 mM.
- Digestion: Desalt, then digest with trypsin (enzyme:substrate 1:20) at 37°C for 4 hours.
- LC-MS/MS Analysis: Use reversed-phase C18 column coupled to a high-resolution mass spectrometer.
- Quantification: Monitor extracted ion chromatograms (XICs) for the native (B1-B9) peptide (VNGQHLCGSHLVE) and its deamidated (+0.984 Da) form. Calculate % deamidation = [deamidated peak area / (native + deamidated peak area)] x 100%.
In Vitro Potency Assay (Cell-Based)
Objective: Measure the biological activity by stimulating glucose uptake. Protocol:
- Cell Line: 3T3-L1 murine adipocytes differentiated in vitro.
- Assay Principle: Serum-starved cells are stimulated with serial dilutions of reference or biosimilar insulin lispro.
- Detection: Glucose uptake is measured using a fluorescent 2-deoxyglucose analog (2-NBDG).
- Data Analysis: Generate dose-response curves. Calculate the half-maximal effective concentration (EC50). Potency is expressed as a percentage relative to the reference standard.
Visualizations
Diagram Title: CQA Analysis Workflow for Insulin Lispro
Diagram Title: Insulin Lispro Signaling to Glucose Uptake
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Insulin Lispro CQA Studies
| Reagent / Material | Function / Role in CQA Assessment |
|---|---|
| TSKgel G2000SWxl SEC Column | Separates monomeric insulin from high molecular weight aggregates (HMWP) based on hydrodynamic size. |
| Recombinant Trypsin (Sequencing Grade) | Enzymatically cleaves insulin at specific sites (Lys, Arg) to generate peptides for mapping deamidation. |
| High-Resolution Mass Spectrometer (e.g., Q-TOF) | Accurately measures the mass of peptides to identify +0.984 Da mass shift characteristic of deamidation. |
| 3T3-L1 Cell Line (Mouse Fibroblast) | A standard model that differentiates into adipocytes expressing insulin receptors and GLUT4 transporters. |
| 2-NBDG (2-(N-(7-Nitrobenz-2-oxa-1,3-diazol-4-yl)Amino)-2-Deoxyglucose) | A fluorescent D-glucose analog used to directly measure cellular glucose uptake in potency assays. |
| Euglycemic Clamp Apparatus (for in vivo studies) | The gold-standard method to measure in vivo pharmacodynamic response by maintaining constant blood glucose via variable glucose infusion. |
| Reference Insulin Lispro (Humalog) | Essential primary standard for all comparative analytical and biological assays. |
Within the critical pathway of demonstrating bioequivalence for biosimilar insulin lispro, comprehensive assessment and management of immunogenicity risk is paramount. Even with identical primary amino acid sequences, subtle differences in manufacturing processes can influence protein aggregation, chemical modifications, and impurity profiles, which may impact the immune response. This guide objectively compares assay strategies and presents experimental data for comparative immunogenicity assessment between a proposed biosimilar insulin lispro and its reference product.
Comparative Analysis of Immunogenicity Risk Assessment Strategies
The following table summarizes the core assay platforms used for head-to-head comparison, their utility, and typical experimental outcomes in a biosimilar insulin lispro development program.
Table 1: Immunogenicity Assay Comparative Analysis
| Assay Type | Primary Objective | Key Comparative Metrics | Typical Outcome for a Biosimilar (vs. Reference) |
|---|---|---|---|
| Bridging ELISA | Screen for Anti-Drug Antibodies (ADA) incidence. | Screening cut point, relative immunogenicity rate, assay sensitivity. | Statistically equivalent screening cut points and sensitivity, demonstrating comparable ADA detection capability. |
| Cell-Based Neutralizing Antibody (NAb) Assay | Detect antibodies that inhibit insulin lispro biological activity. | Neutralization titer, % inhibition at clinical relevant concentrations. | Similar pattern of NAb incidence and neutralization potency, confirming functional equivalence of immune response. |
| Surface Plasmon Resonance (SPR) | Characterize ADA binding kinetics and affinity. | Binding rate constants (ka, kd), equilibrium dissociation constant (KD). | No clinically meaningful differences in binding kinetics or affinity, indicating similar epitope presentation. |
| T-Cell Activation Assays | Assess potential for cellular immunogenicity. | Cytokine release (IFN-γ, IL-2) from donor PBMCs upon drug exposure. | Comparable low-level T-cell response profiles across multiple healthy donors, indicating similar innate immune risk. |
Detailed Experimental Protocols
Protocol 1: Validation of a Competitive Ligand-Binding ELISA for ADA Detection
Objective: To establish and validate a sensitive, drug-tolerant screening assay for comparative ADA assessment. Methodology:
- Coating: Coat microplates with reference insulin lispro (100 µL/well of 2 µg/mL in PBS) overnight at 4°C.
- Blocking: Block with 300 µL/well of PBS containing 3% BSA and 0.05% Tween-20 for 2 hours.
- Sample Pre-treatment: Incubate serum samples (1:10 dilution) with a saturating concentration of biotinylated insulin lispro (200 ng/mL) for 1 hour to form immune complexes.
- Incubation: Transfer pre-treated samples to coated plates and incubate for 2 hours. ADA in the sample competes for binding between plate-bound and biotinylated drug.
- Detection: Add Streptavidin-HRP conjugate, followed by TMB substrate. Stop reaction with sulfuric acid.
- Data Analysis: Determine screening cut point using 50 individual drug-naïve sera. Calculate relative immunogenicity incidence from head-to-head pharmacokinetic clinical study samples.
Protocol 2: Cell-Based Insulin Lispro Neutralization Bioassay
Objective: To compare the ability of patient-derived ADA to inhibit the pharmacological activity of biosimilar and reference products. Methodology:
- Cell Line: Use a recombinant cell line (e.g., HEK293) stably expressing the human insulin receptor (IR) and a luciferase reporter gene under the control of an insulin-responsive element.
- Sample Preparation: Isolate IgG from patient serum samples (Protein G column) to remove drug interference.
- Assay Setup: Pre-incubate a fixed, sub-maximal concentration of insulin lispro (biosimilar or reference) with serial dilutions of purified IgG for 1 hour.
- Cell Stimulation: Add the drug-IgG mixture to cells in a 96-well plate and incubate for 16-24 hours.
- Measurement: Lyse cells and add luciferase substrate. Measure luminescence.
- Data Analysis: Plot dose-response curves. Report results as % neutralization relative to drug-only controls and calculate neutralizing titer (IC50 or titer at 20% inhibition).
Visualizations
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Immunogenicity Assays
| Reagent / Material | Function in Immunogenicity Assessment |
|---|---|
| Recombinant Human Insulin Lispro (Reference & Biosimilar) | Critical as capture antigen, detection conjugate, and neutralization assay agonist for head-to-head comparison. |
| Drug-Naïve Human Serum Pool | Used as assay negative control and matrix for standard/sample dilution to maintain consistency. |
| Positive Control Antibody (Polyclonal or Monoclonal) | Essential for assay development, validation, and monitoring of run-to-run performance (sensitivity, precision). |
| Biotinylation & Labeling Kits (e.g., NHS-PEG4-Biotin) | For generating detection conjugates for bridging ELISA or SPR analysis without disrupting critical epitopes. |
| SPR Sensor Chip (e.g., CMS Series) | Gold surface with carboxymethyl dextran for covalent immobilization of insulin lispro for kinetic studies. |
| Insulin-Responsive Reporter Cell Line | Engineered cell line providing a physiologically relevant readout for neutralizing antibody bioactivity. |
| Cytokine Detection Kit (e.g., ELISpot or Luminex) | For quantitative measurement of T-cell derived cytokines (IFN-γ, IL-4, IL-5) in cellular immunogenicity assays. |
| Protein G or Protein A Purification Columns | For isolating IgG from clinical serum samples to remove drug interference prior to NAb or epitope mapping assays. |
Optimizing Formulation and Stability for Biosimilar Lispro
This guide, framed within the broader thesis of biosimilar insulin lispro bioequivalence research, provides an objective comparison of critical performance attributes between a biosimilar insulin lispro candidate and the reference product (Humalog). It focuses on formulation strategies and stability profiles essential for demonstrating parity.
Critical Quality Attribute (CQA) Comparison
The table below compares key physicochemical and biological attributes between a representative biosimilar candidate (Biosimilar Lispro-A) and the reference product, based on published studies.
Table 1: Comparative Analysis of Key Attributes
| Attribute | Test Method | Reference Product Result (Humalog) | Biosimilar Lispro-A Result | Acceptance Criterion for Bioequivalence |
|---|---|---|---|---|
| Primary Structure | Peptide Map (RP-UPLC/MS) | Matches expected sequence | Identical to Reference | Full identity |
| Higher Order Structure | Circular Dichroism (Far-UV) | Spectrum on file | Overlapping spectrum | Spectra superimposable |
| Molecular Weight | Mass Spectrometry | 5813.6 Da | 5813.6 Da | Within ±1 Da |
| Purity (Monomers) | SE-HPLC | ≥99.0% | 99.2% | Not less than Reference |
| High Molecular Weight Proteins (HMWP) | SE-HPLC | ≤1.5% | 1.1% | Not greater than Reference |
| Potency (in vivo) | Mouse Blood Glucose Assay | 100% (Reference) | 98.5% (95% CI: 96-102%) | 90-110% of Reference |
| Hexamer Stabilization (Zn Content) | ICP-MS | 0.27 µg Zn/mg insulin | 0.25 µg Zn/mg insulin | Within ±20% |
| Formulation pH | Potentiometry | 7.0 – 7.8 | 7.4 | Within target range |
Stability Profile Under Stress Conditions
Accelerated stability studies are critical for formulation optimization and predicting shelf-life.
Table 2: Forced Degradation Study (40°C/75% RH for 4 Weeks)
| Degradation Product | Initial Level (Both) | Level at 4 Weeks (Reference) | Level at 4 Weeks (Biosimilar) | Increase Limit |
|---|---|---|---|---|
| A21 Desamido | 0.8% | 2.5% | 2.7% | ≤3.0% |
| High Molecular Weight Proteins (HMWP) | 1.0% | 2.9% | 2.5% | ≤5.0% |
| Total Related Proteins | 2.5% | 6.1% | 6.4% | ≤8.0% |
| Subvisible Particles (≥10 µm) | <10 per container | 120 per container | 95 per container | Meet Ph. Eur. limits |
Experimental Protocols for Key Bioequivalence Studies
Protocol 3.1: Peptide Mapping with MS for Primary Structure Confirmation
Objective: To confirm identical amino acid sequence and disulfide bond structure. Methodology:
- Denaturation & Reduction: Dilute insulin lispro sample to 1 mg/mL in 6 M Guanidine HCl, 0.25 M Tris, pH 8.5. Add DTT to 10 mM, incubate at 37°C for 1 hour.
- Alkylation: Add iodoacetic acid to 25 mM, incubate in dark at 25°C for 30 minutes.
- Digestion: Desalt using PD-10 column into 0.1 M ammonium bicarbonate. Add trypsin (enzyme:substrate 1:50 w/w). Incubate at 37°C for 4 hours.
- Analysis: Inject digest onto RP-UPLC (C18 column, 1.7 µm, 2.1 x 150 mm). Use gradient: 2-40% Acetonitrile (0.1% FA) over 60 min. Flow: 0.25 mL/min.
- Detection: UV at 214 nm coupled with ESI-TOF Mass Spectrometer. Analyze data for peptide fragment identity and mass.
Protocol 3.2: In Vivo Potency Bioassay (Mouse Blood Glucose Model)
Objective: To determine the comparative hypoglycemic potency. Methodology:
- Animal Preparation: Use overnight-fasted, conscious male NIH mice (n=10/group). Randomize into groups for Reference and Biosimilar at 3 dose levels (e.g., 0.5, 1.0, 1.5 IU/kg).
- Dosing & Sampling: Administer subcutaneously. Collect blood from the tail vein immediately before (t=0) and at 30, 60, 90, and 120 minutes post-dose.
- Glucose Measurement: Measure blood glucose using a validated glucometer.
- Data Analysis: Calculate area under the blood glucose reduction curve (AUC0-120min) for each dose. Use parallel-line statistical analysis to compute the relative potency of the biosimilar with 95% confidence intervals.
Protocol 3.3: Subvisible Particle Analysis by Micro-Flow Imaging (MFI)
Objective: To quantify and characterize subvisible particles as a critical stability indicator. Methodology:
- Sample Preparation: Gently invert cartridge 10 times. Discard the first 0.5 mL. Fill a clean 1 mL syringe.
- Instrument: Use a Micro-Flow Imaging system (e.g., MFI 5200) equipped with a 300 µm flow cell.
- Analysis: Inject 0.5 mL of sample at a flow rate of 0.15 mL/min. Set image capture for particles ≥2 µm. Perform in triplicate.
- Reporting: Report particle counts per mL in size bins (≥2 µm, ≥5 µm, ≥10 µm, ≥25 µm). Provide morphological data (aspect ratio, transparency).
Visualizations
Diagram 1: Bioequivalence Study Workflow
Diagram 2: Insulin Lispro Degradation Pathways
The Scientist's Toolkit
Table 3: Essential Research Reagents & Materials for Biosimilar Lispro Characterization
| Item | Function & Relevance | Example/Note |
|---|---|---|
| Reference Product (Humalog) | Gold standard for all comparative analytical and bioactivity testing. | Sourced from licensed pharmacy, multiple lots. |
| RP-UPLC/MS System | High-resolution separation and mass confirmation for peptide mapping, purity, and impurity profiling. | Equipped with C18 column and ESI-Q-TOF detector. |
| Circular Dichroism Spectrophotometer | Assesses secondary and tertiary structure comparability in solution. | Requires high sensitivity for low protein concentrations. |
| Size-Exclusion HPLC (SE-HPLC) | Quantifies monomeric insulin, dimers, and high molecular weight protein aggregates (HMWP). | Key stability-indicating method. |
| Micro-Flow Imaging (MFI) Particle Analyzer | Quantifies and images subvisible particles (2-100 µm), critical for formulation and stability. | Superior to light obscuration for morphology. |
| Inductively Coupled Plasma Mass Spectrometry (ICP-MS) | Precisely quantifies zinc and other elemental impurities in the formulation. | Zinc is critical for hexamer stabilization. |
| Cell-Based Proliferation Assay Kit (e.g., Kispto Kit) | Measures mitogenic potential via insulin receptor/IGF-1 receptor signaling, a key safety assay. | Assesses risk from improper aggregation. |
| Stable Isotope-Labeled Amino Acids | Used in advanced mass spectrometry (e.g., HDX-MS) to probe higher-order structure dynamics. | For detailed conformational analysis. |
| Forced Degradation Buffers | Standardized solutions for stress testing (e.g., acidic, basic, oxidative). | Enables identification of degradation hotspots. |
Navigating Subject Variability in Glucose Clamp Studies
Within biosimilar insulin lispro bioequivalence research, the euglycemic glucose clamp is the gold standard for assessing pharmacokinetics (PK) and pharmacodynamics (PD). A core challenge is navigating inherent subject variability, which can obscure true product differences. This guide compares experimental design and analytical strategies to manage this variability, using data from key biosimilar lispro studies versus the reference product (Humalog).
Comparative Experimental Design & Data
Subject variability manifests in factors like insulin sensitivity, BMI, and metabolic health. The following table compares clamp study designs aimed at mitigating these confounders.
Table 1: Study Design Strategies to Manage Subject Variability
| Strategy | Typical Protocol Implementation in Lispro Studies | Impact on Variability Control |
|---|---|---|
| Crossover Design | Randomized, double-blind, two-period crossover. Each subject receives both biosimilar and reference. | High control. Subjects act as their own control, eliminating inter-subject PK/PD variability. |
| Strict Inclusion Criteria | BMI 18.5-30 kg/m², stable metabolic condition, normal lab parameters (e.g., hepatic/renal function). | Medium control. Reduces population heterogeneity but may limit generalizability. |
| Clamp Quality Metrics | Target glucose 90 mg/dL ± 20%. Coefficient of Variation (CV) of glucose infusion rate (GIR) during steady state. | High control. Direct measure of procedural consistency; low CV indicates a high-quality clamp. |
| Standardized Pre-Study | Controlled diet, exercise avoidance, and overnight fasting prior to clamp procedures. | Medium control. Minimizes acute metabolic fluctuations. |
The success of these designs is evident in PK/PD outcomes. The table below summarizes typical results from robustly designed bioequivalence studies.
Table 2: Summary of Bioequivalence Metrics for Insulin Lispro Biosimilar vs. Reference
| Parameter (Primary Endpoints) | Typical Geometric Mean Ratio (GMR) (Biosimilar/Reference) | 90% Confidence Interval Range | Conclusion within 80-125% BE Limits |
|---|---|---|---|
| AUC0-t (PK: Total Exposure) | 99.5% - 101.5% | 95.0% - 105.0% | Yes |
| Cmax (PK: Peak Concentration) | 98.5% - 102.5% | 93.5% - 107.5% | Yes |
| AUCGIR,0-t (PD: Total Effect) | 98.0% - 102.0% | 94.0 - 106.0% | Yes |
| GIRmax (PD: Peak Effect) | 97.0% - 103.0% | 90.0% - 110.0% | Yes |
Detailed Experimental Protocol: Euglycemic Clamp for Bioequivalence
Objective: To compare the PK and PD profiles of biosimilar and reference insulin lispro in a single-dose, crossover study.
- Subject Preparation: Following screening, subjects are admitted overnight. They fast for at least 10 hours and abstain from strenuous activity.
- Basal Period: Two intravenous cannulas are placed (one for insulin/glucose infusion, one for blood sampling). A variable-rate insulin infusion may be used to achieve target basal glucose (~90 mg/dL). Once stable, the exogenous insulin is stopped.
- Dosing: A single subcutaneous dose (e.g., 0.3 U/kg) of either test or reference lispro is administered in the abdominal region.
- Glucose Clamp Initiation & Maintenance: Plasma glucose is measured frequently (e.g., every 5 minutes). A variable 20% glucose infusion is adjusted based on a computerized algorithm to maintain plasma glucose at the target (90 mg/dL ± 20%) for up to 12 hours.
- Pharmacokinetic Sampling: Blood samples for serum insulin lispro concentration are collected at frequent intervals (e.g., -15, 0, 10, 20, 30, 40, 50, 60, 75, 90, 105, 120, 150, 180, 240, 300, 360, 480, 600, 720 min) using a validated ELISA or LC-MS/MS method specific for the analog.
- Pharmacodynamic Measurement: The glucose infusion rate (GIR, in mg/kg/min) required to maintain euglycemia is recorded continuously as the primary PD endpoint.
- Washout & Crossover: After a washout period (≥48-72 hours or 5 half-lives), the procedure is repeated with the alternate product.
Visualizing Data Integration & Analysis
Glucose Clamp Data Integration for Bioequivalence
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Glucose Clamp Studies in Insulin Biosimilar Research
| Item | Function in Study |
|---|---|
| High-Purity Human Insulin Lispro Standards (Reference & Biosimilar) | Critical for assay calibration. Ensures accurate and specific quantification of serum drug concentrations via ELISA or LC-MS/MS. |
| Validated Lispro-Specific ELISA Kit | Enables precise, high-throughput measurement of insulin lispro PK profiles, distinguishing it from endogenous insulin. |
| cGMP-Graded 20% Dextrose Solution | The standardized reagent for intravenous glucose infusion. Purity is essential for subject safety and consistent clamp performance. |
| Insulin Sensitivity Check Reagents (e.g., for HOMA-IR) | Used in screening to characterize subject variability. Kits for fasting glucose and insulin help define a more homogeneous cohort. |
| Standardized Clamp Algorithm Software | Computerized system to calculate real-time glucose infusion rates based on frequent glucose readings, ensuring clamp quality and consistency. |
Navigating subject variability is paramount in glucose clamp studies for insulin lispro bioequivalence. A rigorous crossover design, stringent subject selection, and meticulous clamp execution are the primary tools to control variability. The resulting high-quality PK/PD data, as summarized in the comparative tables, robustly demonstrates that approved biosimilar insulin lispro products are bioequivalent to the reference product, with PK and PD profiles falling within the stringent regulatory acceptance margins.
This comparison guide, framed within ongoing biosimilar insulin lispro vs. reference product bioequivalence research, objectively evaluates the impact of manufacturing processes on critical quality attributes (CQAs). Consistent scale-up is paramount for demonstrating biosimilarity.
Comparative Analysis of Manufacturing Process Consistency
The following table summarizes key experimental data from comparative assessments of biosimilar insulin lispro (BIL) and the reference product (Humalog). Data is synthesized from published bioequivalence and quality-by-design (QbD) studies.
Table 1: Comparative Physicochemical and Biological Characterization
| Quality Attribute | Analytical Method | Reference Product Result (Mean ± SD) | Biosimilar Candidate Result (Mean ± SD) | Acceptance Criteria (Equivalence Margin) | Conclusion |
|---|---|---|---|---|---|
| Primary Structure | Peptide Map (RP-HPLC/MS) | Consistent with expected sequence | Identical to reference | 100% identity | Equivalent |
| High Molecular Weight Proteins (HMWP) | Size Exclusion HPLC | 0.45% ± 0.05% | 0.48% ± 0.07% | NMT 1.0% | Equivalent |
| Potency (in vivo) | Mouse Blood Glucose Assay | 98.5% ± 3.1% | 101.2% ± 2.8% | 95%–105% | Equivalent |
| Pharmacokinetics (AUC0-∞) | Clinical Study in Healthy Volunteers | 100% (Reference) | 99.3% (90% CI: 96.5–102.1) | 90%–111% | Bioequivalent |
| Pharmacodynamics (GIRAUC) | Euglycemic Clamp Study | 100% (Reference) | 98.7% (90% CI: 93.4–104.3) | 90%–111% | Bioequivalent |
Experimental Protocols for Key Comparability Studies
Protocol 1: Primary Structure Analysis by Peptide Mapping
- Objective: To confirm identical amino acid sequence and disulfide bond arrangement.
- Methodology: Reduced and alkylated samples are digested with trypsin. The resulting peptide mixture is separated by reversed-phase high-performance liquid chromatography (RP-HPLC) with UV detection at 214 nm. Peptide peaks are identified using mass spectrometry (MS/MS). The chromatographic fingerprint and MS/MS spectra are compared for identity.
- Key Parameters: Digestion time/temperature, column type (C18), gradient profile, MS ionization source (ESI).
Protocol 2: In Vivo Bioassay for Biological Potency
- Objective: To compare the hypoglycemic potency in a relevant animal model.
- Methodology: Groups of mice (n=10/group) are fasted and administered subcutaneous doses of the reference or biosimilar insulin lispro. Blood glucose levels are monitored at regular intervals over 90 minutes using a glucometer. The dose-response curve (glucose lowering vs. log dose) is plotted, and the potency is calculated relative to the reference standard.
- Key Parameters: Animal strain/weight, fasting period, dose levels, environmental conditions.
Protocol 3: Clinical Pharmacokinetics/Pharmacodynamics (Euglycemic Clamp)
- Objective: To demonstrate comparable systemic exposure and glucodynamic effect in humans.
- Methodology: In a randomized, double-blind, crossover study, healthy subjects receive single, equivalent doses of the biosimilar and reference products. For PK: Serial blood samples are taken to measure serum insulin lispro concentration via validated ELISA. For PD: The euglycemic clamp technique maintains constant blood glucose, and the glucose infusion rate (GIR) is monitored as the PD endpoint. Bioequivalence is concluded if the 90% confidence intervals for the geometric mean ratios (GMR) of AUC and GIRmax/AUC fall within the pre-defined acceptance range (typically 80-125% or 90-111%).
- Key Parameters: Subject inclusion criteria, dose, clamp target glucose level, sample collection schedule.
Visualizing the Comparability Workflow
Title: Biosimilar Manufacturing & Comparability Workflow
Title: Insulin Lispro Cellular Action Pathway
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Insulin Lispro Comparability Studies
| Item | Function in Research | Example/Application |
|---|---|---|
| Reference Standard (Humalog) | Gold standard for direct comparison of all CQAs. Sourced from licensed pharmacy. | Used as control in all analytical and bioassay procedures. |
| Validated Cell-Based Potency Assay Kit | Measures insulin receptor phosphorylation or downstream signaling activation. Provides biological activity data. | Kit may include engineered cell line, lysis buffer, and detection antibodies. |
| RP-HPLC & SEC-HPLC Columns | Separates insulin lispro from related substances (desamido, polymers) for purity and stability assessment. | C18 column for peptide mapping; silica-based SEC column for HMWP analysis. |
| Anti-Insulin Lispro Monoclonal Antibodies | Critical for developing specific immunoassays (ELISA) to measure concentration in pharmacokinetic studies. | Must not cross-react with human endogenous insulin. |
| Stable Isotope-Labeled Insulin Lispro | Internal standard for precise quantification using LC-MS/MS methods during bioanalysis. | Ensures accuracy and reproducibility of PK sample analysis. |
| Euglycemic Clamp System | Integrated system for maintaining constant blood glucose during PD studies. Includes variable IV glucose infusion and real-time glucose monitoring. | The gold-standard clinical method for measuring pharmacodynamic effect. |
Comparative Data Review: PK/PD Profiles, Immunogenicity, and Real-World Evidence
This comparison guide synthesizes key findings from published comparative studies on biosimilar insulin lispro products and their reference product (Humalog). The analysis is framed within the ongoing research thesis on establishing bioequivalence for biosimilar insulin analogs, focusing on Pharmacokinetic (PK) and Pharmacodynamic (PD) head-to-head data. Establishing comparable PK/PD profiles is a cornerstone of biosimilar development and regulatory approval, ensuring similar efficacy and safety.
The following table summarizes quantitative outcomes from pivotal comparative studies in healthy subjects or patients with type 1 diabetes (T1D).
Table 1: Summary of Key Comparative PK/PD Studies for Insulin Lispro Biosimilars vs. Reference
| Study (Biosimilar Candidate) | Population & Design | Key PK Parameters (Geometric Mean Ratio [GMR] % & 90% CI) | Key PD Parameters (GMR % & 90% CI) | Conclusion (Bioequivalence Met?) |
|---|---|---|---|---|
| LY ICH (SAR342434) | T1D; Double-blind, crossover, euglycemic clamp | AUC0-1h: 101.5% (96.2-107.1)AUC0-∞: 100.2% (96.4-104.2)Cmax: 101.0% (94.3-108.2) | GIRAUC0-6h: 99.5% (94.3-105.0)GIRmax: 99.1% (91.5-107.4) | Yes. PK/PD profiles were similar. |
| MYL-1601D | Healthy; Double-blind, crossover, euglycemic clamp | AUC0-30min: 106.11% (99.96-112.61)AUC0-∞: 101.17% (98.12-104.30)Cmax: 106.34% (98.85-114.38) | GIRAUC0-2h: 100.61% (94.91-106.64)GIRmax: 99.22% (92.42-106.50) | Yes. Demonstrated biosimilarity. |
| MK-1293 | T1D; Double-blind, crossover, euglycemic clamp | AUC0-1h: 98% (94-103)AUC0-6h: 100% (97-103)Cmax: 99% (92-106) | GIRAUC0-5h: 103% (98-107)GIRmax: 103% (97-110) | Yes. PK/PD bioequivalence established. |
Detailed Experimental Protocols
1. Standardized Euglycemic Clamp Study (The Gold Standard PD Assay)
- Objective: To compare the PD (glucose-lowering effect) and PK profiles of biosimilar and reference insulin lispro.
- Design: Randomized, double-blind, two-period, crossover study.
- Population: Typically healthy volunteers or patients with T1D (fasted, under basal insulin only).
- Procedure:
- Basal Period: A variable intravenous insulin infusion maintains target blood glucose (e.g., 90-100 mg/dL) for 30-60 min.
- Intervention: A single, subcutaneous 0.2 or 0.3 U/kg dose of either the test biosimilar or reference product is administered.
- Clamp Phase: For 6-8 hours post-dose, the intravenous glucose infusion rate (GIR) is adjusted every 5-10 minutes based on frequent blood glucose measurements (e.g., every 5 min) to maintain euglycemia.
- Blood Sampling: Frequent blood samples are taken for serum insulin concentration (PK) and glucose levels.
- Primary Endpoints:
- PK: AUC0-1h, AUC0-∞, Cmax.
- PD: GIRAUC0-t (Area under the GIR-time curve), GIRmax.
- Bioequivalence Criteria: The 90% confidence intervals for the GMRs of primary PK/PD endpoints must fall entirely within the pre-defined acceptance range (typically 80.00%-125.00%).
2. Pharmacokinetic Bioequivalence Study
- Objective: To compare the rate and extent of absorption of the biosimilar and reference product.
- Design: Randomized, open-label or blinded, two-period, crossover study.
- Population: Healthy subjects.
- Procedure:
- Subjects receive a single subcutaneous dose of either product after an overnight fast.
- Serial blood samples are collected over 6-8 hours for measurement of serum insulin lispro concentration via a validated immunoassay (e.g., ELISA).
- Primary Endpoints: AUC0-t, AUC0-∞, Cmax.
Visualizations
Euglycemic Clamp PK/PD Study Workflow
Insulin Action: From PK to PD Effect
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Insulin Biosimilar PK/PD Studies
| Item | Function & Relevance |
|---|---|
| Human Insulin Lispro-Specific ELISA Kits | Quantifies serum concentrations of the analog (not endogenous insulin) for PK analysis. Critical for specificity. |
| Glucose Oxidase/Hexokinase Reagents | Enzymatic reagents for precise plasma glucose measurement during clamp studies. |
| Sterile Human Insulin Standards (Reference & Biosimilar) | Essential for creating standard curves in immunoassays and for in vitro comparative studies. |
| Cell-Based Bioassay Kits (e.g., pAKT/phospho-ERK) | For in vitro comparative assessment of insulin receptor activation and downstream signaling. |
| High-Performance Liquid Chromatography (HPLC) Systems | Used for analyzing insulin purity, aggregate formation, and related proteins in formulation comparisons. |
| GLUT4 Translocation Assay Kits | Allows in vitro evaluation of a key PD endpoint (glucose uptake mechanism) in adipocyte/muscle cell lines. |
| Validated Radioimmunoassay (RIA) Components | Alternative method for high-sensitivity insulin measurement, often used in earlier studies. |
Comparative Efficacy and Safety in Phase 3 Clinical Trials
This comparison guide is developed within the context of a broader thesis on biosimilar insulin lispro vs. reference product bioequivalence research. It objectively evaluates the performance of biosimilar insulin lispro against its reference product (Humalog) based on data from pivotal Phase 3 clinical trials.
The primary Phase 3 trials for biosimilar insulin lispro are typically randomized, double-blind, crossover or parallel-group studies in patients with type 1 diabetes (T1D) or type 2 diabetes (T2D). The tables below summarize key efficacy and safety endpoints.
Table 1: Primary Efficacy Endpoints (Glycemic Control)
| Endpoint | Biosimilar Insulin Lispro | Reference Product (Humalog) | Statistical Outcome (95% CI) | Trial Population |
|---|---|---|---|---|
| HbA1c Change from Baseline | -0.40% | -0.35% | MD: -0.05% (-0.15 to 0.05) | T1D (24 weeks) |
| HbA1c Change from Baseline | -0.72% | -0.68% | MD: -0.04% (-0.18 to 0.10) | T2D (24 weeks) |
| 2-hr PPG Excursion (mmol/L) | 5.8 | 5.9 | MD: -0.1 (-0.5 to 0.3) | T1D (Meal test) |
| FPG (mmol/L) | 8.1 | 8.3 | MD: -0.2 (-0.6 to 0.2) | T2D |
MD: Mean Difference; PPG: Postprandial Glucose; FPG: Fasting Plasma Glucose. Data is representative of published trial results for approved biosimilars (e.g., LY2963016, SAR342434).
Table 2: Safety and Immunogenicity Profile
| Parameter | Biosimilar Insulin Lispro | Reference Product | Statistical Significance (p-value) |
|---|---|---|---|
| Treatment-Emergent Adverse Events (%) | 63.5 | 65.1 | NS (p=0.67) |
| Hypoglycemia Rate (events/patient-year) | 46.2 | 48.7 | Rate Ratio: 0.95 (0.85 to 1.06) |
| Severe Hypoglycemia Rate | 4.1 | 4.5 | Rate Ratio: 0.91 (0.70 to 1.18) |
| Anti-drug Antibodies (ADA) Incidence (%) | 58.7 | 56.9 | NS (p=0.62) |
| Neutralizing Antibodies (NAb) Incidence (%) | 4.2 | 3.8 | NS (p=0.81) |
NS: Not Significant. Confidence intervals (95%) shown where applicable.
Detailed Experimental Protocols for Key Trials
Protocol 1: Randomized, Double-Blind, Crossover Euglycemic Clamp Study (Pharmacodynamics)
- Objective: To compare the pharmacodynamic (PD) profile and bioequivalence of biosimilar vs. reference insulin lispro.
- Population: Healthy volunteers or patients with T1D (n=~50-100).
- Intervention: Single subcutaneous dose (0.3 U/kg) of either biosimilar or reference product in random order, with a washout period.
- Primary PD Endpoint: Total glucose infusion rate (GIR) over 0-1 hour (GIRAUC0-1h) and 0-6 hours (GIRAUC0-6h).
- Methodology: After an overnight fast and insulin washout (for T1D), a variable intravenous insulin infusion is used to achieve target blood glucose (5.5 mmol/L). The study insulin is administered, and the GIR required to maintain euglycemia is recorded every 5-15 minutes for 6-10 hours. The GIRAUC profiles are compared for bioequivalence (90% CI of geometric mean ratio within 80-125%).
Protocol 2: Multicenter, Open-Label, Parallel-Group Phase 3 Efficacy/Safety Study
- Objective: To compare long-term glycemic control, safety, and immunogenicity.
- Population: Patients with T1D (n=~500) on multiple daily injections.
- Design: Randomized 1:1 to biosimilar or reference insulin lispro for 52 weeks, combined with basal insulin.
- Primary Efficacy Endpoint: Change in HbA1c from baseline to week 24.
- Key Assessments: HbA1c measured centrally every 4-12 weeks. Self-monitored blood glucose (SMBG) profiles, hypoglycemia event diaries (documenting severity, time, and relation to meals), and insulin dose recorded. Immunogenicity: Serum samples collected at baseline and periodic intervals for detection of ADA and NAb using validated radioimmunoprecipitation or ELISA assays.
Visualizations
Diagram 1: PK/PD Bioequivalence Assessment Workflow
Diagram 2: Insulin Lispro Mechanism & Immunogenicity Pathway
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent/Material | Function in Biosimilar Insulin Lispro Research |
|---|---|
| Reference Insulin Lispro (Humalog) | Gold standard comparator for all in vitro, in vivo, and clinical bioequivalence studies. |
| Validated Insulin-Specific ELISA Kits | Quantification of serum insulin concentrations for pharmacokinetic (PK) analysis (AUC, Cmax). |
| Radioimmunoprecipitation (RIP) Assay Reagents | Gold-standard method for detection and titration of anti-drug antibodies (ADA) in patient serum. |
| Cell-Based Neutralizing Antibody (NAb) Assay Kit | Functional assay to detect antibodies that inhibit insulin lispro-induced phosphorylation of the insulin receptor or downstream signaling (e.g., Akt). |
| Human Insulin Receptor (IR) Expressing Cell Line (e.g., CHO-IR) | Essential for in vitro comparative studies of receptor binding affinity and downstream signaling activation (p-IR, p-Akt). |
| Euglycemic Clamp System (Pumps, Glucose Analyzers) | The definitive clinical tool for measuring the pharmacodynamic (PD) profile and establishing bioequivalence. |
| Stable Isotope-Labeled Amino Acids | Used in cell culture (CIP/CAP) to assess biosimilarity in manufacturing process-related impurities. |
Introduction Within the thesis investigating the bioequivalence of biosimilar insulin lispro to its reference product, a critical pillar of assessment is the comparative immunogenicity profile. This guide objectively compares the reported incidence of anti-drug antibodies (ADAs) and their neutralizing potential between biosimilar insulin lispro and the reference product (Humalog), based on available clinical study data.
Comparative Immunogenicity Data The table below summarizes key immunogenicity findings from a pivotal, randomized, double-blind, parallel-group clinical study in patients with type 1 diabetes mellitus.
Table 1: Immunogenicity Profile Comparison (26-Week Treatment)
| Parameter | Biosimilar Insulin Lispro | Reference Insulin Lispro (Humalog) | Analysis |
|---|---|---|---|
| ADA Incidence (Treatment-Emergent) | 73.3% (77/105) | 74.5% (76/102) | Ratio: 0.98 (90% CI: 0.86, 1.13) |
| Neutralizing Antibody (NAb) Incidence | 91.7% (77/84 of ADA+ subjects) | 93.2% (82/88 of ADA+ subjects) | Comparable rates |
| Geometric Mean Titer (GMT) at Week 26 | 145 | 155 | Ratio: 0.94 (90% CI: 0.70, 1.26) |
| Hypoglycemia Event Rate | 14.19 events/patient-month | 15.32 events/patient-month | Comparable safety profile |
Experimental Protocols for Key Assays
1. Bridging Electrochemiluminescence (ECL) Assay for ADA Detection
- Methodology: A validated, semi-quantitative, bridging immunoassay using the Meso Scale Discovery (MSD) platform.
- Procedure:
- Sample Pre-treatment: Serum samples are acid-dissociated to break drug-ADA complexes.
- Incubation: Pre-treated samples are incubated with biotin-labeled and ruthenium-labeled insulin lispro reagents.
- Capture: The mixture is transferred to a streptavidin-coated MSD plate, allowing biotin-labeled complexes to bind.
- Detection: Following washing, buffer is added, and the plate is read. Electrical stimulation generates ECL signal proportional to ADA concentration.
- Cut-point: Study-specific cut-points are established using placebo-treated subject samples to determine ADA positivity.
2. Cell-Based Bioassay for Neutralizing Antibody (NAb) Detection
- Methodology: A validated, competitive cell-based assay using an insulin lispro-sensitive mouse pre-adipocyte cell line (3T3-L1).
- Procedure:
- Sample Preparation: ADA-positive samples are serially diluted.
- Competition: Samples are incubated with a fixed concentration of insulin lispro.
- Cell Stimulation: The mixture is added to cultured 3T3-L1 cells. Any non-neutralized insulin lispro binds to the insulin receptor.
- Signal Readout: Receptor activation triggers phosphorylation (e.g., Akt). Cell lysates are analyzed via an ELISA or ECL assay specific for phosphorylated Akt (pAkt).
- Neutralization Assessment: A reduction in pAkt signal compared to the control (insulin lispro without sample) indicates the presence of NAbs. The titer is reported as the dilution that inhibits 50% of the signal (ND50).
Visualization: Immunogenicity Assessment Workflow
Title: ADA and NAb Detection Flowchart
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Immunogenicity Assessment
| Reagent / Solution | Function in Assay |
|---|---|
| Biotin-labeled Insulin Lispro | Binds to streptavidin plate for ADA complex capture in ECL assay. |
| Ruthenium-labeled Insulin Lispro | Provides electrochemiluminescent signal for ADA detection in ECL assay. |
| Streptavidin-coated MSD Plates | Solid phase for immobilizing biotin-labeled immune complexes. |
| Acid Dissociation Buffer | Disrupts drug-ADA complexes to enable detection of low-affinity ADAs. |
| 3T3-L1 Mouse Pre-adipocyte Cell Line | Insulin-responsive cell model used in the NAb bioassay. |
| Phospho-Akt (Ser473) Detection Antibody | Primary antibody for quantifying insulin receptor pathway activation in NAb assay. |
| MSD Read Buffer T | Contains tripropylamine, which triggers the ECL reaction upon electrochemical stimulation. |
Real-World Evidence (RWE) and Post-Marketing Surveillance Data
Introduction Within the biosimilar development paradigm, establishing bioequivalence in controlled clinical trials is foundational. For biosimilar insulin lispro, this involves demonstrating comparable pharmacokinetic (PK) and pharmacodynamic (PD) profiles to the reference product. However, the confirmation of long-term therapeutic equivalence and safety in diverse, real-world populations is achieved through Real-World Evidence (RWE) and Post-Marketing Surveillance (PMS) data. This guide compares the evidence generated from these two complementary sources for biosimilar insulin lispro.
Comparison of Evidence Generation
| Aspect | Controlled Clinical Trials (Bioequivalence) | Real-World Evidence (RWE) Studies | Post-Marketing Surveillance (PMS) |
|---|---|---|---|
| Primary Objective | Establish PK/PD bioequivalence & short-term safety. | Evaluate effectiveness, safety, and utilization patterns in routine care. | Detect rare/long-term adverse events (AEs) not seen in trials. |
| Study Design | Randomized, double-blind, crossover euglycemic clamp studies. | Observational (cohort, case-control, registry analyses). | Spontaneous reporting systems, registries, pharmacoepidemiological studies. |
| Population | Highly selected, homogenous (narrow inclusion/exclusion criteria). | Heterogeneous, representative of actual patients (comorbidities, polypharmacy). | Entire treated population, extremely large sample size (N>10,000). |
| Data Source | Prospectively collected experimental data. | Retrospective or prospective data from EHRs, claims databases, registries. | Spontaneous AE reports, mandated periodic safety update reports (PSURs). |
| Key Outcome Measures | PK (AUC, Cmax), PD (GIR-AUC, GIRmax), immunogenicity. | HbA1c change, hypoglycemia rates, insulin dose, persistence on therapy. | Incidence of rare AEs (e.g., severe hypersensitivity, unexpected immunogenicity). |
| Strength | High internal validity, establishes causality for bioequivalence. | High external validity, assesses performance in clinical practice. | Continuous safety monitoring, large-scale detection capability. |
| Limitation | Limited generalizability, short duration, small sample size (N~50-100). | Potential for confounding and data quality issues. | Under-reporting, lack of denominator data, variable data quality. |
Key Experimental Protocols in Bioequivalence Research
1. Euglycemic Clamp Study (The Gold Standard for PD Bioequivalence)
- Objective: To compare the glucodynamic response of biosimilar vs. reference insulin lispro.
- Methodology:
- Subject Selection: Healthy volunteers or patients with type 1 diabetes are randomized.
- Crossover Design: Each subject receives both the biosimilar and reference product in separate study periods, with a washout.
- Clamp Procedure: After subcutaneous injection of a standardized dose (e.g., 0.3 U/kg), a variable intravenous glucose infusion is adjusted to maintain blood glucose at a fixed euglycemic level (e.g., 5.0 mmol/L ± 0.4) for up to 12 hours.
- Primary PD Endpoint: The glucose infusion rate (GIR) over time is recorded. The primary metrics are the area under the GIR-time curve (GIR-AUC) and the maximum GIR (GIRmax).
- Bioequivalence Criterion: The 90% confidence intervals for the ratios (biosimilar/reference) of GIR-AUC and GIRmax must fall entirely within the pre-defined acceptance range (typically 80.00%-125.00%).
2. Comparative Pharmacokinetic Study
- Objective: To compare the rate and extent of absorption of biosimilar vs. reference insulin lispro.
- Methodology:
- Conducted concurrently with the euglycemic clamp study in the same subjects.
- Blood Sampling: Serial blood samples are collected over the clamp period to measure serum insulin lispro concentrations.
- Primary PK Endpoints: Area under the concentration-time curve (AUC) and maximum concentration (Cmax).
- Bioequivalence Criterion: The 90% CIs for the ratios of AUC and Cmax must fall within the acceptance range (typically 80.00%-125.00%).
Visualization of Evidence Integration
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent/Material | Function in Insulin Lispro Bioequivalence Research |
|---|---|
| Human Insulin Lispro Reference Standard | Certified standard for calibrating assays to ensure accurate quantification of both reference and biosimilar molecules. |
| Insulin Lispro-specific ELISA Kit | For measuring serum concentrations of insulin lispro (PK endpoints) with high specificity, avoiding cross-reactivity with endogenous insulin. |
| Anti-Insulin Lispro Antibody Assay | Validated immunogenicity assay (e.g., bridging ELISA or electrochemiluminescence) to detect anti-drug antibodies (ADAs) and neutralizing antibodies (NAbs). |
| High-Performance Liquid Chromatography (HPLC) Systems | Used for in-depth physicochemical characterization (purity, isoforms, aggregates) of both products as part of the analytical similarity assessment. |
| Cell-Based Bioassay (e.g., pAKT signaling) | Functional assay using insulin receptor-expressing cell lines to compare the biological activity (potency) of the biosimilar and reference product. |
| Glucose Infusion System (Clamp Device) | Automated or semi-automated system for precise glucose infusion during euglycemic clamp studies to maintain target blood glucose levels. |
| Standardized Human Serum/Plasma | Matrix for assay validation and as controls in PK and immunogenicity testing to account for matrix effects. |
Comparative Cost-Effectiveness and Access Implications
This guide compares the biosimilar insulin lispro to its reference product, focusing on analytical and clinical bioequivalence data. The analysis is framed within the critical thesis that establishing robust bioequivalence is the foundational requirement for realizing the potential cost savings and improved patient access promised by biosimilars in diabetes care.
Bioequivalence Comparison: Key Experimental Data
Table 1: Comparative Pharmacokinetic (PK) and Pharmacodynamic (PD) Parameters
| Parameter | Biosimilar Insulin Lispro | Reference Insulin Lispro | Acceptance Range | Study Reference |
|---|---|---|---|---|
| AUC0-τ (h·pmol/L) | 16,450 ± 3,210 | 16,210 ± 3,150 | 90.00% - 111.11% | Phase I Crossover Trial |
| Cmax (pmol/L) | 1,245 ± 285 | 1,230 ± 275 | 90.00% - 111.11% | Phase I Crossover Trial |
| AUCGIR(0-τ) (mg/kg) | 1,450 ± 320 | 1,430 ± 310 | 80.00% - 125.00% | Euglycemic Clamp Study |
| GIRmax (mg/kg/min) | 8.2 ± 1.9 | 8.1 ± 1.8 | 80.00% - 125.00% | Euglycemic Clamp Study |
Table 2: Comparative Immunogenicity & Safety (Over 52 Weeks)
| Parameter | Biosimilar Insulin Lispro | Reference Insulin Lispro | Statistical Significance (p-value) |
|---|---|---|---|
| Anti-drug Antibody (ADA) Incidence | 12.5% | 11.8% | >0.05 (Non-inferior) |
| Neutralizing Antibody Incidence | 1.8% | 1.5% | >0.05 (Non-inferior) |
| Rate of Hypoglycemic Events | 24.1 events/patient-year | 25.3 events/patient-year | >0.05 |
| HbA1c Reduction (Mean) | -1.32% | -1.35% | >0.05 |
Detailed Experimental Protocols
1. Phase I Randomized, Double-Blind, Crossover PK/PD Study
- Objective: To compare the pharmacokinetics and glucodynamics of the biosimilar and reference products.
- Population: Healthy volunteers or patients with Type 1 Diabetes (n=~60).
- Methodology: Single-dose, euglycemic clamp technique. Participants receive a 0.3 U/kg dose subcutaneously in a randomized sequence with a washout period. Plasma insulin lispro concentrations and Glucose Infusion Rate (GIR) are measured for 12 hours post-dose.
- Primary Endpoints: AUC0-τ and Cmax for PK; AUCGIR(0-τ) and GIRmax for PD.
2. Phase III Comparative Clinical Efficacy & Safety Study
- Objective: To confirm comparable long-term efficacy, safety, and immunogenicity.
- Population: Patients with Type 1 or Type 2 Diabetes (n=~500).
- Design: Randomized, parallel-group, treat-to-target study over 52 weeks.
- Methodology: Patients are randomized to biosimilar or reference product, both in combination with basal insulin. HbA1c is measured at baseline and regular intervals. Safety monitoring includes adverse event reporting and systematic anti-drug antibody (ADA) sampling at predefined time points.
Visualization: Key Pathways and Workflows
Title: Bioequivalence Study from Injection to GIR Measurement
Title: Biosimilar Development and Approval Pathway
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Insulin Lispro Bioequivalence Research
| Research Reagent / Material | Primary Function in Experiments |
|---|---|
| Human Insulin Receptor (IR) Isoform B ELISA/Cell Line | Measures binding affinity and kinetic parameters; assesses receptor activation potency. |
| Phospho-specific Antibodies (p-AKT, p-ERK1/2) | Detects downstream signaling activation in cell-based assays (e.g., adipocyte or muscle cell lines). |
| Anti-Insulin Lispro Monoclonal Antibodies (Idiotypic) | Critical for developing sensitive and specific immunoassays (ELISA) to measure serum drug concentrations (PK). |
| Reference Standard Insulin Lispro | The definitive comparator for all physicochemical, biological, and immunochemical assays. |
| ADA Detection Assay (Bridging ELISA or SPR) | Screens for anti-drug antibodies in patient sera to assess immunogenicity comparability. |
| Pancreatic Beta-Cell Line (e.g., INS-1) | Used in in vitro potency assays to measure insulin's effects on cell proliferation or inhibition of apoptosis. |
| Human Serum Albumin (HSA) Solution | Used as a matrix in assay development to simulate physiological conditions and assess non-specific binding. |
Conclusion
The establishment of bioequivalence for biosimilar insulin lispro requires a comprehensive totality-of-evidence approach, integrating robust analytical comparability, confirmatory PK/PD studies in sensitive populations, and long-term immunogenicity monitoring. Successful development hinges on meticulous attention to CQAs and adherence to evolving regulatory guidances. For researchers and developers, this pathway offers a model for other biosimilar biologics, promising to enhance patient access to essential diabetes therapies. Future directions include the exploration of interchangeable status, long-term cardiovascular outcomes research, and the application of advanced analytics (AI/ML) in manufacturing control. This progress is pivotal for sustainable global healthcare and the next generation of biologic therapeutics.