Akkermansia muciniphila and Insulin Sensitivity: A Comprehensive Review of Human Clinical Studies
This article provides a systematic review of human studies investigating the relationship between the gut commensal bacterium Akkermansia muciniphila and insulin sensitivity.
Akkermansia muciniphila and Insulin Sensitivity: A Comprehensive Review of Human Clinical Studies
Abstract
This article provides a systematic review of human studies investigating the relationship between the gut commensal bacterium Akkermansia muciniphila and insulin sensitivity. Targeting researchers, scientists, and drug development professionals, the review covers foundational discoveries linking A. muciniphila abundance to metabolic health, methodological approaches for its quantification and therapeutic application, challenges in study optimization and result interpretation, and comparative validation of its efficacy against other interventions. The synthesis aims to inform future research and therapeutic development targeting the gut microbiome for metabolic disorders.
The Gut-Metabolism Axis: Discovering Akkermansia muciniphila's Role in Human Insulin Sensitivity
Akkermansia muciniphila is a strictly anaerobic, Gram-negative, mucin-degrading bacterium belonging to the Verrucomicrobia phylum. It colonizes the mucus layer of the gastrointestinal tract, constituting 1-4% of the total gut microbiota in healthy adults. Its niche is uniquely defined by its specialization in using host-derived mucins as its sole source of carbon and nitrogen. This symbiotic relationship is central to maintaining mucosal integrity, regulating immune responses, and influencing systemic host metabolism. Within the thesis context of A. muciniphila abundance and insulin sensitivity in human studies, understanding its mucosal niche is foundational, as its metabolic activity generates postbiotic compounds (e.g., short-chain fatty acids, propionate, acetate, and specific amino acids) that are critical mediators of systemic metabolic effects.
A. muciniphila: Core Characteristics and Mucosal Niche
A. muciniphila resides in the outer, looser layer of the intestinal mucus, maintaining a safe distance from the epithelium while actively remodeling the mucin matrix. Its genome encodes a rich repertoire of mucin-degrading enzymes (glycoside hydrolases, sulfatases, proteases). This activity supports its growth and creates a trophic network for other commensals. Crucially, its byproducts signal to the host, reinforcing mucus production (via upregulation of Muc2 expression) and tightening epithelial junctions, thereby improving gut barrier function—a key link to metabolic health.
Table 1: Core Genomic and Physiological Features of A. muciniphila
| Feature | Description |
|---|---|
| Taxonomy | Phylum: Verrucomicrobia; Family: Akkermansiaceae |
| Morphology | Oval-shaped, non-motile, non-spore-forming |
| Growth Substrate | Mucins (primarily), N-Acetylglucosamine, N-Acetylgalactosamine |
| Key Metabolites | Acetate, Propionate, Ethanol, 1,2-Propanediol |
| Optimal Growth | 37°C, pH 6.5, Strict Anaerobe |
| Genome Size | ~2.6 - 2.8 Mb, GC content ~55% |
Mechanistic Link to Insulin Sensitivity: Key Pathways
The proposed pathways linking A. muciniphila to improved insulin sensitivity involve multiple layers: 1) enhanced intestinal barrier function reducing metabolic endotoxemia (LPS), 2) modulation of immune and inflammatory tone, and 3) direct signaling by its outer membrane protein, Amuc_1100, and other metabolites.
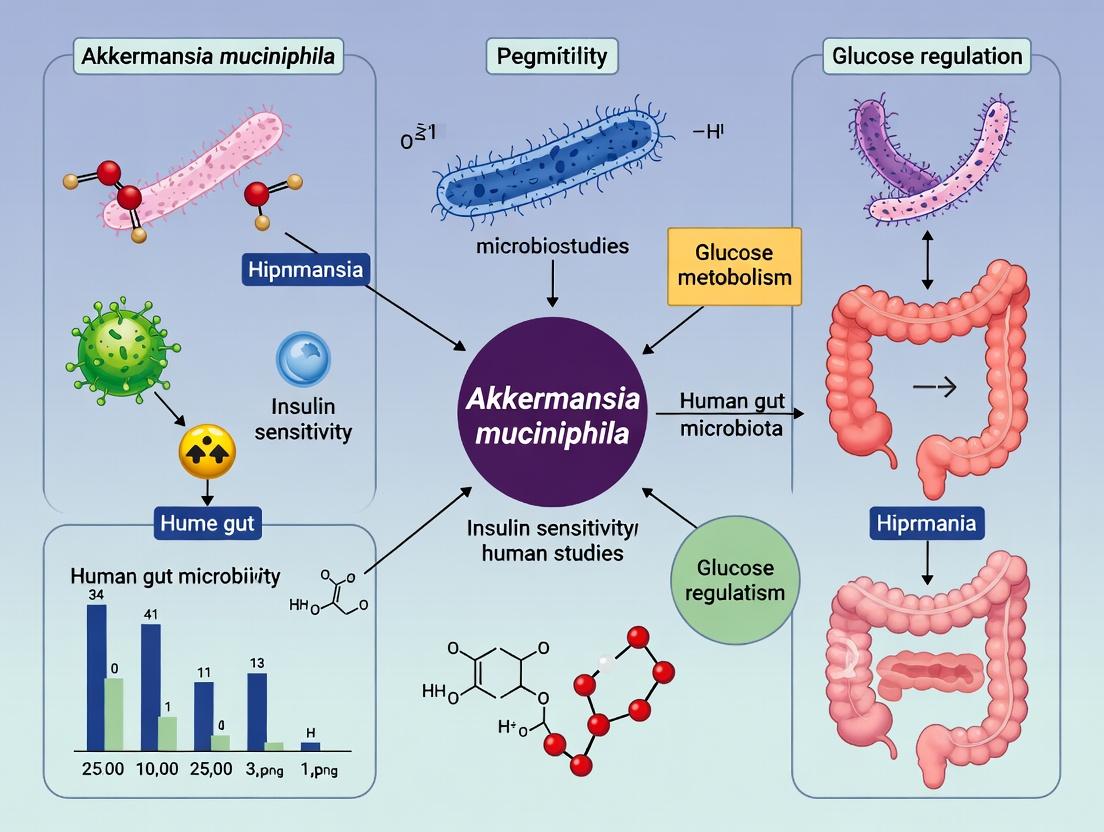
Diagram 1: A. muciniphila and Insulin Sensitivity Pathways
Title: A. muciniphila Mechanisms Driving Insulin Sensitivity
Human observational and interventional studies consistently report an inverse correlation between A. muciniphila abundance and metabolic disorders. Pasteurization of the bacterium appears to enhance its efficacy.
Table 2: Key Human Interventional Studies on A. muciniphila and Metabolic Parameters
| Study (Year) | Population & Design | Intervention | Key Findings on Insulin Sensitivity |
|---|---|---|---|
| Depommier et al. (2019) | n=32, Overweight/Obese insulin-resistant, Randomized, Double-blind, Placebo-controlled | 1) Live A. muciniphila (10¹⁰ CFU/day)2) Pasteurized A. muciniphila (10¹⁰ cells/day)3) Placebo for 3 months | Pasteurized: ↓ Insulin resistance (HOMA-IR by 30% vs placebo, p<0.05), ↓ Plasma insulin. Live: Trends but not significant. |
| Depommier et al. (2021, follow-up) | n=40, Overweight/Obese with prediabetes, Randomized, Double-blind, Placebo-controlled | Pasteurized A. muciniphila (10¹⁰ cells/day) for 3 months | Confirmed ↓ HOMA-IR. Improved postprandial glucose responses, ↓ markers of liver dysfunction and inflammation. |
| Dao et al. (2016) Observational | n=49, Obese/Overweight women | Correlation of baseline abundance with metabolic health after calorie restriction | Higher baseline A. muciniphila associated with better metabolic status (↓ fasting glucose, insulin, HOMA-IR) after intervention. |
Detailed Experimental Protocols for Key Studies
Protocol 1: Human Intervention with Pasteurized A. muciniphila (Adapted from Depommier et al., 2019, 2021)
- Bacterial Preparation: A. muciniphila MucT (ATCC BAA-835) is cultured anaerobically (80% N₂, 10% CO₂, 10% H₂) in mucin-based medium at 37°C. For pasteurization, bacterial suspension is heated at 70°C for 30 min, confirmed sterile by culture, and lyophilized in capsules.
- Study Design: Randomized, double-blind, placebo-controlled, parallel-group trial.
- Participants: Overweight/obese adults with insulin resistance (HOMA-IR >2.5) or prediabetes.
- Intervention: Daily oral intake of 10¹⁰ cells of pasteurized A. muciniphila or placebo (mannitol) for 3 months.
- Primary Outcome: Change in insulin resistance measured by HOMA-IR. Secondary Outcomes: Oral Glucose Tolerance Test (OGTT), markers of inflammation (plasma LPS, CRP), lipids, body composition.
- Sample Collection & Analysis: Fasting blood draws at 0, 1, 2, 3 months. Stool samples for 16S rRNA gene sequencing (e.g., V3-V4 region) to monitor microbiota composition and Akkermansia abundance.
- Statistical Analysis: Per-protocol analysis using ANOVA or non-parametric tests for between-group comparisons. Covariate adjustment for baseline values.
Protocol 2: Assessing Gut Barrier Function In Vivo (Mouse Model Precedent)
- FITC-Dextran Assay: Mice are fasted for 4h, administered FITC-labeled dextran (4 kDa, 600 mg/kg) by oral gavage. Blood is collected via retro-orbital puncture after 4h. Serum fluorescence is measured (excitation 485 nm, emission 535 nm) and compared to a standard curve to quantify intestinal permeability.
- Immunohistochemistry for Tight Junctions: Colon/ileum tissues are fixed, sectioned, and stained for tight junction proteins (ZO-1, Occludin). Fluorescence intensity and continuous linear staining are quantified using confocal microscopy and image analysis software (e.g., ImageJ).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for A. muciniphila and Gut Barrier Research
| Reagent/Material | Function/Application | Example (Non-exhaustive) |
|---|---|---|
| Mucin-Based Growth Medium | Selective cultivation of A. muciniphila. | Modified BHI or synthetic medium with porcine gastric mucin (Type III) as primary carbon source. |
| Anaerobic Chamber or Jar | Provides strict anaerobic conditions (O₂ < 1 ppm) essential for culture viability. | Coy Laboratory Products anaerobic chambers; Mitsubishi AnaeroPack systems. |
| 16S rRNA Gene Sequencing Primers | Profiling microbial communities, quantifying Akkermansia abundance. | 515F/806R (V4), 338F/806R (V3-V4) with appropriate bioinformatic pipelines (QIIME2, MOTHUR). |
| qPCR Probes/Primers (Akkermansia-specific) | Absolute quantification of A. muciniphila genomic DNA in stool/tissue. | Target Akkermansia muciniphila 16S rRNA gene or the highly specific aml gene. |
| Recombinant Amuc_1100 Protein | Investigating host-bacterial protein interaction, TLR2 signaling assays. | Purified His-tagged or tag-free protein for in vitro (cell culture) and in vivo studies. |
| FITC-Dextran (4 kDa) | In vivo measurement of intestinal paracellular permeability. | Administered orally to mice/rats; leakage into serum indicates barrier compromise. |
| ELISA Kits for Metabolic Markers | Quantifying insulin, leptin, adiponectin, inflammatory cytokines (TNF-α, IL-6), LPS. | High-sensitivity kits from vendors (e.g., R&D Systems, Merck, Thermo Fisher). |
| Antibodies for Tight Junctions | Visualizing and quantifying gut barrier integrity in tissue sections. | Anti-ZO-1, Anti-Occludin, Anti-Claudin antibodies for immunofluorescence/Western blot. |
Diagram 2: Workflow for Human Intervention Study Analysis
Title: Human Trial Multi-Omics Analysis Workflow
The search for reliable microbial biomarkers of metabolic health is a cornerstone of modern translational research. This whitepaper examines the epidemiological evidence linking the abundance of the mucin-degrading bacterium Akkermansia muciniphila to improved metabolic parameters, with a specific focus on insulin sensitivity in human studies. This body of correlative data provides the foundational rationale for subsequent mechanistic investigations and interventional trials targeting A. muciniphila as a next-generation therapeutic candidate in metabolic disorders.
The following table synthesizes quantitative data from pivotal observational studies linking A. muciniphila abundance to metabolic health indices.
Table 1: Epidemiological Correlations Between A. muciniphila and Metabolic Parameters in Human Cohorts
| Study (Year) & Cohort | Primary Correlation Metric (Method) | Key Positive Correlations (A. muciniphila Abundance ) | Key Negative Correlations (A. muciniphila Abundance ) | Effect Size / Quantitative Association Notes |
|---|---|---|---|---|
| Dao et al. (2016) - Obese/Overweight Adults (n=49) | 16S rRNA gene sequencing (qPCR) | Improved insulin sensitivity (HOMA-IR, clamp) Lower fasting glycemia Better blood lipid profile | Body fat mass Waist-to-hip ratio | ~4.7-fold higher abundance in metabolically healthy vs. unhealthy obese subjects. Significant inverse correlation with HOMA-IR. |
| Depommier et al. (2019) - Overweight/Obese Insulin-Resistant Adults (n=32, placebo arm) | Metagenomic & qPCR analysis | Improved insulin sensitivity (HOMA-IR) Reduced plasma lipopolysaccharide (LPS) | Insulin resistance (HOMA-IR) | Baseline Akkermansia abundance negatively correlated with HOMA-IR (r = -0.36 to -0.47, p<0.05). |
| Xu et al. (2020) - Newly Diagnosed T2D & Healthy Controls (n=187) | Metagenomic sequencing | Healthy control status Higher HDL-C levels | Type 2 Diabetes status Fasting plasma glucose HbA1c | Relative abundance significantly lower in T2D patients (p<0.001). Abundance inversely correlated with fasting glucose (r=-0.28). |
| Verdi et al. (2023) - TwinsUK Cohort (n=952) | Metagenomic sequencing & LC-MS metabolomics | Favorable cardiometabolic health score Beneficial serum metabolites (e.g., 3-indolepropionic acid) | Visceral fat mass C-reactive protein (CRP) | Strongest microbial association with visceral fat. Mediation analysis suggests A. muciniphila may influence host health via specific metabolites. |
Detailed Experimental Protocols for Cited Studies
Protocol 1: Standardized Methodology for 16S rRNA Gene Sequencing & qPCR Analysis (as in Dao et al., 2016)
- Sample Collection & Stabilization: Collect fresh fecal samples. Immediately aliquot into RNAlater or similar DNA/RNA stabilization buffer. Store at -80°C.
- DNA Extraction: Use a validated kit for tough Gram-negative bacterial lysis (e.g., QIAamp DNA Stool Mini Kit with bead-beating step). Include negative extraction controls.
- Quantitative PCR (qPCR) for Absolute Abundance:
- Primers: A. muciniphila-specific 16S rRNA gene primers (e.g., Amuc16SF: 5'-CAGCACGTGAAGGTGGGGAC-3', R: 5'-CCTTGCGGTTGGCTTCAGAT-3').
- Standard Curve: Generate using a plasmid containing the target amplicon sequence. Perform serial 10-fold dilutions.
- Reaction Mix: SYBR Green master mix, primers, template DNA. Run in triplicate.
- Calculation: Express as log10 gene copies per gram of feces.
- 16S rRNA Gene Sequencing for Relative Abundance:
- Amplify the V3-V4 hypervariable region using universal primers (e.g., 341F/806R).
- Perform paired-end sequencing on an Illumina MiSeq platform.
- Bioinformatics: Process using QIIME2 or DADA2 pipeline. Assign taxonomy against the SILVA or Greengenes database. Data expressed as relative abundance (% of total sequenced community).
Protocol 2: Metabolomic Correlation Analysis (as in Verdi et al., 2023)
- Sample Preparation (Serum): Thaw serum samples on ice. Precipitate proteins using cold methanol/acetonitrile. Centrifuge. Dry supernatant under nitrogen.
- LC-MS Analysis:
- Chromatography: Re-suspend dried extract in water/acetonitrile. Inject onto a reversed-phase C18 column using a gradient elution (water/acetonitrile with 0.1% formic acid).
- Mass Spectrometry: Use a high-resolution tandem mass spectrometer (e.g., Q-TOF) in both positive and negative electrospray ionization modes.
- Data Processing: Convert raw files. Perform peak picking, alignment, and annotation using software (e.g., XCMS, MS-DIAL). Annotate metabolites against public databases (HMDB, METLIN).
- Statistical Integration: Perform Spearman correlation between A. muciniphila relative abundance (from metagenomics) and intensity of all detected metabolites. Adjust for covariates (age, BMI, batch). Apply false discovery rate (FDR) correction.
Visualizing the Epidemiological & Mechanistic Framework
Title: Epidemiological Correlations to Inferred Mechanisms
Title: Workflow for Microbial Abundance-Phenotype Correlation
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for A. muciniphila Correlation Studies
| Item / Reagent | Function & Application | Example Product / Note |
|---|---|---|
| Fecal Sample Stabilizer | Preserves microbial community structure and nucleic acids at room temperature for transport/storage. Critical for cohort studies. | DNA/RNA Shield (Zymo Research), RNAlater (Thermo Fisher) |
| Mechanical Lysis Beads | Ensures efficient rupture of tough Gram-negative bacterial cell walls (including Akkermansia) during DNA extraction. | 0.1mm zirconia/silica beads (e.g., from BioSpec Products) |
| Stool DNA Extraction Kit | Standardized, high-yield nucleic acid isolation with inhibitors removal. | QIAamp PowerFecal Pro DNA Kit (Qiagen), MagAttract PowerMicrobiome Kit (Qiagen) |
| Species-Specific qPCR Assay | Absolute quantification of A. muciniphila 16S rRNA gene copies. Gold standard for targeted abundance. | TaqMan assay (Amuc_16S or Akkermansia-specific), SYBR Green with validated primers. |
| 16S rRNA Gene Primer Set | Amplification of hypervariable regions for community profiling and relative abundance calculation. | 341F/806R (V3-V4), 515F/806R (V4). Must be validated for Akkermansia detection. |
| Metabolomic Internal Standards | Enables accurate quantification and quality control in LC-MS-based metabolomic correlation studies. | Stable isotope-labeled compounds (e.g., d7-glucose, 13C-SCFA mix) |
| Bioinformatics Pipeline | Processing raw sequencing data into taxonomic tables for statistical analysis. | QIIME2, DADA2, MOTHUR. Use SILVA database for taxonomy. |
| Statistical Software Suite | Perform complex correlation analyses, adjust for confounders, and handle high-dimensional data. | R (with vegan, phyloseq, MaAsLin2 packages), Python (SciPy, pandas). |
Within the broader thesis on Akkermansia muciniphila abundance and insulin sensitivity in human research, a growing body of landmark studies provides compelling evidence for a mechanistic connection. This whitepaper synthesizes key human intervention trials and observational studies, detailing experimental protocols, quantitative outcomes, and the molecular pathways implicated. The evidence underscores A. muciniphila as a promising microbial target for metabolic syndrome and type 2 diabetes interventions.
Key Human Studies: Data Synthesis
The following table consolidates quantitative findings from pivotal human studies investigating A. muciniphila abundance and metabolic parameters.
Table 1: Landmark Human Studies on A. muciniphila and Metabolic Health
| Study (Year) | Design & Population | Primary Intervention / Observation | Key Outcome on A. muciniphila Abundance | Key Metabolic Outcome (vs. Control/Placebo) |
|---|---|---|---|---|
| Depommier et al. (2019) | Randomized, double-blind, placebo-controlled pilot (n=32 overweight/obese insulin-resistant volunteers) | Daily supplementation with 10¹⁰ live or pasteurized A. muciniphila for 3 months. | Live: ~10x increase. Pasteurized: ~100x increase. | Pasteurized: Improved insulin sensitivity (HOMA-IR ↓ -30.0%, p=0.002); reduced plasma insulin; lower total cholesterol. Live: Trends for improvement. |
| Dao et al. (2016) | Cross-sectional & Dietary Intervention (n=49 obese/overweight women) | 6-week energy-restricted diet. | Baseline abundance higher in metabolically healthy vs. unhealthy obese. Increased after diet (p<0.01). | Diet-induced improvement in insulin sensitivity & cholesterol linked to higher baseline A. muciniphila. |
| Anhê et al. (2020) | Randomized, controlled (n=40 with metabolic syndrome) | 6-month supplementation with polyphenol-rich cranberry extract. | Significant increase in A. muciniphila (p<0.001). | Improved insulin sensitivity (Matsuda index ↑ 24.6%, p=0.01); reduced HOMA-IR. |
| Rodriguez et al. (2022) | Observational (n=1,135 general population) | Metagenomic profiling (Metacardis cohort). | Abundance inversely correlated with fasting glycemia, HbA1c, and incident type 2 diabetes. | Higher abundance associated with better cardiometabolic health indices. |
Detailed Experimental Protocols
Protocol: Supplementation with PasteurizedA. muciniphila(Depommier et al., 2019)
This landmark RCT established causality in humans.
- Bacterial Preparation: A. muciniphila MucT (ATCC BAA-835) was cultured anaerobically. For the pasteurized arm, bacteria were heat-treated (70°C for 30 min), lyophilized, and encapsulated.
- Study Arms: Participants were randomized to Placebo, Live A. muciniphila (10¹⁰ cells/day), or Pasteurized A. muciniphila (equivalent dose/day).
- Administration: Capsules were taken daily for 3 months. No major dietary changes were instructed.
- Outcome Measures:
- Primary: Insulin resistance (HOMA-IR, Hyperinsulinemic-euglycemic clamp).
- Secondary: Plasma lipids, gut barrier function (LPS, LBP), fecal microbiota composition (16S rRNA sequencing), adiposity.
- Sample Collection: Fecal samples (for microbiota & SCFA), blood (fasting & during clamp), anthropometrics at baseline, 1 month, and 3 months.
Protocol: Dietary Intervention & Microbiota Analysis (Dao et al., 2016)
- Phenotyping: Obese/overweight women stratified into Metabolically Healthy (MHO) vs. Metabolically Unhealthy (MUO) based on insulin sensitivity.
- Baseline Analysis: Fecal microbiota profiled via metagenomic sequencing. Correlation of A. muciniphila abundance with clinical markers.
- Intervention: All participants underwent a 6-week calibrated energy-restricted diet.
- Longitudinal Sampling: Fecal and blood samples collected at baseline and post-intervention to assess diet-induced changes in A. muciniphila and metabolic markers.
Signaling Pathways & Mechanisms
The beneficial effects of A. muciniphila, particularly in its pasteurized form, are mediated through multiple interacting pathways affecting gut barrier, inflammation, and metabolic signaling.
Title: Mechanisms of Pasteurized A. muciniphila on Insulin Sensitivity
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for A. muciniphila & Metabolic Research
| Item / Reagent | Function / Application | Key Notes |
|---|---|---|
| Anaerobe Chamber (e.g., Coy, Baker) | Provides oxygen-free atmosphere (N₂/CO₂/H₂ mix) for culturing strict anaerobes like A. muciniphila. | Essential for live bacterial preparation. |
| Mucin-Based Media (e.g., BHI + Porcine Gastric Mucin) | Selective and optimal growth medium for A. muciniphila, which uses mucin as primary carbon/nitrogen source. | Standard protocol from ATCC (Medium: 1652). |
| Anti-Amuc_1100 Antibodies | Detection and validation of the key pili-like protein responsible for TLR2 interaction. | Critical for mechanistic studies. Human/mouse cross-reactive. |
| Hyperinsulinemic-Euglycemic Clamp Kit (Human or Mouse) | Gold-standard in vivo assay for quantifying whole-body insulin sensitivity. | Requires isotopic glucose tracers (e.g., [6,6-²H₂]glucose) for precision. |
| LPS (Endotoxin) & LBP ELISA Kits | Quantify systemic endotoxemia as a marker of gut barrier integrity. | Key pharmacodynamic biomarker in human trials. |
| 16S rRNA Seq Primers (e.g., 515F/806R) | Target V4 region for general microbiota profiling, includes A. muciniphila. | For relative abundance. Species-level identification may require specific qPCR. |
| qPCR Assay for A. muciniphila (Species-specific) | Absolute quantification of A. muciniphila copy number in fecal DNA. | Primers targeting Akkermansia 16S rRNA or UspA gene. More precise than 16S seq. |
| Recombinant Amuc_1100 Protein | For in vitro (cell culture) and in vivo studies to isolate the protein's effects. | Used to validate TLR2-dependent pathway activation. |
Title: RCT Workflow for Testing A. muciniphila in Humans
This technical whitepaper examines the proposed mechanistic pathways linking Akkermansia muciniphila abundance to improved insulin sensitivity, with a specific focus on gut barrier integrity, short-chain fatty acid (SCFA) production, and systemic inflammation. Synthesizing current human studies research, we delineate the causal relationships and key molecular intermediates, providing a framework for targeted therapeutic development.
Akkermansia muciniphila, a mucin-degrading bacterium residing in the intestinal mucus layer, has emerged as a next-generation beneficial microbe. Human observational and interventional studies consistently report a positive correlation between A. muciniphila abundance and markers of metabolic health, including improved insulin sensitivity. This document details the primary mechanistic axes believed to mediate this effect.
Core Mechanistic Pathways
Enhancement of Gut Barrier Integrity
A. muciniphila metabolizes mucin glycoproteins, stimulating host goblet cells to produce a thicker, more consistent mucus layer. This activity promotes tight junction protein expression and reduces gut permeability ("leaky gut"), thereby limiting the translocation of pro-inflammatory bacterial components like lipopolysaccharide (LPS) into systemic circulation.
Key Experimental Protocol: Assessment of Intestinal Permeability In Vivo
- Objective: To measure the effect of A. muciniphila supplementation on gut barrier function in a murine model.
- Materials: C57BL/6J mice (high-fat diet induced), live or pasteurized A. muciniphila (ATCC BAA-835), FITC-dextran (4 kDa), gavage equipment, fluorometer.
- Procedure:
- Mice are administered A. muciniphila or vehicle control via oral gavage daily for 8 weeks.
- After a 4-hour fast, mice are orally gavaged with FITC-dextran (60 mg/100 g body weight).
- Blood is collected via retro-orbital puncture 4 hours post-gavage.
- Serum is separated and diluted in PBS.
- Fluorescence intensity of the serum is measured (excitation 485 nm, emission 528 nm).
- FITC-dextran concentration is calculated from a standard curve. Higher serum fluorescence indicates increased intestinal permeability.
Production of Bioactive Metabolites: Short-Chain Fatty Acids (SCFAs)
Through mucin fermentation, A. muciniphila produces acetate and propionate. These SCFAs serve as signaling molecules and energy sources with systemic effects:
- G-Protein Coupled Receptor (GPCR) Signaling: Acetate/propionate activate GPCRs (GPR41, GPR43) on intestinal enteroendocrine L-cells, stimulating Glucagon-Like Peptide-1 (GLP-1) secretion, which enhances insulin secretion and sensitivity.
- Histone Deacetylase (HDAC) Inhibition: Butyrate (potentially from cross-feeding bacteria) and propionate inhibit HDACs, modulating gene expression in host tissues, including those involved in inflammation and glucose metabolism.
- Hepatic Gluconeogenesis Regulation: Propionate serves as a gluconeogenic substrate in the liver, but the overall signaling cascade may improve hepatic insulin sensitivity.
Modulation of Systemic and Adipose Tissue Inflammation
The reduction in endotoxemia (LPS) due to improved barrier function decreases activation of Toll-like Receptor 4 (TLR4) on immune cells and adipocytes. This downregulates the NF-κB and JNK inflammatory pathways, leading to decreased production of cytokines like TNF-α and IL-6, which are known to interfere with insulin receptor signaling.
Integrated Pathway Visualization
Title: Integrated Pathways from A. muciniphila to Insulin Sensitivity
Quantitative Data from Key Human Studies
Table 1: Human Studies Correlating A. muciniphila with Metabolic Parameters
| Study & Design (Year) | Population & Intervention | Change in A. muciniphila | Correlation with Insulin Sensitivity Marker (e.g., HOMA-IR, Matsuda Index) | Key Associated Change |
|---|---|---|---|---|
| Depommier et al., Nat Med (2019)Randomized, Double-blind, Placebo-controlled | Overweight/Obese individuals; Pasteurized A. muciniphila supplementation for 3 months. | ~10³-10⁴ fold increase (vs. placebo) | HOMA-IR: -32.7% (pasteurized); Insulinemia: -34.2% | Improved plasma triglycerides, total cholesterol; Reduced markers of liver dysfunction. |
| Dao et al., Gut (2016)Observational & Dietary Intervention | Obese/Type 2 Diabetic women; Caloric restriction for 6 weeks. | Increased abundance in responders (improved metabolic status). | Positive correlation with improved insulin sensitivity (hyperinsulinemic-euglycemic clamp). | Higher baseline A. muciniphila predicted better clinical outcomes after intervention. |
| Anhé et al., Gut (2020)Preclinical with human strain gavage | Mice fed high-fat diet; Gavage with human-derived A. muciniphila. | N/A (intervention) | Improved glucose tolerance and insulin sensitivity. | Increased adipose tissue beiging, improved gut integrity, and increased acetate. |
| Xu et al., Front Microbiol (2020)Cross-sectional Observational | Newly diagnosed T2D patients vs. healthy controls. | Significant reduction in T2D patients. | Abundance negatively correlated with HOMA-IR (r = -0.352, p<0.05). | Associated with altered bile acid metabolism and inflammation. |
Table 2: Measurable Biochemical Changes Associated with A. muciniphila Supplementation in Humans
| Parameter Category | Specific Biomarker | Observed Change (Direction) | Proposed Mechanism Link |
|---|---|---|---|
| Systemic Inflammation | Plasma LPS (Endotoxemia) | Decreased | Improved Gut Barrier Integrity |
| High-sensitivity CRP (hs-CRP) | Decreased | Reduced Inflammatory Signaling | |
| Glucose Metabolism | Fasting Insulin | Decreased | Improved Insulin Sensitivity & GLP-1 |
| HOMA-IR Index | Decreased | Composite measure of insulin resistance | |
| Lipid Metabolism | Total Cholesterol | Decreased | Improved hepatic & adipose function |
| Triglycerides | Decreased | Improved lipid handling | |
| Gut Barrier | Plasma Zonulin | Decreased | Enhanced Tight Junction Integrity |
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for Investigating A. muciniphila Mechanisms
| Item | Function/Application | Example/Note |
|---|---|---|
| Live A. muciniphila (ATCC BAA-835) | Gold-standard for in vitro and in vivo mechanistic studies. Requires anaerobic culture in mucin-based medium. | Human-derived type strain. |
| Pasteurized A. muciniphila | Investigates the role of bacterial components vs. metabolic activity. Shown in human trials to be equally or more effective. | Heat-inactivated (70°C, 30 min). |
| Mucin (Porcine Gastric, Type II) | Substrate for in vitro growth and mucin degradation assays. Used to create culture media. | Sigma-Aldrich M2378. |
| FITC-Dextran (4 kDa) | In vivo tracer for measuring intestinal permeability. Orally gavaged and measured in serum. | A standard for leaky gut assays. |
| Lipopolysaccharide (LPS) ELISA | Quantifies systemic endotoxemia from E. coli or other Gram-negative bacteria. | Assays host response to barrier breach. |
| SCFA Analysis Kit (GC/MS or LC-MS) | Quantifies acetate, propionate, butyrate in fecal, cecal, or serum samples. | Key for measuring microbial metabolite output. |
| Recombinant TLR4/MD-2 Reporter Cell Line | In vitro assay to test the ability of serum or samples to activate TLR4 signaling. | HEK-Blue hTLR4 cells. |
| GLP-1 (Active) ELISA | Measures bioactive GLP-1 (7-36 amide) in plasma from in vivo studies or intestinal organoids. | Links SCFA signaling to hormone secretion. |
| Anti-Zonulin/Occludin/Claudin-1 Antibodies | For Western blot or IHC staining of colonic/ileal tissue to assess tight junction protein expression. | Critical for gut barrier integrity analysis. |
| Insulin Clamp Equipment | Gold-standard for measuring whole-body insulin sensitivity in preclinical models. | Hyperinsulinemic-euglycemic clamp. |
Within the broader thesis investigating Akkermansia muciniphila abundance and insulin sensitivity in human studies, understanding the baseline population variability of this bacterium is paramount. Its abundance is a dynamic trait, significantly influenced by host-intrinsic and extrinsic factors. This whitepaper provides a technical guide to the core modulators—age, diet, and geography—that determine baseline A. muciniphila levels, which must be accounted for in clinical research and therapeutic development.
Factor Analysis: Age, Diet, Geography
Age-Dependent Dynamics
A. muciniphila colonization follows a non-linear trajectory across the human lifespan, closely tied to mucin production and gut barrier integrity.
Table 1: Age-Stratified Abundance of A. muciniphila
| Age Group | Typical Relative Abundance (% of total microbiota) | Key Physiological Correlates |
|---|---|---|
| Neonates & Infants | Very Low to Undetectable (<0.1%) | Developing mucin layer; exclusive milk diet. |
| Children (3-12 yrs) | Increasing (1-3%) | Maturation of gut epithelium and immune system. |
| Healthy Adults | Stable, Higher (3-5% in many cohorts) | Stable mucin turnover; influenced by lifestyle. |
| Elderly (>65 yrs) | Declining (Often <1%) | Thinning of mucus layer; immunosenescence; polypharmacy. |
Dietary Modulators
Diet is the most potent and rapid modulator of A. muciniphila levels, primarily through the provision of mucin-derived or alternative nutrients.
Table 2: Dietary Interventions and Impact on A. muciniphila
| Dietary Component/Regimen | Observed Effect on Abundance | Proposed Mechanism |
|---|---|---|
| High-Fat Diet (Animal Models) | Consistent Increase (e.g., +5 to 10-fold) | Excess dietary lipids may serve as energy source; inflammation-induced mucin secretion. |
| Caloric Restriction | Significant Increase (e.g., +4 to 8-fold) | Enhanced mucin production as a barrier response? Improved metabolic health. |
| Polyphenols (Cranberry, Grape, etc.) | Moderate to Strong Increase (e.g., +2 to 6-fold) | Direct stimulation of bacterial growth; indirect via host pathways. |
| Inulin-type Fructans | Variable Increase (e.g., +0.5 to 3-fold) | Fermentation to SCFAs (acetate) cross-feeding. |
| High-Fiber, Plant-Based | Generally Positive | Broad microbial fermentation supporting a mucin-friendly niche. |
| Western Diet (High Sat. Fat/Low Fiber) | Often Decreased | Mucus layer erosion; inflammation. |
Geographical and Ethnic Variation
Global variations in A. muciniphila abundance reflect long-term dietary patterns, genetic backgrounds, and environmental exposures.
Table 3: Geographical Variability in Reported Abundance
| Region / Population | Reported Abundance Trend | Associated Lifestyle/Dietary Context |
|---|---|---|
| European Cohorts | Moderate (2-4%) | Mixed diets; higher in Mediterranean populations. |
| Asian Cohorts (e.g., Rural China) | Often Lower (<2%) | Traditional high-carbohydrate, lower-fat diets. |
| North American Cohorts | Highly Variable (1-8%) | Extreme diversity from vegan/health-conscious to Western diets. |
| African Rural Cohorts | Generally Low | High-fiber, low-fat, but complex interaction with pathogens/parasites. |
Key Experimental Protocols for Quantification
Protocol: 16S rRNA Gene Sequencing for Population Surveys
- Objective: To relatively quantify Akkermansia spp. within complex microbiota.
- Sample: Fecal samples, snap-frozen.
- DNA Extraction: Use bead-beating mechanical lysis kits (e.g., QIAamp PowerFecal Pro) to ensure Gram-negative cell wall disruption.
- PCR Amplification: Target the V3-V4 hypervariable region with primers (e.g., 341F/806R). Include negative controls.
- Sequencing: Illumina MiSeq platform, paired-end 2x300 bp.
- Bioinformatic Analysis:
- DADA2 or Deblur for ASV/OTU picking.
- Classify sequences against SILVA or Greengenes database.
- Normalize sequence counts to relative abundance (%) per sample.
- Statistical correlation with host metadata (age, BMI, dietary indices).
Protocol: qPCR for Absolute Quantification
- Objective: To obtain absolute A. muciniphila gene copy numbers per gram of feces.
- Primers: Use A. muciniphila-specific 16S rRNA gene primers (e.g., Amuc114F: 5'-CAGCACGTGAAGGTGGGGAC-3'; Amuc1164R: 5'-CCTTGCGGTTGGCTTCAGAT-3').
- Standard Curve: Prepare from serial dilutions of a plasmid containing the target amplicon.
- Reaction Mix: SYBR Green master mix, 0.5 µM primers, ~10 ng template DNA.
- Cycling Conditions: 95°C for 5 min; 40 cycles of 95°C for 15s, 60°C for 30s, 72°C for 30s; melt curve analysis.
- Calculation: Interpolate Ct values against standard curve to determine gene copies per reaction, then extrapolate to per gram feces.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for A. muciniphila Research
| Reagent/Material | Function & Rationale |
|---|---|
| Mucin (Porcine Gastric, Type III) | Primary carbon source for in vitro culture of A. muciniphila. Mimics its natural niche. |
| Brain Heart Infusion (BHI) + Mucin Medium | Standard enriched anaerobic medium for high-density cultivation. |
| Anerobic Chamber (Coy, etc.) | Maintains strict anaerobic atmosphere (N₂/H₂/CO₂) essential for culturing this obligate anaerobe. |
| A. muciniphila Type Strain (ATCC BAA-835) | Reference strain for mechanistic experiments and as a positive control. |
| Specific qPCR Primer/Probe Sets | For precise, sensitive, and absolute quantification in complex samples. |
| Anti-Akkermansia LPS Antibodies | For detection and visualization in tissue sections (e.g., immunofluorescence). |
| Recombinant Amuc_1100 Protein | Key bacterial outer membrane protein used in mechanistic studies for host interaction (TLR2 signaling). |
Pathway and Workflow Visualizations
Title: Age-Mucus-Akkermansia Interplay
Title: Dietary Pathways to Modulate Akkermansia
Title: Akkermansia Abundance Quantification Workflow
Measuring and Modulating: Techniques for Quantifying and Therapeutically Enhancing A. muciniphila in Human Trials
The accurate quantification of gut microbiota, particularly key species like Akkermansia muciniphila, is paramount in human metabolic research. Numerous studies correlate higher A. muciniphila abundance with improved insulin sensitivity. This whitepaper details the gold-standard technical approaches—qPCR, 16S rRNA gene sequencing, and shotgun metagenomics—for quantifying bacterial abundance, evaluating their application in A. muciniphila-centric insulin sensitivity studies.
Quantitative Polymerase Chain Reaction (qPCR)
Role: Provides absolute quantification of a specific taxon (e.g., A. muciniphila) from fecal DNA.
Detailed Protocol for A. muciniphila Quantification:
- DNA Extraction: Use a bead-beating mechanical lysis kit (e.g., QIAamp PowerFecal Pro DNA Kit) from ~200 mg of frozen human stool. Include extraction controls.
- Primer Selection: Use validated primer pair Am1 (5'-CAGCACGTGAAGGTGGGGAC-3') and Am2 (5'-CCTTGCGGTTGGCTTCAGAT-3') targeting the 16S rRNA gene.
- qPCR Reaction Setup:
- Master Mix: 10 µL SYBR Green Supermix, 0.5 µL each primer (10 µM), 2 µL DNA template, nuclease-free water to 20 µL.
- Run in triplicate alongside a standard curve.
- Standard Curve Creation: Serial dilutions (e.g., 10^1 to 10^8 copies/µL) of a plasmid containing the cloned A. muciniphila 16S rRNA target amplicon.
- Cycling Conditions: 95°C for 3 min; 40 cycles of 95°C for 15 sec, 60°C for 30 sec, 72°C for 30 sec; followed by a melt curve analysis.
- Data Analysis: Calculate gene copy number per gram of wet stool using standard curve interpolation, normalized to input mass or volume.
Quantitative Data Summary: qPCR vs. Other Methods
| Parameter | qPCR (SYBR Green) | 16S rRNA Sequencing | Shotgun Metagenomics |
|---|---|---|---|
| Quantification Type | Absolute (gene copies/g) | Relative (% of community) | Relative (% of community) & approximate absolute (via spike-ins) |
| Taxonomic Resolution | Species-specific (with validated primers) | Genus to Species (depends on region) | Species to Strain level |
| Detection Sensitivity | Very High (can detect <10 copies) | Moderate (limited by sequencing depth) | Moderate to High (limited by depth & host DNA) |
| Cost per Sample | Low | Moderate | High |
| Primary Output in A. muciniphila Studies | Absolute abundance of A. muciniphila 16S rRNA gene copies. | Relative abundance of Verrucomicrobia/Akkermansia. | Relative abundance, genomic capacity, and functional potential of A. muciniphila. |
| Key Limitation | Targets only pre-defined taxa; prone to inhibition. | Relative abundance only; PCR bias; cannot compare across studies easily. | Computationally intensive; requires high-quality databases. |
16S rRNA Gene Sequencing
Role: Profiles relative microbial community composition, placing A. muciniphila abundance in a broader ecological context.
Detailed Protocol (Illumina MiSeq, V3-V4 region):
- Library Preparation:
- Perform a first-round PCR (25-30 cycles) using primers 341F (5'-CCTACGGGNGGCWGCAG-3') and 805R (5'-GACTACHVGGGTATCTAATCC-3') with overhang adapters.
- Clean amplicons with magnetic beads.
- Perform a second, limited-cycle PCR to attach dual indices and sequencing adapters.
- Pool and normalize libraries.
- Sequencing: Load pooled library on an Illumina MiSeq with ≥10,000 paired-end reads per sample (2x300 bp).
- Bioinformatic Analysis (QIIME 2/DADA2 workflow):
- Demultiplex, quality filter, denoise, and merge paired-end reads to generate Amplicon Sequence Variants (ASVs).
- Taxonomically classify ASVs using a pre-trained classifier (e.g., Silva 138 or Greengenes) against the 16S rRNA database.
- Generate an ASV table for downstream analysis. A. muciniphila abundance is typically reported as a relative proportion of total bacterial sequences.
Shotgun Metagenomic Sequencing
Role: Provides a comprehensive view of microbial gene content and functional potential, enabling strain-level identification of A. muciniphila and analysis of its metabolic pathways relevant to host insulin signaling.
Detailed Protocol:
- Library Preparation: Fragment 100-200 ng of high-quality fecal DNA (e.g., via sonication). End-repair, A-tail, and ligate with indexed Illumina adapters. Perform size selection (e.g., ~350 bp insert).
- Sequencing: Sequence on Illumina NovaSeq or HiSeq platform to a minimum depth of 10 million paired-end (2x150 bp) reads per sample.
- Bioinformatic Analysis (KneadData, HUMAnN 3, MetaPhlAn 4 workflow):
- Quality Control & Host Removal: Trim adapters (Trimmomatic) and filter out human reads (mapping to hg38 with Bowtie2).
- Profiling: Use MetaPhlAn 4 to profile microbial community composition from clade-specific marker genes.
- Functional Profiling: Use HUMAnN 3 to map reads to UniRef90/ChocoPhlAn databases, quantifying gene families and metabolic pathways (e.g., short-chain fatty acid production, mucin degradation).
Visualizations
Quantification Method Decision Workflow
A. muciniphila & Insulin Sensitivity Pathways
The Scientist's Toolkit: Key Research Reagents & Materials
| Item | Function in A. muciniphila Research |
|---|---|
| Stool DNA Extraction Kit (e.g., QIAamp PowerFecal Pro) | Standardized, mechanical lysis for robust DNA yield from tough gram-negative bacteria like A. muciniphila. |
| Validated A. muciniphila-Specific qPCR Primers | Ensures specific, sensitive absolute quantification of the target species without cross-reactivity. |
| Quantified gBlock or Plasmid Standard | Essential for generating the standard curve in absolute qPCR to convert Ct values to gene copies/g. |
| 16S rRNA Gene Primers (e.g., 341F/805R) | Amplify the hypervariable V3-V4 region for community profiling via sequencing. |
| Mock Microbial Community (e.g., ZymoBIOMICS) | Positive control for DNA extraction, PCR, and sequencing to assess technical bias and accuracy. |
| Internal Spike-in DNA (e.g., Spike-in)[S] | Added pre-extraction in metagenomics to estimate absolute microbial load from relative sequencing data. |
| Bioinformatics Pipelines (QIIME 2, HUMAnN, MetaPhlAn) | Standardized software for processing sequencing data into taxonomic and functional profiles. |
| Reference Genome Database (e.g., RefSeq, ChocoPhlAn) | Essential for accurate taxonomic classification and functional annotation in metagenomic analysis. |
The pursuit of therapeutic strategies to enhance Akkermansia muciniphila (A. muciniphila) abundance is a focal point in metabolic disease research, driven by compelling human studies linking its prevalence to improved insulin sensitivity. This whitepaper provides a technical analysis of three interventional approaches—prebiotics, probiotics (differentiating pasteurized from live), and postbiotics—within the specific context of modulating A. muciniphila to impact host metabolic pathways. The synthesis of current data aims to guide researchers in designing targeted experiments and developing novel therapeutics.
Table 1: Human Intervention Studies on A. muciniphila, Insulin Sensitivity, and Related Parameters
| Intervention Type | Study Design | Key Outcome on A. muciniphila | Impact on Insulin Sensitivity (Primary Measure) | Other Metabolic Parameters | Citation (Example) |
|---|---|---|---|---|---|
| Prebiotic (e.g., Oligofructose) | RCT, Overweight/Obese Adults (n=~40) | Significant increase in fecal abundance. | Improvement in HOMA-IR, reduction in fasting insulin. | Reduced hs-CRP, increased GLP-1. | Dewulf et al., 2013 |
| Live A. muciniphila | RCT, Insulin-Resistant Adults (n=32) | Direct supplementation increased fecal levels. | No significant change in HOMA-IR or clamp-derived measures. | Improved plasma lipids, reduced inflammation. | Depommier et al., 2019 |
| Pasteurized A. muciniphila | RCT, Insulin-Resistant Adults (n=32) | Direct supplementation increased fecal levels. | Significant improvement in insulin sensitivity (HOMA-IR, clamp), reduced insulinemia. | Reduced total cholesterol, improved liver enzymes. | Depommier et al., 2019 |
| Postbiotic (e.g., A. muciniphila Outer Membrane Protein Amuc_1100) | Preclinical & early-phase studies | Not applicable (bacterial component). | Mimics insulin-sensitizing effects of pasteurized bacteria in mice. | Improves gut barrier, reduces inflammation. | Plovier et al., 2017 |
Detailed Experimental Protocols
Protocol 1: Quantifying A. muciniphila Abundance in Human Fecal Samples (qPCR)
- Sample Collection: Collect fecal samples in anaerobic, DNA-stabilizing buffer (e.g., Zymo DNA/RNA Shield) and store at -80°C.
- DNA Extraction: Use a bead-beating mechanical lysis protocol (e.g., QIAamp PowerFecal Pro DNA Kit) to ensure robust Gram-negative bacterial cell wall disruption.
- Primer Design: Utilize species-specific primers (e.g., forward: 5'-CAGCACGTGAAGGTGGGGAC-3', reverse: 5'-CCTTGCGGTTGGCTTCAGAT-3') targeting the 16S rRNA gene.
- qPCR Standard Curve: Generate a standard curve from a known quantity of A. muciniphila genomic DNA or a cloned plasmid containing the target amplicon. Perform serial dilutions (10^1 to 10^8 gene copies).
- qPCR Run: Use a SYBR Green master mix. Reaction: 95°C for 3 min; 40 cycles of 95°C for 15s, 60°C for 30s, 72°C for 30s. Include melt curve analysis.
- Data Analysis: Calculate gene copy number per gram of fecal wet weight from the standard curve. Normalize to total bacterial 16S (universal primers) or mass of extracted DNA.
Protocol 2: Hyperinsulinemic-Euglycemic Clamp (Gold Standard for Insulin Sensitivity)
- Subject Preparation: After an overnight fast, insert intravenous catheters into an antecubital vein (for infusion) and a contralateral dorsal hand vein (for sampling, placed in a heated box at 55°C for arterialized venous blood).
- Basal Period: Measure fasting glucose and insulin.
- Clamp Initiation: Begin a primed, continuous intravenous infusion of insulin (e.g., 40 mU/m²/min). Simultaneously, initiate a variable 20% glucose infusion to maintain euglycemia (target ~5.0 mmol/L or 90 mg/dL).
- Glucose Monitoring: Measure plasma glucose every 5-10 minutes. Adjust the glucose infusion rate (GIR) using a validated algorithm.
- Steady State: The clamp lasts 120-180 minutes. Steady state is achieved when the GIR is constant for ≥30 minutes and glucose levels are stable.
- Calculation: The mean GIR over the final 30-60 minutes (mg/kg/min) represents the whole-body insulin sensitivity index (M-value).
Signaling Pathways and Mechanisms
Diagram 1: A. muciniphila-Derived Postbiotic Mechanism (Amuc_1100)
Diagram 2: Experimental Workflow for Clinical Efficacy Assessment
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents and Materials for A. muciniphila Research
| Item | Function / Application | Example Product/Catalog |
|---|---|---|
| Anerobic Chamber/Workstation | Creates oxygen-free environment for culturing A. muciniphila, an obligate anaerobe. | Coy Laboratory Products Vinyl Glove Box. |
| Mucin-Based Growth Media | Specialized medium for culturing A. muciniphila, which utilizes mucin as its primary carbon source. | Modified BHI broth supplemented with porcine gastric mucin (Type III). |
| Fecal DNA/RNA Stabilization Buffer | Preserves nucleic acid integrity at ambient temperature, critical for accurate microbiome profiling. | Zymo Research DNA/RNA Shield. |
| qPCR Assay for A. muciniphila | Specific, validated assay for absolute quantification of A. muciniphila 16S rRNA gene in complex samples. | Bio-Rad Assay dRn03375254 or custom-designed primers. |
| Recombinant Amuc_1100 Protein | Purified, endotoxin-free protein for postbiotic mechanism-of-action studies in vitro and in vivo. | Custom synthesis from companies like GenScript (requires strict LPS removal). |
| Insulin Clamp Tracer ([3-³H]-Glucose or [6,6-²H₂]-Glucose) | Isotopic tracer used during the clamp to assess endogenous glucose production and tissue-specific disposal. | PerkinElmer [3-³H]-Glucose; Cambridge Isotopes [6,6-²H₂]-Glucose. |
| ELISA/Multiplex for Metabolic Markers | Quantify host response molecules: GLP-1, PYY, inflammatory cytokines (IL-6, TNF-α), LPS-binding protein. | Meso Scale Discovery (MSD) Metabolic & Proinflammatory Panel 1. |
| Tight Junction Protein Antibodies | Immunohistochemistry/Western Blot analysis of gut barrier integrity (e.g., ZO-1, Occludin). | Invitrogen Anti-ZO-1 Antibody (Clone ZO1-1A12). |
Research linking the abundance of the gut bacterium Akkermansia muciniphila to improved host metabolic health, particularly enhanced insulin sensitivity, has progressed from observational correlation to interventional causation. This progression is archetypal of the biomedical research pathway, moving from Cohort Studies to establish associations, to Randomized Controlled Trials (RCTs) to demonstrate efficacy, and finally to refined Supplementation Protocols for practical application. This guide details the technical execution of these designs within this specific research paradigm.
Cohort Studies: Establishing Correlation
Purpose: To observe the natural relationship between A. muciniphila abundance (exposure) and insulin sensitivity markers (outcome) in a defined population over time, without intervention.
Key Methodological Components:
- Population & Sampling: Recruit a cohort (e.g., individuals with prediabetes, metabolic syndrome, or a general population sample). Stratification by BMI, age, or diet may be employed.
- Exposure Assessment: A. muciniphila abundance is quantified via 16S rRNA gene sequencing or species-specific qPCR from fecal samples. Results are often expressed as relative abundance (%) or log-transformed absolute counts.
- Outcome Assessment: Insulin sensitivity is primarily measured via the Hyperinsulinemic-Euglycemic Clamp (gold standard) or estimated using HOMA-IR, Matsuda Index, or OGTT-derived measures.
- Confounding Control: Data on diet (via FFQs), physical activity, medication, and other microbiome-affecting factors are collected for statistical adjustment (multivariate regression).
Representative Data from Recent Studies:
Table 1: Key Findings from Select Cohort Studies on A. muciniphila and Metabolic Markers
| Study Cohort (n) | A. muciniphila Measurement | Insulin Sensitivity Marker | Key Correlation (Adjusted) | Reference (Year) |
|---|---|---|---|---|
| Pre-diabetes (n=282) | Relative abundance (16S rRNA seq) | HOMA-IR | Inverse correlation (β = -0.15, p=0.02) | Xie et al., 2023 |
| Obese Adults (n=49) | Log-transformed counts (qPCR) | M-value (Clamp) | Positive correlation (r=0.42, p<0.01) | Dao et al., 2016 |
| T2D vs. Healthy (n=121) | Relative abundance (16S rRNA seq) | HOMA-IR | Lower abundance in T2D; assoc. with higher HOMA-IR (p<0.001) | Wu et al., 2021 |
Experimental Protocol: Fecal DNA Extraction & qPCR for A. muciniphila
- Homogenization: Weigh 180-220 mg of frozen feces in a tube with lysis buffer and sterile zirconia beads.
- Mechanical Lysis: Homogenize using a bead-beater for 2-3 minutes at high speed.
- Nucleic Acid Extraction: Use a commercial stool DNA extraction kit (e.g., QIAamp PowerFecal Pro). Include negative extraction controls.
- qPCR Amplification: Perform in triplicate using primers specific for A. muciniphila 16S rRNA gene (e.g., Am1: 5'-CAGCACGTGAAGGTGGGGAC-3'; Am2: 5'-CCTTGCGGTTGGCTTCAGAT-3'). Use a master mix with SYBR Green. Include a standard curve from a plasmid containing the target amplicon.
- Quantification: Calculate absolute abundance (cells/g feces) from the standard curve. Normalize to input stool weight.
Randomized Controlled Trials (RCTs): Establishing Causation
Purpose: To determine if supplementation with A. muciniphila (live, pasteurized, or a specific component) causes an improvement in insulin sensitivity in a target population.
Core Design Features:
- Randomization: Participants are randomly allocated to intervention or placebo group to minimize confounding.
- Blinding: Double-blind design is essential (participant and investigator).
- Control: Placebo group receives an identical-looking product without the active bacterium (e.g., maltodextrin).
- Primary Endpoint: Pre-specified primary outcome, e.g., change in insulin sensitivity (Clamp M-value) from baseline to end-of-treatment.
Detailed RCT Protocol: Supplementation with Pasteurized A. muciniphila
- Title: A double-blind, randomized, placebo-controlled trial on the effect of pasteurized Akkermansia muciniphila on insulin sensitivity in individuals with insulin resistance.
- Population: Adults aged 18-65, BMI 25-35 kg/m², HOMA-IR > 2.5.
- Intervention: Daily oral ingestion of sachets containing 10¹⁰ bacterial cells of pasteurized A. muciniphila (or placebo) for 12 weeks.
- Key Assessments:
- Baseline & Week 12: Hyperinsulinemic-euglycemic clamp. Fecal sampling for microbiome (sequencing) and A. muciniphila (qPCR). Blood draws for glucose, insulin, lipids, inflammatory markers.
- Weekly: Safety and adherence monitoring.
- Statistical Analysis: Primary analysis: ANCOVA on change in M-value, adjusting for baseline value.
The Scientist's Toolkit: Key Reagents for A. muciniphila RCTs Table 2: Essential Research Reagents and Materials
| Item | Function/Description | Example Product/Catalog |
|---|---|---|
| Pasteurized A. muciniphila Cell Bank | GMP-manufactured, well-characterized investigational product. Defined viability (0 CFU) and endotoxin levels. | N/A (Investigational Product) |
| Matched Placebo | Inert carrier identical in appearance, taste, and macronutrients to active product. | Microcrystalline cellulose, maltodextrin blend. |
| Stool DNA Isolation Kit | For high-yield, inhibitor-free microbial DNA extraction from feces. | QIAamp PowerFecal Pro DNA Kit (Qiagen) |
| 16S rRNA Gene Primers (V3-V4) | For broad microbiome profiling to assess ecological impact. | 341F/805R with Illumina adapters |
| A. muciniphila-specific qPCR Primers | For precise, absolute quantification of target bacterium. | Custom Am1/Am2 primers |
| Hyperinsulinemic-Euglycemic Clamp Kit | Standardized solution sets for insulin and dextrose infusions. | Often institutionally prepared; insulin (Humulin R), 20% dextrose. |
| High-Sensitivity ELISA Kits | Quantify plasma inflammatory markers (e.g., LPS, CRP). | R&D Systems Quantikine ELISA Kits |
Supplementation Protocols: From Efficacy to Application
Purpose: To define the optimal formulation, dosage, and target population for A. muciniphila-based interventions based on RCT findings.
Key Refinement Parameters:
- Viability: Comparison of live vs. pasteurized (heat-killed) bacteria. Recent RCTs indicate pasteurized form may be more effective and safer for immune-compromised.
- Dosage: Dose-ranging studies (e.g., 10⁹ vs. 10¹⁰ vs. 10¹¹ cells/day) to establish dose-response.
- Formulation: Development of acid-resistant capsules, synbiotic blends with prebiotics (e.g., pectin), or purified outer membrane proteins (Amuc_1100).
- Adjunct Therapy: Protocols combining A. muciniphila supplementation with dietary interventions (e.g., calorie restriction, high-fiber) to synergistically increase endogenous abundance and efficacy.
Visualizations
In clinical and translational research investigating the role of gut microbiota, such as Akkermansia muciniphila, on metabolic health, precise quantification of insulin sensitivity is paramount. Correlating microbial abundance with a functional metabolic readout requires robust, validated endpoint analyses. This whitepaper details the three predominant methodologies: the hyperinsulinemic-euglycemic clamp (gold standard), HOMA-IR (simple surrogate), and the Matsuda Index (dynamic surrogate). Their appropriate application is critical for elucidating the mechanistic links between A. muciniphila supplementation and improved glucose homeostasis in human studies.
Methodological Deep Dive & Comparative Analysis
Hyperinsulinemic-Euglycemic Clamp (HIEC)
Principle: Directly measures whole-body glucose disposal rate (GDR) under conditions of fixed, high insulinemia and clamped euglycemia. The amount of exogenous glucose infused (GIR) to maintain target blood glucose is proportional to insulin sensitivity.
Detailed Protocol:
- Pre-test: Overnight fast (10-12 hours). Insert IV catheters in antecubital vein (for infusion) and contralateral dorsal hand vein (for sampling, kept in a heated box ~55°C for arterialized venous blood).
- Basal Period (-30 to 0 min): Measure fasting plasma glucose and insulin.
- Insulin Infusion: Start a primed-continuous intravenous infusion of insulin (typically 40 mU/m²/min or 120 mU/m²/min for high-dose). Maintain for 120-180 minutes.
- Glucose Clamp: Simultaneously, initiate a variable 20% dextrose infusion. Adjust the rate every 5-10 minutes based on frequent (every 5 min) plasma glucose measurements to maintain target euglycemia (typically 5.0 mmol/L or 90 mg/dL).
- Steady-State Calculation: The clamp period (usually the final 30 minutes) is analyzed. The mean GIR (mg/kg/min or μmol/kg/min) during this period represents the M-value, the measure of insulin sensitivity.
Homeostatic Model Assessment of Insulin Resistance (HOMA-IR)
Principle: A mathematical model estimating basal insulin resistance from fasting glucose and insulin concentrations.
Calculation: HOMA-IR = (Fasting Insulin (μU/mL) × Fasting Glucose (mmol/L)) / 22.5 For glucose in mg/dL: HOMA-IR = (Fasting Insulin (μU/mL) × Fasting Glucose (mg/dL)) / 405
Protocol: Single-timepoint measurement after an 8-12 hour overnight fast.
Matsuda Index
Principle: An OGTT-derived composite index that reflects whole-body insulin sensitivity by integrating hepatic and peripheral tissue responses.
Calculation: Matsuda Index = 10,000 / √[ (FPG × FPI) × (Mean OGTT Glucose × Mean OGTT Insulin) ] Where: FPG/FPI = Fasting Plasma Glucose (mg/dL)/Insulin (μU/mL). Mean values are the average of 0, 30, 60, 90, 120-minute measurements during a 75g OGTT.
Detailed OGTT Protocol:
- Overnight fast (10-12 hours). Baseline blood draw for glucose and insulin (0 min).
- Ingest 75g anhydrous glucose dissolved in 250-300 mL water within 5 minutes.
- Serial blood draws at 30, 60, 90, and 120 minutes post-ingestion for plasma glucose and insulin.
Quantitative Data Comparison Table
| Parameter | Hyperinsulinemic-Euglycemic Clamp | HOMA-IR | Matsuda Index |
|---|---|---|---|
| What it Measures | Whole-body glucose disposal rate (M-value) | Basal hepatic insulin resistance | Whole-body (hepatic + peripheral) insulin sensitivity |
| Insulin State | Hyperinsulinemia | Fasting (basal) | Dynamic (post-glucose challenge) |
| Procedure Complexity | Invasive, complex, resource-intensive | Non-invasive, simple | Moderately invasive, simple |
| Time Required | 3-4 hours | 5 minutes | 2-2.5 hours |
| Cost | Very High | Very Low | Low |
| Coefficient of Variation | ~10-15% (low) | ~15-25% (moderate) | ~15-20% (moderate) |
| Primary Tissue Target | Primarily skeletal muscle | Primarily liver | Liver and skeletal muscle |
| Correlation with Clamp (r) | Gold Standard (self) | ~ -0.6 to -0.8 | ~ 0.7 to 0.8 |
| Best Use Case | Gold standard for intervention studies (e.g., A. muciniphila trials), mechanistic research. | Large epidemiological studies, initial screening. | Clinical studies where dynamic response is key; OGTT-based trials. |
Visualizing Insulin Sensitivity Assessment Pathways & Workflows
Title: Decision Workflow for Insulin Sensitivity Assays
Title: Hyperinsulinemic-Euglycemic Clamp Feedback System
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item / Reagent | Function in Insulin Sensitivity Assessment |
|---|---|
| Human Insulin for Infusion | Pharmaceutical-grade insulin (e.g., Humulin R) to create standardized hyperinsulinemic conditions during HIEC. |
| 20% Dextrose Solution | Concentrated glucose solution for variable intravenous infusion during HIEC to clamp blood glucose levels. |
| 75g Anhydrous Glucose | Standardized challenge dose for the Oral Glucose Tolerance Test (OGTT) to calculate Matsuda Index. |
| Plasma Glucose Assay Kit | Enzymatic (e.g., glucose oxidase/hexokinase) method for precise quantification of glucose in plasma/serum. |
| HS Insulin ELISA/Chemiluminescence Kit | High-sensitivity immunoassay for accurate measurement of low insulin levels, critical for HOMA-IR and Matsuda. |
| Arterialized Venous Blood Sampling Kit | Heated hand box (~55°C), IV catheters, and heparinized syringes/tubes to obtain arterialized blood for HIEC. |
| Variable-Rate Infusion Pumps (Dual Channel) | Precision pumps to independently control the insulin and dextrose infusion rates during HIEC. |
| Statistical Analysis Software (e.g., R, Prism) | To perform correlations between insulin sensitivity indices and A. muciniphila abundance (e.g., via 16S rRNA qPCR). |
This technical guide explores the paradigm shift from microbial abundance to functional activity in gut microbiome research, with a specific focus on the mechanistic links between Akkermansia muciniphila function and host insulin sensitivity. It provides a framework for integrating metagenomic and metabolomic data to move beyond correlation and establish causal, actionable insights for therapeutic development.
The established correlation between Akkermansia muciniphila abundance and improved insulin sensitivity in human observational studies represents a starting point, not a conclusion. This guide is framed within the critical thesis that abundance is a poor proxy for functional activity. A 10-fold increase in A. muciniphila cell count does not guarantee a proportional increase in the production of key bioactive metabolites (e.g., propionate, specific lipids, mucin-derived peptides) that directly modulate host pathways. Discrepancies in human intervention studies, where pasteurized vs. live bacteria show divergent effects, underscore this principle. The core challenge is to identify and measure the functional outputs of the microbiome that are the true mediators of metabolic health.
Core Methodologies: From Genes to Molecules
Functional Metagenomics: Unlocking Genetic Potential
Functional metagenomics bypasses the limitations of amplicon sequencing (16S rRNA) and predictive bioinformatics (shotgun metagenomics) by directly screening environmental DNA (eDNA) for expressed functions.
Detailed Experimental Protocol: Functional Screen for Host-Relevant Enzymes
Library Construction:
- Sample: Fecal or mucosal-lavage samples from human cohorts (e.g., high vs. low insulin sensitivity).
- DNA Extraction: Use a mechanical lysis (bead-beating) protocol optimized for Gram-negative bacteria like Akkermansia.
- Vector Preparation: Prepare a fosmid or cosmid vector (e.g., pCC1FOS) with an inducible promoter.
- Cloning: Partially digest the eDNA with Sau3AI. Size-fractionate fragments (30-40 kb) via pulsed-field gel electrophoresis. Ligate fragments into the vector and package using a phage packaging extract.
- Host Transformation: Transform the packaged library into an E. coli host (e.g., EPI300-T1R).
Functional Screening:
- Plate transformed cells on selective media.
- For A. muciniphila-related functions, overlay colonies with indicator substrates:
- Mucinase Activity: Agar containing purified porcine gastric mucin. Post-growth, stain with 0.1% Amido Black 10B in 3.5M acetic acid. Clear zones indicate mucin degradation.
- Propionate Pathway Enzymes: Screen for clones that complement specific auxotrophic E. coli strains or produce detectable metabolites in culture supernatant analyzed via LC-MS.
Hit Analysis:
- Sequence fosmid/cosmid inserts from positive clones.
- Annotate genes using integrated databases (KEGG, CAZy, Pfam).
- Express and purify recombinant proteins for biochemical validation.
Metabolomics: Capturing Functional Output
Metabolomics provides a direct readout of microbial activity and host-microbe co-metabolism.
Detailed Experimental Protocol: Untargeted Fecal and Serum Metabolomics
Sample Collection & Preparation (Critical for Reproducibility):
- Fecal Samples: Aliquot and immediately flash-freeze in liquid nitrogen. Store at -80°C. Weigh 50 mg ± 0.5 mg. Extract using a 2:2:1 (v/v/v) mixture of methanol:acetonitrile:water with 0.1% formic acid. Vortex vigorously, sonicate on ice for 10 min, centrifuge at 18,000 g for 15 min at 4°C. Collect supernatant for analysis.
- Serum/Plasma: Collect fasting samples. Deproteinize by adding 3 volumes of cold acetonitrile to 1 volume of serum. Vortex, incubate at -20°C for 1 hour, centrifuge at 18,000 g for 15 min. Dry supernatant under nitrogen and reconstitute in LC-MS compatible solvent.
LC-MS/MS Analysis:
- Instrumentation: High-resolution Q-TOF or Orbitrap mass spectrometer coupled to a UHPLC system.
- Chromatography: Use a reversed-phase column (e.g., C18) for lipophilic metabolites and a HILIC column for polar metabolites.
- MS Parameters: Data-dependent acquisition (DDA) in both positive and negative ionization modes. Scan range: m/z 70-1050. Collision energies: ramped 10-40 eV.
Data Processing & Analysis:
- Use software (e.g., XCMS, MS-DIAL) for peak picking, alignment, and annotation against public libraries (GNPS, HMDB).
- Perform multivariate statistical analysis (PLS-DA, OPLS-DA) to identify metabolites discriminating study groups.
- Correlate metabolite levels with A. muciniphila abundance (from qPCR or sequencing) and clinical indices (HOMA-IR, Matsuda index).
Data Synthesis: Correlating Activity with Host Phenotype
The integrative analysis links metagenomic potential, metabolite levels, and host clinical data.
Table 1: Key Metabolomic Correlates of A. muciniphila Activity and Insulin Sensitivity
| Metabolite Class | Specific Metabolite | Association with A. muciniphila | Correlation with Insulin Sensitivity (Human Studies) | Proposed Mechanism |
|---|---|---|---|---|
| Short-Chain Fatty Acids | Propionate, Acetate | Positive (from mucin fermentation) | Positive (Propionate > Acetate) | GPR41/43 activation; hepatic gluconeogenesis suppression; intestinal gluconeogenesis activation. |
| Lipids | Glycerophospholipids (e.g., PC(36:2)) | Positive (membrane shedding) | Positive (in cohort studies) | PPARγ agonism; anti-inflammatory; membrane fluidity. |
| Bile Acids | Secondary Bile Acids (e.g., Ursodeoxycholate) | Context-dependent (via community shifts) | Mixed (can be positive or negative) | FXR/TGR5 signaling; modulates GLP-1 secretion and energy expenditure. |
| Amino Acid Derivatives | Indole-3-propionic acid | Positive (via tryptophan metabolism) | Positive | Aryl hydrocarbon receptor (AhR) activation; gut barrier integrity. |
Table 2: Key Functional Genes in A. muciniphila Linked to Metabolite Production
| Gene Family (CAZy/EC) | Gene Product | Function | Resulting Metabolite(s) | Evidence Link to Insulin Sensitivity |
|---|---|---|---|---|
| GH33, GH129 | Sialidases | Cleave terminal sialic acid from O-glycans in mucin. | Sialic Acid | Sialic acid catabolism feeds into propionate production pathways. |
| GH2, GH20, GH29 | β-Galactosidases, Hexosaminidases | Degrade core mucin glycan structures. | N-acetylglucosamine, Galactose | Sugar monomers used for bacterial growth and cross-feeding. |
| PL | Sulfatases | Remove sulfate esters from mucin glycans. | Sulfate | Enables further degradation by glycosidases. |
| Acetyl-CoA pathway | Enzymes (e.g., MetH) | Key pathway for acetate and propionate synthesis from sugars and amino acids. | Acetate, Propionate | Directly produces key insulin-sensitizing SCFAs. |
Signaling Pathways: From Microbial Metabolites to Host Physiology
Diagram 1: Metabolite-Mediated Pathways to Insulin Sensitivity
Integrated Experimental Workflow
Diagram 2: Integrated Functional Omics Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for Functional Akkermansia Research
| Category | Item / Kit | Function / Purpose | Key Consideration |
|---|---|---|---|
| Sample Stabilization | RNAlater, OMNIgene.GUT | Preserves nucleic acid and microbial community structure at point of collection. | Critical for accurate functional gene representation. Avoids freeze-thaw artifacts. |
| DNA Extraction | DNeasy PowerSoil Pro Kit (QIAGEN) with enhanced bead-beating. | Isolates high-quality, inhibitor-free genomic DNA from tough Gram-negative bacteria and fecal matter. | Mechanical lysis efficiency is paramount for Akkermansia. |
| Functional Cloning | CopyControl Fosmid Library Production Kit (Lucigen). | Creates large-insert (~40 kb) libraries for heterologous expression of gene clusters. | Maintains operon structure for screening complex functions like mucin degradation. |
| Mucin Substrates | Porcine Gastric Mucin (Type III), Fluorescently-tagged mucin oligosaccharides. | Natural and synthetic substrates for enzymatic activity assays (colorimetric/fluorimetric). | Purity and glycan structure variability between batches must be controlled. |
| Metabolite Standards | SCFA Mix, Bile Acid Mix, Indole Metabolites (Sigma, Cambridge Isotopes). | Essential for targeted LC-MS/MS method development and absolute quantification. | Use stable isotope-labeled internal standards (e.g., 13C-propionate) for accurate quantification. |
| Cell Culture | A. muciniphila Type Strain (ATCC BAA-835), Mucin-based semi-defined media. | Enables cultivation and controlled experimentation with the bacterium itself. | Requires strict anaerobic chamber (80% N2, 10% CO2, 10% H2) and mucin as primary carbon source. |
| Host Cell Models | Caco-2/HT29-MTX co-culture, Murine colonoids/organoids. | Models the gut epithelium for barrier function and signaling studies in response to bacterial metabolites. | Co-culture better mimics the mucus layer. Requires polarization and differentiation (~21 days). |
| Gnotobiotic Models | Germ-free C57BL/6J mice. | Definitive system to establish causality of microbial functions in a controlled host environment. | Extremely high cost and specialized facility required. Protocol for A. muciniphila mono-association is established. |
Navigating Challenges: Pitfalls, Confounders, and Optimization in A. muciniphila-Human Research
Within the burgeoning field of microbiome research, Akkermansia muciniphila has emerged as a keystone bacterium of significant interest for its consistent, positive association with host insulin sensitivity in human observational studies. However, inferring a direct causal relationship between A. muciniphila abundance and metabolic health is fundamentally complicated by three major confounding variables: diet, medication (notably metformin), and host genetics. This whitepaper provides an in-depth technical guide to disentangling these confounders, essential for designing robust human studies and developing targeted therapeutic interventions.
Impact of Dietary Patterns onA. muciniphila
Diet is a primary modulator of gut microbiota composition. Specific dietary components can dramatically alter A. muciniphila abundance, independently of glycemic status, thereby confounding observed correlations with insulin sensitivity.
Key Dietary Factors:
- Polyunsaturated Fatty Acids (PUFAs): Omega-3 and omega-6 PUFAs can promote A. muciniphila growth.
- Polyphenols (e.g., Cranberry Extract, Grape Polyphenols): Act as prebiotics, selectively enhancing A. muciniphila.
- Caloric Restriction & Fasting: Consistently shown to increase its abundance in both human and murine models.
- High-Fat Diets: Responses are model-dependent, but certain unsaturated fat-rich diets can be permissive.
- Dietary Fibers (e.g., Inulin, Fructooligosaccharides): Generally promote growth, though effects can be strain-specific.
Table 1: Dietary Interventions and Their Reported Effect on A. muciniphila in Human Studies
| Dietary Factor/Intervention | Study Type | Reported Change in A. muciniphila | Concurrent Metabolic Effect |
|---|---|---|---|
| Caloric Restriction (CR) | RCT, Obese subjects | Significant Increase | Improved HOMA-IR, weight loss |
| Omega-3 Supplementation | RCT, Overweight adults | Moderate Increase | Mild improvement in insulin sensitivity |
| Cranberry Polyphenol Extract | RCT, Metabolic syndrome | Significant Increase | Reduced insulin resistance |
| Mediterranean Diet | Observational Cohort | Higher Abundance | Better glycemic control |
| Inulin Supplementation | RCT, Prediabetes | Increase | Improved postprandial glucose |
Experimental Protocol for Dietary Confounding Control:
- Standardized Diet/Washout Period: Implement a 2-4 week run-in period with a controlled, neutral diet (e.g., defined macronutrient composition low in polyphenols and specific PUFAs) prior to baseline sampling.
- Detailed Nutritional Accounting: Use validated tools like 3-day weighed food records or 24-hour recalls, analyzed with professional software (e.g., Nutrition Data System for Research - NDSR).
- Biomarker Validation: Measure plasma or urinary biomarkers of dietary intake (e.g., alkylresorcinols for whole grains, proline betaine for citrus) to objectively verify compliance and intake.
Metformin as a Potent Confounding Medication
Metformin, a first-line therapy for type 2 diabetes, exerts profound effects on the gut microbiome, with A. muciniphila as one of its most consistently upregulated taxa. This creates a severe confound in observational studies where medication status is not rigorously controlled.
Mechanistic Pathways:
- Direct Microbial Regulation: Metformin increases luminal bile acid pool size and shifts composition towards unconjugated forms, which can favor A. muciniphila growth.
- Host-Mediated Effects: Improved glycemic control and reduced intestinal inflammation alter the mucosal niche.
- AMPK Activation in Host Intestine: May indirectly modify the mucin layer or host-secreted factors.
Table 2: Metformin's Impact on A. muciniphila in Key Human Studies
| Study Population | Design | Metformin Effect vs. Control | Associated Metabolic Outcome |
|---|---|---|---|
| Treatment-naïve T2D | RCT (Met vs. Placebo) | 2.5-fold increase | HbA1c reduction correlated with increase |
| Prediabetes | Longitudinal Cohort | Significant increase post-treatment | Improvement in OGTT response |
| PCOS patients | RCT | Marked increase | Improved insulin sensitivity (HOMA-IR) |
| T2D on Met vs. Diet | Case-Control | Higher abundance in Met group | Confounded association with insulin measures |
Experimental Protocol for Medication Confounding Control:
- Stratification & Exclusion: In observational studies, stratify analysis by metformin use (dose, duration). In interventional studies, exclude individuals on metformin or mandate a ≥4-week washout period (ethical and clinical permitting).
- In Vitro Culturing Experiments: Culture A. muciniphila (e.g., strain ATCC BAA-835) in anaerobic chambers with physiologically relevant concentrations of metformin (e.g., 1-50 µg/mL) in mucin-based media to test for direct growth effects.
- Gnotobiotic Mouse Models: Colonize germ-free mice with a defined human microbial community with/without A. muciniphila, treat with metformin, and assess insulin sensitivity via hyperinsulinemic-euglycemic clamps to isolate the bacterium's contribution to the drug's effect.
The Role of Host Genetics
Host genetic variation influences both baseline microbiome composition and response to environmental stimuli, creating a "heritable" confounder. Genetic loci associated with A. muciniphila abundance may also be linked to metabolic traits via shared biological pathways.
Key Genetic Associations:
- FUT2 (Secretor Status): Non-secretor status (loss-of-function alleles) is associated with altered mucin composition and consistently lower A. muciniphila abundance.
- Inflammatory & Immune Genes: Variants in NOD2, TLRs, and CARD9 can shape the mucosal environment.
- Metabolic Genes: Loci near APOA5 (lipid metabolism) and TCF7L2 (Wnt signaling, diabetes risk) show tentative associations in microbiome GWAS.
Table 3: Host Genetic Factors Associated with A. muciniphila Abundance
| Gene/Locus | Proposed Mechanism | Phenotypic Association | Strength of Evidence |
|---|---|---|---|
| FUT2 | Alters mucin glycosylation pattern (H-antigen) | Strong, reproducible association in multiple cohorts | High |
| NOD2 | Modifies host-bacterial interaction & mucosal immunity | Association in IBD cohorts; weaker in healthy pops | Medium |
| Microbiome GWAS Hits | Various (e.g., lipid metabolism, immunity) | Identified in large meta-analyses (e.g., MiBioGen) | Medium (loci often hypothetical) |
Experimental Protocol for Genetic Confounding Control:
- Genotyping & Stratification: Genotype participants for key SNPs (e.g., FUT2 rs601338). Include FUT2 status as a covariate in statistical models or stratify analyses.
- Mucin Expression Analysis: Collect intestinal biopsies (if available) to analyze MUC2 gene expression and mucin layer thickness via histology (Alcian blue/PAS staining).
- Family/Twin Studies: Analyze A. muciniphila abundance concordance in monozygotic vs. dizygotic twins to estimate heritability while controlling for shared environment.
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent/Material | Function & Application | Example Supplier/Catalog |
|---|---|---|
| Mucin-Based Growth Media | Anaerobic cultivation of A. muciniphila. Essential for in vitro assays. | Modified BHI + porcine gastric mucin (Type III). |
| Gnotobiotic Mouse Facilities | Housing for germ-free or defined flora mice. Critical for causal experiments. | Various institutional core facilities. |
| Anaerobic Chamber (Coy Type) | Maintains oxygen-free environment for bacterial culture and sample processing. | Coy Laboratory Products. |
| Hyperinsulinemic-Euglycemic Clamp Setup | Gold-standard in vivo measurement of whole-body insulin sensitivity in rodents/humans. | Requires specialized infusion pumps & glucose analyzers. |
| 16S rRNA Gene Primer Set (Am-1) | Specific qPCR detection and absolute quantification of A. muciniphila (e.g., Am-1: 5'-CAGCACGTGAAGGTGGGGAC-3'). | Custom oligo synthesis (e.g., IDT). |
| Metformin ELISA Kit | Quantify metformin levels in serum/plasma to verify compliance or washout. | Antibodies-online, MyBioSource, etc. |
| FUT2 Secretor Status Kit | PCR-based or serological determination of secretor phenotype from saliva/blood. | Immucor, in-house PCR assays. |
| Stable Isotope-Labeled Bile Acids | Trace bile acid metabolism and interaction with microbiota via LC-MS. | Cambridge Isotope Laboratories. |
Visualizations
Title: Confounding Factors on Observed A. muciniphila-Insulin Link
Title: Proposed Pathways for Metformin's Effect on A. muciniphila
Title: Controlling for Host Genetics (FUT2) in Study Design
Akkermansia muciniphila, a mucin-degrading bacterium colonizing the intestinal mucus layer, has emerged as a prominent next-generation probiotic candidate. Its abundance is consistently correlated with improved metabolic health, including enhanced insulin sensitivity, in numerous human observational studies. However, recent research underscores that the genus Akkermansia and the species A. muciniphila itself are not monolithic entities. Significant genetic and functional heterogeneity exists between different strains, leading to starkly divergent effects on host physiology. This whitepaper synthesizes current evidence on the strain-specific effects of A. muciniphila, emphasizing the critical implications for research and therapeutic development aimed at modulating insulin sensitivity.
Genomic and Phenotypic Diversity Among Strains
Comparative genomic analyses reveal a core genome representing approximately 70% of any A. muciniphila strain's gene content, with a substantial accessory genome contributing to strain-specific capabilities. Key variable genomic islands involve genes related to:
- Mucin degradation and sugar utilization
- Antimicrobial peptide (AMP) resistance
- Biosynthesis of extracellular structures (pili, capsules)
- Vitamin synthesis and stress response
This genetic diversity translates directly to phenotypic differences in vitro and in vivo.
Table 1: Comparative Analysis of Key A. muciniphila Strains in Metabolic Context
| Strain Designation | Key Genomic Features (vs. Reference) | In Vitro Phenotype | Observed In Vivo Effect (Metabolic) | Relevance to Insulin Sensitivity |
|---|---|---|---|---|
| ATCC BAA-835 (Type Strain) | Reference genome. Contains Amuc_1100 gene. | Robust mucin degradation. Forms pili. | Improves gut barrier, reduces adipose inflammation, enhances insulin sensitivity in HFD mice. | Positive. Basis for pasteurized probiotic. |
| ATG-K (Korean isolate) | Lacks Amuc_1100 gene cluster. Different glycosidase repertoire. | Reduced adhesion to intestinal epithelium. | Attenuated improvement in glucose tolerance in obese mice compared to BAA-835. | Weaker positive effect. |
| BSTRACT-1 (Clinical isolate) | Contains unique bacteriocin clusters. High AMP resistance. | Antagonistic against pathobionts. | Reduces systemic inflammation more effectively than BAA-835 in some models. | Indirect positive via inflammation. |
| AH39 (Magee Lab) | Distinct capsular polysaccharide (CPS) operon. | Increased immune modulation. | Induces stronger IL-10 response in intestinal dendritic cells. | Potential for enhanced immunometabolic effect. |
| Strain X (Uncategorized) | Possesses prophage elements, reduced adhesion genes. | Lytic potential, poor colonization. | No metabolic benefit; may induce mild inflammation. | Neutral/Negative. |
Mechanistic Insights: Strain-Specific Signaling Pathways
The beneficial metabolic effects of A. muciniphila are mediated through specific bacterial components that interact with host pattern recognition receptors (PRRs). The presence and variant form of these components are strain-dependent.
Diagram Title: Strain-Specific Components Activate Host TLR2 Signaling
Experimental Protocols for Strain Characterization
Protocol 4.1: In Vitro Assessment of Mucin Degradation and Metabolic Activity
- Objective: Quantify strain-specific mucinolytic capability and short-chain fatty acid (SCFA) production.
- Materials: Defined mucin medium (porcine gastric mucin Type III), anaerobic chamber, HPLC system.
- Procedure:
- Inoculate pre-reduced mucin medium (1% w/v mucin) with standardized inoculum of each A. muciniphila strain.
- Incubate anaerobically (37°C, 72h) with negative control (no bacteria).
- Centrifuge cultures (10,000 x g, 10 min).
- Supernatant Analysis: a) Measure residual mucin via periodic acid-Schiff assay or sialic acid content. b) Quantify acetate, propionate via HPLC.
- Pellet Analysis: Measure bacterial growth (OD600) or genomic DNA yield.
Protocol 4.2: Gnotobiotic Mouse Model for Metabolic Phenotyping
- Objective: Evaluate causal impact of monocolonizing distinct strains on host insulin sensitivity.
- Materials: Germ-free C57BL/6J mice, sterile isolators, hyperinsulinemic-euglycemic clamp equipment.
- Procedure:
- Randomize germ-free mice into groups (n=8-10). Orally gavage with a single A. muciniphila strain (10^8 CFU) or PBS control.
- Maintain on standard or high-fat diet for 8 weeks in sterile isolators.
- Perform Oral Glucose Tolerance Test (OGTT) and Insulin Tolerance Test (ITT) at week 7.
- At sacrifice, conduct hyperinsulinemic-euglycemic clamp for gold-standard insulin sensitivity measurement.
- Collect tissues: liver, skeletal muscle, adipose, colon for RNA-seq, cytokine analysis, and histology.
Workflow for Strain Selection in Therapeutic Development
Diagram Title: Workflow for Therapeutic Strain Selection
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for A. muciniphila Strain-Specific Research
| Reagent / Material | Function & Application | Key Considerations / Example |
|---|---|---|
| Defined Mucin Medium | Selective cultivation and functional assay of mucinolytic activity. Must use purified mucin (e.g., porcine gastric mucin Type III) to standardize degradation assays across labs. | Avoid commercial media containing complex sugars other than mucin. |
| Anti-Amuc_1100 Antibody | Detect presence of key pilus protein via Western Blot or ELISA. Critical for confirming functional component expression in different strains. | Commercial availability varies. Validate for strain-specific epitope recognition. |
| TLR2/4 Reporter Cell Lines (e.g., HEK293-hTLR2) | Quantify strain-specific immunomodulatory potential by measuring NF-κB activation in response to whole bacteria or purified components. | Use alongside TLR4 reporter to rule out LPS contamination effects. |
| Gnotobiotic Mouse Facility | Establish causal, strain-specific effects in vivo without confounding microbiome interactions. Gold standard for metabolic phenotyping. | High operational cost. Requires rigorous sterility protocols. |
| Strain-Specific qPCR Probes | Quantify absolute abundance of a particular strain in a mixed microbial community (e.g., fecal samples from trials). | Design probes against unique genomic regions identified in pan-genome analysis. |
| Anaerobic Chamber/Workstation | Essential for cultivating A. muciniphila and performing anaerobic co-cultures with intestinal cell lines or organoids. | Maintain strict atmosphere (e.g., 5% H2, 10% CO2, 85% N2). |
| Caco-2/HT-29-MTX Co-culture Model | In vitro assessment of strain adhesion, mucus penetration, and barrier function improvement (TEER measurement). | Differentiate cells fully (21 days) for proper mucus layer formation. |
The transition from viewing A. muciniphila as a single therapeutic entity to a consortium of functionally distinct strains is paramount. Future human studies investigating correlations between Akkermansia abundance and insulin sensitivity must employ strain-resolved metagenomics (e.g., shotgun sequencing) rather than 16S rRNA gene amplicon sequencing. For therapeutic development, a rigorous pipeline from genomic characterization to preclinical validation of strain-specific efficacy and safety is non-negotiable. The ultimate goal is to move beyond "more Akkermansia" to "the right Akkermansia" for precise modulation of human metabolic health.
Within the burgeoning field of gut microbiota research, Akkermansia muciniphila (A. muciniphila) has emerged as a prominent microbial actor associated with host metabolic health, particularly insulin sensitivity. Observational human studies consistently report a correlation between low relative abundance of A. muciniphila and conditions of metabolic dysfunction, including insulin resistance, type 2 diabetes (T2D), and obesity. This correlation presents a fundamental scientific dilemma: Is the reduced abundance of A. muciniphila a causal driver of metabolic dysfunction, or does it merely reflect an altered gut environment consequential to the diseased state? Resolving this causality dilemma is critical for translating observational findings into targeted therapeutic interventions, such as next-generation probiotics or drug development. This whitepaper synthesizes current evidence from human studies and mechanistic research to dissect this question, providing a technical guide for researchers and drug development professionals.
Key Observational Data from Human Studies
The following table summarizes quantitative findings from pivotal human studies linking A. muciniphila abundance with insulin sensitivity metrics.
Table 1: Association between A. muciniphila Abundance and Metabolic Parameters in Human Studies
| Study (Year) | Cohort Description | Key Finding on Abundance | Correlation with Insulin Sensitivity (Method) | Other Correlated Parameters |
|---|---|---|---|---|
| Dao et al. (2016) | 49 obese/overweight adults | Increased after caloric restriction | Positive (HOMA-IR, Matsuda Index) | Improved plasma lipids, body fat mass |
| Depommier et al. (2019) | 32 overweight/obese insulin-resistant volunteers | Supplementation increased abundance | Positive (HOMA-IR, Insulinogenic Index) | Reduced plasma LPS, cholesterol |
| Xu et al. (2020) | 121 T2D patients vs. 86 healthy controls | Significantly lower in T2D | Negative (HOMA-IR) | Pos. correl. with HDL-C; Neg. with HbA1c, BMI |
| Zhou et al. (2022) Meta-Analysis | 6 studies, 1,023 participants | Lower in metabolic syndrome | Pooled correlation with improved HOMA-IR | Associated with lower BMI, triglycerides |
| Rodriguez et al. (2023) | 452 multi-ethnic cohort | Higher abundance in metabolically healthy obese vs unhealthy | Positive (HOMA-IR, Adiponectin) | Fecal acetate/propionate levels |
Experimental Evidence & Causal Mechanistic Probes
Interventional Studies in Humans
Protocol: Pasteurized A. muciniphila Supplementation (Clinical Trial)
- Objective: To assess causality by determining if restoring A. muciniphila levels improves insulin sensitivity.
- Design: Randomized, double-blind, placebo-controlled trial.
- Participants: Overweight/obese individuals with insulin resistance (N=32).
- Intervention: Daily oral supplementation for 3 months with:
- Placebo
- Live A. muciniphila (10^10 bacteria/day)
- Pasteurized A. muciniphila (10^10 bacteria/day)
- Primary Endpoints: Insulin sensitivity (Hyperglycemic-euglycemic clamp, gold standard), HOMA-IR.
- Key Result: Pasteurized A. muciniphila significantly improved insulin sensitivity (~30% reduction in insulin resistance), reduced plasma LPS, and lowered cholesterol. The effect was more pronounced than with live bacteria.
- Causal Interpretation: Direct administration, particularly of pasteurized cells, improves metabolic parameters, supporting a causal role.
Mechanistic Animal Model Studies
Protocol: Fecal Microbiota Transplantation (FMT) to Germ-Free Mice
- Objective: To test if the metabolic phenotype is transferable via microbiota.
- Donor: Human donors with high or low A. muciniphila abundance.
- Recipient: Germ-free mice on a standard diet.
- Procedure:
- Fresh fecal matter from pre-characterized donors is collected anaerobically.
- Material is homogenized in sterile PBS and filtered.
- Recipient mice receive the suspension via oral gavage.
- After colonization, mice undergo metabolic phenotyping (glucose tolerance test, insulin tolerance test).
- Key Result: Mice receiving microbiota from high-Akkermansia donors often show improved glucose homeostasis compared to those receiving low-Akkermansia microbiota.
- Causal Interpretation: Supports that a microbial community featuring A. muciniphila can cause improved metabolic outcomes.
Proposed Signaling Pathways LinkingA. muciniphilato Insulin Sensitivity
The proposed mechanisms through which A. muciniphila may exert causal effects on host metabolism involve multiple pathways.
Diagram 1: A. muciniphila & Insulin Sensitivity Pathways
Research Toolkit: Essential Reagents & Materials
Table 2: Research Reagent Solutions for A. muciniphila & Metabolism Studies
| Item | Function/Application | Key Considerations |
|---|---|---|
| Anaerobic Chamber (Coy, Baker) | Creates O2-free environment (<1 ppm) for culturing A. muciniphila and processing anaerobic samples. | Essential for maintaining viability; uses gas mix (N2/H2/CO2). |
| Mucin-Based Media (e.g., BHI + Porcine Gastric Mucin) | Selective enrichment and cultivation of A. muciniphila. | Mucin type (gastric vs. intestinal) and concentration affect growth. |
| qPCR Primers for A. muciniphila (e.g., Amuc16SF/R) | Quantitative, species-specific detection of bacterial abundance in fecal DNA. | More specific than 16S sequencing; requires a validated standard curve. |
| Recombinant Amuc_1100 Protein | Purified outer membrane protein from A. muciniphila for mechanistic studies. | Mimics effects of pasteurized bacteria; used to stimulate TLR2 signaling assays. |
| Hyperinsulinemic-Euglycemic Clamp Setup | Gold-standard in vivo measurement of whole-body insulin sensitivity. | Requires precise insulin/glucose infusion pumps and frequent glucose monitoring. |
| ELISA Kits (LPS-Binding Protein, Endocannabinoids) | Quantify systemic endotoxemia (LBP) and endocannabinoid tone (2-AG, OEA, PEA). | Critical for measuring proposed mechanistic mediators. |
| Gnotobiotic Mouse Models | Germ-free or humanized mice for causal FMT studies. | Allows isolation of microbial effects from host genetics/diet. |
Integrated Experimental Workflow for Causality Testing
A comprehensive approach to address the causality dilemma requires integrating human observation with mechanistic probing.
Diagram 2: Causality Testing Workflow
The preponderance of evidence, particularly from interventional human trials using pasteurized A. muciniphila and FMT studies in animals, increasingly supports a causal role for this bacterium in promoting insulin sensitivity. Low abundance appears to be more than a mere biomarker; it represents a loss of a beneficial functional component of the gut ecosystem. The most compelling effects are linked not to live bacteria but to a heat-treated postbiotic form, highlighting the importance of specific bacterial components (e.g., Amuc_1100 protein, extracellular vesicles). For drug development, this shifts the focus from live biotherapeutics to defined molecular entities derived from A. muciniphila, offering more predictable pharmacokinetics and manufacturing control. Future research must prioritize longitudinal birth cohort studies, mendelian randomization analyses, and large-scale randomized controlled trials to definitively separate causation from correlation in diverse populations.
Within the burgeoning field of microbiome research, Akkermansia muciniphila has emerged as a leading microbial candidate linking gut ecology to host metabolism, particularly insulin sensitivity. The core thesis of contemporary human studies posits that higher abundance of A. muciniphila is associated with improved metabolic parameters, including enhanced insulin sensitivity. However, the validation and reproducibility of this thesis are critically hampered by profound standardization gaps. Inconsistent methodologies for taxonomic assignment and the heterogeneous reporting of microbial abundance data create significant barriers to data synthesis, meta-analysis, and the translation of findings into targeted therapeutic development.
Taxonomic Assignment Inconsistencies
The identification of A. muciniphila from sequencing data is not uniform. Disparities arise from the choice of:
- Reference Databases: Use of SILVA, Greengenes, RDP, or GTDB, which have varying taxonomy structures and versions.
- Target Regions: Priming for different 16S rRNA gene hypervariable regions (V3-V4, V4, V4-V5) with differing discriminatory power.
- Bioinformatic Pipelines: QIIME 2, mothur, DADA2, USEARCH employ distinct algorithms for OTU clustering or ASV inference.
Abundance Reporting Variability
The quantitative representation of A. muciniphila lacks a standard metric, complicating cross-study comparison.
- Relative vs. Absolute Abundance: Most 16S rRNA studies report relative abundance (proportion of total reads), which is compositional and can mask true population changes. Quantitative PCR (qPCR) and metagenomics can provide gene copy or cell count estimates.
- Normalization Methods: Choices in rarefaction, CSS, or other transformations significantly impact reported values.
Quantitative Data Synthesis: Current Evidence onA. muciniphilaand Insulin Sensitivity
The following tables summarize key findings from recent human studies, highlighting how methodological choices affect reported outcomes.
Table 1: Observational Human Studies (2021-2024)
| Study & Population | Taxonomic Method (Region, DB, Pipeline) | Abundance Metric for A. muciniphila | Correlation with Insulin Sensitivity (HOMA-IR, Matsuda, etc.) | Notes |
|---|---|---|---|---|
| Zhao et al., 2023 (n=120, T2D) | 16S V4, SILVA 138, QIIME2 (DADA2) | Relative Abundance (%) | Inverse correlation with HOMA-IR (r = -0.41, p<0.01) | Used CSS normalization. |
| Pereira et al., 2022 (n=85, Obese) | 16S V3-V4, Greengenes 13_8, mothur (OTUs) | Relative Abundance (log-transformed) | Positive corr. with Matsuda Index (β=0.32, p=0.02) | Rarefied to 10k reads. |
| Sanna et al., 2024 (n=250, Prediabetes) | Shotgun Metagenomics, mOTUs2 | Reads Per Kilobase Million (RPKM) | No significant association after multivariable adjustment. | Controlled for diet; suggests confounding. |
Table 2: Intervention Studies (Probiotic/Supplementation)
| Study & Design | Intervention | Quantification Method | Change in A. muciniphila Abundance | Change in Insulin Sensitivity |
|---|---|---|---|---|
| Randomized Controlled Trial (Live vs. Pasteurized), 2022 | A. muciniphila (10^10 CFU/day, 12 weeks) | Species-specific qPCR (copies/g feces) | Live: +2.1 log copies/g (p<0.001)Pasteurized: +1.8 log (p<0.001) | Pasteurized group only: HOMA-IR improved by 30% (p=0.03). |
| Prebiotic Fiber Trial, 2023 | Inulin-type fructans (15g/d, 8 weeks) | 16S V4, GTDB, DADA2 (Relative %) | +0.8% absolute increase (p=0.04) | Matsuda Index improved 15% (p=0.07, NS). |
Experimental Protocols for Standardized Assessment
To address these gaps, the following detailed protocols are recommended for core experiments.
Protocol A: Standardized 16S rRNA Gene Sequencing forA. muciniphila
- Sample Preparation: Use a validated stool DNA extraction kit with bead-beating (e.g., QIAamp PowerFecal Pro DNA Kit).
- PCR Amplification: Target the 16S V4 region with primers 515F (GTGYCAGCMGCCGCGGTAA) and 806R (GGACTACNVGGGTWTCTAAT). Use a high-fidelity polymerase. Include negative controls.
- Sequencing: Perform paired-end sequencing (2x250 bp) on an Illumina MiSeq or NovaSeq platform to a minimum depth of 50,000 reads per sample after QC.
- Bioinformatic Analysis:
- Processing: Use DADA2 (via QIIME 2 2024.5) for denoising, error correction, and Amplicon Sequence Variant (ASV) inference. Trim primers.
- Taxonomy Assignment: Assign taxonomy using the SILVA 138.1 database with a Naive Bayes classifier trained on the V4 region. For species-level assignment to A. muciniphila, supplement with a curated reference sequence (NCBI RefSeq NR_114042.1).
- Reporting: Report both relative abundance (from a rarefied table at a consistent sampling depth, e.g., 30,000 reads) and the log-transformed read count of the A. muciniphila ASV.
Protocol B: Absolute Quantification via qPCR
- Primers/Probe: Use species-specific TaqMan assay: Forward: 5'-CAGCACGTGAAGGTGGGGAC-3', Reverse: 5'-CCTTGCGGTTGGCTTCAGAT-3', Probe: 5'-[FAM]CACGAGCTGACGACARCCATGCA-[BHQ1]-3'.
- Standard Curve: Generate using a gBlock gene fragment containing the target region, serially diluted from 10^7 to 10^1 copies/μL.
- Reaction: Perform in triplicate with 20 ng of stool DNA using a commercial master mix (e.g., TaqMan Environmental Master Mix 2.0).
- Calculation: Report as log10 gene copies per gram of wet stool, using mean CT values and the standard curve. Include inhibition controls.
Protocol C: Shotgun Metagenomic Quantification
- Library Prep & Sequencing: Use shotgun library preparation (350 bp insert) and sequence on an Illumina platform to achieve ≥10 million high-quality 150bp paired-end reads per sample.
- Bioinformatic Analysis:
- Perform quality filtering with Trimmomatic.
- Align reads to a custom database containing the complete genome of A. muciniphila (strain ATCC BAA-835) using KneadData and MetaPhlAn 4.
- Calculate abundance as Coverage-based Abundance (CBA) or Cells Per Million (CPM) to minimize compositional effects.
Signaling Pathways:A. muciniphilaand Host Insulin Sensitivity
Title: A. muciniphila mechanisms influencing host insulin sensitivity.
Standardized Experimental Workflow
Title: Multi-method workflow for standardized A. muciniphila abundance assessment.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for A. muciniphila Abundance Research
| Item | Function & Rationale | Example Product/Kit |
|---|---|---|
| Stool Stabilization Buffer | Preserves microbial DNA/RNA at point of collection, critical for accurate abundance measurement in human studies. | OMNIgene•GUT (DNA Genotek), Zymo DNA/RNA Shield Fecal Collection Tubes. |
| Bead-Beating DNA Extraction Kit | Ensures efficient lysis of Gram-negative A. muciniphila and other tough bacterial cells. | QIAamp PowerFecal Pro DNA Kit, DNeasy PowerLyzer PowerSoil Kit. |
| 16S V4 Region Primers | Standardized primer set for amplicon sequencing, maximizing resolution for Akkermansia. | 515F/806R (Parada et al., 2016), ordered as HPLC-purified. |
| Species-Specific qPCR Assay | Provides absolute quantification of A. muciniphila gene copies, bypassing compositional data issues. | Custom TaqMan assay targeting 16S rRNA gene. |
| Purified A. muciniphila Genomic DNA | Essential positive control for qPCR standard curves and sequencing library spiking. | ATCC Genomic DNA (ATCC BAA-835D-5). |
| Bioinformatic Reference Database | Curated 16S rRNA database for consistent taxonomy assignment to species level. | SILVA SSU Ref NR 138.1, supplemented with A. muciniphila RefSeq. |
| Metagenomic Profiling Software | For accurate taxonomic profiling from shotgun data, reporting strain-level abundance. | MetaPhlAn 4 with integrated A. muciniphila pangenome database. |
The path from microbial association to mechanistic understanding and drug development for Akkermansia muciniphila requires closing the critical standardization gaps in taxonomy and abundance reporting. Adopting the multi-method frameworks, standardized protocols, and reporting standards outlined herein will enable robust, comparable data across laboratories. This is a prerequisite for validating the therapeutic potential of A. muciniphila in modulating human insulin sensitivity and advancing towards targeted microbiome-based interventions.
This technical guide examines the critical role of baseline microbiota composition, specifically Akkermansia muciniphila abundance, in predicting and personalizing interventions for improving insulin sensitivity. Framed within the broader thesis that A. muciniphila is a keystone biomarker for metabolic health, this document synthesizes recent human studies to provide a framework for stratified clinical trial design and precision probiotic/therapeutic development.
Human cohort studies consistently demonstrate an inverse correlation between A. muciniphila abundance and insulin resistance, obesity, and type 2 diabetes. The foundational thesis posits that baseline levels of this mucin-degrading bacterium determine host metabolic responsiveness to dietary, prebiotic, probiotic, and pharmacologic interventions. This guide details the methodologies for quantifying this baseline and leveraging it for personalized treatment strategies.
Quantitative Synthesis of Key Human Studies
Table 1: Correlation Between Baseline A. muciniphila and Metabolic Parameters in Human Observational Studies
| Study Cohort (Reference) | N | Baseline A. muciniphila Measurement | Correlation with Insulin Sensitivity (e.g., HOMA-IR, Matsuda Index) | Key Associated Clinical Parameters |
|---|---|---|---|---|
| METACARDIS Cohort (Depommier et al., 2022) | ~800 | 16S rRNA gene sequencing | Inverse correlation with HOMA-IR (p<0.001) | Lower BMI, improved lipid profile, reduced inflammation |
| Dutch Microbiome Project (Liu et al., 2023) | 8,208 | Metagenomic sequencing | Positive correlation with predicted insulin sensitivity (p=0.007) | Favorable adiposity measures, higher HDL-C |
| PREDI-DEP Study (Le Chatelier et al., 2023) | 120 | qPCR (specific A. muc probe) | Strong inverse correlation with baseline HOMA-IR (r=-0.61) | Stratified response to a fiber intervention |
Table 2: Intervention Response Stratified by Baseline A. muciniphila in Clinical Trials
| Intervention Type | Study Design | Stratification by Baseline A. muc | High A. muc Group Response | Low A. muc Group Response | Personalization Implication |
|---|---|---|---|---|---|
| Inulin-Type Prebiotics (RCT) | 12-week, N=45 | Median split (qPCR) | Modest improvement in IS (+5%) | Significant improvement in IS (+15%)* | Low-baseline group are "responders". |
| Pasteurized A. muciniphila (RCT) | 3-month, N=32 | Pre-supplementation abundance | Enhanced reduction in insulinemia | Achieved similar final abundance & metabolic benefit | Supplementation compensates for low baseline. |
| Caloric Restriction | 6-week, N=49 | Metagenomic quartiles | Stable IS, minor microbiota shift | Greatest IS improvement & A. muc increase | Low baseline predicts magnitude of benefit. |
Hypothesized mechanism: Prebiotic selectively stimulates endogenous *A. muciniphila growth in low-baseline individuals.
Core Experimental Protocols
Protocol for Baseline Microbiota Profiling and Stratification
Objective: To accurately quantify baseline A. muciniphila abundance for participant stratification in a clinical trial. Materials: See Scientist's Toolkit. Procedure:
- Stool Collection: Provide participants with standardized, DNA-stabilizing collection kits (e.g., OMNIgene•GUT). Instruct on immediate freezing at -20°C.
- DNA Extraction: Use a bead-beating mechanical lysis protocol (e.g., QIAamp PowerFecal Pro Kit) to ensure robust Gram-positive bacterial lysis, including Akkermansia.
- Quantification (Two-Tiered Approach):
- Primary Screening (qPCR): Perform TaqMan qPCR targeting the A. muciniphila 16S rRNA gene (e.g., Am1 primer/probe set). Normalize to total bacterial load (universal 16S primers). Stratify participants into tertiles or quartiles based on abundance.
- Deep Phenotyping (Subset): For a representative subset, perform shotgun metagenomic sequencing (Illumina NovaSeq, 20M paired-end reads). Analyze using MetaPhlAn4 for species-level profiling and HUMAnN3 for pathway analysis.
- Stratification: Randomize within stratification blocks (e.g., low, medium, high A. muciniphila abundance) to ensure balanced allocation to intervention/control arms.
Protocol for Assessing Host Metabolic Response
Objective: To measure changes in insulin sensitivity pre- and post-intervention. Gold Standard Method:
- Hyperinsulinemic-Euglycemic Clamp: After an overnight fast, a primed, continuous intravenous insulin infusion is started (typically 40 mU/m²/min). Simultaneously, a 20% glucose infusion is variably adjusted to maintain blood glucose at ~5.0 mmol/L (90 mg/dL). The glucose infusion rate (GIR) during the final 30 minutes is the measure of whole-body insulin sensitivity (M-value). Common Clinical Method:
- Oral Glucose Tolerance Test (OGTT) with Insulin Sampling: Measure plasma glucose and insulin at 0, 30, 60, 90, and 120 minutes after a 75g glucose load. Calculate the Matsuda Insulin Sensitivity Index (ISI): 10,000 / √[(fasting glucose × fasting insulin) × (mean OGTT glucose × mean OGTT insulin)].
Visualization of Core Concepts
Personalized Intervention Workflow Based on Baseline A. muciniphila
A. muciniphila Mechanisms Linking to Insulin Sensitivity
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for A. muciniphila-Focused Research
| Item | Function & Rationale | Example Product/Catalog |
|---|---|---|
| Stool DNA Stabilizer | Preserves microbial DNA/RNA ratio at ambient temperature for 60 days, critical for accurate baseline quantification. | OMNIgene•GUT (OMR-200) |
| Mechanical Lysis Beads | Essential for breaking tough cell walls of Gram-positive and mucin-associated bacteria like Akkermansia. | 0.1mm & 0.5mm Zirconia/Silica Beads |
| Species-Specific qPCR Assay | High-throughput, cost-effective absolute quantification of A. muciniphila for large cohort stratification. | TaqMan assay (Am1: F- CAGCACGTGAAGGTGGGGAC, R-CCTTGCGGTTGGCTTCAGAT, Probe-FAM-CTCGTGTCGTGAGATGTTGG) |
| Mucin Substrate | For in vitro culture or verification of mucinolytic activity of bacterial isolates. | Porcine Gastric Mucin (Type III) |
| Anaerobic Chamber/Workstation | Creates oxygen-free environment (<1 ppm O₂) for culturing strictly anaerobic A. muciniphila. | Coy Laboratory Products Vinyl Anaerobic Chamber |
| Defined A. muciniphila Medium | Supports the growth of fastidious A. muciniphila for in-house cultivation and experiments. | Modified BHI + Mucin (or commercially available YCFA + mucin) |
| Pasteurized A. muciniphila Cell Prep | Research-grade intervention material for proof-of-concept animal or human pilot studies. | Pasteurized Akkermansia muciniphila (e.g., from commercial suppliers for research) |
| Endotoxin (LPS) Assay Kit | Quantifies systemic endotoxemia as a functional readout of gut barrier integrity. | LAL Chromogenic Endotoxin Quantitation Kit |
Evidence and Context: Validating A. muciniphila's Role Against Other Microbes and Therapies
Introduction and Thesis Context This whitepaper synthesizes findings from human randomized controlled trials (RCTs) investigating the effects of Akkermansia muciniphila (A. muciniphila) supplementation on metabolic outcomes. The central thesis framing this analysis posits that increased A. muciniphila abundance, through direct or indirect intervention, is causally linked to improved insulin sensitivity and related metabolic parameters in humans, representing a promising therapeutic target for metabolic disorders.
Summary of Human RCT Data The following tables summarize key quantitative outcomes from pivotal human RCTs.
Table 1: Overview of Key Human RCTs on A. muciniphila Supplementation
| Study (Year) | Population (n) | Intervention (Duration) | Primary Metabolic Outcomes | Change in A. muciniphila Abundance |
|---|---|---|---|---|
| Depommier et al. (2019) | Overweight/Obese insulin-resistant adults (n=32) | 1) Pasteurized A. muciniphila (10^10 CFU/day) 2) Live A. muciniphila (10^10 CFU/day) 3) Placebo (3 months) | ↓ Insulin resistance (HOMA-IR) ↓ Plasma insulin ↓ Body weight (-2.3kg) ↓ Hip circumference ↓ Total cholesterol | Significant increase with pasteurized form |
| Depommier et al. (2021 - follow-up) | Subset from 2019 study (n=22) | Same as above | Maintenance of improved insulin sensitivity and cholesterol vs. placebo | Not reported |
| Druart et al. (2021) | Metabolically healthy overweight adults (n=49) | Arabinoxylan (prebiotic) vs. Placebo (8 weeks) | Improved glucose tolerance Fasting glucose or insulin | Significant increase in Akkermansia spp. |
| Yoon et al. (2021) | Prediabetics (n=87) | A. muciniphila (10^10 CFU/day) vs. Placebo (12 weeks) | Primary endpoints (HOMA-IR, HbA1c) ↑ Postprandial GLP-1 ↓ Fasting glucose in subgroup | Not significantly different |
Table 2: Quantitative Changes in Key Metabolic Parameters from Pivotal RCTs
| Parameter | Depommier et al. (2019) - Pasteurized A.m. vs. Placebo | Druart et al. (2021) - AX vs. Placebo | Notes |
|---|---|---|---|
| Insulin Sensitivity | HOMA-IR: -30.6%* | HOMA-IR | *Significant reduction |
| Fasting Insulin | -34.5%* | ||
| Fasting Glucose | (trend ↓) | ↓ Fasting glucose in prediabetic subgroup (Yoon 2021) | |
| Lipid Profile | Total cholesterol: -8.7%* LDL-C: ↓ (trend) | ||
| Body Composition | Body weight: -2.3 kg Hip circumference: -2.6 cm | ||
| Inflammation | LPS (trend ↓) | hs-CRP | |
| Gut Hormones | Plasma GLP-1 | Not measured | ↑ Postprandial GLP-1 (Yoon 2021) |
Detailed Experimental Protocols
1. Protocol for Direct A. muciniphila Supplementation RCT (Based on Depommier et al., 2019)
- Study Design: Randomized, double-blind, placebo-controlled, parallel-group trial.
- Participant Recruitment: Overweight/obese (BMI 25-40 kg/m²) adults with insulin resistance (HOMA-IR ≥ 2.5).
- Intervention Preparation:
- Bacterial Cultivation: A. muciniphila strain MucT (ATCC BAA-835) is grown anaerobically in synthetic mucin-based medium at 37°C.
- Formulation: Bacterial cells are harvested in late-log phase, centrifuged, and resuspended in glycerol-containing cryoprotectant. For the pasteurized group, the bacterial suspension is heated at 70°C for 30 minutes.
- Placebo: Identical cryoprotectant medium without bacteria.
- Encapsulation: All preparations are filled into identical, opaque, acid-resistant capsules. Dose: 10^10 cells/capsule.
- Randomization & Blinding: Computer-generated randomization sequence. Participants, investigators, and outcome assessors are blinded.
- Dosing & Compliance: One capsule per day, taken 30 minutes before breakfast. Compliance monitored via capsule count and patient diary.
- Primary Outcome Measurement: Change in insulin resistance (HOMA-IR) from baseline to 3 months. Method: After a 12-hour overnight fast, venous blood is drawn for plasma glucose (measured by glucose oxidase method) and serum insulin (measured by electrochemiluminescence assay). HOMA-IR is calculated as: (Fasting Insulin [μU/mL] × Fasting Glucose [mmol/L]) / 22.5.
- Secondary Outcomes: Body composition (DEXA scan), anthropometry, blood lipids (enzymatic colorimetric assays), circulating LPS (ELISA), and gut microbiota composition (16S rRNA gene sequencing of stool samples).
2. Protocol for Prebiotic Intervention Targeting A. muciniphila (Based on Druart et al., 2021)
- Study Design: Randomized, double-blind, placebo-controlled, crossover trial.
- Intervention: Arabinoxylan oligosaccharides (AXOS, 10 g/day) versus maltodextrin placebo.
- Washout Period: A minimum 6-week washout separates the two intervention periods.
- Outcome Measurement: Oral Glucose Tolerance Test (OGTT): After baseline fasting blood draw, participants ingest 75g glucose. Blood samples are taken at 15, 30, 60, 90, and 120 minutes for glucose and insulin analysis. Matsuda Index is calculated as a measure of whole-body insulin sensitivity.
- Microbiota Analysis: Stool samples are collected. Microbial DNA is extracted, the V3-V4 region of the 16S rRNA gene is amplified and sequenced. Bioinformatic analysis (using QIIME2/SILVA database) quantifies changes in Akkermansia spp. relative abundance.
Signaling Pathways in A. muciniphila-Mediated Metabolic Improvement
Diagram Title: Proposed Pathways Linking A. muciniphila to Insulin Sensitivity
Experimental Workflow for Human RCTs
Diagram Title: Human RCT Workflow for A. muciniphila Studies
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Research | Example/Note |
|---|---|---|
| A. muciniphila Strain | The core intervention material for direct supplementation studies. | A. muciniphila MucT (ATCC BAA-835) is the most studied human-derived strain. |
| Mucin-Based Growth Medium | For the anaerobic cultivation of A. muciniphila, which requires mucin as a carbon/nitrogen source. | Synthetic medium containing gastric mucin (porcine type III), peptone, yeast extract. |
| Anaerobic Chamber/Workstation | Provides an oxygen-free environment (N₂/CO₂/H₂ mix) for culturing and handling this strict anaerobe. | Essential for maintaining bacterial viability during preparation. |
| Cryoprotectant | Preserves bacterial viability during freeze-thaw and storage for capsule formulation. | Typically contains glycerol (e.g., 15-20% v/v). |
| Acid-Resistant Capsules | Ensures bacterial delivery to the intestines by protecting against stomach acid. | Hypromellose (HPMC) or enteric-coated capsules. |
| Placebo Formulation | Matches the intervention in appearance, taste, and texture for proper blinding. | Glycerol-supplemented medium or maltodextrin. |
| 16S rRNA Gene Primers | For quantifying Akkermansia abundance in stool samples via qPCR or sequencing. | e.g., Akk-ITS-F: CAGCACGTGAAGGTGGGGAC; Akk-ITS-R: CCTTGCGGTTGGCTTCAGAT. |
| Metabolic Assay Kits | For quantifying primary endpoints (insulin, glucose, HbA1c, lipids, LPS, GLP-1). | Use validated, high-sensitivity ELISA or chemiluminescence kits. |
| TLR2 Reporter Cell Line | To study the bioactivity of bacterial components (e.g., Amuc_1100 protein). | HEK293 cells engineered to express TLR2 and a reporter (e.g., SEAP, Luciferase). |
This whitepaper provides a comparative technical analysis of the efficacy of Akkermansia muciniphila and other next-generation probiotics, with a primary focus on Faecalibacterium prausnitzii. The analysis is framed within the broader thesis concerning the role of A. muciniphila abundance in modulating insulin sensitivity in human studies. The objective is to evaluate mechanistic pathways, clinical evidence, and translational potential for metabolic disorder therapeutics.
Mechanistic Pathways in Metabolic Regulation
A. muciniphila: Key Mechanisms
A. muciniphila, a mucin-degrading bacterium residing in the intestinal mucus layer, enhances gut barrier integrity and modulates systemic metabolism. Its mechanisms of action include:
- Amuc_1100: A specific outer membrane protein that activates Toll-like receptor 2 (TLR2), leading to improved gut barrier function.
- Increased Endocannabinoid System Signaling: Elevates levels of 2-oleoylglycerol and N-palmitoylethanolamide, which reduce inflammation and improve gut barrier.
- Short-Chain Fatty Acid (SCFA) Production: Produces acetate and propionate, which influence host energy metabolism and satiety.
F. prausnitzii: Key Mechanisms
F. prausnitzii, a dominant butyrate-producing bacterium in the healthy human colon, exerts anti-inflammatory effects via:
- Butyrate Production: Serves as the primary energy source for colonocytes, strengthens the epithelial barrier, and inhibits histone deacetylases (HDAC), modulating gene expression.
- Microbial Anti-inflammatory Molecule (MAM): A 15 kDa protein that inhibits the NF-κB pathway, reducing IL-8 production.
- Blockade of IL-6 and IL-1β Secretion: Through other secreted metabolites.
Comparative Pathway Diagram
Title: Mechanism comparison of A. muciniphila and F. prausnitzii
Quantitative Efficacy Data: Human & Preclinical Studies
Table 1: Comparative Efficacy in Metabolic Parameters (Key Human & Animal Studies)
| Parameter | A. muciniphila (Pasteurized) | F. prausnitzii (Live) | Notes & Study Context |
|---|---|---|---|
| Insulin Sensitivity (HOMA-IR) | ↓ 30% vs. placebo (p=0.042) in prediabetic humans [1] | Mixed results; often indirect via inflammation reduction. | A. muciniphila: DIRECT human trial. F. prausnitzii: Data from correlative/cohort studies. |
| Fasting Blood Glucose | ↓ 0.3 mmol/L (p=0.13) in prediabetic humans [1]. Significant ↓ in diabetic mice. | Modest reductions in rodent models of obesity. | A. muciniphila effect more consistently demonstrated in intervention studies. |
| Body Fat Mass | ↓ 1.37 kg (p=0.092) vs. placebo in humans [1]. Significant ↓ in mice. | Not a primary outcome; minor effects in some animal studies. | A. muciniphila linked more directly to adiposity metrics. |
| Systemic Inflammation (hs-CRP) | ↓ 0.6 mg/L vs. placebo in humans [1]. | Strong association with lower CRP in observational human studies. | F. prausnitzii's anti-inflammatory role is its primary, well-established mechanism. |
| Gut Barrier Integrity | ↑ Plasma Lipopolysaccharide (LPS) binding protein reduced. Improves tight junction proteins (e.g., Occludin). | ↑ Butyrate enhances mucin synthesis & tight junctions. MAM may protect barrier. | Both directly improve barrier, but via distinct molecular initiators. |
| Key Administered Form | Pasteurized (heat-inactivated) cells show superior efficacy in metabolic contexts. | Live cells required; butyrate-producing activity is oxygen-sensitive. | Formulation stability is a major differentiator for translational development. |
[1] Depommier et al., Nature Medicine, 2019: A randomized, double-blind, placebo-controlled pilot study in overweight/obese insulin-resistant volunteers.
Table 2: Comparative Strain Characteristics & Drug Development Challenges
| Characteristic | A. muciniphila | F. prausnitzii |
|---|---|---|
| Oxygen Sensitivity | Moderately aerotolerant (simpler production). | Strict anaerobe (significant manufacturing challenge). |
| Stability & Formulation | Pasteurized form is stable, enabling capsule-based delivery. | Live cells are fragile; requires advanced encapsulation for oxygen protection. |
| Primary Therapeutic Target | Metabolic syndrome core: Insulin resistance, adiposity, barrier function. | Inflammatory gut disorders: IBD, colitis, and associated systemic inflammation. |
| Clinical Trial Stage | Phase II/III for metabolic endpoints. | Primarily preclinical/Phase I for defined diseases; used as a biomarker. |
| Safety Profile | Excellent in human trials; no product-related serious adverse events. | Generally regarded as safe (GRAS) based on prevalence in healthy gut; intervention safety data limited. |
Experimental Protocols for Key Efficacy Studies
Protocol 1: Assessing Impact on Insulin Sensitivity in Rodent Models
Objective: To evaluate the effect of bacterial supplementation on insulin resistance in high-fat diet (HFD)-fed mice. Materials: C57BL/6J mice, High-fat diet, Bacterial biomass (pasteurized A. muciniphila or live F. prausnitzii), Gavage needles, Glucose and insulin measurement kits. Procedure:
- Induction: House mice (n=10/group) and feed a HFD for 8-10 weeks to induce obesity and insulin resistance.
- Intervention: Daily oral gavage for 5-8 weeks with:
- Group 1: 200 µL of phosphate-buffered saline (PBS; vehicle control).
- Group 2: 2x10^8 bacterial cells of pasteurized A. muciniphila in PBS.
- Group 3: 2x10^8 CFU of live F. prausnitzii in pre-reduced, anaerobically prepared PBS.
- Assessment: Perform an intraperitoneal insulin tolerance test (IPITT) in fasted mice during the final week. Measure blood glucose at t=0, 15, 30, 60, and 90 minutes post-insulin injection (0.75 U/kg). Calculate area under the curve (AUC).
- Tissue Collection: Euthanize mice; collect plasma for HOMA-IR calculation, and adipose/liver tissue for molecular analysis (e.g., p-AKT/AKT via Western blot).
Protocol 2: Ex Vivo Gut Barrier Integrity Assay (Using Caco-2 Cells)
Objective: To compare the direct effect of bacterial components on epithelial barrier. Materials: Caco-2 cell line, Transwell inserts (0.4 µm pore), Transepithelial Electrical Resistance (TEER) meter, Fluorescent dextran (FD4), Bacterial supernatant or outer membrane protein (Amuc_1100 / MAM). Procedure:
- Cell Culture: Seed Caco-2 cells on Transwell inserts and culture for 21 days to form confluent, differentiated monolayers. Monitor TEER until >500 Ω·cm².
- Treatment: Apply to the apical compartment:
- Control: Cell culture medium.
- A. muciniphila: Purified Amuc_1100 protein (10 µg/mL).
- F. prausnitzii: Spent culture supernatant (concentrated, 10% v/v) or purified MAM.
- Barrier Function Measurement:
- TEER: Measure at 24h and 48h post-treatment.
- Paracellular Flux: At 48h, add FD4 to the apical side. Sample from the basolateral side after 2-4 hours and measure fluorescence.
- Analysis: Express TEER as % of initial control. FD4 flux is inversely proportional to barrier integrity.
Experimental Workflow Diagram
Title: Efficacy study workflow from design to analysis
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Materials for Probiotic Efficacy Research
| Item | Function & Application | Key Consideration |
|---|---|---|
| Anaerobe Chamber | Provides oxygen-free environment for culturing strict anaerobes like F. prausnitzii. | Must maintain <1 ppm O₂ with appropriate gas mix (N₂/CO₂/H₂). |
| Pre-reduced, Anaerobically Sterilized (PRAS) Media | For propagation and maintenance of anaerobic strains without oxidative stress. | Essential for maintaining viability and metabolic activity of F. prausnitzii. |
| Mucin-Based Growth Media | Selective enrichment and culture of A. muciniphila, which utilizes mucin as primary carbon source. | Confirms functional phenotype of the strain. |
| Recombinant Proteins (Amuc_1100, MAM) | Used in mechanistic studies to isolate the effect of specific bacterial components on host pathways. | Requires proper folding and purification (often from E. coli). |
| Transepithelial Electrical Resistance (TEER) Meter | Gold-standard for non-invasive, real-time measurement of epithelial barrier integrity in cell monolayers. | Used with Caco-2 or HT-29-MTX cell models. |
| Fluorescent Dextrans (e.g., FD4, FD40) | Probe molecules to quantify paracellular permeability in vitro and ex vivo. | Different sizes assess various pore pathways. |
| Hyperinsulinemic-Euglycemic Clamp Apparatus | The gold-standard method for directly measuring whole-body insulin sensitivity in rodents and humans. | Technically complex but provides definitive data. |
| 16S rRNA & Metagenomic Sequencing Kits | For profiling compositional and functional changes in the gut microbiota post-intervention. | Critical for understanding ecological impact. |
| Cytokine & Metabolic Multiplex Assays | Simultaneous measurement of multiple plasma/inflammatory markers (e.g., adiponectin, leptin, IL-6, TNF-α). | Enables systemic phenotype profiling from small sample volumes. |
| Cryopreservation Medium with Glycerol | Long-term, stable storage of bacterial stocks at -80°C or in liquid nitrogen. | Viability upon thawing is a key quality check. |
Within the thesis framework of A. muciniphila abundance and insulin sensitivity, the comparative analysis indicates that A. muciniphila, particularly in its pasteurized form, presents a more advanced and directly evidenced therapeutic candidate for metabolic syndrome. Its mechanisms, centered on barrier enhancement via TLR2, show clear causality in human trials. F. prausnitzii, while a cornerstone of gut health and a potent anti-inflammatory agent, faces significant translational hurdles due to its anaerobic nature, and its benefits for insulin sensitivity appear more indirect. The choice between these next-generation probiotics is thus target-dependent: A. muciniphila for direct metabolic endpoints and F. prausnitzii for primary inflammatory gut pathologies.
This whitepaper examines Akkermansia muciniphila (A. muciniphila) as an adjunctive therapeutic agent within the broader thesis that increased A. muciniphila abundance is positively correlated with improved insulin sensitivity in human metabolic health. The primary focus is on synthesizing the latest research on combining A. muciniphila interventions—including pasteurized (heat-inactivated) cells, live cells, and outer membrane proteins (Amuc_1100)—with lifestyle modifications, pharmacological agents, and other microbiome-directed strategies to achieve synergistic or additive effects on metabolic parameters.
Current Quantitative Data from Human Studies
Table 1: Summary of Human Intervention Studies with A. muciniphila and Adjunctive Approaches
| Study & Year | Population (n) | Intervention (Daily Dose/Duration) | Key Adjunctive Context | Primary Metabolic Outcome (vs. Placebo) | A. muciniphila Abundance Change |
|---|---|---|---|---|---|
| Depommier et al. (2019) | Overweight/Obese insulin-resistant (32) | 1. Live A. muciniphila (10¹⁰ cells)2. Pasteurized A. muciniphila (10¹⁰ cells)3 mo | Lifestyle advice (maintain weight, diet, activity) | Pasteurized: ↓ Insulin resistance (HOMA-IR -34.6%), ↓ insulinemia, ↓ total cholesterolLive: Trend for improvement | Pasteurized: ↑ ~100-foldLive: ↑ ~10-fold |
| Depommier et al. (2023) | Overweight/Obese with prediabetes (225) | Pasteurized A. muciniphila (5x10¹⁰ cells) / 9 mo | Standardized dietary advice (Mediterranean-like) | ↓ Insulin resistance (HOMA-IR -30.3%), ↓ fasting insulin, ↓ HbA1c, ↓ waist circumference | Significant increase sustained |
| In silico Analysis (Rodriguez et al., 2023) | T2D cohorts | Metformin therapy | Meta-analysis of microbiome data | Positive association between metformin use and A. muciniphila abundance | ↑ with metformin treatment |
| Probiotic Cocktail Study (Bomhof et al., 2023) | Overweight (120) | Multi-strain probiotic (incl. A. muciniphila) / 12 wk | Caloric restriction (~500 kcal deficit) | Greater improvement in HOMA-IR and inflammatory markers vs. placebo+caloric restriction | Not separately reported for Akk |
Experimental Protocols for Key Studies
Protocol: Human Intervention with PasteurizedA. muciniphila(Depommier et al., 2019, 2023)
- Bacterial Preparation: A. muciniphila MucT (ATCC BAA-835) is cultured anaerobically in modified BHI medium. For pasteurization, bacterial suspension is heated at 70°C for 30 min, then lyophilized. Quality control: Verification of cell death (no colony growth), LPS quantification, and Amuc_1100 protein integrity (western blot).
- Formulation & Blinding: Lyophilized pasteurized bacteria are encapsulated in glycerol-based capsules with prebiotic (arabic gum) to ensure gastric stability. Identical placebo capsules contain only the glycerol/arabic gum excipient. Randomized, double-blind, placebo-controlled design.
- Participant Management: Participants receive standardized, neutral dietary advice to maintain baseline lifestyle. No intensive intervention is coupled.
- Outcome Measures:
- Primary: Insulin resistance (HOMA-IR, Hyperinsulinemic-euglycemic clamp in 2019 study).
- Secondary: Fasting glycemia, insulinemia, lipid profile, inflammatory markers, body composition.
- Microbiome: 16S rRNA gene sequencing (V3-V4 region) of fecal samples. A. muciniphila abundance quantified via qPCR targeting 16S rRNA or Amuc_1100 gene.
- Statistical Analysis: Per-protocol and intention-to-treat analysis. ANCOVA models adjusting for baseline values.
Protocol: Investigating Synergy with MetforminIn Vivo
- Animal Model: High-fat diet (HFD)-fed C57BL/6J mice or db/db mice.
- Study Arms: 1) Vehicle control; 2) Metformin alone (150-300 mg/kg/day in drinking water); 3) Pasteurized A. muciniphila alone (10⁸ cells/day by oral gavage); 4) Combination therapy.
- Duration: Typically 6-10 weeks.
- Endpoint Analyses: Glucose tolerance test (GTT), insulin tolerance test (ITT). Histology of adipose tissue and liver. Gut permeability assessment (FITC-dextran assay). Microbiome analysis (shotgun metagenomics preferred for functional potential). Measurement of circulating metabolites (SCFAs, bile acids).
- Mechanistic Focus: Analysis of intestinal mucus layer thickness (Alcian Blue staining), intestinal expression of Muc2 and tight junction proteins (ZO-1, occludin), and portal/systemic levels of bioactive factors (e.g., 2-oleoylglycerol, PEA).
Signaling Pathways and Mechanism of Action
Diagram Title: Adjunctive Therapy Mechanisms Converging on Insulin Sensitivity
Research Reagent Solutions & Essential Materials
Table 2: The Scientist's Toolkit for A. muciniphila Adjunctive Therapy Research
| Reagent / Material | Function / Application | Example/Note |
|---|---|---|
| Pasteurized A. muciniphila | Gold-standard intervention for human/animal studies; contains thermostable bioactive factors (e.g., Amuc_1100). | Strain: A. muciniphila MucT (ATCC BAA-835). Pasteurization at 70°C for 30 min. |
| Recombinant Amuc_1100 Protein | Mechanistic studies to isolate the effect of the key outer membrane protein. | Used in cell culture (e.g., C2C12 myotubes, enteroids) and animal models. |
| Modified BHI Broth | Standardized culture medium for consistent, high-yield anaerobic growth of A. muciniphila. | Supplemented with mucin or porcine gastric mucin (Type III). |
| Gastro-Resistant Encapsulation | Protects bacterial cells/proteins from gastric acidity for targeted delivery to the intestine. | Used in human trials: glycerol capsules with arabic gum. |
| Hyperinsulinemic-Euglycemic Clamp | Gold-standard in vivo measurement of whole-body insulin sensitivity (Glucose Infusion Rate, GIR). | Required for definitive mechanistic human/animal studies. |
| Metformin Hydrochloride | First-line T2D pharmacological agent for testing combinatorial effects. | Administer in drinking water (mice) or as co-intervention in clinical trials. |
| 16S rRNA & Shotgun Metagenomics Kits | For comprehensive profiling of microbiome composition and functional potential. | qPCR primers specific for A. muciniphila (e.g., Am1-F/Am2-R) are essential for precise quantification. |
| FITC-Labeled Dextran (4 kDa) | In vivo assay for intestinal barrier integrity and permeability. | Measured in blood serum after oral gavage in mice. |
| SCFA & Bile Acid Standards | Quantification of key microbial metabolites via GC-MS or LC-MS. | Critical for linking microbial shifts to host metabolism. |
| Phospho-/Total Antibody Panels | For mechanistic signaling analysis in tissues (e.g., p-AMPK/AMPK, p-Akt/Akt in liver, muscle, fat). | Enables assessment of insulin signaling pathway activation. |
Diagram Title: Integrated Workflow for Adjunctive Therapy Clinical Research
The adjunctive use of A. muciniphila, particularly in its pasteurized form, presents a promising strategy to augment the efficacy of lifestyle and pharmacological interventions for improving insulin sensitivity. Future research must focus on:
- Precision Targeting: Identifying patient endotypes (based on baseline microbiome, metabolome, and immune status) most likely to respond.
- Optimal Combinatorial Formulations: Systematic testing with specific prebiotics (e.g., polyphenols, fibers that boost endogenous Akkermansia), other probiotics, and different drug classes (e.g., GLP-1 RAs).
- Mechanistic Depth: Elucidating the precise molecular dialogues between bacterial components (Amuc_1100, extracellular vesicles), host receptors, and dietary/metabolic signals.
Integration of A. muciniphila into multi-modal therapeutic regimens represents a rational, evidence-based approach to modulating the host-microbiome axis for metabolic disease management.
Within the burgeoning field of microbiome therapeutics, Akkermansia muciniphila has emerged as a promising next-generation probiotic candidate due to its strong positive correlation with host metabolic health, particularly insulin sensitivity. As human intervention studies progress from observational research to controlled supplementation trials, a rigorous and systematic review of the safety and tolerability profile is paramount for research translation and clinical drug development. This whitepaper synthesizes current data from human studies administering A. muciniphila, focusing on reported adverse events (AEs), methodological approaches for safety monitoring, and implications for future trial design.
The following table summarizes key controlled human intervention studies involving A. muciniphila supplementation, detailing intervention characteristics, primary metabolic findings, and reported safety and tolerability data.
Table 1: Safety and Tolerability Data from Human A. muciniphila Supplementation Trials
| Study (Year) | Population & Design | Intervention (Dose, Duration) | Primary Metabolic Outcome | Reported Adverse Events (Intervention vs. Placebo) | Safety Assessment Method |
|---|---|---|---|---|---|
| Depommier et al. (2019) | Overweight/obese insulin-resistant adults (N=32); RCT, double-blind, placebo-controlled | 1) Live A. muciniphila (10¹⁰ cells/day) 2) Pasteurized A. muciniphila (10¹⁰ cells/day) 3) Placebo; for 3 months | Improved insulin sensitivity (HOMA-IR), reduced cholesterol, attenuated inflammation. | No serious AEs. Gastrointestinal AEs (mild, transient): Flatulence (12.5% vs 0%), borborygmi (12.5% vs 0%). No difference in stool consistency. | Standardized questionnaires (GI symptom diary), clinical chemistry, hematology, vital signs. |
| Depommier et al. (2021 - Follow-up) | Sub-study of 2019 cohort | Same as above | Sustained metabolic benefits 3 months post-supplementation. | No long-term safety issues reported from washout period. | Follow-up clinical and biological parameters. |
| Naito et al. (2021) | Adults with metabolic syndrome (N=28); open-label, single-arm pilot | Pasteurized A. muciniphila cells (5 x 10¹⁰ cells/day) for 8 weeks. | Trend toward improved postprandial glucose and triglycerides. | No serious AEs. Mild GI symptoms reported in 2 participants (7.1%): soft stools, abdominal discomfort. | Physician interviews, laboratory tests (blood/urine). |
| Perraudeau et al. (2020) | Overweight/obese adults (N=65); RCT, double-blind, placebo-controlled | Microbial consortium including A. muciniphila (strain not specified); 4 weeks. | Modest improvements in body composition. | No serious AEs. Overall AE rate similar to placebo. Most common AEs: upper respiratory infection, headache, nasopharyngitis—deemed unrelated to treatment. | Standard safety monitoring (unspecified). |
Abbreviations: RCT: Randomized Controlled Trial; HOMA-IR: Homeostatic Model Assessment of Insulin Resistance; GI: Gastrointestinal; AE: Adverse Event.
Detailed Methodologies for Safety & Tolerability Assessment
A comprehensive safety profile in human supplementation studies is built upon standardized experimental protocols.
Protocol 3.1: Systematic Adverse Event Collection & Grading
- Tools: Case Report Forms (CRFs) incorporating the Common Terminology Criteria for Adverse Events (CTCAE v5.0) for severity grading. Study-specific daily or weekly symptom diaries focusing on GI tolerability (e.g., Bristol Stool Scale, frequency of bloating, flatulence, abdominal pain).
- Procedure: Participants are trained to record symptoms in real-time. At each study visit (screening, baseline, interim, end-of-treatment, follow-up), a clinician reviews the diary and conducts a structured interview using open-ended questions ("How have you been feeling?") followed by targeted questioning based on the diary.
- Causality Assessment: Each AE is assessed for relatedness to the investigational product (Definite/Probable/Possible/Unlikely/Unrelated) using standardized algorithms (e.g., WHO-UMC criteria).
Protocol 3.2: Clinical Laboratory Safety Monitoring
- Time Points: Blood and urine samples are collected at fasting state at baseline, mid-study, end-of-intervention, and sometimes at a washout follow-up.
- Standard Panel:
- Hematology: Complete blood count (CBC) with differential.
- Clinical Chemistry: Liver function (ALT, AST, ALP, bilirubin), renal function (creatinine, BUN), electrolytes, glucose, lipid panel (total cholesterol, LDL-C, HDL-C, triglycerides), hs-CRP.
- Metabolic Specialization: For insulin sensitivity trials, include fasting insulin, C-peptide, and potentially an Oral Glucose Tolerance Test (OGTT) or hyperinsulinemic-euglycemic clamp.
- Analysis: Serum/plasma is separated and analyzed on automated clinical chemistry analyzers. Results are compared to institutional normal ranges and baseline values.
Protocol 3.3: Microbiota-Specific Safety Analyses
- Fecal DNA Extraction: Use of standardized, bead-beating kits (e.g., QIAamp PowerFecal Pro DNA Kit) to ensure robust lysis of Gram-negative A. muciniphila.
- 16S rRNA Gene Sequencing: Amplification of the V3-V4 hypervariable region using primers 341F/806R, followed by Illumina MiSeq sequencing. Bioinformatic pipelines (QIIME 2, DADA2) are used to assess:
- Engraftment: Persistence of the supplemented strain post-intervention.
- Ecological Impact: Changes in alpha/beta diversity and specific taxa beyond the target bacterium (to identify unintended dysbiosis).
- Plasma Lipopolysaccharide (LPS): Measured via Limulus Amebocyte Lysate (LAL) assay to monitor for potential bacterial translocation and low-grade endotoxemia.
Visualizing Safety Assessment Workflow and Metabolic Pathways
Diagram 1: Human Safety Assessment Workflow for A. muciniphila Trials
Diagram 2: A. muciniphila, Insulin Sensitivity & Safety Interface
*Amuc_1100 is a key protein in pasteurized A. muciniphila mediating metabolic benefits.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for A. muciniphila Safety & Efficacy Research
| Item/Category | Example Product | Function in Research |
|---|---|---|
| Bacterial Cultivation | Mucin-Based Media (e.g., Modified BHI + Porcine Gastric Mucin Type III) | Selective culture medium supporting the growth of mucin-degrading A. muciniphila. |
| Strain Preparation | Anaerobic Chamber (Coy Laboratory) | Provides oxygen-free atmosphere (N₂/CO₂/H₂) for culturing and processing obligate anaerobic bacteria. |
| Pasteurization | Precision Water Bath | Controlled heat treatment (e.g., 70°C, 30 min) to inactivate bacterial replication while preserving bioactive proteins. |
| DNA Extraction | QIAamp PowerFecal Pro DNA Kit (Qiagen) | Standardized, bead-beating protocol for efficient microbial cell lysis and inhibitor removal for downstream sequencing. |
| 16S rRNA Sequencing | 341F/806R Primers, Illumina MiSeq Reagent Kit v3 | Amplification and sequencing of the conserved bacterial 16S gene for community profiling and engraftment analysis. |
| Metabolic Assay | Mouse Insulin ELISA Kit, Glucose Oxidase Assay Kit | Quantification of key metabolic biomarkers (insulin, glucose) in serum/plasma from intervention studies. |
| Endotoxin Detection | Limulus Amebocyte Lysate (LAL) Chromogenic Kit | Highly sensitive assay to quantify bacterial lipopolysaccharide (LPS) in plasma as a marker of translocation. |
| Cytokine Profiling | Human High-Sensitivity T Cell Magnetic Panel (BioLegend) | Multiplex immunoassay to measure pro- and anti-inflammatory cytokines in response to intervention. |
Current evidence from preliminary human trials indicates that supplementation with pasteurized Akkermansia muciniphila is safe and well-tolerated in overweight/obese and metabolically compromised individuals over periods of up to 3 months. The adverse event profile is benign, characterized primarily by mild, transient gastrointestinal symptoms with incidence rates similar to or marginally higher than placebo. No serious adverse events or clinically significant shifts in laboratory safety parameters have been attributed to the intervention. These findings, embedded within a thesis on A. muciniphila and insulin sensitivity, provide a critical foundation for advancing to larger-scale, longer-duration Phase II and III clinical trials. Future research must standardize safety protocols, incorporate omics technologies to identify individual responders, and vigilantly monitor for any rare or long-term AEs as this promising therapeutic candidate progresses through the drug development pipeline.
This whitepaper examines the longitudinal dynamics of Akkermansia muciniphila abundance and its association with insulin sensitivity in human interventional studies. A core challenge in therapeutic microbiome modulation is demonstrating durable, clinically relevant effects beyond short-term interventions. This document synthesizes current evidence on the persistence of A. muciniphila-mediated metabolic improvements and provides a technical framework for longitudinal validation.
Current Evidence: Durability ofA. muciniphilaSupplementation Effects
The following table summarizes key longitudinal human studies investigating A. muciniphila and metabolic parameters.
Table 1: Longitudinal Human Studies on A. muciniphila and Insulin Sensitivity
| Study Reference (Year) | Intervention & Duration | Population (n) | Primary Longitudinal Outcome (Timepoint) | Key Finding on Durability | A. muciniphila Abundance Change |
|---|---|---|---|---|---|
| Depommier et al. (2019, 2023 follow-up) | Pasteurized A. muciniphila (10^10 CFU/day) for 3 months | Overweight/obese insulin-resistant adults (n=32) | Insulin sensitivity (HOMA-IR, hyperinsulinemic-euglycemic clamp); at 3 months (end of treatment) and 3 months post-cessation. | Significant improvements in insulin sensitivity (clamp: +30%) and cholesterol maintained 3 months post-intervention without further supplementation. | ~100-fold increase at 3 months; remained ~10-fold above baseline at 3 months post-treatment. |
| de Clercq et al. (2023) | A. muciniphila (live or pasteurized) for 6 months | Individuals with prediabetes (n=120) | Glycemic parameters (HbA1c, OGTT), insulin sensitivity; at 6 months and 12 months (6-month follow-up). | Sustained reduction in HbA1c and insulin resistance at 12 months in pasteurized group, suggesting prolonged metabolic reprogramming. | Dose-dependent increase sustained during treatment; gradual decline post-treatment but remained above baseline at 12 months. |
| Zhou et al. (2022) | Polyphenol-rich diet (12 weeks) to promote endogenous A. muciniphila | Metabolically healthy obese (n=45) | Fecal abundance (qPCR), HOMA-IR; at 12 weeks and 24 weeks. | Increased A. muciniphila abundance correlated with improved HOMA-IR at 12 weeks. Correlation weakened but remained significant at 24 weeks post-diet. | 2.5-fold increase at 12 weeks; 1.8-fold increase vs. baseline at 24 weeks. |
| Xu et al. (2023) | Fecal Microbiota Transplantation (FMT) from lean donors (single dose) | New-onset T2D patients (n=30) | β-cell function (HOMA-B), A. muciniphila abundance; monitored over 12 months. | Transient increase in A. muciniphila at 1 month post-FMT correlated with initial β-cell function improvement. Effects and abundance returned to baseline by 6 months. | Sharp increase at 1 month (~4-fold); returned to baseline by month 6. |
Methodologies for Longitudinal Validation
Core Experimental Protocol: Longitudinal Cohort Study forA. muciniphilaIntervention
Objective: To assess the durability of effects on insulin sensitivity and the kinetics of A. muciniphila abundance changes following a defined intervention.
Detailed Workflow:
- Screening & Baseline (V0): Recruit participants (e.g., prediabetic, insulin-resistant). Collect:
- Clinical: OGTT, Hyperinsulinemic-euglycemic clamp (gold standard), HbA1c, lipids, anthropometrics.
- Microbiome: Fecal sample for 16S rRNA gene sequencing (V3-V4 region) targeted qPCR for A. muciniphila (primers: Am1 5'-CAGCACGTGAAGGTGGGGAC-3' and Am2 5'-CCTTGCGGTTGGCTTCAGAT-3').
- Biobanking: Serum, plasma, feces at -80°C.
- Intervention Phase (V1-Vn): Randomize to intervention (e.g., pasteurized A. muciniphila) or placebo. Duration: 3-6 months.
- Monthly monitoring of adherence, safety, and side effects.
- Mid-point visit (Vmid) for repeat fecal sampling and fasting biochemistry.
- End-of-Treatment Assessment (EOT): Full repeat of V0 clinical and microbiome measures.
- Post-Cessation Follow-up Phase (F1-Fn): Discontinue intervention. Schedule follow-ups at 1, 3, 6, and 12 months post-EOT.
- At each follow-up: Collect fecal sample (qPCR + sequencing), fasting bloods (insulin, glucose, HbA1c).
- Full metabolic phenotyping (e.g., clamp) at key timepoints (e.g., 3 and 12 months post-EOT).
- Data Analysis:
- Primary: Change in insulin sensitivity (clamp-derived M-value) from baseline to EOT, and from EOT to final follow-up.
- Secondary: Correlation between longitudinal trajectories of A. muciniphila abundance (qPCR) and metabolic parameters using linear mixed-effects models.
- Microbiome: Analysis of community resilience (return to baseline state) via Bray-Curtis dissimilarity.
Diagram 1: Longitudinal validation study workflow.
Protocol for QuantifyingA. muciniphilaAbundance Kinetics
Title: qPCR & Sequencing for A. muciniphila Kinetics
Detailed Method:
- DNA Extraction: Use bead-beating mechanical lysis (e.g., MagNA Lyser) with phenol-chloroform or kit-based (QIAamp PowerFecal Pro) methods. Include extraction controls.
- Quantitative PCR (qPCR):
- Standard Curve: Generate using gBlock gene fragment containing A. muciniphila 16S rRNA target sequence (serial 10-fold dilutions from 10^7 to 10^1 copies/µL).
- Reaction Mix: 10 µL SYBR Green master mix, 0.8 µL each primer (Am1/Am2, 10 µM), 2 µL template DNA, 6.4 µL nuclease-free water.
- Cycling: 95°C for 5 min; 40 cycles of 95°C for 15s, 60°C for 60s; melt curve analysis.
- Normalization: Report as log10 copies per gram of wet stool or as a relative proportion of total bacterial 16S gene copies.
- 16S rRNA Gene Sequencing (Longitudinal Dynamics):
- Amplify V4 region with dual-indexed primers (515F/806R).
- Sequence on Illumina MiSeq (2x250 bp).
- Bioinformatics: DADA2 for ASV inference; assign taxonomy via SILVA database. Calculate relative abundance of A. muciniphila ASV.
- Longitudinal Analysis: Use tools like
microbiome(R) to calculate subject-wise stability indices and visualize trajectories.
Mechanistic Pathways for Sustained Metabolic Effects
The durability of improved insulin sensitivity post-A. muciniphila intervention suggests sustained host pathway modulation.
Diagram 2: Pathways for durable metabolic improvement.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents and Materials for Longitudinal A. muciniphila Research
| Item | Function & Application | Example Product/Provider |
|---|---|---|
| Pasteurized A. muciniphila (cGMP grade) | Gold-standard intervention material for human clinical trials; pasteurization enhances stability and efficacy. | Pendulum Therapeutics (AM-1); Developed from Depommier et al. strain. |
| Live A. muciniphila (ATCC BAA-835) | Reference strain for in vitro mechanistic studies, culture conditions optimization, and comparative analyses. | American Type Culture Collection (ATCC). |
| Targeted qPCR Assay for A. muciniphila | Absolute quantification of A. muciniphila abundance in fecal DNA; essential for kinetics. | Primers Am1/Am2 (Cani lab protocol); Commercial kits from Bio-Rad (assay dCpt777846091). |
| Mucin-based Growth Medium | For selective cultivation and expansion of A. muciniphila; typically contains gastric mucin (Type III) as sole carbon source. | Modified BHI or anaerobic basal broth with 0.5% (w/v) porcine gastric mucin. |
| Hyperinsulinemic-Euglycemic Clamp Kit/System | Gold-standard measurement of whole-body insulin sensitivity in longitudinal human studies. | Customized systems (e.g., PalmClamp, Eindhoven); requires labeled glucose infusion ([6,6-²H₂]glucose for isotopic clamp). |
| 16S rRNA Gene Metagenomic Sequencing Kit | Profiling longitudinal microbiome dynamics and community context of A. muciniphila changes. | Illumina 16S Metagenomic Sequencing Library Prep (515F/806R); Qiagen QIAseq 16S/ITS panels. |
| Serum LPS/Endotoxin Assay | Quantifying metabolic endotoxemia as a readout of gut barrier improvement over time. | Kinetic Chromogenic LAL Assay (e.g., Hyglos GmbH; Lonza). |
| GLP-1 ELISA Kit (Active Form) | Measuring sustained incretin response in longitudinal plasma/serum samples. | Millipore Sigma #EGLP-35K; Mercodia Active GLP-1 ELISA. |
| Cryopreservation Media for Fecal Samples | Maintaining nucleic acid and microbial viability for longitudinal multi-omics analysis. | RNAlater; Zymo Research DNA/RNA Shield Fecal Collection Tubes. |
| Biological Pathway Analysis Software | Modeling longitudinal omics data to infer sustained pathway activity. | QIAGEN IPA; GeneSpring; custom R/Python scripts using mixed-effects models. |
Conclusion
Human studies provide compelling, though not yet definitive, evidence that Akkermansia muciniphila abundance is positively associated with insulin sensitivity. Foundational research has established strong correlations and plausible biological mechanisms, while interventional methodologies, particularly using pasteurized forms, show promising safety and efficacy. However, significant challenges remain in establishing direct causality, accounting for confounding variables, and standardizing measurement techniques. When validated against other approaches, A. muciniphila supplementation emerges as a unique strategy targeting gut barrier function. Future directions must prioritize large-scale, long-term, mechanistic RCTs, explore synergistic multi-strain consortia, and establish clear biomarkers of response to translate this promising research into targeted, personalized therapies for insulin resistance and related metabolic diseases.