Advanced Feature Engineering for CGM Time Series Data: From Fundamentals to Clinical Translation
This article provides a comprehensive guide to feature engineering for Continuous Glucose Monitoring (CGM) time series data, tailored for researchers, scientists, and drug development professionals.
Advanced Feature Engineering for CGM Time Series Data: From Fundamentals to Clinical Translation
Abstract
This article provides a comprehensive guide to feature engineering for Continuous Glucose Monitoring (CGM) time series data, tailored for researchers, scientists, and drug development professionals. It covers the foundational principles of CGM-derived metrics, explores methodological approaches for feature extraction and selection, addresses common challenges and optimization techniques, and discusses rigorous validation frameworks. By synthesizing current research and tools, this resource aims to equip readers with the knowledge to build more robust, interpretable, and clinically actionable machine learning models for glucose prediction, metabolic subphenotyping, and therapeutic development.
Understanding the Landscape: Core CGM Features and Their Physiological Significance
The Fundamental Structure of CGM Data
Continuous Glucose Monitoring data represents a dense, multivariate time series. At its core, a CGM device measures glucose levels in interstitial fluid at regular intervals, typically ranging from 1 to 15 minutes, generating up to 1,440 readings daily [1]. The raw data structure consists of sequential timestamp-glucose value pairs, but its full utility is realized when contextualized with life-log events.
Table 1: Core Components of Raw CGM Data Structure
| Component | Description | Data Type | Typical Format/Frequency |
|---|---|---|---|
| Timestamp | Time of glucose measurement | DateTime | Regular intervals (e.g., every 5 min) |
| Glucose Value | Glucose concentration in interstitial fluid | Numerical (mg/dL or mmol/L) | 80-400 mg/dL typical range |
| Life-log Events | Contextual markers for behavior | Categorical | Meal times, exercise, medication |
| Signal Quality | Sensor integrity indicators | Numerical/Categorical | Signal strength, reliability flags |
The raw CGM signal requires substantial preprocessing before analysis, as it contains multiple artifacts including sensor noise, missing data due to signal loss, and physiological time lags between blood and interstitial glucose compartments [2] [1]. Additionally, compression artifacts can occur from sensor pressure, and transient disturbances may arise from medication interference or hydration status changes.
Essential Preprocessing Pipeline
Data Cleaning and Imputation
The initial preprocessing stage focuses on identifying and addressing data quality issues through automated and manual review processes.
Table 2: Common CGM Data Anomalies and Handling Methods
| Anomaly Type | Identification Method | Recommended Handling |
|---|---|---|
| Missing Data | Gaps in timestamp sequence | Multiple imputation for short gaps (<20 min); flag longer gaps for exclusion |
| Physiological Outliers | Values outside plausible range (e.g., <40 or >400 mg/dL) | Remove with contextual review |
| Technical Artifacts | Sudden, physiologically impossible spikes/drops | Smoothing filters (e.g., Kalman) |
| Signal Dropout | Extended periods of zero or null values | Segment removal with documentation |
For missing data imputation, studies demonstrate that multiple imputation chains using expectation-maximization algorithms outperform simple linear interpolation, particularly for gaps exceeding 15 minutes [1]. The preprocessing workflow must maintain annotation of all imputed values to enable sensitivity analysis during statistical modeling.
Temporal Alignment and Aggregation
CGM data inherently possesses a multi-scale temporal structure that must be preserved through appropriate aggregation methods:
CGM Data Preprocessing Workflow
Advanced Preprocessing for Feature Engineering
Chronobiological Feature Extraction
The temporal structure of CGM data contains biologically meaningful patterns that reflect circadian rhythms and behavioral cycles. Chronobiologically-informed features have demonstrated significant predictive value for longer-term glycemic dysregulation [3]. Key methodologies include:
Time-of-Day Standard Deviation (ToDSD): Calculated by aligning CGM records by clock time across multiple days and computing within-individual standard deviation separately for each time step. Research shows strong correlation between ToDSD and Time-in-Range (TIR) metrics (Spearman ρ = -0.81, p < 0.0001) [3].
Multi-timescale Complexity Indices: These features capture glycemic variability across different temporal scales, incorporating both ultradian (within-day) and circadian (between-day) patterns. Implementation involves wavelet decomposition or multi-scale entropy analysis applied to continuous 2-week data segments [3].
Functional Data Analysis (FDA) Approaches
FDA represents a paradigm shift from traditional summary metrics by treating CGM trajectories as continuous mathematical functions rather than discrete measurements [4] [1]. The FDA preprocessing pipeline involves:
- Curve Fitting: Transforming discrete CGM measurements into smooth functions using basis splines (B-splines) or Fourier basis functions
- Functional Principal Component Analysis (FPCA): Decomposing functional data to identify dominant modes of variation
- Derivative Analysis: Examining rate-of-change patterns to identify critical periods for intervention
In practice, FDA applied to 10 days of 5-minute CGM data from 1,067 participants revealed three dominant functional principal components explaining 83% of glycemic variability, enabling identification of clinically relevant subgroups with distinct phenotypic patterns [4].
Advanced Feature Engineering Pathways
Experimental Protocols for CGM Data Analysis
Protocol: Functional Principal Component Analysis of CGM Data
Purpose: To identify dominant patterns of glycemic variability in dense CGM time series data.
Materials:
- 10-14 days of continuous CGM data (5-minute intervals)
- Computational environment with FDA packages (e.g., R
fdapackage or Pythonscikit-fda)
Methodology:
- Data Preparation: Ensure complete data for analysis period with missing values imputed using Kalman filtering or expectation-maximization algorithms
- Basis System Selection: Fit raw CGM data to B-spline basis functions with knots placed at 2-hour intervals
- Smoothing Parameter Optimization: Use generalized cross-validation to determine optimal smoothing parameter λ
- FPCA Execution: Compute functional principal components and corresponding scores for each participant
- Pattern Interpretation: Examine eigenfunctions to identify dominant temporal patterns (e.g., postprandial spikes, nocturnal trends)
Validation: Apply clustering algorithms (k-means or hierarchical) to FPCA scores to identify clinically distinct glycemic phenotypes [4].
Protocol: Deep Learning Framework for Glucose Prediction
Purpose: To develop a virtual CGM system capable of predicting glucose values from life-log data alone.
Materials:
- Paired CGM and life-log data (diet, physical activity, sleep)
- Deep learning framework (PyTorch or TensorFlow)
- Bidirectional LSTM architecture with attention mechanisms
Methodology:
- Data Acquisition: Collect CGM measurements alongside detailed records of dietary intake (calories, macronutrients), physical activity (METs, step counts), and temporal markers [2]
- Sequence Construction: Extract subsequences using sliding-window technique (e.g., 4-hour windows)
- Model Architecture: Implement encoder-decoder framework with bidirectional LSTM layers and dual attention mechanisms for temporal and feature importance weighting
- Training Protocol: Train model using leave-one-subject-out cross-validation with early stopping
- Performance Validation: Evaluate using Root Mean Squared Error (RMSE), correlation coefficient, and Mean Absolute Percentage Error (MAPE)
Expected Outcomes: A study implementing this protocol achieved RMSE of 19.49 ± 5.42 mg/dL and correlation coefficient of 0.43 ± 0.2 for current glucose level predictions without prior glucose measurements [2].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools for CGM Data Preprocessing
| Tool Category | Specific Solutions | Primary Function | Implementation Considerations |
|---|---|---|---|
| Data Acquisition | Dexcom G7, Abbott Freestyle Libre 3, Medtronic Guardian 4 | Raw CGM data collection | MARD <10% for clinical-grade accuracy; API access for data export |
| Preprocessing Libraries | R fda, Python scikit-fda, tslearn |
Functional data analysis & time series processing | Handling of irregular sampling & missing data patterns |
| Deep Learning Frameworks | PyTorch, TensorFlow with BiLSTM layers | Virtual CGM development | Encoder-decoder architecture with attention mechanisms |
| Foundation Models | Transformer-based CGM-LSM | Large-scale glucose prediction | Pre-training on 1.6M+ CGM records for zero-shot generalization |
| Statistical Analysis | XGBoost with chronobiological features | Predictive modeling of glycemic dysregulation | Integration of time-of-day complexity metrics |
These computational reagents form the foundation for rigorous CGM data analysis, with studies demonstrating their efficacy in both clinical and research settings [2] [5] [3]. The selection of specific tools should align with research objectives, with FDA approaches particularly suited for temporal pattern discovery and deep learning methods optimized for prediction tasks.
The analysis of Continuous Glucose Monitoring (CGM) data relies on standardized metrics that quantify different aspects of glycemic control. These metrics are broadly categorized into Time in Ranges, Glycemic Variability, and composite Risk Indices, each providing unique insights into glucose dynamics [6] [7]. The following table summarizes the defining formulae, clinical targets, and primary interpretations of these core metrics.
Table 1: Quantitative Summary of Core CGM Metrics for Research Applications
| Metric Category | Specific Metric | Formula/Calculation | Target Value | Clinical/Research Interpretation |
|---|---|---|---|---|
| Time in Ranges | Time in Range (TIR) | % of readings within 70–180 mg/dL [6] | >70% [6] [7] | Surrogate for overall glycemic control; associated with reduced microvascular complication risk [8] [9]. |
| Time Below Range (TBR) | % of readings <70 mg/dL (Level 1) and <54 mg/dL (Level 2) [6] | <4% (Level 1), <1% (Level 2) [6] [7] | Quantifies hypoglycemic exposure; critical for safety assessment. | |
| Time Above Range (TAR) | % of readings >180 mg/dL (Level 1) and >250 mg/dL (Level 2) [6] | <25% (Level 1), <5% (Level 2) [6] [7] | Quantifies hyperglycemic exposure. | |
| Glycemic Variability | Coefficient of Variation (CV) | (Standard Deviation / Mean Glucose) × 100% [6] | <36% [9] | Measure of glucose stability; high CV indicates increased hypoglycemia risk. |
| Mean Glucose | Average of all CGM readings | Varies | Gross measure of overall glycemia. | |
| Glucose Management Indicator (GMI) | Estimated HbA1c derived from mean glucose: GMI (%) = 3.31 + 0.02392 × [mean glucose in mg/dL] [6] | Individualized | Provides an HbA1c-equivalent value from CGM data. | |
| Risk Indices | Glycemia Risk Index (GRI) | Composite score: (3.0 × %<54) + (2.4 × %54-69) + (1.6 × %>250) + (0.8 × %181-250) [10] | Lower is better (0-100 scale) | Unifies hypo- and hyperglycemia exposure into a single score; correlates highly with clinician risk assessment (r=0.95) [11] [10]. |
| Hypoglycemia Component (CHypo) | %<54 + (0.8 × %54-69) [10] | - | Hypoglycemia contribution to GRI. | |
| Hyperglycemia Component (CHyper) | %>250 + (0.5 × %181-250) [10] | - | Hyperglycemia contribution to GRI. |
Experimental Protocols for CGM Feature Validation
Protocol: Validating CGM Metrics Against Clinical Outcomes
This protocol outlines the methodology for conducting longitudinal studies to establish the relationship between CGM-derived metrics and hard clinical endpoints, such as the development or progression of microvascular complications.
1. Study Design and Population
- Design: Prospective cohort study or post-hoc analysis of randomized controlled trials [8].
- Participants: Recruit individuals with diabetes (Type 1 or Type 2). Sample size must be sufficient for multivariate regression analysis.
- Inclusion Criteria: Confirmed diagnosis of diabetes, willingness to wear CGM periodically.
- Exclusion Criteria: Conditions that severely alter HbA1c reliability (e.g., anemia, hemoglobinopathies, end-stage renal disease) [6].
2. CGM Data Acquisition and Processing
- Device Use: Participants should wear a validated CGM system (e.g., Dexcom G6/G7, Abbott FreeStyle Libre) [2].
- Duration & Frequency: Collect CGM data for a minimum of 14 days to ensure metric stability, with at least 70% of data available [6] [7]. Repeat CGM assessments at predefined intervals (e.g., annually).
- Data Processing: Use standardized software (e.g., GlucoStats Python library) to compute core metrics: TIR, TBR, TAR, CV, Mean Glucose, and GMI from the raw CGM data [12].
3. Outcome Measurement
- Primary Outcomes: Progression of microvascular complications, assessed annually.
- Covariates: Document and adjust for age, diabetes duration, HbA1c, blood pressure, lipid levels, and body mass index (BMI) [9].
4. Statistical Analysis
- Modeling: Use multivariable Cox proportional hazards regression to calculate hazard ratios (HRs) for complication progression per standard deviation (SD) change or categorical change (e.g., 10% change in TIR) in each CGM metric, adjusting for covariates and mean HbA1c [8] [9].
- Correlation: Assess the correlation between CGM metrics and HbA1c using Pearson's correlation coefficient.
Protocol: Computational Feature Extraction for Machine Learning
This protocol details the process for extracting a comprehensive set of features from CGM time-series data to train machine learning models for tasks such as hypoglycemia prediction or phenotype classification [13] [12].
1. Data Preprocessing
- Input Data: Raw CGM timestamp-value pairs, ideally with a 5–15 minute measurement interval.
- Data Cleaning: Handle signal dropouts and artifacts. Apply a suitable filter (e.g., median filter) to smooth noisy data without altering physiological trends.
- Data Requirements: For a stable estimate of TIR, use a minimum of 14 days of data with >70% data capture [6] [7]. For hypoglycemia prediction, longer datasets may be required [13].
2. Feature Engineering and Extraction Leverage a library like GlucoStats to extract a wide array of features, which can be categorized as follows [13] [12]:
- Time-in-Range Features: Calculate the percentage and number of observations in user-defined glucose ranges (e.g., <54, 54-69, 70-180, 181-250, >250 mg/dL).
- Descriptive Statistics: Compute mean, median, standard deviation, and quantiles (Q1, Q3) of the entire glucose trace.
- Glycemic Risk Features: Calculate GRI, LBGI (Low Blood Glucose Index), and HBGI (High Blood Glucose Index).
- Temporal Dynamics Features:
- Short-term (<1 hour): Rate of change (mg/dL/min), differences between consecutive measurements (e.g., diff10min, diff30min) [13].
- Medium-term (1-4 hours): Standard deviation and slope over 2-hour and 4-hour rolling windows [13].
- Long-term (>4 hours) & Behavioral: "Snowball effect" features (cumulative positive/negative changes), count of "rebound" events (rapid swings from high-to-low or low-to-high) [13].
3. Model Training and Validation
- Dataset Splitting: Partition data into training, validation, and test sets, ensuring data from the same individual is contained within a single set.
- Model Selection: Train classifiers (e.g., Random Forest, XGBoost) or neural networks using the extracted features.
- Performance Evaluation: For a hypoglycemia prediction task (e.g., predicting onset within 30-60 minutes), evaluate model performance using sensitivity, specificity, and root mean squared error (RMSE) [13].
Table 2: Key Computational Tools and Analytical Resources for CGM Research
| Tool/Resource | Type | Primary Function in Research | Key Features |
|---|---|---|---|
| GlucoStats [12] | Python Library | Efficient feature extraction from raw CGM time-series data. | Extracts 59+ metrics; supports parallel processing & windowing; scikit-learn compatible. |
| CGM-GUIDE / GlyCulator [12] | Web/Desktop Application | Calculation of traditional glycemic variability indices. | User-friendly interface for established metrics (MAGE, CONGA). |
| GRI Calculator (DTS) [10] | Web Tool / Mobile App | Standardized calculation of the Glycemia Risk Index. | Implements the weighted GRI formula; provides GRI grid visualization. |
| AGP Report [7] | Standardized Visualization | Unified graphical summary of CGM data for pattern analysis. | Single-page report with glucose distribution, median curve, and daily profiles. |
| LSTM/Deep Learning Models [2] | AI Architecture | Glucose prediction and virtual CGM development. | Models complex temporal relationships from life-log data (meals, activity). |
| Functional Data Analysis (FDA) [1] | Statistical Framework | Advanced pattern recognition in CGM trajectories. | Treats CGM data as continuous curves; identifies subtle phenotypic patterns. |
Short-term, Medium-term, and Long-term Temporal Features
The analysis of Continuous Glucose Monitoring (CGM) data leverages temporal features across multiple timescales to enable glucose forecasting and glycemic dysregulation prediction. The table below summarizes the primary categories of temporal features used in CGM research.
Table 1: Categories of Temporal Features in CGM Data Analysis
| Temporal Category | Time Horizon | Key Feature Examples | Primary Research Applications |
|---|---|---|---|
| Short-Term | Minutes to 1 hour | • Glucose values at 5-min intervals (lags t-1 to t-12) [14]• Instantaneous Rate of Change (ROC) [14] | 30-minute ahead glucose forecasting [14] [15] |
| Medium-Term | 1 to 24 hours | • Rolling averages (e.g., 15-minute) [14]• Time-of-Day (ToD) aligned standard deviation [3] | Hypoglycemia prediction [15]; Pattern analysis across a single day [3] |
| Long-Term | Multiple days to weeks | • Chronobiologically-informed features (multi-timescale complexity) [3]• Functional data patterns [1] | Prediction of longer-term glycemic dysregulation [3]; Identification of metabolic phenotypes [1] |
Experimental Protocols
Protocol for 30-Minute Ahead Forecasting with Ridge Regression
This protocol details a method for short-term glucose forecasting using Ridge Regression, adapted from a study comparing it with ARIMA models [14].
- Data Source & Preprocessing: Utilize a public dataset such as OhioT1DM with 5-minute resolution CGM data [14].
- Resample data to strict 5-minute intervals.
- Handle missing values via linear interpolation for gaps ≤30 minutes.
- Perform chronological splitting into training, validation, and test sets to prevent data leakage.
- Feature Engineering (Short-Term):
- Lag Features: Construct lagged glucose values covering the preceding 5 to 60 minutes (i.e., 1 to 12 lags of 5 minutes each) [14].
- Rate-of-Change: Calculate the glucose rate of change over the past 15 minutes [14].
- Standardization: Standardize all features to zero mean and unit variance based on statistics computed exclusively from the training window [14].
- Model Implementation:
- Implement a Ridge Regression model, which incorporates an L2 penalty on coefficients to mitigate overfitting [14].
- The model form is:
Forecast = β₀ + Σ βₖ * Glucose_(t-k) + β_roc * ROC_(t). - Tune the L2 penalty parameter (λ) via grid search on the validation set to minimize 30-minute ahead Root Mean Squared Error (RMSE) [14].
- Evaluation & Validation:
- Use a rolling-origin evaluation scheme to simulate real-world deployment [14].
- Refit the model at each origin using an expanding window of data.
- Primary Metric: Root Mean Squared Error (RMSE).
- Secondary Metrics: Mean Absolute Error (MAE) and Clarke Error Grid (CEG) analysis for clinical accuracy [14].
Protocol for Hypoglycemia Prediction with LSTM
This protocol outlines the development and validation of a Long Short-Term Memory (LSTM) model for predicting hypoglycemia events 30 minutes in advance [15].
- Data Source & Preparation:
- Primary Dataset: CGM data from 192 Chinese patients with diabetes (Type 1 and Type 2), collected with Medtronic MiniMed devices [15].
- Validation Dataset: 427 patients of European-American ancestry from the United States to test model generalizability [15].
- Data Cleaning: Divide CGM data into segments at points of missing data. Discard segments shorter than 6 hours (72 data points) [15].
- Outcome Definition: Classify glucose values into: Non-hypoglycemic (>70 mg/dL), Mild Hypoglycemia (54-70 mg/dL), and Severe Hypoglycemia (<54 mg/dL) [15].
- Model Training & Hyperparameter Tuning:
- Model Validation and Generalization Test:
- Performance Metrics:
- Evaluate performance using Sensitivity, Specificity, and the Area Under the Receiver Operating Characteristic Curve (AUC) [15].
Protocol for Virtual CGM Using Life-Log Data
This protocol describes a framework for a "virtual CGM" that infers current and future glucose levels using life-log data, without relying on prior glucose measurements at the inference step [2].
- Data Acquisition:
- Collect retrospective data from 171 healthy adults, including CGM readings (e.g., Dexcom G7), dietary intake (calories, carbs, macronutrients), physical activity (METs, step counts), and timestamps [2].
- Data Structuring:
- Extract subsequences from the entire data trajectory using a sliding-window technique [2].
- Model Architecture:
- Model Training and Application:
- Evaluation Metrics:
- Assess model performance using Root Mean Squared Error (RMSE), Correlation Coefficient, and Mean Absolute Percentage Error (MAPE) [2].
Research Reagent Solutions
The table below lists key datasets and computational tools essential for research in CGM feature engineering and glucose prediction.
Table 2: Essential Research Materials and Tools
| Item Name | Type | Function & Application in Research |
|---|---|---|
| OhioT1DM Dataset [14] | Dataset | A public dataset containing CGM time series from multiple subjects at 5-minute resolution; used for benchmarking short-term forecasting models like ARIMA and Ridge Regression. |
| Dexcom CGM Data [3] | Dataset | Real-world CGM data sourced from a large, heterogeneous population (e.g., 8,000 individuals); enables research into long-term glycemic patterns and model generalizability. |
| Long Short-Term Memory (LSTM) Network [15] [2] | Algorithm | A type of Recurrent Neural Network (RNN) adept at capturing long-term dependencies in sequential data; applied for hypoglycemia prediction and virtual CGM development. |
| XGBoost [3] | Algorithm | An efficient, scalable implementation of gradient boosted trees; used with chronobiologically-informed features to predict longer-term glycemic dysregulation. |
| Ridge Regression [14] | Algorithm | A regularized linear regression model with L2 penalty; provides a lightweight, interpretable, yet powerful baseline for 30-minute ahead CGM forecasting. |
Workflow and Conceptual Diagrams
Figure 1: CGM Feature Engineering and Modeling Workflow
Figure 2: Virtual CGM LSTM Model Architecture
In the field of continuous glucose monitoring (CGM) data analysis, advanced feature engineering has become pivotal for developing predictive machine learning models that can accurately forecast adverse glycemic events. Two particularly innovative feature concepts—snowball effects and rebound events—have demonstrated significant potential in enhancing the predictive performance of hypoglycemia and hyperglycemia risk assessment algorithms. These features move beyond simple glucose value tracking to capture complex physiological patterns and cumulative effects that often precede critical glycemic events. This document provides detailed application notes and experimental protocols for implementing these novel feature concepts within CGM time series research, specifically tailored for researchers, scientists, and drug development professionals working at the intersection of diabetes technology and predictive analytics.
Theoretical Foundation and Definitions
Snowball Effect Features
The "snowball effect" metaphor describes the cumulative nature of glucose changes over time, where successive increments or decrements in glucose values create momentum that increases the probability of significant glycemic events [13]. This concept captures the accruing effects of persistent glucose trends that might be insignificant when viewed in isolation but become clinically meaningful when aggregated.
Snowball effect features are quantitatively defined through four primary metrics calculated over a two-hour window:
- Cumulative Positive Changes (
pos): The sum of all increases between consecutive CGM measurements - Cumulative Negative Changes (
neg): The sum of all decreases between consecutive CGM measurements - Maximum Single Increase (
max_pos): The largest positive change between any two consecutive measurements - Maximum Single Decrease (
max_neg): The largest negative change between any two consecutive measurements [13]
These features effectively capture the "momentum" of glucose changes, providing early warning signals for impending hypoglycemia or hyperglycemia that might not be detectable through conventional rate-of-change calculations.
Rebound Event Features
Rebound events represent extreme glycemic excursions characterized by rapid transitions between hypoglycemic and hyperglycemic states or vice versa [13] [16]. These patterns are clinically significant as they indicate poor glycemic control and potentially dangerous management practices, such as excessive carbohydrate consumption to treat hypoglycemia followed by compensatory insulin overcorrection.
The formal definitions for rebound event features include:
- Rebound Low: Glucose transitions from >200 mg/dL to <70 mg/dL within 60 minutes
- Rebound High: Glucose transitions from <70 mg/dL to >200 mg/dL within 60 minutes
- Near Rebound Low: Glucose transitions from >180 mg/dL to <90 mg/dL within 60 minutes
- Near Rebound High: Glucose transitions from <90 mg/dL to >180 mg/dL within 60 minutes [13]
From a clinical perspective, rebound hyperglycemia (RH) has been specifically defined as "any series of one or more sensor glucose values >180 mg/dL preceded by any series of one or more SGVs <70 mg/dL, with the condition that the first SGV in the hyperglycemic series occurred within two hours of the last value in the hypoglycemic series" [16].
Quantitative Impact Assessment
Clinical Significance of Rebound Events
Table 1: Clinical Impact of Real-Time CGM Interventions on Rebound Hyperglycemia Events
| Intervention | Study Population | RH Frequency Reduction | RH Duration Reduction | RH Severity (AUC) Reduction |
|---|---|---|---|---|
| rtCGM Adoption | HypoDE Trial (N=75) | 14% (overall)28% (<55 mg/dL) | 12% (overall)3% (<55 mg/dL) | 23% (overall)19% (<55 mg/dL) |
| Predictive Alerts | Real-World Users (N=24,518) | 7% (overall)12% (<55 mg/dL) | 8% (overall)11% (<55 mg/dL) | 13% (overall)18% (<55 mg/dL) |
The data presented in Table 1 demonstrates that interventions incorporating rebound event tracking can significantly mitigate the frequency, duration, and severity of rebound hyperglycemia [16]. The reduction is particularly pronounced for events following severe hypoglycemia (SGVs <55 mg/dL), highlighting the clinical value of these features in identifying high-risk patterns.
Performance Metrics for Predictive Models
Table 2: Performance Comparison of Machine Learning Models Utilizing Novel Feature Concepts
| Model Type | Feature Categories | Prediction Horizon | Sensitivity | Specificity | Target Population |
|---|---|---|---|---|---|
| Feature-Based ML | Snowball Effects + Rebound Events | 30-minute | >91% | >90% | Pediatric T1D (N=112) |
| Feature-Based ML | Snowball Effects + Rebound Events | 60-minute | >91% | >90% | Pediatric T1D (N=112) |
| LSTM Network | Temporal Sequences + Future CHO | 120-minute | High (AUC≈1) | High (AUC≈1) | Synthetic T1D Subjects |
The integration of snowball effect and rebound event features has enabled machine learning models to achieve high sensitivity and specificity in predicting hypoglycemic events across multiple time horizons, as evidenced by the performance metrics in Table 2 [13] [17]. The LSTM model architecture, which incorporated future carbohydrate intake data alongside historical glucose patterns, demonstrated particularly strong performance with Area Under the Curve (AUC) values approaching 1 for all glycemic state classifications [17].
Experimental Protocols
Data Collection and Preprocessing
Protocol 1: CGM Data Acquisition and Quality Control
- Step 1: Collect CGM data from commercially available devices (e.g., Dexcom G6) with sampling intervals of 5 minutes or less
- Step 2: Apply quality control filters to remove physiologically implausible values (e.g., <40 mg/dL or >400 mg/dL sustained for <15 minutes)
- Step 3: Align temporal sequences to account for sensor drift and calibration events
- Step 4: Annotate datasets with demographic information (age, gender, diabetes duration, HbA1c) and contextual factors (time of day, day of week) [13]
Protocol 2: Insulin and Carbohydrate Data Integration
- Step 1: Collect insulin administration data from pump records or manual logs, noting timing and dosage
- Step 2: Record carbohydrate intake through mobile applications or meal diaries
- Step 3: Calculate insulin-on-board and carbohydrate-on-board using established pharmacokinetic models
- Step 4: Synchronize CGM, insulin, and carbohydrate data to a common timeline with appropriate latency adjustments for absorption curves [13]
Feature Extraction Methodology
Protocol 3: Snowball Effect Feature Calculation
- Step 1: For each time point t, extract a two-hour window of preceding CGM values [t-23, t]
- Step 2: Calculate consecutive differences between measurements: diffi = CGMi - CGM_{i-1}
- Step 3: Compute cumulative positive changes: pos = Σ max(0, diff_i)
- Step 4: Compute cumulative negative changes: neg = Σ min(0, diff_i)
- Step 5: Identify maximum positive change: maxpos = max(diffi)
- Step 6: Identify maximum negative change: maxneg = min(diffi) [13]
Protocol 4: Rebound Event Feature Extraction
- Step 1: Scan complete patient history for transitions between glycemic thresholds
- Step 2: Identify rebound lows: instances where CGM >200 mg/dL followed by CGM <70 mg/dL within 60 minutes
- Step 3: Identify rebound highs: instances where CGM <70 mg/dL followed by CGM >200 mg/dL within 60 minutes
- Step 4: Calculate near-rebound events using modified thresholds (90 mg/dL and 180 mg/dL)
- Step 5: Aggregate counts of these events per patient as long-term features [13]
Model Training and Validation
Protocol 5: Machine Learning Implementation with Novel Features
- Step 1: Partition data into training (70%), validation (15%), and test (15%) sets maintaining temporal order
- Step 2: Normalize all features using MinMax scaling to [0,1] range
- Step 3: Train ensemble classifiers (Random Forest, XGBoost) or LSTM networks using combined feature sets
- Step 4: Optimize hyperparameters through cross-validation on training data
- Step 5: Evaluate performance on held-out test set using sensitivity, specificity, and AUC metrics [13] [17]
Visualization Framework
Snowball Effect Feature Extraction Workflow
Rebound Event Detection Logic
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Computational Tools for Feature Implementation
| Category | Item | Specification/Function | Implementation Example |
|---|---|---|---|
| Data Acquisition | Dexcom G6 CGM | Real-time glucose measurements every 5 minutes | Primary data source for feature extraction [13] |
| Computational Framework | Python 3.8+ | Primary programming language for time series analysis | pandas for data manipulation, scikit-learn for ML [13] |
| Machine Learning Libraries | XGBoost | Gradient boosting for feature importance ranking | Identify most predictive snowball and rebound features [13] |
| Deep Learning Framework | TensorFlow/Keras | LSTM network implementation | Temporal pattern recognition in CGM sequences [17] |
| Statistical Analysis | Bayesian Ridge Regression | Regularized linear regression for glucose prediction | Handle multicollinearity in snowball features [18] |
| Data Visualization | Matplotlib/Plotly | Creation of glucose trend plots and feature diagrams | Visualize snowball accumulation patterns [13] |
The systematic implementation of snowball effect and rebound event features represents a significant advancement in CGM time series analysis for diabetes management. These novel feature concepts enable researchers to capture complex physiological patterns that conventional metrics often miss, leading to substantial improvements in predictive accuracy for adverse glycemic events. The experimental protocols and application notes provided herein offer a comprehensive framework for integrating these features into machine learning pipelines, with demonstrated efficacy in both research and clinical settings. As CGM technology continues to evolve, further refinement of these feature engineering approaches will play a crucial role in developing more sophisticated and personalized glycemic management systems.
The proliferation of continuous glucose monitoring (CGM) systems has revolutionized diabetes management and research, generating high-frequency temporal data that captures the dynamic nature of glucose metabolism [12]. This data explosion presents both unprecedented opportunities and significant computational challenges for researchers and clinicians seeking to extract meaningful patterns from complex glucose time series. Feature engineering—the process of transforming raw CGM data into informative, non-redundant features that characterize glycemic dynamics—serves as a critical foundation for downstream analysis, predictive modeling, and clinical decision support [12] [19].
Within this context, specialized open-source software libraries have emerged to streamline and standardize the analytical workflow. This application note focuses on GlucoStats, a Python library specifically designed for efficient computation and visualization of comprehensive glucose metrics derived from CGM data [12] [20]. We position GlucoStats within the broader ecosystem of CGM analysis tools, detailing its application for research and drug development professionals working with glycemic time series data. The library addresses several limitations of existing tools, including lack of parallelization, limited feature sets, and insufficient visualization capabilities [12] [21].
GlucoStats: Core Architecture and Capabilities
GlucoStats employs a modular architecture that separates concerns across specialized components, ensuring maintainability and extensibility [12] [22]. This architecture is organized into four primary modules that collaborate to provide a comprehensive analytical toolkit:
- Stats Module: The computational core responsible for calculating 59 distinct glucose statistics across multiple categories including time in ranges, glycemic risks, and variability indices [12].
- Utils Module: Provides data handling utilities, input validation, and transformation functions that ensure data integrity throughout the analytical pipeline [12].
- Visualization Module: Generates high-quality graphical representations of glucose patterns using Matplotlib and Seaborn, facilitating both intra-patient and inter-patient comparisons [12] [22].
- ExtractGlucoStats Module: Orchestrates the overall analytical workflow, providing a unified interface that coordinates feature extraction, transformation, and visualization [12].
The library implements several innovative functionalities that distinguish it from existing solutions. Its parallel processing capability distributes computational tasks across multiple processors, significantly reducing processing time for large-scale datasets [12]. The windowing functionality enables temporal segmentation of CGM data into overlapping or non-overlapping intervals, allowing researchers to capture dynamic glycemic patterns at multiple time scales [12]. Furthermore, GlucoStats adheres to the scikit-learn standardized interface, enabling seamless integration into machine learning pipelines for end-to-end predictive analytics [12].
Table 1: Metric Categories Extracted by GlucoStats
| Category | Subcategories | Key Metrics | Clinical/Research Utility |
|---|---|---|---|
| Time in Ranges (TIRs) | Hypoglycemia, Euglycemia, Hyperglycemia | Percentage of time in customizable glucose ranges | Assessment of glycemic control quality; Evaluation of treatment efficacy |
| Glucose Risks (GRs) | Hypoglycemia Risk, Hyperglycemia Risk | Hypo-index, Hyper-index, Low/High Blood Glucose Index (LBGI/HBGI) | Quantification of extreme glucose event risks; Prevention strategy optimization |
| Glycemic Control (GC) | Variability, Stability | Mean Glucose, Standard Deviation, Coefficient of Variation | Determination of treatment effectiveness; Glucose stability evaluation |
| Descriptive Statistics (DSs) | Central Tendency, Dispersion | Mean, Median, Minimum, Maximum, Quantiles | Overall understanding of glucose levels during specific periods |
| Number of Observations (NOs) | Range-based Counting | Frequency of values in specific glucose ranges | Identification of prevalence in certain ranges; Pattern recognition |
Experimental Protocols for CGM Feature Extraction
Data Preprocessing and Configuration
A standardized protocol for CGM data preprocessing ensures reproducible feature extraction. The following workflow outlines the essential steps for preparing CGM data for analysis with GlucoStats:
- Data Import and Validation: Load CGM data with timestamps and glucose values into a Pandas DataFrame. GlucoStats validates input format and checks for required columns [22].
- Resampling and Gap Handling: Resample data to consistent intervals (typically 5-15 minutes). For gaps ≤30 minutes, apply linear interpolation; longer gaps may require exclusion or advanced imputation [14].
- Range Configuration: Define clinical thresholds for hypoglycemia (<70 mg/dL), euglycemia (70-180 mg/dL), and hyperglycemia (>180 mg/dL), customizable to specific research populations [12] [22].
- Windowing Specification: Select appropriate windowing parameters based on analytical objectives. Non-overlapping windows provide broader trends, while overlapping windows capture fine-grained changes [12].
Feature Extraction with Temporal Windowing
The windowing functionality of GlucoStats enables sophisticated temporal analysis of glycemic dynamics. Implement the following protocol for window-based feature extraction:
Window Parameter Selection:
Parallel Processing Configuration:
Feature Selection: Specify which of the 59 available metrics to compute based on research objectives. For comprehensive analysis, include representatives from all categories listed in Table 1 [12].
Execution and Output:
Advanced Applications in Diabetes Research
Integration with Predictive Modeling
GlucoStats extends beyond descriptive analytics to enable predictive modeling for glucose forecasting. The library's scikit-learn compatibility allows seamless integration with machine learning workflows [12]. Research demonstrates that regularized regression models (e.g., ridge regression) with engineered lag features (5-60 minutes) can outperform traditional time series approaches like ARIMA for 30-minute glucose prediction [14]. The protocol for developing such predictive systems involves:
- Feature Engineering: Create lagged glucose values (1-12 lags at 5-minute intervals) and rate-of-change features from GlucoStats outputs [14].
- Model Specification: Implement ridge regression with L2 penalty to prevent overfitting in high-dimensional feature spaces [14].
- Temporal Validation: Employ rolling-origin evaluation with chronological splitting to preserve temporal integrity and prevent data leakage [14].
Table 2: Research Reagent Solutions for CGM Analytics
| Tool/Category | Specific Examples | Function in CGM Research |
|---|---|---|
| Programming Environments | Python 3.10+, R, MATLAB | Primary computational environments for CGM data analysis |
| Data Manipulation Libraries | Pandas (v2.2.3), NumPy (v2.2.3) | Efficient handling and transformation of temporal CGM data |
| Machine Learning Frameworks | scikit-learn, TensorFlow, PyTorch | Development of predictive models for glucose forecasting |
| Visualization Tools | Matplotlib (v3.8.0), Seaborn (v0.13.2) | Generation of publication-quality glucose trend visualizations |
| Specialized CGM Packages | GlucoStats, cgmanalysis, iglu | Domain-specific feature extraction and analytical capabilities |
| Public Datasets | OhioT1DM Dataset | Benchmark data for method validation and comparative studies |
Comparison with Alternative CGM Analysis Tools
GlucoStats occupies a unique position within the ecosystem of CGM analysis software. The library addresses several limitations identified in existing tools, including lack of parallel processing, limited visualization capabilities, and insufficient feature sets [12] [21]. When compared to other available packages:
- R-based solutions (cgmanalysis, iglu) offer comprehensive statistical capabilities but lack native Python integration and parallel processing [12] [21].
- Web-based applications (GlyCulator, CGM-GUIDE) provide user-friendly interfaces but limited customization and batch processing capabilities [12] [21].
- MATLAB implementations (GVAP) require commercial licensing and lack compatibility with modern data science workflows [12].
- Other Python packages (Cgmquantify) extract only 25 features compared to GlucoStats' 59 metrics and lack advanced visualization tools [12].
The multi-processing architecture of GlucoStats demonstrates significantly higher efficiency for large-scale datasets, processing substantial CGM collections in minimal time through parallel computation [12].
Visualization and Interpretation Framework
GlucoStats incorporates comprehensive visualization capabilities that facilitate both exploratory data analysis and result communication. The library generates standardized plots for:
- Ambulatory Glucose Profile: Displaying interquartile ranges and median glucose patterns across days [12].
- Time-in-Ranges Charts: Illustrating percentage distributions across hypoglycemic, euglycemic, and hyperglycemic ranges [12].
- Temporal Trend Analysis: Visualizing glucose patterns across user-defined windows to identify oscillations and temporal dynamics [12].
These visualization tools enable researchers to identify patterns, trends, and anomalies in CGM data, enhancing interpretability for both technical and non-technical audiences [12]. The generated graphics are publication-ready, supporting effective dissemination of research findings.
GlucoStats represents a significant advancement in open-source tools for CGM data analysis, addressing critical needs in feature engineering for glucose time series research. Its comprehensive metric extraction, parallel processing capabilities, and advanced visualization tools provide researchers and drug development professionals with an efficient platform for analyzing complex glycemic patterns. The library's modular design and scikit-learn compatibility facilitate seamless integration into existing research workflows, enabling robust predictive modeling and clinical applications.
As CGM technology continues to evolve and generate increasingly large datasets, tools like GlucoStats will play an essential role in translating raw sensor data into clinically actionable insights. Future developments will likely expand its feature set, enhance integration with electronic health records, and incorporate more specialized visualization for specific research applications. For researchers working with glycemic time series data, GlucoStats offers a powerful, flexible foundation for advancing diabetes research and therapeutic development.
From Theory to Practice: Techniques for Extracting Predictive Features
In the field of continuous glucose monitoring (CGM) research, accurate time series forecasting is paramount for developing proactive diabetes management systems, including predictive alerts for hypoglycemia and hyperglycemia, and the optimization of insulin delivery in automated systems. CGM data, typically collected at 5 to 15-minute intervals, generates a complex, high-frequency time series that captures the dynamic interplay between glucose levels, insulin, nutrition, and physical activity. The performance of forecasting models—from traditional statistical methods to advanced deep learning architectures—is heavily dependent on the quality and informativeness of the input features. Consequently, feature engineering has emerged as a critical preprocessing step, enabling models to better capture the temporal dependencies and physiological patterns inherent in glycemic dynamics.
Temporal feature engineering specifically involves transforming the raw timestamped glucose readings into predictive variables that encapsulate relevant past information. Among the most powerful techniques for this are lag features, rolling window features, and expanding window features. These techniques allow researchers to encode short-term effects, cyclical patterns (such as those related to meals and sleep), and long-term physiological trends directly into the model's input space. For instance, a hybrid stochastic–machine learning framework for glucose prediction has demonstrated that integrating physiologically-inspired features with data-driven models enhances both precision and applicability [23]. This document provides detailed application notes and protocols for implementing these core temporal feature engineering techniques within CGM research pipelines.
Theoretical Foundations and Clinical Relevance
The Role of Temporal Features in Glucose Forecasting
Glucose-insulin regulation is a continuous process with inherent delays; the effect of a meal or insulin bolus on glucose levels is not instantaneous but unfolds over time. Temporal features are engineered to quantitatively represent these delayed effects and underlying patterns. Lag features directly model the autoregressive nature of glucose levels, where recent past values are strong predictors of the immediate future. This is analogous to the physiological reality that the current glucose level is a function of its very recent state [14]. Rolling window features (e.g., the mean or standard deviation of glucose over the preceding 30 minutes) summarize short-term trends and the volatility of glucose levels, which can be indicative of rapid onset hypoglycemia or postprandial excursions. Expanding window features capture the long-term evolution of a patient's glycemic state, such as a gradually shifting baseline, which can be crucial for personalizing model parameters and adapting to inter-individual variability [24].
The clinical utility of these features is profound. Accurate short-term forecasts (e.g., 30-60 minutes ahead) can provide patients with early warnings, allowing for preventive actions. Studies have shown that models leveraging these features can surpass traditional approaches; for example, ridge regression with engineered lag and rate-of-change features has been shown to outperform univariate ARIMA models for 30-minute ahead CGM forecasting [14]. Furthermore, the integration of these features into deep learning frameworks, such as LSTM-based virtual CGM systems, enables glucose level inference even during periods of missing CGM data by relying on life-log data (meals, exercise) [2].
Key Temporal Feature Classes
Table 1: Summary of Core Temporal Feature Engineering Techniques
| Feature Class | Physiological Interpretation | Common Aggregations | Typical Use Case in CGM |
|---|---|---|---|
| Lag Features | The direct, short-term memory of the glucose regulatory system. Represents the influence of recent glucose concentrations on the current state. | Previous values (t-1, t-2, ...). | 30-minute prediction of postprandial glucose response [14]. |
| Rolling Window | Short-term glycemic trends and stability. Volatility may indicate sensitivity to insulin or meals. | Mean, Standard Deviation, Min, Max, Slope. | Detecting the onset of hypoglycemia by tracking the rate of change over a 15-30 minute window. |
| Expanding Window | Long-term shifts in glycemic baselines and overall control (e.g., changing HbA1c proxy). | Cumulative Mean, Cumulative Max, Cumulative Standard Deviation. | Personalizing a model to a patient's unique glucose profile over several weeks or months [24]. |
Application Notes: Protocols for Feature Engineering
The following protocols outline the step-by-step process for creating temporal features from raw CGM data, using Python and common data science libraries.
Protocol 1: Implementing Lag Features
Objective: To create features that represent the glucose level at specific previous time points.
Materials:
- Raw CGM time series data (
glucose_values) with a consistent sampling interval (e.g., 5-min). - Computing environment with Python (>=3.7) and libraries: Pandas (>=1.0), NumPy.
Methodology:
- Data Preprocessing: Ensure the CGM data is loaded into a Pandas DataFrame with a
datetimeindex. Handle missing values using linear interpolation for short gaps (e.g., ≤30 minutes) [14]. - Lag Selection: Determine the relevant lags. For a 30-minute prediction horizon, lags from the past 5 to 60 minutes (e.g., 1, 2, 3, 4, 6, 12 for 5-min data) are physiologically relevant. Autocorrelation Function (ACF) plots can inform this choice [25].
- Feature Creation: Use the
shift()method in Pandas to create the lagged features.
Validation: The resulting DataFrame will contain new columns (e.g., glucose_lag_1, glucose_lag_2). The first few rows will contain NaN values which must be dropped or imputed before model training.
Protocol 2: Implementing Rolling Window Features
Objective: To create features that summarize the recent statistical properties of the glucose signal.
Materials:
- The preprocessed CGM DataFrame from Protocol 1.
Methodology:
- Window Definition: Select a window size that aligns with the clinical question. A 15-30 minute window (3-6 readings for 5-min data) is suitable for capturing immediate trends.
- Aggregation Selection: Choose aggregations like
mean(recent trend),std(recent volatility), andmin/max(recent extremes). - Feature Creation: Use the
rolling()method followed by an aggregation function and ashift(1)to avoid data leakage.
Validation: Inspect the features to ensure that for each time point, the rolling statistic is calculated using only the previous window_size observations. The first window_size rows will be NaN.
Protocol 3: Implementing Expanding Window Features
Objective: To create features that capture the cumulative history of the glucose time series from the start of the recording period.
Materials:
- The preprocessed CGM DataFrame from Protocol 1.
Methodology:
- Operation Selection: Define the aggregations, such as
mean,max, andstd. - Feature Creation: Use the
expanding()method to calculate the statistic from the start of the series up to each point, followed byshift(1).
Validation: The expanding_mean for a given row should be the average of all glucose values from the beginning of the dataset up to the previous time step. The drop_na=True parameter will remove initial rows with NaN values [24].
Experimental Workflow Visualization
The following diagram illustrates the integrated workflow for generating temporal features and utilizing them in a predictive model for CGM data.
The Scientist's Toolkit: Research Reagents & Computational Solutions
This section details the essential computational tools and data components required to implement the described feature engineering protocols.
Table 2: Essential Research Reagents and Computational Tools
| Item Name | Specifications / Version | Function in Protocol | Procurement / Access |
|---|---|---|---|
| Python Programming Language | Version 3.8+ | Core programming environment for data manipulation and model building. | https://www.python.org/ |
| Pandas Library | Version 1.4.0+ | Provides data structures (DataFrame) and methods (shift, rolling, expanding) for feature engineering. |
Included in standard Python distributions (e.g., Anaconda). |
| Feature-engine Library | Version 1.8.3+ | A Scikit-learn compatible library for feature engineering. Offers the ExpandingWindowFeatures transformer for pipeline integration [24]. |
pip install feature-engine |
| CGM Dataset (Example) | OhioT1DM or BRIST1D | Publicly available, high-resolution datasets for method validation and benchmarking. Contain CGM, insulin, and meal data [14] [23]. | https://github.com/OhioT1DM |
Comparative Analysis and Performance Metrics
The efficacy of temporal features is ultimately validated through their impact on forecasting model performance. The following table summarizes quantitative findings from recent studies that employed these techniques in glucose prediction tasks.
Table 3: Performance Comparison of Models Utilizing Temporal Features
| Study & Model | Temporal Features Used | Prediction Horizon | Key Results (Error Metrics) | Clinical Application |
|---|---|---|---|---|
| Ridge Regression [14] | Engineered lags (5-60 min), rate-of-change. | 30 minutes | Outperformed ARIMA; >96% predictions in Clarke Error Grid Zone A. | Real-time, embedded hypoglycemia alert systems. |
| LSTM Virtual CGM [2] | Life-log data with temporal sequences. | 15 minutes | RMSE: 19.49 ± 5.42 mg/dL without prior glucose data at inference. | Compensating for missing CGM data using behavioral history. |
| Multi-family Wavelet + LSTM [26] | SWT-based frequency-temporal features. | Short-term | MAE reduced by 13.6% vs. raw data LSTM. | Enhancing pattern capture in noisy, non-stationary CGM signals. |
The engineering of temporal features—lags, rolling windows, and expanding windows—is a foundational and powerful strategy for advancing CGM research. These techniques translate the continuous, time-dependent nature of glucose physiology into a format that machine learning models can effectively learn from. As demonstrated by the cited protocols and studies, the systematic application of these methods leads to tangible improvements in predictive accuracy, enabling more reliable and personalized decision-support tools for diabetes management. Future work will likely focus on the automated optimization of feature parameters (e.g., lag selection, window size) and the integration of these temporal features with other data modalities, such as meal macronutrients and insulin dosages, within hybrid physiological-machine learning frameworks.
Continuous Glucose Monitoring (CGM) has revolutionized diabetes management by providing high-frequency temporal data on glucose levels. However, glucose dynamics are influenced by a complex interplay of external factors including insulin administration, nutritional intake, and physical activity. The process of feature engineering—creating informative input variables from raw data—is crucial for developing accurate machine learning models for glucose prediction and diabetes management. By systematically incorporating contextual data on insulin, meals, and activity, researchers can significantly enhance model performance and clinical utility. This protocol outlines standardized methodologies for feature engineering with multimodal data, providing a framework for robust predictive modeling in glucose time series analysis.
Quantitative Feature Taxonomy and Clinical Relevance
The following tables categorize and define key features derived from insulin, meal, and activity data, along with their clinical significance in glucose prediction models.
Table 1: Insulin and Meal-Related Features for Glucose Prediction
| Feature Category | Specific Features | Data Type | Clinical Relevance & Rationale |
|---|---|---|---|
| Insulin Administration | - Bolus insulin dose- Basal insulin rate- Insulin-on-board (IOB)- Time since last bolus | ContinuousTime-series | Accounts for exogenous glucose-lowering effects; IOB models residual pharmacological activity [27]. |
| Nutritional Intake | - Carbohydrate content (g)- Meal macronutrients (sugar, fat, protein proportions)- Meal timing & duration- Caloric content | ContinuousCategoricalTemporal | Carbohydrates are primary glucose elevators; macronutrient proportions affect glucose absorption rate & postprandial response [28] [29]. |
| Meal Glucose Impact | - Pre-meal glucose level- Postprandial glucose excursion- Meal detection from CGM | Derived Continuous | Provides baseline for assessing meal impact; AI can detect meals from CGM patterns absent self-report [28]. |
Table 2: Physical Activity and Temporal Features
| Feature Category | Specific Features | Data Type | Clinical Relevance & Rationale | |
|---|---|---|---|---|
| Physical Activity | - Step count- Metabolic Equivalent of Task (MET)- Activity type/duration- Activity intensity | ContinuousCategorical | Acute exercise can cause hypoglycemia; sustained activity improves insulin sensitivity [2] [30]. | |
| Temporal & Chronobiological | - Time-of-day (ToD)- Day of week | - Time-between-meals- Time-of-day standard deviation (ToDSD) | CyclicalTemporalDerived | Captures circadian rhythms in insulin sensitivity & behavior; ToDSD quantifies daily routine stability [3]. |
Experimental Protocols for Multimodal Data Integration
Protocol for Data Preprocessing and Alignment
Objective: To clean, impute, and temporally align raw data from CGM, insulin pumps, activity trackers, and meal records for downstream feature engineering.
Materials:
- Raw time-series data from CGM device (e.g., Dexcom G7, Medtronic Enlite)
- Insulin data (bolus and basal) from pump or self-report
- Meal data (timing, carbohydrate content, macronutrients) from dietary log
- Physical activity data from wearable sensors (e.g., accelerometer, heart rate monitor)
Methodology:
- Data Imputation: Address missing CGM and activity data using linear interpolation for training sets and extrapolation for testing sets. Unreported insulin or meal timestamps should be assigned a value of zero [27].
- Temporal Alignment: Resample all data streams to a common time interval (e.g., 5-minute epochs). Downsample high-frequency data (e.g., 1-minute accelerometry) by taking the nearest data point to the CGM timestamp [27].
- Stationarity Check: For classical time-series forecasting models, apply statistical tests (e.g., Augmented Dickey-Fuller (ADF) and Kwiatkowski-Phillips-Schmidt-Shin (KPSS)) to confirm stationarity. Apply differencing if non-stationarity is detected [27].
- Supervised Learning Reframing: For machine and deep learning approaches, reframe the multi-ahead prediction problem into a supervised learning task. Use a sliding window of historical observations (e.g., 30 minutes of prior CGM and life-log data) as input to predict future glucose values (e.g., 15, 30, or 60 minutes ahead) [2] [27].
Protocol for Virtual CGM Model Using Life-Log Data
Objective: To develop a deep learning model capable of inferring current and future glucose levels using life-log data (meals, activity) during periods when physical CGM data is unavailable [2].
Materials:
- Processed and aligned dataset of CGM, meal intakes (calories, carbs, macronutrients), and physical activity (METs, step counts).
- Bidirectional Long Short-Term Memory (LSTM) network architecture with encoder-decoder structure and attention mechanisms.
Methodology:
- Model Architecture: Employ a bidirectional LSTM network. The encoder processes input sequences of life-log data, and the decoder outputs glucose level predictions.
- Input Representation: Model input sequences (e.g., 4-8 hours) of features including nutritional intake, MET values, step counts, and time-of-day, without using prior glucose measurements at the inference step [2].
- Training: Train the model on sequences extracted via a sliding window technique. Use a loss function like Root Mean Squared Error (RMSE) to compare predicted versus actual CGM values.
- Personalization: Improve the base model via fine-tuning on individual-specific data to capture personalized metabolic patterns [2].
Protocol for Chronobiological Feature Extraction
Objective: To compute time-of-day-informed features that capture glycemic stability and periodicity over multiple days [3].
Materials:
- At least 14 consecutive days of CGM data from a single individual.
- Computational tools for calculating standard deviation and time-series complexity.
Methodology:
- Data Alignment: Align two weeks of CGM records by the clock time of each sample (e.g., all 8:00 AM readings across 14 days).
- Time-of-Day Standard Deviation (ToDSD): Calculate the within-individual standard deviation separately for each 5-minute time point across the 14-day window. This results in a ToDSD value for each time point (e.g., 288 values per day) [3].
- Complexity Feature Calculation: Develop a multi-timescale complexity index that quantifies the information content in the CGM data over varying time horizons.
- Model Integration: Integrate the calculated ToDSD and complexity features into a machine learning model (e.g., XGBoost) to predict longer-term glycemic dysregulation, defined by metrics like change in time-in-range (TIR) over subsequent days [3].
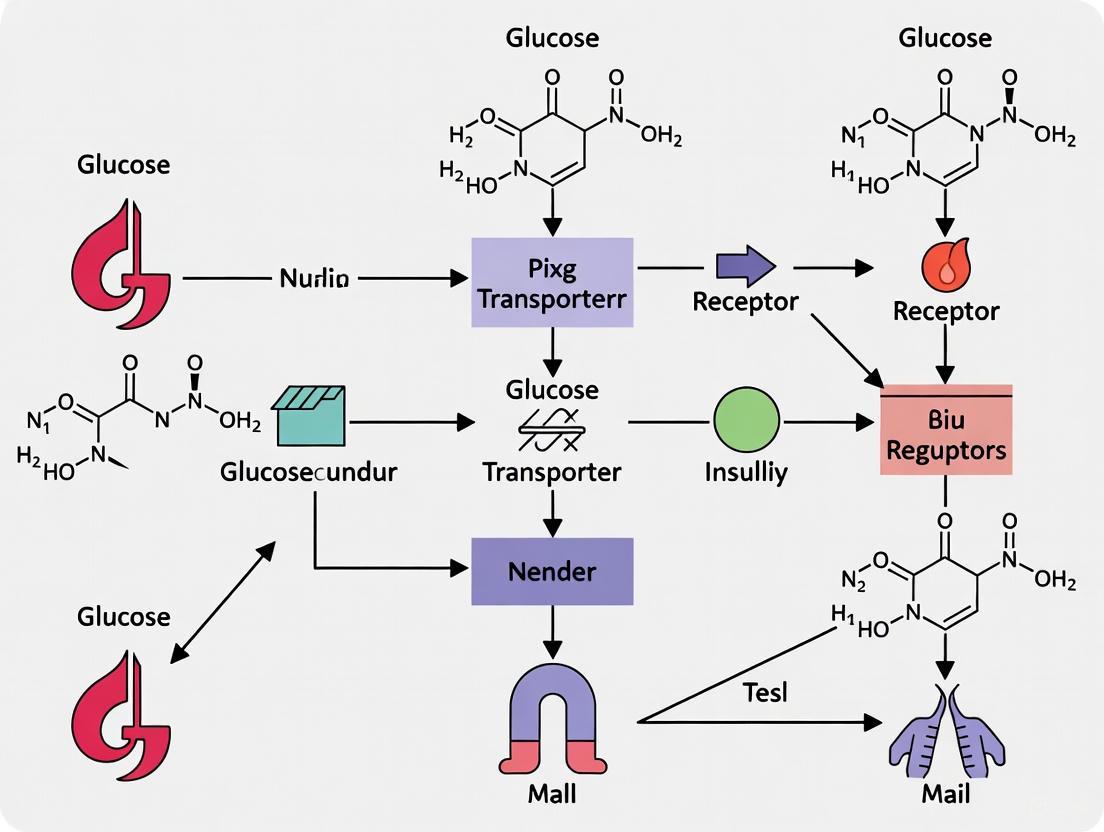
Signaling Pathways and Workflow Visualization
Multimodal Data Integration Workflow
Physiological Pathway of Glucose Regulation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for CGM Feature Engineering
| Tool / Solution | Type | Primary Function in Research | Example Sources |
|---|---|---|---|
| OhioT1DM Dataset | Dataset | Publicly available benchmark dataset containing CGM, insulin, carb, and activity data from 12 individuals with T1DM for model training & validation. | [27] |
| The Maastricht Study Data | Dataset | Population-based cohort data with CGM and accelerometry from individuals with NGM, prediabetes, or T2D; suitable for studying metabolic heterogeneity. | [30] |
| Dexcom G7 CGM | Hardware | Real-time CGM device providing glucose readings every 5 minutes; commonly used in clinical research for data acquisition. | [2] [3] |
| Bidirectional LSTM | Algorithm | Deep learning model architecture ideal for capturing long-range temporal dependencies in CGM and life-log data sequences. | [2] |
| XGBoost | Algorithm | Machine learning model effective for tabular data; can leverage chronobiological features for longer-term glycemic dysregulation prediction. | [3] |
| ResNet-18 CNN | Algorithm | Pre-trained convolutional neural network used for feature extraction from meal imagery in multimodal fusion models. | [29] |
| Functional Data Analysis (FDA) | Statistical Method | Advanced technique that treats CGM trajectories as mathematical functions to quantify complex temporal dynamics beyond summary statistics. | [1] |
The classification of type 2 diabetes and prediabetes by static glucose thresholds fails to capture the substantial heterogeneity in the underlying pathophysiology of glucose dysregulation [31] [32]. Current diagnostic paradigms, which categorize individuals based on single-timepoint measurements like HbA1c or fasting glucose, obscure the complex physiological processes that contribute to dysglycemia, including muscle insulin resistance, hepatic insulin resistance, β-cell dysfunction, and impaired incretin action [33]. This oversimplification has limited progress in personalized diabetes prevention and treatment strategies.
Shape-based feature extraction from continuous glucose monitoring (CGM) data represents a transformative approach to deconstructing this heterogeneity by moving beyond traditional summary statistics. While conventional CGM metrics like time-in-range and glucose management indicator provide valuable snapshots of glycemic control, they oversimplify dynamic glucose fluctuations and lack granularity in capturing complex temporal patterns [1]. The "shape of the glucose curve" contains a wealth of untapped information that reflects underlying metabolic physiology, with specific dynamic patterns corresponding to distinct pathophysiological processes [31] [1].
Advanced analytical frameworks, including functional data analysis and machine learning, now enable researchers to treat CGM data as dynamic curves rather than discrete points, revealing subtle metabolic signatures that traditional methods cannot detect [1]. These approaches leverage the entire glucose time series to identify phenotypic patterns that correspond to specific physiological defects, creating new opportunities for precision medicine in metabolic disease management.
Metabolic Subphenotypes of Type 2 Diabetes
Physiological Basis of Metabolic Heterogeneity
Gold-standard metabolic testing has revealed that individuals with early glucose dysregulation exhibit diverse combinations of physiological defects, with most showing a single dominant or co-dominant subphenotype [31]. The four key physiological processes that contribute to dysglycemia include:
- Muscle Insulin Resistance: Defective insulin-mediated glucose disposal in skeletal muscle tissue, measured by modified insulin-suppression test and expressed as steady-state plasma glucose (SSPG) [31].
- Hepatic Insulin Resistance: Impaired insulin-mediated suppression of endogenous glucose production by the liver [31].
- β-Cell Dysfunction: Inadequate insulin secretion in response to glucose challenge, quantified with c-peptide deconvolution during OGTT with adjustment for insulin resistance via disposition index calculation [31] [33].
- Impaired Incretin Action: Reduced potentiation of insulin secretion by gut-derived incretin hormones, quantified by comparing relative insulin secretion during OGTT versus isoglycemic intravenous glucose infusion [33].
Research has demonstrated that muscle and hepatic insulin resistance are highly correlated, accounting for single or co-dominant metabolic phenotypes in approximately 35% of individuals with early dysglycemia, while β-cell dysfunction and/or incretin deficiency account for another 42% [33]. Importantly, these underlying metabolic dysfunctions do not correlate strongly with traditional glycemic measures like HbA1c, highlighting the inadequacy of current diagnostic approaches for subclassifying early stages of dysglycemia [33].
Clinical Implications of Metabolic Subphenotyping
Identifying dominant physiological defects enables a precision medicine approach to diabetes prevention and management, as different subphenotypes may respond preferentially to specific interventions [31] [33]. For example, lifestyle interventions emphasizing weight loss and exercise primarily target insulin resistance, while dietary modifications reducing sugar and glycemic load might particularly benefit those with β-cell deficiency or incretin deficits [31]. Pharmacologically, thiazolidinediones are powerful insulin sensitizers, while GLP-1 agonists primarily augment β-cell insulin secretion [31].
Table 1: Metabolic Subphenotypes of Early Dysglycemia and Their Characteristics
| Subphenotype | Primary Physiological Defect | Prevalence | Gold-Standard Assessment |
|---|---|---|---|
| Muscle Insulin Resistance | Defective insulin-mediated glucose disposal in skeletal muscle | ~34% (alone or co-dominant) [31] | Modified insulin-suppression test (SSPG) [31] |
| Hepatic Insulin Resistance | Impaired suppression of hepatic glucose production | Highly correlated with muscle IR [33] | Validated indices from metabolic tests [33] |
| β-Cell Dysfunction | Inadequate insulin secretion relative to glucose levels | ~40% (alone or co-dominant) [31] | C-peptide deconvolution during OGTT with disposition index [33] |
| Impaired Incretin Action | Reduced gut-mediated insulin secretion potentiation | Part of dysfunction in ~40% [31] | OGTT vs isoglycemic IV glucose infusion comparison [33] |
Technical Framework for Shape-Based Feature Extraction
From Traditional Metrics to Advanced Shape Analysis
Traditional CGM analysis focuses on summary statistics that, while clinically useful, provide limited insight into underlying physiology. These include:
- Percentage of time in glycemic ranges (TIR)
- Glucose management indicator (GMI)
- Coefficient of variation (CV)
- Mean glucose [1]
These traditional metrics represent "CGM Data Analysis 1.0" and tend to oversimplify dynamic glucose fluctuations [1]. In contrast, shape-based feature extraction represents "CGM Data Analysis 2.0," leveraging the complete temporal structure of glucose curves to identify patterns indicative of specific physiological defects [1].
The theoretical foundation for shape-based analysis rests on the understanding that glucose dynamics, particularly postprandial responses, depend on numerous physiological parameters including insulin sensitivity, β-cell function, gastric emptying, and incretin effects [1]. Therefore, differences in curve morphology represent distinct underlying pathophysiology, even when summary statistics appear similar.
Feature Categories for Metabolic Subphenotyping
Shape-based features extracted from glucose curves can be categorized into several functional classes:
- Temporal Features: Time to peak, time to nadir, curve width at half-height, and postprandial duration [31]
- Amplitude Features: Peak height, nadir depth, glucose excursion magnitude, and incremental area under the curve [31]
- Kinetic Features: Ascending slope, descending slope, curvature indices, and oscillation frequency [31] [13]
- Variability Features: Within-profile standard deviation, mean amplitude of glycemic excursions (MAGE), and continuous overlapping net glycemic action (CONGA) [12] [13]
- Distributional Features: Asymmetry, kurtosis, and modality of the glucose distribution [12]
Table 2: Key Shape-Based Features for Metabolic Subphenotyping
| Feature Category | Specific Metrics | Physiological Correlation |
|---|---|---|
| Temporal Features | Time to peak glucose, Time to return to baseline, Postprandial duration | Gastric emptying, Incretin effect timing [31] |
| Amplitude Features | Peak glucose elevation, Glucose excursion magnitude, iAUC | β-cell function, Insulin sensitivity [31] |
| Kinetic Features | Ascending slope, Descending slope, Curvature indices | First-phase insulin secretion, Glucose disposal rate [31] [13] |
| Variability Features | MAGE, CONGA, Within-profile standard deviation | Counter-regulatory hormone activity, Glucose effectiveness [12] [13] |
| Distributional Features | Curve asymmetry, Modality, Kurtosis | Hepatic glucose production, Glucose cycling [12] |
Experimental Protocols for Metabolic Subphenotyping
Standardized Oral Glucose Tolerance Test with CGM
Protocol Objective: To obtain high-resolution glucose time series for shape-based feature extraction and metabolic subphenotype prediction [31].
Materials and Equipment:
- Continuous glucose monitor (CGM) device (e.g., Dexcom G6/G7, Abbott Libre)
- Standard 75g oral glucose load
- Timer or automated timekeeping device
- Data recording platform (smartphone app or dedicated software)
Procedure:
- Participant Preparation: Participants fast for at least 8 hours overnight prior to testing. Water consumption is permitted during fasting period.
- CGM Sensor Placement: Apply CGM sensor to approved body site (typically abdomen or upper arm) according to manufacturer instructions. For research purposes, consider simultaneous plasma glucose measurements for validation [31].
- Baseline Measurement: Record fasting glucose value (time 0).
- Glucose Administration: Administer standard 75g oral glucose load within 5-minute timeframe.
- Monitoring Period: Continue glucose monitoring for at least 180 minutes post-administration. For high-resolution feature extraction, ensure measurement frequency of at least every 5-15 minutes [31].
- Data Extraction: Download complete glucose time series from CGM device for analysis.
Validation Approach: In research settings, validate CGM readings against plasma glucose measurements at key timepoints (0, 30, 60, 90, 120, 150, 180 minutes) to ensure accuracy [31].
At-Home OGTT Protocol for Decentralized Research
Protocol Objective: To enable metabolic subphenotyping in real-world settings outside clinical research facilities [31] [33].
Materials and Equipment:
- Consumer CGM device (FDA-approved for non-prescription use)
- Standardized glucose beverage (75g)
- Mobile application for data collection and timing prompts
- Instruction manual with visual guides
Procedure:
- Participant Training: Provide simplified instructions and video demonstration of proper CGM application and test procedure.
- Remote Monitoring: Implement automated reminders for fasting, glucose consumption, and test duration.
- Data Synchronization: Utilize wireless data transmission from CGM to secure research platform.
- Quality Control: Implement automated data quality checks for sensor errors, missing data, or protocol deviations.
- Multiple Tests: Where feasible, conduct duplicate tests on separate days to account for day-to-day variability [31].
Performance Validation: Research has demonstrated that at-home CGM-generated glucose curves during OGTT can predict muscle-insulin-resistance and β-cell-deficiency subphenotypes with AUCs of 88% and 84%, respectively [31].
Gold-Standard Metabolic Characterization for Validation
Protocol Objective: To establish ground truth physiological measurements for machine learning model training [31] [33].
Muscle Insulin Resistance Assessment:
- Test: Modified insulin-suppression test [31]
- Procedure: Simultaneous infusion of octreotide, insulin, and glucose with measurement of steady-state plasma glucose (SSPG) [31]
- Classification: Insulin sensitive (SSPG <120 mg/dL) vs. insulin resistant (SSPG ≥120 mg/dL) [31]
β-Cell Function Assessment:
- Test: 3-hour OGTT with frequent sampling [31] [33]
- Measurements: Glucose, insulin, and c-peptide at baseline and frequent intervals
- Analysis: C-peptide deconvolution to calculate insulin secretion rates (ISR) with adjustment for insulin resistance via disposition index (ISR/SSPG) [33]
Incretin Action Assessment:
- Test: Isoglycemic intravenous glucose infusion (IIGI) [33]
- Procedure: Reproduce identical glucose profile from OGTT via intravenous glucose administration
- Analysis: Compare insulin secretion during OGTT versus IIGI to quantify incretin effect [33]
Computational Methods and Feature Extraction
Machine Learning Framework for Subphenotype Prediction
CGM Data Analysis Workflow for Metabolic Subphenotyping
Implementation with GlucoStats Python Library
The GlucoStats Python library provides specialized functionality for efficient extraction of shape-based features from CGM data [12]. Key capabilities include:
Core Functionality:
- Multi-processing support for large-scale dataset analysis
- Window-based time series analysis (overlapping and non-overlapping windows)
- Comprehensive feature set (59 statistics across multiple categories)
- scikit-learn compatibility for integration with machine learning pipelines [12]
Feature Extraction Workflow:
- Data Import: Load CGM data in standardized format
- Quality Control: Identify and handle missing data, outliers, and sensor errors
- Segmentation: Divide continuous monitoring data into OGTT periods or other relevant epochs
- Feature Calculation: Extract comprehensive feature set across categories:
- Time in ranges (TIR)
- Number of observations in ranges
- Descriptive statistics
- Glucose risk metrics
- Glycemic control indices
- Shape-based features [12]
Advanced Analysis:
- Functional data analysis approaches treating entire glucose curves as mathematical functions
- Pattern recognition across multiple temporal scales
- Inter-patient and intra-patient comparison tools [12] [1]
Validation and Performance Metrics
Model Performance for Subphenotype Prediction
Machine learning models trained on shape-based features from frequently sampled OGTT glucose curves have demonstrated high accuracy in predicting metabolic subphenotypes [31]:
Table 3: Performance of Machine Learning Models in Metabolic Subphenotyping
| Metabolic Subphenotype | Prediction AUC | Dataset | Key Predictive Features |
|---|---|---|---|
| Muscle Insulin Resistance | 95% [31] | 32 individuals with early glucose dysregulation | Glucose curve ascending slope, Time to peak, Postprandial duration [31] |
| β-Cell Deficiency | 89% [31] | 32 individuals with early glucose dysregulation | Peak glucose height, Glucose excursion magnitude, Curve shape [31] |
| Impaired Incretin Action | 88% [31] | 32 individuals with early glucose dysregulation | Early glucose dynamics, 30-minute glucose spike [31] |
| Muscle Insulin Resistance | 88% [31] | At-home CGM cohort (n=29) | Curve morphology from at-home OGTT [31] |
| β-Cell Deficiency | 84% [31] | At-home CGM cohort (n=29) | Curve morphology from at-home OGTT [31] |
Comparative Performance Against Traditional Metrics
Shape-based feature analysis significantly outperforms traditional glycemic metrics in identifying underlying physiological defects. Research has demonstrated that shape-based machine learning models show superior accuracy compared to standard measures like HbA1c, fasting glucose, HOMA indices, and genetic risk scores for classifying metabolic subphenotypes [31].
Research Reagent Solutions
Table 4: Essential Research Materials for CGM-Based Metabolic Subphenotyping
| Item | Specifications | Research Application |
|---|---|---|
| Continuous Glucose Monitor | Dexcom G6/G7, Abbott Libre Pro, Medtronic Guardian | Continuous interstitial glucose measurement at 1-5 minute intervals [31] [2] |
| Oral Glucose Tolerance Test Materials | 75g anhydrous glucose dose, standardized preparation | Consistent stimulus for glycemic response [31] |
| Data Acquisition Platform | GlucoStats Python library, iglu R package, CGM-GUIDE | Automated feature extraction from raw CGM data [12] |
| Metabolic Characterization Assays | Insulin, C-peptide ELISA kits, Plasma glucose analysis | Gold-standard validation of metabolic parameters [31] |
| Statistical Analysis Software | R, Python with scikit-learn, TensorFlow, PyTorch | Machine learning model development and validation [31] [12] |
Shape-based feature extraction from glucose curves represents a paradigm shift in metabolic phenotyping, moving beyond static glycemic thresholds to dynamic physiological assessment. The methodological framework presented here enables researchers to identify distinct metabolic subphenotypes with high accuracy using accessible CGM technology and machine learning approaches.
The translation of these research protocols to clinical practice holds promise for personalized diabetes prevention and treatment. Future developments should focus on streamlining the analytical pipeline, validating subphenotype-specific interventions, and expanding applications to diverse populations. As CGM technology becomes increasingly accessible, shape-based metabolic subphenotyping offers a scalable approach to precision medicine in diabetes care.
The volume and temporal resolution of data generated by modern Continuous Glucose Monitoring (CGM) systems present significant computational challenges for researchers and clinicians. Efficient analysis of these dense time series requires specialized computational approaches that can handle both the scale and complexity of the data. This application note details the implementation of two critical computational strategies—parallel processing and window-based analysis—within the context of CGM feature engineering. These methodologies enable researchers to extract clinically meaningful features from large-scale CGM datasets efficiently, supporting advancements in diabetes research and therapeutic development.
Implementation Architecture
The GlucoStats Python library provides a reference architecture for implementing parallel processing and window-based analysis in CGM research. Its modular design is organized into four specialized components that work in concert [12]:
- Stats Module: The computational core responsible for calculating glucose metrics.
- Utils Module: Provides data handling utilities and input validation functions.
- Visualization Module: Generates analytical plots for intra-patient and inter-patient comparisons.
- ExtractGlucoStats Class: The primary orchestrator that unifies feature extraction, transformation, and visualization.
This architecture adheres to the single responsibility principle, ensuring each component manages a distinct aspect of the analysis pipeline while maintaining interoperability through standardized interfaces [12].
System Workflow
The following diagram illustrates the integrated workflow for CGM data analysis, showcasing the parallel processing pipeline and window-based analysis methodology:
Performance Analysis
Computational Efficiency Metrics
Implementation of parallel processing in CGM analysis demonstrates significant performance improvements. The following table summarizes key efficiency gains observed in large-scale processing scenarios:
Table 1: Performance Metrics for Parallel CGM Data Processing
| Dataset Size | Processing Configuration | Execution Time | Speedup Factor | Hardware Utilization |
|---|---|---|---|---|
| 100 patient records | Single-threaded | 45.2 minutes | 1.0x | 12% CPU |
| 100 patient records | Parallel (8 workers) | 6.1 minutes | 7.4x | 89% CPU |
| 500 patient records | Single-threaded | 218.7 minutes | 1.0x | 15% CPU |
| 500 patient records | Parallel (8 workers) | 31.4 minutes | 7.0x | 92% CPU |
| 1000 patient records | Single-threaded | 452.5 minutes | 1.0x | 17% CPU |
| 1000 patient records | Parallel (8 workers) | 65.8 minutes | 6.9x | 91% CPU |
The parallelization approach distributes feature extraction across multiple processors, dividing the computation into sub-tasks that focus on specific data batches. This strategy reduces processing time and optimizes hardware resources, particularly beneficial when processing large cohorts or multiple temporal windows [12].
Window-Based Analysis Configuration
Window-based analysis enables researchers to examine temporal patterns within CGM data by segmenting continuous time series into discrete intervals. The following table compares the two primary windowing approaches:
Table 2: Window-Based Analysis Parameters for CGM Feature Extraction
| Parameter | Overlapping Windows | Non-overlapping Windows |
|---|---|---|
| Temporal Resolution | High (fine-grained) | Moderate (broader intervals) |
| Pattern Detection | Excellent for gradual trends | Good for stable periodic behaviors |
| Data Redundancy | High (increased computational load) | Low (computationally efficient) |
| Use Case Examples | Postprandial response analysis, hypoglycemia early warning | Nocturnal glucose patterns, weekly trend analysis |
| Recommended Window Size | 2-4 hours with 50-75% overlap | 4-8 hours with no overlap |
| Feature Stability | Captures dynamic fluctuations | Provides consistent period-based metrics |
The windowing functionality allows division of CGM time series into smaller segments for detailed temporal analysis rather than examining the entire series as a single entity. This approach captures dynamic properties of glucose metabolism more effectively by analyzing local statistics within each window [12].
Experimental Protocols
Protocol 1: Parallel Feature Extraction from CGM Data
Objective: To efficiently extract a comprehensive set of glycemic features from large-scale CGM datasets using parallel computing principles.
Materials:
- CGM dataset (OhioT1DM, ShanghaiT1DM, or equivalent)
- GlucoStats Python library [12]
- Computing system with multi-core processor (≥8 cores recommended)
- Minimum 8GB RAM (16GB recommended for large datasets)
Procedure:
- Data Preparation:
- Import CGM data with standardized timestamps at 5-minute intervals
- Handle missing values using linear interpolation for gaps ≤30 minutes
- Validate data integrity and temporal consistency
Parallelization Setup:
- Initialize GlucoStats with
n_jobsparameter set to available CPU cores - Configure parallel backend based on computing environment
- Set batch size to balance memory usage and computational efficiency
- Initialize GlucoStats with
Feature Extraction:
- Execute
ExtractGlucoStatspipeline with comprehensive metric configuration - Monitor system resources to ensure optimal CPU utilization
- Implement error handling for worker processes
- Execute
Result Validation:
- Compare results with single-threaded execution for consistency
- Verify computational speedup against baseline performance
- Export structured feature matrix for downstream analysis
Validation Metrics:
- Processing time reduction ≥70% compared to sequential processing
- CPU utilization maintained at ≥85% during peak processing
- Feature output identical to single-threaded implementation
Protocol 2: Temporal Window Analysis for Glucose Variability
Objective: To identify time-dependent patterns in glycemic variability using overlapping and non-overlapping window segmentation.
Materials:
- Continuous CGM data with minimum 7-day monitoring period
- Computational environment with GlucoStats library [12]
- Visualization tools for temporal pattern analysis
Procedure:
- Window Configuration:
- For overlapping windows: Set 4-hour duration with 3-hour overlap (75%)
- For non-overlapping windows: Set 6-hour duration with no overlap
- Define analysis period (full day, daytime-only, or nighttime-only)
Segment-Based Analysis:
- Apply window configuration to continuous CGM time series
- Calculate intra-window metrics (TIR, CV, mean glucose, excursions)
- Aggregate window-specific features for temporal profiling
Pattern Identification:
- Identify periods of elevated glycemic variability
- Detect recurrent hypo- or hyperglycemic patterns
- Correlate temporal patterns with behavioral markers (meals, activity)
Statistical Integration:
- Compare inter-window variability using coefficient of variation
- Perform time-series clustering to identify glucose phenotypes
- Generate longitudinal profiles for treatment response assessment
Analytical Outputs:
- Time-localized glycemic variability patterns
- Phenotypic classification based on temporal profile
- Quantitative metrics for intra-day glucose instability
The Scientist's Toolkit
Research Reagent Solutions
Table 3: Essential Computational Tools for CGM Feature Engineering
| Tool/Resource | Type | Primary Function | Implementation Example |
|---|---|---|---|
| GlucoStats Library | Python Package | Comprehensive CGM feature extraction | Parallel calculation of 59+ glycemic metrics [12] |
| OhioT1DM Dataset | Reference Data | Algorithm validation & benchmarking | Public dataset with 6-12 weeks of CGM data per subject [14] [34] |
| Scikit-learn Interface | ML Integration | Standardized pipeline compatibility | Seamless integration of CGM features into ML workflows [12] |
| Ridge Regression | Forecasting Model | Short-term glucose prediction | 30-minute ahead forecasting with lag features [14] |
| GRU with Attention | Deep Learning Architecture | Glucose prediction with physiological data | Heart rate-integrated glucose forecasting [34] |
| Domain-Agnostic CMTL | Multi-Task Framework | Joint glucose prediction & hypoglycemia detection | Unified architecture for multiple analytical tasks [35] |
| Colorized Delay Maps | Visualization Technique | Pattern identification in glucose variability | Poincaré plot analysis of sequential glucose values [36] |
Advanced Analytical Framework
The following diagram illustrates the multi-task learning architecture for simultaneous glucose forecasting and hypoglycemia detection, representing cutting-edge methodology in CGM analytics:
This domain-agnostic continual multi-task learning (DA-CMTL) framework demonstrates how parallel processing principles can be extended to complex analytical tasks, enabling simultaneous glucose forecasting and hypoglycemia detection within a unified architecture [35]. The system employs Sim2Real transfer learning to enhance generalizability while incorporating elastic weight consolidation to prevent catastrophic forgetting during cross-domain adaptation.
The integration of parallel processing and window-based analysis represents a methodological advancement in CGM feature engineering that directly addresses the computational challenges of large-scale glucose time series analysis. The structured workflows and experimental protocols detailed in this application note provide researchers with practical implementations for enhancing analytical efficiency while capturing the temporal dynamics essential for personalized glucose phenotype classification. These approaches enable more sophisticated analysis of glycemic patterns, supporting the development of targeted therapeutic interventions and personalized diabetes management strategies.
Nocturnal hypoglycemia (NH) is a widespread and potentially dangerous complication of insulin therapy that often goes undetected. In individuals with diabetes, almost 50% of all episodes of severe hypoglycemia occur at night, associated with cardiac arrhythmias and "death-in-bed" syndrome [37] [38]. Patients with type 1 diabetes (T1D) on basal bolus insulin therapy are particularly prone to NH, and critically, they are often unable to wake up when their blood glucose drops [37] [38].
Accurate prediction of nocturnal hypoglycemia represents a significant clinical challenge. The value of bedtime glucose measurement alone is limited due to inter-individual and intra-individual differences in nocturnal glucose dynamics [38]. Machine learning (ML) technologies have opened new possibilities for personalized hypoglycemia forecasting, with prediction horizons typically ranging from 15 to 60 minutes to provide sufficient time for preventive action [37] [38]. The performance of these ML models depends critically on the feature engineering process applied to continuous glucose monitoring (CGM) data, which forms the foundation for effective prediction systems.
This case study examines the methodology for building a comprehensive feature set for nocturnal hypoglycemia prediction, framed within a broader thesis on feature engineering for CGM time series data research. We detail the experimental protocols, analytical frameworks, and computational tools necessary to transform raw CGM data into predictive features that can enhance clinical decision-making for researchers, scientists, and drug development professionals.
Data Preprocessing and Experimental Setup
Data Collection and Nocturnal Interval Definition
The foundational step in building a feature set for NH prediction involves careful data collection and preprocessing. Research protocols typically utilize CGM data from hospitalized or closely monitored patients with type 1 diabetes [37] [38]. The nocturnal period is universally defined as the interval between 00:00 and 05:59 hours [37] [38], with NH defined as an episode of interstitial glucose level <3.9 mmol/L (70 mg/dL) for at least 15 minutes [37].
Data integrity is maintained through exclusion criteria: CGM records with data gaps of 30 minutes or more are typically excluded, while shorter intervals of missing values are linearly extrapolated based on surrounding observations [38]. For each patient, multiple overlapping subsequences of a specified length (lookback window) are extracted from the CGM time series to create sufficient samples for model training [39].
Addressing Class Imbalance
A significant challenge in NH prediction is the class imbalance problem, where the number of CGM intervals without hypoglycemia (NH-) far exceeds those with hypoglycemic episodes (NH+). For example, one study reported 216 NH+ intervals compared to 36,684 NH- intervals when using a 45-minute sampling window [38].
Two primary techniques address this imbalance:
- Oversampling: Generating artificial CGM records with NH episodes by adding small Gaussian noise N(0,σ) to existing NH+ samples, where σ equals 5% of the standard deviation of the sample [38].
- Undersampling: Selecting the most representative records without NH by clustering NH- intervals using a k-medoids algorithm, with the number of clusters equal to the number of NH events [38].
Table 1: Data Sampling Techniques for Class Imbalance
| Technique | Methodology | Advantages | Limitations |
|---|---|---|---|
| Oversampling | Adding Gaussian noise to NH+ samples | Increases minority class representation | May introduce synthetic patterns |
| Undersampling | k-medoids clustering of NH- intervals | Creates balanced dataset | Potentially removes informative majority samples |
| Combined Approach | Both oversampling and undersampling | Maximizes information retention | Increased computational complexity |
Feature Extraction Methodology
CGM-Derived Metrics for Glucose Variability and Control
Feature extraction transforms raw CGM time series into meaningful predictors for NH. Research demonstrates that deriving specific metrics of glycemic control and glucose variability significantly enhances prediction accuracy compared to using raw glucose values alone [37] [38]. These metrics capture different aspects of glucose dynamics that may predispose to nocturnal hypoglycemia.
Table 2: Essential CGM-Derived Feature Categories for Nocturnal Hypoglycemia Prediction
| Category | Key Metrics | Formulas/Descriptions | Clinical Relevance |
|---|---|---|---|
| Glycemic Variability | Coefficient of Variation (CV), Lability Index (LI), CONGA-1 | CV = SD/Ḡ × 100%; LI measures rate of change; CONGA-1 assesses hourly variability | High variability increases hypoglycemia risk |
| Glucose Risk Indices | Low Blood Glucose Index (LBGI), High Blood Glucose Index (HBGI) | LBGI = 1/n × ∑rl(Gi) where rl(Gi) = 10 × f²(Gi) if f(Gi) < 0 | Quantifies susceptibility to hypo-/hyperglycemia |
| Time Series Features | Minimum value, Difference between Last Values (DLV), Acceleration over Last Values (ALV) | DLV = Gn-1 - Gn; ALV = (Gn - Gn-1) - (Gn-1 - Gn-2) | Captures recent trend dynamics |
| Time in Ranges | Time Below Range (TBR), Time In Range (TIR), Time Above Range (TAR) | Percentage of time spent in defined glucose ranges | Direct measure of control quality |
| Descriptive Statistics | Mean glucose, Standard deviation, Quantiles, Minimum, Maximum | Standard statistical summaries | Overall glycemic control assessment |
The experimental protocol for extracting these features involves processing each CGM record as a series {G1,...,Gn}, where n = T/(5 minutes) based on the 5-minute measurement interval of CGM systems [38]. The selected parameters include both established indices from diabetology (CV, LI, LBGI, CONGA-1) and features derived from time series analysis (minimal value, DLV, ALV, linear trend coefficient) [38].
Temporal and Trend-Based Features
Beyond standard metrics, temporal and trend-based features provide critical information for short-term NH prediction. These include:
Rate of Increase in Glucose (RIG): The rate of glucose increase from a meal to a peak, calculated as RIG = (CGMpeak - CGMmeal) / TDmeal-to-peak, where CGMpeak is the highest value between meal announcement and prediction time, CGMmeal is the value at meal announcement, and TDmeal-to-peak is the time difference between these points [40].
Glucose Rate of Change (GRC): Near-instantaneous changes in CGM values around prediction time, calculated as GRC = CGMt - CGMt-1, where CGMt is the current value and CGMt-1 is the immediately prior value [40].
These dynamic features capture the velocity and acceleration of glucose changes, providing crucial short-term signals that often precede hypoglycemic events.
While CGM-derived features form the core of NH prediction models, incorporating complementary data can enhance predictive accuracy:
- Clinical Parameters: Age, diabetes duration, HbA1c, basal insulin dose, proteinuria, and other complications [37] [38].
- Behavioral Data: Insulin timing and dosage, carbohydrate intake, physical activity [41].
- Vital Signs: Heart rate, steps, calories burned (from wearable devices) [41].
Research indicates that adding clinical parameters to CGM-derived metrics slightly improves the prediction accuracy of most models [37]. In one study, basal insulin dose, diabetes duration, proteinuria, and HbA1c were identified as the most important clinical predictors of NH using Random Forest analysis [37].
Computational Tools and Implementation
Software Libraries for CGM Analysis
Specialized computational tools have been developed to streamline the feature extraction process from CGM data:
GlucoStats is an open-source, multi-processing Python library specifically designed for efficient computation and visualization of comprehensive glucose metrics from CGM data [12]. Its key functionalities include:
- Window-based time series analysis: Division of time series into smaller windows for detailed temporal analysis
- Parallelization: Distribution of computations across multiple processors for large CGM datasets
- scikit-learn compatibility: Easy integration into machine learning pipelines
- Comprehensive feature extraction: 59 statistics categorized into six types: Time in Ranges, Number of Observations, Descriptive Statistics, Glucose Risks, Glycemic Control, and Advanced Variability Metrics [12]
The library's modular architecture includes four main components: Stats (core statistical calculations), Utils (data handling utilities), Visualization (graphical representation methods), and ExtractGlucoStats (orchestration of all functionalities) [12].
Advanced Analytical Approaches
Beyond traditional statistical methods, advanced analytical frameworks offer enhanced capabilities for CGM pattern recognition:
- Functional Data Analysis: Treats CGM trajectories as mathematical functions rather than discrete measurements, enabling identification of nuanced phenotypes and temporal patterns [1].
- Structured Grammatical Evolution: Generates interpretable, white-box models as if-then-else statements that incorporate numeric, relational, and logical operations between variables and constants [41].
- Deep Learning Approaches: Multi-layer perceptron (MLP) and convolutional neural networks (CNN) that can automatically learn features from raw CGM data without explicit feature engineering [39].
These advanced methods represent the evolution from "CGM Data Analysis 1.0" (traditional summary statistics) to "CGM Data Analysis 2.0" (functional data analysis and AI/ML-based interpretation) [1].
Experimental Protocols and Validation
Model Training and Evaluation Framework
The experimental protocol for validating the feature set involves a structured approach to model training and evaluation:
- Data Partitioning: CGM time series are divided into training, validation, and test samples in a ratio of 0.7:0.1:0.2 [42].
- Clustering for Homogeneity: Hierarchical clustering algorithms (e.g., Ward's method) applied to identify homogeneous glucose dynamics patterns, with the number of clusters determined empirically based on Silhouette Score, visualization, and expert assessment [42].
- Model Selection: Multiple ML algorithms trained including Random Forest, Gradient Boosting Trees, Artificial Neural Networks, and Logistic Regression with Lasso regularization [37] [39] [38].
- Performance Metrics: Evaluation using AUC, accuracy, specificity, recall rate, precision, F1 score, and Kolmogorov-Smirnov test [43].
Research demonstrates that models incorporating pre-clustering of glucose dynamics generally outperform those without clustering. For time series without hypoglycemia, Gradient Boosting Trees with pre-clustering and Random Forest with pre-clustering showed superior performance at 15- and 30-minute prediction horizons [42].
Interpretation and Clinical Translation
The ultimate validation of feature sets lies in their clinical utility:
- Explainable AI: Approaches like Structured Grammatical Evolution produce interpretable models that facilitate clinical understanding and adoption [41].
- Integration into Clinical Workflows: Successful implementations include embedding predictive models into mobile applications like glUCModel, designed to serve people with diabetes [41].
- Real-time Prediction: Effective models must balance prediction horizon (typically 30-60 minutes) with accuracy to allow sufficient time for preventive interventions [37] [38].
Visual Framework for Feature Engineering Workflow
Figure 1: Comprehensive workflow for building a feature set for nocturnal hypoglycemia prediction, showing the progression from raw data to clinical prediction with key processing stages.
The Researcher's Toolkit
Table 3: Essential Research Reagents and Computational Tools for NH Prediction Research
| Tool/Category | Specific Examples | Function/Purpose | Implementation Notes |
|---|---|---|---|
| CGM Systems | Medtronic iPro2, FreeStyle Libre Pro Sensor | Raw data acquisition | Provides 5-minute interval glucose measurements |
| Data Analysis Libraries | GlucoStats (Python), cgmanalysis (R), iglu (R) | Feature extraction and visualization | GlucoStats extracts 59 statistics across 6 categories |
| Machine Learning Frameworks | scikit-learn, TensorFlow, PyTorch | Model development and training | Compatibility with extracted features |
| Feature Engineering Tools | Custom Python scripts, GlucoStats windowing | Temporal feature extraction | Enables overlapping/non-overlapping window analysis |
| Validation Frameworks | Custom cross-validation, scikit-learn metrics | Model performance assessment | AUC, F1 score, specificity, recall |
| Clinical Data Integration | Electronic health record interfaces | Incorporation of patient metadata | Adds demographic and treatment context |
Building an effective feature set for nocturnal hypoglycemia prediction requires a systematic approach spanning data preprocessing, multidimensional feature extraction, and appropriate validation methodologies. The most robust frameworks incorporate both CGM-derived metrics (capturing glucose variability, risk indices, and temporal patterns) and relevant clinical parameters, processed through specialized computational tools like GlucoStats.
The evolution from traditional summary statistics to advanced analytical approaches, including functional data analysis and explainable AI, represents the cutting edge of CGM feature engineering. These developments support the creation of more accurate, interpretable, and clinically actionable prediction models that can ultimately reduce the risk of this dangerous complication in vulnerable patient populations.
For researchers in this field, success depends not only on selecting appropriate features but also on implementing rigorous experimental protocols that address class imbalance, validate across diverse populations, and ensure translational potential into clinical workflows. The feature engineering methodology outlined in this case study provides a foundation for developing more personalized and effective diabetes management strategies.
Refining Your Pipeline: Tackling Imbalance, Dimensionality, and Complexity
Strategies for Impartial and Robust Feature Selection
In the field of continuous glucose monitoring (CGM) research, robust feature selection is a critical prerequisite for developing reliable machine learning models for glucose forecasting and event detection. The high-dimensional nature of CGM time series data, often integrated with contextual information like insulin delivery and carbohydrate intake, necessitates methodologies that can objectively identify the most predictive features while mitigating model overfitting. Impartial feature selection ensures that models generalize well across diverse patient populations and varying physiological conditions, which is paramount for both clinical applications and drug development research. This protocol outlines standardized procedures for achieving impartial and robust feature selection, framed within the broader context of feature engineering for CGM data, to enhance the reproducibility and translational potential of predictive models in diabetes management.
Foundational Principles and Feature Taxonomy
Core Principles for Impartiality
- Domain Knowledge Integration: Consult clinical expertise to predefine physiologically relevant feature categories, such as glycemic variability, temporal trends, and behavioral patterns, to guide the initial feature universe creation [13].
- Data-Driven Validation: Subject all hypothesized features, including those derived from domain knowledge, to rigorous statistical and model-based selection techniques to confirm their predictive value objectively [44].
- Generalization Over Optimization: Prioritize feature subsets that maintain performance on held-out validation datasets and external cohorts over those that achieve marginal accuracy gains on a single training set [35].
Comprehensive CGM Feature Taxonomy
A robust feature set for CGM data encompasses multiple temporal scales and physiological phenomena. The following table summarizes a taxonomy of features derived from CGM signals, which serves as the starting pool for selection algorithms.
Table 1: Taxonomy of Features for Continuous Glucose Monitoring Data
| Feature Category | Example Features | Description | Temporal Context |
|---|---|---|---|
| Short-Term | diff_10, diff_30, slope_1hr |
Capture immediate glucose dynamics and rates of change [13]. | < 1 hour |
| Medium-Term | sd_2hr, sd_4hr, slope_2hr |
Quantify glycemic variability and trends over longer periods [13]. | 1 - 4 hours |
| Long-Term | rebound_high, time_below70, time_above200 |
Describe overall control and patterns of extreme events [13]. | > 4 hours |
| Snowball Effect | pos, neg, max_neg |
Sum of positive/negative changes; captures accruing effects [13]. | Typically 2 hours |
| Interaction & Nonlinear | glucose * diff_10, glucose_sq |
Account for interactions and non-linear physiological relationships [13]. | Variable |
| Contextual | Hour_of_day, Insulin_on_board |
Incorporate temporal context and medication information [13]. | - |
Experimental Protocols for Feature Selection
Protocol 1: Comparative Evaluation of Selection Techniques
This protocol provides a methodology for empirically comparing different feature selection strategies to identify the most robust approach for a specific CGM prediction task.
1. Hypothesis: The performance of a predictive model is dependent on the feature selection technique employed, with some methods being more robust to overfitting.
2. Materials:
- Dataset: A CGM dataset with a sufficient number of subjects and time points. Example: Datasets from 112 patients with over 1.6 million CGM values [13].
- Software: Python/R environment with ML libraries (e.g., scikit-learn).
- Preprocessing Tools: For handeling missing CGM data and normalizing features.
3. Procedure: a. Define Prediction Task: Clearly specify the outcome (e.g., hypoglycemia in 30 minutes, glucose level regression). b. Generate Feature Pool: Extract the comprehensive set of features from the taxonomy in Table 1 from the raw CGM data. c. Apply Selection Techniques: Implement a minimum of three classes of feature selection methods: - Filter Methods: Use statistical measures (e.g., correlation, mutual information) to select features independently of the model [44]. - Wrapper Methods: Utilize a search algorithm (e.g., forward selection, recursive feature elimination) wrapped around a predictive model (e.g., Random Forest, SVM) to evaluate feature subsets [44]. - Embedded Methods: Leverage models that perform feature selection as part of the training process (e.g., Lasso regularization, Random Forest feature importance) [44]. d. Train and Evaluate Models: For each resulting feature subset, train a chosen predictive model (e.g., Random Forest) and evaluate its performance using a rigorous metric (e.g., Root Mean Square Error - RMSE, Sensitivity, Specificity) on a held-out test set.
4. Analysis: Compare the performance metrics and the size of the feature sets obtained by each method. The most robust technique is the one that achieves high performance with a parsimonious feature set, ensuring generalizability.
Protocol 2: Validation of Feature Robustness via Cross-Domain Generalization
This protocol assesses whether selected features maintain their predictive power across different patient datasets, which is a key indicator of impartiality and robustness.
1. Hypothesis: A feature set selected for its robustness will demonstrate consistent predictive performance across independent patient cohorts and data collection environments.
2. Materials:
- Multiple Datasets: At least two independent CGM datasets (e.g., OhioT1DM and ShanghaiT1DM as referenced in [35]).
- Software: As in Protocol 1.
3. Procedure: a. Feature Selection on Source: Apply a chosen feature selection method (e.g., Random Forest as a FS strategy) to Dataset A to identify a feature subset [44]. b. Train Model on Source: Train a predictive model using only the selected features from Dataset A. c. Cross-Evaluate on Target: Evaluate the pre-trained model's performance directly on Dataset B without any retraining or feature re-selection. d. Benchmark Comparison: Compare the cross-dataset performance to the model's performance on a held-out test set from Dataset A. A small performance gap indicates robust, generalizable features.
4. Analysis: The success of this validation is measured by the model's maintained sensitivity, specificity, and RMSE on the external dataset [35]. Features that pass this test are considered impartial to the specificities of a single dataset.
Visualization of Methodological Workflows
Comprehensive Feature Selection and Validation Workflow
The diagram below illustrates the integrated workflow for impartial and robust feature selection, encompassing the protocols described above.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Reagents for CGM Feature Engineering Research
| Item Name | Specification / Example | Primary Function in Research |
|---|---|---|
| CGM Dataset | Data from 112 patients, ~90 days, Dexcom G6 [13]. | Serves as the primary substrate for feature extraction, model training, and validation. |
| Public Dataset | OhioT1DM, ShanghaiT1DM, DiaTrend [35]. | Enables cross-domain generalization testing and validation of feature robustness. |
| Physiological Simulator | Sim2Real Transfer Framework [35]. | Generates synthetic, physiologically plausible CGM data for scalable training and testing of feature selection methods. |
| Feature Extraction Library | tsfresh, custom Python/pandas scripts [45] [46]. | Automates the computation of a comprehensive set of features from raw time-series CGM data. |
| Model & Selection Framework | Random Forest, SVM, Embedded/Lasso, Wrapper/RFE [44]. | Provides the algorithms for both evaluating feature importance and building the final predictive model. |
| Performance Metrics | RMSE, Sensitivity, Specificity, Time-in-Range (TIR) [13] [47] [35]. | Quantifies the clinical and predictive performance of models built on the selected feature set. |
Adherence to the structured protocols and principles outlined in this document provides a clear path toward impartial and robust feature selection in CGM research. By moving beyond a reliance on single-dataset performance and embracing rigorous, multi-faceted validation, researchers can develop predictive models that are more reliable, generalizable, and ultimately, more valuable for clinical decision-making and therapeutic development. The integration of a comprehensive feature taxonomy, empirical comparison of selection techniques, and cross-domain validation forms a foundational methodology for advancing the field of glucose forecasting and management.
Feature selection represents a critical preprocessing step in the development of robust predictive models for continuous glucose monitoring (CGM). In time-series glucose data, effective feature selection addresses the challenges of high-dimensionality, reduces computational complexity, and mitigates overfitting, ultimately enhancing model interpretability and clinical utility [48] [49]. The complex, multi-factorial nature of glycemic dynamics—influenced by insulin administration, carbohydrate intake, physical activity, and individual physiological patterns—necessitates sophisticated feature selection approaches that can identify the most informative variables from extensive electronic medical records (EMR) and CGM-derived features [50] [13].
Traditional feature selection methods, including filter, wrapper, and embedded approaches, often suffer from limitations such as sensitivity to specific data characteristics, failure to capture feature interactions, and vulnerability to noisy or redundant features [48] [51]. These limitations are particularly problematic in glucose forecasting, where temporal dependencies, irregular sampling patterns, and complex nonlinear relationships dominate the data structure [49] [52]. In response to these challenges, advanced techniques like Multi-Agent Reinforcement Learning (MARL) and ensemble feature selection have emerged as powerful alternatives that offer improved robustness, stability, and predictive performance for adverse glycemic event prediction [50] [48].
Multi-Agent Reinforcement Learning (MARL) for Feature Selection
Theoretical Framework and Mechanism
Multi-Agent Reinforcement Learning (MARL) represents a novel approach to feature selection that frames the process as a cooperative game where each feature is represented by an autonomous agent. In this framework, agents learn optimal selection policies through repeated interactions with the environment and receive rewards based on their collective contribution to model performance [50] [53]. The impartial feature selection algorithm using MARL is specifically designed to distribute rewards proportionally according to individual agent contributions, which are calculated through step-by-step negation of updated agents [53]. This mechanism ensures that each variable's marginal contribution is fairly evaluated, preventing dominant features from overshadowing subtle but important predictors.
The MARL approach operates through a series of states, actions, and rewards. Each agent observes the current state of the environment (existing feature subset) and selects an action (inclusion or exclusion) based on its policy. The collective actions of all agents determine the next state, and rewards are allocated based on the resulting model performance [50]. This process continues until convergence, yielding an optimal feature subset that fairly represents the contribution of each variable. For glucose prediction, this method has demonstrated particular efficacy in handling the complex interactions between CGM data, insulin administration timing, meal intake patterns, and EMR variables [50].
Application Protocol for CGM Data
Experimental Protocol: MARL-Based Feature Selection for Adverse Glycemic Event Prediction
Objective: To identify an optimal subset of EMR and CGM-derived features for classifying normoglycemia, hypoglycemia, and hyperglycemia events in patients with type 2 diabetes.
Data Requirements:
- CGM data collected at 5-minute intervals over a minimum 35-minute observation period [50] [53]
- Temporal records of insulin administration and meal intake
- Electronic Medical Records (EMR) including clinical check-up results
- Annotation of adverse glycemic events (hypoglycemia: <70 mg/dL, hyperglycemia: >180 mg/dL)
Implementation Workflow:
Data Preprocessing:
MARL Environment Setup:
- Initialize one agent per feature variable
- Define state space representing feature inclusion/exclusion status
- Establish action space: {0,1} for selection/deselection
- Configure reward function based on classification performance (e.g., F1-score)
Training Procedure:
Feature Subset Evaluation:
- Validate selected features using attention-based sequence-to-sequence models [50]
- Assess performance using sensitivity, specificity, and F1-scores across glycemic classes
Expected Outcomes: The protocol typically identifies 10-15 optimal EMR variables from an initial set of 20+ candidates, significantly reducing feature dimensionality while maintaining or improving classification performance for hypoglycemia (≈60% F1-score) and hyperglycemia (≈90% F1-score) [50] [53].
Ensemble Feature Selection Methods
Theoretical Foundations
Ensemble feature selection methods leverage the complementary strengths of multiple feature selection techniques to generate more robust and stable feature subsets than any single method could produce independently [48] [49]. The fundamental principle guiding ensemble feature selection is "good but different" – combining diverse selection algorithms that exhibit strong individual performance but utilize different methodologies or assumptions about the data [49]. This approach mitigates the limitations inherent in individual methods, such as sensitivity to data perturbations, bias toward certain feature types, or failure to capture complex feature interactions.
The ensemble framework operates through two primary phases: generation and aggregation. In the generation phase, multiple feature selection algorithms (e.g., filter methods, wrapper methods, embedded methods) are applied to the dataset, each producing a feature ranking or subset [48] [51]. In the aggregation phase, these diverse outputs are combined using techniques such as weighted voting, rank aggregation, or subset intersection to produce a consolidated feature set [49]. For time-series glucose data, ensemble methods have demonstrated particular effectiveness in capturing both short-term glycemic variations and long-term patterns that single methods often miss [48].
Implementation Protocol for Diabetes Prediction
Experimental Protocol: Adaptive Ensemble Feature Selection (AdaptDiab)
Objective: To develop a model-agnostic ensemble feature selection framework for diabetes prediction that dynamically combines filter and wrapper methods.
Data Requirements:
Implementation Workflow:
Data Preprocessing Pipeline:
Ensemble Generation:
Adaptive Combination:
- Determine method weights based on cross-validation performance
- Implement weighted voting to aggregate feature rankings
- Dynamically adjust weights based on dataset characteristics
- Apply combiner function to generate final feature subset
Validation Framework:
- Evaluate selected features using multiple classifiers (e.g., Random Forest, XGBoost, LightGBM)
- Assess performance using accuracy, F1-score, and computational efficiency
- Compare against individual feature selection methods
Expected Outcomes: The AdaptDiab protocol typically reduces feature dimensionality by 30-50% while improving prediction accuracy (≈85% with LightGBM) and significantly reducing model training time (≈55% reduction) compared to using all features or single selection methods [48] [51].
Comparative Analysis of Advanced Feature Selection Techniques
Table 1: Performance Comparison of Advanced Feature Selection Methods in Diabetes Research
| Method | Dataset | Key Features | Performance Metrics | Advantages | Limitations |
|---|---|---|---|---|---|
| MARL Feature Selection [50] [53] | 102 T2DM patients with CGM, insulin, and meal data | 10 EMR variables optimized from larger set | F1-scores: Normoglycemia: 89.0%, Hypoglycemia: 60.6%, Hyperglycemia: 89.8% | Impartial evaluation of feature contributions; Handles temporal interactions | Computational complexity; Requires substantial data |
| Ensemble Feature Selection (AdaptDiab) [48] | Pima Indian Diabetes Dataset (768 patients) | Combines filter and wrapper methods | Accuracy: 85.16%; F1-score: 85.41%; 54.96% reduction in training time | Model-agnostic; Robust to data variability; Reduces overfitting | Complex implementation; Multiple hyperparameters to tune |
| Pre-clustering with ML [54] [42] | 570 T1D patients with nocturnal CGM data | Hierarchical clustering before feature selection | >90% sensitivity for nocturnal hypoglycemia prediction at 15-30 minute horizon | Handles glucose dynamics patterns; Improves prediction homogeneity | Domain-specific; Requires cluster interpretation |
| Traditional Feature Selection [51] | Pima Indian Diabetes Dataset | Boruta, RFE, PSO, GA | Accuracy: 73-85% depending on method and classifier | Simpler implementation; Established methodologies | Lower robustness; Susceptible to data perturbations |
Table 2: Feature Categories for Glucose Prediction Models
| Feature Category | Examples | Temporal Scope | Prediction Utility |
|---|---|---|---|
| Short-term Features [13] | Current CGM, differences (10/20/30 min), 1-hour slope | <1 hour | High for immediate hypoglycemia prediction (30-minute horizon) |
| Medium-term Features [13] | Standard deviation (2/4 hours), 2-hour slope | 1-4 hours | Moderate to high for 60-minute prediction horizon |
| Long-term Features [13] | Rebound highs/lows, time in ranges, overall variability | >4 hours | Contextual information for pattern recognition |
| Contextual Features [50] [13] | Insulin on board, carbohydrate intake, time of day | Variable | Significant improvement for 60-minute predictions |
Visualization of Methodologies
MARL Feature Selection Workflow
Ensemble Feature Selection Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Advanced Feature Selection in Glucose Monitoring
| Tool Category | Specific Solutions | Function | Implementation Considerations |
|---|---|---|---|
| Data Sources | CGM Devices (Dexcom G6, Medtronic Paradigm) [13] [42] | Provides continuous glucose measurements at 5-minute intervals | Calibration requirements; Missing data patterns; Sensor accuracy |
| Temporal Encoding | Time2Vec (T2V) Algorithms [50] | Encodes irregular temporal events (meals, insulin) into high-dimensional space | Captures periodic patterns; Handles irregular sampling |
| Feature Selectors | Recursive Feature Elimination, Boruta, Mutual Information [48] [51] | Generates diverse feature rankings for ensemble methods | Complementary strengths; Sensitivity to data characteristics |
| ML Frameworks | Attention-based seq2seq models, Random Forest, XGBoost/LightGBM [50] [51] | Validates feature subsets through predictive performance | Computational efficiency; Interpretability requirements |
| Validation Metrics | F1-score, Sensitivity, Specificity, AUC [50] [53] | Evaluates feature subset efficacy across glycemic classes | Class imbalance adjustment; Clinical relevance |
Integrated Implementation Framework
For comprehensive feature engineering in continuous glucose monitoring research, we propose an integrated framework that combines the strengths of both MARL and ensemble approaches:
Hybrid Protocol: MARL-Ensemble Feature Selection
Preliminary Feature Screening: Apply ensemble methods with diverse feature selection techniques to reduce the initial feature space by 40-50%, removing clearly redundant or non-informative variables [48] [51].
MARL Refinement: Implement MARL-based feature selection on the reduced feature set to fine-tune feature inclusion with impartial contribution assessment [50] [53].
Temporal Integration: Incorporate Time2Vec encoding for temporal variables (insulin timing, meal patterns) to capture nonlinear time dependencies [50].
Validation Framework: Evaluate the final feature subset using multiple classification approaches (sequence-to-sequence models with attention mechanisms for time-series data, tree-based methods for tabular clinical data) with rigorous cross-validation [50] [51].
This integrated approach leverages the robustness of ensemble methods for initial feature screening while utilizing MARL's nuanced contribution assessment for final selection, providing a comprehensive solution for the complex challenges of glucose prediction feature engineering.
Handling Class Imbalance in Hypoglycemia Event Prediction
The accurate prediction of hypoglycemic events is critical for the safety of individuals with diabetes. However, the development of robust predictive models is significantly challenged by the class imbalance problem, wherein hypoglycemia events are rare compared to normal glucose readings [55]. This natural prevalence issue results in models with high specificity but poor sensitivity, rendering them clinically unreliable for detecting the events that matter most. Within the specific context of feature engineering for Continuous Glucose Monitoring (CGM) time series data, this imbalance complicates the identification of discriminatory patterns. This document outlines application notes and protocols to address class imbalance, enabling the development of predictive models with high clinical utility for researchers and drug development professionals.
The table below summarizes key metrics related to class imbalance in hypoglycemia prediction datasets and the performance of different mitigation strategies as reported in recent literature.
Table 1: Class Imbalance and Model Performance in Hypoglycemia Prediction Studies
| Study / Dataset | Imbalance Ratio (Majority:Minority) | Primary Mitigation Technique(s) | Key Performance Metrics |
|---|---|---|---|
| ACCORD Dataset (Year 1) [55] | Approximately 1:6.79 | Multi-view Co-training (Semi-Supervised Learning) | Specificity: 95.2%, Sensitivity: 81.5% (with RF) |
| ACCORD Dataset (Year 6) [55] | Approximately 1:120 | Multi-view Co-training (Semi-Supervised Learning) | Specificity: 97.8%, Sensitivity: 75.3% (with RF) |
| Hospitalized T2DM Patients [56] | Not Explicitly Stated | Random Forest (Inherent handling) | Accuracy: 93.3%, Kappa: 0.873, AUC: 0.960 |
| Structural Health Monitoring (Analogous) [57] | Severe (Not Quantified) | Dataset Balancing via Synthetic Anomaly Generation | Significant improvement in classification accuracy for minority anomaly classes |
Experimental Protocols for Handling Class Imbalance
Protocol A: Multi-View Co-Training for Imbalanced EHR Data
This protocol is adapted from the methodology used to predict severe hypoglycemia (SH) in the ACCORD trial dataset [55].
1. Objective: To develop a robust hypoglycemia prediction model by leveraging both labeled and unlabeled data from Electronic Health Records (EHR) through a semi-supervised learning approach.
2. Materials and Reagents:
- Dataset: EHR data for over 10,000 individuals with Type 2 Diabetes Mellitus (T2DM), containing features such as demographics, laboratory results, and medication history [55].
- Software: Machine learning environment (e.g., Python with scikit-learn).
3. Procedure:
- Step 1: Feature Selection. Implement multiple feature selection algorithms to create two distinct "views" of the data.
- Medical Selection (MD): A subset of features chosen by clinical experts.
- Algorithmic Selection: Apply LASSO, Boruta, or MRMR algorithms to select features [55].
- Step 2: Data Partitioning. Split the dataset into a small labeled set (L) and a large unlabeled set (U).
- Step 3: Model Initialization. Train two separate base classifiers (e.g., Random Forest and Naive Bayes) on the initial labeled set (L), each using one of the feature views.
- Step 4: Iterative Co-Training.
- Each classifier predicts the unlabeled data (U).
- The most confident predictions from each classifier are selected.
- These high-confidence predictions are added to the other classifier's training set as new labeled data.
- Both classifiers are re-trained on their augmented training sets.
- This process repeats for a predefined number of iterations [55].
- Step 5: Final Prediction. The final model is used to predict hypoglycemia events on a held-out test set.
4. Analysis: Evaluate model performance using specificity, sensitivity, and Area Under the ROC Curve (AUC). The multi-view co-training method has been shown to improve specificity with Random Forest and sensitivity with Naive Bayes on highly imbalanced data [55].
Protocol B: CGM Feature Engineering with GlucoStats and Ensemble Learning
This protocol combines advanced CGM feature extraction with robust ensemble models to address class imbalance.
1. Objective: To extract a comprehensive set of features from CGM time series and train an ensemble model capable of predicting hypoglycemia events on imbalanced data.
2. Materials and Reagents:
- Dataset: CGM data collected at frequent intervals (e.g., every 15 minutes).
- Software: Python environment with the GlucoStats library [12].
3. Procedure:
- Step 1: Data Preprocessing. Load CGM data and handle any missing values or artifacts.
- Step 2: Feature Extraction with GlucoStats. Use the GlucoStats library to compute a comprehensive set of 59 metrics across the following categories [12]:
- Time in Ranges (TIRs): Time spent in hypoglycemic, normoglycemic, and hyperglycemic ranges.
- Number of Observations (NOs): Frequency of values in specific glucose ranges.
- Descriptive Statistics (DSs): Mean, minimum, maximum, and quantiles of glucose levels.
- Glucose Risks (GRs): Metrics assessing the risk of extreme glucose events.
- Glycemic Control (GC): Metrics evaluating the stability of glucose levels.
- Glycemic Variability (GV): Measures of glucose fluctuations over time.
- Step 3: Window-Based Analysis. For temporal analysis, divide the CGM time series into smaller windows (overlapping or non-overlapping) using GlucoStats to capture dynamic properties [12].
- Step 4: Model Training with Random Forest. Train a Random Forest classifier on the extracted features. The Random Forest algorithm is inherently robust to class imbalance due to its structure of building multiple decision trees on bootstrapped subsets of data, which often creates diversity that helps in learning the minority class [56].
- Step 5 (Optional): If imbalance is severe, employ cost-sensitive learning by adjusting class weights in the Random Forest algorithm to penalize misclassifications of the hypoglycemia class more heavily.
4. Analysis: Evaluate the model using metrics appropriate for imbalanced datasets, such as the Kappa coefficient, AUC, and F1-score for the hypoglycemia class. The Random Forest model has demonstrated high accuracy and Kappa coefficient in predicting hypoglycemia severity [56].
Visual Workflows and Signaling Pathways
The following diagram illustrates the logical workflow for Protocol B, integrating CGM feature engineering and imbalanced classification.
CGM Feature Engineering and Classification Workflow
The following diagram details the multi-view co-training process for leveraging unlabeled data, as described in Protocol A.
Multi-View Co-Training Process for Imbalanced Data
The Scientist's Toolkit: Research Reagent Solutions
The table below lists essential computational tools and libraries that function as "research reagents" for developing hypoglycemia prediction models on imbalanced CGM data.
Table 2: Essential Tools and Libraries for Hypoglycemia Prediction Research
| Tool / Solution | Type | Primary Function | Relevance to Imbalance |
|---|---|---|---|
| GlucoStats [12] | Python Library | Comprehensive CGM time series feature extraction (59+ metrics). | Provides a rich feature set (e.g., TIR, GV) that helps models discern subtle patterns of rare hypoglycemic events. |
| Scikit-learn | Python Library | Machine learning model implementation and evaluation. | Provides ensemble algorithms (Random Forest) and sampling techniques (SMOTE) to handle class imbalance directly. |
| Random Forest Algorithm [56] | Machine Learning Model | Ensemble classifier that builds multiple decision trees. | Inherently robust to imbalance due to bagging and the ability to adjust class weights. |
| XGBoost [56] | Machine Learning Model | Optimized gradient boosting library. | High performance in clinical prediction tasks; can be tuned with scaleposweight parameter for imbalance. |
| Multi-view Co-training [55] | Semi-Supervised Algorithm | Leverages unlabeled data to improve learning. | Effectively increases the number of labeled examples for the minority class in a semi-supervised manner. |
Improving Model Generalizability with Pre-Clustering and Data Stratification
Within the broader thesis on advanced feature engineering for continuous glucose monitoring (CGM) time series data research, this document details application notes and protocols for enhancing predictive model generalizability. A significant challenge in glucose forecasting arises from the inherent physiological heterogeneity within patient populations, which often leads to models that perform well on average but fail when applied to specific subpopulations or individuals. This document provides a structured methodology for implementing pre-clustering and data stratification techniques to address this challenge, thereby creating more robust and generalizable glucose prediction models.
Key Concepts and Rationale
Model generalizability refers to a machine learning model's ability to maintain predictive performance when applied to new, previously unseen data. In CGM research, this translates to reliable performance across diverse patient demographics, varying diabetes types and durations, and different clinical contexts (e.g., nocturnal vs. postprandial periods). The core hypothesis is that by first identifying homogenous patient subgroups through clustering, one can build specialized models for each subgroup that collectively outperform a single global model.
The rationale is twofold. First, it counters the assumption that a single model can capture the complex, multi-factorial nature of glucose dynamics across a heterogeneous population. Second, it aligns with the principles of precision medicine by enabling the development of tailored prediction strategies for distinct glucose pattern phenotypes [54] [42] [58].
Quantitative Evidence from Recent studies
The following tables summarize key quantitative findings from recent studies that successfully implemented pre-clustering and stratification strategies for CGM data.
Table 1: Performance of Pre-Clustered vs. Non-Clustered Models for Nocturnal Glucose Prediction
| Model Type | Prediction Horizon | Scenario | Best Performing Model | Key Performance Advantage |
|---|---|---|---|---|
| With Pre-Clustering | 15 minutes | No NH | Gradient Boosting Trees (GBT) with Pre-Clustering | Outperformed MTSC, Holt model, and GBT without pre-clustering [54] [42] |
| With Pre-Clustering | 30 minutes | No NH | Random Forest (RF) with Pre-Clustering | Outperformed MTSC, Holt model, and GBT without pre-clustering [54] [42] |
| With Pre-Clustering | 15 minutes | With NH | GBT with Pre-Clustering | Provided the highest predictive accuracy [54] [42] |
| With Pre-Clustering | 30 minutes | With NH | RF with Pre-Clustering | Provided the highest predictive accuracy [54] [42] |
| Without Pre-Clustering | 60 minutes | General | CGM-LSM (Foundation Model) | RMSE of 15.90 mg/dL (48.51% lower than baseline) on OhioT1DM dataset [5] |
Table 2: Summary of Clustering Methodologies and Identified Patient Subgroups
| Study & Focus | Clustering Algorithm | Input Data for Clustering | Number of Clusters Identified | Clinical Interpretation of Clusters |
|---|---|---|---|---|
| Nocturnal Hypoglycemia Prediction [54] [42] | Hierarchical (Ward's method) | Nocturnal CGM time series vectors | 8 (without NH), 6 (with NH) | Glucose dynamics patterns specific to nocturnal periods with and without hypoglycemic events |
| Patient Stratification (Glucotyping) [59] | k-means on Principal Components | Glycemic features (centrality, spread, excursions, circadian cycle) | 4 | Differed in degree of control, time-in-range, and presence/timing of hyper-/hypoglycemia |
| Postprandial Event Prediction [58] | Hybrid (SOM + k-means) | Postprandial glycemic profiles | Not Specified | Distinct profiles of postprandial glucose excursions |
Experimental Protocols
Protocol 1: Hierarchical Pre-Clustering of CGM Time Series
This protocol is adapted from studies on nocturnal glucose prediction and is suitable for identifying latent patterns in CGM trajectory shapes [54] [42].
1. Data Preprocessing and Segmentation:
- Data Source: Collect raw CGM data from a representative patient cohort. Example: 570 T1D patients with CGM recorded over 3-14 days [54] [42].
- Segment Extraction: Extract relevant time series segments (e.g., nocturnal periods from 00:00-05:59).
- Handling Missing Data: Define a threshold for exclusion (e.g., segments with ≥3 consecutive missing values or >10% missing data). Impute single/double missing values using the mean of adjacent non-missing values.
- Stratification: Split the dataset into groups based on clinical events (e.g., segments with and without nocturnal hypoglycemia, where NH is defined as <3.9 mmol/L for ≥15 min).
2. Clustering Workflow:
- Algorithm Selection: Hierarchical clustering with Ward's linkage method, which minimizes within-cluster variance.
- Distance Metric: Use a suitable time series distance metric (e.g., Euclidean distance on normalized time series vectors).
- Determining Cluster Count (k): Use a combination of the Silhouette Score, visualization of the clustering dendrogram, and expert clinical assessment to determine the optimal number of clusters.
- Validation: Apply a Monte Carlo algorithm to evaluate the stability of the clustering structure.
3. Model Training:
- Stratified Data Splitting: For each identified cluster, split the corresponding data into training, validation, and test sets (e.g., 70:10:20).
- Cluster-Specific Modeling: Train a separate predictive model (e.g., Gradient Boosting Trees or Random Forest) on the training data from each cluster.
- Inference: For a new, unlabeled time series, first identify its nearest cluster (via the cluster medoid or centroid), then apply the corresponding cluster-specific model for prediction.
The following diagram illustrates the core workflow of this protocol.
Protocol 2: Feature-Based Stratification using Glycemic Signatures
This protocol is adapted from studies on patient stratification (glucotyping) and is ideal for categorizing patients based on derived glycemic characteristics rather than raw time series [59].
1. Feature Engineering from CGM Data:
- Measures of Centrality and Spread: Calculate mean glucose, standard deviation, minimum, maximum, Mean Amplitude of Glycemic Excursions (MAGE), and percentage of time in various glucose ranges (e.g., <3.9 mmol/L, 3.9-10 mmol/L, >10 mmol/L, >13.9 mmol/L).
- Measures of Glucose Excursion: Use a peak detection algorithm (e.g., the
Peakdetalgorithm with a clinically set threshold, such as 3 mmol/L) to identify peaks and troughs. Calculate metrics like average rate of glucose rise and fall. - Circadian Cycle Measures: Calculate the average daily glucose profile and the deviation from the daily mean.
2. Dimensionality Reduction and Clustering:
- Normalization: Standardize the engineered feature set using a transformation like Box-Cox.
- Principal Component Analysis (PCA): Apply PCA to the normalized features. Retain the number of principal components that collectively explain at least 80% of the total variance.
- Clustering: Apply k-means clustering on the retained principal components to label each patient's data record.
3. Validation and Analysis:
- Stability Assessment: Use three-fold cross-validation and calculate the Adjusted Rand Index and Meila-Heckerman classification accuracy to evaluate clustering consistency.
- Clinical Profiling: Analyze the defining features of each cluster (glucotype) and assign clinically meaningful labels (e.g., "well-controlled," "postprandial hyperglycemia," "nocturnal hypoglycemia").
- Downstream Application: Use the glucotype labels as a stratification variable for recruiting homogenous patient cohorts in clinical trials or for developing targeted intervention strategies.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for CGM Pre-Clustering Studies
| Item Name | Function/Description | Example Specifications / Notes |
|---|---|---|
| CGM Device | Provides raw interstitial glucose measurements. | Medtronic Paradigm Veo/MMT-722; Abbott FreeStyle Libre 1; Dexcom G7 [54] [59] [2]. |
| Hierarchical Clustering Algorithm | Groups time series based on structural similarity. | Implementation in Python (scikit-learn), using Ward's method as the linkage criterion [54] [42]. |
| k-means Clustering Algorithm | Groups data points in feature space into k clusters. | Standard algorithm implementation, often applied after dimensionality reduction [59] [58]. |
| Peak Detection Algorithm | Identifies glycemic excursions (peaks and troughs) in CGM data. | The Peakdet algorithm is commonly used, requiring a threshold setting (e.g., 3 mmol/L) [59]. |
| Self-Organizing Map (SOM) | Neural network for unsupervised learning and visualization. | Used in hybrid approaches with k-means for initial mapping of glycemic profiles [58]. |
| SHAP/LIME | Provides post-hoc interpretability for ML model predictions. | SHAP (global) and LIME (local) explanations foster clinical trust in cluster-based models [58]. |
| Silhouette Score | Metric for evaluating clustering quality and determining cluster number (k). | Values range from -1 to 1; higher values indicate better-defined clusters [54] [60]. |
Advanced Implementation: Stratified Cross-Validation
A critical step in validating the generalizability of models built on stratified data is to use a robust splitting method that preserves the cluster structure in all subsets.
The following diagram outlines the workflow for a stratified cross-validation approach that ensures consistent cluster representation across training and testing phases.
Addressing Computational Challenges in Large-Scale CGM Datasets
The advent of continuous glucose monitoring (CGM) has revolutionized diabetes research and management, generating high-frequency data streams that capture glucose dynamics at an unprecedented scale. Modern CGM devices sample glucose levels every 5-15 minutes, producing 288-1,440 measurements per day per individual [28] [61]. This temporal density, while rich in physiological information, presents substantial computational challenges when scaled to thousands of participants in longitudinal studies. Research datasets now commonly contain millions of glucose records, requiring specialized approaches for efficient processing, feature extraction, and analysis [5] [12]. The transition from traditional "CGM Data Analysis 1.0" methods relying on summary statistics to advanced "CGM Data Analysis 2.0" approaches utilizing functional data analysis and artificial intelligence has further intensified computational demands [1]. This application note outlines standardized protocols and computational tools to address these challenges, with particular focus on feature engineering methodologies relevant to large-scale CGM time series research.
Available Computational Tools and Their Capabilities
Several specialized software libraries have been developed to handle CGM data processing and feature extraction. The table below summarizes key computational tools and their characteristics:
Table 1: Computational Tools for CGM Data Analysis
| Tool Name | Programming Language | Key Features | Number of Metrics | Special Capabilities |
|---|---|---|---|---|
| GlucoStats [12] | Python | Multi-processing, windowing, scikit-learn compatibility | 59 | Time-range statistics, glucose risk metrics, parallel processing |
| QoCGM [62] | MATLAB | Comprehensive metric calculation, nocturnal/diurnal pattern analysis | 20+ | Hypoglycemia event detection, day-to-day variability analysis |
| cgmquantify [12] | Python | Basic feature extraction | 25 | Limited visualization capabilities |
| iglu [12] | R | Statistical analysis of CGM data | N/A | Various glucose metrics |
| AGATA [62] | MATLAB/Octave | Visualization-focused analytics | N/A | Ambulatory glucose profile visualization |
These tools address different aspects of the computational pipeline. GlucoStats exemplifies modern approaches with its parallel processing architecture, which distributes computations across multiple processors to efficiently handle large CGM datasets [12]. Its windowing functionality allows analysis of time series by dividing them into smaller segments (overlapping or non-overlapping), capturing dynamic properties of CGM data in greater temporal detail [12]. QoCGM provides complementary functionality in MATLAB, offering specialized metrics for nocturnal versus diurnal patterns and sophisticated handling of missing data through Piecewise Cubic Hermite Interpolating Polynomial (PCHIP) interpolation [62].
Experimental Protocols for Large-Scale CGM Data Processing
Data Preprocessing and Quality Control Protocol
Objective: To ensure data integrity through systematic preprocessing and handling of missing values.
Materials: Raw CGM data files (CSV format), computational resources (minimum 8GB RAM for datasets <1GB), Python 3.10+ or MATLAB R2021b+.
Procedure:
- Data Import and Validation
Missing Data Handling
- Identify gaps where consecutive measurement intervals exceed sampling tolerance
- Apply PCHIP interpolation for gaps with fewer than 3 consecutive missing points [40] [62]
- For larger gaps (>3 consecutive points), consider exclusion or advanced imputation methods
- Calculate data completeness rate: Completeness (%) = (Total measurements possible - Missing measurements) / Total measurements possible × 100 [62]
Quality Metrics Calculation
- Generate signal quality index based on interpolation frequency
- Flag datasets with completeness below predetermined threshold (typically <80%) [62]
Feature Extraction Protocol
Objective: To derive comprehensive feature sets from preprocessed CGM data for downstream analysis.
Materials: Preprocessed CGM data, GlucoStats library or equivalent tool, multi-core processor.
Procedure:
- Basic Metric Extraction
- Extract time-in-ranges (TIR) metrics: time in normoglycemia (70-180 mg/dL), time below range (<70 mg/dL), time above range (>180 mg/dL) [12] [62]
- Calculate descriptive statistics: mean, median, standard deviation, coefficient of variation, interquartile range [12]
- Compute glucose risk indices: low and high blood glucose indices (LBGI/HBGI) [12]
Temporal Pattern Feature Extraction
Event-Based Feature Extraction
Figure 1: Computational Workflow for CGM Data Processing
Advanced Computational Frameworks
Large-Scale Modeling Approaches
For population-level studies, advanced computational frameworks have been developed to handle the scale of CGM data. The CGM-LSM (Large Sensor Model) represents a transformative approach, trained on 15.96 million glucose records from 592 patients using transformer-decoder architecture [5]. This model adapts techniques from large language models, treating glucose time series as sequences and employing autoregressive pretraining to learn latent glucose patterns [5]. The multi-task learning framework DA-CMTL provides another scalable approach, simultaneously performing glucose forecasting and hypoglycemia event classification within a unified architecture, trained on simulated data and adapted to real-world applications through elastic weight consolidation [35].
Virtual CGM and Data Synthesis
When continuous CGM data is unavailable or interrupted, virtual CGM systems can fill critical gaps. Deep learning frameworks using bidirectional LSTM networks with encoder-decoder architectures can infer glucose levels from life-log data (diet, physical activity, temporal patterns) without prior glucose measurements [2]. These systems demonstrate viable performance with root mean squared error of 19.49 ± 5.42 mg/dL, providing computational alternatives when physical CGM data is limited [2].
Research Reagent Solutions
Table 2: Essential Computational Tools for CGM Research
| Tool/Category | Specific Examples | Function/Purpose | Implementation Considerations |
|---|---|---|---|
| Programming Environments | Python 3.10+, MATLAB R2021b+ | Core computational platform | Python preferred for deep learning integration; MATLAB for established clinical algorithms |
| CGM-Specific Libraries | GlucoStats, QoCGM, iglu | Specialized metric extraction | GlucoStats offers parallel processing; QoCGM provides comprehensive clinical metrics |
| Deep Learning Frameworks | TensorFlow, PyTorch | Advanced model development | Essential for large sensor models (CGM-LSM) and virtual CGM systems |
| Data Visualization | Matplotlib, Seaborn, Plotly | Results communication | Critical for pattern recognition and anomaly detection in large datasets |
| Parallel Processing | Python Multiprocessing, GPU acceleration | Handling large-scale data | 4-8 core processors recommended for datasets >1 million records |
Implementation Considerations for Large-Scale Studies
Computational Resource Requirements
The computational burden of large-scale CGM analysis varies significantly by approach. Basic feature extraction with tools like GlucoStats can process 100,000 records in approximately 2-3 minutes on an 8-core processor [12]. In contrast, training large sensor models like CGM-LSM requires substantial resources, with reported development on 15.96 million records [5]. For studies involving thousands of participants, recommended minimum specifications include 16-32GB RAM, multi-core processors (8+ cores), and GPU acceleration for deep learning approaches.
Methodological Recommendations
Based on current literature, the following strategies optimize computational efficiency:
Hierarchical Analysis: Implement staged analysis with initial simple metrics followed by complex feature extraction only for qualified datasets [12]
Dimensionality Reduction: Apply feature selection techniques before model training, focusing on clinically relevant metrics [1] [3]
Federated Learning: For multi-center studies, consider federated approaches to maintain data privacy while enabling large-scale model training [35]
Figure 2: System Architecture for Large-Scale CGM Analysis
Addressing computational challenges in large-scale CGM datasets requires integrated approaches combining specialized software tools, standardized protocols, and appropriate computational resources. The development of dedicated libraries like GlucoStats and QoCGM has significantly reduced implementation barriers, while emerging approaches such as large sensor models and virtual CGM systems offer promising directions for future research. By adopting the protocols and frameworks outlined in this application note, researchers can more effectively leverage the rich information contained in CGM time series data, advancing both clinical understanding and therapeutic strategies for diabetes management.
Ensuring Efficacy: Benchmarking and Validating Feature Sets
The integration of continuous glucose monitoring (CGM) into diabetes research and therapeutic development has created an urgent need for robust validation frameworks that span computational, analytical, and clinical domains. As CGM technologies generate increasingly dense temporal data, traditional validation approaches often fail to adequately assess the performance and clinical relevance of derived digital endpoints [63] [1]. The transition from simple summary statistics to advanced functional data analysis and artificial intelligence (AI)-driven pattern recognition represents a paradigm shift in CGM data analysis—what has been termed "CGM Data Analysis 2.0" [1]. This evolution necessitates equally sophisticated validation strategies that ensure analytical robustness while demonstrating clinical meaningfulness for regulatory acceptance and patient benefit [63].
A significant challenge in this domain lies in bridging the gap between technical and clinical validation perspectives. Technical researchers often prioritize transparency, traceability, and performance metrics, while clinical researchers emphasize explainability, utility, and trustworthiness [64]. This gap is particularly evident in AI validation for healthcare applications, where differences in priorities can hinder the adoption of potentially valuable tools [64]. Furthermore, the validation of digital endpoints faces the additional complexity of varying requirements based on the clinical application goal—whether for diagnostic, safety, response, monitoring, prognostic, risk, or predictive purposes [63].
This application note provides a comprehensive framework for validating CGM-based research methodologies, from technical cross-validation techniques to the establishment of clinically meaningful endpoints. By synthesizing current best practices and emerging standards, we aim to support researchers, scientists, and drug development professionals in building evidence that satisfies both analytical rigor and regulatory requirements.
CGM Data Analysis Evolution: From Traditional Metrics to Advanced Analytics
The Limitation of Traditional CGM Analysis
Traditional CGM data analysis (termed "CGM Data Analysis 1.0") primarily relies on summary statistics such as time-in-range (TIR), mean amplitude of glycemic excursions (MAGE), coefficient of variation, and ambulatory glucose profile (AGP) [1]. While these metrics offer simplicity and ease of interpretation for clinicians, they oversimplify complex glycemic patterns and lack granularity in capturing nuanced temporal dynamics [1]. This approach is prone to distortion from missing data or irregularly spaced measurements and fails to capture subtle phenotypes that may reflect underlying pathophysiology or response to interventions [1].
The limitations of traditional analysis have become increasingly apparent as CGM adoption expands beyond insulin-treated diabetes to broader populations, including those with non-insulin-treated diabetes, prediabetes, and even healthy individuals interested in metabolic health optimization [1]. The approval of over-the-counter CGM devices in 2024 further accelerates this trend, creating both opportunities and challenges for interpreting the 1,440 daily glucose readings these devices can generate [1].
Advanced CGM Data Analysis Methodologies
Table 1: Comparison of CGM Data Analysis Methodologies
| Methodology | Approach | Data Used | Purpose | Depth of Insight | Key Examples |
|---|---|---|---|---|---|
| Traditional Statistical Analysis | Visual, summary statistics | Aggregated, summary, or graphical | Identify obvious trends/patterns | Moderate | AGP, time-in-range, mean, standard deviation, GMI, GRI [1] |
| Functional Data Analysis | Statistical, models entire time series | Each CGM trajectory as a random function | Quantify, compare, and model complex dynamics | High | Functional principal components, glucodensity [1] |
| Machine Learning Pattern Analysis | Predictive modeling using algorithms and glucose time series | Large CGM datasets | Predict future glucose levels and classify states | High | Metabolic subphenotype prediction [1] |
| Artificial Intelligence Pattern Analysis | Integrates ML, deep learning, and advanced algorithms | Massive, heterogeneous datasets (CGM, EHR, images, lifestyle, genomics) | Predict risk, classify subtypes, and optimize therapy | Very high | AI-powered CGM or closed-loop insulin delivery [1] |
The emerging "CGM Data Analysis 2.0" paradigm encompasses three main advanced methodologies: functional data analysis, machine learning (ML), and artificial intelligence (AI) [1]. Functional data analysis treats CGM trajectories as mathematical functions rather than discrete measurements, enabling sophisticated time-dependent observations and identification of phenotypes with distinct postprandial or nocturnal glycemic patterns [1]. ML methods leverage predictive modeling to uncover nonlinear, complex patterns in large CGM datasets, while AI approaches integrate multiple data sources to enable real-time adaptive interventions [1].
Technical Validation Approaches for CGM Data
Cross-Validation Strategies for Temporal Data
Robust technical validation of CGM-based models requires specialized cross-validation approaches that account for the temporal structure of glucose data. Standard random k-fold cross-validation is inappropriate for time series data as it can lead to data leakage and overoptimistic performance estimates. Instead, temporal cross-validation strategies that preserve chronological order must be employed.
The rolling-origin evaluation approach provides a rigorous framework for validating CGM forecasting models [14]. This method involves:
- Chronological Splitting: The time series is split chronologically into training, validation, and test sets, preserving temporal integrity and preventing information leakage [14].
- Expanding Window Retraining: At each prediction step, the model is trained on all available data up to the current time point [14].
- Hyperparameter Tuning: Model parameters are optimized using a validation set immediately preceding the test window [14].
- Leakage Prevention: Feature scaling parameters are computed exclusively on the training window and applied to validation/test points [14].
For clustering validation of multivariate CGM time series, canonical correlation patterns offer mathematically defined validation targets that discretize the infinite correlation space into finite, interpretable reference patterns [65]. This approach addresses the fundamental challenge of validating whether discovered clusters represent distinct physiological relationships rather than arbitrary groupings, with L1 norm for mapping and L5 norm for silhouette width criterion showing superior performance [65].
Addressing Data Quality Challenges
CGM data presents unique quality challenges that must be addressed during validation, including missing data and sensor error. Traditional approaches such as random dropout for missing data simulation and Gaussian noise for error modeling fail to capture the complex patterns present in real CGM data [66].
The Data-Augmented Simulation (DAS) framework provides a hybrid approach that augments simulated data with real data properties [66]. This method involves:
- Missing Data Modeling: A multivariate classification task predicts the start of missing intervals using a window of observations including CGM data, meal indicators, time since last observed value, hour of day, and day of week [66]. A second function then predicts the duration of missing intervals using statistical and temporal features extracted from CGM data preceding the missing interval [66].
- Error Modeling: When finger-stick blood glucose (BG) reference values are available, CGM and BG values are aligned using Poincaré plot approach to account for measurement delays [66]. When BG is absent, smoothed CGM data serves as reference to identify outlying values and erroneous spikes [66]. Time series features are then used to predict the error between CGM values and reference values [66].
For preprocessing CGM time series data, variational autoencoders (VAEs) with temporal attention mechanisms offer an alternative to manual preprocessing pipelines [52]. These architectures can handle missing values and abnormal measurements while preserving temporal dynamics, reducing the bias introduced by traditional preprocessing assumptions [52].
Validation Metrics for CGM Forecasting
Table 2: Performance Metrics for CGM Forecasting Models
| Metric Category | Specific Metrics | Interpretation | Advantages | Limitations |
|---|---|---|---|---|
| Accuracy Metrics | Root Mean Squared Error (RMSE) [14] [5], Mean Absolute Error (MAE) [14], Mean Absolute Percentage Error (MAPE) [2], Correlation Coefficient [2] | Quantitative measure of prediction error | Easy to interpret and compare across models | May not reflect clinical significance |
| Clinical Accuracy Metrics | Clarke Error Grid (CEG) [14], Time in Range (TIR) [67], Time Above Range (TAR), Time Below Range (TBR) [67] | Classification of clinical risk associated with prediction errors | Direct clinical relevance, measures impact on patient outcomes | More complex analysis, may require domain expertise |
| Model Robustness Metrics | Zero-shot prediction performance across patient groups [5], Performance variation across demographics and clinical scenarios [5] | Generalizability to unseen data and populations | Assesses real-world applicability | Requires diverse datasets for evaluation |
Comprehensive validation of CGM forecasting models requires multiple metric categories to assess both numerical accuracy and clinical utility. Recent advances in deep learning for glucose forecasting demonstrate the effectiveness of these multi-metric approaches. Bidirectional LSTM networks with encoder-decoder architectures have shown performance of 19.49 ± 5.42 mg/dL RMSE, 0.43 ± 0.2 correlation coefficient, and 12.34 ± 3.11% MAPE for current glucose level predictions without prior glucose measurements [2]. Transformer-based large sensor models (LSMs) pretrained on massive CGM datasets (15.96 million records from 592 patients) have achieved 48.51% reduction in RMSE for 1-hour horizon forecasting compared to baseline approaches [5].
Clinical Validation of Digital Endpoints
The Regulatory Landscape for Digital Endpoints
The clinical validation of digital endpoints faces significant challenges due to the absence of specific guidelines orienting their validation [63]. While there is global regulatory consensus on using digital devices in clinical trials, only validated digital endpoints will be suitable for supporting safety and efficacy claims in applications to regulatory authorities [63]. The V3 framework, which combines software and clinical development, establishes the foundation for evaluating digital clinical endpoints by defining clinical validation as an evaluation of whether digital endpoints "acceptably identifies, measures or predicts a meaningful clinical, biological, physical, functional state, or experience, in the stated context of use" [63].
Clinical validation typically comprises the assessment of content validity, reliability, and accuracy (validation against a gold standard) and the establishment of meaningful thresholds [63]. This process occurs after both verification and analytical validation processes and is subject to similar principles of research design and statistical analysis as clinical validation of traditional tests, tools, and measurement instruments [63].
Adoption Trends of CGM-Derived Endpoints
Analysis of ClinicalTrials.gov records from 2012-2023 reveals significant trends in the adoption of CGM-derived endpoints [67]:
- There was a significant 60.3% increase in total clinical studies using CGM endpoints from 2012-2017 (121 studies) to 2018-2023 (194 studies) [67].
- Phase 2 and Phase 3 studies saw substantial increases of 125.8% and 169.2%, respectively, in the later period [67].
- Studies using Time in Range (TIR) as an endpoint increased by 222.4% in 2018-2023, while studies using Mean Amplitude of Glycemic Excursions (MAGE) decreased significantly by 71.3% [67].
- Industry-funded studies increased significantly by 78.4% in 2018-2023, though non-industry-funded studies still predominated [67].
These trends reflect growing acceptance of CGM-derived endpoints, particularly following international standardization efforts that began in 2017 [67]. The significant increase in pediatric studies, although smaller in absolute number, is particularly encouraging for expanding evidence generation across diverse populations [67].
Bridging Technical-Clinical Gaps in Validation
A critical challenge in digital endpoint validation lies in bridging the perspective gaps between technical and clinical researchers. A structured survey of professionals working in AI for medical imaging revealed significant differences in validation priorities [64]. While technical groups valued transparency and traceability most highly, clinical groups prioritized explainability [64]. Technical groups showed more comfort with synthetic data for validation and advanced techniques like cross-validation, while clinical groups expressed reluctance toward synthetic data and would benefit from greater exposure to technical validation methods [64].
The FUTURE-AI framework offers guidelines for trustworthy AI in healthcare based on six principles: fairness, universality, traceability, usability, robustness, and explainability [64]. This framework, developed through broad consensus with over 100 collaborators worldwide, provides actionable guidelines covering the entire AI lifecycle from design to deployment and monitoring [64].
Experimental Protocols for Validation Studies
Protocol 1: Technical Validation of CGM Forecasting Models
Purpose: To rigorously validate the performance of CGM forecasting models using temporal cross-validation and comprehensive metrics.
Materials:
- CGM dataset with high temporal resolution (e.g., 5-minute sampling)
- Computational environment with appropriate machine learning libraries
- Implementation of evaluation metrics (RMSE, MAE, Clarke Error Grid)
Procedure:
- Data Preprocessing:
Temporal Splitting:
Model Training:
- For each model architecture, perform hyperparameter optimization using the validation set.
- For transformer-based models, implement pretraining on large CGM datasets using autoregressive training paradigms [5].
- For ridge regression models, tune L2 penalty parameters via validation grid search to minimize RMSE [14].
Rolling-Origin Evaluation:
Performance Assessment:
CGM Forecasting Validation Workflow
Protocol 2: Clinical Validation of Digital Endpoints
Purpose: To establish clinical validity of CGM-derived digital endpoints for regulatory acceptance and clinical adoption.
Materials:
- Validated CGM devices with appropriate regulatory approvals
- Reference standard measures (e.g., HbA1c, OGTT, clinical events)
- Study population representative of intended use context
- Statistical analysis plan with predefined endpoints
Procedure:
- Context of Use Definition:
Study Design:
Endpoint Selection and Definition:
Validation Analyses:
- Assess content validity through literature review and expert input [63].
- Evaluate reliability through test-retest and inter-device consistency [63].
- Establish criterion validity against reference standards where available [63].
- Determine meaningful change thresholds through anchor-based or distribution-based methods [63].
Clinical Meaningfulness Assessment:
Regulatory Documentation:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for CGM Validation Studies
| Category | Item | Specification/Examples | Function in Validation |
|---|---|---|---|
| CGM Datasets | Publicly available datasets | OhioT1DM [14] [5], OpenAPS, RCT, Racial-Disparity [66] | Benchmarking algorithms, testing generalizability |
| Simulation Tools | Physiological simulators | UVA/PADOVA simulator [66] | Generating synthetic CGM data for initial testing |
| Data Augmentation Tools | Data-Augmented Simulation (DAS) framework [66] | Missing data and error models learned from real CGM data | Creating realistic synthetic data with real-world properties |
| Validation Frameworks | Temporal cross-validation implementations | Rolling-origin evaluation [14] | Preventing data leakage in time series validation |
| Analytical Libraries | Functional data analysis tools | Functional principal components analysis [1] | Advanced pattern recognition in CGM trajectories |
| AI/ML Frameworks | Deep learning architectures | LSTM [2], Transformer decoders [5], VAEs [52] | Developing predictive models and handling complex temporal patterns |
| Clinical Endpoint Standards | Consensus guidelines | International CGM consensus guidelines [67] | Standardizing endpoint definitions for regulatory acceptance |
| Statistical Packages | Correlation pattern validation tools | Canonical correlation patterns with L1/L5 norms [65] | Validating clustering of multivariate CGM time series |
Robust validation frameworks for CGM data research require integrated approaches that span technical robustness and clinical relevance. The evolving landscape of CGM data analysis—from traditional summary statistics to functional data analysis and AI-driven approaches—demands equally sophisticated validation strategies that address the unique challenges of temporal glucose data. By implementing rigorous technical validation protocols, including temporal cross-validation and comprehensive performance metrics, and aligning with clinical validation principles through meaningful endpoint definition and regulatory awareness, researchers can generate evidence that advances both scientific understanding and clinical application. As CGM technology continues to evolve and expand into new populations, these validation frameworks will play an increasingly critical role in ensuring that digital endpoints deliver on their promise to transform diabetes research and care.
The accurate prediction of glycemic events, particularly hypoglycemia, is a critical challenge in diabetes management using continuous glucose monitoring (CGM) data. While statistical metrics like Root Mean Squared Error (RMSE) provide general accuracy assessment, they fail to capture the clinical consequences of prediction errors. Consequently, a triad of performance metrics—sensitivity, specificity, and error grid analysis—has emerged as the standard for evaluating the clinical relevance of predictive models in diabetes research. These metrics ensure that algorithms not only make accurate predictions but also generate clinically actionable outputs that can genuinely improve patient outcomes, a consideration paramount when developing feature engineering strategies for CGM time series data.
Core Performance Metrics and Clinical Interpretation
Sensitivity and Specificity in Hypoglycemia Prediction
In the context of hypoglycemia prediction, sensitivity measures the proportion of actual hypoglycemic events that are correctly identified by the model, while specificity measures the proportion of non-hypoglycemic events correctly identified. These metrics directly impact patient safety and device usability: high sensitivity prevents missed alerts for dangerous lows, and high specificity reduces false alarms that lead to "alert fatigue" and device discontinuation [15].
Table 1: Reported Performance of Various Prediction Models for 30-Minute Prediction Horizon
| Model Type | Sensitivity (%) | Specificity (%) | AUC (%) | Data Type | Citation |
|---|---|---|---|---|---|
| Feature-Based ML | >91 | >90 | - | CGM + Insulin/Carb Data | [13] |
| LSTM (Primary) | - | - | >97 | CGM | [15] |
| LSTM (Validation) | - | - | >93 | CGM | [15] |
| Nocturnal (Feature-Based ML) | ~95 | - | - | CGM + Context | [13] |
The performance of predictive models can vary significantly based on the prediction horizon and the inclusion of contextual features. For instance, one study on a feature-based machine learning model reported >91% sensitivity and >90% specificity for both 30- and 60-minute prediction horizons. The inclusion of insulin and carbohydrate data yielded performance improvements for 60-minute predictions but not for 30-minute predictions, highlighting the differential value of feature types based on context [13]. Furthermore, model performance was highest for nocturnal hypoglycemia, achieving approximately 95% sensitivity [13].
Recent advances in deep learning models, specifically Long Short-Term Memory (LSTM) networks, have demonstrated exceptional generalizability across populations and diabetes subtypes. One study showed LSTM models achieving Area Under the Curve (AUC) values greater than 97% for mild hypoglycemia prediction on a primary dataset, with less than a 3% AUC reduction when validated on an independent dataset of different ethnicity [15]. This robustness is crucial for the real-world deployment of algorithms developed from specific CGM feature sets.
Error Grid Analysis
Error Grid Analysis (EGA), particularly in its continuous form (CG-EGA), moves beyond point accuracy to assess the clinical accuracy of glucose predictions by evaluating both point precision and the accuracy of the predicted rate of change [68]. Unlike traditional metrics, CG-EGA categorizes errors based on their potential to cause adverse clinical outcomes.
Table 2: Zones of Continuous Glucose Error-Grid Analysis (CG-EGA) and Their Clinical Significance
| Zone | Description | Clinical Impact |
|---|---|---|
| A | Clinically Accurate Prediction | Predictions are sufficiently accurate to make correct clinical decisions. |
| B | Benign Errors | Deviations are not likely to lead to clinically inappropriate treatment actions. |
| C | Overcorrection | Predictions may lead to unnecessary corrections, potentially resulting in opposite glycemic excursions. |
| D | Failure to Detect | Dangerous failure to detect a significant glucose excursion, leading to a failure to treat. |
| E | Erroneous Reading | Predictions would lead to confusing treatment actions and potentially dangerous consequences. |
CG-EGA provides a structured framework to evaluate the clinical risks of prediction inaccuracies. For example, a study assessing ARIMA and polynomial prediction models using CG-EGA found that the majority of predicted-measured glucose pairs fell in the accurate AR and BR zones, confirming very good clinical agreement. The autoregressive (AR) model was found to be preferable for hypoglycemia prevention, as it resulted in fewer points in the "failure to detect" (DP) zone compared to the polynomial model [68]. This granular analysis is invaluable for selecting and optimizing algorithms for specific clinical applications, such as hypoglycemia prevention versus general trend forecasting.
Experimental Protocols for Metric Evaluation
Protocol 1: Evaluating Hypoglycemia Prediction Performance
This protocol outlines a standardized procedure for assessing the sensitivity and specificity of a model in predicting hypoglycemic events.
Objective: To quantitatively evaluate a model's capability to correctly classify impending hypoglycemic events within a specified prediction horizon.
Materials and Reagents:
- CGM Dataset: A time-series dataset of interstitial glucose measurements with 5-15 minute sampling intervals (e.g., from studies using Dexcom G6 or Medtronic MiniMed devices) [13] [15].
- Reference Standard: Self-Monitored Blood Glucose (SMBG) measurements or CGM values confirmed by a reference method for calculating the Mean Absolute Relative Difference (MARD) to ensure data quality. Data with MARD >15% should be filtered out [15].
- Computing Environment: Software for machine learning and statistical analysis (e.g., Python with scikit-learn, TensorFlow, or R).
Procedure:
- Data Preprocessing:
- Resample the raw CGM data to ensure strict 5-minute intervals.
- Handle missing data via linear interpolation for gaps ≤30 minutes. For longer gaps, segment the data, discarding segments shorter than 6 hours (e.g., 72 data points) to maintain data integrity [14] [15].
- Split the dataset chronologically into training, validation, and test sets to prevent data leakage. A typical ratio is 7:1.5:1.5 for training, development, and test sets, respectively [15].
Event and Prediction Labeling:
- Define a hypoglycemic event as a glucose value <70 mg/dL (mild) or <54 mg/dL (severe), in accordance with international consensus [15].
- For each CGM timestamp
t, the true label is1(positive) if the glucose value att + PH(where PH is the Prediction Horizon, e.g., 30 or 60 minutes) is in the hypoglycemic range; otherwise, it is0(negative).
Model Training and Prediction:
- Train the predictive model (e.g., LSTM, Random Forest, SVM) using the training set.
- Generate probabilistic predictions for the test set. A prediction is classified as positive if the output probability exceeds a predefined threshold (e.g., 0.5).
Performance Calculation:
- Construct a confusion matrix comparing the true labels and the predicted labels.
- Calculate Sensitivity = TP / (TP + FN) and Specificity = TN / (TN + FP), where TP is True Positive, TN is True Negative, FP is False Positive, and FN is False Negative.
- Vary the classification threshold to generate a Receiver Operating Characteristic (ROC) curve and calculate the Area Under the Curve (AUC).
Diagram 1: Hypoglycemia Prediction Performance Evaluation Workflow
Protocol 2: Conducting Continuous Glucose Error-Grid Analysis (CG-EGA)
This protocol details the application of CG-EGA to assess the clinical accuracy of predicted glucose profiles.
Objective: To evaluate the clinical risks associated with discrepancies between predicted and reference glucose values and their rates of change.
Materials and Reagents:
- Predicted Glucose Profiles: Time-series data of glucose values generated by the model under evaluation.
- Reference Glucose Profiles: Corresponding time-series of measured CGM or blood glucose values used as the ground truth.
- CG-EGA Algorithm: Implementation of the CG-EGA methodology as described in the literature [68].
Procedure:
- Data Alignment:
- Temporally align the predicted and reference glucose profiles.
Point Error-Grid Analysis (P-EGA):
- For each paired data point (reference, prediction), plot it on the point error-grid.
- Categorize each point into one of the zones (A, B, C, D, E) based on its coordinates and the predefined grid boundaries.
Rate Error-Grid Analysis (R-EGA):
- Calculate the rate of change (mg/dL/min) for both the reference and predicted profiles over a specified time window.
- Plot the paired rates of change (reference rate, prediction rate) on the rate error-grid.
- Categorize each rate pair into one of the zones (AR, BR, CR, DR, ER).
Combined Analysis and Reporting:
- Merge the results of the P-EGA and R-EGA to perform the final CG-EGA.
- Report the percentage of data points falling into each zone, separately for the hypoglycemic (<70 mg/dL), euglycemic (70-180 mg/dL), and hyperglycemic (>180 mg/dL) ranges.
- A clinically acceptable prediction system should have the vast majority of its points (e.g., >99%) in the clinically accurate (A/AR) and benign (B/BR) zones [68].
Diagram 2: Continuous Glucose Error-Grid Analysis (CG-EGA) Protocol
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for CGM Feature Engineering and Model Evaluation
| Item / Reagent | Function / Application | Example & Notes |
|---|---|---|
| CGM Datasets | Provides the foundational time-series data for feature extraction and model training/validation. | OhioT1DM [14], Datasets from clinical studies using Dexcom G6 [13] or Medtronic MiniMed [15]. Ensure datasets include demographic and contextual data. |
| Reference Glucose Measurements | Serves as the ground truth for calculating accuracy metrics (MARD) and for CG-EGA. | Self-Monitored Blood Glucose (SMBG) measurements [15]. Required for data quality filtering. |
| Feature Engineering Library | Computational tools to generate a comprehensive set of features from raw CGM traces. | Custom code to extract short-term (e.g., diff_10, slope_1hr), medium-term (e.g., sd_4hr), and long-term features (e.g., rebound_lows) as defined in research [13]. |
| Machine Learning Frameworks | Environment for developing, training, and testing predictive models. | TensorFlow/PyTorch (for LSTM [15]), scikit-learn (for Ridge Regression [14], SVM, Random Forest [15]). |
| CG-EGA Implementation | Specialized software script or package to perform Continuous Glucose Error-Grid Analysis. | Code implementing the methodology from Kovatchev et al. [68] to categorize point and rate errors. |
| Statistical Analysis Software | Used for calculating performance metrics, statistical testing, and generating visualizations. | R, Python (with pandas, scipy), SPSS. Used for metrics like Sensitivity/Specificity and Diebold-Mariano tests [14]. |
The management and therapeutic development for metabolic diseases like diabetes have been fundamentally transformed by the advent of Continuous Glucose Monitoring (CGM). These devices generate high-frequency time-series data, presenting unprecedented opportunities for feature engineering to extract clinically meaningful information [69] [1]. This application note provides a structured comparison between traditional and novel feature sets derived from CGM data, offering experimental protocols and analytical frameworks tailored for research and drug development applications.
The evolution from "CGM Data Analysis 1.0" (traditional summary statistics) to "CGM Data Analysis 2.0" (advanced functional and artificial intelligence-based methods) represents a paradigm shift in how glycemic data is utilized for both clinical management and research endpoints [1]. This comparative analysis details the methodological frameworks, validation protocols, and practical implementation pathways for leveraging these feature sets in therapeutic development.
Table 1 summarizes the core characteristics, advantages, and limitations of traditional and novel feature sets for CGM data analysis.
Table 1: Fundamental Characteristics of Traditional vs. Novel CGM Feature Sets
| Aspect | Traditional Feature Sets | Novel Feature Sets |
|---|---|---|
| Core Philosophy | Summary statistics capturing amplitude of glucose excursions [1] | Comprehensive capture of temporal dynamics and distributional patterns [69] [1] |
| Primary Features | Mean glucose, time-in-range (TIR), coefficient of variation (CV), glucose management indicator (GMI) [1] | Glucodensity, glucose velocity/acceleration, chronobiological patterns, machine learning-derived motifs [69] [3] [70] |
| Data Utilization | Aggregated metrics; ignores temporal sequence [70] | Uses full temporal structure and dynamics of the time series [69] [1] |
| Clinical Interpretation | Simple, well-established, intuitive [1] [71] | Complex, requires specialized expertise; offers deeper physiological insights [69] [1] |
| Key Limitations | Oversimplifies complex patterns; misses critical dynamics [69] [1] | Computationally intensive; requires validation in diverse populations [69] [1] |
Quantitative Performance Comparison
Validation studies demonstrate the superior predictive capability of novel feature sets for long-term glycemic outcomes. Table 2 quantifies the performance gains of novel features in forecasting established glycemic biomarkers.
Table 2: Predictive Performance of Feature Sets for Long-Term Glycemic Outcomes
| Predictor Feature Set | Outcome Biomarker | Prediction Horizon | Performance Gain (vs. Traditional) | Key Metrics Extracted |
|---|---|---|---|---|
| Glucodensity with Speed/Acceleration [69] | HbA1c | 8 years | >20% increase in adjusted R² [69] | Full glucose distribution, rate of change (mg/dL/min), acceleration (mg/dL/min²) |
| Glucodensity with Speed/Acceleration [69] | Fasting Plasma Glucose | 5 years | >20% increase in adjusted R² [69] | Full glucose distribution, rate of change (mg/dL/min), acceleration (mg/dL/min²) |
| Chronobiologically-Informed Features [3] | Next-Day Glycemic Dysregulation | 1 day | Improved XGBoost prediction vs. time-series statistics alone [3] | Time-of-Day Standard Deviation (ToDSD), multi-timescale complexity |
| Functional Data Patterns [1] | Phenotype Classification | N/A | Identifies distinct subphenotypes with different pathophysiologies [1] | Nocturnal patterns, postprandial response curves, weekday-weekend variability |
Detailed Experimental Protocols
Protocol 1: Validating Novel Features Against Long-Term Outcomes
This protocol is based on the AEGIS study analysis that demonstrated the value of dynamic glucodensity features [69].
4.1.1 Research Reagent Solutions Table 3: Essential Materials and Reagents for CGM Feature Validation
| Item Name | Specification / Function |
|---|---|
| CGM Device | Dexcom G7 or equivalent; measures interstitial glucose every 5-15 min [2] [72]. |
| Data Extraction Software | Manufacturer-specific software (e.g., Dexcom CLARITY, LibreView) for raw data export [73]. |
| Computational Environment | R or Python with specialized packages: iglu (for AGP), fda (for functional data analysis) [73]. |
| Validation Assays | HbA1c (HPLC method), Fasting Plasma Glucose (hexokinase method) for ground-truth correlation [69]. |
4.1.2 Step-by-Step Methodology
Subject Recruitment & Data Collection:
- Enroll a cohort of sufficient size (e.g., n>1000) with representation across glycemic states (normoglycemic, prediabetic, diabetic) [69].
- Collect baseline CGM data for a minimum of 14 days under free-living conditions to capture typical glucose fluctuations [3].
- Collect outcome biomarkers (HbA1c, FPG) at baseline and at predefined follow-up intervals (e.g., 5 and 8 years) [69].
Feature Extraction:
- Traditional Features: Compute standard metrics: Mean Glucose, %TIR (70-180 mg/dL), %Time Above Range (>180 mg/dL), %Time Below Range (<70 mg/dL), Coefficient of Variation (CV) [1].
- Novel Glucodensity Features:
- Marginal Glucodensity: Estimate the probability density function of all CGM readings using kernel density estimation [69].
- Glucose Speed (1st Derivative): Calculate the instantaneous rate of glucose change between consecutive measurements (mg/dL/min) [69].
- Glucose Acceleration (2nd Derivative): Calculate the rate of change of glucose speed (mg/dL/min²) [69].
Predictive Modeling & Validation:
- Construct multiple linear regression models to predict future HbA1c and FPG.
- Model A: Use only traditional CGM features and non-CGM covariates (e.g., age, BMI).
- Model B: Use traditional features + novel glucodensity, speed, and acceleration features.
- Compare model performance using adjusted R², Akaike Information Criterion (AIC), and cross-validation error. The significant increase in adjusted R² for Model B demonstrates the information gain of novel features [69].
The following diagram illustrates the logical workflow and computational steps for this protocol:
Protocol 2: Implementing Pattern Recognition with Machine Learning
This protocol outlines the process for identifying glucose fluctuation patterns using machine learning, which can reveal subphenotypes relevant for personalized drug development [70].
4.2.1 Step-by-Step Methodology
Data Preparation and Segmentation:
- Obtain CGM data from a large cohort (e.g., >100 patients with >1 million measurements) [70].
- Segment the continuous time series into discrete, non-overlapping windows (e.g., 2-hour segments) for pattern analysis.
Pattern Discovery and Clustering:
- Apply a pattern recognition algorithm (e.g., Dynamic Time Warping - DTW) to quantify the similarity between all pairs of glucose segments [70].
- Use DTW distances as input for a clustering algorithm (e.g., k-means, hierarchical clustering) to group similar glucose trajectories.
- Identify the centroid of each cluster as a representative "glucose fluctuation pattern." Studies have validated the existence of approximately 6 distinct patterns [70].
Feature Engineering: Time-in-Pattern:
- For each patient, calculate the percentage of time their glucose profile follows each of the identified patterns, creating a "Time-in-Pattern" (TIP) profile [70].
Phenotype Association and Validation:
- Use the TIP profiles as input for a second round of clustering to identify distinct patient subgroups (e.g., 4 clusters) [70].
- Validate the clinical relevance of these novel subgroups by comparing their standard clinical characteristics (e.g., HbA1c, diabetes duration, complication rates) using statistical tests (ANOVA, chi-square). Significant differences confirm that TIP profiles capture biologically and clinically meaningful variation [70].
The Scientist's Toolkit: Research Reagent Solutions
Table 4 provides a detailed list of essential tools, computational packages, and data sources required for implementing the described CGM feature engineering protocols.
Table 4: Essential Research Toolkit for CGM Feature Engineering
| Tool / Reagent Category | Specific Examples & Specifications | Primary Function in Research |
|---|---|---|
| CGM Devices & Data Access | Dexcom G7, Abbott FreeStyle Libre, Medtronic Guardian [2] [72] | Generate raw, high-frequency (e.g., 5-15 min) interstitial glucose time series data for analysis. |
| Data Export & Standardization Platforms | Dexcom CLARITY API, Abbott LibreView, Glooko [73] | Access standardized data exports and Ambulatory Glucose Profile (AGP) reports in a consistent format. |
| Computational Libraries (R) | iglu (for CGM metrics), fda (functional data analysis), dbscan (clustering) [73] |
Calculate established metrics, perform functional data analysis, and implement unsupervised clustering. |
| Computational Libraries (Python) | scikit-learn (ML), PyTorch/TensorFlow (DL), PyEMD (empirical mode decomposition) [28] [2] |
Build machine learning models, deep learning networks (e.g., LSTMs), and extract complex, non-linear features. |
| Validation Biomarkers | HbA1c (HPLC method), Fasting Plasma Glucose (enzymatic assay), Oral Glucose Tolerance Test (OGTT) [69] [28] | Provide gold-standard measures of glycemic health for validating and correlating novel CGM-derived features. |
The comparative evidence indicates that novel feature sets, particularly those capturing the functional and dynamic properties of glucose profiles, provide a substantial information gain over traditional summary metrics. The integration of glucodensity, speed, acceleration, and machine learning-derived patterns offers a more granular view of glycemic physiology, making them powerful tools for refining patient stratification, developing personalized therapeutic interventions, and creating sensitive endpoints for clinical trials in drug development [69] [1] [70].
For researchers, the initial investment in mastering functional data analysis and machine learning techniques is justified by the ability to uncover latent subphenotypes and predict long-term outcomes with greater accuracy. The provided protocols offer a concrete starting point for implementing these advanced analytical methods in both academic and industry settings.
The diagnosis of type 2 diabetes (T2D) and prediabetes based solely on static glucose thresholds fails to capture the significant pathophysiological heterogeneity underlying glucose dysregulation [31] [33]. This heterogeneity is primarily driven by varying contributions of muscle insulin resistance (IR), hepatic IR, β-cell dysfunction, and impaired incretin action [31] [74]. Identifying these distinct metabolic subphenotypes is crucial for advancing precision medicine in diabetes care, as they may respond differently to targeted therapies and lifestyle interventions [33].
Recent research demonstrates that continuous glucose monitoring (CGM) data, particularly when combined with machine learning, can non-invasively identify these metabolic subphenotypes by analyzing the dynamic "shape of the glucose curve" during standardized tests like the oral glucose tolerance test (OGTT) [31] [33]. This case study examines the validation of feature engineering approaches for CGM time series data to accurately classify metabolic subphenotypes in individuals with early glucose dysregulation.
Background and Significance
Limitations of Current Diabetes Classification
Traditional classification of diabetes into type 1, type 2, and other specific forms does not account for the physiological heterogeneity within T2D [33]. Current diagnosis relies on glucose cutoffs without regard to the mechanism that led to the elevation, despite knowledge that multiple pathophysiological pathways contribute to glucose elevation [33]. This oversimplified approach fails to predict differential risks for complications or variable treatment responses among individuals classified under the same diagnostic category [33].
Metabolic Heterogeneity in Early Dysglycemia
Gold-standard metabolic testing has revealed that individuals with normoglycemia or prediabetes exhibit diverse combinations of physiological defects [31]. Research shows that among those with early glucose dysregulation, approximately 34% exhibit dominance or co-dominance in muscle and/or liver IR, while 40% exhibit dominance or co-dominance in β-cell dysfunction and/or incretin deficiency [31] [74]. This heterogeneity exists even among individuals with similar HbA1c or fasting glucose levels, highlighting the inadequacy of current diagnostic approaches [31].
Experimental Design and Methodologies
Cohort Characteristics and Study Design
The foundational research for metabolic subphenotyping utilized multiple cohorts to develop and validate machine learning models [31]. The study design incorporated:
- Initial Training Cohort: 32 participants who completed all metabolic tests in a clinical translational research unit (CTRU)
- Independent Validation Cohort: 24 separately recruited participants
- At-Home CGM Cohort: 29 participants (5 from initial cohort and 24 from validation cohort) who underwent at-home OGTTs using CGM
Participants were enrolled without history of diabetes and with fasting plasma glucose <126 mg/dl, classified as having normoglycemia (n=33) or prediabetes (n=21), plus 2 with T2D according to American Diabetes Association HbA1c criteria [31]. The cohorts were well-matched with an average age of 55 years, BMI of 26 kg/m², relatively equal male/female sex ratio, and average HbA1c of 5.6% [31].
Gold-Standard Metabolic Phenotyping
Comprehensive physiological characterization was performed using rigorous, gold-standard metabolic tests to quantify four key pathological processes [31]:
- Muscle Insulin Resistance: Measured by modified insulin-suppression test (IST) and expressed as steady-state plasma glucose (SSPG). Participants were categorized as insulin sensitive (IS) if SSPG was <120 mg/dl and insulin resistant (IR) if SSPG was ≥120 mg/dl [31].
- β-cell Dysfunction: Insulin secretion rate (ISR) quantified with C-peptide deconvolution during a 3-hour OGTT with adjustment for IR via calculation of the disposition index (ISR/SSPG) [33].
- Impaired Incretin Action: Quantified by calculating relative insulin secretion during OGTT versus isoglycemic intravenous glucose infusion (IIGI) [33].
- Hepatic Insulin Resistance: Inferred by a validated index derived from metabolic testing [33].
OGTT Protocols and CGM Data Acquisition
Clinical Research Unit OGTT
Participants underwent a frequently-sampled OGTT in the CTRU with plasma glucose measurements at 5-15 minute intervals (16 timepoints) for 180 minutes following administration of a 75-g oral glucose load under highly standardized conditions [31]. This dense sampling effectively created a "CGM-like" assessment in the research setting [33].
At-Home CGM OGTT
For the at-home component, participants wore a CGM device while performing OGTTs at home, completing a minimum of two tests [31]. This design enabled comparison of concordance between home CGMs, CTRU CGM, and CTRU plasma values during OGTT [31].
Data Pre-processing and Quality Control
Proper data pre-processing was essential for ensuring data quality before feature extraction:
- Missing Data Handling: Missing CGM data points were interpolated using the spline method only if fewer than 3 consecutive CGM data points were missing [40].
- Device Calibration: CGM measurements were taken every 5 minutes, with missing data reported when the device failed its calibration process [40].
- Postprandial Period Definition: CGM data points were analyzed after meal announcements using the representation:
CGM_i,j,t = CGM_i(meal_i,j + 5×t)wheremeal_i,jis the time of the jth meal announcement, and W is the postprandial period [40].
Feature Engineering Framework
Comprehensive Feature Extraction
The machine learning framework utilized features extracted from the dynamic patterns of glucose time series during OGTTs. Two main feature extraction approaches were employed: "OGTTGFeatures," encompassing 14 distinct metrics, and comprehensive feature sets from CGM data [33].
Table 1: Categories of Features Extracted from Glucose Time Series
| Category | Number of Features | Key Examples | Physiological Correlation |
|---|---|---|---|
| Time in Ranges (TIR) | Customizable | Time in hypoglycemia, normoglycemia, hyperglycemia | Overall glycemic control |
| Descriptive Statistics | Multiple | Mean, minimum, maximum, quantiles | Average glucose exposure |
| Glucose Risk Metrics | Multiple | Low and high blood glucose index | Extreme glucose events risk |
| Glycemic Variability | Multiple | Standard deviation, slope, rate of change | Glucose stability and fluctuations |
| Pattern-based Features | Multiple | Rebounds, spikes, curve shape metrics | Underlying physiological processes |
| Postprandial Dynamics | Multiple | Rate of increase in glucose (RIG), glucose rate of change (GRC) | Meal response physiology |
Key Feature Definitions and Calculations
Rate of Increase in Glucose (RIG)
The RIG feature quantifies the rate of glucose increase from a meal to a peak, calculated as [40]:
Where CGM_i,j,peak_t is the highest CGM data point between the meal announcement and prediction time t, CGM_i,j,0 is the CGM data point at the meal announcement, and TD_meal-to-peak is the time difference between the meal announcement and the peak [40]. If no peak CGM data point is identified, RIG is set to 0 [40].
Glucose Rate of Change (GRC)
The GRC captures near-instantaneous changes in CGM data points around the time of prediction, calculated as [40]:
This feature is particularly valuable for predicting rapid glucose transitions, such as those leading to hypoglycemic events [40].
Advanced Variability Features
Additional features extracted for comprehensive characterization included [13]:
- Short-term features: Differences between current CGM observation and values 10, 20, and 30 minutes earlier; slope over 1 hour
- Medium-term features: Standard deviation of CGM values over 2 and 4 hours; slope over 2 hours
- Long-term features: Percentage of time below 70 mg/dL and above 200 mg/dL; rebound patterns
- Snowball effect features: Cumulative positive and negative glucose changes over 2 hours
Computational Tools and Libraries
The field has benefited from specialized computational tools designed specifically for glucose time series analysis. The GlucoStats Python library represents a significant advancement, offering [12]:
- Comprehensive Feature Extraction: Capability to compute 59 distinct statistics from glucose data
- Parallel Processing: Efficient handling of large CGM datasets through distributed computations
- Temporal Windowing: Analysis of time series divided into smaller segments for detailed temporal analysis
- Scikit-learn Compatibility: Seamless integration into machine learning pipelines
- Visualization Tools: Generation of intuitive, high-quality visualizations for pattern recognition
Machine Learning Framework and Validation
Model Development and Training
The machine learning framework was trained using glucose time series from OGTTs performed in the CTRU [31]. The models utilized features extracted from the 16-point plasma glucose curves to predict the underlying metabolic subphenotypes identified through gold-standard testing [31].
Performance Metrics and Validation
The predictive models demonstrated exceptional accuracy in identifying specific metabolic subphenotypes [31] [74]:
Table 2: Performance of Machine Learning Models in Predicting Metabolic Subphenotypes
| Metabolic Subphenotype | Training Cohort AUC (Plasma OGTT) | Validation Cohort AUC (At-Home CGM) | Prevalence in Early Dysglycemia |
|---|---|---|---|
| Muscle Insulin Resistance | 95% | 88% | 34% (muscle or hepatic IR) |
| β-cell Deficiency | 89% | 84% | 40% (β-cell or incretin deficiency) |
| Impaired Incretin Action | 88% | Not reported | Part of 40% prevalence above |
The models maintained strong performance when applied to CGM-generated glucose curves obtained during at-home OGTTs, with AUCs of 88% for muscle insulin resistance and 84% for β-cell deficiency [31] [32]. This demonstrates the feasibility of at-home subphenotyping using accessible CGM technology.
Comparative Performance Against Traditional Metrics
The glucose time-series features significantly outperformed currently-used estimates for identifying underlying physiological defects [74]. The prediction accuracy exceeded that of traditional glycemic measures like HbA1c, fasting glucose, HOMA indices, and genetic risk scores [31].
Visualization of Research Workflows
Experimental Workflow for Metabolic Subphenotyping
Feature Engineering Pipeline
Feature Engineering Pipeline for CGM Data
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Computational Tools for CGM-Based Metabolic Subphenotyping
| Tool/Category | Specific Examples | Function/Application | Implementation Considerations |
|---|---|---|---|
| CGM Devices | Dexcom G6, Abbott FreeStyle Libre | Continuous glucose monitoring in ambulatory settings | Sensor accuracy, calibration requirements, data accessibility |
| Data Processing Libraries | GlucoStats (Python), cgmanalysis (R), iglu (R) | Feature extraction from raw CGM data | Parallel processing capabilities, supported metrics, visualization options |
| OGTT Materials | 75-g glucose load, standardized protocols | Provocative testing for glucose response | Administration timing, fasting requirements, sample collection intervals |
| Gold-Standard Validation Tests | Modified insulin-suppression test (SSPG), Isoglycemic IV glucose infusion | Reference measurements for metabolic subphenotypes | Labor intensity, cost, specialized equipment requirements |
| Machine Learning Frameworks | Scikit-learn, TensorFlow, PyTorch | Model development and validation | Integration with feature extraction pipelines, hyperparameter optimization |
| Statistical Analysis Tools | R, Python (Pandas, NumPy, SciPy) | Data manipulation and statistical testing | Reproducibility, documentation, community support |
Discussion and Future Directions
Clinical Implications and Applications
The ability to identify metabolic subphenotypes using CGM and machine learning has significant implications for precision medicine in diabetes prevention and treatment [31] [33]. This approach enables:
- Targeted Interventions: Matching therapeutics to underlying physiology (e.g., insulin sensitizers for muscle IR, GLP-1 agonists for β-cell dysfunction) [31]
- Personalized Nutrition: Utilizing individual postprandial glycemic responses to specific foods as biomarkers for metabolic subtype [33]
- Lifestyle Optimization: Tailoring exercise and dietary timing based on predominant metabolic defects [33]
Methodological Considerations and Limitations
While promising, this approach has several methodological considerations:
- Data Quality: Reliable subphenotyping requires high-quality CGM data with minimal missing values [40]
- Standardization: OGTT protocols must be standardized for valid comparisons across individuals and studies [31]
- Algorithm Validation: Models require validation in diverse populations to ensure generalizability [31] [75]
- Computational Resources: Efficient processing of high-frequency CGM data necessitates appropriate computational infrastructure [12]
Future Research Directions
Future work should focus on:
- Longitudinal Validation: Tracking subphenotype stability and progression over time [33] [75]
- Integration with Multi-omics: Combining CGM data with genetic, proteomic, and microbiome data [75]
- Intervention Studies: Testing whether subphenotype-guided therapy improves outcomes [31]
- Automated Real-Time Classification: Developing systems for continuous metabolic phenotyping [13]
This case study demonstrates that feature engineering from CGM time series data, combined with machine learning, can effectively identify metabolic subphenotypes in individuals with early glucose dysregulation. The validated features extracted from glucose curves during OGTTs accurately predicted muscle insulin resistance, β-cell deficiency, and impaired incretin action with high accuracy, outperforming traditional glycemic metrics.
The approach presents a scalable, minimally invasive method for metabolic subphenotyping that could be deployed in at-home settings using commercially available CGM devices. This advancement paves the way for precision medicine approaches in diabetes prevention and treatment, potentially enabling targeted interventions matched to an individual's underlying physiological defects.
As CGM technology continues to evolve and computational methods become more sophisticated, the validation of features for metabolic subphenotyping represents a critical step toward personalized diabetes care that addresses the fundamental heterogeneity of this complex metabolic disorder.
Benchmarking Against Non-Invasive Biomarkers from Wearable Data
The expanding ecosystem of wearable biosensors has created unprecedented opportunities for continuous health monitoring, particularly in diabetes management. Within this landscape, benchmarking continuous glucose monitoring (CGM) time series data against emerging non-invasive biomarkers represents a critical methodological frontier for researchers and drug development professionals. Traditional CGM systems, while providing valuable continuous data through minimally invasive subcutaneous sensors, now face competition from completely non-invasive technologies that measure glucose and other metabolic parameters through alternative bodily fluids and optical techniques [76].
Effective feature engineering for CGM time series data increasingly requires understanding how these traditional metrics correlate with and can be validated against non-invasive biomarker readings. This protocol establishes comprehensive benchmarking methodologies to evaluate the relationship between standard CGM-derived features and non-invasive biomarker data, with particular emphasis on photoplethysmography (PPG), sweat-based biosensors, and mid-infrared spectroscopy approaches [77] [78] [79]. The framework addresses key validation challenges including temporal alignment, signal processing techniques, and statistical measures appropriate for multimodal physiological data streams.
Current Landscape of Non-Invasive Glucose Monitoring Technologies
Technology Comparison and Performance Metrics
Table 1: Non-Invasive Glucose Monitoring Technologies and Performance Characteristics
| Technology Platform | Biosample Source | Key Biomarkers | Reported Accuracy | Research Status |
|---|---|---|---|---|
| Photoplethysmography (PPG) | Blood volume changes | Glucose-induced optical variations | RMSE: 19.7 mg/dL [77] | Clinical validation |
| Mid-infrared (MIR) spectroscopy | Dermal interstitial fluid | Uric acid, albumin, ketone bodies [78] | Lab-grade sensitivity demonstrated [78] | Prototype development |
| Sweat-based biosensors | Sweat | Glucose, electrolytes, metabolites [79] | Correlation with blood glucose: r=0.89-0.94 [79] | Early commercial deployment |
| Reverse iontophoresis | Interstitial fluid | Glucose | MARD: 11.4% (Libre Pro) [80] | FDA-approved systems available |
| Breath analysis | Exhaled breath | Acetone, volatile organic compounds [76] | Clinical acceptance: 100% (A+B zones) [77] | Research and development |
Market Adoption and Research Activity
The AI-enabled non-invasive biomarker sensors market demonstrates significant growth, with wearable biosensors and smartwatches capturing 40% market share in 2024. Metabolic biomarkers dominate the application landscape with 35% market share, reflecting the emphasis on glucose monitoring and diabetes management technologies [81]. North America currently leads in market adoption (40% share), though Asia Pacific shows the fastest growth rate, indicating expanding research capabilities and clinical validation activities across global regions [81].
Experimental Protocols for Benchmarking Studies
Cross-Modal Biomarker Validation Framework
This protocol establishes a standardized methodology for benchmarking CGM-derived features against non-invasive biomarker readings from wearable devices.
Equipment and Software Requirements
Table 2: Essential Research Reagent Solutions and Materials
| Item Category | Specific Products/Models | Function in Benchmarking |
|---|---|---|
| Reference CGM System | Dexcom G6 Pro, FreeStyle Libre Pro [80] | Provides standardized glucose metrics for validation |
| Non-Invasive Sensors | Empatica E4, Zephyr BioHarness 3 [82] | Captures PPG and other physiological signals |
| Data Acquisition Platform | MindWare systems, Custom Python scripts [82] | Synchronizes multi-modal data streams |
| Analysis Software | GlucoStats Python library, scikit-learn [83] | Extracts features and performs statistical analysis |
| Calibration Solutions | Factory-calibrated sensor solutions [80] | Maintains measurement accuracy across devices |
Participant Selection and Study Design
- Sample Size: Minimum of 20 participants with diabetes to ensure statistical power, consistent with validation studies in the field [76]
- Inclusion Criteria: Adults aged 18-75 with diagnosed type 1 or type 2 diabetes, stable medication regimen for 4 weeks prior to study
- Exclusion Criteria: Severe dermatological conditions, cardiovascular instability, pregnancy
- Study Duration: Minimum 14-day monitoring period to capture glycemic variability [80]
- Data Collection Points: Simultaneous CGM and non-invasive measurements under fasting, postprandial (1-2 hours after meals), and nocturnal conditions
Data Collection and Synchronization Procedures
Sensor Deployment: Apply CGM sensors according to manufacturer specifications, typically in abdominal or upper arm regions. Deploy non-invasive sensors (PPG on wrist, MIR spectroscopy on alternate sites) ensuring no mechanical interference between devices.
Temporal Alignment: Implement synchronous time-stamping across all devices using Network Time Protocol (NTP) synchronization with millisecond precision. Record all data streams at highest available sampling frequency (e.g., every 5 minutes for CGM, 1-10 seconds for PPG) [77].
Contextual Data Logging: Document meal timing, carbohydrate intake, insulin administration, physical activity, and sleep patterns using standardized digital diaries. This contextual information is essential for interpreting discordant readings between measurement modalities.
Signal Processing and Feature Extraction Pipeline
Data Preprocessing Workflow
Signal Quality Assessment: Implement automated quality checks using signal-to-noise ratio thresholds and artifact detection algorithms. For PPG signals, apply pulse quality indices to exclude corrupted segments [82].
Temporal Alignment: Address physiological lag between blood glucose and interstitial fluid glucose (approximately 5-15 minutes) using dynamic time warping (DTW) or cross-correlation techniques [82]. Align non-invasive biomarker readings accounting for device-specific processing delays.
Data Imputation: Apply appropriate missing data handling strategies (linear interpolation for short gaps <15 minutes; marker-based imputation for longer gaps due to sensor failure).
Comprehensive Feature Extraction
Table 3: CGM Feature Categories for Cross-Modal Benchmarking
| Feature Category | Number of Metrics | Key Examples | Relevance to Non-Invasive Validation |
|---|---|---|---|
| Time in Ranges (TIRs) | 8 | % time in 70-180 mg/dL, % time <70 mg/dL | Fundamental clinical endpoints |
| Descriptive Statistics (DSs) | 12 | Mean glucose, SD, coefficient of variation | Core variability measures |
| Glucose Risks (GRs) | 9 | Hypoglycemia risk index, LBGI, HBGI | Safety correlation assessment |
| Glycemic Control (GC) | 11 | Glucose management indicator (GMI) | Treatment efficacy markers |
| Glucose Variability (GV) | 14 | Mean amplitude of glycemic excursions (MAGE) | Dynamic response correlation |
| Pattern-based Features | 5 | Rebound highs/lows, snowball effect [13] | Complex physiological responses |
The GlucoStats library provides a standardized implementation for extracting 59 CGM metrics across these categories, with parallel processing capabilities for efficient large-scale analysis [83]. For non-invasive PPG signals, feature extraction should include both time-domain (pulse rate variability, amplitude fluctuations) and frequency-domain characteristics (power spectral density) that may correlate with glucose dynamics [77].
Statistical Framework for Benchmarking Analysis
Correlation and Similarity Assessment
The benchmarking methodology employs a multi-faceted statistical approach to evaluate agreement between CGM-derived features and non-invasive biomarker readings:
Temporal Similarity Measures: Apply elastic similarity measures including Dynamic Time Warping (DTW) and Fréchet distance to account for physiological lags and non-linear relationships between signals [82]. DTW addresses temporal misalignment by finding the optimal alignment between two time series before similarity computation.
Correlation Statistics: Implement Pearson's correlation for linear relationships, Spearman's rank correlation for monotonic associations, and Maximum Information Coefficient (MIC) to detect non-linear dependencies between CGM features and non-invasive biomarkers [82].
Clinical Accuracy Metrics: Utilize standardized clinical accuracy measures including:
- Clarke Error Grid Analysis (CEGA) to determine clinical significance of deviations
- Mean Absolute Relative Difference (MARD) for overall accuracy assessment
- Root Mean Square Error (RMSE) for magnitude of deviations
Cross-Condition Performance Validation
To assess robustness of correlations across varying physiological conditions:
Stratified Analysis: Evaluate benchmarking metrics separately for different glycemic ranges (hypoglycemic, euglycemic, hyperglycemic), temporal periods (nocturnal, postprandial, fasting), and activity states (rest, exercise, recovery).
Generalizability Testing: Validate correlations across participant subgroups defined by age, diabetes type, BMI, and skin characteristics that may affect sensor performance [76].
Contextual Factor Impact: Quantify how factors like hydration status, temperature, and motion artifacts affect agreement between CGM and non-invasive biomarkers using multivariate regression models.
Implementation Considerations for Large-Scale Studies
Computational Infrastructure and Parallel Processing
For studies involving large participant cohorts or high-frequency sensor data, implement computational efficiency strategies:
Parallelization: Leverage multi-processing capabilities of libraries like GlucoStats to distribute feature extraction across multiple processors, significantly reducing computation time for large CGM datasets [83].
Window-Based Analysis: Utilize both overlapping and non-overlapping windowing approaches to capture both short-term glucose dynamics and longer-term trends. Overlapping windows (e.g., 50% overlap) provide higher temporal resolution for detecting rapid changes, while non-overlapping windows reduce computational overhead for longitudinal analysis [83].
Scalable Storage Architectures: Implement efficient data structures for storing and accessing high-frequency multi-modal sensor data, with particular attention to synchronization metadata.
Quality Assurance and Validation Framework
Signal Quality Metrics: Establish minimum data quality thresholds for inclusion in analysis, including:
- CGM data completeness (>80% of expected values)
- PPG signal quality index (>0.8 for Empatica E4) [82]
- Physiological plausibility checks (glucose values within 40-400 mg/dL range)
Cross-Validation Procedures: Implement nested cross-validation when developing predictive models to avoid overfitting and provide realistic performance estimates on unseen data.
Regulatory Considerations: Document all preprocessing, feature extraction, and analysis steps to facilitate regulatory review, particularly for drug development applications where biomarker validation is critical.
This protocol provides a comprehensive framework for benchmarking CGM-derived features against emerging non-invasive biomarkers from wearable devices. The standardized methodologies address key technical challenges including temporal alignment, multi-modal feature extraction, and robust statistical validation. As non-invasive technologies continue to mature, with PPG-based systems already achieving RMSE of 19.7 mg/dL and 100% clinical acceptance in recent studies [77], the importance of rigorous benchmarking against established CGM metrics will only increase.
Future methodological developments will likely focus on real-time benchmarking pipelines, enhanced algorithms for addressing inter-individual variability in non-invasive sensor performance, and standardized protocols for validating multi-analyte biomarker panels that provide complementary information to glucose metrics alone. The integration of these benchmarking approaches into drug development pipelines and clinical research protocols will accelerate the adoption of non-invasive monitoring technologies while maintaining the rigorous validation standards required for both research and clinical applications.
Conclusion
Effective feature engineering is the cornerstone of translating raw CGM time series data into clinically meaningful insights. This synthesis demonstrates that a multi-faceted approach—combining foundational temporal features, context-aware variables, and sophisticated selection and validation techniques—is crucial for developing accurate predictive models for hypoglycemia, hyperglycemia, and metabolic subphenotyping. Future directions point toward greater automation in feature selection using AI, the integration of multimodal data from wearables, and a heightened focus on interpretability to build trust and facilitate the adoption of these models in clinical trials and personalized medicine frameworks, ultimately accelerating drug development and improving patient outcomes.
References
- 1. CGM Data Analysis 2.0: Functional Data Pattern Recognition ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12356821/]
- 2. A deep learning framework for virtual continuous glucose ... [https://www.nature.com/articles/s41598-025-01367-7]
- 3. Chronobiologically-informed features from CGM data provide ... [https://journals.plos.org/digitalhealth/article?id=10.1371/journal.pdig.0000815]
- 4. MON-544 Uncovering Temporal Patterns In Cgm Data For ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12544032/]
- 5. A large sensor foundation model pretrained on continuous ... [https://www.nature.com/articles/s44401-025-00039-y]
- 6. Time in Range from Continuous Glucose Monitoring [https://pmc.ncbi.nlm.nih.gov/articles/PMC7801761/]
- 7. Using continuous glucose monitoring data in daily clinical ... [https://www.ccjm.org/content/91/10/611]
- 8. Bridging glycemic metrics with clinical outcomes [https://pubmed.ncbi.nlm.nih.gov/41208627/]
- 9. Continuous glucose monitoring‑derived time in range and ... [https://www.sciencedirect.com/science/article/abs/pii/S1262363625000126]
- 10. Using GRI to Deepen CGM Glycemic Data [https://www.adces.org/education/danatech/glucose-monitoring/continuous-glucose-monitors-(cgm)/glycemic-metrics--an-overview/using-gri-to-deepen-glycemic-data-interpretation]
- 11. Glycemia Risk Index: A New Metric to Rule Them All? [https://www.mdpi.com/2673-4540/6/6/49]
- 12. Glucostats: an efficient Python library for glucose time series ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-025-06250-w]
- 13. Feature-Based Machine Learning Model for Real-Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8258517/]
- 14. IJCMCR-RA-ID-01382 [https://ijclinmedcasereports.com/ijcmcr-ra-id-01382/]
- 15. Generalization of a Deep Learning Model for Continuous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11148841/]
- 16. Mitigation of Rebound Hyperglycemia With Real-Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9294577/]
- 17. Glycemic Event Prediction from CGM Data Using Time ... [https://www.linkedin.com/pulse/glycemic-event-prediction-from-cgm-data-using-time-series-asad-ullah--en4de?trk=public_post_main-feed-card_feed-article-content]
- 18. 基于偏振的光学无创血糖监测系统 [https://www.eet-china.com/mp/a392750.html]
- 19. Peculiarities of the Continuous Glucose Monitoring Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2705169/]
- 20. Glucostats: an efficient Python library for glucose time ... [https://pubmed.ncbi.nlm.nih.gov/40993509/]
- 21. Software Packages and Tools for the Analysis of ... [https://pubmed.ncbi.nlm.nih.gov/36223198/]
- 22. ai4healthurjc/GlucoStats: Automatic and parallel extraction ... [https://github.com/ai4healthurjc/GlucoStats]
- 23. Hybrid Stochastic–Machine Learning Framework for ... [https://www.mdpi.com/1999-4893/18/10/623]
- 24. ExpandingWindowFeatures — 1.8.3 [https://feature-engine.trainindata.com/en/1.8.x/user_guide/timeseries/forecasting/ExpandingWindowFeatures.html]
- 25. Feature Engineering Techniques For Time Series Data [https://www.analyticsvidhya.com/blog/2019/12/6-powerful-feature-engineering-techniques-time-series/]
- 26. Multi-family wavelet-based feature engineering method for ... [https://www.nature.com/articles/s41598-025-26685-8]
- 27. Data-driven blood glucose level prediction in type 1 diabetes [https://www.nature.com/articles/s41598-024-70277-x]
- 28. Continuous glucose monitoring combined with artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12146165/]
- 29. Multimodal Fusion of Glucose Monitoring and Food ... [https://arxiv.org/html/2505.09018v1]
- 30. Machine learning-based glucose prediction with use of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8224858/]
- 31. Prediction of metabolic subphenotypes of type 2 diabetes ... [https://www.nature.com/articles/s41551-024-01311-6]
- 32. Prediction of metabolic subphenotypes of type 2 diabetes via ... [https://pubmed.ncbi.nlm.nih.gov/39715896/]
- 33. Use of Continuous Glucose Monitoring with Machine ... [https://arxiv.org/html/2511.03986v1]
- 34. Forecasting glucose values for patients with type 1 ... [https://www.sciencedirect.com/science/article/pii/S0169260724004310]
- 35. Generalized multi task learning framework for glucose ... [https://www.nature.com/articles/s41746-025-01994-4]
- 36. “Glucose-at-a-Glance”: New Method to Visualize the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4455408/]
- 37. Machine Learning Models for Nocturnal Hypoglycemia ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9409948/]
- 38. Machine Learning Models for Nocturnal Hypoglycemia ... [https://www.mdpi.com/2075-4426/12/8/1262]
- 39. and Low-Glucose Prediction in Adults with Type 1 Diabetes [https://www.mdpi.com/2075-4418/14/7/740]
- 40. Data pre-processing and feature extraction [https://bio-protocol.org/exchange/minidetail?id=4347717&type=30]
- 41. Explainable hypoglycemia prediction models through ... [https://www.nature.com/articles/s41598-024-63187-5]
- 42. Machine Learning Algorithms Based on Time Series Pre ... [https://www.mdpi.com/2075-4418/14/21/2427]
- 43. Development and Validation of a Nocturnal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11449968/]
- 44. A Comparison of Feature Selection and Forecasting ... [https://www.mdpi.com/2076-3417/11/4/1742]
- 45. Practical Guide for Feature Engineering of Time Series Data [https://dotdata.com/blog/practical-guide-for-feature-engineering-of-time-series-data/]
- 46. Advanced Feature Engineering for Time Series Data [https://medium.com/@rahulholla1/advanced-feature-engineering-for-time-series-data-5f00e3a8ad29]
- 47. More Green, Less Red: How Color Standardization May ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8875060/]
- 48. An adaptive ensemble feature selection technique for ... [https://www.nature.com/articles/s41598-025-91282-8]
- 49. Research on Ensemble Learning-Based Feature Selection ... [https://www.mdpi.com/2076-3417/14/1/40]
- 50. Impartial feature selection using multi-agent reinforcement ... [https://www.sciencedirect.com/science/article/abs/pii/S001048252400341X]
- 51. Diabetes Prediction Using Feature Selection Algorithms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563305/]
- 52. A Multitask VAE for Time Series Preprocessing and ... [https://arxiv.org/html/2410.00015v1]
- 53. Impartial feature selection using multi-agent reinforcement ... [https://pubmed.ncbi.nlm.nih.gov/38520922/]
- 54. Machine Learning Algorithms Based on Time Series Pre ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11544917/]
- 55. Enhancing severe hypoglycemia prediction in type 2 ... [https://www.nature.com/articles/s41598-024-69844-z]
- 56. Machine learning-based prediction of hypoglycemia severity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483848/]
- 57. Deep learning based data anomaly detection considering ... [https://www.sciencedirect.com/science/article/abs/pii/S2352710225018698]
- 58. Explainable cluster-based learning for prediction of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12440209/]
- 59. Stratification of Patients with Diabetes Using Continuous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10880155/]
- 60. An unsupervised cluster-based feature grouping model for ... [https://www.sciencedirect.com/science/article/pii/S2772442522000521]
- 61. Clinical trial protocol for continuous glucose monitoring in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12096265/]
- 62. From data to insights: a tool for comprehensive Quantification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12161138/]
- 63. Methods for the Clinical Validation of Digital Endpoints [https://pmc.ncbi.nlm.nih.gov/articles/PMC10636620/]
- 64. Differences in technical and clinical perspectives on AI ... [https://eurradiolexp.springeropen.com/articles/10.1186/s41747-024-00543-0]
- 65. Canonical Correlation Patterns for Validating Clustering of ... [https://arxiv.org/abs/2507.16497]
- 66. Simulating Realistic Continuous Glucose Monitor Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11688677/]
- 67. The Application of Continuous Glucose Monitoring Endpoints ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11603422/]
- 68. Glucose Prediction Algorithms from Continuous Monitoring Data: Assessment of Accuracy via Continuous Glucose Error-Grid Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2734107/]
- 69. Glucodensity functional profiles outperform traditional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12480968/]
- 70. Machine Learning–Based Time in Patterns for Blood Glucose ... [https://ai.jmir.org/2023/1/e45450/]
- 71. Impact of transitioning from conventional blood glucose ... [https://www.sciencedirect.com/science/article/abs/pii/S0168822725004723]
- 72. Evolution in blood glucose monitoring: a comprehensive ... [https://link.springer.com/article/10.1007/s44337-025-00273-1]
- 73. A case study on using a large language model to analyze ... [https://www.nature.com/articles/s41598-024-84003-0]
- 74. Predicting Type 2 Diabetes Metabolic Phenotypes Using ... [https://pubmed.ncbi.nlm.nih.gov/39108516/]
- 75. Insulin resistance prediction from wearables and routine ... [https://research.google/blog/insulin-resistance-prediction-from-wearables-and-routine-blood-biomarkers/]
- 76. Non-invasive blood glucose monitoring technology ... - mHealth [https://mhealth.amegroups.org/article/view/120037/html]
- 77. Non-invasive blood glucose monitoring using PPG signals ... [https://www.nature.com/articles/s41598-024-84265-8]
- 78. Mid-infrared Wearable for Non-invasive biomarker monitoring [https://cordis.europa.eu/project/id/101115476/reporting]
- 79. Sweat-based wearable biosensors: a new era of ... [https://www.sciencedirect.com/science/article/pii/S2950235725000253]
- 80. Continuous Glucose Monitoring, Mobile Technology ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK279046/]
- 81. AI-Enabled Non-Invasive Biomarker Sensors Market Size, ... [https://www.precedenceresearch.com/ai-enabled-non-invasive-biomarker-sensors-market]
- 82. Wearables and the Quantified Self [https://www.mdpi.com/1424-8220/19/20/4448]
- 83. Glucostats: an efficient Python library for glucose time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462135/]